#also like.. a) i have an autoimmune condition so getting sick is more difficult for me to get over
Explore tagged Tumblr posts
Text
Random update per my fics:
Sorry I haven't updated in the last few days. I usually try to write some every day, but I took a day off to plan Golden Glint and then finished the mini fic (Reckoning of Mike Carrera) I started before it because that's what I wanted to write and I wanted to finish it.
On the topic of all my in-progress fics, my writing just isn't consistent right now. I mentioned a while ago that I'm going through AO3 author's curse and would eventually expand on that, so since I'm extremely frustrated and paralyzed from being productive today I'll do that now.
Starting from winter/late fall of 2022 I got sick and basically never got better. I was having illness after illness that meds weren't solving, and my headaches just got more and more frequent until they were every day for at least three months. By the time I came home from Korea, I was having full-blown debilitating migraines every day and attacks where I would almost pass out and couldn't breathe. It took me a couple months but I got on insurance, started a new job, and managed to convince my parents to let me focus on getting my health together this year.
It's been extremely difficult and frustrating because US healthcare, but I found out I do not in fact have ANY allergies despite doctors telling me I do, literally putting me on allergy shots for a year, and telling me that was the cause of migraines, inability to breathe, and constant illness, none of which were true. I had to prove this to them by fighting to see an actual allergist and getting re-tested which costs me hundreds of dollars out of pocket, but at least the allergist was a good dude who wrote a SCATHING letter to my primary care demanding I be sent to the proper specialists for my symptoms. Several blood tests and medications later, we have whammy number two:
The hypoglycemia I was diagnosed with as a teenager was not in fact random. Instead, I have hyperthyroidism caused by Graves Disease. Except I ALSO have Hashimoto's Disease, because I am just so special like that. Basically, rather than allergies like I was always told, I have been getting every single sickness that rolled by for the past several decades and because I was so used to being sick and so criminally gaslit about it, I didn't even know I was ill and just kept going. Thyroid also has tumors on it. I may also have other autoimmune disorders, or thyroid cancer, but I won't know until I finally see an endocrinologist an hour away later this month.
Though my daily migraines stopped last summer, I still get frequent headaches and now extremely bad ones (or migraines) every time it rains. Generally, there seems to be some kind of inflammation issue where my body over-reacts to literally everything by swelling up and causing more problems.
Possibly tied to that, I was in pain every single day at work. Considering my age, there is no normal reason I should be crippled by joint pain but that is yet to be solved. I now only work two days a week, which has helped significantly, but I am still consistently in a ton of pain two days a week, sometimes three as a rebound.
In January, before I had gotten any diagnoses, my parents gave me an ultimatum that they were kicking me out in May. I had to beg them to go part-time because I simply could not keep up with job applications while I was so constantly tired and pain. After sobbing for two straight days about the inevitability of becoming homeless because I can't afford to or logistically live on my own, my mom convinced my dad to let me go part time on the condition that I continue to pay the same rent Ive been paying to live in one of their empty spare rooms.
In February, I went in for the first appointment toward getting an Autism screening. The therapist suggested I get an ADHD test and recommended me for the official autism screening, saying I have a solid case for suspecting. After a little computer game and another talking appointment, slightly to my own surprise (especially because of how easy it was) I was clinically diagnosed with ADHD. I recently started meds for that and it has made basic tasks and job applications infinitely easier to the extent it's insane, plus my final Autism screening is next week and based on my results every step of the process so far diagnosis seems likely.
All that said, the job search process has been soul-destroyingly frustrating. I have a masters degree in a specialized field, backed up by a Bachelor's in a relevant field, years of study abroad and work abroad (which is relevant to my career path) and a track record of excellent academic achievement. I also speak French and Korean near-fluently and am conversational in Romanian and Russian, as well as knowing a fair few phrases in a number of other languages. Every job I've had has stressed me out to the point of quitting by around a year (hello Autism), but also none were related to what I studied at all, highly customer service oriented, and still every one would tell you I was one of the best employees they ever had and begged me to stay. Even with this track record, after literally HUNDREDS AND HUNDREDS of applications (which in my field almost always require a cover letter, often questionnaires and lengthy short answers, or even writing samples in addition) I have had ONE interview in four years. ONE. And I was so heinously underqualified for that hail-Mary I'm 99% certain they only interviewed me to meet a quota. As you can imagine, for someone with highly probable AuDHD, doing the same thing over and over for 4 years with a 100% failure rate is enough to make me want to dive into a lake with a pile of bricks chained to my back.
I'm still months out from seeing a neurologist about my headaches and general constant pain, I don't have a plan of action for my buck-wild medical anomaly thyroid, and I don't know if my parents are kicking me out next month. They haven't brought it up so maybe with my recent headway on the Peace Corps application (was told I stand a very good chance, but that's another contract job overseas, further pushing back my ability to find a stable, long term career job) and slew of diagnoses and medications, my dad is cooling off a bit. I don't know.
All that to say my body is crumbling out from under me, my job is stressful, and despite being extremely qualified and putting in so much effort, I have zero long-term life prospects. Sometimes, that results in me diving whole-hog into writing for fun and as an outlet, other times I'm too tired or need to bury myself in mindless content consumption or days of spending every spare moment staring at my ceiling in silence until I maybe fall asleep. Did I also mention the crippling lifelong insomnia which my ADHD meds (along with rapid weight loss I'm desperately trying to curb because I'm already borderline underweight due to my thyroid) are exacerbating?
Anywyay. Point is I'm very tired and stressed so my writing is going to be much less consistent than in the past. Hope you understand. Also just an update for my online friends. TMI but I needed to rant and put it out there for those wondering to lower expectations.
6 notes
·
View notes
Text
desperately trying to tell a friend that no, jst because i already caught covid doesn’t mean i’m comfy w being near another confirmed covid case
#memorie.txt#delete later#also PLEASE WEAR A MASK WHEN YOUR FAMILY MEMBER IS SICK…. AT THE VERY FUCKING LEAST.#also like.. a) i have an autoimmune condition so getting sick is more difficult for me to get over#and b) getting reinfected w covid is a THING!!! that HAPPENS!!! and it can get worse!!!!#i feel like i’m the only one concerned abt this in our friend group#i’m rlly uncomfortable w all of this#and everyone’s acting like i’m being overly cautious#hiiiii yes um. multiple ppl in my family have autoimmune conditions and i do too soooo. this is a problem for me <3#im so!!! frustrated!!!
3 notes
·
View notes
Note
r.e. disabled les amis headcanons: omg please add yours
yay someone wants to hear mine! some of this will be projection on my part. i’m disabled myself, i need a cane to walk because of a condition called Amplified Musculoskeletal Pain Syndrome (AMPS) which is very similar to fibromyalgia. i’m also going to include some neurodivergent and mental illness headcanons, but i know some people don’t consider those disabilities, but from my own experience with them, i do, so that’s why i’m adding them!
jean valjean has chronic back pain, specifically a problem with the discs in the upper spine, from his time in prison. gradually gets worse as he gets older because of lack of treatment and him triggering the pain himself by lifting the crashes cart and then marius in the sewers. in my modern aus i like to think he gets an upper back/neck and shoulder brace that he wears, and he’s a bit insecure about it so that’s why he’s always wearing big coats even in aus where he’s not being pursued by javert
javert, marius, and enjolras are autistic. javert has known most of his life but marius wasn’t diagnosed until his late teens due to lack of familial support. enjolras would have been diagnosed as a kid but he’s afab and there’s lack of diagnosis for afab children and he doesn’t get diagnosed until he’s in his 20s after doing his own research.
enjolras, grantaire, courfeyrac, and bossuet have adhd. enjolras and bossuet have more hyperactive traits, enjolras’ manifesting in his need to constantly be doing something and chronic boredom, while bossuet doesn’t display his as physical hyperactivity but more racing thoughts and an inability to slow his mind down. courfeyrac and grantaire have more attention deficit issues. they can’t focus on one topic for a while unless they go into hyperfocus or it’s a hyperfixation. grantaire has a lot of self worth issues because of his adhd because growing up he was seen as a bad student and a bad child because of his attention issues and executive dysfunction. courfeyrac got medicated really early on in childhood. enjolras did too and it becomes a bit of an issue between him and grantaire because grantaire doesn’t start medication until he’s about 24 and enjolras has been on medication for a long time and he’s kinda forgotten about how difficult it can be being unmedicated so he thinks grantaire isn’t trying enough. that changes when the pharmacy won’t refill enjolras’ medicine and he has to go a week without it. it’s a really humbling experience he apologizes to grantaire once he’s back on meds (this is based on personal experience actually… i didn’t start meds until a few months ago and i had a friend who started meds in middle school do what enjolras did and ur sucked)
joly had to get his knee joint replaced through surgery and still can’t walk properly without pain in the area so he walks with a cane. he also has an autoimmune disorder that makes him get sick really easily, as well as chronic fatigue and brain fog that makes it hard to complete daily tasks even when he has a low pain day. he also has very bad anxiety that sometimes manifests in worrying about his health excessively and vigilance about staying healthy because he knows that if he even gets a cold, it will be worse for his body than someone without a chronic illness
cosette and eponine both have c-ptsd from living with the thenardiers, and i have so much to say about this that i’m thinking about making an entirely separate post about it. just know that both of them have trauma responses, with cosette becoming very docile and a chronic people pleaser because she doesn’t want to get in trouble even though she won’t be punished like that anymore, while eponine has become hardened by her trauma and puts up walls so she doesn’t get hurt. she also gets frequent nightmares about her siblings being hurt and wakes up sweaty and almost screaming. gavroche came home late one day and eponine was on the verge of a panic attack even though it had only been half an hour
combeferre is blind in one eye and his other eye is partially damaged so he doesn’t have very good depth perception in what he can see, and he also has very limited color vision
feuilly is deaf and grantaire is HoH. feuilly’s primary form of communication is sign language, though he can lip read but not very well. all the amis know basic signs like how to ask if he wants some water/food, hellos and goodbyes, and how to sign their names. once feuilly becomes close with them, he creates signs specifically for their names, which at least in the american d/Deaf/HoH community is very special. a very close family friend of mine is HoH and he gave me a name sign when i came out as trans (it’s a quick movement of the letters R and Y up in the position where male signs are signed like “father”) grantaire is hard of hearing and has hearing aids. sometimes when he fights with enjolras he just takes out his hearing aids and just lets enjolras keep going until he realizes what’s going on.
this next one is very personal to me and is something i don’t think i’ve ever seen before, but i hc jehan with having schizoaffective disorder (bipolar type). i personally have this disorder and i have found some comfort thinking jehan has it too. they started having mood symptoms first, which started as a depressive episode and then suddenly they felt like they had been shocked into a manic episode. once the mania started they began having delusions of grandeur and the belief that they were a prophet sent to help the world. they began thinking people were after them and they heard voices from “angels” telling them what to do. they started writing poetry as a way to get the voices out of their head and onto paper. it took two years to get a diagnosis and a some very rough nights where they weren’t sleeping and would show up to meetings with delusional ideas, and they were scared. they refused to go to the hospital but needed help, so grantaire took them to the community out reach center that he goes to for alcohol addiction treatment and jehan got a psychiatrist who started them on antipsychotics and a mood stabilizer. i like to think that jehan got better quickly, just because i’ve had this disorder for a very long time and i’ve tried almost every antipsychotic out there and im not really better, so i want them to not have my experience. they were accepting of treatment pretty easily, but they did worry that their poetry wouldn’t be the same afterwards. fortunately, they channeled their frustration into poetry as opposed to writing what they were hearing and even though their poetry changed once they got on medicine, they didn’t lose their ability to write it. they’ve also learned how to have confidence in themself and the revolution without becoming delusional, which did take time because hearing enjolras’ strong ideas, it just felt like too much for a while. but the longer they’ve been stable and connected to reality, the easier it becomes to believe that yes, some things may seem improbable, but they can still happen AND some ideas are delusions and can be differentiated between the improbably ideas
bahorel has hypermobile joints and has to be careful when boxing with grantaire because he has subluxed or even fully dislocated his shoulders, elbows, and finger joints while boxing. jehan bought him some colorful finger braces and has stitched patterns into his knee and elbow braces
that’s enough for now because this is getting really long but yeah. lots of projection on my part (whoops) but what is this blog without me projecting my issues onto les mis characters? is this not what this blog is based on 😂
40 notes
·
View notes
Note
Since ghouls heal so fast, does that mean they’re always healthy? Do they ever get permenant injuries or do they always heal?
I’ve been wanting to talk about this! Even with increased healing ability, it’s possible and not at all uncommon for ghouls to have scars and disabilities
Sometimes even advanced healing isnt enough. Repeated injuries with not enough food or heal time between them can be disabling. It’s uncommon, but missing limbs, lost senses, and chronic pain can be caused later in life
The most common way ghouls get disabilities is just by birth. Sometimes ghoul kids are born blind or deaf or paralyzed or with chronic issues same as humans. In their culture it’s treated very differently than it is with humans though, since they’re quite community oriented and adaptable. It’s understood that they won’t be able to function the way abled ones do, but with the right conditions and supports, they can thrive alone or even outmatch others
Blind or deaf ghouls can often use their kagune to sense vibrations more effectively than abled ghouls, making them terrifyingly effective fighters and hunters in environments with harsh light or sound that would cause others distress, and the CCG is ill equipped to fight them since their tactics rely a lot on the assumption that their enemies are relying on sight and sound to fight. Since feeling and smell is a large part of how they hunt, losing other senses isn’t too much of a blow.
Sign language is a common practice with many ghouls because of how useful it is when hunting in silence, so deaf ghouls or ones with speech issues don’t have as many issues communicating as the average human would
Mobility impaired ghouls will have some difficulty hunting, whether they’re paralyzed or have disorders that make their ability to move unreliable, they will have problems there. That’s why they tend to join up with groups. Since almost every ghoul has had a debilitating injury in the past, they’re better at understanding how loss of physical functions can impair daily life and what they can help with
Scarring happens sometimes when a ghoul is injured while too hungry to heal for a long time, so when they do heal the tissue stands out. It can also happen from being bitten by other ghouls as they have an enzym in their saliva that drastically slows the healing process. It’s a big part of how marriage bites work, but can be annoying for people who got in a fight a month ago and still have teeth marks on them
Sometimes scars or damaged organs that get injured again grow back working better, leading to a gruesome type of healthcare. You can’t hear out of one ear? Just take out the ear bone! Don’t like that scar on your arm? Take the skin off! Paralyzed stomach? Just remove it! If it works it works, if not then damn bro you really did all that for nothing, oof. Try again maybe?
Rc disorders are more common and can be disabling. Some underproduce and can’t maintain a decently sized kagune or any kagune at all, but that’s still less difficult to deal with than overproduction. Those who overproduce may be able to grow larger kagune and heal faster, but it comes at a cost. Extra rc will cause patches of kagune mass to grow around the kakuhou, make containing kagune difficult, and even form claws on the hands and feet since it can escape the body through keratin easier than through skin. It’s a sort of psuedo kakuja, especially when it gets so out of hand that it makes them grow another kakuhou. It’s not very well understood, especially by ghouls who think of it as extra power, but those who have it know that it’s stressful, can cause spikes of pain, and makes hiding one’s ghoul identity next to impossible. It can be managed with rc suppressants, but those are expensive. It’s just something that every individual has to find ways to deal with, and hearing other ghouls go “Oh I wiSh I hAd Rc OvErPrOdUcTiOn I wOuLd Be So StRoNg” isn’t helping them in the Enxhausted Rage department since it gets tiring to explain to every single person that this isn’t a cool superpower, it sucks
Certain autoimmune diseases can effect them. Though they aren’t as deadly to ghouls as they are to humans, but they still leave them more vulnerable to illnesses and infections. They can usually survive these, but it certainly isn’t fun and they need to boil their meat before eating it to prevent catching anything
Ghouls, obviously, have little to no access to healthcare. Anything they do they do themselves, and they’re lucky to find a ghoul who knows a little about how healing works, and a single ghoul doctor within fifty miles is a windfall. The best most of them can do is frontier medicine and a small list of safe over the counter meds. Though when they can find a ghoul doctor, they tend to be very good about prescribing things that can help with chronic issues. Much less of that “are you sure it’s not in your head?” Bullshit since they know better than anyone that if someone is spending the time and money to see a doctor, they obviously know it’s not. Even when ghouls are decriminalized, ones that are chronically ill will be more likely to request a ghoul doctor because they’re sick of dealing with humans who callously second guess everything
30 notes
·
View notes
Photo

A diet composed mostly of plant foods can be considered sacred for weight loss and Healthy Lifestyle. At least according to respected employee George Malcolm and his wife, Landa, they devised a Bible–inspired diet.. Marcos claims to have been saved from a diet of raw fruits, vegetables and carrot juice after being diagnosed with cancer 35 years ago.
A few years ago, Alleluia’s diet consisted of 85% raw plant foods and 15% cooked vegetarian foods. how did you come The authors claim that meat can “clog” our systems, delay clearance, and cause toxicity and disease. At the heart of this program is the belief that eating raw vegetables is the best way to get the nutrients you need, repair damaged cells and stay healthy longer.
Hallelujah Diet basics
The Hallelujah Diet was developed by priest George M. Marcolmos after he was diagnosed with cancer. 29 And he said, “God said, I will give you every vegetable I plant in the ground and every tree that produces fruit, and this is your food.
This section focuses on plants. Food that is not animal feed. The Glory of God system replaces processed and refined animal foods with organic, clean, raw, plant-based foods. Fruits are predominant.
In addition to dietary supplements, the diet includes natural fruit juices, organic plant-based diets, and a variety of health supplements designed to flush out disease-causing toxins. This includes protein bars, exercise programs and webinars.
According to suggestions and recipes. Arthritis, Diabetes, Irritable Bowel Syndrome, Alzheimer’s and Heart Disease and Autoimmunity This program boosts your immune system. Helps keep you healthy – just take 6 supplements of daily lenses.
What You Can and Can’t Eat
The raw part of the diet includes fruits, vegetables, grains, beans, nuts, seeds, fats and oils, herbs, milk substitutes and beverages such as fresh vegetable juices, recycled distilled water, steamed vegetables and baked potatoes. Cereals, whole wheat pasta, squash (cooked or steamed) and beans can be used for cooked meals.
As with other plant-based diets, no meat, dairy or eggs are served. If you‘re used to drinking a glass of wine at night, you need to find a new way to relax. Bringing alcohol is prohibited. Most soy products, processed fruits and vegetables, refined grains and some nuts, seeds, oils, spices, soups and sweets are nowhere to be found.
Level of Effort: High
This diet can potentially change your diet. Dieting begins by choosing one of three “paths of entry”: health promotion, Healthy living, Healthy Lifestyle and recovery. These choices will guide your diet.
Limitations
Switching to a Healthy diet that mostly includes raw vegetables can be difficult. Dieting requires a lot of planning and preparation. It’s also a good idea to take food supplements at certain times of the day.
Cooking and shopping
You have to spend a lot of time loading fresh fruits and vegetables into the grocery store. If your local grocery store doesn’t have a lot of dairy, you may need to buy a specialty store. Water requires a lot of preparation, but this quirky design actually has a minimal boiling point.
Packaged foods or meals
shouldn’t However, Hallelujah Acres Market sells vitamins, supplements, snacks and more online.
In-person meetings
None required, although dieters can attend healthy living workshops and seminars.
Exercise
Expect to exercise every day for at least 30 minutes.
Look Here For More Hallelujah Diet Recipes
Does It Allow for Dietary Restrictions or Preferences?
The diet is suitable for both plant- based and vegetarian diets, so it is suitable for vegetarians, vegans and fat, salt or gluten-free diets.

What Else You Should Know
Cost: Fresh fruits, vegetables and fruit juices can be expensive, but Marx says it can help you lose weight. They say you can save money by eliminating meat, dairy, white flour, sugar, salt and junk food. Taking a recommended supplement can cost you $2,000 per year.
Support: None. However , for more information on the Hallelujah Acres diet and Healthy Lifestyle
Healthy Lifestyle–Does it Work
Eating lots of plant foods like fruits, vegetables and beans can improve health and weight and avoid processed animal foods.
Read More about: Healthy Lifestyle-Hallelujah Diet
How it works
The hallelujiah diet consists of 85% aromatic herbs and 15% cooked herbs. A lot of dietary supplements have been developed to compensate for malnutrition and improve health. The diet can be divided into 4 stages:
Step 1. The first step is to eat raw vegetables, fruits, nuts and seeds.
Step 2. The move is to replace meat, dairy, refined carbohydrates, sugar, and salt (all known as toxic foods) with healthier plant-based alternatives.
Step 3.The third part requires nutritional supplements and supplements from the Barlymax program, which is a non-flammable powder to improve digestion.
Step 4. The final step is to take a dietary supplement to prevent deficiency of vitamin B12, vitamin D3, iodine, selenium and docosahexaenoic acid (DHA).
The diet provides a combination of nutritional supplements depending on your condition. You can start with a kit that includes BarleMax and Fiber Cleanser, choose an immune stimulation or detox kit, or purchase a dietary supplement containing probiotics separately. Protein and Targeted Menopause: The app’s website will do an online test and say the company will assess your health and tell you which dietary supplement is right for you and your Healthy Lifestyle.
>>Visit Healthy Lifestyle-Hallelujah Diet Official Website<<
Is It Good for Certain Conditions?
Health experts recommend eating more plant-based foods to prevent and treat a variety of health problems. This raw vegetarian food is low in saturated fat, added sugar and sodium. It may be helpful for people with high blood pressure, diabetes, heart disease, and high cholesterol.
The Final Word
Positive? This app is full of fruits, vegetables, whole grains and beans that can improve your health and weight. The downside is that raw foods can lower vitamin B12, vitamin D, and calcium levels. You may need to take supplements and fortified foods to make up for lost nutrients.
Vegetarians can find it difficult to follow this program as there is plenty of space for candy and alcohol. The focus is on raw food. Make sure you are getting enough iron, zinc, vitamin D, vitamin B12, omega-3 fatty acids, and calcium. Check your weight regularly to make sure you are not sick.
3 notes
·
View notes
Photo

Sick Beats.
Blade-reboot director Bassam Tariq talks to Alicia Haddick about partnering with Riz Ahmed on Mogul Mowgli, how to open a film, the clash of colonialism and art, and the escapist joys of comic-book movies.
“We’ll make films, we’ll die, who gives a shit? Right? But how we lived and all that stuff, I feel like that matters.” —Bassam Tariq
Standing alone on a dimly lit stage in a New York music venue, Zed appears to have it all. He’s on the brink of a musical breakthrough in his rap career, with a growing legion of fans and fellow artists inspired by his work. Yet at this moment, on this stage, with the audience barely visible in the shadows, there is so much more going on.
Riz Ahmed has had a couple of blistering opening performances in films this past year, but where Sound of Metal’s first moments track his character’s hearing loss, the opening scene of Mogul Mowgli—written by Ahmed and director Bassam Tariq—feels like a physical manifestation of the emotions that come with tackling what it means to be a London-bred, Pakistani-Muslim rapper.
Zed is unsure where he belongs in a complex web of cultural and social ideas defined by a family that raised him, a religion he treats with skepticism, and a country that colonized his parents and their ancestors. Transforming these questions into art won’t make them disappear, but music at least gives Zed a measure of indirect control over his problems. That is, until the diagnosis of a degenerative autoimmune disease puts the brakes on his career.
As Zed’s father struggles to reconcile his own past with caring for his son, Zed’s illness manifests itself in apparitions of a mysterious figure, whose face is veiled by a sehra (the decorative groom’s headdress worn at Pakistani weddings). The man refers to himself as Toba Tek Singh, which is both a reference to a city in Pakistan named after a Sikh religious figure, and the name of a satirical story about Partition.
Mogul Mowgli is Tariq’s debut narrative feature. It had its premiere at Berlin in 2020, winning the FIPRESCI International Critics Prize and gaining notice for its director, who has been confirmed to helm MCU’s Blade reboot, with Mahershala Ali in the leading role. Tariq previously co-directed the highly rated 2013 documentary These Birds Walk, and the 2019 documentary short, Ghosts of Sugar Land, each centered on Muslim life and experiences, one on the streets of Karachi, the other in Texas. Mogul Mowgli is a more introspective—and more surreal—exploration of these ideas, couched in the dingy halls of a UK hospital, and in the lyrics of a rapper searching for himself.
Tariq chatted with us over Zoom about his friendship with Ahmed, the production challenges of keeping a set alive, and his film inspirations, from Abbas Kiarostami to the Marvel Cinematic Universe.

Riz Ahmed and Bassam Tariq on the set of ‘Mogul Mowgli’.
I know that you and Riz worked together on the film for a number of years while you were coming up with the story, and there was also a lot of mutual respect for each other’s work. How did the two of you first meet? Bassam Tariq: We met through my co-director of These Birds Walk, Omar Mullick, who introduced Riz and I to each other. At that time, I was running a butchery in the East Village in Manhattan. That’s where Riz and I met and we just became fast friends. Things kind of took a few years for us to figure out what the project would be that we would do together, it took me about three years, four years. But you know, he was shooting The Night Of, and then slowly his career was skyrocketing and it was like, “oh, great, we’ll probably never see him again”.
Yet he would always stay in touch because I think he had a desire to tell something that was very specific to him. All I knew was how to tell things that are specific to me, I didn’t know anything else. So I think that’s why it kind of worked really well for both of us, because he became quite great at playing other characters, but to do something that was very close to him, I think that was quite new.
And it gave you both the opportunity to tell your own stories through that. That’s the exciting thing. It’s so exciting when you’re able to pull from some unique things that only you can tell, and particularly working with actors that also share that part and then bringing it alive through them. It’s just gold, it’s such a gift. Why would you try to hide that from them or mask that from them?
Speaking of These Birds Walk, I couldn’t help but notice the similarities between how you observed and captured the work going on in Karachi and the intimate filming style used in this movie. What were the challenges in jumping from documentaries to this film, and were there any lessons you learned from that field of work that then factored into the production of Mogul Mowgli? I would say that the big learning curve for me was timing, like, you’re burning money as you have a day of production. Every day that you’re in prep and every day that you’re in production, you’re burning money. So the financing is very different because there are stakeholders involved. We were blessed with amazing partners with BBC and Cinereach that weren’t the crazy ones that you would expect when you think of stakeholders, they were amazing partners. It was more of a family vibe than anything. But you’re still burning someone else’s money, right?
I think that was something that I didn’t take stock of and I wish I was a little bit better with, but I think I finally realized what it means to “make your days”, to “make your minutes”. How do you keep everybody engaged? How do you keep your crew engaged? Is this going to be a long production? How do you do this? How do you keep it all alive? And we’re doing it in the thick of winter in London, you know, we couldn’t afford heaters and stuff.
And we were just blessed with such an amazing crew. I didn’t have a crew with These Birds Walk. It was just me and my co-director, and then I had an editor, Sonejuhi Sinha, who came on board for free. It was just people out of the goodness of their hearts, whereas with Mogul Mowgli, it was both the goodness of their hearts and they were getting paid a little bit. No one was getting paid great money. But it was still this desire to make an excellent film.
I think what I had to learn was to communicate clearly what this film was with everybody involved. That was a really exciting and new thing for me, because it wasn’t just me and a co-director. We have a ship and everyone on the ship needs to know what this film is and how we’re going to make it look, how we’re going to make it feel. These are friends I care about, I care about Riz, he’s a dear friend of mine. And I wanted to make sure that he was being respected, that I was being respected and I was doing right by everybody on my team.
And I think that’s really the most important thing for me, because man, who cares? We’ll make films, we’ll die, who gives a shit? Right? But how we lived and all that stuff, I feel like that matters. You could give somebody a very empowering experience.

Riz Ahmed as Zed in ‘Mogul Mowgli’.
While your own experiences were a major inspiration on a number of areas of the film, what research did you do for the medical aspects of the movie, especially with how crucial it is to telling this story? Oh, it was massive, we did a lot of research. We pulled a lot from our own families’ histories, but we never named the illness. That was quite important to us. It was quite allegorical, but also based in a very real concern, a very real thing.
I think something that I will say that is true is that a lot of first-generation immigrants have autoimmune illnesses, and it’s because of the body coming into a new terrain and new climate. Sometimes there’s trauma in the body from past generations. The Body Keeps the Score is a book that I think everyone’s been reading these days, but it’s about epigenetics and this idea that the psyche doesn’t know time. It doesn’t understand time, so you can’t hide it.
We have this false idea that time will heal wounds, but it’s such bullshit, because if we don’t confront these traumas, we can then pass those traumas onto our family members, which is something that I think is very real.
There are a few moments while Zed’s coming to terms with his condition in which he encounters the image of Toba Tek Singh. What inspired their appearance in the film and their place as a confronting figure for Zed? I think there’s a few things. One is that he’s an allegory, he very much symbolizes the illness, he is the illness. But then there’s another part of it where, like, I feel that I never know how to connect with our culture. I’ve always had a hard time understanding how to connect with it. So that’s the reason why he’s almost veiled from us as well. It’s like I don’t want to be able to see him—I don’t know what he is.
We have this very social-realist film, and we filmed the movie chronologically. So what I remember is that in the prayer scene, the first time he looks over and he looks back and then we have the guy in flowers I was like, “I can’t believe I’m making this movie, am I really doing this?” And you know, good on Riz. This is why having good partners along with you to be like “yeah, this is what we’re doing and we’re committing to this”, because there’s a version where they didn’t exist.
I also have to ask about the opening scene with the concert. I know that you had originally taken footage from one of Riz’s own concerts, but then you re-recorded it. How difficult was that scene to put together? It was scary! It was our first day of shooting, it was the first day of Riz and I working together. I’d filmed him a little bit here and there, like in a hotel or this or that, I filmed him in Pakistan when we were having fun, but it was all fun. Now we’re putting on the concert, people are there to see Riz perform, it’s the first day of filming, you know what I mean? The crew doesn’t have the language yet, we’re still figuring out who we are, how we’re all going to speak to one another, and then we have to do this big concert scene.
I will say that it was so important to make it feel like he is a real performer. I think I wanted to see him unleash a bit, because I wanted that energy from Riz to be real. I want him to unleash in a way that we haven’t seen him perform in concerts before. We did a few takes on it and then it was like, no, we got to go further, now we got to go further. And that was great to see how both of us were egging each other on to go further with it.
It was a really powerful introduction. It’s something that makes you sit up and take notice, if that makes sense. Thank you. I love openings of films. I remember my co-director on These Birds Walk, they taught me that how you open is everything. So I always knew that I wanted to open with a concert and then end with the concert. But I wanted the last concert to be in the bathroom. And I’m happy they were able to bring it to life.

‘Mogul Mowgli’ director Bassam Tariq. / Photo by Ryan Lash
Were there any opening scenes that inspired you when thinking about that scene? One of my favorite movie openings is Under the Skin, because I think it tells you very clearly what the film’s about, it grabs your attention. You’re about to watch a story about humanity and about, you know, what does the construction of a human look like, which is phenomenal, like, what is under the skin? Literally, what is under our skin? There are others. Narc has an incredible opening.
What were the films that most inspired the overall production of Mogul Mowgli? You know, there’s this one film by Alonso Ruizpalacios called Güeros. It’s one of the best debut films I’ve ever seen in my life. It’s so radical. It’s so singular. It’s so special. It’s so specific. And there’s probably a thousand things I don’t understand about it, but I love that about it. I’m walking into a world that I haven’t seen.
I would also say that the TV show Atlanta is a deep inspiration for me. Another film that I’m just so in love with that I watched a few times with Omar Mullick was Ida. Then I would say Son of Saul, and how that dealt with trauma, was really powerful. And all three of these films were also shot in the Academy ratio, which is the 4:3 ratio that I think we unwittingly decided to do.
Were there any particular filmmakers that really inspired you growing up or that made you think “yeah, this is what I want to do”, and pushed you to make the films you are today? No, I don’t think it was in the filmmakers I looked at, but more just the wonder of film that I loved, the escape of film. So my earliest films that I always loved were, like, Back to the Future. I watched a lot of, it’s weird to say, but even the bad Marvel movies I’ve seen, like The Punisher, Captain America, those early ones, I would watch those because I loved the comics. So for me, the comics were an escape, and ’90s X-Men, the ’90s Spider-Man, that was my life. My first introduction to Blade was that bit when Blade [appeared] on Spider-Man in one of those episodes of the animated series. And then, of course, the movie Blade.
I will say that one filmmaker I’ve come to who’s given me permission to make films is Abbas Kiarostami, the Iranian filmmaker who died a few years ago. He’s just a phenomenal voice, a singular voice in Iran. And Mohsen Makhmalbaf and then his daughter Marziyeh Meshkiny, who made the film The Day I Became a Woman. But these are films that are so unapologetically unique and of them. I want to be able to do that as well. They’re not in response to, or reacting as a discriminated member of some community, but instead they’re like, “no, I exist and I am”.
I feel like so much of the content that comes from communities that I’m a part of can sometimes feel like we’re sloganeering to white people or to the heteronormative or whatever. It’s just, like, come on. Andrew Haigh’s Weekend is one of the films that really moved me and made me be like: “Oh, wow, this is uniquely queer, it could only be two queer people having a one-night stand. It couldn’t be anybody else. And it had to be made only by that filmmaker.”
That’s it, that’s filmmaking, that’s cinema to me, that’s exciting. Just like the movie The Fits, where it could have only been written by women, directed by a woman, edited by a woman, it’s so specific. It’s one of the films that I also look to that I’m, like, what she did in that film, I’m still in awe. I can never have that experience, but I can relate. I can connect to something so vulnerable and so true. Because when it’s true, it’s undeniable.
Just one last question, the obvious question: top three films of all time, what would you say they are? I’m going to go with Stalker by Andrei Tarkovsky, and I will say The Matrix because, you know, whatever, I’m lame like that. Then I’ll say another very expected answer, City of God. If I could add two more to the list, though, I would say Güeros and Dog Day Afternoon, for sure.
They’re all very different from one another. Yeah, but that’s what’s so great about cinema. You’re fluid. Genre, it could be anything.
Related content
Citizen Bane’s list of films and shows that pass the Riz Test
Hip Hop Hooray: Darren’s comprehensive list of hip hop and rap films
Best Directorial Debuts of 2020: as voted by Letterboxd members on Twitter
Follow Alicia on Letterboxd
‘Mogul Mowgli’ is currently screening at Film Forum (NY) and Nuart (LA), and coming to more screens soon.
#mogul mowgli#sound of metal#riz ahmed#bassam tariq#blade#marvel cinematic universe#mcu#mcu blade#mahershala ali#pakistan cinema#pakistani cinema#bipoc filmmaker#the riz test#muslim film#south asian film#letterboxd
3 notes
·
View notes
Text
COVID-19 myths to beware:
(last updated April 24, 2020; links to sources)
There is not yet a vaccine or official treatment for COVID-19, though work is in progress around the world.
The FDA briefly approved the drug chloroquine to treat COVID-19, but there is no hard evidence that this drug will actually work for treating this virus. The drug is no longer being studied as a treatment [source 1], as several people taking it daily for COVID-19 experienced heart problems and some died [source 2]. This drug is an anti-malarial that is sometimes used to treat autoimmune conditions such as lupus. There is one study suggesting it could inhibit COVID-19, but this study was small and had serious methodology concerns. ***4/24/2020 update: the study has since been retracted, due to lack of proper vetting and serious methodology issues.*** It’s not a reliable (or even safe) treatment for COVID-19; it might also create a life-threatening shortage for people who need this drug for other conditions. Do not take chloroquine unless it is prescribed to you by a doctor, and definitely do not self-administer this drug.
Injecting disinfectants will not help you, and may cause serious harm. Do not consume or inject disinfectants of any kind.
No, summer weather or living in a warm climate does not mean you’re safe from COVID-19. Likewise, winter weather does not kill COVID-19. In either climate, the virus lives in the human body, which is fairly consistent in temperature -- so, what the weather is like doesn’t affect it much.
On that note, the approach of summer will not inherently kill off the virus. It can live in hot, humid weather. Also, just because it’s no longer cold and flu season in the US doesn’t mean it’s not cold and flu season elsewhere (like in the southern hemisphere).
Also, no, trying to raise your body temperature (by taking a hot bath or by some other means) will not stop you from getting sick. Again, your internal body temperature changes very little, so this won’t help you. But washing your hands or showering after going out can! So do those instead!
No, 5G does not spread COVID-19. Viruses cannot travel on radio waves, and we’ve seen the virus spread in areas without 5G mobile networks. COVID-19 is spread through respiratory droplets (from talking, coughing, sneezing) or touching surfaces that have been exposed to these droplets.
No, you can’t protect yourself with a detox treatment, detox supplement, or detox “tea” of any kind (and shame on the influencers pushing this).
No, you cannot “self-test” for COVID-19 by holding your breath. The claim that you can self-test by attempting to hold your breath for 10 seconds is a social media hoax which gained traction when it was shared by Fox News. It has been completely debunked. Also, plenty of people who have COVID-19 are asymptomatic and can breathe normally.
Be skeptical of home tests. Produced primarily by Everlywell, they are expensive, and the chance for a false negative is very high (they require swabbing VERY far up your own nose, which is difficult to do on yourself if you’re not a medical professional or someone with experience doing this). If you’re worried that you may be sick, call your doctor; there are also lots of drive-in testing locations around the country.
Hand sanitizers made with only essential oils do not work -- essential oils do not disinfect. Beware of DIY hand sanitizer, as it is easy to make an ineffective one. Soap and water are the most effective means of disinfecting your hands. DO NOT consume essential oils unless it is specifically a food-grade product; most are not and are harmful if consumed.
It’s unclear if ibuprofen can worsen cases of COVID-19 -- this information was circulated by the French Health Minister, but there is no scientific data to support their claim. Ibuprofen is probably still safe to take. If you have any doubts, you can take Tylenol instead.
COVID-19 has nothing to do with beer or eating meat.
Beware of conspiracy theories in general.
Beware of phishing scams pretending to be official press releases. Many appear from fake CDC emails.
Facebook, Twitter, and other social media sites are struggling to stop misinformation campaigns. Don’t consider these sites a reliable source of information -- look for the primary source to confirm what you see online, and do what you can to report or remove false information.
Beware articles or sources that use the current situation to excuse discrimination or prejudice. It is wrong to blame Asians and Asian culture for COVID-19 -- that’s just racism. Similarly, stories blaming migrants are just as wrongly biased.
---------------------------
How to determine if something is bullshit (a short guide): ask the following questions:
(1) Are there sources included with the statement? (2) Are the sources credible (namely, are they from a primary source, such as a research group, recognized health agency, or other medical institution)? (3) Can I find more than one account of the information? (4) Is the statement objective (meaning ‘based on fact’, rather than subjective or ‘based on emotion or feeling’, which creates a bias)?
If the answer to any of those 4 questions is “no”, there’s a chance the information could be bullshit, OR, at the very least, it may be incomplete.
In health news, be skeptical of things involving very small test groups (a test on 12 people does not speak for the general public!) or that never went to human testing (things work differently in petri dishes than in our bodies). Also be skeptical of things made by for-profit laboratories. Big pharma can make great things, but it can also be misleading or skewed. Read the literature from sources that are not invested in the product (again -- the CDC, WHO, and FDA are good places to start) to get a better sense of how reliable, safe, or effective a thing is.
---------------------------
Check out the CDC’s list of COVID-19 myths here: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters
*** Note: I’m not a doctor or any other type of medical professional. I am a geologist who knows a lot about source evaluation and is worried about people being misinformed
#covid19#covid-19#coronavirus#public health#i have most of this info in my other covid19 post but i keep seeing misinformation being spread around#so this is me trying to do my part to counter that#updated for more and new links
158 notes
·
View notes
Text
A Guide to Gluten: Does Everybody Need To Go Gluten-Free?
A Guide to Gluten: Does Everybody Need To Go Gluten-Free?
📷
Gluten-free foods have recently become quite popular. Nowadays, you’ll find gluten-free breads, pastries, candies, and more at your local grocery store. Because of this you might be wondering whether gluten is good or bad for you.
There’s no one-size-fits-all answer to this: gluten can harm some people, but it seems to be totally fine for others.
In the health and wellness world, many influencers and companies claim that cutting out gluten will give you more energy, help you lose weight, and lift your mood. But in truth, your ideal diet depends on your body’s unique biology, which means that dietary requirements differ from one person to the next.
Here’s what you need to know about gluten, gluten intolerance, and celiac disease.
What is gluten?
Gluten refers to a group of proteins (prolamins) found in wheat, barley, and rye. These prolamins give these ingredients a glue-like consistency when mixed with water. This is why wheat flour is ideal for baking. It also helps bread rise and increases the shelf-life of baked goods and baking ingredients.
Gluten can be found in breads, pastas, and baked goods, but it can also be found in pre-made foods like soups and stews. Flour is often added to sweet treats and pre-made foods as a thickening agent, and added gluten can be used to improve the shelf-life of certain foods.
Gluten can also found in:
Brewer’s yeast
Malt
Beer
Certain candies
Certain chocolate drink mixes
Certain cereals and granolas
Sauces and dressings
Some meat substitutes
Gluten can also be found in places you wouldn’t expect, like in certain multivitamins and dietary supplements.
How does gluten harm the body?
As mentioned, gluten is an umbrella term that includes a number of different proteins. While some people can digest those proteins adequately, others can’t.
Proteins are typically broken down by the protease enzymes in your digestive tract. However, gluten proteins are resistant to these enzymes. These gluten proteins can cross over through the tissue in your digestive tract and into the rest of your body.
Your body’s immune system might attempt to fight these proteins. For some people, this immune response might make them sick. Those who have celiac disease – an autoimmune disease – could get severely sick if they eat gluten.
What is gluten intolerance?
“Gluten intolerance” is a broad term that refers to three health conditions: celiac disease, non-celiac gluten sensitivity, and wheat allergies.
While the symptoms differ from one condition to the next, they all generally cause you to feel ill after you consume gluten.
What is celiac disease?
Celiac disease is an autoimmune condition that involves the inflammation of your small intestine.
When someone with celiac disease consumes gluten, their small intestine will be damaged. This can make it difficult for their body to absorb nutrients, which can lead to weight loss, diarrhea, and pain. People with celiac disease might also have anemia, osteoporosis, and skin diseases.
About 1 percent of the world’s population has celiac disease, although it’s far more common in certain countries, like Finland, Mexico, and some northern African regions. Research shows that, in these areas, celiac disease can affect about 2 to 5 percent of the population.
Celiac disease is usually diagnosed by intestinal biopsy. It could also be diagnosed by blood testing for antibodies. There is no way to treat celiac disease other than avoiding gluten entirely.
What is non-celiac gluten sensitivity?
Some people who don’t seem to have celiac disease or wheat allergies find that they have a negative reaction to eating gluten. This is called non-celiac gluten sensitivity (NCGS).
If you have NCGS, you might find that gluten causes you to have symptoms like intestinal pain and diarrhea as well as fatigue, joint pain, and headaches.
To be diagnosed with NCGS, your doctor will first rule out a wheat allergy and celiac disease.
What is a wheat allergy?
Wheat allergies and celiac disease are often confused. They are two different conditions, and it’s possible to have both at the same time.
These allergies are particularly common in children, who might outgrow it. However, many adults have wheat allergies too. They might have uncomfortable symptoms when they eat or inhale wheat.
The symptoms of wheat allergies can include:
Nausea and vomiting
Nasal congestion
Hives or rashes on skin
Bloating
Anaphylaxis (a potentially fatal allergic reaction that causes difficulty breathing)
Symptoms vary from person to person. For some, it might look like mild nausea and a stuffy nose. In others, wheat exposure can be fatal.
To diagnose a wheat allergy, an allergist will usually test your blood or do a skin-prick test.
Autoimmune disorders and gluten
Celiac disease is one kind of autoimmune disease. Other common autoimmune diseases include:
Hashimoto’s thyroiditis, which causes hypothyroidism
Psoriasis, a painful skin condition
Rheumatoid arthritis, where your joints become swollen and stiff
Lupus, which can affect the whole body
Inflammatory bowel disease (IBD), not to be confused with IBS
Type 1 diabetes
Multiple sclerosis
If you have an autoimmune disease of any kind, including those not listed here, your doctor might advise you to avoid gluten. Gluten seems to worsen the symptoms of autoimmune diseases, according to research. This might be because people with celiac disease are likely to have other autoimmune disorders. Some studies have found that people with autoimmune diseases benefit from a gluten-free diet.
So, if you have an autoimmune disease, you might want to eliminate gluten from your diet. Monitor your symptoms and see if they improve. As always, it’s wise to seek your doctor’s advice before making a major change in your diet.
Should everybody cut out gluten?
If you don’t have one of the above conditions, should you avoid gluten? That’s not 100% clear. Although some people claim that everybody should cut out gluten, there’s no evidence that shows it will benefit people without those conditions.
However, many people who don’t seem to have gluten intolerance feel better after they start avoiding gluten. This might not be because of gluten itself, but because of other factors. For example, going gluten-free might lead you to cut down on high-carbohydrate foods and processed foods. Eating these foods in excess can make you feel ill.
If you suspect you have gluten intolerance, you might find it helpful to temporarily cut out gluten and monitor how you feel. You can keep a notebook where you write down what you eat and what your symptoms are like.
How do I cut out gluten?
When you think about it, gluten is nearly everywhere. It’s in obvious places, like breads and pastas, but also in sauces, certain chocolate drinks, and candies.
Fortunately, since more people are aware of gluten sensitivities nowadays, it’s now easier to find gluten-free foods than ever. Gluten-free foods are often labeled as such. Remember that wheat-free is not the same as gluten-free – a wheat-free food can still contain gluten.
It’s important to read the labels of everything you eat. Read the ingredients list and avoid foods that contain:
Wheat
Barley
Rye
Malt
Oats (unless gluten-free oats)
Brewer’s yeast
Check the allergens list for gluten and any of the above ingredients.
Although many people confuse gluten with all grains, some grains don’t contain gluten. This includes corn, quinoa, teff, certain rices, sorghum, and millet. Gluten-free grains are often used to make gluten-free versions of bread, crackers, pastas, and more.
Thankfully, it’s now a little easier to find gluten-free alternatives to your favorite foods. Gluten-free oats, breads, and pastas are now far more common. You might even find gluten-free cakes, beers, and cookies that taste just as good as your favorite treats. Some bakeries and cafes are specifically gluten-free.
Eating out?
One of the most difficult aspects of having a gluten-free diet is navigating restaurants and pre-made food. Flour is often used as a thickening agent, for example. Even if a meal doesn’t contain any gluten itself, it might have come into contact with gluten during the preparation process. For some people, this alone can trigger an immune response.
Opt for gluten-free meal services, premade foods, and restaurants. Depending on your sensitivity level, you might get away with choosing a gluten-free option in a restaurant that uses gluten in other meals. Don’t be afraid to enquire with a company or business about whether or not they use gluten.
The Celiac Disease Foundation has helpful resources on eliminating gluten. They have lists of foods to avoid as well as meal plans, recipes, and tip sheets for gluten-free living. Although eliminating gluten can be difficult, it’s possible to still enjoy a variety of tasty, nutritious food.
Getting diagnosed with gluten intolerance
If you suspect that you’re gluten intolerant, you’ll probably want an official diagnosis.
Your first port-of-call is to go to your GP. They might order blood tests, or they will refer you to a dietician and/or allergist. Some people might struggle to get a diagnosis straight away, and they might have to see a few specialists to get to the bottom of their symptoms.
Gluten intolerance is often diagnosed by a blood test, skin-prick test, or biopsy. But as mentioned, your doctor or dietitian might also suggest you simply eliminate gluten from your diet and monitor your symptoms.
How we can help
Food allergy tests are the best way to figure out whether you have a food intolerance of any kind. However, they’re often extremely expensive. In a country where medical expenses are unaffordable for many, a great number of people might be sensitive to gluten without knowing it.
Discounted lab work is one of the many services we offer Knew Health Members. We include food allergy tests as well as fasting insulin tests and hormone checks. These tests help you identify any current or potential health issues. You’ll be equipped to make better decisions about your lifestyle and diet.
Gluten is a controversial topic in health and wellness circles. Some people believe everyone should cut out gluten entirely. But many people seem to be able to tolerate gluten well. If you suspect you have a gluten intolerance, whether it’s a wheat allergy or celiac disease, talk with your doctor about getting a diagnosis.
Visit for more
2 notes
·
View notes
Text
They Had Mild Covid. Then Their Serious Symptoms Kicked In.
Pam Belluck is a health and science writer whose honors include sharing a Pulitzer Prize and winning the Nellie Bly Award for Best Front Page Story. She is the author of Island Practice, a book about an unusual doctor. @PamBelluckMs. Khan said that she experienced “heart palpitations if I just got up to open the curtains.” Her cardiologist said she was the fifth previously healthy young person to walk into his office that week. In the beginning, her fatigue was so severe that walking two or three laps around her 600-square-foot apartment would exhaust her for the rest of the day. In addition, she said that she had “really intense mood fluctuations that don’t feel like they’re mine.”“Waking up every day in this body, sometimes hope feels a little dangerous,” said Ms. Khan, who will soon start the cognitive rehab program. “I have to wonder: Am I going to recover, or am I going to just figure out how to live with my new brain?”In his job, “my clients would tell me things like a passcode or an address and I couldn’t remember it,” he said.At Mr. Palacios’s first appointment with the Northwestern clinic, “I did the cognitive tests, and I failed them all,” he said. On a return visit, he did another battery of tests, he said, “and I didn’t do so hot on that, either.”Mr. Palacios was referred for cognitive rehab at a long-established program in Chicago that helps give patients strategies to manage and improve memory, organizational and cognitive difficulties. But he didn’t go, he said, because “I completely forgot.” He plans to go now.In the Northwestern study, 43 percent of the patients had depression before having Covid-19; 16 percent had previous autoimmune diseases, the same percentage of patients who had previous lung disease or had struggled with insomnia.Experts cautioned that because the study was relatively small, these pre-existing conditions might or might not be representative of all long-term patients. “We are all seeing very small pieces of the elephant in terms of the long Covid group,” Dr. Bell said. “Some of us are seeing tail; some of us are seeing trunk.”Along with neurological symptoms, 85 percent of the patients were experiencing fatigue, and nearly half had shortness of breath. Some also had chest pain, gastrointestinal symptoms, variable heart rate or blood pressure. Nearly half of the participants were experiencing depression or anxiety.“I was cleaning my gutters and I forgot where I was, I forgot what I was doing on the roof,” Mr. Palacios said. When he remembered, he added, the idea of doing “something as simple as climbing on a ladder all of a sudden became a mountain.”Dr. Allison P. Navis, a neuro-infectious disease specialist at Mount Sinai Health System in New York City who was not involved in the study, said that about 75 percent of her 200 post-Covid patients were experiencing issues like “depression, anxiety, irritability or some mood symptoms.”Participants in the study were overwhelmingly white, and 70 percent were women. Dr. Navis and others said that the lack of diversity quite likely reflected the demographics of people able to seek care relatively early in the pandemic rather than the full spectrum of people affected by post-Covid neurological symptoms.“Especially in New York City, the majority of patients who got sick with Covid are people of color and Medicaid patients, and that’s absolutely not the patients one sees at the post-Covid center,” Dr. Navis said. “The majority of patients are white, often they have private insurance, and I think we have to figure out a little bit more what’s going on there with those disparities — if it’s purely just a lack of access or are symptoms being dismissed in people of color or if it’s something else.”In the Northwestern study, Dr. Koralnik said that because coronavirus testing was difficult to obtain early in the pandemic, only half of the participants had tested positive for the coronavirus, but all had the initial physical symptoms of Covid-19. The study found very little difference between those who had tested positive and those who had not. Dr. Koralnik said that those who tested negative tended to contact the clinic about a month later in the course of the disease than those who tested positive, possibly because some had spent weeks being evaluated or trying to have their problems addressed by other doctors.Ms. Khan was among the participants who had a negative test for the virus, but she said she later tested positive for coronavirus antibodies, proof that she had been infected.Another study participant, Eddie Palacios, 50, a commercial real estate broker who lives in Naperville, a Chicago suburb, tested positive for the coronavirus in the fall, experiencing only a headache and loss of taste and smell. But “a month later, things changed,” he said.Across the country, doctors who are treating people with post-Covid neurological symptoms say the study’s findings echo what they have been seeing.“We need to take this seriously,” said Dr. Kathleen Bell, the chairwoman of the physical medicine and rehabilitation department at the University Texas Southwestern Medical Center, who was not involved in the new study. “We can either let people get worse and the situation gets more complicated, or we can really realize that we have a crisis.”Dr. Bell and Dr. Koralnik said many of the symptoms resembled those of people who had concussions or traumatic brain injuries or who had mental fogginess after chemotherapy.In the case of Covid, Dr. Bell said, experts believe that the symptoms are caused by “an inflammatory reaction to the virus” that can affect the brain as well as the rest of the body. And it makes sense that some people experience multiple neurological symptoms simultaneously or in clusters, Dr. Bell said, because “there’s only so much real estate in the brain, and there’s a lot of overlap” in regions responsible for different brain functions.“If you have inflammation disturbances,” she said, “you can very well have cognitive effects and things like emotional effects. It’s really hard to have one neurological problem without having multiple.”In the Northwestern study, many experienced symptoms that fluctuated or persisted for months. Most improved over time, but there was wide variation. “Some people after two months are 95 percent recovered, while some people after nine months are only 10 percent recovered,” said Dr. Koralnik. Five months after contracting the virus, patients estimated, they felt on average only 64 percent recovered.The study of 100 patients from 21 states, published on Tuesday in The Annals of Clinical and Translational Neurology, found that 85 percent of them experienced four or more neurological issues like brain fog, headaches, tingling, muscle pain and dizziness.“We are seeing people who are really highly, highly functional individuals, used to multitasking all the time and being on top of their game, but, all of a sudden, it’s really a struggle for them,” said Dr. Igor J. Koralnik, the chief of neuro-infectious diseases and global neurology at Northwestern Medicine, who oversees the clinic and is the senior author of the study.The report, in which the average patient age was 43, underscores the emerging understanding that for many people, long Covid can be worse than their initial bouts with the infection, with a stubborn and complex array of symptoms.This month, a study that analyzed electronic medical records in California found that nearly a third of the people struggling with long Covid symptoms — like shortness of breath, cough and abdominal pain — did not have any signs of illness in the first 10 days after they tested positive for the coronavirus. Surveys by patient-led groups have also found that many Covid survivors with long-term symptoms were never hospitalized for the disease.A new study illuminates the complex array of neurological issues experienced by people months after their coronavirus infections.
In the fall, after Samar Khan came down with a mild case of Covid-19, she expected to recover and return to her previous energetic life in Chicago. After all, she was just 25, and healthy.
But weeks later, she said, “this weird constellation of symptoms began to set in.”
She had blurred vision encircled with strange halos. She had ringing in her ears, and everything began to smell like cigarettes or Lysol. One leg started to tingle, and her hands would tremble while putting on eyeliner.
She also developed “really intense brain fog,” she said. Trying to concentrate on a call for her job in financial services, she felt as if she had just come out of anesthesia. And during a debate about politics with her husband, Zayd Hayani, “I didn’t remember what I was trying to say or what my stance was,” she said.
By the end of the year, Ms. Khan was referred to a special clinic for Covid-related neurological symptoms at Northwestern Memorial Hospital in Chicago, which has been evaluating and counseling hundreds of people from across the country who are experiencing similar problems.
Now, the clinic, which sees about 60 new patients a month, in-person and via telemedicine, has published the first study focused on long-term neurological symptoms in people who were never physically sick enough from Covid-19 to need hospitalization, including Ms. Khan.
2 notes
·
View notes
Text
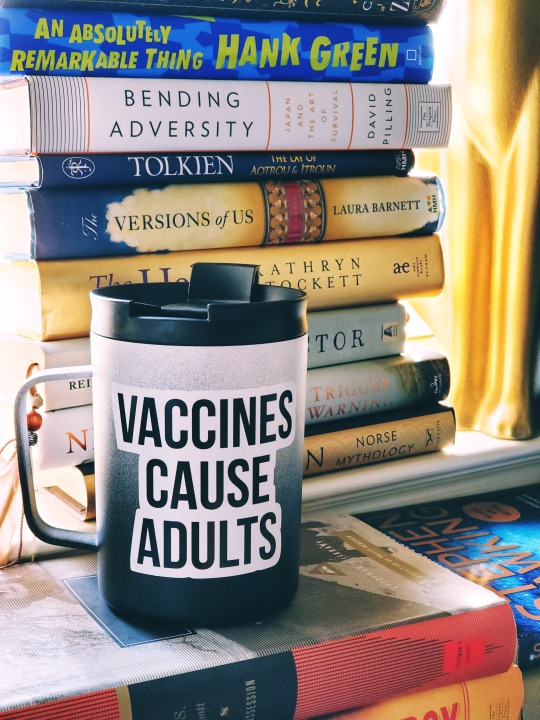
This mug is trending in my hospital right now. Legit it's more popular than me. I am sharing it this morning, post-shift and full of matcha latte, as a part of my effort in fulfilling my civic & professional duty of getting you all to just
GET THE DAMN FLU SHOT!!!
If you have insurance, it will be free somewhere (CVS, Walgreens, the grocery store, or your doctor’s office if you haven’t done anything that prevents you from showing your face there). If you don't have insurance, vaccinefinder.org can get you to somewhere that won't cost you an arm and a leg. Alternatively, here is a table of how much it'll cost you at the usual places in the US for the quadrivalent formulation as an uninsured consumer.
As for my vaccine spiel: I’m sure you’ve read all the articles swimming around in media about this, so I won’t go into the usual why’s. (Yes, for those outside of the USA, here people debate about something as elementary as why should we vaccinate.) I will, however, pull apart a few excuses anti-vaxxers use as shields, excuses I have personally heard before. (Full disclosure, I am a physician.)
"The flu shot makes people sick immediately after vaccination because the vaccine introduces the flu virus into the body, so it actually impedes the immune system from working properly! It doesn’t work!”
This shows very poor to non-existent understanding of how vaccination & the immune system works. The flu vaccine contains inactive, dead virus parts. It introduces your immune system to what the virus looks like; remember the third Harry Potter movie, where they posted pictures of Sirius Black the Death Eater Fugitive on pamphlets to warn the wizarding world about him so they know what he looks like? It’s exactly that. The faster the immune system can recognize an intruder, the faster it can kill it.
“The flu shot has other ingredients in it (like mercury) that cause various side effects from depression and memory loss to cardiovascular disease, ADHD, and autism.”
The flu vaccine used to contain a preservative called thimerosal (ethyl mercury), which is NOT the same as methyl mercury (the toxic kind). Let’s review a little chem here, as painful as those long-buried memories are. Thimerosal is a stable preservative that has been in use in tons of things since the 1920s. There is more mercury in breastmilk than there is in a single flu shot, guys.
A dude named Andrew Wakefield and a few of his buddies published a whack case series in the Lancet in 1998 suggesting that the MMR (measles, mumps, rubella) vaccine, preserved using thimerosal, predisposed behavioral regression & developmental disorders in children. But the sample size was 12 patients. Twelve. That is negligibly tiny. Obviously they didn’t do their power calcs. And it was a case series - the least reliable type of research you can publish because a case series is anecdotal. Their “data” did not show strong correlation between the MMR vaccine and autism; indeed, their analytical model wasn’t even constructed to examine that hypothesis. Multiple epidemiological studies followed hot on the heels of this paper, refuting its wild claims, but the damage was done & the publicity was already on fire. It sparked a huge anti-vaxxer movement that is responsible, frankly speaking, for the recurrence of eradicated diseases such as measles, which is deadly to little children. [ You can read more about this whole debacle here. ] It was all about the MMR vaccine at first, but “MMR” disappeared and eventually it became “all vaccines cause autism.” This is what happens when you combine poor health education, an irresponsible publishing journal, and an immoral media. The Lancet only formally withdrew this paper from publication in Feb 2010. To this day, I find it difficult to trust the Lancet.
The studies that came after Wakefield’s stupid one all refuted Wakefield’s claims with stronger data, proper analyses, systematic reviews, and actual fucking power calcs, like actual fucking researchers.
Finally, we don’t even fully understand autism. How can you definitely claim that one specific thing can cause it? Remember: correlation =/= causation.
“The CDC promotes flu vaccines because they have financial ties & get kickbacks from Big Pharma. It’s all big business. The flu vaccine doesn’t work.”
Bars and clubs will promote alcohol to you because they get kickbacks from the breweries. It’s all big business. Does that mean that the alcohol doesn’t work?
Why are you okay giving Big Pharma your money for vitamins you don’t really need (most people don’t really need multivitamins, it just makes your pee expensive) but you can’t give them money for life-saving, pandemic-fighting vaccines that COST LESS?
And since we’re talking about business, you should know that vaccines are actually not profitable for pharmaceutical companies, because they have to make entirely new batches EVERY. SINGLE. YEAR. The overheads on that must cost $$$$, I mean, they have to pay the researchers a living wage, and it takes months to make the vaccines. Come on, we all know the real money is made with ridiculously expensive life-saving medications such as insulin and the EpiPen. Duh.
Health is worth more than money, honey. Spend a day in a hospital hooked up to a ventilator with tubes coming out of every orifice and you will never deny this.
“I still get sick after the flu shot. It doesn’t work for me.”
The flu has various strains every year, and the vaccine is only made with the strains they (the researchers) predict will be the most widely distributed across a certain population. It involves a lot of statistics. Does this mean that you should skip the shot? No. Statistically, your chances of getting the most virulent, widely distributed strain is HIGHER than your chances of getting a different strain the vaccine isn’t made with. That statistics course really matters, you know.
Yes, you get a different type of flu vaccine depending on where you are in the world. The northern & southern hemispheres get different vaccine formulations because they typically get different strains. This is also why a flu strain from, say, southern China or India is fucking TERRIFYING for Europe or the US, because we likely will not have any immunity to that shit. (And vice versa.)
The flu virii evolve every year. They get more virulent, more adaptable, and more insidious every time. And do you know how they evolve? Because some asshole somewhere had partial/augmented immunity and the virus evolves under these conditions. This asshole was sick with a different strain of the flu before, but doesn’t believe in the flu shot, so he doesn’t get the one issued this year. He then gets maybe mildly sick with the new flu strain, while his wife is still sick with the previous flu strain he carried. The two strains are exposed to each other and under these conditions, the virus can evolve by mutation or genetic reassortment. Cross-exposure to other viral strains (antigenic drift) is a mechanism for viral variation & results in newer, deadlier strains that both partially immune people (infected before with other strains) AND vaccinated people cannot fight off. Then it spreads to their kid, who spreads it at the daycare, and those kids give it to their parents, who spread it at work... this, folks, is how you get an epidemic.
Vaccination really only works to eliminate a disease when you unilaterally vaccinate the entire population across the board. (As best as you can, anyway.) The vaccine will never work 100% - there is always a margin of error - but if you cover the entire population, your margin becomes more acceptable. Whereas if only some people get vaccinated, then you open up chances for viral mutation.
By the way, you might FEEL sick immediately after the flu shot, but you aren’t sick. That’s your immune system sucking your entire body dry of resources, making your muscles ache & giving you fatigue as it revs up & prepares brand new antibodies for this new virus. This takes a toll on your body, but you can combat the “sick” feeling by exercising lightly, hydrating very well, eating clean, and getting some sleep.
“My child already has a disease that lowers their immune system. If I give them the shot, that’ll completely deplete their remaining reserve. They might get a different infection and die!”
Again, a poor understanding of immune biology. 100% wrong. I give flu vaccines to immunodeficient patients with HIV, transplant patients who are taking immunosuppressants, and patients who are taking meds like Humira (immunosuppressing side effect). In fact, I prioritize the vaccine for them. They, above everyone else, need to be prepared for the coming strains of flu. I am giving their immune system time to prepare. - Of course I will monitor them closely & take appropriate precautions to prevent them from contracting other infections. I’ll support their physiological needs while they convalesce. But immunosuppression is no excuse. (That being said, have a conversation with your physician. Dosing, type, and timing of the vaccine can vary depending on your individual situation & condition.)
“Evidence now suggests that ingredients in flu shots can actually cause serious neurological disorders, like Guillain-Barre syndrome or similar neuromuscular diseases thought to be of autoimmune origin.”
In 1976, the CDC published that there was a risk of Guillain-Barre syndrome happening after a patient got a flu vaccine IF they have had the swine flu vaccine before. The risk was calculated to be 1 in 100,000 people who got the swine flu vaccine. The Institute of Medicine (IOM) did a scientific review on this issue in 2003 and concluded that the people who got the swine flu vaccine in 1976 were at increased risk, but otherwise, there has been no significant change or increase since then. Did you get the swine flu vaccine in 1976? No? Okay, go get the flu shot.
It is true that there have been observed cases where neuromuscular disorders like Guillain-Barre or chronic inflammatory demyelinating polyneuropathy (CIDP) seems to be triggered, or occur after the patient gets the vaccine. We don’t fully understand how or why. I have treated these patients (they are relatively rare, I see maybe 1-2 every year) and they recover well provided competent care at a good hospital. Look out for research on this, but until we definitively know a causative link, it’s foolish to skip a perfectly safe, proven, and highly recommended vaccine to avoid a very narrow “maybe.”
If you have questions, guys, I will answer. Drop me an ask or PM me. But please, please spread the word and get vaccinated.
If you get scared or doubt your decision to get the shot, remember that the only reason we are not all dead from smallpox (it was an epidemic) and cholera (a pandemic) and rabies (from all your pets) and typhoid (also a pandemic) and the fucking black plague is because of that 5ml of liquid in that tiny little syringe.
Vaccines do not cause autism. Vaccines cause adults.
GET. THE. SHOT.
#vaccine#vaccination#get vaccinated#science#medicine#medical science#research#medical history#infectious diseases#medical#flu vaccine#flu shot#influenza#immunity#immune system#flu virus#listen here#pay attention#BE SMART#VACCINATE#nerd moments
18 notes
·
View notes
Note
1) Mr ENTJ, I'm a 20 year old ENTJ university student doing a double degree in humanities and science (philosophy and computer science respectively). I made that decision at 18 because I have always found utility and inspiration in being versatile/interdisciplinary. However, in my first year I was diagnosed with an incurable autoimmune disease.
2) (double degree anon) In the periods of remission I am able to study, in times of sickness I am stuck in hospital. Next year I’ve been forced to go back home to focus on health because my health has since declined. I am struggling to reconcile this with my ambitious, over-achieving personality. I am thriving in what many rankings and people see as the best uni in my country (it’s got the country in the name and is federally funded) and I inevitably see returning as backsliding, or a failure.
3) (double degree anon) I am spending the year volunteering where possible, developing soft and hard skills (I already have experience with working for UN Youth and also research assistance in labs) but have been strongly advised against committing to something like a paid job. After the year back home is up I expect to return to my studies. How do I adapt to this reality without feeling like a failure? And how do I overcome this in being hired in the future?
________________
Related answers:
Can you talk about the quality(ies) or trait(s) that contributed most to your success? I read about your adversity and I want to know what is your personal mindset of getting through those challenges.
Dealing with failure and overcoming adversity
Your question’s timing is impeccable because I’m writing this response as I recover from yet another surgery that removed a potentially cancerous tumor.
“How do I adapt to this reality without feeling like a failure?”
You adapt to this reality by accepting that you haven’t failed at all. You’re not a failure, you were diagnosed with an incurable autoimmune disease, and unless there’s a new competition where all the winners don’t get an incurable autoimmune disease and all the losers do get an incurable autoimmune disease, it’s a safe bet this situation wasn’t the result of any personal actions. A setback like this can be a delay in schedule, an inconvenience, and an overall pain in the ass but it’s by no means a final outcome that will wreck years of planning and hard work. It’s simply a new variable that’s been introduced into the equation of your life that must be accounted for moving forward.
“And how do I overcome this in being hired in the future?”
It’s illegal for employers to discriminate based on physical conditions/disabilities/etc. With that said, to get hired, you still need to be able to do the job but can ask for special accommodations. I’d research your country’s labor laws but without a clear idea of what career you’re pursuing, I can’t elaborate. The focus now should be on excelling in school and doing all the right things so that when the time comes to graduate you’ve built a solid springboard to launch your career.
Additional thoughts:
Give yourself credit for the things you’ve already done right. That’s first and foremost because it’s easy to beat yourself up during a difficult time like this. It’s easy to think about all the things that can go wrong moving forward because of your condition without remembering all the things that have already gone right. You’re a student in a top university pursuing a double degree with research and UN experience under your belt plus the foresight, ambition, and desire to pursue even bigger goals for your life. That counts for a lot. Start there.
Focus on your health and adjust to your new normal. Take the time to get physically, mentally, and emotionally strong. Learn how your condition has altered your energy levels, daily routine, thought process, study habits, etc. so that you can create a new system. Take this time to seriously invest in your health instead of trying to catch up on work or school, don’t be in the hospital with tubes in your arms but a textbook on algorithms wide open because skipping steps and cheating the process can turn a one year break into a two year break.
“Do what you can, with what you have, where you are.” – Teddy Roosevelt. This is more for when it’s time to return to college. What’s within your control should be done to the best of your ability. Look for accommodations at the university, reduce class loads if required, explore online classes, and leave no stone unturned as you keep moving towards your goals. Progress is better than perfection.
16 notes
·
View notes
Text
So, I’m on a new med. It was FDA approved in AUGUST of this year, and insurance doesn’t cover it yet. It retails for $5000. They’re giving to me free, in what I call “open beta” and my husband says, “They’re doing it for the exposure!” Which, given how fast-tracked many drugs are these days for FDA approval, is pretty much exactly the case.
A friend said, “I just don’t like my friends being medical guinea pigs.”
My response? “Someone’s gotta.”
Medical meandering behind the cut.
I’m not normally an early adopter. It took me until 2014 to move from an old style cell phone that I usually didn’t bother putting minutes on, to an actual smartphone. I tend to buy my phones 2 years out of date, and my computers anywhere from 6 months out of date to 8 years out of date, depending on who they’re for. (The 7 year old gets an 8 year old WIndows 7 refurb desktop that I can stuff my old RAM and hard drives into. I get a reasonably new laptop with a good graphics card, but at least 6-12 months off the current “better”.)
But my kid was diagnosed with a rare chromosome condition at the age of 7 weeks and we were told that the chance of dying in 2 years was 70% and that there were no treatments, and that she wouldn’t develop language. And she’s 14 and has thousands of words and we experimented for YEARS with supplements to get there in ways that would let us avoid things like antipsychotics and constant doses of a variety of other drugs with serious side effects... and it worked. She doesn’t get sick often, she doesn’t get seizures, she has no kidney issues, she has language, she sleeps at night without powerful sedatives, and maybe we’ll need more meds for her at some point but the experiments were done VERY carefully, and always with an eye to her best interest and well being. Her fucking life was at stake. Her ability to interact with the world on her terms was at stake. OF COURSE we experimented.
And at 42, I was diagnosed with EDS, after already having fibro, and 7 years later I have rheumatoid arthritis of a variety that comes with a really poor prognosis because my RA factor and involved joints # was so astronomically high when I was first diagnosed, just 2 months after symptoms appeared. (584 for RA factor, and 27 involved joints, probably liver involvement by my guess, and since 2017 I’ve also had a bout of drug induced lupus, so that’s fun*.)
There are a lot of drugs out there for RA. People with “mild” RA may start out on methotrexate or plaquenil and have a great result and not need to look any farther for 15-30 years.
But my immune system is bitchy as hell. Once you go through things like steroids or NSAIDS, and methotrexate or leflunomide, and they don’t work enough, the next step is called Biologics. These are complex proteins which because of something something garbanzo, make the body dial down the inflammation by suppressing some specific part of immune function. When you quash tumor necrosis factor, for example, it pushes down inflammation all the way down the line, so it’s pretty much like hitting a china cabinet with a hammer.
Only, the china cabinet fights back if given half a chance.
So I tried half a dozen TnF inhibitors, and they varied from eh to okay. None were completely useless, the only one which seemed pretty okay, I had to go off of for surgery. And when I went back on it? My immune system had decided that the complex protein was the Enemy, and freaked the fuck out. So I went on Xeljanz, which inhibits a different part of the immune system, and a couple of great things happened, like 3 weeks of increasing energy and reduced pain, an ongoing reduction of pain, and some of my hair grew back. And then the immune suppression side effects hit. Namely, I get infections ALL the fucking time. It’s like whack a mole. Deal with the bacterial infection, get a fungal infection. Deal with the fungal infection, get shingles. Deal with that, get fungal infection again (because the meds don’t play well together.) I was off Xeljanz for a whopping 12 hours the other day, and TWO sources of ongoing difficult just magically cleared up, as my immune system reestablished itself.
ALL of these drugs, even the ones that have been around for a while, have huge black box warnings about things like “This can make you more likely to die of infection, cancer or pulmonary embolism. They can destroy your liver and make your hair fall out.” All of them.
And yet, when I went on methotrexate for the first time, which made me feel like absolute shit and made some things worse...
My liver enzymes improved. Methotrexate is ACTUALLY hepatoxic, but you know what’s also hepatoxic?
My OWN fucking immune system, apparently. We’ve never done a biopsy, because blood thinners and high clotting risk even without all this bullshit going on, but yeah, I was showing signs of gland and organ autoimmune issues YEARS before my joints got in on the party. Anyway, my liver enzymes aren’t great right now, which is part of why we switched me.
So, someone’s got to try these things out, and it’s not like they’re going to find someone else with my exact constellation of bizarre genetics and wonky immune and collagen issues.
I’ve taken two pills. Their retail would be $166 each, which is probably significantly more expensive than its weight in gold. (pills on average are about half a gram, give or take, and gold is $47-ish per gram right now.)
I don’t feel a lot better yet, but these take time. I also don’t feel worse, which is encouraging. We’ll see.
*if by fun you take it to mean fucking excruciating on every possible level
2 notes
·
View notes
Text
@soltheshiny I’ve got a lot to start with and it might be easier to save this way than in messages. 👌
If you’re on mobile, I heartily apologize, there’s a read more you won’t see and beneath it is some discussion of bodily functions.
1) Try not to dwell. I know, it sounds impossible. You can’t ignore the pain, let alone the other symptoms. However, our monkey brains are really dumb. The more you think about something, the more extreme your emotions surrounding it become. So if you feel 4/10 bad about something, but then think about it for ages, you’ll suddenly feel 6/10 bad.
Look at cute pictures
Color in a coloring book (also good for anxiety)
Play a video game
Read a book
Listen to a podcast
I know, it’s like “think of anything but a purple elephant” and it will still be there in your head, but when it’s not the focus, your brain doesn’t do the whole “MAKE IT WORSE” thing.
2) Say goodbye to bathroom shame. Also impossible, I know, but you’re going to have to ACT shameless and let your behavior train your stupid monkey brain.
“I need to sit by the door.” “Why?” “Because I will shit myself, Karen.”
People are TERRIFIED of poop and mentioning even the possibility of shit getting on something will make them much more accommodating of your condition.
3) Accidents will happen. Period.
Keep an extra set of clothes in your car with a plastic bag for soiled ones
Stock yourself with feminine hygiene pads for leaks
Stock yourself with bathroom wipes
Stock your chaffing treatment of choice
Stock yourself with water. It dehydrates the hell out of you.
Become the patron Saint of preparedness. Have snacks, pens, whatever.
Accidents attack your mental health and can ruin your day. You can mitigate this by having means to clean yourself up and get to a state where you can pretend it never happened.
The last item might seem a little strange, but consider this: a person gets their period early. Who’s their new hero? You. Your condition just saved someone else’s day. How amazing and nice is that? Having something good come from how ill you are is really a beacon of hope when things are at their worst.
4) Adjust your life to maximize your mental health. Autoimmune conditions are subject to massive fluctuations based on mood and other factors. Becoming the happiest bunny in the field won’t make flares go away by any means, but it will lessen them, make them less severe and leave you in a better place to deal with them.
5) Prepare for doctor and specialist visits.
Make a list of all medications, including over the counter and vitamins
Have your regular doctor’s details as well as your pharmacy’s on hand
Make a list of things you want to discuss
Have a record of symptoms and flares ups (more on this later)
Accept that the doctor not having answers right now is just the reality, not the doctor being terrible.
You will cry. Just accept it. It’s overwhelming and terrible and it feels like no one has any answers. You will get emotional. You will forget things. You’ll leave feeling like you wasted your time if you don’t have a list that you run through of everything you want to cover. I have been sick 14 years. I still cry when I see the doctor.
There are not a lot of answers for people with autoimmune conditions. There’s a lot of “We’ll try this and see how it works” there’s a lot of changing your diagnosis. This is normal. This does not mean your doctor is bad. If your doctor is compassionate and listens to you try to stick it out. No one has the answers. Human brains aren’t equipped to handle “We don’t know.” It will be incredibly difficult. Literally have a mantra in your head: “No one has any answers.”
They will change your medications and change your diagnosis and it’s frustrating as hell, but it’s so that you can get better treatment and so that the next person has to suffer less. So the next person CAN have answers. You are a critical data point in making treatment better for everyone. You are important and you are making a difference for others who are suffering. Let those thoughts bolster you through the hard times.
6) Keep a log of your symptoms, how you’re responding to medication and what you’re eating. Pick a time, set an alarm on your phone and then write notes about what you ate and how you felt in the last 24 hours. This is a common theme, but human brains are fucking stupid. If you are having a good day when you see your doctor, you will report that the medicine is more effective and you’ve been healthier and feeling better than you really have been. It’s critical that you have an accurate record of how things affect you.
The secondary benefit of this: every single medical professional suddenly takes you 100% more seriously. Doctors have to spend a lot of time and energy evaluating how accurate patient reporting is and translating that into usable information. If you just have piles of usable information, it’s like CHRISTMAS for them. I was in the emergency room recently and the staff’s eyes literally LIT UP when they saw that I had notes and information on my condition. I have a history of having my symptoms dismissed: not anymore.
I can literally just walk into my doctor’s office, look and sound completely fine and say, “Hey, this is happening, I think I need a run of [x] medication” and they will just prescribe it because they know that I know my body. (Obviously this doesn’t go for painkillers, but opiates are strictly inadvisable for most chronic conditions anyway)
And most importantly
7) Learn to forgive yourself. It’s impossible to do all of these things all of the time. Especially when you’re first diagnosed. You’ll get into slumps and dwell. You’ll forget your go-bag. You’ll be depressed and not take notes. You’ll have a cold and think it’s not worth it to record how you’re feeling because the cold is ruining it. It’s natural. It’s fine. We all do it.
These are all habits that you have to build and building habits is really difficult. What matters is that you’re trying. What matters is that you know what you have to do. What matters is that you continue to live your life. Your life can’t revolve around your condition or you’ll be miserable. Does your favorite food always cause a flare? It’s okay to say “Fuck it, I want to treat myself” and then suffer later. It’s okay. You’re not a failure. You’re not “making it worse.”
You’re not at fault for your condition. Nothing you did made it happen. You did nothing to deserve it. You shouldn’t have to do all of these things. Doing any of them, trying to do them, already sets you above the average person. You’re doing your best. You’re flourishing despite the hardships, even if you don’t feel like it now.
This list is actionable things. Things you can do to make your life better. The worst part is feeling helpless and you’re not helpless anymore. You can affect your treatment and your fate. You can put yourself back in control.
You can do this. You’re not alone.
You’re always welcome to message me directly about things. I will tell you upfront if I don’t have the spoons, so you never have to worry that you’re “bothering” me or “dragging me down” or “using up all of my energy.”
Additionally, my brother who has UC is available if you ever need to chat with him. He’s @shutupbeard here on tumblr, but we’re both more easily reached on discord - I’ll DM you our IDs.
Feel free to reblog this post, if you think someone needs to read it.
11 notes
·
View notes
Text
What Thyroid Blood Tests to Get & How to Interpret Them
When it comes to thyroid blood testing, there’s a lot of confusion. For those newly diagnosed. For veterans like myself. And especially for those who manage to never get an official diagnosis, but still feel like a hot mess.
After dealing with my own Hashimoto’s for a decade, I’ve gotten a little better about glancing at my numbers and being able to evaluate what it means about the state of my endocrine system. But it’s taken years of practice, and many far more knowledgable practitioners helping me advocate for myself, get the right panels one, and interpret the results properly.
Even though The Wellness Project has helped me manage my symptoms, the state of my thyroid is still a moving target, one that I try to check in with on paper every few months. I get a full thyroid panel to check my levels quarterly, which helps me tie some of my changing symptoms to my thyroid function and ensure I’m medicating properly through food and supplements.
I’ve been meaning to share the in’s and out’s of thyroid function testing for some time–what panels to request, and how to interpret the end results–but I’m glad I waited until I had one of those far more knowledgable practitioners willing to help me clue you in on the best course of action!
We’re so lucky to have Jill Grunewald as our guide for this portion of the #HashiPosse journey. She’s a Functional Medicine Certified Health Coach, founder of Healthful Elements, and most importantly, co-author of the fabulous resource: The Essential Thyroid Cookbook.
Read on for the biggest mistakes practitioners make when it comes to testing your thyroid, and Jill’s amazing advice for how to advocate for yourself at the doctor’s office. And if you’re in need of thyroid-friendly recipes, make sure to pick up her book!
With health and hedonism,
Phoebe
The Best Thyroid Blood Tests to Ask For and How to Read Them
It’s a common yet unfortunate scenario.
You don’t quite feel like yourself, so you go to the doctor. Fatigue, constipation, dry skin, and stubborn weight gain have been your constant companions for too long. Perhaps you’re frequently cold and your brush is revealing just how much hair you’re losing.
Your doctor may isolate these symptoms (with an anti-depressant, laxative, or a suggestion to “eat less and work out harder”). Or he or she may say, “Let’s check your thyroid.” (Right answer.)
“Checking” can have vastly different meanings, again, depending on the doctor’s worldview.
Many medical professionals (endocrinologists included) operate under the conventional medical conviction that low thyroid function (hypothyroidism) can be diagnosed via one blood test and one blood test only: thyroid stimulating hormone (TSH), a pituitary hormone that tells the thyroid to do its job.
But TSH can be “normal” in the face of raging hypothyroidism. It’s not wholly irrelevant, but it tells a small part of the story and should always be taken in the context of other thyroid hormones. (More on this in the chart below.)
Regarding the evaluation of TSH as a sole indicator of what kind of shape your thyroid is in, women’s health expert, Aviva Romm, MD states, “In a world where medical over-testing is rampant, I have to say, I find myself confounded by the fact that so many physicians are resistant to ordering anything but a TSH … as the first form of evaluation, when from a scientific and medical standpoint, that test can be normal and there can still be a low functioning thyroid. It’s outdated medical dogma to order solely this test.”
To add a third layer to this story, many doctors utilize outdated lab reference ranges—those parenthetical numbers next to your lab value that tell you whether you’re within the acceptable range.
This type of thyroid “treatment” leaves many un- or under-diagnosed.
“You may be told you have borderline thyroid problems or sub-clinical thyroid disease and your doctor will watch it,”says Dr. Mark Hyman. “What will he or she watch for? For you to get really sick?”
These archaic practices cast aside a vast group of people who often have subclinical hypothyroidism, meaning they will experience a bevy of symptoms, yet only see slight changes in their TSH blood labs.
An equally important layer: the antibodies that show the presence of Hashimoto’s/autoimmune hypothyroidism–thyroid peroxidase antibody (TPOAb) and thyroglobulin antibody (TgAb)–are tests that are infrequently performed.
You deserve to know if you have Hashimoto’s, which indicates thyroid tissue attack.
It’s estimated that a whopping 97 percent of people with hypothyroidism have Hashimoto’s. And it’s been shown that once you have one manifestation of autoimmunity—any manifestation—if it goes unmanaged, the likelihood of developing yet another autoimmune condition is significantly increased.
By using old guidelines and limited thinking, conventional medicine glosses over the millions who suffer with low thyroid function.
As the saying goes, “Don’t guess, test.” It’s important to do the right tests and to evaluate your labs based on the functional reference ranges, not antiquated ranges that often lead to misdiagnosis, mistreatment, and the passage of time with continued suffering.
Here’s a Cheat Sheet for the Top Issues in Thyroid Blood Testing:
Telltale symptoms, thyroid not suspect (or tested)
Testing TSH only
Using outdated reference ranges
Not testing for thyroid antibodies (TPOAb and TgAb)
Why is the Thyroid So Important?
The thyroid is a butterfly-shaped gland in your neck below your Adam’s apple and is hailed as “the master gland” of our complex and interdependent endocrine (hormonal) system. It’s the spoon that stirs our hormonal soup. It produces several hormones, with tri-iodothyronine (T3) and thyroxine (T4) being the most critical to our health.
Given that our endocrine system is responsible for growth, reproduction, energy, and repair and the thyroid is largely at the helm of this complex and interdependent system, an underfunctioning thyroid can have profound implications for the whole body.
Thyroid hormones transport oxygen into your cells and are critical for energy production. Every cell in the body has receptors for thyroid hormone and the thyroid is a master toggle that flips on the genes that keep cells doing their jobs.
It’s the boss of our metabolism and an underactive thyroid can affect weight, mental health, and heart disease risk.
Thyroid hormones affect our health systemically and directly act on the brain, the gastrointestinal tract, the cardiovascular system, bone metabolism, red blood cell metabolism, gall bladder and liver function, steroid hormone production, glucose metabolism, protein metabolism, neuromuscular function, digestion, and body temperature regulation.
Given the thyroid’s far-reaching impact, it’s not difficult to understand how misdiagnosis and under-diagnosis is nothing short of a public health concern.
You Are Your Best Advocate
If you have a cluster of symptoms pointing to hypothyroidism (find a list here), listen to your body and trust your intuition. Managing hypothyroidism and Hashimoto’s is an exercise in becoming the CEO of your health.
Reject the notion that TSH alone determines your thyroid status.
Don’t allow your doctor to use outdated lab reference ranges or to neglect testing for the antibodies that could reveal Hashimoto’s thyroiditis.
Arm yourself with the right information. Use the chart below as a cheat sheet. You can use this to get a new set of labs or to compare values with any recent labs you’ve done.
This is what I feel are the most clinically relevant thyroid tests and reference ranges. Ask your doctor for a “full thyroid panel”and make sure the following are included:
Lab
Functional reference range
Free T3 (FT3)3.2 – 4.2 pg/mLFree T4 (FT4)1.1 – 1.8 ng/dLReverse T3 (RT3)90 – 350 pg/mL or < 10:1 ratio RT3:FT3Thyroid stimulating hormone (TSH)0.9 – 2.0 mU/LThyroid peroxidase antibody (TPOAb)< 4 or negativeThyroglobulin antibody (TgAb)< 4 or negative
Some important notes:
T3 is “the big daddy” of thyroid hormones and the most metabolically active, affecting almost every physiological process. The “free” in front of T3 (and T4) tells you what is available and unbound and therefore usable by the body.
Reverse T3 is just that—the “reverse” of T3. It blocks thyroid receptors and can cause patients to be unresponsive or resistant to T3. When the body is in conservation mode due to stress, including fatigue, nutritional deficiencies, or infection, it will reroute thyroid hormones. You want RT3 low, and high RT3 is often brought about by intense or prolonged periods of stress. RT3 is typically high in people with more advanced adrenal dysfunction (aka HPA (hypothalamic-pituitary-adrenal) axis dysfunction). You can see that there are two metrics in the chart above for RT3; while RT3 alone is an indicator of thyroid hormone resistance, calculating your RT3: FT3 ratio can also provide information on thyroid status. Click here www.stopthethyroidmadness.com/rt3-ratio/ to calculate your RT3:FT3 ratio.
According to many in the functional medicine community, anyone with TSH over 2.0 is hypothyroid, although TSH is an overall poor marker of thyroid function and should always be taken in the context of other thyroid labs, especially given that TSH can be normal in the face of low thyroid function.
This was a guest post courtesy of the wonderful Jill Grunewald, HNC, Functional Medicine Certified Health Coach, and founder ofHealthful Elements, is a thyroid health, Hashimoto’s, and alopecia (autoimmune hair loss) specialist and co-author of the #1 best selling Essential Thyroid Cookbook.
Have more questions about interpreting thyroid labs? Ask away in the comments section!
Source: https://feedmephoebe.com/what-thyroid-blood-tests-to-get-how-to-interpret-them/
1 note
·
View note
Link
More information from an IHS physician in Kayenta explaining why this pandemic is so devastating for the Diné:
"A Plea from the Navajo Nation...from both Indian Health Service (IHS) and tribally run hospitals, of which there are only a handful serving an area the size of West Virginia... Please read.
Many are feeling alone on the Navajo Nation right now, especially in the remote community of Chilchenbito, which is essentially on lockdown due to the major outbreak of SARS-CoV-2, the virus causing COVID-19.
As a public health physician living in this area for the past 8 years, I am part of the Epi Response Team, and have already witnessed the terrible impact this virus has had, and it’s only just the beginning. It is rapidly spreading to surrounding communities, mostly due to a multi-church gathering that occurred in Chilchenbito in early March, and the handful of emergency rooms on the Reservation are already overwhelmed with people presenting in respiratory distress. Many are being intubated, stabilized, and flown out to tertiary care centers scattered across AZ, NM, UT, and CO; but some are also dying at home or shortly after arrival to the ER, and not being tested at all because we don’t have a system in place for post-mortem testing. General testing is also not widespread, so the true numbers are grossly underestimated. Our tertiary care centers in the surrounding states are filling up fast - likely reaching capacity by next week - and we will have to keep these incredibly sick patients at our facilities on the Rez, without enough critical care nurses or PPE. We have smart doctors and nurses here and we are actively surge planning: designing respiratory care units in existing spaces and purchasing more ventilators (that are on back order), but it’s just not going to be enough.
I want to share why the Navajo Nation, is so incredibly vulnerable to this virus (and pretty much every communicable disease in existence):
The Navajo (Dine) people suffer from high rates of obesity, diabetes, hypertension, lung disease, and autoimmune conditions (to name a few), but this is only a small part of the story here.
Poverty - It’s hard to practice proper hand hygiene when there is no running water. Many have to haul water, but as the more physically mobile members of the family get sick, they are no longer able to do so. And many do not have the income to purchase soap, hand sanitizer, or even food... especially when they have to drive an hour to the closest store (if they have the money for gas) only to find that things are out of stock. USPS does not deliver to homes on the Rez, and many homes do not have a physical address where items can be delivered by even UPS or FedEx.
Overcrowding - When there are multiple generations, and perhaps multiple families, living in one small household, it’s hard to isolate those that are sick from those that are well. Entire households are falling ill.
Limitations of sheltering in place - related to overcrowding, if an entire household is sheltering in a small place, and unable to isolate those that are sick, and do not have the resources for proper hand hygiene and disinfection, it is easy for the virus to spread to everyone in the house. Additionally, it is difficult for these families to obtain things like groceries and other goods when they don’t have anyone that can safely leave the house...
Numbers - There are over 160,000 living on the Nation. There are only 28 ventilators on the entire Reservation. We need at least double this amount if the models/projections for this disease are correct. And that doesn’t take into account the number of medical professionals needed to take care of these critically ill patients: doctors and nurses that are continually getting exposed to the virus and being quarantined because they do not have enough personal protective equipment (PPE)
Access to information - When much of this community is comprised of elders that speak their traditional language and do not have a smartphone or social media, it is hard to disseminate information quickly to stay up to date... many households do not have land lines or television or even electricity. And when this information isn’t disseminated widely and effectively, many are uninformed and/or scared, many don’t know what to do if they or someone in their household develops symptoms, many don’t know to socially distance/isolate... traditional gatherings and ceremonies, including funerals, continue to take place... and spreading occurs.
Access to care - many live far from the health centers and don't have reliable transportation. Additionally, if there is a medical emergency in the home, often times EMS has difficulty reaching folks in a timely manner because of distance and/or unpaved, unmaintained roads.
Protection for healthcare workers - When the nearby health centers do not have enough PPE to safely see patients presenting to the hospital, let alone to perform vital home visits for assessments and face-to-face education, everyone is put at risk. The EMTs responding to 911 calls are also put at tremendous risk!
And here is some alarming data (as of March 31, 2020):
There are 1289 positive cases in Arizona (24 deaths). There are 148 cases in Navajo Nation (174 cases updated 3/31/20) Of the 148 cases, 49% of the cases are from Kayenta Service unit (KSU) and 16% from Chinle Service Unit (CSU). Kayenta Service Unit has been most impacted by the pandemic where almost half of the cases have required hospitalization (48%).
About 50% of those hospitalized required ICU level of care (not included in this analysis, but extrapolated from reports from KSU and CSU emergency physicians transferring patients from the ER to tertiary care centers).
These numbers are really striking, especially since it points to the Navajo becoming quite ill (requiring hospitalization and ICU care) at higher rates than the general US.
The Navajo Nation population represents about 2% of the Arizona state's population, yet Navajo positive COVID-19 cases are representing at least 11% of all Arizona cases at this time.
We are trying our best out here, but it is so incredibly difficult.
Please be mindful of the challenges we face.
But also be aware of the grassroots efforts by the local health centers, the Johns Hopkins Center for American Indian Health, and the Navajo Nation to obtain and allocate resources (including food, water, soap, disinfectants, educational materials, etc) and to provide the best care possible.
That being said, the Navajo Nation government and Indian Health Service Area Office doesn’t seem to have the infrastructure or organization to handle what is happening (and what is about to happen) at this kind of scale. Plus, it seems that these two entities are not communicating effectively with each other to truly determine what is needed "on the ground."
President Nez is being proactive about reaching out to the state for any form of assistance, but the "assistance" we are receiving so far is not the most applicable.
The National Guard made press releases yesterday about how they set up a "federal medical station" in Chinle (my home) and how they are providing assistance to the Navajo Nation... but what they failed to share with the press is that they basically delivered a kit to set up a hurricane-like shelter (or, rather, camp) in an existing structure that is too far away from the hospital to serve as medical overflow, and only has a couple of restrooms, NO staff, and no essential medical supplies.
Had they discussed any of this with the local IHS Hospital beforehand, they could have learned key things about the area and potential resources already in place to develop a better plan (which the local IHS has formulated), but again, communication between these entities has not been very straightforward.
I spoke with the National Guard and FEMA in Kayenta on March 30, 2020 about all of the above concerns, and the National Guard, pointblank to my face, said that they are "spread too thin" and that "your hospitals need to focus on your ethics plan for rationing care."
Despite this answer, they are reportedly airlifting a bunch of PPE to the area soon 🙏
We need more manpower, more communication between key entities, more critical care nurses, more PPE and other supplies, and more people who can get the word out and who will LISTEN and ACT. We need applicable solutions to face this crisis.
Sure, there have been funds from the stimulus package slated for the IHS and tribe, but this will take precious time to actually reach this area... and will likely get here after the worst has already occurred. Plus, the money is not worth a whole lot when vendors are out of stock of much needed supplies and we can't find nurses and other staff to pay."
Thank you for reading.
Sincerely,
Nina Ritchie, M.D.
MedPeds Physician
“Navajo Nation — in the “Four Corners” area, with land that borders part of Northeastern Arizona, Southeastern Utah, and Northwestern New Mexico — has been hit hard by COVID-19. So far there are 354 confirmed cases with 15 confirmed deaths. As with much of the nation, the testing picture is incomplete. Navajo Schools stayed open two days longer than non-reservation schools, but the Navajo Nation has taken up strong distancing precautions since then. The Diné have now issued stay-at-home orders and instituted a strict curfew. They’ve also declared a state of emergency.
The seriousness of this response isn’t without precedent. The Spanish Flu pandemic of 1918-1920 was devastating for the Navajo Nation. According to historical records, 12 percent of the population perished, or 3,377 people. So far, COVID-19 has mortality rates anywhere from less than one percent to ten percent or more, depending on a long list of factors. But preparedness seems to be a major determiner and Navajo Nation is woefully ill-equipped to fight off a virus like this. It’s certainly worth noting that 2009’s Swine Flu was four times more deadly in Indian Country than the rest of the U.S.
Diné attorney and leader Ethel Branch has set up the Navajo & Hopi Families COVID-19 Relief Fund on GoFundMe (she also set up a Relief Fund for the Havasupai). This is the fastest and most direct way you can help people right now.
So far the Relief Fund has 2,000 families seeking assistance. The money is going to packages that are being dispatched throughout Navajo Nation. The Guardian reports that each package is filled with “flour, beans, rice, canned soups, dried meat, fever and cough medicine, as well as fresh vegetables, fruit, and meat when available.” These are crucial lifelines for many Diné.
So far, the Navajo & Hopi Families COVID-19 Relief Fund is at about 50 percent of its goal. You can donate directly right here.”
Read the full piece here
20K notes
·
View notes
Text
Dying Patients With Rare Diseases Struggle to Get Experimental Therapies
At 15, Autumn Fuernisen is dying. She was diagnosed at age 11 with a rare degenerative brain disorder that has no known cure or way to slow it down: juvenile-onset Huntington’s disease.
“There’s lots of things that she used to be able to do just fine,” said her mom, Londen Tabor, who lives with her daughter in Gillette, Wyoming. Autumn’s speech has become slurred and her cognitive skills slower. She needs help with many tasks, such as writing, showering and dressing, and while she can walk, her balance is off.
Autumn has been turned down for clinical trials because she is too young.
“It is so frustrating to me,” Tabor said. “I would sell my soul to try to get any type [of treatment] to help my daughter.”
For patients like Autumn with serious or immediately life-threatening conditions who do not qualify for clinical trials and have exhausted all treatment options, there may be another option: seeking approval from the Food and Drug Administration for expanded access, or compassionate use, of experimental therapies.
Definitive numbers are hard to find, but studies from researchers, actions by drugmakers and insights from experts suggest that getting expanded access to unproven therapies for rare diseases is more difficult than for more common illnesses, such as cancer.
Even with experimental treatments on the rise, patients with rare diseases frequently face an unwillingness by drug companies to provide them before clinical studies are completed. Developing drugs for these diseases is an especially fragile process because the patient populations are small and often diverse, having different genetics, symptoms and other characteristics, which makes studying the drugs’ effects difficult.
Drugmakers believe offering a drug before studies are finished could impair its development and jeopardize FDA approval.
Companies working on therapies for rare diseases, especially smaller ones, could feel those repercussions acutely, said Lisa Kearns, a researcher in the ethics division of New York University’s medical school and member of the division’s working group on compassionate use and preapproval access. “There’s not as much investment in rare diseases, so an [adverse] event could frighten the already limited number of potential investors.”
Drugs that were not made available for compassionate use last year until studies were completed include Evrysdi, for spinal muscular atrophy; Enspryng, for an autoimmune disease of the optic nerve and spinal cord called neuromyelitis optica spectrum disorder; and Viltepso, for certain patients with Duchenne muscular dystrophy.
A spokesperson for Roche, which makes Evrysdi and Enspryng and is working on a treatment for Huntington’s disease, said the decision was tied not to the type of disease but to company policy: Roche does not set up expanded access programs for any drugs until results are available from a phase 3 clinical trial. (Those phase 3 studies are typically the last testing done before the company seeks drug approval.)
Another company’s experimental drug for myasthenia gravis, an autoimmune disease that leads to skeletal muscle weakness, similarly was not available through an expanded access program until research was completed last year, and no programs have started for a therapy being studied in a phase 3 clinical trial for Huntington’s disease and for amyotrophic lateral sclerosis (ALS), a fatal neurodegenerative disease often referred to as Lou Gehrig’s disease.
One slight, but notable, deviation: Drugmaker Biogen agreed this year to allow certain ALS patients to receive an experimental drug as early as July 15, after the testing was to be completed but before the results are known.
Dr. Merit Cudkowicz, a neurologist at Massachusetts General Hospital in Boston, has helped patients get therapies through expanded access. Since September 2018, she and colleagues launched 10 programs that seek to match people with ALS therapies being developed by drug companies, but only about 120 patients have received therapies this way. More than 16,000 people in the United States were estimated in 2015 to have ALS and most do not qualify for clinical trials because of the progression of their disease or very strict eligibility requirements.
These examples contrast with some drugs for more common problems. Gleevec, for leukemia, was offered to thousands of patients through expanded access programs before the manufacturer completed the clinical studies that led to FDA approval. Videx, for HIV/AIDS, and Iressa, for the most common type of lung cancer, were similarly offered to large numbers of patients even as clinical trials were ongoing.
Last year, Novartis gave more than 7,000 patients worldwide early access to cancer drugs.
Doctors also report that getting experimental drugs for cancer patients is relatively simple. More than 200 physicians around the country were surveyed, and among those who applied for access, nearly 90% said they had secured drugs still being investigated for patients who were not responding to approved therapies.
California researchers found similar trends in a review of 23 social media campaigns launched by patients between 2005 and 2015 seeking a variety of experimental treatments. While seven of the 19 patients with cancer received early access to requested drugs, no access was allowed for three patients with rare diseases, although one of those patients was allowed to enroll in a clinical trial.

Companies base their decisions on whether to provide a therapy through expanded access on a number of factors, said Jess Rabourn, CEO of WideTrial, which helps pharmaceutical companies run compassionate use programs. In general, there should be evidence that patients can tolerate the treatment and an expectation that any benefit outweighs the risk, he said.
“This idea that you have to wait until the research is done is baloney,” he said. “We’re talking about patients who are going to die if they’re told to wait.”
But drugmakers often view it differently, even though evidence suggests that granting early access very rarely disrupts drug approval.
Kearns explained that companies often wait until phase 3, or after, because they can be “relatively” confident of a drug’s safety and effectiveness. “They don’t want to harm patients, of course, but they also do not want to threaten the drug’s eventual regulatory approval with an adverse event in [a] very sick patient population.”
Melissa Hogan, who consults on clinical trials for rare diseases and is an FDA patient representative, attributes the lack of access to the high cost of therapies and the tightknit nature of the rare disease community, where patients and their families often set up social media groups and exchange ideas and treatment plans. Companies “know that if one patient gains access, other patients will know” and ask for access, said Hogan, who has a son with mucopolysaccharidosis type II. That could overwhelm small drugmakers with little manufacturing capacity.
These concerns cause “many companies [to] just throw up their hands and take a hard line of no [expanded access] until they reach approval stage,” said Hogan.
The 2018 Right to Try law offers another option for some patients. Unlike expanded access, the law applies only to requests for medicines — not medical devices — and does not require approval from the FDA or an institutional review board, a committee that reviews and monitors people participating in research for their protection. The legislation, however, doesn’t oblige companies to grant a request.
For Cali Orsulak, expanded access may be her husband’s only option. He was diagnosed with ALS in 2019 at age 43.
“We did our best with the skill level we had to search clinical trials all over Canada and the U.S., and then covid hit and it became increasingly difficult,” said Orsulak, explaining that they live in Canada but seek medical care in the United States. “Now that my husband has progressed, it’s even harder to get into clinical trials.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
USE OUR CONTENT
This story can be republished for free (details).
Dying Patients With Rare Diseases Struggle to Get Experimental Therapies published first on https://nootropicspowdersupplier.tumblr.com/
0 notes