#bipap indications
Text
Understanding BiPAP Therapy: A Comprehensive Guide to Bilevel Positive Airway Pressure Machines

Bilevel Positive Airway Pressure (BiPAP) machines are essential devices used in the management of various respiratory conditions. Unlike Continuous Positive Airway Pressure (CPAP) machines, which deliver a constant level of air pressure, BiPAP machines provide two distinct levels of pressure: one for inhalation (Inspiratory Positive Airway Pressure, or IPAP) and one for exhalation (Expiratory Positive Airway Pressure, or EPAP). This unique feature makes BiPAP machines particularly beneficial for patients with conditions that cause breathing difficulties, such as chronic obstructive pulmonary disease (COPD), sleep Apnea, and certain neuromuscular disorders.
How BiPAP Machines Work
BiPAP machines function by delivering pressurized air through a mask that covers the nose and/or mouth. The device is equipped with a motor that generates airflow, which is then channelled through a hose connected to the mask. The dual pressure settings allow for a higher pressure when the patient inhales, making it easier to draw air into the lungs, and a lower pressure during exhalation, which reduces the effort needed to breathe out. This mechanism not only aids in maintaining open airways but also improves oxygenation and reduces carbon dioxide levels in the blood.
The configuration of a BiPAP machine typically includes several components:
- Machine: The main unit that generates pressurized air.
- Hose: A flexible tube that connects the machine to the mask.
- Mask: A device that fits over the nose, mouth, or both, ensuring a tight seal to prevent air leaks.
- Filter: Helps to purify the air before it enters the lungs.
- Humidifier: Often included to add moisture to the air, which can alleviate dryness in the airways.
Indications for Use
BiPAP machines are often recommended for patients suffering from:
- Obstructive Sleep Apnea: A condition characterized by repeated interruptions in breathing during sleep.
- Chronic Obstructive Pulmonary Disease (COPD): A progressive lung disease that makes it difficult to breathe.
- Obesity Hypoventilation Syndrome: A condition where obesity leads to inadequate breathing.
- Neuromuscular Disorders: Such as amyotrophic lateral sclerosis (ALS), which can impair the muscles involved in breathing.
- Acute Respiratory Failure: Where immediate intervention is needed to support breathing.
Benefits of BiPAP Therapy
The primary advantage of BiPAP therapy is its ability to improve ventilation and oxygenation in patients with compromised respiratory function. By providing two levels of pressure, it allows for a more natural breathing pattern, which can enhance patient comfort and compliance. Studies have shown that early application of BiPAP in emergency settings can significantly reduce the need for invasive intubation and improve patient outcomes, particularly in cases of pulmonary edema and respiratory failure.
Additionally, BiPAP machines are generally well-tolerated, though patients may experience some initial discomfort. Common side effects include nasal dryness, mouth dryness, and skin irritation from the mask. Adjustments to the mask fit or the use of humidifiers can often mitigate these issues. It is crucial for patients to communicate any discomfort to their healthcare providers, as modifications can often enhance the overall experience.
Considerations and Challenges
While BiPAP machines are effective, they are not suitable for everyone. Patients with severe respiratory distress who cannot tolerate a mask or those with certain swallowing difficulties may require alternative forms of ventilation. Additionally, the cost of BiPAP machines can be higher than that of CPAP machines, and insurance coverage varies, which may pose a financial challenge for some patients.
Proper maintenance of the BiPAP machine is essential to prevent infections. Regular cleaning of the mask, tubing, and humidifier is recommended to ensure hygiene and optimal performance. Patients should also be educated about the signs of potential complications, such as increased shortness of breath or persistent discomfort, which may require re-evaluation of their therapy.
Conclusion
BiPAP machines play a vital role in managing various respiratory conditions by facilitating easier and more effective breathing. Their unique design allows for tailored pressure delivery, making them suitable for a wide range of patients. As with any medical device, ongoing communication with healthcare providers is essential to ensure the best possible outcomes and to address any challenges that may arise during therapy. With proper use and care, BiPAP machines can significantly enhance the quality of life for individuals with breathing difficulties.
0 notes
Text
Understanding Chronic Obstructive Pulmonary Disease (COPD)

Introduction:
Chronic Obstructive Pulmonary Disease (COPD) is a progressive respiratory condition that significantly impacts the quality of life for millions of people worldwide. This article aims to provide an overview of COPD, including its causes, symptoms, diagnosis, and management.
Definition and Causes:
COPD is a collective term for a group of chronic lung diseases that obstruct airflow, making it difficult to breathe. The primary causes of COPD are long-term exposure to irritating gases or particulate matter, most commonly from cigarette smoke. Other risk factors include exposure to indoor air pollutants, occupational dust and chemicals, and a history of respiratory infections.
Symptoms:
The symptoms of COPD often develop slowly and worsen over time. Common signs include shortness of breath, chronic cough, wheezing, and excessive production of mucus. Individuals with COPD may also experience fatigue, frequent respiratory infections, and a bluish tint to the lips or fingernails, indicating a lack of oxygen.
Diagnosis:
COPD is diagnosed through a combination of medical history, physical examination, and pulmonary function tests. These tests measure the amount of air a person can exhale and how quickly they can do it, providing crucial information about lung function. Imaging studies such as chest X-rays and CT scans may also be used to assess the extent of lung damage.
Stages of COPD:
COPD is categorized into four stages (mild, moderate, severe, and very severe) based on the severity of symptoms and lung function. Early detection and intervention are crucial for slowing the progression of the disease and improving the patient's quality of life.
Treatment Options and the Role of Non-Invasive Ventilation (NIV):
Effective management of COPD involves a combination of pharmacological and non-pharmacological interventions. Medications such as bronchodilators, which help widen the airways, and anti-inflammatory drugs, such as corticosteroids, are commonly prescribed to alleviate symptoms and reduce exacerbations.
In addition to medications, pulmonary rehabilitation programs play a crucial role in the comprehensive treatment of COPD. These programs typically include exercise training, education, and emotional support, aiming to improve physical endurance, enhance breathing techniques, and provide essential information about the disease.
For individuals with severe COPD, especially during acute exacerbations, non-invasive ventilation (NIV) can be a valuable therapeutic option. NIV involves the delivery of ventilatory support through a mask, without the need for invasive procedures like intubation. This approach can help relieve respiratory distress, improve oxygenation, and decrease the work of breathing. Common forms of NIV include continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP).
NIV is particularly useful in managing acute respiratory failure in COPD patients, reducing the likelihood of invasive mechanical ventilation and its associated complications. It is often employed in hospital settings but can also be utilized in home care for selected individuals with chronic respiratory failure. NIV not only improves symptoms but can also contribute to a better quality of life for COPD patients by enhancing their ability to perform daily activities and reducing hospital readmissions.
However, it's important to note that NIV is not suitable for all COPD patients, and its use requires careful assessment by healthcare professionals. Patient selection, appropriate mask fitting, and ongoing monitoring are crucial aspects of successful NIV therapy. The decision to use NIV is typically based on factors such as the severity of respiratory failure, the patient's overall health status, and their ability to tolerate the treatment.
In conclusion, the treatment landscape for COPD is diverse, encompassing medications, pulmonary rehabilitation, and in selected cases, non-invasive ventilation. The individualized approach to care, including the consideration of NIV when appropriate, reflects the evolving nature of COPD management and the ongoing commitment to improving the lives of those affected by this chronic respiratory condition.
Prevention:
Preventing COPD involves avoiding exposure to lung irritants, especially cigarette smoke. This includes quitting smoking and taking precautions in occupational settings with potential respiratory hazards. Regular exercise and a healthy lifestyle can also contribute to lung health and reduce the risk of developing COPD.
Conclusion:
COPD is a serious respiratory condition that requires a comprehensive approach to diagnosis, management, and prevention. Early detection, lifestyle changes, and adherence to prescribed treatments can significantly improve the prognosis and enhance the quality of life for individuals living with COPD. Increased awareness, education, and support for those affected by this condition are essential in the global effort to reduce the burden of COPD on individuals and healthcare systems alike.
0 notes
Text
What are the key differences between CPAP and BiPAP therapy?
As per CPAP or BIPAP machine for rent in Delhi NCR, CPAP (Continuous Positive Airway Pressure) and BiPAP (Bilevel Positive Airway Pressure) therapy are both employed for the management of sleep apnea and respiratory ailments, but they possess distinct characteristics:
Pressure Levels:
CPAP: CPAP administers a continuous and unchanging airflow at a predetermined pressure level, as determined by a sleep specialist. This pressure remains steady throughout the entire night.
BiPAP: BiPAP, on the other hand, dispenses two varying pressure levels. It applies higher pressure during inhalation (known as IPAP) and lower pressure during exhalation (EPAP). This dual-pressure mechanism enhances comfort for some users.
Treatment Versatility:
CPAP: As per CPAP or BIPAP machine for rent in Delhi NCR, CPAP is primarily utilized for managing obstructive sleep apnea (OSA), where airway obstruction is the issue. It is less adaptable when it comes to accommodating fluctuations in a user's breathing pattern.
BiPAP: BiPAP boasts greater versatility and can be employed to address an array of respiratory conditions, including complex sleep apnea, central sleep apnea (CSA), and neuromuscular disorders. It is especially valuable for individuals who encounter difficulties exhaling against continuous high-pressure airflow.

Breathing Patterns:
CPAP: As per CPAP or BIPAP machine for rent in Delhi NCR, CPAP is engineered to uphold a constant airway pressure, which can feel less comfortable for some users during exhalation, particularly if they struggle with expelling air against the prevailing pressure.
BiPAP: BiPAP adjusts pressure levels during both inhalation and exhalation, mirroring a more natural breathing pattern. This feature enhances tolerability for individuals who require pressure relief during exhalation.
Prescription and Indications:
CPAP: As per CPAP or BIPAP machine for rent in Delhi NCR, CPAP serves as the initial treatment choice for moderate to severe obstructive sleep apnea (OSA) and is typically prescribed for this condition.
BiPAP: As per CPAP or BIPAP machine for rent in Delhi NCR, While BiPAP might be prescribed for OSA if CPAP is intolerable, it is also commonly recommended for conditions like CSA, mixed sleep apnea, or other respiratory disorders.
Comfort and Adherence:
CPAP: Some individuals encounter difficulties adapting to the sustained pressure provided by CPAP, especially during exhalation.
BiPAP: The capacity of BiPAP to modulate pressure levels throughout the breathing cycle can heighten comfort and adherence for specific users, rendering it a preferred choice for them.
Cost and Complexity:
CPAP: As per CPAP or BIPAP machine for rent in Delhi NCR, Generally, CPAP machines are more budget-friendly and exhibit simpler designs in comparison to BiPAP machines, making them more accessible and easier to maintain.
BiPAP: As per CPAP or BIPAP machine for rent in Delhi NCR, BiPAP machines tend to be more intricate and may carry a higher price tag than CPAP machines. Nonetheless, insurance coverage and specific medical requirements may factor into the decision between the two.
In summary, the distinguishing features between CPAP and BiPAP therapy revolve around pressure delivery, adaptability, and their applicability to a range of respiratory conditions. The selection between the two hinges on an individual's diagnosis, comfort level, and capacity to tolerate the prescribed treatment. Healthcare professionals collaborate closely with patients to determine the most suitable treatment option, considering their unique needs and medical circumstances.
Visit: https://wellsleepsolution.com/
Instagram: https://www.instagram.com/well_sleep_solution/
Twitter: https://twitter.com/WellSleep_Delhi
Medium: https://medium.com/@polysomnography.test
Tumbler: https://www.tumblr.com/blog/sleep-study-test-delhiYouTube:https://www.youtube.com/channel/UC1deNLTKSMWTS_UKT6nZrpw
#sleepdisorders#sleepdisorder#sleepapnea#sleepproblems#sleep#apnea#sleepstudy#sleepmedicine#sleeping#sleephealth#sleepdeprived#sleeps#healthcare#respiratoryhealth#sleepsupport#sleepisimportant#sleepexpert#sleeptherapy#instadive#physicalhealth
0 notes
Text
2/8
Now transferred to the step down unit, my job is now to monitor my father and try to keep him on the bipap machine he is hooked up to. He hates it, complains that it makes him cold and nauseous, but everyone-doctor, nurse, respiratory therapist, mother- has communicated to him the necessity of the treatment, and so begrudgingly he keeps it on. When someone else rotates in from our family to watch him, a triangle of mother, sister, and myself, he tries to convince said new person to let him take it off, and each of us must put on a steely resolve to say no.
When my father has the bipap machine, sometimes it's easy to understand him and other times it is difficult. Sometimes he mumbles. We have devised a system, one finger for yes, two fingers for no, to see if it's absolutely necessary for me to take off the mask, in order to better understand the thing he is asking me. Today he mumbled, I asked him if I need to take off the mask, and in response he put up his middle finger. I was silent for a couple seconds. He then switched to the index finger to indicate yes.
For those scant seconds, I felt my anger boiling. Something broke, something began to press against my temple. How dare you, I thought to myself. When I was ten years old, i pleaded for him to quit smoking and then he bellowed at me, shouting that whatever happens happens and he'll deal with it on his own, and now twenty something years later I am attending to him for the entirety of the night and yet you had insisted that living irresponsibly was fine and when you were my age, when I was a baby, did you sacrifice anything? or did you continue to live however you wanted, leaving our mother alone saddled with three too young children saddled with all of that responsibility how dare you, how DARE you. In those scant seconds I wanted to beat my fists against everything in this hospital room. I wanted to beat the shit out of the monitors, the breathing machine, him.
I had to calm myself. He's probably not lucid. He probably didn't mean it. Or he realized the rudeness of the finger meant as a joke meant to lighten the tension meant to make light of so heavy a situation meant to make me laugh how come I don't laugh around him anymore? God, goddammit I wish I were a kinder son. A less frustrated one, less quick to turn to anger, more forgiving of the past, more easy going, more understanding. At least I have my health. I scroll on Instagram and see a friend memorialize their deceased mother's birthday on Instagram and knowing that I wouldn't do the same, so private of my love that is lacking, and I feel a deep, pernicious shame.
0 notes
Text
Why use ICU Service at Home.
In certain really serious circumstances, a patient must be admitted to an intensive care unit for an extended period of time. This can be intellectually, emotionally, and financially stressful for both the sufferer and his or her family. In such circumstances, an ICU setup at home can be constructed so that the patient is among loved ones and in a familiar environment, all of which can help with therapy. Long - lasting hospital stays can drain one's funds, and patients may develop intolerance to the hospital atmosphere. In such instances, a home ICU Setup can be useful.

What Include in ICU setup at Home.
Medical Equipment on Rent: - Critical medical equipment is required for a home ICU setup. Trilogy 100 Ventilator , Phillips A 40 Bipap , Phillips Bipap , Hospital bed , Phillips Oxygen Concentrator 5 litres, DVT pump with Cuffs, Portable Oxygen concentrator, Cardiac Monitor. It is critical to have a constant power source at home or a powerful generator backup for these gadgets to function properly.
Critical Care Nurses: - Nursing is the most critical part of a home ICU setting. ICU patients often do not cooperate and are helpless in many ways, thus highly skilled, kind, and disciplined nursing staff is required for ICU setup at home. Depending on the patient's health, nursing personnel may be assigned a range of tasks. They are typically in charge of the patient's daily medical requirements, such as dispensing medications, conferring with doctors, delivering injections, keeping track of daily progress, and managing any medical equipment with care. A caring nursing team may actually help the patient recover quickly.
Physiotherapy: - This feature is based on the patient's condition and mobility. Even in the case of severely inactive patients, physiotherapy is essential so that they can practice whatever minimum movement they are capable of. Physiotherapy aids in the improvement of bodily mobility.
Why Choose Paeonia Healthcare.
We provide complete solutions for ICU setup at home. We provide critical medical equipment such as Trilogy 100 Ventilator , Phillips A 40 Bipap , Phillips Bipap , Hospital bed , Phillips Oxygen Concentrator 5 litres, DVT pump with Cuffs, Portable Oxygen concentrator, Cardiac Monitor on a simple and Easy rental basis so that the patient and his/her family receive maximum cooperation and a trouble-free transfer from the hospital to an Home ICU setup.
Thing to keep in mind in case of use ICU setup at Home.
Ensure that the critical equipment has constant power supply. There should also be a backup power supply.
• Stay alert at all times and look for indications that you should visit a doctor.
• The patient's and ICU setup's room must be cleaned at least twice a day, and proper hygiene must be maintained at all times by family and friends visiting.
For more informaton & enquiry.
Website:- www.paeoniahealthcare.com
Email Id:- [email protected]
Phone No:- 7290060030.
0 notes
Text
How to Purchase Durable Medical Equipment from Medical Supply Stores
In the field of clinical inventories, innumerous individualities have been helped as the times progressed. The clinical tackle field is snappily propelling step by step. This suggests a huge extent of growing better and further developed machines for the enhancement of medical care and drug as a wisdom.
constantly it's unconceivable under financial contemplations to do the drawn- out remedy of a case in an authority clinical office like an exigency clinic. The case is dealt with by a relative or some other individual not a pukka clinical expert in that frame of mind of nursing. It's likewise indicated to as Solid Clinical Gear or DME in clinical speech as it's fabricated to effectively endure normal and rehashed use. Looking for the stylish sanitarium bed price?Primehealers.com is then to help you offer a wide selection of sanitarium beds at the stylish prices. We give satisfaction service to our guests.
Individualities these days could in fact pick clinical inventories at online clinical cache stores. There's multitudinous clinical force store that has their own spots and they offer clinical types of gear to poor individualities at a reasonable cost without settling for lower with the quality. Notwithstanding, there are chances related to it. You can take counsel and tips from your PCP for that specific gear or device. Without going by the traditional way, one might in fact take different helpers like specialists or a neighbor or relation who has the experience of getting clinical inventories for treatment. Try not to go by argumentative advertisements of these clinical providers. Browsing for a sanitarium bed reimbursement?Primehealers.com is the right place for you. We offer a variety of medical beds for rent, perfect for any medical or healthcare installation.
Be conservative previous to opting to buy strong clinical tackle on the web. probe assembling and expiry date on the off chance that any are added with the clinical pack. You ought to constantly ask your clinical provider online for applicable plutocrat bills; keep the damage with yourself on the off chance that you want a negotiation of your bought item. You can likewise challenge providers with similar bills assuming they supply you with date particulars to you. Be careful with dupe particulars or alternate- hand( old) particulars as these can be parlous too for your body and life.
individualities with hindered portability can now carry on with a further ordinary life through strong clinical gear. This is uniquely intended to give help to individualities who are passing injuries and infections that strain their development and give them trouble completing their ordinary exercises. Looking for an oxygen cylinder for home use?Primehealers.com has a wide selection of oxygen cylinders and accessories to choose from.
For more info:-
bipap machine price
Healthy lifestyle tips
CPAP for rent
CPAP Machine Price
Blog:-https://www.primehealers.com/post/guide-to-buy-medical-equipment-online
Source url:-https://sites.google.com/view/primehealersasdda/home
0 notes
Link
#cpap vs bipap#bipap settings#bipap ventillations#bipap medical equipments#bipap uses#bipap indications#bipap medical supplies#bipap avaps
0 notes
Link
The Philips Respironics Remstar Auto A-Flex CPAP enhanced System One sleep therapy system is designed to deliver exceptional therapy, enhance patient comfort, and provide essential compliance tools.
0 notes
Note
✿: feeling so out of it, they need constant attention
You’ve got it! 💕 Thanks for the ask!
Someone asked me to write asthmatic Matthew in the ER a while ago, and I didn’t do it, but here it is now. 😂 I hope it's not total trash.
Sweet Normalcy
Word Count: 1555
Chest pain, the dull aching kind that flares up every time he inhales, that’s all he feels. Keeping his eyes open takes a great deal of effort, but the constant hissing flow of nebulized albuterol being delivered through the mask on his face makes it hard to get any sleep. Maintaining a train of thought for longer than fifteen seconds is also a sudden challenge. When he rolls his head to the right and looks up at the monitor behind him, he sees his heart rate is in the 140s and his oxygen saturation is at ninety-five percent on albuterol and oxygen. That’s not normal for him. None of this is normal. He can’t remember the last time things got this out of control.
“Matthew? Any better, love?” Dad asks him from the chair to his left. He’s been sitting there for hours now, continuously keeping vigilant watch.
It’s a busy night in the emergency department, and it feels a bit like he’s in a bad fever dream. The doctor checking in on him introduced herself earlier, but he can’t recall her name. An alarm goes off every few minutes from someone’s monitor, and it takes him longer than it should to recognize that it’s his monitor making that noise and alerting his nurse to keep coming over to assess him due to his seesawing oxygen saturation and heart rate.
Matthew’s not even sure what time it is anymore. He barely remembers anything. Every hour or so, he will doze off into a fitful half-sleep for twenty minutes or so before waking again and feeling disoriented. A nurse could tell him he’s been here for a week, and he’d believe them.
“Matthew? I asked if you’re feeling any better?” Dad asks again, leaning forward in his seat to grab his clammy left hand and squeeze it gently.
“A little,” Matthew lies, for his father’s sake. He wonders where Alfred and Papa are. They were here earlier, he’s pretty sure.
“I can tell when you’re not being truthful,” Dad sighs, squeezing his hand harder. “You’re not improving. You need to be admitted. This is ridiculous. You should have been admitted hours ago.”
Matthew hates seeing him stressed like this, but he also knows there’s nothing he can do about it at the moment. He feels himself slipping into momentary sleep again, and his eyes flutter shut. He wants to go home. Wants to be in his bed…Is it morning yet?
“Sixteen-year-old with a history of asthma…Patient accompanied by his father. Patient began oral corticosteroid treatment two days ago at home after experiencing wheezing, chest tightness, and coughing that was not fully improving with usual rescue medications…”
They’re talking about him—Matthew realizes that much, at least. He opens his glazed eyes and sees a new doctor approaching him. His ID badge says he’s a critical care doctor. Matthew’s not sure what the difference is between him and the other doctor he saw earlier, but he honestly can’t be bothered to care. He wants to sleep. Desperately. And he wants the chest pain to stop.
“Matthew, buddy?” the doctor says, putting a hand on his shoulder.
He doesn’t want to breathe anymore. His chest hurts too much, and speaking would require taking another agonizing breath.
"Mmmrgh" is all he can manage.
“He’s been less and less responsive,” Dad supplies from the other side of the room, and Matthew can hear the nervousness in his voice, which is unsettling. Dad rarely ever shows how anxious he is when someone’s sick. “I can’t get him to talk to me in full sentences anymore—just phrases.”
The doctor carefully sits him up, and Matthew feels his whole body shake. He rests his elbows against the stretcher to brace himself. A cold stethoscope touches his back, and he shivers.
“He’s still not moving air. He needs to be brought upstairs to intensive care to be monitored. We’ll continue IV steroid treatment and continuous albuterol. If he’s still like this, we can consider non-invasive ventilation and take it from there. Our main priority is to protect his airway.”
Dad says something, but Matthew doesn’t hear it over the noise of the nebulizer. He just knows he’s going to be moved soon and the treatment is going to become more serious now. If he weren’t so tired, he might be scared.
The doctor leaves, and Dad goes back to holding Matthew’s hand. “It’s going to be all right, love. You’ll receive better care soon and hopefully, you’ll start to feel better,” Dad tells him before using his other hand to pet his head. “Try to rest. I’ll be right here, and I won’t let anything happen to you, understand?”
Matthew nods. His eyes do close again, and he does get some brief rest. The next time he’s aware of his surroundings and wakes up, he’s already in the ICU, which means he slept through his transport. The respiratory therapist is setting him up on a BiPAP machine, and once it’s on, it makes his chest hurt even more, which he didn’t think was possible. He grits his teeth against the pain and tries not to make a fuss about it—it would just make Dad worry even more. The air being forced into his lungs is welcome yet excruciating at the same time.
But he doesn’t have to say anything for Dad to know he’s suffering. It’s written all over his face. “I know, poppet. It’s just temporary. It should help.”
It’s so exhausting that he falls asleep again without even needing to think about it. Again, he has no idea how much time passes until he sees the sun shining through the windows of the hospital, indicating that it’s finally morning. The BiPAP mask squeezing his face gets replaced with a regular oxygen mask again, and it occurs to him that his chest feels much lighter and his head is clearer. The worst is over. The air in his lungs feels crisp and refreshing...Almost sweet, even.
“How are you feeling?” Dad asks for the millionth time, still perched next to him.
“Better…For real this time.”
Dad hasn’t slept, of course. He never sleeps in such situations. He was likely watching him all night and conversing with his care team. “Good. You gave us all quite a scare.”
“Sorry.”
“Oh, no, it’s not your fault, love. Not at all…Do you think you’re feeling well enough to have some breakfast?”
“Yeah.”
Dad gives him a relieved smile and then goes off to request a breakfast tray for him. It gets brought up within half an hour, and even though Matthew feels a bit nauseous from the steroids in his system, he knows he needs to eat to gain some energy back.
He’s given some pancakes, a fruit cup, and orange juice. He decides to make a move for the orange juice first because his mouth feels incredibly dry and gross. He picks up the carton and that’s when he notices just how shaky he still is. His hands are trembling violently from all of the bronchodilators in his system.
Dad quickly takes the carton from him, sticks a straw into it, and then brings it back up to Matthew’s lips. “Here, poppet, I’ll hold it for you.”
“…I can do it.”
“You’ll spill it. Don’t be stubborn.”
It doesn’t feel great to have poorer motor skills than a toddler, but Matthew sips some juice through the straw anyway, allowing himself to be fed because he doesn’t have a choice. He finishes the entire carton, one pancake, and half of the fruit cup before his stomach protests. Dad doesn’t seem too happy about him not finishing the meal, but he doesn’t push it either.
And just as he’s finishing up, he finds out Alfred and Papa are outside of the unit, waiting to be allowed in. He’s only permitted to have two visitors at a time, so Dad leaves to take a quick trip home to eat and shower while Alfred and Papa take watch next.
“Dude, you’re alive! Thank God, man. No offense, but you were looking really rough and out-of-it yesterday,” Alfred exclaims upon arrival, bright-eyed and full of pep as always. “It’s good to see you’re looking more like yourself now.”
“We’re so relieved, mon chou. Your father said you may be able to come home as soon as the day after tomorrow.”
“I hope so…Sorry for making everyone worry.”
Alfred throws his hands up in the air and shakes his head dramatically. “I have to teach you everything, don’t I, Mattie? You’re not supposed to apologize for being sick. You’re supposed to milk it for all its worth and make everyone feel bad for you and buy you get well soon gifts. Tell Dad when he comes back that you wanna play the new Pokemon Snap on the Switch.”
“That’s what you want to play, Alfred.”
“Yeah, but we can share it, right?”
“Alfred, your brother is seriously ill, and all you’re thinking about are video games again! Where did your father and I go wrong? You could show some sympathy!” Papa scolds, pinching the bridge of his nose in aggravation.
“It was a joke! Kinda…Obviously, I love ya, Matt! I was really worried, too!”
And he has never craved normalcy as much as he does now.
Yup. Things are already going back to normal.
#hetalia#aph canada#hws canada#aph england#hws england#aph france#hws france#aph america#hws america#aph face family#hws face family#drabbles#hurt comfort#asthmatic matthew
43 notes
·
View notes
Note
Can you give some examples of a clinically indicated need for BiPAP/CPAP?
Thanks!
Good question-
Let’s start with CPAP:
CPAP (Continuous Positive Airway Pressure) is a therapy in which a machine delivers a continuous stream of pressurized air through a mask strapped tightly over the mouth and nose. This pressurized air holds the airway (particularly the throat and tiny air sacs in the lungs called alveoli) open in situations where the patient may not be able to maintain their airway on their own, allowing them to breathe uninterrupted.

1. Obstructive Sleep Apnea: CPAP's most well known use is for obstructive sleep apnea, a condition in which the upper airway (throat) collapses when a person sleeps, causing the patient to briefly (10-30 seconds at a time) but frequently (up to 400 times per night) stop breathing. While not immediately life threatening, sleep apnea causes extremely poor quality sleep, extreme fatigue during the day, and contributes to other health problems like high blood pressure, diabetes, and stroke. The CPAP machine, worn while sleeping, holds these patients’ airways open and allows them to breathe normally through the night.
2. Pulmonary Edema: Pulmonary edema is a fancy word for swelling in the lungs. This can be caused by many problems, including heart failure, infections (pneumonia), poisons (irritants), high altitude (HAPE, a medical emergency where ascending to a high altitude without proper adjustment periods causes a fast-onset pulmonary edema), allergic reactions (causing inflammation in the lung passages), and injuries to the lung tissue.
You can think of the lungs as made of sponge-like tissue, filled with passages that split many times into smaller and smaller tubes that ultimately end in tiny air sacs called alveoli. It is in the alveoli that tiny blood vessels pick up oxygen from the air we breathe and release carbon dioxide to be breathed out (a process called gas exchange). In pulmonary edema, swelling in the lung passages and alveoli make it incredibly difficult to get air all the way to the blood vessels. The hardest part of this is re-opening the alveoli with each breath. The pressurized air pushed in by a CPAP machine can help keep these passages and alveoli open and decrease the work of breathing.
3. Chest Trauma: We breathe in when our diaphragm (a muscle that covers the bottom part of our ribcage) pulls downward, creating extra space within the ribcage that is filled by air entering the lungs. This process requires a mostly-intact ribcage. If the ribcage is significantly damaged (say, flail chest or badly broken ribs), the lungs may not inflate completely, or may not inflate in certain areas. If the lung passages do not inflate fully, not only is the patient not getting all the oxygen/carbon dioxide exchange they might need, but those areas are at risk for developing pneumonia. A CPAP can again keep these passages open and decrease the need for an intact chest while the chest ribcage heals.
Now let’s talk about NIV:
NIV (Non-Invasive Ventilation, sometimes known by the trade name BiPAP) is a therapy that is similar to a CPAP, but instead of a constant flow of pressurized air into the person’s airway, it alternates between two different pressures over the course of a breath- The pressure is higher when the person breathes in and lower when the person breathes out.
Like CPAP, this pressure (both high and low), can “splint” the airway open, decreasing the work of breathing. Unlike CPAP, however, NIV can also monitor a person’s breathing and force them to take a breath if they go too long without taking one themselves. In this way, it is similar to a ventilator (in fact, most ventilators have an NIV setting)- the breaths are just delivered through a mask worn on the face or a full-head “helmet” instead of a tube that goes down the person’s throat.


NIV is used for:
1. Prior to/weaning from an endotracheal (ET) tube: The least amount of time a patient has an ET tube in their throat, the better off they will be. Tubes are extremely uncomfortable, require a lot of medication to make them tolerable for patients, require the patient to be immobilized which leads to increasing muscle weakness the longer the patient goes without moving, and they can cause sores and other injuries to the airway.
NIV can be used to support breathing until a patient absolutely needs an ET tube, and it can be used when the patient no longer needs the tube but still needs support breathing. Both of these decrease the total amount of time the person needs a tube down their throat, which hopefully makes their outcome better. NIV can also be used (to a limited degree) as an alternative for people who refuse an ET tube but still need breathing support.
2. CO2 buildup/respiratory failure not responding to CPAP: If a person can’t get rid of enough CO2 (for example, in a COPD exacerbation or acute respiratory failure) a CPAP and medication alone might not be enough to correct this problem. In this case, CO2 builds up in the blood, causing it to become acidic, which can quickly become dangerous. Since NIV has a lower pressure when breathing out, it can help encourage the patient to “blow off” some of the excess CO2 when they exhale and return their CO2 levels to normal.
3. Neuromuscular diseases: Some people have diseases that cause their breathing muscles to be too weak to breathe adequately, or have had an accident that left them paralyzed and unable to breathe enough to support themselves. In this case, they may wear an NIV mask constantly or while sleeping to support or take over the work of breathing.
4. Central sleep apnea: Unlike obstructive sleep apnea (OSA), which is a problem with the airway, central sleep apnea is a problem where the brain doesn’t always correctly send signals to the breathing muscles during sleep. It manifests similarly to OSA (excessive daytime fatigue, increased risk for various chronic illnesses) but instead of a device that just keeps the airway open, central sleep apnea also requires a device that can initiate breaths if the patient doesn’t take them on their own.
57 notes
·
View notes
Photo




Philips Dreamstation Auto CPAP Respironics
#CPAP Equipment CPAP Machine CPAP Machine For Sleep Apnea CPAP for Sleep Apnea#bipap ventilation bipap settings cpap vs bipap bipap indications bipap avaps bipap uses cpap and bipap bipap for copd cpap vs bipap for copd#cpaproblems#cpap equipment#bipap for copd cpap vs bipap for copd bipap medical equipment nasal bipap bipap machine copd bipap machine supplies bipap for copd bipap sup#cpap#bipap#CPAP Equipment CPAP Machine CPAP Machine For Sleep Apnea CPAP for Sleep Apnea cpap machine side effects where can i buy a cpap machine buy a#cpap machine#sleep apenea
0 notes
Text
Pleural effusions:
Fluid should be sent for cell count and differential, chemistries (protein and lactate dehydrogenase [LDH]), Gram stain and culture with additional inoculation of fluid into blood culture bottles (aerobic and anaerobic), pH (drawn directly into an arterial blood gas syringe and analyzed within one hour), and cytology.
So for the elderly pt who had a pleural effusion, we did a thoracentesis yesterday. The fluid that came out looked yellow. His serum LDH is 208 and his serum protein is 5.2.
The pt's pleural fluid:
LDH = 135
Protein = 2.7
pH = 7.579
Glucose = 215
Neutrophils = 64%
Lymphocytes = 30%
Monocytes = 3%
Fluid mesothelial cells = 2 per 100 WBCs
Macrophages = 3%
So, LDH fluid/LDH serum = 135/208 = 0.64; protein of the fluid/protein of the serum = 2.7/5.2 = 0.51. [Normal serum LDH is 140 to 280 U/L.] So based on Light's criteria, this is an exudative pleural effusion because LDH fluid/LDH serum is greater than 0.6 and protein fluid/protein serum is greater than 0.5. You only need one of Light's criteria in order for it to be an exudative pleural effusion. Light's criteria misidentifies transudative pleural effusions as exudative pleural effusions 25% of the time. One of the reasons can be that the pt was given furosemide, which gets rid of the fluid and thus the protein will be apparently elevated. The fellow told me that these are called discordant pleural effusions.
Light’s criteria is widely utilised to differentiate pleural effusions as exudative or transudative. In a subsect of pleural effusions, there is discordance between protein and lactate dehydrogenase (protein high, LDH low or vice versa).
A significant proportion of pleural effusions that are initially classified as exudative display discordance between LDH and protein. Discordance occurs in older patients, possibly due to increased capillary permeability with age. Within discordant groups, more effusions occurred secondary to global fluid overloaded states (11% of discordant versus less than 2% concordant). Further analysis beyond Light’s criteria is warranted, particularly with increasing age. In patients with discordant pleural fluid, attention should be paid to cardiac and renal investigations to ensure the correct aetiology is determined.
This pt is 97 years old, so maybe he has a discordant pleural effusion.
The pleural fluid neutrophil count of 64% could indicate that it's a parapneumonic pleural effusion; less than 5 mesothelial cells can indicate TB or malignancy. We need the cytology.
Another obese pt has Obesity Hypoventilation Syndrome (OHS), which eventually causes pulmonary hypertension and right heart failure (cor pulmonale). Not breathing enough leads to hypoxic vasoconstriction in the lungs-> increased resistance in the pulmonary vasculature-> right heart has to pump against increased resistance-> cor pulmonale. There are WHO classifications for pulmonary HTN.
Not all pulmonary hypertension (PH) is the same. PH is a general term used to describe high blood pressure in the lungs from any cause. There are five different groups of PH based on different causes. These groups are defined by the World Health Organization (WHO) and are referred to as PH WHO Groups.
WHO Group 1: Pulmonary Arterial Hypertension (PAH)
WHO Group 2: Pulmonary Hypertension Due to Left Heart Disease
WHO Group 3: Pulmonary Hypertension Due to Lung Disease
WHO Group 4: Pulmonary Hypertension Due to Chronic Blood Clots in the Lungs
WHO Group 5: Pulmonary Hypertension Due to Unknown Causes
If you hypoventilate all the time, you can end up with pulmonary HTN and eventually die from the cardiovascular complications!
This obese pt with OHS has a high bicarbonate (30) because the body compensates for respiratory acidosis by maintaining bicarbonate. His creatinine was also elevated, which could be due to dehydration. After giving furosemide, his heart was able to pump better and his creatinine improved, which means the elevated creatinine was due to poor perfusion of the kidneys. He has an ejection fraction of 50% (in school, In learned that a normal EF is 55%, but the fellow told me that often, cardiologists won't necessarily say the pt has HFrEF unless the EF is 45% or less); but this pt was diagnosed as having HFpEF. Anyway, his heart isn't pumping well, so not enough blood is getting to the kidneys, ergo creatinine was elevated. After diuresing, the heart could pump better and perfuse the kidneys better so creatinine improved.
The pt with OHS needs BiPAP, which will help by increasing oxygenation of the alveoli, ergo the hypoxic vasoconstriction in the lungs will decrease, decreasing pulmonary HTN. He also qualifies for gastric bypass surgery. The fellow was telling me that anyone with BMI greater than 35 and any comorbidities qualifies for gastric bypass surgery. Anyone with BMI greater than 40, regardless of comorbidities, qualifies for gastric bypass surgery.
Ground Glass Opacity (GGO) can be due to atypical pneumonia, interstitial lung disease, pulmonary edema. From Radiopaedia:
Ground-glass opacities have a broad etiology: Normal expiration
-on expiratory acquisitions, which can be detected if the posterior membranous wall of the trachea is flattened or bowed inwards partial filling of air spaces
partial collapse of alveoli
interstitial thickening
inflammation
edema
fibrosis
lepidic proliferation of neoplasm
On the OHS pt's CT, they read it as pericardial effusion, but it's actually a fat pad. He has fat around his heart.
Pleural effusions push to the opposite side whereas atelectasis pulls to the ipsilateral side.
#pleural effusion#pulmonary hypertension#pulmonary HTN#cor pulmonale#pulmonary#pulmonology#OHS#obesity#GGO#ground glass opacity
1 note
·
View note
Text
5 Signs You Might Have Sleep Apnea

Introduction: Sleep apnea is a prevalent sleep disorder that often goes undiagnosed, impacting the overall health and well-being of individuals. Being aware of the signs associated with sleep apnea is crucial for early detection and effective management. In this article, we will explore five common indicators that might suggest you are experiencing sleep apnea.
Loud and Persistent Snoring: One of the primary signs of sleep apnea is loud and persistent snoring. While occasional snoring is normal, intense and disruptive snoring can be a cause for concern. If your snoring is accompanied by pauses, gasps, or irregular breathing patterns, it could be indicative of sleep apnea. Partners or family members who observe these patterns should encourage seeking professional advice.
Excessive Daytime Fatigue: Feeling excessively tired and drowsy during the day, despite spending what seems like a sufficient amount of time in bed, may be a red flag for sleep apnea. The interruptions in breathing throughout the night can lead to fragmented sleep, preventing the individual from reaching the deeper, more restorative stages of the sleep cycle. Persistent daytime fatigue should not be ignored and warrants further investigation.
Episodes of Choking or Gasping: Individuals with sleep apnea often experience episodes of choking or gasping for breath during the night. These instances occur when normal breathing resumes after a temporary pause. If you wake up abruptly with a sensation of breathlessness or choking, it is essential to consult with a healthcare professional to assess the likelihood of sleep apnea.
Difficulty Concentrating and Memory Issues: Sleep apnea can impact cognitive function, leading to difficulties in concentration and memory issues. The lack of quality sleep hinders the brain's ability to consolidate memories and perform cognitive tasks effectively. If you find yourself struggling with focus or experiencing memory lapses, it may be linked to sleep apnea, and seeking medical advice is recommended.
Morning Headaches: Frequent morning headaches can be another potential sign of sleep apnea. The intermittent pauses in breathing during the night can result in reduced oxygen levels, triggering headaches upon waking. If morning headaches persist and are accompanied by other signs such as snoring and daytime sleepiness, it is crucial to consult a healthcare professional for a comprehensive evaluation.
Treatment Options for Sleep Apnea:
Once sleep apnea is identified, various treatment options are available to help manage and alleviate its symptoms. The choice of treatment depends on the severity of the condition and its underlying causes. Here are some common approaches:
Lifestyle Changes: Making certain lifestyle modifications can significantly improve sleep apnea symptoms. These may include losing weight, avoiding alcohol and sedatives, changing sleep position, and establishing a regular sleep schedule. Lifestyle changes can be particularly effective for individuals with mild to moderate sleep apnea.
Continuous Positive Airway Pressure (CPAP): CPAP therapy is a widely used and effective treatment for sleep apnea. It involves wearing a mask over the nose or mouth during sleep, which delivers a continuous stream of air to keep the airways open. CPAP is highly successful in preventing the interruptions in breathing that characterize sleep apnea.
Bi-level Positive Airway Pressure (BiPAP): BiPAP machines, similar to CPAP, deliver pressurized air but allow for different pressures during inhalation and exhalation. This can be beneficial for individuals who find it challenging to exhale against the constant pressure of a CPAP machine.
youtube
Adaptive Servo-Ventilation (ASV): ASV devices are designed to monitor breathing patterns and adjust air pressure accordingly. This type of therapy is often prescribed for individuals with complex or central sleep apnea.
Oral Appliances: Dental devices, such as mandibular advancement devices, can be used to reposition the lower jaw and tongue to keep the airway open. These are especially recommended for those with mild to moderate sleep apnea who cannot tolerate CPAP therapy.
Surgery: In severe cases or when other treatments are ineffective, surgery may be considered. Surgical options may include uvulopalatopharyngoplasty (UPPP), genioglossus advancement (GA), or maxillomandibular advancement (MMA). However, surgery is typically reserved for cases where other interventions have proven unsuccessful.
Positional Therapy: Some individuals experience sleep apnea primarily when sleeping in certain positions. Positional therapy involves techniques or devices to encourage sleeping in positions that minimize airway obstruction.
It's important to note that the most suitable treatment will be determined through consultation with healthcare professionals who specialize in sleep medicine. Regular follow-ups and adjustments to treatment plans may be necessary to ensure optimal effectiveness. Seeking timely and appropriate treatment not only improves the quality of sleep but also contributes to overall health and well-being.
1 note
·
View note
Text
The Essential Role of CPAP Therapy in Overcoming Obstructive Sleep Apnea
As per CPAP or BIPAP machine on sale(in ghaziabad), sleep holds the key to a refreshed body and mind. However, for individuals grappling with Obstructive Sleep Apnea (OSA), sleep becomes a battlefield. The erratic breathing, nighttime noises, and perpetual fatigue transform sleep into a challenge. Fortunately, scientific breakthroughs have introduced Continuous Positive Airway Pressure (CPAP) therapy, a game-changer in managing Obstructive Sleep Apnea. This article unveils the crucial part CPAP therapy plays in reshaping the landscape of sleep health.
The Mechanics of CPAP Therapy
As per CPAP or BIPAP machine on sale(in ghaziabad), Enter CPAP therapy, a groundbreaking approach to managing OSA. This therapy introduces a CPAP machine that administers a continuous flow of pressurized air to the individual through a mask. The precision-engineered air pressure acts as a pneumatic brace, thwarting the airway's collapse and guaranteeing a consistent flow of oxygen.
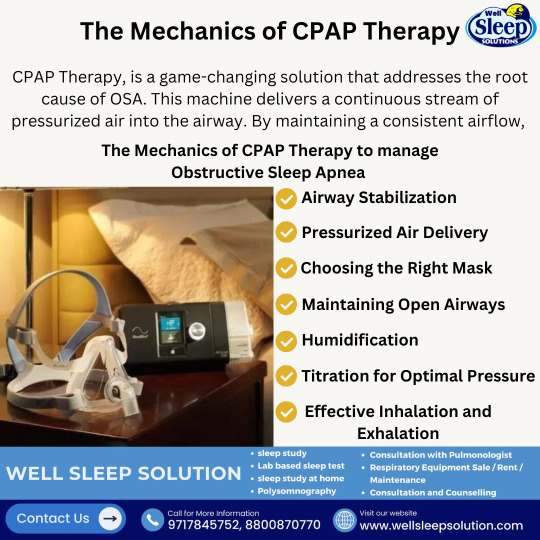
CPAP therapy's role in tackling OSA is multi-faceted and invaluable:
Airway Fortification: The primary objective of CPAP therapy is to fortify the upper airway. By maintaining steady positive pressure, the therapy fends off the collapse of soft tissues that triggers breathing disruptions.
Seamless Breathing: As per CPAP or BIPAP machine for rent in Delhi NCR, With CPAP therapy at the helm, breathing becomes a seamless rhythm. The unceasing stream of air guarantees an unobstructed airway throughout inhalation and exhalation, eradicating the breathing gaps that typify OSA.
Reinstated Sleep Structure: OSA frequently upends the conventional patterns of sleep, leading to fragmented rest. CPAP therapy reinstates the natural sleep structure, enabling individuals to immerse in profound, restorative sleep.
Daytime Alertness: Enhanced sleep quality translates into heightened daytime vigilance. CPAP therapy empowers individuals to stay vigilant and focused during their waking hours, significantly curtailing daytime fatigue.
Cardiovascular Wellness: As per CPAP or BIPAP machine for rent in Delhi NCR, Untreated OSA escalates the risk of heart disease, hypertension, and stroke. CPAP therapy alleviates these perils by assuring a steady supply of oxygen, mitigating the strain on the cardiovascular system.
Elevated Mood: Sleep and mood share a profound connection. CPAP therapy's influence on sleep quality often leads to mood elevation and a reduction in indicators of depression and anxiety.
Enhanced Quality of Life: As per CPAP or BIPAP machine on sale(in ghaziabad), Beyond the physical benefits, CPAP therapy possesses the potential to elevate overall quality of life. Better sleep, amplified energy levels, and enhanced cognitive function contribute to a more gratifying daily existence.
The Odyssey to Enhanced Sleep
Embarking on CPAP therapy necessitates a collaborative effort with a healthcare professional. As per CPAP or BIPAP machine for rent in Delhi NCR, the success of the therapy hinges on factors like mask suitability, pressure adjustments, and acclimatization to the equipment. It's a partnership that charts the course to a healthier, more serene life.
Visit: https://wellsleepsolution.com/
Instagram: https://www.instagram.com/well_sleep_solution/
Twitter: https://twitter.com/WellSleep_Delhi
Medium: https://medium.com/@polysomnography.test
Tumbler: https://www.tumblr.com/blog/sleep-study-test-delhi
YouTube: https://www.youtube.com/channel/UC1deNLTKSMWTS_UKT6nZrpw
#sleepdisorders#sleepdisorder#sleepapnea#sleepproblems#sleep#apnea#sleepstudy#sleepmedicine#sleeping#sleephealth#sleepdeprived#sleeps#healthcare#respiratoryhealth#sleepsupport#sleepisimportant#sleepexpert#blessthismess#sleeptherapy#instadive#physicalhealth
0 notes
Text
From Majid Tayyarah
"I am an ER MD in New Orleans. Class of 98. Every one of my colleagues have now seen several hundred Covid 19 patients and this is what I think I know.
Clinical course is predictable.
2-11 days after exposure (day 5 on average) flu like symptoms start. Common are fever, headache, dry cough, myalgias(back pain), nausea without vomiting, abdominal discomfort with some diarrhea, loss of smell, anorexia, fatigue.
Day 5 of symptoms- increased SOB, and bilateral viral pneumonia from direct viral damage to lung parenchyma.
Day 10- Cytokine storm leading to acute ARDS and multiorgan failure. You can literally watch it happen in a matter of hours.
81% mild symptoms, 14% severe symptoms requiring hospitalization, 5% critical.
Patient presentation is varied. Patients are coming in hypoxic (even 75%) without dyspnea. I have seen Covid patients present with encephalopathy, renal failure from dehydration, DKA. I have seen the bilateral interstitial pneumonia on the xray of the asymptomatic shoulder dislocation or on the CT's of the (respiratory) asymptomatic polytrauma patient. Essentially if they are in my ER, they have it. Seen three positive flu swabs in 2 weeks and all three had Covid 19 as well. Somehow this ***** has told all other disease processes to get out of town.
China reported 15% cardiac involvement. I have seen covid 19 patients present with myocarditis, pericarditis, new onset CHF and new onset atrial fibrillation. I still order a troponin, but no cardiologist will treat no matter what the number in a suspected Covid 19 patient. Even our non covid 19 STEMIs at all of our facilities are getting TPA in the ED and rescue PCI at 60 minutes only if TPA fails.
Diagnostic
CXR- bilateral interstitial pneumonia (anecdotally starts most often in the RLL so bilateral on CXR is not required). The hypoxia does not correlate with the CXR findings. Their lungs do not sound bad. Keep your stethoscope in your pocket and evaluate with your eyes and pulse ox.
Labs- WBC low, Lymphocytes low, platelets lower then their normal, Procalcitonin normal in 95%
CRP and Ferritin elevated most often. CPK, D-Dimer, LDH, Alk Phos/AST/ALT commonly elevated.
Notice D-Dimer- I would be very careful about CT PE these patients for their hypoxia. The patients receiving IV contrast are going into renal failure and on the vent sooner.
Basically, if you have a bilateral pneumonia with normal to low WBC, lymphopenia, normal procalcitonin, elevated CRP and ferritin- you have covid-19 and do not need a nasal swab to tell you that.
A ratio of absolute neutrophil count to absolute lymphocyte count greater than 3.5 may be the highest predictor of poor outcome. the UK is automatically intubating these patients for expected outcomes regardless of their clinical presentation.
An elevated Interleukin-6 (IL6) is an indicator of their cytokine storm. If this is elevated watch these patients closely with both eyes.
Other factors that appear to be predictive of poor outcomes are thrombocytopenia and LFTs 5x upper limit of normal.
Disposition
I had never discharged multifocal pneumonia before. Now I personally do it 12-15 times a shift. 2 weeks ago we were admitting anyone who needed supplemental oxygen. Now we are discharging with oxygen if the patient is comfortable and oxygenating above 92% on nasal cannula. We have contracted with a company that sends a paramedic to their home twice daily to check on them and record a pulse ox. We know many of these patients will bounce back but if it saves a bed for a day we have accomplished something. Obviously we are fearful some won't make it back.
We are a small community hospital. Our 22 bed ICU and now a 4 bed Endoscopy suite are all Covid 19. All of these patients are intubated except one. 75% of our floor beds have been cohorted into covid 19 wards and are full. We are averaging 4 rescue intubations a day on the floor. We now have 9 vented patients in our ER transferred down from the floor after intubation.
Luckily we are part of a larger hospital group. Our main teaching hospital repurposed space to open 50 new Covid 19 ICU beds this past Sunday so these numbers are with significant decompression. Today those 50 beds are full. They are opening 30 more by Friday. But even with the "lockdown", our AI models are expecting a 200-400% increase in covid 19 patients by 4/4/2020.
Treatment
Supportive
worldwide 86% of covid 19 patients that go on a vent die. Seattle reporting 70%. Our hospital has had 5 deaths and one patient who was extubated. Extubation happens on day 10 per the Chinese and day 11 per Seattle.
Plaquenil which has weak ACE2 blockade doesn't appear to be a savior of any kind in our patient population. Theoretically, it may have some prophylactic properties but so far it is difficult to see the benefit to our hospitalized patients, but we are using it and the studies will tell. With Plaquenil's potential QT prolongation and liver toxic effects (both particularly problematic in covid 19 patients), I am not longer selectively prescribing this medication as I stated on a previous post.
We are also using Azithromycin, but are intermittently running out of IV.
Do not give these patient's standard sepsis fluid resuscitation. Be very judicious with the fluids as it hastens their respiratory decompensation. Outside the DKA and renal failure dehydration, leave them dry.
Proning vented patients significantly helps oxygenation. Even self proning the ones on nasal cannula helps.
Vent settings- Usual ARDS stuff, low volume, permissive hypercapnia, etc. Except for Peep of 5 will not do. Start at 14 and you may go up to 25 if needed.
Do not use Bipap- it does not work well and is a significant exposure risk with high levels of aerosolized virus to you and your staff. Even after a cough or sneeze this virus can aerosolize up to 3 hours.
The same goes for nebulizer treatments. Use MDI. you can give 8-10 puffs at one time of an albuterol MDI. Use only if wheezing which isn't often with covid 19. If you have to give a nebulizer must be in a negative pressure room; and if you can, instruct the patient on how to start it after you leave the room.
Do not use steroids, it makes this worse. Push out to your urgent cares to stop their usual practice of steroid shots for their URI/bronchitis.
We are currently out of Versed, Fentanyl, and intermittently Propofol. Get the dosing of Precedex and Nimbex back in your heads.
One of my colleagues who is a 31 yo old female who graduated residency last may with no health problems and normal BMI is out with the symptoms and an SaO2 of 92%. She will be the first of many.
I PPE best I have. I do wear a MaxAir PAPR the entire shift. I do not take it off to eat or drink during the shift. I undress in the garage and go straight to the shower. My wife and kids fled to her parents outside Hattiesburg. The stress and exposure at work coupled with the isolation at home is trying. But everyone is going through something right now. Everyone is scared; patients and employees. But we are the leaders of that emergency room. Be nice to your nurses and staff. Show by example how to tackle this crisis head on. Good luck to us all."
2 notes
·
View notes
Text
Shared post Covid-19 USA
Copied from another group. I do not know who wrote this but it is worth sharing.
I am an ER MD in New Orleans. Class of 98. Every one of my colleagues has now seen several hundred Covid 19 patients and this is what I think I know.
The clinical course is predictable.
2-11 days after exposure (day 5 on average) flu-like symptoms start. Common are fever, headache, dry cough, myalgias(back pain), nausea without vomiting, abdominal discomfort with some diarrhea, loss of smell, anorexia, fatigue.
Day 5 of symptoms- increased SOB, and bilateral viral pneumonia from direct viral damage to the lung parenchyma.
Day 10- Cytokine storm leading to acute ARDS and multiorgan failure. You can literally watch it happen in a matter of hours.
81% mild symptoms, 14% severe symptoms requiring hospitalization, 5% critical.
Patient presentation is varied. Patients are coming in hypoxic (even 75%) without dyspnea. I have seen Covid patients present with encephalopathy, renal failure from dehydration, DKA. I have seen the bilateral interstitial pneumonia on the Xray of the asymptomatic shoulder dislocation or on the CT’s of the (respiratory) asymptomatic polytrauma patient. Essentially if they are in my ER, they have it. Seen three positive flu swabs in 2 weeks and all three had Covid 19 as well. Somehow this ***** has told all other disease processes to get out of town.
China reported 15% of cardiac involvement. I have seen covid 19 patients present with myocarditis, pericarditis, new-onset CHF and new-onset atrial fibrillation. I still order a troponin, but no cardiologist will treat no matter what the number in a suspected Covid 19 patient. Even our non-covid 19 STEMIs at all of our facilities are getting TPA in the ED and rescue PCI at 60 minutes only if TPA fails.
Diagnostic
CXR- bilateral interstitial pneumonia (anecdotally starts most often in the RLL so bilateral on CXR is not required). The hypoxia does not correlate with the CXR findings. Their lungs do not sound bad. Keep your stethoscope in your pocket and evaluate with your eyes and pulse ox.
Labs- WBC low, Lymphocytes low, platelets lower than their normal, Procalcitonin normal in 95%
CRP and Ferritin elevated most often. CPK, D-Dimer, LDH, Alk Phos/AST/ALT commonly elevated.
Notice D-Dimer- I would be very careful about CT PE these patients for their hypoxia. The patients receiving IV contrast are going into renal failure and on the vent sooner.
Basically, if you have bilateral pneumonia with normal to low WBC, lymphopenia, normal procalcitonin, elevated CRP and ferritin- you have covid-19 and do not need a nasal swab to tell you that.
A ratio of absolute neutrophil count to absolute lymphocyte count greater than 3.5 may be the highest predictor of poor outcome. the UK is automatically intubating these patients for expected outcomes regardless of their clinical presentation.
An elevated Interleukin-6 (IL6) is an indicator of their cytokine storm. If this is elevated watch these patients closely with both eyes.
Other factors that appear to be predictive of poor outcomes are thrombocytopenia and LFTs 5x upper limit of normal.
Disposition
I had never discharged multifocal pneumonia before. Now I personally do it 12-15 times a shift. 2 weeks ago we were admitting anyone who needed supplemental oxygen. Now we are discharging with oxygen if the patient is comfortable and oxygenating above 92% on the nasal cannula. We have contracted with a company that sends a paramedic to their home twice daily to check on them and record a pulse ox. We know many of these patients will bounce back but if it saves a bed for a day we have accomplished something. Obviously we are fearful some won’t make it back.
We are a small community hospital. Our 22 bed ICU and now a 4-bed Endoscopy suite are all Covid 19. All of these patients are intubated except one. 75% of our floor beds have been courted into covid 19 wards and are full. We are averaging 4 rescue intubations a day on the floor. We now have 9 vented patients in our ER transferred down from the floor after intubation.
Luckily we are part of a larger hospital group. Our main teaching hospital repurposed space to open 50 new Covid 19 ICU beds this past Sunday so these numbers are with significant decompression. Today those 50 beds are full. They are opening 30 more by Friday. But even with the “lockdown”, our AI models are expecting a 200-400% increase in covid 19 patients by 4/4/2020.
Treatment
Supportive
worldwide 86% of covid 19 patients that go on a vent die. Seattle reporting 70%. Our hospital has had 5 deaths and one patient who was extubated. Extubation happens on day 10 per the Chinese and day 11 per Seattle.
Plaquenil which has a weak ACE2 blockade doesn’t appear to be a savior of any kind in our patient population. Theoretically, it may have some prophylactic properties but so far it is difficult to see the benefit to our hospitalized patients, but we are using it and the studies will tell. With Plaquenil’s potential QT prolongation and liver-toxic effects (both particularly problematic in covid 19 patients), I am not longer selectively prescribing this medication as I stated in a previous post.
We are also using Azithromycin, but are intermittently running out of IV.
Do not give these patient’s standard sepsis fluid resuscitation. Be very judicious with the fluids as it hastens their respiratory decompensation. Outside the DKA and renal failure dehydration, leave them dry.
Proning vented patients significantly helps oxygenation. Even self proning the ones on nasal cannula helps.
Vent settings- Usual ARDS stuff, low volume, permissive hypercapnia, etc. Except for Peep of 5 will not do. Start at 14 and you may go up to 25 if needed.
Do not use Bipap- it does not work well and is a significant exposure risk with high levels of aerosolized virus to you and your staff. Even after a cough or sneeze this virus can aerosolize up to 3 hours.
The same goes for nebulizer treatments. Use MDI. you can give 8-10 puffs at one time of an albuterol MDI. Use only if wheezing which isn’t often with covid 19. If you have to give a nebulizer must be in a negative pressure room; and if you can, instruct the patient on how to start it after you leave the room.
Do not use steroids, it makes this worse. Push out to your urgent care to stop their usual practice of steroid shots for their URI/bronchitis.
We are currently out of Versed, Fentanyl, and intermittently Propofol. Get the dosing of Precedex and Nimbex back in your heads.
One of my colleagues who is a 31 yo old female who graduated residency last May with no health problems and normal BMI is out with the symptoms and a SaO2 of 92%. She will be the first of many.
I PPE best I have. I do wear a MaxAir PAPR the entire shift. I do not take it off to eat or drink during the shift. I undress in the garage and go straight to the shower. My wife and kids fled to her parents outside Hattiesburg. The stress and exposure at work coupled with the isolation at home is trying. But everyone is going through something right now. Everyone is scared; patients and employees. But we are the leaders of that emergency room. Be nice to your nurses and staff. Show by example how to tackle this crisis head-on. Good luck to us all.”
Unknown Writer Thank You
Everything Nursey
Shared post Covid-19 USA syndicated from https://everythingnursey.com/
Shared post Covid-19 USA syndicated from https://everythingnursey.com/
1 note
·
View note