#Covid-19 patient tracking app
Explore tagged Tumblr posts
Text
Long COVID symptom severity varies widely by age, gender, and socioeconomic status - Published Sept 2, 2024
By Dr. Sushama R. Chaphalkar, PhD.
In a recent study published in the journal JRSM Open, researchers analyze self-reported symptoms of long coronavirus disease 2019 (LC) from individuals using a healthcare app to examine the potential impact of demographic factors on the severity of symptoms. The researchers found that LC symptom severity varied significantly by age, gender, race, education, and socioeconomic status.
Research highlights the urgent need for targeted interventions as age, gender, and social factors play a crucial role in the intensity of long COVID symptoms. What factors increase the risk of long COVID? Several months after recovering from coronavirus disease 2019 (COVID-19), patients with LC may continue to suffer from numerous symptoms, some of which include fatigue, brain fog, and chest pain. The prevalence of LC varies, with estimates ranging from 10-30% in non-hospitalized cases to 50-70% in hospitalized patients.
Although several digital health interventions (DHIs) and applications have been developed to monitor acute symptoms of COVID-19, few have been designed to track long-term symptoms of the disease. One DHI called "Living With COVID Recovery" (LWCR) was initiated to help individuals manage LC by self-reporting symptoms and tracking their intensity. However, there remains a lack of evidence on the risk factors, characteristics, and predictors of LC, thereby limiting the accurate identification of high-risk patients to target preventive strategies.
About the study In the present study, researchers investigate the prevalence and intensity of self-reported LC symptoms to analyze their potential relationship with demographic factors to inform targeted interventions and management strategies. To this end, LWCR was used to monitor and analyze self-reported LC symptoms from individuals in 31 LC clinics throughout England and Wales.
The study included 1,008 participants who reported 1,604 unique symptoms. All patients provided informed consent for the use of their anonymized data for research.
Multiple linear regression analysis was used to explore the relationship between symptom intensity and factors such as time since registration, age, ethnicity, education, gender, and socioeconomic status through indices of multiple deprivation (IMD) on a scale of one to 10.
Education was classified into four levels denoted as NVQ 1-2, NVQ 3, NVQ 4, and NVQ 5, which reflected those who were least educated at A level, degree level, and postgraduate level, respectively. The intensity of symptoms was measured on a scale from zero to 10, with zero being the lowest and 10 the highest intensity. Descriptive statistics identified variations in symptom intensity across different demographic groups.
Study findings Although 23% of patients experienced symptoms only once, 77% experienced symptoms multiple times. Corroborating with existing literature, the most prevalent symptoms included pain, neuropsychological issues, fatigue, and dyspnea, which affected 26.5%, 18.4%, 14.3%, and 7.4% of the cohort, respectively. Symptoms such as palpitations, light-headedness, insomnia, cough, diarrhea, and tinnitus were less prevalent.

Fifteen most prevalent LC symptoms. Multiple linear regression analysis revealed that symptom intensity was significantly associated with age, gender, ethnicity, education, and IMD decile. More specifically, individuals 68 years of age and older reported higher symptom intensity by 32.5% and 86%, respectively. These findings align with existing literature that highlights the increased risk of LC symptoms with age, which may be due to weakened immunity or the presence of comorbidities. Thus, they emphasize the need for targeted interventions for this population.
Females also reported higher symptom intensity than males, by 9.2%. Non-White individuals experienced higher symptom intensity by 23.5% as compared to White individuals.
Individuals with higher education levels reported up to 47% reduced symptom intensity as compared to those with lower education levels. Higher IMD deciles, which reflect less deprived areas, were associated with lower symptom intensity; however, no significant association was observed between the number of symptoms reported and the IMD decile.

Regression results with 95% confidence interval. Note: For age, the base group is people in the age category 18–27. For IMD, the base group is people from IMD decile 1. For education, the base group is people who left school before A-level (NVQ 1–2). A significant positive association was observed between symptom intensity and the duration between registration on the app and initial symptom reporting. This finding suggests individuals may become more aware of their symptoms or that worsening symptoms prompt reporting.
Some limitations of the current study include the lack of data on comorbidities, hospitalization, and vaccine status. There is also a potential for bias against individuals lacking technological proficiency or access, which may affect the sample's representativeness, particularly for older, socioeconomically disadvantaged, or non-English-speaking individuals. Excluding patients with severe symptoms or those who were ineligible for the app may also skew the findings.
Conclusions There remains an urgent need to develop targeted interventions to address the severity of LC in relation to age, ethnicity, and socioeconomic factors. LC treatment should prioritize prevalent symptoms like pain, neuropsychological issues, fatigue, and dyspnea while also considering other possible symptoms. Furthermore, sustained support for LC clinics is essential to effectively manage the wide range of symptoms and complexities associated with LC and improve public health outcomes in the post-pandemic era.
Journal reference:
Sunkersing, D., Goodfellow, H., Mu, Y., et al. (2024). Long COVID symptoms and demographic associations: A retrospective case series study using healthcare application data. JRSM Open 15(7). doi:10.1177/20542704241274292.
journals.sagepub.com/doi/10.1177/20542704241274292
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator#long covid
38 notes
·
View notes
Text
Toward the end of last year, US health authorities got a tip-off about an upcoming wave of respiratory syncytial virus, a seasonal virus that kills 160,000 people globally every year. Before hospitals reported an uptick in patients, they could see that RSV was more acute in the northeast of the country, with concentrations of the virus ultimately reaching levels more than five times greater than in the western United States. Their early warning system? Wastewater.
By regularly testing virus levels in public wastewater, health institutions are able to target treatments and interventions to the worst-affected areas before doctors on the ground realize something’s going on. “If you can get the information to hospitals or clinics weeks earlier, that gives the opportunity to start thinking about what treatments they might need,” says Marisa Donnelly, senior principal epidemiologist at Biobot Analytics, which helped develop a wastewater surveillance system for the US Centers for Disease Control.
RSV is very common: Every year, 64 million people worldwide get an RSV infection, according to the US National Institute for Allergy and Infectious Diseases—but it’s particularly problematic for the very old and very young. Preventative measures are available, including vaccines and monoclonal antibodies. But often, by the time a community recognizes it has an RSV outbreak, it’s too late to mount the most effective response. Getting hold of enough drugs can also be tricky. “Wastewater analysis gives you better situational awareness of what’s going on and how much it’s fluctuating over time, because we have [historically] very much underdetected RSV cases,” says Bill Hanage, associate director of the Center for Communicable Disease Dynamics at the Harvard T.H. Chan School of Public Health.
The concept of tracking a virus through wastewater came to prominence in the early days of the Covid-19 pandemic in 2020, says Tyson Graber, associate scientist at the Children's Hospital of Eastern Ontario Research Institute, who worked on wastewater analysis as part of Ontario’s Covid response. Initially, researchers weren’t too hopeful. “Nobody thought that you could actually detect bits and pieces of material from a respiratory virus,” says Graber. Yet it proved possible: The scientists were able to detect the presence of SARS-CoV-2, the virus behind Covid-19.
This near-real-time analysis of the virus’s spread helped improve responses to the pandemic not just in Ontario, but worldwide. In the US, the CDC launched its National Wastewater Surveillance System in September 2020.
While each pathogen has its own “predilections and eccentricities,” says Graber, it was possible to adapt the process to look for RSV. Regular RSV testing in wastewater now takes place in the US, Canada, Finland, and Switzerland.
A study of the Ontario experiment in RSV wastewater tracking found that it gives more than a month’s notice in identifying when RSV season begins, and nearly two weeks’ warning of a surge, compared to waiting for people to turn up sick. “We definitely see increases in [RSV in] wastewater starting before we see those same increases in clinical data like hospitalizations,” says Donnelly.
Jasmine Reed, a CDC spokesperson, says that wastewater analysis complements other surveillance systems. “It can capture asymptomatic cases and other cases independent from medical systems, and provides a broader population-level perspective on disease spread,” she says.
The CDC’s program is set up so that, if RSV levels are high in a particular community, local health departments can prioritize interventions, including testing, infection control, and vaccination efforts.
Donnelly envisions wastewater surveillance becoming like a public health “weather app” where communities can check virus activity in their area and make informed decisions on behaviors like masking or vaccination. “We want this system to be expanded across the United States so that everybody has access to wastewater information and add additional tools to keep themselves healthy,” she says. Hanage foresees wastewater analysis being used to track other communicable viruses, like mpox.
While there’s plenty of excitement about the technique, others are more cautious. “It’s one of those sciences that has got a lot of people really excited,” says Paul Hunter, a virologist and professor in medicine at the University of East Anglia. “You either think it’s brilliant or you think it’s pointless, and there’s very little in between.”
Hunter recognizes that wastewater analysis can pick up the spread of disease—and points to evidence that it did so in the Covid-19 pandemic—but questions whether the extra cost is worth the extra insights it provides. “Certainly in Covid, we didn’t think it was [necessary] in the UK, and I think that was the correct judgment,” he says.
But proponents say it’s worth it for RSV—especially given some of the challenges around drug shortages. Last year’s RSV season proved particularly vexing to the US health system, as shortages of nirsevimab, an antibody injection given to infants, were reported across the country.
There’s hope that things will be different when RSV season begins again in the coming weeks. “If you can get the information to hospitals or clinics weeks earlier, that gives the opportunity to start thinking about what treatments they might need,” says Donnelly.
3 notes
·
View notes
Text
Public Health Campaigns & Communities
What is public health?
Public health, as a multidisciplinary field, is dedicated to enhancing the health and overall well-being of communities (Lee, 2023). It strives to create safe environments for people to live, learn, work, and enjoy their lives. Many people mistakenly believe that public health is the same as healthcare. However, it is important to distinguish between the two, as public health focuses on entire populations with the objective of preventing illnesses and injuries, while the healthcare industry concentrates on treating individual patients who are already sick (APHA, 2023).
For example, public health is responsible for the following:

"Public health is the science and art of preventing disease, prolonging life, and promoting health through the organized efforts and informed choices of society, organizations, public and private communities, and individuals." — Winslow, 1920
The 10 Essential Public Health Services
The 10 Essential Public Health Services (EPHS), first created in 1994 by a federal working group, serves as the description of the activities that public health systems should undertake in all communities. EPHS is organised around the three core functions of public health: assessment, policy development and assurance. Health departments and community partners collaborators across the nation structure their work around the EPHS model, while educational institutions and public health programs also incorporate it into their teachings (CDC, 2023).
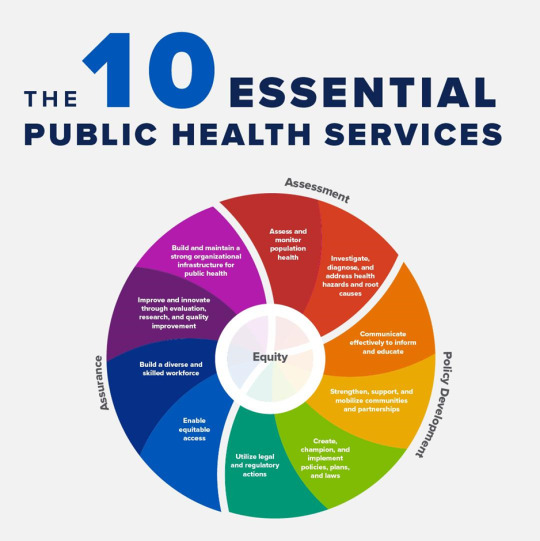
In 2020, a revised version of the 10 EPHS was unveiled during a virtual launch event. The revised EPHS centres around equity and promotes policies that enable optimal health for all and seek to remove systemic and structural barriers such as poverty, racism, gender discrimination and others, that have resulted in health inequities (CDC, 2023).
“The revised 10 EPHS not only centres equity but acknowledges the importance of community voice and the different roles public health plays.” — Jessica Fisher, Vice President of Strategic Initiatives at Public Health National Center for Innovations (PHNCI).
COVID-19 and Public Health
COVID-19, caused by an infection of the SARS-CoV-2 virus, was initially detected in December 2019 in Wuhan, a city in China's Hubei province. The COVID-19 pandemic has posed a substantial threat to nations across the world, and it is regarded as the biggest public health crisis the world has confronted in over a century (Miyah, 2022). In late 2020, the World Health Organisation (WHO) declared the COVID-19 outbreak as a Public Health Emergency of International Concern in which countries with vulnerable healthcare facilities may be at an excessive hazard (Tabari, 2020).
In response to this crisis, many countries have enacted travel restrictions, including flight suspensions and measures to limit incoming travellers. Others have introduced social distancing and quarantine policies as well as encouraging the reduction of social interactions, postponing events, locking down schools, and isolating suspected cases. Furthermore, some regions have utilized telemedicine for remote consultations and monitoring during the outbreak (Tabari, 2020).

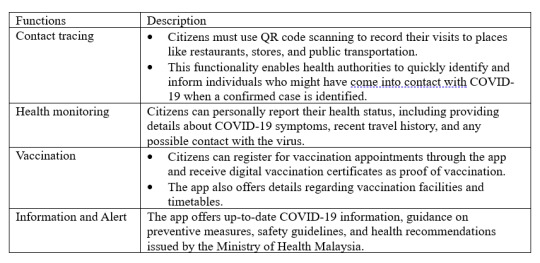
MySejahtera is a mobile app developed by the Malaysian government to support various aspects of public health throughout the COVID-19 pandemic. This app enables citizens to conduct self-health assessments, track their health status, and communicate information with the Ministry of Health (MOH), so that necessary actions could be implemented.
Here are its primary functions:
Explore https://www.maaedicare.org/wp-content/uploads/2021/11/MySejahtera_compressed.pdf for detailed function and process of using MySejahtera.
Mental Health Problem Attribute to Social Media
Last but not least, mental health is a crucial aspect of public health, and the well-being of individuals, particularly those in the 16-24 age group, is a matter of significant concern. A survey conducted in Malaysia in May 2022 revealed that a considerable portion of young respondents in this age range reported experiencing heightened levels of stress and anxiety over the past year (Statista Research Department, 2023). Furthermore, this research suggests that social media plays a substantial role in contributing to this mental health problem.
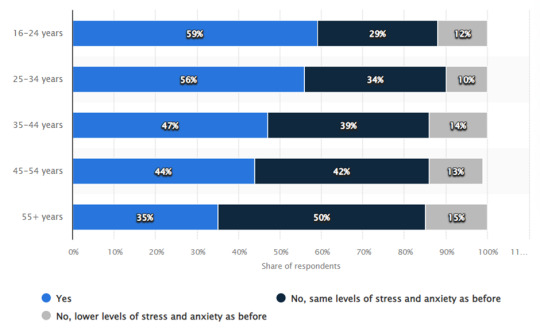
Source: Statista Research Department, 2023
Multiple studies have demonstrated a strong connection between heavy use of social media and the risk for mental health issues (Robinson, 2023). Social media platforms can be hotspots for the dissemination of hurtful rumours, lies and online harassment. About 10 percent of teens report being bullied on social media and many other users are subjected to offensive comments (Robinson, 2023). Additionally, fear of missing out (FOMO) can compel someone to pick up their phone every few minutes to check for updates, or compulsively respond to every alert. When individuals prioritize online interactions over in-person relationships, they become more vulnerable to mood disorders, such as anxiety and depression.

These findings highlight the importance of recognizing the influence of social media on mental health, especially among young adults. In summary, striking a balance between the advantages of digital connectivity and the preservation of mental well-being is crucial to ensure that social media serves as a positive and constructive tool in the lives of young individuals.
References:
American Public Health Association. (n.d.). What is public health. https://www.apha.org/what-is-public-health
CDC. (2021). Public health system and the 10 essential public health services. Centers for Disease Control and Prevention. https://www.cdc.gov/publichealthgateway/publichealthservices/essentialhealthservices.html
C.-E. A. Winslow, The Untilled Fields of Public Health.Science51,23-33(1920).DOI:10.1126/science.51.1306.23
Lee, D., Chen, K., & Kruger, J. S. (2023, January 1). Chapter 93 - Public health (A. E. M. Eltorai, J. A. Bakal, P. C. Newell, & A. J. Osband, Eds.). ScienceDirect; Academic Press. https://www.sciencedirect.com/science/article/abs/pii/B9780323903004000616
Malaysia: stress levels by age group 2022. (2023, August 25). Statista. https://www.statista.com/statistics/1322323/malaysia-share-of-people-feeling-more-stressed-or-anxious-by-gender/#:~:text=According%20to%20a%20survey%20on
Miyah, Y., Benjelloun, M., Lairini, S., & Lahrichi, A. (2022). COVID-19 Impact on Public Health, Environment, Human Psychology, Global Socioeconomy, and Education. TheScientificWorldJournal, 2022, 5578284. https://doi.org/10.1155/2022/5578284
Robinson, L., & Smith, M. (2020, September). Social Media and Mental Health - HelpGuide.org. Https://Www.helpguide.org. https://www.helpguide.org/articles/mental-health/social-media-and-mental-health.htm#:~:text=Since%20it
Tabari, P., Amini, M., Moghadami, M., & Moosavi, M. (2020). International Public Health Responses to COVID-19 Outbreak: A Rapid Review. Iranian journal of medical sciences, 45(3), 157–169. https://doi.org/10.30476/ijms.2020.85810.1537
World Health Organization (WHO). (2022, June 17). Mental Health. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/mental-health-strengthening-our-response
2 notes
·
View notes
Text
How Are Digital Respiratory Devices Revolutionizing Healthcare?
The Digital Respiratory Devices Market is experiencing rapid growth, with a projected value of USD 307.2 billion by 2030. The rise in chronic respiratory diseases, coupled with advancements in digital healthcare technologies, is transforming the landscape of respiratory care. But what exactly are digital respiratory devices, and how are they changing the way we approach respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD)? Let’s explore this emerging market and its potential for the future.
What Are Digital Respiratory Devices?
Digital respiratory devices are sophisticated tools that combine therapeutic and diagnostic functions with digital technologies. These devices are designed to connect with smartphones, mobile apps, or other data collection modules, enabling real-time monitoring and management of respiratory diseases. The most common types of digital respiratory devices include smart inhalers, nebulizers, spirometers, and asthma monitors. These devices track important health data such as inhaler usage, lung function, and environmental factors like pollution levels.
One key feature of these devices is their ability to sync with mobile applications, which store data and provide real-time feedback to patients and healthcare providers. For example, a smart inhaler can wirelessly transmit information about the number of doses used, helping patients better manage their asthma or COPD. Additionally, some digital respiratory devices allow patients to track symptoms, medication adherence, and environmental conditions like air quality—all crucial factors in managing respiratory health.
For a deeper dive into the growing digital respiratory market, check out this Digital Respiratory Devices Market Report.
Why Is the Digital Respiratory Devices Market Growing?
The digital respiratory devices market is growing rapidly, driven by several key factors. Here are some of the main drivers:
1. The Rise of Chronic Respiratory Diseases
Respiratory diseases like asthma, COPD, and pneumonia are becoming increasingly prevalent worldwide. According to the World Health Organization (WHO), asthma alone affects approximately 235 million people globally. COPD, which is often linked to smoking and air pollution, is also a leading cause of death. As the incidence of these diseases rises, there is a greater need for effective and efficient tools to manage symptoms, improve patient outcomes, and reduce hospital admissions.
Digital respiratory devices provide patients with a convenient and effective way to manage their conditions from home. This is crucial as patients with chronic respiratory diseases often need to monitor their symptoms regularly to prevent exacerbations.
2. Technological Advancements in Healthcare
Healthcare is undergoing a major technological transformation, with digital health tools becoming more accessible and user-friendly. The integration of artificial intelligence (AI), data analytics, and mobile health apps has significantly enhanced the functionality of digital respiratory devices. These technologies help track patient data, predict flare-ups, and provide recommendations for better disease management.
Smart inhalers, for instance, use sensors to detect when the inhaler is used and record data, which is then sent to an app or cloud platform. This provides patients and doctors with real-time insights into medication usage, helping to prevent misuse or missed doses.
3. COVID-19 Pandemic and Demand for Respirators
The COVID-19 pandemic has put a spotlight on the importance of respiratory care devices. With the spread of the virus, which targets the respiratory system, there has been an increased demand for ventilators and other respiratory equipment. Hospitals and healthcare facilities have faced shortages of critical equipment, driving the need for more advanced digital solutions.
As the virus has spread globally, governments and healthcare providers have scrambled to increase the availability of respiratory devices. Digital respiratory devices offer a solution for home monitoring and management of respiratory conditions, reducing the pressure on healthcare facilities and enabling patients to manage their symptoms more effectively at home.
4. Increased Adoption of Remote Monitoring
Remote monitoring of health conditions has become more important in the post-pandemic era. Patients with chronic respiratory diseases need regular monitoring to manage their symptoms and avoid complications. Digital respiratory devices allow healthcare providers to remotely track patient data, offering a more personalized approach to care.
For example, a doctor can monitor a patient’s peak flow measurements or track their inhaler usage without the patient needing to visit the clinic. This remote monitoring capability helps doctors intervene earlier when problems arise, potentially reducing hospital admissions and improving patient outcomes.
Types of Digital Respiratory Devices
The digital respiratory devices market encompasses a variety of products, each catering to different aspects of respiratory care. Some of the most common devices include:
1. Therapeutic Devices
These devices deliver medication or treatment to patients. They include:
Smart Inhalers: Inhalers equipped with sensors that track usage and send data to mobile apps.
Nebulizers: Devices that turn liquid medicine into a mist, making it easier for patients to inhale.
Smart inhalers have become a game-changer for managing asthma and COPD. These devices not only ensure medication adherence but also provide data that can be used to adjust treatment plans.
2. Diagnostic Devices
Diagnostic devices are used to measure lung function and diagnose respiratory conditions. Common examples include:
Spirometers: Devices that measure the amount of air a person can inhale and exhale, helping to diagnose asthma, COPD, and other respiratory diseases.
Asthma Monitors: These devices help track asthma symptoms and provide feedback to both patients and doctors.
Diagnostic devices are essential for identifying potential problems early on and ensuring that patients receive the right treatment for their condition.
3. Mobile Apps
Mobile apps play a crucial role in the digital respiratory ecosystem. These apps connect to devices like smart inhalers and nebulizers, allowing patients to track their symptoms, medication usage, and other health data. The apps also provide alerts and reminders, helping patients stay on track with their treatment plans.
For more insights into the different types of devices, you can explore our Digital Respiratory Devices Market Overview.
Regional Growth and Key Players in the Market
The demand for digital respiratory devices varies across different regions, with North America expected to dominate the market due to its advanced healthcare infrastructure and high adoption rates of digital medical devices. Europe and Asia-Pacific are also witnessing significant growth, driven by increasing healthcare investments and a rise in respiratory diseases.
Several key players dominate the digital respiratory devices market, including:
Teva Pharmaceutical Industries Ltd.
Propeller Health
3M
AstraZeneca
Adherium Ltd.
These companies are at the forefront of developing innovative digital respiratory solutions to address the growing global demand for respiratory care.
Future Trends in the Digital Respiratory Devices Market
As we look toward the future, several trends are expected to shape the digital respiratory devices market:
1. Integration with Artificial Intelligence (AI)
AI can enhance the functionality of digital respiratory devices by analyzing large sets of data and providing insights that improve patient outcomes. For instance, AI could help predict when a patient’s condition is likely to worsen, allowing doctors to intervene before an emergency arises.
2. More Personalized Treatment
With advancements in data analytics, digital respiratory devices will become even more personalized. Devices will be able to tailor treatment plans based on individual patient data, such as medication usage patterns and lung function.
3. Improved Connectivity
The future of digital respiratory devices will likely include better integration with electronic health records (EHRs), making it easier for healthcare providers to access and monitor patient data.
Conclusion
The Digital Respiratory Devices Market is set for significant growth, driven by increasing demand for efficient and user-friendly respiratory care solutions. With the rise in chronic respiratory diseases and technological advancements in healthcare, digital devices like smart inhalers and nebulizers are revolutionizing the way we manage respiratory conditions. As the market continues to evolve, these devices will play a critical role in improving patient outcomes, reducing healthcare costs, and enhancing the overall quality of care.
To learn more about the digital respiratory devices market and stay updated on the latest trends, check out the detailed report on Digital Respiratory Devices Market.
0 notes
Text
The Connected Drug Delivery Devices Industry: Transforming Patient-Centric Healthcare
The healthcare industry is undergoing a technological transformation, and connected drug delivery devices are at the forefront of this evolution. These smart devices, equipped with connectivity features such as Bluetooth, IoT (Internet of Things), and mobile applications, are revolutionizing the way medications are administered, monitored, and managed. By improving adherence, optimizing treatment outcomes, and enabling real-time data sharing, connected drug delivery devices are redefining patient care and healthcare systems globally.
The connected drug delivery devices market, valued at USD 1.18 billion in 2024, is projected to grow to USD 5.30 billion by 2029, expanding at a compound annual growth rate (CAGR) of 35.13% during the forecast period (2024–2029).
What Are Connected Drug Delivery Devices?
Connected drug delivery devices integrate technology with traditional drug administration tools like inhalers, auto-injectors, syringes, and infusion pumps. These devices collect and transmit real-time data on medication usage, dosage, and adherence via digital platforms, mobile applications, or cloud systems. Designed to enhance patient monitoring, they empower both healthcare providers and patients with actionable insights to optimize treatment.
For chronic diseases such as diabetes, asthma, and autoimmune conditions, where adherence to medication regimens is critical, connected drug delivery devices offer an innovative solution to streamline patient engagement and improve therapy outcomes.
Key Factors Driving the Growth of Connected Drug Delivery Devices
1. Rising Prevalence of Chronic Diseases
The growing burden of chronic diseases such as diabetes, respiratory disorders, and cardiovascular conditions has amplified the need for more effective drug administration and monitoring solutions. Patients managing long-term conditions often struggle with medication adherence, which can lead to poor outcomes. Connected devices provide reminders, real-time feedback, and data reporting to ensure patients stick to their treatment plans.
2. Increasing Focus on Patient-Centric Care
The healthcare industry is shifting toward patient-centric care, where technology plays a central role in empowering patients. Connected drug delivery devices put patients in control by providing feedback on their medication usage, tracking progress, and offering personalized insights. This approach improves engagement and outcomes while reducing the burden on healthcare providers.
3. Advancements in Digital Health and IoT
Technological advancements in IoT, sensor technology, and data analytics have enabled the development of smart drug delivery devices. These devices seamlessly connect to mobile apps, healthcare platforms, and electronic health records (EHRs), ensuring that healthcare providers can remotely monitor and intervene when necessary.
4. Growing Adoption of Telemedicine and Remote Monitoring
Telemedicine has become an integral part of healthcare delivery, especially in the wake of the COVID-19 pandemic. Connected drug delivery devices complement telehealth platforms by enabling remote monitoring of medication adherence and patient progress, reducing the need for in-person visits while ensuring continuity of care.
5. Regulatory Push for Digital Healthcare Solutions
Governments and regulatory bodies are actively promoting digital healthcare solutions, recognizing their role in improving patient outcomes and reducing healthcare costs. Regulatory support for connected devices, especially in regions like North America and Europe, is driving their adoption across healthcare systems.
6. Need for Better Medication Adherence
Medication non-adherence is a significant challenge in healthcare, leading to worsening health outcomes and increased costs. Connected devices address this issue by sending reminders, tracking usage, and alerting healthcare providers if adherence declines, ensuring patients follow their prescribed treatment regimens.
Challenges in the Connected Drug Delivery Devices Industry
1. High Development and Implementation Costs
Developing connected drug delivery devices requires significant investment in technology, research, and compliance with stringent regulatory standards. The high initial costs can limit adoption, particularly in resource-constrained healthcare systems.
2. Data Privacy and Security Concerns
As connected devices transmit sensitive patient data, concerns about cybersecurity and privacy are prominent. Ensuring that data is securely stored and compliant with regulations such as GDPR and HIPAA is critical to gaining patient and provider trust.
3. Complexity of Integration with Healthcare Systems
While connected devices generate valuable data, integrating this data into existing healthcare systems and electronic health records (EHRs) can be complex. Seamless interoperability remains a challenge for widespread
For a detailed overview and more insights, you can refer to the full market research report by Mordor Intelligence: https://www.mordorintelligence.com/industry-reports/connected-drug-delivery-devices-market
#Connected Drug Delivery Devices Market#Connected Drug Delivery Devices Market Size#Connected Drug Delivery Devices Market Share#Connected Drug Delivery Devices Market Analysis#Connected Drug Delivery Devices Market Report
0 notes
Text
Comprehensive Guide to Telemedicine App Development: Features, Benefits, and Costs

In today's fast-paced world, telemedicine has revolutionized healthcare by making it more accessible and efficient. Telemedicine app development empowers healthcare providers to deliver seamless medical services through digital platforms.
This guide explores the top features of telemedicine app development, its benefits, and the cost to develop a telemedicine app development solution.
Key Features of Telemedicine App Development
To build a telemedicine app that meets modern healthcare demands, you must include the following top features:
Video ConferencingA critical feature of telemedicine app development, video conferencing enables real-time communication between patients and healthcare professionals.
Appointment SchedulingPatients can effortlessly book, reschedule, or cancel appointments through an intuitive interface.
E-prescriptionsFacilitate seamless prescription issuance and management, ensuring patient convenience and accuracy.
Electronic Health Records (EHR) IntegrationThis feature allows secure storage and quick access to patient health records.
Real-Time ChatInstant communication between doctors and patients enhances engagement and responsiveness.
Payment Gateway IntegrationSecure payment solutions streamline financial transactions within the app.
Analytics and ReportingTelemedicine apps can track patient data and engagement trends, aiding in decision-making and performance optimization.
Top Benefits of Telemedicine App Development
Enhanced AccessibilityTelemedicine apps bridge the gap between healthcare providers and patients, especially in underserved or remote areas. They eliminate geographical barriers, ensuring that individuals can access quality medical consultations without the need to travel. This feature is particularly beneficial for elderly patients or those with limited mobility.
ConvenienceThe flexibility of telemedicine apps allows patients to consult doctors from the comfort of their homes. These platforms provide 24/7 availability, enabling individuals to seek medical attention outside of traditional office hours, which is particularly useful for emergencies or second opinions.
Cost SavingsTelemedicine significantly reduces operational costs for healthcare providers by minimizing the need for physical infrastructure. Patients also save on travel expenses and time off work. Affordable virtual consultations make healthcare more accessible, driving higher adoption rates.
Efficient Resource UtilizationReal-time data tracking and appointment scheduling systems ensure that resources like staff time, consultation slots, and equipment are used effectively. This efficiency helps clinics and hospitals reduce waiting times and streamline patient management.
Better Patient EngagementTelemedicine apps foster improved patient engagement by offering interactive features like health tracking, medication reminders, and lifestyle tips. Push notifications keep patients informed about their health, enhancing compliance with treatment plans and leading to better health outcomes.
Improved Chronic Disease ManagementPatients with chronic conditions such as diabetes, hypertension, or asthma can benefit from regular monitoring through telemedicine apps. Remote consultations and wearable integrations help doctors track vital signs, adjust treatments, and provide timely interventions.
Greater Scalability for ProvidersHealthcare providers can expand their reach to a larger patient base without investing heavily in additional infrastructure. Telemedicine platforms allow doctors to consult patients across different cities or even countries, boosting their practice’s scalability.
Reduced Exposure to InfectionsVirtual consultations minimize the risk of infection spread, especially in the context of contagious diseases like COVID-19. Patients can seek medical advice without exposing themselves to crowded clinics, reducing the risk of cross-contamination.
Faster Diagnosis and TreatmentWith features like electronic health record (EHR) integration, telemedicine apps provide doctors with immediate access to patient history, test results, and other critical information. This access speeds up the diagnostic process and enables quicker decision-making for treatment plans.
Increased Privacy and SecurityModern telemedicine platforms prioritize data privacy and adhere to regulations like HIPAA and GDPR. Advanced encryption methods ensure that sensitive patient information remains secure, building trust between patients and providers.
Cost to Develop a Telemedicine App Development
The cost to develop a telemedicine app depends on various factors, including the app's features, platform choice, complexity, and the development team's location. Whether you're building a simple telemedicine app or an advanced solution with AI-powered analytics and integrations, each factor plays a role in determining the final price.
Basic Telemedicine App Development
A basic telemedicine app includes essential features like video calls, appointment booking, and basic chat functionality. These features are fundamental for establishing an online consultation platform that allows patients to connect with healthcare providers remotely. Here's an overview of the cost breakdown:
Core Features: Video calling, appointment scheduling, push notifications, and basic patient-doctor interaction.
Estimated Cost: $20,000–$40,000.
This type of app is ideal for startups or healthcare providers looking to offer virtual consultations without extensive additional features. However, while it's cost-effective, it may lack some of the advanced capabilities that would enhance patient engagement and provider efficiency.
Mid-Level Telemedicine App Development
A mid-level telemedicine app offers more advanced functionalities like Electronic Health Record (EHR) integration, real-time chat, and prescription management. These features ensure better patient data management and smoother communication between doctors and patients. Here's a breakdown:
Core Features: Video conferencing, appointment scheduling, real-time chat, patient profiles, EHR integration, and prescriptions.
Estimated Cost: $40,000–$80,000.
This range of telemedicine apps is suitable for healthcare organizations that need more advanced features to support patient care, including secure access to medical records and enhanced communication.
Advanced Telemedicine App Development
An advanced telemedicine app incorporates sophisticated technologies like AI-powered analytics, wearable device integration, and a scalable infrastructure capable of handling large user bases. These apps often include high-end features for personalized care, data analysis, and real-time health monitoring.
Core Features: AI-powered analytics, wearable integration, EHR systems, video calling, advanced real-time chat, scalable backend, health data tracking, and more.
Estimated Cost: $80,000–$150,000.
This level of app development is typically suited for large healthcare providers, hospitals, or telemedicine platforms offering specialized care with robust data security and predictive healthcare solutions.
Factors Affecting the Cost of Telemedicine App Development
Platform Choice (iOS, Android, or Both): Developing an app for multiple platforms (iOS and Android) increases the cost, as it requires separate development processes for each operating system.
App Complexity: The more advanced the features—such as AI, machine learning, and IoT integration—the higher the cost. Advanced apps require a larger development team and more time.
Location of Development Team: Telemedicine app development cost can vary significantly based on the location of your development team. For instance:
North America: The average hourly rate for developers ranges from $100 to $250.
Eastern Europe: Development teams charge between $40 and $100 per hour.
Asia (India, Philippines): Rates here are more affordable, often ranging from $20 to $60 per hour.
Hiring a development team in regions with lower hourly rates can reduce costs without sacrificing quality.
Security and Compliance: Given that telemedicine apps handle sensitive patient data, incorporating HIPAA compliance, encryption standards, and data protection measures can increase costs. Ensuring that your app complies with regional regulations such as GDPR or HIPAA is crucial for safeguarding patient information.
Maintenance and Updates: After launching your app, ongoing maintenance and regular updates to fix bugs, improve features, and comply with changing healthcare regulations will incur additional costs.
How to Develop a Telemedicine App?
Developing a telemedicine app involves several critical steps. Here’s a roadmap for how to build a telemedicine app:
Research and PlanningDefine the target audience, analyze market trends, and determine must-have features.
UI/UX DesignCreate a user-friendly interface that ensures smooth navigation for patients and healthcare providers.
Backend and Frontend DevelopmentDevelop robust backend systems for secure data handling and frontend interfaces for seamless user interaction.
Integration of FeaturesIncorporate the top features of telemedicine app development, ensuring all functionalities operate smoothly.
Testing and Quality AssuranceRigorously test the app to identify and resolve any bugs or issues.
Deployment and MaintenanceLaunch the app on various platforms and provide ongoing updates to enhance performance and security.
Final Thoughts
Telemedicine app development is a transformative solution for modern healthcare. By understanding the features, benefits, and costs, you can create an innovative app that meets the needs of patients and providers alike. If you're ready to build a telemedicine app, ensure you prioritize security, compliance, and user experience.
Let Comfygen's expert team guide you through the process of how to develop a telemedicine app with precision and excellence. Contact us today to bring your vision to life!
#healthcareappdeveloper#healthcareappdevelopmentcompany#healthcareapplication#mobile app development
0 notes
Text
Choose Best Pathology Services in Noida for blood test home collection

Healthcare is not an exception today in this fast-paced world, where efficiency and convenience are in dominant positions. In Noida, the blood collection services are changing the way medical analysis is conducted. Hence, the residents feel comfortable and easy.
Today, people need not wait too long at the diagnostic centers or commute at early hours to avoid crowds. A trained professional by the pathology lab in Sector 121 Noida comes to your home with home collection services at your own convenience, collects a blood sample, and assures you it is a secure and safe dispatch to the certified laboratory. This method saves time and minimizes the hassles, especially for senior citizens, busy professionals, and people with mobility issues.
One of the crucial benefits of this service is its capacity to minimize exposure to environments that are potentially hazardous. It became particularly important during the COVID-19 pandemic period. By preventing visits to crowded labs or hospitals, patients can reduce the health risks, and yet you can get an accurate diagnosis.
Many reputed diagnostic labs and startups have implemented advanced technologies in Noida to channelize this procedure. Using user-friendly apps or websites, customers can book appointments or track sample collection and get reports directly on smartphones or emails directly. Many service providers also give specialized examinations customized to the needs of an individual, from daily check-ups to advanced monitoring for chronic diseases.
Blood test home collection in Noida, moreover, are cost-effective with lovely health packages and competitive pricing. These services are suitable for the people who give preference to health without compromising their daily schedule.
The pathlab in Noida are establishing new benchmarks in Noida as the demand for convenient health care grows. They symbolize the need for modern healthcare, efficiency, accessibility, and a patient-centric approach that is easier.
Cherish the future of medical diagnosis, as your health deserves the most!
#pathology#pathology in noida#bes pathology lab in noida#blood test#blood test home collecton#pathlab
0 notes
Text
Smart Pulse Oximeters Market Size, Trends & Forecast 2025-2035
Smart Pulse Oximeters Market: A Growing Trend in Health Monitoring The Smart Pulse Oximeters Market is revolutionizing healthcare by offering accurate, real-time monitoring of vital health parameters such as blood oxygen levels and heart rate. These advanced devices are not only used in clinical settings but are increasingly adopted by individuals for personal health management, reflecting a shift toward preventive and at-home care.
In 2024, the market was valued at USD 2.1 billion, and it is projected to reach USD 5.8 billion by 2030, growing at a CAGR of 12.8% during this period. This remarkable growth is driven by the rising prevalence of respiratory and cardiovascular diseases, an aging population, and increased health awareness post-COVID-19. Smart Pulse Oximeters Market: A Growing Trend in Health Monitoring The Smart Pulse Oximeters Market is revolutionizing healthcare by offering accurate, real-time monitoring of vital health parameters such as blood oxygen levels and heart rate. These advanced devices are not only used in clinical settings but are increasingly adopted by individuals for personal health management, reflecting a shift toward preventive and at-home care.
In 2024, the market was valued at USD 2.1 billion, and it is projected to reach USD 5.8 billion by 2030, growing at a CAGR of 12.8% during this period. This remarkable growth is driven by the rising prevalence of respiratory and cardiovascular diseases, an aging population, and increased health awareness post-COVID-19.
For in-depth insights, visit Smart Pulse Oximeters Market: A Growing Trend in Health Monitoring The Smart Pulse Oximeters Market is revolutionizing healthcare by offering accurate, real-time monitoring of vital health parameters such as blood oxygen levels and heart rate. These advanced devices are not only used in clinical settings but are increasingly adopted by individuals for personal health management, reflecting a shift toward preventive and at-home care.
In 2024, the market was valued at USD 2.1 billion, and it is projected to reach USD 5.8 billion by 2030, growing at a CAGR of 12.8% during this period. This remarkable growth is driven by the rising prevalence of respiratory and cardiovascular diseases, an aging population, and increased health awareness post-COVID-19.
For in-depth insights, visit https://www.metatechinsights.com/industry-insights/smart-pulse-oximeters-market-1166
Market Drivers and Innovations
Rising Demand for Health Monitoring The surge in chronic conditions like COPD, asthma, and sleep apnea has elevated the demand for smart pulse oximeters. These devices enable early detection of health issues, providing critical data that supports timely medical intervention.
Technological Advancements Modern smart pulse oximeters incorporate Bluetooth, Wi-Fi connectivity, and smartphone integration, making them highly convenient for continuous health tracking. Features like app-based analytics and cloud storage allow users to share data with healthcare providers seamlessly.
Post-Pandemic Health Awareness The COVID-19 pandemic highlighted the importance of tracking blood oxygen saturation (SpO2) levels, leading to widespread adoption of these devices for home use. This trend has persisted, with individuals increasingly prioritizing proactive health monitoring.
Challenges and Opportunities
Cost and Accessibility Despite their benefits, the high cost of smart pulse oximeters limits adoption, especially in developing regions. Manufacturers must address affordability to tap into these markets.
Growth in Telemedicine The rise of telemedicine presents a significant opportunity for smart pulse oximeters. By integrating with telehealth platforms, these devices enable remote patient monitoring, ensuring healthcare access even in rural or underserved areas.
Personalized Healthcare The integration of AI and predictive analytics in smart pulse oximeters opens doors for personalized healthcare solutions. These technologies can analyze trends and provide actionable health insights, improving user engagement and outcomes.
Conclusion The Smart Pulse Oximeters Market is poised for significant growth as consumers increasingly adopt wearable health technologies. With ongoing innovations and expanding applications, these devices are set to become a cornerstone of modern healthcare. For detailed market analysis, visit metatechinsights.com.
Market Drivers and Innovations
Rising Demand for Health Monitoring The surge in chronic conditions like COPD, asthma, and sleep apnea has elevated the demand for smart pulse oximeters. These devices enable early detection of health issues, providing critical data that supports timely medical intervention.
Technological Advancements Modern smart pulse oximeters incorporate Bluetooth, Wi-Fi connectivity, and smartphone integration, making them highly convenient for continuous health tracking. Features like app-based analytics and cloud storage allow users to share data with healthcare providers seamlessly.
Post-Pandemic Health Awareness The COVID-19 pandemic highlighted the importance of tracking blood oxygen saturation (SpO2) levels, leading to widespread adoption of these devices for home use. This trend has persisted, with individuals increasingly prioritizing proactive health monitoring.
Challenges and Opportunities
Cost and Accessibility Despite their benefits, the high cost of smart pulse oximeters limits adoption, especially in developing regions. Manufacturers must address affordability to tap into these markets.
Growth in Telemedicine The rise of telemedicine presents a significant opportunity for smart pulse oximeters. By integrating with telehealth platforms, these devices enable remote patient monitoring, ensuring healthcare access even in rural or underserved areas.
Personalized Healthcare The integration of AI and predictive analytics in smart pulse oximeters opens doors for personalized healthcare solutions. These technologies can analyze trends and provide actionable health insights, improving user engagement and outcomes.
Conclusion The Smart Pulse Oximeters Market is poised for significant growth as consumers increasingly adopt wearable health technologies. With ongoing innovations and expanding applications, these devices are set to become a cornerstone of modern healthcare. For detailed market analysis, visit metatechinsights.com
Market Drivers and Innovations
Rising Demand for Health Monitoring The surge in chronic conditions like COPD, asthma, and sleep apnea has elevated the demand for smart pulse oximeters. These devices enable early detection of health issues, providing critical data that supports timely medical intervention.
Technological Advancements Modern smart pulse oximeters incorporate Bluetooth, Wi-Fi connectivity, and smartphone integration, making them highly convenient for continuous health tracking. Features like app-based analytics and cloud storage allow users to share data with healthcare providers seamlessly.
Post-Pandemic Health Awareness The COVID-19 pandemic highlighted the importance of tracking blood oxygen saturation (SpO2) levels, leading to widespread adoption of these devices for home use. This trend has persisted, with individuals increasingly prioritizing proactive health monitoring.
Challenges and Opportunities
Cost and Accessibility Despite their benefits, the high cost of smart pulse oximeters limits adoption, especially in developing regions. Manufacturers must address affordability to tap into these markets.
Growth in Telemedicine The rise of telemedicine presents a significant opportunity for smart pulse oximeters. By integrating with telehealth platforms, these devices enable remote patient monitoring, ensuring healthcare access even in rural or underserved areas.
Personalized Healthcare The integration of AI and predictive analytics in smart pulse oximeters opens doors for personalized healthcare solutions. These technologies can analyze trends and provide actionable health insights, improving user engagement and outcomes.
Conclusion The Smart Pulse Oximeters Market is poised for significant growth as consumers increasingly adopt wearable health technologies. With ongoing innovations and expanding applications, these devices are set to become a cornerstone of modern healthcare. For detailed market analysis, visit metatechinsights.com.
0 notes
Text
How Virtual Care is Reshaping Patient Engagement?

Telehealth Transformation
Telehealth has come to revolutionize the way patients engage with medical professionals. Indeed, through the digital platforms it employs, telehealth brings remote consultation closer, improves accessibility, and increases the control patients wield over their own care. As this technology matures, it not only addresses barriers in traditional healthcare delivery but also fosters deeper, more meaningful patient engagement.
The New Normal in Virtual Care
The COVID-19 pandemic accelerated telehealth adoption as healthcare providers transitioned to digital modes of delivering care to ensure that patients continue to receive uninterrupted care. The shift is here to stay, and telehealth has become an integral component of daily healthcare services. Telehealth utilization in the United States has remained at 38 times pre-COVID-19 levels, concluded a McKinsey report
Some key factors that have prompted this shift are:
Convenience: Access to virtual consultations from the comfort of their own homes saves time and costs.
Access to Specialist Care: Rural and underserved communities get access to specialists who are not commonly found in such facilities.
Personalized Care: Most virtual care platforms offer services such as tracking health metrics and tailored communication, enhancing patient care.
Improved Patient Engagement
The Empowered Patient
Telehealth platforms can engage patients in their care. Tools such as wearable devices, mobile apps, and patient portals give them actual-time health data that will help them make informed decisions about their healthcare. For example, chronic disease patients can check their vital signs and report them to doctors remotely, creating a teamwork approach.
Better Communication
Virtual care bridges communication gaps between patients and providers. Features like video consultations, instant messaging, and follow-up notifications ensure ongoing dialogue. A study in Telemedicine and e-Health found that virtual consultations often result in higher patient satisfaction due to increased communication and convenience.
Culturally Competent Care
Telehealth services can also offer multilingual services, making healthcare more accessible and inclusive. Access to treatment in a preferred language enhances understanding and adherence to the medication advice.
Technological Innovations Driving Engagement
Artificial Intelligence
Chatbots and virtual assistants powered by AI enable telehealth systems to provide immediate answers to patient queries, schedule appointments, and educate patients on health. For instance, Babylon Health has used AI for symptom triaging while directing patients to proper pathways for receiving care.
RPM
RPM devices, like glucometers and blood pressure monitors, allow patients to track their health metrics constantly. These devices alert healthcare providers of possible issues and keep patients engaged with their health.
Gamification in Health Apps
Gamification techniques, such as providing rewards for reaching fitness-related objectives or monitoring chronic conditions, can make healthcare exciting. Applications like MySugr for managing diabetes have gamified features to encourage adherence and usage.
Barriers to Telehealth Engagement
Digital Divide
The use of telehealth services is not uniform; rural people and low-income populations generally lack internet access infrastructure or the proper skills in using the web. This gap needs considerable investments in broadband access and digital education.
Security of Data
The rapid uptake of telehealth reveals issues regarding data privacy and security. To maintain patients’ trust, the rules under HIPAA in the U.S. and the new GDPR in the EU must be adhered to.
Provider Adaptation
Healthcare providers will not all be comfortable with the use of telehealth. Training programs and user-friendly platforms help facilitate rapid uptake.
Telehealth in the Future-Creating a New Era for Patient Engagement
This development in telehealth further emphasizes an integrated model that incorporates virtual and physical patient care for better outcomes. Evolving trends include:
Integrated Ecosystems: Platforms that integrate telehealth, EHRs, and RPM will streamline care delivery and data sharing.
Increased Utilization of AR/VR: Augmented and virtual reality tools are being increasingly used in remote rehabilitation and therapy sessions as a mode to enhance engaging behaviour among patients.
Focus on Preventive Care: Telehealth has been shifting its focus toward preventive care, using analytics to identify risks early and intervene. Conclusion
Know More: https://medtechreviewmagazine.com/how-virtual-care-is-reshaping-patient-engagement/
#TransformingRemoteHealthcareandTelemedicine#MedTechReviewMagazine#LeadingMedicalandHealthcareMagazines#VirtualCare#VirtualCareisReshaping#PatientEngagement
0 notes
Text
The Role of Visitor Management Systems in Healthcare Facilities
Healthcare facilities are often bustling hubs of activity, welcoming patients, staff, and visitors daily. However, with the importance of security, patient privacy, and overall operational efficiency, managing visitors effectively becomes crucial. Visitor management systems (VMS) play a pivotal role in enhancing the safety, efficiency, and organization of healthcare environments. These systems help healthcare facilities monitor and control who enters and exits their premises, improving the overall patient and staff experience while maintaining high levels of security.

In this article, we will explore how visitor management systems are transforming healthcare facilities and why they are indispensable in ensuring a safe, secure, and streamlined environment.
1. Improved Security and Access Control
One of the primary concerns of healthcare facilities is ensuring that only authorized individuals gain access to certain areas. With the increasing risks of unauthorized access, including potential threats or the spread of infectious diseases, the need for controlled access has become more urgent.
Visitor management systems, particularly those that integrate with access control solutions, help healthcare organizations track, monitor, and regulate access to different parts of the facility. Upon arrival, visitors are typically required to sign in through a digital kiosk or mobile app, providing relevant details such as their name, purpose of visit, and the person they are visiting. The system can then issue a visitor badge that grants access to specific areas within the facility, limiting their movement to authorized spaces.
This system of controlled access ensures that healthcare workers and patients are protected from unwanted interactions, and sensitive areas like treatment rooms, operating theaters, or administrative offices remain secure.
2. Streamlined Check-in Process
Gone are the days of manual sign-in sheets or lengthy paper-based visitor logs, which can cause delays and are prone to errors. Visitor management systems allow healthcare facilities to streamline the check-in process, making it faster and more efficient.
By using digital check-in kiosks or smartphone apps, visitors can sign in within seconds, providing their identification and any necessary health-related details such as vaccination status or COVID-19 screenings. This approach reduces wait times and ensures that patient care can proceed without disruption, as staff do not need to spend valuable time managing visitor check-ins.
Moreover, these systems can automatically notify the relevant department or individual when their visitor arrives, saving time and ensuring smoother transitions between departments.
3. Enhanced Visitor Experience
A well-implemented visitor management system does more than just secure the premises; it also helps improve the overall visitor experience. Long wait times, confusing directions, and lack of information can add unnecessary stress for those coming to healthcare facilities, especially in emergency situations.
Visitor management systems can improve the visitor experience by offering real-time information through user-friendly interfaces. Visitors can be greeted with digital displays showing clear instructions, directions, or even information about available amenities. Additionally, many systems offer multilingual support, making it easier for non-native speakers to navigate the healthcare facility.
Some visitor management platforms even allow family members or friends to schedule visits, receive notifications, and track the status of patient visits. By removing barriers and reducing confusion, these systems enhance the comfort of visitors while promoting a more positive atmosphere in what can often be a stressful environment.
4. Compliance with Health and Safety Regulations
In recent years, health and safety regulations have become increasingly stringent, particularly in healthcare settings. Compliance with these regulations is essential to prevent the spread of infections and safeguard both patients and staff. One area where visitor management systems shine is their ability to integrate health and safety checks directly into the visitor sign-in process.
For example, healthcare facilities can collect health screening data from visitors as part of the sign-in process, ensuring that visitors comply with necessary health checks before entering the facility. Systems can be configured to require visitors to answer questions related to symptoms, recent travel, or exposure to infectious diseases, and some can even integrate with health apps to verify vaccination statuses.
In the event of an outbreak or other health emergency, visitor management systems provide a comprehensive, auditable log of who has entered the facility, which can help healthcare organizations trace contacts quickly and effectively.
5. Reduced Administrative Workload
The manual tracking of visitors can create significant administrative burden for healthcare staff, especially when large numbers of people need to be managed daily. Staff members must verify visitor credentials, track visitor movements, and keep paper logs, all of which are time-consuming and inefficient.
Automating the visitor check-in process with a VMS significantly reduces administrative workload by eliminating paper-based systems and minimizing human error. With digital records, healthcare administrators can easily pull up visitor logs, which are organized, searchable, and stored securely for future reference. This reduces the chances of mistakes, such as missed visitors or incorrect data entry, and allows staff to focus on more critical tasks, like patient care.
Additionally, the system can send automated notifications to the relevant parties when visitors arrive, enabling faster responses and better coordination between departments. This improves the overall flow of the healthcare facility and helps maintain optimal staff productivity.
6. Real-Time Monitoring and Reporting
In large healthcare facilities, tracking the movement of visitors can be a logistical challenge. However, real-time monitoring provided by visitor management systems ensures that healthcare administrators can see where visitors are at any given moment. This provides peace of mind and allows for more accurate oversight of visitor traffic within the premises.
If needed, healthcare facilities can also generate real-time reports detailing visitor activity, including arrival times, durations of visits, and specific areas visited. This data can be used for various purposes, such as optimizing the flow of people within the building or assessing the efficiency of the visitor management process. Reports can also be invaluable when auditing visitor activity for compliance or security purposes.
Conclusion
In an era where healthcare facilities are under increasing pressure to provide a high standard of care while also maintaining a safe and secure environment, visitor management systems are proving to be an indispensable tool. From improving security and compliance with health regulations to streamlining operations and enhancing the visitor experience, these systems provide a wide range of benefits that can significantly improve the functioning of healthcare facilities.
As the demand for contactless solutions and digital security continues to rise, healthcare organizations that embrace modern visitor management systems will find themselves better equipped to handle the challenges of today and tomorrow. For businesses looking to implement advanced and reliable visitor management systems, exploring innovative platforms like Spintly in the access control and security space can offer solutions that meet both operational needs and security standards.
Incorporating such systems helps healthcare organizations create a safer, more efficient environment for both visitors and staff, contributing to overall satisfaction and enhanced care delivery.
#visitor management system#spintly#accesscontrol#mobile access#access control system#biometrics#access control solutions#smartacess#smartbuilding
0 notes
Text
Telemedicine market: $87.6B in 2023 to $380.3B by 2033, CAGR: 15.8%.
Telemedicine Market : Telemedicine is revolutionizing healthcare by offering patients the ability to consult with doctors remotely, eliminating the need for in-person visits. Through secure video calls, phone consultations, and online messaging, telemedicine allows for convenient access to healthcare services, especially in rural or underserved areas where medical professionals are scarce. This innovative approach not only saves time for patients but also reduces the burden on healthcare facilities. With its ability to provide medical advice, prescription refills, mental health support, and follow-up care, telemedicine is making healthcare more accessible, efficient, and cost-effective for everyone.
To Request Sample Report : https://www.globalinsightservices.com/request-sample/?id=GIS10073 &utm_source=SnehaPatil&utm_medium=Article
As technology advances, telemedicine is expanding to include virtual health monitoring, AI-driven diagnostics, and even remote surgeries. With wearable devices and apps that track vital signs, telemedicine is becoming a crucial tool for managing chronic conditions and improving preventive care. The COVID-19 pandemic accelerated the adoption of telemedicine, and it’s now becoming a permanent fixture in modern healthcare systems worldwide. With ongoing improvements in cybersecurity, patient education, and digital infrastructure, telemedicine is paving the way for a healthier and more connected future in healthcare.#Telemedicine #RemoteHealthcare #VirtualCare #HealthTech #DigitalHealth #EHealth #Telehealth #RemoteConsultation #HealthcareInnovation #AccessToCare #VirtualMedicine #MedicalTechnology #HealthcareRevolution #PreventiveCare #HealthMonitoring
0 notes
Text
HEALTHAYST
A patient check in system is an application or tool designed to streamline the process of patients arriving at a medical facility. It simplifies and automates the check-in, making it easier for both patients and staff to handle information efficiently. Here’s a basic overview of a typical patient intake software system:
Key Features of a Patient Check-In System
Patient Identification:
Verifies patient check in systems identity, often using ID cards, QR codes, or biometrics (like fingerprints or facial recognition).
Allows returning patients to check in more quickly using stored information.
Appointment Verification:
Confirms upcoming appointments or schedules new ones.
Provides reminders and notifications for appointments (via text, email, or app notifications).
Data Collection:
Collects patient information (address, contact info, insurance details).
Gathers health history or updates current records.
Allows patients to update forms and documentation online before arriving.
Insurance Verification and Billing:
Checks insurance coverage for treatments and procedures.
Allows upfront payment or estimates for upcoming services, reducing waiting times.
Wait-Time Management:
Displays estimated wait times on a screen or mobile device.
Allows patients to join a virtual queue and monitor their position.
Self-Check-In Kiosk (optional):
Provides on-site kiosks where patients can enter information or scan ID to check in independently.
Reduces waiting lines and paperwork at the front desk.
COVID-19 Screening:
Many systems now include health questionnaires to screen for symptoms.
Some integrate temperature checks or symptom screening for added safety.
Integration with EHR (Electronic Health Record) Systems:
Synchronizes patient data with medical records.
Provides medical staff immediate access to updated records.
Notification and Communication:
Sends automatic reminders for follow-ups, prescriptions, or upcoming visits.
Allows patients to communicate any delays or changes.
Feedback and Satisfaction Tracking:
Gathers feedback through surveys post-appointment.
Helps facilities improve service based on real patient experiences.
Types of Check-In Systems
Web-Based and Mobile Apps:
Patients check in from home or mobile devices.
On-Site Kiosks:
Allows quick check-in at the facility.
Staff-Assisted:
Traditional model with digital support for faster processing.
Benefits
Efficiency: Faster check-ins, less waiting, and streamlined paperwork.
Patient Satisfaction: Patients appreciate convenience and reduced wait times.
Data Accuracy: Minimizes errors in patient information entry.
Improved Workflow: Staff focus more on patient care rather than administrative tasks.
Implementation Considerations
Privacy and Security: Ensure compliance with HIPAA or relevant privacy laws.
Ease of Use: Make sure it's user-friendly, especially for older or less tech-savvy patients.
Integration: Compatibility with existing EHR or billing systems
A digital patient check-in system streamlines the arrival and intake process at healthcare facilities, allowing patients to check in through electronic devices such as kiosks, tablets, or their own mobile phones. This modern approach simplifies data entry, reduces waiting times, and improves the overall patient experience. Here’s an in-depth look at a digital check-in system and how it benefits both patients and healthcare providers:
Core Features of a Digital Patient Check-In System
Mobile Check-In:
Allows patients to check in through a mobile app or website before arriving at the facility.
Patients can complete forms, verify insurance, and update personal information from their own devices.
Kiosk or Tablet Check-In:
In-office kiosks or tablets let patients check in upon arrival by entering personal information or scanning a code.
This feature helps streamline the process and reduces the need for front desk staff to handle every step.
QR Code and Barcode Scanning:
Patients receive a unique code in their appointment confirmation, which they can scan to check in immediately upon arrival.
Minimizes contact and further reduces waiting time.
Real-Time Insurance Verification:
Verifies insurance eligibility and coverage for upcoming services.
Enables upfront payments or co-pay collection, improving the efficiency of the billing process.
Patient Data Collection and Update:
Allows patients to confirm or update personal information, medical history, and current symptoms.
Simplifies the updating of essential records and reduces errors in data entry.
E-Signature for Consent Forms:
Patients can sign consent forms and other necessary documents digitally.
Ensures compliance with legal requirements while eliminating paper-based records.
Appointment and Wait-Time Management:
Provides estimated wait times or alerts patients when it’s their turn.
Reduces congestion in waiting rooms, improving patient financial engagement software flow and satisfaction.
Symptom and Health Screening:
Collects pre-appointment health information, including COVID-19 or other specific screenings.
Ensures safety and preparedness by identifying any additional needs prior to consultation.
Integration with EHR and Billing Systems:
Syncs with Electronic Health Record (EHR) and practice management software for seamless data access.
Ensures that all relevant patient information is up-to-date and readily accessible to providers.
Multi-Language Support:
Offers check-in options in multiple languages to accommodate diverse patient populations.
Enhances accessibility and ensures better comprehension for non-English speakers.
Benefits of a Digital Patient Check-In System
Increased Efficiency: Speeds up the check-in process and frees up front desk staff for other tasks.
Improved Patient Experience: Patients appreciate the ease and speed of digital check-ins, as well as reduced time spent in waiting areas.
Enhanced Data Accuracy: Reduces errors associated with manual data entry, as patients enter their own information directly.
Greater Privacy and Security: Many digital systems are HIPAA-compliant, ensuring that patient data is securely handled and stored.
Reduced Administrative Costs: Digital systems decrease the need for paper forms and physical storage, leading to long-term savings.
Scalable for Different Practice Sizes: Digital check-in systems can be scaled up or down depending on the needs of the facility, from small practices to large hospitals.
Types of Digital Patient Check-In Solutions
Web-Based Solutions:
Patients can access the check-in system via a website link or patient portal.
Ideal for remote check-ins and can be used on any internet-enabled device.
Mobile Apps:
A dedicated app allows patients to check in, schedule appointments, receive reminders, and complete forms.
Enhances patient engagement and encourages repeat visits by improving convenience.
In-House Kiosks:
Patients can check in upon arrival at a physical kiosk or tablet station.
Useful for practices with high foot traffic, as it allows for faster patient processing.
Considerations for Implementing a Digital Check-In System
HIPAA Compliance: Ensure the system adheres to HIPAA standards to protect patient privacy and data security.
User-Friendly Interface: Choose an intuitive and easy-to-navigate system for patients of all ages and tech abilities.
Customization Options: Ensure the system allows for customizable forms, fields, and check-in workflows to match practice requirements.
Integration Capabilities: Opt for a system that integrates with your EHR, billing, and appointment scheduling software.
Technical Support and Training: Choose a patient engagement software vendorsthat offers comprehensive support, training, and troubleshooting for seamless implementation.
Popular digital patient check in Software Options
Phreesia: Known for its extensive features, including digital forms, insurance verification, and integration with various EHR systems.
Solutionreach: Offers check-in, reminders, and two-way communication between patients and healthcare providers.
Kareo: A versatile option for smaller practices with features for intake, scheduling, and EHR integration.
ModMed: Specializes in digital check-ins and telehealth services for specialty practices, particularly dermatology and orthopedics.
Clearwave: Provides streamlined digital check-in solutions with a focus on patient self-service and multi-site practices.
A digital check-in system can significantly improve operational efficiency, streamline administrative tasks, and enhance the overall patient experience. If you’re considering implementing a system, I can provide more specific recommendations based on the needs of your practice.
An electronic patient check-in system digitizes the process of patient arrival and data entry at healthcare facilities, streamlining check-ins and improving the flow of information. This approach has become popular for its efficiency, ease of use, and ability to integrate seamlessly with Electronic Health Records (EHR) and billing systems. Here’s a breakdown of electronic patient check-in systems, their features, and their benefits:
Key Features of an Electronic Patient Check-In System
Self-Service Check-In:
Patients can check in themselves at kiosks or on their mobile devices, entering or verifying their information directly.
Reduces the need for front desk involvement, speeding up the process.
Mobile and Web Check-In Options:
Patients can check in remotely via a mobile app or a secure web link before arriving.
Reduces wait times and allows for better planning of patient flow in the office.
Pre-Appointment Form Completion:
Patients fill out medical histories, consent forms, and other necessary documents before arrival.
Ensures records are updated and readily available for the healthcare provider.
Insurance Verification and Co-Pay Collection:
Checks insurance eligibility and allows co-pays to be collected electronically, either before or at the time of check-in.
Reduces back-office work and minimizes billing delays.
Symptom and Health Screening:
Customizable health questionnaires can collect symptom information or screen for specific conditions (e.g., COVID-19).
Allows for safer, more efficient triage and prepares providers in advance.
E-Signature for Consent and Compliance:
Collects electronic signatures for required documents such as consent, privacy policies, and financial agreements.
Provides legal compliance with fewer paper forms.
Appointment and Queue Management:
Patients receive estimated wait times and updates about their position in the queue.
Helps manage patient flow and reduces overcrowding in waiting areas.
Data Synchronization with EHR and PMS:
Automatically updates the Electronic Health Record (EHR) and Practice Management System (PMS) with patient data.
Provides clinicians with real-time access to updated patient information.
Multi-Language Support:
Supports multiple languages, enhancing accessibility for diverse patient populations.
Improves patient experience and comprehension for non-native speakers.
Compliance with Privacy Regulations:
Ensures secure storage and transmission of patient data in line with HIPAA and other regulatory standards.
Incorporates data encryption, secure logins, and limited access to sensitive information.
Types of Electronic Patient Check-In Systems
Mobile-Based Check-In:
Patients use a mobile app or a web portal for check-in, typically linked to the healthcare provider’s system.
Allows remote check-in and form completion before arrival, reducing in-office wait times.
Kiosk-Based Check-In:
Patients use an on-site kiosk or tablet, scanning an ID or entering their details upon arrival.
Ideal for facilities with high patient volumes, as it automates the intake process and minimizes front desk tasks.
Hybrid Systems:
Combines mobile and kiosk options, giving patients flexibility to check in remotely or upon arrival.
Offers a more comprehensive solution for practices of varying sizes.
Benefits of an Electronic Patient Check-In System
Streamlined Operations: Reduces paperwork and administrative tasks, allowing staff to focus on patient care.
Enhanced Patient Experience: Improves convenience and reduces waiting times, leading to greater patient satisfaction.
Improved Data Accuracy: Direct patient entry of data minimizes the risk of errors and reduces redundancies.
Secure and Compliant: Ensures that sensitive patient information is securely managed, stored, and accessed.
Reduced Costs: Minimizes the need for paper forms, filing, and physical storage, saving on materials and time.
Scalability: These systems can scale to fit the needs of small practices, large hospitals, or multi-site facilities.
Popular Electronic Patient Check-In Solutions
: Known for robust self-service capabilities, Phreesia offers tools for patient check-in, payment processing, and data integration with EHRs.
IntakeQ: Offers HIPAA-compliant forms, online check-in, and secure data handling, making it popular with small to mid-sized practices.
SimplePractice: A versatile patient intake management software option with electronic check-in, telehealth integration, and EHR features tailored for smaller practices.
Kareo: Provides all-in-one features that include patient check-in, billing, and EHR integration, suitable for smaller healthcare providers.
Clearwave: Specializes in self-service check-in and patient engagement software for larger, multi-location practices, helping to streamline high patient volumes.
Considerations for Implementing an Electronic Check-In System
User Friendliness: Ensure the system is intuitive and accessible for all patient demographics, including those who may not be tech-savvy.
Compatibility with Existing Systems: Choose software that integrates smoothly with your current EHR, billing, and appointment scheduling systems.
Compliance with Privacy and Security Standards: Verify that the system complies with HIPAA and other relevant privacy laws.
Customization: Look for a system that allows form customization, language options, and configurable check-in workflows.
Technical Support and Training: A good vendor should offer comprehensive support, training, and resources to help both patients and staff.
Automated patient intake systems digitize and streamline the entire process of gathering patient information, verifying insurance,
e steps, healthcare practices can improve efficiency, accuracy, and patient satisfaction, allowing patients to complete intake tasks on their own time, from any location, using web-based or mobile solutions.
A patient intake system streamlines the process of gathering and managing patient information before an appointment, typically using digital tools to enhance efficiency, data accuracy, and the overall patient experience. This type of system is especially useful for reducing paperwork, shortening wait times, and improving the accuracy of medical records by allowing patients to input data directly. Here’s an overview of the core features, benefits, and types of patient intake systems:
A patient check in app digitizes the arrival automated patient check in system process at healthcare facilities, allowing patients to check in, complete forms, verify insurance, and even make payments from their mobile device. These best patient intake softwareautomated patient check in system apps streamline the patient intake process, improve data accuracy, reduce wait times, and enhance the overall patient experience. Here’s a closer look at the features, benefits, and considerations for implementing a patient check-in app:
An automated patient check-in system streamlines the check-in process by using technology to handle routine administrative tasks, enabling patients to check in efficiently with minimal staff intervention. This type of system improves patient flow, reduces wait times, enhances data accuracy, and provides a more convenient experience for patients and staff alike.
There are several highly-regarded patient intake software for patient engagement options available, each offering unique features designed to improve the efficiency and effectiveness of the patient intake medical check in software process. Here are some of the best patient check in systems software solutions, highlighting their strengths and the types of healthcare practices they best serve:
Medical check-in software is designed to streamline the patient arrival process in healthcare facilities by automating tasks like form completion, insurance verification, and payments. These systems improve automated patient check in flow, reduce waiting times, enhance data accuracy, and allow staff to focus more on patient care rather than administrative tasks. Here are some of the top medical check-in software solutions, including their key features, benefits, and ideal practice settings:
Medical check-in best patient engagement software is designed to streamline the patient arrival process in healthcare facilities by automating tasks like form completion, insurance verification, and payments. These systems improve patient self check in flow, reduce waiting times, enhance data accuracy, and allow staff to focus more on patient care rather than administrative tasks. Here are some of the top medical check-in software solutions, including their key features, benefits, and ideal practice settings:
what is patient engagement software
Online patient intake software allows healthcare practices to collect patient self check in system information digitally before or during their visit. This can be done through web portals, mobile apps, or email links, helping to streamline the intake process. online patient intake software intake software typically includes forms for personal, medical, and insurance details, as well as features for e-signatures, consent collection, insurance verification, and payment processing. It’s particularly beneficial for reducing paperwork, enhancing patient experience, and improving data accura
Patient intake management software is designed to help healthcare practices streamline and automate the intake process, from the moment a patient schedules an appointment to when they complete all necessary forms, verify their insurance, and make payments. This type of urgent care patient engagement software typically includes features such as customizable forms, e-signatures, insurance verification, patient communications, and integration with EHR/Practice Management systems.
Patient intake management software is designed to help healthcare practices streamline and automate the intake process, from the moment a patient schedules patient engagement software pricing an appointment to when they complete all necessary forms, verify their insurance, and make payments. This type of software typically includes features such as customizable forms, e-signatures, insurance verification, patient communications, and integration with EHR/Practice Management systems.
patient payment software refers to digital patient engagement software check in tools and platforms designed to enhance communication, interaction, and overall involvement of patients in their healthcare journey. These patient engagement software solution focus on improving the patient experience by offering features such as appointment scheduling, reminders, telemedicine, patient engagement software companies education, and personalized care plans, while fostering stronger relationships between patients and providers. Engaging patients throughout their healthcare process can lead to better outcomes, improved patient satisfaction, and more efficient practice operations.
Hospital patient payment software is designed to streamline the process of collecting electronic patient check in, reducing administrative overhead, and improving revenue cycle management. These dental patient engagement software systems can handle everything from co-pays and patient engagement software solutions deductibles to patient balances and insurance claims, making it easier for hospitals to process payments, improve cash flow, and enhance the patient experience.
Integrated patient payment software refers to systems that seamlessly connect with a healthcare provider's existing EHR (Electronic Health Record), EMR (Electronic Medical Record), practice management software, and revenue cycle management (RCM) tools to streamline the entire billing and payment process. These systems automate the patient payment experience, allowing for real-time tracking of patient balances, offering online payment portals, and integrating billing information into clinical trial patient engagement software workflows. The integration ensures smooth data flow between clinical, administrative, and financial departments, improving operational efficiency and patient satisfaction.
Automated patient payment software is designed to simplify and streamline the entire billing and payment process for healthcare providers and patients. These platforms automate various aspects of the payment cycle, including sending payment reminders, processing online payments, offering payment plans, and integrating seamlessly with Electronic Health Record (EHR) and Revenue Cycle Management (RCM) systems. The goal is to reduce administrative burden, accelerate payment collections, and enhance the patient experience by providing an easy and efficient way to manage their medical bills.
0 notes
Text
Discover the Latest in Orthodontics at Avenue Dentistry

Discover the Latest in Orthodontics at Avenue Dentistry
We at Morgan Hill's Avenue Dentistry are committed to giving our patients the newest developments in orthodontic treatment. With the introduction of cutting-edge technologies and Premium Dentist in Morgan Hill alternatives that improve patient outcomes and experience, the orthodontics industry is expanding quickly. The most important developments in braces and alignment technology will be discussed in this blog, with an emphasis on how these developments benefit our patients' comfort, effectiveness, and appearance.
1. Clear Aligners: The Discrete Choice
By providing an almost undetectable substitute for conventional metal braces, clear aligners have completely transformed orthodontic therapy. Without the need of brackets or wires, these specially designed trays gently move teeth into the appropriate positions. Better materials that increase comfort and efficacy have been made possible by recent developments in aligner technology. More precise tooth movement predictions are now possible because to improved software algorithms, which enable individualized treatment programs that meet each patient's demands.
2. Digital Impressions and 3D Printing
The days of unpleasant dental molds are over. High-resolution 3D pictures of a patient's teeth and jaw are produced by digital impressions taken with intraoral scanners, guaranteeing accurate diagnosis and treatment planning. By doing away with the clutter that comes with taking traditional impressions, this technique not only increases accuracy but also improves patient comfort.
The quick creation of personalized braces and aligners made possible by 3D printing has further revolutionized orthodontics. This technology makes it possible to create complex designs that are customized to the particular dental anatomy of each patient, greatly cutting down on appliance waiting times and increasing treatment effectiveness overall.
3. Smart Braces: Real-Time Monitoring
The development of smart braces marks a substantial advancement in orthodontic technology. These cutting-edge gadgets have sensors that track tooth movement in real time. When smart braces are linked to a smartphone app, they can instantly update orthodontists on progress, facilitating prompt changes and minimizing the need for frequent office visits. In addition to improving patient engagement, this interactive strategy guarantees that treatments continue as planned.
4. Tele Orthodontics: Convenient Care
The use of tele orthodontics has grown, particularly since the COVID-19 epidemic. Through virtual appointments, this method enables patients to consult with their orthodontists at a distance. Orthodontists can track development without frequent in-person appointments by having patients submit pictures of their teeth from home. By making care more accessible, tele orthodontics helps busy people stick to their treatment regimens.
5. Accelerated Orthodontics: Faster Results
The need for faster orthodontic results has prompted the creation of accelerated orthodontic treatments that move teeth more quickly without sacrificing efficacy. High-frequency vibrations (HFV) are one technique that has showed promise in speeding up the bone remodeling around teeth, which could shorten treatment periods overall. Thanks to these developments, patients can now get the results they want more quickly than they could with conventional techniques.
6. Self-Ligating Braces
Self-ligating braces are growing in popularity because they are comfortable and effective. Self-ligating braces use a unique clip mechanism that lessens pressure and friction on teeth, in contrast to standard braces that use elastic bands to hold the archwire in place. Patients will find this design to be more convenient overall because it permits less adjustments and shorter appointment periods.
7. Advanced Orthodontic Appliances
Treatment options for complicated situations are being improved by advancements in orthodontic appliances. By giving orthodontists extra points of support for tooth movement, Temporary Anchorage Devices (TADs) enable more effective malocclusion repairs without depending entirely on patient compliance with detachable equipment like headgear.
Furthermore, lingual braces—which are affixed to the back of the teeth—keep developing with new designs that provide patients looking for discrete treatment alternatives with increased comfort and beauty.
8. Personalized Treatment Plans
Orthodontics also exhibits the trend toward individualized medicine. Orthodontists may produce incredibly detailed images of a patient's dental structure using sophisticated diagnostic equipment like Cone Beam Computed Tomography (CBCT), which helps them make more precise diagnoses and develop individualized treatment plans. We can guarantee the best results by taking into account the distinct anatomy and requirements of every patient.
9. Patient-Centered Care
At Avenue Dentistry, we put the needs of our patients first by emphasizing their comfort, contentment, and involvement during the course of treatment. By talking through choices and answering any worries they may have, we actively involve our patients in the planning of their therapy. We enable our patients to actively participate in their dental health journey by encouraging open communication and educating them about their available treatment options.
Conclusion
Thanks to technological developments that improve patient care at Avenue Dentistry in Morgan Hill, the orthodontics industry is undergoing tremendous change. These advancements, which range from digital impressions and transparent aligners to smart braces and tele orthodontics, are making treatments more effective, pleasant, and widely available than in the past.
Get in touch with us right now if you're thinking about getting orthodontic treatment or if you have inquiries about the newest developments in braces and alignment technology! Our committed staff is here to use cutting-edge methods customized specifically for you to help you attain a gorgeous smile! This is where your path to the best possible oral health begins!
0 notes
Text
How RF Antennas are Used in Healthcare: Telemedicine and Beyond
The healthcare business is undergoing a technological transition, and RF (Radio Frequency) antennas play an important role in this revolution. RF antennas are essential in modern healthcare for enabling telemedicine and remote patient monitoring, as well as powering IoT medical equipment and wireless imaging systems. These antennas allow for seamless connection between devices, resulting in accurate and fast delivery of medical data.
In this article, we'll look at how RF antennas are utilized in healthcare, with a focus on telemedicine and other applications, as well as the advantages they provide to medical technology.
The Function of RF Antennas in Healthcare Communication Systems
RF antennas serve as the primary link between medical devices, healthcare practitioners, and patients. They provide wireless communication across several frequency bands, allowing devices to broadcast and receive data reliably. Some of their core roles include:
Data Transmission: Allows for wireless communication between devices such as ECG monitors, infusion pumps, and diagnostic equipment.
Remote monitoring enables real-time tracking of patient vitals, even in remote or rural locations.
IoT Integration: Providing smart medical devices and systems with smooth data sharing.
RF antennas have applications in healthcare, including telemedicine. Telemedicine has evolved as a critical component of modern healthcare, particularly following the COVID-19 pandemic. RF antennas power communication systems, which enable:
Video consultations: High-frequency antennas enable stable video conferencing between patients and doctors.
Remote Diagnostics: Sensors with built-in antennas capture and transmit critical data to healthcare providers.
Wearable Health Devices: Smartwatches with heart rate monitors use RF transmission to deliver health data to telemedicine platforms.
2. Remote patient monitoring (RPM). RPM employs RF antennas to continually monitor patients' vital indicators, including as heart rate, blood pressure, and glucose levels. These antennas ensure consistent data transfer from wearable sensors to healthcare systems, allowing for proactive care and lowering hospital readmissions.
3. Medical IoT devices. IoT in healthcare, often known as the Internet of Medical Things (IoMT), relies largely on RF antennas. Examples include:
Smart Pills: ingestible sensors with small antennas monitor medicine efficacy.
Connected Insulin Pens: Antennas send usage information to healthcare apps.
Hospitals employ RFID antennae to track medical equipment and supplies.
4. Wireless Imaging Systems. Advanced diagnostic instruments, such as MRIs, CT scans, and ultrasound devices, communicate wirelessly with control systems using RF antennas. This reduces the need for large wires while improving operational efficiency.
5. Implantable Medical Devices. Pacemakers and neurostimulators frequently use tiny antennas to interact with external monitoring systems. These antennas must be engineered to work safely within the human body.
6. Emergency Response Systems. In emergency situations, RF antennas enable wireless communication for ambulance telemetry, which sends patient data to hospitals in real time, allowing doctors to plan for the patient's arrival.
Advantages of RF Antennas in Healthcare:
Real-time Data Transmission RF antennas offer quick communication between medical devices and healthcare systems, allowing for faster decision-making.
Enhanced Mobility Wireless communication overcomes the limitations of wired systems, giving patients and healthcare practitioners greater mobility.
Improved patient outcomes. Continuous monitoring and proactive care enabled by RF antennas result in improved health outcomes.
Scalability and Flexibility Wireless technologies can be quickly scaled and adaptable to various healthcare situations without requiring significant infrastructure improvements.
Cost-effective solutions RF antennas reduce hospital visits and enable remote care, resulting in significant cost reductions for both patients and providers.
Challenges and Considerations
Interference Management In a hospital setting with many wireless devices, minimizing RF interference is critical to ensuring reliable connection.
Signal Security Sensitive medical information must be delivered securely to avoid unauthorized access.
Device Miniaturization Wearable and implantable device antennas must be small while still providing enough performance.
Regulatory Compliance RF antennas used in medical devices must meet stringent safety and electromagnetic compatibility standards.
Future of RF Antennas in Healthcare
As healthcare embraces digital transformation, the use of RF antennas will grow. Emerging technologies such as 5G, AI, and sophisticated IoT will expand the capabilities of medical devices, allowing:
URLLC is an ultra-reliable low-latency communication protocol for critical care applications. Smart hospitals feature completely networked gadgets and systems. AI-Driven Diagnostics using real-time data collected via RF antennas.
Conclusion
RF antennas are transforming healthcare by providing wireless connectivity for telemedicine, remote monitoring, IoT devices, and more. Their ability to ensure dependable, secure, and efficient data transfer is vital to the success of current medical devices.
At Eteily Technologies, we specialize in creating high-performance RF antennas for the healthcare and other industries. Whether you want antennas for wearable devices, telemedicine systems, or IoMT applications, we provide unique solutions adapted to your requirements. Contact us today to learn more about how we can help you advance your healthcare innovations!
0 notes
Text
The Role of Indian App Development Companies in Healthcare Digital Transformation
The healthcare industry has undergone a significant digital transformation in recent years, driven by the need to enhance patient care, streamline processes, and increase accessibility. A major player in this revolution has been the mobile app, which has become an essential tool for healthcare providers and patients alike.
Mobile app development companies in India have been at the forefront of this transformation, leveraging their expertise in technology to create innovative solutions that address the unique challenges of the healthcare sector.
In this blog, we explore the critical role that Indian app development firms play in reshaping healthcare through digital solutions.
1. Enhancing Patient Care with Custom Healthcare Apps
One of the most significant contributions of Indian app development companies to healthcare is the creation of custom apps that enhance patient care. These apps are designed to improve communication between patients and healthcare providers, allowing for better monitoring, timely interventions, and more personalised treatment plans.
For instance, Indian developers have created apps that allow patients to track their health metrics, such as blood pressure, glucose levels, and heart rate. This data can be shared in real-time with doctors, enabling them to make informed decisions and provide timely feedback. Such innovations have proven invaluable, especially for managing chronic conditions like diabetes and hypertension, where continuous monitoring is crucial.
Indian app developers have also focused on creating apps for remote patient monitoring (RPM). These apps collect data from wearable devices and home health equipment, sending it to healthcare providers who can monitor patient conditions from afar. This not only enhances patient care but also reduces the need for frequent hospital visits, making healthcare more accessible and convenient.
2. Driving the Growth of Telemedicine Solutions
Telemedicine has emerged as a game-changer in healthcare, particularly during the COVID-19 pandemic when in-person visits were restricted. Indian app development companies have played a vital role in this surge by developing secure and user-friendly telemedicine platforms. These apps allow patients to consult doctors remotely through video calls, chat, or voice calls, making healthcare services more accessible, especially in rural and underserved areas.
Telemedicine apps developed by Indian firms often feature integrated appointment scheduling, electronic medical records (EMR), and secure payment gateways, providing a seamless experience for both patients and healthcare providers. By reducing the need for physical consultations, these apps have helped decongest healthcare facilities and offer timely care to patients who might otherwise have limited access to medical services.
Furthermore, Indian developers have been proactive in incorporating features such as AI-driven chatbots for initial patient assessment and symptom checking, which can help triage patients effectively before a doctor’s consultation. This innovation enhances the efficiency of telemedicine platforms, allowing healthcare providers to focus on patients who require immediate attention.
3. Improving Healthcare Accessibility through mHealth Apps
Mobile health (mHealth) apps have become a cornerstone of healthcare accessibility, and Indian app development companies are leading the charge in creating solutions that cater to a diverse range of healthcare needs. These apps cover various aspects of healthcare, from fitness tracking and mental health support to medication reminders and appointment booking.
Indian developers have a deep understanding of the challenges faced in healthcare accessibility, particularly in rural and remote areas. As a result, they have created mHealth apps that provide educational resources, medication reminders, and basic health assessments, all of which can be accessed with limited internet connectivity. This focus on inclusivity ensures that even those with limited access to healthcare facilities can benefit from digital healthcare solutions.
Additionally, Indian app development firms are integrating regional language support in mHealth apps, breaking down language barriers and ensuring that users from different linguistic backgrounds can easily use the apps. This approach helps reach a broader audience, enhancing the overall impact of digital healthcare solutions.
4. Fostering Innovation with AI and Data Analytics in Healthcare Apps
Indian app development companies are increasingly incorporating artificial intelligence (AI) and data analytics into healthcare apps to drive innovation and improve patient outcomes. AI-powered apps can analyse patient data to predict potential health issues, recommend preventive measures, and provide personalised health advice. For instance, AI algorithms can identify patterns in patient symptoms and provide early warnings for conditions like heart disease or stroke.
Data analytics also plays a critical role in enhancing the functionality of healthcare apps. By analysing patient data, Indian developers can create insights that help healthcare providers tailor treatment plans, improve patient engagement, and optimise resource allocation. This data-driven approach not only enhances patient care but also contributes to more efficient healthcare delivery.
Mobile app development company in India are at the forefront of the healthcare digital transformation, creating innovative solutions that enhance patient care, expand the reach of telemedicine, and improve healthcare accessibility. Their expertise in developing custom healthcare apps, telemedicine platforms, and mHealth solutions is reshaping the industry, and making healthcare services more efficient, accessible, and patient-centric.
#mobile app development#mobile app development company in india#app development#mobile app development company
0 notes
Text
The Connected Drug Delivery Devices Industry: Transforming Patient-Centric Healthcare
The healthcare industry is undergoing a technological transformation, and connected drug delivery devices are at the forefront of this evolution. These smart devices, equipped with connectivity features such as Bluetooth, IoT (Internet of Things), and mobile applications, are revolutionizing the way medications are administered, monitored, and managed. By improving adherence, optimizing treatment outcomes, and enabling real-time data sharing, connected drug delivery devices are redefining patient care and healthcare systems globally.
The connected drug delivery devices market, valued at USD 1.18 billion in 2024, is projected to grow to USD 5.30 billion by 2029, expanding at a compound annual growth rate (CAGR) of 35.13% during the forecast period (2024–2029).
What Are Connected Drug Delivery Devices?
Connected drug delivery devices integrate technology with traditional drug administration tools like inhalers, auto-injectors, syringes, and infusion pumps. These devices collect and transmit real-time data on medication usage, dosage, and adherence via digital platforms, mobile applications, or cloud systems. Designed to enhance patient monitoring, they empower both healthcare providers and patients with actionable insights to optimize treatment.
For chronic diseases such as diabetes, asthma, and autoimmune conditions, where adherence to medication regimens is critical, connected drug delivery devices offer an innovative solution to streamline patient engagement and improve therapy outcomes.
Key Factors Driving the Growth of Connected Drug Delivery Devices
1. Rising Prevalence of Chronic Diseases
The growing burden of chronic diseases such as diabetes, respiratory disorders, and cardiovascular conditions has amplified the need for more effective drug administration and monitoring solutions. Patients managing long-term conditions often struggle with medication adherence, which can lead to poor outcomes. Connected devices provide reminders, real-time feedback, and data reporting to ensure patients stick to their treatment plans.
2. Increasing Focus on Patient-Centric Care
The healthcare industry is shifting toward patient-centric care, where technology plays a central role in empowering patients. Connected drug delivery devices put patients in control by providing feedback on their medication usage, tracking progress, and offering personalized insights. This approach improves engagement and outcomes while reducing the burden on healthcare providers.
3. Advancements in Digital Health and IoT
Technological advancements in IoT, sensor technology, and data analytics have enabled the development of smart drug delivery devices. These devices seamlessly connect to mobile apps, healthcare platforms, and electronic health records (EHRs), ensuring that healthcare providers can remotely monitor and intervene when necessary.
4. Growing Adoption of Telemedicine and Remote Monitoring
Telemedicine has become an integral part of healthcare delivery, especially in the wake of the COVID-19 pandemic. Connected drug delivery devices complement telehealth platforms by enabling remote monitoring of medication adherence and patient progress, reducing the need for in-person visits while ensuring continuity of care.
5. Regulatory Push for Digital Healthcare Solutions
Governments and regulatory bodies are actively promoting digital healthcare solutions, recognizing their role in improving patient outcomes and reducing healthcare costs. Regulatory support for connected devices, especially in regions like North America and Europe, is driving their adoption across healthcare systems.
6. Need for Better Medication Adherence
Medication non-adherence is a significant challenge in healthcare, leading to worsening health outcomes and increased costs. Connected devices address this issue by sending reminders, tracking usage, and alerting healthcare providers if adherence declines, ensuring patients follow their prescribed treatment regimens.
Challenges in the Connected Drug Delivery Devices Industry
1. High Development and Implementation Costs
Developing connected drug delivery devices requires significant investment in technology, research, and compliance with stringent regulatory standards. The high initial costs can limit adoption, particularly in resource-constrained healthcare systems.
2. Data Privacy and Security Concerns
As connected devices transmit sensitive patient data, concerns about cybersecurity and privacy are prominent. Ensuring that data is securely stored and compliant with regulations such as GDPR and HIPAA is critical to gaining patient and provider trust.
3. Complexity of Integration with Healthcare Systems
While connected devices generate valuable data, integrating this data into existing healthcare systems and electronic health records (EHRs) can be complex. Seamless interoperability remains a challenge for widespread
For a detailed overview and more insights, you can refer to the full market research report by Mordor Intelligence: https://www.mordorintelligence.com/industry-reports/connected-drug-delivery-devices-market
#Connected Drug Delivery Devices Market#Connected Drug Delivery Devices Market Size#Connected Drug Delivery Devices Market Share#Connected Drug Delivery Devices Market Analysis#Connected Drug Delivery Devices Market Report
0 notes