#Prolactin and Infertility
Explore tagged Tumblr posts
Text
The Role of Yoga and Ayurveda in Women’s Reproductive Health

Women’s reproductive health is a crucial aspect of overall well-being, influencing not just fertility but also hormonal balance, menstrual health, and emotional stability. With modern lifestyles becoming increasingly stressful and sedentary, reproductive health issues are on the rise. From irregular periods and hormonal imbalances to polycystic ovarian syndrome (PCOS) and infertility, many women face challenges that affect their quality of life.
While modern medicine offers various treatments, many women seek holistic approaches that support long-term wellness without side effects. Yoga and Ayurveda, two ancient Indian sciences, provide natural and effective solutions to improve reproductive health. Ayurveda focuses on restoring balance through diet, lifestyle, and herbal remedies, while yoga enhances physical, mental, and emotional health through movement and breathwork.
Yoga and Ayurveda play a vital role in enhancing women’s reproductive health, offering practical strategies to integrate these ancient wisdom practices into daily life for better well-being.
Understanding Women's Reproductive Health Issues
Women experience a wide range of reproductive health challenges, often influenced by lifestyle, diet, stress levels, and genetic factors. Some of the most common reproductive health concerns include:
1. Menstrual Irregularities:
Irregular periods, painful cramps (dysmenorrhea), and heavy bleeding (menorrhagia) can indicate underlying hormonal imbalances. Factors such as stress, poor diet, and lack of physical activity contribute to menstrual disorders.
2. Polycystic Ovarian Syndrome (PCOS):
PCOS affects millions of women worldwide and is characterized by irregular periods, excessive hair growth, acne, and weight gain. It is often linked to insulin resistance and inflammation.
3. Endometriosis:
This condition occurs when tissue similar to the uterine lining grows outside the uterus, leading to severe pain, heavy periods, and fertility issues.
4. Infertility and Hormonal Imbalances:
Conditions like thyroid disorders, high prolactin levels, and premature ovarian failure can impact fertility, making it difficult for women to conceive.
5. Menopause and Perimenopause Symptoms:
As women age, hormonal fluctuations cause symptoms like hot flashes, mood swings, insomnia, and reduced bone density.
The good news is that yoga and Ayurveda offer natural ways to manage and improve these conditions by restoring hormonal balance, reducing stress, and promoting overall reproductive health.
Ayurveda: A Holistic Approach to Women's Reproductive Health
Ayurveda, the ancient science of life, believes that reproductive health is deeply connected to the balance of the three doshas: Vata, Pitta, and Kapha. When these doshas are in harmony, the body functions optimally, but any imbalance can lead to reproductive issues.
1. Ayurvedic Diet for Reproductive Health:
• Vata Imbalance: Causes irregular cycles and infertility. Eat warm, nourishing foods like ghee, milk, and cooked vegetables.
• Pitta Imbalance: Leads to heavy bleeding and inflammation. Consume cooling foods like cucumbers, coconut, and aloe vera juice.
• Kapha Imbalance: Can cause PCOS and weight gain. Eat light, dry foods like lentils, bitter greens, and turmeric.
2. Herbal Remedies:
• Ashwagandha: Helps manage stress and balance hormones.
• Shatavari: Supports fertility and regulates menstrual cycles.
• Turmeric: Reduces inflammation and improves digestion.
• Triphala: Detoxifies the system and enhances gut health.
3. Panchakarma Therapy:
This Ayurvedic detoxification process helps remove toxins, balance hormones, and rejuvenate reproductive organs.
Ayurveda teaches that by following a proper diet, using natural remedies, and adopting a balanced lifestyle, women can significantly enhance their reproductive health.
The Power of Yoga in Supporting Women's Reproductive Health
Yoga plays a vital role in enhancing reproductive health by improving blood circulation, reducing stress, and balancing hormones. Certain yoga postures are specifically designed to strengthen the reproductive organs and promote fertility.
1. Best Yoga Poses for Reproductive Health:
• Baddha Konasana (Butterfly Pose): Improves blood flow to the pelvic region and regulates menstrual cycles.
• Bhujangasana (Cobra Pose): Stimulates the ovaries and enhances hormonal balance.
• Setu Bandhasana (Bridge Pose): Strengthens the pelvic muscles and relieves menstrual discomfort.
• Supta Baddha Konasana (Reclining Bound Angle Pose): Relaxes the reproductive organs and reduces stress.
2. Breathing Techniques (Pranayama):
• Anulom Vilom (Alternate Nostril Breathing): Balances hormones and calms the nervous system.
• Bhramari (Bee Breath): Reduces anxiety and promotes relaxation.
3. Meditation and Relaxation:
Stress is a major factor in reproductive health issues. Practicing mindfulness and guided meditation can significantly lower cortisol levels, improving overall well-being.
Practical Tips to Integrate Yoga and Ayurveda into Your Daily Life for Better Reproductive Health Results
1. Start Your Day with Warm Water and Lemon: Helps detoxify and improve digestion.
2. Practice Yoga Daily: Even 15-20 minutes can bring noticeable improvements.
3. Eat Seasonal and Wholesome Foods: Prioritize fresh, home-cooked meals over processed foods.
4. Use Herbal Supplements Mindfully: Consult an Ayurvedic practitioner before taking herbs like Ashwagandha and Shatavari.
5. Maintain a Regular Sleep Cycle: Proper rest is essential for hormonal balance.
6. Manage Stress with Meditation and Breathing Exercises: Reducing stress is key to a healthy reproductive system.
7. Stay Active but Avoid Overexertion: Moderate physical activity like walking or gentle yoga helps maintain balance.
Conclusion
Women’s reproductive health is deeply connected to their overall lifestyle, mental well-being, and daily habits. While modern medicine provides effective treatments, integrating yoga and Ayurveda into daily life can offer long-term benefits without side effects. By focusing on balanced nutrition, stress management, and mindful movement, women can naturally improve their reproductive health and overall vitality.
Whether dealing with PCOS, menstrual irregularities, or fertility concerns, these holistic practices offer a natural path to healing. With consistency and awareness, every woman can harness the power of Ayurveda and yoga to achieve better reproductive health and a higher quality of life.
4 notes
·
View notes
Text
August 2024 Astrology Review
I thought it would be interesting to go over the predictions I made for August and see how well some of them matched up.
August 2024 Transits:
5th - Mercury Retrograde
7th - Mercury conjunct Venus
14th - Mercury reenters Leo
18th - Mercury square Uranus
18th - Mercury Cazimi (Mercury conjunct Sun)
23rd - Mercury trine Chiron
24th - Mercury sextile Mars
28th - Mercury goes direct
5th - Mercury Retrograde through 9th House
Prediction: When Mercury retrogrades through Virgo; I will first try to analyze and communicate about life philosophy and spirituality in a precise and methodical way that seeks to improves things/get reassurance but I generally will not get the connection I seek.
Had a big fight with my partner that ended with her going to a mental health outpatient clinic to calm down and get her meds looked over. So fairly spot on there.
7th - Mercury conjunct Venus (in 9th House)
Prediction: I will seek connection through analyzing my life philosophies and spirituality with others. This may not make me feel connected but it will likely bring new perspectives and clarity for someone involved.
Meh on this one. The big thing that happened was I had GI issues and quite literally shit the bed. Though I suppose I did spend a lot of time watching dharma talks this day too to help me through the illness.
14th - Mercury Retrograde through 8th House
Prediction: When Mercury retrogrades through Leo; I will then try be seeking to better understand death and/or my shared resources through a creative outlet or play. Either I’m unlikely to get the release I seek in this time or it will come about in unexpected ways.
I mean this was vague enough to be accurate lol. I did wind up thinking about death and shared resources a lot because I had to go get my prolactin checked a second time to confirm it was high and it was. Finding out I might have a little tumor in my head was rough. I also had a fight with my partner that day that was sparked by me saying I didn't feel supported. So it fits but more specifics would have been helpful.
18th - Mercury in Leo/8th House Square Uranus in Taurus/5th House
Prediction: My desire to communicate about my shared resources or death in a commanding way will be at odds with a sudden change that’s been building for some time in my creative or sex life.
Kind of a miss on the interpretation for this. I can see in retrospect what it was likely talking about. This was a longer term transit and has been present all through me finding out that I have PCOS and am thus likely infertile. It really highlighted my painful feelings around having children - wanting badly to adopt or foster but not being healthy enough or wealthy enough to afford to.
18th - Mercury Cazimi (Mercury conjunct Sun in Leo/8th House)
Prediction: I will have the ability to speak clearly and commandingly about my shared resources or death. My own perspectives may overpower those of others if I give into ego/vanity.
The Cazimi was indeed probably the least difficult day of the retrograde. Got out and did Pokemon Go Community Day with my partner that day and had a nice time. It was like one day her mania wasn't driving the interaction. I was careful not to talk over people this day and I think that really helped.
23rd - Mercury in Leo/8th House trine Chiron
Prediction: I will be supported in speaking commandingly or publicly about my past experiences and trauma, particularly on topics such as family. This may overlap with discussions of death, inheritance, or shared resources.
I decided to skip my brothers birthday party - he'd been incredibly self centered during my illness in July, didn't want to mask or have it outside, and was ignoring my texts - so I told my mom that I wouldn't be going and surprisingly received absolutely zero pushback. Usually there's at least some guilt tripping involved. So this one was spot on.
24th - Mercury in Leo/8th House sextile Mars in Gemini/6th House
Prediction: Difficulty with illness or a subordinate/pet will bring an opportunity to frankly discuss death or shared resources.
This one was unfortunately very correct. This is the day my cat went missing. It's very likely he's passed. I also was laid up on the couch for most of the day with GI issues.
28th - Mercury goes direct
Prediction: I will get more of a release around death/shared resources and clarity around spirituality and philosophy as Mercury retraces its steps.
Bit vague so technically fits. Had a big fight with my partner but it really clarified my ideas around self care - including the role my spirituality plays in my decision making - that I've been thinking on a lot this month. I imagine that will only continue as it exits the shadow.
So overall - pretty accurate. I wish I had a bit more clarity on some of them so I could have taken some steps to remediate it but some transits will find a way to manifest poorly no matter what. It's clear from my notes that this month was a difficult one emotionally and that's more or less what I expected from the transits. I was surprised I wasn't ill more but I think some of the medical leaning aspects wound up manifesting through all the doctors visits and procedures I had to do this month.
Also - we left early for every appointment this month and despite often hitting traffic we were never late to all but one important engagement. So it is possible to remediate some aspects it seems.
I will likely try doing Septembers some too so that I can have a bit of a heads up as I'm trying to navigate the health stuff August turned up. I would recommend doing this kind of analysis to other folks as well. It's genuinely helpful to know what might cause problems and at least be prepared.
Check out this post for more on how to find and interpret transits.
5 notes
·
View notes
Text
Female infertility

Diagnosis:
If you have been unable to conceive within an acceptable time frame, consult your doctor for an examination and treatment of infertility. You and your spouse should be assessed. Your doctor will obtain a complete medical history and do a physical examination.
Fertility testing may include:
Ovulation tests: An at-home, over-the-counter ovulation prediction test detects the rise in luteinizing hormone (LH) that happens before to ovulation. A blood test for progesterone, a hormone generated during ovulation, can also confirm if you’re ovulating. Other hormone levels, such as prolactin, may be tested.
Hysterosalpingography: Hysterosalpingography (his-tur-o-sal-ping-GOG-ruh-fee) involves injecting X-ray contrast into your uterus and taking an X-ray to look for issues within the uterus. The test also determines if the fluid exits the uterus and pours out of your fallopian tubes. If any issues are discovered, you will most certainly require additional assessment.
Ovarian reserve testing: This test helps to assess the quality and amount of eggs accessible for ovulation. Women who are at risk of having a decreased egg supply, especially those over the age of 35, may undergo this battery of blood and imaging tests.
Other hormone tests: Other hormone tests measure levels of ovulatory hormones, as well as thyroid and pituitary hormones, which regulate reproductive processes. If you’re seeking expert infertility treatment in Jaipur, Dr. Mamta Mehta is a leading specialist renowned for her compassionate care and advanced techniques. Her clinic offers state-of-the-art solutions tailored to each patient’s unique needs, ensuring the best possible outcomes.
Imaging testing: A pelvic ultrasound detects uterine or fallopian tube illness. A sonohysterogram, also known as a saline infusion sonogram or hysteroscopy, may be used to reveal things inside the uterus that a standard ultrasound cannot.
2 notes
·
View notes
Text
The Comprehensive Compilation of Adverse Reactions Associated with Cabergoline 0.25mg
Cabergoline 0.25mg is a frequently given prescription for many medical disorders. However, it is important for users to be aware of the possible negative effects that may accompany its usage, as is the case with any pharmaceutical. This page provides an extensive list of side effects linked to Cabergoline 0.25mg, including both typical responses and more severe cautions and long-term concerns. Through comprehending these adverse consequences and acquiring the knowledge to handle them, people may make well-informed choices about their therapy and overall state of health.
Cabergoline is a medication used to treat medical conditions such as hyperprolactinemia and Parkinson's disease
Cabergoline is a pharmaceutical compound classified as a dopamine agonist. It is often used in the treatment of disorders such as hyperprolactinemia, which may result in complications such as infertility, irregular menstruation, and lactation in both males and females.
Medical uses of Cabergoline 0.25mg
Cabergoline 0.25mg is often used for the treatment of hyperprolactinemia, a medical disorder defined by elevated levels of prolactin in the bloodstream. This medicine effectively reduces prolactin levels and effectively manages symptoms such as infertility, decreased libido, and irregular menstruation.
Adverse effects on the digestive system
Typical gastrointestinal adverse effects of Cabergoline 0.25mg may include nausea, emesis, constipation, and stomach discomfort. To reduce side effects, it is crucial to consume this drug with meals.
Neurological Adverse Reactions
Individuals using Cabergoline 0.25mg may encounter symptoms such as vertigo, somnolence, or cephalalgia. It is recommended to refrain from driving or operating heavy equipment until you are aware of the impact of this drug on your abilities.
Adverse effects on the cardiovascular system
Certain people may encounter alterations in blood pressure or heart rate while consuming Cabergoline 0.25mg. Regularly monitoring these measures and promptly reporting any major changes to your healthcare professional is essential.
Cabergoline 0.25mg is used to treat a variety of illnesses that arise from excessive production of the hormone prolactin. It may be used to treat pituitary prolactinomas, which are tumors of the pituitary gland, as well as certain menstruation issues and issues with fertility in both sexes.
Possible cardiac valve impairment
An important concern connected with Cabergoline is the possibility of cardiac valve injury, especially in those who are prescribed greater dosages for a prolonged duration. Consistent monitoring of the heart is crucial in order to promptly identify any anomalies in the valves.
Potential for Fibrotic Reactions
The use of Cabergoline has been associated with the emergence of fibrotic responses in diverse tissues, such as the cardiac, pulmonary, and abdominal tissues. If you encounter symptoms such as respiratory distress or edema in the limbs, it is advisable to promptly seek medical assistance.
Potential for the Development of Tolerance
Prolonged usage of Cabergoline might result in the development of tolerance, necessitating greater dosages to get the same therapeutic outcome. It is essential to adhere to the recommendations of your healthcare practitioner and refrain from altering your dose without seeking their advice.
Effect on Hepatic Function
Cabergoline has the potential to impact liver function in some people, resulting in increased levels of liver enzymes. It is advisable to undergo regular liver function tests while taking this drug in order to monitor any changes and avoid any problems.
Controlling and Reducing Side Effects
If you are encountering adverse reactions as a result of consuming Cabergoline 0.25mg, do not worry; there are strategies to address them. Here is a method to effectively control and reduce undesired consequences.
Titration and Surveillance of Dosage
Seek guidance from your healthcare professional about the possibility of modifying your Cabergoline dose. Regular surveillance may aid in monitoring the body's response to the medicine.
Implementing lifestyle modifications to mitigate adverse effects
Modest lifestyle adjustments may significantly alleviate adverse effects. To promote your general well-being, it is important to ensure that you stay well hydrated, follow a balanced diet, and make regular exercise a priority.
Drug Interactions
It is essential to be aware of the potential interactions between Cabergoline and other drugs for your safety and well-being. Now, let's explore the possible interactions and contraindications that need to be monitored.
Important Drug Interactions to Be Mindful Of
Cabergoline may have adverse interactions with some drugs. Ensure that you regularly update your healthcare practitioner about all the drugs you are currently taking in order to prevent any possible drug interactions.
Interactions with Specific Medications
Certain drugs should be avoided while using Cabergoline owing to the potential for adverse interactions. Take note of these contraindications to avoid any potential consequences.
Specific considerations for certain demographics
Customized strategies may be necessary for administering Cabergoline to various groups. Below are important factors to consider for pregnant or nursing women and geriatric patients.
Cabergoline is used to treat hyperprolactinemia (high levels of prolactin, a natural substance that helps breast-feeding women produce milk but can cause symptoms such as infertility, sexual problems, and bone loss in women who are not breast-feeding or men). Cabergoline is in a class of medications called dopamine receptor agonists. It works by decreasing the amount of prolactin in the body.
Women who are currently pregnant or breastfeeding
When you are pregnant or breastfeeding, it is crucial to have a conversation with your healthcare professional about the potential advantages and disadvantages of using Cabergoline. The utmost importance should be placed on ensuring the well-being of both you and your kid.
Geriatric Patients
Cabergoline may need special care for elderly people. Close surveillance and possible dose modifications may be required to guarantee the safety and efficacy of the medication.
Summary and Concluding Remarks
Understanding and addressing the possible side effects, interactions, and concerns of Cabergoline 0.25mg may seem challenging, but with enough information and help, you can successfully handle them. It is important to constantly seek advice from your healthcare professional for specialized assistance that is specifically targeted to your individual requirements.
Ultimately, it is essential for both patients and healthcare practitioners to have a thorough understanding of the potential adverse effects of Cabergoline 0.25mg. By being knowledgeable about the possible hazards, closely monitoring for any worrisome symptoms, and seeking advice from a healthcare expert as necessary, people may manage their course of treatment with more assurance and security. It is important to emphasize that taking a proactive approach to managing and maintaining open lines of communication are crucial in achieving the most favorable results while using Cabergoline 0.25mg.
1 note
·
View note
Text
How Does Homeopathy Helps in PCOD/PCOS ?
WHAT IS PCOD/PCOS?
PCOD (Polycystic ovarian disease) or PCOS (Polycystic ovarian syndrome) is a hormonal disorder that affects approximately10- 15% of all women, which are very commonly found in day-to-day practice and increasing nowadays. It interferes with their fertility during the reproductive years. There are multiple (‘poly’) cysts (small sacs filled with fluid) in the ovaries, on either side or both sides.
WHAT CAUSES PCOD?
PCOD is caused by hormonal imbalance i.e. altered hormones.
1) Raised level of Testosterone:
A higher level of male hormone (Androgen Hormone). Normally androgen hormone is present in small amounts, but if the level increases then it leads to restricting the ovaries from releasing an egg (ovulation) during each menstrual cycle.
2) A higher level of LH Hormone: –
A higher level of Luteinizing Hormone disturbs the ovulation during the menstrual cycle.
3) Raised level of Prolactin:-
Prolactin levels of between 30 ng/mL and 200 ng/mL are considered moderately high. This level of prolactin in the blood can have many causes. Conditions related to raised levels of prolactin include pituitary disorders.
4) A higher level of Insulin: –
The excess level of insulin affects the ovaries by increasing androgen hormone thus affecting ovulation.
SYMPTOMS :
SymptomsOther signs includeIrregular menses or No mensesHair fallExcess hair on face, Chest, Stomach.DepressionHair ThinningAnxietyWeight GainDifficulty in getting pregnantAcneMood swings
HOMEOPATHY TREATMENT FOR PCOD/PCOS :
Homeopathy works on regulating hormonal imbalance, regularizing ovulation as well as maintaining a normal menstrual cycle. Homeopathy helps to treat other signs and symptoms also.
Homeopathy treatment varies from patient to patient. Homeopathic treatment is based on the extent of the problem, physiological and mental health of the patient. Homeopathic treatment is a holistic treatment. Dr. Vaseem Choudhary studies both the mental and physical condition of patients before giving any medicine. In PCOS there is careful observation of symptoms and regular follow up.
WHY HOMEO CARE CLINIC ??
Dr. Vaseem Choudhary has been treating PCOS with homeopathy treatment for many years. Dr. Vaseem Choudhary is a well-known homeopathy doctor in Pune. His treatment is safe and doesn’t have any adverse effects on the patient. Homeopathy treatment for PCOS varies from patient to patient. Patients with PCOD may experience some complications like Difficulty in getting pregnant (Infertility) and another bleeding from the uterus can be successfully treated with Homeopathy.
A complete approach at Homeo Care Clinic is harmless. So, it’s very easy to completely get rid of the side effects of conventional medication, as homeopathy treats the root cause and thereby regulate hormonal imbalance and treats PCOS.
#homeopathicdoctor#pune#pcodtreatment#homeopathyworks#homeocareclinic in hadapsar#best tablet for pcod
2 notes
·
View notes
Text
Prolactin Hormone Q Badhta Hai
Many people often wonder – Prolactin Hormone Q Badhta Hai? Prolactin is a hormone mainly responsible for milk production in women. However, when its levels rise abnormally, it can lead to symptoms like irregular periods, infertility, or unexpected breast discharge in both men and women. Prolactin Hormone Q Badhta Hai – this can happen due to stress, thyroid issues, certain medications, or a brain tumor known as prolactinoma. If you’re experiencing such symptoms, it’s important to get tested
0 notes
Text
Ovulation Induction Treatment in Gachibowli | Hyderabad - Dr Sravya Buggana
Ovulation Induction Treatment in Gachibowli, Hyderabad – Expert Fertility Support by Dr. Sravya Buggana
If you're looking for expert Ovulation Induction Treatment in Gachibowli, Hyderabad, Dr. Sravya Buggana offers personalized, evidence-based solutions to help you conceive naturally or with assisted reproductive support. Ovulation issues are one of the most common causes of female infertility, and timely medical intervention can make a life-changing difference. At her clinic in Gachibowli, Dr. Sravya combines advanced diagnostics with compassionate care to improve your chances of successful ovulation and conception.
What is Ovulation Induction?
Ovulation induction is a fertility treatment that uses medications to stimulate the ovaries to release one or more eggs during the menstrual cycle. It is often recommended for women who do not ovulate regularly or at all, such as those with:
Polycystic Ovary Syndrome (PCOS)
Irregular menstrual cycles
Anovulation (absence of ovulation)
Hormonal imbalances
Women seeking Ovulation Induction Treatment in Gachibowli, Hyderabad often start with this non-invasive method to restore ovulation and improve fertility outcomes.
Why Choose Dr. Sravya Buggana?
Dr. Sravya Buggana is a leading fertility specialist and reproductive psychologist offering complete care for couples and individuals experiencing infertility. Known for her ethical and holistic approach, Dr. Sravya has helped hundreds of women overcome ovulatory disorders through customized treatment plans.
Here’s why she’s the trusted choice for Ovulation Induction Treatment in Gachibowli, Hyderabad:
✅ Expertise in Hormonal Management
Dr. Sravya accurately diagnoses the root cause of ovulation issues using hormonal profiling, ultrasound, and cycle tracking to deliver optimal outcomes.
✅ Personalized Protocols
Not all bodies respond the same way to medications. Dr. Sravya customizes dosage, duration, and monitoring based on your medical history and response.
✅ Combination with Lifestyle Support
For women with PCOS or metabolic disorders, she offers dietary, lifestyle, and mental health guidance in conjunction with medical therapy.
✅ Advanced Monitoring Techniques
Her clinic provides advanced cycle monitoring with regular ultrasounds and hormone testing to ensure timely and safe ovulation.
✅ Transparent Communication
Patients receive detailed information on every stage of the process, from medication choices to timing of intercourse or IUI.
These attributes make her clinic a top destination for Ovulation Induction Treatment in Gachibowli, Hyderabad.
How Does the Treatment Work?
The goal of ovulation induction is to help you ovulate in a predictable and healthy way, so you can conceive naturally or through procedures like IUI (Intrauterine Insemination).
Here’s a step-by-step breakdown:
Initial Evaluation Includes pelvic ultrasound, hormone blood tests (FSH, LH, AMH, TSH, prolactin), and partner semen analysis.
Ovulation Induction Medications Clomiphene Citrate, Letrozole, or Gonadotropins are prescribed to stimulate egg development.
Cycle Monitoring Frequent scans and hormonal assessments are done to track follicle growth and determine ovulation timing.
Timed Intercourse or IUI Based on follicular response, couples are advised on the optimal time for intercourse or scheduled for IUI.
Follow-Up A luteal phase scan and beta-hCG blood test are done to confirm ovulation and check for early pregnancy.
Patients undergoing Ovulation Induction Treatment in Gachibowli, Hyderabad with Dr. Sravya appreciate the combination of medical precision and human warmth at every step.
Who is a Candidate?
Ovulation induction may be right for you if:
You have irregular or absent periods
You’ve been diagnosed with PCOS
You’re under 35 and trying to conceive for over 12 months
You’re over 35 and trying for more than 6 months
Your hormone levels indicate anovulation
The treatment is often the first step in a fertility journey and may eliminate the need for IVF in many cases.
Success Rates and Expectations
Success depends on several factors including age, ovarian reserve, and underlying conditions. However, most women who undergo Ovulation Induction Treatment in Gachibowli, Hyderabad see improvement in cycle regularity and ovulation within 1–3 cycles.
Dr. Sravya’s patients report high satisfaction and improved fertility outcomes thanks to her meticulous care and timely interventions.
Why Gachibowli?
Gachibowli is a major medical and IT hub in Hyderabad, making it a convenient location for working professionals seeking quality fertility care. Dr. Sravya Buggana’s clinic offers flexible appointment slots, affordable packages, and minimal wait times—ideal for those juggling work and personal life.
Whether you’re at the beginning of your fertility journey or exploring your next step, you’ll find excellent Ovulation Induction Treatment in Gachibowli, Hyderabad here.
Book Your Consultation Today
Don’t let irregular cycles or ovulation disorders stand in the way of your dreams. Take control of your fertility with expert Ovulation Induction Treatment in Gachibowli, Hyderabad under the care of Dr. Sravya Buggana.
0 notes
Text
Struggling with Irregular Periods or Hormonal Imbalance? Here's How Dr. Seema Jain Best Gynac in Ravet Diagnoses PCOD and PCOS
Understanding the Basics: What Are PCOD and PCOS?
PCOD (Polycystic Ovarian Disease) and PCOS (Polycystic Ovary Syndrome) are hormone-related conditions that impact women’s reproductive health. While both share overlapping symptoms like irregular periods, acne, and weight gain, PCOS is a more severe metabolic disorder with long-term implications on fertility and health.
These conditions have become increasingly common among urban women. Stress, lifestyle, and dietary habits play a major role in their development. Understanding them deeply is the first step toward effective diagnosis and treatment.
How Do PCOD and PCOS Differ?
While often used interchangeably, PCOD and PCOS are not the same. PCOD (Polycystic Ovarian Disease) is primarily a result of ovarian dysfunction, where the ovaries release immature or partially mature eggs, leading to hormonal imbalance. Ovulation in PCOD is often delayed, but not completely absent, and the impact on fertility is generally less severe.
In contrast, PCOS (Polycystic Ovary Syndrome) is a more complex endocrine and metabolic disorder that can affect ovulation more significantly, often causing it to stop altogether. This makes PCOS more impactful on fertility. While both conditions require medical attention, PCOD can often be managed with simple lifestyle changes and medications.
PCOS, however, usually demands a more long-term, hormonal approach to management, especially when fertility is a concern. If you’re confused about your symptoms, consulting a Fertility Specialist in Ravet, such as Dr. Seema Jain, can help distinguish between the two with clarity and compassion.
Why Timely Diagnosis Matters
PCOD/PCOS, if left undiagnosed, can lead to:
Infertility or Difficulty Conceiving
Insulin Resistance and Diabetes
High Blood Pressure and Heart Problems
Mental Health Issues Like Anxiety And Depression
This is why Dr. Seema Jain always says, “Early diagnosis isn’t just medical—it’s empowering.” Women often spend years struggling with unexplained symptoms before seeking help. But the sooner you act, the more you control your outcome.
Step-by-Step Guide to Diagnosing PCOD and PCOS
Detailed Medical History & Symptom Review
Dr. Seema Jain begins with understanding your cycle history, lifestyle, family history, skin/hair changes, and weight fluctuations.
Physical Examination
Checking for signs like excessive facial hair, acne, scalp hair thinning, and abdominal fat distribution.
Ultrasound Scan (Pelvic)
Transvaginal or abdominal ultrasound to check for enlarged ovaries and the presence of multiple follicles.
Hormonal Blood Tests
To measure:
AMH (Anti-Müllerian Hormone)
LH & FSH ratio
Testosterone and DHEA
TSH (thyroid function)
Prolactin
Fasting insulin and glucose levels
These tests are often done on Day 2 or Day 3 of the menstrual cycle.
Additional Metabolic Screenings
If PCOS is suspected, additional screenings may include:
Lipid profile
HbA1c for blood sugar control
Blood pressure monitoring
The goal is to not just confirm a diagnosis, but to map a treatment that supports fertility, metabolism, and mental wellbeing.
Role of a Fertility Specialist in Managing PCOD/PCOS
Diagnosis is only the beginning. What you truly need is a fertility specialist who listens, customizes, and walks with you through this. That’s where Dr. Seema Jain, Fertility Specialist in Ravet, comes in. With over 30 years of experience, she focuses on simple, sustainable solutions. Her approach includes:
Personalized Lifestyle Corrections
Realistic Fertility Planning
Minimal Interventions Wherever Possible
Avoiding unnecessary tests or medication
When Should You See Dr. Seema Jain, Fertility Specialist in Ravet?
Don’t wait until things get complicated. Book a consultation if you:
Have Irregular Or Missed Periods
Experience Unexplained Weight Gain
Are Dealing With Acne, Facial Hair, Or Hair Thinning
Feel Emotionally Drained By Your Symptoms
Are Trying To Conceive Without Success For 6–12 Months
You Deserve a Diagnosis That Makes Sense—And Care That Feels Human.

0 notes
Text
Role of Hormonal Imbalance in Female Infertility in Urban India

In today’s fast-paced urban lifestyle, health challenges are on the rise—especially when it comes to fertility. One of the most common yet often overlooked causes of infertility among women in India’s metropolitan cities is hormonal imbalance. With more women delaying childbirth due to career and personal choices, understanding hormonal health has become more important than ever.
If you are struggling with conception, the best female infertility treatment in Delhi can offer both advanced diagnosis and personalized care.
What Is Hormonal Imbalance?
Hormonal imbalance occurs when there is too much or too little of a hormone in the bloodstream. Even a small change can disrupt reproductive health. For women trying to conceive, this imbalance can interfere with:
Ovulation
Menstrual cycle
Egg quality
Implantation of the embryo
Common Hormonal Conditions Linked to Infertility
🔸 Polycystic Ovary Syndrome (PCOS)
PCOS is one of the leading causes of infertility. It disrupts ovulation and causes irregular periods, acne, and weight gain.
🔸 Thyroid Disorders
Both hyperthyroidism and hypothyroidism can affect the menstrual cycle and ovulation.
🔸 High Prolactin Levels
Prolactin is the hormone that helps in breast milk production. When it's too high, it can stop ovulation.
🔸 Low Progesterone
Progesterone prepares the uterus for pregnancy. Low levels can lead to failed implantation or early miscarriage.
If you're experiencing any of these issues, seeking the best female fertility in Delhi is the first step toward finding a solution.
Causes of Hormonal Imbalance in Urban Women
The urban lifestyle is often stressful and sedentary, contributing to hormonal fluctuations. Common triggers include:
High stress levels
Poor diet
Lack of physical activity
Exposure to pollution and endocrine-disrupting chemicals
Irregular sleep patterns
These factors collectively affect the body’s natural hormonal rhythm, making it harder to conceive.
Treatment Options Available
When you choose the best female infertility treatment in Delhi, a thorough evaluation will be conducted, including:
Hormonal blood tests
Ultrasound scans
Lifestyle assessment
Personalized fertility treatment
Depending on the diagnosis, treatments may include:
Hormone therapy
Lifestyle modifications
Ovulation induction medications
IVF or IUI (for severe cases)
Why Delhi is a Hub for Female Fertility Treatment
Delhi is home to some of India’s most reputed fertility specialists and modern clinics. Many offer:
State-of-the-art labs
Highly experienced doctors
World-class patient care
Affordable treatment plans
Whether you're facing PCOS, thyroid issues, or unexplained hormonal disorders, the best female fertility in Delhi can offer you a clear path to parenthood.
Conclusion
Hormonal imbalance is a silent disruptor of fertility, especially in the fast-paced lives of urban women. However, with the right medical support and timely intervention, it is manageable. If you or a loved one is facing challenges in conceiving, consult the experts offering the best female infertility treatment in Delhi. With proper care and guidance, motherhood is within reach.
#Best female infertility treatment in Delhi#Hormonal imbalance and infertility in women#Female infertility specialist in Delhi#Female hormonal infertility treatment Delhi#Best fertility clinic for women in Delhi#Infertility due to PCOS Delhi#Female hormone testing in Delhi#Women's fertility treatment in Delhi#Top fertility doctor in Delhi for female infertility#Hormonal imbalance fertility treatment Delhi#Female reproductive health specialist Delhi#Best gynecologist for infertility in Delhi#Causes of infertility in women Delhi#Advanced female infertility treatment Delhi
0 notes
Text
Affordable Hormonal Assay Test in Indore with Quick Turnaround Time
Hormonal balance is key to good health. From thyroid regulation to fertility, energy levels, and mental well-being—hormones play a pivotal role in our lives. At Ultrascan Diagnostics, we offer affordable hormonal assay tests in Indore with quick turnaround times to help patients make informed decisions swiftly and accurately. As one of the best diagnostic centres in Indore, Ultrascan prioritizes accuracy, speed, and patient comfort. Our lab uses advanced technology to provide timely and reliable results across a wide range of hormonal tests.
What is a Hormonal Assay Test?
A hormonal assay test measures specific hormone levels in your blood, saliva, or urine. These tests are critical for diagnosing and monitoring conditions like:
Thyroid disorders
PCOD/PCOS
Infertility issues
Adrenal gland problems
Menopause-related changes
Growth abnormalities
Diabetes (Insulin levels)
At Ultrascan Diagnostics, we offer a comprehensive range of hormone tests tailored to your medical needs.
Why Choose Ultrascan Diagnostics in Indore?
At Ultrascan Diagnostics, your health is our priority. Here’s why we’re a trusted name for health scan diagnostics in Indore:
NABL-Accredited Lab
We maintain the highest quality standards with fully certified lab technicians and equipment.
Quick Report Turnaround
Most hormonal test results are available within 24–48 hours, helping you begin treatment faster.
Affordable Pricing
We offer cost-effective packages without compromising on accuracy or quality.
Expert Consultation
Discuss your report with in-house consultants for better understanding and medical direction.
Advanced Diagnostic Equipment
We use state-of-the-art analyzers that reduce false positives and ensure precise measurements.
Types of Hormonal Assay Tests Available
At Ultrascan Diagnostics, we conduct a wide range of hormonal tests, including:
1. Thyroid Profile (T3, T4, TSH)
Detects overactive or underactive thyroid gland.
2. Female Hormone Panel
FSH (Follicle Stimulating Hormone)
LH (Luteinizing Hormone)
Estrogen
Progesterone
Prolactin
3. Male Hormone Panel
Testosterone
DHEA
FSH & LH
4. Adrenal Function Test
Cortisol (AM/PM)
ACTH (Adrenocorticotropic Hormone)
5. Insulin & Glucose Tests
Assesses diabetes risk and insulin resistance.
Frequently Asked Questions
Q1: What is a hormonal assay test and why is it important?
A hormonal assay test evaluates the concentration of hormones in the body to detect imbalances. It helps diagnose issues like thyroid dysfunction, fertility problems, or stress disorders. Early detection enables faster treatment and better health outcomes.
Q2: How long do hormonal assay test results take at Ultrascan Diagnostics?
At Ultrascan Diagnostics, most hormonal test results are delivered within 24 to 48 hours, ensuring timely diagnosis and medical intervention. Urgent cases may be prioritized based on request.
Q3: Is fasting necessary before taking a hormonal test?
Fasting is required for certain tests like insulin or early morning cortisol. However, it’s not mandatory for all hormone panels. Our staff will guide you about test-specific preparation at the time of booking.
Conclusion
Don’t let hormonal imbalance affect your health or lifestyle. At Ultrascan Diagnostics, we combine affordability, accuracy, and prompt reporting to offer the best hormonal testing experience in Indore. Call Now to Book Your test. Take control of your health with Ultrascan – The Best Diagnostic Centre in Indore for Hormonal Assay Tests and Health Scan Diagnostics.
0 notes
Text
Can You Conceive When Your Periods Have Stopped? Insights from Dr. Hima Deepthi V.
If your periods have stopped and you’re worried about fertility, you're not alone—and there are still paths to conception. In this video, Dr. Hima Deepthi V, a respected fertility specialist at Nova IVF Fertility in Banjara Hills, explains what’s happening and the options available.
What’s Going On When Menstruation Stops?
Possible Causes
Premature ovarian insufficiency (early menopause)
Polycystic ovary syndrome (PCOS)
Extreme stress, weight changes, or intense exercise
Hormonal imbalances or medical conditions Dr. Deepthi emphasizes the importance of identifying the root cause to guide effective treatment.
Does it Always Mean Infertility? Not always. While a lack of menstruation often indicates irregular ovulation, with thorough evaluation and targeted interventions, many women can still conceive.
How Dr. Deepthi Approaches Treatment
1. Thorough Diagnostic Workup
Blood tests for hormone levels (FSH, LH, AMH, thyroid, prolactin)
Pelvic ultrasound to assess ovarian and uterine health
Reviewing history of illnesses, medications, lifestyle factors
2. Personalized Treatment Plans
Depending on the diagnosis, possible treatments include:
Ovulation induction using drugs like clomiphene citrate or letrozole
Hormonal therapy to restore menstrual cycles (e.g. estrogen, progesterone)
Assisted reproductive technologies such as IUI or IVF if needed
3. Supportive Lifestyle Advice
Nutrition counseling to reach a healthy weight
Stress reduction techniques (yoga, meditation)
Exercise moderation—find a balance to support ovulation
4. Ongoing Monitoring
Regular follow-ups to adjust medication doses
Tracking cycles and follicle development
Decision point on whether to escalate to ART based on response
Hope for Conceiving After Menstrual Cessation
Dr. Deepthi reassures that while absence of periods can be concerning, it doesn’t necessarily rule out pregnancy. With proper diagnosis and personalized intervention, many women regain cycles and achieve successful pregnancies—even if assisted reproductive methods become necessary.
Key Takeaways
Stopped periods ≠ permanent infertility
Diagnosing the cause is essential
Treatment options range from medication to IVF
Lifestyle factors play a crucial supportive role
Consistent monitoring ensures timely adjustments
Want to Take the Next Step?
If you’re facing this concern, consider consulting a qualified fertility specialist like Dr. Hima Deepthi V. A proper evaluation can open the door to treatment options and bring hope for conception.
0 notes
Text
Thyroid Disorders: Their Impact on Infertility and Pregnancy – Insights from a Gynecologist in Kalyani Nagar
The thyroid gland, though small in size, plays a massive role in regulating several bodily functions, especially in women’s reproductive health. Thyroid disorders, whether hyperthyroidism (overactive thyroid) or hypothyroidism (underactive thyroid), can significantly affect a woman's ability to conceive and sustain a healthy pregnancy. For couples trying to conceive or expecting a baby, understanding the link between thyroid health, infertility, and pregnancy is crucial. Consulting a qualified gynecologist in Kalyani Nagar can make a meaningful difference in diagnosis and treatment.

How Thyroid Function Affects Fertility
Thyroid hormones influence the menstrual cycle, ovulation, and even implantation. An imbalance in these hormones can disrupt these processes and lead to infertility. Here’s how:
Menstrual Irregularities Hypothyroidism can cause irregular periods or even amenorrhea (absence of menstruation), which can lead to difficulty tracking ovulation or conceiving. Conversely, hyperthyroidism may lead to lighter or shorter cycles.
Anovulation One of the most common ways thyroid disorders cause infertility is by disrupting ovulation. Without regular ovulation, the chances of natural conception decrease significantly.
Hormonal Imbalance Thyroid dysfunction can also alter levels of prolactin, a hormone that, when elevated, may inhibit ovulation. Furthermore, thyroid hormones interact with estrogen and progesterone, further affecting the reproductive cycle.
A comprehensive thyroid panel test can help determine if thyroid dysfunction is the root cause of infertility. A gynecologist in Kalyani Nagar will guide you through the appropriate testing and interpret results with precision.
Thyroid Health and Pregnancy
Thyroid hormones are critical during pregnancy—not only for the mother but also for the developing baby, especially in the first trimester when the fetus is entirely dependent on the mother's thyroid hormone supply.
Increased Risk of Miscarriage Untreated hypothyroidism has been associated with a higher risk of early miscarriage. This is why thyroid function should ideally be assessed before conception or in the early weeks of pregnancy.
Preterm Birth and Low Birth Weight Uncontrolled thyroid disorders can lead to complications such as preterm labor, low birth weight, and developmental issues in the baby.
Preeclampsia Hypothyroidism can increase the risk of preeclampsia—a condition characterized by high blood pressure during pregnancy, which can be life-threatening if not properly managed.
Developmental Delays in Children Inadequate maternal thyroid hormone levels, especially in the first trimester, can lead to delays in cognitive development in the child.
A gynecologist in Kalyani Nagar will typically monitor thyroid levels closely during pregnancy and adjust medication as needed to ensure both maternal and fetal health.
Treatment and Management
Managing thyroid-related infertility and ensuring a healthy pregnancy typically involve:
Medication: Hypothyroidism is often treated with levothyroxine, a synthetic thyroid hormone. Hyperthyroidism may require anti-thyroid drugs, beta-blockers, or in some cases, surgery.
Regular Monitoring: Thyroid function should be checked every 4–6 weeks during pregnancy, or more frequently if advised by your gynecologist.
Lifestyle Modifications: Adequate nutrition, stress management, and regular physical activity can support thyroid health and overall reproductive well-being.
When to See a Gynecologist in Kalyani Nagar
If you’ve been trying to conceive for several months without success or are experiencing symptoms such as fatigue, weight changes, irregular periods, or anxiety, it might be time to consult a gynecologist in Kalyani Nagar. These symptoms may indicate a thyroid issue that, if addressed, can improve your fertility outcomes and ensure a healthier pregnancy.
Conclusion
Thyroid disorders are a common but often overlooked cause of infertility and pregnancy complications. Fortunately, with early diagnosis and expert medical care, most thyroid-related reproductive issues can be effectively managed. Women in and around Pune should consider consulting a trusted gynecologist in Kalyani Nagar to get personalized guidance, timely diagnosis, and supportive care for all fertility and pregnancy-related concerns.
Don’t let thyroid issues stand in the way of your dreams of parenthood—take the first step toward clarity and care today.
0 notes
Text
Female Infertility in Pimpri-Chinchwad – Causes, Diagnosis & Treatment at Pune IVF
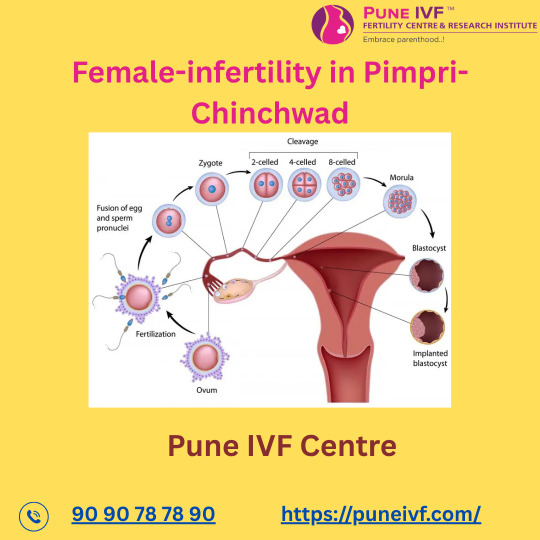
Infertility can be a challenging and emotional experience for many women. If you're struggling to conceive and are looking for expert help, Pune IVF offers compassionate and advanced care for female infertility in Pimpri-Chinchwad. With state-of-the-art technology and experienced fertility specialists, we provide individualized treatment plans that increase your chances of conception and help you achieve your dream of parenthood.
What is Female Infertility?
Female infertility refers to a woman's inability to get pregnant after 12 months of regular, unprotected intercourse. It may be caused by a variety of physical, hormonal, or lifestyle-related factors. At Pune IVF, we understand that every woman's fertility journey is unique, which is why we take a holistic and personalized approach to identify and treat the root cause of infertility.
Common Causes of Female Infertility
Understanding the underlying cause of infertility is the first step toward successful treatment. Some of the most common causes include:
1. Ovulation Disorders
Problems with ovulation are among the most frequent causes of female infertility. Conditions such as Polycystic Ovary Syndrome (PCOS), thyroid disorders, and hormonal imbalances can interfere with ovulation, making it difficult to conceive.
2. Fallopian Tube Blockage
Blocked or damaged fallopian tubes can prevent the egg from reaching the uterus. This can result from infections, pelvic inflammatory disease (PID), or previous surgeries.
3. Endometriosis
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, causing inflammation, pain, and potential infertility.
4. Uterine or Cervical Abnormalities
Conditions such as fibroids, polyps, or structural abnormalities in the uterus can interfere with implantation or increase the risk of miscarriage.
5. Age-Related Factors
Female fertility naturally declines with age, especially after 35. The number and quality of eggs decrease, making conception more challenging.
6. Lifestyle Factors
Poor nutrition, stress, smoking, alcohol use, and being underweight or overweight can all affect fertility.
Signs & Symptoms of Female Infertility
Many women may not experience any obvious symptoms until they try to conceive. However, some signs that may indicate an underlying fertility issue include:
Irregular or absent menstrual cycles
Painful periods or pelvic pain
Unexplained weight gain
Acne or excessive hair growth (hirsutism)
History of miscarriages
Difficulty conceiving after a year of regular intercourse
If you're experiencing any of these symptoms, it's important to consult a fertility specialist in Pimpri-Chinchwad at the earliest.
Female Infertility Diagnosis at Pune IVF
At Pune IVF, we offer comprehensive diagnostic services to determine the exact cause of female infertility. Our evaluation process includes:
Hormonal blood tests to check for thyroid, prolactin, and reproductive hormone levels.
Ultrasound scans to assess the ovaries, uterus, and endometrial lining.
Ovulation tracking to confirm if and when ovulation is occurring.
Hysterosalpingography (HSG) to check for blocked fallopian tubes.
Laparoscopy or hysteroscopy, if needed, to investigate uterine or pelvic conditions.
Our advanced lab facilities and experienced team ensure accurate diagnosis and a clear plan for treatment.
Female Infertility Treatment Options in Pimpri-Chinchwad
Once the cause is identified, a suitable treatment plan is created. At Pune IVF, we offer a wide range of fertility treatments:
1. Ovulation Induction
Medications such as Clomiphene Citrate or Letrozole are used to stimulate ovulation in women with irregular or absent periods.
2. Intrauterine Insemination (IUI)
Sperm is directly placed into the uterus during the fertile window, increasing the chance of fertilization.
3. In Vitro Fertilization (IVF)
A highly effective procedure where eggs are fertilized outside the body and the resulting embryo is transferred into the uterus.
4. Intracytoplasmic Sperm Injection (ICSI)
ICSI is recommended in cases of male factor infertility or repeated IVF failures. A single sperm is injected directly into an egg.
5. Surgical Treatments
Minimally invasive surgeries like laparoscopy may be performed to treat endometriosis, fibroids, or remove blockages.
6. Lifestyle Counseling
Nutritional guidance, weight management, and stress-reduction techniques are also part of our holistic approach to improving fertility.
Why Choose Pune IVF for Female Infertility in Pimpri-Chinchwad?
Experienced Specialists: Our team of fertility experts has years of experience in diagnosing and treating complex infertility cases.
Advanced Technology: We use cutting-edge technology and evidence-based protocols to ensure the highest success rates.
Personalized Care: Each patient receives a customized treatment plan tailored to their specific needs and medical history.
Supportive Environment: We understand the emotional aspects of infertility and offer counseling and emotional support at every stage.
Convenient Location: Located in the heart of Pimpri-Chinchwad, Pune IVF is easily accessible for patients across PCMC and Pune.
Take the First Step Toward Parenthood
If you're facing difficulties in conceiving, don't wait. Early diagnosis and treatment can make a significant difference. Pune IVF is here to support you with world-class care, advanced infertility treatments, and compassionate guidance every step of the way.
📞 Book your consultation today and begin your journey toward parenthood with confidence.
0 notes
Text
Conditions Commonly Treated by an Endocrinologist in Inner West
Your endocrine system regulates hormones that control metabolism, growth, stress response, and reproduction. When hormone levels go awry, you may experience fatigue, weight changes, mood swings, or serious organ dysfunction. Consulting an endocrinologist in Inner West ensures you receive expert diagnosis and tailored treatment plans to restore balance and optimise health.

Diabetes Mellitus
Types of Diabetes
Type 1 Diabetes: Autoimmune destruction of insulin-producing cells
Type 2 Diabetes: Insulin resistance often linked to lifestyle factors
Specialist Care
An endocrinologist in Inner West will perform glucose tolerance tests, monitor HbA1c levels, and design personalised insulin or medication regimens. Ongoing education on diet, exercise, and self-monitoring is also a core component of care.
Thyroid Disorders
Hypothyroidism vs. Hyperthyroidism
Hypothyroidism: Low thyroid hormone leads to fatigue, weight gain, and cold sensitivity
Hyperthyroidism: Excess thyroid hormone causes weight loss, anxiety, and palpitations
Diagnostic Approach
Blood tests for TSH, T3, and T4 levels, along with ultrasound imaging when needed, allow your endocrinologist in Inner West to pinpoint the cause and recommend therapies such as hormone replacement or antithyroid medications.
Osteoporosis and Bone Health
Understanding Bone Density Loss
Osteoporosis weakens bones, increasing fracture risk—especially in postmenopausal women.
Management Strategies
Bone density scans (DEXA) to assess fracture risk
Calcium and vitamin D supplementation
Bisphosphonates or other bone-strengthening drugs
Your endocrinologist will create a prevention and treatment plan that includes lifestyle advice and medication when appropriate.
Adrenal Gland Disorders
Common Adrenal Issues
Addison’s Disease: Insufficient cortisol production
Cushing’s Syndrome: Excess cortisol leading to weight gain and hypertension
Specialist Interventions
Through hormone assays and imaging, an endocrinologist diagnoses adrenal imbalances and provides hormone replacement or surgical referrals as needed.

Pituitary Gland Conditions
Pituitary Adenomas and Hormone Disorders
Tumours in the pituitary can disrupt growth hormone, prolactin, and other key hormones.
Diagnostic and Treatment Options
MRI scans to visualise pituitary structure
Medication or surgery to normalize hormone secretion
Working closely with neurosurgical teams, your endocrinologist in Inner West ensures comprehensive management.
Reproductive Endocrinology
PCOS and Menopause Management
Polycystic Ovary Syndrome (PCOS): Causes irregular periods, infertility, and metabolic issues
Menopause: Hormone changes leading to hot flushes, mood swings, and bone loss
Your endocrinologist in Inner West provides hormonal therapies, lifestyle guidance, and monitoring to ease symptoms and protect long-term health.
Calcium and Lipid Metabolism
Managing Mineral and Cholesterol Imbalances
Hyperparathyroidism: Excess parathyroid hormone can raise calcium levels
Dyslipidaemia: Abnormal cholesterol and triglyceride levels increase cardiovascular risk
Through bloodwork and genetic assessments, an endocrinologist in Inner West customises treatments including dietary counselling, medications, and monitoring to reduce complications.
Conclusion
Endocrine disorders can impact nearly every aspect of your health—from metabolism and bone strength to stress response and reproductive function. By understanding the range of conditions treated by an endocrinologist, you’re better equipped to recognise warning signs and seek specialised care early. With expert diagnostics, personalised treatment plans, and ongoing support, you can restore hormonal balance and improve long-term well-being. Don’t wait for symptoms to worsen—partner with a trusted local specialist to take control of your endocrine health today. Connect with us today to take the next step in managing your endocrine health.
0 notes
Text
How Hormonal Imbalance Affects Fertility in Women
Hormones play a vital role in regulating every aspect of a woman’s reproductive system—from ovulation and menstruation to successful conception. When these hormones fall out of balance, fertility challenges often arise.
In this blog post, we’ll explore:
What hormonal imbalance is and how it affects fertility
Key hormones involved in reproduction
Common conditions linked to hormonal disruptions
Signs to watch out for and when to seek help
Available treatments and how Trinity IVF Ahmedabad can support you
Understanding your hormonal health is a powerful first step toward overcoming infertility and planning a successful pregnancy.
What Is Hormonal Imbalance?
Hormonal imbalance occurs when there's too much or too little of a hormone in the bloodstream. Even minor fluctuations can significantly impact the menstrual cycle, ovulation, and your ability to conceive.
The female reproductive system is regulated by a delicate balance of hormones. When that balance is disrupted, it can affect egg production, uterine lining development, and embryo implantation.
Key Hormones That Impact Female Fertility
Understanding which hormones play essential roles in fertility can help you better grasp how imbalance affects your body.
1. Follicle-Stimulating Hormone (FSH)
Stimulates egg production in the ovaries.
High levels may indicate reduced ovarian reserve.
2. Luteinizing Hormone (LH)
Triggers ovulation.
An imbalance can result in irregular or absent ovulation.
3. Estrogen
Builds the uterine lining for embryo implantation.
Low levels can interfere with ovulation and menstruation.
4. Progesterone
Prepares the uterus for pregnancy after ovulation.
Low levels may result in implantation failure or miscarriage.
5. Prolactin
Elevated levels can suppress ovulation.
6. Thyroid Hormones
Hypothyroidism and hyperthyroidism can both affect menstrual cycles and fertility.
Explore more about female fertility care at Trinity IVF Ahmedabad.
Common Conditions Linked to Hormonal Imbalance
Hormonal imbalance isn’t a disease in itself—it’s often a symptom of an underlying condition. Below are some of the most common causes:
1. Polycystic Ovary Syndrome (PCOS)
One of the leading causes of female infertility.
Characterized by high androgen (male hormone) levels, irregular periods, and cystic ovaries.
2. Thyroid Disorders
Both underactive and overactive thyroids can disrupt the menstrual cycle.
3. Hyperprolactinemia
Caused by excess prolactin, often due to a benign pituitary tumor.
Leads to ovulatory dysfunction.
4. Premature Ovarian Failure (POF)
Early decline in ovarian function before age 40.
5. Adrenal Disorders
Affect cortisol and DHEA levels, interfering with other reproductive hormones.
Learn more about how fertility issues are diagnosed and treated at Trinity IVF.
Symptoms of Hormonal Imbalance in Women
Recognizing the signs of a hormone imbalance is crucial. Common symptoms include:
Irregular or missed periods
Excessive acne or facial hair
Unexplained weight gain or loss
Fatigue and mood swings
Hot flashes or night sweats
Low libido
Difficulty getting pregnant
If you notice one or more of these symptoms, consider speaking with a fertility specialist.
How Hormonal Imbalance Affects Fertility
Here’s how imbalanced hormones can make conception difficult:
🔹 Disrupted Ovulation
Hormonal irregularities can prevent eggs from being released regularly or at all.
🔹 Poor Egg Quality
Imbalances can impair the development and maturity of eggs.
🔹 Uterine Lining Issues
Without proper hormonal support, the lining may not be suitable for embryo implantation.
🔹 Luteal Phase Defect
Inadequate progesterone levels can shorten the post-ovulation phase, reducing chances of implantation.
Diagnosis and Testing
To detect a hormonal imbalance, your doctor may recommend:
Blood tests to measure FSH, LH, estrogen, progesterone, prolactin, and thyroid levels
Ultrasound scans to evaluate ovarian function and endometrial thickness
Lifestyle assessment to understand factors like stress and diet
Discover how Trinity IVF Ahmedabad customizes diagnostic tests based on each patient's unique fertility profile.
Treatment Options for Hormonal Imbalance
Depending on the underlying cause, fertility specialists may recommend the following:
✅ Medications
Clomiphene citrate or letrozole to induce ovulation
Metformin for insulin resistance in PCOS patients
Thyroid hormone replacement for hypothyroidism
✅ Lifestyle Changes
Weight management
Stress reduction
Diet rich in antioxidants and whole foods
✅ Hormone Therapy
Supplemental estrogen or progesterone to regulate menstrual cycles
✅ Assisted Reproductive Technologies (ART)
When hormonal therapies alone aren't enough, options like IVF can help. Trinity IVF Ahmedabad offers advanced treatment plans tailored to your hormone profile.
Final Thoughts: Take Control of Your Fertility
Hormonal imbalance is a common but treatable cause of infertility. With the right diagnosis, medical guidance, and lifestyle adjustments, many women go on to conceive and enjoy a healthy pregnancy.
If you're experiencing symptoms of hormonal imbalance or have been trying to conceive without success, don’t wait. Trinity IVF Ahmedabad’s expert team is here to support your journey with compassion, technology, and trusted care.
Ready to Get Started?
Book your consultation with Trinity IVF Ahmedabad today and take the first step toward restoring your hormonal health and achieving your dream of parenthood.
0 notes
Text
tbh ever since i got diagnosed with prolactinoma i been thinking about getting pregnant... just because of the infertility that this condition brought me... too much prolactin could've made me sterile... it's just i can't find the right person... and it's been years...
0 notes