#COPD diagnosis
Explore tagged Tumblr posts
Text

Explore cutting-edge COPD treatment options. Stay informed with new developments in COPD care.
0 notes
Text
#Sudden shortness of breath#Dyspnea causes#Asthma attacks#Heart failure symptoms#Pulmonary embolism treatment#Pneumonia breathing issues#COPD exacerbation#Anxiety shortness of breath#Panic attacks and breathing#Allergic reactions anaphylaxis#Obesity and breathing problems#Respiratory infections#ARDS causes#Shortness of breath emergency#Breathing difficulties#When to seek medical help for breathlessness#Emergency shortness of breath#Breathing problems solutions#Breathing exercises for anxiety#Shortness of breath diagnosis#health & fitness
1 note
·
View note
Text
Copd Awareness: Types, Causes, Symptoms, and Prevention Tips
Delve into COPD Awareness: Chronic lung diseases like emphysema & chronic bronchitis caused by smoking. Symptoms include coughing & shortness of breath.
To know more: https://lalithachestandskinhospital.com/blog/copd-awareness-types-causes-symptoms-and-prevention-tips/
chest specialist doctor,best lung doctor in Karimnagar,good pulmonologist near me,breathing problem specialist doctor,copd diagnosis treatment,pulmonologist hospital near me,chronic obstructive pulmonary treatment

#chest specialist doctor#best lung doctor in Karimnagar#good pulmonologist near me#breathing problem specialist doctor#copd diagnosis treatment#pulmonologist hospital near me#chronic obstructive pulmonary treatment
0 notes
Text
Ultimate Guide to Respiratory Tract Infections: Symptoms, Diagnosis, and Evidence-Based Treatments for URTIs and LRTIs
Upper Respiratory Tract Infections (URTIs) Introduction Respiratory tract infections (RTIs) encompass a wide range of conditions affecting the upper and lower respiratory tracts. They are common ailments that cause significant global morbidity and economic loss. This comprehensive guide covers everything you need to know about RTIs, from symptoms and diagnosis to evidence-based treatments and…
#Acute Bronchitis#Acute Bronchitis Management Guidelines#Bronchiolitis#Clinical Scores for Strep Throat#COPD Exacerbation#COPD Exacerbation Causes and Solutions#COVID-19 Symptoms#COVID-19 vs Influenza Symptoms#How to Treat Sinusitis and Pharyngitis#Lower Respiratory Tract Infections#Pharyngitis#Pneumonia#Pneumonia Diagnosis and Care#Respiratory Tract Infections#Respiratory Tract Infections Treatment#RSV Symptoms and Treatment#Sinusitis
0 notes
Note
Have you seen the terrifying animal-shaped kids' exam tables, and if so what is your opinion as a medical professional
i.e. should every hospital room have vaguely uncomfortable animal sculpture furniture perhaps
I have never seen or heard of them, lemme google them real quick




THEY SHOULD BE MANDATORY. THAT IS WHAT YOU SHOULD BE SITTING ON AS YOU GET YOUR COPD DIAGNOSIS.
2K notes
·
View notes
Note
I wanna know ur HCs for Mod AU jayvik 💕
OOOO this is an interesting one because I usually don't indulge in most modern aus of anything, but I shall try.
ask me about arcane!
Both are graduate students at the academy. Both double-majored in Engineering for undergrad, but Jayce's is Mechanical and Electrical, and Viktor's is Mechanical and Chemical. They are in graduate school for Mechanical Engineering, though. Over-achievers, they are. The school is equivalent to MIT. Or is MIT, technically, if you want to make it USA-centered.
They met in a Thermodynamics class (yes, i had to look up types of classes for this lmao) and became fast friends because everyone else around them was extremely obnoxious and very annoying. They started dating two semesters before Viktor graduated, three before Jayce graduated.
For a few semesters, everyone thought they would be rivals, because they were always trading spots in GPA rankings and scores. Everyone thought the tension they were catching was academic hatred, until a library assistant caught them making out in a study room, and then everyone in the engineering school collectively went "ohhhhh"
Both are at the academy on scholarship, Jayce has a few for welding competitions and even some money from art competitions, and Viktor's schooling is being paid for from essays and whatever grants he can get his hands on. Both are determined to have very little student loans. Viktor is also a graduate assistant to the dean of engineering (similar to canon) which pays for his portion of housing (with Jayce).
Jayce has been offered spots on sports teams all the time. He does not know how to explain he has the coordination of a baby deer on ice. He likes to work out, but it's mostly for long days in the labs and blacksmithing he does, which is something he likes to be traditional for. His excuse is that his schooling and work take up too much time for sports.
Viktor is also an international student, having transferred from his home-country university his sophomore year. He and Jayce (who moved to the city when he was 15 from out of the country) related on this very fast.
Sky, Mel and Elora are all apart of the international student club with Viktor. They are all besties. Caitlyn and Vi are Jayce's friends from home (Caitlyn is his "cousin" and he teases Vi, the GF, all the time) and Catvi are undergrad students. All of them like to meet at the "secret" coffeeshop on campus (aka the one people can never find, because it's in the back of an office building).
Jayce and Viktor organized a sit-in when the campus president and campus board (not Dean of Engineering Heimerdinger) routed money from programs that helped campus-accessibility for students with disabilities to a new stadium. It lasted twenty days, five members quit the board, and the money was routed back to fixing elevators, automatic doors, and providing more covered benches.
Jayce was student-class president his junior year, but stopped working on the student council when it took too much time away from Viktor and his friends. Viktor is thankful for it. (Jayce also ran away screaming from the guys trying to get him to rush for frats).
Both want to start their own company when they graduate, focusing on public health and progress, with things like air and water purifiers, teaming up with medical companies for robotic prosthetics, lung + heart mechanical help.
Viktor got sick the winter between his graduation and what was supposed to be the start of grad school. He was diagnosed with severe acute asthma, pneumonia, but just barely avoided a COPD diagnosis with treatment. He was in the hospital for a month and a half, now takes breathing treatments a few days a week, and goes to doctor appointments once a month.
Jayce was so worried, he almost had to delay his own graduation. Viktor managed to convince him to get it together in time to pass with good marks and keep his spot in his grad cohort, while Viktor had to delay his grad school start by a semester, rather than in the spring like he planned. This is why they are in the same cohort, because Viktor had to start later than planned. (Jayce secretly likes that they have all their classes together, even if he's sad for the reason why).
im sure ill have more at some point, bc it is a little interesting!
41 notes
·
View notes
Text
Also preserved on our archive
Another perfect example of how masking to help prevent covid keeps us *all* safer from *all* airborne illness.
by Tamara Schneider
Lingering respiratory viruses set the stage for chronic lung disease, mouse study shows
Doctors have long known that children who become seriously ill with certain respiratory viruses such as respiratory syncytial virus (RSV) are at elevated risk of developing asthma later in life. What they haven’t known is why.
A new study by researchers at Washington University School of Medicine in St. Louis may have solved the mystery. The study, in mice, shows that respiratory viruses can hide out in immune cells in the lungs long after the initial symptoms of an infection have resolved, creating a persistently inflammatory environment that promotes the development of lung disease. Further, they showed that eliminating the infected cells reduces signs of chronic lung damage before they progress to a full-blown chronic respiratory illness.
The findings, published Oct. 2 in Nature Microbiology, point to a potential new approach to preventing asthma, chronic obstructive pulmonary disease (COPD) and other chronic lung diseases by eradicating the persistent respiratory viruses that fuel these conditions.
“Right now, children who have been hospitalized for a respiratory infection such as RSV are sent home once their symptoms resolve,” said senior author Carolina B. López, PhD, a professor of molecular microbiology and a BJC Investigator at WashU Medicine. “To reduce the risk that these children will go on to develop asthma, maybe in the future we will be able to check if all of the virus is truly gone from the lung, and eliminate all lingering virus, before we send them home.”
About 27 million people in the U.S. are living with asthma. Many factors influence a person’s likelihood of developing the chronic breathing illness, including living in a neighborhood with poor air quality, having exposure to cigarette smoke and being hospitalized for viral pneumonia or bronchitis while young. Some researchers — López included — suspected that the link between serious lung infection and subsequent asthma diagnosis was due to lingering virus in the lungs that causes ongoing damage, but a direct link between the ongoing presence of virus and chronic lung disease has not been previously shown.
López and first author Ítalo Araújo Castro, PhD, a postdoctoral researcher in her lab, developed a unique system involving a natural mouse virus known as Sendai virus, and fluorescent markers of infection. Sendai is related to human parainfluenza virus, a common respiratory virus that, like RSV, has been linked to asthma in children. Sendai behaves in mice in very much the same way that human parainfluenza virus behaves in people, making it an excellent model of the kinds of infections that could lead to chronic lung disease.
Using the fluorescent trackers, the researchers could observe signs of the virus throughout infection. After about two weeks, the mice recovered, but viral RNA and protein were still detectable several weeks later in their lungs, hidden away in immune cells.
“Finding persistent virus in immune cells was unexpected,” López said. “I think that’s why it had been missed before. Everyone had been looking for viral products in the epithelial cells that line the surface of the respiratory system, because that’s where these viruses primarily replicate. But they were in the immune cells.”
Moreover, the presence of the virus changed the behavior of the infected immune cells, causing them to become more inflammatory than the uninfected immune cells. Persistent inflammation sets the stage for chronic lung disease to arise, the researchers said. Indeed, seven weeks after infection, the mice’s lungs exhibited inflammation of air sacs and blood vessels, abnormal development of lung cells and excess immune tissue — all signs of chronic inflammatory lung damage, even though the mice appeared outwardly to have recovered. Once the infected immune cells were eliminated, the signs of damage diminished.
“We use a perfectly matched virus-host pairing to prove that a common respiratory virus can be maintained in immunocompetent hosts for way longer than the acute phase of the infection, and that this viral persistence can result in chronic lung conditions,” Castro said. “Probably the long-term health effects we see in people who are supposed to be recovered from an acute infection are actually due to persistence of virus in their lungs.”
The findings point to new ways to think about preventing chronic lung diseases, the researchers said.
“Pretty much every single child gets infected with these viruses before the age of 3, and maybe 5% get serious enough disease that they could potentially develop persistent infection,” López said. “We’re not going to be able to prevent children from getting infected in the first place. But if we understand how these viruses persist and the effects that persistence has on the lungs, we may be able to reduce the risk of serious long-term problems.”
Study: Castro IA, Yang Y, Gnazzo V, Kim DH, Van Dyken SJ, López CB. Murine parainfluenza virus persists in lung innate immune cells sustaining chronic lung pathology. Nature Microbiology. Oct. 2, 2024. DOI: 10.1038/s41564-024-01805-8
www.nature.com/articles/s41564-024-01805-8 (PAYWALLED)
#mask up#covid#pandemic#covid 19#wear a mask#public health#sars cov 2#coronavirus#still coviding#wear a respirator#flu#influenza#RSV#respiratory syncytial virus
43 notes
·
View notes
Note
Hiyaa lovely mods!
First of all, thank you for making this blog! I have read a lot of the posts you have linked in the FAQ, but still have some questions I need help with.
I am visually impaired myself, and am autistic, but I'm not physically disabled, which is why I want to make sure I do proper research (which I will do myself, but I've found that I need some pointers) for a character I'm writing.
It is an Arcane fanfic, the character in question is Viktor. He was born with a limp and chronically ill due to growing up in 'a toxic atmosphere', which was caused by fissures (in Zaun). In my fic he will be a veterinarian, but he will (still) be using a cane, and occasionally crutches or a wheelchair for low spoons/pain days. (I haven't been able to completely specify what diagnosis he has in my fic that matches canon, but I refuse to make him able-bodied.) I have tried to find the name/type of a (manual) wheelchair that has a feature to push the user up to stand (for brief periods) after fastening the legs, but so far I haven't been able to find an answer. Since he'll have to go out on calls sometimes to ranches/farms, he needs to be able to treat large animals too, even on days where his cane or crutches aren't enough.
Could you possibly point me in the right direction so I can continue doing research? Either way, I thank you for your time to read this and for all the work you all do! <3
Kind regards, Jeem
Hello, thank you for your ask! The type of wheelchair you’re looking for is called a manual standing wheelchair or a manual wheelchair with power stand up. Here are two sites that sell them if you need references [x] [x] (NOTE: I myself have not verified if these websites are safe to buy from, but they are safe to visit and have good photos!)
As for a starting place for deciding his disabilities, you can try looking up side effects of long term exposure to pollutants or radiation (just make sure what you’re reading is about the symptoms of chronic/long term exposure instead of acute).
Some common symptoms are:
- cancer
- asthma
- COPD
- cardiovascular disease
- issues with the kidney, lungs, brain, reproductive system and/or hormones
- immunodeficiency
And more!
And since I know a bit about Arcane, I’d like to mention that Viktor has hypertropia, which is when one eye points upward. It’s a small design detail so I understand a lot of fans missing it, but I just wanted to point it out because I appreciate it and hope any Arcane fans following consider adding it to their stories!
Here are two screenshots that I think show it well :] (smiley face


If you need any more help feel free to ask again!
Have a nice day!
Mod Rot
44 notes
·
View notes
Text
WOOOOT! I'm getting into pulmonary therapy almost two months earlier than planned! It was originally schedule for October 23rd, but I'm on the waiting list and someone cancelled their appointment. It's in just a few days! As for what it is, my asthma has been a nightmare, and the asthma specialist I've been seeing doesn't know what more they can do for me seeing as I'm allergic to one of the ingredients (milk protein, which is used to mask the flavor of the medicine) in the COPD medication she wants me to use. It makes my eczema flare up like fireworks on New Years Eve. She suggested and immunosuppressant, which I'm strongly opposed to seeing as I already get sick with extreme ease. The therapy is going to help me figure out how to basically breathe again. My doctor thinks I may also have reduced lung capacity due to the covid infection I had in 2022. Fun times!
Next week is going to be packed with doctor appointments now. Let's see, I have pulmonary therapy, an appointment with my PCP, and my twice monthly therapy. The following week, I'm getting an ECHO and EKG on the same day, and will leave with very angry skin because I'm allergic to adhesives. I'm still waiting for a PT clinic to contact me about the referral my doctor sent out when she diagnosed me with hEDS.
The place I had gone to for PT before the diagnosis is horrible. The doctor I was assigned to was an absolute nightmare, and the PT specialist was less than helpful. That doctor diagnosed me as hypermobile, but wouldn't say anymore "because that's not what this appointment is for." She spoke to me for less than ten minutes, told me I'm just imagining the pain in my wrists, informed me I must be incorrect about the ligament removal" in my right wrist "because that's not how things are done," and I need to give up my hobbies if I don't want to have problems.
Y'all, I gave up drawing, jewelry making, calligraphy, and writing by hand because of my right wrist. I'm not giving up making quilts nor playing video games, and need a keyboard I can physically split and set up at angles most favorable to me. A friend has helped me with the latter, but it's out of my budget for now.
Busy busy busy!
7 notes
·
View notes
Note
while idk if they're Offensive all the time some of the other personality disorder names piss me the hell off. Like actually "histrionic" sucks it's literally "wow ur overreacting" stupid disorder name. BPD- the borderline is bc it was seen as being on "The Borderline Between Psychotic and Neurotic" like. What. also looking up differences between OCD and COPD is. Quote from a website "The primary difference is that OCD includes obsessions/compulsions, while OCPD does not" THEN WHY IS IT CALLED OBSESSIVE COMPULSIVE PERSONALITY DISORDER. Anyway probably less stupid but more confusing is the disorders beginning with the Schizo prefix. Schizophrenia - generally known as a psychosis disorder, also has negative symptoms like flat affect/anhedonia/etc. Schizoaffective - generally seem to be defines as schizophrenia in conjunction with a mood disorder. Schizotypal PD - generally lacks hallucinations or delusions, but still have negative symptoms and "odd beliefs" that may not align with reality. Schizoid personality disorder: this one's just social it's literally just social. Also one of the core diagnostic criteria is asexuality (or some places say "lack of interest in sexual relationships" like can we please just redo this whole shit. Also schizoid USED to be synonymous with schizophrenia but now it refers to the more social disorder. (it's a little funny when ppl try to use "schizoid" as an insult similar to psychotic bc it's much closer to saying antisocial.) WAIT I FORGOT ASPD.... CRIME DISORDER tho that's more diagnosis than name. Personality disorder names/diagnoses are just a mess we gotta start over (also in other countries personality disorders have been like re categorized with new names in the International Classification of Diseases, being more... Umbrella terms now?? It's something idk) sorry for this long fuckin rant I gt fixated on Schizoid personality disorder bc Mental Illness and now my brain is full of ????
signed cause that was some TRUE SHIT you said!!!!
29 notes
·
View notes
Text
Health update!
So for those following health stuff, I got some great news today. I don't have COPD or Pulmonary Hypertension.
I did find out that my lungs are smaller than the average population (maybe about 90% the size) so they're working a bit harder than everyone else's and that's part of why I've been prone to pneumonia (which I started getting as a teen) and chronic bronchitis.
I also have a new trial medication to start, and some bloodtests to get. But my lungs overall are doing really well and I don't have to see the lung specialist again unless things get suddenly worse.
We've been staring down a possible diagnosis that would give me 2-5 years left to live for 6 months now, and getting a reprieve has been a huge relief and in its own way kind of exhausting.
But good good good news, and that makes me super happy <333
#personal#health stuff#cw chronic illness#still have all the other stuff#he asked me if i wanted a follow up re: the prescribed medicine#and i kind of said that while he was amazing#i do not want more specialists in the roster#i already have to see an endocrinologist#rheumatologist#orofacial pain specialist#psychiatrist#and more on a regular / semi-regular basis and it's like i'm good#how about we leave that there lol
97 notes
·
View notes
Text
It’s been 24 years since I retired. Today, I was called upon by one of my men whose father is in ICU with a diagnosis of COPD. I’m no longer in the business of practicing. I don’t like being called in to second guess. Yet there I was, as a favor. I asked him to sit his father up right, and with a stethoscope, listen to all five lobes and have his father say the letter Eee. As he was performing this test, the ICU nurse came in and asked what he was doing. He explained it: “Egophony”. She’d never heard of it. He explained it: “Old School.”
When you’re stomping in a triple canopy jungle, sweating it out in the sand box, or are sucking for air in a mountain top, you don’t have the luxury of X-Ray. You have a small bag of tricks tied to your belt. Egophony or Pectoriloquy are handy tricks to know. Infiltrates in the lung change the sound of things. Eee should sound like Eee. If it sounds like Aaa, you’re looking at fluid build-up. The fact that she was never taught this is in and of itself, disconcerting. Physics. Old school.
2 notes
·
View notes
Note
before I come apart
what is this about? 😍
HI GIRLIE!!!
This ask game
So before I come apart is a marauders au that is very very close to my heart. It is also extremely heavy, so I’ve put the summery under the cut!
I’ve been working on it for about two years in bits and pieces, but it will take me a long time before I’m comfortable posting it just because of how personal it is to me! That being said I do love talking abt it because there is a lot of love in my heart for this project.
Regulus Black runs away from home during his third year of university after [redacted] traumatic event, and flees to his brothers apartment.
There, he has to soothe all the bridges he burned years ago and ends up re-kindling his budding romance with his high school partner (now firefighter) James Potter, but shortly after this James is diagnosed with COPD, Chronic obstructive pulmonary disease.
This fic is an extremely healing/difficult one for me to write because im basically processing my mother’s diagnosis of COPD through it.
This fic is a tribute to how life changes when a loved one is diagnosed with a terminal illness. It’s a love letter to travel, art, and all the beauties we have on this earth. It is about the terror of loving, and the broken bones left by trauma.
4 notes
·
View notes
Text
Copd Awareness: Types, Causes, Symptoms, and Prevention Tips
Delve into COPD Awareness: Chronic lung diseases like emphysema & chronic bronchitis caused by smoking. Symptoms include coughing & shortness of breath.
To Know More: https://lalithachestandskinhospital.com/blog/copd-awareness-types-causes-symptoms-and-prevention-tips/

#chest specialist doctor#best lung doctor in Karimnagar#good pulmonologist near me#breathing problem specialist doctor#copd diagnosis treatment#pulmonologist hospital near me#chronic obstructive pulmonary treatment
0 notes
Text
14 Common Lung Diseases

Introduction
Lung diseases represent some of the most severe health threats globally. The rise of industrialization, environmental pollution, and tobacco usage significantly contribute to the prevalence of these diseases. This article, outlines the most common lung diseases, their symptoms, causes, and treatments.
1. Pneumonia

Pneumonia is an inflammation of the lung parenchyma caused by bacteria, viruses, fungi, or other pathogens. It poses a significant risk to the elderly, immunocompromised individuals, and those with chronic conditions but can also affect healthy individuals. Pneumonia can be classified based on the causative agent, such as bacterial pneumonia (e.g., Streptococcus pneumoniae), viral pneumonia (e.g., influenza virus), or fungal pneumonia (e.g., Pneumocystis jirovecii).
Symptoms
Fever
Cough with sputum
Chest pain
Shortness of breath
Fatigue
Sweating and shaking chills
Nausea, vomiting, or diarrhea (less common)
Diagnosis Diagnosis of pneumonia typically involves a combination of patient history, physical examination, chest X-rays, and sputum cultures. Blood tests may also be conducted to identify the causative agent.
Treatment Depending on the cause, treatments may include:
Antibiotics for bacterial pneumonia.
Antiviral medications for viral pneumonia.
Antifungal therapies for fungal pneumonia. Supportive care such as rest, fluids, and over-the-counter medications to reduce fever and manage pain can also alleviate symptoms. In severe cases, hospitalization may be required to provide intravenous antibiotics, oxygen therapy, or mechanical ventilation.
2. Bronchitis
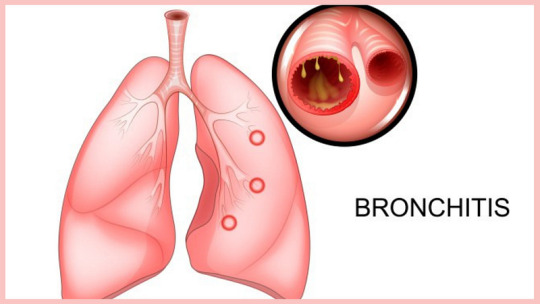
Bronchitis involves the inflammation of the bronchial tubes, which carry air to and from the lungs. It can be acute, often following colds or the flu, or chronic, usually resulting from smoking or long-term exposure to irritants like pollution or dust.
Symptoms
Persistent cough (productive or dry)
Sputum production (clear, white, yellowish-gray, or green)
Fatigue
Shortness of breath
Slight fever and chills
Chest discomfort
Diagnosis Diagnosis typically involves a physical examination, where a doctor listens to the patient’s lungs with a stethoscope. Additional tests, such as a chest X-ray, sputum tests, or pulmonary function tests, may be conducted to rule out other conditions like pneumonia or asthma.
Treatment
Acute bronchitis: Symptomatic treatment includes rest, fluids, and over-the-counter pain relievers and cough medications. Inhalers or nebulizers may be prescribed to ease breathing.
Chronic bronchitis: Management may involve bronchodilators, steroids, and pulmonary rehabilitation. Smoking cessation and avoiding lung irritants are crucial for treatment.
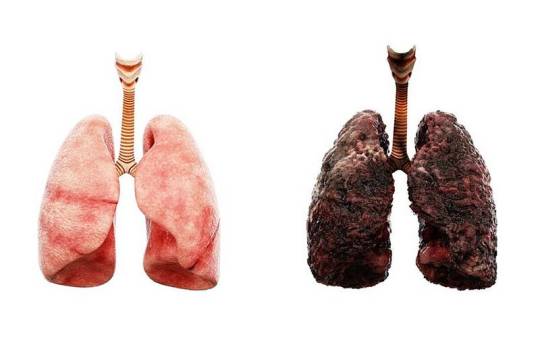
3. Chronic Obstructive Pulmonary Disease (COPD)
COPD is a progressive, irreversible disease characterized by chronic inflammation of the airways, primarily due to smoking, environmental pollutants, or long-term exposure to respiratory irritants. COPD includes chronic bronchitis and emphysema, conditions that often coexist and lead to airflow obstruction.
Symptoms
Chronic cough
Sputum production
Shortness of breath, especially during physical activities
Wheezing
Chest tightness
Frequent respiratory infections
Fatigue
Unintended weight loss (in advanced stages)
Diagnosis COPD is diagnosed through a combination of patient history, physical examination, and spirometry, a test that measures the amount of air a person can exhale and how quickly they can do so. Chest X-rays, CT scans, and arterial blood gas analysis may also be used.
Prevention and Treatment Preventive measures include:
Smoking cessation
Vaccinations (influenza and pneumococcal vaccines)
Reducing exposure to lung irritants
Treatments involves;
Bronchodilators to relax the muscles around the airways
Inhaled steroids to reduce airway inflammation
Pulmonary rehabilitation programs
Oxygen therapy for severe cases
Surgery (e.g., lung volume reduction surgery or lung transplant) in advanced cases
4. Lung Cancer
Lung cancer involves the uncontrolled growth of malignant cells in the lung tissues. Major risk factors include smoking, exposure to secondhand smoke, exposure to carcinogens (e.g., asbestos, radon), and genetic predisposition.
Types
Small cell lung cancer (SCLC): Often linked to heavy smoking, SCLC is aggressive and spreads quickly.
Non-small cell lung cancer (NSCLC): More common and includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
Symptoms
Persistent cough
Chest pain
Weight loss
Hemoptysis (coughing up blood)
Shortness of breath
Hoarseness
Bone pain (in advanced stages)
Headache (if cancer spreads to the brain)
Diagnosis Diagnosis involves imaging tests (chest X-rays, CT scans, PET scans), sputum cytology, and tissue biopsy. Molecular testing may be done to identify specific genetic mutations that can be targeted with specific treatments.
Treatment
Surgery to remove the tumor or part of the lung
Chemotherapy to kill cancer cells
Radiation therapy to destroy cancer cells or shrink tumors
Targeted drug therapies to attack specific genetic changes in cancer cells
Immunotherapy to help the immune system fight cancer
5. Pleurisy
Pleurisy, or pleuritis, is the inflammation of the pleura, the tissue lining the lungs and chest cavity. It can be caused by infections (viral, bacterial, or fungal), injuries, autoimmune diseases (e.g., lupus, rheumatoid arthritis), or other underlying conditions.
Symptoms
Sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing
Shortness of breath
Cough
Fever (if infection is present)
Diagnosis Diagnosis involves a physical examination, chest X-rays, ultrasound, CT scans, and blood tests to identify the underlying cause. Thoracentesis, a procedure to remove and analyze pleural fluid, may be performed.
Treatment Treatment depends on the underlying cause and may include:
Antibiotics for bacterial infections
Antiviral medications for viral infections
Anti-inflammatory medications (e.g., NSAIDs) to reduce pain and inflammation
Pain management with medications
Thoracentesis to drain excess fluid from the pleural space
6. Pulmonary Embolism
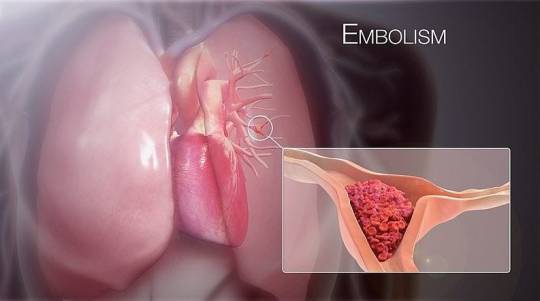
A pulmonary embolism (PE) occurs when a blood clot, usually originating in the legs (deep vein thrombosis), travels to the lungs, blocking blood flow and causing tissue damage. Risk factors include prolonged immobility, surgery, cancer, and certain genetic conditions.
Symptoms
Sudden shortness of breath
Chest pain (may be sharp and worsen with deep breathing or coughing)
Cough (sometimes with bloody sputum)
Rapid or irregular heartbeat
Lightheadedness or dizziness
Leg pain or swelling (if DVT is present)
Diagnosis: Diagnosis involves imaging tests such as chest X-rays, CT pulmonary angiography, and ventilation-perfusion (V/Q) scans. D-dimer blood tests and ultrasound of the legs may also be conducted.
Treatment Immediate treatment includes:
Anticoagulants (blood thinners) to prevent further clotting
Thrombolytics (clot-dissolving medications) for severe cases
Surgical or catheter-based procedures to remove the clot
Long-term anticoagulation therapy to prevent recurrence
7. Pulmonary Edema
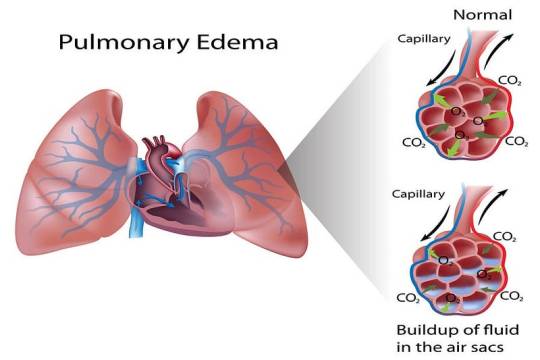
Pulmonary edema is the accumulation of fluid in the lung alveoli, making breathing difficult. It can result from heart failure (cardiogenic pulmonary edema), acute respiratory distress syndrome (ARDS), or exposure to high altitudes (non-cardiogenic pulmonary edema).
Symptoms
Difficulty breathing (dyspnea), especially when lying down
Rapid heartbeat (tachycardia)
Wheezing or gasping for breath
Coughing up frothy, pink-tinged sputum
Excessive sweating
Cyanosis (bluish skin or lips)
Diagnosis Diagnosis involves physical examination, chest X-rays, and blood tests. Echocardiography and pulmonary artery catheterization may be used to determine the underlying cause and severity.
Treatment Treatment involves addressing the underlying cause and may include:
Diuretics to remove excess fluid
Medications to improve heart function (for cardiogenic pulmonary edema)
Supplemental oxygen or mechanical ventilation
Treating underlying conditions such as infections or high altitude exposure
8. Pulmonary Fibrosis
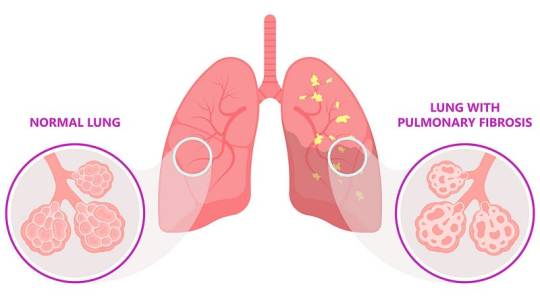
Pulmonary fibrosis is the thickening and scarring of lung tissue, leading to reduced oxygen absorption. Causes include chronic exposure to environmental pollutants, infections, genetic factors, and autoimmune diseases (e.g., scleroderma).
Symptoms
Shortness of breath (dyspnea)
Persistent dry cough
Fatigue
Unexplained weight loss
Aching muscles and joints
Clubbing (widening and rounding) of the fingertips or toes
Diagnosis Diagnosis involves a combination of patient history, physical examination, imaging tests (chest X-rays, high-resolution CT scans), pulmonary function tests, and sometimes lung biopsy. Blood tests may be used to identify underlying autoimmune diseases.
Treatment While there is no cure for pulmonary fibrosis, treatments focus on symptom management and slowing progression:
Medications such as pirfenidone and nintedanib to slow disease progression
Oxygen therapy
Pulmonary rehabilitation
Lung transplant in severe cases
9. Pneumoconiosis
Pneumoconiosis is a lung disease caused by inhaling dust particles, such as asbestos, silica, or coal dust, leading to lung scarring. It is a type of occupational lung disease commonly seen in miners, construction workers, and industrial workers.
Symptoms:
Chronic cough
Shortness of breath
Chest tightness
Progressive loss of lung function
Diagnosis: Diagnosis involves a detailed occupational history, physical examination, chest X-rays, and CT scans. Pulmonary function tests may also be conducted to assess the extent of lung damage.
Treatment Treatment includes:
Avoiding further exposure to dust
Medications to manage symptoms, such as bronchodilators and corticosteroids
Respiratory therapies
Pulmonary rehabilitation
10. Pulmonary Arterial Hypertension (PAH)
PAH is a form of high blood pressure affecting the arteries in the lungs and the right side of the heart. It can be idiopathic, familial, or associated with other conditions such as connective tissue diseases, congenital heart disease, or chronic liver disease.
Symptoms
Breathing difficulties (dyspnea), especially during physical activities
Dizziness or fainting (syncope)
Chest pain
Fatigue
Swelling in the ankles, legs, and abdomen (edema)
Cyanosis (bluish lips and skin)
Diagnosis Diagnosis involves echocardiography, right heart catheterization, chest X-rays, and CT scans. Blood tests and pulmonary function tests may also be conducted to assess lung and heart function.
Treatment Treatment strategies include:
Medications to relax blood vessels and improve blood flow, such as endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs
Diuretics to reduce fluid retention
Oxygen therapy
Anticoagulants to prevent blood clots
In severe cases, surgical procedures such as atrial septostomy or lung transplant
11. Cystic Fibrosis
Cystic fibrosis (CF) is a genetic disorder caused by mutations in the CFTR gene, leading to thick, sticky mucus buildup in the lungs and other organs. This results in frequent infections, respiratory issues, and digestive problems.
Symptoms
Persistent cough with thick mucus
Recurrent lung infections
Wheezing or shortness of breath
Poor growth and weight gain in children
Salty-tasting skin
Severe constipation
Frequent greasy, bulky stools
Diagnosis Diagnosis involves genetic testing, sweat chloride tests, and newborn screening. Pulmonary function tests, chest X-rays, and sputum cultures may also be conducted to assess lung health.
Treatment Management includes:
Medications to thin mucus, antibiotics to treat infections, and bronchodilators to open airways
Chest physiotherapy to clear mucus
Enzyme supplements and high-calorie diets to manage digestive issues
Newer therapies targeting the underlying genetic defect, such as CFTR modulators
12. Respiratory Distress Syndrome (RDS)
RDS primarily affects premature infants due to a lack of surfactant, a substance necessary to keep the lungs open and facilitate gas exchange. Risk factors include premature birth, maternal diabetes, and multiple births.
Symptoms
Rapid, shallow breathing
Grunting sounds while breathing
Nasal flaring
Chest retractions (pulling in of the chest muscles)
Cyanosis (bluish color of the skin and mucous membranes)
Diagnosis Diagnosis involves clinical assessment, chest X-rays, and blood gas analysis to measure oxygen and carbon dioxide levels. Prenatal tests can also help identify at-risk pregnancies.
Treatment Treatment includes:
Surfactant replacement therapy to improve lung function
Mechanical ventilation or continuous positive airway pressure (CPAP) to support breathing
Oxygen therapy
Supportive care such as fluids and nutrition
13. Sarcoidosis
Sarcoidosis is characterized by the growth of granulomas (small clusters of inflammatory cells) in the lungs and other organs, likely as an immune response to unknown triggers. The exact cause remains unclear, but genetic and environmental factors are believed to play a role.
Symptoms
Dry cough
Shortness of breath
Chest pain
Fatigue
Fever
Swollen lymph nodes
Skin lesions (e.g., erythema nodosum)
Diagnosis Diagnosis involves a combination of patient history, physical examination, chest X-rays, CT scans, and pulmonary function tests. Biopsy of affected tissues may be performed to confirm the presence of granulomas.
Treatment While sarcoidosis is often self-limiting and may resolve without treatment, severe cases may require:
Corticosteroids to reduce inflammation
Immunosuppressive medications (e.g., methotrexate, azathioprine)
Antimalarial drugs (e.g., hydroxychloroquine) for skin lesions
Regular monitoring and follow-up care to manage chronic cases
14. Asthma
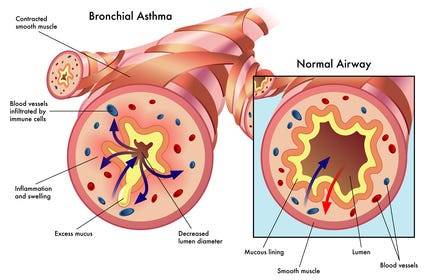
Definition and Causes: Asthma is a chronic inflammatory condition of the airways, causing episodes of wheezing, coughing, and chest tightness, often triggered by allergens, exercise, cold air, or respiratory infections. Genetic and environmental factors contribute to its development.
Symptoms
Wheezing
Shortness of breath
Chest tightness
Coughing, especially at night or early morning
Increased mucus production
Diagnosis: Diagnosis involves a detailed medical history, physical examination, and lung function tests (spirometry, peak flow measurement). Allergy testing and chest X-rays may also be conducted to identify triggers and rule out other conditions.
Treatment Management includes:
Avoiding known triggers
Inhalers (bronchodilators for quick relief, corticosteroids for long-term control)
Long-term control medications (e.g., leukotriene modifiers, long-acting beta agonists)
Immunotherapy (allergy shots) for severe allergies
Asthma action plans to manage symptoms and prevent attacks
Conclusion
Lung diseases encompass a wide range of conditions, each with distinct causes, symptoms, and treatments. Preventive measures such as avoiding smoking, reducing exposure to environmental pollutants, and timely vaccinations can significantly reduce the risk of developing many of these diseases. Early diagnosis and appropriate management are crucial in improving outcomes and quality of life for individuals affected by lung diseases. For personalized medical advice and treatment, consult with healthcare professionals.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Email us: [email protected] for professional guidance.
#medical students#nursing school#nursing student#assignment help#medicine#medical university#medical school#medical student#studying#studyspo#student#student life#college student#study inspiration#study blog#academic writing#writters on tumblr#online writing#do my online class
4 notes
·
View notes
Text
im doing better at getting a copd diagnosis than i am at getting my degree
2 notes
·
View notes