#Credentialing
Explore tagged Tumblr posts
Text

cspmsolutions for medical billing, accounting, Digital marketing
2 notes
·
View notes
Text
HSPD-12: Government Badging & Credentialing Specialist (San Diego - REF1827L)
Job title: HSPD-12: Government Badging & Credentialing Specialist (San Diego – REF1827L) Company: Citizant Job description: Company Description Citizant is a leading provider of professional IT services to the U.S. government. We seek… Expected salary: $44000 – 52300 per year Location: San Diego, CA Job date: Sun, 29 Jun 2025 05:05:48 GMT Apply for the job now!
0 notes
Text
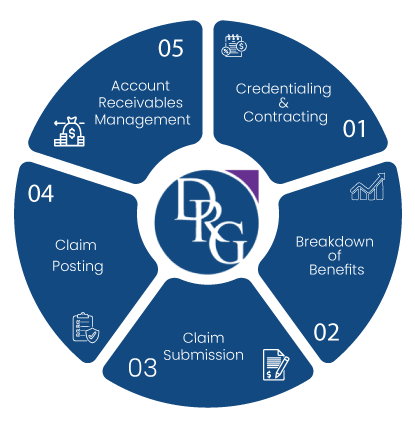
What’s your billing bottleneck?
Claim denials, credentialing, or AR? #BillingStress #PollTime #HealthcareRevenue #KnowYourPain #RevenueCycle #BillingBottlenecks #MedicalBillingPoll #MedCurers
#medcurers#medicalbilling#What's your billing bottleneck?#Claim denials#credentialing#or AR?#BillingStress#PollTime#HealthcareRevenue#KnowYourPain#RevenueCycle#BillingBottlenecks#MedicalBillingPoll#MedCurers
0 notes
Text


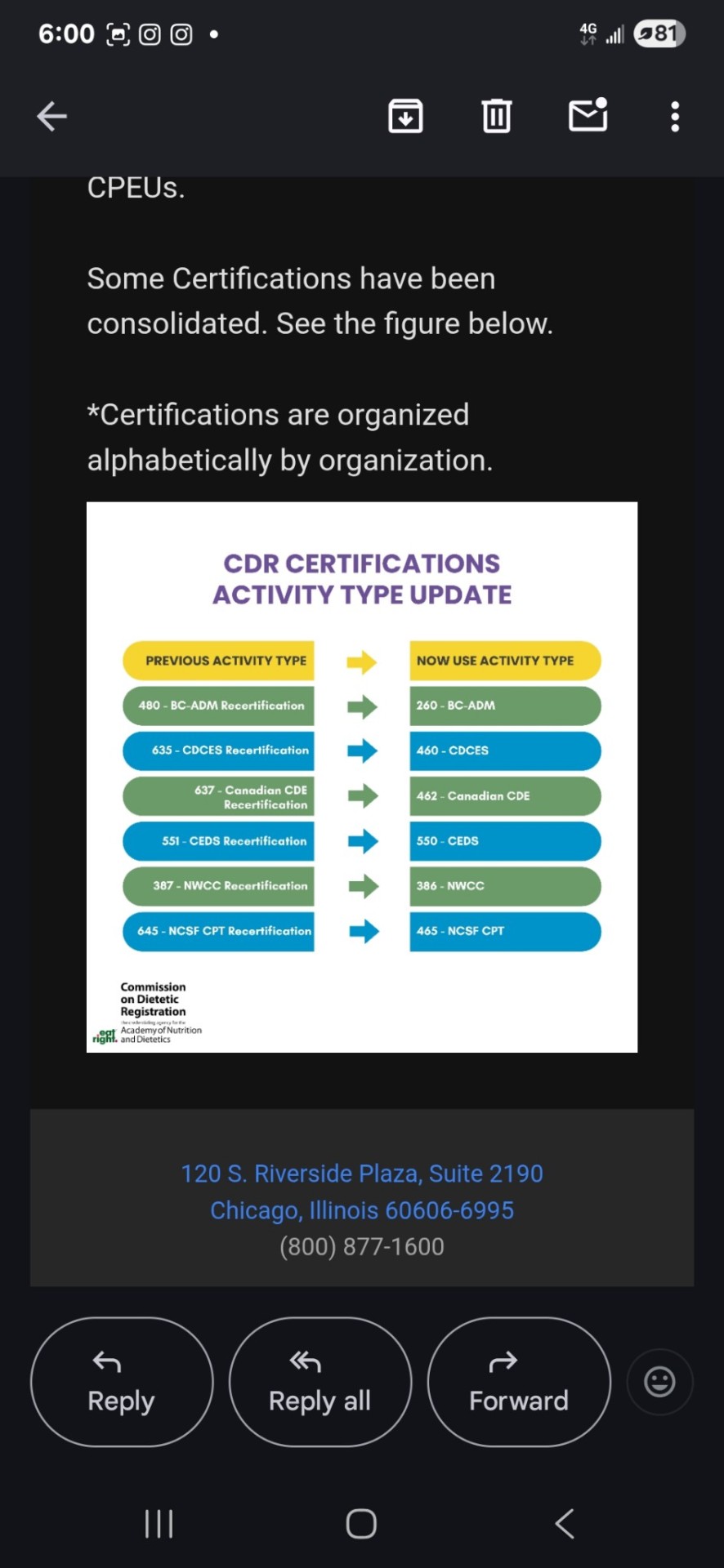
https://www.cdrnet.org/competencies
https://www.cdrnet.org/cdr-cpe-activity-type-definitions
0 notes
Text
Mastering Credentialing for Group Practices

Credentialing doesn’t have to be complex. This guide breaks down how group practices can streamline the process, stay compliant, and reduce delays in insurance approval and billing cycles.
0 notes
Text
Credentialing: The Most Underrated Backbone of Healthcare Revenue
Credentialing isn’t just a regulatory formality—it’s the foundation of every healthcare provider’s ability to deliver services, get reimbursed, and stay in network. Yet, too many practices continue to underestimate its significance until denials start piling up or payment delays threaten operations.
At its core, credentialing is the process of verifying a provider’s qualifications, licenses, board certifications, and practice history. Insurance companies require this verification to grant network access and allow providers to bill for their services. Without this, even the most skilled physician cannot get paid.
The consequences of poor credentialing are felt industry-wide. According to the Medical Group Management Association, 1 in every 4 denied claims is directly tied to credentialing or enrollment issues. Moreover, CAQH reports show that delays in initial credentialing cost practices an average of $9,000 per month in missed reimbursements.
Practices often run into issues like outdated CAQH profiles, missing documents, or late renewals—all of which cause bottlenecks. These errors multiply in multi-specialty or multi-provider settings, where each physician must be individually credentialed with each insurance payer.
While many smaller clinics try to manage this manually, it often results in more back-and-forth with insurance carriers, extended wait times for payer enrollment, and denied claims. This is why a growing number of practices are turning to managed solutions for credentialing. Teams like Medical Billing Wholesalers specialize in payer enrollment, document management, and deadline tracking, offering full transparency while reducing credentialing turnaround time.
As healthcare evolves and provider mobility increases, credentialing is no longer a one-time task—it’s an ongoing requirement. With recredentialing timelines, audits, and stricter payer policies, staying compliant means staying ahead. If your revenue cycle is showing signs of strain, credentialing may be the first place to look.
For Provider Credentialing Service - https://www.medicalbillingwholesalers.com/revenue-cycle-services/provider-credentialing/
1 note
·
View note
Text
Overcoming Medical Credentialing Challenges

Credentialing is that vital aspect of provider enrolment, compliance, and further by way of its long verification processes; difference between payers; a venue of administrative delays. Automated credentialing tool applications, meticulous record keeping, and constant regulatory know-how for healthcare organizations speed up the credentialing process and ensure that reimbursement comes in timely.
0 notes
Text

Ensure seamless provider enrollment and credentialing with our expert services. We handle paperwork, verifications and compliance, streamlining the process for faster approvals. Trust us for hassle-free #credentialing and network enrollments.
.
.
.
#PhysicianCredentialing#providercredentialing#InsuranceCredentialing#MedicalCredentialing#medicalbillingcompany
#medical credentialing services#physician credentialing services#physician credentialing#credentialing#Insurance Credentialing
1 note
·
View note
Text

From well-visits to complex cases, pediatricians manage it all—but growing a practice and staying compliant shouldn’t add to the workload. SMCG’s pediatric consultants help with expansion strategy, credentialing, and regulatory compliance, so your practice runs smoothly at every stage of growth.
Thinking about adding locations, streamlining payer enrollments, or strengthening financial sustainability? We handle the business side so you can focus on patient care.
Learn more and request a free consultation with our one of our experts: https://sullivanmcg.com/industry/beyond-medicine-cultivating-excellence-in-pediatric-practice-management-consulting/
0 notes
Text
Navigating Credentialing in Medical Billing the Essential Guide

In the tricky worldwide of healthcare, credentialing plays a pivotal characteristic that frequently is going ignored. For medical billers, healthcare agencies, and billing experts, knowledge this vital method isn't always actually beneficial—it’s critical. Credentialing guarantees that healthcare carriers are well vetted, certified, and authorized to serve patients and acquire reimbursement from insurance companies. This comprehensive guide will solve the complexities of credentialing in medical billing, provide an explanation for why it's far critical in your exercise, and provide actionable insights to streamline the technique.
Understanding Credentialing a Fundamental Overview
Credentialing is the system with the resource of which healthcare carriers are evaluated and authorized to offer medical services. This includes verifying a provider's qualifications, inclusive of their education, schooling, licensure, and work history. Credentialing is important to make certain that vendors meet organization necessities and might deliver steady, effective care to sufferers.
The technique of credentialing is greater than best a formality; it’s a meticulous exam of a provider’s heritage that consists of peer references, malpractice records, and any disciplinary movements. This complete evaluation permits preserve excessive requirements within the medical network. For clinical billers and billing experts, expertise credentialing is critical because it without delay affects the reimbursement approach and the economic health of a healthcare workout.
In modern-day years, the significance of credentialing has extended extensively. With the rise in healthcare fraud and malpractice instances, coverage agencies and regulatory our bodies have tightened credentialing necessities. This method that staying knowledgeable and adhering to the ones requirements is extra important than ever for healthcare carriers and billers.
Why Credentialing Matters for Healthcare Providers
For healthcare carriers, credentialing is a gateway to taking element in coverage networks. Without proper credentialing, vendors can't invoice coverage businesses or achieve charge for services rendered to insured patients. This makes credentialing a critical step for any healthcare exercise trying to function efficiently and profitably.
Credentialing moreover enhances an employer’s credibility and reputation. Patients are much more likely to agree with providers who are credentialed by way of identified institutions and coverage companies. This trust interprets to extended affected character retention and delight, which can be key drivers of a successful healthcare exercise.
Additionally, credentialing enables mitigate prison dangers. By making sure that everyone business meet stringent qualifications and cling to moral necessities, healthcare companies can lessen the probability of malpractice claims and other jail problems. This protecting measure is beneficial in safeguarding each the company's and the exercise’s pastimes.
The Credentialing Process Step by using the use of Step
The credentialing gadget usually starts off evolved with the submission of an software to a credentialing business enterprise or an insurance company. This application includes precise statistics approximately the company’s training, education, licensure, and professional enjoy. It may additionally require documentation together with diplomas, certificate, and letters of recommendation.
Once the application is submitted, the credentialing commercial enterprise employer conducts an intensive evaluate and verification of the information provided. This includes contacting academic institutions, licensing forums, and former employers to validate the enterprise’s credentials. The company additionally checks for any disciplinary movements or malpractice claims inside the organization’s records.
After the verification technique, the company may be required to participate in an interview or go through extra checks, relying at the company’s guidelines. Once all steps are finished, the credentialing organization makes a selection and affords or denies credentialing popularity. This choice is communicated to the organization and the healthcare workout, finishing the credentialing technique.
Common Challenges in Credentialing and How to Overcome Them
One of the most not unusual worrying situations in credentialing is the lengthy and time-eating method. Gathering and verifying the essential documentation can take several months, delaying a organization’s capability to appearance patients and generate sales. To overcome this, providers must begin the credentialing technique as early as viable and make certain all documentation is entire and correct.
Another mission is preserving song of the various credentialing necessities for one-of-a-kind coverage agencies and businesses. Each entity also can have its very very own set of standards and methods, making it tough to manipulate multiple programs simultaneously. Using credentialing software or operating with a credentialing professional can help streamline this manner and make sure compliance with all requirements.
Finally, keeping credentialing fame requires ongoing strive. Providers need to preserve their credentials up to date and file any modifications of their qualifications or exercise reputation. Regularly reviewing and renewing credentials is important to keep away from lapses that would disrupt billing and repayment processes.
The Role of Credentialing Specialists in Healthcare
Credentialing specialists play a critical position in managing the credentialing procedure for healthcare carriers. These professionals have understanding in navigating the complicated requirements of diverse coverage networks and credentialing corporations. They manage the administrative workload, permitting agencies to awareness on affected character care.
Credentialing professionals are answerable for amassing and filing the important documentation, tracking application statuses, and ensuring compliance with credentialing necessities. They moreover maintain organizations knowledgeable of any updates or adjustments in credentialing requirements, assisting to save you lapses or troubles that could affect billing and repayment.
In addition to their administrative obligations, credentialing experts act as advocates for companies. They communicate with insurance businesses and credentialing organizations on behalf of the organization, addressing any issues or discrepancies that may rise up within the course of the way. This advocacy is critical in expediting credentialing selections and resolving potential problems.
Credentialing and Its Impact on Medical Billing
Credentialing directly impacts medical billing and the financial viability of healthcare practices. Without right credentialing, businesses cannot bill coverage businesses for services rendered, leading to sales loss and monetary instability. Ensuring that all carriers are credentialed is vital for keeping steady cash drift and optimizing the billing way.
Inaccurate or incomplete credentialing facts can bring about declare denials and price delays. Billing specialists must verify that every one company data is current and correctly reflected in billing structures to save you those troubles. Regular audits and updates to credentialing information can assist keep away from disruptions inside the billing method.
Furthermore, credentialing impacts the contracts and repayment prices negotiated with insurance companies. Providers with robust credentials and a high exceptional reputation may also additionally have extra leverage in securing favorable phrases and charges. This underscores the importance of retaining excessive standards and constantly enhancing credentialing profiles.
Credentialing Software Tools Streamlining the Process
In today’s digital age, credentialing software program system have end up valuable in streamlining the credentialing system. These tools automate some of the administrative responsibilities associated with credentialing, which consist of accumulating documentation, tracking software program progress, and sending reminders for renewals.
Credentialing software program gives centralized databases in which providers and practices can save and manipulate all credentialing information. This centralization reduces the threat of mistakes and omissions, ensuring that each one vital documentation is readily to be had and updated. It moreover presents analytics and reporting functions to display credentialing overall performance and identify areas for development.
By leveraging credentialing software, healthcare practices can considerably reduce the time and assets required for credentialing. This lets in providers to attention on handing over extraordinary patient care even as making sure compliance with credentialing requirements.
Credentialing and Compliance Meeting Industry Standards
Compliance with credentialing necessities is not best important for billing and reimbursement however moreover for meeting organization regulations and ethical requirements. Credentialing guarantees that carriers adhere to federal and country legal guidelines, in addition to the recommendations set forth through using professional agencies and accrediting bodies.
Maintaining compliance with credentialing necessities permits guard healthcare practices from crook and monetary risks. Non-compliance can bring about consequences, loss of accreditation, and harm to the practice’s reputation. Regular audits and updates to credentialing facts are important to make sure ongoing compliance and avoid capability issues.
Credentialing moreover allows fine guarantee obligations inside healthcare groups. By verifying company qualifications and monitoring ongoing compliance, credentialing allows keep excessive standards of care and enhances affected man or woman protection and pleasure.
Building a Culture of Credentialing Excellence
Creating a tradition of credentialing excellence inside a healthcare organization calls for collaboration and willpower from all stakeholders. Providers, billing professionals, credentialing specialists, and administrators ought to paintings collectively to prioritize credentialing and ensure its fulfillment.
Educating carriers and body of workers approximately the importance of credentialing and its effect at the exercising is a critical first step. Regular education periods and workshops can help strengthen credentialing quality practices and maintain every body knowledgeable of any adjustments in requirements or suggestions.
Establishing easy protocols and strategies for credentialing is also important. These protocols want to outline the roles and obligations of each crew member, further to the stairs concerned in the credentialing procedure. Regularly reviewing and updating those protocols ensures that the organization remains aligned with organization standards and excellent practices.
Credentialing Trends and Innovations What's Next
The credentialing panorama is continuously evolving, driven with the resource of improvements in era and changes in regulatory necessities. One rising fashion is the increased use of blockchain technology in credentialing. Blockchain offers secure, obvious, and immutable facts, improving the accuracy and reliability of credentialing data.
Another fashion is the aggregate of synthetic intelligence (AI) in credentialing strategies. AI algorithms can automate the verification of credentials, come to be aware about discrepancies, and predict capability problems in advance than they get up. This reduces the govt burden on credentialing specialists and improves the performance and accuracy of the gadget.
Finally, there can be a growing emphasis on enterprise engagement and delight in credentialing. Forward-wondering businesses are exploring approaches to streamline the credentialing technique and enhance the provider revel in. This includes lowering administrative workload, enhancing conversation, and presenting personalized assist at some point of the credentialing lifecycle.
Conclusion Empowering Your Practice with Credentialing
Credentialing is a critical difficulty of medical billing and healthcare operations. It guarantees that carriers are qualified, compliant, and licensed to deliver outstanding care and obtain repayment for their services. By know-how and optimizing the credentialing manner, healthcare carriers, medical billers, and billing professionals can decorate their exercise’s recognition, economic balance, and operational performance.
To correctly navigate the complexities of credentialing, it is important to stay informed of agency traits, leverage era, and foster a tradition of excellence within your company. By doing so, you may empower your practice to thrive in nowadays competitive healthcare landscape and supply great care for your sufferers.
For the ones searching out similarly facts or help, consider exploring extra sources or consulting with credentialing professionals to make sure your practice is located for success.
0 notes
Text
Emma's Journey: Mastering the Credentialing Maze to Begin Her Dream
Dr. Emma had just received the exciting news—she had been offered a position at Western University of Health Sciences (WesternU). The opportunity to work at one of their Health Clinical facilities was a dream come true. But before she could begin her journey, there was one crucial step she had to complete: the credentialing process.
Emma knew this was no small task. The university required a thorough background check, and she understood that her career in the clinic hinged on the completion of this process. The College had sent her a detailed list of documents that needed to be gathered and submitted before anything could move forward.
She began by carefully reviewing the list. The first item was the California Participating Practitioner Application (CPPA). Emma made sure to answer every question meticulously, knowing that any missing information could cause delays. She gathered all the supporting documentation, double-checking that everything was in order.
Next, she updated her Curriculum Vitae (CV). Every date and detail of her professional history had to be accurate and current. She knew that the Credentialing Office would scrutinize every entry.
Her California State Professional License was next on the list. Emma had just updated her address on the license, so she was confident it would meet the university’s requirements. She also made sure to provide proof that she had applied for her California License, just in case.
The documents continued to pile up. She photocopied her California Driver’s License, her DEA License, and her NPI notification from the National Plan and Provider Enumeration System (NPPES). Emma was diligent, ensuring that each copy was clear and legible.
Board certifications were critical. Emma was board-certified and made sure to include the exact dates she had received and would renew her certification. The Credentialing Office needed these details to verify her qualifications.
One of the more challenging tasks was gathering her Malpractice Claims History. Emma contacted her insurance carrier to obtain the necessary documents. The process took a bit of time, but she knew it was essential to prove that she was covered.
Her Dental College transcripts and Continuing Education (CE) records from the past two years were also on the list. Emma contacted her alma mater and the relevant professional bodies to get these documents. She wanted to ensure there would be no delays due to missing paperwork.
As she compiled the necessary forms provided by the Credentialing Office, Emma took a deep breath. She knew that her background check would be thorough, but she was confident that her records were in order. She completed the Background Release Form, signed the Notice and Authorization to Obtain Background Check for Employment Purposes, and acknowledged her responsibility as a mandated reporter for child abuse and neglect.
Emma also had to provide proof of her communicable disease clearance. She made sure her MMR, varicella, Hepatitis B, TB, and Tdap vaccinations were up to date, knowing these were non-negotiable for her new role.
There was one last thing—if there had been any name changes since graduating from Dental School, she would need to provide documentation. Thankfully, this didn’t apply to her, but she made a mental note of the requirement just in case.
Finally, Emma prepared to submit everything to the Credentialing Office. She knew that once her background check was complete, and all her documents were verified, she would be credentialed with the various payer sources used at Tranquil Medsolutions. Only then would she be able to step into the clinic and begin the work she was so passionate about.
With a mix of anticipation and relief, Emma sent off her documents. She knew the process could take up to 120 days, but she was ready for the wait. After all, this was the final step before she could embark on her new adventure at Tranquil Medsolutions. All that was left to do now was to wait for the green light to begin her journey as a credentialed dentist at Tranquil.
0 notes
Text

New patient visits can be bustling hubs of activity, but ensuring flawless billing for new patient visits shouldn’t add to the chaos. This article equips primary care providers with the latest knowledge and technical expertise to navigate the process seamlessly, maximizing new patient visit billing accuracy and minimizing compliance risks.
#claim#Claims#Credentialing#healthcare#medicaid#medicalbilling#MedicalBillingServices#medicalcoding#patient#physician#PrimaryCare#PrimaryCareMedicalBilling#medicare#Reimbursement
0 notes
Text

Struggling with ABA billing? Imagnum Healthcare Solutions in Cherry Hill, NJ, understands the challenges. Trust our local team to handle your ABA billing needs with precision and care, so you can focus on making a difference in your clients' lives.
#medicalbilling#abatherapy#brmb#aba#autism#physicaltherapy#insurance#credentialing#betterresults#familypractice#medicalbillingservices
1 note
·
View note
Text
QuantumNest LLC offers top-tier Medical Billing Services in California, ensuring seamless revenue management for healthcare providers. Our comprehensive solutions optimize billing processes, reduce errors, and maximize reimbursement. Trust QuantumNest for efficient, accurate, and compliant medical billing tailored to your practice's needs, elevating your financial performance.
#QuantamNest LLC#top medical billing companies in usa#best medical billing company#top rcm companies in usa#medical billing service near me#quality medical billing services#home health medical billing#Best medical billing company#Top RCM services company#Medical billing#Best medical billing service in my area#Home health billing services#billing medicare for home health services#Top tier RCM services company#home health care services in medical billing#Behavioural health billing#home health billing medicare#Oasis#Quality assurance#Credentialing#Best credentialing company#Insurance billing
0 notes