#14 can make yaz fit in this life
Explore tagged Tumblr posts
Text
the thing with yaz&14 is that like,,, the best thing thats ever happened to you in your life happens to you, and you learn some things about yourself, and you grow up in the process, and find the thing you love to do, and youre really good at it, and you get a taste of a life that you can see yourself doing until you die (even if it might make that death come a little sooner than expected), and you fall in love with the person who kind of embodies that life,
and then that person is like actually im 10 times happier not doing that
#and it's not 'not doing that With You'#but With Her is very much part of the life for yaz i think#like clara can get her own tardis and become her own gay doctor#but i think for yaz like yes she loves travelling but it's not just that. it's specifically what she did with 13#it's specifically 'i see something need fixing i do what i can'#it's specifically that#i think 14 still like would LOVE to have yaz in their life#as im writing it currently 14 is very much like please come hang out any time#14 can make yaz fit in this life#but i think yaz doesnt know how she fits here#with All these other people who love and surround the doctor too right? and without travelling#and it's so rough bc it's like#for yaz it's like she sort of wants the old life back but at the same time thats wishing for the doctor to be so much more miserable
26 notes
·
View notes
Text
No, Ncuti Gatwa's Casting Isn't Regressive
Chapter 3 - Dancing Queen/Conclusion
‘I’ve experienced racism my whole life, and while I always believed in myself, always knew [racists] were stupid and uneducated, I guess it did misinform my view of how the world works. It makes you think everyone has that opinion and you’ll constantly have to fight through life – then you learn that you don’t: you can find a tribe, you can find your people.’ - Ncuti Gatwa for Elle

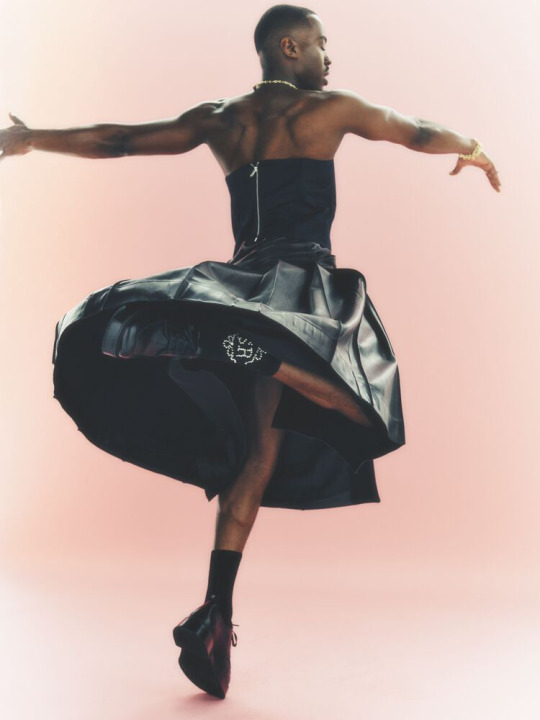
So with the treatment of Who’s Black men and the neglect of Black women in its representations of womanhood, consider the Fifteenth Doctor. A dark-skinned Black queer man, wearing a kilt and a bold smile, spinning to his heart’s content on the dancefloor. This is an image of Blackness, an image of queerness and an image of manhood and masculinity the show has never seen before. Gatwa is fully aware of this and has gone in depth in his interviews. He’s also addressed his Rwandan heritage and his family fleeing genocide against the Tutsi. Gatwa knows the feeling of being an outsider, heavily mirroring the revelation of the Timeless Child. Black Britishness is already a form of representation mainstream British media has only recently acknowledged and in this case, Black Scottishness is taking the forefront. Despite being a British cultural stape, Doctor Who’s been shy about representing Black Britishness specifically. We’ve had three Black companions, but little references to the culture (minus Ryan’s mention of grime music in Arachnids). We know Yaz is Pakistani. But is Ryan African? If yes, is he Nigerian, Ghanaian etc.? Is Ryan West Indian? If so, is he Trini, Bajan etc.? Is he both? What was Martha and Bill’s heritage? Many Black people in the British Isles are 2nd and 3rd gen immigrants, some of us are African, some are West Indian and some of us are both. Black British identity is complex as it is a melting pot of different African and West Indian cultures blended to create something new. Gatwa’s Black Scottishness provides this insight to Fifteen. Gatwa’s Rwandan heritage is included in Fifteen’s sonic too, with Gallifreyan symbols translating the phrase ‘the sharpness of the tongue always defeats the sharpness of the warrior’. Other Black cultural references have appeared for Fifteen too, with Gatwa noting his wardrobe is inspired by Black American HBCU fits. Even though it isn’t yet confirmed (and unlikely for series 14/season 1 seeing as there are no Black writers… yay!), Gatwa has shown interest in a Nigerian historical stating he’d love for the Doctor to meet the Orishas, goddesses of West African folklore. Again, with many different Black cultures not only is this an opportunity for representation but also new stories, new locations and new concepts the show has yet to discover. To fit in so many spaces but none at all is a perfect summary of the Black British experience and other Black experiences in Western countries.
“We choose our families. And the Doctor is a lonely wanderer, looking for their next adventure … I know many a gay man, MANY a gay man, I could describe that way!” - Ncuti Gatwa for the Guardian
Queer Black manhood and masculinity is rich and diverse and with this new era, we could see the tip of its iceberg. There have already been representations of this before in media such as Moonlight and Noah’s Arc so for a mainstream British show like Doctor Who to feature a queer Black man as the lead, we have the opportunity to show something special. With Nine and Jack’s kiss and Fourteen’s cosign of Isaac Newton already showing this potential, we could see a canon longer term mlm pairing involving the Doctor for the first time. And not only that but with a Black doctor for the first time. A queer Black man showing love and being loved is a reminder for queer Black people that universe-defying romance includes us too and that our DoctorRiver or TenRose moments can exist.
There is so much to look forward to in this new era and even more potential for the type of representation it can bring. So with that in mind, I hope the greater fandom at large can see this and that newer fans will get to experience that same joy we did when we first fell in love with this show.
‘This person survived a genocide. This person fits in everywhere and nowhere. I am the Doctor. The Doctor is me. I decided that I had to get this role’ - Ncuti Gatwa for Rolling Stone
<- Chapter 2
#fifteenth doctor#15th doctor#ncuti gatwa#doctor who#nuwho#new who#black representation#doctor who analysis#fandom analysis#doctor who fandom#fandom antiblackness#fandom racism#fandom history
35 notes
·
View notes
Text
The Timeless Children
I hated everything about this.
Like - EVERYTHING.
1. The companions had nothing to do with the Doctor the whole episode and contributed literally nothing to her story - they didn't even SAVE HER BECAUSE SHE SAVED HERSELF. They somehow find her in the centre of the ruins after they have a ‘touching’ moment about willing to risk their lives to save her - but they come into the room JUST after it’s become completely irrelevant - it was like a fucking PARODY. They never even learned what the fuck was up with her. Yaz gets nothing in return for her classic faith in the Doctor - this is worse than fucking Martha. And still no hugs - loveless. COMPLETELY LOVELESS.
2. There was zero suspense. Zero. Who CARES about the mystery of the Timeless Child and their society if the Time Lords are fucking dead. Who CARES about the companions being in danger when they’re in a completely separate plot - like - COMPLETELY. I thought the Doctor trying to bargain her life for theirs was a juicy line - too bad it meant NOTHING - had NO impact whatsoever. Half of this episode was pure exposition dump?
3. Why was this the Master show? - he just talked for 30 minutes (I think it might genuinely have been 30 ACTUAL minutes) while the Doctor said NOTHING - even Sasha Dhawan can’t carry that off???? I can’t believe that Chibs had me get bored of Sasha’s performance???? HOW. It was so repetitive - truth truth truth. I’m so weepy - I’m so mad - I’m so clever. Oh I’ve broken you - yep I’ve broken you. Why is there even the fuckin assumption?? I could not parse why this would be SO devastating to anyone that Chibs would hang the whole plot and emotional arc on this. Literally immobilising the Doctor and making her mute K.O.’d their INCREDIBLE chemistry. JEzus Christ.
4. This episode went: weapons are good though. Use bombs and guns!
5. ‘You can’t pretend to be cybermen for ANY amount of time’ - yet somehow they manage to masquerade as cybermen to such an extent that they can join a platoon, teleport down, shoot at people, and kill the cybermen remaining. Well why didn’t anyone else think of this???
6. Reduced cybermen down to - armour that you can fuckin PUT ON?????
7. NO attempt at body horror was made even when there was the opportunity. Human remains? we see nothing of the Cybermen’s previous humanity and their nature as victims. No threat of conversion for any of the companions. This was possibly the least scary chib episode yet and that says something.
8. If Ryan had lobbed a bomb at Yaz and Graham they would have been DEAD.
9. Why kill that girl when she should know that Cybermen don’t even falter at gunfire so how can she provide ‘cover’ lol
10. Needless explanation and repetition resulting in ZERO suspense. The Master explaining that he sent the Doctor those visions - useless minutiae. The Doctor retreading everything the Master has just told the audience - making her seem dumb and making me FEEL like he thinks I’m fuckin dumb.
11. Completely anticlimactic end for the Lone Cyberman.
12. The Doctor did not start out a rebel - did not start out looking at the stars going: ah....I want to go there. They interfered because they had been primed for it by years of working for the ‘Division’ - they weren’t a rebel who wanted to see more and then realised they could actually do good - in defiance of the conservative society they were part of. No. They’d been the Doctor even before Ian called One that. Well that cool and wonderful theory of being Named and taught by humans can go out the window.
13. First, the particle would destroy all life in the universe. Then - suddenly - as though they rewrote the script while they were filming - it would only destroy all life on the planet. Right.
14. Why even MENTION that nobody can enter the TARDIS in this very series if you end it on the fucking JUDOON!!!! JUDOON!!!! teleporting in.
15. It was repeatedly said that the Cybermen can ‘read’ human lifesigns but not uhhhhhh when it’s inconvenient I guess.
16. Is Tec-Teun Rassilon? Because I didn’t get the sense that the Time Lords’ rise to power on the back of their seemingly harmless genetic splicing was presented as a bad thing per se. So what the fuck is the issue. The Master was just mad that the Doctor was essential to the creation of his being. Ok. I guess there was no moral argument behind it or anything. They didn’t deserve to get wiped out - it really was just a lunatic who somehow gained the power to destroy one of the greatest civilisations ever (which is certainly also never explained).
17. Still no idea where Missy and her character development fits in this. Apparently this Gallifrey destruction wasn’t because of anything clever like that the Master learned from the Doctor and obliterated the Time Lords for being quite particularly evil by their new rules - no he just...... killed them because his ego got hurt? right.
18. Somehow not a single cyberman notices them disassembling 5 cybermen making a lots of noise - not even the fucking CYBERIUM - the hub of all strategic fuckin cyberknowledge or whatever - apparently they haven’t thought of sensors and AI interfaces being able to use them when plugged into a damn ship yet in the far future. Nobody notices them boarding, planting bombs, running away. None of the Cybermen can shoot straight. What a fuckin threat.
19. The Doctor really just needed a goddamn peptalk from her way more Doctor-ish past self to blow the Matrix out? That sequence was pretty fucking shit-looking. And then the emotional resolution is that she’s totally ok with being more than she remembers? Oh ok. ‘You’re afraid - not me!’ OK?? Why? Why? Would the Master have expected the Doctor to respond like it’s some awful truth. Ok the founders lied bc the Time Kid got out of control but then they lost track of them again? I mean yikes they suck. Isn’t the goddamn emotional punch really that their people are dead - again?? Dead??? forever??? what about its children??? what about the horror and the guilt and - does none of that matter any more? Guess we have another Dimension to travel to to see where the Doctor actually came from. Old conflictual but significant relationship with ‘home’ ended- mysterious dimension is the Doctor’s home now.
20. The end implies that the Doctor wasn’t hesitating to kill the Master, the last remains of the Time Lords and every single living thing on her home planet - she was just hesitating to kill herself. I said Chibnall had no moral intelligence but - he truly does not understand the Doctor in any way!? I cannot express how much I despise this. This was worse than mediocre it was fucking CRIMINAL. And it wasn’t even a triumph - it wasn’t even a defeat of the fuckin Master either (and who even CARES about Ko Sharmus????).
I lied I liked four things:
1. Graham and Yaz having their heart to heart.
2. Ginger-haired Brandon being the Doctor. That was a great visual parallel.
3. The overall backstory to the start of the Time Lords was like - fine. I prefer mythological backstories to be nebulous. But alright. Put the focus on the ability to regenerate instead of time travelling - ok, that makes sense - sure - whatever. All the diversity was pretty beautiful too.
4. At least the Master got choked this time (jfc chibnall - can you write NO other shorthand for the willingness to use deadly force???)
#yknow what i think would be good for chibs scripts?#them having to be shorter#scrap scrap scrap#kill all you fucking useless darlings#dw#ok so uhhhhhhhhh#spoilers#the timeless children#i hope my first sentence gave enough warning about my negativity#SALT#im a fuckin salt pillar blowing away in the wind#this is TV CANON#goddamn#GOD#damn#my stuff#vidi
1 note
·
View note
Text
Premenstrual Syndrome describes
Overview
Premenstrual syndrome (PMS) describes a wide range of severe, recurrent symptoms that occur from several days to two weeks before your period. PMS affects up to 75 percent of women in their childbearing years. The symptoms of PMS can appear any time between puberty and menopause, although the most common age for it to start to become a problem is during the late 20s to early 30s. Symptoms of PMS may get worse with age and stress, although the underlying causes are not well understood. Even women who have had hysterectomies can have PMS if at least one functional ovary is left. Women who are vulnerable to depressive illness, panic disorder, other psychiatric disorders orchronic medical conditions may also be susceptible to PMS, although these conditions may occur in women without PMS as well. Heredity may also play a role: if your mother or sister suffers from PMS, you may find you experience it, too. As many as 150 physical and behavioral symptoms have been assigned to PMS, but the number of PMS symptoms that most women experience is much more limited. The most common symptoms include irritability, bloating, mood swings, anxiety, depressed mood, fatigue, appetite changes, water retention and breast tenderness, among others. Menstrual cramps, or dysmenorrhea, are not considered a PMS symptom, although women with PMS may experience cramps. PMS appears to be caused by rising and falling levels of the hormones estrogen andprogesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. Calcium may play a role in PMS. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. Dietary changes and exercise may also help relieve the discomfort of PMS symptoms. When symptoms are severe, serotonergic antidepressant medication may be prescribed. It is thought that increased serotonin reduces PMS symptoms. One of the most important strategies for coping with premenstrual discomfort is to be aware of any pattern your symptoms follow. The more aware you are of your symptoms—when they start and stop and what works best to relieve them, for example—the better you can develop strategies to recognize and cope with them—whatever they may be. Premenstrual Dysphoric Disorder Approximately three to eight percent of women experience premenstrual dysphoric disorder (PMDD), a condition that, like PMS, is associated with the menstrual cycle. The symptoms of PMDD are the same as PMS symptoms, although women with PMDD may experience more dysphoric (depressive) symptoms and more severe symptoms. In fact, to be diagnosed with PMDD, symptoms must be severe enough to disrupt a woman's daily function. Symptoms must also meet diagnostic criteria specific to PMDD developed by the American Psychiatric Association. The most important criteria for a PMDD diagnosis are mood symptoms. Physical symptoms may also be present but aren't as critical to the diagnosis. The difference between PMDD and mild PMS is like the difference between a mild tension headache and a migraine, experts say. Women who have a history of depression are at higher risk for PMDD than other women. Treatment for PMDD includes serotonergic antidepressant medications and a particular brand of birth control pills, called Yaz. Yaz contains drospirenone (aprogestin) and ethinyl estradiol (a form of estrogen) and has been shown to be clinically effective at treating the emotional and physical symptoms of PMDD, but should only be used to treat PMDD if you choose to use it for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Another form of birth control pill containing drospirenone plus a daily dose of folic acid also is FDA-approved to treat PMDD. It is sold under the brand names Beyaz and Safyral. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. Diagnosis There is no specific laboratory test to determine if you suffer from PMS, and diagnosis can take some time because symptoms are so varied. But there are certain characteristics that health care professionals consider. To qualify as PMS, symptoms must follow this general pattern: They tend to increase in severity as your cycle progresses. They improve within a few days of your menstrual period starting. They are present for at least two to three consecutive menstrual cycles. More than 150 physical and behavioral symptoms may be associated with PMS. The most common are irritability and anxiety/tension. Other symptoms include: Sudden mood swings Depression Headaches Joint and muscle aches Food cravings Fluid retention Forgetfulness Clumsiness Sleep disturbances Breast swelling and tenderness The timing and severity of these symptoms are key to a PMS diagnosis. An average menstrual cycle spans 21 to 35 days. The follicular phase extends from menses to ovulation, and the luteal phase extends from ovulation to menses. PMS occurs during the luteal phase—approximately the last 14 days of your cycle, usually during the five to seven days before you get your period. A premenstrual symptom chart or checklist (also called a menstrual cycle diary) is the most common method used to evaluate menstrual cycle symptoms. With this tool, you and your health care professional can track the type and severity of your symptoms, as well as when they occur, to identify a pattern that may indicate PMS. Follow these simple steps to determine if your symptoms fit the PMS pattern: Track your symptoms using the first day of menstrual flow as Day 1. (Note: Don't be surprised if you do not have any symptoms to record before day 18 or so.) Have a person close to you (your partner, roommate, friend) chart his or her impression of your symptoms, when they occur and their severity. Chart your symptoms for at least three consecutive months to help you and your health care professional identify a pattern that may indicate PMS. Record the date when/if any of the following symptoms occur over three consecutive months and note their severity (1 = mild; 2 = moderate; 3 = severe) Physical Symptoms Abdominal bloating Breast tenderness Constipation Diarrhea Dizziness Fatigue Headache Swelling of hands/feet Emotional Symptoms Anger Anxiety Depressed mood Irritability Mood swings Tension Behavioral Symptoms Crying spells and tearfulness Decreased or increased appetite Difficulty concentrating Difficulty sleeping Forgetfulness Hostility In addition to suggesting that you keep a menstrual cycle diary, your health care professional likely will ask about your personal and family medical history and will give you a physical exam. Laboratory tests are not routine but may be obtained to rule out other conditions with similar symptoms, such as low blood sugar (hypoglycemia), mania, depression, thyroid disorders, anemia, endometriosis, allergies, fibroids, dysmenorrhea, lupus, endocrine abnormalities, neurological problems such as brain tumors and heart problems. Menopause and PMS share some of the same symptoms, so depending on your age and health history, your health care professional may want to make sure that you are indeed ovulating and therefore experiencing PMS, not menopausal symptoms. To do this, you will probably be asked to use an over-the-counter ovulation testing kit. This is a simple test that you can do at home. The results tell you when ovulation is likely. If you are approaching menopause (the average age is about 51 for U.S. women, but ranges from 42 to 60 years), blood hormone tests may also be used to confirm if you are menopausal. However, a single blood test is not informative because hormone levels change often. Treatment Many premenstrual syndrome (PMS) symptoms improve with treatment. Treatment options range from medication therapy to birth control pills to diet modification, including vitamin and mineral supplementation, herbal medicines and exercise. Antidepressant drugs called selective serotonin reuptake inhibitors (SSRIs) are typically recommended to women with severe mood-related symptoms such as anxiety, depression or mood swings. Overall, common treatment options include: Nonsteroidal anti-inflammatory drugs (NSAIDs). These medications are used to relieve premenstrual headache and other menstrual-cycle related pain. A variety of NSAIDs are available including over-the-counter ibuprofen products (Motrin) and others or naproxen sodium (Aleve). They usually cost less and have fewer side effects than other treatments. Prescription NSAIDs also are available.Note: NSAIDS carry some risks, such as an increased risk of serious cardiovascular (CV) events, including heart attack and stroke. As a result, the FDA has issued a "black box" warning highlighting this risk, as well as the risk of potentially life-threatening stomach bleeding. If you've recently had heart surgery, you shouldn't take NSAIDS. All other women considering NSAIDS to ease PMS or any other condition should discuss these potential risks with their health care professional. Contraceptive hormones. Some women with PMS or PMDD experience relief of their symptoms after they start taking birth control pills. (Other women, however, feel worse on birth control pills.) You can take the pill continuously to avoid having a menstrual period, thus preventing the hormonal changes that can lead to PMS/PMDD. The combination birth control pills Yaz (containing 3 mg of drospirenone, a progestin, and 20 mcg ethinyl estradiol, a form of estrogen) and Beyaz and Safyral (containing 3 mg of drospirenone, 20 mcg ethinyl estradiol and a daily dose of folic acid) are FDA approved for the treatment of PMDD. However, these contraceptives should only be used to treat PMDD if you choose to use them for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. GnRH agonists (gonadotropin-releasing hormone). These medications include leuprolide (Lupron), among others. They belong to a class of hormones used to temporarily shrink fibroids and relieve endometriosis. They also may be recommended to treat PMS because they "turn off" the menstrual cycle by blocking estrogen production. Side effects may include menopausal symptoms like hot flashes, vaginal dryness and bone loss. That's why low-dose hormone therapy, a combination of estrogen and progestin hormones, is typically prescribed along with GnRH agonists. Some women may experience a return of their PMS symptoms with the additional hormone therapy. GnRH agonists are usually considered only as a short-term treatment option (given for no longer than six months) because of the increased health risks such as osteoporosis associated with low estrogen levels. Antidepressant medications. Antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are the preferred antidepressants for treating severe PMS and PMDD symptoms, including depression. SSRIs include sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac). Other types of antidepressants may also be prescribed to treat PMS and PMDD, including venlafaxine (Effexor) and clomipramine (Anafranil). The U.S. Food and Drug Administration warns that women taking antidepressants should monitor their symptoms closely, with the help of their health care professional, for signs that their condition is getting worse or that they are becoming suicidal, especially when they first start therapy or when their dose is increased or decreased. Danazol. Danazol (Danocrine) is a medication that works similarly to GnRH agonists to prevent ovulation. Danocrine works to improve PMS symptoms in some women, but it has some unpleasant side effects, such as acne and facial hair growth, so it is usually only used in women who do not respond to other treatments. Anti-anxiety medications such as alprazolam (Xanax) are sometimes prescribed when anxiety is the main symptom associated with PMS or PMDD. These drugs can be taken during the 14 days between ovulation and menstruation (the luteal phase) when symptoms occur (rather than daily). Dependence and serious withdrawal reactions can occur with Xanax, so its dosage and discontinuation should be carefully monitored. Calcium supplements (1,200 mg daily). Additional calcium in any form may help relieve some PMS symptoms. Low-fat dairy products (milk, yogurt and cheese) are a primary source of calcium, but you can also gain calcium from the following: Tofu and other soy products Rice milk Broccoli Dark greens, like turnip greens Green or red cabbage (raw) Salmon and sardines Taking an over-the-counter calcium supplement can also help. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. But be patient; it may take two to three months to relieve PMS symptoms with calcium supplementation. If symptoms persist, have your vitamin D levels checked or change the type of calcium supplement you're using. Low levels of vitamin D can affect how the body absorbs calcium, and some generic supplements may not have enough calcium available for absorption. Exercise. Regular exercise can also help relieve and possibly prevent PMS symptoms. You will get the greatest benefits if you exercise for at least 30 minutes, at least five days a week. But even taking a 20- to 30-minute walk three times a week can improve your mood. Chasteberry. The extract of the fruit of the chasteberry tree is shown to be a safe and effective treatment for PMS. This therapy is used primarily outside the United States. It may be obtained over the counter, but the dose and purity may be uncertain. In addition, there's some evidence that some nutritional supplements such as vitamin E, magnesium and vitamin B-6 may help ease symptoms of PMS. Discuss these and other strategies with your health care professional before taking any dietary supplement. There is no single treatment that works well for every woman who experiences PMS. Typically, it's wise to try the most conservative treatment options first, which include lifestyle changes such as modifying your diet and exercising more. Discuss your symptoms with your health care professional if strategies you've tried don't work, so he or she can recommend other treatment options. Prevention Can premenstrual syndrome (PMS) be prevented? Many women report benefits from a variety of lifestyle change including dietary changes, exercise and stress management. Dietary changes may include: Increasing calcium intake. Decreasing consumption of refined sugar. Decreasing or avoiding caffeine and nicotine, which act as stimulants and can increase tension and anxiety as well as interfere with sleep patterns. For some women, the severity of PMS symptoms increases as caffeine consumption increases. Decreasing alcohol consumption, which can act as a depressant. If you experience PMS, you may have an increased sensitivity to alcohol at certain points during your cycle. Decreasing salt intake and increasing water consumption to avoid water retention and bloating. Avoiding sodas, which may contain high levels of caffeine, salt, sugar and/or artificial sweeteners. Drinking natural diuretics, such as herbal teas. Ironically, some PMS symptoms, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume foods that aggravate the condition. Premenstrually, you may crave either refined sugar (usually combined with chocolate) or fat (combined with salt). Generally, foods high in refined sugars and fat temporarily raise energy levels. But within several hours or less, as your body metabolizes these foods, you may "crash," meaning you'll feel worse than before you ate them. Foods high in sugar content can also leave you feeling jittery. To alleviate mood swings and fatigue, try adding more high-quality, complex carbohydrates to your diet such as: Whole grain breads, pastas and cereals Potatoes (white or sweet) Rice (preferably brown or wild) Fresh vegetables, particularly corn and peas, such as chickpeas and lentils Fresh fruits These complex carbohydrates help keep blood sugar levels even while providing your body with a long-lasting source of energy. It's not uncommon for your appetite to increase just before your period begins. To combat the munchies and extra weight gain, try eating smaller, low-fat healthful meals using the food choices listed above. Make sure you include adequate calcium in your diet; calcium may help prevent irritability, anxiety and other PMS symptoms. Good sources of calcium include: Low-fat milk and milk products like yogurt, ice cream and cheese Broccoli Dark greens (like turnip greens) Green or red cabbage (raw) Cooked collards Salmon and sardines Soy products, such as tofu and soy milk Calcium-fortified orange and grapefruit juices Another good way to prevent PMS symptoms is through regular exercise in the form of aerobic activities such as brisk walking, jogging, biking or swimming. You will get the greatest benefits from exercise if you do it for at least 30 minutes, five or more days a week. But even taking a 20- to 30-minute walk three times a week can: Increase endorphin and serotonin production, brain chemicals that may help decrease pain and discomfort and improve mood, respectively Decrease stress and anxiety Increase REM sleep Other lifestyle changes that will help you control PMS include: Sleeping consistent hours Establishing a bedtime routine to help cue body and mind for sleeping Keeping a PMS symptom checklist, also called a menstrual cycle diary, to identify when symptoms and which symptoms occur so you can be prepared for them Facts to Know An estimated 75 percent of women of childbearing age suffer from PMS in some form. Approximately 3 to 8 percent of women experience premenstrual symptoms severe enough to disrupt their daily function and meet criteria for premenstrual dysphoric disorder (PMDD)––a severe form of PMS. Taking additional calcium in any form may help improve or even prevent PMS symptoms. Ideally, increase daily amounts of low-fat dairy products and other calcium-containing foods to reach the 1,200 mg of calcium daily health care professionals recommend. If you have trouble reaching this goal from your diet alone, consider using over-the counter calcium supplements. Symptoms of PMS may get worse with age. If you experience PMS, you may experience an increased sensitivity to alcohol at certain points in your menstrual cycle. Some evidence suggests that women who are vulnerable to depressive illness, panic disorder or other psychiatric or chronic medical disorders may be particularly susceptible to PMS. Strategies for PMS symptom relief include medication, dietary changes, exercise and stress management. Dietary changes to relieve PMS symptoms include increasing daily amounts of dietary or supplemental calcium, drinking more water and adding more complex carbohydrates (fruits, vegetables and grains) to your meals. Decreasing foods in your diet that contain refined sugar, limiting or avoiding caffeine and nicotine, decreasing alcohol consumption, decreasing salt intake and avoiding sodas may also help. Some of the PMS symptoms you may experience, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume high-fat foods and/or foods high in refined sugar, which actually aggravate these symptoms. Try to avoid them. Even women who have had hysterectomies can have symptoms of PMS if at least one functional ovary is left intact following the hysterectomy. Key Q&A What exactly is premenstrual syndrome (PMS)?There are more than 150 documented symptoms of PMS, but the number of symptoms seen in the vast majority of patients is much more limited. Some of the most common PMS symptoms include bloating, fatigue, sudden mood swings, irritability,anxiety, depression, weight gain, headaches, joint and muscle aches, food cravings and fluid retention. To be considered PMS symptoms, they must occur exclusively in the last 14 days of your menstrual cycle (usually about five to seven days before your period begins). True PMS symptoms tend to increase in severity as the cycle progresses, are relieved within a few days after the start of the menstrual flow and are present for at least two to three consecutive menstrual cycles. Cramps are not considered a symptom of PMS, but they can occur in women with PMS. What causes PMS?PMS appears to be caused by rising and falling levels of the hormones estrogen and progesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. How is PMS diagnosed?There is no single laboratory test for PMS, but one of the most common ways to diagnosis PMS is by keeping a daily checklist, chart or "menstrual cycle diary" that tracks when your premenstrual symptoms occurs for at least three months. Your health care professional should rule out other disorders or diseases that mimic or are identical to the symptoms caused by PMS before diagnosing you with the condition. These conditions include thyroid disorders, depression, endocrine abnormalities, menopause, heart problems, allergies and low blood sugar, among other conditions. Laboratory tests, personal and family medical histories and a physical exam are also part of the diagnostic process. Is PMS treatable?Yes! Many women experience some relief from PMS symptoms if they make diet and lifestyle changes, particularly increasing consumption of calcium, complex carbohydrates (fruits, vegetables, grains and beans) and water, and decreasing caffeine, alcohol, salt and refined sugar intake. Regular exercise and sleep may also help relieve symptoms. Certain medications can provide relief. When does PMS typically appear?PMS symptoms can appear any time between puberty and menopause, though the most common age for PMS to start to become a problem is during your late 20s to mid-30s. Will my PMS symptoms get better as I age?Probably not until you reach menopause. In some women, symptoms of PMS worsen with age and stress. Even women who have had hysterectomies can have PMS if at least one functional ovary is left intact following the hysterectomy. Once you reach menopause, your PMS symptoms will end with the end of menstruation. If I regularly take the recommended steps to relieve my PMS symptoms, how long before I may see results?It may take two to three months to experience relief from PMS symptoms. If you don't see any improvements by then, check with your health care professional for a new action plan. Are menstrual cramps a symptom of PMS?Cramps are not considered a symptom of PMS, although they may occur in women who have PMS. Called dysmenorrhea, cramps typically begin just before (24 to 48 hours) the onset of menstruation and disappear by the end of flow. Read the full article
0 notes
Text
Premenstrual Syndrome
Overview
Premenstrual syndrome (PMS) describes a wide range of severe, recurrent symptoms that occur from several days to two weeks before your period. PMS affects up to 75 percent of women in their childbearing years. The symptoms of PMS can appear any time between puberty and menopause, although the most common age for it to start to become a problem is during the late 20s to early 30s. Symptoms of PMS may get worse with age and stress, although the underlying causes are not well understood. Even women who have had hysterectomies can have PMS if at least one functional ovary is left. Women who are vulnerable to depressive illness, panic disorder, other psychiatric disorders orchronic medical conditions may also be susceptible to PMS, although these conditions may occur in women without PMS as well. Heredity may also play a role: if your mother or sister suffers from PMS, you may find you experience it, too. As many as 150 physical and behavioral symptoms have been assigned to PMS, but the number of PMS symptoms that most women experience is much more limited. The most common symptoms include irritability, bloating, mood swings, anxiety, depressed mood, fatigue, appetite changes, water retention and breast tenderness, among others. Menstrual cramps, or dysmenorrhea, are not considered a PMS symptom, although women with PMS may experience cramps. PMS appears to be caused by rising and falling levels of the hormones estrogen andprogesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It’s not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. Calcium may play a role in PMS. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. Dietary changes and exercise may also help relieve the discomfort of PMS symptoms. When symptoms are severe, serotonergic antidepressant medication may be prescribed. It is thought that increased serotonin reduces PMS symptoms. One of the most important strategies for coping with premenstrual discomfort is to be aware of any pattern your symptoms follow. The more aware you are of your symptoms—when they start and stop and what works best to relieve them, for example—the better you can develop strategies to recognize and cope with them—whatever they may be. Premenstrual Dysphoric Disorder Approximately three to eight percent of women experience premenstrual dysphoric disorder (PMDD), a condition that, like PMS, is associated with the menstrual cycle. The symptoms of PMDD are the same as PMS symptoms, although women with PMDD may experience more dysphoric (depressive) symptoms and more severe symptoms. In fact, to be diagnosed with PMDD, symptoms must be severe enough to disrupt a woman’s daily function. Symptoms must also meet diagnostic criteria specific to PMDD developed by the American Psychiatric Association. The most important criteria for a PMDD diagnosis are mood symptoms. Physical symptoms may also be present but aren’t as critical to the diagnosis. The difference between PMDD and mild PMS is like the difference between a mild tension headache and a migraine, experts say. Women who have a history of depression are at higher risk for PMDD than other women. Treatment for PMDD includes serotonergic antidepressant medications and a particular brand of birth control pills, called Yaz. Yaz contains drospirenone (aprogestin) and ethinyl estradiol (a form of estrogen) and has been shown to be clinically effective at treating the emotional and physical symptoms of PMDD, but should only be used to treat PMDD if you choose to use it for birth control because other forms of treatment don’t carry the same risks as oral contraceptives. Another form of birth control pill containing drospirenone plus a daily dose of folic acid also is FDA-approved to treat PMDD. It is sold under the brand names Beyaz and Safyral. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks.
Diagnosis
There is no specific laboratory test to determine if you suffer from PMS, and diagnosis can take some time because symptoms are so varied. But there are certain characteristics that health care professionals consider. To qualify as PMS, symptoms must follow this general pattern: They tend to increase in severity as your cycle progresses. They improve within a few days of your menstrual period starting. They are present for at least two to three consecutive menstrual cycles. More than 150 physical and behavioral symptoms may be associated with PMS. The most common are irritability and anxiety/tension. Other symptoms include:
Sudden mood swings Depression Headaches Joint and muscle aches Food cravings Fluid retention Forgetfulness Clumsiness Sleep disturbances Breast swelling and tenderness
The timing and severity of these symptoms are key to a PMS diagnosis. An average menstrual cycle spans 21 to 35 days. The follicular phase extends from menses to ovulation, and the luteal phase extends from ovulation to menses. PMS occurs during the luteal phase—approximately the last 14 days of your cycle, usually during the five to seven days before you get your period. A premenstrual symptom chart or checklist (also called a menstrual cycle diary) is the most common method used to evaluate menstrual cycle symptoms. With this tool, you and your health care professional can track the type and severity of your symptoms, as well as when they occur, to identify a pattern that may indicate PMS. Follow these simple steps to determine if your symptoms fit the PMS pattern: Track your symptoms using the first day of menstrual flow as Day 1. (Note: Don’t be surprised if you do not have any symptoms to record before day 18 or so.) Have a person close to you (your partner, roommate, friend) chart his or her impression of your symptoms, when they occur and their severity. Chart your symptoms for at least three consecutive months to help you and your health care professional identify a pattern that may indicate PMS. Record the date when/if any of the following symptoms occur over three consecutive months and note their severity (1 = mild; 2 = moderate; 3 = severe)
Physical Symptoms Abdominal bloating Breast tenderness Constipation Diarrhea Dizziness Fatigue Headache Swelling of hands/feet Emotional Symptoms Anger Anxiety Depressed mood Irritability Mood swings Tension Behavioral Symptoms Crying spells and tearfulness Decreased or increased appetite Difficulty concentrating Difficulty sleeping Forgetfulness Hostility
In addition to suggesting that you keep a menstrual cycle diary, your health care professional likely will ask about your personal and family medical history and will give you a physical exam. Laboratory tests are not routine but may be obtained to rule out other conditions with similar symptoms, such as low blood sugar (hypoglycemia), mania, depression, thyroid disorders, anemia, endometriosis, allergies, fibroids, dysmenorrhea, lupus, endocrine abnormalities, neurological problems such as brain tumors and heart problems. Menopause and PMS share some of the same symptoms, so depending on your age and health history, your health care professional may want to make sure that you are indeed ovulating and therefore experiencing PMS, not menopausal symptoms. To do this, you will probably be asked to use an over-the-counter ovulation testing kit. This is a simple test that you can do at home. The results tell you when ovulation is likely. If you are approaching menopause (the average age is about 51 for U.S. women, but ranges from 42 to 60 years), blood hormone tests may also be used to confirm if you are menopausal. However, a single blood test is not informative because hormone levels change often. Treatment
Many premenstrual syndrome (PMS) symptoms improve with treatment. Treatment options range from medication therapy to birth control pills to diet modification, including vitamin and mineral supplementation, herbal medicines and exercise. Antidepressant drugs called selective serotonin reuptake inhibitors (SSRIs) are typically recommended to women with severe mood-related symptoms such as anxiety, depression or mood swings. Overall, common treatment options include: Nonsteroidal anti-inflammatory drugs (NSAIDs). These medications are used to relieve premenstrual headache and other menstrual-cycle related pain. A variety of NSAIDs are available including over-the-counter ibuprofen products (Motrin) and others or naproxen sodium (Aleve). They usually cost less and have fewer side effects than other treatments. Prescription NSAIDs also are available.Note: NSAIDS carry some risks, such as an increased risk of serious cardiovascular (CV) events, including heart attack and stroke. As a result, the FDA has issued a “black box” warning highlighting this risk, as well as the risk of potentially life-threatening stomach bleeding. If you’ve recently had heart surgery, you shouldn’t take NSAIDS. All other women considering NSAIDS to ease PMS or any other condition should discuss these potential risks with their health care professional. Contraceptive hormones. Some women with PMS or PMDD experience relief of their symptoms after they start taking birth control pills. (Other women, however, feel worse on birth control pills.) You can take the pill continuously to avoid having a menstrual period, thus preventing the hormonal changes that can lead to PMS/PMDD. The combination birth control pills Yaz (containing 3 mg of drospirenone, a progestin, and 20 mcg ethinyl estradiol, a form of estrogen) and Beyaz and Safyral (containing 3 mg of drospirenone, 20 mcg ethinyl estradiol and a daily dose of folic acid) are FDA approved for the treatment of PMDD. However, these contraceptives should only be used to treat PMDD if you choose to use them for birth control because other forms of treatment don’t carry the same risks as oral contraceptives. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. GnRH agonists (gonadotropin-releasing hormone). These medications include leuprolide (Lupron), among others. They belong to a class of hormones used to temporarily shrink fibroids and relieve endometriosis. They also may be recommended to treat PMS because they “turn off” the menstrual cycle by blocking estrogen production. Side effects may include menopausal symptoms like hot flashes, vaginal dryness and bone loss. That’s why low-dose hormone therapy, a combination of estrogen and progestin hormones, is typically prescribed along with GnRH agonists. Some women may experience a return of their PMS symptoms with the additional hormone therapy. GnRH agonists are usually considered only as a short-term treatment option (given for no longer than six months) because of the increased health risks such as osteoporosis associated with low estrogen levels. Antidepressant medications. Antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are the preferred antidepressants for treating severe PMS and PMDD symptoms, including depression. SSRIs include sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac). Other types of antidepressants may also be prescribed to treat PMS and PMDD, including venlafaxine (Effexor) and clomipramine (Anafranil). The U.S. Food and Drug Administration warns that women taking antidepressants should monitor their symptoms closely, with the help of their health care professional, for signs that their condition is getting worse or that they are becoming suicidal, especially when they first start therapy or when their dose is increased or decreased. Danazol. Danazol (Danocrine) is a medication that works similarly to GnRH agonists to prevent ovulation. Danocrine works to improve PMS symptoms in some women, but it has some unpleasant side effects, such as acne and facial hair growth, so it is usually only used in women who do not respond to other treatments. Anti-anxiety medications such as alprazolam (Xanax) are sometimes prescribed when anxiety is the main symptom associated with PMS or PMDD. These drugs can be taken during the 14 days between ovulation and menstruation (the luteal phase) when symptoms occur (rather than daily). Dependence and serious withdrawal reactions can occur with Xanax, so its dosage and discontinuation should be carefully monitored. Calcium supplements (1,200 mg daily). Additional calcium in any form may help relieve some PMS symptoms. Low-fat dairy products (milk, yogurt and cheese) are a primary source of calcium, but you can also gain calcium from the following: Tofu and other soy products Rice milk Broccoli Dark greens, like turnip greens Green or red cabbage (raw) Salmon and sardines Taking an over-the-counter calcium supplement can also help. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. But be patient; it may take two to three months to relieve PMS symptoms with calcium supplementation. If symptoms persist, have your vitamin D levels checked or change the type of calcium supplement you’re using. Low levels of vitamin D can affect how the body absorbs calcium, and some generic supplements may not have enough calcium available for absorption. Exercise. Regular exercise can also help relieve and possibly prevent PMS symptoms. You will get the greatest benefits if you exercise for at least 30 minutes, at least five days a week. But even taking a 20- to 30-minute walk three times a week can improve your mood. Chasteberry. The extract of the fruit of the chasteberry tree is shown to be a safe and effective treatment for PMS. This therapy is used primarily outside the United States. It may be obtained over the counter, but the dose and purity may be uncertain. In addition, there’s some evidence that some nutritional supplements such as vitamin E, magnesium and vitamin B-6 may help ease symptoms of PMS. Discuss these and other strategies with your health care professional before taking any dietary supplement. There is no single treatment that works well for every woman who experiences PMS. Typically, it’s wise to try the most conservative treatment options first, which include lifestyle changes such as modifying your diet and exercising more. Discuss your symptoms with your health care professional if strategies you’ve tried don’t work, so he or she can recommend other treatment options.
Prevention
Can premenstrual syndrome (PMS) be prevented? Many women report benefits from a variety of lifestyle change including dietary changes, exercise and stress management. Dietary changes may include: Increasing calcium intake. Decreasing consumption of refined sugar. Decreasing or avoiding caffeine and nicotine, which act as stimulants and can increase tension and anxiety as well as interfere with sleep patterns. For some women, the severity of PMS symptoms increases as caffeine consumption increases. Decreasing alcohol consumption, which can act as a depressant. If you experience PMS, you may have an increased sensitivity to alcohol at certain points during your cycle. Decreasing salt intake and increasing water consumption to avoid water retention and bloating. Avoiding sodas, which may contain high levels of caffeine, salt, sugar and/or artificial sweeteners. Drinking natural diuretics, such as herbal teas. Ironically, some PMS symptoms, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume foods that aggravate the condition. Premenstrually, you may crave either refined sugar (usually combined with chocolate) or fat (combined with salt). Generally, foods high in refined sugars and fat temporarily raise energy levels. But within several hours or less, as your body metabolizes these foods, you may “crash,” meaning you’ll feel worse than before you ate them. Foods high in sugar content can also leave you feeling jittery. To alleviate mood swings and fatigue, try adding more high-quality, complex carbohydrates to your diet such as: Whole grain breads, pastas and cereals Potatoes (white or sweet) Rice (preferably brown or wild) Fresh vegetables, particularly corn and peas, such as chickpeas and lentils Fresh fruits These complex carbohydrates help keep blood sugar levels even while providing your body with a long-lasting source of energy. It’s not uncommon for your appetite to increase just before your period begins. To combat the munchies and extra weight gain, try eating smaller, low-fat healthful meals using the food choices listed above. Make sure you include adequate calcium in your diet; calcium may help prevent irritability, anxiety and other PMS symptoms. Good sources of calcium include: Low-fat milk and milk products like yogurt, ice cream and cheese Broccoli Dark greens (like turnip greens) Green or red cabbage (raw) Cooked collards Salmon and sardines Soy products, such as tofu and soy milk Calcium-fortified orange and grapefruit juices Another good way to prevent PMS symptoms is through regular exercise in the form of aerobic activities such as brisk walking, jogging, biking or swimming. You will get the greatest benefits from exercise if you do it for at least 30 minutes, five or more days a week. But even taking a 20- to 30-minute walk three times a week can: Increase endorphin and serotonin production, brain chemicals that may help decrease pain and discomfort and improve mood, respectively Decrease stress and anxiety Increase REM sleep Other lifestyle changes that will help you control PMS include: Sleeping consistent hours Establishing a bedtime routine to help cue body and mind for sleeping Keeping a PMS symptom checklist, also called a menstrual cycle diary, to identify when symptoms and which symptoms occur so you can be prepared for them Facts to Know
An estimated 75 percent of women of childbearing age suffer from PMS in some form. Approximately 3 to 8 percent of women experience premenstrual symptoms severe enough to disrupt their daily function and meet criteria for premenstrual dysphoric disorder (PMDD)––a severe form of PMS. Taking additional calcium in any form may help improve or even prevent PMS symptoms. Ideally, increase daily amounts of low-fat dairy products and other calcium-containing foods to reach the 1,200 mg of calcium daily health care professionals recommend. If you have trouble reaching this goal from your diet alone, consider using over-the counter calcium supplements. Symptoms of PMS may get worse with age. If you experience PMS, you may experience an increased sensitivity to alcohol at certain points in your menstrual cycle. Some evidence suggests that women who are vulnerable to depressive illness, panic disorder or other psychiatric or chronic medical disorders may be particularly susceptible to PMS. Strategies for PMS symptom relief include medication, dietary changes, exercise and stress management. Dietary changes to relieve PMS symptoms include increasing daily amounts of dietary or supplemental calcium, drinking more water and adding more complex carbohydrates (fruits, vegetables and grains) to your meals. Decreasing foods in your diet that contain refined sugar, limiting or avoiding caffeine and nicotine, decreasing alcohol consumption, decreasing salt intake and avoiding sodas may also help. Some of the PMS symptoms you may experience, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume high-fat foods and/or foods high in refined sugar, which actually aggravate these symptoms. Try to avoid them. Even women who have had hysterectomies can have symptoms of PMS if at least one functional ovary is left intact following the hysterectomy.
Key Q&A
What exactly is premenstrual syndrome (PMS)?There are more than 150 documented symptoms of PMS, but the number of symptoms seen in the vast majority of patients is much more limited. Some of the most common PMS symptoms include bloating, fatigue, sudden mood swings, irritability,anxiety, depression, weight gain, headaches, joint and muscle aches, food cravings and fluid retention. To be considered PMS symptoms, they must occur exclusively in the last 14 days of your menstrual cycle (usually about five to seven days before your period begins). True PMS symptoms tend to increase in severity as the cycle progresses, are relieved within a few days after the start of the menstrual flow and are present for at least two to three consecutive menstrual cycles. Cramps are not considered a symptom of PMS, but they can occur in women with PMS. What causes PMS?PMS appears to be caused by rising and falling levels of the hormones estrogen and progesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It’s not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. How is PMS diagnosed?There is no single laboratory test for PMS, but one of the most common ways to diagnosis PMS is by keeping a daily checklist, chart or “menstrual cycle diary” that tracks when your premenstrual symptoms occurs for at least three months. Your health care professional should rule out other disorders or diseases that mimic or are identical to the symptoms caused by PMS before diagnosing you with the condition. These conditions include thyroid disorders, depression, endocrine abnormalities, menopause, heart problems, allergies and low blood sugar, among other conditions. Laboratory tests, personal and family medical histories and a physical exam are also part of the diagnostic process. Is PMS treatable?Yes! Many women experience some relief from PMS symptoms if they make diet and lifestyle changes, particularly increasing consumption of calcium, complex carbohydrates (fruits, vegetables, grains and beans) and water, and decreasing caffeine, alcohol, salt and refined sugar intake. Regular exercise and sleep may also help relieve symptoms. Certain medications can provide relief. When does PMS typically appear?PMS symptoms can appear any time between puberty and menopause, though the most common age for PMS to start to become a problem is during your late 20s to mid-30s. Will my PMS symptoms get better as I age?Probably not until you reach menopause. In some women, symptoms of PMS worsen with age and stress. Even women who have had hysterectomies can have PMS if at least one functional ovary is left intact following the hysterectomy. Once you reach menopause, your PMS symptoms will end with the end of menstruation. If I regularly take the recommended steps to relieve my PMS symptoms, how long before I may see results?It may take two to three months to experience relief from PMS symptoms. If you don’t see any improvements by then, check with your health care professional for a new action plan. Are menstrual cramps a symptom of PMS?Cramps are not considered a symptom of PMS, although they may occur in women who have PMS. Called dysmenorrhea, cramps typically begin just before (24 to 48 hours) the onset of menstruation and disappear by the end of flow.
For more Information visit us our website: safegenericpharmacy.com
0 notes
Text
Premenstrual Syndrome describes
Overview
Premenstrual syndrome (PMS) describes a wide range of severe, recurrent symptoms that occur from several days to two weeks before your period. PMS affects up to 75 percent of women in their childbearing years. The symptoms of PMS can appear any time between puberty and menopause, although the most common age for it to start to become a problem is during the late 20s to early 30s. Symptoms of PMS may get worse with age and stress, although the underlying causes are not well understood. Even women who have had hysterectomies can have PMS if at least one functional ovary is left. Women who are vulnerable to depressive illness, panic disorder, other psychiatric disorders orchronic medical conditions may also be susceptible to PMS, although these conditions may occur in women without PMS as well. Heredity may also play a role: if your mother or sister suffers from PMS, you may find you experience it, too. As many as 150 physical and behavioral symptoms have been assigned to PMS, but the number of PMS symptoms that most women experience is much more limited. The most common symptoms include irritability, bloating, mood swings, anxiety, depressed mood, fatigue, appetite changes, water retention and breast tenderness, among others. Menstrual cramps, or dysmenorrhea, are not considered a PMS symptom, although women with PMS may experience cramps. PMS appears to be caused by rising and falling levels of the hormones estrogen andprogesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. Calcium may play a role in PMS. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. Dietary changes and exercise may also help relieve the discomfort of PMS symptoms. When symptoms are severe, serotonergic antidepressant medication may be prescribed. It is thought that increased serotonin reduces PMS symptoms. One of the most important strategies for coping with premenstrual discomfort is to be aware of any pattern your symptoms follow. The more aware you are of your symptoms—when they start and stop and what works best to relieve them, for example—the better you can develop strategies to recognize and cope with them—whatever they may be. Premenstrual Dysphoric Disorder Approximately three to eight percent of women experience premenstrual dysphoric disorder (PMDD), a condition that, like PMS, is associated with the menstrual cycle. The symptoms of PMDD are the same as PMS symptoms, although women with PMDD may experience more dysphoric (depressive) symptoms and more severe symptoms. In fact, to be diagnosed with PMDD, symptoms must be severe enough to disrupt a woman's daily function. Symptoms must also meet diagnostic criteria specific to PMDD developed by the American Psychiatric Association. The most important criteria for a PMDD diagnosis are mood symptoms. Physical symptoms may also be present but aren't as critical to the diagnosis. The difference between PMDD and mild PMS is like the difference between a mild tension headache and a migraine, experts say. Women who have a history of depression are at higher risk for PMDD than other women. Treatment for PMDD includes serotonergic antidepressant medications and a particular brand of birth control pills, called Yaz. Yaz contains drospirenone (aprogestin) and ethinyl estradiol (a form of estrogen) and has been shown to be clinically effective at treating the emotional and physical symptoms of PMDD, but should only be used to treat PMDD if you choose to use it for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Another form of birth control pill containing drospirenone plus a daily dose of folic acid also is FDA-approved to treat PMDD. It is sold under the brand names Beyaz and Safyral. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. Diagnosis There is no specific laboratory test to determine if you suffer from PMS, and diagnosis can take some time because symptoms are so varied. But there are certain characteristics that health care professionals consider. To qualify as PMS, symptoms must follow this general pattern: They tend to increase in severity as your cycle progresses. They improve within a few days of your menstrual period starting. They are present for at least two to three consecutive menstrual cycles. More than 150 physical and behavioral symptoms may be associated with PMS. The most common are irritability and anxiety/tension. Other symptoms include: Sudden mood swings Depression Headaches Joint and muscle aches Food cravings Fluid retention Forgetfulness Clumsiness Sleep disturbances Breast swelling and tenderness The timing and severity of these symptoms are key to a PMS diagnosis. An average menstrual cycle spans 21 to 35 days. The follicular phase extends from menses to ovulation, and the luteal phase extends from ovulation to menses. PMS occurs during the luteal phase—approximately the last 14 days of your cycle, usually during the five to seven days before you get your period. A premenstrual symptom chart or checklist (also called a menstrual cycle diary) is the most common method used to evaluate menstrual cycle symptoms. With this tool, you and your health care professional can track the type and severity of your symptoms, as well as when they occur, to identify a pattern that may indicate PMS. Follow these simple steps to determine if your symptoms fit the PMS pattern: Track your symptoms using the first day of menstrual flow as Day 1. (Note: Don't be surprised if you do not have any symptoms to record before day 18 or so.) Have a person close to you (your partner, roommate, friend) chart his or her impression of your symptoms, when they occur and their severity. Chart your symptoms for at least three consecutive months to help you and your health care professional identify a pattern that may indicate PMS. Record the date when/if any of the following symptoms occur over three consecutive months and note their severity (1 = mild; 2 = moderate; 3 = severe) Physical Symptoms Abdominal bloating Breast tenderness Constipation Diarrhea Dizziness Fatigue Headache Swelling of hands/feet Emotional Symptoms Anger Anxiety Depressed mood Irritability Mood swings Tension Behavioral Symptoms Crying spells and tearfulness Decreased or increased appetite Difficulty concentrating Difficulty sleeping Forgetfulness Hostility In addition to suggesting that you keep a menstrual cycle diary, your health care professional likely will ask about your personal and family medical history and will give you a physical exam. Laboratory tests are not routine but may be obtained to rule out other conditions with similar symptoms, such as low blood sugar (hypoglycemia), mania, depression, thyroid disorders, anemia, endometriosis, allergies, fibroids, dysmenorrhea, lupus, endocrine abnormalities, neurological problems such as brain tumors and heart problems. Menopause and PMS share some of the same symptoms, so depending on your age and health history, your health care professional may want to make sure that you are indeed ovulating and therefore experiencing PMS, not menopausal symptoms. To do this, you will probably be asked to use an over-the-counter ovulation testing kit. This is a simple test that you can do at home. The results tell you when ovulation is likely. If you are approaching menopause (the average age is about 51 for U.S. women, but ranges from 42 to 60 years), blood hormone tests may also be used to confirm if you are menopausal. However, a single blood test is not informative because hormone levels change often. Treatment Many premenstrual syndrome (PMS) symptoms improve with treatment. Treatment options range from medication therapy to birth control pills to diet modification, including vitamin and mineral supplementation, herbal medicines and exercise. Antidepressant drugs called selective serotonin reuptake inhibitors (SSRIs) are typically recommended to women with severe mood-related symptoms such as anxiety, depression or mood swings. Overall, common treatment options include: Nonsteroidal anti-inflammatory drugs (NSAIDs). These medications are used to relieve premenstrual headache and other menstrual-cycle related pain. A variety of NSAIDs are available including over-the-counter ibuprofen products (Motrin) and others or naproxen sodium (Aleve). They usually cost less and have fewer side effects than other treatments. Prescription NSAIDs also are available.Note: NSAIDS carry some risks, such as an increased risk of serious cardiovascular (CV) events, including heart attack and stroke. As a result, the FDA has issued a "black box" warning highlighting this risk, as well as the risk of potentially life-threatening stomach bleeding. If you've recently had heart surgery, you shouldn't take NSAIDS. All other women considering NSAIDS to ease PMS or any other condition should discuss these potential risks with their health care professional. Contraceptive hormones. Some women with PMS or PMDD experience relief of their symptoms after they start taking birth control pills. (Other women, however, feel worse on birth control pills.) You can take the pill continuously to avoid having a menstrual period, thus preventing the hormonal changes that can lead to PMS/PMDD. The combination birth control pills Yaz (containing 3 mg of drospirenone, a progestin, and 20 mcg ethinyl estradiol, a form of estrogen) and Beyaz and Safyral (containing 3 mg of drospirenone, 20 mcg ethinyl estradiol and a daily dose of folic acid) are FDA approved for the treatment of PMDD. However, these contraceptives should only be used to treat PMDD if you choose to use them for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. GnRH agonists (gonadotropin-releasing hormone). These medications include leuprolide (Lupron), among others. They belong to a class of hormones used to temporarily shrink fibroids and relieve endometriosis. They also may be recommended to treat PMS because they "turn off" the menstrual cycle by blocking estrogen production. Side effects may include menopausal symptoms like hot flashes, vaginal dryness and bone loss. That's why low-dose hormone therapy, a combination of estrogen and progestin hormones, is typically prescribed along with GnRH agonists. Some women may experience a return of their PMS symptoms with the additional hormone therapy. GnRH agonists are usually considered only as a short-term treatment option (given for no longer than six months) because of the increased health risks such as osteoporosis associated with low estrogen levels. Antidepressant medications. Antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are the preferred antidepressants for treating severe PMS and PMDD symptoms, including depression. SSRIs include sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac). Other types of antidepressants may also be prescribed to treat PMS and PMDD, including venlafaxine (Effexor) and clomipramine (Anafranil). The U.S. Food and Drug Administration warns that women taking antidepressants should monitor their symptoms closely, with the help of their health care professional, for signs that their condition is getting worse or that they are becoming suicidal, especially when they first start therapy or when their dose is increased or decreased. Danazol. Danazol (Danocrine) is a medication that works similarly to GnRH agonists to prevent ovulation. Danocrine works to improve PMS symptoms in some women, but it has some unpleasant side effects, such as acne and facial hair growth, so it is usually only used in women who do not respond to other treatments. Anti-anxiety medications such as alprazolam (Xanax) are sometimes prescribed when anxiety is the main symptom associated with PMS or PMDD. These drugs can be taken during the 14 days between ovulation and menstruation (the luteal phase) when symptoms occur (rather than daily). Dependence and serious withdrawal reactions can occur with Xanax, so its dosage and discontinuation should be carefully monitored. Calcium supplements (1,200 mg daily). Additional calcium in any form may help relieve some PMS symptoms. Low-fat dairy products (milk, yogurt and cheese) are a primary source of calcium, but you can also gain calcium from the following: Tofu and other soy products Rice milk Broccoli Dark greens, like turnip greens Green or red cabbage (raw) Salmon and sardines Taking an over-the-counter calcium supplement can also help. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. But be patient; it may take two to three months to relieve PMS symptoms with calcium supplementation. If symptoms persist, have your vitamin D levels checked or change the type of calcium supplement you're using. Low levels of vitamin D can affect how the body absorbs calcium, and some generic supplements may not have enough calcium available for absorption. Exercise. Regular exercise can also help relieve and possibly prevent PMS symptoms. You will get the greatest benefits if you exercise for at least 30 minutes, at least five days a week. But even taking a 20- to 30-minute walk three times a week can improve your mood. Chasteberry. The extract of the fruit of the chasteberry tree is shown to be a safe and effective treatment for PMS. This therapy is used primarily outside the United States. It may be obtained over the counter, but the dose and purity may be uncertain. In addition, there's some evidence that some nutritional supplements such as vitamin E, magnesium and vitamin B-6 may help ease symptoms of PMS. Discuss these and other strategies with your health care professional before taking any dietary supplement. There is no single treatment that works well for every woman who experiences PMS. Typically, it's wise to try the most conservative treatment options first, which include lifestyle changes such as modifying your diet and exercising more. Discuss your symptoms with your health care professional if strategies you've tried don't work, so he or she can recommend other treatment options. Prevention Can premenstrual syndrome (PMS) be prevented? Many women report benefits from a variety of lifestyle change including dietary changes, exercise and stress management. Dietary changes may include: Increasing calcium intake. Decreasing consumption of refined sugar. Decreasing or avoiding caffeine and nicotine, which act as stimulants and can increase tension and anxiety as well as interfere with sleep patterns. For some women, the severity of PMS symptoms increases as caffeine consumption increases. Decreasing alcohol consumption, which can act as a depressant. If you experience PMS, you may have an increased sensitivity to alcohol at certain points during your cycle. Decreasing salt intake and increasing water consumption to avoid water retention and bloating. Avoiding sodas, which may contain high levels of caffeine, salt, sugar and/or artificial sweeteners. Drinking natural diuretics, such as herbal teas. Ironically, some PMS symptoms, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume foods that aggravate the condition. Premenstrually, you may crave either refined sugar (usually combined with chocolate) or fat (combined with salt). Generally, foods high in refined sugars and fat temporarily raise energy levels. But within several hours or less, as your body metabolizes these foods, you may "crash," meaning you'll feel worse than before you ate them. Foods high in sugar content can also leave you feeling jittery. To alleviate mood swings and fatigue, try adding more high-quality, complex carbohydrates to your diet such as: Whole grain breads, pastas and cereals Potatoes (white or sweet) Rice (preferably brown or wild) Fresh vegetables, particularly corn and peas, such as chickpeas and lentils Fresh fruits These complex carbohydrates help keep blood sugar levels even while providing your body with a long-lasting source of energy. It's not uncommon for your appetite to increase just before your period begins. To combat the munchies and extra weight gain, try eating smaller, low-fat healthful meals using the food choices listed above. Make sure you include adequate calcium in your diet; calcium may help prevent irritability, anxiety and other PMS symptoms. Good sources of calcium include: Low-fat milk and milk products like yogurt, ice cream and cheese Broccoli Dark greens (like turnip greens) Green or red cabbage (raw) Cooked collards Salmon and sardines Soy products, such as tofu and soy milk Calcium-fortified orange and grapefruit juices Another good way to prevent PMS symptoms is through regular exercise in the form of aerobic activities such as brisk walking, jogging, biking or swimming. You will get the greatest benefits from exercise if you do it for at least 30 minutes, five or more days a week. But even taking a 20- to 30-minute walk three times a week can: Increase endorphin and serotonin production, brain chemicals that may help decrease pain and discomfort and improve mood, respectively Decrease stress and anxiety Increase REM sleep Other lifestyle changes that will help you control PMS include: Sleeping consistent hours Establishing a bedtime routine to help cue body and mind for sleeping Keeping a PMS symptom checklist, also called a menstrual cycle diary, to identify when symptoms and which symptoms occur so you can be prepared for them Facts to Know An estimated 75 percent of women of childbearing age suffer from PMS in some form. Approximately 3 to 8 percent of women experience premenstrual symptoms severe enough to disrupt their daily function and meet criteria for premenstrual dysphoric disorder (PMDD)––a severe form of PMS. Taking additional calcium in any form may help improve or even prevent PMS symptoms. Ideally, increase daily amounts of low-fat dairy products and other calcium-containing foods to reach the 1,200 mg of calcium daily health care professionals recommend. If you have trouble reaching this goal from your diet alone, consider using over-the counter calcium supplements. Symptoms of PMS may get worse with age. If you experience PMS, you may experience an increased sensitivity to alcohol at certain points in your menstrual cycle. Some evidence suggests that women who are vulnerable to depressive illness, panic disorder or other psychiatric or chronic medical disorders may be particularly susceptible to PMS. Strategies for PMS symptom relief include medication, dietary changes, exercise and stress management. Dietary changes to relieve PMS symptoms include increasing daily amounts of dietary or supplemental calcium, drinking more water and adding more complex carbohydrates (fruits, vegetables and grains) to your meals. Decreasing foods in your diet that contain refined sugar, limiting or avoiding caffeine and nicotine, decreasing alcohol consumption, decreasing salt intake and avoiding sodas may also help. Some of the PMS symptoms you may experience, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume high-fat foods and/or foods high in refined sugar, which actually aggravate these symptoms. Try to avoid them. Even women who have had hysterectomies can have symptoms of PMS if at least one functional ovary is left intact following the hysterectomy. Key Q&A What exactly is premenstrual syndrome (PMS)?There are more than 150 documented symptoms of PMS, but the number of symptoms seen in the vast majority of patients is much more limited. Some of the most common PMS symptoms include bloating, fatigue, sudden mood swings, irritability,anxiety, depression, weight gain, headaches, joint and muscle aches, food cravings and fluid retention. To be considered PMS symptoms, they must occur exclusively in the last 14 days of your menstrual cycle (usually about five to seven days before your period begins). True PMS symptoms tend to increase in severity as the cycle progresses, are relieved within a few days after the start of the menstrual flow and are present for at least two to three consecutive menstrual cycles. Cramps are not considered a symptom of PMS, but they can occur in women with PMS. What causes PMS?PMS appears to be caused by rising and falling levels of the hormones estrogen and progesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. How is PMS diagnosed?There is no single laboratory test for PMS, but one of the most common ways to diagnosis PMS is by keeping a daily checklist, chart or "menstrual cycle diary" that tracks when your premenstrual symptoms occurs for at least three months. Your health care professional should rule out other disorders or diseases that mimic or are identical to the symptoms caused by PMS before diagnosing you with the condition. These conditions include thyroid disorders, depression, endocrine abnormalities, menopause, heart problems, allergies and low blood sugar, among other conditions. Laboratory tests, personal and family medical histories and a physical exam are also part of the diagnostic process. Is PMS treatable?Yes! Many women experience some relief from PMS symptoms if they make diet and lifestyle changes, particularly increasing consumption of calcium, complex carbohydrates (fruits, vegetables, grains and beans) and water, and decreasing caffeine, alcohol, salt and refined sugar intake. Regular exercise and sleep may also help relieve symptoms. Certain medications can provide relief. When does PMS typically appear?PMS symptoms can appear any time between puberty and menopause, though the most common age for PMS to start to become a problem is during your late 20s to mid-30s. Will my PMS symptoms get better as I age?Probably not until you reach menopause. In some women, symptoms of PMS worsen with age and stress. Even women who have had hysterectomies can have PMS if at least one functional ovary is left intact following the hysterectomy. Once you reach menopause, your PMS symptoms will end with the end of menstruation. If I regularly take the recommended steps to relieve my PMS symptoms, how long before I may see results?It may take two to three months to experience relief from PMS symptoms. If you don't see any improvements by then, check with your health care professional for a new action plan. Are menstrual cramps a symptom of PMS?Cramps are not considered a symptom of PMS, although they may occur in women who have PMS. Called dysmenorrhea, cramps typically begin just before (24 to 48 hours) the onset of menstruation and disappear by the end of flow. Read the full article
0 notes
Text
Premenstrual Syndrome describes
Overview
Premenstrual syndrome (PMS) describes a wide range of severe, recurrent symptoms that occur from several days to two weeks before your period. PMS affects up to 75 percent of women in their childbearing years. The symptoms of PMS can appear any time between puberty and menopause, although the most common age for it to start to become a problem is during the late 20s to early 30s. Symptoms of PMS may get worse with age and stress, although the underlying causes are not well understood. Even women who have had hysterectomies can have PMS if at least one functional ovary is left. Women who are vulnerable to depressive illness, panic disorder, other psychiatric disorders orchronic medical conditions may also be susceptible to PMS, although these conditions may occur in women without PMS as well. Heredity may also play a role: if your mother or sister suffers from PMS, you may find you experience it, too. As many as 150 physical and behavioral symptoms have been assigned to PMS, but the number of PMS symptoms that most women experience is much more limited. The most common symptoms include irritability, bloating, mood swings, anxiety, depressed mood, fatigue, appetite changes, water retention and breast tenderness, among others. Menstrual cramps, or dysmenorrhea, are not considered a PMS symptom, although women with PMS may experience cramps. PMS appears to be caused by rising and falling levels of the hormones estrogen andprogesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. Calcium may play a role in PMS. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. Dietary changes and exercise may also help relieve the discomfort of PMS symptoms. When symptoms are severe, serotonergic antidepressant medication may be prescribed. It is thought that increased serotonin reduces PMS symptoms. One of the most important strategies for coping with premenstrual discomfort is to be aware of any pattern your symptoms follow. The more aware you are of your symptoms—when they start and stop and what works best to relieve them, for example—the better you can develop strategies to recognize and cope with them—whatever they may be. Premenstrual Dysphoric Disorder Approximately three to eight percent of women experience premenstrual dysphoric disorder (PMDD), a condition that, like PMS, is associated with the menstrual cycle. The symptoms of PMDD are the same as PMS symptoms, although women with PMDD may experience more dysphoric (depressive) symptoms and more severe symptoms. In fact, to be diagnosed with PMDD, symptoms must be severe enough to disrupt a woman's daily function. Symptoms must also meet diagnostic criteria specific to PMDD developed by the American Psychiatric Association. The most important criteria for a PMDD diagnosis are mood symptoms. Physical symptoms may also be present but aren't as critical to the diagnosis. The difference between PMDD and mild PMS is like the difference between a mild tension headache and a migraine, experts say. Women who have a history of depression are at higher risk for PMDD than other women. Treatment for PMDD includes serotonergic antidepressant medications and a particular brand of birth control pills, called Yaz. Yaz contains drospirenone (aprogestin) and ethinyl estradiol (a form of estrogen) and has been shown to be clinically effective at treating the emotional and physical symptoms of PMDD, but should only be used to treat PMDD if you choose to use it for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Another form of birth control pill containing drospirenone plus a daily dose of folic acid also is FDA-approved to treat PMDD. It is sold under the brand names Beyaz and Safyral. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. Diagnosis There is no specific laboratory test to determine if you suffer from PMS, and diagnosis can take some time because symptoms are so varied. But there are certain characteristics that health care professionals consider. To qualify as PMS, symptoms must follow this general pattern: They tend to increase in severity as your cycle progresses. They improve within a few days of your menstrual period starting. They are present for at least two to three consecutive menstrual cycles. More than 150 physical and behavioral symptoms may be associated with PMS. The most common are irritability and anxiety/tension. Other symptoms include: Sudden mood swings Depression Headaches Joint and muscle aches Food cravings Fluid retention Forgetfulness Clumsiness Sleep disturbances Breast swelling and tenderness The timing and severity of these symptoms are key to a PMS diagnosis. An average menstrual cycle spans 21 to 35 days. The follicular phase extends from menses to ovulation, and the luteal phase extends from ovulation to menses. PMS occurs during the luteal phase—approximately the last 14 days of your cycle, usually during the five to seven days before you get your period. A premenstrual symptom chart or checklist (also called a menstrual cycle diary) is the most common method used to evaluate menstrual cycle symptoms. With this tool, you and your health care professional can track the type and severity of your symptoms, as well as when they occur, to identify a pattern that may indicate PMS. Follow these simple steps to determine if your symptoms fit the PMS pattern: Track your symptoms using the first day of menstrual flow as Day 1. (Note: Don't be surprised if you do not have any symptoms to record before day 18 or so.) Have a person close to you (your partner, roommate, friend) chart his or her impression of your symptoms, when they occur and their severity. Chart your symptoms for at least three consecutive months to help you and your health care professional identify a pattern that may indicate PMS. Record the date when/if any of the following symptoms occur over three consecutive months and note their severity (1 = mild; 2 = moderate; 3 = severe) Physical Symptoms Abdominal bloating Breast tenderness Constipation Diarrhea Dizziness Fatigue Headache Swelling of hands/feet Emotional Symptoms Anger Anxiety Depressed mood Irritability Mood swings Tension Behavioral Symptoms Crying spells and tearfulness Decreased or increased appetite Difficulty concentrating Difficulty sleeping Forgetfulness Hostility In addition to suggesting that you keep a menstrual cycle diary, your health care professional likely will ask about your personal and family medical history and will give you a physical exam. Laboratory tests are not routine but may be obtained to rule out other conditions with similar symptoms, such as low blood sugar (hypoglycemia), mania, depression, thyroid disorders, anemia, endometriosis, allergies, fibroids, dysmenorrhea, lupus, endocrine abnormalities, neurological problems such as brain tumors and heart problems. Menopause and PMS share some of the same symptoms, so depending on your age and health history, your health care professional may want to make sure that you are indeed ovulating and therefore experiencing PMS, not menopausal symptoms. To do this, you will probably be asked to use an over-the-counter ovulation testing kit. This is a simple test that you can do at home. The results tell you when ovulation is likely. If you are approaching menopause (the average age is about 51 for U.S. women, but ranges from 42 to 60 years), blood hormone tests may also be used to confirm if you are menopausal. However, a single blood test is not informative because hormone levels change often. Treatment Many premenstrual syndrome (PMS) symptoms improve with treatment. Treatment options range from medication therapy to birth control pills to diet modification, including vitamin and mineral supplementation, herbal medicines and exercise. Antidepressant drugs called selective serotonin reuptake inhibitors (SSRIs) are typically recommended to women with severe mood-related symptoms such as anxiety, depression or mood swings. Overall, common treatment options include: Nonsteroidal anti-inflammatory drugs (NSAIDs). These medications are used to relieve premenstrual headache and other menstrual-cycle related pain. A variety of NSAIDs are available including over-the-counter ibuprofen products (Motrin) and others or naproxen sodium (Aleve). They usually cost less and have fewer side effects than other treatments. Prescription NSAIDs also are available.Note: NSAIDS carry some risks, such as an increased risk of serious cardiovascular (CV) events, including heart attack and stroke. As a result, the FDA has issued a "black box" warning highlighting this risk, as well as the risk of potentially life-threatening stomach bleeding. If you've recently had heart surgery, you shouldn't take NSAIDS. All other women considering NSAIDS to ease PMS or any other condition should discuss these potential risks with their health care professional. Contraceptive hormones. Some women with PMS or PMDD experience relief of their symptoms after they start taking birth control pills. (Other women, however, feel worse on birth control pills.) You can take the pill continuously to avoid having a menstrual period, thus preventing the hormonal changes that can lead to PMS/PMDD. The combination birth control pills Yaz (containing 3 mg of drospirenone, a progestin, and 20 mcg ethinyl estradiol, a form of estrogen) and Beyaz and Safyral (containing 3 mg of drospirenone, 20 mcg ethinyl estradiol and a daily dose of folic acid) are FDA approved for the treatment of PMDD. However, these contraceptives should only be used to treat PMDD if you choose to use them for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. GnRH agonists (gonadotropin-releasing hormone). These medications include leuprolide (Lupron), among others. They belong to a class of hormones used to temporarily shrink fibroids and relieve endometriosis. They also may be recommended to treat PMS because they "turn off" the menstrual cycle by blocking estrogen production. Side effects may include menopausal symptoms like hot flashes, vaginal dryness and bone loss. That's why low-dose hormone therapy, a combination of estrogen and progestin hormones, is typically prescribed along with GnRH agonists. Some women may experience a return of their PMS symptoms with the additional hormone therapy. GnRH agonists are usually considered only as a short-term treatment option (given for no longer than six months) because of the increased health risks such as osteoporosis associated with low estrogen levels. Antidepressant medications. Antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are the preferred antidepressants for treating severe PMS and PMDD symptoms, including depression. SSRIs include sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac). Other types of antidepressants may also be prescribed to treat PMS and PMDD, including venlafaxine (Effexor) and clomipramine (Anafranil). The U.S. Food and Drug Administration warns that women taking antidepressants should monitor their symptoms closely, with the help of their health care professional, for signs that their condition is getting worse or that they are becoming suicidal, especially when they first start therapy or when their dose is increased or decreased. Danazol. Danazol (Danocrine) is a medication that works similarly to GnRH agonists to prevent ovulation. Danocrine works to improve PMS symptoms in some women, but it has some unpleasant side effects, such as acne and facial hair growth, so it is usually only used in women who do not respond to other treatments. Anti-anxiety medications such as alprazolam (Xanax) are sometimes prescribed when anxiety is the main symptom associated with PMS or PMDD. These drugs can be taken during the 14 days between ovulation and menstruation (the luteal phase) when symptoms occur (rather than daily). Dependence and serious withdrawal reactions can occur with Xanax, so its dosage and discontinuation should be carefully monitored. Calcium supplements (1,200 mg daily). Additional calcium in any form may help relieve some PMS symptoms. Low-fat dairy products (milk, yogurt and cheese) are a primary source of calcium, but you can also gain calcium from the following: Tofu and other soy products Rice milk Broccoli Dark greens, like turnip greens Green or red cabbage (raw) Salmon and sardines Taking an over-the-counter calcium supplement can also help. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. But be patient; it may take two to three months to relieve PMS symptoms with calcium supplementation. If symptoms persist, have your vitamin D levels checked or change the type of calcium supplement you're using. Low levels of vitamin D can affect how the body absorbs calcium, and some generic supplements may not have enough calcium available for absorption. Exercise. Regular exercise can also help relieve and possibly prevent PMS symptoms. You will get the greatest benefits if you exercise for at least 30 minutes, at least five days a week. But even taking a 20- to 30-minute walk three times a week can improve your mood. Chasteberry. The extract of the fruit of the chasteberry tree is shown to be a safe and effective treatment for PMS. This therapy is used primarily outside the United States. It may be obtained over the counter, but the dose and purity may be uncertain. In addition, there's some evidence that some nutritional supplements such as vitamin E, magnesium and vitamin B-6 may help ease symptoms of PMS. Discuss these and other strategies with your health care professional before taking any dietary supplement. There is no single treatment that works well for every woman who experiences PMS. Typically, it's wise to try the most conservative treatment options first, which include lifestyle changes such as modifying your diet and exercising more. Discuss your symptoms with your health care professional if strategies you've tried don't work, so he or she can recommend other treatment options. Prevention Can premenstrual syndrome (PMS) be prevented? Many women report benefits from a variety of lifestyle change including dietary changes, exercise and stress management. Dietary changes may include: Increasing calcium intake. Decreasing consumption of refined sugar. Decreasing or avoiding caffeine and nicotine, which act as stimulants and can increase tension and anxiety as well as interfere with sleep patterns. For some women, the severity of PMS symptoms increases as caffeine consumption increases. Decreasing alcohol consumption, which can act as a depressant. If you experience PMS, you may have an increased sensitivity to alcohol at certain points during your cycle. Decreasing salt intake and increasing water consumption to avoid water retention and bloating. Avoiding sodas, which may contain high levels of caffeine, salt, sugar and/or artificial sweeteners. Drinking natural diuretics, such as herbal teas. Ironically, some PMS symptoms, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume foods that aggravate the condition. Premenstrually, you may crave either refined sugar (usually combined with chocolate) or fat (combined with salt). Generally, foods high in refined sugars and fat temporarily raise energy levels. But within several hours or less, as your body metabolizes these foods, you may "crash," meaning you'll feel worse than before you ate them. Foods high in sugar content can also leave you feeling jittery. To alleviate mood swings and fatigue, try adding more high-quality, complex carbohydrates to your diet such as: Whole grain breads, pastas and cereals Potatoes (white or sweet) Rice (preferably brown or wild) Fresh vegetables, particularly corn and peas, such as chickpeas and lentils Fresh fruits These complex carbohydrates help keep blood sugar levels even while providing your body with a long-lasting source of energy. It's not uncommon for your appetite to increase just before your period begins. To combat the munchies and extra weight gain, try eating smaller, low-fat healthful meals using the food choices listed above. Make sure you include adequate calcium in your diet; calcium may help prevent irritability, anxiety and other PMS symptoms. Good sources of calcium include: Low-fat milk and milk products like yogurt, ice cream and cheese Broccoli Dark greens (like turnip greens) Green or red cabbage (raw) Cooked collards Salmon and sardines Soy products, such as tofu and soy milk Calcium-fortified orange and grapefruit juices Another good way to prevent PMS symptoms is through regular exercise in the form of aerobic activities such as brisk walking, jogging, biking or swimming. You will get the greatest benefits from exercise if you do it for at least 30 minutes, five or more days a week. But even taking a 20- to 30-minute walk three times a week can: Increase endorphin and serotonin production, brain chemicals that may help decrease pain and discomfort and improve mood, respectively Decrease stress and anxiety Increase REM sleep Other lifestyle changes that will help you control PMS include: Sleeping consistent hours Establishing a bedtime routine to help cue body and mind for sleeping Keeping a PMS symptom checklist, also called a menstrual cycle diary, to identify when symptoms and which symptoms occur so you can be prepared for them Facts to Know An estimated 75 percent of women of childbearing age suffer from PMS in some form. Approximately 3 to 8 percent of women experience premenstrual symptoms severe enough to disrupt their daily function and meet criteria for premenstrual dysphoric disorder (PMDD)––a severe form of PMS. Taking additional calcium in any form may help improve or even prevent PMS symptoms. Ideally, increase daily amounts of low-fat dairy products and other calcium-containing foods to reach the 1,200 mg of calcium daily health care professionals recommend. If you have trouble reaching this goal from your diet alone, consider using over-the counter calcium supplements. Symptoms of PMS may get worse with age. If you experience PMS, you may experience an increased sensitivity to alcohol at certain points in your menstrual cycle. Some evidence suggests that women who are vulnerable to depressive illness, panic disorder or other psychiatric or chronic medical disorders may be particularly susceptible to PMS. Strategies for PMS symptom relief include medication, dietary changes, exercise and stress management. Dietary changes to relieve PMS symptoms include increasing daily amounts of dietary or supplemental calcium, drinking more water and adding more complex carbohydrates (fruits, vegetables and grains) to your meals. Decreasing foods in your diet that contain refined sugar, limiting or avoiding caffeine and nicotine, decreasing alcohol consumption, decreasing salt intake and avoiding sodas may also help. Some of the PMS symptoms you may experience, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume high-fat foods and/or foods high in refined sugar, which actually aggravate these symptoms. Try to avoid them. Even women who have had hysterectomies can have symptoms of PMS if at least one functional ovary is left intact following the hysterectomy. Key Q&A What exactly is premenstrual syndrome (PMS)?There are more than 150 documented symptoms of PMS, but the number of symptoms seen in the vast majority of patients is much more limited. Some of the most common PMS symptoms include bloating, fatigue, sudden mood swings, irritability,anxiety, depression, weight gain, headaches, joint and muscle aches, food cravings and fluid retention. To be considered PMS symptoms, they must occur exclusively in the last 14 days of your menstrual cycle (usually about five to seven days before your period begins). True PMS symptoms tend to increase in severity as the cycle progresses, are relieved within a few days after the start of the menstrual flow and are present for at least two to three consecutive menstrual cycles. Cramps are not considered a symptom of PMS, but they can occur in women with PMS. What causes PMS?PMS appears to be caused by rising and falling levels of the hormones estrogen and progesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. How is PMS diagnosed?There is no single laboratory test for PMS, but one of the most common ways to diagnosis PMS is by keeping a daily checklist, chart or "menstrual cycle diary" that tracks when your premenstrual symptoms occurs for at least three months. Your health care professional should rule out other disorders or diseases that mimic or are identical to the symptoms caused by PMS before diagnosing you with the condition. These conditions include thyroid disorders, depression, endocrine abnormalities, menopause, heart problems, allergies and low blood sugar, among other conditions. Laboratory tests, personal and family medical histories and a physical exam are also part of the diagnostic process. Is PMS treatable?Yes! Many women experience some relief from PMS symptoms if they make diet and lifestyle changes, particularly increasing consumption of calcium, complex carbohydrates (fruits, vegetables, grains and beans) and water, and decreasing caffeine, alcohol, salt and refined sugar intake. Regular exercise and sleep may also help relieve symptoms. Certain medications can provide relief. When does PMS typically appear?PMS symptoms can appear any time between puberty and menopause, though the most common age for PMS to start to become a problem is during your late 20s to mid-30s. Will my PMS symptoms get better as I age?Probably not until you reach menopause. In some women, symptoms of PMS worsen with age and stress. Even women who have had hysterectomies can have PMS if at least one functional ovary is left intact following the hysterectomy. Once you reach menopause, your PMS symptoms will end with the end of menstruation. If I regularly take the recommended steps to relieve my PMS symptoms, how long before I may see results?It may take two to three months to experience relief from PMS symptoms. If you don't see any improvements by then, check with your health care professional for a new action plan. Are menstrual cramps a symptom of PMS?Cramps are not considered a symptom of PMS, although they may occur in women who have PMS. Called dysmenorrhea, cramps typically begin just before (24 to 48 hours) the onset of menstruation and disappear by the end of flow. Read the full article
0 notes
Text
Premenstrual Syndrome describes
Overview
Premenstrual syndrome (PMS) describes a wide range of severe, recurrent symptoms that occur from several days to two weeks before your period. PMS affects up to 75 percent of women in their childbearing years. The symptoms of PMS can appear any time between puberty and menopause, although the most common age for it to start to become a problem is during the late 20s to early 30s. Symptoms of PMS may get worse with age and stress, although the underlying causes are not well understood. Even women who have had hysterectomies can have PMS if at least one functional ovary is left. Women who are vulnerable to depressive illness, panic disorder, other psychiatric disorders orchronic medical conditions may also be susceptible to PMS, although these conditions may occur in women without PMS as well. Heredity may also play a role: if your mother or sister suffers from PMS, you may find you experience it, too. As many as 150 physical and behavioral symptoms have been assigned to PMS, but the number of PMS symptoms that most women experience is much more limited. The most common symptoms include irritability, bloating, mood swings, anxiety, depressed mood, fatigue, appetite changes, water retention and breast tenderness, among others. Menstrual cramps, or dysmenorrhea, are not considered a PMS symptom, although women with PMS may experience cramps. PMS appears to be caused by rising and falling levels of the hormones estrogen andprogesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. Calcium may play a role in PMS. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. Dietary changes and exercise may also help relieve the discomfort of PMS symptoms. When symptoms are severe, serotonergic antidepressant medication may be prescribed. It is thought that increased serotonin reduces PMS symptoms. One of the most important strategies for coping with premenstrual discomfort is to be aware of any pattern your symptoms follow. The more aware you are of your symptoms—when they start and stop and what works best to relieve them, for example—the better you can develop strategies to recognize and cope with them—whatever they may be. Premenstrual Dysphoric Disorder Approximately three to eight percent of women experience premenstrual dysphoric disorder (PMDD), a condition that, like PMS, is associated with the menstrual cycle. The symptoms of PMDD are the same as PMS symptoms, although women with PMDD may experience more dysphoric (depressive) symptoms and more severe symptoms. In fact, to be diagnosed with PMDD, symptoms must be severe enough to disrupt a woman's daily function. Symptoms must also meet diagnostic criteria specific to PMDD developed by the American Psychiatric Association. The most important criteria for a PMDD diagnosis are mood symptoms. Physical symptoms may also be present but aren't as critical to the diagnosis. The difference between PMDD and mild PMS is like the difference between a mild tension headache and a migraine, experts say. Women who have a history of depression are at higher risk for PMDD than other women. Treatment for PMDD includes serotonergic antidepressant medications and a particular brand of birth control pills, called Yaz. Yaz contains drospirenone (aprogestin) and ethinyl estradiol (a form of estrogen) and has been shown to be clinically effective at treating the emotional and physical symptoms of PMDD, but should only be used to treat PMDD if you choose to use it for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Another form of birth control pill containing drospirenone plus a daily dose of folic acid also is FDA-approved to treat PMDD. It is sold under the brand names Beyaz and Safyral. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. Diagnosis There is no specific laboratory test to determine if you suffer from PMS, and diagnosis can take some time because symptoms are so varied. But there are certain characteristics that health care professionals consider. To qualify as PMS, symptoms must follow this general pattern: They tend to increase in severity as your cycle progresses. They improve within a few days of your menstrual period starting. They are present for at least two to three consecutive menstrual cycles. More than 150 physical and behavioral symptoms may be associated with PMS. The most common are irritability and anxiety/tension. Other symptoms include: Sudden mood swings Depression Headaches Joint and muscle aches Food cravings Fluid retention Forgetfulness Clumsiness Sleep disturbances Breast swelling and tenderness The timing and severity of these symptoms are key to a PMS diagnosis. An average menstrual cycle spans 21 to 35 days. The follicular phase extends from menses to ovulation, and the luteal phase extends from ovulation to menses. PMS occurs during the luteal phase—approximately the last 14 days of your cycle, usually during the five to seven days before you get your period. A premenstrual symptom chart or checklist (also called a menstrual cycle diary) is the most common method used to evaluate menstrual cycle symptoms. With this tool, you and your health care professional can track the type and severity of your symptoms, as well as when they occur, to identify a pattern that may indicate PMS. Follow these simple steps to determine if your symptoms fit the PMS pattern: Track your symptoms using the first day of menstrual flow as Day 1. (Note: Don't be surprised if you do not have any symptoms to record before day 18 or so.) Have a person close to you (your partner, roommate, friend) chart his or her impression of your symptoms, when they occur and their severity. Chart your symptoms for at least three consecutive months to help you and your health care professional identify a pattern that may indicate PMS. Record the date when/if any of the following symptoms occur over three consecutive months and note their severity (1 = mild; 2 = moderate; 3 = severe) Physical Symptoms Abdominal bloating Breast tenderness Constipation Diarrhea Dizziness Fatigue Headache Swelling of hands/feet Emotional Symptoms Anger Anxiety Depressed mood Irritability Mood swings Tension Behavioral Symptoms Crying spells and tearfulness Decreased or increased appetite Difficulty concentrating Difficulty sleeping Forgetfulness Hostility In addition to suggesting that you keep a menstrual cycle diary, your health care professional likely will ask about your personal and family medical history and will give you a physical exam. Laboratory tests are not routine but may be obtained to rule out other conditions with similar symptoms, such as low blood sugar (hypoglycemia), mania, depression, thyroid disorders, anemia, endometriosis, allergies, fibroids, dysmenorrhea, lupus, endocrine abnormalities, neurological problems such as brain tumors and heart problems. Menopause and PMS share some of the same symptoms, so depending on your age and health history, your health care professional may want to make sure that you are indeed ovulating and therefore experiencing PMS, not menopausal symptoms. To do this, you will probably be asked to use an over-the-counter ovulation testing kit. This is a simple test that you can do at home. The results tell you when ovulation is likely. If you are approaching menopause (the average age is about 51 for U.S. women, but ranges from 42 to 60 years), blood hormone tests may also be used to confirm if you are menopausal. However, a single blood test is not informative because hormone levels change often. Treatment Many premenstrual syndrome (PMS) symptoms improve with treatment. Treatment options range from medication therapy to birth control pills to diet modification, including vitamin and mineral supplementation, herbal medicines and exercise. Antidepressant drugs called selective serotonin reuptake inhibitors (SSRIs) are typically recommended to women with severe mood-related symptoms such as anxiety, depression or mood swings. Overall, common treatment options include: Nonsteroidal anti-inflammatory drugs (NSAIDs). These medications are used to relieve premenstrual headache and other menstrual-cycle related pain. A variety of NSAIDs are available including over-the-counter ibuprofen products (Motrin) and others or naproxen sodium (Aleve). They usually cost less and have fewer side effects than other treatments. Prescription NSAIDs also are available.Note: NSAIDS carry some risks, such as an increased risk of serious cardiovascular (CV) events, including heart attack and stroke. As a result, the FDA has issued a "black box" warning highlighting this risk, as well as the risk of potentially life-threatening stomach bleeding. If you've recently had heart surgery, you shouldn't take NSAIDS. All other women considering NSAIDS to ease PMS or any other condition should discuss these potential risks with their health care professional. Contraceptive hormones. Some women with PMS or PMDD experience relief of their symptoms after they start taking birth control pills. (Other women, however, feel worse on birth control pills.) You can take the pill continuously to avoid having a menstrual period, thus preventing the hormonal changes that can lead to PMS/PMDD. The combination birth control pills Yaz (containing 3 mg of drospirenone, a progestin, and 20 mcg ethinyl estradiol, a form of estrogen) and Beyaz and Safyral (containing 3 mg of drospirenone, 20 mcg ethinyl estradiol and a daily dose of folic acid) are FDA approved for the treatment of PMDD. However, these contraceptives should only be used to treat PMDD if you choose to use them for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. GnRH agonists (gonadotropin-releasing hormone). These medications include leuprolide (Lupron), among others. They belong to a class of hormones used to temporarily shrink fibroids and relieve endometriosis. They also may be recommended to treat PMS because they "turn off" the menstrual cycle by blocking estrogen production. Side effects may include menopausal symptoms like hot flashes, vaginal dryness and bone loss. That's why low-dose hormone therapy, a combination of estrogen and progestin hormones, is typically prescribed along with GnRH agonists. Some women may experience a return of their PMS symptoms with the additional hormone therapy. GnRH agonists are usually considered only as a short-term treatment option (given for no longer than six months) because of the increased health risks such as osteoporosis associated with low estrogen levels. Antidepressant medications. Antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are the preferred antidepressants for treating severe PMS and PMDD symptoms, including depression. SSRIs include sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac). Other types of antidepressants may also be prescribed to treat PMS and PMDD, including venlafaxine (Effexor) and clomipramine (Anafranil). The U.S. Food and Drug Administration warns that women taking antidepressants should monitor their symptoms closely, with the help of their health care professional, for signs that their condition is getting worse or that they are becoming suicidal, especially when they first start therapy or when their dose is increased or decreased. Danazol. Danazol (Danocrine) is a medication that works similarly to GnRH agonists to prevent ovulation. Danocrine works to improve PMS symptoms in some women, but it has some unpleasant side effects, such as acne and facial hair growth, so it is usually only used in women who do not respond to other treatments. Anti-anxiety medications such as alprazolam (Xanax) are sometimes prescribed when anxiety is the main symptom associated with PMS or PMDD. These drugs can be taken during the 14 days between ovulation and menstruation (the luteal phase) when symptoms occur (rather than daily). Dependence and serious withdrawal reactions can occur with Xanax, so its dosage and discontinuation should be carefully monitored. Calcium supplements (1,200 mg daily). Additional calcium in any form may help relieve some PMS symptoms. Low-fat dairy products (milk, yogurt and cheese) are a primary source of calcium, but you can also gain calcium from the following: Tofu and other soy products Rice milk Broccoli Dark greens, like turnip greens Green or red cabbage (raw) Salmon and sardines Taking an over-the-counter calcium supplement can also help. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. But be patient; it may take two to three months to relieve PMS symptoms with calcium supplementation. If symptoms persist, have your vitamin D levels checked or change the type of calcium supplement you're using. Low levels of vitamin D can affect how the body absorbs calcium, and some generic supplements may not have enough calcium available for absorption. Exercise. Regular exercise can also help relieve and possibly prevent PMS symptoms. You will get the greatest benefits if you exercise for at least 30 minutes, at least five days a week. But even taking a 20- to 30-minute walk three times a week can improve your mood. Chasteberry. The extract of the fruit of the chasteberry tree is shown to be a safe and effective treatment for PMS. This therapy is used primarily outside the United States. It may be obtained over the counter, but the dose and purity may be uncertain. In addition, there's some evidence that some nutritional supplements such as vitamin E, magnesium and vitamin B-6 may help ease symptoms of PMS. Discuss these and other strategies with your health care professional before taking any dietary supplement. There is no single treatment that works well for every woman who experiences PMS. Typically, it's wise to try the most conservative treatment options first, which include lifestyle changes such as modifying your diet and exercising more. Discuss your symptoms with your health care professional if strategies you've tried don't work, so he or she can recommend other treatment options. Prevention Can premenstrual syndrome (PMS) be prevented? Many women report benefits from a variety of lifestyle change including dietary changes, exercise and stress management. Dietary changes may include: Increasing calcium intake. Decreasing consumption of refined sugar. Decreasing or avoiding caffeine and nicotine, which act as stimulants and can increase tension and anxiety as well as interfere with sleep patterns. For some women, the severity of PMS symptoms increases as caffeine consumption increases. Decreasing alcohol consumption, which can act as a depressant. If you experience PMS, you may have an increased sensitivity to alcohol at certain points during your cycle. Decreasing salt intake and increasing water consumption to avoid water retention and bloating. Avoiding sodas, which may contain high levels of caffeine, salt, sugar and/or artificial sweeteners. Drinking natural diuretics, such as herbal teas. Ironically, some PMS symptoms, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume foods that aggravate the condition. Premenstrually, you may crave either refined sugar (usually combined with chocolate) or fat (combined with salt). Generally, foods high in refined sugars and fat temporarily raise energy levels. But within several hours or less, as your body metabolizes these foods, you may "crash," meaning you'll feel worse than before you ate them. Foods high in sugar content can also leave you feeling jittery. To alleviate mood swings and fatigue, try adding more high-quality, complex carbohydrates to your diet such as: Whole grain breads, pastas and cereals Potatoes (white or sweet) Rice (preferably brown or wild) Fresh vegetables, particularly corn and peas, such as chickpeas and lentils Fresh fruits These complex carbohydrates help keep blood sugar levels even while providing your body with a long-lasting source of energy. It's not uncommon for your appetite to increase just before your period begins. To combat the munchies and extra weight gain, try eating smaller, low-fat healthful meals using the food choices listed above. Make sure you include adequate calcium in your diet; calcium may help prevent irritability, anxiety and other PMS symptoms. Good sources of calcium include: Low-fat milk and milk products like yogurt, ice cream and cheese Broccoli Dark greens (like turnip greens) Green or red cabbage (raw) Cooked collards Salmon and sardines Soy products, such as tofu and soy milk Calcium-fortified orange and grapefruit juices Another good way to prevent PMS symptoms is through regular exercise in the form of aerobic activities such as brisk walking, jogging, biking or swimming. You will get the greatest benefits from exercise if you do it for at least 30 minutes, five or more days a week. But even taking a 20- to 30-minute walk three times a week can: Increase endorphin and serotonin production, brain chemicals that may help decrease pain and discomfort and improve mood, respectively Decrease stress and anxiety Increase REM sleep Other lifestyle changes that will help you control PMS include: Sleeping consistent hours Establishing a bedtime routine to help cue body and mind for sleeping Keeping a PMS symptom checklist, also called a menstrual cycle diary, to identify when symptoms and which symptoms occur so you can be prepared for them Facts to Know An estimated 75 percent of women of childbearing age suffer from PMS in some form. Approximately 3 to 8 percent of women experience premenstrual symptoms severe enough to disrupt their daily function and meet criteria for premenstrual dysphoric disorder (PMDD)––a severe form of PMS. Taking additional calcium in any form may help improve or even prevent PMS symptoms. Ideally, increase daily amounts of low-fat dairy products and other calcium-containing foods to reach the 1,200 mg of calcium daily health care professionals recommend. If you have trouble reaching this goal from your diet alone, consider using over-the counter calcium supplements. Symptoms of PMS may get worse with age. If you experience PMS, you may experience an increased sensitivity to alcohol at certain points in your menstrual cycle. Some evidence suggests that women who are vulnerable to depressive illness, panic disorder or other psychiatric or chronic medical disorders may be particularly susceptible to PMS. Strategies for PMS symptom relief include medication, dietary changes, exercise and stress management. Dietary changes to relieve PMS symptoms include increasing daily amounts of dietary or supplemental calcium, drinking more water and adding more complex carbohydrates (fruits, vegetables and grains) to your meals. Decreasing foods in your diet that contain refined sugar, limiting or avoiding caffeine and nicotine, decreasing alcohol consumption, decreasing salt intake and avoiding sodas may also help. Some of the PMS symptoms you may experience, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume high-fat foods and/or foods high in refined sugar, which actually aggravate these symptoms. Try to avoid them. Even women who have had hysterectomies can have symptoms of PMS if at least one functional ovary is left intact following the hysterectomy. Key Q&A What exactly is premenstrual syndrome (PMS)?There are more than 150 documented symptoms of PMS, but the number of symptoms seen in the vast majority of patients is much more limited. Some of the most common PMS symptoms include bloating, fatigue, sudden mood swings, irritability,anxiety, depression, weight gain, headaches, joint and muscle aches, food cravings and fluid retention. To be considered PMS symptoms, they must occur exclusively in the last 14 days of your menstrual cycle (usually about five to seven days before your period begins). True PMS symptoms tend to increase in severity as the cycle progresses, are relieved within a few days after the start of the menstrual flow and are present for at least two to three consecutive menstrual cycles. Cramps are not considered a symptom of PMS, but they can occur in women with PMS. What causes PMS?PMS appears to be caused by rising and falling levels of the hormones estrogen and progesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. How is PMS diagnosed?There is no single laboratory test for PMS, but one of the most common ways to diagnosis PMS is by keeping a daily checklist, chart or "menstrual cycle diary" that tracks when your premenstrual symptoms occurs for at least three months. Your health care professional should rule out other disorders or diseases that mimic or are identical to the symptoms caused by PMS before diagnosing you with the condition. These conditions include thyroid disorders, depression, endocrine abnormalities, menopause, heart problems, allergies and low blood sugar, among other conditions. Laboratory tests, personal and family medical histories and a physical exam are also part of the diagnostic process. Is PMS treatable?Yes! Many women experience some relief from PMS symptoms if they make diet and lifestyle changes, particularly increasing consumption of calcium, complex carbohydrates (fruits, vegetables, grains and beans) and water, and decreasing caffeine, alcohol, salt and refined sugar intake. Regular exercise and sleep may also help relieve symptoms. Certain medications can provide relief. When does PMS typically appear?PMS symptoms can appear any time between puberty and menopause, though the most common age for PMS to start to become a problem is during your late 20s to mid-30s. Will my PMS symptoms get better as I age?Probably not until you reach menopause. In some women, symptoms of PMS worsen with age and stress. Even women who have had hysterectomies can have PMS if at least one functional ovary is left intact following the hysterectomy. Once you reach menopause, your PMS symptoms will end with the end of menstruation. If I regularly take the recommended steps to relieve my PMS symptoms, how long before I may see results?It may take two to three months to experience relief from PMS symptoms. If you don't see any improvements by then, check with your health care professional for a new action plan. Are menstrual cramps a symptom of PMS?Cramps are not considered a symptom of PMS, although they may occur in women who have PMS. Called dysmenorrhea, cramps typically begin just before (24 to 48 hours) the onset of menstruation and disappear by the end of flow. Read the full article
0 notes
Text
Premenstrual Syndrome describes
Overview
Premenstrual syndrome (PMS) describes a wide range of severe, recurrent symptoms that occur from several days to two weeks before your period. PMS affects up to 75 percent of women in their childbearing years. The symptoms of PMS can appear any time between puberty and menopause, although the most common age for it to start to become a problem is during the late 20s to early 30s. Symptoms of PMS may get worse with age and stress, although the underlying causes are not well understood. Even women who have had hysterectomies can have PMS if at least one functional ovary is left. Women who are vulnerable to depressive illness, panic disorder, other psychiatric disorders orchronic medical conditions may also be susceptible to PMS, although these conditions may occur in women without PMS as well. Heredity may also play a role: if your mother or sister suffers from PMS, you may find you experience it, too. As many as 150 physical and behavioral symptoms have been assigned to PMS, but the number of PMS symptoms that most women experience is much more limited. The most common symptoms include irritability, bloating, mood swings, anxiety, depressed mood, fatigue, appetite changes, water retention and breast tenderness, among others. Menstrual cramps, or dysmenorrhea, are not considered a PMS symptom, although women with PMS may experience cramps. PMS appears to be caused by rising and falling levels of the hormones estrogen andprogesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. Calcium may play a role in PMS. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. Dietary changes and exercise may also help relieve the discomfort of PMS symptoms. When symptoms are severe, serotonergic antidepressant medication may be prescribed. It is thought that increased serotonin reduces PMS symptoms. One of the most important strategies for coping with premenstrual discomfort is to be aware of any pattern your symptoms follow. The more aware you are of your symptoms—when they start and stop and what works best to relieve them, for example—the better you can develop strategies to recognize and cope with them—whatever they may be. Premenstrual Dysphoric Disorder Approximately three to eight percent of women experience premenstrual dysphoric disorder (PMDD), a condition that, like PMS, is associated with the menstrual cycle. The symptoms of PMDD are the same as PMS symptoms, although women with PMDD may experience more dysphoric (depressive) symptoms and more severe symptoms. In fact, to be diagnosed with PMDD, symptoms must be severe enough to disrupt a woman's daily function. Symptoms must also meet diagnostic criteria specific to PMDD developed by the American Psychiatric Association. The most important criteria for a PMDD diagnosis are mood symptoms. Physical symptoms may also be present but aren't as critical to the diagnosis. The difference between PMDD and mild PMS is like the difference between a mild tension headache and a migraine, experts say. Women who have a history of depression are at higher risk for PMDD than other women. Treatment for PMDD includes serotonergic antidepressant medications and a particular brand of birth control pills, called Yaz. Yaz contains drospirenone (aprogestin) and ethinyl estradiol (a form of estrogen) and has been shown to be clinically effective at treating the emotional and physical symptoms of PMDD, but should only be used to treat PMDD if you choose to use it for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Another form of birth control pill containing drospirenone plus a daily dose of folic acid also is FDA-approved to treat PMDD. It is sold under the brand names Beyaz and Safyral. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. Diagnosis There is no specific laboratory test to determine if you suffer from PMS, and diagnosis can take some time because symptoms are so varied. But there are certain characteristics that health care professionals consider. To qualify as PMS, symptoms must follow this general pattern: They tend to increase in severity as your cycle progresses. They improve within a few days of your menstrual period starting. They are present for at least two to three consecutive menstrual cycles. More than 150 physical and behavioral symptoms may be associated with PMS. The most common are irritability and anxiety/tension. Other symptoms include: Sudden mood swings Depression Headaches Joint and muscle aches Food cravings Fluid retention Forgetfulness Clumsiness Sleep disturbances Breast swelling and tenderness The timing and severity of these symptoms are key to a PMS diagnosis. An average menstrual cycle spans 21 to 35 days. The follicular phase extends from menses to ovulation, and the luteal phase extends from ovulation to menses. PMS occurs during the luteal phase—approximately the last 14 days of your cycle, usually during the five to seven days before you get your period. A premenstrual symptom chart or checklist (also called a menstrual cycle diary) is the most common method used to evaluate menstrual cycle symptoms. With this tool, you and your health care professional can track the type and severity of your symptoms, as well as when they occur, to identify a pattern that may indicate PMS. Follow these simple steps to determine if your symptoms fit the PMS pattern: Track your symptoms using the first day of menstrual flow as Day 1. (Note: Don't be surprised if you do not have any symptoms to record before day 18 or so.) Have a person close to you (your partner, roommate, friend) chart his or her impression of your symptoms, when they occur and their severity. Chart your symptoms for at least three consecutive months to help you and your health care professional identify a pattern that may indicate PMS. Record the date when/if any of the following symptoms occur over three consecutive months and note their severity (1 = mild; 2 = moderate; 3 = severe) Physical Symptoms Abdominal bloating Breast tenderness Constipation Diarrhea Dizziness Fatigue Headache Swelling of hands/feet Emotional Symptoms Anger Anxiety Depressed mood Irritability Mood swings Tension Behavioral Symptoms Crying spells and tearfulness Decreased or increased appetite Difficulty concentrating Difficulty sleeping Forgetfulness Hostility In addition to suggesting that you keep a menstrual cycle diary, your health care professional likely will ask about your personal and family medical history and will give you a physical exam. Laboratory tests are not routine but may be obtained to rule out other conditions with similar symptoms, such as low blood sugar (hypoglycemia), mania, depression, thyroid disorders, anemia, endometriosis, allergies, fibroids, dysmenorrhea, lupus, endocrine abnormalities, neurological problems such as brain tumors and heart problems. Menopause and PMS share some of the same symptoms, so depending on your age and health history, your health care professional may want to make sure that you are indeed ovulating and therefore experiencing PMS, not menopausal symptoms. To do this, you will probably be asked to use an over-the-counter ovulation testing kit. This is a simple test that you can do at home. The results tell you when ovulation is likely. If you are approaching menopause (the average age is about 51 for U.S. women, but ranges from 42 to 60 years), blood hormone tests may also be used to confirm if you are menopausal. However, a single blood test is not informative because hormone levels change often. Treatment Many premenstrual syndrome (PMS) symptoms improve with treatment. Treatment options range from medication therapy to birth control pills to diet modification, including vitamin and mineral supplementation, herbal medicines and exercise. Antidepressant drugs called selective serotonin reuptake inhibitors (SSRIs) are typically recommended to women with severe mood-related symptoms such as anxiety, depression or mood swings. Overall, common treatment options include: Nonsteroidal anti-inflammatory drugs (NSAIDs). These medications are used to relieve premenstrual headache and other menstrual-cycle related pain. A variety of NSAIDs are available including over-the-counter ibuprofen products (Motrin) and others or naproxen sodium (Aleve). They usually cost less and have fewer side effects than other treatments. Prescription NSAIDs also are available.Note: NSAIDS carry some risks, such as an increased risk of serious cardiovascular (CV) events, including heart attack and stroke. As a result, the FDA has issued a "black box" warning highlighting this risk, as well as the risk of potentially life-threatening stomach bleeding. If you've recently had heart surgery, you shouldn't take NSAIDS. All other women considering NSAIDS to ease PMS or any other condition should discuss these potential risks with their health care professional. Contraceptive hormones. Some women with PMS or PMDD experience relief of their symptoms after they start taking birth control pills. (Other women, however, feel worse on birth control pills.) You can take the pill continuously to avoid having a menstrual period, thus preventing the hormonal changes that can lead to PMS/PMDD. The combination birth control pills Yaz (containing 3 mg of drospirenone, a progestin, and 20 mcg ethinyl estradiol, a form of estrogen) and Beyaz and Safyral (containing 3 mg of drospirenone, 20 mcg ethinyl estradiol and a daily dose of folic acid) are FDA approved for the treatment of PMDD. However, these contraceptives should only be used to treat PMDD if you choose to use them for birth control because other forms of treatment don't carry the same risks as oral contraceptives. Birth control pills containing drospirenone may cause some serious side effects in rare cases, including blood clots in the legs and lungs, so be sure and talk to your health care provider about your risks and benefits. Oral contraceptives are not recommended for women who smoke because of increased cardiovascular risks. GnRH agonists (gonadotropin-releasing hormone). These medications include leuprolide (Lupron), among others. They belong to a class of hormones used to temporarily shrink fibroids and relieve endometriosis. They also may be recommended to treat PMS because they "turn off" the menstrual cycle by blocking estrogen production. Side effects may include menopausal symptoms like hot flashes, vaginal dryness and bone loss. That's why low-dose hormone therapy, a combination of estrogen and progestin hormones, is typically prescribed along with GnRH agonists. Some women may experience a return of their PMS symptoms with the additional hormone therapy. GnRH agonists are usually considered only as a short-term treatment option (given for no longer than six months) because of the increased health risks such as osteoporosis associated with low estrogen levels. Antidepressant medications. Antidepressant medications called selective serotonin reuptake inhibitors (SSRIs) are the preferred antidepressants for treating severe PMS and PMDD symptoms, including depression. SSRIs include sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), escitalopram (Lexapro), and fluoxetine (Prozac). Other types of antidepressants may also be prescribed to treat PMS and PMDD, including venlafaxine (Effexor) and clomipramine (Anafranil). The U.S. Food and Drug Administration warns that women taking antidepressants should monitor their symptoms closely, with the help of their health care professional, for signs that their condition is getting worse or that they are becoming suicidal, especially when they first start therapy or when their dose is increased or decreased. Danazol. Danazol (Danocrine) is a medication that works similarly to GnRH agonists to prevent ovulation. Danocrine works to improve PMS symptoms in some women, but it has some unpleasant side effects, such as acne and facial hair growth, so it is usually only used in women who do not respond to other treatments. Anti-anxiety medications such as alprazolam (Xanax) are sometimes prescribed when anxiety is the main symptom associated with PMS or PMDD. These drugs can be taken during the 14 days between ovulation and menstruation (the luteal phase) when symptoms occur (rather than daily). Dependence and serious withdrawal reactions can occur with Xanax, so its dosage and discontinuation should be carefully monitored. Calcium supplements (1,200 mg daily). Additional calcium in any form may help relieve some PMS symptoms. Low-fat dairy products (milk, yogurt and cheese) are a primary source of calcium, but you can also gain calcium from the following: Tofu and other soy products Rice milk Broccoli Dark greens, like turnip greens Green or red cabbage (raw) Salmon and sardines Taking an over-the-counter calcium supplement can also help. In one study, women who took 600 mg of calcium twice a day experienced fewer PMS symptoms than women who took a placebo. But be patient; it may take two to three months to relieve PMS symptoms with calcium supplementation. If symptoms persist, have your vitamin D levels checked or change the type of calcium supplement you're using. Low levels of vitamin D can affect how the body absorbs calcium, and some generic supplements may not have enough calcium available for absorption. Exercise. Regular exercise can also help relieve and possibly prevent PMS symptoms. You will get the greatest benefits if you exercise for at least 30 minutes, at least five days a week. But even taking a 20- to 30-minute walk three times a week can improve your mood. Chasteberry. The extract of the fruit of the chasteberry tree is shown to be a safe and effective treatment for PMS. This therapy is used primarily outside the United States. It may be obtained over the counter, but the dose and purity may be uncertain. In addition, there's some evidence that some nutritional supplements such as vitamin E, magnesium and vitamin B-6 may help ease symptoms of PMS. Discuss these and other strategies with your health care professional before taking any dietary supplement. There is no single treatment that works well for every woman who experiences PMS. Typically, it's wise to try the most conservative treatment options first, which include lifestyle changes such as modifying your diet and exercising more. Discuss your symptoms with your health care professional if strategies you've tried don't work, so he or she can recommend other treatment options. Prevention Can premenstrual syndrome (PMS) be prevented? Many women report benefits from a variety of lifestyle change including dietary changes, exercise and stress management. Dietary changes may include: Increasing calcium intake. Decreasing consumption of refined sugar. Decreasing or avoiding caffeine and nicotine, which act as stimulants and can increase tension and anxiety as well as interfere with sleep patterns. For some women, the severity of PMS symptoms increases as caffeine consumption increases. Decreasing alcohol consumption, which can act as a depressant. If you experience PMS, you may have an increased sensitivity to alcohol at certain points during your cycle. Decreasing salt intake and increasing water consumption to avoid water retention and bloating. Avoiding sodas, which may contain high levels of caffeine, salt, sugar and/or artificial sweeteners. Drinking natural diuretics, such as herbal teas. Ironically, some PMS symptoms, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume foods that aggravate the condition. Premenstrually, you may crave either refined sugar (usually combined with chocolate) or fat (combined with salt). Generally, foods high in refined sugars and fat temporarily raise energy levels. But within several hours or less, as your body metabolizes these foods, you may "crash," meaning you'll feel worse than before you ate them. Foods high in sugar content can also leave you feeling jittery. To alleviate mood swings and fatigue, try adding more high-quality, complex carbohydrates to your diet such as: Whole grain breads, pastas and cereals Potatoes (white or sweet) Rice (preferably brown or wild) Fresh vegetables, particularly corn and peas, such as chickpeas and lentils Fresh fruits These complex carbohydrates help keep blood sugar levels even while providing your body with a long-lasting source of energy. It's not uncommon for your appetite to increase just before your period begins. To combat the munchies and extra weight gain, try eating smaller, low-fat healthful meals using the food choices listed above. Make sure you include adequate calcium in your diet; calcium may help prevent irritability, anxiety and other PMS symptoms. Good sources of calcium include: Low-fat milk and milk products like yogurt, ice cream and cheese Broccoli Dark greens (like turnip greens) Green or red cabbage (raw) Cooked collards Salmon and sardines Soy products, such as tofu and soy milk Calcium-fortified orange and grapefruit juices Another good way to prevent PMS symptoms is through regular exercise in the form of aerobic activities such as brisk walking, jogging, biking or swimming. You will get the greatest benefits from exercise if you do it for at least 30 minutes, five or more days a week. But even taking a 20- to 30-minute walk three times a week can: Increase endorphin and serotonin production, brain chemicals that may help decrease pain and discomfort and improve mood, respectively Decrease stress and anxiety Increase REM sleep Other lifestyle changes that will help you control PMS include: Sleeping consistent hours Establishing a bedtime routine to help cue body and mind for sleeping Keeping a PMS symptom checklist, also called a menstrual cycle diary, to identify when symptoms and which symptoms occur so you can be prepared for them Facts to Know An estimated 75 percent of women of childbearing age suffer from PMS in some form. Approximately 3 to 8 percent of women experience premenstrual symptoms severe enough to disrupt their daily function and meet criteria for premenstrual dysphoric disorder (PMDD)––a severe form of PMS. Taking additional calcium in any form may help improve or even prevent PMS symptoms. Ideally, increase daily amounts of low-fat dairy products and other calcium-containing foods to reach the 1,200 mg of calcium daily health care professionals recommend. If you have trouble reaching this goal from your diet alone, consider using over-the counter calcium supplements. Symptoms of PMS may get worse with age. If you experience PMS, you may experience an increased sensitivity to alcohol at certain points in your menstrual cycle. Some evidence suggests that women who are vulnerable to depressive illness, panic disorder or other psychiatric or chronic medical disorders may be particularly susceptible to PMS. Strategies for PMS symptom relief include medication, dietary changes, exercise and stress management. Dietary changes to relieve PMS symptoms include increasing daily amounts of dietary or supplemental calcium, drinking more water and adding more complex carbohydrates (fruits, vegetables and grains) to your meals. Decreasing foods in your diet that contain refined sugar, limiting or avoiding caffeine and nicotine, decreasing alcohol consumption, decreasing salt intake and avoiding sodas may also help. Some of the PMS symptoms you may experience, such as mood swings, irritability, bloating, hunger, carbohydrate cravings and fatigue, may lead you to consume high-fat foods and/or foods high in refined sugar, which actually aggravate these symptoms. Try to avoid them. Even women who have had hysterectomies can have symptoms of PMS if at least one functional ovary is left intact following the hysterectomy. Key Q&A What exactly is premenstrual syndrome (PMS)?There are more than 150 documented symptoms of PMS, but the number of symptoms seen in the vast majority of patients is much more limited. Some of the most common PMS symptoms include bloating, fatigue, sudden mood swings, irritability,anxiety, depression, weight gain, headaches, joint and muscle aches, food cravings and fluid retention. To be considered PMS symptoms, they must occur exclusively in the last 14 days of your menstrual cycle (usually about five to seven days before your period begins). True PMS symptoms tend to increase in severity as the cycle progresses, are relieved within a few days after the start of the menstrual flow and are present for at least two to three consecutive menstrual cycles. Cramps are not considered a symptom of PMS, but they can occur in women with PMS. What causes PMS?PMS appears to be caused by rising and falling levels of the hormones estrogen and progesterone, which may influence brain chemicals, including serotonin, a substance that has a strong affect on mood. It's not clear why some women develop PMS or PMDD and others do not, but researchers suspect that some women are more sensitive than others to changes in hormone levels. How is PMS diagnosed?There is no single laboratory test for PMS, but one of the most common ways to diagnosis PMS is by keeping a daily checklist, chart or "menstrual cycle diary" that tracks when your premenstrual symptoms occurs for at least three months. Your health care professional should rule out other disorders or diseases that mimic or are identical to the symptoms caused by PMS before diagnosing you with the condition. These conditions include thyroid disorders, depression, endocrine abnormalities, menopause, heart problems, allergies and low blood sugar, among other conditions. Laboratory tests, personal and family medical histories and a physical exam are also part of the diagnostic process. Is PMS treatable?Yes! Many women experience some relief from PMS symptoms if they make diet and lifestyle changes, particularly increasing consumption of calcium, complex carbohydrates (fruits, vegetables, grains and beans) and water, and decreasing caffeine, alcohol, salt and refined sugar intake. Regular exercise and sleep may also help relieve symptoms. Certain medications can provide relief. When does PMS typically appear?PMS symptoms can appear any time between puberty and menopause, though the most common age for PMS to start to become a problem is during your late 20s to mid-30s. Will my PMS symptoms get better as I age?Probably not until you reach menopause. In some women, symptoms of PMS worsen with age and stress. Even women who have had hysterectomies can have PMS if at least one functional ovary is left intact following the hysterectomy. Once you reach menopause, your PMS symptoms will end with the end of menstruation. If I regularly take the recommended steps to relieve my PMS symptoms, how long before I may see results?It may take two to three months to experience relief from PMS symptoms. If you don't see any improvements by then, check with your health care professional for a new action plan. Are menstrual cramps a symptom of PMS?Cramps are not considered a symptom of PMS, although they may occur in women who have PMS. Called dysmenorrhea, cramps typically begin just before (24 to 48 hours) the onset of menstruation and disappear by the end of flow. Read the full article
0 notes