#How Long Does Codeine Stay In System?
Explore tagged Tumblr posts
Text
CREON SNOW
The Prince of Panem.


Creon Snow.
President Snow’s beloved grandson.
The heir.
The mystery boy.
ISTJ
Direct.
Strong-willed.
Dutiful.
Practical.
Jacks-of-all-Trades.
Solitary child.
Likes.
Books. (The smell of them. Favours fiction, mystery and low-key romance.)
Privacy. (Time alone)
Flowers. (Mostly roses)
Spending time with his ‘grandma.’ (Tigris.)
Calmness. (Enjoys the peacefulness of the library)
Drawing. (Secret hobby that’s not really a secret)
Fresh air. (Enjoys the air of the mountains)
Warmth. (Sunshine)
Sleeping late. (Can’t do morning & night howl)
Dry humor (Like his own)
Sweets. (Has a sweet tooth)
Neutral colors. (Mostly black)
Xanthos Dovecote. ( Childhood friend/ best friend)
Dislikes.
Crowds. (Not liking being around a lot of people)
Capitol Parties. (Social burn-out)
Loud people. (Unnecessary noise)
Willful ignorance. (He mostly is self aware)
The Academy. (Hates the uniform)
Genetics. (Despises the subject)
Fakeness. (People who favour him for status)
Fawning (Happens often)
Flair (Not really interested in the glitz and glamour)
Showing his drawings (shy/ insecure about it)
Onions. (No further explanation)
Winter (Ironically, not a fan of the snow)
Annoying people (Xanthos Dovecote & Medea Price)
Creon does not enjoy being the center of attention and often stays in the background. When he must be social, he prefers speaking with one person rather than a group.
While Creon is smart and independent, he does have a few weaknesses. He finds himself easily frustrated and overwhelmed when dealing with overly emotional or needy people. He struggles with social anxiety and is a bit awkward when interacting with new people. He's always unsure of how to act around new people and prefers to avoid any uncomfortable interactions.
Though he has been afforded every luxury since birth, Creon's life isn't all glitz and glamour. He often finds himself out of place amongst the flashy citizens of the Capitol. He appreciates his cushy life, but he also longs for something more meaningful because despite having more material comforts than he could ever possibly need, Creon has never known a true sense of love or belonging. He struggles with his relationship with his family and mostly his grandfather, President Snow. Their relationship is complex and Creon is often unsure of where he stands with him.
As a Capitol citizen and grandson of the president, Creon has a complex understanding of the world around him and recognizes that the Capitol system is far from perfect. Though he is comfortable with his privilege, he also finds the Capitol's flashy lifestyle exhausting. His views on the Hunger Games are complex but for the most part he finds it to be a distasteful event. (He wouldn’t dare to say it out loud, though.)
Fun facts about Creon Snow.
Photographic memory.
Swears he saw a ghost walking around the hallway of his house when he 8.
Needs glasses.
Knows all the 50 digits of pi.
Makes over-exaggerated faces when he doesn't understand a subject of school.
Isn't sure he wants to attend University but knows he doesn't have a choice.
Gets hyperfixate on a book he enjoys. Re-reads most of them soon after finishing them.
Xanthos is his only friend though his family doesn’t like Creon hanging out with him because Xanthos is, for lack of better words, the local dumbass.
Has a tell when lying.
Can’t swallow pills.
Never asks for help; always tries to do everything himself.
When he was younger, he found the Avox to be creepy but after (unintentionally) witnessing how one of them got their tongue cut off he started to feel sorry for them and is discreetly nice to them whenever he can.
Left handed.
Daydreams often.
Angel Of Small Death And The Codeine Scene - HOZIER
I watch the work of my kin, bold and boyful
Toying somewhere between love and abuse
Calling to join them, the wretched and joyful
Shaking the wings of their terrible youths
Freshly disowned in some frozen devotion
No more alone or myself could I be
Lurched like a stray to the arms that were open
No shortage of sordid, no protest from me.
“Snow lands on top, right?”
Creon will be a love interest in my Hunger Games fic, The Worm, if you want to read more about him and his relationship with the MC.
Divider by @firefly-graphics
#the hunger games fic#the hunger games x reader#the hunger games oc#oc#my oc stuff#oc description#coriolanus snow#panem#capitol#the hunger games fanfic#president snow#tigris snow#snow family#ocsnowmale#thg oc
44 notes
·
View notes
Note
jm prompts you say? hmm how about martin hiding an injury and jon freaking out and fussing over him, but with a happy ending?
post-160, jonmartin,hurt/comfort and fluff in some apocalypse-blighted Scottish forest--
Martin realises that he's made a mistake in a sort of chronological tripodal structure of regret.
Primarily, it consists of the dazzling moment when Jon – striding ahead, jaw set and trying to work out where they should have started to go up-hill from the out-of-date ordinance survey map clenched in his hands – suddenly stopped with all the forewarning of a stubbed toe. Holding a hand up to signal that there might be something up ahead in the foliage. Martin, committedly focused on regular breathing and maintaining his ongoing argument with his oesophagus about whether he's going to be sick or not, didn't dodge. Bashing the whole front of his body against Jon's backpack, the arm he's kept so industriously curled up against his chest knocked hard. He thinks he might have made a bitten-off shriek. That shining testament to his mistakes was compounded by his follow-up action, which was to collapse like a felled tree, almost taking Jon down with him, paying fervent and painful homage to the undergrowth with his face.
Mostly he knows that he's really fucked up when he wakes up a few minutes later. Still lying on the ground, and apparently the tent sans-ground sheet has been abruptly set up around him like he's some sort of pop-up installation. The contents of the forest floor have made union with his now knotted hair, and it snags and tugs as he sits up. He can taste grit and dirt in his mouth and there's a stinging dampness on his upper lip. He blinks, coming to terms slowly, and it's then that he realises, just from a brief glance, that Jon is absolutely fuming.
The backpack has been upended without much dignity, its innards rifled through viciously, a platoon of bandages and medicines hastily assembled and called to order off to one side. Jon is hunched, squatted over the spoilers of his ravagings, his fingers gripping two packets of co-codamol that they snaffled from a gutted Lloyds pharmacy near Glasgow, looking for all the world like he's trying to read their instructions like rune-stones.
“J'n?” Martin mumbles blearily, and Jon looks over with all the focus of sunlight caught in glass. Once he's apparently satisfied that Martin isn't in any immediate danger, his glower returns like a storm front.
He should have told him, Martin knows. He should have, he should have. It had been so fast, and it had hurt but it had been manageable and they'd escaped so quickly, he would have told him eventually, he would have.
“Jon, will you,” he says, struggling to stand and failing rather dramatically at it. His apologies form a queue in his throat. “Will you just, Jon, come over here...”
Jon makes a harsh cutting gesture that rather obviously means shut up. He makes it again when Martin makes a token protest, and then – watching Martin's strenuous attempts to rise – forms another gesture and very clearly mouths the word sit.
Jon doesn't talk much these days. Not after Jonah Magnus stole his words from his throat. He avoids anything that might be read as an instruction, a command, a question, which exhaustively limits most of his conversation. He doesn't need to say anything now, not at the moment because usefully he's being really fucking obvious. Stony-faced and cloaked in the miasma of his prickling temper.
Martin flinches when Jon slams something. Jon stops immediately, has the decency to look shamefaced, if mulish, cooling his gestures into perfunctory and quiet actions that can't be read as threatening. He's letting his upset out like a bled radiator and Martin doesn't know what to do.
He passes Martin a water bottle and two small oval tablets expectantly, but quickly realises his own stupidity and takes them back with a frustrated huff. Finally, finally, Jon stops pacing, stops moving, going to his knees and edging closer to where Martin's sitting to help him take the medicine. His rough dry-skinned hand set like a brace at Martin's neck as he carefully tips the water back against his lips for Martin to drink. After he's swallowed, his hand lingers, and after Martin's sheepish thank you, it tentatively moves to thread into the outgrowth of hair at the nape of his neck.
“I'm sorry,” Martin says miserably, his arm now transitioning from smarting to a rather concerted throbbing, and he means it. “I – we needed to keep walking, and there was nowhere safe to stop yet and I know it was – I know I should have....”
Jon's hand has a tremor like a trapped nerve. Martin angles his head to look up at him, and there's messy tracks in the grubby dirt on his cheeks.
“I'm sorry,” Martin repeats, and Jon's head makes port against his own for a second.
“I thought...” comes a raspy, scraping voice, and Jon moves back to study him with wet eyes, and his face twisted in something pained. “I didn't know....”
He doesn't finish the sentence. He sucks in a steadying breathe that doesn't really help before he motions with his hand at the materials he's assembled like a medicinal hunter-gatherer. Martin understands exactly what he's not saying.
“We can't just leave it?” Martin asks, already knowing the answer with dread making a kernel in his stomach. Jon presses his lips tight and shakes his head and looks as though he'd rather do anything else but this.
To his credit, Jon's as professional and mercifully quick as can be expected. He cuts Martin's now swollen, bruise-bright arm out of his sleeve, padding the feverish skin with wadding and gauze without jostling it. He looks right at Martin and exaggeratedly demonstrates that it might be a good idea for Martin to copy his breathing, a deep in-and-out that Martin shakily joins in harmony with. Jon squeezes the unencumbered hand that's curling into a claw against Martin's upper thigh before letting go.
Martin's breathing staggers and slips over into ragged whimpering cry when Jon sets the splint snugly against the injured bone, tries to bury his wet, gasping face into Jon's neck as the stick is tied in place with shoelaces and strips of ripped-up t-shirt at the elbow and wrist. Jon is shushing him, running his hands up and down his back once it's done, his voice plugged up with apologises and despairing, Martin sniffling and hiccuping through the after-shocks.
Martin begins to get drowsy after that, the codeine clearly sneaking into his system and blanketing him in a blissful muted haze, like someone's turned the sound down on the world. Jon takes his meek acceptance of further care as permission to fuss, and briskly rises to the occasion. He brushes out the leaves and small sticks from Martin's hair with a precise and focused intensity until the tangles meet with his internal satisfaction. Soaks a wash-cloth with the dregs of water from the bottle, cleaning away the dirt and small spots of blood from the minor scratches on Martin's face. A measured, stroking left-right motion that leaves Martin blinking heavily, content to half-mindedly watch a host of flickering expressions cross the pathways of Jon's face.
When Jon's done, he looks solemnly over his handiwork like he's overseeing some great project, sealing the act with a dry kiss against Martin's cheek.
“C'mere,” Martin slurs dozily, and Jon enfolds against him like two seas merging, careful not to knock his arm. The ground beneath them is chill, will turn frosty as it dips into nightfall, and they can't stay here, they've got miles to go before the nearest town, they're fast losing light.
Martin tries to say this, or he thinks he does, but Jon shushes him again and kisses the space between left eyebrow and hairline, over the cuts on his cheek that have long stopped smarting.
Jon doesn't tell him to rest. To close his eyes. Jon doesn't tell him to do anything any more, doesn't trust himself with it. But his body is still knelt down as a bedrock, and Martin thinks he might be rocking them both ever so faintly, his fingers trailing ouroboros maps into the weft of his newly combed hair. Martin takes it as permission enough.
361 notes
·
View notes
Text
Top Surgery Experience
Okay, so I said I would do a write up of my top surgery experience and I’ve finally gotten around to it. Uni started right after so I’ve been fairly frazzled.
Please feel free to ask any questions you may have! I’ll do my best to answer them.
To start with, I currently live in NSW, Australia. There are a few Australian top surgeons, but as a NSW resident my best bet was Dr Steven Merten, with Pure Aesthetics in Sydney. Because Australia has a public healthcare system I was able to get my top surgery under that scheme. As far as I’m aware Dr Merten is the only top surgeon who offers this surgery through the public system. He works in partnership with Concord Hospital in Sydney, and that’s where I had my surgery. If you go privately there are other options for the hospital you stay at. There are pros and cons to the public system, which I’ll detail below.
Pros:
I paid $500~ out of pocket instead of between $5k and $10k (if you have private health insurance it may cover some)
Since he’s in my state I didn’t have to travel far
He’s one of the most experienced top surgeons in the state
there’s two places for appointments, either at his clinic or at the Macquarie uni rooms
Cons:
because I went publicly he didn’t perform the surgery personally, rather a registrar did. However, he was in the room the entire time overseeing the operation.
because he’s so popular I had to wait a full year from the first consultation to the actual surgery date
it was extremely hard to get onto the wait list due to how popular he is.
the public system is only available to NSW residents over 18
I was lucky in that my GP at the time knew him professionally and called in a favour so that I knew the moment his books were open, and I am forever grateful for that. It is MUCH easier to get an appointment with him through the private system, but that’s a lot more expensive. For me, the pros far outweighed the cons here, and I decided I could wait a year for my surgery. I had also intended to lose weight beforehand, but that didn’t happen. Woops.
Prior to my first consultation I needed a referral both from my GP, and a registered psychologist or psychiatrist detailing my transition and documented dysphoria surrounding my breasts. The first consultation was $300 iirc, and I paid a $100 deposit, so only paid $200 on the day. Medicare also gave me a $100-something rebate.
The first consultation was fairly quick. He asked some questions about my transition, what my expectations were regarding surgery, detailed my options, and explained the procedures. He measured my breasts, but never touched me (I kinda just picked them up and moved them where he asked). He also took a photo of my chest, with my consent.
I didn’t actually hear from them until about three months before my surgery because my details got lost, but USUALLY the hospital will get in contact with you regarding your surgery date, what you should expect, and when your pre-op consultation is. I also had to fill out a pre-op health questionnaire and personal details. Due to my high level of haemoglobin as a side effect of T, I was required to provide them with more recent blood test results, but you may not have to do this. Usually there is also a pre-op appointment with the nurses and anethetist at the hospital, but the nurse I spoke to said that I didn’t need to go if I didn’t have any pressing concerns.
My pre-op consult with Dr Merten was a couple of weeks before my surgery, however, it’s usually around the same time. This one was $100, and I also had to pay $130 for a medical compression vest which I have to wear for up to three weeks post-op. Again, Medicare partially reimbursed my consultation fee, but not the vest.
During this consultation we basically covered the same things, and I also saw a nurse who told me what medications to avoid, and briefed me on post op care. She also gave me my medical vest, wound tape, and some pamphlets.
Some things she covered:
smokers should stop smoking 12 weeks before surgery
you should limit your alcohol intake the week before surgery, and don’t drink alcohol AT ALL during the two days immediately prior to surgery
no herbal medications, asparin, ibuprofen, or other blood thinners for two weeks prior to surgery. IF YOU ARE ON BLOOD THINNERS FOR MEDICAL REASONS THIS MAY BE DIFFERENT FOR YOU.
do not eat or drink anything from midnight the night before your surgery. Morning medication (antidepressants in my case) can be taken with a sip of water.
the night before and morning of surgery I had to shower with a special soap that was provided in order to kill bacteria on my skin.
I did have to call the admissions centre the day before my surgery to confirm my appointment time. For me it was 8:30. Before going in I had a brief interview with a nurse, who took down my details and checked me for allergies and medical conditions. I was given my wrist bands (red, since I have a codeine allergy), and directed up to where I would meet the nurses. There I changed into the operating gown (you can keep your undies on) and compression socks due to my weight.
I was taken to a prep room before the operating theatre where Dr Merten marked my chest. Basically where things would be cut, lipo’d, etc. I was feeling nervous so the anethetist also came in, did my canula and gave me something to relax (don’t know what it was). He was extremely kind and friendly, and said he was honoured to be included in this part of my journey, which I honestly thought was an incredibly sweet thing to say, and I’m very grateful for how he looked after me.
The relaxation shit kinda made me dopey, and pretty much immediately I was wheeled into the theatre. They had me wriggle from the bed onto the table, I nearly fell off, but it was all good. I don’t really remember much from here, but there was some music playing, and the nurses and registrar were setting up.
At this point the anethetist put the mask on and told me to take some deep breaths. I remember it tasting and smelling really weird, and the next thing I know I was waking up in recovery.
I’m not sure how long I was in recovery for because I kept drifting in and out, but they gave me something for the pain and then wheeled me to the ward. I started waking up properly around this time, had a chat with the people transporting me, and by the time I was in the ward I was fully alert (and really needed to pee).
Because of my size and the way the surgery worked out, I did have a few staples at the ends of my incisions, and I also had to put the compression vest on. I also had drains, with bags that needed to be changed every twelve hours. Nurses would also come and take my blood pressure and check that everything was okay and that I wasn’t in too much pain. They were all extremely welcoming and accepting, never misgendered me once, and even double checked my name and pronouns to ensure that everyone knew. My mate was also allowed to stay with me pretty much the whole day until dinner, which really helped me cos I’m bad with hospitals.
After surgery I was stiff and ached a little, but there wasn’t too much pain. I was able to go to the toilet myself, although wiping was very difficult for the first week.
I stayed overnight, and was discharged the next day. They gave me anti-inflammatories, antibiotics, and some opiates to help the pain. I should note here that I do have an extremely high pain tolerance, so outside of days where I pushed myself a bit too far, I generally didn’t need to use them.
I’m unsure if my experience is unusual, as I was able to do pretty much everything immediately post-op. Of course, I’ve been taking it easy, but dressing, sleeping, cooking, moving, has all so far been generally okay. I have had some pain on days where I moved about too much, or sat up too much, but that’s also partially chronic pain flaring up due to my bad back.
I was discharged with my drains still in, as I’m a bleeder. Usually with Dr Merten they’re removed before discharge, but I was sent home with some bags and instructed to change them every 24 hours and keep a record of how much had drained. I think I wound up keeping my drains in for around a week before they were removed.
I went to the medical centre twice to have my dressings changed and drains checked (and eventually removed), and was sent home with a sterile staple remover for my GP to remove my staples with. They’ll be coming out at the end of the week. The drains didn’t hurt when removed, it just felt like an odd tugging sensation. The stitches Dr Merten used are dissolving ones, so no need to get them taken out.
I do have to change my nipple dressings every three days, and the tape on my incisions can stay on for up to a week. The stuff I use is extremely strong and has glue on it, so I’m a bit hesitant to change it on my own (nearly ripped a staple out last time I changed my dressings).
I’m roughly three weeks post-op now, and I have pretty much all my mobility back. Showering is difficult, as is bending over or reaching to one side (tugs on my incisions). There is pain when I do things, but unless something actively tugs at, touches, or puts pressure on my wounds I’m not in any pain. Mostly its just an annoyance at this stage.
I’m still sleeping on my back, although I can lie on my side for short periods of time. There’s some bruising around my armpits where I had liposuction, and there is a small numb patch on my left side. I can’t feel my nipples, but I also couldn’t feel them prior to this so it’s not a huge loss.
I’ve seen some people say that they felt depressed post-op because of a hormone fluctuation, but personally when I saw my chest it felt natural and right. I didn’t cry (not a big crier) and I wasn’t surprised or shocked or… overwhelmed. To me it was my outer body finally reflecting my inner self. I already looked like this in my own mind, so it was just natural that it looks the way it does post-op.
Unfortunately some dysmorphia and self-esteem issues surrounding my weight have resurfaced, but that’s not really related to the top surgery, and it’s something I’m able to work on as I recover.
If there’s something I haven’t covered that you’re curious about, please send an ask! I’ve tried to be as thorough as possible, but its been a few weeks and some details are fuzzy.
15 notes
·
View notes
Text
How Long Does Heroin Stay in your System?
Like other hard drugs, heroin is a highly addictive and dangerous illegal substance obtained from the seed pods of the opium poppy plant. Due to its adverse effects on human health, it is indubitably illegal to grow opium poppies in many countries. However, India, China, Korea, and Japan make the major exceptions by legally producing opium gum. Mexico, Colombia, Southeast, and Southwest Asia are also among the world’s largest opium suppliers. The opium poppy plant produces a milky latex found in unripe seed capsules which are processed to produce morphine, codeine, and heroin.

Now that we know where the substance originates from, let’s look into some of its other features.
What does heroin look like?
According to the National Institute on Drug Abuse (NIDA), heroin is sold as a white or brownish powder that dealers ‘cut’ with impurities of sugar, painkillers, powdered milk, quinine, or starch. This is majorly to increase the quantity of the product and thus, make more profit. A rather common impurity known as fentanyl is added to heroin to reduce the risk of overdose and increase the potency of the substance. Owing to its wide range of impurities, the drug has acquired various street names over the years including: - Junk - Horse - White horse - Smack - Skag - Dope - China white - Brown sugar Pure heroin is a white, pink, brown, or beige powder (depending on the reagents used to process it) known as diamorphine hydrochloride/ white heroin. It is a highly refined form of heroin and has a bitter taste. Other than white heroin, there are several other forms of heroin, such as: - Black tar heroin – this type differs from powder heroin in that it has a tar-like appearance with a sticky feel and is dark brown or black. Being cheaper and easier to produce, it is less costly than the rest. - Asian heroin – depending on its origin, it can either be powdered, white, and highly soluble in water to indicate Southeast Asian origin, or course brown powdered with poor solubility in water to indicate Southwest Asian origin. - Brown heroin – is not as refined as white heroin and is produced in its first stage of purification. This makes it cheaper and easier to produce.
How is heroin used?

Heroin can be injected, snorted, sniffed, or smoked. White heroin, due to its high quality, is usually injected or snorted because of its high-temperature requirement which makes it harder to burn and smoke. Black tar, brown and Asian forms of heroin can be melted down and injected, or smoked.
Side effects of heroin
Although there are different forms of heroin, their side effects are pretty much the same. At a glance, some of the common immediate side effects of heroin include: - Nausea or vomiting; - A rush of relaxation or pleasure; - Low sex drive; - Poor motor skills; - Dry mouth; - Shallow breathing and a slow heart rate; - Drowsiness; - Warm skin; - Narrowing of pupils. The intensity of these effects, however, may differ depending on the following factors: - Dosage ingested. - Quality of substance ingested. - Height and weight of the user. - Body fat content. - Genetics - Hydration - Rate of metabolic reactions. How long does it take for heroin to hit? Essentially, the effects of heroin are felt within the first few minutes of ingestion. The most perceptible being euphoria. These effects may last for the next 45 minutes – one or two hours before wearing off. Nonetheless, depending on the amount ingested and quality, a heroin high may last longer. How long does heroin last in the body? Research reveals that heroin has an average half-life of about three to eight minutes. This implies that within this time, 50% of the initial volume ingested would have been broken down. Generally, it takes 4-5 half-lives for a drug to be completely eliminated from the system. Therefore, in about 30-40 minutes, all heroin will have been flushed out of your system. Once broken down, two compounds are formed; morphine and 6-acetyl morphine, the former of which has a longer half-life. Various drug testing methods are employed in the detection of heroin in the body for varying periods. Each test type has its own duration under which heroin can still be detected in the body. Urine test Commonly known as urine drug screening (UDS), it is the most commonly administered drug test. With a urine sample, one can detect traces of heroin (or morphine) within one to four days since the last use. To know how to collect a urine sample and submit it for testing click here. Saliva test This is a rather quick method with quick results. Due to this, it should be administered soon after the last use of heroin for accurate results. For this reason, a saliva test for heroin can only be valid an hour after the last consumption. Blood test Heroin metabolites can be detected in blood within two to three days since last use. Previous studies reveal that the 6-acetyl morphine (6 AM) assay test can distinguish between recent heroin use and therapeutic use of opioids as painkillers. Hair test Frequent heroin users with long hair have a larger window of detection as the 6 AM metabolite remains detectable in hair follicles for up to 90 days since last use. For more information on drug testing methods, visit our blog. False-positive A false positive drug test result is likely to occur following the ingestion of foods containing poppy seeds. Poppy seeds may contain opiate residues, which even by a small amount may trigger false-positive results. Alternatively, certain medications such as rifampin and diphenhydramine may trigger similar results for opiate testing. How to flash heroin out of your body As earlier mentioned, heroin metabolizes darn quickly and will, therefore, be out of sight for the majority of the standard drug testing methods. This is good news for a novice user. Therefore, you can only clean your system off of heroin by avoiding continuous usage of the illicit drug once the body eliminates it through metabolic processes. However, for an addict, it is dangerous to quit cold turkey as this would trigger severe withdrawal symptoms. It is advisable to enroll in a rehabilitation center or seek professional help for sound treatment plans. Read the full article
0 notes
Text
Understanding Naloxone
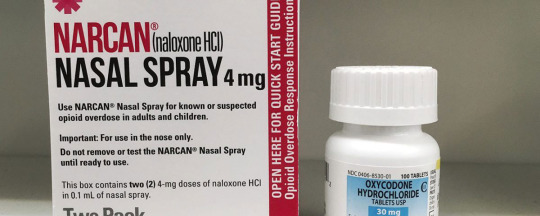
The opioid epidemic that started in the late 1990s continues to be a serious concern in the United States. The increase in prescription opioids resulted in many patients developing tolerance and dependence on them. As a result, opioid abuse has become a widespread problem. In response to this crisis, there have been efforts to combat opioid abuse. One of the ways to address this issue is through the use of naloxone. This medication can be lifesaving, yet many people are not aware of its benefits. In this ultimate guide to naloxone, we will explore what it is used for, how it works, its side effects, and which version is better.
What Is Naloxone Used For?
Naloxone is a medication that is used to reverse an opioid overdose. It has been approved by the Food and Drug Administration (FDA) as a safe and effective way to reverse the effects of an opioid overdose. When administered, naloxone gives people enough time to get medical attention, which can be lifesaving. The drug is beneficial to individuals who struggle with opioid abuse or take high doses of opioids for pain. However, naloxone is not a formal kind of treatment for opioid dependence. Individuals who have struggled with opioid addiction can begin their recovery with medically monitored detox, which provides patients with 24-hour care and medical assistance as needed.
How Does Naloxone Work?
Naloxone is an opioid antagonist that blocks the effects of opioids. It can be used as a nasal spray, injected into the muscle, injected under the skin, or injected into the veins. When administered, naloxone works by binding to opioid receptors, reversing and blocking the effect of opioids like heroin, morphine, fentanyl, oxycodone, codeine, hydromorphone, hydrocodone, buprenorphine, and methadone. It is important to note that naloxone cannot be used to treat overdose caused by substances like alcohol, cocaine, methamphetamine, or benzodiazepines.
What Are The Side Effects Of Naloxone?
Naloxone does not cause side effects in an individual who is not overdosing or does not have opioids in their system. However, when administered to individuals who abuse opioids or have an opioid addiction, naloxone can cause withdrawal symptoms. The more naloxone medicine is given, the more intense these symptoms would be. These symptoms usually subside after half an hour to an hour. The side effects of naloxone include flushed skin, dizziness, fatigue, restlessness, anxiety, irritability, body aches, diarrhea, stomach pains, fever, and shortness of breath. It is important to note that these side effects are opioid withdrawal symptoms and would not occur in a person who is not overdosing or who does not have opioids in their system.
How Long Does Naloxone Stay In Your System?
Naloxone may stay in your system for 30 minutes to 12 hours. The duration of its effects is dependent on the dose and the severity of the individual’s condition, as well as their weight and height. Since naloxone is a fast-acting and temporary solution for opioid overdose, it mitigates overdose symptoms to give the individual enough time to receive medical assistance.
1 note
·
View note
Text
How Long Does Soma (Carisoprodol) Stay in Your System?
What is Soma (Carisoprodol)
Soma (Carisoprodol) is a generic brand Pain relief medication that is sold in the market, while Carisoprodol is its generic name. The medication has muscle relaxing properties that create a barrier wall against the painful sensations transmitting between the nerves and the brain.
Common side effects include headache, dizziness, and sleepiness.Serious side effects may include addiction, allergic reactions, and seizures. In people with a sulfa allergy certain formulations may result in problems. Safety during pregnancy and breastfeeding is not clear. How it works is not clear. Some of its effects are believed to occur following being converted into meprobamate.

While it varies for each person, Soma usually stays in your system for an average of 11 hours. Soma metabolites remain in your system for up to four days after you stop taking it.
Standard drug tests do not screen for Soma, so it is only detectable if a person is specifically tested for it. Soma may be detectable on some tests for up to a month.
Blood: Around 24 hours
Urine: Several days
Hair: Up to a month
Factors That Affect How Long Soma Will Stay In The System
Soma is believed to affect GABA receptors in the brain and, in doing so, it changes how nerve signals are sent. The drug is a central nervous system depressant. This means that people may feel drowsy or intoxicated when using Soma -particularly at higher doses. Some of the side effects of Soma can include sedation, dizziness and headaches. If someone takes too much Soma, they can overdose. Signs of a Soma overdose can include confusion, problems breathing, hallucinations, muscle stiffness, uncontrolled eye movements and weakness of the arms and legs.
Although the half-life of Soma can be approximated, the estimated time on how long it stays in the body varies from individual to individual and depends on some factors.
Several Variables Can Influence the Time This Medication Stays in the System, Such As:
Dosage
How it was used
Frequency of administration
Metabolism rate
Age
Body mass and weight
Food intake
Water amount in the body
Liver and kidney health
Side Effects of Soma (Carisoprodol)
Soma can have side effects. Some of the most common include:
Confusion
Drowsiness
Fast heartbeat
Headache
Skin rash
Slowed thinking
Sluggish movements
Upset stomach
Soma can make you drowsy, so it's important to take precautions for driving or operating machinery.
Carisoprodol 350mg Precautions

Carisoprodol, when interacted with other drugs, could lead to a severe impact on your health. It is advisable to have a word with your doctor regarding your current medications or past medical history. Tell your physician about other complementary medicines you may use for strength or muscle building, such as vitamins, muscle gaining supplements, steroids, or protein powder. Combining carisoprodol, aspirin, and codeine may also lead to serious drug interactions.
Do not forget to inform, if you had a history of addiction, abuse, or have used antidepressants and tranquillisers in your past. This proactive discussion will help you to protect yourself from drug interactions and adverse reactions.
If you are an asthma patient or have lung disorders, you should try to have alternative medication which will have a lesser impact on respiratory depression. Also, stop drinking adulterated drinks while you are on course, as Carisoprodol 350mg may get you high, with boosted sedative feeling.
Before initiating your first dose, make sure to read the label carefully. Verify the expiry date and look for ingredients to know if you are allergic to any of them. Read the doctor’s private prescription and follow the instructions given to avoid Carisoprodol abuse.
0 notes
Text
Tapaday 200mg
Tapaday 200mg Tablet is a pain reliever for individuals who have tried and failed with other medications.
Medical research shows it to be effective for a wide range of ailments, including migraine headaches, fever symptoms such as clammy skin and sweaty palms, cramping in the lower abdomen during menstruation, and toothaches caused by dental plaque buildup on the gums near the root canal, which is where the nerves are located in the tooth.
When mucus gets stuck in your throat, traditional medicines may not be able to help much with sore throats and swallowing problems, but Tapaday does.
It includes tapentadol hydrochloride hydrate.
What's involved in the process?
The FDA has approved Tapaday 200 mg as a brand-new painkiller.
When we take tapapdlay, our "pain receptors," which are located in our brains, are told not to respond as they normally would, so we don't experience any pain at all.
Only those with a strong tolerance for pain and long-term discomfort can benefit from taking Tapaday extended-release pills.
Morphine and codeine are also opioid painkillers like tapentadol that work by changing how your brain reacts to pain.
When should I take Tapaday 200 mg?
In order to alleviate discomfort, patients might take Tapaday 200 mg orally.
Doctors recommend taking it with food every 4-6 hours, depending on the severity of your ailment and the length of time you have been having symptoms.
To avoid unpleasant side effects including nausea, vomiting, and a rise in blood pressure, never take more than the recommended dose of Tapaday 200 mg without first contacting your doctor.
Also, the best way to take the medicine is by swallowing it whole with a glass of water.
If you aren't getting any comfort from Tapaday reviews, your doctor may need to modify your dosage.
Make a phone call if this is the case, and they'll find a solution!
Buy Tapaday 200mg, doctors prescribe specific treatment guidelines that must be followed closely in order for the patient to avoid overdosing or becoming addicted. Only after consulting with your physician should you decide if changing dosages may benefit you more than staying on track with what was prescribed initially.
It's always a good idea to check their website for the Medication Guide for all of the components if you're concerned that anything in it might trigger an allergic reaction.
If you've tried it, discuss your results with your physician.
The illness of the kidneys
Disorders of the central nervous system
Breathing problems
A condition affecting the gallbladder
Cirrhosis of the liver
Your doctor needs to know if you're taking any of the following drugs while you're taking this medicine.
The following interactions were chosen because they could be important, but the list is by no means complete.
It is possible that an interaction between two pharmaceuticals is necessary in some situations, even if certain medications should never be used together.
When a doctor finds out that a patient is also taking one of the above-mentioned drugs along with their own medication, they will usually ask that the patient's dose be changed or that something else be done to keep them safe.
Buy tapaday online tablet treats severe pain like acute, injury, surgery, chronic and musculoskeletal pain at Genericshub.com
0 notes
Link
It’s an opioid medication whose generic name is Hydrocodone while it is sold in the market with the brand name of Hysingla. A patient can buy hydrocodone online from any of the trusted online medical stores.
What is Hydrocodone used for?
This medication is used for treating severe pain of a prolonged duration if other measures are not sufficient. Its other use includes using it as a cough suppressant in the adults.
How long does Hydrocodone stay in your system?
The pain relief effect of Hydrocodone will wear off within four to six hours. But the presence of drugs may still be detected in the saliva for up to 36 hours, in urine for four days and in the hair for 90 days after the last dose.
How to take the dosage of Hydrocodone?
The intake of Hydrocodone medication can be habit-forming thus it should be taken exactly as directed. Thus this point should be kept in mind while buying Hydrocodone online from any of the online medical stores.
While taking Hydrocodone to discuss with your doctor about your pain treatment goals, length of treatment and other ways to manage the pain. The patient should not fully crush or chew the extended-release capsules. This may cause serious problems, including overdose and death in the worst condition.
What are the Hydrocodone possible side effects?
If the patient is not taking Hydrocodone as told by the doctor then they may face certain side effects. Below are a few side effects of Hydrocodone:-
Sleepy
Dizzy
Lightheadedness
Nausea
Vomiting
Constipation
Severe headache
Increased urination
Visual disturbances
Hydrocodone Bitartrate
This is made from Codeine and it binds to opioid receptors in the central nervous system. It is a type of analgesic agent, a type of antitussive and a type of opiate.
Difference between oxycodone & Hydrocodone
Oxycodone is a semi-synthetic and is synthesized from thebaine (an opium alkaloid) and will only relieve pain, not cough while Hydrocodone is also semi-synthetic but it is derived from Codeine and while more potent than Codeine, stills retain cough suppressant properties.
Hydrocodone Paracetamol interactions
Hydrocodone Paracetamol is a high power drug thus take it with extra caution. Hydrocodone Paracetamol does interact with several medications listed below:-
Acetaminophen
Ambien
Aspirin low strength
Celebrex
Cymbalta
Ibuprofen
Lyrica
Tylenol
Zyrtec
Synthroid
Vitamin B12
Is Hydrocodone a narcotic?
Hydrocodone is a narcotic pain reliever and a cough suppressant, similar to Codeine. Hydrocodone blocks the receptors on nerve
cells in the brain that give rise to the sensation of the pain. Acetaminophen is a non-narcotic analgesic (pain reliever) and antipyretic (fever reducer).
Hydrocodone & Alcohol
Combining the prescription opioid Hydrocodone with alcohol can produce a range of health effects, from Drowsiness to severe liver problems. In some cases, drinking while using medication can lead to death. Alcohol increases the effects of opioids on the central nervous system. Consuming painkillers and Alcohol together produces sedative effects causing people to feel extremely tired.
Hydrocodone for dogs
The use of Hydrocodone is primarily as a cough suppressant ( antitussive ) in dogs, working on receptors within the brain. Hydrocodone is often paired with another drug, homatropine, mostly for purpose of preventing abuse.
Which is stronger oxycodone or Hydrocodone?
Both oxycodone and Hydrocodone are powerful painkillers and they have been shown to be highly effective at treating pain. A study shows that a combination of oxycodone and acetaminophen was 1.5 times more potent than hydrocodone with acetaminophen when taken at equal doses.
Hydrocodone withdrawal
Hydrocodone is known to produce painful withdrawal symptoms (akin to a very severe flu) in people with chemical dependency or addiction that may need a detox. The withdrawal symptoms of Hydrocodone are essentially the opposite of the effects that the drug produces. The withdrawal of Hydrocodone induces depression. They experience a significant amount of discomfort as the brain and body learn to function without Hydrocodone. It includes withdrawal symptoms such as Nausea and physical pain.
0 notes
Text
How to Avoid the Opioid Epidemic (for Dentists, Patients, and Families)
Saturday, April 27, 2019 is National Prescription Drug Takeback Day. Between 10 AM—2 PM, you can turn in unused prescription drugs, including opioids, at locations throughout the United States. Check out Google’s Location Finder for a location near you.
You may have heard of the “opioid epidemic” rumbling through our nation, but what does that term mean?
If you’re unfamiliar with this crisis in the United States, it may shock you to learn that dental offices can be starting points for this epidemic.
Let’s look at how this works for everyone from the dentist to the patient (and those in between). There is hope for opioid addiction.
What are opioids?
Dentists often prescribe opioids for pain management after surgeries or major procedures. It’s a convenient choice, since opioids are a class of drugs that have pain-blocking qualities. Unfortunately, improperly using these pills can have lasting, devastating consequences.
It’s possible to become addicted to opioids in as little as five days. (1)
Despite this, many dental opioid prescriptions can last for up to 10 days. The severity of this prescription issue makes it important for dentists, dental patients, and their loved ones to learn more. Your knowledge could be the difference between a routine prescription and a painful battle with opioid addiction.
You can stay safe from the opioid epidemic by knowing the risks of using opioids, educating yourself on taking prescribed opioids correctly, and understanding what to do if addiction takes hold.
List of Opioids Prescribed in Dentistry
The following are opioid drugs often prescribed for pain management by dentists:
Hydrocodone (Vicodin)—The prescription rate for this drug doubled between 1999 and 2011.
Oxycodone (Percocet® or OxyContin®)—This prescription rate increased 500% in the same timeframe. (2)
Acetaminophen with codeine (Tylenol® No. 3 and Tylenol® No. 4).
Opioids also branch beyond prescribed medications. Other forms include heroin, morphine, tramadol, and synthetic opioids like Fentanyl (Duragesic). Though each of these opioids vary in strength, they all have addictive qualities and harmful effects if used long-term.
According to the Centers for Disease Control and Prevention, the U.S. is in the midst of the “worst drug overdose epidemic in history.” (3)
Unfortunately, the data shows that prescription rates for opioids are still climbing. The government, researchers, and dental experts all warn against prescribing unnecessary opioids. Instead, they are urging patients to consider other viable options for pain relief.
What is the opioid epidemic?
The opioid epidemic is caused, in part, by nonmedical use of prescription drugs. This may include: (4)
Taking a larger prescription than needed
Using drugs prescribed to someone else
Taking your prescription with alcohol or other legal or illegal drugs
Abusing prescription drugs to feel a sense of euphoria—this behavior is much more likely to occur with opioid pain relievers than with other medicines
Due to their addictive nature, these pills are in high demand, and not always for medicinal use. What’s the delineation between necessary and nonmedicinal use? Well, for one, the effect on the user’s life.
The definition of opioid use disorder is a pattern of misuse that leads to emotional or functional distress.
A simple study of third molar extractions reveals how sinister this issue can be. A recent study found that young Americans prescribed opioids for their wisdom teeth were at greater risk for addiction.
Patients who filled their opioid prescription had a 13% chance of persistent opioid use. This puts them at high risk of addiction. On the other hand, only 5% of patients who didn’t fill their prescription struggled with long-term opioid issues. (5)
Statistics like these are why I urge dentists and their patients to consider choosing anti-inflammatory drugs or non-opioid pain relievers. One prescription, especially in younger people, can have long-term effects. Consider several options before jumping immediately to opioid prescribing with addictive potential.
If prescriptions for opioids slow down, this epidemic may as well.
Opioid Abuse Statistics
How many people abuse opioids?
In 2016, the U.S. Department of Health and Human Services (HHS) found that 11.8 million people over the age of 12 misused opioids. 2.3 million had begun the habit within the past year, highlighting the growing epidemic. (6)
Prescription Opioids vs. Heroin
In 2016, 11.5 million Americans misused prescription opioids, a number far greater than the 948,000 who had used heroin. That’s an astronomical difference in users.
Unfortunately, only 17.5% of those addicted to opioid painkillers sought professional help. This totals far less recovery treatment per capita than those fighting a heroin addiction. (7)
Both are issues of drug abuse, but for some reason, opioid drug users aren’t seeking help like they should. Perhaps this is due to the fact opioid addiction affects people who don’t seem like drug abusers, or because the addiction began with a legal prescription. Whatever the reason, the statistics are alarming.
Can prescribed opioids function as a gateway drug?
In a recent interview with heroin users entering treatment, 80% had abused prescription opioids before turning to heroin. (8) These numbers highlight that opioid use is a road that can lead to other harmful narcotics.
Substance abuse is always a real threat. Prescribed opioids present no less inherent danger and can lead to other addictions.
Can prescribed opioids hurt my job performance?
Research has linked an increase in opioid prescriptions to a decrease in the number of people participating in the labor force. Men with less than a bachelor’s degree are the most vulnerable.
Nationwide, the number of men participating in the workforce has significantly decreased, with 44% of the decline attributed to opioid misuse. (9) Simply put, opioid use causes overall employment numbers to drop.
What does prescription opioid misuse cost society?
Opioid addictions have a wider-reaching and more injurious impact than you may think. Opioid misuse cost a staggering $11.8 billion in the U.S in 2011. 53% of these costs came from losses in workplace productivity, and 30% was due to unnecessary cost in our health care systems. 17% of the money went to the criminal justice system to handle cases. (10)
This epidemic impacts taxpayers, patients, public health, members of the workforce, our courts, and more.
How do people get addicted to an opioid?
Most people swept up in the opioid crisis were originally prescribed the pills they now find addictive. That’s why it’s crucial to know the warning signs of nonmedical use and prescription drug addiction.
The first symptom to note is a feeling of dependence. Dependance can manifest in several forms. These include missing the drug when you are no longer taking it or experiencing opioid withdrawal symptoms.
Withdrawal symptoms include restlessness, trouble sleeping, vomiting, and more. If you notice these sensations, contact your doctor immediately. Never continue use of opioids or a prescription when you notice signs of dependence or withdrawal.
Addiction is defined as continued use of a drug despite negative consequences, so avoid it at all costs. (11)
Prescription opioids, while occasionally helpful for severe pain, are also highly chemically addictive. Opioids access opioid receptors in the brain and body. This process leads to relaxation, euphoria, and blocked pain messages.
It also gives the brain a surge of dopamine, a neurotransmitter. This is where the real problem lies. Our brains can become addicted to this rush of dopamine, causing us to crave the opioids that provide it.
You can learn more about the brain’s response to drugs in this video from the National Institute on Drug Abuse.
youtube
Short-term and Long-term Effects of Opioids
So, other than addiction, what risks and effects are you facing if you use medical opioids?
Short term use can have fewer side effects, though still potentially unpleasant ones. A few of these pesky problems include constipation, nausea, drowsiness, and slowed breathing.
Furthermore, most states have strict laws against driving under the influence of opiates due to delayed response times in users. Be aware that you may need to make appropriate transportation arrangements to continue life as usual. That is, if your body will let you.
Long-term effects of opioid use are even more concerning. Research suggests harmful side effects increase with length of use. Your organs can suffer due to vomiting, abdominal bloating, and liver damage. Furthermore, your brain may sustain damage or develop chemical dependence.
As you continue, your tolerance will increase, which demands higher, more harmful doses to feel the opioids’ impact. These negative side effects will continue to compound with prolonged use. (12)
Improper use of these prescribed medications can pose some of the same terrors as more infamous substances like heroin! Here’s a visual depiction of what’s going on inside the body when opioid abuse occurs. It’s clear that the less opioids in your system, the less risk of ugly side effects.
Risk Factors for Opioid Addiction
Risk factors for opioid use disorder are complex, but there are a few considerations that could raise your chances of getting hooked.
Ignoring directions. Taking opioids instead of opting for other pain relievers will require precision on your part. The federal government has estimated that 21-29% of patients given opioids for chronic pain take them incorrectly. If you receive a prescription for opioids, follow your dentist’s exact directions. Misusing them or treating them casually could build dependence.
Chronic pain. It seems that chronic pain patients are more likely to develop an addiction than the general population. Up to 60% of major trauma patients are estimated to develop an addictive issue. (13) Due to their pain-blocking nature, opioids can be particularly attractive. If you have chronic pain and your dentist prescribes opioids, proceed with caution.
A history of addiction. If you’ve experienced past addiction, it can be a potential indicator for opioid use disorder. Talk with your dentist to ensure this addictive pattern won’t repeat with your dental pain medications. (14)
Mental health conditions. Any struggles with mental illness can make taking opioids more risky, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).
Personalized effect. Your own physiological reactions to opioids can heighten your risk of addiction. Biological makeup can determine individual experience. Certain people are more or less likely to experience an addictive, dopamine-driven “euphoria.” This feeling is subjective and ranges between patients. (15)
Education level. Congrats to all you grads out there! The more scholastic achievements you have under your belt, the less likely you are to succumb to an opioid addiction. That’s one more reason to be a lifelong learner! (16)
This list of symptoms can help you and your doctor assess if you are struggling with substance use disorder.
If you begin to experience thoughts of self-harm or are looking for opioid treatment options, do not hesitate to contact the National Suicide Prevention Lifeline. They are always available by call, text, or online chat. Reach out 24/7 at 1-800-273-TALK.
The good news is that you have more treatment options than you may realize. This problem is treatable with time, effort, and intentional steps toward change.
Can you overdose on prescription opioids?
Overdosing on prescription opioids is 100% possible. The problem in abusing these drugs is that you build up tolerance over time. Users seek “higher highs” and bigger doses to feel satiated.
Most opioid deaths are from taking prescriptions in doses much larger than prescribed or ingesting them in combination with other drugs. Both of these choices tend to become dangerous habits in long-term users seeking a fix. (17)
Taking a high dose of opioids can lead to death from cardiac or respiratory arrest.
The danger here? Tolerance. Building a tolerance to opioids from long-term use is treacherous. Tolerance to the drug’s euphoric effect will increase faster than your body’s tolerance to the dangerous side effects.
Users may be taking more to get high, but at some point, their body can’t keep up. In fact, this is the reason that many opioid overdoses are accidental. The need for more dopamine and higher doses can be fatal. Did you know that opioid overdoses actually kill more people than car accidents each year? These tragic accidents can be avoided with addiction treatment.
This is a crucial juncture in history for understanding and preventing overdoses. The opioid epidemic mortality rate is skyrocketing. Overdose deaths in this category have risen 200% since 2000.
In fact, the CDC found that 61% of all drug overdose deaths were linked to an opioid. (18) As it steals over 130 lives each day, this crisis has established itself as a real national threat.
Wondering if you’re in danger of abusing opioids? This quiz can help you and your doctor assess if you need treatment for substance abuse.
If you’re looking for a next step, there are resources available.
SAMHSA has a directory of opioid treatment programs.
You might join a meeting of Narcotics Anonymous for support.
Finally, consider this thorough list of National Institute of Health-approved options to treat opioid addiction.
Most importantly, if you feel you are in danger of an overdose, call 911 right away. Your treatment plan can be determined once you are safe and in stable condition.
How to Prevent Opioid Addiction
Now that we’ve covered the seriousness of this crisis, it’s time for one of my favorite subjects: prevention.
As a family member, dentist, or patient, you’re likely to come into contact with opioids at some juncture. Here are some of my tips to stay safe and use your educated judgment about prescription opioids:
1. For Dentists
As healthcare providers, we are the first line of defense against these chilling statistics. It’s more important each year to stay updated, conscious, and preventative in your care. Here are my top tips for protecting your patients and prescriptions:
Stay up to date. The NIH is clear that “partnerships between researchers and practitioners are increasingly important as we face crises of the scale of the current opioid overdose epidemic.” Staying current with ADA standards creates a safety net for your practice and provides clear guidelines in this ever-changing area.
Continue your education. One of my favorite things about medicine is the constant opportunity to access fresh ideas and information. Here’s a joint webinar presentation from the ADA and CDC presenting alternatives to opioid prescriptions. These steps can cut down on addiction rates after dental procedures.
Avoid generalized prescriptions. Talk to your patients about their individualized needs and the risks of opioids. Each prescription is personal, so ask thoughtful questions and suggest non-opioid pain relievers and anti-inflammatories first. You will communicate how much you care about your patients by your candor.
Limit the quantity of opioids that you prescribe. Data suggests that likelihood of opioid dependence starts climbing on the third day. (19) Offer as few doses as possible without leaving your patient uncomfortable. Many times, after a few days, a NSAID will handle the pain level.
Do your homework. Check in with your state prescription database to be sure your patient does not already have an opioid prescription.
Be observant. Remember, not all patients who are drug-seeking will present with obvious symptoms. (2) Before prescribing opioids, take a few moments to look for more subtle signs of drug-seeking behavior (DSB).
2. For Patients
Communicate and comply with instructions. Prevent potential pitfalls with prescription opioids by following your doctor’s orders as carefully as possible. Also, please don’t hesitate to let your dentist know if you develop any concerns. If you notice withdrawal symptoms, make your doctor or dentist aware right away. Your dentist is here to help your health, not hurt it. Good communication is key for safe and exceptional results.
Hands off! It’s common for opioid misuse to start with buying, “borrowing,” or being given someone else’s prescribed medications. Leftover medications around the house can also increase the risk of opioid abuse. Don’t give family, friends, children, or pets a chance to get to your opioids. Dispose of unused medicine quickly and properly, for everyone’s sake. (20)
Limit your use. Even if your dentist prescribed several days’ worth of opioids, see if you can go without after a day or two. Each day you remain on opioids increases your chance of addiction, so if you can limit your usage, go for it!
Don’t be afraid to advocate for yourself. Be sure your dentist is fully aware of you and your family’s medical history, especially if it involves addiction. Knowing the circumstances will help your dentist prescribe the best, most personalized option. You have many options for pain management. Don’t feel forced into taking opioid medication! Your health is uniquely yours—if opioids make you uncomfortable, your dentist can assist in finding a better treatment plan for you.
Ask away. Useful questions could include:
inquiring about less addictive medicine for pain management,
asking for an addiction risk assessment, and
investigating drug interactions between your prescriptions.
Believe it or not, good dentists aren’t bothered by questions. Taking your health seriously and learning your needs is a great step for any patient! The more you know, the more you can feel confident that your dental and overall health is thriving.
3. For Families
Wisdom tooth wellness plan. As mentioned, teens are likely to be given opioids for wisdom tooth removal. Unfortunately, this practice can intensify the likelihood of continued opioid use. Before your make any medication decisions for this procedure, try reviewing the facts together. You could start with this guide created specifically for teens. Discussing prescription options for oral surgery is a fantastic opportunity. Your conversation now could help your teenager navigate the opioid epidemic in the future.
Know what you’re dealing with. Do your best to stay informed on all possible drug threats your teen is facing, including opioids. This recent report on drug use among teens is a helpful resource. A bit of good news: there is no significant spike in opioid use disorder in teens until they reach 12th grade.
Protect the next generation. Pregnant women should know that abusing opioids while expecting is highly dangerous. The decision to misuse prescription opioids can result in your baby experiencing withdrawal symptoms or birth defects. In more severe cases, mothers with opioid use disorder can even lose their child. (21) This list outlines options for a healthier lifestyle and safer baby. Your child and your body are too important to put through opioid addiction!
Build a support network. IECMH consultants offer support and tools to families that have been affected by opioid misuse. If you or someone in your family is struggling, call 1-800-662-4357 for referrals to nearby programs. You can still receive the help and care you need for your child and family. It’s never too late, and you are not alone.
Sharing (information) is caring. If you suspect a teen in your family is misusing pain medicine, you can direct them to this guide. Ask their pediatrician for any recommended resources, and offer to talk if they’re ready.
Storing and Disposing of Opioid Medications
[Saturday, April 27, 2019 is National Prescription Drug Takeback Day. Between 10 AM—2 PM, you can turn in unused prescription drugs, including opioids, at locations throughout the United States. Check out Google’s Location Finder for a location near you.]
Imagine that you were prescribed a week of opioids for a dental surgery.
Being aware of the dangers they can pose, you stopped use by day three. You wanted to control your addiction risk, even if you had more pills. I’d say that’s a great job of prevention! However, even if you don’t finish your opioid prescription, it still poses a significant risk.
“Leftovers” are never safe to keep around your residence. In particular, unused opioids from dental procedures are common targets for drug abusers. (22)
To put an end to nonmedical drug use in your home, you cannot leave them lying around. Luckily, patients have many safe options for storing and disposing of opioid medications.
Until you can remove the opioid medication from your home, the best way to store your pills is in a safe place. Choose a space out of sight and beyond children’s reach, ideally in a locked cabinet. The only person who should be able to access those pills is the person responsible for them. Taking this measure prevents future addictions, accidental poisonings, and more.
To say goodbye to your medication, here are a few safe disposal options:
Medicine take-back sites and events,
Collection receptacles. (Your local law enforcement agency can direct you to any nearby community receptacles).
Flushing certain, potentially dangerous medicines in the toilet. For a guide on how to do this safely, click here.
What’s the best time to dispose of your opioids? As soon as possible. The more time that elapses before disposal, the higher the odds of abuse.
Key Takeaways: How to Avoid the Opioid Epidemic
Before you fill your prescription to treat your dental pain, think twice about the highly addictive nature of opioids. The opioid epidemic in the U.S. increases every year. Education, awareness, and prevention can reverse this terrible trend.
There are other choices for pain relief with notably safer side effects. These include options such as ibuprofen, acetaminophen, and aspirin.
So, whether you’re a dentist, patient, or family member, don’t be afraid to discuss options when it comes to pain management!
If you do decide on opioids for dental pain, be sure to limit your intake. Be sure to communicate with your dentist, follow instructions to the letter, and dispose of any unused pills quickly and appropriately. It’s possible to use opioids safely if you are communicative with your dentist and disciplined in your approach.
Lastly, if you or a loved one is struggling with opioid use disorder, know that there is a network of recovery, support and treatment that’s poised to help. You have more resources available than you may know. Informed and empowered, patients and dentists can stop dentistry prescribed opiate abuse and choose safe pain management.
read next: Know Before You Go: Root Canals
22 References
Phillips, J. K., Ford, M. A., Bonnie, R. J., & National Academies of Sciences, Engineering, and Medicine. (2017). Trends in Opioid Use, Harms, and Treatment. In Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. National Academies Press (US). Abstract: https://www.ncbi.nlm.nih.gov/books/NBK458661/
Kolodny, A., Courtwright, D. T., Hwang, C. S., Kreiner, P., Eadie, J. L., Clark, T. W., & Alexander, G. C. (2015). The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annual review of public health, 36, 559-574. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/25581144
Nadelmann, E., & LaSalle, L. (2017). Two steps forward, one step back: current harm reduction policy and politics in the United States. Harm reduction journal, 14(1), 37. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5469032/
Novak, S. P., Håkansson, A., Martinez-Raga, J., Reimer, J., Krotki, K., & Varughese, S. (2016). Nonmedical use of prescription drugs in the European Union. BMC psychiatry, 16(1), 274. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4972971/
Harbaugh, C. M., Nalliah, R. P., Hu, H. M., Englesbe, M. J., Waljee, J. F., & Brummett, C. M. (2018). Persistent opioid use after wisdom tooth extraction. Jama, 320(5), 504-506. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/30088000
Varma, A., Sapra, M., & Iranmanesh, A. (2018). Impact of opioid therapy on gonadal hormones: focus on buprenorphine. Hormone molecular biology and clinical investigation, 36(2). Abstract: https://www.ncbi.nlm.nih.gov/pubmed/29453925
Myers, L., & Wodarski, J. S. (2015). Using the Substance Abuse and Mental Health Services Administration (SAMHSA) evidence-based practice kits in social work education. In E-Therapy for Substance Abuse and Co-Morbidity (pp. 53-73). Springer, Cham. Abstract: https://link.springer.com/chapter/10.1007/978-3-319-12376-9_5
Cicero, T. J., Ellis, M. S., Surratt, H. L., & Kurtz, S. P. (2014). The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA psychiatry, 71(7), 821-826. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/24871348
Aliprantis, D., & Schweitzer, M. E. (2018). Opioids and the Labor Market. Abstract: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3179068
Birnbaum, H. G., White, A. G., Schiller, M., Waldman, T., Cleveland, J. M., & Roland, C. L. (2011). Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain medicine, 12(4), 657-667. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/21392250
Angres, D. H., & Bettinardi-Angres, K. (2008). The disease of addiction: origins, treatment, and recovery. Disease-a-month: DM, 54(10), 696. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/18790142
Clarke, H., Soneji, N., Ko, D. T., Yun, L., & Wijeysundera, D. N. (2014). Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. Bmj, 348, g1251. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3921439/
Savage, S. R. (2002). Assessment for addiction in pain-treatment settings. The Clinical journal of pain, 18(4), S28-S38. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/12479252
Webster, L. R. (2017). Risk factors for opioid-use disorder and overdose. Anesthesia & Analgesia, 125(5), 1741-1748. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/29049118
Bieber, C. M., Fernandez, K., Borsook, D., Brennan, M. J., Butler, S. F., Jamison, R. N., … & Katz, N. P. (2008). Retrospective accounts of initial subjective effects of opioids in patients treated for pain who do or do not develop opioid addiction: a pilot case-control study. Experimental and clinical psychopharmacology, 16(5), 429. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3153468/
Arkes, J., Iguchi, M. How Predictors of Prescription Drug Abuse Vary by Age. Journal of Drug Issues (2008) Abstract: https://www.ncjrs.gov/App/AbstractDB/AbstractDBDetails.aspx?id=248641
Rudd, R. A., Aleshire, N., Zibbell, J. E., & Matthew Gladden, R. (2016). Increases in drug and opioid overdose deaths—United States, 2000–2014. American Journal of Transplantation, 16(4), 1323-1327. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/26720857
Rudd, R. A., Aleshire, N., Zibbell, J. E., & Matthew Gladden, R. (2016). Increases in drug and opioid overdose deaths—United States, 2000–2014. American Journal of Transplantation, 16(4), 1323-1327. Abstract: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm?s_cid=mm6450a3_w
Shah A, Hayes CJ, Martin BC. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use — United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017;66:265–269. Abstract: http://dx.doi.org/10.15585/mmwr.mm6610a1
Denisco, R. C., Kenna, G. A., O’Neil, M. G., Kulich, R. J., Moore, P. A., Kane, W. T., … & Katz, N. P. (2011). Prevention of prescription opioid abuse: The role of the dentist. The Journal of the American Dental Association, 142(7), 800-810. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/21719802
Finnegan, L. P., Connaughton, J. J., Kron, R. E., & Emich, J. P. (1975). Neonatal abstinence syndrome: assessment and management. Addictive diseases, 2(1-2), 141-158. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/30819342
Maughan, B. C., Hersh, E. V., Shofer, F. S., Wanner, K. J., Archer, E., Carrasco, L. R., & Rhodes, K. V. (2016). Unused opioid analgesics and drug disposal following outpatient dental surgery: a randomized controlled trial. Drug and alcohol dependence, 168, 328-334. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/27663358
The post How to Avoid the Opioid Epidemic (for Dentists, Patients, and Families) appeared first on Ask the Dentist.
How to Avoid the Opioid Epidemic (for Dentists, Patients, and Families) published first on https://wittooth.tumblr.com/
0 notes
Link
Saturday, April 27, 2019 is National Prescription Drug Takeback Day. Between 10 AM—2 PM, you can turn in unused prescription drugs, including opioids, at locations throughout the United States. Check out Google’s Location Finder for a location near you.
You may have heard of the “opioid epidemic” rumbling through our nation, but what does that term mean?
If you’re unfamiliar with this crisis in the United States, it may shock you to learn that dental offices can be starting points for this epidemic.
Let’s look at how this works for everyone from the dentist to the patient (and those in between). There is hope for opioid addiction.
What are opioids?
Dentists often prescribe opioids for pain management after surgeries or major procedures. It’s a convenient choice, since opioids are a class of drugs that have pain-blocking qualities. Unfortunately, improperly using these pills can have lasting, devastating consequences.
It’s possible to become addicted to opioids in as little as five days. (1)
Despite this, many dental opioid prescriptions can last for up to 10 days. The severity of this prescription issue makes it important for dentists, dental patients, and their loved ones to learn more. Your knowledge could be the difference between a routine prescription and a painful battle with opioid addiction.
You can stay safe from the opioid epidemic by knowing the risks of using opioids, educating yourself on taking prescribed opioids correctly, and understanding what to do if addiction takes hold.
List of Opioids Prescribed in Dentistry
The following are opioid drugs often prescribed for pain management by dentists:
Hydrocodone (Vicodin)—The prescription rate for this drug doubled between 1999 and 2011.
Oxycodone (Percocet® or OxyContin®)—This prescription rate increased 500% in the same timeframe. (2)
Acetaminophen with codeine (Tylenol® No. 3 and Tylenol® No. 4).
Opioids also branch beyond prescribed medications. Other forms include heroin, morphine, tramadol, and synthetic opioids like Fentanyl (Duragesic). Though each of these opioids vary in strength, they all have addictive qualities and harmful effects if used long-term.
According to the Centers for Disease Control and Prevention, the U.S. is in the midst of the “worst drug overdose epidemic in history.” (3)
Unfortunately, the data shows that prescription rates for opioids are still climbing. The government, researchers, and dental experts all warn against prescribing unnecessary opioids. Instead, they are urging patients to consider other viable options for pain relief.
What is the opioid epidemic?
The opioid epidemic is caused, in part, by nonmedical use of prescription drugs. This may include: (4)
Taking a larger prescription than needed
Using drugs prescribed to someone else
Taking your prescription with alcohol or other legal or illegal drugs
Abusing prescription drugs to feel a sense of euphoria—this behavior is much more likely to occur with opioid pain relievers than with other medicines
Due to their addictive nature, these pills are in high demand, and not always for medicinal use. What’s the delineation between necessary and nonmedicinal use? Well, for one, the effect on the user’s life.
The definition of opioid use disorder is a pattern of misuse that leads to emotional or functional distress.
A simple study of third molar extractions reveals how sinister this issue can be. A recent study found that young Americans prescribed opioids for their wisdom teeth were at greater risk for addiction.
Patients who filled their opioid prescription had a 13% chance of persistent opioid use. This puts them at high risk of addiction. On the other hand, only 5% of patients who didn’t fill their prescription struggled with long-term opioid issues. (5)
Statistics like these are why I urge dentists and their patients to consider choosing anti-inflammatory drugs or non-opioid pain relievers. One prescription, especially in younger people, can have long-term effects. Consider several options before jumping immediately to opioid prescribing with addictive potential.
If prescriptions for opioids slow down, this epidemic may as well.
Opioid Abuse Statistics
How many people abuse opioids?
In 2016, the U.S. Department of Health and Human Services (HHS) found that 11.8 million people over the age of 12 misused opioids. 2.3 million had begun the habit within the past year, highlighting the growing epidemic. (6)
Prescription Opioids vs. Heroin
In 2016, 11.5 million Americans misused prescription opioids, a number far greater than the 948,000 who had used heroin. That’s an astronomical difference in users.
Unfortunately, only 17.5% of those addicted to opioid painkillers sought professional help. This totals far less recovery treatment per capita than those fighting a heroin addiction. (7)
Both are issues of drug abuse, but for some reason, opioid drug users aren’t seeking help like they should. Perhaps this is due to the fact opioid addiction affects people who don’t seem like drug abusers, or because the addiction began with a legal prescription. Whatever the reason, the statistics are alarming.
Can prescribed opioids function as a gateway drug?
In a recent interview with heroin users entering treatment, 80% had abused prescription opioids before turning to heroin. (8) These numbers highlight that opioid use is a road that can lead to other harmful narcotics.
Substance abuse is always a real threat. Prescribed opioids present no less inherent danger and can lead to other addictions.
Can prescribed opioids hurt my job performance?
Research has linked an increase in opioid prescriptions to a decrease in the number of people participating in the labor force. Men with less than a bachelor’s degree are the most vulnerable.
Nationwide, the number of men participating in the workforce has significantly decreased, with 44% of the decline attributed to opioid misuse. (9) Simply put, opioid use causes overall employment numbers to drop.
What does prescription opioid misuse cost society?
Opioid addictions have a wider-reaching and more injurious impact than you may think. Opioid misuse cost a staggering $11.8 billion in the U.S in 2011. 53% of these costs came from losses in workplace productivity, and 30% was due to unnecessary cost in our health care systems. 17% of the money went to the criminal justice system to handle cases. (10)
This epidemic impacts taxpayers, patients, public health, members of the workforce, our courts, and more.
How do people get addicted to an opioid?
Most people swept up in the opioid crisis were originally prescribed the pills they now find addictive. That’s why it’s crucial to know the warning signs of nonmedical use and prescription drug addiction.
The first symptom to note is a feeling of dependence. Dependance can manifest in several forms. These include missing the drug when you are no longer taking it or experiencing opioid withdrawal symptoms.
Withdrawal symptoms include restlessness, trouble sleeping, vomiting, and more. If you notice these sensations, contact your doctor immediately. Never continue use of opioids or a prescription when you notice signs of dependence or withdrawal.
Addiction is defined as continued use of a drug despite negative consequences, so avoid it at all costs. (11)
Prescription opioids, while occasionally helpful for severe pain, are also highly chemically addictive. Opioids access opioid receptors in the brain and body. This process leads to relaxation, euphoria, and blocked pain messages.
It also gives the brain a surge of dopamine, a neurotransmitter. This is where the real problem lies. Our brains can become addicted to this rush of dopamine, causing us to crave the opioids that provide it.
You can learn more about the brain’s response to drugs in this video from the National Institute on Drug Abuse.
Short-term and Long-term Effects of Opioids
So, other than addiction, what risks and effects are you facing if you use medical opioids?
Short term use can have fewer side effects, though still potentially unpleasant ones. A few of these pesky problems include constipation, nausea, drowsiness, and slowed breathing.
Furthermore, most states have strict laws against driving under the influence of opiates due to delayed response times in users. Be aware that you may need to make appropriate transportation arrangements to continue life as usual. That is, if your body will let you.
Long-term effects of opioid use are even more concerning. Research suggests harmful side effects increase with length of use. Your organs can suffer due to vomiting, abdominal bloating, and liver damage. Furthermore, your brain may sustain damage or develop chemical dependence.
As you continue, your tolerance will increase, which demands higher, more harmful doses to feel the opioids’ impact. These negative side effects will continue to compound with prolonged use. (12)
Improper use of these prescribed medications can pose some of the same terrors as more infamous substances like heroin! Here’s a visual depiction of what’s going on inside the body when opioid abuse occurs. It’s clear that the less opioids in your system, the less risk of ugly side effects.
Risk Factors for Opioid Addiction
Risk factors for opioid use disorder are complex, but there are a few considerations that could raise your chances of getting hooked.
Ignoring directions. Taking opioids instead of opting for other pain relievers will require precision on your part. The federal government has estimated that 21-29% of patients given opioids for chronic pain take them incorrectly. If you receive a prescription for opioids, follow your dentist’s exact directions. Misusing them or treating them casually could build dependence.
Chronic pain. It seems that chronic pain patients are more likely to develop an addiction than the general population. Up to 60% of major trauma patients are estimated to develop an addictive issue. (13) Due to their pain-blocking nature, opioids can be particularly attractive. If you have chronic pain and your dentist prescribes opioids, proceed with caution.
A history of addiction. If you’ve experienced past addiction, it can be a potential indicator for opioid use disorder. Talk with your dentist to ensure this addictive pattern won’t repeat with your dental pain medications. (14)
Mental health conditions. Any struggles with mental illness can make taking opioids more risky, according to the Substance Abuse and Mental Health Services Administration (SAMHSA).
Personalized effect. Your own physiological reactions to opioids can heighten your risk of addiction. Biological makeup can determine individual experience. Certain people are more or less likely to experience an addictive, dopamine-driven “euphoria.” This feeling is subjective and ranges between patients. (15)
Education level. Congrats to all you grads out there! The more scholastic achievements you have under your belt, the less likely you are to succumb to an opioid addiction. That’s one more reason to be a lifelong learner! (16)
This list of symptoms can help you and your doctor assess if you are struggling with substance use disorder.
If you begin to experience thoughts of self-harm or are looking for opioid treatment options, do not hesitate to contact the National Suicide Prevention Lifeline. They are always available by call, text, or online chat. Reach out 24/7 at 1-800-273-TALK.
The good news is that you have more treatment options than you may realize. This problem is treatable with time, effort, and intentional steps toward change.
Can you overdose on prescription opioids?
Overdosing on prescription opioids is 100% possible. The problem in abusing these drugs is that you build up tolerance over time. Users seek “higher highs” and bigger doses to feel satiated.
Most opioid deaths are from taking prescriptions in doses much larger than prescribed or ingesting them in combination with other drugs. Both of these choices tend to become dangerous habits in long-term users seeking a fix. (17)
Taking a high dose of opioids can lead to death from cardiac or respiratory arrest.
The danger here? Tolerance. Building a tolerance to opioids from long-term use is treacherous. Tolerance to the drug’s euphoric effect will increase faster than your body’s tolerance to the dangerous side effects.
Users may be taking more to get high, but at some point, their body can’t keep up. In fact, this is the reason that many opioid overdoses are accidental. The need for more dopamine and higher doses can be fatal. Did you know that opioid overdoses actually kill more people than car accidents each year? These tragic accidents can be avoided with addiction treatment.
This is a crucial juncture in history for understanding and preventing overdoses. The opioid epidemic mortality rate is skyrocketing. Overdose deaths in this category have risen 200% since 2000.
In fact, the CDC found that 61% of all drug overdose deaths were linked to an opioid. (18) As it steals over 130 lives each day, this crisis has established itself as a real national threat.
Wondering if you’re in danger of abusing opioids? This quiz can help you and your doctor assess if you need treatment for substance abuse.
If you’re looking for a next step, there are resources available.
SAMHSA has a directory of opioid treatment programs.
You might join a meeting of Narcotics Anonymous for support.
Finally, consider this thorough list of National Institute of Health-approved options to treat opioid addiction.
Most importantly, if you feel you are in danger of an overdose, call 911 right away. Your treatment plan can be determined once you are safe and in stable condition.
How to Prevent Opioid Addiction
Now that we’ve covered the seriousness of this crisis, it’s time for one of my favorite subjects: prevention.
As a family member, dentist, or patient, you’re likely to come into contact with opioids at some juncture. Here are some of my tips to stay safe and use your educated judgment about prescription opioids:
1. For Dentists
As healthcare providers, we are the first line of defense against these chilling statistics. It’s more important each year to stay updated, conscious, and preventative in your care. Here are my top tips for protecting your patients and prescriptions:
Stay up to date. The NIH is clear that “partnerships between researchers and practitioners are increasingly important as we face crises of the scale of the current opioid overdose epidemic.” Staying current with ADA standards creates a safety net for your practice and provides clear guidelines in this ever-changing area.
Continue your education. One of my favorite things about medicine is the constant opportunity to access fresh ideas and information. Here’s a joint webinar presentation from the ADA and CDC presenting alternatives to opioid prescriptions. These steps can cut down on addiction rates after dental procedures.
Avoid generalized prescriptions. Talk to your patients about their individualized needs and the risks of opioids. Each prescription is personal, so ask thoughtful questions and suggest non-opioid pain relievers and anti-inflammatories first. You will communicate how much you care about your patients by your candor.
Limit the quantity of opioids that you prescribe. Data suggests that likelihood of opioid dependence starts climbing on the third day. (19) Offer as few doses as possible without leaving your patient uncomfortable. Many times, after a few days, a NSAID will handle the pain level.
Do your homework. Check in with your state prescription database to be sure your patient does not already have an opioid prescription.
Be observant. Remember, not all patients who are drug-seeking will present with obvious symptoms. (2) Before prescribing opioids, take a few moments to look for more subtle signs of drug-seeking behavior (DSB).
2. For Patients
Communicate and comply with instructions. Prevent potential pitfalls with prescription opioids by following your doctor’s orders as carefully as possible. Also, please don’t hesitate to let your dentist know if you develop any concerns. If you notice withdrawal symptoms, make your doctor or dentist aware right away. Your dentist is here to help your health, not hurt it. Good communication is key for safe and exceptional results.
Hands off! It’s common for opioid misuse to start with buying, “borrowing,” or being given someone else’s prescribed medications. Leftover medications around the house can also increase the risk of opioid abuse. Don’t give family, friends, children, or pets a chance to get to your opioids. Dispose of unused medicine quickly and properly, for everyone’s sake. (20)
Limit your use. Even if your dentist prescribed several days’ worth of opioids, see if you can go without after a day or two. Each day you remain on opioids increases your chance of addiction, so if you can limit your usage, go for it!
Don’t be afraid to advocate for yourself. Be sure your dentist is fully aware of you and your family’s medical history, especially if it involves addiction. Knowing the circumstances will help your dentist prescribe the best, most personalized option. You have many options for pain management. Don’t feel forced into taking opioid medication! Your health is uniquely yours—if opioids make you uncomfortable, your dentist can assist in finding a better treatment plan for you.
Ask away. Useful questions could include:
inquiring about less addictive medicine for pain management,
asking for an addiction risk assessment, and
investigating drug interactions between your prescriptions.
Believe it or not, good dentists aren’t bothered by questions. Taking your health seriously and learning your needs is a great step for any patient! The more you know, the more you can feel confident that your dental and overall health is thriving.
3. For Families
Wisdom tooth wellness plan. As mentioned, teens are likely to be given opioids for wisdom tooth removal. Unfortunately, this practice can intensify the likelihood of continued opioid use. Before your make any medication decisions for this procedure, try reviewing the facts together. You could start with this guide created specifically for teens. Discussing prescription options for oral surgery is a fantastic opportunity. Your conversation now could help your teenager navigate the opioid epidemic in the future.
Know what you’re dealing with. Do your best to stay informed on all possible drug threats your teen is facing, including opioids. This recent report on drug use among teens is a helpful resource. A bit of good news: there is no significant spike in opioid use disorder in teens until they reach 12th grade.
Protect the next generation. Pregnant women should know that abusing opioids while expecting is highly dangerous. The decision to misuse prescription opioids can result in your baby experiencing withdrawal symptoms or birth defects. In more severe cases, mothers with opioid use disorder can even lose their child. (21) This list outlines options for a healthier lifestyle and safer baby. Your child and your body are too important to put through opioid addiction!
Build a support network. IECMH consultants offer support and tools to families that have been affected by opioid misuse. If you or someone in your family is struggling, call 1-800-662-4357 for referrals to nearby programs. You can still receive the help and care you need for your child and family. It’s never too late, and you are not alone.
Sharing (information) is caring. If you suspect a teen in your family is misusing pain medicine, you can direct them to this guide. Ask their pediatrician for any recommended resources, and offer to talk if they’re ready.
Storing and Disposing of Opioid Medications
[Saturday, April 27, 2019 is National Prescription Drug Takeback Day. Between 10 AM—2 PM, you can turn in unused prescription drugs, including opioids, at locations throughout the United States. Check out Google’s Location Finder for a location near you.]
Imagine that you were prescribed a week of opioids for a dental surgery.
Being aware of the dangers they can pose, you stopped use by day three. You wanted to control your addiction risk, even if you had more pills. I’d say that’s a great job of prevention! However, even if you don’t finish your opioid prescription, it still poses a significant risk.
“Leftovers” are never safe to keep around your residence. In particular, unused opioids from dental procedures are common targets for drug abusers. (22)
To put an end to nonmedical drug use in your home, you cannot leave them lying around. Luckily, patients have many safe options for storing and disposing of opioid medications.
Until you can remove the opioid medication from your home, the best way to store your pills is in a safe place. Choose a space out of sight and beyond children’s reach, ideally in a locked cabinet. The only person who should be able to access those pills is the person responsible for them. Taking this measure prevents future addictions, accidental poisonings, and more.
To say goodbye to your medication, here are a few safe disposal options:
Medicine take-back sites and events,
Collection receptacles. (Your local law enforcement agency can direct you to any nearby community receptacles).
Flushing certain, potentially dangerous medicines in the toilet. For a guide on how to do this safely, click here.
What’s the best time to dispose of your opioids? As soon as possible. The more time that elapses before disposal, the higher the odds of abuse.
Key Takeaways: How to Avoid the Opioid Epidemic
Before you fill your prescription to treat your dental pain, think twice about the highly addictive nature of opioids. The opioid epidemic in the U.S. increases every year. Education, awareness, and prevention can reverse this terrible trend.
There are other choices for pain relief with notably safer side effects. These include options such as ibuprofen, acetaminophen, and aspirin.
So, whether you’re a dentist, patient, or family member, don’t be afraid to discuss options when it comes to pain management!
If you do decide on opioids for dental pain, be sure to limit your intake. Be sure to communicate with your dentist, follow instructions to the letter, and dispose of any unused pills quickly and appropriately. It’s possible to use opioids safely if you are communicative with your dentist and disciplined in your approach.
Lastly, if you or a loved one is struggling with opioid use disorder, know that there is a network of recovery, support and treatment that’s poised to help. You have more resources available than you may know. Informed and empowered, patients and dentists can stop dentistry prescribed opiate abuse and choose safe pain management.
read next: Know Before You Go: Root Canals
22 References
Phillips, J. K., Ford, M. A., Bonnie, R. J., & National Academies of Sciences, Engineering, and Medicine. (2017). Trends in Opioid Use, Harms, and Treatment. In Pain Management and the Opioid Epidemic: Balancing Societal and Individual Benefits and Risks of Prescription Opioid Use. National Academies Press (US). Abstract: https://www.ncbi.nlm.nih.gov/books/NBK458661/
Kolodny, A., Courtwright, D. T., Hwang, C. S., Kreiner, P., Eadie, J. L., Clark, T. W., & Alexander, G. C. (2015). The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annual review of public health, 36, 559-574. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/25581144
Nadelmann, E., & LaSalle, L. (2017). Two steps forward, one step back: current harm reduction policy and politics in the United States. Harm reduction journal, 14(1), 37. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5469032/
Novak, S. P., Håkansson, A., Martinez-Raga, J., Reimer, J., Krotki, K., & Varughese, S. (2016). Nonmedical use of prescription drugs in the European Union. BMC psychiatry, 16(1), 274. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4972971/
Harbaugh, C. M., Nalliah, R. P., Hu, H. M., Englesbe, M. J., Waljee, J. F., & Brummett, C. M. (2018). Persistent opioid use after wisdom tooth extraction. Jama, 320(5), 504-506. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/30088000
Varma, A., Sapra, M., & Iranmanesh, A. (2018). Impact of opioid therapy on gonadal hormones: focus on buprenorphine. Hormone molecular biology and clinical investigation, 36(2). Abstract: https://www.ncbi.nlm.nih.gov/pubmed/29453925
Myers, L., & Wodarski, J. S. (2015). Using the Substance Abuse and Mental Health Services Administration (SAMHSA) evidence-based practice kits in social work education. In E-Therapy for Substance Abuse and Co-Morbidity (pp. 53-73). Springer, Cham. Abstract: https://link.springer.com/chapter/10.1007/978-3-319-12376-9_5
Cicero, T. J., Ellis, M. S., Surratt, H. L., & Kurtz, S. P. (2014). The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA psychiatry, 71(7), 821-826. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/24871348
Aliprantis, D., & Schweitzer, M. E. (2018). Opioids and the Labor Market. Abstract: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3179068
Birnbaum, H. G., White, A. G., Schiller, M., Waldman, T., Cleveland, J. M., & Roland, C. L. (2011). Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain medicine, 12(4), 657-667. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/21392250
Angres, D. H., & Bettinardi-Angres, K. (2008). The disease of addiction: origins, treatment, and recovery. Disease-a-month: DM, 54(10), 696. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/18790142
Clarke, H., Soneji, N., Ko, D. T., Yun, L., & Wijeysundera, D. N. (2014). Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. Bmj, 348, g1251. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3921439/
Savage, S. R. (2002). Assessment for addiction in pain-treatment settings. The Clinical journal of pain, 18(4), S28-S38. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/12479252
Webster, L. R. (2017). Risk factors for opioid-use disorder and overdose. Anesthesia & Analgesia, 125(5), 1741-1748. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/29049118
Bieber, C. M., Fernandez, K., Borsook, D., Brennan, M. J., Butler, S. F., Jamison, R. N., … & Katz, N. P. (2008). Retrospective accounts of initial subjective effects of opioids in patients treated for pain who do or do not develop opioid addiction: a pilot case-control study. Experimental and clinical psychopharmacology, 16(5), 429. Abstract: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3153468/
Arkes, J., Iguchi, M. How Predictors of Prescription Drug Abuse Vary by Age. Journal of Drug Issues (2008) Abstract: https://www.ncjrs.gov/App/AbstractDB/AbstractDBDetails.aspx?id=248641
Rudd, R. A., Aleshire, N., Zibbell, J. E., & Matthew Gladden, R. (2016). Increases in drug and opioid overdose deaths—United States, 2000–2014. American Journal of Transplantation, 16(4), 1323-1327. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/26720857
Rudd, R. A., Aleshire, N., Zibbell, J. E., & Matthew Gladden, R. (2016). Increases in drug and opioid overdose deaths—United States, 2000–2014. American Journal of Transplantation, 16(4), 1323-1327. Abstract: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm?s_cid=mm6450a3_w
Shah A, Hayes CJ, Martin BC. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use — United States, 2006–2015. MMWR Morb Mortal Wkly Rep 2017;66:265–269. Abstract: http://dx.doi.org/10.15585/mmwr.mm6610a1
Denisco, R. C., Kenna, G. A., O’Neil, M. G., Kulich, R. J., Moore, P. A., Kane, W. T., … & Katz, N. P. (2011). Prevention of prescription opioid abuse: The role of the dentist. The Journal of the American Dental Association, 142(7), 800-810. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/21719802
Finnegan, L. P., Connaughton, J. J., Kron, R. E., & Emich, J. P. (1975). Neonatal abstinence syndrome: assessment and management. Addictive diseases, 2(1-2), 141-158. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/30819342
Maughan, B. C., Hersh, E. V., Shofer, F. S., Wanner, K. J., Archer, E., Carrasco, L. R., & Rhodes, K. V. (2016). Unused opioid analgesics and drug disposal following outpatient dental surgery: a randomized controlled trial. Drug and alcohol dependence, 168, 328-334. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/27663358
The post How to Avoid the Opioid Epidemic (for Dentists, Patients, and Families) appeared first on Ask the Dentist.
from Ask the Dentist https://askthedentist.com/opioid-epidemic/
0 notes
Text
Is Poppy Seed Tea Safe to Drink?
Table of Contents
What Is Poppy Seed Tea?
What Health Benefits and Nutrients May Be Derived From Poppy Seed Tea?
Does Poppy Seed Tea Contain Caffeine?
Here's How You Can Brew Poppy Seed Tea at Home
What's the Correct Way to Store Poppy Seeds?
Watch Out for These Poppy Seed Tea Side Effects
Poppy Seed Tea May Have Benefits, but Only if Prepared Properly and Consumed in Moderation
Frequently Asked Questions (FAQs) About Poppy Seed Tea
Poppy seeds are popular in the culinary world, whether used as a pastry ingredient, an oil source or for brewing tea.1 Their nutty and fruity taste can be irresistible to many people, which is one of the reasons why it's such a well-loved ingredient.2
However, poppy tea, a drink brewed with poppy seeds, has been demonized because of the uncertainty surrounding its safety. This is due to its possible toxicity and opiate content, especially when the seeds are improperly harvested or prepared incorrectly. Some batches of poppy seeds may contain high amounts of opiate alkaloids, including morphine and codeine.3 To learn more about poppy seed tea, its benefits and the proper preparation, continue reading this article.
What Is Poppy Seed Tea?
Many people may be familiar with poppy plants due to their vibrant and eye-catching flowers, which are usually in full bloom in late spring or early summer.4 But aside from the pop of color, the poppy plant is the source of numerous properties, although not all of them may be categorized as inherently good.
One of its most infamous products is opium, a narcotic substance taken from the sap inside unripe opium pods. This drug is extremely addictive and may lead to dangerous and, at times, fatal complications.5 This is one of the reasons why poppy seeds have been cited to have specific side effects when taken in excessive amounts.
However, this doesn’t mean that poppy seeds are necessarily bad. It all boils down to moderation and the proper handling and preparation of the seeds. Poppy seeds are loaded with calcium, magnesium and phosphorus, which means that they may offer you good health benefits once you add them to your diet.6
Unfortunately, the abuse of or having insufficient knowledge about this tea has led to a few fatal incidences. The most recent case happened in 2016, when a college student from James Madison University passed away after drinking a potent batch of poppy tea.7
If you're planning on trying this tea, it's important that you're aware of your own threshold and sensitivities. It's also imperative that you test each batch of poppy seed tea to make sure that you're not unknowingly ingesting high amounts of the opiate alkaloids.
What Health Benefits and Nutrients May Be Derived From Poppy Seed Tea?
Even though there have been numerous controversies on the safety of poppy seeds, the nutrients and active components that they contain may help the body function more efficiently. Poppy seeds contain vitamins and minerals that are crucial in optimizing and maintaining the skeletal, immune and muscular systems. Some of these include calcium, phosphorus, magnesium, folate and iron.8 When brewed as tea, these minerals may transfer to the liquid, giving your health a boost.
Through the years, poppy seed tea has been known to be an antidiarrheal, anxiolytic and analgesic.9 However, the exact mechanism on how it works is not clear.10
It is also worthwhile to know that most of the benefits of poppy seed tea are rooted in certain active alkaloids that, when taken in large amounts, may lead to addiction and other dangerous complications. These alkaloids are found in unpredictable doses in poppy seeds, which might make it difficult to safely ingest this tea. Namely, these active compounds are codeine, morphine, thebaine and papaverine.11
Does Poppy Seed Tea Contain Caffeine?
There is no clear indication whether poppy seed tea contains caffeine. However, poppy seeds are widely used for their mild sedative function, which is a benefit that could be passed on to the tea.12 But take note that this doesn’t mean that poppy seed tea does not cause any of the possible side effects that caffeine has. In fact, excessive intake of poppy seed tea was found to cause anxiety, abdominal cramps and diarrhea.13
Here's How You Can Brew Poppy Seed Tea at Home
If you want to gain the numerous health benefits of poppy seeds, you can follow this recipe from Chew the World:14
Healthy Poppy Seed Tea Recipe
Ingredients
200 grams (7.04 ounces) poppy seeds
400 milliliters (13.5 ounces) water
Lemon juice, optional
Procedure
In a small saucepan, heat water for a couple of minutes until warm.
Carefully pour the poppy seeds in a sealable glass bottle. Pour the water into the bottle, submerging the poppy seeds completely.
Secure the bottle's lid. Shake vigorously for a few minutes.
Let it steep for about 15 minutes, and shake again. Let the tea sit for about an hour.
Drain the liquid using a clean tea towel to remove all the debris from the seeds.
If you want to mask the bitter flavor of poppy seed tea, add lemon juice. Serve.
Take note that poppy seed tea should not be ingested in excessive quantities. If you're just starting out, limit your poppy seeds to 100 grams. Make sure that you test each batch of poppy seeds, as the exact levels of alkaloids present in each batch cannot be ensured.
The fastest way to determine strength is by checking the tea that the seeds yield, depending on its color and taste. A darker and bitterer batch of poppy seed tea is typically stronger. If your current batch is darker than normal, it's best that you avoid drinking it to eliminate the risk of an accidental overdose.15
To make sure that you're not accidentally exposing yourself to opiates, rinse the seeds before using them in cooking or brewing. In a 2006 study, it was found that rinsing poppy seeds in hot water (60 degrees Celsius or 140 degrees Fahrenheit) might reduce their morphine content up to about 70 percent.16
What's the Correct Way to Store Poppy Seeds?
Poppy seeds are available at grocery shops and online stores. Just make sure that you're getting your supply from trustworthy sources. This will ensure that the seeds you're using to brew your tea are of the highest quality. To correctly buy and store your poppy seeds, here is a guide from Hunker:17
Check the expiration date on the package. It would also be worthwhile to ask your grocer how long the seeds have been on the shelves. This will help you determine whether the seeds are fresh.
After purchase, transfer the poppy seeds into an airtight glass container.
Store the container in the refrigerator. The seeds may last for up to six months, or a year if kept in the freezer.
Watch Out for These Poppy Seed Tea Side Effects
Although poppy seed tea could offer nutrients and compounds that may help boost your health, improper preparation of this tea may also lead to serious health repercussions. If poppy seeds aren’t cleaned properly before brewing, you might be unknowingly adding opiates to your cup of tea. Some of the most common side effects and complications drinkers may suffer from include:18
Headaches
Loss of concentration
Slowed breathing and lethargy
Death
A 2010 study documented the possible interaction of this tea with certain medications, especially Phenazepam, a drug prescribed for anxiety. In one instance, a patient drank poppy seed tea before taking Phenazepam, which eventually led to his death.19
Because of the absence of studies done on the safe consumption of poppy seed tea during pregnancy, it would be best that you veer away from it if you’re currently pregnant or breastfeeding to avoid any possible risks on your and your child’s well-being.
Poppy Seed Tea May Have Benefits, but Only if Prepared Properly and Consumed in Moderation
Poppy seed tea contains various nutrients and minerals, making it an effective ingredient for combating various ailments. However, it may come with possible side effects and complications. Moderation and caution are extremely important when drinking poppy seed tea so you can reap the benefits without side effects. Make sure that you get only the highest quality product when it comes to poppy seeds, and that you regulate your intake.
Frequently Asked Questions (FAQs) About Poppy Seed Tea
Q: How long does poppy seed tea stay in your system?
A: You may start feeling the effects of poppy seed tea 15 minutes to 30 minutes upon ingestion, the effects of which may last for a few hours to a day, depending on the amount and the strength of the tea.20
Q: What color is poppy seed tea?
A: Poppy seed tea typically has an amber to a brownish hue, depending on the strength of the tea. The darker the tea, the stronger and more concentrated it is.21
Q: How much poppy seed tea can I drink?
A: The amount of poppy seed tea that is safe for consumption is not clear, as it depends on the strength of the tea brewed and the tolerance of the person. It would be best to ask your physician for the ideal dosage.
In addition, poppy seeds usually come with varying amounts of the active alkaloids, which may make it hard for you to gauge its strength. One of the easiest ways to determine your tea's strength is to observe its color and bitterness level. If your tea is darker or more bitter than your usual brew, consider throwing it out to eliminate the risk of an accidental overdose.22
from http://articles.mercola.com/sites/articles/archive/2019/04/13/xdjm18-teas-18mcsa-poppy-seed-tea.aspx
source http://niapurenaturecom.weebly.com/blog/is-poppy-seed-tea-safe-to-drink
0 notes
Text
Is Poppy Seed Tea Safe to Drink?
Table of Contents
What Is Poppy Seed Tea?
What Health Benefits and Nutrients May Be Derived From Poppy Seed Tea?
Does Poppy Seed Tea Contain Caffeine?
Here’s How You Can Brew Poppy Seed Tea at Home
What’s the Correct Way to Store Poppy Seeds?
Watch Out for These Poppy Seed Tea Side Effects
Poppy Seed Tea May Have Benefits, but Only if Prepared Properly and Consumed in Moderation
Frequently Asked Questions (FAQs) About Poppy Seed Tea
Poppy seeds are popular in the culinary world, whether used as a pastry ingredient, an oil source or for brewing tea.1 Their nutty and fruity taste can be irresistible to many people, which is one of the reasons why it’s such a well-loved ingredient.2
However, poppy tea, a drink brewed with poppy seeds, has been demonized because of the uncertainty surrounding its safety. This is due to its possible toxicity and opiate content, especially when the seeds are improperly harvested or prepared incorrectly. Some batches of poppy seeds may contain high amounts of opiate alkaloids, including morphine and codeine.3 To learn more about poppy seed tea, its benefits and the proper preparation, continue reading this article.
What Is Poppy Seed Tea?
Many people may be familiar with poppy plants due to their vibrant and eye-catching flowers, which are usually in full bloom in late spring or early summer.4 But aside from the pop of color, the poppy plant is the source of numerous properties, although not all of them may be categorized as inherently good.
One of its most infamous products is opium, a narcotic substance taken from the sap inside unripe opium pods. This drug is extremely addictive and may lead to dangerous and, at times, fatal complications.5 This is one of the reasons why poppy seeds have been cited to have specific side effects when taken in excessive amounts.
However, this doesn’t mean that poppy seeds are necessarily bad. It all boils down to moderation and the proper handling and preparation of the seeds. Poppy seeds are loaded with calcium, magnesium and phosphorus, which means that they may offer you good health benefits once you add them to your diet.6
Unfortunately, the abuse of or having insufficient knowledge about this tea has led to a few fatal incidences. The most recent case happened in 2016, when a college student from James Madison University passed away after drinking a potent batch of poppy tea.7
If you’re planning on trying this tea, it’s important that you’re aware of your own threshold and sensitivities. It’s also imperative that you test each batch of poppy seed tea to make sure that you’re not unknowingly ingesting high amounts of the opiate alkaloids.
What Health Benefits and Nutrients May Be Derived From Poppy Seed Tea?
Even though there have been numerous controversies on the safety of poppy seeds, the nutrients and active components that they contain may help the body function more efficiently. Poppy seeds contain vitamins and minerals that are crucial in optimizing and maintaining the skeletal, immune and muscular systems. Some of these include calcium, phosphorus, magnesium, folate and iron.8 When brewed as tea, these minerals may transfer to the liquid, giving your health a boost.
Through the years, poppy seed tea has been known to be an antidiarrheal, anxiolytic and analgesic.9 However, the exact mechanism on how it works is not clear.10
It is also worthwhile to know that most of the benefits of poppy seed tea are rooted in certain active alkaloids that, when taken in large amounts, may lead to addiction and other dangerous complications. These alkaloids are found in unpredictable doses in poppy seeds, which might make it difficult to safely ingest this tea. Namely, these active compounds are codeine, morphine, thebaine and papaverine.11
Does Poppy Seed Tea Contain Caffeine?
There is no clear indication whether poppy seed tea contains caffeine. However, poppy seeds are widely used for their mild sedative function, which is a benefit that could be passed on to the tea.12 But take note that this doesn’t mean that poppy seed tea does not cause any of the possible side effects that caffeine has. In fact, excessive intake of poppy seed tea was found to cause anxiety, abdominal cramps and diarrhea.13
Here’s How You Can Brew Poppy Seed Tea at Home
If you want to gain the numerous health benefits of poppy seeds, you can follow this recipe from Chew the World:14
Healthy Poppy Seed Tea Recipe
Ingredients
200 grams (7.04 ounces) poppy seeds
400 milliliters (13.5 ounces) water
Lemon juice, optional
Procedure
In a small saucepan, heat water for a couple of minutes until warm.
Carefully pour the poppy seeds in a sealable glass bottle. Pour the water into the bottle, submerging the poppy seeds completely.
Secure the bottle’s lid. Shake vigorously for a few minutes.
Let it steep for about 15 minutes, and shake again. Let the tea sit for about an hour.
Drain the liquid using a clean tea towel to remove all the debris from the seeds.
If you want to mask the bitter flavor of poppy seed tea, add lemon juice. Serve.
Take note that poppy seed tea should not be ingested in excessive quantities. If you’re just starting out, limit your poppy seeds to 100 grams. Make sure that you test each batch of poppy seeds, as the exact levels of alkaloids present in each batch cannot be ensured.
The fastest way to determine strength is by checking the tea that the seeds yield, depending on its color and taste. A darker and bitterer batch of poppy seed tea is typically stronger. If your current batch is darker than normal, it’s best that you avoid drinking it to eliminate the risk of an accidental overdose.15
To make sure that you’re not accidentally exposing yourself to opiates, rinse the seeds before using them in cooking or brewing. In a 2006 study, it was found that rinsing poppy seeds in hot water (60 degrees Celsius or 140 degrees Fahrenheit) might reduce their morphine content up to about 70 percent.16
What’s the Correct Way to Store Poppy Seeds?
Poppy seeds are available at grocery shops and online stores. Just make sure that you’re getting your supply from trustworthy sources. This will ensure that the seeds you’re using to brew your tea are of the highest quality. To correctly buy and store your poppy seeds, here is a guide from Hunker:17
Check the expiration date on the package. It would also be worthwhile to ask your grocer how long the seeds have been on the shelves. This will help you determine whether the seeds are fresh.
After purchase, transfer the poppy seeds into an airtight glass container.
Store the container in the refrigerator. The seeds may last for up to six months, or a year if kept in the freezer.
Watch Out for These Poppy Seed Tea Side Effects
Although poppy seed tea could offer nutrients and compounds that may help boost your health, improper preparation of this tea may also lead to serious health repercussions. If poppy seeds aren’t cleaned properly before brewing, you might be unknowingly adding opiates to your cup of tea. Some of the most common side effects and complications drinkers may suffer from include:18
Headaches
Loss of concentration
Slowed breathing and lethargy
Death
A 2010 study documented the possible interaction of this tea with certain medications, especially Phenazepam, a drug prescribed for anxiety. In one instance, a patient drank poppy seed tea before taking Phenazepam, which eventually led to his death.19
Because of the absence of studies done on the safe consumption of poppy seed tea during pregnancy, it would be best that you veer away from it if you’re currently pregnant or breastfeeding to avoid any possible risks on your and your child’s well-being.
Poppy Seed Tea May Have Benefits, but Only if Prepared Properly and Consumed in Moderation
Poppy seed tea contains various nutrients and minerals, making it an effective ingredient for combating various ailments. However, it may come with possible side effects and complications. Moderation and caution are extremely important when drinking poppy seed tea so you can reap the benefits without side effects. Make sure that you get only the highest quality product when it comes to poppy seeds, and that you regulate your intake.
Frequently Asked Questions (FAQs) About Poppy Seed Tea
Q: How long does poppy seed tea stay in your system?
A: You may start feeling the effects of poppy seed tea 15 minutes to 30 minutes upon ingestion, the effects of which may last for a few hours to a day, depending on the amount and the strength of the tea.20
Q: What color is poppy seed tea?
A: Poppy seed tea typically has an amber to a brownish hue, depending on the strength of the tea. The darker the tea, the stronger and more concentrated it is.21
Q: How much poppy seed tea can I drink?
A: The amount of poppy seed tea that is safe for consumption is not clear, as it depends on the strength of the tea brewed and the tolerance of the person. It would be best to ask your physician for the ideal dosage.
In addition, poppy seeds usually come with varying amounts of the active alkaloids, which may make it hard for you to gauge its strength. One of the easiest ways to determine your tea’s strength is to observe its color and bitterness level. If your tea is darker or more bitter than your usual brew, consider throwing it out to eliminate the risk of an accidental overdose.22
from Articles http://articles.mercola.com/sites/articles/archive/2019/04/13/xdjm18-teas-18mcsa-poppy-seed-tea.aspx source https://niapurenaturecom.tumblr.com/post/184148274031
0 notes
Text
How to Find Adolescent and Teen Rehabs Near Me
Undergoing a search for the right treatment center for a teenage child is a more common journey for parents than previously thought. In 2016, four percent of adolescents between 12 and 17 years old had a substance use disorder and approximately 180,000 adolescents between 12 and 17 years old were treated at a treatment center for substance abuse. The growing epidemic of opioid misuse is exponentially impacting teens with every passing year.Though signs and consequences of substance abuse are similar between teens and adults, there are programs that specialize in the specific emotional and intellectual needs of teenagers.Receiving treatment with peers of the same age can foster a safe and supportive environment for adolescents that can nurture long-lasting friendships and a support system after treatment. Searching for the right treatment for your teen can be overwhelming and terrifying. There are so many options that can be tailored to meet your child’s treatment needs.Experimentation or Addiction?Before beginning a search for a adolescent rehab or treatment center for your teen, it is recommended to first learn what substances your teen is using, the degree of the use and if there are signs of addiction or chemical dependency. There is a difference between experimenting with substances and being addicted to them.Addiction is when your teen is no longer using and abusing a substance occasionally but now physically needs to use it and depends on its use. Like adults, healthy, smart and high functioning adolescents are susceptible to drug addictions. By knowing the signs and symptoms, parents can look out for red flags in their teens’ behavior before misuse evolves into addiction.In addition to a drug test that will give you clear evidence of substance use, observing sudden changes in your teen’s behavior as described in the following list will give you an idea if your child is abusing drugs or alcohol and has become addicted. It is normal for teens to experience fluctuations in mood and disposition. A consistent pattern of unpredictable behavior may indicate that your teenager has a substance use disorder.Different substances can produce different changes in behavior. Behavioral changes that indicate ongoing misuse or addiction include:Changes in sleeping and eating: A change in appetite is often one of the first signs of substance abuse. Depending on the type of substance being used, your teen’s appetite may either increase or decrease. If your teen frequently smokes marijuana, she may want to eat more frequently or increase her portion. If your teen is abusing stimulants, there might be a sharp decrease in appetite. Extreme changes in sleep patterns like staying up all night or sleeping for long periods during the day may also be an early sign of substance misuse or addiction.New friends and neglecting long-lasting friendships and social circles: Teenagers struggling with addiction may change friends and no longer socialize with friends they have known for a long time. They may stop spending time with old friends in order to hide their substance use and create new relationships with those who also use drugs or alcohol. Other changes in behavior include breaking curfew and lying about their location.Neglecting personal grooming and hygiene: Teenagers are known for being overly conscious about their appearance, wardrobe choices, and overall look and hygiene. Teens who are using or addicted to drugs and/or alcohol often neglect personal hygiene, may shower less, and lose interest in style and clothing.Frequently asking for money: Teens with a substance use disorder tend to ask for money without communicating a reason. They may also be secretive about spending habits. A common behavior for both teen and adult addicts is to ask regularly for small amounts of money or lie about how much they need for a necessity so they can keep the extra money.Other signs of substance abuse and addiction include:Increased anger and aggression and getting into conflicts.Receiving disciplinary action at school.Signs of antisocial behavior and withdrawing from family and friends.Skipping classes and neglecting school work which result in a drop in grades.Losing interest in hobbies and after school activities and sports.Finding drug and alcohol paraphernalia like pill bottles, pipes, needles, liquor bottles.Specific Signs of Substance Abuse in TeensThough signs of abuse and addiction are similar regardless of the substance, there are some drugs that offer specific warning signs:Marijuana: Symptoms of ongoing marijuana use include excessive sleep, overeating, weight gain, loss of motivation, decreased interest in hobbies and activities, red and glassy eyes.Depressants (Examples include Xanax, GHB, and Valium): Symptoms of the abuse of depressants include blurry vision, drunk-like behavior, clumsiness, difficulty concentrating, slurred speech, sleepiness and poor judgment.Stimulants (Examples include cocaine, amphetamines, crystal meth): Symptoms of the abuse of stimulants includes hyperactivity, dilated pupils, irritability, euphoria, excessive talking, anxiety, going long periods of time without eating or sleeping, dry mouth and nose.Opioids (Examples include heroin, morphine, codeine, fentanyl, oxycodone also known as OxyContin, Roxicodone, or Percocet, hydrocodone also known as Vicodin, Lortab, or Norco): Symptoms of opioid abuse include contracted pupils, wearing long sleeves and long pants even during warm weather to hide marks from injecting, excessive sweating, coughing and sniffling, sleeping at unusual times and nodding off, twitching, loss of appetite, noticeable elation or euphoria, slowed breathing, constipation.Hallucinogens (Examples include PCP and LSD): Symptoms of the abuse of hallucinogens include dilated pupils, aggression, frequent mood swings, bizarre and irrational behavior, paranoia, hallucinations, slurred speech, confusion, absorption with objects or self, detachment from others.Inhalants (Examples include aerosols, glues, and vapors): Symptoms of the abuse of inhalants include loss of memory, interrupted thought, watery eyes, frequent headaches, nausea, secretions from the nose, rashes around the mouth and nose, poor muscle control, anxiety, drowsiness, drunk-like appearance, drastic change in appetite.How to find a residential adolescent treatment programOnce parents have identified that their teens have a substance use disorder, it can be daunting to know where to begin to find treatment. Your child’s pediatrician and school counselor may help navigate available options. A drug treatment professional can help diagnose your teen’s drug use or addiction and suggest the most effective treatment approach. Every adolescent is different and so is their treatment plan. What may work well for one teen might not be the most effective journey for another teen.Though outpatient rehab has benefits, some experts recommend that inpatient treatment is the best, most effective course of treatment for teens.Residential treatment usually entails staying in a facility that offers both treatment and accommodations onsite, for 28 to 90 days or longer. During that time, the teens take part in group and individual therapy to identify the underlying causes of addiction, discover negative beliefs and issues that led them to drug use, and build tools and skills that will help them remain drug-free after treatment.The idea of residential treatment for adolescents can be scary for parents. Most inpatient facilities have family days where family members are encouraged to participate in therapy sessions. Residential programs that cater to teens are designed to stabilize them so they can be reunited with families as soon as possible. The most effective programs collaborate with families and ensure families feel like they are an active part in their child’s treatment.While in treatment, teens will live in an environment that supports sobriety and offers them structure and protection from the temptations of the outside world. Adolescent residential treatment programs are located throughout the country. There are also residential treatment programs that accept both adults and teens. Your family may prefer to find a program close to home while others may opt for a program further away from their teen’s daily life and routines.Aside from insurance coverage, deciding on where to admit your teen and how far to travel depends on many considerations. Does the treatment center allow visitations after a certain time? Will you be able to travel to that facility easily? Research has shown that out of state facilities can benefit patients because it decreases the chance of a patient leaving early.What happens in residential treatment?Before a teenager enters a residential rehabilitation program, they are evaluated by staff during detoxification to determine the best course of treatment. An individualized course of treatment depends on what substances the patient is addicted to. Often teen clients are addicted to more than one drug or they use drugs and alcohol. In these instances, treatment professionals craft a poly-substance dependence treatment plan.All clients in an adolescent treatment program should be treated as individuals with their own specific circumstances and have a written treatment plan that includes specialized care for dual diagnosis and co-occurring disorders to meet their needs.Since teens are especially vulnerable to the lasting dangers of substance abuse because their bodies and brains are still growing and developing, adolescent clients in treatment go through a particular order of steps to overcome their addiction which includes:Detoxification with assistance from medications if necessaryCommitment to cooperate with counselors during treatmentHave co-occurring conditions assessed and diagnosedMonitoring and re-adjusting treatment plansMaking sure a teenager does not have a relapse during treatmentAttending one-on-one and group counseling sessionsAttending daily mutual aid meetings such as Alcoholics AnonymousCounseling sessions with relatives and friendsMaking aftercare plans for after residential treatmentHaving follow-up treatment plans after leaving a facilityTypes of Counseling OfferedCounseling sessions for teenagers are held in both group and one-on-one settings. Eventually, parents, siblings, and friends also attend counseling sessions to help a teenager adjust to returning home or to school. Teens undergo several types of therapies in order to change their mental attitude when it comes to drug and alcohol use.Some of the therapies include Motivational Interviewing (MI), multidimensional family counseling, Cognitive Behavioral Therapy (CBT) and motivational incentives.Teenagers seeking detox and rehabilitation may also have co-occurring conditions that make treatment more complex. Some of these conditions include panic, social, and generalized anxiety disorders, bipolar disorder, dysthymia and depression, attention deficit and hyperactivity attention disorders and more serious mental illnesses like schizophrenia.While in treatment, a teenager may need medications, treatment, and counseling for both their substance use disorder and co-occurring mental health conditions. When a teenager has a co-occurring disorder, a rehabilitation program will probably need to last longer. Clinicians will monitor and adjust a teenager’s medications carefully in order to help them overcome their addiction while also treating a mental illness or mood disorder.What to look for in an inpatient treatment facilityThe most important factor when choosing a rehab center for your teen is knowing that the center chosen will effectively provide the services necessary for a successful rehabilitation. It is important to attend any scheduled visitations, and while in the facility, take note of how your child appears. For example, does your teen seem comfortable and do they appear to feel safe. Not all treatment centers may value making a profit over the best interest of your teen. To ensure the safety and well-being of your teen, here are certain characteristics in residential treatment programs you should look for before admitting your child:How long is the residential treatment program?Is the facility fully licensed? The federal law requires facilities that provide any type of treatment, including detox, therapy, treatment planning and rehabilitation, to be licensed.Is the facility accredited by CARF? CARF, the Commission on Accreditation of Rehabilitation Facilities, assesses treatment centers to determine the level of care they can administer. When a program has CARF accreditation, it means the rehab center has been assessed and meets the high standards of care requirements.Is the staff professional and well trained? When visiting potential rehab centers for your teen, it is important to pay careful attention to the treatment provided by the staff and how they interact with clients. Are clients comfortable with the staff? Does the staff exhibit genuine concern for the well being of their clients? Do clients appear to be comfortable and safe around the staff? Does the facility conduct background checks on all staff members including support staff? What credentials do the therapists and treatment professionals have?What is the facility’s success rate? When interviewing potential rehab centers, make sure to ask about their success rate. Generally, the higher the success rate is, the better the outcome may be for your teen.What condition is the facility? The facility should be clean, well-organized and have appropriate living quarters. What are the living and sleeping arrangements?What are the amenities? Amenities can include gym and exercise, recreational activities, off-site trips and events. Is there a gym and exercise program? A media center and access to the Internet?When in the day do clients receive schooling? Are computer and access to the Internet available for educational purposes only?What is the facility’s rules for personal cell phone and device use?What are meals like? Are high sugar snacks restricted?What is a typical schedule for clients? What time is lights out?How often can families visit and speak with a client? What are visitation hours?How do you include families in a child’s treatment?How will the facility communicate with parents and how often?Will you be kept up to date regularly about your teen’s recovery?Is the program teens only or are adults clients also admitted? It’s important that an inpatient treatment facility is able to cater to teens’ evolving emotional and intellectual needs and the professional staff understand how to care for an adolescent who in undergoing rapid hormonal changes.How will this program support my teen’s schooling? Parents are concerned if a long term residential treatment program can cause a teen to fall behind in school. Usually residential treatment programs for teens will offer tutoring and assign curriculum based classes and assignments.What aftercare is provided? Many inpatient treatment programs will have aftercare which means they offer groups and resources for patients who have been released from inpatient care so they can continue to receive treatment and therapy while returning to their lives.Covering The Cost Of Your Teen’s RehabIn 2014, the Affordable Care Act impacted the way in which most insurance companies approach mental health and substance use treatment. They are now legally required to offer coverage for these issues. However, it’s important to note not all policies are the same, especially when it comes to mental health care.Before moving forward with deciding on a residential adolescent rehab, first speak with your insurance provider to determine if your child’s treatment will be covered. Many residential treatment centers accept insurance, but some insurance policies do not cover the cost of addiction treatment or may not cover out-of-state treatment. When you have determined that your teen will qualify for insurance coverage, you can then identify a rehab center that accepts your insurance. If a residential program doesn’t accept insurance or your insurance doesn’t cover addiction treatment, ask if the program offers a sliding scale fee that’s contingent on your income.
from RSSMix.com Mix ID 8241841 https://www.thefix.com/how-find-adolescent-and-teen-rehabs-near-me
0 notes
Text
How to Find Adolescent and Teen Rehabs Near Me
Undergoing a search for the right treatment center for a teenage child is a more common journey for parents than previously thought. In 2016, four percent of adolescents between 12 and 17 years old had a substance use disorder and approximately 180,000 adolescents between 12 and 17 years old were treated at a treatment center for substance abuse. The growing epidemic of opioid misuse is exponentially impacting teens with every passing year.Though signs and consequences of substance abuse are similar between teens and adults, there are programs that specialize in the specific emotional and intellectual needs of teenagers.Receiving treatment with peers of the same age can foster a safe and supportive environment for adolescents that can nurture long-lasting friendships and a support system after treatment. Searching for the right treatment for your teen can be overwhelming and terrifying. There are so many options that can be tailored to meet your child’s treatment needs.Experimentation or Addiction?Before beginning a search for a adolescent rehab or treatment center for your teen, it is recommended to first learn what substances your teen is using, the degree of the use and if there are signs of addiction or chemical dependency. There is a difference between experimenting with substances and being addicted to them.Addiction is when your teen is no longer using and abusing a substance occasionally but now physically needs to use it and depends on its use. Like adults, healthy, smart and high functioning adolescents are susceptible to drug addictions. By knowing the signs and symptoms, parents can look out for red flags in their teens’ behavior before misuse evolves into addiction.In addition to a drug test that will give you clear evidence of substance use, observing sudden changes in your teen’s behavior as described in the following list will give you an idea if your child is abusing drugs or alcohol and has become addicted. It is normal for teens to experience fluctuations in mood and disposition. A consistent pattern of unpredictable behavior may indicate that your teenager has a substance use disorder.Different substances can produce different changes in behavior. Behavioral changes that indicate ongoing misuse or addiction include:Changes in sleeping and eating: A change in appetite is often one of the first signs of substance abuse. Depending on the type of substance being used, your teen’s appetite may either increase or decrease. If your teen frequently smokes marijuana, she may want to eat more frequently or increase her portion. If your teen is abusing stimulants, there might be a sharp decrease in appetite. Extreme changes in sleep patterns like staying up all night or sleeping for long periods during the day may also be an early sign of substance misuse or addiction.New friends and neglecting long-lasting friendships and social circles: Teenagers struggling with addiction may change friends and no longer socialize with friends they have known for a long time. They may stop spending time with old friends in order to hide their substance use and create new relationships with those who also use drugs or alcohol. Other changes in behavior include breaking curfew and lying about their location.Neglecting personal grooming and hygiene: Teenagers are known for being overly conscious about their appearance, wardrobe choices, and overall look and hygiene. Teens who are using or addicted to drugs and/or alcohol often neglect personal hygiene, may shower less, and lose interest in style and clothing.Frequently asking for money: Teens with a substance use disorder tend to ask for money without communicating a reason. They may also be secretive about spending habits. A common behavior for both teen and adult addicts is to ask regularly for small amounts of money or lie about how much they need for a necessity so they can keep the extra money.Other signs of substance abuse and addiction include:Increased anger and aggression and getting into conflicts.Receiving disciplinary action at school.Signs of antisocial behavior and withdrawing from family and friends.Skipping classes and neglecting school work which result in a drop in grades.Losing interest in hobbies and after school activities and sports.Finding drug and alcohol paraphernalia like pill bottles, pipes, needles, liquor bottles.Specific Signs of Substance Abuse in TeensThough signs of abuse and addiction are similar regardless of the substance, there are some drugs that offer specific warning signs:Marijuana: Symptoms of ongoing marijuana use include excessive sleep, overeating, weight gain, loss of motivation, decreased interest in hobbies and activities, red and glassy eyes.Depressants (Examples include Xanax, GHB, and Valium): Symptoms of the abuse of depressants include blurry vision, drunk-like behavior, clumsiness, difficulty concentrating, slurred speech, sleepiness and poor judgment.Stimulants (Examples include cocaine, amphetamines, crystal meth): Symptoms of the abuse of stimulants includes hyperactivity, dilated pupils, irritability, euphoria, excessive talking, anxiety, going long periods of time without eating or sleeping, dry mouth and nose.Opioids (Examples include heroin, morphine, codeine, fentanyl, oxycodone also known as OxyContin, Roxicodone, or Percocet, hydrocodone also known as Vicodin, Lortab, or Norco): Symptoms of opioid abuse include contracted pupils, wearing long sleeves and long pants even during warm weather to hide marks from injecting, excessive sweating, coughing and sniffling, sleeping at unusual times and nodding off, twitching, loss of appetite, noticeable elation or euphoria, slowed breathing, constipation.Hallucinogens (Examples include PCP and LSD): Symptoms of the abuse of hallucinogens include dilated pupils, aggression, frequent mood swings, bizarre and irrational behavior, paranoia, hallucinations, slurred speech, confusion, absorption with objects or self, detachment from others.Inhalants (Examples include aerosols, glues, and vapors): Symptoms of the abuse of inhalants include loss of memory, interrupted thought, watery eyes, frequent headaches, nausea, secretions from the nose, rashes around the mouth and nose, poor muscle control, anxiety, drowsiness, drunk-like appearance, drastic change in appetite.How to find a residential adolescent treatment programOnce parents have identified that their teens have a substance use disorder, it can be daunting to know where to begin to find treatment. Your child’s pediatrician and school counselor may help navigate available options. A drug treatment professional can help diagnose your teen’s drug use or addiction and suggest the most effective treatment approach. Every adolescent is different and so is their treatment plan. What may work well for one teen might not be the most effective journey for another teen.Though outpatient rehab has benefits, some experts recommend that inpatient treatment is the best, most effective course of treatment for teens.Residential treatment usually entails staying in a facility that offers both treatment and accommodations onsite, for 28 to 90 days or longer. During that time, the teens take part in group and individual therapy to identify the underlying causes of addiction, discover negative beliefs and issues that led them to drug use, and build tools and skills that will help them remain drug-free after treatment.The idea of residential treatment for adolescents can be scary for parents. Most inpatient facilities have family days where family members are encouraged to participate in therapy sessions. Residential programs that cater to teens are designed to stabilize them so they can be reunited with families as soon as possible. The most effective programs collaborate with families and ensure families feel like they are an active part in their child’s treatment.While in treatment, teens will live in an environment that supports sobriety and offers them structure and protection from the temptations of the outside world. Adolescent residential treatment programs are located throughout the country. There are also residential treatment programs that accept both adults and teens. Your family may prefer to find a program close to home while others may opt for a program further away from their teen’s daily life and routines.Aside from insurance coverage, deciding on where to admit your teen and how far to travel depends on many considerations. Does the treatment center allow visitations after a certain time? Will you be able to travel to that facility easily? Research has shown that out of state facilities can benefit patients because it decreases the chance of a patient leaving early.What happens in residential treatment?Before a teenager enters a residential rehabilitation program, they are evaluated by staff during detoxification to determine the best course of treatment. An individualized course of treatment depends on what substances the patient is addicted to. Often teen clients are addicted to more than one drug or they use drugs and alcohol. In these instances, treatment professionals craft a poly-substance dependence treatment plan.All clients in an adolescent treatment program should be treated as individuals with their own specific circumstances and have a written treatment plan that includes specialized care for dual diagnosis and co-occurring disorders to meet their needs.Since teens are especially vulnerable to the lasting dangers of substance abuse because their bodies and brains are still growing and developing, adolescent clients in treatment go through a particular order of steps to overcome their addiction which includes:Detoxification with assistance from medications if necessaryCommitment to cooperate with counselors during treatmentHave co-occurring conditions assessed and diagnosedMonitoring and re-adjusting treatment plansMaking sure a teenager does not have a relapse during treatmentAttending one-on-one and group counseling sessionsAttending daily mutual aid meetings such as Alcoholics AnonymousCounseling sessions with relatives and friendsMaking aftercare plans for after residential treatmentHaving follow-up treatment plans after leaving a facilityTypes of Counseling OfferedCounseling sessions for teenagers are held in both group and one-on-one settings. Eventually, parents, siblings, and friends also attend counseling sessions to help a teenager adjust to returning home or to school. Teens undergo several types of therapies in order to change their mental attitude when it comes to drug and alcohol use.Some of the therapies include Motivational Interviewing (MI), multidimensional family counseling, Cognitive Behavioral Therapy (CBT) and motivational incentives.Teenagers seeking detox and rehabilitation may also have co-occurring conditions that make treatment more complex. Some of these conditions include panic, social, and generalized anxiety disorders, bipolar disorder, dysthymia and depression, attention deficit and hyperactivity attention disorders and more serious mental illnesses like schizophrenia.While in treatment, a teenager may need medications, treatment, and counseling for both their substance use disorder and co-occurring mental health conditions. When a teenager has a co-occurring disorder, a rehabilitation program will probably need to last longer. Clinicians will monitor and adjust a teenager’s medications carefully in order to help them overcome their addiction while also treating a mental illness or mood disorder.What to look for in an inpatient treatment facilityThe most important factor when choosing a rehab center for your teen is knowing that the center chosen will effectively provide the services necessary for a successful rehabilitation. It is important to attend any scheduled visitations, and while in the facility, take note of how your child appears. For example, does your teen seem comfortable and do they appear to feel safe. Not all treatment centers may value making a profit over the best interest of your teen. To ensure the safety and well-being of your teen, here are certain characteristics in residential treatment programs you should look for before admitting your child:How long is the residential treatment program?Is the facility fully licensed? The federal law requires facilities that provide any type of treatment, including detox, therapy, treatment planning and rehabilitation, to be licensed.Is the facility accredited by CARF? CARF, the Commission on Accreditation of Rehabilitation Facilities, assesses treatment centers to determine the level of care they can administer. When a program has CARF accreditation, it means the rehab center has been assessed and meets the high standards of care requirements.Is the staff professional and well trained? When visiting potential rehab centers for your teen, it is important to pay careful attention to the treatment provided by the staff and how they interact with clients. Are clients comfortable with the staff? Does the staff exhibit genuine concern for the well being of their clients? Do clients appear to be comfortable and safe around the staff? Does the facility conduct background checks on all staff members including support staff? What credentials do the therapists and treatment professionals have?What is the facility’s success rate? When interviewing potential rehab centers, make sure to ask about their success rate. Generally, the higher the success rate is, the better the outcome may be for your teen.What condition is the facility? The facility should be clean, well-organized and have appropriate living quarters. What are the living and sleeping arrangements?What are the amenities? Amenities can include gym and exercise, recreational activities, off-site trips and events. Is there a gym and exercise program? A media center and access to the Internet?When in the day do clients receive schooling? Are computer and access to the Internet available for educational purposes only?What is the facility’s rules for personal cell phone and device use?What are meals like? Are high sugar snacks restricted?What is a typical schedule for clients? What time is lights out?How often can families visit and speak with a client? What are visitation hours?How do you include families in a child’s treatment?How will the facility communicate with parents and how often?Will you be kept up to date regularly about your teen’s recovery?Is the program teens only or are adults clients also admitted? It’s important that an inpatient treatment facility is able to cater to teens’ evolving emotional and intellectual needs and the professional staff understand how to care for an adolescent who in undergoing rapid hormonal changes.How will this program support my teen’s schooling? Parents are concerned if a long term residential treatment program can cause a teen to fall behind in school. Usually residential treatment programs for teens will offer tutoring and assign curriculum based classes and assignments.What aftercare is provided? Many inpatient treatment programs will have aftercare which means they offer groups and resources for patients who have been released from inpatient care so they can continue to receive treatment and therapy while returning to their lives.Covering The Cost Of Your Teen’s RehabIn 2014, the Affordable Care Act impacted the way in which most insurance companies approach mental health and substance use treatment. They are now legally required to offer coverage for these issues. However, it’s important to note not all policies are the same, especially when it comes to mental health care.Before moving forward with deciding on a residential adolescent rehab, first speak with your insurance provider to determine if your child’s treatment will be covered. Many residential treatment centers accept insurance, but some insurance policies do not cover the cost of addiction treatment or may not cover out-of-state treatment. When you have determined that your teen will qualify for insurance coverage, you can then identify a rehab center that accepts your insurance. If a residential program doesn’t accept insurance or your insurance doesn’t cover addiction treatment, ask if the program offers a sliding scale fee that’s contingent on your income.
from RSSMix.com Mix ID 8241841 https://ift.tt/2TMHa3q
0 notes
Text
How to Find Adolescent and Teen Rehabs Near Me
Undergoing a search for the right treatment center for a teenage child is a more common journey for parents than previously thought. In 2016, four percent of adolescents between 12 and 17 years old had a substance use disorder and approximately 180,000 adolescents between 12 and 17 years old were treated at a treatment center for substance abuse. The growing epidemic of opioid misuse is exponentially impacting teens with every passing year.Though signs and consequences of substance abuse are similar between teens and adults, there are programs that specialize in the specific emotional and intellectual needs of teenagers.Receiving treatment with peers of the same age can foster a safe and supportive environment for adolescents that can nurture long-lasting friendships and a support system after treatment. Searching for the right treatment for your teen can be overwhelming and terrifying. There are so many options that can be tailored to meet your child’s treatment needs.Experimentation or Addiction?Before beginning a search for a adolescent rehab or treatment center for your teen, it is recommended to first learn what substances your teen is using, the degree of the use and if there are signs of addiction or chemical dependency. There is a difference between experimenting with substances and being addicted to them.Addiction is when your teen is no longer using and abusing a substance occasionally but now physically needs to use it and depends on its use. Like adults, healthy, smart and high functioning adolescents are susceptible to drug addictions. By knowing the signs and symptoms, parents can look out for red flags in their teens’ behavior before misuse evolves into addiction.In addition to a drug test that will give you clear evidence of substance use, observing sudden changes in your teen’s behavior as described in the following list will give you an idea if your child is abusing drugs or alcohol and has become addicted. It is normal for teens to experience fluctuations in mood and disposition. A consistent pattern of unpredictable behavior may indicate that your teenager has a substance use disorder.Different substances can produce different changes in behavior. Behavioral changes that indicate ongoing misuse or addiction include:Changes in sleeping and eating: A change in appetite is often one of the first signs of substance abuse. Depending on the type of substance being used, your teen’s appetite may either increase or decrease. If your teen frequently smokes marijuana, she may want to eat more frequently or increase her portion. If your teen is abusing stimulants, there might be a sharp decrease in appetite. Extreme changes in sleep patterns like staying up all night or sleeping for long periods during the day may also be an early sign of substance misuse or addiction.New friends and neglecting long-lasting friendships and social circles: Teenagers struggling with addiction may change friends and no longer socialize with friends they have known for a long time. They may stop spending time with old friends in order to hide their substance use and create new relationships with those who also use drugs or alcohol. Other changes in behavior include breaking curfew and lying about their location.Neglecting personal grooming and hygiene: Teenagers are known for being overly conscious about their appearance, wardrobe choices, and overall look and hygiene. Teens who are using or addicted to drugs and/or alcohol often neglect personal hygiene, may shower less, and lose interest in style and clothing.Frequently asking for money: Teens with a substance use disorder tend to ask for money without communicating a reason. They may also be secretive about spending habits. A common behavior for both teen and adult addicts is to ask regularly for small amounts of money or lie about how much they need for a necessity so they can keep the extra money.Other signs of substance abuse and addiction include:Increased anger and aggression and getting into conflicts.Receiving disciplinary action at school.Signs of antisocial behavior and withdrawing from family and friends.Skipping classes and neglecting school work which result in a drop in grades.Losing interest in hobbies and after school activities and sports.Finding drug and alcohol paraphernalia like pill bottles, pipes, needles, liquor bottles.Specific Signs of Substance Abuse in TeensThough signs of abuse and addiction are similar regardless of the substance, there are some drugs that offer specific warning signs:Marijuana: Symptoms of ongoing marijuana use include excessive sleep, overeating, weight gain, loss of motivation, decreased interest in hobbies and activities, red and glassy eyes.Depressants (Examples include Xanax, GHB, and Valium): Symptoms of the abuse of depressants include blurry vision, drunk-like behavior, clumsiness, difficulty concentrating, slurred speech, sleepiness and poor judgment.Stimulants (Examples include cocaine, amphetamines, crystal meth): Symptoms of the abuse of stimulants includes hyperactivity, dilated pupils, irritability, euphoria, excessive talking, anxiety, going long periods of time without eating or sleeping, dry mouth and nose.Opioids (Examples include heroin, morphine, codeine, fentanyl, oxycodone also known as OxyContin, Roxicodone, or Percocet, hydrocodone also known as Vicodin, Lortab, or Norco): Symptoms of opioid abuse include contracted pupils, wearing long sleeves and long pants even during warm weather to hide marks from injecting, excessive sweating, coughing and sniffling, sleeping at unusual times and nodding off, twitching, loss of appetite, noticeable elation or euphoria, slowed breathing, constipation.Hallucinogens (Examples include PCP and LSD): Symptoms of the abuse of hallucinogens include dilated pupils, aggression, frequent mood swings, bizarre and irrational behavior, paranoia, hallucinations, slurred speech, confusion, absorption with objects or self, detachment from others.Inhalants (Examples include aerosols, glues, and vapors): Symptoms of the abuse of inhalants include loss of memory, interrupted thought, watery eyes, frequent headaches, nausea, secretions from the nose, rashes around the mouth and nose, poor muscle control, anxiety, drowsiness, drunk-like appearance, drastic change in appetite.How to find a residential adolescent treatment programOnce parents have identified that their teens have a substance use disorder, it can be daunting to know where to begin to find treatment. Your child’s pediatrician and school counselor may help navigate available options. A drug treatment professional can help diagnose your teen’s drug use or addiction and suggest the most effective treatment approach. Every adolescent is different and so is their treatment plan. What may work well for one teen might not be the most effective journey for another teen.Though outpatient rehab has benefits, some experts recommend that inpatient treatment is the best, most effective course of treatment for teens.Residential treatment usually entails staying in a facility that offers both treatment and accommodations onsite, for 28 to 90 days or longer. During that time, the teens take part in group and individual therapy to identify the underlying causes of addiction, discover negative beliefs and issues that led them to drug use, and build tools and skills that will help them remain drug-free after treatment.The idea of residential treatment for adolescents can be scary for parents. Most inpatient facilities have family days where family members are encouraged to participate in therapy sessions. Residential programs that cater to teens are designed to stabilize them so they can be reunited with families as soon as possible. The most effective programs collaborate with families and ensure families feel like they are an active part in their child’s treatment.While in treatment, teens will live in an environment that supports sobriety and offers them structure and protection from the temptations of the outside world. Adolescent residential treatment programs are located throughout the country. There are also residential treatment programs that accept both adults and teens. Your family may prefer to find a program close to home while others may opt for a program further away from their teen’s daily life and routines.Aside from insurance coverage, deciding on where to admit your teen and how far to travel depends on many considerations. Does the treatment center allow visitations after a certain time? Will you be able to travel to that facility easily? Research has shown that out of state facilities can benefit patients because it decreases the chance of a patient leaving early.What happens in residential treatment?Before a teenager enters a residential rehabilitation program, they are evaluated by staff during detoxification to determine the best course of treatment. An individualized course of treatment depends on what substances the patient is addicted to. Often teen clients are addicted to more than one drug or they use drugs and alcohol. In these instances, treatment professionals craft a poly-substance dependence treatment plan.All clients in an adolescent treatment program should be treated as individuals with their own specific circumstances and have a written treatment plan that includes specialized care for dual diagnosis and co-occurring disorders to meet their needs.Since teens are especially vulnerable to the lasting dangers of substance abuse because their bodies and brains are still growing and developing, adolescent clients in treatment go through a particular order of steps to overcome their addiction which includes:Detoxification with assistance from medications if necessaryCommitment to cooperate with counselors during treatmentHave co-occurring conditions assessed and diagnosedMonitoring and re-adjusting treatment plansMaking sure a teenager does not have a relapse during treatmentAttending one-on-one and group counseling sessionsAttending daily mutual aid meetings such as Alcoholics AnonymousCounseling sessions with relatives and friendsMaking aftercare plans for after residential treatmentHaving follow-up treatment plans after leaving a facilityTypes of Counseling OfferedCounseling sessions for teenagers are held in both group and one-on-one settings. Eventually, parents, siblings, and friends also attend counseling sessions to help a teenager adjust to returning home or to school. Teens undergo several types of therapies in order to change their mental attitude when it comes to drug and alcohol use.Some of the therapies include Motivational Interviewing (MI), multidimensional family counseling, Cognitive Behavioral Therapy (CBT) and motivational incentives.Teenagers seeking detox and rehabilitation may also have co-occurring conditions that make treatment more complex. Some of these conditions include panic, social, and generalized anxiety disorders, bipolar disorder, dysthymia and depression, attention deficit and hyperactivity attention disorders and more serious mental illnesses like schizophrenia.While in treatment, a teenager may need medications, treatment, and counseling for both their substance use disorder and co-occurring mental health conditions. When a teenager has a co-occurring disorder, a rehabilitation program will probably need to last longer. Clinicians will monitor and adjust a teenager’s medications carefully in order to help them overcome their addiction while also treating a mental illness or mood disorder.What to look for in an inpatient treatment facilityThe most important factor when choosing a rehab center for your teen is knowing that the center chosen will effectively provide the services necessary for a successful rehabilitation. It is important to attend any scheduled visitations, and while in the facility, take note of how your child appears. For example, does your teen seem comfortable and do they appear to feel safe. Not all treatment centers may value making a profit over the best interest of your teen. To ensure the safety and well-being of your teen, here are certain characteristics in residential treatment programs you should look for before admitting your child:How long is the residential treatment program?Is the facility fully licensed? The federal law requires facilities that provide any type of treatment, including detox, therapy, treatment planning and rehabilitation, to be licensed.Is the facility accredited by CARF? CARF, the Commission on Accreditation of Rehabilitation Facilities, assesses treatment centers to determine the level of care they can administer. When a program has CARF accreditation, it means the rehab center has been assessed and meets the high standards of care requirements.Is the staff professional and well trained? When visiting potential rehab centers for your teen, it is important to pay careful attention to the treatment provided by the staff and how they interact with clients. Are clients comfortable with the staff? Does the staff exhibit genuine concern for the well being of their clients? Do clients appear to be comfortable and safe around the staff? Does the facility conduct background checks on all staff members including support staff? What credentials do the therapists and treatment professionals have?What is the facility’s success rate? When interviewing potential rehab centers, make sure to ask about their success rate. Generally, the higher the success rate is, the better the outcome may be for your teen.What condition is the facility? The facility should be clean, well-organized and have appropriate living quarters. What are the living and sleeping arrangements?What are the amenities? Amenities can include gym and exercise, recreational activities, off-site trips and events. Is there a gym and exercise program? A media center and access to the Internet?When in the day do clients receive schooling? Are computer and access to the Internet available for educational purposes only?What is the facility’s rules for personal cell phone and device use?What are meals like? Are high sugar snacks restricted?What is a typical schedule for clients? What time is lights out?How often can families visit and speak with a client? What are visitation hours?How do you include families in a child’s treatment?How will the facility communicate with parents and how often?Will you be kept up to date regularly about your teen’s recovery?Is the program teens only or are adults clients also admitted? It’s important that an inpatient treatment facility is able to cater to teens’ evolving emotional and intellectual needs and the professional staff understand how to care for an adolescent who in undergoing rapid hormonal changes.How will this program support my teen’s schooling? Parents are concerned if a long term residential treatment program can cause a teen to fall behind in school. Usually residential treatment programs for teens will offer tutoring and assign curriculum based classes and assignments.What aftercare is provided? Many inpatient treatment programs will have aftercare which means they offer groups and resources for patients who have been released from inpatient care so they can continue to receive treatment and therapy while returning to their lives.Covering The Cost Of Your Teen’s RehabIn 2014, the Affordable Care Act impacted the way in which most insurance companies approach mental health and substance use treatment. They are now legally required to offer coverage for these issues. However, it’s important to note not all policies are the same, especially when it comes to mental health care.Before moving forward with deciding on a residential adolescent rehab, first speak with your insurance provider to determine if your child’s treatment will be covered. Many residential treatment centers accept insurance, but some insurance policies do not cover the cost of addiction treatment or may not cover out-of-state treatment. When you have determined that your teen will qualify for insurance coverage, you can then identify a rehab center that accepts your insurance. If a residential program doesn’t accept insurance or your insurance doesn’t cover addiction treatment, ask if the program offers a sliding scale fee that’s contingent on your income.
0 notes
Text
Details Regarding Opiate Addiction Therapy Utah
Details Regarding Opiate Dependency Treatment Utah
youtube
Visit a drug treatment center near you:
In instance you notice that a person close to you could not endure without heroine or morphine or perhaps codeine you have to try assisting them. When bordered by such people is not to evaluate however aid them obtain opiate dependency treatment Utah, anybody can be stuck in this roadway as a result best one can do. They have to improve promptly to make sure that they proceed with their lives. Finding Axis Treatment West Los Angeles is the primary step in the direction of recovery. Axis Treatment Indian Wells should be surrounded by a strong as well as sober support system given that a lot of them feel afraid to start the procedure. One is made to select between an outpatient facility or an inpatient one relying on exactly how poor the problem of their liked one is. Different centers vary relying on what a private demands. They will certainly be offered private and also team therapies to complement the education they are obtaining. The ideal feature of inpatient programs is that individuals obtain detox drug first to handle withdrawal signs before actual education and learning begins which somewhat makes it much less challenging to deal with. Not every person who might have abusive these substances at one factor are referred to as an addict.
Unlike Morgellons condition Lyme condition is currently recognized as a legitimate illness that can be identified through medical analysis skills and also laboratory tests. The real pathogen that is triggering Morgellons illness is at the existing unknown. It may be an old infection that has been around for eons. It might be a new kind of infection that has actually entered play via evolution, international traveling, the destruction of the Amazon.com and also African jungle or even external space. It might be a new sort of infection - a parasite, a worm, germs, a virus, a preon or something not also known yet. No one understands. Perhaps it is also sent in a concealed fashion comparable to mad cow illness. The signs of clients presenting with Morgellons are diverse as well as sadly for the endured might match numerous various other clinical conditions the majority of which are widely recognized which clinical pupils and also medical professionals are taught to swiftly treat and also recognize. One of the most unsafe compounds to this day is heroin. Heroin misuse causes thousands of overdoses daily in the US. The number of friends have you shed to overdose? Will you be the next target? STOP. Change your life now as well as allow us assist you find the most effective heroin rehab offered! We have a network of hundreds of rehab centers. We'll aid you locate the ideal one for your one-of-a-kind requirements. Your life does not need to revolve heroin misuse and also addiction. We will help you damage the cycle, all you should do is get the phone and also call us. If you're like most individuals with substance use problems, you have actually postponed substance abuse treatment for months- maybe years. Addiction is an illness, and like any various other it can be efficiently dealt with. Following to heroin, alcohol material use conditions are among one of the most severe dependencies that don't get the nationwide interest the condition is worthy of. Alcohol dependency could be conveniently hidden as a social activity, and proceeds in seriousness rapidly as resistance starts to establish itself in the body.- simply like heroin. It's not far too late obtain alcoholic abuse therapy! Call us now to start alcoholism therapy! Including alcohol detox facilities, we provide the most effective in drug detox facilities, specializing in safe cocaine detox. Therapy adheres to comparable procedures, and also yields essentially no negative medicine detox signs!
Have you had terrible outbursts that you did not experience prior to doing meth
15 Neglected Signs of Methamphetamine Usage
Increase appetite
Experience statements
Does Dependency Run in Families? (National Institute on Drug Abuse) Additionally in Spanish
On the off opportunity that you see your oral practitioner and they presume that you require an origin trench, there are a few exercises that they will lead in order to spare your tooth as well as improve help to you. 1. A X-beam: This is the major action that the dental professional will do when they speculate that you might require a root river. They will take X-beams to evaluate your tooth and also identify where the rot or boil could be. 2. Anesthetic: When you at long last most likely to their office for the origin trench approach, the dental expert will certainly put you on some neighborhood anesthetic. It is attached to the tooth that is affected. This keeps you from really feeling torture as well as various kind of distress in the middle of the technique. 3. A pulpectomy: In this system, the dental professional makes an opening in your tooth as well as leaves the tainted mash inside it. 4. A filling: This is a strategy that is routed upon the roots which have actually been opened up. The mash has actually been expelled from them and they are filled up with a product understood as gutta-percha. From that point onward, the dental expert seals them with concrete. After the method, you will really feel somewhere in the variety of special in the area where the Endodontic therapy was led. This is an indication of recovering. Regardless of that, your jaw can really feel fragile and also sore. Since of opening your mouth for the size of the root network method, this is. The oral practitioner will recommend some torture assistance drug. You should take them based on their guidelines as well as additionally recall not to work apparatus since the torture executioners can make you tired. When the insensible disposition in your mouth has actually used off, assurance that you don't eat anything at all up until the factor. Regardless of that, do not munch or attack using the tooth that obtained the root trench. In addition, maintain dental cleanliness by cleaning your teeth after each supper as well as flossing also.
Hair as well as sweat tests may also be called for as part of a drug screening procedure. Blood screening can also be required for Adderall medication examination. Just how is Adderall discovered? In many medicine testing treatments, an individual undertaking Adderall medication test will certainly be requested pee example. Based on your pee evaluation, the existence of Adderall can still be found after four days or a week of consumption, regardless it is a solitary dose or numerous usage of this medicine. The variety required for it to verify the presence of amphetamine is a test result of 500 ng/ml in the person's system. How is Adderall abuse discovered on blood? If you wish to examine whether an individual is abusing Adderall or otherwise, blood screening is executed as well as should a minimum of give a blood test outcome of above 0.2 mg/L to confirm a situation of Adderall abuse. Can visibility of Adderall affect your medication test? Does Adderall appear on medicine examination is amongst the concerns of people who are under this medication. Yes, without a doubt in can appear on your drug test, however do not fret. All you have to do is bring your prescription bottle and a letter from your medical professional if you are actually suggested with this medicine. Your physician's info have to exist, so that if the laboratory clinic where you had your Adderall drug test wishes to make inquiries regarding the legitimacy of your prescription, they could easily call your physician. Having traces of amphetamine in your system doesn't imply incompetency to a task you are applying if you are legitimately enabled to take Adderall. You simply need to reveal evidence of authenticity of your physician's prescription as well as have larger chances of obtaining hired.
It's one for the most common reasons that eyelashes drop completely out. You may not notice it since it feels so all-natural, particularly when you made it occur as a child. If males and females to ensure that your eyelashes expand, don't rub your adoring. The less you touch your eyelashes, desire they'll increase. When it comes to drawing your eye location is constantly to examine the subject's eyes, the very first point. Have a look at at the details of the eyes, much longer eyelashes the application as well as discover the specific feeling of individual to catch it within your illustration canine pen. This mascara has sticks on they can be kept. One side has the lash primer that's white together with the opposite has the mascara. Entailed with water resistant and smudge evidence yet not every customers, including me, were pleased with its outcomes. The standards of my eyelashes stayed white and also this looked actually funny. One on the eye services that a great deal of individuals state jobs well is the LiLash Cleansed eyelash activator. Although the item has been tested by medical professionals, however has some side possessions. Keep reading to extra details.
0 notes