#Medical Coding Outsourcing Services
Explore tagged Tumblr posts
Text
#Medical Coding Services#Medical Coding Solutions#Medical Coding Outsourcing Services#Medical Coding Company
0 notes
Text
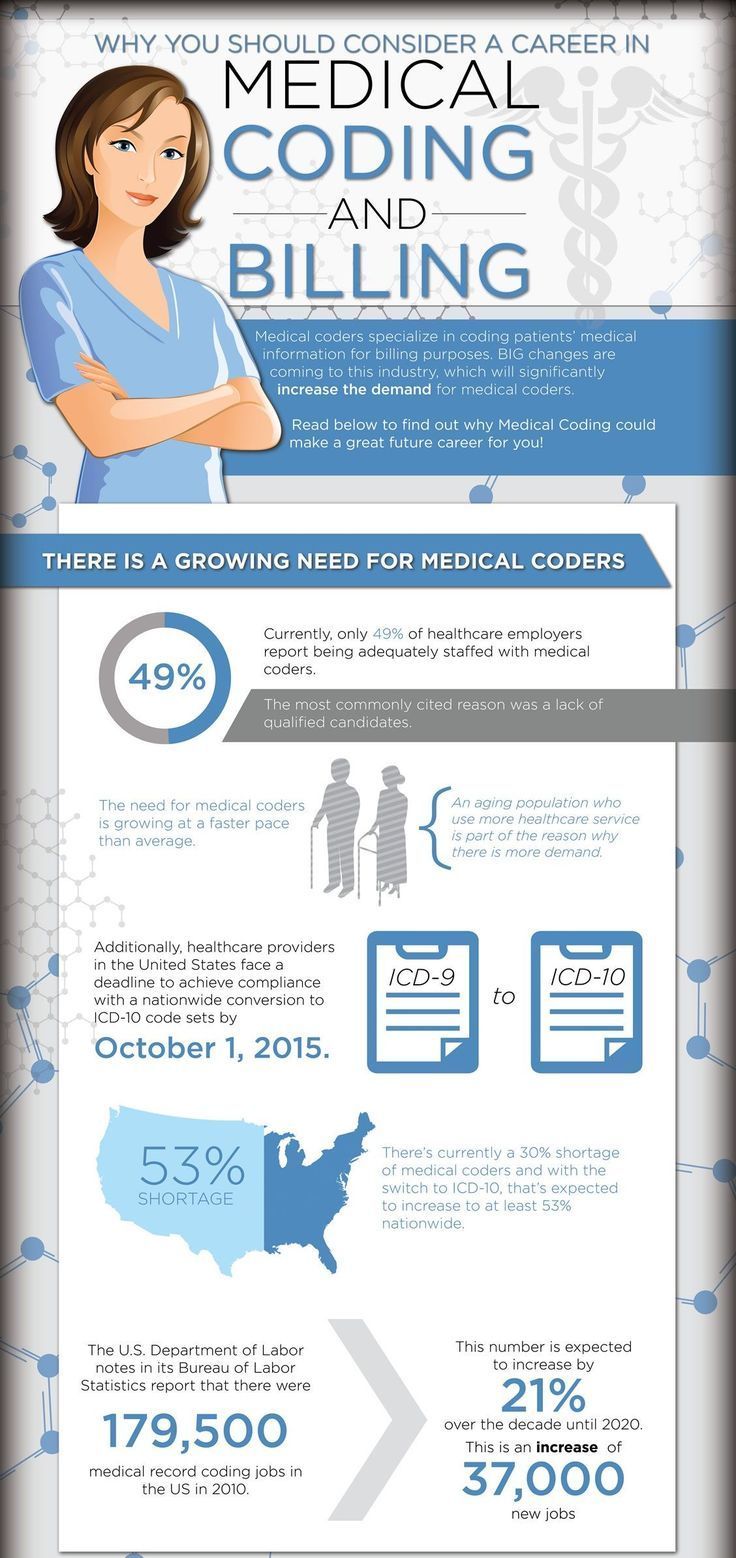
The Role of Medical Coding in Medical Research and Analysis
Source Link: https://theomnibuzz.com/the-role-of-medical-coding-in-medical-research-and-analysis/ In the intricate tapestry of the healthcare landscape, medical coding stands as the linchpin that connects disparate elements into a coherent and actionable whole. It serves as the language that harmonizes the diverse symphony of patient diagnoses, clinical procedures, and treatments, converting…

View On WordPress
#Medical coding#medical coding in medical research#medical coding outsourcing services#Medical Coding Services
0 notes
Link
Get the best medical billing and coding outsourcing services from ecare india. they provides medical billing services more than 20 years.
0 notes
Text
#Healthcare coding and consulting services#Medical Coding Audit in new york#Medical Coding Audit Services in US#Outsource Medical Coding Audit Services in US#Outsource Medical Coding Audit Services#Medical Coding Audit Service Providing Company#Medical Coding Audit Service Provider#Medical Coding Auditing Company#Medical Coding Auditing Company in US
3 notes
·
View notes
Text

I’d rather die than owe medical bills
#I’d rather die than owe medical bills#medical billing services#medical billing company#medical billing and coding#medical billing outsourcing#medical billing agency#medical bills#bills#extortion#exploitation#exploitative#ausgov#politas#auspol#tasgov#taspol#australia#fuck neoliberals#neoliberal capitalism#anthony albanese#albanese government#health#mental health#healthcare#health & fitness#health and wellness#healthylifestyle#class war#fascism#capitalism
3 notes
·
View notes
Text
#Healthcare coding and consulting services#Medical Coding Audit in new york in US#Medical Coding Audit Services in US#Outsource Medical Coding Audit Services in US#Outsource Medical Coding Audit Services#Medical Coding Audit Service Providing Company#Medical Coding Audit Service Provider#Medical Coding Auditing Company#Medical Coding Auditing Company in US
2 notes
·
View notes
Text
CPC COACHING CENTERS IN HYDRERABAD
Thought Flows Academy, revolutionizing medical coding education since 2016, is the preferred destination in Hyderabad. As the top medical coding training institute, our 20,000 success stories and advanced CPC coaching centers make us the epitome of success in south India. Join our 6-year legacy of shaping skilled professionals and unlocking endless opportunities.
#medical billing agencies near me#medical billing outsourcing#medical billing services#medical billing service provider#medical billing company#medical coding#medical billing solutions#medical billing and coding#medical billing software#medical bill
4 notes
·
View notes
Text
Maximizing Reimbursement with CPT Codes
Reimbursement of healthcare services is an easy method of putting CPT codes on claim forms. In reality, it is a complex matter and requires a team approach to accomplish timely filing to receive accurate and fair reimbursement. CPT (Current Procedural Terminology) codes are commonly used in the medical profession to report medical services, procedures, and services of healthcare professionals. These codes play a crucial role in determining reimbursement from insurance companies. CPT (Current Procedural Terminology) codes are critical factors in maximizing reimbursement. The article will discuss some tips that help to optimize reimbursement with the CPT (Current Procedural Terminology) codes. Read More…
For further details and daily updates, Follow us on LinkedIn or Visit.
#medical billing outsourcing#medical billing service companies#healthcare#medical billing solutions#hospital#medical billing florida#physician#cardiology#cpt codes
3 notes
·
View notes
Text

Strategies to Prevent a Medical Coding Audit
Reduce the risk of medical audits by following best practices and ensuring regulatory compliance. Partnering with a medical coding company helps healthcare providers streamline and optimize coding processes.
0 notes
Text
Efficient Billing for Allergy and Immunology Practices

In the specialized field of allergy and immunology, accurate and timely billing is essential to ensure financial stability and compliance with insurance requirements. Medical billing services play a vital role in helping healthcare providers streamline their billing processes, reduce errors, and secure timely reimbursements for their services. Allergy and immunology billing involves complex coding and documentation due to the wide range of diagnostic tests, treatments, and ongoing patient care. In this blog, we’ll explore what allergy and immunology billing services entail, their importance, benefits, and how Mediclaim Management supports healthcare providers in this niche area.
What Are Allergy and Immunology Billing Services?
Allergy and immunology billing services are a subset of Revenue Cycle Management (RCM) services, specifically tailored to the needs of practices treating allergic reactions, asthma, autoimmune disorders, and other immunological conditions. These services encompass the documentation, coding, and submission of claims to insurance providers, ensuring that the unique complexities of this specialty are addressed. Providers often perform intricate diagnostic tests, administer immunotherapy treatments, and manage chronic conditions, all of which require precise coding and compliance with insurance policies. RCM services streamline the billing process, minimize claim denials, and optimize revenue collection for these specialized practices.
The Importance of Allergy and Immunology Billing
In allergy and immunology practices, accurate medical billing and coding are critical to financial health and operational success. Given the intricate nature of immunotherapy, allergy testing, and long-term patient care, improper coding can lead to claim denials, delayed reimbursements, or even non-compliance with regulatory standards. Medical billing and coding ensure that each service provided is translated into the correct procedural codes, enabling seamless claim submissions and reducing the risk of errors. Furthermore, precise billing is essential for tracking patient services and maintaining transparency with insurance providers, which helps build trust and reliability in the billing process.
Benefits of Allergy and Immunology Billing Services
The integration of Healthcare IT services into allergy and immunology billing brings a host of benefits, such as improved accuracy, faster claims processing, and enhanced data security. Automated systems and electronic health records (EHRs) simplify the documentation and coding process, allowing for real-time claim tracking and efficient denial management. Healthcare IT services also provide analytics tools that help providers identify patterns in denied claims, track revenue trends, and implement proactive strategies for financial optimization. By reducing administrative burdens and streamlining billing workflows, Healthcare IT enables healthcare providers to focus more on patient care and less on paperwork.
How Mediclaim Management Enhances Allergy and Immunology Billing
Mediclaim Management specializes in providing tailored allergy and immunology billing services, designed to address the unique challenges faced by practices in this field. Their team of experienced billing professionals ensures accurate coding, timely claim submissions, and effective follow-up with insurance providers. By leveraging advanced technology and expertise, Mediclaim Management helps practices minimize denials, reduce errors, and maintain compliance with billing regulations. Their allergy and immunology billing services not only improve revenue collection but also allow providers to concentrate on delivering exceptional care to their patients.
In conclusion, efficient billing processes are essential for the success of allergy and immunology practices, ensuring timely payments and compliance with complex billing requirements. With Mediclaim Management’s expert allergy and immunology billing services, providers can enhance their financial stability, streamline operations, and focus on improving patient outcomes.
#medical billing agency#medical billing company#medical billing and coding#medical billing outsourcing#medical billing and credentialing services
0 notes
Text
#Medical Coding Services#Medical Coding Solutions#Medical Coding Outsourcing Services#Medical Coding Company
0 notes
Text
The Importance of Medical Coding in the Healthcare Industry
Source Link: https://articlescad.com/the-importance-of-medical-coding-in-the-healthcare-industry-243134.html Medical coding, a seemingly inconspicuous aspect of healthcare administration, wields a far-reaching influence on the entire healthcare industry. At its core, medical coding services serves as the bridge between the intricate world of healthcare and the structured realm of data. It…

View On WordPress
#Importance of medical coding#Medical coding#medical coding outsourcing services#Medical Coding Services
0 notes
Text
How to Find and Hire the Right Virtual Medical Billing Expert in India
To find and hire the right virtual medical billing expert in India, start by identifying your specific billing needs—whether it's insurance claims, coding, or payment processing. Look for professionals with expertise in medical billing software like Kareo or AdvancedMD and knowledge of international healthcare billing standards. Use trusted platforms or agencies specializing in virtual healthcare services to find qualified candidates. Check their experience, qualifications, and past client reviews. Conduct interviews to assess their technical skills and communication. By thoroughly evaluating candidates, you can hire a reliable expert to streamline your billing process and improve cash flow. Contact Hire in Any Domain at 876-633-4467 or email [email protected] to find the right accountant for your business.
#Hire Medical Billing Expert in India#Virtual Medical Billing in India#Medical Billing Experts India#Outsource Medical Billing Services#Medical Billing Solutions India#Hire Virtual Medical Billers#Best Medical Billers in India#Healthcare Billing Services India#Certified Medical Billing Experts#Remote Medical Billing Solutions#Medical Billing and Coding India#Virtual Billing Team#Medical Billing for Healthcare Facilities#Medical Billing Outsourcing India
0 notes
Text
Medical Billing with CPT Codes

Navigating the world of medical billing can be complex, but understanding CPT codes is key to unlocking efficient and accurate billing practices. At Reliable Billing Solutions, we specialize in simplifying the intricacies of medical billing, ensuring you can focus on providing top-notch patient care.
What are CPT Codes?
CPT (Current Procedural Terminology) codes are essential for medical billing. Developed by the American Medical Association (AMA), these codes standardize the reporting of medical procedures and services. Accurate CPT coding is crucial for timely reimbursements and minimizing claim denials.
The Importance of Accurate CPT Coding
Ensuring Compliance: Adhering to the latest CPT coding guidelines helps healthcare providers stay compliant with industry regulations, avoiding potential penalties and audits.
Optimizing Reimbursements: Proper use of CPT codes ensures that healthcare providers receive the correct reimbursement for their services, improving cash flow.
Reducing Errors: Accurate CPT coding minimizes the risk of billing errors, leading to fewer claim denials and re submissions.
Enhancing Patient Trust: Transparent and accurate billing practices build trust with patients, contributing to a positive patient experience.
Key Components of Effective CPT Coding
Regular Training: Keeping billing staff up-to-date with the latest CPT coding changes and guidelines through continuous education and training.
Advanced Software Tools: Utilizing advanced billing software to automate and streamline the coding process, reducing manual errors.
Comprehensive Documentation: Ensuring all medical procedures and services are thoroughly documented to support accurate CPT coding.
Audits and Reviews: Regular internal audits and reviews to identify and correct any coding discrepancies.
Keywords to Enhance SEO
Medical billing CPT codes
CPT coding guidelines
Healthcare billing solutions
Billing software
Revenue cycle management
Conclusion
Mastering the art of medical billing with CPT codes is essential for healthcare providers aiming to streamline their revenue cycle management.
Implementing the strategies mentioned above will lead to accurate reimbursements, improved compliance, and enhanced patient satisfaction.
At Reliable Billing Solutions, we're here to help you navigate the complexities of CPT coding with confidence. Read More
#medical billing services#medical billing company#medical billing outsourcing#medical coding services
1 note
·
View note
Text
Mastering Medical Billing: Essential Tips for Healthcare Providers
Medical billing is more than just a step to be complied with in a healthcare system; it is aimed toward ensuring that there is an orderly flow of funds that enable the providers to be paid appropriately and on time for the services rendered. At Reliable Business Solutions, we constantly endeavor to facilitate medical billing processes in order for health care service providers to stick to their primary purpose – offering hands on care to the patients. In this article we will explore the medical billing dynamics, the challenges faced in this area and how to improve your billing operations. read more

0 notes
Text
The Comprehensive Guide for Medical Electronic Claims Submission

The healthcare industry is constantly evolving, and medical electronic claims submission has emerged as a critical process to streamline billing, reduce errors, and enhance efficiency. For healthcare providers, adopting electronic claims submission is no longer just an option but a necessity to improve revenue cycle management and reduce administrative costs. In this comprehensive guide, we explore the benefits, process, and strategies to optimize medical billing with electronic claims submission, ensuring faster reimbursements and fewer denials.
What is Medical Electronic Claims Submission?
Medical electronic claims submission refers to the process of submitting healthcare claims electronically to insurance companies or payers for reimbursement of medical services. Unlike traditional paper-based methods, electronic submission allows for quicker processing, tracking, and more accurate claim filing. This system integrates with Electronic Health Records (EHR) or Practice Management Systems (PMS) to streamline data entry and eliminate the need for manual input, reducing the likelihood of errors.
The Importance of Electronic Claims Submission in Medical Billing
Speed and Efficiency: Electronic claims submission accelerates the entire billing process. Traditional claims submissions require paperwork, mailing, and manual processing, leading to delays and potential rejections due to incomplete or inaccurate information. By using an electronic system, healthcare providers can automate claims submission, ensuring that the necessary data is correctly formatted and sent to payers immediately.
Reducing Errors: The use of medical billing software reduces the chances of human error. With automated checks for compliance with insurance guidelines and the ability to validate information before submission, electronic claims are less likely to be rejected. Systems often include built-in coding verification tools that flag errors such as incorrect CPT codes, ICD-10 mismatches, or missing data, allowing for corrections before claims are submitted.
Enhanced Tracking and Reporting: Electronic claims submission offers real-time tracking of claims, allowing healthcare providers to monitor the status of each claim from submission to payment. This level of transparency not only improves accountability but also enables quicker identification of any delays or issues. With built-in reporting features, providers can analyze denial patterns, pinpoint inefficiencies, and implement strategies to improve claim approval rates.
Lower Administrative Costs: Submitting claims electronically minimizes the need for paper-based documentation, mailing costs, and manual labor. By adopting an electronic approach, providers can significantly reduce administrative overheads and free up resources to focus on patient care.
Steps to Implementing Medical Electronic Claims Submission
Choose the Right Software: The first step to implementing electronic claims submission is selecting the right medical billing software or Practice Management System. It’s crucial to choose a system that integrates with your existing EHR and offers features like batch claims submission, coding verification, and real-time tracking. Look for software that complies with HIPAA regulations to ensure patient data remains secure.
Train Staff: Transitioning to an electronic system requires proper training for your billing and administrative staff. Ensure that your team is familiar with how to use the software, troubleshoot issues, and keep up with any updates or changes in medical coding requirements. Effective training will help reduce errors and improve the speed at which claims are submitted.
Verify Patient Information: Accurate patient information is essential for successful claims submission. Ensure that all patient demographics, insurance details, and medical histories are up-to-date and correctly entered into the system. Double-checking information before submission will reduce the likelihood of denials due to incomplete or inaccurate data.
Implement a Denial Management Strategy: Even with electronic claims submission, not all claims will be approved on the first attempt. Having a strong denial management strategy in place is critical to improving revenue flow. Use software that allows for denial tracking and appeals automation, so your team can quickly identify reasons for denials and resubmit claims as necessary.
The Future of Medical Electronic Claims Submission
As technology continues to evolve, medical electronic claims submission is expected to become even more efficient and streamlined. Artificial Intelligence (AI) and machine learning are already making an impact on the industry by automating more complex aspects of the billing process, such as claims adjudication and denial prediction. As these technologies advance, they will enable healthcare providers to further reduce administrative burdens and focus more on delivering quality care.
Additionally, the rise of value-based care models will place even more emphasis on accurate and efficient claims processing. Providers will need to ensure that their electronic claims systems can handle the additional complexity associated with these models, which often involve bundled payments and shared savings programs.
Best Practices for Optimizing Your Electronic Claims Submission Process
Medical billing is heavily regulated, and compliance is key to avoiding fines and penalties. Ensure that your staff is up-to-date on any changes to HIPAA regulations, payer policies, or coding standards that may impact the claims submission process.
Auditing your billing process regularly can help you identify inefficiencies and correct them before they affect your revenue. Use your software’s reporting capabilities to generate detailed reports on claim rejections, payment delays, and other key metrics, and use this data to make informed adjustments.
Building strong relationships with insurance payers can help resolve issues more quickly and improve overall claims approval rates. Regular communication with payers ensures that you stay informed of any changes to submission processes or requirements.
Frequently Asked Questions (FAQs)
1- What is the difference between electronic and paper claims submission? Electronic claims submission is faster and more accurate than paper-based methods. It eliminates the need for manual data entry and mailing, leading to fewer errors and quicker processing times. Paper claims can take longer to process and are more prone to human error, resulting in delays and denials.
2- How long does it take for an electronic claim to be processed? Electronic claims are typically processed much faster than paper claims. While paper claims can take up to 30 days to process, electronic claims can be processed in as little as 24-48 hours, depending on the payer.
3- What happens if a claim is rejected? If an electronic claim is rejected, most billing software will provide a reason for the rejection, such as incorrect coding or missing information. Once the error is corrected, the claim can be resubmitted. It's essential to track rejected claims and address issues promptly to ensure timely reimbursement.
4- Are there any compliance requirements for electronic claims submission? Yes, electronic claims submission must comply with HIPAA regulations, which govern the secure handling of patient information. Your software should also meet payer-specific requirements to ensure claims are accepted and processed efficiently.
5- How can I reduce claim denials with electronic submissions? To reduce denials, ensure all patient information, coding, and insurance details are accurate before submission. Using medical billing software with built-in coding verification and real-time tracking can help minimize errors and identify issues early on, reducing the chances of denials.
#medical billing services#medical billing outsourcing#medical billing company#medical billing and coding#medical billing#electronic claims submission#AcuteMD
0 notes