#Cochrane risk of bias
Explore tagged Tumblr posts
Text
Impact of intervention of community pharmacists on cardiovascular outcomes in Spain: A systematic review
Article published in J. Pharm. Pharmacogn. Res., vol. 10, no. 5, pp. 952-976, September-October 2022. DOI: https://doi.org/10.56499/jppres22.1422_10.5.952 Marjan Manouchehri1,2, María S. Fernández-Alfonso1,2, Marta Gil-Ortega3* 1Instituto Pluridisciplinar, Unidad de Cartografía Cerebral, Universidad Complutense de Madrid, 28040 Madrid, Spain. 2Departamento de Farmacología, Facultad de…

View On WordPress
#cardiovascular interventions#Cochrane risk of bias#Community pharmacy#PRISMA-S#Spanish cohort#systematic review
0 notes
Note
Is male circumcision as harmful as female circumcision? I have had multiple discussions about this, but someone said that certain types of FGM are equally or less invasive than MGM
Hi! No, no it is not.
Male circumcision
So, the big question about male circumcisions is if it's ethical or not. A while ago, I would have said, no definitely not, since it's a violation of bodily autonomy. However, someone has since pointed out to me that we do a lot of things to infants (and children) that are technically violations of bodily autonomy.
We consider this morally acceptable because we are providing some intervention that they (the children) are not capable of either requesting or refusing on the basis of it's benefits outweighing the harms. The best example of this, in my opinion, is vaccines. We give children a lot of vaccines because we know that they have (and do) substantially lower the chance of the child getting sick and/or dying from a preventable disease. In this case, the minor violation of bodily autonomy (vaccination of a child) is permitted because waiting until they are able to give their consent would introduce a substantially larger risk of harm.
How does this relate to male circumcision? Given this framework, we could accept male circumcision if (1) there are benefits to the procedure, (2) the benefits outweigh any risk of harm, (3) waiting until the child is able to consent to the procedure is not feasible (i.e., some significant portion of the benefits would be lost).
There is some mixed evidence for these three claims. Evidence in favor includes:
There are a number of reviews [1-3] by the same team that provide support for all three points. In particular this review [3] directly reviews the evidence of "arguments opposing male circumcision", debunking each one in detail. However, the fact that they are all by the same team is less encouraging. The evidence here is substantial, but there's a potential for bias.
That being said, the American Academy of Pediatric [4] also concludes that the "health benefits of newborn male circumcision outweigh the risks".
This Cochrane Review (essentially the highest quality evidence) [5] found male circumcision substantially reduces acquisition risk of HIV by heterosexual men and that incidence of adverse events is very low.
And this review and meta-analysis [6] found the same reduction for HPV.
Evidence against:
This review [7] suggests the benefits of male circumcision may not apply in North American countries
This article [8] claims the same for developed countries in general
This commentary [9] claims the same, suggesting that "from the perspective of the individual boy, there is no medical justification for performing a circumcision prior to an age that he can ... choose to give or withhold informed consent himself"
That being said these papers have also been challenged by advocates for male circumcision [10] and even opponents [9, 11] recognize that the rates of complications are very low, and the rates of serious complications even lower. In addition to that, complication rate was greater for older children [11], which provides support for the third point I highlighted above (i.e., waiting until they are older may introduce more harms than benefits).
And all of that being said, if the procedure is done, it should absolutely be done with some form of pain relief. Thankfully, it appears that the vast majority are performed in this fashion [11].
In the end, there is strong evidence supporting male circumcision for infants in developing countries. There are research gaps concerning if these benefits apply to developed countries (i.e., little work has examined this population specifically), which indicates a need for such research. That being said, with the extremely low complication rate and moderate evidence of benefits, there also isn't a strong argument against the procedure.
---
Female Genital Mutilation
Comparing this to female genital mutilation (FGM) will highlight just how egregious such equivalencies are.
First, a brief detour into biology. Men and women have various embryological precursors that develop into either male or female sex organs. These are called biological homologues, and they are roughly (although not perfectly) comparable. For example, an embryo has the gonad which, during sex differentiation, develops into the ovary in women and the testicle in men [12].
This framework allows us to make some rough comparisons between male circumcision and FGM. For example, it's likely that the "less invasive" form of FGM you were referred to is type 1A [13]. In this type, only the clitoral hood is removed. Both the clitoral hood and the foreskin develop from the prepuce, as they are homologous structures. Notably, even here, male circumcision and FGM type 1A would still only be homologous if (1) FGM type 1A has a similarly low risk profile as male circumcision and (2) male circumcision actually provides no benefits to the infant.
For the first point, we have little to no data on the complication rate of type 1A FGM, specifically because it is essentially never performed in isolation [14]. This is – almost entirely – a theoretical form of FGM. Despite this, even if it were more common it doesn't necessarily follow that the procedures would have a similar adverse effect profile. In fact, one of the most common arguments against male circumcision involves the numerous nerve endings in the glans (head of the) penis, generally in reference to how the foreskin "protects" the penis head or "preserves sensitization" (neither of which are proven assertions). But while the glans penis and glans clitoris have a similar number of nerve endings in absolute terms, the clitoral head is much smaller and therefore much more densely innervated [15]. As a result, it would be much more likely for the removal of the clitoral hood to result in irritation than the removal of the foreskin.
And for the second point, I've discussed the mixed literature on the topic in developed countries. However, most FGM is performed in developing countries (although certainly not exclusively so) [14], and in this context there is strong evidence of a health benefit to male circumcision and absolutely no health benefit to FGM.
To complete the comparisons between FGM and male circumcision in terms of homologous structures [12, 13]:
Type 1B involves the removal of the clitoris with the prepuce (clitoridectomy). This, anatomically speaking, would be similar to removal of (minimally) the penis head.*
Type 2 involves partial or total removal of the clitoris and the labia minora, with or without excision of the labia majora. This would be roughly comparable to the removal of the penis head, mutilation/cutting/removal of penile raphe (underside of the penis) with or without mutilation/cutting/removal of the scrotum.*
Type 3 is infibulation, or the narrowing of the vaginal orifice with creation of a covering seal by cutting and apposition the labia minora and/or the labia majora, with or without excision of the clitoris. There is no direct comparison for men, as they do not have a vaginal orifice or any similar structure.
Type 4 is all other mutilation/anything that cannot be categorized as above.
*Note: these comparisons aren't perfect due to differences in how the homologous structures are arranged. For example, removal of the penis head would also impact the urethra, whereas removal of the clitoris would not. That being said, these comparisons are far more accurate than between FGM types 1B - 4 and male circumcision.
To further drive home the differences, FGM results in substantial, severe health complications (unlike male circumcision) and has absolutely no known health benefits (possibly unlike male circumcision). These articles [16-21] go into great detail on this; the complications range from: infection, incontinence, infertility, severe and sometimes chronic pain, pregnancy complications, PTSD and post-traumatic symptoms, other psychiatric disorders, greater risk of STDs, and death.
There is no evidence of any benefits.
---
Conclusion
Hopefully, it's clear that male circumcision and female genital mutilation are in no way comparable.
The opponents of male circumcision often suggest that any violation of the bodily autonomy of infants is morally wrong, but this fails to consider the nuanced situation inherent to infant-hood and early childhood. They are physically and mentally unable of consenting to or refusing any medical procedure, which is why we have a – generally recognized – moral caveat to this principle that allows caregivers to act in the best interests of the child, particularly when waiting for the child to grow older before allowing any intervention would increase the risk of harm. (Childhood vaccinations and, really, any other medical procedure done on children, are other examples of this.)
It's possible that future research may indicate that male circumcision is not associated with benefits in developed countries. (This would remove male circumcision from the category of procedures described above.) Even then, however, it would not be comparable to FGM due to the vastly different complication rates.
I hope this helps you!
References under the cut:
Morris, B. J., & Krieger, J. N. (2013). Does male circumcision affect sexual function, sensitivity, or satisfaction?—a systematic review. The journal of sexual medicine, 10(11), 2644-2657.
Morris, B. J., Kennedy, S. E., Wodak, A. D., Mindel, A., Golovsky, D., Schrieber, L., ... & Ziegler, J. B. (2017). Early infant male circumcision: systematic review, risk-benefit analysis, and progress in policy. World journal of clinical pediatrics, 6(1), 89.
Morris, B. J., Moreton, S., & Krieger, J. N. (2019). Critical evaluation of arguments opposing male circumcision: A systematic review. Journal of Evidence‐based Medicine, 12(4), 263-290.
Task Force on Circumcision, Blank, S., Brady, M., Buerk, E., Carlo, W., Diekema, D., ... & Wegner, S. (2012). Male circumcision. Pediatrics, 130(3), e756-e785.
Siegfried, N., Muller, M., Deeks, J. J., & Volmink, J. (2009). Male circumcision for prevention of heterosexual acquisition of HIV in men. Cochrane database of systematic reviews, (2).
Shapiro, S. B., Laurie, C., El-Zein, M., & Franco, E. L. (2023). Association between male circumcision and human papillomavirus infection in males and females: a systematic review, meta-analysis, and meta-regression. Clinical Microbiology and Infection, 29(8), 968-978.
Bossio, J. A., Pukall, C. F., & Steele, S. (2014). A review of the current state of the male circumcision literature. The Journal of Sexual Medicine, 11(12), 2847-2864.
Frisch, M., & Earp, B. D. (2018). Circumcision of male infants and children as a public health measure in developed countries: a critical assessment of recent evidence. Global public health, 13(5), 626-641.
Deacon, M., & Muir, G. (2023). What is the medical evidence on non-therapeutic child circumcision?. International journal of impotence research, 35(3), 256-263.
Moreton, S., Cox, G., Sheldon, M., Bailis, S. A., Klausner, J. D., & Morris, B. J. (2023). Comments by opponents on the British Medical Association’s guidance on non-therapeutic male circumcision of children seem one-sided and may undermine public health. World Journal of Clinical Pediatrics, 12(5), 244.
Shabanzadeh, D. M., Clausen, S., Maigaard, K., & Fode, M. (2021). Male circumcision complications–a systematic review, meta-analysis and meta-regression. Urology, 152, 25-34.
26: The Reproductive System . (n.d.). In Anatomy and Physiology (Boundless) . LibreTexts. https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Anatomy_and_Physiology_(Boundless)/26%3A_The_Reproductive_System
Abdulcadir, J., Catania, L., Hindin, M. J., Say, L., Petignat, P., & Abdulcadir, O. (2016). Female genital mutilation: a visual reference and learning tool for health care professionals. Obstetrics & Gynecology, 128(5), 958-963.
WHO, U. O. (2008). Eliminating female genital mutilation: An interagency statement. World Health Organization.
Shih, C., Cold, C. J., & Yang, C. C. (2013). Cutaneous corpuscular receptors of the human glans clitoris: descriptive characteristics and comparison with the glans penis. The Journal of Sexual Medicine, 10(7), 1783-1789.
Utz-Billing, I., & Kentenich, H. (2008). Female genital mutilation: an injury, physical and mental harm. Journal of Psychosomatic Obstetrics & Gynecology, 29(4), 225-229.
Klein, E., Helzner, E., Shayowitz, M., Kohlhoff, S., & Smith-Norowitz, T. A. (2018). Female genital mutilation: health consequences and complications—a short literature review. Obstetrics and gynecology international, 2018(1), 7365715.
Iavazzo, C., Sardi, T. A., & Gkegkes, I. D. (2013). Female genital mutilation and infections: a systematic review of the clinical evidence. Archives of gynecology and obstetrics, 287, 1137-1149.
Berg, R. C., & Underland, V. (2018). Immediate Health Consequences of Female Genital Mutilation/Cutting (FGM/C).
Sarayloo, K., Roudsari, R. L., & Elhadi, A. (2019). Health consequences of the female genital mutilation: a systematic review. Galen medical journal, 8, e1336.
Reisel, D., & Creighton, S. M. (2015). Long term health consequences of Female Genital Mutilation (FGM). Maturitas, 80(1), 48-51.
59 notes
·
View notes
Text
Reference saved in our archive
TL;DR: even mild covid has massive impacts on the cardiovascular systems of *everyone*, preexisting conditions or no.
Objectives: The COVID-19 pandemic has challenged global health systems since December 2019, with the novel virus SARS-CoV-2 causing multi-systemic disease, including heart complications. While acute cardiac effects are well-known, long-term implications are understudied. This review hopes to fill a gap in the literature and provide valuable insights into the long-term cardiac consequences of the virus, which can inform future public health policies and clinical practices.
Methods: This systematic review was prepared using PRISMA reporting guidelines. The databases searched were PubMed, Scopus, Web of Science, and Cochrane. Risk of Bias was assessed using ROBINS-I. The GRADE approach was employed to evaluate the level of certainty in the evidence for each outcome. A meta-analysis was conducted using the Comprehensive Meta-Analysis (CMA) software. In order to identify the underlying cause of high heterogeneity, a subgroup analysis was conducted. Sensitivity analysis was checked.
Results: Sixty-six studies were included in this review. Thirty-two of them enrolled in meta-analysis and the rest in qualitative synthesis. Most outcomes showed a moderate certainty of evidence according to the GRADE framework. Post-COVID individuals with no prior heart diseases showed significant changes in left ventricular (LV) and right ventricular (RV) echocardiographic indices compared to controls. These significant findings were seen in both post-acute and long-COVID survivors regardless of the severity of initial infection.
Conclusion: This review implies that individuals recovering from post-acute and long-term effects of COVID-19 may experience changes in myocardial function as a result of the novel coronavirus. These changes, along with cardiac symptoms, have been observed in patients without prior heart diseases or comorbidities.
#mask up#public health#wear a mask#pandemic#wear a respirator#covid#covid 19#still coviding#coronavirus#sars cov 2#long covid#covid is not over
12 notes
·
View notes
Text
The stance by the Centers for Disease Control and Prevention (CDC) on face masks has taken many twists and turns throughout the COVID pandemic.
After initially claiming face coverings weren’t necessary, the CDC changed course in April 2020, calling on all Americans — even children as young as 2 years old — to mask up.
That September, then-CDC Director Dr. Robert Redfield said during a Senate hearing that “face masks are the most important powerful health tool we have,” even suggesting that they might offer more protection than vaccines.
Those recommendations likely played a large part in 39 U.S. states eventually enacting mask mandates.
Now, a new scientific review — led by 12 researchers from esteemed universities around the world — suggests that widespread masking may have done little to nothing to curb the transmission of COVID-19.
Published by Cochrane Library, the review dug into the findings of 78 randomized controlled trials to determine whether “physical interventions” — including face masks and hand-washing — lessened the spread of respiratory viruses.
When comparing the use of medical/surgical masks to wearing no masks, the review found that “wearing a mask may make little to no difference in how many people caught a flu-like illness/COVID-like illness (nine studies; 276,917 people); and probably makes little or no difference in how many people have flu/COVID confirmed by a laboratory test (six studies; 13,919 people).”
Next, the review compared medical/surgical masks to N95 respirators (or P2 respirators, which are used in Europe).
It found that “wearing N95/P2 respirators probably makes little to no difference in how many people have confirmed flu (five studies; 8407 people); and may make little to no difference in how many people catch a flu-like illness (five studies; 8407 people), or respiratory illness (three studies; 7799 people).”
The 78 studies looked at participants from countries of all income levels.
Data was gathered during the H1N1 flu pandemic in 2009, non-epidemic flu seasons, epidemic flu seasons up to 2016 and the COVID-19 pandemic, the study authors wrote.
Doctor says review had some key limitations
The new findings seem to call into question the CDC’s enthusiastic embrace of widespread masking.
However, Dr. Marc Siegel, professor of medicine at NYU Langone Medical Center and a Fox News medical contributor, pointed out a key limitation: “The researchers focus primarily on randomized trials, but most of the studies that have been done on masks are population studies,” he said.
“There are very few randomized trials on masks.”
In a randomized trial, researchers place participants in different groups and observe the results in a controlled environment.
By contrast, population-based studies measure outcomes in a “real-world” setting.
The study authors did admit to some limitations and a risk of bias, including the low number of people who followed mask guidance and the wide variation of outcomes.
“The results might change when further evidence becomes available,” they wrote.
‘Be sure of consistency’
Dr. Siegel said he has never supported mask mandates.
He believes that while masks might be effective on an individual level, they don’t work as well on a population level.
“If you’re going to mandate something, you’d have to be sure of consistency across the population, and that’s never happened,” he said.
However, the physician pointed out that the CDC never actually mandated masks — with the exception of a public transportation mandate in January 2021.
“It was the state and local authorities that took the CDC’s recommendations and implemented the mandates,” Dr. Siegel said.
“The recommendations may have been wrong, but the CDC doesn’t deserve the blame for everything. I think they were aware that masks may have value on a personal basis, but they got carried away with the politics.”
What do you think? Post a comment.
As of right now, no U.S. states have mask mandates in place.
On Sunday, New York dropped its state-wide mask requirement in hospitals — leaving the decision up to individual facilities. Many healthcare facilities are currently still requiring them.
258 notes
·
View notes
Text
Literature Search and Study
Clinical evaluation in healthcare involves assessing the safety and effectiveness of medical interventions or devices in humans. This process requires a thorough literature search to collect relevant information on the device, including clinical investigations, side effects, and medical alternatives. MEDDEV 2.7/1 revision 4 outlines the importance of using objective, non-biased, systematic search, and review methods to ensure that the selected papers accurately reflect the intended use of the device.
Examples are –
PICO (patient characteristics, type of intervention, control, and outcome queries)
Cochrane Handbook for Systematic Reviews of Interventions
PRISMA (The Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Statement
MOOSE Proposal (Meta-analysis Of Observational Studies in Epidemiology) The protocol should specify the elements described in the examples given below, addressing the background, objective, methods for identification, selection, and collection of relevant publications to address the literature review questions
Step 1: Define the research question
The first step in conducting a literature search and study is to define the research question. This involves identifying the intervention or device that needs to be evaluated and the population that will be studied. The research question should be focused and specific to ensure that the literature search is targeted and efficient. Research question(s) should be consistent with the scope of the clinical evaluation and carefully constructed using a process, example PICO:
P- Population(s)/disease(s) or condition(s)
I- Intervention(s)
C- Comparator group(s)/control(s)
O- Outcome(s)/endpoint(s)
Step 2: Conduct a literature search
Once the research question has been defined, the next step is to conduct a literature search. This involves searching for relevant studies in electronic databases such as PubMed, Cochrane Library, and Embase. The search terms should be carefully selected to ensure that all relevant studies are captured. In addition to electronic databases, relevant grey literature such as conference proceedings, dissertations, and government reports should also be searched.
Step 3: Screen and select studies
After conducting the literature search, the next step is to screen and select studies for inclusion in the study. This involves reviewing titles and abstracts of the studies identified in the literature search and selecting those that meet the inclusion criteria. The inclusion criteria should be defined in advance and should be based on the research question. The selected studies should then be reviewed in detail to determine their relevance and quality.
Step 4: Evaluate study quality
The quality of the studies selected for inclusion in the study should be evaluated using established criteria such as the Cochrane Risk of Bias tool or the appraisal criteria defined in the literature search protocol for the device under assessment. The quality of the studies is important because it affects the reliability and validity of the results. Studies with a high risk of bias should be excluded from the study.
Step 5: Extract data and analyse results
The next step is to extract data from the selected studies and analyse the results. Data extraction involves collecting information on the study design, sample size, intervention or device being evaluated, and outcomes measured. The data should be analysed using appropriate statistical methods to determine the effectiveness and safety of the intervention or device.
Step 6: Interpret and communicate results
The final step is to interpret and communicate the results of the study. The results should be interpreted considering the research question and the study objectives. The implications of the results for clinical practice should be discussed, and recommendations for further research should be made. The results should be communicated clearly and accurately to ensure that they are understood by all stakeholders, including patients, healthcare professionals, and regulators.
In conclusion, conducting a literature search and study for clinical evaluation is a complex and important process that requires careful planning and execution. By following the steps outlined above, healthcare professionals can ensure that the evaluation of medical interventions and devices is evidence-based and of high quality.
At IZiel, we prioritize clarity and structure in alignment with the expectations of European Authorities. Our primary goals are to ensure thoroughness and scientific accuracy throughout the process of gathering and presenting data in the CER. Obtaining approval serves as the definitive endpoint for every report we produce. According to the EU MDR, clinical Evaluation is recognized as a means of evaluating the balance between benefits and risks associated with medical devices. Additionally, conducting risk assessments is crucial for justifying foreseeable risks to subjects in relation to the advantages. These assessments must be well-documented in the clinical evaluation plan, which should also incorporate an ongoing monitoring strategy for risks and the benefit-risk ratio.
At IZiel we provide complete expertise in Literature Search & Study to assist in the clinical evaluation of the product.
0 notes
Text
#JamesDonaldson On #MentalHealth – #Exercise Decreases #SuicideAttempts in Those With #Mental And Physical Illness

Summary: Engaging in an #exercise program reduced #suicidalthoughts and actions in patients with #mental and physical health problems who previously had #suicidalideations Source: University of Ottawa A new study from the University of Ottawa’s Faculty of Medicine found #patients with #mental or physical illness were able to successfully adhere to #exercise regimes despite previous thinking, resulting in decreased #suicideattempts. The findings cast doubt on the misconception that #patients suffering from #mental or physical illness are not motivated to participate in a physical #exercise regime, which has similar efficacy to antidepressants and cognitive #behavioraltherapy in the treatment of #depression. It’s effect on #suicidalbehaviors, however, was unclear. A new study from the University of Ottawa’s Faculty of Medicine found #patients with #mental or physical illness were able to successfully adhere to exercise regimes despite previous thinking, resulting in decreased #suicideattempts. Image is in the public domain “This misconception has led to primary care providers under-prescribing exercise, resulting in further deterioration of #patients’ #mental and physical health,” says Dr. Nicholas Fabiano, a psychiatry resident and lead author of the study with medical student Arnav Gupta. “The findings of this study “debunk” this belief as #exercise was well tolerated in those with #mental or physical illness. Therefore, providers should not have apprehension about prescribing exercise to these #patients.” Under the supervision of Dr. Marco Solmi and Dr. Jess Feidorowicz from the Department of Psychiatry, Fabiano and Gupta evaluated 17 randomized control trials with over 1,000 participants to deduct their findings. #James Donaldson notes:Welcome to the “next chapter” of my life… being a voice and an advocate for #mentalhealthawarenessandsuicideprevention, especially pertaining to our younger generation of students and student-athletes.Getting men to speak up and reach out for help and assistance is one of my passions. Us men need to not suffer in silence or drown our sorrows in alcohol, hang out at bars and strip joints, or get involved with drug use.Having gone through a recent bout of #depression and #suicidalthoughts myself, I realize now, that I can make a huge difference in the lives of so many by sharing my story, and by sharing various resources I come across as I work in this space. #http://bit.ly/JamesMentalHealthArticleOrder your copy of James Donaldson's latest book,#CelebratingYourGiftofLife:From The Verge of Suicide to a Life of Purpose and Joy www.celebratingyourgiftoflife.com About this #exercise and #mentalhealth research news Author: Paul LogothetisSource: University of OttawaContact: Paul Logothetis – University of OttawaImage: The image is in the public domain Original Research: Open access.“The effect of #exercise on #suicidalbehaviors: A systematic review and meta-analysis of randomized controlled trials” by Nicholas Fabiano et al. Journal of Affective Disorders Abstract The effect of exercise on #suicidalbehaviors: A systematic review and meta-analysis of randomized controlled trials Background Although #exercise may positively impact those with #mental or other medical illnesses, there is a lack of understanding on how it influences #suicidalideation or risk. Methods We conducted a PRISMA 2020-compliant systematic review searching MEDLINE, EMBASE, Cochrane, and PsycINFO from inception to June 21, 2022. Randomized controlled trials (RCTs) investigating #exercise and #suicidalideation in subject with #mental or physical conditions were included. Random-effects meta-analysis was conducted. The primary outcome was #suicidalideation. We assessed bias of studies with risk of bias tool 2. Results We identified 17 RCTs encompassing 1021 participants. #Depression was the most included condition (71?%, k?=?12). Mean follow up was 10.0?weeks (SD?=?5.2). Post-intervention #suicidalideation (SMD?=?-1.09, CI -3.08–0.90, p?=?0.20, k?=?5) was not significantly different between #exercise and control groups. #Suicideattempts were significantly reduced in participants randomized to exercise interventions as compared to inactive controls (OR?=?0.23, CI 0.09–0.67, p?=?0.04, k?=?2). Fourteen studies (82?%) were at high risk of bias. Limitations This meta-analysis is limited by few, and underpowered and heterogenous studies. Conclusion Overall, our meta-analysis did not find a significant decrease in #suicidalideation or mortality between #exercise and control groups. However, #exercise did significantly decrease #suicideattempts. Results should be considered preliminary, and more and larger studies assessing suicidality in RCTs testing #exercise are needed. Read the full article
0 notes
Text
Endometriosis and irritable bowel syndrome: A systemic review and meta-analyses
Michelle Y. Nabi, Samal Nauhria, [...], and Prakash V. A. K. Ramdass
Abstract
Objective
To estimate the pooled odds ratio of endometriosis and irritable bowel syndrome, and to estimate the pooled prevalence of irritable bowel syndrome in patients with endometriosis.
Data sources
Using Cochrane Library, MEDLINE, Science Direct, ClinicalTrials.gov, Web of Science, and CINAHL, we conducted a systematic literature search through October 2021, using the key terms “endometriosis” and “irritable bowel syndrome.” Articles had to be published in English or Spanish. No restriction on geographical location was applied.
Methods of study selection
The following eligibility criteria were applied: full-text original articles; human studies; studies that investigated the association between endometriosis and irritable bowel syndrome. Two investigators screened and reviewed the studies. A total of 1,776 studies were identified in 6 separate databases. After screening and applying the eligibility criteria, a total of 17 studies were included for analyses. The meta-analysis of association between endometriosis and irritable bowel syndrome included 11 studies, and the meta-analysis on the prevalence of irritable bowel syndrome in endometriosis included 6 studies.
Tabulation, integration, and results
Overall 96,119 subjects were included in the main meta-analysis (11 studies) for endometriosis and irritable bowel syndrome, with 18,887 endometriosis patients and 77,171 controls. The odds of irritable bowel syndrome were approximately 3 times higher among patients with endometriosis compared with healthy controls (odds ratio 2.97; 95% confidence interval, 2.17 – 4.06). Similar results were obtained after subgroup analyses by endometriosis diagnosis, irritable bowel syndrome diagnostic criteria, and Newcastle-Ottawa Scale scores. Six studies reported prevalence rates of irritable bowel syndrome in people with endometriosis, ranging from 10.6 to 52%. The pooled prevalence of irritable bowel syndrome in people with endometriosis was 23.4% (95% confidence interval, 9.7 – 37.2).
Conclusion
Patients with endometriosis have an approximately threefold increased risk of developing irritable bowel syndrome. Development and recent update of Rome criteria has evolved the diagnosis of IBS, potential bias should still be considered as there are no specific tests available for diagnosis.
Systemic Review Registration
Keywords: irritable bowel syndrome, endometriosis, systematic review, meta-analyses, functional gastrointestinal disorders
Introduction
Endometriosis and irritable bowel syndrome (IBS) are two common medical conditions that markedly affect a substantial proportion of adults and teenagers, and even some menopausal adults (1, 2). Even though they are two distinct conditions with different etiologies, a significant percentage of people experience both concurrently (3). Endometriosis, with an estimated worldwide prevalence ranging from 0.7 to 8.6%, (4) is characterized by the existence of endometrial-like tissue that has been disseminated beyond the uterine cavity. Patients with endometriosis commonly experience menstrual disturbance, infertility, abdominal and pelvic pain, and irregularities with bowel movements (5, 6).
Irritable bowel syndrome, which shares many clinical features with endometriosis, is a gastrointestinal disorder that primarily affects the large intestine, and is characterized by an array of symptoms such as alteration in bowel movements, abdominal discomfort, pain, and cramping (7). The prevalence of irritable bowel syndrome ranges from 0.4 (in India and Ghana) to 20.9% (in Singapore), with a pooled global prevalence of 5.9% (8). Moreover, approximately 61% of adults and teenagers who were assigned female at birth are affected by irritable bowel syndrome (9).
Irritable bowel syndrome and endometriosis have a significant overlap in symptom presentation due to chronic inflammation thus leading to chronic pelvic pain (10). Endometriosis may even masquerade as irritable bowel syndrome in some patients (11). However, despite these similarities in clinical presentation, a recent nationwide study in the U.S. has shown that endometriosis increases the risk of irritable bowel syndrome approximately threefold (3). Possible explanations for this increased risk include chronic low grade inflammation resulting from mast cell activation, neuronal inflammation, leaky gut, and dysbiosis (12).
It is unclear if endometriosis is an independent risk factor for irritable bowel syndrome. The main purpose of this study was to quantify the association between endometriosis and irritable bowel syndrome, and to estimate the prevalence of irritable bowel syndrome in patients with endometriosis through pooled analysis.
Materials and methods
Sources
This systematic review and meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and protocols (PRISMA-P) statement (13). The study protocol was registered in the PROSPERO database (University of York, United Kingdom).1 A systematic search of the following electronic databases was conducted to identify peer-reviewed literature from inception until October 2021: MEDLINE, Science Direct, ClinicalTrials.gov, Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, CINAHL, and Web of Science. Key words or MeSH terms used were “irritable bowel syndrome” AND “endometriosis.”
Study selection
Citation files from the searched databases were imported into Endnote reference management software and duplicates were removed. Using the eligibility criteria, two investigators independently screened titles and abstracts of the studies for relevance. The potential full texts articles were further assessed to be included in the review. Any disagreements between the authors were resolved with a discussion. Inclusion criteria were any observational or experimental studies that investigated both endometriosis and irritable bowel syndrome. Studies were included if irritable bowel syndrome was diagnosed by pre established criteria. Endometriosis had to be confirmed surgically, by clinical inspection, or reported as the International Classification of Diseases code for endometriosis. Meta-analyses, reviews, conference summaries, abstracts, case reports, opinions, letters, and animal studies were excluded. There was no search restriction for year of publication or the age group of patients. Articles were restricted to English and Spanish.
Data extraction and quality assessment
Data were extracted into a standardized data-collection sheet using the following headings: first author name, date of publication, study site, study design, irritable bowel syndrome diagnosis criteria, endometriosis diagnostic criteria, sample size, event rate, and quality assessment score. Two investigators (MN and PR) assessed the quality of all included studies using the Newcastle-Ottawa Scale (NOS), and the overall scores were recorded (14). NOS scale is widely used for assessing quality of each included study in meta-analyses and is based on ranking studies on according to the selection criteria, group comparability and ascertainment of exposure.
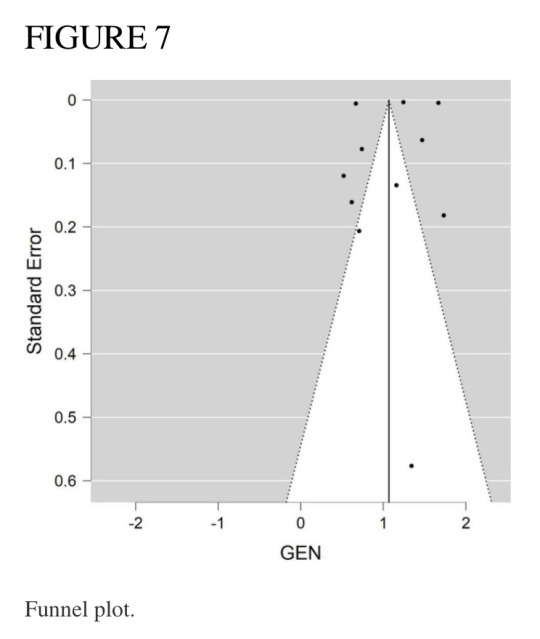
Data synthesis and analysis
Forest plots were generated with Review Manager version 5.4 (Nordic Cochrane Centre, Cochrane Collaboration, Denmark) and funnel plots were created with JASP statistical software. The primary outcome of the association of irritable bowel syndrome and endometriosis in this meta-analysis was performed using the random effects model to produce odds ratios (OR) with 95% confidence interval (CI). We conducted subgroup analyses based on diagnosis of endometriosis (surgical versus ICD-9-CM 617.x codes), method of diagnosis of irritable bowel syndrome, NOS scores (>6 vs. <6), and a combination of all criteria (endometriosis diagnosis; irritable bowel syndrome criteria; NOS score; and study design). In the subgroup analysis based on all criteria, studies were grouped as having met all criteria (surgical diagnosis of endometriosis, irritable bowel syndrome diagnosed with Rome criteria (15–17), NOS score > 6, and longitudinal studies), or not. This allowed for strong epidemiological evidence for the association between endometriosis and irritable bowel syndrome.
According to Rome III criteria, IBS patients can be classified into four subtypes and can be useful for treating specific symptoms of the patient. The subtypes include: IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), IBS with mixed features (IBS-M) or IBS, unsubtyped. Whereas Rome IV criteria defined IBS as a functional bowel disorder in which recurrent abdominal pain is associated with defecation or a change in bowel habits.
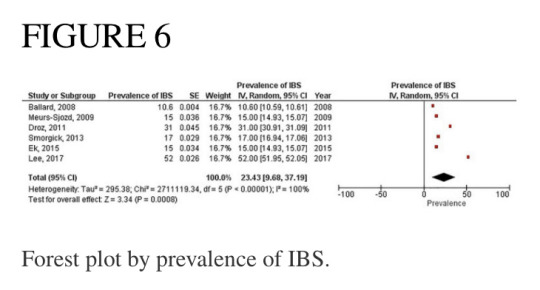
A separate forest plot was generated for the prevalence of irritable bowel syndrome in patients with endometriosis, for studies that provided only prevalence data. The random effects model account for between-study heterogeneity by weighting studies similarly. Heterogeneity was assessed using the I2 statistic. Values of I2 > 50% were considered as indicative of large heterogeneity (18). We used the Begg’s and Egger’s funnel plot, which is a subjective visual method, to estimate risk of publication bias. A funnel plot that appears asymmetrical suggests publication bias. A p-value of <0.05 for all analyses was considered statistically significant. Although p-values are poor predictors of outcome, all quantitative studies included in our analyses mention p-values in accordance to the AM Stat recommendation.
Results
Search results and study inclusion
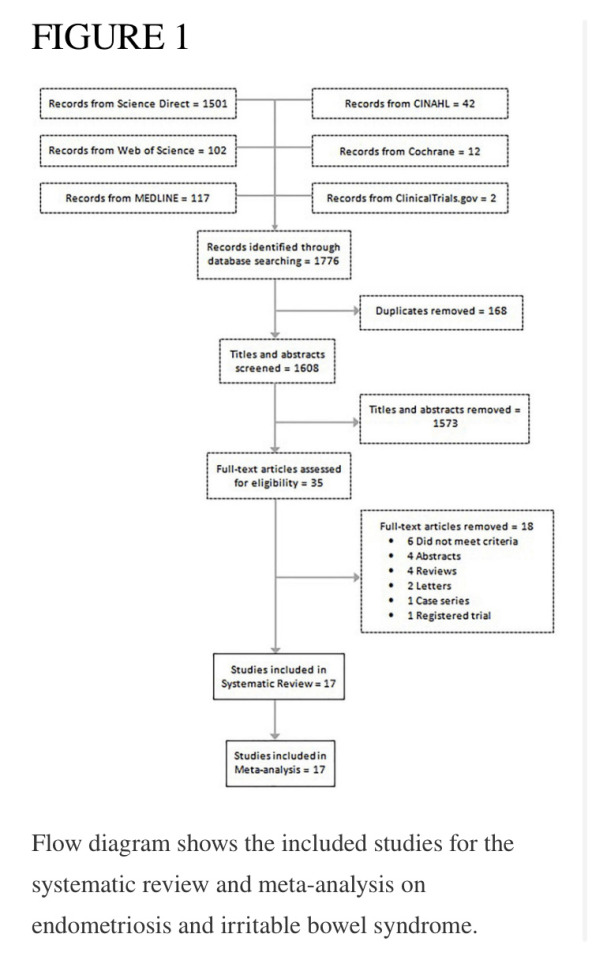
A total of 1,776 studies were identified in 6 separate databases. After removal of 168 duplicates, there were 1,608 eligible studies (titles/abstracts) which were independently screened by two reviewers. Of the 1,608 screened studies, 1,573 did not meet inclusion criteria and 35 full-text articles were reviewed. A total of 17 studies met criteria to be included in the systematic review. Eighteen studies were excluded for the following reasons: did not meet criteria; conference abstracts; reviews; letters; case series; and registered trials. The meta-analysis of the association of endometriosis and irritable bowel syndrome included 11 studies, and the meta-analysis on the prevalence of irritable bowel syndrome in endometriosis included 6 studies (see flow chart in Figure 1).
Study characteristics
Overall 96,119 subjects were included in the main meta-analysis (11 studies) for endometriosis and irritable bowel syndrome association, with 18,887 endometriosis patients and 77,171 controls (patients without symptoms). The participants in the study by Ballard et al. (19) were already reported in the study by Seaman et al. (2), thus they were not added to the main meta-analysis twice. The meta-analysis on the prevalence of irritable bowel syndrome in endometriosis included 6,395 subjects. Almost all articles were published during the last decade, with two exceptions, which were published in 2005 and 2008. Of the 17 studies in this review, the majority were conducted in the United States, the United Kingdom, and Sweden. Table 1 describes the key characteristics of the included studies. Most studies used either Rome II (15), Rome III (16), Rome IV (17), or the visual analog scale for irritable bowel syndrome (VAS-IBS) (20) questionnaires to diagnose irritable bowel syndrome. Endometriosis diagnosis was confirmed either by laparoscopy or laparotomy. Each study had a quality assessment score between 5 and 10 on the Newcastle-Ottawa Scale (14), with most studies having a score of 7 or greater.
Meta-analysis of studies
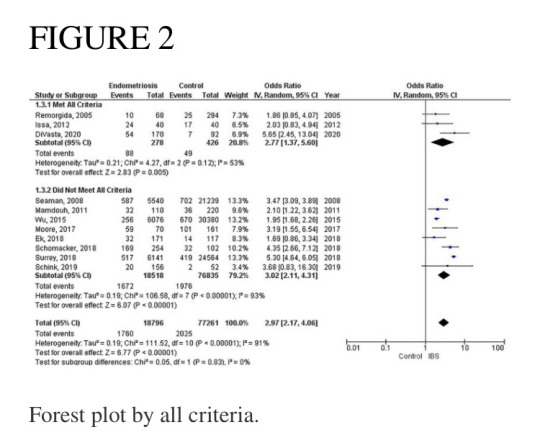
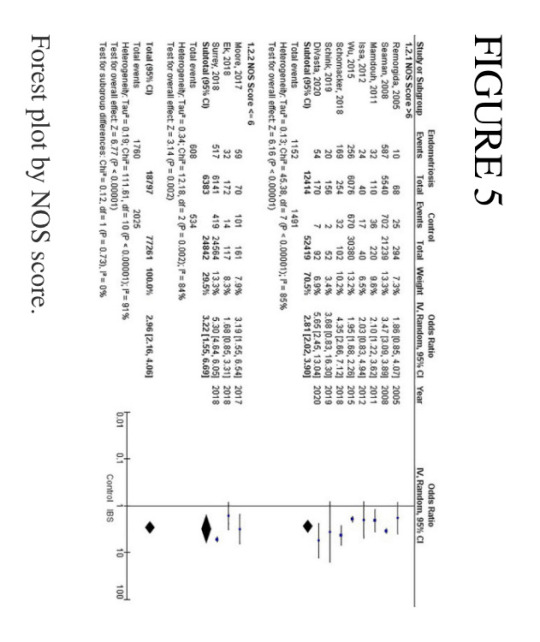
Of the 11 studies in the main meta-analysis (1–3, 10, 21–27), most were cohort and case control. Studies were conducted from 2005 to 2020, and sample sizes ranged from 80 to 36,456. In this meta-analysis the pooled odds ratio of endometriosis and irritable bowel syndrome was 2.97 (95% CI = 2.17 – 4.06), based on all selected criteria (see details in Figure 2). Odds ratio for the individual studies ranged from 1.69 (26) to 5.65 (10). There was a large heterogeneity in this study (I2 = 91%, [P < 0.00001]). In our subgroup analyses, the odds ratio for each subgroup was approximately 3, regarding endometriosis diagnosis (see Figure 3), criteria used for irritable bowel syndrome (see Figure 4), and NOS score (see Figure 5). Visual inspection of the funnel plot appears asymmetrical, suggesting the presence of publication bias (see Figure 7).

Endometriosis diagnosis
There were 9 studies (28,888 patients) in the meta-analysis that confirmed endometriosis surgically, and 2 studies (67,161 patients) that used the ICD-9-CM 617.x codes to diagnosis endometriosis. The random effects model showed a significant association between endometriosis and irritable bowel syndrome with a pooled odds ratio of 3.0 (95% CI = 2.18, 4.11) (see Figure 3).
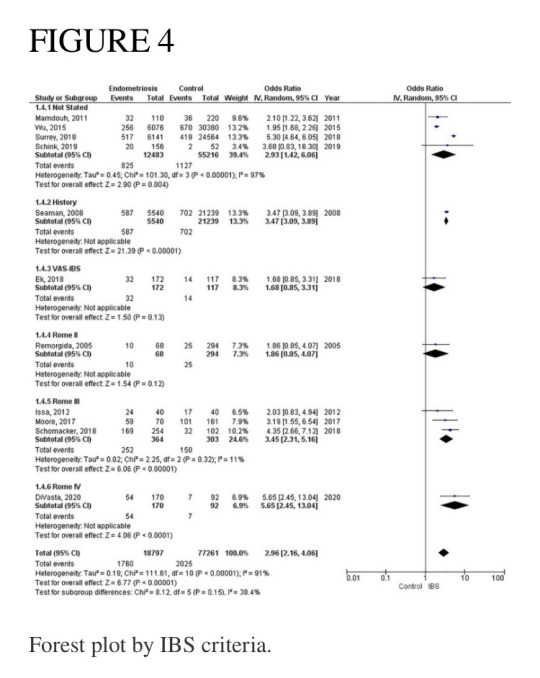
Irritable bowel syndrome diagnostic criteria
Four studies (67,699 patients) did not state what criteria were used to diagnose irritable bowel syndrome, three studies (667 patients) used the Rome III criteria, and one study each used the following as their criteria: history (26,779 patients); VAS-IBS (289 patients); Rome II (362 patients), and Rome IV (323 patients). The random effects model shows a significant association between endometriosis and irritable bowel syndrome, with a combined odds ratio of 2.96 (95% CI = 2.16, 4.06) (see Figure 4).
Pooled prevalence of irritable bowel syndrome
There were six studies (6, 19, 28–31) that estimated the prevalence of irritable bowel syndrome in people with endometriosis. These studies ranged in sample size from 101 to 5,540. The prevalence of irritable bowel syndrome in patients with endometriosis ranged from 10.6 to 52%, with a pooled estimate of 23.4% (95% CI = 9.7%, 37.2%) (see Figure 6).
Discussion
This systematic review and meta-analysis was designed to estimate the association of endometriosis and irritable bowel syndrome. Our literature search included all available original studies investigating irritable bowel syndrome and endometriosis, thereby allowing us to include a large number of subjects (17 studies; n = 96,974).
The most significant finding of our study is that the pooled analysis showed endometriosis was associated with an almost three-fold increase in risk of irritable bowel syndrome, and that more than 1 in 5 people with endometriosis have irritable bowel syndrome. Of particular significance, all 11 studies in the main meta-analysis showed a positive association of irritable bowel syndrome and endometriosis. Moreover, almost all subjects in this analysis were followed longitudinally, either retrospectively or prospectively, thus allowing for inference on temporality vis-à-vis risk factor and disease. In addition, five studies (n = 68,129) included in this meta-analysis showed a positive association of endometriosis and irritable bowel syndrome, even after adjustments were made for potential confounding variables (3, 10, 21, 25, 26). Furthermore, there were significant findings in our subgroup analyses based on diagnostic method for endometriosis, diagnostic criteria for irritable bowel syndrome, and NOS scores. More importantly, after the studies in the main meta-analysis were categorized based on the following criteria: longitudinal study design; surgical confirmation of endometriosis; Rome diagnostic criteria for irritable bowel syndrome; and NOS scores > 6, the pooled odds ratio was 2.77 (95% CI = 1.37, 5.60). Thus, this provides strong epidemiological evidence for the increased association of endometriosis and irritable bowel syndrome.
Endometriosis is characterized as a chronic, estrogen-dependent inflammatory disorder with the presence of endometrial tissue outside the uterine cavity (3). Affected areas encompass the pelvic peritoneum, ovaries, rectovaginal septum, the abdominal cavity, and the gastrointestinal tract.
Histologically, endometriosis can be characterized into superficial endometriosis, ovarian endometrioma (OE) and deep infiltrating endometriosis (DIE). DIE can present with severe symptoms as the lesions penetrate deeper into the peritoneum and thus produce more pain as compared to the superficial. DIE also tends to involve the uterine ligaments, pouch of Douglas, rectum, or vagina. OE on the other hand, is the most common type of endometriosis and located in the pelvic areas or along the intestines. Multifocality of such a variably distributed lesion thus, predisposes to a variable clinical presentation the patients.
The relationship between endometriosis and irritable bowel syndrome has not yet been fully elucidated, and multiple theories have been proposed. One such theory is the immunological linkage through increased mast cell activation seen in both conditions (32). The major hallmarks postulated in this immunological linkage are the abnormal levels of inflammatory cytokines and immune cell activation in the peritoneal cavity (33). Retrograde menstruation has been a plausible explanation, which causes the dissemination of menstrual blood containing endometrial cells into the pelvic cavity, thus triggering symptoms of irritable bowel syndrome (34). Specifically, in endometriosis, the activated mast cells have been activated near nerve endings within the pelvic and abdominal regions, and in irritable bowel syndrome they have been shown to be activated near the bowel mucosa (35). Moreover, Remorgida et al. (22) have found that the severity of gastrointestinal symptoms was directly related to the extent of infiltration of endometriotic foci in the bowel, and reversal of symptoms occurred after removal of those lesions. However, they did not find any conclusive evidence regarding endometriosis and predisposition to a specific subtype of irritable bowel syndrome.
Another theory for the increased association between these two disorders is through a hormonal linkage. This hormonal connection involves the presence of gonadotropin releasing hormone-containing neurons (36) and receptors for luteinizing hormone within the pelvic organs (37) and the enteric nervous system (38). It is hypothesized that the pain experienced in some people with irritable bowel syndrome could be as a result of the sex hormones found in afab people, as reports have shown a fluctuating exacerbation of symptoms of irritable bowel syndrome during menstruation (39). Likewise, it was observed that patients with endometriosis had worsening of gastrointestinal symptoms during the time of menstruation (30). It is posited that patients with endometriosis and irritable bowel syndrome both experience visceral hypersensitivity, which is likely to contribute to the severity of gastrointestinal symptoms (24). A large population-based study reported that the highest prevalence rate for endometriosis was for the 40–44-year age group (40), and Oka et al. reported that afab people between the ages of 30–39 years were more likely to have irritable bowel syndrome when compared to those less than 30 years old (8). Thus, the prevalence for both conditions peak at approximately the same age range, just around the beginning of the menopausal period. Moreover, postmenopausal patients with irritable bowel syndrome experience symptoms more severely than premenopausal patients with irritable bowel syndrome, most likely due to modulation in the brain-gut axis as a result of hormonal changes (41). Our study was not analyzed according the age of the patient.
Furthermore, a meta-analysis on the sex differences of irritable bowel syndrome reveals that afab people are more likely to experience abdominal pain when compared to amab people, and this may be because of sex hormonal differences (42).
Other important factors to consider when examining the relationship between endometriosis and irritable bowel syndrome are race/ethnicity and geographical region. In their study, Bougie et al. showed that Black people were less likely than White people to have endometriosis, and that Asian people were more likely than White people to have endometriosis (43). Similarly, Wigington et al. reported that Black people were less likely than White people to have irritable bowel syndrome (44). Thus, White people were more likely to have both endometriosis and irritable bowel syndrome when compared to Black people. Interestingly, of the 11 studies in our meta-analysis, only two studies stated the race of the participants (10, 27), and of these, the study by Schink investigated only Caucasian people (27).
As discussed previously, endometriosis is a chronic and multifactorial (genes, hormones, immune and environmental) and multi risk factor (family history, long menstrual cycle, low parity, and poor physical activity) associated disease (45, 46). An association between endometriosis and heavy metal sensitivity has been discussed in research that can potentially play a role in producing produce an IBS-like syndrome. Specifically, heavy metal nickel has been shown to interfere with estrogen and its receptors and thus plays a role in the pathogenesis of IBS. Researchers have even demonstrated a higher nickel level in endometriosis tissue (46, 47).
Recent global studies showed that the prevalence of irritable bowel syndrome varies from country to country, ranging from 0.2% in India to 29.2% in Croatia, using the Rome III criteria, and ranging from 0.4% in India and Ghana to 21.3% in United States, using the Rome IV criteria (8). Similarly, the global prevalence rates for endometriosis in the general population ranged from 0.7 to 8.6% (4). This highlights the importance of recognizing that irritable bowel syndrome and endometriosis can burden people of any race and from any country of origin, even though they can vary widely regarding presentation and response to treatment (43). Studies investigating endometriosis or irritable bowel syndrome individually were sparse for the geographical regions of South America, Central America, Africa, and Asia (8). However, the studies conducted in the United States reported the highest prevalence rate of endometriosis (48), and the highest prevalence rate of irritable bowel syndrome when using the Rome IV diagnostic criteria (11). Moreover, the studies conducted in the United States showed that people with endometriosis had the highest odds (5.65, 5.30) of having irritable bowel syndrome (see Figure 2). Thus, this points to further evidence that endometriosis is a significant contributory factor leading to irritable bowel syndrome. Needless to say, more investigation is needed regarding race/ethnicity and the association between endometriosis and irritable bowel syndrome.
Studies included in our meta-analysis used the Rome II, Rome III, and Rome IV criteria. The odds of irritable bowel syndrome in endometriosis increased with each subsequent updated version of the Rome criteria (odds ratio from 1.86 to 3.45 to 5.65), respectively. However, when interpreting these differences, one should also consider the significant heterogeneity that exists regarding study design and sample size. Moreover, recent studies have shown that the diagnostic outcomes for Rome II and Rome III criteria differ significantly (49), whereas there were comparable findings for Rome III and Rome IV criteria (50). Nevertheless, there is a markedly increased risk associated with endometriosis and irritable bowel syndrome, regardless of the criteria used to diagnose irritable bowel syndrome. The basis of the Rome criteria relies on its definition of irritable bowel syndrome in which recurrent abdominal pain is associated with defecation or a change in bowel habits (17). Thus, the Rome criteria classifies patients as different subtypes based on bowel habits: irritable bowel syndrome with predominant constipation (IBS-C), irritable bowel syndrome with predominant diarrhea (IBS-D), irritable bowel syndrome with mixed bowel habits (IBS-M) or irritable bowel syndrome, unclassified (IBS-U) (17). However, our data does not include information on these subtypes. Therefore, we cannot conclusively state whether endometriosis increases the risk of a specific subtype of irritable bowel syndrome over another, or if it increases the risk of all subtypes of irritable bowel syndrome.
Our meta-analysis included one study that used the visual analog scale for irritable bowel syndrome (VAS-IBS) to diagnose patients with irritable bowel syndrome. The VAS-IBS is a patient-centered questionnaire comprised of six categories: Abdominal Pain, Diarrhea, Constipation, Bloating and Flatulence, Abnormal bowel passage, and Vomiting and Nausea (20). The items in the VAS-IBS capture the main physical concerns people with irritable bowel syndrome might experience. All symptoms, except vomiting and nausea, support the diagnosis of irritable bowel syndrome. Even though the majority of studies in our meta-analysis used the Rome criteria to establish a diagnosis of irritable bowel syndrome, the VAS-IBS was shown to be an accurate and reliable questionnaire to diagnose irritable bowel syndrome (20).
Our literature search found two meta-analyses on endometriosis and irritable bowel syndrome (51, 52). Even though they had similar findings to ours regarding the increased association of endometriosis and irritable bowel syndrome, we believe that our review provides a more detailed analysis on various factors such as endometriosis diagnosis and irritable bowel syndrome diagnosis, and the pooled prevalence of irritable bowel syndrome in patients with endometriosis.
Strengths and limitations
Strengths of this meta-analysis include incorporation of all available studies, with subsequent sub-analyses. Both observational and interventional studies were included. In addition, most studies included in the meta-analysis have a quality assessment rating greater than 6. Moreover, by independently reviewing articles and selecting those that fit our criteria, we concluded with a large-scale study from various geographic regions of the world that include North America, Europe, Asia, Africa, and Oceana. This allowed us to interpret the risk of irritable bowel syndrome in people with endometriosis from an extensive and multiethnic perspective. In addition, this is the first meta-analysis to include a pooled estimate of the prevalence of irritable bowel syndrome in people with endometriosis.
Our study has a number of potential limitations. While select studies employed either the Rome II, Rome III, Rome IV, or the visual analog scale for irritable bowel syndrome (VAS-IBS) as their criteria to gather symptomatic data on irritable bowel syndrome, the majority of studies in this meta-analysis did not state what criteria were used to diagnose irritable bowel syndrome. The anatomical location of endometriosis and the IBS subtypes was not described as relevant description was not available in the included studies. Nonetheless, after subgroup analysis by whether criteria was used or not, pooled estimates revealed similar results in these groups. These estimates were also reflected in the overall combined odds ratio for all studies. Thus, omitting the criteria used for establishing irritable bowel syndrome did not pose any significant error in this analysis. Another limitation of this study is that data from the two largest retrospective cohort studies identified patients with endometriosis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) 617.x codes, whereas all other studies stated that laparoscopy/laparotomy/clinical inspection was used as the mode of diagnosis. There is a significant variation in clinical diagnosis of endometriosis due to the costs and invasive diagnostic techniques including laparoscopic or surgical diagnosis. This has led to more reliance on radiological diagnosis for the same. Nevertheless, the surgical diagnostic methods are still considered the gold standard. Additionally, IBS diagnostic criteria are not based on standard guidelines or criteria. Most commonly used are the Manning and the Rome criteria which are possibly too general and vague for a specific diagnosis. Thus, an inevitable overlap occurs in the diagnosis of endometriosis and IBS (53).
Therefore, there was some inconsistency regarding identification of endometriosis. Nevertheless, our subgroup analysis regarding endometriosis diagnosis showed similar pooled estimates. However, despite these limitations, the diagnosis of irritable bowel syndrome remains a challenge with the fluctuation in symptoms and its symptoms mimicking other disorders like endometriosis (17).
Recommendations
Our database search revealed that no studies were conducted in Central America or South America, and only a solitary study each arose out of Africa and Asia. Thus, we recommend that studies be conducted in these regions of the world to give globally representative estimates of the risk associated with these conditions. Furthermore, since the majority of participants were investigated in retrospective cohort studies, we recommend that researchers conduct large-scale prospective cohort studies to investigate the risk of irritable bowel syndrome (preferably using the Rome IV criteria) in people with endometriosis (with diagnosis confirmed surgically). Moreover, we suggest that studies be conducted to investigate whether endometriosis predisposes to any specific subtypes of irritable bowel syndrome.
Conclusion
This review provides significant epidemiological evidence for the association between endometriosis and irritable bowel syndrome. People with endometriosis are three times more likely to have irritable bowel syndrome compared to people without endometriosis. Doctors should be mindful that patients with endometriosis can also have irritable bowel syndrome.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MN, MR, and SL contributed to the conception and design of the study. ME organized the database. PR and SN performed the statistical analysis. AV wrote the first draft of the manuscript. MN, MR, AV, and ME wrote the sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
#frontiers in medicine#pubmed central#endometriosis#gender neutral language#trans healthcare#afab health#endowarrior#ibs#irritable bowel disease#irritable bowel syndrome#scientific study#scientific news#comorbid conditions
1 note
·
View note
Text
Ladies, ask for a doctor that is a woman. It could save your life.
Women are at a potentially fatal disadvantage on the operating room table, according to a “troubling” new study of more than 1.3 million patients treated by 2,937 doctors.
Gender presents a life-or-death risk for women, the study finds, with females 15% more likely to die or incur serious complications if operated on by a male surgeon, medical researchers at Vanderbilt University in Nashville, Tennessee and University of Toronto in Ontario, Canada reported.
They based their joint analysis — conducted from November 2020 to March 2021 and published this month in JAMA Surgery — on data from 1,320,108 patients who received both elective and medically necessary surgeries between 2007 and 2019.
Of that group, 717,548 were “sex discordant” — meaning the surgeon and patient were of different genders (more than 180,000 of those being women with male surgeons — and adverse outcomes). However, average rates of patient mortality and related complications improved about equally among all other scenarios, whether women operated on women, women on men or men on men.
“What is surprising and troubling is that negative outcomes, including complications and death, were linked to sex discordance,” said Florida surgeon Dr. Amalia Cochran in a published research letter tied to the study. “Unfortunately, this association disproportionately affected female patients. The association between surgeon-patient sex discordance and outcomes sounds the alarm for urgent action.”
The research team co-led by Dr. Cochran and Dr. Andrea N. Riner also accounted for age, health and other conditions that could give way to surgical complications.
Study authors said more research is needed to determine the root of the results, but Cochran suggested a greater need to promote more women going into medicine, as men by far dominate the field, with male doctors still outnumbering female doctors, 64% to 36%, according to 2019 data from the Kaiser Family Foundation.
“In 2019, only 22% of general surgeons in the US were women, and orthopedic surgery had the lowest representation of female surgeons at 5.8%,” Dr. Cochran said, citing statistics from the Association of American Medical Colleges.
“However, self-reflection is warranted on the way in which we provide care,” she added. “Surgeons likely believe they provide the same quality of care to patients irrespective of identity. However, these data underscore an under-appreciated phenomenon and highlight a measurable repercussion of implicit bias.”
Meanwhile, past studies suggest that women may actually make more ideal doctors. Similar research published in 2018 found that death rates among 580,000 heart patients in Florida emergency rooms were overall lower if treated by female doctors compared to when men wore the white coats.
The difference was marginal in another 2016 study — a margin of 32,000 lives, that is. More than 1.5 million hospitalized Medicare patients were found less likely to die at the hospital or be readmitted after seeing a female doctor. The difference was only a half percentage point overall, but made tens of thousands of lives of difference.
717 notes
·
View notes
Note
What did you learn about people? How might a person who is not studying develop their bullshit-ometer?
“What did you learn about people” is much too broad to answer given how much is covered in a three year bachelors degree. Everything from theories of the self, errors biases and heuristics, attitudes and emotions, theories behind behaviours, social influence, group affiliation, psychological development from childhood to adulthood and its effect, models of personality and individual differences, memory, how we learn, the psychology of choice and decisions, and the genetic/biological/social/environmental factors of all of the above and what happens when it goes wrong and becomes pathology.
In terms of developing a bullshit-ometer, or improving your judgement and understanding of evidence, the key is practice. For a module in my first year we were given a paper every week and a prompt sheet to fill in that effectively helped you tear the paper apart. Prompts included everything from the method and sample size, to the statistical tests used, whether they were used appropriately, and whether all of the assumptions of each test were met, etc. It would take me upwards of two hours to get through a ten page paper, and even then I’d miss things. Three years on, I can skim a paper or article or hear a person’s argument, spot any major red flags, and tear it apart under exam conditions in thirty minutes. It takes a lot of time and work to be able to do it quickly. Having it embedded as a philosophy into everything you’re learning helps as you start doing it unconsciously eventually.
Resources:
Bad Science by Ben Goldacre. To me, an absolutely essential read.
The Art of Statistics by David Spiegelhalter. Spiegelhalter is a statistical genius, and he’s now spending his time trying to change the way statistics is taught, moving it away from learning loads of formulas and then trying to figure out how they relate to evidence, towards the PPDAC (problem, plan, data, analysis, conclusion) model. To understand evidence and pick up the misuse of statistics (aka bullshit) you need at least a basic understand of stats. This book does it perfectly, in plain English, with interesting examples. I wish it had been published when I first started my degree.
I Think You’ll Find It’s A Bit More Complicated Than That by Ben Goldacre. This is a collection of most of Ben Goldacre’s columns which used to appear in The Guardian, in which he takes a claim in the media or a new study and tears it apart. It’s an interesting read, might change your perception on a few things, and is him tackling bullshit in practice.
Reckoning With Risk by Gerd Gigerenzer. There are lots of complex statistics in this (which he signposts and you can just pass over), but understanding how statistics of risk work, and what they mean, will completely change how you read and assess a lot of claims made in the news.
The Students 4 Best Evidence blog. It mainly covers evidence based medicine, but the key concepts transfer to all research and claims outside of medicine. Anything under the bias, critical thinking, intro to evidence-based practice, and statistics topics is relevant. Particularly anything tagged ‘tutorials and fundamentals’. Their Key Concepts Archive is a good place to start.
The Testing Treatments website. Again, covers medicine, but most of the points generalise out. Under each concept, say ‘association is not causation’, there is a ‘find learning resources’ link that will find papers, online courses/modules, and books about that concept.
Cochrane Training. Cochrane are the gods of the systematic review. All their online learning modules surrounding assessing evidence are here.
Think Again: How to Reason and Argue, either the book, or the online course. The perfect crash course in reasoning, arguing, avoiding fallacies, picking apart other people’s arguments, and finding bullshit.
The Clearer Thinking website has a range of tools/mini modules. Relevant ones here:
How well can you tell reality from B.S.?
Interpreting evidence
Belief challenger, making your views more accurate
Guess which experiments replicate
More books.
A Field Guide to Lies and Statistics: A Neuroscientist on How to Make Sense of a Complex World by Daniel Levitin
How To Lie With Statistics by Darrell Huff
306 notes
·
View notes
Text
Topic selected comparing Average Length of Stay between Acute Care and Not Acute Care Hospitals”. He wants us to review 5 articles on literature reviewed. There are 2 parts to this assignment. Part 1 is a qualitative analysis using Review Manager 5 tools to analyze the risk of bias for 5 articles from the literature on the topic your group selected. Part 2 is a quantitative data analysis design, the report on that design, the actual analysis of the data, (again) based on the topic your group selected, and a report of the findings. The following are the main steps to perform this team project. When writing your report for this assignment, please use the section headers and the numbering for the various steps outlined below (starting from step #2.1): Step #2: Performing the Qualitative analysis 2.1. This section of the assignment is aimed at giving students an opportunity to select and analyze at least 5 articles using the ‘Review Manager 5’ tools. The tools will enable you to analyze the risk of bias for the 5 selected articles following these steps: Setting Up Review Manager 5 Make sure that RevMan is currently in the ‘Non-Cochrane’ mode (not “Standard” mode). You can set that as Tools > Preferences > General > enable ‘Non-Cochrane mode’ When RevMan 5 opens, click on the blank page icon in the top left-hand corner. This will bring up the new review wizard and you can then write your review and save it to your computer. You should not see any interface with the Cochrane login or the Cochrane server. Information sources and search strategy Report on which published literature sources you searched, which keywords you used, and whether you limited your search to particular publication years. Create your keywords from your research topic. So, your objective should be to select from the published literature, at least 5 studies based on the keywords you created. They should be studies that were published to answer the same research question you are answering with your group research topic. For each of the studies you decide to include in your review, complete “Table 1 – Literature Review Analysis – by Your Name” in your assignment report. As we discussed earlier two separate members of your group should do this independently (that means you don’t share information while you are doing any of this). At the end when you have put together your final group report, of course, everyone in the group will see these two sets of separate tables (Table 1 and Table 2.) Using Review Manager 5 Note: There is a Tutorial for RevMan that comes in PDF format that accompanies the software when you install it on your computer desktop. It is called “rm5tutorial.pdf” The data you used to complete Table 1 is then analyzed using non-Cochrane mode in the RevMan 5.4 software. The methodological quality of each study is assessed using The Cochrane collaboration’s tool for assessing the risk of bias. Follow the guidance in the Cochrane Handbook for Systematic Reviews (Higgins, 2011), to assess whether study authors took adequate steps to reduce the risk of bias across five domains: – Selection bias, – Performance bias, – Detection bias – Attrition bias, – Reporting bias. The judgment of studies for potential bias should be reported in “Table 2 – Literature Review, Table of Biases – by Your Name” using only one of the following letters: Y, N, or U, where ‘Y=low risk’, ‘N=high risk, or ‘U=unclear risk’, for each respective source of bias. So, I expect to see in your group report two sets of the following 2 tables (4 tables) for the Qualitative Analysis: Table 1: Literature Review Analysis – by 1st Team member (specify name) Table 2. Literature Review, Table of Biases – by 1st Team member (specify name) Table 1: Literature Review Analysis – by 2nd Team member (specify name) Table 2. Literature Review, Table of Biases – by 2nd Team member (specify name) Report your method and procedure for performing the qualitative analysis in this section (2.1) of your report.
Reference Cochrane Handbook for Systematic Reviews of Interventions. (n.d.). Retrieved July 12, 2019, from https://training.cochrane.org/handbook 2.2. Report your findings in a Literature Review Analysis table and using Bias-Tables and Bias-Plots. Table 1: Literature Review Analysis – by Your Name Authors, Year of Publication Intervention/ Policy evaluated Study design/ Time Period Data/ Study Population Relevant Findings/ Recommendations Author1, YYYY Author2, YYYY Author3, YYYY Author4, YYYY Author5, YYYY ETC. Table 2. Literature Review, Table of Biases – by Your Name Selection Bias Performance Bias Detection Bias Attrition Bias Reporting Bias Authors, Year of Publication Systematic differences between baseline characteristics of the groups that are compared. Systematic differences between groups in the care that is provided, or in exposure to factors other than the interventions of interest. Systematic differences between groups in how outcomes are determined. Systematic differences between groups in withdrawals from a study. Systematic differences between reported and unreported findings. Author1, XXXX Y Y Y Y Y Author2, XXXX Author3, XXXX Author4, XXXX Author5, XXXX ETC. Note: Y: Low risk N: High risk U: Unclear Figure 1 – Bias Plot – You may create a plot of your bias findings. Your plot should be to illustrate your major findings from your bias analysis in Table 2. For example a funnel plot or just a column or bar chart. Comment on your findings in Table 2, and Figure 1. ORDER THIS PAPER NOW. 100% CUSTOM PAPER CategoriesMarketing homework help Leave a Reply Cancel replyYour email address will not be published. Required fields are marked *Comment * Name * Email * Website Save my name, email, and website in this browser for the next time I comment. Post navigation Previous PostPrevious The paper for HCM 1143 is to view one of the movies listed below and write a research paper on an aspect of the film related to healthcare administration.Next PostNext Data Analysis and Report
0 notes
Text
Association of COVID-19 infection and the risk of new incident diabetes: a systematic review and meta-analysis - Published Aug 25, 2024
Background: As the world population recovers from the COVID-19 infection, a series of acute sequelae emerge including new incident diabetes. However, the association between COVID-19 infection and new incident diabetes is not fully understood. We purpose to determine the risk of new incident diabetes after COVID-19 infection.
Methods: PubMed, Embase, and Cochrane Library were used as databases to search for cohort studies published from database inception to February 4, 2024. Two reviewers independently conducted the study screening, data extraction, and risk of bias assessment. A random-effects model was adopted to pool the hazard ratio (HR) with corresponding 95% confidence intervals (CI). Subgroup analysis was conducted to explore the potential influencing factors.
Results: A total of 20 cohort studies with over 60 million individuals were included. The pooling analysis illustrates the association between COVID-19 infection and an increased risk of new incident diabetes (HR = 1.46; 95% CI: 1.38-1.55). In subgroup analysis, the risk of type 1 diabetes was HR=1.44 (95% CI: 1.13-1.82), and type 2 diabetes was HR=1.47 (95% CI: 1.36-1.59). A slightly higher risk of diabetes was found in males (HR=1.37; 95% CI: 1.30-1.45) than in females (HR=1.29; 95% CI: 1.22-1.365). The risk of incident diabetes is associated with hospitalization: non-hospitalized patients have an HR of 1.16 (95% CI: 1.07-1.26), normal hospitalized patients have an HR of 2.15 (95% CI: 1.33-3.49), and patients receiving intensive care have the highest HR of 2.88 (95% CI: 1.73-4.79).
Conclusions: COVID-19 infection is associated with an elevated risk of new incident diabetes. Patients ever infected with COVID-19 should be recognized as a high-risk population with diabetes.
#mask up#pandemic#covid#covid 19#wear a mask#public health#coronavirus#sars cov 2#still coviding#wear a respirator#diabetes#long covid
5 notes
·
View notes
Text
Systematic review of the prevalence of Long Covid
Preliminary report; Background: Long Covid occurs in those infected with SARSCoV2 whose symptoms persist or develop beyond the acute phase. We conducted a systematic review to determine the prevalence of persistent symptoms, functional disability or pathological changes in adults or children at least 12 weeks post-infection. Methods: We searched MEDLINE (Ovid), Embase (OVID), the Cochrane Covid-19 Study register, WHO ICTRP, medRxiv, Cochrane CENTRAL, MEDLINE (PubMed), ClinicalTrials.gov, and the WHO Global research on coronavirus disease (COVID-19) database from 1st January 2020 to 2nd November 2021, limited to publications in English. We included studies with at least 100 participants. Studies where all participants were critically ill were excluded. Articles were screened independently by two reviewers, with disagreements resolved by a third. Long Covid (primary outcome) was extracted as prevalence of at least one symptom or pathology, or prevalence of the most common symptom or pathology, at 12 weeks or later. Heterogeneity was quantified in absolute terms and as a proportion of total variation and explored across pre-defined subgroups (PROSPERO ID CRD42020218351). Findings: In total 120 studies in 130 publications were included. Length of follow-up varied from 12 weeks to over 12 months. Few studies had low risk of bias. All complete and subgroup analyses except one had I2 [≥] 90%, with prevalence of persistent symptoms ranging between 0% and 93%. Studies using routine healthcare records tended to report lower prevalence of persistent symptoms/pathology than self-report. However, studies systematically investigating pathology in all participants at follow up tended to report the highest estimates of all three. Studies of hospitalised cases had generally higher estimates than community-based studies. Interpretation: The way in which Long Covid is defined and measured affects prevalence estimation. Given the widespread nature of SARSCoV2 infection globally, the burden of chronic illness is likely to be substantial even using the most conservative estimates. https://www.medrxiv.org/content/10.1101/2022.11.06.22281979v1?rss=1%22&utm_source=dlvr.it&utm_medium=tumblr Read more ↓
0 notes
Text
931 da paina

Results Of 4212 citations reviewed, 60 reports with 6404 participants were included in the meta-analysis. The secondary outcomes were opioid dose, opioid misuse, opioid craving, disability, or function. Main Outcomes and Measures The primary outcome was pain intensity. Meta-analyses were conducted using standardized mean differences in pain and opioid dose to obtain aggregate estimates of effect size with 95% CIs. Study Selection Randomized clinical trials that evaluated the use of MBTs for symptom management in adults also prescribed opioids for clinical pain.ĭata Extraction and Synthesis Independent reviewers screened citations, extracted data, and assessed risk of bias. The gray literature,, and relevant bibliographies were also searched. Search logic included (pain OR analgesia OR opioids) AND mind-body therapies. Objective To evaluate the association of MBTs with pain and opioid dose reduction in a diverse adult population with clinical pain.ĭata Sources For this systematic review and meta-analysis, the MEDLINE, Embase, Emcare, CINAHL, PsycINFO, and Cochrane Library databases were searched for English-language randomized clinical trials and systematic reviews from date of inception to March 2018. Knowing whether mind-body therapies may benefit patients treated with opioids for acute, procedural, and chronic pain conditions may be useful for prescribers, payers, policy makers, and patients. Importance Mind-body therapies (MBTs) are emerging as potential tools for addressing the opioid crisis. Shared Decision Making and Communication.Scientific Discovery and the Future of Medicine.Health Care Economics, Insurance, Payment.Clinical Implications of Basic Neuroscience.Challenges in Clinical Electrocardiography.RoB for Guided Imagery StudiesĮFigure 13. Meta-analysis of Cognitive-Behavioral Therapy Studies on Pain OutcomesĮFigure 12. Meta-analysis of Suggestion Studies on Pain OutcomesĮFigure 5. Meta-analysis of Relaxation Studies on Pain OutcomesĮFigure 4. Meta-analysis of Hypnosis Studies on Pain OutcomesĮFigure 3. Meta-analysis of Meditation Studies on Pain OutcomesĮFigure 2. Findings of Therapeutic Suggestion StudiesĮFigure 1. Characteristics of Therapeutic Suggestion StudiesĮTable 9. Findings of Guided Imagery StudiesĮTable 8. Characteristics of Guided Imagery StudiesĮTable 7. Characteristics of Relaxation StudiesĮTable 6. Characteristics of Hypnosis StudiesĮTable 5. Characteristics of Meditation StudiesĮTable 3.

0 notes
Text
Risk Factors for Severe Hemorrhage Requiring Blood Transfusion Associated With Percutaneous Nephrolithotomy: A Systematic Review and Meta-Analysis
Abstract
Purpose: The aim of this meta-analysis was to systematically assess the risk factors for severe hemorrhage requiring blood transfusion associated with percutaneous nephrolithotomy, so that the urologist can prevent the occurrence of severe bleeding as soon as possible.
Materials and Methods: PubMed, Embase and The Cochrane Library were searched to collect the case-control studies on risk factors for severe hemorrhage requiring blood transfusion associated with percutaneous nephrolithotomy (PCNL) through Nov. 9, 2020. Eligible data was screened, extracted, and the risk of bias assessed independently by two qualified investigators. We then calculated the odds risks (ORs) and corresponding 95% confidence intervals (CIs) to assess the relationships between risk factors and severe hemorrhage requiring blood transfusion associated with PCNL.
Results: Eight case-control studies involving 5,974 patients were screened. In this meta-analysis, the risk factors were extracted as follow: gender, hypertension, diabetes mellitus, multiple tracts, staghorn calculi, previous PCNL, grade of hydronephrosis (moderate and severe), calyx of puncture (lower, middle, upper, multiple calices). Among them, diabetes mellitus (95% CI: 1.13 – 3.22, OR = 1.90, P = .016), multiple tracts (95% CI: 2.28 – 7.02, OR = 4.00, P = .000), staghorn calculi (95% CI: 1.34 - 4.08, OR = 2.34, P = .003), upper calyx (calyx of puncture) (95% CI: 0.40 - 0.86, OR = 0.59, P = .006), multiple calices (calyx of puncture) (95% CI: 1.79 - 3.20, OR = 2.39, P = .006) were statistically significant (all P < 0.05).
Conclusions: Our meta-analysis showed that diabetes mellitus, multiple tracts, staghorn calculi, multiple calices (calyx of puncture) are risk factors for severe hemorrhage requiring blood transfusion associated with PCNL, so we should focus on their prevention. Moreover, upper calyx (calyx of puncture) is a protective factor, the urologist may choose upper pole access as percutaneous nephrolithotomy tract to minimize intraoperative and postoperative blood loss
Read more about this article: https://lupinepublishers.com/pharmacology-clinical-research-journal/fulltext/risk-factors-for-severe-hemorrhage-requiring-blood-transfusion.ID.000146.php
Read more Lupine Publishers Google Scholar articles: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=iaV0YGcAAAAJ&citation_for_view=iaV0YGcAAAAJ:NJ774b8OgUMC
0 notes
Text
Science and Chemistry Classes
Stars align for fintech, but regulators are wary of dangerous risks
But as the stars promote the digitalization of financial services, tossing phrases such as fintech, blockchain, artificial intelligence, digital assets, Bitcoin and machine learning into popular culture, regulators and lawmakers are moving more slowly, worried about the downside of innovations that could transform daily life.
Among the fears are that the technology is too complicated for many consumers; poses security, privacy, consumer protection and discrimination risks; and consumes too much energy as politicians, companies and consumers increasingly worry about climate change. The decentralized character of some of the technology even raises questions about what entity can be regulated.

"The velocity and magnitude of marketplace change coming in the crypto space—cryptoassets, blockchains, central bank digital currencies, DeFi, Web3, DAOs, the metaverse—is unlike anything we've seen in our lifetimes," said Jo Ann Barefoot, CEO of the Alliance for Innovative Regulation.
A former deputy comptroller of the currency and staff member for the Senate Banking Committee, Barefoot said industry and regulators don't even agree on a catchall term for all the innovations, much less on how to regulate it.
"These innovations are also mold-breakers, in terms of who is supposed to regulate what at the federal, state and international level, and in terms of how to get leverage on them," she said.
Government reports, including from international organizations, hint at the challenge.
"Economies rely on central authorities and trusted intermediaries to facilitate business transactions. Blockchain is a technology that could reduce the need for such entities," the Government Accountability Office said in a March report. It also said blockchain-based financial applications can facilitate illicit activity and may reduce consumer and investor protections compared to traditional finance.
The GAO found that blockchain is useful for some applications but limited or even problematic for others. Blockchain's resistance to tampering, for example, may make it suitable for applications with many participants who don't trust each other, but it may be too complex for uses where the participants trust each other, the GAO said.
The International Organization of Securities Commissions warned last month that decentralized finance, or DeFi, may remove intermediaries such as banks and brokers, institutions that are closely regulated. The result may be investors deprived of advice, lack of capital controls and compliance measures, it said.
"Absent these intermediaries—and without appropriate substitute mechanisms—the risk for investor and market harm may be exacerbated," IOSCO said. "Most of the new services which are emerging replicate more traditional financial services and activities, but with weaker regulation and increased risks for investors."
Melissa Koide, the CEO of FinRegLab, a Washington research group, and Kelly Thompson Cochran, the group's deputy director, are trying to use their ties to the fintech industry and to Capitol Hill to draw attention to the technology's potential benefits, but also to raise red flags about over-reliance.
Koide said by email and in an interview that artificial intelligence and machine learning, combined with new types of data, present enormous potential to improve financial inclusion and equality but also enormous risk of deepening bias and exclusion.
"Careful, use-case specific research to understand how AI/ML with new data may affect consumers is essential to getting the rules of the road right in terms of how we regulate to protect people while making sure the benefits of the more complex analytics are trustworthy, inclusive, and beneficial," she said.
Koide said FinRegLab will release empirical research evaluating just those questions in the context of consumer credit this month at a symposium on artificial intelligence that the group is co-hosting with the Commerce Department, the National Institute of Standards and Technology, and the Stanford Institute for Human-Centered Artificial Intelligence.
She said the symposium will have representatives of government, industry, advocacy and academia address how these technologies, particularly in sectors like financial services and health care, relate to ensuring inclusive economic growth, supporting diversity and financial inclusion, and mitigating risks such as bias and unfairness.
Before establishing FinRegLab, Koide spent four-and-a-half years in President Barack Obama's administration as the Treasury Department's assistant secretary for consumer policy. She helped lead the creation of Treasury's "myRA" program, designed to help low- and middle-income earners begin saving for retirement. The Trump administration shut down the program in 2017, saying it wasn't cost effective.
Utopia or dystopia?
Barefoot said the technology is offering a utopian versus dystopian moment.
"New financial technologies, broadly defined, are either going to make financial services a lot better or a lot worse, depending on how we regulate them," she said.
"Every innovation, from AI to encryption to blockchain, has potential to bring breakthroughs in fixing longstanding problems like financial access, inclusion and fairness," she said. "They also could make everything worse by introducing or exacerbating bias and eroding privacy."
Barefoot said Congress and regulators face challenges that are arguably even greater than those in the financial crisis because the issues are more novel.
"Regulators are facing incredible challenges in figuring out how best to regulate new technologies in finance. Speaking as a former bank regulator, I think the single best step they can take is to use these technologies, themselves. That will be the fastest way to understand them."
As regulators and the industry assess the financial strengths and weaknesses of the innovation, others are seeing it against a backdrop of climate change and global warming.
The GAO report noted evidence that blockchains use more energy than traditional centralized databases because they must store copies of transactions across several or many computers.
A 2019 study in the energy journal Joule estimated that Bitcoin, the most popular cryptocurrency, had annual emissions between 22 million and 22.9 million metric tons of carbon dioxide, about as much as the nations of Jordan and Sri Lanka combined. A 2021 report by Galaxy Digital Holdings Ltd., an asset management company, estimated that Bitcoin networks consume around half the energy of the banking or gold industries.
Bitcoin's electricity use also results from its miners' need for high-powered computers to solve the complex mathematical equations that unlock new bitcoins, of which there is a finite amount. Unlocking Bitcoins gives the miners a big payout, which in turn provides the incentive to maintain the network.
The influx of Bitcoin miners to areas with access to cheap and plentiful energy has brought attention from Congress. Energy costs and demands of blockchain technology are of particular concern to lawmakers from states that have access to cheap power. Bitcoin miners have flooded to areas such as Washington state, New York and Montana because of the availability of low-cost hydroelectricity.
Washington state is experiencing "a tremendous increase in electricity demand attributed to mining of Bitcoin," Sen. Maria Cantwell, D-Wash., said at a Senate Energy and Natural Resources Committee hearing in August 2018. "To put this into context, a recent estimate found that a single bitcoin transaction uses as much electricity as an average household in the Netherlands uses in a month."
Montana Sen. Steve Daines, a Republican, said at the same hearing that his state has two Bitcoin mining facilities that collectively require about 80 megawatts of electricity, "sometimes surpassing even traditional mining projects." He expressed concern that as the demand from Bitcoin miners increases, it could pose a threat to energy supply and prices for Montana as a whole.
Brandon Dalling, a partner at the New York office of the international law firm King & Spalding, agreed that coin-mining is "energy intensive." He said the Pacific Northwest's cheap, low-cost hydro power has made it an attractive location for crypto-mining. This has proved popular with some segments of the local population who see the miners adding to the tax base.
20/04/2022
_Shiv Prakash
0 notes
Text
Use of Anti-Inflammatory Drugs in the Treatment of Parkinson’s Disease: A Systematic Review of Perimental Studies - BJSTR Journal

Use of Anti-Inflammatory Drugs in the Treatment of Parkinson’s Disease: A Systematic Review of Perimental Studies by Roberto de Barros Silva* in Biomedical Journal of Scientific & Technical Research
https://biomedres.us/fulltexts/BJSTR.MS.ID.006255.php
The inflammatory nature of Parkinson’s disease (PD) in the central nervous system contains inflammatory structures such as alpha-synuclein, interleukins and several other modulators. In view of this characteristic, it is observed the possibility of using anti-inflammatory drugs to combat the injury profile of structures related to the pathophysiology of the disease. This study aims to do a review of the literature on preclinical studies addressing the efficacy of anti-inflammatory drugs in PD. For this study has performed a systematic review elaborated according to the Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P)5. Pubmed, LILACS, EMBASE, MEDLINE and Web of Science databases were searched in the period 2000-2019, without language restriction, containing clinical or pre-clinical studies based on the association of keywords: Parkinson’s; corticosteroid; anti-inflammatory; neuroprotection. The articles were independently selected by two reviewers in three stages: screening by title, by abstract and by full reading of the article. All articles were investigated for their methodological quality using the ACROBAT-NRSI scale (“A Cochrane Risk of Bias Assessment Tool for Non-Randomized Studies”) 4. We have found Twenty-one articles that were analyzed and separated between two groups according to the drug used for preclinical study, anti-parkinsonian drugs of anti-inflammatory nature and drugs properly anti-inflammatory drugs (IINES and corticosteroids). Improvement in motor function, decreased movement patriotization, increased levels of striatal dopamine, decreased interleukins and blockage of inflammatory pathways, such as those participating in MPP+ and COX-2, as well as increased and/or decreased loss of neurons armed with tyrosine hydroxylase (TH) enzyme, an important marker of neuroprotection, were identified. Thus the analyzed articles demonstrated an effective anti-flame response and effective neuroprotection in the two groups of drugs, with a therapeutic alternative and promising line of study in PD.
For more articles Journals of Biomedical Science please click here
bjstr
Follow on Twitter : https://twitter.com/Biomedres01 Follow on Blogger :https://biomedres01.blogspot.com/ Like Our Pins On : https://www.pinterest.com/biomedres/
#Biomedical Research Articles#Biomedical Science Articles#Journal of Scientific and Technical Research#Open access medical journal#Free medical journal
0 notes