Don't wanna be here? Send us removal request.
Text
How Real-Time CGM Can Benefit Both Diabetes Patients and Health-Conscious Individuals
Continuous glucose monitoring (CGM) technology, once seen as a tool exclusively for diabetes management, is now recognized for its broader health applications. Real-time CGM provides continuous insights into glucose levels, offering valuable data that can benefit both individuals with diabetes and health-conscious individuals looking to optimize their well-being. This article delves into the multifaceted benefits of real-time CGM and how it can be a game-changer for a diverse range of users.
Understanding Real-Time CGM
Real-time CGM systems consist of a small sensor inserted under the skin, typically on the abdomen or upper arm. This sensor measures glucose levels in the interstitial fluid and transmits the data to a display device or smartphone app every few minutes. The real-time feedback allows users to monitor their glucose levels continuously, offering a dynamic picture of their glucose fluctuations throughout the day and night.
Benefits for Diabetes Patients
For individuals with diabetes, maintaining blood glucose levels within a target range is crucial to managing the condition and preventing complications. Real-time CGM provides several key benefits:
1. Improved Glycemic Control
Real-time CGM enables patients to track their glucose levels continuously, helping them maintain tighter glycemic control. By providing real-time feedback, CGM helps users adjust their insulin doses, diet, and activity levels more accurately, leading to better overall glucose management.
2. Early Detection of Hypoglycemia and Hyperglycemia
One of the most significant advantages of CGM is its ability to alert users to dangerously low (hypoglycemia) or high (hyperglycemia) glucose levels. These alerts allow for immediate intervention, which is crucial in preventing severe complications such as seizures, loss of consciousness, or diabetic ketoacidosis.
3. Reduced HbA1c Levels
Numerous studies have demonstrated that CGM use is associated with significant reductions in HbA1c levels, a marker of long-term glucose control. Lower HbA1c levels correlate with a reduced risk of diabetes-related complications, such as neuropathy, retinopathy, and cardiovascular disease.
4. Enhanced Quality of Life
Real-time CGM can significantly improve the quality of life for diabetes patients by reducing the frequency of finger-stick blood tests and offering greater peace of mind. The ability to monitor glucose levels continuously allows for more flexibility and confidence in managing daily activities, including exercise, travel, and social events.
Benefits for Health-Conscious Individuals
While the primary use of CGM has been for diabetes management, health-conscious individuals without diabetes can also reap significant benefits from real-time glucose monitoring:
1. Personalized Dietary Insights
Real-time CGM provides valuable feedback on how different foods and dietary habits impact glucose levels. Health-conscious individuals can use this data to tailor their diets, choosing foods that promote stable glucose levels and avoiding those that cause spikes. This can lead to better energy levels, improved mood, and enhanced overall health.
2. Optimized Exercise Routines
Exercise has a profound effect on glucose metabolism. Real-time CGM allows users to monitor how different types of physical activity affect their glucose levels. By understanding these patterns, individuals can optimize their exercise routines to enhance performance, manage weight more effectively, and improve metabolic health.
3. Weight Management
Monitoring glucose responses to various foods and activities can be a powerful tool for weight management. Stable glucose levels are associated with reduced hunger and fewer cravings, making it easier to adhere to a healthy diet and avoid overeating.
4. Stress and Sleep Management
Stress and sleep quality have significant impacts on glucose metabolism. Real-time CGM helps individuals identify patterns between their glucose levels and their stress or sleep patterns. By recognizing these relationships, users can implement strategies to manage stress and improve sleep, such as mindfulness practices, regular exercise, and proper sleep hygiene.
Practical Applications of Real-Time CGM
Integrating real-time CGM into daily life can be straightforward and highly beneficial for both diabetes patients and health-conscious individuals:
1. User-Friendly Devices
Modern CGM systems are designed to be user-friendly, with simple sensor insertion and intuitive interfaces. These devices often connect seamlessly with smartphones, providing real-time data and alerts through dedicated apps. This ease of use encourages consistent monitoring and data utilization.
2. Wearable Technology
Many CGM devices are discreet and can be worn comfortably on the body, even during physical activities. They are often water-resistant, allowing users to wear them during exercise and showers without interruption. This continuous monitoring capability is essential for maintaining a comprehensive view of glucose trends.
3. Data Interpretation and Sharing
CGM systems come with software that helps users interpret their glucose data. Features such as trend analysis, pattern recognition, and predictive alerts make it easier for users to understand their glucose levels and take appropriate actions. Additionally, data can be shared with healthcare providers, facilitating more informed consultations and personalized treatment plans.
The Future of CGM Technology
The future of CGM technology is bright, with ongoing advancements aimed at improving accuracy, convenience, and integration with other health monitoring systems:
1. Enhanced Accuracy
Researchers are continually working to improve sensor accuracy, reducing the margin of error and ensuring that CGM devices provide the most reliable data possible. Enhanced accuracy will make CGM an even more valuable tool for both diabetes management and general health monitoring.
2. Non-Invasive Options
Developments in non-invasive CGM technology are underway. These systems would eliminate the need for sensor insertion, making glucose monitoring more accessible and comfortable for a broader audience.
3. Integration with Other Health Metrics
Future CGM systems are likely to integrate with other health monitoring devices, such as fitness trackers and smartwatches. This integration will provide a holistic view of an individual's health, combining glucose data with other vital metrics like heart rate, activity levels, and sleep patterns.
4. Artificial Intelligence and Machine Learning
The incorporation of artificial intelligence (AI) and machine learning in CGM technology can enhance data analysis, offering personalized insights and predictive analytics. AI-driven algorithms can identify patterns and suggest proactive measures to maintain optimal glucose levels and overall health.
Conclusion
Real-time continuous glucose monitoring is a powerful tool that benefits both diabetes patients and health-conscious individuals. For those managing diabetes, CGM provides critical data that improves glycemic control, reduces the risk of complications, and enhances quality of life. For health-conscious individuals, CGM offers personalized insights into diet, exercise, stress, and sleep, promoting better overall health and well-being.
As CGM technology continues to evolve, its potential to enhance well-being and prevent chronic diseases will only grow. By integrating real-time CGM into daily life, individuals can take proactive steps toward optimizing their health, making it an indispensable part of modern health care. Whether managing a chronic condition or striving for peak health, real-time CGM offers a wealth of benefits that can lead to a healthier, more informed lifestyle.

0 notes
Text
The Emotional and Psychological Impact of Type 1 vs. Type 2 Diabetes
Diabetes, whether Type 1 or Type 2, profoundly impacts not only physical health but also emotional and psychological well-being. While both types share similarities in their management and complications, the emotional and psychological challenges faced by individuals with Type 1 and Type 2 diabetes can differ significantly due to differences in disease onset, management, and social perceptions. This article delves into these emotional and psychological impacts, highlighting how each type of diabetes uniquely affects mental health and quality of life.
Understanding the Basics
Type 1 Diabetes (T1D) is an autoimmune condition usually diagnosed in childhood or adolescence, though it can occur at any age. It involves the body’s immune system attacking insulin-producing beta cells in the pancreas, leading to little or no insulin production. Individuals with T1D require lifelong insulin therapy.
Type 2 Diabetes (T2D) is more common and typically develops in adulthood, though it is increasingly diagnosed in younger populations. It is characterized by insulin resistance and a gradual decline in insulin production. Management often includes lifestyle changes, oral medications, and sometimes insulin therapy.
The Emotional Impact of Type 1 Diabetes
Diagnosis and Adjustment
Being diagnosed with T1D often occurs at a young age, which can be a traumatic experience for both the child and their family. The sudden need for daily insulin injections, blood glucose monitoring, and dietary restrictions can be overwhelming. Children and adolescents may struggle with feelings of being different from their peers, which can lead to social isolation and emotional distress.
Daily Management Stress
The constant vigilance required to manage T1D can lead to significant stress. Fear of hypoglycemia (low blood sugar) is a constant concern, as severe episodes can be life-threatening. This fear can lead to anxiety and hypervigilance, impacting daily activities and quality of life. The necessity of planning meals, monitoring blood glucose, and administering insulin can be exhausting and contribute to burnout.
Social and Peer Relationships
Children and teenagers with T1D may feel self-conscious about their condition. They might face teasing or bullying from peers, leading to feelings of isolation and low self-esteem. Managing diabetes in social settings, such as school or parties, can also be challenging, making it difficult to participate in activities without worry.
Long-term Psychological Effects
The chronic nature of T1D means that individuals must manage their condition for life, which can lead to long-term psychological effects. Depression and anxiety are common among those with T1D. The constant stress of managing the disease, combined with the potential for serious complications, can contribute to these mental health issues. Additionally, the burden of diabetes management can lead to diabetes distress, a condition characterized by feeling overwhelmed and helpless about managing diabetes.
The Emotional Impact of Type 2 Diabetes
Diagnosis and Adjustment
A diagnosis of T2D typically occurs later in life, often after a period of declining health. Individuals may experience shock, denial, or even guilt, especially if lifestyle factors such as diet and exercise contributed to the development of the disease. Adjusting to the need for lifestyle changes and medication can be daunting, leading to frustration and a sense of loss of control.
Lifestyle Changes and Compliance
Managing T2D often requires significant lifestyle changes, including dietary modifications, increased physical activity, and weight management. These changes can be difficult to implement and maintain, leading to feelings of frustration and helplessness. Non-compliance with lifestyle changes and medication regimens is a common issue, often resulting from these emotional challenges.
Stigma and Social Perceptions
There is a significant amount of stigma associated with T2D, often linked to misconceptions about the disease being solely caused by poor lifestyle choices. This stigma can lead to feelings of shame and embarrassment, discouraging individuals from seeking support or discussing their condition openly. The social stigma can exacerbate feelings of isolation and negatively impact mental health.
Psychological Comorbidities
Depression and anxiety are prevalent among individuals with T2D, influenced by the stress of managing the disease and fear of complications. The association between T2D and obesity also contributes to body image issues and low self-esteem. Furthermore, the progressive nature of T2D can lead to feelings of hopelessness as individuals face the potential for increasing medication needs and complications over time.
Comparative Analysis
Disease Onset and Life Stage
The life stage at which diabetes is diagnosed plays a significant role in the emotional and psychological impact of the disease. T1D, often diagnosed in childhood, affects developmental years and can shape an individual's identity and self-esteem. T2D, typically diagnosed in adulthood, can disrupt established lifestyles and lead to feelings of regret or guilt.
Management Burden
The daily management of T1D is more intensive due to the need for continuous insulin therapy and frequent blood glucose monitoring. This can lead to higher levels of daily stress and anxiety compared to T2D, which may be managed initially with lifestyle changes and oral medications. However, T2D management can also become complex over time, especially if insulin therapy is required.
Social Impact and Stigma
Both types of diabetes carry social implications, but the nature of these implications differs. T1D is often perceived as an unavoidable autoimmune condition, which can garner sympathy and support. In contrast, T2D is frequently stigmatized due to its association with lifestyle factors, leading to shame and social isolation. This stigma can significantly affect the mental health of individuals with T2D.
Long-term Psychological Effects
The chronic nature of both T1D and T2D leads to long-term psychological effects, including depression, anxiety, and diabetes distress. However, the progressive nature of T2D, with its potential for worsening over time, can contribute to feelings of hopelessness. T1D individuals, facing a lifetime of intensive management, may experience burnout and fatigue more acutely.
Coping Strategies and Support
Education and Awareness
Improving education and awareness about both types of diabetes can help reduce stigma and promote understanding. Educating the public about the differences between T1D and T2D and the challenges faced by individuals with each type can foster empathy and support.
Psychological Support
Access to psychological support, including counseling and support groups, is crucial for individuals with both T1D and T2D. Mental health professionals can help individuals develop coping strategies, manage stress, and address feelings of depression and anxiety.
Peer Support
Peer support groups can provide a sense of community and understanding for individuals with diabetes. Sharing experiences and challenges with others who understand can reduce feelings of isolation and improve emotional well-being.
Comprehensive Care
Integrating mental health care into diabetes management is essential. Healthcare providers should routinely screen for depression, anxiety, and diabetes distress and provide resources and referrals to mental health professionals as needed.
Conclusion
The emotional and psychological impacts of Type 1 and Type 2 diabetes are profound and multifaceted. While both conditions involve significant mental health challenges, the nature and intensity of these challenges can differ due to differences in disease onset, management requirements, and social perceptions. By recognizing and addressing these emotional and psychological aspects, healthcare providers can offer more holistic care, improving the overall well-being and quality of life for individuals with diabetes.

0 notes
Text
How to Handle Sick Days: Managing Diabetes When You’re Unwell
Introduction
Managing diabetes requires consistent attention to diet, exercise, and medication. However, when you're unwell, maintaining this balance can become more challenging. Illness can cause fluctuations in blood sugar levels, potentially leading to dangerous complications. This article provides a comprehensive guide on how to handle sick days effectively while managing diabetes, ensuring you stay safe and in control of your health.
Understanding the Impact of Illness on Blood Sugar
When you're sick, your body releases stress hormones, which can cause blood sugar levels to rise. Common illnesses like the flu, colds, or infections can affect your appetite and hydration levels, further complicating diabetes management. Additionally, the medications used to treat these illnesses, such as decongestants and cough syrups, can also impact blood sugar levels.
Preparing for Sick Days
Preparation is key to managing diabetes during illness. Here are some steps to take before you get sick:
1. Create a Sick Day Plan
Work with your healthcare provider to develop a personalized sick day plan. This plan should include guidelines for monitoring blood sugar levels, adjusting medications, and knowing when to seek medical help.
2. Stock Up on Supplies
Ensure you have an adequate supply of diabetes medications, testing strips, and ketone strips. Also, keep a stock of easy-to-digest foods and drinks that can help you maintain your nutrition and hydration.
3. Know Your Medications
Be aware of how over-the-counter medications for colds, flu, and other common illnesses can affect your blood sugar. Choose sugar-free options when possible, and consult your healthcare provider before taking any new medications.
Managing Blood Sugar Levels When Sick
1. Monitor Blood Sugar Frequently
Check your blood sugar levels more often than usual, typically every 2-4 hours. Illness can cause unexpected fluctuations, and frequent monitoring helps you respond promptly to changes.
2. Test for Ketones
High blood sugar levels can lead to the production of ketones, especially in people with type 1 diabetes. Use ketone strips to test your urine for ketones every 4-6 hours. High ketone levels can indicate diabetic ketoacidosis (DKA), a serious condition that requires immediate medical attention.
3. Adjust Medication as Needed
Your insulin needs may increase during illness. Follow your healthcare provider's instructions on adjusting your insulin dosage. Never skip insulin, even if you're unable to eat normally, as this can lead to dangerously high blood sugar levels.
Maintaining Nutrition and Hydration
1. Stay Hydrated
Dehydration can be a serious risk during illness, particularly if you're vomiting or have diarrhea. Drink plenty of fluids such as water, broth, or electrolyte solutions. Avoid sugary drinks that can spike blood sugar levels.
2. Eat Carbohydrates
If you're able to eat, try to consume carbohydrates to maintain your energy levels. If solid foods are hard to tolerate, opt for carbohydrate-containing liquids like juice, gelatin, or popsicles.
3. Follow a Soft Diet if Needed
If solid foods are difficult to eat, try bland, easy-to-digest foods such as:
Applesauce
Crackers
Rice
Toast
Soup
These can help you get the necessary nutrients without upsetting your stomach.
Recognizing When to Seek Medical Help
It's crucial to know when your symptoms require professional medical attention. Contact your healthcare provider if you experience any of the following:
Blood sugar levels consistently above 240 mg/dL or below 70 mg/dL
Moderate to large ketones in your urine
Persistent vomiting or diarrhea
Signs of dehydration (dry mouth, dark urine, dizziness)
Difficulty breathing
Chest pain
Confusion or disorientation
Coping with Specific Illnesses
Different illnesses can present unique challenges for people with diabetes. Here are some tips for managing common ailments:
1. Colds and Flu
Stay Hydrated: Drink plenty of fluids, even if you don't feel thirsty.
Rest: Allow your body to recover by getting plenty of rest.
Monitor Symptoms: Keep an eye on your blood sugar and ketone levels frequently.
2. Stomach Bugs
Replace Fluids: Use oral rehydration solutions to replace lost fluids and electrolytes.
Gradually Reintroduce Food: Start with small amounts of bland foods and gradually increase as tolerated.
Monitor for Dehydration: Watch for signs of dehydration and seek medical help if necessary.
3. Infections
Antibiotics: Follow your doctor's instructions for taking antibiotics, if prescribed.
Wound Care: If you have an infection related to a wound, keep the area clean and follow proper wound care procedures.
Monitor Blood Sugar: Infections can cause significant changes in blood sugar levels, so monitor frequently.
Managing Stress and Emotional Well-being
Being sick can be stressful, and stress can further affect blood sugar levels. Here are some strategies to manage stress and support your emotional well-being during illness:
1. Practice Relaxation Techniques
Engage in relaxation techniques such as deep breathing exercises, meditation, or gentle stretching to help reduce stress.
2. Stay Connected
Reach out to friends and family for support. Talking to loved ones can help alleviate feelings of isolation and stress.
3. Seek Professional Support
If you're feeling overwhelmed, consider speaking to a mental health professional who can provide coping strategies and support.
Conclusion
Managing diabetes during illness requires careful planning, frequent monitoring, and proactive management of blood sugar levels and hydration. By preparing in advance and knowing how to adjust your diabetes care plan when you're unwell, you can reduce the risk of complications and support your recovery. Always consult with your healthcare provider for personalized advice and guidelines tailored to your specific needs. Remember, taking care of your health during sick days is crucial for maintaining overall diabetes management and ensuring your well-being.

0 notes
Text
Diabetes and Dehydration: Warning Signs and Prevention Tips
Dehydration is a common concern for everyone, but for individuals with diabetes, it can pose serious health risks. Maintaining proper hydration is crucial for managing blood sugar levels and overall health. This comprehensive guide explores the warning signs of dehydration, its impact on diabetes, and practical tips for prevention.
Understanding Dehydration and Its Impact on Diabetes
Dehydration occurs when your body loses more fluids than it takes in, leading to an insufficient amount of water to carry out normal functions. For people with diabetes, dehydration can be particularly dangerous because it can elevate blood glucose levels, complicate diabetes management, and increase the risk of diabetic ketoacidosis (DKA) in those with type 1 diabetes.
Blood Sugar Levels: When dehydrated, the concentration of glucose in the bloodstream increases. This can lead to higher blood sugar levels and potentially hyperglycemia, making it more challenging to manage diabetes effectively.
Diabetic Ketoacidosis (DKA): DKA is a serious condition that occurs when the body starts breaking down fats at an accelerated rate, leading to a build-up of ketones in the blood. Dehydration can accelerate this process, particularly in individuals with type 1 diabetes, and can become life-threatening if not treated promptly.
Kidney Function: Proper hydration is essential for kidney function. Dehydration can strain the kidneys, which are already at risk of complications from diabetes, increasing the likelihood of kidney damage or failure.
Warning Signs of Dehydration
Recognizing the early signs of dehydration is key to preventing severe complications. Common symptoms include:
Increased Thirst: One of the earliest and most obvious signs of dehydration is a persistent feeling of thirst. For diabetics, this can also indicate high blood sugar levels.
Dry Mouth and Skin: A dry mouth, chapped lips, and dry skin are common indicators of dehydration.
Dark Urine: Dark yellow or amber-colored urine typically suggests that you need to drink more fluids.
Fatigue and Weakness: Dehydration can lead to a general sense of tiredness, weakness, and reduced energy levels.
Dizziness or Lightheadedness: Feeling dizzy or lightheaded, especially when standing up quickly, can be a sign of dehydration.
Decreased Urine Output: Urinating less frequently or in smaller amounts can indicate dehydration.
Headaches: Dehydration often leads to headaches or migraines due to reduced fluid levels affecting brain function.
Muscle Cramps: Lack of fluids can cause muscle cramps, particularly during exercise or physical activity.
Prevention Tips for Dehydration
To avoid dehydration, especially during hot weather or periods of increased physical activity, consider the following tips:
Drink Plenty of Water: Aim to drink at least 8-10 glasses of water a day. Carry a water bottle with you and take small sips throughout the day to maintain steady hydration.
Monitor Fluid Intake: Keep track of your fluid intake to ensure you’re drinking enough. Apps and hydration trackers can help you stay on top of your water consumption.
Eat Hydrating Foods: Incorporate fruits and vegetables with high water content into your diet. Cucumbers, watermelon, strawberries, and oranges are excellent choices.
Avoid Diuretics: Limit beverages that can dehydrate you, such as alcohol, caffeine, and sugary drinks. These can increase urine output and exacerbate dehydration.
Stay Cool: In hot weather, seek shade, wear lightweight clothing, and use fans or air conditioning to keep cool. Avoid direct sunlight and peak heat hours.
Adjust Exercise Routines: Exercise during cooler parts of the day, such as early morning or late evening. Drink water before, during, and after physical activity to replenish lost fluids.
Use Hydration Aids: Sports drinks containing electrolytes can help replenish fluids lost through sweat, but choose low-sugar options to avoid blood sugar spikes.
Recognize Personal Risk Factors: Be aware of your personal risk factors for dehydration, such as age, medication, and overall health status. Older adults and those on certain medications may need to take extra precautions.
Managing Dehydration for Diabetics
If you suspect you’re becoming dehydrated, it’s important to take immediate action:
Rehydrate Gradually: Start by drinking small amounts of water frequently. Avoid drinking large quantities of water at once, which can overwhelm your body.
Electrolyte Solutions: Consider drinking an oral rehydration solution or electrolyte-enhanced water to quickly restore fluid balance.
Monitor Blood Sugar Levels: Check your blood sugar levels more frequently if you suspect dehydration. High blood sugar can be both a cause and a consequence of dehydration, so it’s crucial to keep it under control.
Adjust Insulin Dosage: Consult your healthcare provider about adjusting your insulin dosage if necessary. Dehydration can affect how your body absorbs insulin.
Seek Medical Attention: If you experience severe symptoms of dehydration, such as confusion, rapid heartbeat, fainting, or signs of DKA (like fruity-smelling breath, shortness of breath, or nausea), seek medical attention immediately.
Long-Term Strategies for Hydration
Adopting long-term strategies can help maintain proper hydration and prevent dehydration-related complications:
Develop a Hydration Routine: Make drinking water a regular part of your daily routine. Set reminders or create habits, such as drinking a glass of water with every meal.
Educate Yourself: Learn about the signs of dehydration and how it affects diabetes management. Educating yourself empowers you to take proactive steps to prevent it.
Regular Health Check-Ups: Regular visits to your healthcare provider can help monitor your overall health and address any issues related to hydration and diabetes management.
Community Support: Join diabetes support groups or online communities to share tips and experiences related to managing hydration and diabetes.
Conclusion
Dehydration poses significant risks for individuals with diabetes, but with awareness and proactive management, these risks can be mitigated. By recognizing the warning signs of dehydration and adopting effective prevention strategies, you can maintain better control over your blood sugar levels and overall health. Remember, staying hydrated is not just about drinking water; it’s about creating a balanced approach to fluid intake and managing diabetes effectively. Always consult your healthcare provider for personalized advice tailored to your specific needs.

0 notes
Text
How to Use Technology to Track and Improve Your Cognitive Health
Introduction
In the digital age, technology has become an indispensable part of our lives, revolutionizing the way we manage our health. For individuals looking to enhance and maintain their cognitive health, technological tools offer practical and innovative solutions. Whether you're aiming to track your mental acuity, manage stress, or improve your memory and focus, there are various apps, devices, and online platforms designed to support these goals. This article explores how you can effectively use technology to track and improve your cognitive health.
Understanding Cognitive Health
Cognitive health refers to the ability to think clearly, learn, and remember. It encompasses a range of mental functions including memory, attention, language skills, and problem-solving abilities. Maintaining cognitive health is crucial for overall well-being, particularly as we age. Factors such as stress, poor nutrition, lack of sleep, and certain medical conditions (like diabetes) can negatively impact cognitive function. By leveraging technology, you can monitor these factors and implement strategies to enhance your cognitive health.
Tracking Cognitive Health with Technology
1. Cognitive Health Apps
There are numerous apps specifically designed to monitor and improve cognitive function. These apps offer various features such as brain training exercises, memory games, and cognitive assessments.
Popular Apps:
Lumosity: This app provides a series of brain games designed to enhance memory, attention, flexibility, speed of processing, and problem-solving skills. It offers personalized training programs based on your performance.
CogniFit: Offering scientifically validated cognitive assessments and training programs, CogniFit helps users track their cognitive skills and provides exercises tailored to their needs.
Peak: Peak features over 40 games aimed at boosting mental agility, focusing on skills such as memory, attention, and problem-solving.
2. Wearable Devices
Wearable technology, such as smartwatches and fitness trackers, can also contribute to cognitive health. These devices monitor physical activity, sleep patterns, and heart rate, all of which are important for maintaining cognitive function.
Key Wearables:
Fitbit: Tracks physical activity, sleep, and heart rate. It also offers mindfulness and relaxation exercises to manage stress.
Apple Watch: Besides fitness tracking, the Apple Watch includes features like the Breathe app for mindfulness and the Sleep app for monitoring sleep quality.
3. Smart Home Devices
Smart home devices can help create an environment conducive to cognitive health. These devices can remind you to take breaks, practice mindfulness, or maintain a regular sleep schedule.
Examples:
Amazon Echo & Google Home: These smart speakers can set reminders for medication, prompt you to take mental breaks, or play guided meditation sessions.
Smart Lighting: Systems like Philips Hue can be programmed to dim lights at night to promote better sleep hygiene, which is crucial for cognitive health.
Improving Cognitive Health with Technology
1. Brain Training Programs
Engaging in regular brain training exercises can help maintain and improve cognitive functions. Apps and online platforms offer a variety of exercises to challenge different aspects of your cognition.
How to Get Started:
Choose an app or platform that offers a comprehensive set of exercises.
Dedicate 15-20 minutes daily to brain training.
Track your progress and adjust the difficulty level as needed.
2. Mindfulness and Meditation Apps
Stress is a major factor that can impair cognitive function. Mindfulness and meditation apps can help manage stress, improve focus, and enhance overall mental well-being.
Popular Apps:
Headspace: Offers guided meditation sessions, mindfulness exercises, and sleep aids to reduce stress and improve focus.
Calm: Provides meditation sessions, breathing exercises, and sleep stories designed to enhance relaxation and mental clarity.
3. Sleep Tracking
Quality sleep is essential for cognitive health. Poor sleep can lead to memory problems, reduced attention, and slower processing speeds. Sleep tracking apps and devices can help monitor your sleep patterns and provide insights into how to improve sleep quality.
Effective Tools:
Sleep Cycle: This app tracks your sleep cycles and wakes you up during the lightest phase of sleep, helping you feel more refreshed.
Oura Ring: A wearable that provides detailed insights into your sleep patterns, readiness, and overall health.
4. Diet and Nutrition Apps
Nutrition plays a significant role in brain health. Certain nutrients, such as omega-3 fatty acids, antioxidants, and vitamins, are crucial for cognitive function. Nutrition tracking apps can help ensure you’re getting the right nutrients.
Helpful Apps:
MyFitnessPal: Tracks your diet and nutrition, providing detailed information about your intake of essential nutrients.
Lifesum: Offers personalized diet plans and tracks your food intake to help you maintain a balanced diet.
Integrating Technology into Your Daily Routine
1. Set Realistic Goals
Start by setting achievable goals for your cognitive health. Whether it’s improving memory, increasing focus, or managing stress, having clear objectives will help you choose the right tools and measure progress effectively.
2. Create a Routine
Incorporate the use of cognitive health tools into your daily routine. For example, you could do a brain training exercise in the morning, practice mindfulness during lunch, and review your sleep data each night.
3. Monitor Progress
Regularly check your progress using the tracking features of the apps and devices. Adjust your activities based on the insights you gain to continually improve your cognitive health.
4. Stay Consistent
Consistency is key to seeing improvements. Make sure to use the apps and devices regularly, and be patient as cognitive health improvements can take time.
Conclusion
Technology offers a plethora of tools to help track and improve cognitive health. From brain training apps and wearable devices to mindfulness platforms and sleep trackers, there are numerous ways to support your cognitive function. By integrating these technologies into your daily routine, setting realistic goals, and consistently monitoring your progress, you can effectively enhance your cognitive health and overall well-being. Embrace the digital tools available and take proactive steps towards a sharper, healthier mind.

0 notes
Text
Hope in Research: Promising Breakthroughs in Diabetes Prevention and Cure
Introduction: Diabetes, a chronic condition characterized by high blood sugar levels, affects millions of people worldwide. While current treatments focus on managing symptoms and preventing complications, ongoing research holds promise for advancements in diabetes prevention and potential cures. In this article, we'll explore some of the most exciting breakthroughs in diabetes research, offering hope for a future where this pervasive disease is more effectively prevented and treated.
1. Genetic Discoveries:
Recent advancements in genetic research have uncovered key insights into the underlying causes of diabetes. Scientists have identified numerous genetic variants associated with an increased risk of developing type 1 and type 2 diabetes. This knowledge has paved the way for personalized medicine approaches, allowing healthcare providers to tailor treatments based on an individual's genetic profile. Additionally, gene editing technologies such as CRISPR hold promise for correcting genetic mutations associated with diabetes, offering potential cures for certain forms of the disease.
2. Beta Cell Regeneration:
One of the hallmarks of diabetes is the destruction or dysfunction of insulin-producing beta cells in the pancreas. However, researchers are exploring innovative approaches to regenerate or replace these cells. Stem cell therapy, for example, holds promise for generating new beta cells that can restore insulin production in individuals with diabetes. Furthermore, scientists are investigating ways to protect existing beta cells from immune attack or stimulate their regeneration through targeted therapies.
3. Immunotherapy:
Type 1 diabetes is an autoimmune condition in which the immune system mistakenly attacks and destroys insulin-producing beta cells. Immunotherapy approaches aim to modulate the immune system to prevent this destructive process. Recent studies have shown promising results with immunomodulatory drugs and therapies that target specific immune cells involved in the pathogenesis of type 1 diabetes. These approaches not only help preserve remaining beta cell function but also hold potential for preventing the onset of the disease in at-risk individuals.
4. Artificial Pancreas Systems:
Advancements in technology have led to the development of artificial pancreas systems, also known as closed-loop systems, which automate insulin delivery based on real-time glucose monitoring. These devices combine continuous glucose monitoring (CGM) with insulin pumps, algorithms, and smart controllers to mimic the function of the pancreas more closely. Clinical trials have demonstrated the effectiveness and safety of artificial pancreas systems in improving glucose control and reducing the risk of hypoglycemia in individuals with type 1 diabetes. Continued research aims to further refine these systems and expand their use to individuals with type 2 diabetes.
5. Metabolic Surgery:
Metabolic surgery, such as gastric bypass or sleeve gastrectomy, has emerged as a promising treatment option for individuals with type 2 diabetes, particularly those who are obese or have difficulty managing their blood sugar levels with conventional therapies. These procedures not only promote weight loss but also have profound effects on metabolism, insulin sensitivity, and glucose homeostasis. Research suggests that metabolic surgery can lead to long-term remission of type 2 diabetes in a significant proportion of patients, offering a potential cure for this metabolic disorder.
6. Lifestyle Interventions:
While medications and surgical procedures play a crucial role in diabetes management, lifestyle interventions remain the cornerstone of prevention and treatment. Studies have consistently shown that healthy eating habits, regular physical activity, weight management, and stress reduction can help prevent or delay the onset of type 2 diabetes and improve outcomes for individuals with the condition. Ongoing research aims to identify the most effective lifestyle interventions and strategies for promoting long-term behavior change.
Conclusion:
In conclusion, the field of diabetes research is brimming with hope and optimism, fueled by groundbreaking discoveries and innovative technologies. From genetic insights to immunotherapy, artificial pancreas systems to metabolic surgery, researchers are exploring a diverse array of approaches to prevent and cure diabetes. While challenges remain, including funding limitations, regulatory hurdles, and the complex nature of the disease, the progress made to date offers promise for a future where diabetes is more effectively prevented, managed, and ultimately cured. By continuing to invest in research, support innovation, and prioritize public health efforts, we can work towards a world where diabetes no longer poses a significant threat to global health and well-being.

0 notes
Text
Wellness Over Diabetes: A Holistic Approach to Management
Introduction: Diabetes is a complex condition that requires a multifaceted approach to management. While medications and blood sugar monitoring are essential components of diabetes care, taking a holistic approach that addresses the physical, emotional, and lifestyle factors can lead to better outcomes and improved overall wellness. In this guide, we'll explore the principles of holistic diabetes management and provide practical tips for incorporating holistic practices into your diabetes care routine.
Understanding Holistic Diabetes Management: Holistic diabetes management takes into account the whole person, recognizing that physical health, emotional well-being, and lifestyle factors all play a role in managing the condition. Rather than focusing solely on controlling blood sugar levels, holistic management aims to optimize overall health and quality of life.
Nutrition and Diet: A key aspect of holistic diabetes management is adopting a balanced and nutritious diet. Focus on whole, unprocessed foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats. Aim to include a variety of nutrients in your meals to support overall health and well-being. Consider working with a registered dietitian who can help you create a personalized meal plan that meets your nutritional needs and supports your diabetes management goals.
Physical Activity: Regular exercise is essential for managing diabetes and promoting overall wellness. Engage in a variety of physical activities that you enjoy, such as walking, swimming, cycling, or yoga. Aim for at least 150 minutes of moderate-intensity exercise per week, spread out over several days. Incorporating strength training exercises can also help improve insulin sensitivity and promote better blood sugar control.
Stress Management: Chronic stress can have a negative impact on blood sugar levels and overall health. Incorporating stress management techniques into your daily routine can help reduce stress levels and improve diabetes management. Practices such as deep breathing, meditation, mindfulness, and progressive muscle relaxation can help promote relaxation and emotional well-being. Additionally, finding activities that you enjoy and spending time with loved ones can help reduce stress and improve overall quality of life.
Sleep Hygiene: Quality sleep is essential for overall health and well-being, especially for individuals with diabetes. Aim for 7-9 hours of uninterrupted sleep per night and establish a consistent sleep schedule. Create a relaxing bedtime routine to signal to your body that it's time to wind down, and avoid stimulants such as caffeine and electronics before bed. If you're having trouble sleeping, talk to your healthcare provider for guidance and support.
Mind-Body Practices: Incorporating mind-body practices such as yoga, tai chi, qigong, and meditation can help promote physical, emotional, and spiritual well-being. These practices can help reduce stress, improve sleep, increase mindfulness, and enhance overall quality of life. Consider exploring different mind-body practices to find the ones that resonate with you and incorporate them into your daily routine.
Social Support: Building a strong support network can be invaluable for managing diabetes and promoting overall wellness. Surround yourself with supportive friends, family members, healthcare providers, and fellow individuals with diabetes who can offer encouragement, guidance, and understanding. Participating in support groups or online communities can also provide a sense of connection and belonging.
Holistic Healthcare Team: In addition to your primary care physician or endocrinologist, consider building a holistic healthcare team that includes other healthcare providers such as a registered dietitian, certified diabetes educator, mental health counselor, and alternative medicine practitioner. Working with a multidisciplinary team can provide you with comprehensive care that addresses all aspects of your health and well-being.
Conclusion: Taking a holistic approach to diabetes management can lead to better outcomes and improved overall wellness. By addressing the physical, emotional, and lifestyle factors that influence diabetes, you can optimize your health and quality of life. Incorporate principles such as nutrition and diet, physical activity, stress management, sleep hygiene, mind-body practices, social support, and holistic healthcare into your diabetes care routine to achieve wellness over diabetes. Remember that managing diabetes is a journey, and it's essential to find the approaches that work best for you and support your individual needs and goals.

0 notes
Text
Guardian Angels: How Blucon Nightrider CGM Supports Parents of Diabetic Children
Introduction: Parenting a child with diabetes comes with its unique set of challenges and responsibilities. From managing blood glucose levels to administering insulin and navigating dietary considerations, every day presents new hurdles for caregivers. Amidst these challenges, technology has emerged as a beacon of hope, offering innovative solutions to ease the burden of diabetes management. One such solution is the Blucon Nightrider Continuous Glucose Monitoring (CGM) system—a guardian angel for parents of diabetic children. In this article, we'll explore how Blucon Nightrider CGM provides unwavering support and peace of mind to caregivers, empowering them to navigate the complexities of pediatric diabetes with confidence and grace.
Understanding the Journey of Caregiving: The journey of caregiving for a child with diabetes is a deeply personal and often overwhelming experience. From the moment of diagnosis, parents are thrust into a world of constant vigilance and decision-making. Every meal, every activity, and every moment becomes an opportunity to manage their child's condition and safeguard their health. However, amidst the daily challenges, there is also profound love, resilience, and unwavering determination to provide the best possible care for their child.
The Role of Blucon Nightrider CGM: Blucon Nightrider CGM serves as a silent yet powerful ally in the journey of caregiving for parents of diabetic children. This innovative system consists of a small sensor that is attached to the skin, continuously measuring glucose levels and transmitting real-time data to a mobile app. The benefits of Blucon Nightrider CGM extend far beyond mere convenience—it offers a lifeline of support and reassurance to parents, serving as a guardian angel watching over their child's health.
Empowering Peace of Mind: One of the most significant advantages of Blucon Nightrider CGM is the peace of mind it provides to parents. Instead of relying on sporadic fingerstick tests or waking up multiple times during the night to check their child's blood glucose levels, caregivers can simply glance at their smartphone to monitor real-time data. This continuous monitoring offers a sense of security and confidence, knowing that they will be alerted to any fluctuations or trends that require attention.
Early Detection and Intervention: Blucon Nightrider CGM empowers parents with the ability to detect trends and patterns in their child's glucose levels, allowing for early intervention and adjustment of treatment plans. By observing real-time data, caregivers can identify potential highs or lows before they escalate into more serious complications. This proactive approach to diabetes management can significantly improve outcomes and enhance the quality of life for both children and their parents.
Enhanced Sleep and Quality of Life: For many parents of diabetic children, sleepless nights spent worrying about their child's health are all too familiar. Blucon Nightrider CGM offers a reprieve from this constant anxiety, allowing caregivers to enjoy more restful sleep knowing that they will be alerted to any issues as they arise. By reducing the disruption to their sleep patterns, Blucon Nightrider CGM enhances the overall quality of life for parents, enabling them to be more present and engaged in both their caregiving responsibilities and other aspects of their lives.
Real-Life Testimonials: The impact of Blucon Nightrider CGM on the lives of families navigating pediatric diabetes cannot be overstated. Countless parents have shared their stories of how this innovative technology has transformed their daily routine and provided newfound peace of mind. From allowing children to participate in activities without constant supervision to enabling parents to confidently delegate caregiving responsibilities to others, Blucon Nightrider CGM has become an indispensable tool in the arsenal of caregivers.
Conclusion: In the journey of caregiving for a child with diabetes, parents are the unsung heroes—selflessly devoting themselves to providing love, support, and unwavering care. Blucon Nightrider CGM serves as a guardian angel for these parents, offering support, reassurance, and peace of mind as they navigate the complexities of pediatric diabetes. With Blucon Nightrider CGM by their side, parents can rest assured that they have a powerful ally in their corner, empowering them to face the challenges ahead with confidence, grace, and resilience.

0 notes
Text
Small Device, Big Impact: The Surprising Advantages of Smart Rings in Wearable Gadgets
In the world of wearable technology, size doesn't always correlate with significance. While smartwatches and fitness trackers often dominate the conversation, there's a small yet powerful player quietly making waves: the smart ring. These unassuming devices may be diminutive in size, but they pack a punch when it comes to functionality and impact. In this exploration, we uncover the surprising advantages of smart rings in the realm of wearable gadgets and why these compact devices are poised to make a big impact on our lives.
A New Dimension of Wearable Technology
Smart rings represent a new frontier in wearable technology, offering a fresh perspective on what it means to interact with our digital world. Unlike their bulkier counterparts, these devices are designed to be discreet and unobtrusive, blending seamlessly into our everyday lives. Yet, despite their small size, smart rings offer a wealth of features and capabilities that rival those of larger wearables.
1. Portability and Convenience
One of the most obvious advantages of smart rings is their portability. Unlike smartwatches, which can feel cumbersome and bulky on the wrist, smart rings are lightweight and compact, making them ideal for everyday wear. Whether you're running errands, hitting the gym, or attending a formal event, smart rings can accompany you wherever you go, without weighing you down or getting in the way.
2. Seamless Integration
Despite their small size, smart rings are surprisingly powerful when it comes to integration with other devices and platforms. Whether you're syncing data with your smartphone, connecting to your smart home devices, or accessing your favorite apps and services, smart rings offer seamless compatibility across the board. This level of integration ensures that you can stay connected and productive, no matter what devices you're using.
3. Gesture Control and Intuitive Interaction
One of the most compelling features of smart rings is their ability to offer intuitive interaction through gesture control. By simply moving your fingers or tapping on the surface of the ring, you can navigate menus, control multimedia playback, and interact with apps and services with ease. This intuitive interface makes smart rings accessible to users of all ages and technical abilities, eliminating the need for complicated buttons or touchscreens.
4. Privacy and Security
With growing concerns about privacy and security in the digital age, smart rings offer a welcome solution. Unlike smartphones or smartwatches, which are often left unattended or accessible to others, smart rings remain securely on your finger at all times. This reduces the risk of unauthorized access to your personal data and ensures that your information remains private and protected.
5. Health and Wellness Tracking
In addition to their convenience and security features, smart rings also offer valuable health and wellness tracking capabilities. Equipped with sensors such as heart rate monitors, activity trackers, and sleep monitors, these devices can provide valuable insights into your physical health and well-being. From monitoring your heart rate during workouts to tracking your sleep patterns at night, smart rings empower you to take control of your health and make informed decisions about your lifestyle.
6. Fashion and Personalization
Last but not least, smart rings offer a level of fashion and personalization that is unmatched by other wearables. With a wide range of styles, colors, and materials to choose from, you can find a smart ring that perfectly complements your personal style and preferences. Whether you prefer a sleek and modern design or a more classic and understated look, there's a smart ring out there for everyone.
Looking Ahead: The Future of Smart Rings
As we look to the future, the potential of smart rings seems limitless. From enhancing convenience and productivity to improving health and wellness, these devices are poised to play an increasingly integral role in our daily lives. With their compact size, powerful features, and intuitive interaction, smart rings offer a unique combination of functionality and style that is unmatched by other wearables. As technology continues to evolve, smart rings are sure to remain at the forefront of innovation, reshaping the way we interact with our digital world one gesture at a time.
In conclusion, smart rings may be small in size, but they offer a big impact when it comes to wearable technology. With their portability, seamless integration, intuitive interaction, and focus on privacy and security, these devices are redefining what it means to wear technology on your finger. Whether you're tracking your fitness goals, staying connected on the go, or simply expressing your personal style, smart rings offer a versatile and stylish solution that is sure to stand the test of time. As we continue to embrace the possibilities of wearable technology, smart rings are poised to lead the way into a future where convenience, connectivity, and style go hand in hand.

0 notes
Text
Achieving Wellness: Integrating Smartwatches into Type 1 Diabetes Fitness Plans
Living with Type 1 diabetes requires a proactive approach to health management, especially concerning fitness and exercise routines. Integrating smartwatches into Type 1 diabetes fitness plans represents a significant advancement in personalized health monitoring and management. These wearable devices offer a range of features tailored to the unique needs of individuals with diabetes, empowering them to achieve wellness goals while effectively managing their condition. In this article, we'll explore the benefits and strategies for integrating smartwatches into Type 1 diabetes fitness plans.
Monitoring Blood Glucose Levels in Real-Time
One of the most critical aspects of managing Type 1 diabetes during exercise is maintaining stable blood glucose levels. Smartwatches equipped with continuous glucose monitoring (CGM) systems provide users with real-time insights into their blood sugar levels, allowing for proactive adjustments to insulin dosages, dietary intake, and physical activity levels. By monitoring blood glucose levels continuously, individuals with Type 1 diabetes can prevent hypo- or hyperglycemic episodes during exercise, ensuring safe and effective workouts.
Tracking Physical Activity and Exercise
Smartwatches offer comprehensive fitness tracking capabilities that cater to the specific needs of individuals with Type 1 diabetes. These devices can accurately monitor various aspects of physical activity, including steps taken, distance traveled, calories burned, and exercise duration. By tracking exercise metrics in real-time, individuals can gauge the intensity of their workouts and make informed decisions about their insulin requirements and carbohydrate consumption to maintain optimal blood glucose levels.
Moreover, smartwatches can detect specific types of physical activity, such as running, cycling, or swimming, and provide customized feedback and insights tailored to each activity type. This allows individuals to fine-tune their fitness routines based on their preferred activities and goals, whether it's improving cardiovascular health, building strength, or enhancing endurance.
Setting Personalized Fitness Goals and Targets
Integrating smartwatches into Type 1 diabetes fitness plans enables users to set personalized fitness goals and targets aligned with their health objectives. Whether aiming to increase daily step count, achieve a certain distance in running or cycling, or improve overall fitness levels, smartwatches provide users with the tools and motivation to track their progress and stay on course.
By setting achievable goals and tracking progress over time, individuals with Type 1 diabetes can maintain motivation and focus on their fitness journey. Smartwatches offer features such as goal tracking, milestone celebrations, and progress insights, which help users stay motivated and engaged with their fitness plans. Additionally, smartwatches can adjust goals dynamically based on users' performance and preferences, ensuring continuous improvement and adaptation to changing circumstances.
Leveraging Smartwatch Apps and Integrations
Smartwatches for Type 1 diabetes often come with dedicated health and fitness apps designed to support individuals in managing their condition effectively. These apps offer a range of features, including glucose trend analysis, insulin dose calculation, and personalized workout recommendations, tailored to the unique needs of individuals with diabetes.
Furthermore, smartwatch apps can integrate with other health and wellness platforms, such as nutrition trackers, sleep monitors, and stress management apps, to provide a holistic view of users' overall health and well-being. By leveraging data from multiple sources, individuals can gain deeper insights into the factors influencing their blood glucose levels and make informed decisions about their lifestyle habits and behaviors.
Fostering Accountability and Support
Integrating smartwatches into Type 1 diabetes fitness plans fosters a sense of accountability and support among users, enabling them to connect with peers, healthcare providers, and fitness communities for encouragement and guidance. Many smartwatch platforms offer social sharing features, activity challenges, and support groups where individuals can share their experiences, seek advice, and celebrate achievements together.
By participating in online communities and engaging with like-minded individuals, individuals with Type 1 diabetes can find inspiration, motivation, and practical tips for managing their condition while pursuing their fitness goals. Additionally, healthcare providers can leverage smartwatch data to monitor patients' progress remotely, provide personalized recommendations, and intervene if necessary to optimize diabetes management and improve health outcomes.
Conclusion
In conclusion, integrating smartwatches into Type 1 diabetes fitness plans offers numerous benefits for individuals striving to achieve wellness goals while effectively managing their condition. From monitoring blood glucose levels in real-time to tracking physical activity, setting personalized fitness goals, and leveraging smartwatch apps and integrations, these wearable devices provide a comprehensive solution for optimizing health and fitness outcomes.
By embracing smartwatch technology and incorporating it into their daily routines, individuals with Type 1 diabetes can take control of their health and well-being, one step at a time. With continuous innovation and advancement in wearable technology, the future looks promising for individuals seeking to achieve wellness and thrive with Type 1 diabetes.

0 notes
Text
Living Vibrantly with Diabetes: Lifestyle Hacks for Optimal Health
Living with diabetes doesn't have to mean sacrificing joy, vitality, or quality of life. In fact, with the right mindset and lifestyle adjustments, it's entirely possible to thrive with diabetes and lead a vibrant, fulfilling life. In this guide, we'll explore a variety of lifestyle hacks and strategies designed to optimize health, manage blood sugar levels, and promote overall wellness for individuals living with diabetes.
Embracing a Positive Mindset
Maintaining a positive mindset is essential for navigating the challenges of diabetes with resilience and grace. Instead of viewing diabetes as a limitation, see it as an opportunity to prioritize your health and well-being. Cultivate gratitude for your body and all that it does for you, despite the challenges it may face. Surround yourself with positivity, whether through uplifting affirmations, inspiring role models, or supportive communities of fellow individuals living with diabetes.
Nourishing Your Body with Nutrient-Rich Foods
A healthy diet is the cornerstone of diabetes management, providing the essential nutrients your body needs to thrive while helping to regulate blood sugar levels. Focus on incorporating a variety of nutrient-rich foods into your meals, including:
Vegetables: Fill your plate with colorful vegetables like leafy greens, bell peppers, broccoli, and carrots, which are packed with vitamins, minerals, and fiber.
Fruits: Choose whole fruits over fruit juices or sugary snacks, opting for lower glycemic options like berries, apples, and citrus fruits.
Whole Grains: Opt for whole grains such as quinoa, brown rice, oats, and whole wheat bread, which provide sustained energy and fiber to help stabilize blood sugar levels.
Lean Proteins: Include lean protein sources like poultry, fish, tofu, beans, and lentils in your meals to promote satiety and muscle health.
Healthy Fats: Incorporate sources of healthy fats such as avocados, nuts, seeds, and olive oil into your diet to support heart health and improve insulin sensitivity.
By prioritizing whole, minimally processed foods and paying attention to portion sizes, you can nourish your body and optimize your health while living with diabetes.
Staying Active and Fit
Regular physical activity is crucial for managing diabetes and promoting overall well-being. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, cycling, swimming, or dancing. Additionally, include strength training exercises at least two days per week to build muscle mass and improve insulin sensitivity.
Find activities that you enjoy and make them a regular part of your routine. Whether it's taking a daily walk in nature, practicing yoga, or joining a group fitness class, staying active doesn't have to feel like a chore. Remember to listen to your body and adjust your activity level as needed, especially if you experience fluctuations in blood sugar levels or other diabetes-related symptoms.
Prioritizing Sleep and Stress Management
Getting enough quality sleep and managing stress are often overlooked but critical aspects of diabetes management. Chronic stress and inadequate sleep can contribute to imbalanced blood sugar levels, increased insulin resistance, and other health issues. prioritize self-care practices that promote relaxation and restful sleep, such as:
Establishing a Consistent Sleep Schedule: Aim for seven to nine hours of sleep per night and maintain a consistent sleep-wake cycle, even on weekends.
Practicing Mindfulness and Meditation: Incorporate mindfulness techniques, deep breathing exercises, or meditation into your daily routine to reduce stress and promote mental well-being.
Engaging in Relaxing Activities: Find activities that help you unwind and relax, whether it's reading a book, listening to music, taking a warm bath, or spending time in nature.
By prioritizing sleep and stress management, you can support your overall health and well-being while living with diabetes.
Monitoring Blood Sugar Levels and Medication Adherence
Regular monitoring of blood sugar levels is essential for managing diabetes effectively and avoiding complications. Work with your healthcare team to develop a monitoring schedule that meets your individual needs and goals. Keep track of your blood sugar readings, medication doses, and any changes in your symptoms or health status. Additionally, adhere to your prescribed medication regimen as directed by your healthcare provider, taking medications as prescribed and following any recommended lifestyle modifications.
Building a Supportive Network
Living with diabetes can sometimes feel overwhelming, but you don't have to navigate it alone. Build a supportive network of family, friends, healthcare providers, and fellow individuals living with diabetes who can offer encouragement, guidance, and understanding along your journey. Share your experiences, ask for help when needed, and celebrate your successes together. Remember that you are not alone, and there is strength in community.
Conclusion
Living vibrantly with diabetes is not only possible but entirely achievable with the right mindset, lifestyle habits, and support network in place. By embracing a positive mindset, nourishing your body with nutrient-rich foods, staying active and fit, prioritizing sleep and stress management, monitoring blood sugar levels, adhering to your medication regimen, and building a supportive network, you can optimize your health and well-being while thriving with diabetes. Remember that you are resilient, capable, and deserving of a vibrant, fulfilling life, regardless of your diabetes diagnosis.

0 notes
Text
Balancing Act: Navigating High and Low Calorie Effects on Blood Glucose
Introduction: Balancing blood glucose levels is akin to walking a tightrope, requiring precise management of dietary intake, particularly calories. Whether you're aiming to stabilize blood sugar for health reasons or seeking optimal energy levels, understanding how both high and low-calorie diets influence blood glucose is crucial. In this comprehensive exploration, we'll delve into the complex dynamics of calorie intake and its impact on blood sugar regulation, offering insights to help you navigate this delicate balancing act.
The Dynamics of Blood Glucose Regulation: Before we delve into the effects of calorie consumption, let's establish a foundational understanding of blood glucose regulation. Glucose, derived from the foods we eat, serves as the primary source of energy for our cells. When we consume carbohydrates, they are broken down into glucose, which enters the bloodstream, prompting the release of insulin from the pancreas.
Insulin plays a key role in facilitating the uptake of glucose by cells, thereby lowering blood sugar levels. Conversely, when blood glucose levels drop, glucagon signals the release of stored glucose from the liver to maintain stable blood sugar levels. This intricate interplay of hormones ensures that our bodies maintain an equilibrium of blood glucose, crucial for optimal function.
High-Calorie Diets and Blood Glucose: High-calorie diets, often characterized by excessive intake of refined sugars, processed foods, and high-fat meals, can have significant implications for blood glucose regulation. When we consume a meal high in calories, especially from simple carbohydrates and sugars, it can lead to rapid spikes in blood glucose levels.
For instance, indulging in sugary snacks, sweetened beverages, and high-fat meals can overwhelm the body's insulin response, causing blood sugar levels to soar. These rapid fluctuations in blood glucose can contribute to insulin resistance over time, increasing the risk of type 2 diabetes and other metabolic disorders.
Moreover, high-calorie diets often lack essential nutrients and fiber, further exacerbating blood sugar imbalances. Without adequate fiber to slow down digestion and nutrient absorption, the body struggles to regulate blood glucose effectively, leading to instability and potential health complications.
Low-Calorie Diets and Blood Glucose: On the flip side, low-calorie diets, popular for weight loss purposes, also pose challenges for blood glucose management. While reducing calorie intake can promote weight loss and improve metabolic health, extreme calorie restriction can trigger hypoglycemia, or low blood sugar levels.
When we consume too few calories, especially from carbohydrates, our bodies may not have enough glucose to fuel essential functions, leading to symptoms such as weakness, dizziness, and irritability. Moreover, prolonged periods of low-calorie intake can disrupt hormone balance, including insulin and glucagon secretion, further complicating blood glucose regulation.
Finding Balance: Achieving balance in calorie intake is essential for maintaining stable blood glucose levels and overall health. Here are some strategies to help navigate the high and low-calorie effects on blood glucose:
Focus on nutrient-dense foods: Prioritize whole, unprocessed foods rich in vitamins, minerals, and fiber. Opt for complex carbohydrates such as whole grains, fruits, vegetables, and legumes, which provide sustained energy and promote stable blood glucose levels.
Monitor portion sizes: Be mindful of portion sizes, especially when consuming high-calorie foods. Pay attention to serving sizes and aim for moderation to prevent excessive calorie intake and blood sugar spikes.
Choose quality over quantity: Instead of focusing solely on calorie counting, prioritize the quality of your food choices. Emphasize nutrient-dense, whole foods that nourish your body and support optimal metabolic function.
Incorporate balance into meals: Aim for balanced meals that include a combination of carbohydrates, proteins, and healthy fats. Pairing carbohydrates with protein and fiber-rich foods can slow down digestion and help mitigate blood sugar fluctuations.
Listen to your body: Pay attention to hunger and satiety cues, and eat mindfully. Tune into your body's signals and eat when you're hungry, stopping when you're comfortably full.
Conclusion: Balancing the effects of high and low-calorie diets on blood glucose is a multifaceted endeavor that requires mindful eating, moderation, and a focus on nutrient-dense foods. By understanding the dynamics of blood glucose regulation and adopting strategies to support stable blood sugar levels, you can optimize your metabolic health and overall well-being. Remember, finding balance is key to navigating the complex interplay of calories and blood glucose, paving the way for a healthier, more vibrant life.

0 notes
Text
Sizzling Summer Solutions: How Blucon NightRider CGM Can Enhance Diabetes Management
Introduction:
As temperatures rise and summer approaches, individuals with diabetes often face unique challenges in managing their condition. The combination of warmer weather, changes in routine, and the temptation of summer treats can make it difficult to keep blood sugar levels in check. However, with advancements in technology like continuous glucose monitoring (CGM) systems such as Blucon NightRider, managing diabetes during the summer months has become more manageable than ever before. In this article, we will explore how Blucon NightRider CGM can enhance diabetes management and empower individuals to stay on top of their health during the sizzling summer season.
Understanding the Challenges of Summer Diabetes Management:
Before diving into the role of Blucon NightRider CGM, it's essential to understand the unique challenges that individuals with diabetes may face during the summer months.
Heat and Hydration: Warmer temperatures can lead to increased perspiration and fluid loss, which can affect hydration levels and blood sugar control.
Changes in Routine: Summer often brings vacations, outdoor activities, and social gatherings, which can disrupt regular meal and exercise schedules, making it challenging to maintain consistent blood sugar levels.
Temptation of Summer Foods: Barbecues, picnics, and ice cream outings are all staples of summer, but they can also lead to indulging in high-carbohydrate and high-sugar foods, which can spike blood sugar levels.
Blucon NightRider CGM: A Game-Changer in Diabetes Management:
Blucon NightRider CGM is a revolutionary device that provides continuous glucose monitoring in real-time. It consists of a small sensor attached to the skin, which continuously measures glucose levels in the interstitial fluid. This data is then transmitted wirelessly to a mobile device, allowing users to monitor their blood glucose levels conveniently throughout the day and night.
Key Features and Benefits:
Real-Time Monitoring: Blucon NightRider CGM provides users with real-time glucose readings, allowing them to see how their blood sugar levels are trending at any given moment. This enables timely intervention and adjustment of insulin dosages or carbohydrate intake as needed.
Trend Analysis: In addition to real-time monitoring, Blucon NightRider CGM tracks glucose trends over time, providing valuable insights into patterns and fluctuations in blood sugar levels. This information can help users identify triggers and make informed decisions about their diabetes management strategies.
Customizable Alerts: Blucon NightRider CGM offers customizable high and low glucose alerts, allowing users to set personalized thresholds based on their individual needs and preferences. This ensures that users are promptly notified of any concerning changes in their blood sugar levels, even when they are not actively monitoring.
Data Sharing: Blucon NightRider CGM allows users to share their glucose data with healthcare providers, family members, or caregivers, facilitating collaboration and informed decision-making. This can lead to more personalized and effective diabetes management recommendations tailored to each individual's unique needs.
Enhancing Summer Diabetes Management with Blucon NightRider CGM:
Now that we've covered the basics of Blucon NightRider CGM, let's explore how this innovative device can enhance diabetes management during the sizzling summer months.
Temperature Compensation: Blucon NightRider CGM is designed to provide accurate glucose readings even in extreme temperatures, ensuring reliable data regardless of the summer heat. This gives users peace of mind knowing that they can trust the device to provide accurate readings no matter the weather conditions.
Hydration Monitoring: Staying hydrated is crucial for individuals with diabetes, especially during hot weather when the risk of dehydration is higher. Blucon NightRider CGM can help users track their hydration levels by monitoring how changes in fluid intake affect their blood sugar levels. This information can empower users to stay adequately hydrated, promoting better blood sugar control and overall health.
Exercise Management: Summer often brings opportunities for outdoor activities and exercise, which can have a significant impact on blood glucose levels. With Blucon NightRider CGM, users can monitor their glucose levels in real-time during exercise, allowing them to adjust their insulin dosages or carbohydrate intake as needed to prevent hypoglycemia or hyperglycemia.
Diet Tracking: Summer festivities often revolve around food, making it challenging to stick to a healthy diet. Blucon NightRider CGM enables users to track how different foods affect their blood sugar levels, empowering them to make smarter dietary choices and maintain optimal diabetes control even when faced with tempting summer treats.
Conclusion:
Managing diabetes during the summer months comes with its own set of challenges, but with the help of technology like Blucon NightRider CGM, individuals can take control of their diabetes management and enjoy everything that summer has to offer. By providing real-time glucose monitoring, trend analysis, customizable alerts, and data sharing capabilities, Blucon NightRider CGM empowers individuals to make informed decisions about their diabetes care, even in the midst of rising temperatures and changing routines. So this summer, stay cool, stay hydrated, and stay in control with Blucon NightRider CGM.

0 notes
Text
Finding Your Fit: Exercise, Diabetes, and the Journey to Better Well-being"
Exercise plays a pivotal role in the management of diabetes, offering numerous benefits for physical and mental health. For individuals living with diabetes, incorporating regular physical activity into their routine is not only essential for blood sugar control but also contributes to overall well-being. In this article, we'll delve into the importance of exercise in diabetes management, explore various types of physical activity suitable for different fitness levels, and provide practical tips for integrating exercise into daily life.
Understanding Exercise and Diabetes
Regular exercise offers a multitude of benefits for individuals with diabetes. It helps improve insulin sensitivity, allowing cells to better utilize glucose for energy and reducing the need for insulin medication. Exercise also helps lower blood sugar levels, both during and after physical activity, which can lead to better long-term glycemic control. Additionally, regular exercise contributes to weight management, lowers blood pressure, improves cholesterol levels, and reduces the risk of cardiovascular disease – all of which are crucial considerations for individuals with diabetes.
Types of Exercise for Diabetes Management
Aerobic Exercise: Aerobic activities, such as walking, jogging, swimming, cycling, and dancing, are excellent choices for improving cardiovascular health and burning calories. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, spread out over several days.
Strength Training: Strength training exercises, including weightlifting, resistance band workouts, and bodyweight exercises, help build muscle mass, increase metabolism, and improve overall body composition. Incorporate strength training sessions at least two days per week, targeting major muscle groups.
Flexibility and Balance Exercises: Flexibility exercises, such as yoga and Pilates, improve range of motion and reduce the risk of injury. Balance exercises, such as tai chi, can help prevent falls, especially in older adults with diabetes who may experience neuropathy or vision problems.
Benefits of Exercise for Diabetes Management
Improved Blood Sugar Control: Regular exercise helps lower blood sugar levels by increasing glucose uptake into muscles and improving insulin sensitivity.
Weight Management: Exercise contributes to weight loss or weight maintenance by burning calories, building lean muscle mass, and increasing metabolism.
Reduced Cardiovascular Risk: Exercise lowers the risk of heart disease by improving cholesterol levels, lowering blood pressure, and reducing inflammation.
Stress Reduction: Physical activity releases endorphins, which are natural mood elevators, helping reduce stress, anxiety, and depression commonly associated with diabetes.
Enhanced Quality of Life: Engaging in regular exercise improves overall well-being, energy levels, and self-esteem, leading to a better quality of life for individuals with diabetes.
Practical Tips for Integrating Exercise into Daily Life
Start Slowly and Progress Gradually: Begin with activities that are enjoyable and manageable, gradually increasing intensity, duration, and frequency over time.
Set Realistic Goals: Establish achievable exercise goals that align with your fitness level, health status, and lifestyle. Celebrate small victories along the way to stay motivated and encouraged.
Find Activities You Enjoy: Choose activities that you genuinely enjoy and look forward to, whether it's walking in nature, dancing to music, playing a sport, or practicing yoga.
Make It Social: Exercise with friends, family members, or join group fitness classes to make physical activity more enjoyable and motivating.
Schedule Regular Exercise Sessions: Treat exercise like any other important appointment and schedule it into your daily or weekly routine. Consistency is key to reaping the benefits of regular physical activity.
Listen to Your Body: Pay attention to how your body feels during and after exercise, and adjust intensity or duration as needed. Stay hydrated, wear appropriate footwear and clothing, and take breaks when necessary.
Monitor Blood Sugar Levels: Check your blood sugar before, during, and after exercise to understand how different activities affect your glucose levels. Adjust food intake, medication, or exercise intensity accordingly to prevent hypoglycemia or hyperglycemia.
Incorporate Exercise into Daily Activities: Look for opportunities to be more active throughout the day, such as taking the stairs instead of the elevator, walking or cycling instead of driving short distances, or doing household chores or gardening.
Conclusion
Exercise is a powerful tool for diabetes management, offering a wide range of physical, mental, and emotional benefits. By incorporating regular physical activity into their routine, individuals with diabetes can improve blood sugar control, manage weight, reduce cardiovascular risk, and enhance overall well-being. Finding activities that are enjoyable, setting realistic goals, and making exercise a priority in daily life are essential steps toward better diabetes management and a healthier, happier lifestyle. Remember, the journey to better well-being begins with finding your fit and making exercise a sustainable part of your life.

0 notes
Text
From Beer to Tea: Finding Diabetic-Friendly Alternatives to Alcohol
For many people, social gatherings, celebrations, and even everyday meals often include alcoholic beverages like beer, wine, or cocktails. However, for individuals with diabetes, managing blood sugar levels while enjoying these traditional drinks can be challenging. Alcohol consumption can affect blood sugar levels unpredictably, leading to potential complications for those with diabetes. As a result, finding diabetic-friendly alternatives to alcohol becomes crucial for maintaining health and well-being.
Understanding the Impact of Alcohol on Blood Sugar
Before delving into alternatives, it's essential to understand how alcohol affects blood sugar levels in individuals with diabetes. Unlike carbohydrates, alcohol does not directly raise blood sugar levels. In fact, alcohol can initially lower blood sugar levels, especially for those taking insulin or certain diabetes medications.
However, the real challenge lies in the body's response to alcohol. When consumed in excess or without food, alcohol can lead to hypoglycemia (low blood sugar) hours after drinking. On the other hand, sugary alcoholic beverages, like cocktails or sweet wines, can cause blood sugar levels to spike.
Furthermore, alcohol can impair the liver's ability to produce glucose, increasing the risk of hypoglycemia, especially for those who rely on liver glycogen to maintain blood sugar levels while fasting or sleeping.
Diabetic-Friendly Alternatives: Exploring the Options
Fortunately, there are plenty of diabetic-friendly alternatives to alcohol that can still provide enjoyment and social engagement without the potential negative effects on blood sugar levels. One popular option is tea, which comes in a wide variety of flavors and types, offering something for every palate.
Herbal Teas: Herbal teas are a great alcohol alternative for individuals with diabetes. These teas are typically caffeine-free and come in a variety of flavors, including mint, chamomile, and fruit-infused blends. Herbal teas offer a comforting and soothing beverage option that can be enjoyed hot or cold.
Green Tea: Known for its antioxidant properties and potential health benefits, green tea is another excellent choice for individuals with diabetes. Green tea contains compounds called catechins, which may help improve insulin sensitivity and regulate blood sugar levels. Enjoyed hot or cold, green tea can be a refreshing and healthful alternative to alcohol.
Black Tea: With its robust flavor and caffeine content, black tea is a popular choice for those looking for a more stimulating beverage option. Like green tea, black tea contains antioxidants that may offer health benefits, including improved heart health and blood sugar regulation. Black tea can be enjoyed plain or with a splash of milk and a sprinkle of cinnamon for added flavor.
Fruit-Infused Teas: For those craving a sweeter beverage option without the added sugar, fruit-infused teas are a delicious alternative. These teas are made by infusing herbal or black tea with fresh or dried fruits, offering a natural sweetness without the need for added sugars. Popular fruit-infused tea flavors include berry, peach, and citrus.
Iced Tea: During the warmer months, iced tea is a refreshing and hydrating alternative to alcoholic beverages. Whether brewed at home or purchased from a store, iced tea can be customized with lemon slices, fresh herbs, or a splash of fruit juice for added flavor. Opting for unsweetened iced tea can help keep blood sugar levels in check while still enjoying a cool and satisfying drink.
Sparkling Tea: For those who enjoy the effervescence of beer or champagne, sparkling tea offers a bubbly alternative without the alcohol or added sugars. Sparkling teas come in a variety of flavors and can be enjoyed on their own or mixed with fruit juice for a fizzy mocktail experience.
Tea Cocktails: Get creative in the kitchen by experimenting with tea-based mocktails. Mix brewed tea with fresh herbs, fruit juice, and sparkling water to create refreshing and flavorful beverages that rival traditional cocktails in taste and presentation. With endless flavor combinations to explore, tea cocktails offer a fun and customizable alternative to alcohol.
Benefits of Choosing Tea Over Alcohol
Opting for tea over alcohol offers numerous benefits for individuals with diabetes, including:
Blood Sugar Control: Unlike alcohol, tea does not contain carbohydrates or sugars that can spike blood sugar levels, making it a safer choice for those with diabetes.
Hydration: Tea is a hydrating beverage option that can help maintain proper hydration levels, essential for overall health and well-being.
Antioxidants: Many types of tea, such as green and black tea, are rich in antioxidants that may offer protective benefits against chronic diseases, including diabetes and heart disease.
Variety: With countless flavors and types to choose from, tea offers endless possibilities for enjoyment and experimentation, ensuring there's something for everyone to savor.
Incorporating Tea into Your Lifestyle
Incorporating tea into your daily routine is easy and convenient, whether enjoyed as a morning pick-me-up, an afternoon treat, or a relaxing evening ritual. To make the most of your tea-drinking experience:
Experiment with Flavors: Try different types of tea and flavor combinations to find your favorites. Whether you prefer bold and robust or light and fruity, there's a tea out there to suit your taste buds.
Brew with Care: Follow brewing instructions carefully to ensure optimal flavor and enjoyment. Pay attention to water temperature, steeping time, and tea-to-water ratio for the best results.
Pair with Healthy Snacks: Enjoy your tea alongside nutritious snacks like nuts, fruit, or whole-grain crackers for a satisfying and balanced snack option.
Make it a Social Event: Invite friends or family over for a tea-tasting party and explore a variety of teas together. Share your favorites and experiment with different flavor combinations for a fun and interactive experience.
Final Thoughts
From beer to tea, finding diabetic-friendly alternatives to alcohol offers a way to enjoy social gatherings and celebrations without compromising health and well-being. With its endless variety of flavors, health benefits, and versatility, tea provides a satisfying and flavorful beverage option that's sure to please even the most discerning palate. Whether enjoyed hot or cold, on its own or mixed with other ingredients, tea offers a delicious and refreshing alternative to alcohol that's perfect for individuals with diabetes and anyone looking to make healthier beverage choices. So, the next time you're craving a drink, reach for a cup of tea and toast to your health and happiness. Cheers!

0 notes
Text
The Key to Longevity: Why Diabetics Should Make Blood Sugar Monitoring a Priority
Introduction
Diabetes is a chronic condition that affects millions of people worldwide, posing significant challenges to their health and well-being. Among the various aspects of diabetes management, blood sugar monitoring stands out as a critical component. For individuals with diabetes, maintaining optimal blood sugar levels is not just about managing symptoms—it's about ensuring longevity and a high quality of life. In this comprehensive discussion, we'll explore why diabetics should prioritize blood sugar monitoring for their overall health and longevity.
Understanding Diabetes and Blood Sugar
Diabetes is a metabolic disorder characterized by elevated blood sugar levels, resulting from either insufficient insulin production (Type 1 diabetes) or the body's inability to effectively use insulin (Type 2 diabetes). Insulin, a hormone produced by the pancreas, plays a crucial role in regulating blood sugar levels by facilitating the uptake of glucose into cells for energy.
When blood sugar levels are consistently high, it can lead to a myriad of complications, including cardiovascular disease, kidney damage, nerve damage, vision problems, and an increased risk of infections. Therefore, maintaining blood sugar levels within a healthy range is paramount for individuals with diabetes to prevent these complications and promote longevity.
The Significance of Blood Sugar Monitoring
Regular blood sugar monitoring is essential for several reasons:
Early Detection and Intervention: Monitoring blood sugar levels allows individuals to detect fluctuations early, whether it's hyperglycemia (high blood sugar) or hypoglycemia (low blood sugar). Early detection enables prompt intervention, helping to prevent complications and maintain optimal health.
Customized Treatment Plans: Blood sugar monitoring provides valuable data that healthcare professionals use to tailor treatment plans to individual needs. By tracking blood sugar trends over time, healthcare providers can adjust medication dosages, dietary recommendations, and lifestyle modifications to optimize diabetes management and promote longevity.
Prevention of Long-Term Complications: Consistently high blood sugar levels can lead to long-term complications that significantly impact longevity. By monitoring blood sugar levels regularly and keeping them within target ranges, individuals can reduce the risk of developing complications such as heart disease, kidney failure, nerve damage, and vision problems, thereby promoting longevity and a better quality of life.
Empowerment and Self-Management: Blood sugar monitoring empowers individuals with diabetes to take an active role in their health management. By understanding how their daily habits, including diet, exercise, stress management, and medication adherence, affect their blood sugar levels, individuals can make informed decisions to maintain better control over their condition and promote longevity.
Feedback Loop for Lifestyle Modifications: Monitoring blood sugar levels provides immediate feedback on the impact of lifestyle modifications. Whether it's adjusting meal timing, incorporating more physical activity, managing stress levels, or making changes to medication regimens, monitoring blood sugar levels allows individuals to assess the effectiveness of these changes and make adjustments as needed to promote longevity and overall well-being.
Practical Tips for Effective Blood Sugar Monitoring
To make blood sugar monitoring a priority and reap its benefits for longevity, here are some practical tips:
Use Reliable Glucose Monitoring Devices: Invest in high-quality glucose monitoring devices that provide accurate and reliable readings. Follow the manufacturer's instructions for proper use, calibration, and maintenance of the device.
Establish a Monitoring Routine: Develop a consistent routine for blood sugar monitoring, incorporating it into your daily schedule. Set specific times for testing, such as before meals, before bedtime, and as recommended by your healthcare provider.
Keep Detailed Records: Maintain a logbook or use a smartphone app to record blood sugar readings, along with details such as meal times, medication doses, physical activity, and any symptoms experienced. Keeping detailed records helps identify patterns and trends over time, enabling better management of diabetes and promoting longevity.
Stay Aware of Symptoms: Be vigilant for symptoms of high or low blood sugar, such as increased thirst, frequent urination, fatigue, blurred vision, dizziness, sweating, or confusion. Promptly test your blood sugar levels if you experience any of these symptoms and take appropriate actions to prevent complications.
Communicate with Healthcare Providers: Share your blood sugar monitoring data with your healthcare team during regular check-ups or as needed. Your healthcare provider can offer insights, adjustments to your treatment plan, and guidance on managing fluctuations to promote longevity and overall health.
Stay Informed and Educated: Continuously educate yourself about diabetes management, blood sugar monitoring techniques, and the latest advancements in diabetes care. Attend diabetes education classes, workshops, or support groups to enhance your knowledge and skills, empowering you to take control of your health and promote longevity.
Conclusion
In conclusion, blood sugar monitoring is not just a routine task for individuals with diabetes—it's the key to longevity and a high quality of life. By prioritizing blood sugar monitoring and following practical tips for effective monitoring, individuals with diabetes can detect fluctuations early, customize treatment plans, prevent long-term complications, empower themselves to manage their condition effectively, and make informed decisions to promote longevity and overall well-being. Every drop of blood contains valuable information that can make a significant difference in the lives of individuals living with diabetes. Embrace the importance of blood sugar monitoring, and unlock the door to longevity and optimal health.
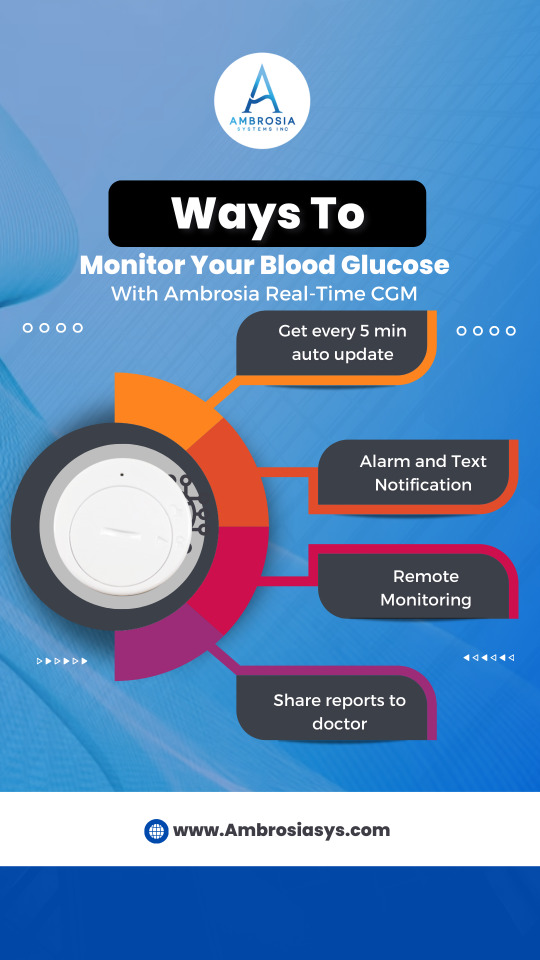
0 notes
Text
Self-Care for Diabetic Souls: Mental Health Practices for Ambrosia CGM Users
Living with diabetes can be challenging, both physically and emotionally. The constant monitoring of blood sugar levels, dietary restrictions, and potential complications can take a toll on one's mental well-being. However, with advancements in technology like the Ambrosia Continuous Glucose Monitoring (CGM) system, managing diabetes has become more manageable. In this article, we'll explore various mental health practices specifically tailored for Ambrosia CGM users to help them navigate the emotional aspects of living with diabetes.
Understanding the Emotional Impact: The first step in caring for your mental health as a diabetic using Ambrosia CGM is acknowledging the emotional impact of the condition. It's normal to feel a range of emotions, including frustration, anxiety, and even depression. Recognizing and accepting these feelings is crucial to your overall well-being.
Seeking Support: You're not alone in your journey with diabetes. Whether it's friends, family, or support groups, reaching out for support can make a significant difference in how you cope with your condition. Additionally, connecting with other Ambrosia CGM users can provide a sense of community and understanding.
Practicing Mindfulness: Mindfulness techniques, such as deep breathing exercises, meditation, and yoga, can help you manage stress and anxiety associated with diabetes. Take time each day to practice mindfulness and focus on the present moment, allowing yourself to let go of worries about the future.
Setting Realistic Goals: Living with diabetes requires making lifestyle changes, but it's essential to set realistic goals for yourself. Break down larger goals into smaller, achievable steps, and celebrate your progress along the way. This can help you stay motivated and positive about managing your condition.
Staying Active: Regular exercise not only helps control blood sugar levels but also boosts mood and reduces stress. Find physical activities that you enjoy, whether it's walking, swimming, or dancing, and incorporate them into your routine. Even small amounts of exercise can make a big difference in your overall well-being.
Eating Well: Proper nutrition is essential for managing diabetes, but it's also important for your mental health. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help stabilize your mood and energy levels. Avoid skipping meals or relying on processed foods, as they can negatively impact both your physical and mental health.
Managing Stress: Stress can wreak havoc on blood sugar levels, so it's crucial to find healthy ways to manage it. In addition to mindfulness practices and exercise, consider other stress-reducing activities such as spending time in nature, journaling, or listening to music. Find what works best for you and make it a priority in your daily routine.
Getting Adequate Sleep: Diabetes and sleep have a bidirectional relationship – poor sleep can affect blood sugar control, and uncontrolled diabetes can disrupt sleep. Aim for seven to eight hours of quality sleep each night by establishing a consistent sleep schedule, creating a relaxing bedtime routine, and optimizing your sleep environment.
Practicing Self-Compassion: Living with a chronic condition like diabetes can be challenging, so it's important to be kind to yourself. Practice self-compassion by acknowledging your efforts and successes, even on difficult days. Remember that managing diabetes is a journey, and it's okay to ask for help when you need it.
Celebrating Victories: Finally, don't forget to celebrate your victories, no matter how small they may seem. Whether it's reaching a blood sugar target, sticking to your meal plan, or trying a new form of exercise, every achievement deserves recognition. Celebrating your successes can help boost your confidence and motivation to continue managing your diabetes effectively.
In conclusion, self-care is essential for diabetic souls using Ambrosia CGM to manage their condition effectively. By prioritizing your mental health and incorporating these practices into your daily life, you can navigate the emotional challenges of living with diabetes with resilience and positivity. Remember that you are capable of managing your diabetes and thriving despite the challenges it may present.

0 notes