Posts and reblogs that strike my fancy. I follow as @thingsthatscaremycat and I am also known as @randomstoryprompts.
Don't wanna be here? Send us removal request.
Text
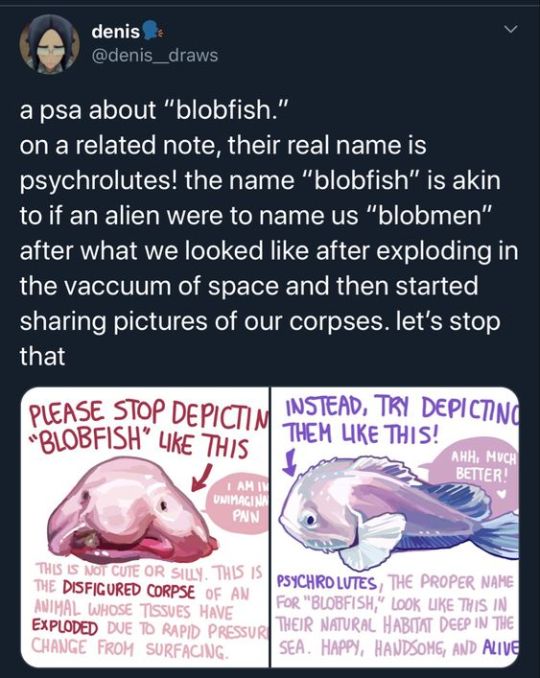
THANK YOU. JESUS CHRIST THIS DRIVES ME INSANE EVERY FUCKING TIME BE NICE TO THE PSYCHROLUTES GOD
30K notes
·
View notes
Text
One of my favorite hobbies is thinking about the fucked up implications of this fantasy world map my parents got me for christmas
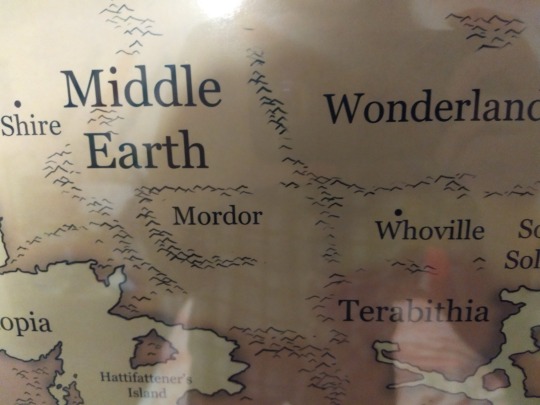
[Image ID: photo of a map. On the left side of the map is Middle Earth, with the Shire and Mordor labeled. To the direct right of Mordor is Whoville.]
73K notes
·
View notes
Text

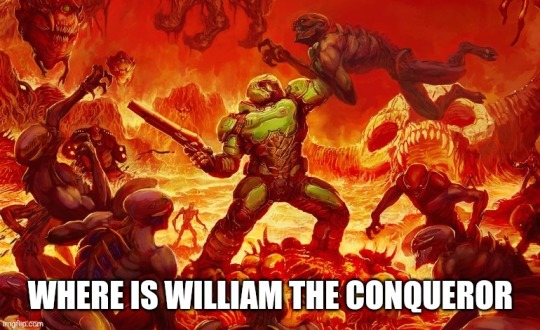
i found the image without the ugly instagram overlay!
6K notes
·
View notes
Text
59K notes
·
View notes
Text
so the thing about english is that people think it's so divorced from other germanic languages based on like. words. I've even heard people try to insist that english is a romance language. because of that whole messy business in 1066 with out-of-wedlock willy and his band of naughty normans. and now a good chunk of the vocabulary is french or whatever and they're prestigious so not using them makes you sound like a rube and this and that and the other
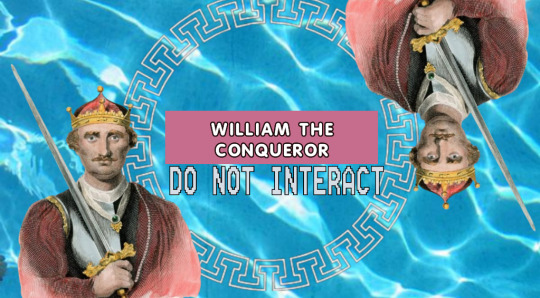
and yes william the conqueror will never be safe from me. I will have my revenge on him. he fucked up a perfectly good germanic language is what he did. this will be me in hell
but the thing is that most words in, say, german do have a one to one english equivalent. not all hope is lost, for those who still dare to see it. it's just that you 1066pilled normancels aren't looking in the right place
dog (en) ≠ der Hund (de) but der Hund (de) -> hound (en)
look with your special eyes. that one was easier. not all of them are this intuitive because of semantic narrowing and broadening and waltzing and hokey-pokeying and whatever else. I'll give you a few more
animal (en) ≠ das Tier (de)
aha! you think. I've got him on the ropes now.
but then
das Tier (de) -> deer (en)
nooooo!! you whine and cry in gay baby jail. the consonants are different!!! listen to me. listen, I say, putting both my hands on your shoulder. /t/and /d/ are the same sound. you just put your voice behind one of them.
nooooooooo!! you wail. deer are animals but not all animals are deer!!! listen to me. LISTEN. they used to be. animals used to be deer. that's just what we called them. it was a long time ago. it was a weird time in all our lives. it's okay.
let's try for a verb this time
to die (en) ≠ sterben (de) but sterben (de) -> to starve
same principle with the consonants, we're just changing a stop (where we completely stop the airflow and then let it through) for a fricative (where we still let some air go through. idk where it's going. maybe to its job or something.)
to starve used to mean generally to die, not just to die of malnourishment. we do that a lot. we take one word for a lot of things and make it mean one thing. or take one word for one thing and make it mean a lot of things. this is common and normal.
"okay but roland," you say, suddenly coming up with an argument. "what about tree? trees are super common. I don't think we'd fuck around too much with that. the german word is baum! what about THAT?"
"when did you learn german?" I ask, but then decide it isn't relevant right at this very moment. but fine.
tree (en) ≠ der Baum (de) but der Baum (de) -> beam (en)
beam??? you ask incredulously. beam???? BEAM?????? you continue with the same tone and cadence of captain holt from brooklyn 99.
yes. beam. like the evil beams from my eye I'm going to hit you with if you don't stop shouting.
but the vowels!!! you howl.
listen. listen to me. the vowels mean nothing. absolutely nothing. they're fluid like water. it got raised in english.
"WHAT DOES RAISED MEAN"
it doesn't matter right now. they were raised better than you, at least. stop shouting. open your eyes and see what god has given you. they're the same word.
"they're NOT the same word. they mean different things!"
we've been over this. they didn't used to. a beam was (and is) a long solid piece of wood. much like the long solid piece of wood I showed your mother last night.
FAQ:
Q: could english be some kind of germanic-romance hybrid?
A: do you become a sexy thing from the black lagoon just because you dressed up as one for halloween? english may have gotten a lot of vocabulary from norman french, but its history and syntax are distinctly germanic. that's what we base these things on.
Q: okay but what does it matter? this doesn't actually affect my day to day life
A: you come into my house? you come into my house, the house of an autistic man living in vienna austria and studying english linguistics and you ask me what does it matter? sit back down. I was going to let you go but now I have powerpoints to show you
Q: you're stupid and wrong and gay and a bad person
A: I know it's you, Willy
6K notes
·
View notes
Text
Some people say that there are no stupid questions, which is blatantly false. Of course there are stupid questions, and if you have one, you had better ask it, before you go and do make a stupider mistake. Stupid questions are more important than intelligent ones. I’m willing to bet more people die because of stupid mistakes than because of intelligent ones.
10K notes
·
View notes
Text
explaining executive dysfunction to people is so embarrassing yeah I have the be useless for days at a time disease
9K notes
·
View notes
Text
what ever happened to personality!!! i want decorative towels that arent boring!!! i want NOVELTY!! i want people to come over to my house and look at my trinkets and immediately think this lady is a wacko and also her stuff is haunted
168K notes
·
View notes
Text
i think one of the reasons i get mildly annoyed about worldbuilding threads that are 200 tweets of why you should care about where blue dye comes from in your world before saying someone is wearing blue is that so few of them go up to the second level of "and that should impact your characters somehow" - i don't care that blue dye comes from pressing berries that only grow in one kingdom a thousand miles away if people are casually wearing blue
35K notes
·
View notes
Text
you could never make blazing saddles today. movies take a really long time to film and it's already 11am on the west coast. also most actors and film staff would probably like to spend christmas eve with their families.
17K notes
·
View notes
Text






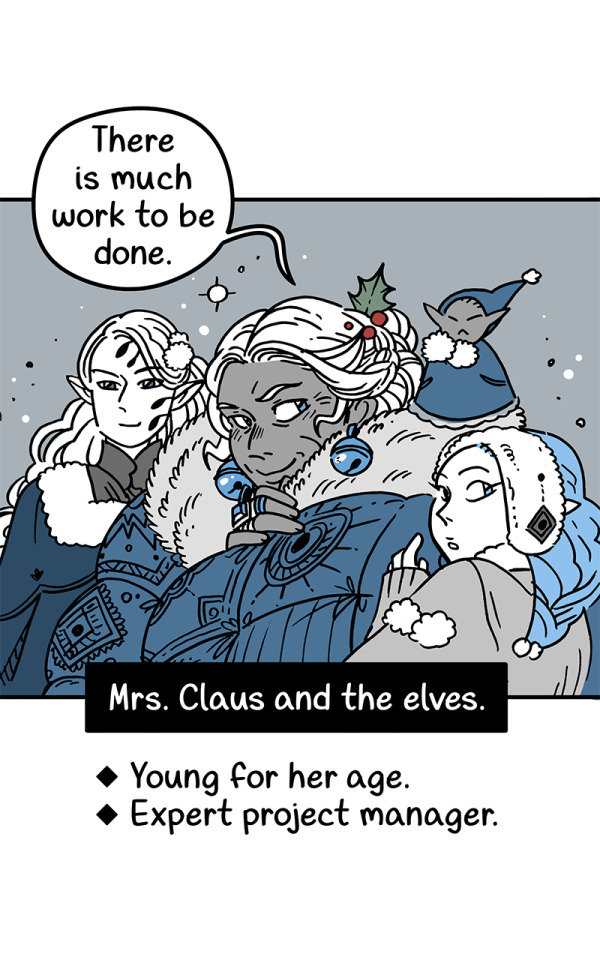
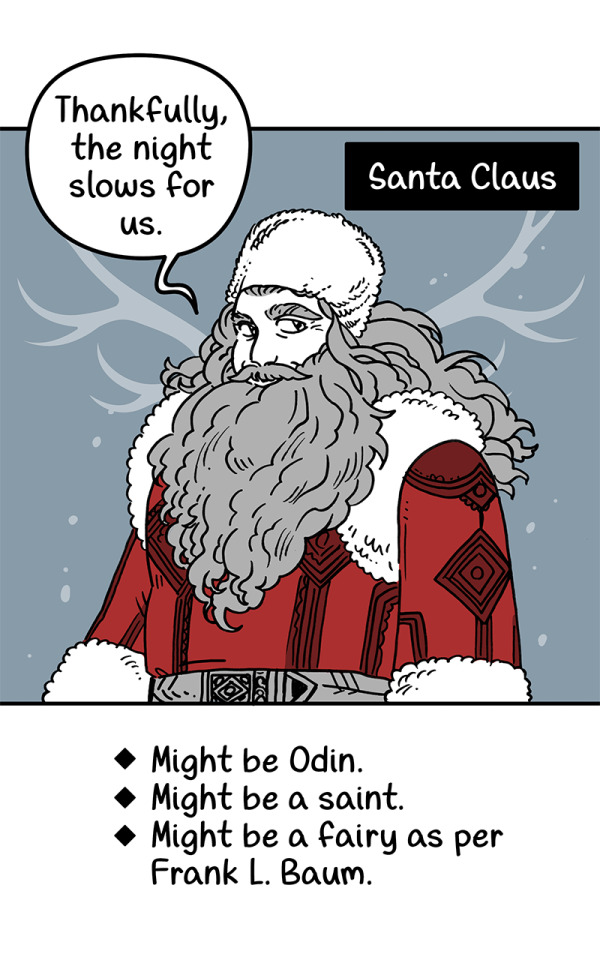

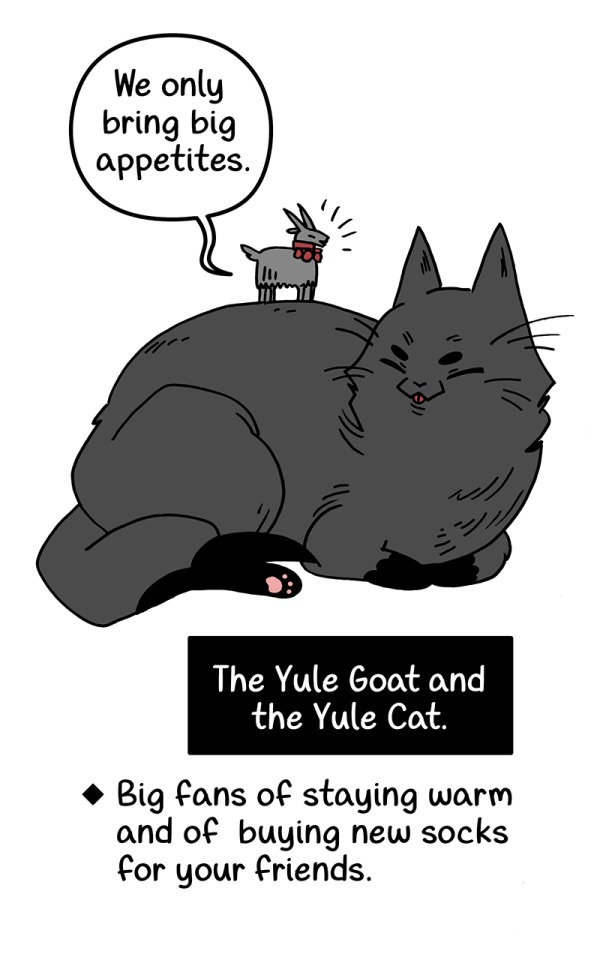




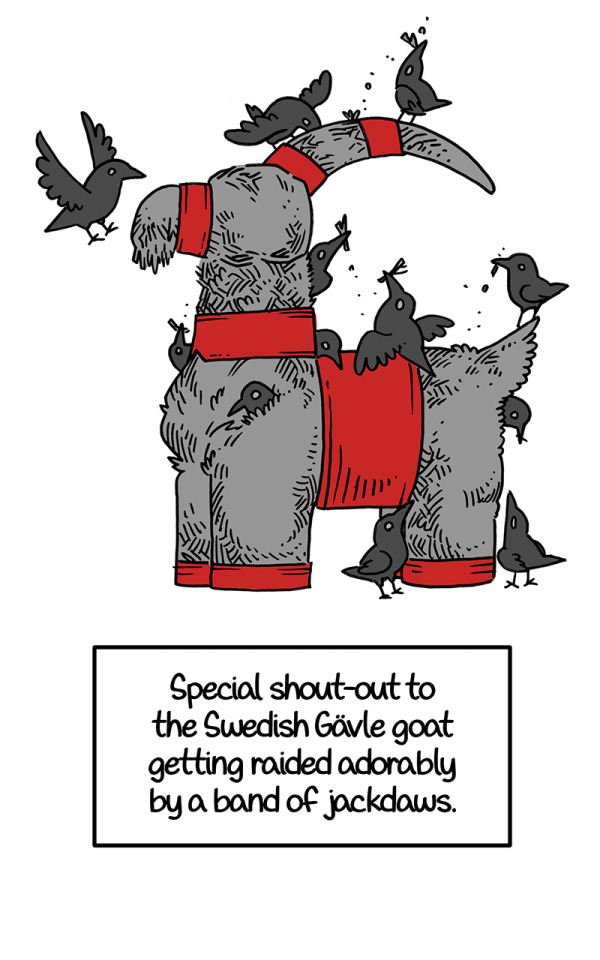
Happy Crowy Yule! It's a reall whose who of Yuletide.
64K notes
·
View notes
Text
"waow i really wanna be this persons friend.." continues to not talk to them but likes every single one of their tumblr posts i come along
809 notes
·
View notes
Text

I have tried for years to discover something, anything, about this card with no success.
25K notes
·
View notes
Text





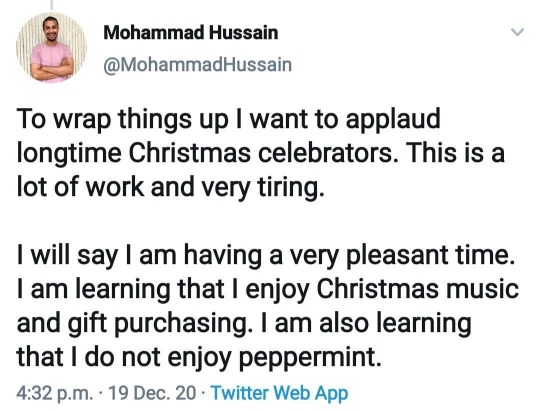
https://twitter.com/mohammadhussain/status/1340439172687998981?s=21
160K notes
·
View notes
Text

We're cycling back around to fake sick pet scams, nature is healing.
Also, obligatory

76 notes
·
View notes
Text
it’s so important to me I show you my birthday cake this year

the bakery forgot the s on shrimps so we added it on with a bit of apple
10K notes
·
View notes
