#Allergy Immunology
Text
"A clinical trial studying severe allergic reactions in the U.K. is being called “life-transforming.”
Five United Kingdom National Health Service (NHS) hospitals are participating in the £2.5 million ($3.2 million) trial to help patients live with their food allergies.
The study is being funded by the Natasha Allergy Research Foundation, Sky News reported. The foundation was formed in the memory of Natasha Ednan-Laperouse, who died in 2016 after eating a baguette that had sesame in it...
The trial is studying clinical oral immunotherapy treatments in which patients are given small doses of the food to which they are allergic to build up their tolerance. The food is given under medical supervision by trained staff, The Telegraph reported.
The study has 139 people participating who have allergies to peanuts or cow’s milk. They range in age from 2 to 23 years old, the BBC reported.
The Food Standards Agency said 2 million people in the U.K. have a diagnosed food allergy. In the U.S., about 5.5. million children have a food allergy, the National Institutes of Health reported.
One 11-year-old who was diagnosed with a severe peanut allergy when he was an infant can now eat six peanuts.
A 5-year-old with a milk allergy can drink 120 ml of milk every day and can enjoy a daily hot chocolate, the BBC reported.
“To have a patient who has had anaphylaxis [Note: Anaphylaxis is an allergic reaction so severe that it's potentially fatal without immediate treatment. It is very common with peanut allergies in particular. x] to 4mls of milk to then tolerate 90mls within six to eight months is nothing less than a miracle,” Sibel Donmez-Ajtai, a pediatric allergy consultant and principal investigator at Sheffield Children’s NHS Foundation Trust, said, according to Sky News.
The final results of the study are expected to be released in 2027.
Similar studies have been conducted in the U.S. To find one, visit FoodAllergy.org.
Earlier this year, the NIH released the findings of a study of an antibody treatment that would help children consume allergy triggers safely."
-via WHIO 7 Local News, May 8, 2024
#allergies#allergic reaction#anaphylaxis#epipen#peanut allergy#milk allergy#peanuts#milk#medical news#public health#immune system#immunology#united kingdom#good news#hope
3K notes
·
View notes
Text

#Adaptive Immunity#Allergy Immunology#Autism Vaccines#Cancer Vaccines#Cellular Immunology#Chicken pox Vaccines
0 notes
Text
A drug can make life safer for children with food allergies by preventing dangerous allergic responses to small quantities of allergy-triggering foods, according to a new study led by scientists at the Stanford School of Medicine.
The research was published Feb. 25 in the New England Journal of Medicine. The findings suggest that regular use of the drug, omalizumab, could protect people from severe allergic responses, such as difficulty breathing, if they accidentally eat a small amount of a food they are allergic to.
Continue Reading.
173 notes
·
View notes
Text

Allergy Alarm
Allergic inflammation in the lungs and airways, such as underlies asthma, is initiated by cooperation of a protein called TL1A with another called IL-33 – together part of an 'alarm system' activated on first exposure to the allergen
Read the published research article here
Image from work by Pauline Schmitt and Anais Duval, and colleagues
Institut de Pharmacologie et de Biologie Structurale (IPBS), Université de Toulouse, CNRS, Université Toulouse III—Paul Sabatier (UPS), Toulouse, France
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in Journal of Experimental Medicine, April 2024
You can also follow BPoD on Instagram, Twitter and Facebook
6 notes
·
View notes
Text
As a follow-up to my rant about mRNA vaccines, there's a question I get a lot about acellular and mRNA type vaccines:
"If there's no virus in there, why did the COVID shot make me sick as a dog the next day??"
Because viruses generally aren't what makes you feel sick.
Your immune system is.
Few viral infections, on their own, give you a fever, joint aches, and a stuffy nose. If you had no immune system, a virus could kill you without producing most of the signs and symptoms we associate with viral illness.
Those things you have with a flu are the direct result of your immune system fighting back.
Lots of microorganisms are vulnerable to temperature fluctuations. Fever is your body trying to cook the germs.
Inflammation is a concentration of immune cells at a given location doing their job. Lots of them go to where the infection is, which makes tissues puffy and painful.
Cough, congestion, and nausea are your body trying to flush out attacking organisms by removing them from your airways and digestive system. If it can get rid of them before they get into your cells, that's half the battle.
Which means that you don't actually need to have an infectious illness to feel like you have a cold or flu.
Your immune system just needs to THINK you do.
Vaccines trick your body into fighting an intruder that isn't actually a threat, much like allergies do. Your immune system throws everything it's got at the vaccine material, and creates antibodies against future infections from the same attacker.
So when you actually get COVID, or measles, or seasonal influenza, it'll be ready.
That immune response that makes you feel like dirt the day after your COVID shot is actually a good sign, because it tells us your immune system bought the ruse and treated it like an actual disease.
Which means it's also planning ahead in case you catch that disease again someday.
Working at the vaccine clinic, I heard from a lot of people about how the COVID vaccine affected them, and what I heard was incredibly consistent: maybe swollen lymph nodes on the first vaccine, but otherwise nothing. On the 2nd, 3rd, and later doses, almost everyone felt sick enough to stay home/in bed within about 24 hours.
This is good news, because it means the mRNA vaccines are producing a very similar immune response in most of the people who get it, and it keeps producing a strong immune response after multiple doses.
Anyway, the moral of the story is we need to feel sick for many vaccines to work. Think of it like a building fire in a big city: a building catches fire, the fire department is called, and traffic slows to a crawl.
This isn't because the fire slowed down traffic; fires don't do that, but firetrucks rushing to put it out do.
The same thing happens if somebody's kid wants to know what'll happen if they pull the fire alarm: the firefighters rush to the scene, traffic slows down.
But in this case there's no actual fire; the fire department gets the signal for a fire and responds accordingly without the building actually being in danger.
Vaccines pull the fire alarm for your immune system to make sure the firefighters know how to do their thing when a fire actually starts. Your immune system responding like there's actually something wrong is what makes you feel sick the next day.
#vaccines#science#microbiology#immunology#this is also why autoimmune conditions maje people so sick#but that's a rant for another day#also why allergies can feel like a cold#get your vaccines kiddos#tell your immune system to attack the right stuff#you get a day off work now and anti-viral superpowers later
7 notes
·
View notes
Text




The ACR provides a handy pocket guide for contrast reaction management (be sure to look at all 4 images!), which can be printed and placed in your badge holder with your hospital ID (PDF link below, including the pediatric version). Note that premedication regimens are also included. Key points include:
--Patients with bronchospasm (expiratory wheezing) should receive albuterol. 2 puffs x 3, but if not responding or severe, you can administer epinephrine.
--HYPOtension with tachycardia should be considered anaphylaxis and the patient should receive epinephrine. Diffuse hives or erythema with hypotension or respiratory distress can also be considered anaphylaxis.
--Laryngeal edema (inspiratory stridor) is an indication for epinephrine.
--Do not give epinephrine for HYPOtension with bradycardia. That is an indication for atropine.
--Diphenhydramine can be used, but remember that it can potentiate hypotension
--The preferred route for epinephrine in a hypotensive patient is IV, as the extremities may not be sufficiently perfused for the IM route to be effective. However, note that 1 mL of 1 mg/10mL (1:10,000) is the appropriate volume and concentration of epinephrine to administer IV to an adult. This is a critical point if your contrast reaction kit requires you to draw up your own epinephrine (some may have pre-filled syringes). It behooves you to be familiar with what the contrast reaction kits at your institution contain.
Source:
ADULT
PEDIATRIC
1 note
·
View note
Text
IgE decided to react with something and started producing histamines and now I need to take anti histamines ITS 1 AM FUCKING STOP HELP WHEN YOU'RE NEEDED FAALTU ME PARESHAN MAAT KARO
2 notes
·
View notes
Text
Despite that tag ramble, brain is like "now I want some kiwifruit."
:I
#what i do know abt immunology is that allergies are fucking weird#you can develop them at any pt in life#they can remit at any pt in life#one day it's just a mild/localized rxn#another you're in the damn hospital#physiology is just fuckign wild - my dude#bodies are jank and i kinda love that absurdity#(aaand now i'm just thinking of remus chugging the spoiler spray)
2 notes
·
View notes
Text
After the (......eventually) successful attempt at getting my blood drawn, I received my results, and while a few things were on the edge of healthy, they were so much improved from my last labs that my doctor was unusually positive and reassuring about them :)
#the only real concern was some immunological thing i don't quite follow that /could/ be a marrow issue#but could also be asthma and allergies. which i have.#so! i'm taking it as a win#anghraine babbles#medical malfeasance
13 notes
·
View notes
Text
I discovered a patient didn't know this, brought it up to my mom and sister and neither of them knew either. Like this is why you have to watch babies with new foods several times, to make sure they don't develop an allergic reaction. I just want to know if this is common knowledge or not.
Like you can eat a food the first time and be okay. Then the second time, be allergic.
This happened to a lady getting her lash extensions refilled, at the refill (2nd exposure) she had an extreme allergic reaction to the adhesive.
#optometry#gradblr#doc life#polls#allergies#medicine#immunology#anatomy and physiology#biology#I'm pretty sure I learned this in highschool#allergic reaction
6 notes
·
View notes
Text

Immunotherapy for Allergy and Asthma treatment in Kolkata
In the bustling city of Kolkata, where diverse cultures intersect and vibrant traditions thrive, the prevalence of allergies and asthma poses significant challenges for individuals seeking relief from respiratory ailments. Immunotherapy, a groundbreaking treatment approach, offers hope for those grappling with allergies and asthma by targeting the underlying causes of these conditions. This comprehensive guide explores the landscape of immunotherapy for allergy and asthma treatment in Kolkata, including top hospitals, renowned specialists, treatment costs, efficacy, and frequently asked questions.
Best Allergy & Asthma Treatment Center in Kolkata
Are allergies and asthma making it hard for you to breathe easy in the bustling city of Kolkata? Don’t worry, because we’ve got you covered! In this blog post, we will explore the best allergy and asthma treatment center in Kolkata that can provide you with the relief you’ve been searching for. Whether it’s finding the right doctor or discovering effective treatment options, we have all the information you need to take control of your respiratory health. So let’s dive in and discover how this exceptional treatment center can help alleviate your allergy and asthma symptoms, allowing you to live a happier, healthier life in the City of Joy!
Best Hospital for Allergy Treatment in kolkata
The Allergy & Asthma Treatment Centre also boasts state-of-the-art facilities equipped with advanced diagnostic technologies. This ensures accurate diagnosis so that effective treatment can be initiated promptly. From comprehensive allergy testing to lung function assessments, they leave no stone unturned in providing top-notch care. Moreover, this hospital takes a holistic approach towards managing allergies and asthma by offering education programs to patients. They believe that empowering individuals with knowledge about their condition plays a crucial role in long-term management.
Allergy & Asthma Treatment Centre kolkata
The Allergy & Asthma Treatment Centre in Kolkata offers a comprehensive range of services to cater to all your needs. With a team of highly skilled doctors specializing in allergies and asthma, you can be assured that you are receiving top-notch care. These specialists have years of experience in diagnosing and treating various allergic conditions, ensuring accurate diagnosis and personalized treatment plans. One of the key factors that sets this centre apart is their commitment to research. The Allergy & Asthma Research Centre associated with the treatment centre conducts cutting-edge studies on allergies and asthma, contributing valuable insights to medical advancements in these fields.
Allergy & Asthma Treatment Centre Reviews
Reading reviews from patients who have already visited a particular centre can give you insight into their experiences and help you make an informed decision. One thing to keep in mind is that everyone’s experience may vary, so it’s important not to rely solely on one or two negative reviews. Look for patterns in the feedback – are there multiple positive reviews praising the doctors’ expertise? Are there consistent mentions of excellent customer service? Additionally, take note of any specific treatments or therapies mentioned in the reviews. If you’re looking for a specific type of treatment, such as immunotherapy or specialized testing, see if patients mention these services being offered at the centre.
Allergy Specialist Doctors in Kolkata
One such renowned allergy specialist doctor in Kolkata is Dr. Saibal Moitra. With years of experience under his belt, Dr. Saibal Moitra has successfully treated numerous patients suffering from various types of allergies. His expertise lies not only in diagnosing and treating allergies but also in providing personalized care and guidance to his patients. Dr. Saibal Moitra. Known for his compassionate approach towards patient care, Dr. Saibal Moitra takes the time to listen to each patient’s concerns and provides them with effective solutions tailored to their specific needs. Dr. Saibal Moitra is yet another esteemed allergist based out of Kolkata who specializes in treating both adult and pediatric patients with allergies. With a vast knowledge base and access to state-of-the-art diagnostic tools, Dr. Saibal Moitra ensures accurate diagnosis and comprehensive treatment plans for all his patients.
#Best Allergy Treatment Centre in Kolkata#Best Asthma Treatment Centre in Kolkata#Allergy Specialist Near Me#Allergist Near Me#Best Allergy Specialist Near Me#Allergy and asthma specialist near me#immunologist near me#allergist near me#allergy and asthma specialist near me#best allergy specialist near me#allergist immunologist near me#immunology doctor near me#allergy and immunology near me#best doctor for allergy near me#food allergy doctor near me#Immunotherapy for Allergy and Asthma treatment#Immunotherapy for Allergy
0 notes
Text
Welcome to the well-known center of asthma allergy and immunology Tampa that provides the most effective allergic treatment. To help you manage your symptoms and improve your quality of life, our expert allergists employ cutting-edge diagnostic procedures and treatments. We at “Advanced Allergy and Asthma Care, PLLC” provide personalized treatment strategies based on your specific needs, such as allergy injections and rapid desensitization. Make an appointment as soon as possible to see the difference for yourself! Please follow the link https://www.allergydoc.us/
0 notes
Text
#allergy and immunology billing services#allergy and immunology billing services in US#immunology medical billing#immunology billing#allergy billing services#allergy and immunology medical billing services#Medical Billing For Allergy & Immunology#medical billing for Allergy and Immunology#allergy and immunology billing specialist
0 notes
Photo
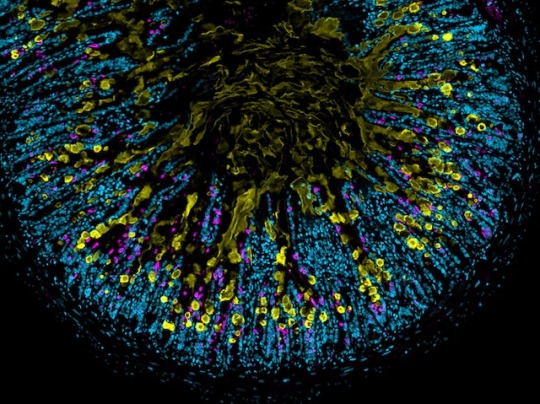
Great Innate
Two prongs of your immune system tackle invaders with a precision pincer movement to keep infections at bay. The innate immune system is fast-responding and unspecialised, while the adaptive develops tailored defences against specific foes with each infection it encounters. How precisely the innate system works, or even whether some parts might be redundant accompaniments to the adaptive elements, is not fully understood. A new study examined the effect of blocking one component of the innate system, group 2 innate lymphoid cells, in mice. Without these cells, the inflammatory response – key to staving off attacks – could not develop properly, and mucus (yellow in the infected intestine cross-section pictured) production was limited meaning parasites could not be expelled. Allergy responses were also worsened by a lack of these cells, highlighting the innate immune system’s integral importance, and perhaps pointing to new treatment approaches.
Written by Anthony Lewis
Image by Patrycja M. Topczewska from work by Katja J. Jarick and colleagues
Department of Microbiology, Infectious Diseases and Immunology, Charité–Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin and Humboldt-Universität zu Berlin, Berlin, Germany
Image copyright held by the original authors
Research published in Nature, November 2022
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunology#immune system#innate immunity#innate immune response#immunofluorescence#inflammation#allergy
8 notes
·
View notes
Text
The sardonic, reductionist headline here could be "Scientists finally figured out why you get more colds in winter: bEcAuSe iT's CoLd!"—but the actual science involved here is both interesting, and potentially very relevant to everyday life and especially the immunocompromised:
It turns out the cold air itself damages the immune response occurring in the nose. [...] In fact, reducing the temperature inside the nose by as little as 9 degrees Fahrenheit (5 degrees Celsius) kills nearly 50% of the billions of virus and bacteria-fighting cells in the nostrils, according to the study published Tuesday in The Journal of Allergy and Clinical Immunology.
“Cold air is associated with increased viral infection because you’ve essentially lost half of your immunity just by that small drop in temperature,” said rhinologist Dr. Benjamin Bleier, director of otolaryngology at Massachusetts Eye and Ear and an associate professor at Harvard Medical School in Boston.
Want to avoid catching or spreading respiratory viruses like CoVid-19, RSV, influenza, or a common cold? Mask up, please, but also bundle up! Wrap up in a scarf, wear a balaclava, and just generally keep your face warm. There's no single magic solution, but that's not a reason to do nothing. Rather, it's a reason to take several simple precautions that help avoid the spread of disease and protect those around you. (I can't tell you how much "this isn't 100% effective so I shouldn't do it at all" frustrates me.)
Oh, and #knitblr? This is your time to shine.
#covid 19#rsv#respiratory illness#science#immunocompromised#face masks#masks work#knitblr#knitting#crochet
53K notes
·
View notes
Text
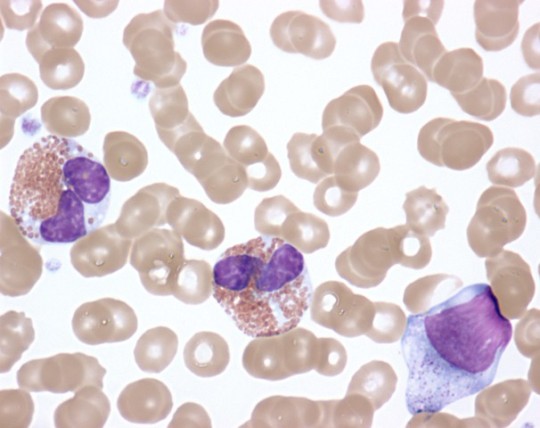
Q. What is nonallergic rhinitis with nasal eosinophilia syndrome (NARES)?
.
.
.
.
.
A. Nonallergic rhinitis with nasal eosinophilia syndrome is the most common inflammatory kind of nonallergic rhinitis. Sufferers have high eosinophils on nasal smear but negative skin or serum tests for IgE. It is associated with asthma and may reflect hyperactive nasal mucosal inflammation.
Credit: NIH Image Gallery
#TeachingRounds, #FOAMed, #pulmonology, #allergy, #immunology, #ENT
6 notes
·
View notes