Welcome to my Radiology Teaching files. Everything is organized as unknowns so feel free to browse chronologically or by Subsection. Looking for a specific case? Use the search box up top.
Don't wanna be here? Send us removal request.
Text
Season 9 Case 6
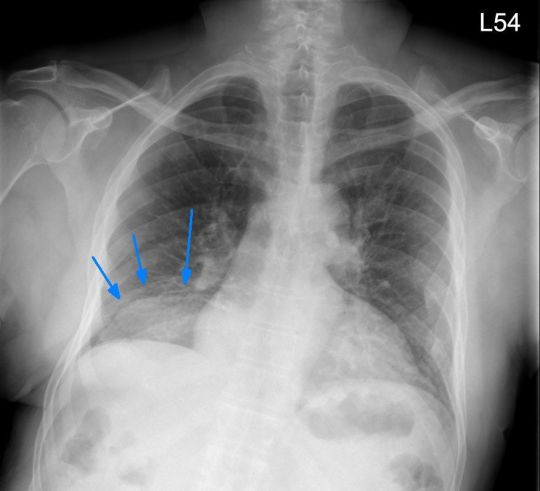
Hx: survey CXR after MVA

Answer: Continuous Diaphragm sign of Pneumomediastinum
The heart rests on the medial diaphragms, so normally they are silhouetted out. When we see them (blue arrows) it means there is air between the heart and diaphragm


This can be seen with pneumomediastinum or pneumopericardium.
There is a more subtle lucency about the high left heart border (yellow arrow) which is also consistent with pneumomediastinum.
These findings can be difficult to see on CXRs, esp when not involving the neck/axilla.

Multitude of causes but besides penetrating trauma, my experience has been tracheobronchial barotrauma is very common.
Boerhaave's always seems to come up so inquire for correct hx (wretching/vomiting ?pill stuck?) and for pleural fluid. Esophagram still gold standard to r/o
FYI: There does seem to be an association of this with inhaled illicit drug use (marijuana, cocaine). Typically in young males, ?barotrauma from breathe hold and deep coughing (I hear ) Condition is generally benign but often gets big w/u to exclude more concerning etiologies.
3 notes
·
View notes
Text
Season 9 Case 5
Hx: Abdominal pain


Answer: Ischemic Bowel
Fluid filled ?dilated bowel loops? YES
So they all look the same? No
Right abdominal loops (red) = thickened w/o enhancement vs those in the left abdomen (blue) which = early obstruction or ileus.
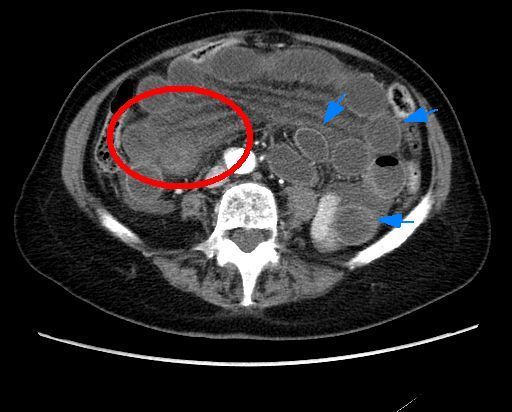
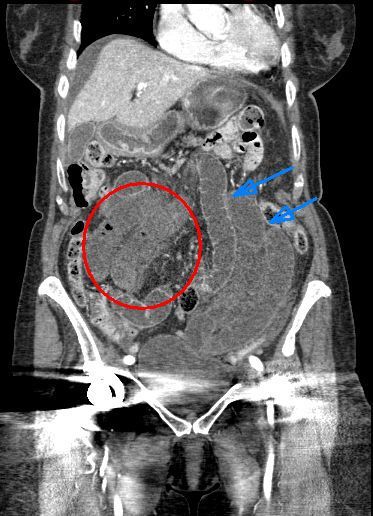


Surgery=necrotic bowel!
Small Bowel Ischemia
-life threatening EMERGENCY!!
- +wall thickening +/- dilation
-absent enhancement (use other bowel for comparison)
-bowel wall hyperdensity can be due to intramural hemorrhage (can on non-con!) so I look at the mucosa
-pneumatosis = infarction ( for PV gas!)
-CTA helpful to look for arterial etiology (majority)
-Also venous occlusion, systemic hypoTN (shock bowel), trauma, obstruction (ie closed-loop).
-Don't forget this on non-con exams! UGLY segment of bowel + lactate = CALL SURGERY!!
Time = bowel = survival!!
3 notes
·
View notes
Text
Season 9 Case 4
Hx: MVA, neck pain


Answer: Unilateral Facet Dislocation
Normal L & R superior articular facets overlap/aligned to the C6-C7 where 1 is shifted anterior(red dash)
-Ant & post vertebral lines (green) ?ok
-Spinolaminar line (orange)=broken
-Poseriort spinous line (purple) = gap
Perched facet = subluxed joint with tip of inferior facet resting on tip of super facet of lower body
Dislocated/jumped/locked facet = complete dislocation with inferior tip ANTERIOR to superior facet of lower body (thus "locked")
Get the CT and ALWAYS look for the fracture!

Unilateral jumped facets can be tough on X-ray as the vert body doesn't have to displace much (vert lines ok).
ALWAYS look at spinolaminar & posterior spinous lines!
Facets = "shingles on a roof"
Any abrupt change/rotation should be concerning!


For completeness, here is a bilateral facet dislocation.
ALL spinal lines disrupted. No rotation. Both inferior facets jumped and locked anterior to the superior facets of the lower body.
- MRI=diffuse ligamentous injury
- neurologically devastating

2 notes
·
View notes
Text
Season 9 Case 3
Hx: Chest pain
Diagnosis?


Answer: Bochdalek Hernia
Large round opacity right lung base.
On frontal does NOT obscure anterior diaphragm or R heart border - ie posterior/RLL
On lateral DOES "obscure" entire posterior R diaphragm

-congenital defect in posterior diaphragm attachment
- Can be either side (classic =L side in symptomatic infantslung hypoplasia, but R m/c in adults?)
- typically only fat but ~25% can contain abd organs
Hint: Bochdalek = Back

0 notes
Text
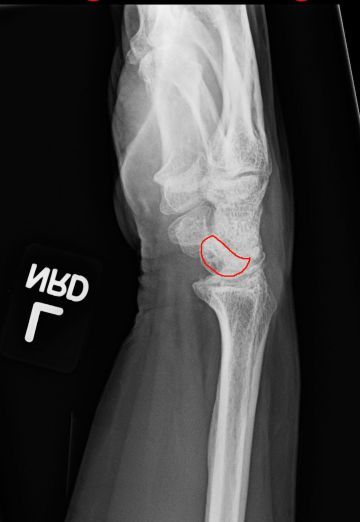
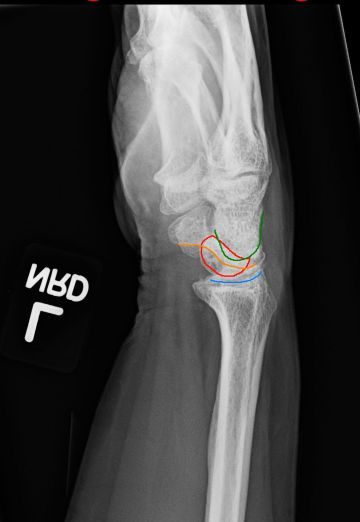
Season 9 Case 2
History: fall, pain
Do you know my name?


Answer: Barton Fracture
Distal radial fx but only involves dorsal aspect of the distal radius (volar aspect is intact). Radial styloid ok on oblique?
Barton fx = shear fx of dorsal distal radius
Shear off volar aspect = reverse Barton fx
This fx is not too displaced, but as the fx fragment displaces more, the carpal bones often dislocate with it. If we cone in tightly we can see the scaphoid/lunate are starting to migrate with the dorsal fragment
W/o proper trt, this can cause long term wrist pain/instability

I know eponyms are falling out of style. So why teach them?
Pathology is often named bc it is common or important. I don't care if you can spit out the name, but IMHO, by educating you about the name it should reinforce either it's prevalence or it's clinical significance
0 notes
Text
Season 9 Case 1
History: line placement for the OR. Everything look ok?

Answer:
1)Malpositioned Left subclavian catheter (extends into R IJ)
2)Malpositioned Right jugular Swan-Ganz catheter (extends into hepatic vein)
Did you see both? You have to check every one!


Let go through them. Correct ones first.
ETT - tip below the thoracic inlet and >2cm above carina
GI tube - tip/side port below GE junction (hard to see but I think so)
Mediastinal drain
Right chest tubes x 2 (No pneumothorax)

What about that left subclavian catheter?
Tip extends up into the right jugular vein.
Ideal = tip at SVC-atrial junction.
Repositioning needed!

What about that right jugular Swan-Ganz catheter?
Coils in the right atrium then extends caudal with the tip in one of the hepatic veins
Ideal = extends through right atrium with tip in the right or left main pulmonary artery.
Repositioning needed!

Shortcut? Not that I know of. Check every tube/line on every image.
But remember, the more you do anything, the faster you get at it. Repetition breeds speed. Try and get faster by experience, not by shortcuts.
0 notes
Text
Wetread Case 40 Answer
History: elbow swelling


Answer: Olecranon Bursitis secondary to Gout
Obviously we have focal mass-like soft tissue swelling posterior to the olecranon with minimal soft tissue edema otherwise about the elbow. This is classic picture of olecranon bursitis
Etiologies for olecranon bursitis:
-trauma
-excessive use (aka “student’s elbow” or “baker’s” or Popeye elbow)
-infection
-inflammation (classically gout, although RA and CPPD as well)
In this case we also see soft tissue Ca++ which we wouldn’t expect to see in trauma or overuse but can be seen with gout.
The issue that often comes up by inexperienced clinicians is concern for infection and desire to aspirate (heck just google “OB” and one of the first pics has a needle). I highly suggest you DO NO ASPIRATE. Gouty OB can be swollen, tender even mildly red/warm due to the inflammation. But if it isn’t infected when you tap it, it will be afterwards. And an infected bursa can be extremely difficult to treat with Abx and might even require surgical removal.
This is not an uncommon findings and almost always due to overuse or gout/RA.So keep the needle away!
1 note
·
View note
Text
Season 8 Case 39
History: altered mental status

Answer: Psuedosubarachnoid hemorrhage secondary to hypoxicischemic brain injury
In these 2 images we see hyperdensity (increased attenuation) along the basilar cisterns. While this is a common appearance of subarachnoid hemorrhage secondary to Circle of Willis Aneurysm rupture, we need to look at the entire image and the entire exam!


How about the basilar cisterns? - They are effaced
How about the grey-white junction? - It is gone. In fact, Normally grey matter is slightly hyperdense compared to the white matter, but here we have the peripheral grey matter actually lower in density than the central white matter (aka the reversal sign)
How about the central grey matter structures? Similarly, the caudate nuclei, basal ganglia and even thalami are all low in density - which again is not normal
How about the normal sulcal pattern of the cerebrum? - It’s gone. In fact can you even find a sulcus? (and the patient isn’t 15 years old)

This is an example of global anoxic injury aka hypoxic-ischemic encephalopathy. Global anoxia leads to neuron injury. Since grey matter is more metabolic than white matter, it is effected earlier and more severely. Anoxia/Ischemic -> neuron injury -> edema -> decreasing grey matter density.
So what about that increased density all throughout the basilar cisterns, sylvian fissure, falx and tentorium? While it may look like blood, it’s actually artifact - ie pseudosubarachnoid hemorrhage.
Because of the cerebral edema, particularly the grey matter edema, the parenchymal density decreases. This combined with outflow venous dilation and thrombosis secondary to the increasing intracranial pressure, yields the appearance of increased density particularly throughout the basilar cisterns.
If you can get a good density measurement you will see it is more in the normal 30-40 HU venous density range compared to extra-vascular or true subarachnoid hemorrhage in the 60-70 HU range.
0 notes
Text
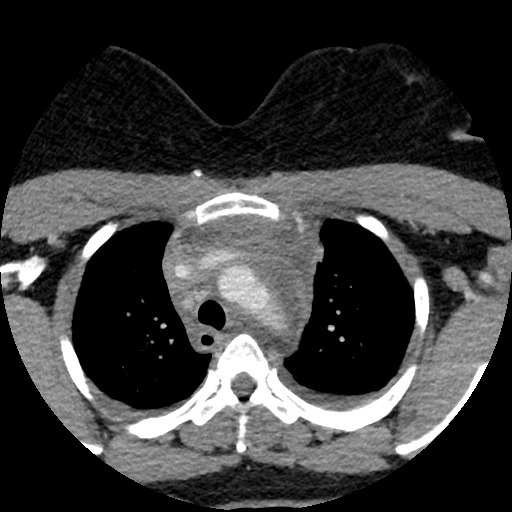
Wetread Case 38
History: chest pain
Diagnosis?


Answer: Penetrating Atheromatous Ulcer (PAU)
What? How you say? Let’s walk through this.
Here’s the current Chest X-ray and I’ve added labels (blue = heart border, red = aorta, orange = hilar vessels).
We see a left infrahilar mass that doesn’t obscure the left hear border (blue) but does obscure the aortic border (red, with dashed lines being where we think it should go and the dark red line outlining the mass). We can still see the hilar vessels (orange) so this mass can not be the vessels nor silhouette the vessels (ie the hilum overlay sign)

So this mass has to either obscure the border of the descending thoracic aorta or be the descending thoracic aorta. And if it is the aorta, we have a focal mass or enlargement of the aorta.
Can we confirm?

It is difficult to see the entire aorta, but red lines are my guestimate suggesting increased diameter over the mid throacic spine.
So when the answer box (aka CT scanner) comes back up, here is what we see.

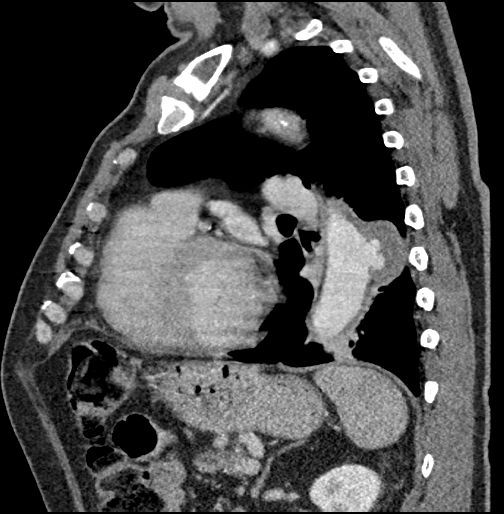
Sure enough there we see focal bulging of the aorta which just so happens to contain contrast in keeping with a PAU.
Aortic wall pathology can be a bit confusing. There are a bunch of good articles including Radiology Assistant from which I am borrowing their wonderful images. I encourage everyone to go read their wonderful write-up. In summary:
Intramural hematoma is isolated blood within the vessel wall with no connection to the inner lumen

Ulcerated plaque is just that, an ulcer in atheromatous plaque but it does NOT extend beyond the intimal layer
If the ulceration errodes beyond the normal intimal layer into the vessel wall (ie the media layer), now we have a penetrating atheromatous ulcer (PAU)
All of the above can progress to an aortic dissection. So there is injury to the vessel intima allowing blood into the media layer and then the pressure gradient causes extension of the injury through the vessel wall (ie media layer)

While that may be a bit simplistic, hopefully that helps understand the different types of aortic wall pathology.
2 notes
·
View notes
Text
Season 8 Case 37
History: Abdominal pain. Palpable mass


Answer: De Garengeot Hernia with acute appendicitis!
A De Garengeot hernia is a femoral hernia containing the appendix, which is exactly what we have here but the appendix is hyperenhancing with wall thickening and surrounding fluid consistent with acute appendicitis.
Named after a French surgeon from the 1700s, these are fairly rare (<3% of femoral hernias), with complicating appendicitis even more rare.
Understanding groin hernias can take time and they are not always easy to figure out. There are 2 major types:
Inguinal hernia
~80% of abdominal wall hernias
MLF ratio of 7:1
Types:
1) Indirect
-more common
-Can be a)congenital defect in a patent process vaginalis in young males or b) acquired do to stretching/weakness of the inguinal ring in older patients
- passes through deep inguinal ring
- LATERAL to the inferior epigastric artery
- anterior to spermatic cord or may insinuate around the inguinal contents
2) Direct
- less common
- secondary to weakness in floor of inguinal canal (Hesselbach’s triangle)
- MEDIAL to inferior epigastric artery (therefore inguinal contents generally displaced laterally)
Image below shows the inferior epigastric vessels labeled as Orange so the fat lateral to the vessels would be the INDIRECT hernia (blue) and the fat medial the the vessels (red) would be the DIRECT hernia.But both go into the inguinal canal, just through different routes.
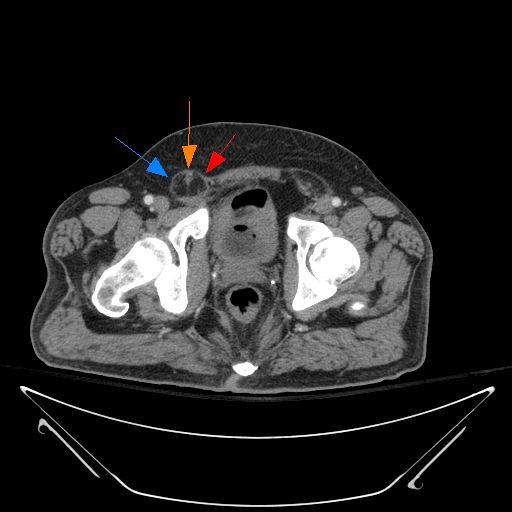
A femoral hernia is a hernia through the femoral ring, so it is inferior to inguinal ligament and lateral to the inguinal canal. As it protrudes through the femoral ring, it can compress the normal femoral canal contents, primarily the femoral vein. You tend to see it seeing more on top of the pectineus muscle as it lies on the superior pubic ramus.
Here we see a small fat containing femoral hernia (yellow) compared to a normal inguinal canal (blue)

Groin hernia summary: Inguinal hernia extend inf and medial into inguinal canal. Direct take a "direct course" medial to inf epigastric artery vs Indirect go more "indirectly" lateral to vessels Femoral hernias go inf and lateral through femoral ring compressing the femoral vein.
"Fancy" Groin hernias:
Amyand hernia = inguinal hernia containing appendix (some say specifically appendicitis)
De Garengeot hernia = femoral hernia containing appendix (or appendicitis as we see here!)
Here we have a De Garengeot Hernia. Labels: Hernia yellow, appendix red


0 notes
Text
Wetread Case 36
History: wrist pain


Answer: Dorsal Intercalated Segment Instability (DISI)
So what findings do we see:
1) Widened scapholunate distance =Injury to the S-L ligament yields widening of the distance, commonly referred to as the Terry Thomas sign (or for younger Rads the David Letterman Sign, the Madonna Sign, or the Michael Strahan Sign)
2) Abnormal scaphoid - Note the scaphoid’s appearance on the frontal exam. The radial margin is not normal consistent with a prior fracture deformity. Since scaphoid fracture is the most common carpal fracture, it makes sense a single injury could cause both the fracture and the S-L ligament injury
But what about the lateral exam?
3) Dorsal rotation of the lunate bone
The carpal bones and their ligaments have a complex relationship. Primarily the proximal and distal rows form a kind of “ring”. However, there is a three dimensional twist or torque to that ring. What that means is that when the is disruption of the ring, such as by complete tearing of the scapholunate ligament, not only does the ring widen, but the bones are allowed to “un-torque” or untwist.
When this happens the scaphoid will start rotating volarly (towards the palm) and the triquetrum/pisiform will start rotating dorsal (to the back of the hand). The lunate goes along with whichever it is connected to. And since we have torn the Scapholunate ligament, it rotates with the triquetrum dorsally - ie DORSAL intercalated segment instability.
Interestingly, if instead you tear your lunotriquetral ligament, the lunate will then rotate with the scaphoid towards the palm (volarly) = VOLAR intercalated segment instability (VISI)
Orthopedics like measuring things so you can measure:
scapholunate angle (nl 30-60)
capitolunate angle (nl <30)
radiolunate angle (nl <15).
Here I drew in the bone outlines and measured the capitolunate angle which is >30 degrees (ie the dorsal tilt of the lunate)

Generally these findings can be seen on X-ray. You can measure the S-L distance (nl <2-3) but it does vary upon gender. Generally >3mm abnl If you want fancy pictures you can do an MRI to look for bone contusions or even an MR Arthrogram to eval the S-L ligament directly.
Clinically:
- Radial/dorsal wrist pain, esp w radial deviation or extension
- weakness/instability
Concurrently, as the bones are “untwisting”, you will get abnormal wear and osteoarthritis at the radioscaphoid joint and the capitate bone will gradually migrate proximally to fill the scaphol-lunate interval. This is termed Scapholunate Advance Collapse (SLAC wrist)
1 note
·
View note
Text
Case 35
History: neck and check pain. Swelling


Answer: Thrombophlebitis of the Left bracheocephalic vein with mediastinitis
Check out the new X-ray. We definitely see widening of the upper mediastinum. But can we be more specific? Where is the “mass”

We can see from our current exam that the contour of the aortic silhouette (red arrow) is maintained so it should not be adjacent to the aorta. If fact it actually obscures the left subclavianartery silhouette (yellow arrows) so it has to be in that region of the anterior mediastinum.
So what’s next? How about the CT?

Now we clearly see the extensive stranding throughout the anterior mediastinal fat, with severe narrowing of the left bracheocephalic vein and left jugular vein.
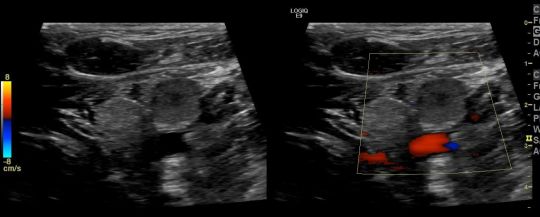
Finally we have the Doppler Ultrasound of the left jugular vein showing occlusion. In fact the left jugular and subclavian veins were thrombosed as centrally as able to be visualized.
What’s the source? Here’s a higher slice from the neck CT showing retropharengeal fluid likely relating to pharengeal infection.

In summary, we have thrombosis of the left jugular, subclavian and bracheocephalic veins with associated thrombophlebitis and mediastinitis preumably secondary to a pharyngeal infection. This is similar to a Lemierre’s Syndrome however classically that involved the internal jugular vein but here we have common jugular and distal thrombophlebitis.
Lemierre’s Syndrome:
Presentation:
Neck pain and swelling with ongoing/recent oropharengeal inection
Male predominance
generally 16-25 years old
Pathology:
80% caused by Gram (-) Fusobacterium necrophorum but can get polymicrobial even including MRSA
Radiology:
shows jugular vein thrombosis. US generally easiest and most straight forward but can be limited in the chest
CT/MR can be helpful for more central venous evaluation and to identify source/site of primary infection
Complications: Pulmonary Septic emboli and systemic dissemination
Treatment: Anticoagulation and IV Abx. Mortality rates can be as high at 18%.
3 notes
·
View notes
Text
Case 34 Answer
History: palpable mass


Answer: Calcinosis of Chronic Renal Failure (ie secondary tumoral calcinosis)
The exact name of this is somewhat confusing. True Tumoral Calcinosis (TC) is generally reserved for the hereditary dysfunction of phosphate regulation which results in large, painless, periarticular calcifications.
So here we have the exact same finding except secondary to chronic renal failure, thus “secondary” or “uremic” tumoral calcinosis. The exact cause is not fully understood by generally believed related to hyperparathyroidism. Interestingly chronic renal failure is actually the most frequent cause of a periarticular calcified mass. And there are no radiographic or histologic differences between the primary or secondary TC.
Findings of TC:
- Amorphous, sometimes cystic, multilobulated calcifications located about a joint.
- Can see layering milk of calcium (sedimentation sign).
- Can be homogeneous (suggesting less metabolic activity and growth)
- Not connected to underlying bone
- No osseous erosion of destruction by the mass
- Typically painless
- Hip > shoulder > elbow > foot > wrist
Treatment: Primarily dialysis and phosphate depletion (diet, phosphate binders)
0 notes
Text
Case 33 Answer
History: abdominal pain. h/o prior abdominal surgery


Answer: Chronic Barium Peritonitis
I think this is a tough one especially without windowing/leveling but what or should I say where is the abnormality?


Lots of high density material right? But hopefully these images show you that this material is NOT within the GI tract.
While Calcium is a possibility, it's all over the abdomen and pelvis and although some may be intranodal or granulomatous, some is clearly intraperitoneal - surrounding the splenic flexure of the colon and linear collections in the upper pelvis

Barium sulfate is (or was <wink>) a commonly used hyperdense oral contrast agent used for intraluminal evaluation of the GI tract
Unfortunately, if leaked into the abdominal cavity it can induce an inflammatory response (even in the absence of leakage of fecal material).
Barium Peritonitis comes in two forms:
Acute - Barium causes a chemical induced inflammation. This can cause large volume exudative ascites actually resulting in severe hypovolemia requiring aggressive fluid resuscitation. This is in addition to any necessary antibiotic therapy for fecal/bacterial contamination.
Chronic - If not removed promptly, barium quickly clumps and adheres to parietal and visceral surfaces and becomes extremely difficult to remove. Fibrosis develops which can yield to repeated bowel obstructions.
Treatment is early laporatomy and extensive peritoneal washout.
Historic mortality rates are as high at 53%. However, despite our improved understanding of the underlying pathophysiology, more recent studies still show mortality rates in the 20-35% range, sometimes higher when there is associated bacterial peritonitis.
Take home message: It can be easy to see scattered hyperdense material throughout the abdomen and assume it is lymph node calcifications or retained barium within diverticula. I keep this case in mind to remind myself of the possibility and morbidty if it isn’t
1 note
·
View note
Photo

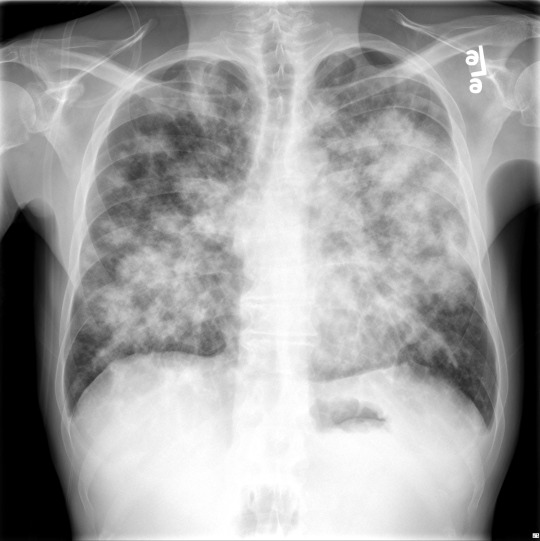
Season 8 Case 32
History: cough, shortness of breath, fever
Answer: Kaposi’s Sarcoma
KS is a low-mid grade mesenchymal tumor that involves blood/lymphatic vessels of the skin, lymph nodes, lungs, GI tract, etc. Not considered a true “sarcoma”. Believed related to human herpes virus type 8 (HHV8)
Comes in 4 variants:
Classic - generally limited to lower limb w/ purple dermal plaques
Iatrogenic - related to immunosuppression during organ transplantation
AIDS-related - HIV+ patients with CD4 <200 (considered an AIDS defining illness)
Endemic - men in equatorial Africa
Imaging:
XR -- linear interstitial nodules vs fluffy ill-defined nodules often in a peri-hilar to mid/lower lung predominance. +pleural effusion + adenopathy
CT - flame shaped nodular opacities in a symmetric/perihilar distribution often with surrounding glass-glass appearance +adneopathy (?high attentuation)
Nucs - can be helpful to differentiate from lymphoma
Th-201 is positive in both KS and lymphoma
Ga67 usually negative in KS but positive in lymphoma/infection
0 notes
Text
Season 8 Case 31
History: altered mental status. Weakness




Answer: Dyke-Davidoff-Masson Syndrome (DDMS)
Early infection/infarction/insult to one of the cerebral hemispheres -> hemi-cerebral atrophy + homolateral hypertrophy of the skull and sinuses (to fill the space)
CT shows large area of encephalomalacia of the R MCA distribution + R calvarial thickening and hyperpneumatization of the frontal sinuses
Bony findings are apparent on the X-ray, just a little more difficult to appreciate (in fact originally described on plain films I believe)
Clinically patients are young presenting with hemiparesis (contralateral of course), seizures and intellectual disability
1 note
·
View note
Text
Season 8 Case 30
History: foot pain

Answer: Intraosseous lipoma of the calcaneous
but I bet everyone knew that!
Classic appearance = a well circumscribed lytic lesion in the calcaneal body with central Ca++ (aka cockade sign)
Whats a cockade?
= a rosette - a knot of ribbon rolled into a badge.

So central density surrounded by well circumscribed low density area
Differential diagnosis (for calcaneous):
1) normal triangular lucency in this same area due to the normal stress related trabecular struts (more 🔺 in appearance) 2) Unicameral bone cyst - often very similar looking BUT NO central Calcification
Intraosseous Lipoma: - most common lipogenic bone tumor - majority in lower limbs - ~1/3 in calcaneous** - most common calcaneal bone lesion** -CT/MR can confirm internal fat -often incidental on XR but can present with heal pain
0 notes