#Dr. Deepika Doshi
Explore tagged Tumblr posts
Text
What are the common symptoms in pregnancy?

Headache,
Feeling Feverish,
Backache,
Leg cramps,
Pelvic pain,
Tiredness,
Fatigue,
Feeling exhausted
Dr. Deepika Doshi competent in handling normal delivery as well as cesarean section, practicing at Dhanvantari Hospital the best Maternity Hospital in Borivali.
0 notes
Text
Who is the Best Doctor for Irregular Periods in Mumbai?
If you are searching for the best doctor for irregular periods in Mumbai, look no further than Dr. Deepika Doshi. Renowned for her expertise and compassionate approach, Dr. Deepika Doshi specializes in diagnosing and treating irregular menstrual cycles with precision. Whether you're dealing with PCOS, hormonal imbalances, or stress-related issues, her patient-centric care ensures you receive a tailored treatment plan.
Located conveniently in Mumbai, Dr. Deepika Doshi's clinic is easily accessible by local trains from both the Central and Western lines. Out-of-town patients also have straightforward travel options to reach her clinic, making her a top choice for comprehensive gynecological care.
What Causes Irregular Periods and Why Should You Consult Dr. Deepika Doshi?
Hormonal imbalances and lifestyle factors are common triggers of irregular periods.
Ignoring irregular periods can lead to complications such as infertility or chronic conditions.
Dr. Deepika Doshi brings years of experience and a proven track record of success in addressing these issues. Her personalized treatment approach combines advanced diagnostics and compassionate care to help you regain balance in your menstrual cycle.
How Can You Reach Dr. Deepika Doshi Using Local Trains?
From the Central Line:
Board a train heading to Dadar Station.
Switch to the Western Line and alight at Vile Parle or Andheri, as both are convenient stops.
The clinic is a short auto ride or walk from the station.
From the Western Line:
Get off at Vile Parle or Andheri station, the closest stops to the clinic.
From there, follow the easy directions provided in the Google Maps link here.
What If You’re Traveling from Out of Town for Treatment?
By Air: Mumbai’s Chhatrapati Shivaji Maharaj International Airport is just 20-30 minutes away from the clinic.
By Train: Arrive at Mumbai Central or Bandra Terminus and take a taxi or local train to Vile Parle/Andheri.
By Road: Mumbai is well-connected via highways, and several intercity bus services can bring you close to the clinic’s location.
Dr. Deepika Doshi ensures a seamless experience for out-of-town patients, offering support for scheduling and consultation planning.
Why Choose Dr. Deepika Doshi as the Best Doctor for Irregular Periods in Mumbai?
Expertise in treating PCOS, endometriosis, and other menstrual disorders.
Proven success rates with minimally invasive treatments.
Comprehensive care tailored to individual patient needs.
Can Lifestyle Changes Help with Irregular Periods?
Yes! Regular exercise, a healthy diet, and stress management can improve your menstrual health.
However, consulting Dr. Deepika Doshi ensures you address the root cause of your irregular periods.
For the best doctor for irregular periods in Mumbai, trust Dr. Deepika Doshi to provide top-tier medical care. Whether you’re a local or traveling from out of town, her expertise and patient-first approach will guide you toward better health and well-being.
0 notes
Text
What is the time limit for having an abortion? Dr Deepika Doshi | Abortion Doctor in Borivali

An abortion may only be carried out up to the 24th week of the pregnancy. If you are less than 17 days overdue, the mandatory five-day wait time does not apply.
To know more, Consult Dr. Deepika Doshi, Abortion Doctor in Borivali at Dhanvantari Hospital, Abortion Clinic in Borivali - Call 9324263464
#abortion#abortion doctor#abortion doctor in borivali#abortion clinic#abortion clinic in borivali#pregnant#pregnancy#women#borivali
4 notes
·
View notes
Photo
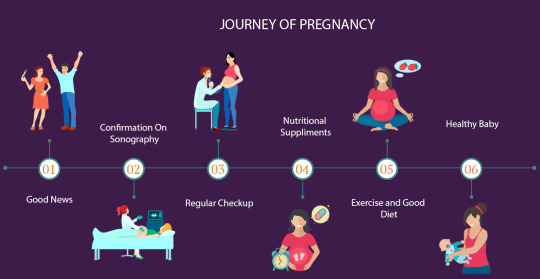
The Journey Of Pregnancy
Consultant with:
Dr. Deepika Doshi or Dr. Bhavesh Doshi
2 notes
·
View notes
Text
Padma Awards 2016
Ms. Deepika Kumari Sports-Archery Shri Sushil Doshi Sports-commentary Shri Mahesh Sharma Trade & Industry Shri Saurabh Srivastava Trade & Industry Sh Dilip Sanghvi Trade & Industry Dr. Keki Hormusji Gharda Trade & Industry Late Shri Prakash Chand Surana (Posthumous) Art-Classical Music Late Shri Saeed Jaffrey (NRI/PIO/Posthumous) Art-Cinema Shri Michael Postel (Foreigner) Art-Archaeology Shri…
View On WordPress
0 notes
Text
Are there non-surgical treatment options for uterine fibroids, and how effective are they?
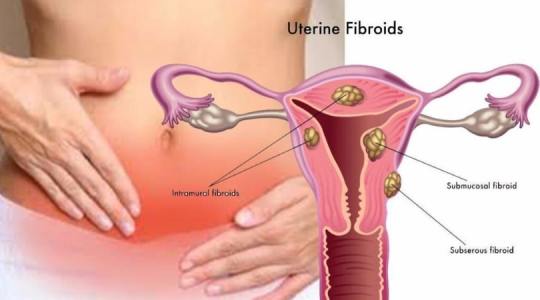
Yes, there are non-surgical treatment options for uterine fibroids, and their effectiveness can vary based on factors such as the size and location of the fibroids, as well as individual patient characteristics. Some common non-surgical treatment options include:
1- Uterine Artery Embolization (UAE):
How it Works: In UAE, the blood supply to the fibroids is blocked, leading to their shrinkage.
Effectiveness: UAE is effective in reducing symptoms such as heavy menstrual bleeding and pelvic pain. It is considered a less invasive alternative to surgery.
2- Hormone Therapy:
How it Works: Hormonal medications, such as birth control pills, may help regulate menstrual bleeding and alleviate symptoms associated with fibroids.
Effectiveness: Hormone therapy can be effective in managing symptoms, but it does not eliminate the fibroids. Its impact varies among individuals.
3- Gonadotropin-Releasing Hormone (GnRH) Agonists:
How it Works: GnRH agonists induce a temporary state of menopause, causing fibroids to shrink.
Effectiveness: While effective in reducing fibroid size and symptoms, the benefits are temporary, and long-term use is limited due to potential side effects.
4- Selective Estrogen Receptor Modulators (SERMs)
How it Works: SERMs, such as tamoxifen, may be used to modulate estrogen activity and manage fibroid-related symptoms.
Effectiveness: SERMs can be effective in certain cases, but their use is often determined based on the specific characteristics of the fibroids and the patient.
5- Non-Invasive Focused Ultrasound (MRgFUS):
How it Works: MRgFUS uses focused ultrasound waves to heat and destroy fibroid tissue without incisions.
Effectiveness: This approach is less invasive and has shown effectiveness in reducing symptoms, but its availability may be limited, and not all fibroids may be suitable for this treatment.
6- Lifestyle and Dietary Modifications:
How it Works: A healthy lifestyle, including regular exercise and a balanced diet, may help manage symptoms and promote overall well-being.
Effectiveness: While lifestyle changes alone may not eliminate fibroids, they can contribute to improved health and symptom management.
It's essential for women with uterine fibroids to consult with their gynecologist to determine the most appropriate treatment plan based on their individual circumstances. The choice of non-surgical options depends on factors such as the severity of symptoms, reproductive goals, and the specific characteristics of the fibroids.
Experience personalized care with Dr. Deepika Doshi, your trusted Gynecologist in Mira Road. Prioritize your reproductive health. Book your consultation today for expert gynecological care.
#dhanvantari hospital#gynecologist in borivali#maternity hospital in borivali#gynecologist in mira road#gynecologist in mumbai#abortion clinic in mumbai#best gynecologist in borivali#Dr. Deepika Doshi#Gynecologist in Mira Road#uterine fibroids#uterine fibroids treatment#gynecological care
0 notes
Text
What facilities should a good delivery hospital have?

A good delivery hospital should have a range of facilities to ensure the safety and well-being of both the mother and the newborn. Here are key facilities that a reputable delivery hospital should provide:
1- Labor and Delivery Suites:
Spacious, well-equipped rooms where the mother can labor and deliver comfortably.
2- Operating Theaters:
Equipped with the necessary medical tools and technology for Cesarean sections or other surgical interventions if needed.
3- Neonatal Care Unit (NICU):
A specialized unit equipped to provide care for premature or ill newborns, staffed with experienced neonatal healthcare professionals.
4- Prenatal and Postpartum Care Facilities:
Dedicated areas for prenatal and postpartum care, including examination rooms and facilities for routine check-ups.
5- Emergency Services:
24/7 emergency services to handle any unexpected complications during labor and delivery.
6- Diagnostic Services:
Facilities for on-site diagnostics, including ultrasound, fetal monitoring, and laboratory services.
7- Anesthesia Services:
Access to anesthesia services for pain management options during labor, such as epidurals or other medications.
8- Lactation Support:
Services and support for breastfeeding, including lactation consultants and educational resources.
9- Comfortable Accommodations:
Comfortable and clean rooms for both the mother and the newborn during their stay.
10- Security Measures:
Strict security measures to ensure the safety of mothers, newborns, and hospital staff.
These facilities collectively contribute to creating a supportive and positive environment for expectant parents during the childbirth journey. Prospective parents are encouraged to tour the hospital, ask questions, and discuss their preferences with healthcare providers to ensure a personalized and comfortable birthing experience.
Choose excellence in maternity care! Dhanvantari Hospital, your trusted Delivery Hospital in Borivali, offers state-of-the-art facilities and expert Gynaecologist Dr. Deepika Doshi for Delivery healthcare. Schedule your consultation for a nurturing and safe birthing experience today.
#dhanvantari hospital#gynecologist in borivali#maternity hospital in borivali#gynecologist in mumbai#abortion clinic in mumbai#best gynecologist in borivali#Delivery Hospital in Borivali#maternity care#healthcare#Dr. Deepika Doshi
0 notes
Text
What are the advantages of laparoscopic hysterectomy?

Laparoscopic hysterectomy offers several advantages compared to traditional open abdominal hysterectomy. Some of the key benefits include:
Minimally Invasive Approach: Laparoscopic hysterectomy is a minimally invasive surgical technique, requiring only small incisions in the abdomen. This leads to reduced trauma to the surrounding tissues compared to open surgery.
Smaller Incisions and Less Scarring: The incisions made during laparoscopic hysterectomy are much smaller than the larger abdominal incision required for traditional hysterectomy. As a result, patients typically experience smaller scars, which are often less noticeable and may fade over time.
Reduced Blood Loss: The precise nature of laparoscopic surgery allows for better visualization and control of blood vessels, contributing to reduced blood loss during the procedure.
Quicker Recovery Time: Patients undergoing laparoscopic hysterectomy often experience a faster recovery compared to those undergoing traditional open surgery. Smaller incisions lead to less postoperative pain, shorter hospital stays, and an earlier return to normal activities.
Lower Risk of Infection: Because laparoscopic hysterectomy involves smaller incisions, there is a lower risk of infection compared to open surgery. Smaller wounds are generally associated with faster healing and reduced susceptibility to infections.
Decreased Pain and Discomfort: Patients undergoing laparoscopic hysterectomy may experience less postoperative pain and discomfort compared to those undergoing traditional open surgery. This can contribute to an overall more comfortable recovery.
Improved Cosmesis: The smaller incisions and reduced scarring associated with laparoscopic hysterectomy contribute to improved cosmesis, allowing patients to feel more satisfied with the aesthetic outcome of the surgery.
Shorter Hospital Stay: Laparoscopic hysterectomy often allows for a shorter hospital stay compared to open surgery. Many patients can go home within 24 to 48 hours after the procedure.
Quicker Return to Normal Activities: Patients undergoing laparoscopic hysterectomy typically experience a faster return to normal activities and daily routines compared to those undergoing open surgery, contributing to an improved quality of life during the recovery period.
Preservation of Ovaries in Some Cases: In certain cases, laparoscopic hysterectomy allows for the preservation of the ovaries, maintaining hormonal function and delaying the onset of menopause.
It's important to note that the appropriateness of laparoscopic hysterectomy depends on various factors, including the patient's medical history, the nature of the underlying condition, and the surgeon's expertise. Patients should discuss their specific case with their healthcare provider to determine the most suitable surgical approach.
Are you seeking compassionate and specialized care on your path to motherhood? Look no further! Dr. Deepika Doshi is your dedicated partner, specializing in comprehensive pregnancy care with a woman-centric approach. As a renowned lady doctor for pregnancy.
#dhanvantari hospital#gynecologist in borivali#best gynecologist in borivali#lady doctor for pregnancy#Dr. Deepika Doshi
0 notes
Text
How can I manage morning sickness during pregnancy?

Managing morning sickness during pregnancy can be challenging, but there are several strategies that may help alleviate symptoms. It's important to note that what works for one person may not work for another, so it may take some trial and error to find what works best for you. Here are some general tips:
1. Eat Small, Frequent Meals:
Strategy: Instead of three large meals, opt for smaller, more frequent meals throughout the day.
Reason: Keeping your stomach from being empty may help prevent nausea.
2. Stay Hydrated:
Strategy: Sip fluids throughout the day, particularly between meals.
Reason: Dehydration can worsen nausea, so it's essential to stay hydrated.
3. Choose Bland, Easy-to-Digest Foods:
Strategy: Opt for plain crackers, dry toast, or simple carbohydrates.
Reason: These foods are generally easier on the stomach and may help alleviate nausea.
4. Ginger:
Strategy: Try ginger in various forms—ginger tea, ginger ale, or ginger candies.
Reason: Ginger has natural anti-nausea properties and may provide relief.
5. Avoid Strong Odors:
Strategy: Steer clear of strong-smelling foods and cooking odors.
Reason: Strong smells can trigger nausea in some pregnant women.
6. Take Prenatal Vitamins with Food:
Strategy: Take prenatal vitamins with a meal or before bed.
Reason: Taking vitamins on an empty stomach can contribute to nausea.
7. Get Plenty of Rest:
Strategy: Ensure you're getting enough sleep and rest during the day.
Reason: Fatigue can exacerbate feelings of nausea.
8. Acupressure Bands:
Strategy: Try acupressure bands, which are worn on the wrists.
Reason: Some women find relief from nausea through acupressure.
9. Stay Cool and Well-Ventilated:
Strategy: Keep your environment cool and well-ventilated.
Reason: Warm or stuffy environments can trigger or worsen nausea.
10. Consult Your Healthcare Provider:
Strategy: If symptoms are severe or persistent, consult your healthcare provider.
Reason: They can provide guidance and may suggest medications if necessary.
11. Experiment with Aromatherapy:
Strategy: Some women find relief from certain scents, like citrus or peppermint.
Reason: Pleasant smells can sometimes help alleviate nausea.
12. Consider Professional Guidance:
Strategy: If morning sickness is severe, consider seeking guidance from a dietitian or healthcare professional.
Reason: They can provide personalized advice and support.
13. Prescribed Medications:
Strategy: In severe cases, your healthcare provider may prescribe medications.
Reason: Some medications are considered safe during pregnancy and can help manage nausea.
It's crucial to communicate with your healthcare provider about your symptoms and any remedies you're considering. If morning sickness is severe, persistent, or affecting your ability to eat and drink, seeking professional advice is important to ensure the health and well-being of both you and your baby.
Begin your path to optimal women's health alongside Dr. Deepika Doshi an experienced and trusted gynecologist in Dahisar With expertise in comprehensive gynecological care, Dr. Arohi offers individualized solutions tailored to meet the distinct needs of each patient, ensuring a journey towards optimal well-being.
0 notes
Text
Can I have a vaginal birth after a caesarean section (VBAC)?

Yes, it is possible to have a vaginal birth after a caesarean section (VBAC), but it depends on various factors. Here are key considerations:
1- Type of Previous Incision: The type of incision made during the previous caesarean section plays a crucial role. A low transverse incision (horizontal) is generally associated with a higher likelihood of success for VBAC compared to a vertical incision.
2- Reason for Previous C-Section: The reason for the previous caesarean section is important. If the c-section was due to a non-recurring issue, such as breech presentation, there might be a greater chance for VBAC.
3- Number of Previous C-Sections: VBAC success rates tend to be higher for women with one previous c-section compared to those with multiple c-sections.
4- Uterine Rupture Risk: VBAC is associated with a small risk of uterine rupture, where the scar from the previous c-section tears. This risk is typically low but is an important consideration.
5- Medical Monitoring: During a VBAC, continuous monitoring of the mother and baby is often required to detect any signs of complications promptly.
6- Availability of Emergency Services: Given the slight risk of complications, it's important that the hospital has the capability to provide emergency services, including an immediate c-section if needed.
7- Patient's Preferences and Comfort Level: Some women may prefer attempting VBAC for various reasons, while others may choose a repeat c-section. Personal preferences and comfort level play a significant role in the decision-making process.
It's crucial for women considering VBAC to have open and thorough discussions with their healthcare provider. The decision should be based on an individualized assessment of the woman's medical history, the specific circumstances of the previous c-section, and her preferences. Healthcare providers carefully weigh the potential benefits of VBAC against the associated risks to make informed decisions that prioritize the safety of both the mother and the baby.
For more information, consult Dr. Deepika Doshi one of the renowned Gynecologist in Dahisar practicing in Dhanvantari Hospital or you Can contact us on 9324263464.
#dhanvantari hospital#maternity hospital in Dahisar#gynecologist in mumbai#gynecologist in Dahisar#best gynecologist in Dahisar#abortion clinic in mumbai#Dr. Deepika Doshi#Dhanvantari Hospital#caesarean section#c section#VBAC
0 notes
Text
What are the diagnostic methods of fibroids?
The diagnostic methods for fibroids, also known as uterine fibroids or leiomyomas, include:
1- Pelvic Exam:
A pelvic examination allows a healthcare provider to feel for any abnormalities in the uterus, including the presence of fibroids.
2- Imaging Tests:
Ultrasound: Trans vaginal or abdominal ultrasound provides detailed images of the uterus, helping identify the size, number, and location of fibroids.
MRI (Magnetic Resonance Imaging): MRI can offer more detailed images of the uterus and fibroids, assisting in treatment planning.
3- Hysteroscopy:
A hysteroscopy involves the insertion of a thin, lighted tube (hysteroscope) through the cervix to examine the inside of the uterus, allowing direct visualization of fibroids within the uterine cavity.
4- Sonohysterography:
This procedure involves the injection of sterile saline into the uterus before a trans vaginal ultrasound, enhancing the imaging of the uterine cavity and fibroids.
5- Blood Tests:
Blood tests may be conducted to assess the levels of certain hormones, such as estrogen and progesterone, which can be associated with fibroid growth.
6- Biopsy:
In rare cases, a biopsy may be performed to rule out other conditions that can cause similar symptoms. However, fibroids are typically diagnosed based on imaging and clinical evaluation rather than biopsy.
These diagnostic methods help healthcare providers determine the presence, size, and location of fibroids, guiding appropriate treatment options based on the individual's symptoms and reproductive goals.
For expert gynecological care, consult Dr. Deepika Doshi, your trusted Gynecologist in Dahisar. Schedule your appointment for personalized women's health solutions.
#dhanvantari hospital#maternity hospital in Dahisar#gynecologist in mira road#gynecologist in mumbai#abortion clinic in mumbai#best gynecologist in Dahisar#pediatric surgeon in mumbai.#gynecologist in Dahisar#Dr. Deepika Doshi#gynecological care#uterine fibroids
0 notes
Text
When should I start antenatal care?

It's generally recommended that you start antenatal care as soon as you know you're pregnant. Early prenatal care is important for monitoring and promoting the health of both you and your baby throughout the pregnancy. Ideally, you should schedule your first prenatal appointment during the first trimester, or within the first 8 to 10 weeks of pregnancy.
Early antenatal care allows healthcare providers to:
Confirm your pregnancy.
Estimate your due date.
Assess your overall health and identify any pre-existing conditions.
Identify and address any potential risks or complications early on.
Provide information on a healthy lifestyle during pregnancy, including nutrition, exercise, and prenatal vitamins.
Discuss genetic testing options if desired.
Establish a relationship with your healthcare provider for ongoing support and monitoring.
If you suspect you are pregnant or have confirmed your pregnancy through a home pregnancy test, it's a good idea to contact your healthcare provider promptly to schedule your first prenatal appointment.
For more information, consult Dr. Deepika Doshi one of the top notch Gynecologist in Mira Road or you can contact us on 9324263464.
#dhanvantari hospital#gynecologist in mumbai#gynecologist in mira road#PrenatalCare#MaternalHealth#PregnancyHealth#AntenatalCheckup#Dr. Deepika Doshi#Gynecologist#Best Gynecologist
0 notes
Text
What are common causes of heavy menstrual bleeding?
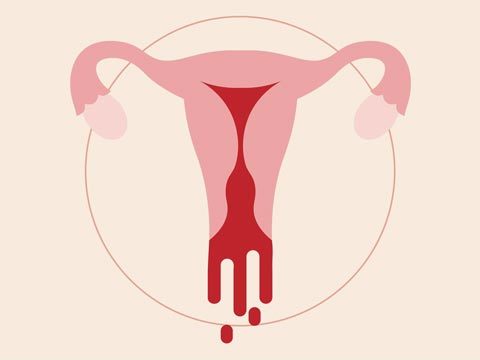
Heavy menstrual bleeding, medically known as menorrhagia, can be caused by various factors. Some common causes include:
Hormonal Imbalance: Hormonal fluctuations, particularly imbalances in estrogen and progesterone levels, can disrupt the normal menstrual cycle and lead to heavy bleeding.
Uterine Fibroids: Fibroids are noncancerous growths in the uterus that can cause heavy or prolonged periods.
Adenomyosis: Adenomyosis occurs when the tissue lining the uterus (endometrium) grows into the muscular wall of the uterus, leading to heavy menstrual bleeding and pelvic pain.
Polyps: Uterine polyps are small growths on the inner lining of the uterus that can cause heavy or irregular bleeding.
Endometrial Hyperplasia: An overgrowth of the uterine lining (endometrium) can lead to heavy menstrual bleeding.
Pelvic Inflammatory Disease (PID): Infections in the reproductive organs, such as PID, can cause inflammation and contribute to heavy bleeding.
Coagulation Disorders: Conditions that affect blood clotting, such as von Willebrand disease or other bleeding disorders, can lead to heavy menstrual bleeding.
IUD (Intrauterine Device): While hormonal IUDs are sometimes prescribed to reduce menstrual bleeding, copper IUDs may lead to heavier periods in some individuals.
Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder that can cause irregular periods, and in some cases, heavy menstrual bleeding.
Certain Medications: Some medications, such as anticoagulants or anti-inflammatory drugs, may contribute to heavy bleeding.
Ectopic Pregnancy: Though rare, an ectopic pregnancy (a pregnancy outside the uterus) can cause heavy bleeding and requires immediate medical attention.
Thyroid Disorders: Thyroid dysfunction, particularly an underactive thyroid (hypothyroidism), can disrupt the menstrual cycle and lead to heavy bleeding.
Cancer: In rare cases, uterine or cervical cancer may cause heavy menstrual bleeding. It's important to rule out malignancies, especially in postmenopausal women.
Intrauterine Synechiae (Asherman's Syndrome): Scar tissue inside the uterus, often caused by surgery or infection, can lead to adhesions and heavy menstrual bleeding.
If someone is experiencing heavy menstrual bleeding, it is advisable to consult with a healthcare professional for a thorough evaluation and proper diagnosis. Treatment options will depend on the underlying cause and may include medications, hormonal therapies, minimally invasive procedures, or surgery, depending on the severity and specific condition.
Take the first step towards reproductive health and well-being with Dr. Deepika Doshi, your trusted Gynecologist in Mira Road.
#dhanvantari hospital#maternity hospital in borivali#gynecologist in mumbai#best gynecologist in borivali#Dr. Deepika Doshi#Gynecologist in Mira Road
0 notes
Text
How is Uterine Prolapse Diagnosed?
Uterine prolapse is diagnosed through a medical history review, pelvic examination, and sometimes imaging studies. Here's an overview:
1-Medical History:
The healthcare provider inquires about symptoms, pelvic organ prolapse, pregnancies, and childbirth experiences.
2-Pelvic Examination:
A crucial part of diagnosis, it involves visually inspecting external genitalia and performing an internal examination to assess uterus position and pelvic floor muscle strength.
3-Assessment of Prolapse Severity:
The provider uses a grading system (mild to severe) based on the extent of uterine descent into the vaginal canal.
4-Imaging Studies:
In some cases, imaging studies may be recommended:
Ultrasound: Non-invasive imaging for visualizing pelvic organs.
MRI: Provides detailed pelvic region images in complex cases.
5-Urodynamic Testing:
If urinary symptoms are present, testing assesses bladder function and rules out conditions like urinary incontinence.
The combination of these methods guides the healthcare provider in determining the appropriate treatment for uterine prolapse. Diagnosis is individualized based on symptoms, medical history, and findings from examinations and studies. Early intervention can manage symptoms and prevent complications. Always consult with a healthcare professional for personalized advice based on your specific health condition.
Looking for expert gynecological care in Mira Road? Schedule a consultation with Dr. Deepika Doshi for compassionate and personalized women's health services. Your well-being is our priority
#dhanvantari hospital#gynecologist in mira road#gynecologist in mumbai#Dr. Deepika Doshi#Uterine prolapse#Gynecologist#women's health#HealthCare
0 notes
Text
What are the common signs and symptoms of breast cancer that women should be aware of?
Common signs and symptoms of breast cancer that women should be aware of include:
1-Lump or Thickening: The most common sign is a new lump or thickening in the breast or underarm area.
2-Change in Breast Size or Shape: Any noticeable change in the size, shape, or appearance of the breast.
3-Nipple Changes: Look for nipple discharge, inversion, pain, or scaling of the skin around the nipple.
4-Breast Skin Changes: Unexplained redness, dimpling, or puckering of the breast skin.
5-Breast Pain: While breast pain is more commonly associated with benign conditions, it can sometimes be a sign of breast cancer.
6-Swelling or Irritation: Swelling, irritation, or redness in the breast that does not go away.
It's important to note that these symptoms can also be caused by non-cancerous conditions. However, if you notice any of these changes or experience persistent symptoms, it's essential to consult a healthcare provider for a clinical evaluation. Regular breast self-exams and routine breast cancer screening can aid in the early detection of breast cancer, improving the chances of successful treatment.
Ready to prioritize your breast health and well-being? Schedule a consultation with Dr. Deepika Doshi, your trusted Gynecologist in Mira Road. Contact us on 9324263464 .
#dhanvantari hospital#maternity hospital in borivali#gynecologist in mira road#gynecologist in mumbai#Dr. Deepika Doshi#BreastCancerAwareness#CancerSigns#WomenHealth#Gynecologist
0 notes
Text
Is there a link between heavy menstrual bleeding and fertility issues?
Yes, there can be a link between heavy menstrual bleeding (menorrhagia) and fertility issues, although it's important to note that not all cases of heavy menstrual bleeding are necessarily linked to fertility problems. The relationship between heavy periods and fertility can vary depending on the underlying causes of the menorrhagia. Here are some ways in which heavy menstrual bleeding can be related to fertility issues:
Polycystic Ovary Syndrome (PCOS): Women with PCOS may experience irregular and heavy menstrual bleeding. PCOS is a common cause of infertility due to irregular ovulation or anovulation (lack of ovulation).
Uterine Fibroids: Uterine fibroids are noncancerous growths in the uterus that can lead to heavy menstrual bleeding. Large fibroids or those that affect the uterine cavity can interfere with implantation or block the fallopian tubes, which can affect fertility.
Endometriosis: Heavy menstrual bleeding can be a symptom of endometriosis. Endometriosis is a condition in which tissue similar to the uterine lining grows outside the uterus. It can cause inflammation and scarring that may obstruct the fallopian tubes, making it harder for the egg to meet the sperm.
Adenomyosis: Adenomyosis is a condition in which the tissue that lines the uterus grows into the muscular walls of the uterus. It can cause heavy menstrual bleeding and may also be associated with fertility issues.
Hormonal Imbalances: Certain hormonal imbalances, such as thyroid disorders or problems with the hypothalamus or pituitary gland, can lead to both heavy periods and fertility problems. Hormones play a crucial role in regulating the menstrual cycle and fertility.
Anovulation: In some cases, heavy menstrual bleeding may be associated with anovulation (lack of ovulation). If you're not ovulating, you cannot conceive, which is a fertility issue.
Consult a healthcare provider for heavy menstrual bleeding and fertility concerns. They can diagnose the issue, recommend treatments to improve your chances of conceiving, and enhance your quality of life.
Connect with Dr. Deepika Doshi, your Gynecologist in Mira Road , for expert women's health care or you can Contact us on 9324263464.
#HeavyPeriods#dhanvantari hospital#gynecologist in mira road#Dr. Deepika Doshi#FertilityAwareness#Gynecology#WomensHealth#HeavyBleeding
0 notes