#Pediatric Celiac Specialists
Explore tagged Tumblr posts
Text
Discover why early detection of celiac disease in children is crucial. Learn about symptoms, health benefits, and the role of healthcare professionals in ensuring your child's well-being.
#Celiac Disease#Children's Health#Pediatric Celiac Disease#Early Detection#Childhood Nutrition#Symptoms in Kids#Gluten Intolerance#Childhood Digestive Disorders#Best Gastro Surgeon Ahmedabad#Celiac Disease Specialists#Celiac Disease Doctors#Gastroenterologists in Ahmedabad#Pediatric Gastroenterologists#Gluten-Free Healthcare#Celiac Disease Diagnosis#Digestive Health Experts#Ahmedabad Celiac Disease Clinics#Gluten Intolerance Treatment#Celiac Disease Consultation#Gluten-Sensitive Physicians#Gluten-Free Diet Advice#Celiac Disease Testing#Top Gastroenterologists in Ahmedabad#Gluten-Free Healthcare Providers#Pediatric Celiac Specialists
0 notes
Text
I got a celiac diagnosis on Thursday after having unresolved GI issues for my entire life that pediatric specialists just labeled as “overweight.” The pediatric specialists (at UCLA nonetheless) told me I was anemic and then didn’t run any further diagnostics. And now, 20-some odd years later, I have confirmation with my celiac gene and extreme response to gluten!
My current doctor said it’s also still possible I go on to develop (or have already developed) Crohn’s Disease because of the damage that gluten has done to my gut! Wow! Fun!
Also my on/off lifelong butt and thigh rash is likely dermatitis herpetiformis from my autoimmune response to gluten. Which makes a lot of sense as it tended to clear up when I periodically went gluten free. Funny how that works.
Don’t get me wrong, I’m glad I have more information, but fuuuuuuck I was not really prepared for a celiac diagnosis. And because I’m so sensitive, my husband and I have to replace basically everything in our kitchen to avoid any cross contamination. I’m talking new pots & pans, silverware, knives, bakeware, Tupperware containers, baking sheets, glassware, cutting boards, and utensils—everything that’s scratched and can trap gluten, which is like 90% of our kitchenware. We can’t afford this shit so we’re going to have to put it on my credit cards.
If anyone is able to help out at all with the cost of making our kitchen celiac friendly and totally gluten free, my Venmo is linked at the bottom. I also have ko-fi and buymeacoffee but I haven’t started using them yet.
#in your face to all the shitty doctors and specialists I’ve seen throughout the years who have just written me off as a hypochondriac#celiac disease#celiac#disability#disabled#disabled and in need of assistance#olive blogs#mutual aid request#crowdfunding#disabled mutual aid#dermatitis herpetiformis#autoimmune
2 notes
·
View notes
Text
Comprehensive Pediatric Care in Madurai: Why Preethi Hospitals is the Best Choice
Introduction: Why Choosing the Right Pediatric Hospital Matters
Ensuring the health and well-being of children is a top priority for parents. Finding the best pediatric hospital involves considering the quality of care, medical expertise, and available facilities. In Madurai, a city known for its cultural richness, having a trusted healthcare provider that specializes in pediatric care is essential. This blog explores why Preethi Hospitals, Madurai, stands out as the premier choice for pediatric services.
Advanced Pediatric Healthcare Services
At Preethi Hospitals, Madurai, comprehensive pediatric care is more than just medical treatment; it encompasses holistic support tailored to the unique needs of every child. The hospital is equipped with cutting-edge technology and facilities designed specifically for pediatric patients, ensuring that young patients receive care in a child-friendly environment.
State-of-the-Art Neonatal Intensive Care Unit (NICU): Preethi Hospitals features a well-equipped NICU, offering specialized care for premature and critically ill newborns. The NICU is designed to provide advanced monitoring and treatment, ensuring the highest standards of safety and comfort for newborns who require specialized attention.
Pediatric Intensive Care Unit (PICU): The Pediatric Intensive Care Unit at Preethi Hospitals is staffed with highly trained pediatric specialists and nurses, ensuring that children who need critical care receive timely and effective treatment. The PICU is equipped with modern technology to manage complex pediatric emergencies, providing parents with peace of mind during difficult times.
Comprehensive Pediatric Specialties
Preethi Hospitals, Madurai, offers a wide range of pediatric specialties to cater to various health needs. Whether it's general pediatrics, pediatric surgery, or specialized care for chronic conditions, the hospital is a one-stop destination for all pediatric health services.
Pediatric Cardiology: Children with congenital or acquired heart conditions require specialized attention. Preethi Hospitals’ pediatric cardiology services provide thorough assessments, diagnostic procedures, and treatments tailored to each child's needs, utilizing modern diagnostic tools for precise care.
Pediatric Gastroenterology: Digestive health in children often requires specialized treatment approaches. The hospital’s pediatric gastroenterology department focuses on managing and treating conditions like celiac disease, chronic abdominal pain, and other gastrointestinal issues in children, with a focus on comfort and minimal discomfort during procedures.
Child-Centric Approach and Comfort
Preethi Hospitals, Madurai, adopts a child-centric approach that prioritizes the emotional and psychological well-being of young patients. From the decor of the pediatric wards to the behavior of the healthcare professionals, every aspect is designed to create a nurturing and calming atmosphere.
Pediatric-Friendly Environment: The hospital’s pediatric units are designed to be colorful, warm, and welcoming. This helps create a comfortable and positive environment where children feel safe and less anxious. Engaging play areas and interactive spaces keep children occupied and help ease the stress often associated with hospital visits.
Compassionate Care Team: The nursing and support staff at Preethi Hospitals are specially trained to handle pediatric patients with empathy and patience. The team focuses on building a rapport with young patients to make them feel at ease, which significantly aids in their treatment and recovery process.
Preventive Care and Health Education
An essential aspect of pediatric healthcare is prevention and education. Preethi Hospitals, Madurai, places great emphasis on preventive measures and parental education, empowering families with the knowledge needed to maintain their child's health.
Regular Health Check-Ups: Routine health check-ups are crucial in identifying any potential health issues at an early stage. Preethi Hospitals conducts comprehensive wellness checks to monitor developmental milestones, nutritional health, and other growth parameters, ensuring that children thrive during their formative years.
Immunization Programs: Preethi Hospitals runs robust vaccination and immunization programs aligned with national guidelines. Parents can rely on the hospital to provide timely vaccinations that protect against various diseases and contribute to community-wide immunity.
Emergency Pediatric Services
Children can face medical emergencies at any time, and quick access to quality healthcare can be life-saving. Preethi Hospitals, Madurai, provides round-the-clock emergency pediatric services, supported by an experienced medical team capable of handling a variety of urgent situations with precision and care.
Conclusion: The Go-To Pediatric Hospital in Madurai
For parents seeking the best pediatric care in Madurai, Preethi Hospitals offers a blend of expert medical services, state-of-the-art facilities, and a compassionate approach. Their commitment to ensuring that children receive the best possible care makes them the top choice for pediatric healthcare in the region. From neonatal care to specialized treatments and preventive services, Preethi Hospitals truly stands out as the most reliable pediatric hospital in Madurai.

0 notes
Text
Track 13- Pediatric Gastroenterology

Pediatric gastroenterology is a specialized branch of medicine dedicated to the diagnosis, treatment, and management of digestive disorders in children, ranging from infancy through adolescence. With a focus on compassionate care, early intervention, and holistic support, pediatric gastroenterologists play a vital role in safeguarding the digestive health and well-being of young patients. In this blog, we delve into the unique aspects of pediatric gastroenterology and the importance of nurturing young digestive systems.
Understanding Pediatric Digestive Disorders
Children may experience a wide spectrum of digestive disorders, including gastroesophageal reflux disease (GERD), inflammatory bowel disease (IBD), celiac disease, food allergies, functional gastrointestinal disorders (FGIDs), and liver disorders. These conditions can significantly impact a child's growth, development, and quality of life, necessitating prompt diagnosis and tailored treatment approaches.
Pediatric gastroenterologists possess specialized expertise in evaluating pediatric digestive symptoms, interpreting diagnostic tests, and formulating comprehensive management plans tailored to the unique needs of each child and family.
Multidisciplinary Approach to Care
Pediatric gastroenterology emphasizes a multidisciplinary approach to care, involving collaboration among pediatric gastroenterologists, pediatricians, dietitians, nurses, psychologists, and other allied healthcare professionals. This collaborative model ensures holistic support for children and families, addressing not only the physical aspects of digestive disorders but also the emotional, nutritional, and psychosocial dimensions.
Furthermore, pediatric gastroenterologists often work closely with pediatric surgeons, nutritionists, and developmental specialists to optimize treatment outcomes and support the overall well-being of pediatric patients with complex gastrointestinal conditions.
Diagnostic Modalities and Therapeutic Interventions
Pediatric gastroenterologists utilize a variety of diagnostic modalities to assess digestive health in children, including endoscopy, imaging studies, laboratory tests, and non-invasive procedures. Endoscopic techniques tailored to pediatric patients, such as upper endoscopy and colonoscopy, enable precise visualization of the gastrointestinal tract while minimizing discomfort and risks.
Therapeutic interventions in pediatric gastroenterology encompass a range of treatments, including medications, dietary modifications, nutritional support, and procedural interventions. Pediatric gastroenterologists work closely with families to develop individualized treatment plans that address the specific needs and preferences of each child.
Supportive Care and Patient Education
Supportive care and patient education are integral components of pediatric gastroenterology practice. Pediatric gastroenterologists and allied healthcare professionals provide families with comprehensive information about their child's diagnosis, treatment options, dietary recommendations, and long-term management strategies.
Empowering families with knowledge and resources enables them to actively participate in their child's care, make informed decisions, and advocate for their child's health and well-being. Additionally, pediatric gastroenterologists offer ongoing support and guidance to help families navigate the challenges associated with pediatric digestive disorders, fostering resilience and promoting positive outcomes.
Conclusion
Pediatric gastroenterology embodies a compassionate and comprehensive approach to caring for children with digestive disorders. By combining clinical expertise, multidisciplinary collaboration, and family-centered care, pediatric gastroenterologists strive to optimize digestive health outcomes and enhance the quality of life for pediatric patients and their families.
As advocates for children's health, pediatric gastroenterologists are committed to fostering a nurturing environment where young digestive systems can thrive. Through dedication, innovation, and unwavering compassion, the field of pediatric gastroenterology continues to advance, offering hope and healing to children facing digestive challenges around the world.
Important Information:
Conference Name: 14th World Gastroenterology, IBD & Hepatology Conference Short Name: 14GHUCG2024 Dates: December 17-19, 2024 Venue: Dubai, UAE Email: [email protected] Visit: https://gastroenterology.universeconferences.com/ Call for Papers: https://gastroenterology.universeconferences.com/submit-abstract/ Register here: https://gastroenterology.universeconferences.com/registration/ Exhibitor/Sponsor: https://gastroenterology.universeconferences.com/exhibit-sponsor-opportunities/ Call Us: +12073070027 WhatsApp Us: +442033222718
0 notes
Text
Gastro Health for Kids: Compassionate Treatment for Gastrointestinal Disease
Gastrointestinal diseases in children can be concerning for both parents and young patients. These conditions can range from common tummy troubles to more complex issues, but the key to successful treatment lies in finding experienced pediatric specialists. At Children's Oasis Pediatrics, conveniently located at 535 Jesse Jewell Parkway SE, Suite A, Gainesville, we prioritize the health and well-being of your little ones. Our team of dedicated professionals is here to provide top-notch care and guidance for your child's gastrointestinal health.

Understanding Pediatric Gastrointestinal Disease
Pediatric gastrointestinal diseases encompass a wide range of conditions affecting the digestive system. These may include common concerns such as acid reflux, constipation, or food allergies, but they can also involve more complex issues like Crohn's disease or celiac disease. When a child experiences digestive health problems, it's essential to seek timely and expert medical attention.
Why Choose Children's Oasis Pediatrics?
1. Specialized Expertise: Our team of pediatric specialists focuses exclusively on children's gastrointestinal health, ensuring that your child receives the highest level of specialized care.
2. Compassionate Approach: We understand that young patients may feel anxious about medical appointments. Our compassionate approach aims to create a welcoming and supportive environment, making children and parents feel at ease.
3. Personalized Treatment: We recognize that every child is unique, and so are their healthcare needs. Our specialists work closely with each family to develop tailored treatment plans that address the child's specific condition and concerns.
4. Convenient Location: Located at 535 Jesse Jewell Parkway SE, Suite A, Gainesville, our clinic offers easy access to residents in the Gainesville area, ensuring that your child's care is both effective and convenient.
Treatment for Gastrointestinal Disease
The treatment for pediatric gastrointestinal disease can vary widely based on the specific condition, its severity, and the child's age. At Children's Oasis Pediatrics, we offer a comprehensive range of services to address these concerns, including:
Diagnostic procedures to identify the cause of symptoms.
Medications and therapies tailored to your child's needs.
Nutritional guidance to support overall health.
Emotional support to help children and families navigate the challenges of living with a gastrointestinal condition.
Conclusion:
Gastrointestinal diseases in children require specialized care and a compassionate approach. At Children's Oasis Pediatrics, located at 535 Jesse Jewell Parkway SE, Suite A, Gainesville, we are committed to providing exceptional care for your child's digestive health. Whether it's a common concern or a complex condition, our team of experts is here to support your family on the path to better gastrointestinal health. Your child's well-being is our top priority, and we look forward to partnering with you on this journey towards better health and peace of mind.

0 notes
Text
Children Ages 0-18 With Gastrointestinal Problems
A belly ache or rumbling tummy is quite common in children and teenagers of all ages. But what happens when the aches and pains occur on a regular basis? If your child requires paediatric digestive care in Aurangabad,it is critical to contact a gastroenterology provider to find relief. Adult Gastroenterology Associates can guide you in the right direction. Continue reading to learn more about common childhood digestive conditions, as well as some helpful hints.
How Frequently Are Kids Affected by GI Disorders?
According to the International Foundation for Gastrointestinal Disorders, functional gastrointestinal disorders account for 40 to 50% of paediatric gastroenterology physician visits. Encopresis or constipation occurs in approximately 10 to 25% of children referred to a pediatric GI specialist, and approximately 17% of high school students report symptoms consistent with IBS (irritable bowel syndrome). Our gastroenterology providers in Aurangabad find treatment options for pediatric GI conditions.
GI Conditions that Affect Teens, Children and Infants
A number of the pediatric gastrointestinal conditions that are commonly identified in infants, children, and teenagers involve:
Gastroesophageal reflux disease (GERD): Continuous heartburn in infants and children can lead to GERD diagnosis. Belching, not eating, vomiting, stomach discomfort, hiccups, and choking or gagging are all common GERD symptoms.
Lactose intolerance: This treatable condition is one of several digestive disorders that can affect adolescents, children, and infants. It occurs when a child is unable to process the sugar found in dairy, known as lactose. Lactose intolerance is characterized by loose or watery stools, gas, a stomach ache, or bloating after consuming dairy. Taking lactase enzymes before consuming dairy products can help the body properly digest lactose.
Constipation: Constipation occurs when the stool becomes dry, large, or difficult to pass. Constipation in children can cause them to avoid routine bathroom habits. Avoiding bowel movements can lead to additional constipation issues and discomfort.
Inflammatory bowel disease (IBD):This digestive issue can arise in teenagers and children. It refers to two distinct digestive conditions. Ulcerative colitis causes inflammation in the large intestine (colon), whereas Crohn's disease affects the entire GI tract. Bloody or watery bowel movements and stomach discomfort are common signs and symptoms of both conditions.
Celiac disease: Celiac disease is a digestive disorder in which an adverse reaction occurs after consuming gluten products. Gluten is a protein found in wheat, barley, and rye grains. When the disease is not under control, it can cause serious damage to the small intestine and prevent your child from absorbing essential nutrients from the food they eat.
Eosinophilic esophagitis (EoE): This condition is found in the oesophagus. Chronic allergic inflammatory disease can be caused by EoE. Nausea, vomiting, abdominal pain, regurgitation, and a burning sensation similar to acid reflux may occur in children. They may also gag frequently and have difficulty swallowing.
What Can Parents Do to Maintain Good Digestive Health in Kids?
As a parent, you want the best for your children, from scheduling appointments to ensuring they eat a balanced and healthy diet. Implementing the following suggestions into your child's daily life can help them maintain GI health:
Keep an eye on portion sizes: the amount of food consumed can affect how food is processed and digested. Excessive eating by a child can cause digestion problems and stomach discomfort.
Gather the family for a meal: Make meals enjoyable for all family members and include a family mealtime. This provides stability and consistency, allowing everyone to enjoy the time spent sharing family meals. Allowing your toddlers to feed themselves during family meals is another excellent way to help them develop a positive relationship with food.
Eat more slowly: With after-school activities and socialising, it's easy for your teen to grab a snack from the pantry and go. Encourage them to enjoy their food in order to avoid digestive discomfort.
Find Treatment for Pediatric Digestive Conditions in Aurangabad
Pediatric digestive issues do not have to cause uncontrollable symptoms. When GI issues arise, you can find options for care for all members of your family. At Adult Gastroenterology Associates, we want everyone in your family to have long-term digestive health.Dr. Ashok Jhunjhunwala is the best gastroenterologist in Aurangabad. He is also Endoscopist, and Laparoscopic surgeon in Aurangabad.
#gastroenterologistinAurangabad#gastroenterologist#LaparoscopicsurgeoninAurangabad#Laparoscopicsurgeon#Endoscopistinaurangabad#drashokjhunjhunwala#jhunjhunwalahospital
0 notes
Text
Scalp Psoriasis

Overview
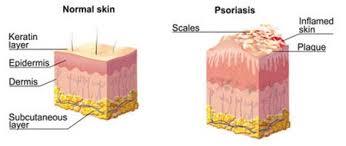
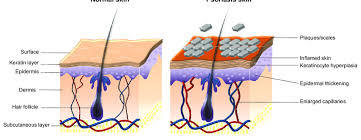
Psoriasis is a skin infection that causes red, irritated layered patches, most normally on the knees, elbows, trunk and scalp.
Psoriasis is a typical, long haul (constant) sickness with no fix. It will in general experience cycles, flaring for half a month or months, at that point dying down for some time or going into reduction. Medicines are accessible to assist you with overseeing manifestations
Symptoms
Symptoms of gentle scalp psoriasis may incorporate just slight, fine scaling. Manifestations of moderate to serious scalp psoriasis include:
Scaly, red, uneven patches
Silvery-white scales
Dandruff-like chipping
Dry scalp
Itching
Burning or touchiness
Hair misfortune
Scalp psoriasis itself doesn't cause balding, yet scratching a ton or exceptionally hard, picking at the flaky spots, brutal medicines, and the pressure that accompanies the condition can prompt impermanent going bald. Luckily, your hair as a rule becomes back after your skin clears.
Causes
Psoriasis is believed to be an invulnerable framework issue that makes the skin recover at quicker than typical rates. In the most widely recognized sort of psoriasis, known as plaque psoriasis, this quick turnover of cells brings about scales and red patches. Exactly what makes the safe framework breakdown isn't totally clear. Specialists accept both hereditary qualities and natural elements assume a job. The condition isn't infectious.
Psoriasis triggers
Numerous individuals who are inclined to psoriasis might be liberated from indications for a considerable length of time until the infection is set off by some natural factor. Basic psoriasis triggers include:
Infections, for example, strep throat or skin diseases
Weather, particularly cool, dry conditions
Injury to the skin, for example, a cut or scratch, a bug chomp, or a serious burn from the sun
Stress
Smoking and introduction to used smoke
Heavy liquor utilization
Certain prescriptions — including lithium, hypertension meds and antimalarial drugs
Rapid withdrawal of oral or foundational corticosteroids
Hazard factors
Anybody can create psoriasis. About 33% of cases start in the pediatric years. These components can build your hazard:
Family history. The condition runs in families. Having one parent with psoriasis builds your danger of getting the illness, and having two guardians with psoriasis expands your hazard considerably more.
Stress. Since stress can affect your safe framework, high feelings of anxiety may expand your danger of psoriasis.
Smoking. Smoking tobacco builds your danger of psoriasis as well as may expand the seriousness of the sickness. Smoking may likewise assume a job in the underlying improvement of the malady.
Intricacies
On the off chance that you have psoriasis, you're at more serious danger of creating different conditions, including:
Psoriatic joint inflammation, which causes torment, solidness and growing in and around the joints
Eye conditions, for example, conjunctivitis, blepharitis and uveitis
Obesity
Type 2 diabetes
High circulatory strain
Cardiovascular illness
Other immune system illnesses, for example, celiac malady, sclerosis and the incendiary entrail infection called Crohn's sickness.Mental wellbeing conditions, for example, low confidence and melancholy
Treatment
Psoriasis medicines mean to prevent skin cells from developing so rapidly and to evacuate scales. Choices incorporate creams and treatments (skin treatment), light treatment (phototherapy), and oral or infused medicine.

Which medicines you use relies upon how extreme the psoriasis is and how responsive it has been to past treatment. You may need to attempt various medications or a blend of medicines before you discover a methodology that works for you. Normally, be that as it may, the sickness returns.
Effective treatment
Corticosteroids. These medications are the most habitually recommended prescriptions for getting gentle moderate psoriasis. They are accessible as treatments, creams, moisturizers, gels, froths, showers and shampoos. Gentle corticosteroid salves (hydrocortisone) are typically suggested for delicate territories, for example, your face or skin folds, and for treating across the board fixes. Effective corticosteroids may be applied once per day during flares, and on exchange days or ends of the week just to look after reduction
Vitamin D analogs. Manufactured types of nutrient D, for example, calcipotriene and calcitriol (Vectical) slow skin cell development. This sort of medication might be utilized alone or with skin corticosteroids. Calcitriol may cause less bothering in delicate regions. Calcipotriene and calcitriol are normally more costly than effective corticosteroids.
Retinoids. Tazarotene (Tazorac, Avage) is accessible as a gel and cream and applied on more than one occasion every day. The most widely recognized reactions are skin aggravation and expanded affectability to light.Tazarotene isn't suggested when you're pregnant or bosom taking care of or on the off chance that you plan to get pregnant.
Calcineurin inhibitors. Calcineurin inhibitors —, for example, tacrolimus (Protopic) and pimecrolimus (Elidel) — lessen aggravation and plaque development. They can be particularly useful in territories of flimsy skin, for example, around the eyes, where steroid creams or retinoids are too bothering or may cause destructive impacts.
Calcineurin inhibitors are not suggested when you're pregnant or bosom taking care of or on the off chance that you plan to get pregnant. This medication is likewise not expected for long haul use due to a possible expanded danger of skin malignancy and lymphoma.
Salicylic corrosive. Salicylic corrosive shampoos and scalp arrangements lessen the scaling of scalp psoriasis. It might be utilized alone, or to improve the capacity of different meds to all the more effectively infiltrate the skin.
Coal tar. Coal tar decreases scaling, tingling and aggravation. It's accessible over-the-counter or by remedy in different structures, for example, cleanser, cream and oil. These items can aggravate the skin. They're likewise muddled, stain attire and bedding, and can have a solid smell.Coal tar treatment isn't suggested for ladies who are pregnant or bosom taking care of.
Goeckerman treatment. A few specialists consolidate coal tar treatment with light treatment, which is known as Goeckerman treatment. The two treatments together are more powerful than either alone on the grounds that coal tar makes skin more responsive to UVB light.
Anthralin. Anthralin (another tar item) is a cream used to slow skin cell development. It can likewise evacuate scales and make skin smoother. It ought not be utilized on the face or private parts. Anthralin can aggravate skin, and it recolors nearly anything it contacts. It's normally applied for a brief timeframe and afterward washed off.
Various medicines may be provided by various specialist in your clinical group.Buy your medicines online now at Indias best online store-3MEDS
Elective medication
Various elective treatments guarantee to facilitate the side effects of psoriasis, including uncommon eating regimens, creams, dietary enhancements and spices. None have completely been demonstrated compelling. Yet, some elective treatments are esteemed commonly protected and may lessen tingling and scaling in individuals with mellow to direct psoriasis. Other elective treatments are helpful in maintaining a strategic distance from triggers, for example, stress.
Aloe separate cream. Taken from the leaves of the aloe vera plant, aloe separate cream may lessen redness, scaling, tingling and aggravation. You may need to utilize the cream a few times each day for a month or more to perceive any improvement in your skin.
Fish oil supplements. Oral fish oil treatment utilized in mix with UVB treatment may diminish the measure of influenced skin. Applying fish oil to the influenced skin and covering it with a dressing for six hours per day for about a month may improve scaling.
Oregon grape. Otherwise called barberry, this item is applied to the skin and may lessen the seriousness of psoriasis.
Essential oils. Basic oils utilized for fragrance based treatment have been appeared to diminish pressure and uneasiness.
Purchase all your medicines online at the click of your finger on 3MEDS-Indias online medical store
Way of life and home cures
Attempt these self-care measures to all the more likely deal with your psoriasis and feel your best:
Take day by day showers. Washing day by day helps evacuate scales and quiet aggravated skin. Include shower oil, colloidal oats and Epsom salts to the water and splash for in any event 15 minutes. Utilize tepid water and mellow cleansers that have included oils and fats.
Use cream. Subsequent to washing, delicately wipe off and apply an overwhelming, treatment based cream while your skin is as yet sodden. For dry skin, oils might be ideal — they have more resilience than creams or salves do. On the off chance that saturating appears to improve your skin, apply it one to multiple times day by day.
Cover the influenced territories short-term. Prior to hitting the sack, apply a balm based cream to the influenced skin and wrap with cling wrap. At the point when you wake, expel the plastic and wash away scales.
Expose your skin to modest quantities of daylight. Get some information about the most ideal approach to utilize characteristic daylight to treat your skin. A controlled measure of daylight can improve psoriasis, yet a lot of sun can trigger or exacerbate flare-ups and increment the danger of skin malignancy
Apply cured cream or salve. Apply an over-the-counter cream or salve containing hydrocortisone or salicylic corrosive to decrease tingling and scaling. On the off chance that you have scalp psoriasis, attempt a sedated cleanser that contains coal tar. Avoid psoriasis triggers. Notice what triggers your psoriasis, and find a way to forestall or maintain a strategic distance from them. Diseases, wounds to your skin, stress, smoking and extraordinary sun presentation would all be able to intensify psoriasis.
Avoid drinking liquor. Liquor utilization may diminish the viability of some psoriasis medicines. On the off chance that you that you might have psoriasis.
On The Off Chance
It is difficult to prevent scalp psoriasis, because the exact cause remains unclear.However, treating the condition as soon as symptoms appear may prevent it from becoming worse.
3MEDS-online pharmacy store in India,is concerned with health and fitness of their customers and therefore believes in providing knowledge about healthcare to their customers.
Scalp psoriasis affects individuals differently. Some people have an occasional flare-up while others deal with the condition frequently.If a person knows what triggers symptoms for them, they can try to avoid these factors.
-Vikrant Bhagat
#3Meds#bestmedicineppinindia#24hoursmedicinedelivery#drinkingliquor#Coal tar#eczema#vegan#psoriasistreatment#psoriasisawareness#natural#drykin#kosmetic#psoriasislife
0 notes
Text
'Dr. Bob' Sears Accused Of Issuing Invalid Vaccine Medical Exemptions--Again
https://sciencespies.com/news/dr-bob-sears-accused-of-issuing-invalid-vaccine-medical-exemptions-again/
'Dr. Bob' Sears Accused Of Issuing Invalid Vaccine Medical Exemptions--Again
Bob Sears, a pediatrician from Orange County, right, testifies against a measure by state Sen. Dr. Richard Pan, D-Sacramento, left, who is also a pediatrician, that would give public health officials oversight of doctors that may be giving fraudulent medical expeditions from vaccinations during a hearing of the Assembly Health Committee at the Capitol in Sacramento, Calif., Thursday, June 20, 2019. (AP Photo/Rich Pedroncelli)
ASSOCIATED PRESS
“Dr. Bob” Sears, MD, the controversial California physician known for his Godwin-esque advocacy against vaccination requirements and a vaccine book filled with misinformation, is facing another accusation from the Medical Board of California, less than a year after he was placed on probation for medically negligent practices. Ironically, the complaint was filed just two days before Sears testified at a California legislative committee hearing against SB 276, a bill that aims to prevent exactly the behavior that led to his previous censure and this complaint.
“I find it astonishing that a person who is on probation with the medical board is going to be the main spokesperson to say the bill is bad, the person the bill is designed to protect against,” California State Senator Richard Pan, MD, FAAP, (D – Sacramento) told me after the bill he’s sponsoring passed out of the Assembly Health Committee 9-2 yesterday.
What Happened?
The complaint, brought by Kimberly Kirchmeyer, executive director of the Medical Board of California, alleges that Sears filed medical vaccination exemptions for a pair of siblings who did not have medically recognized contraindications for any vaccines, based on what he recorded in their medical records.
Medical exemptions allow children to attend California schools without having received immunizations required by the state for school attendance. Following SB 277 in 2015, California became the third state to only allow medical exemptions. Similar bills have since become law in Maine this May and in New York last week.
The patients are a 7-year-old unvaccinated boy with psoriasis and his sister, whose only medical history is a bee sting allergy. Both saw Sears on May 4, 2016 for a complaint of “vaccine exemption appt.”
Sears recorded the children’s family medical history as “autoimmune disorders, lupus, psoriasis (in Dad), inflammatory bowel disease, irritable bowel disease, irritable bowel syndrome (in Dad), gluten sensitivity severe in Mom and Aunt, suspect CD [celiac disease] in aunt, neurodevelopmental disorders, ADD/ADHD (in Dad), psychiatric disorders, schizophrenia (Dad), bipolar, and depression.”
The boy’s exam included “psoriatic plaques on scalp, back of neck and ears,” and the girl’s exam was normal, though Sears documented no vital signs for her (blood pressure and temperature). Both children were diagnosed with “viral infection, unspecified” and “feeding difficulties” despite the purpose of the appointments being solely recorded as “vaccine exemption” visits.
Sears determined that the boy “qualified for medical exemption from vaccines for family history of autoimmune disorders (Dad and others), inflammatory bowel disease (Dad), neurodevelopmental disorders (Dad), psychiatric disorders (Dad), and the child’s own autoimmune disorder.” Sears determined the girl qualified “based on review of her past medical history, family history, and current state of health.” He filed letters for both children “exempting [them] from all vaccines for the rest of [their] childhood.”
None of the conditions or family history, as noted in the children’s records, meet the criteria for contraindications to any CDC-recommended childhood vaccines, according to the CDC. The complaint notes for the boy that a “childhood long medical vaccine exemption… based on diagnosis of psoriasis, without immunosuppressive medication, is a simple departure from standard of care.”
Immunosuppressive medication, including that used to treat autoimmune disease such as psoriasis, is a contraindication for live vaccines, such as the MMR and chickenpox vaccines, explained Jaime Friedman, MD, FAAP from Children’s Primary Care Medical Group in San Diego. The complaint goes on to say the boy’s diagnosis and both children’s family history “are not a known contraindication or precaution to routine childhood vaccination.”
The father of the children appeared to agree. Seven months later, on January 25, 2017, the children’s mother called to tell Sears’ office that the children’s father “retract his consent regarding the medical exemption letter.” Since exemptions require consent from both custodial parents, Sears told her the exemption letter was no longer valid. To get another letter, both parents would need to come in and bring the children’s past medical records, he said. Both children’s records “contain an amended copy of the medical exemption letter dated May 4, 2017, stating the original exemption letter is no longer valid and should be disregarded due to a change in family circumstances and consent.”
The Medical Board accusation includes “failure to maintain adequate records” as a second cause for discipline because Sears “failed to obtain and document an appropriate and accurate past medical history, physical exam and family/social history” for the children. This charge was also in the previous accusation that led to Sears’ 35-month probation in July 2018. Sears did not return my emailed request for comment.
Medical Exemptions Appear Inappropriate
“Without being able to review the child’s medical chart and assuming the child was not on immunosuppressive medication, I don’t see a reason for the child to have a vaccine exemption,” Friedman told me. With the “viral infection, unspecified” in the chart, Friedman said that “could be a contraindication to giving the vaccine that day but not to giving it in the future.”
Friedman, who has written three medical exemptions for her patients, said contraindications certainly exist for certain vaccines but are rare. “These are the patients you want to protect, so these are the kids you want to surround with vaccinated people, like their classmates and their siblings,” she said. If she had a patient on immunosuppressive medication for an autoimmune disease, she said she would work with the child’s specialist, such as a dermatologist or rheumatologist, to determine if and when it was safe for the child to receive vaccines.
Pan agreed that if children “had a skin rash so severe that they would need immunosuppression significantly enough that they can’t be vaccinated, probably a specialist is involved, especially for something like psoriasis.” He also noted the unusual decision to provide an exemption until “the end of childhood.” “Unless you have proof that this condition suddenly terminates at the end of childhood,” Pan said, a doctor would issue either a permanent exemption for a chronic, permanent contraindicated condition or a temporary exemption until the contraindicated condition or medication resolves.
The complaint contains other “much more fundamental issues,” said Sonia Khan, MD, FAAP, director of Pediatric Crisis Solutions, a consulting firm, and medical director of the Team Substance Use Disorder Program at City of Fremont in California. Khan testified for SB 276 at the California Assembly.
“He didn’t even do vital signs on these kids. If you don’t do vital signs on the kids, right off the bat, the medical exam isn’t complete,” Khan told me. “If these do prove to be valid accusations, then there are some pretty flagrant violations.”
She said this complaint reveals the need for the California Department of Public Health (CDPH) to be able to track down medical exemptions and determine the exams and exemptions were done properly.
What SB 276 Would Do
SB 276 bill requires guardians whose children receive a medical vaccine exemption to sign a form that releases the medical records to CDPH and the Medical Board of California for review. The current incarnation of the bill includes two potential triggers for review: if the child attends a school with an immunization rate below 95% or if the physician who wrote the exemption has issued more than five medical exemptions in the previous year.
The second requirement is not a cap, Pan said. A pediatric oncologist, for example, may need to write many more than five exemptions in a year. It simply means the CDPH can review the exemptions. If multiple exemptions appear invalid, the CDPH can refer the case to the medical board, the disciplinary agency. Currently, both the CDPH and medical board have difficulty reviewing exemptions because they lack access to the medical records of children with exemptions.
“The difficulty up until now in chasing down potentially fraudulent exemptions is that the families are complicit,” Khan said. “When a doctor gets reported, the family or someone else is triggering an investigation. In a fraudulent exemptions, the families aren’t going to cooperate.”
“HIPAA [Health Insurance Portability and Accountability Act of 1996] has a specific exception for public health agencies engaged in ‘public health surveillance, public health investigations, and public health investigations,’ that covers SB276 and board investigations,” said Dorit Reiss, a professor of law at the University of California Hastings College of Law who specializes in vaccine policy. Reiss formally entered her name in support of SB 276.
But that doesn’t mean the records are easy to get. Another ongoing case illustrates this problem: The Medical Board of California sued Bay Area pediatrician Ron Kennedy, MD, to compel him to produce patient records “of three minors for whom Dr. Kennedy provided vaccination exemptions.” Kennedy refused, and the San Francisco city and count court compelled him to provide the records. Kennedy filed an appeal, and this most recent filing denied his request to stay the court’s demand that he turn over the medical records.
Sears’ complaint does not note who reported him or provided the medical records. His previous accusation arose from a parent who provided the records, according to an unnamed, verified source.
Parents are typically not the ones who trigger medical exemptions, Pan explained. In fact, pediatricians do not have “medical exemption appts” at all. Appointments are typically well visits, acute care visits, chronic care visits or follow-ups.
“A medical exemption should usually result from the pediatrician or a specialist seeing them saying ‘given the condition or situation you have, I would recommend we either don’t vaccinate or hold off on these vaccines,’” Pan said. “It’s odd for parents to ask for a medical exemption.”
Increased Medical Exemptions Triggered SB 276
Yet that appears to have become a trend after SB 277 eliminated personal belief exemptions. In late 2018, a study in Pediatrics found problems that had emerged from implementation of the law, including confusion and frustration over which medical exemptions were valid, how schools and health departments should track them, high fees doctors were charging for them and concerns that medical exemptions were increasing.
Indeed, just this month, some of the same researchers found California medical exemptions had increased despite an overall decline in unvaccinated children entering school in California. A year after the bill took effect, 4.4% of kindergartens entered school without all required vaccinations, down from 7.2% the previous year. But medical exemptions quadrupled from 0.6% to 2.4%. The following year, non-up-to-date kindergartners ticked up slightly, by 0.5%. In a state of nearly 40 million people, that’s a couple hundred thousand additional children not fully vaccinated in a year with the most measles cases since the disease was eliminated from the US.
Another study in the American Journal of Public Health found that SB 277 was interpreted and implemented unevenly in school districts and local health departments throughout California due to “vague legislative and regulatory language.” The researchers also found “lack of centralized review of medical exemptions allowed medical exemptions that are not consistent with valid contraindications for immunizations to be accepted.” Among the uncertainties were what kinds of physicians can write vaccine medical exemptions, which health conditions qualify for one and how to report dubious or suspicious ones.
Those are precisely the issues that SB 276 aims to address.
“The major purpose of SB276 is to prevent unscrupulous doctors from selling unnecessary exemptions so we can restore community immunity,” said Leah Russin, executive director of Vaccinate California, who is co-sponsoring SB 276 with the California Medical Association and the California chapter of the American Academy of Pediatrics.
She noted that 835 schools in California—with nearly 400,000 students—have kindergarten MMR immunization rates under 95%, according to CDPH data.
“If true, the new complaint against Dr. Bob Sears demonstrates exactly why SB276 is needed. Currently no entity in state or local government, including the schools, have the authority to reject an exemption letter signed by a doctor,” she said. “The exemptions described in the complaint do not follow the standard of care, and if issued after implementation of SB276 and subject to the triggers specified in it, they would likely be flagged as unjustified.”
Sears’ History May Prevent Leniency
Some observers believe the medical board’s previous ruling on Sears’ misconduct was forgiving but hope that won’t be the case again, especially since his case could be an example to other physicians writing spurious medical exemptions.
“I certainly hope that as the medical board is looking at these issues and investigating and evaluating them, they recognize his previous history, that he’s already on probation, that he hasn’t expressed remorse for what happened and acknowledged the error of his ways,” Pan said. “He has continued to proclaim he did nothing wrong, which I find very disturbing. You’re put on probation for acts of negligence, and you go on Facebook and say you’re not in the wrong.”
Even if the board does not fully revoke Sears’ medical license—which is one potential outcome of the complaint—Pan hopes the consequences will ensure he cannot continue to issue medical exemptions.
“If that’s the issue he’s being cited for, then certainly whatever sanction he receives needs to stop him from continuing that behavior,” Pan said. “Otherwise, one could argue that’s sending the signal to other people that the consequences aren’t very serious.”
#News
0 notes
Text
Beyond Gluten: Could It Be Wheat Sensitivity?
Public-health messages often tout whole wheat as an important source of vital nutrients. Yet, in many health circles, wheat is eyed with suspicion as increasing numbers of people report digestive problems, headaches, joint pain, skin irritation, sapped energy, and mood disruptions when they eat it. In addition, some integrative-health experts have raised concerns about wheat’s suspected role in certain chronic diseases.
The grain has long been a corner-stone of the human diet, but the wheat we eat today is not the same wheat our grandparents enjoyed. The way it is produced, processed, and consumed has changed significantly in the past 50 years, which goes a long way in explaining the controversies surrounding it.
Modern wheat varieties are bred for increased production, pest resistance, and improved baking qualities. They also often produce higher levels of the protein gluten and other compounds that can be problematic for some.
The wheat-based foods we eat are different as well, usually made from ungerminated grains, which contain more reactive compounds than traditionally prepared sprouted wheat. And fast-acting yeast is commonly used for fermentation, which delivers fewer and less-diverse bacteria than old-school sourdough methods. It’s also less effective at degrading wheat’s reactive components.
At the same time, wheat consumption has risen significantly, thanks in part to the rapid expansion of the fast-food and packaged-food industries. Consumption dipped slightly in the most recent decade, largely due to a rise in gluten-free diets; still, the average American today consumes 134 pounds of wheat flour annually.
We spoke with health experts and researchers about some of the problems associated with wheat. While they acknowledge there is still much to learn about the grain’s properties — including the mechanisms that cause health problems in some people — many expressed concern with the quality and quantity of the wheat we consume.
“Adverse food reactivity is a consideration in every patient I see,” explains Minneapolis-based functional-medicine specialist Gregory Plotnikoff, MD, whose patients have often struggled with unresolved health problems before seeking him out. “And on top of the adverse-food-reactivity list is wheat.”
Protein of Interest: Gluten
The rise in wheat consumption coincides with an increased prevalence of celiac disease, a condition in which the protein gluten (found in wheat, barley, and rye) triggers an autoimmune response that attacks the small intestine in some genetically susceptible individuals.
Celiac affects 1 percent of Americans, a number that is expected to grow with increased awareness and better testing methods.
Some people have a wheat allergy, which generates an antibody to proteins (including gluten) in the grain. Up to 1 percent of children in the United States are allergic to wheat (though they often outgrow it), while just 0.4 percent of adults are.
Harder to pin down is the apparent rise in nonceliac gluten sensitivity (NCGS), a condition characterized by digestive and nondigestive symptoms that improve when gluten-containing foods are removed from the diet.
Researchers estimate that 6 to 8 percent of Americans have NCGS, but it’s difficult to diagnose. There are no established biomarkers, and symptoms can mimic other conditions, including irritable bowel syndrome and fructose malabsorption. Further, people often self-diagnose and adopt gluten-free diets on their own without screening for other potential causes of their symptoms.
Opinions differ on exactly how gluten may trigger NCGS symptoms, though many experts point to its role in creating gut permeability — the opening of microscopic spaces in the thin layer of cells lining the intestinal wall.
Humans cannot completely digest gluten, explains pioneering celiac-disease researcher Alessio Fasano, MD, the W. Allan Walker Chair in Pediatric Gastroenterology and Nutrition at Massachusetts General Hospital. Specifically, we can’t digest a smaller protein within gluten called gliadin, whose presence spurs the release of zonulin, a molecule that regulates gut permeability.
Excessive intestinal permeability — known as leaky gut — can allow bacteria, toxins, and undigested food to enter directly into the bloodstream and cause bodywide inflammation. This can, in turn, be a precursor to autoimmune conditions and manifest in symptoms of conditions such as eczema and neurological issues.
Gluten’s role in triggering gut permeability has caused some experts to view it as an inherently dangerous substance.
“Anything that increases intestinal permeability increases the risk of celiac disease and other autoimmune conditions in individuals who are genetically predisposed,” says Florida-based neurologist David Perlmutter, MD, author of Grain Brain. He further argues that gluten’s ability to disrupt the gut lining is reason enough for everyone to avoid it. “Gluten-containing foods exacerbate problems with gut health and the inflammation that ensues from it.”
Other experts disagree that everyone should avoid gluten, including some celiac-disease researchers who argue that their findings have been misinterpreted and overstated.
“Some information has been taken out of context,” Fasano says. With regard to gluten’s role in intestinal permeability, for instance, he explains: “This happens to everybody — though for the vast majority of people, this increased permeability is temporary. It’s switched on and off, and therefore does not have any long-term consequences and doesn’t cause inflammation. The phenomenon of gut permeability is general, but the consequences affect just a small percentage of individuals.”
For people with adverse symptoms — whether or not they have an official diagnosis — elimination diets are an invaluable tool for identifying foods to avoid. But elimination diets are not diagnostic, notes Plotnikoff.
“They provide qualitative, nonspecific guidance,” he explains. Unless a specific reactive component can be isolated, some patients continue to have complaints even after eliminating gluten-containing foods.
“The majority of people who self-identify as being gluten-sensitive in a controlled, double-blind study are not actually gluten-sensitive,” says Celiac Disease Center director Peter Green, MD, the Phyllis and Ivan Seidenberg Professor of Medicine at Columbia University. “Most studies show that people aren’t responding to gluten in wheat — it’s something else in the diet.”
The Modern-Wheat Factor
Tens of thousands of wheat varieties are now grown worldwide, each with a unique reactivity profile, which refers to the potency and amount of reactive components in the grain. Most have moderately higher levels of gluten and other reactive compounds compared with varieties grown a generation or two ago.
Some experts speculate that the following factors may also be behind the rise in wheat-related sensitivities:
• Amylase-trypsin inhibitors (ATIs): These proteins help wheat protect itself against common parasites, and, like gluten, they can instigate an immune response. ATI sensitivity may help explain why people without a demonstrable gluten sensitivity nonetheless feel better on a diet that eliminates the same foods.
“ATIs could be the long-sought inducers of innate immunity in patients with celiac or NCGS,” Fasano and colleagues write in a 2015 paper published in the journal Gastroenterology. The researchers state that, as with gluten, most people don’t respond negatively to ATIs.
• Fructans: These groups of sugar molecules are a type of FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols — a category of carbohydrates) that are found in a wide range of foods. Fructans can ferment in the colon, causing digestive symptoms in sensitive people.
Reaction to FODMAPs is considered a food intolerance (because the body lacks an enzyme needed to digest certain nutrients) rather than a food sensitivity (in which the body mounts an immune response). The FODMAPs in wheat are thought to cause a comparatively mild wheat intolerance that’s limited to intestinal issues. If eliminating wheat doesn’t completely resolve the issues, FODMAPs in other foods may be to blame as well.
• Agricultural chemicals: Another concern is the use of pesticides and herbicides, including glyphosate, the world’s most popular broad-spectrum herbicide. Marketed as Roundup, glyphosate is used on a third of planted wheat acreage in the United States. (Nearly 60 percent of durum-wheat acreage is treated with glyphosate; this is the wheat typically used in pasta.)
Roundup is also occasionally used to help dry wheat prior to harvesting, though this practice is limited.
“Glyphosate was approved by the U.S. Food and Drug Administration because it wasn’t known to interfere with mammalian biology,” Plotnikoff explains. But glyphosate residue in wheat and other crops we eat has been found to interfere with our microbiomes, he says. It can disrupt the production of aromatic amino acids, which our bodies use to make neurotransmitters that affect our mood, memory, energy, and sleep.
In July 2017, California officials classified glyphosate as a human carcinogen.
• Other suspicious compounds: Plotnikoff says some people also react to contaminants in wheat, such as mycotoxins, which are produced by fungi that grow in damp storage conditions, or nickel, a heavy metal that may accumulate when farmers use inorganic nickel salts for rust control in wheat cultivation.
Because multiple components in wheat can trigger symptoms associated with nonceliac gluten sensitivity, some experts now prefer the term “nonceliac wheat sensitivity.” This reflects not only the potentially troublesome proteins and carbohydrates but also other properties in the grain that may be making people ill.
The Processing Problem
Like the wheat itself, today’s wheat-based foods differ from those of the past. Additives in these products are common. For example, bread manufacturers will add extra gluten — known as vital wheat gluten — to improve texture. (This is made by extracting gluten from wheat, leaving behind just the starch.)
“If you buy cheap white bread, it’s probably made with cheap flour that doesn’t have a lot of gluten in it, but it has this added vital wheat gluten,” explains Green.
Numerous commercial food products also contain an added enzyme called microbial transglutaminase, which facilitates certain chemical reactions in bakery goods, dairy products, and processed meats. It activates gluten and causes an immune response in celiac patients, says Green. “This could be responsible for the increase in celiac disease, and it could be responsible for people becoming sensitive to gluten.”
Finally, today’s breads, cereals, pastas, crackers, pastries, and desserts are often created from wheat stripped of its bran and germ and ground into white flour, a refinement process that all but eliminates wheat’s important nutrients, including dietary fiber. Some nutrients are added to “enriched” flour, but most flours are shadows of their former nutritional selves.
Worse, they can trigger erratic spikes in blood glucose and insulin, which bring other health problems. “The refined stuff is the worst,” says Paul Kriegler, RD, a nutrition program manager for Life Time in Chanhassen, Minn. “It’s basically like eating table sugar.”
Overloaded Systems
On top of all these concerns, countless environmental and lifestyle factors can disrupt the integrity and microbial balance of the gut, which houses 70 percent of the immune system — making us more vulnerable to the potential problems associated with wheat.
“Our immune systems are challenged by 21st-century living,” says Liz Lipski, PhD, CCN, CHN, professor and director of academic development for the nutrition programs at Maryland University of Integrative Health and author of Digestive Wellness. A lifetime of exposure to medications, processed foods, tobacco smoke, alcohol, pollutants, chemicals in personal-care products, and even stress can set us up for a host of symptoms and diseases, she explains.
For people with compromised gut health, whether or not they have an official wheat-related diagnosis, “wheat is just one more assault,” Lipski says.
Have Your Wheat and Eat It, Too?
Clearly, people with celiac disease and wheat allergies must avoid all wheat products. But can the rest of us — even those of us with apparent sensitivities — ever enjoy wheat again?
For some, respite may be found in foods made from organic heritage grains, which are varieties developed prior to the 1950s. The data is limited, but it suggests that some heritage varieties, including einkorn, emmer, and Khorasan (marketed as Kamut), may have lower levels of reactive proteins and fructans compared with most modern wheat. Some people with wheat sensitivities find they have fewer problems with heritage wheats. At this point, however, no wheat species or varieties have been proven safe for people with celiac or wheat allergies.
Lipski and other experts recommend fermenting flour (from organic heritage grains, if possible) to further reduce the challenges associated with digesting wheat. “When you make sourdough, you’re picking up the microbes that are in your own kitchen, and you are harmonizing yourself with your own environment,” she explains.
Even for those of us who don’t notice any problems after eating breads and pastas, moderation is wise, says Kriegler — and we should all be cautious about processed foods.
“I teach my clients to reverse-engineer what they should be eating in a day, and then see where wheat fits in,” he says. “If you’re getting plenty of produce, healthy proteins, and fats, your appetite’s going to be stable. Do you still want bread? Sure, you can eat it, but it becomes more of a condiment than a main dish.”
This originally appeared as “What’s Up With Wheat?” in the September 2018 print issue of Experience Life.
Get the full story at https://experiencelife.com/article/beyond-gluten-could-it-be-wheat-sensitivity/
0 notes
Text
Soccer Player Kicks Crohn’s to the Sideline
New Story has been published on https://enzaime.com/soccer-player-kicks-crohns-sideline/
Soccer Player Kicks Crohn’s to the Sideline
https://www.childrensmercy.org/My_Story/Gastroenterology/Soccer_Player_Kicks_Crohn_s_to_the_Sideline/ From a young age, Lily Smith loved soccer. Nothing distracted her from smacking the ball down the field and fighting off competitors—not even the Celiac disease she had endured since age four.
But near the end of Lily’s fifth-grade year, she began complaining of vertigo-like symptoms that were so bad they left her nauseous and prone to vomiting. She became extremely fatigued and began suffering from severe joint pain, headaches, high fevers and swelling in her face and under her jawbone. Despite a variety of treatments, the symptoms persisted through the summer and into the fall.
By the end of the first semester of sixth grade, Lily had missed 33 days of school. “She was so exhausted she would go to bed at 7:30 just to make it through the next day,” her mother Gail said.
Despite her fatigue, Lily remained committed to her favorite sport—soccer. Lily’s coach was extremely compassionate. He had watched her health decline that year and, though she often missed practice and frequently had to be subbed out of games, he supported his dedicated player.
Reassessing a diagnosis “We took Lily to her pediatrician many times and had quite a few tests done,” Gail said. But when the doctor diagnosed Periodic Fever, Aphthous Stomatitis, Pharyngitis, Adenitis Syndrome (PFAPA), Gail wasn’t convinced. She took her daughter to see a specialist at The University of Kansas Health System who referred Lily to Maria F. Ibarra, MD, a pediatric rheumatologist at Children’s Mercy.
“Even though Lily had to endure a lot more tests, she didn’t complain because Dr. Ibarra helped her understand the importance of every one,” Gail said. When Dr. Ibarra asked Julie A. Bass, DO, a Children’s Mercy gastroenterologist, to examine Lily the family was hesitant.
“We were so spoiled by the amazing care we’d received from Dr. Ibarra we were a little reluctant to move on,” Gail said. “In the end, we trusted Dr. Ibarra. And that was the best decision we ever made!”
Trust and testing In the spring of her sixth-grade year, Dr. Bass diagnosed Lily with Crohn’s disease, a form of inflammatory bowel disease (IBD) that usually affects the intestines.
“Dr. Bass spent a lot of time explaining her diagnosis and treatment options. And, even though we were very upset by Lily’s diagnosis, we never left Dr. Bass’s office feeling hopeless,” Gail said. “It helped that Lily loved Dr. Bass. From the first appointment, she included Lily in the conversation, which made her feel like she was part of the decision-making process.”
Lily’s began taking oral medications to handle the illness. After a few months, however, she wasn’t making the progress Dr. Bass anticipated. Thus, a new treatment was prescribed with included two-hour infusions, every seven weeks.
The treatments did the trick. Lily’s appetite returned, she gained weight and she grew close to a foot over the next two-and-a-half years. When Lily later developed antibodies to the drug, Dr. Bass switched her to a new treatment regimen.
Today, Lily is doing great, Gail said. “She continues to grow and become stronger and is pretty much symptom-free.”
Now a 16 year old, Lily follows up with Dr. Bass twice a year. The high school junior continues to pursue her favorite sport, playing on both a club team and her high school team.
0 notes