#Palliative medicine
Explore tagged Tumblr posts
Text
All the world's a stage
By William Shakespeare
(from As You Like It, spoken by Jaques)
All the world’s a stage,
And all the men and women merely players;
They have their exits and their entrances;
And one man in his time plays many parts,
His acts being seven ages. At first the infant,
Mewling and puking in the nurse’s arms;
And then the whining school-boy, with his satchel
And shining morning face, creeping like snail
Unwillingly to school. And then the lover,
Sighing like furnace, with a woeful ballad
Made to his mistress’ eyebrow. Then a soldier,
Full of strange oaths, and bearded like the pard,
Jealous in honour, sudden and quick in quarrel,
Seeking the bubble reputation
Even in the cannon’s mouth. And then the justice,
In fair round belly with good capon lin’d,
With eyes severe and beard of formal cut,
Full of wise saws and modern instances;
And so he plays his part. The sixth age shifts
Into the lean and slipper’d pantaloon,
With spectacles on nose and pouch on side;
His youthful hose, well sav’d, a world too wide
For his shrunk shank; and his big manly voice,
Turning again toward childish treble, pipes
And whistles in his sound. Last scene of all,
That ends this strange eventful history,
Is second childishness and mere oblivion;
Sans teeth, sans eyes, sans taste, sans everything.
2 notes
·
View notes
Text
Expert Anesthetist Services | Balaji Hospital
Balaji Hospital offers expert anesthetist services ensuring safe and pain-free surgical procedures with advanced anesthesia care. Learn more about our specialists.

#Anesthetist#Neurosurgeon#Complete cancer care#Onco Physician#Multi disciplinary treatment to rehabilitation#Onco Surgery#Children with spine and limb deformities#Orthopedic Surgery#Pediatrician#Spinal cord injury#Physiotherapist#Reconstructive surgery#Hand surgery#Microsurgery#Treatment of burns#Plastic Surgery#Emotional illness#Psychiatric#Interventional radiology#vascular radiology#Palliative medicine#Radiologist#Comprehensive diagnostic and treatment services#Urology#Ventilator for artificial breathing#40-bed hospital#Holistic approach to illness#4 Different Health checkup Plans#Delivering quality health care#40 beds ISO 9001:2000 certified Hospital
0 notes
Text
When you get sicker, it's clear to us that your time is getting short. What do you want that time to look like? Would you be willing to risk spending your very last days hooked up to machines to buy you a bit more time? Or would you like to prioritise peace and comfort while your illness runs its natural course? Because with a serious illness, CPR won't change if you die, but it can change how you die.
— Matthew Tyler, MD, 'How I talk to patients about CPR' (TikTok, 11 October 2024).
Dr Tyler is board certified in internal medicine and hospice & palliative medicine, and runs How To Train Your Doctor.
1 note
·
View note
Text
Podcast - Paediatric Palliative Care in the ED
This post accompanies the podcast 'Paediatric Palliative Care' recorded live at the Premier Conference 2024. Learn how you can best help children with life limiting illness and their families if they need your care in the Emergency Department.
Working in the emergency department (ED) is always challenging, but caring for children with life-limiting conditions adds an extra layer of complexity and emotion. In this podcast, Dr Timothy Warlow, a consultant in Paediatric Palliative Medicine at University Hospitals Southampton & Naomi House & Jacksplace Hospices, shares some top tips for how we can best care for these children and their…
0 notes
Text
Doing research for hours without a break isn't good for me. My mind is so mushy that I just spend five minutes completely in awe of the word Implementationsempfehlungen before I remembered that that's just a basic compound noun
#yesterday i wrote anals of phalliative medicine instead of annals of palliative medicine#god I cant wait for that research to be done#live from the cave
4 notes
·
View notes
Text


23/7/23 // 12.37
Some quick pretty diagrams about vomiting before I go off to camp. Very excited for a few days away but not excited for how tired I will be by the end of it!
#mine#studyblr#studyspo#notes#studying#pharmblr#pharmacy#revision#Maria does diploma#medblr#medicine#palliative care#study space#study notes#biology
25 notes
·
View notes
Text
I dont hate these clients theyre usually nice but i do get frustrated when it seems they dont really understand that their animals are BAD about being handled. lol
#gab gabs#cat does ok with medicine when hes hungry for breakfast.#at night it is extremely difficult to get him his medicine bc hes not as hungry. and he gets pissy and he hides#i had to wait for him to use the litter box and then just grab him when he left it and he was NOT happy lol#sorry dude you have fucking epilepsy.#they're usually fine when all im doing is like. basic animal care. but doing meds with them and any sort of extra palliative care is so hard#the cat has already injured me before lmao#and the dog has put her mouth on me in the past#and this week the snapping is just. too much
2 notes
·
View notes
Text
New on in-House, a captivating piece exploring the interconnectivity of dance and non-verbal communication in the ICU. The piece is authored by The Aseemkala Initiative - a group of brilliant activists presenting diverse dance-based narrative medicine.
https://in-housestaff.org/chinnamastas-do-not-resuscitate-order-using-classical-indian-dance-to-improve-intensive-care-unit-non-verbal-communication-2057
#medblr#pablr#nurseblr#medical school#residency#fellowship#medical humanities#narrative medicine#diversity#palliative care#art#dance#communication#end of life care
2 notes
·
View notes
Text
If your doctor, in almost any setting hasn’t asked you for your goal with your care, then tell them without prompting. They should ask, but everyone gets in a hurry (it’s not an excuse, just a very unfortunate reality) with the case load every specialty in every setting is balancing - in patient & out patient, ER to primary care to cardiology to oncology to nephrology and every else in between. They’re human. They forget. The good ones anyways. The bad ones, and there are bad doctors in every specialty, don’t care.
Advocate for yourself. Call healthcare professionals out. Don’t get steamrolled. Don’t get pressured into doing things you don’t want.
A doctor discovers an important question patients should be asked
This patient isn’t usually mine, but today I’m covering for my partner in our family-practice office, so he has been slipped into my schedule.
Reading his chart, I have an ominous feeling that this visit won’t be simple.
A tall, lanky man with an air of quiet dignity, he is 88. His legs are swollen, and merely talking makes him short of breath.
He suffers from both congestive heart failure and renal failure. It’s a medical Catch-22: When one condition is treated and gets better, the other condition gets worse. His past year has been an endless cycle of medication adjustments carried out by dueling specialists and punctuated by emergency-room visits and hospitalizations.
Hemodialysis would break the medical stalemate, but my patient flatly refuses it. Given his frail health, and the discomfort and inconvenience involved, I can’t blame him.
Now his cardiologist has referred him back to us, his primary-care providers. Why send him here and not to the ER? I wonder fleetingly.
With us is his daughter, who has driven from Philadelphia, an hour away. She seems dutiful but wary, awaiting the clinical wisdom of yet another doctor.
After 30 years of practice, I know that I can’t possibly solve this man’s medical conundrum.
A cardiologist and a nephrologist haven’t been able to help him, I reflect,so how can I? I’m a family doctor, not a magician. I can send him back to the ER, and they’ll admit him to the hospital. But that will just continue the cycle… .
Still, my first instinct is to do something to improve the functioning of his heart and kidneys. I start mulling over the possibilities, knowing all the while that it’s useless to try.
Then I remember a visiting palliative-care physician’s words about caring for the fragile elderly: “We forget to ask patients what they want from their care. What are their goals?”
I pause, then look this frail, dignified man in the eye.
“What are your goals for your care?” I ask. “How can I help you?”
The patient’s desire
My intuition tells me that he, like many patients in their 80s, harbors a fund of hard-won wisdom.
He won’t ask me to fix his kidneys or his heart, I think. He’ll say something noble and poignant: “I’d like to see my great-granddaughter get married next spring,” or “Help me to live long enough so that my wife and I can celebrate our 60th wedding anniversary.”
His daughter, looking tense, also faces her father and waits.
“I would like to be able to walk without falling,” he says. “Falling is horrible.”
This catches me off guard.
That’s all?
But it makes perfect sense. With challenging medical conditions commanding his caregivers’ attention, something as simple as walking is easily overlooked.
A wonderful geriatric nurse practitioner’s words come to mind: “Our goal for younger people is to help them live long and healthy lives; our goal for older patients should be to maximize their function.”
Suddenly I feel that I may be able to help, after all.
“We can order physical therapy — and there’s no need to admit you to the hospital for that,” I suggest, unsure of how this will go over.
He smiles. His daughter sighs with relief.
“He really wants to stay at home,” she says matter-of-factly.
As new as our doctor-patient relationship is, I feel emboldened to tackle the big, unspoken question looming over us.
“I know that you’ve decided against dialysis, and I can understand your decision,” I say. “And with your heart failure getting worse, your health is unlikely to improve.”
He nods.
“We have services designed to help keep you comfortable for whatever time you have left,” I venture. “And you could stay at home.”
Again, his daughter looks relieved. And he seems … well … surprisingly fine with the plan.
I call our hospice service, arranging for a nurse to visit him later today to set up physical therapy and to begin plans to help him to stay comfortable — at home.
Back home
Although I never see him again, over the next few months I sign the order forms faxed by his hospice nurses. I speak once with his granddaughter. It’s somewhat hard on his wife to have him die at home, she says, but he’s adamant that he wants to stay there.
A faxed request for sublingual morphine (used in the terminal stages of dying) prompts me to call to check up on him.
The nurse confirms that he is near death.
I feel a twinge of misgiving: Is his family happy with the process that I set in place? Does our one brief encounter qualify me to be his primary-care provider? Should I visit them all at home?
Two days later, and two months after we first met, I fill out his death certificate.
Looking back, I reflect: He didn’t go back to the hospital, he had no more falls, and he died at home, which is what he wanted. But I wonder if his wife felt the same.
Several months later, a new name appears on my patient schedule: It’s his wife.
“My family all thought I should see you,” she explains.
She, too, is in her late 80s and frail, but independent and mentally sharp. Yes, she is grieving the loss of her husband, and she’s lost some weight. No, she isn’t depressed. Her husband died peacefully at home, and it felt like the right thing for everyone.
“He liked you,” she says.
She’s suffering from fatigue and anemia. About a year ago, a hematologist diagnosed her with myelodysplasia (a bone marrow failure, often terminal). But six months back, she stopped going for medical care.
I ask why.
“They were just doing more and more tests,” she says. “And I wasn’t getting any better.”
Now I know what to do. I look her in the eye and ask:
“What are your goals for your care, and how can I help you?”
-Mitch Kaminski
Source
119K notes
·
View notes
Text
I hope death is like
being carried to your bedroom
when you were a child
& fell asleep on the couch
during a family party.
I hope you can hear the laughter
from the next room
1 note
·
View note
Text
Comprehensive Hospital Services | Balaji Hospital
Explore a wide range of medical services at Balaji Hospital, including specialized treatments, diagnostics, and patient care. Providing quality healthcare for all.

#Palliative medicine#Radiologist#Vascular radiology#Periodical medical examinations#First aid training programs#Intensive Care Medicine#Neurophysician#Neurosurgeon#Cancer#Health awareness programs#Factory act 1948#Guj.Factory rules#Work of H.I.R.A#Vadodara
0 notes
Text




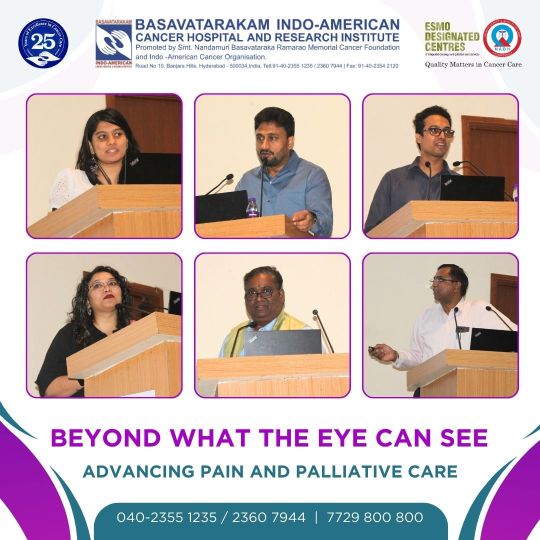




We are delighted to share the successful completion of our CME and Workshop, "Beyond What the Eye Can See," organized by the Department of Pain and Palliative Medicine. This event brought together leading experts and practitioners to share their knowledge and advancements in pain and palliative care.
Eminent speakers presented on a range of topics, including physician approaches, psycho-social and spiritual issues, the role of psychologists, and compassion fatigue among professionals. Interactive panel discussions provided valuable insights into the challenges and future directions in palliative care.
Participants had the opportunity to engage in hands-on ultrasound training, covering the basics of ultrasound, prognostication of palliative patients, venous access, and more. POCUS Stations offered hands-on experience with ultrasound stations, including USG Abdomen, DVT Screening, USG Chest, USG Head and Neck, and Long Term Venous Access and Maintenance.
The event concluded with participants enriched with the latest knowledge and skills in palliative medicine. We extend our heartfelt gratitude to all our speakers, participants, and organizers for making this event a remarkable success. Together, we continue to strive for excellence in compassionate and comprehensive patient care.
Special thanks to our esteemed experts and faculty members: Dr. Vidya Viswanath, Dr. Seema Rao, Dr. Raghu Thota, and Dr. Raghavendra Ramanajulu. We also recognize the efforts of Dr. Praveen Kumar K and Dr. Praneeth Suvvari for organizing this event under the able guidance of Dr. Basanth Kumar Rayani, Chief and HOD of Onco-Anesthesiology.
We also express our sincere gratitude to our CEO, Dr. K Krishnaiah, our Medical Director, Dr. T Subramaneswara Rao, and our Associate Director of Academics, Dr. Kalpana Raghunath, for their unwavering support and leadership.
#painandpalliative #PalliativeCare
#BasavatarakamCancerHospital
#IndoAmericanCancerHospitalHyderabad
#BasavatarakamIndoAmericanCancerHospital
#Pain And Palliative Medicine#Pain and Palliative Care#Palliative care#basavatarakamcancerhospital basavatarakam#basavatarakam cancer hospital#basavatarakam#best cancer treatment in india#basavatarakam hospital#best cancer hospitals in india#best cancer hospital#indo american cancer hospital#indo american hospital#best cancer specialist in india
0 notes
Text
bad news week evidently isn't over yet, my mother's dog likely has cancer, it turns out
#honestly not that surprised. at this point it was the only thing that still made sense#but still. sucks.#haven't seen the pics yet but i trust the vets involved to make an accurate diagnosis#they don't know which type and my mother decided on not putting him through another surgery#especially since it's not even clear if that would change the outcome#so it's palliative medicine now#and well. currently he's responding well to the meds so we'll see for how long this goes#they didn't see anything in that regard four weeks ago so that's rather bad for prognosis but well. it is what it is.#surprisingly calm about all of this. kinda weird. ask me again in three business days#when i'm not fresh out of telling felv cat grandma that she isn't cursed#tw cancer#tw pet illness
1 note
·
View note
Text
Consultant in Palliative Care Medicine
Job title: Consultant in Palliative Care Medicine Company: Job description: Consultant in Palliative Care MedicineRequirements : Experience: With minimum 2 years of experience in the same role Candidate’s Availability: Inside UAE Immediate joining Location : Dubai Expected salary: Location: Dubai Job date: Thu, 25 Jul 2024 05:11:22 GMT
#@Vacany#consultant#Dubai#hiring#Jobs#UAE#Care#job in ajman#jobs in abu dhabi#jobs in dubai#jobs sharjah#Medicine#Palliative
0 notes
Text
Person First, Patient Second
I have tried to reflect on my experiences from my palliative care rotation and have given up several times, not being able to put my thoughts into words. Too many patient interactions and emotional experiences impacted the way I view medicine. Learning about death, dying, and end-of-life care during my last medical school rotation added color to my clinical lens and gave me several vital perspectives that have been etched into how I would like to practice medicine.
One of the primary takeaways I had on palliative was learning to accept the futile efforts of medicine in controlling life’s plans. We often have a work-up and management plan for illnesses that we encounter, but as it turns out, they don’t always work. While that sounds intellectually easy to understand, I was surprised at how difficult it was to emotionally accept while caring for patients, both in chronic and emergent settings. Witnessing illness consume an individual despite aggressive exhaustive medical treatment makes you wonder whether we are doing more harm than good- a core topic that I heard many of my palliative attendings broach with patients during family meetings. Are we prolonging the patient’s life or their suffering?
These questions are tough to process and answer as a family member of someone who went from their baseline functionality to death due to metastatic disease within 11 days. I listened to our patient’s husband try to understand how this happened, how “she was doing fine! Suddenly, she woke up and fell yesterday morning”, how he nit-picked about every recent doctor’s visit, how he told me he was fearful to even step out of the room to use the restroom in fear that his wife may pass away. I had never felt so unhelpful. To my surprise, my only reaction was to put my arms out and hug him.
Exploring whether medical management for a patient should be life-prolonging or palliative helped me understand another fundamental learning point: to meet your patients and their families where they are. I learned that one of the most meaningful ways to do this is to know who your patient is; by that, I mean asking questions to understand their values in life and what they find meaningful. While the importance of getting to know your patients and building rapport is emphasized in medical education, I’m not sure we are provided with the right tools, framework, or knowledge to implement this.
I don’t recall learning what questions to ask to know who my patients are, what is important to them, and, most importantly, how to ask them these questions. I’m not sure this aspect of patient care is necessarily encompassed within the umbrella term “bedside manner.” With this knowledge, I’ve learned you can better provide your perspective and guidance as a physician on the next steps regarding their care and care that best aligns with their values. I used to feel worried that a physician should not provide their opinion on what to do to their patients, that that would be stepping on “patient autonomy,” but truly centering the patient seems to allow you to move with their wave, not against it, and not with an agenda of your own.
I could go on forever about this, but I’ll end with one of my favorite quotes from a patient: “I’m a person first and a patient second. I don’t care if you’re the best doctor in the world; if you can’t see that, then I don’t want to see you.”
0 notes
Text
I missed you quietly today. So quietly that no one noticed.
I missed you as I climbed out of bed and as I brushed my teeth; when I waited at the lights on the drive into work and as I heard the rain outside my window.
I missed you as I ordered lunch and as I kicked off my shoes when I got home; as I switched off the lights and climbed into bed for the night.
I missed you without tears or noise or fanfare.
But oh how I felt it.
I felt it in the morning, at lunchtime, in the evening and at night. I felt it as I woke, as I waited, as I worked. I felt it at home, on the road, in the light, in the dark, in the rain.
I felt it in every one of those moments, each one sitting heavier and heavier as the weight of me missing you kept growing and growing.
Yes, I missed you so quietly today.
But I felt it so loudly.
-Becky Hemsley
0 notes