#writingaboutschizophrenia
Explore tagged Tumblr posts
Text
Schizophrenia: Putting It All Together

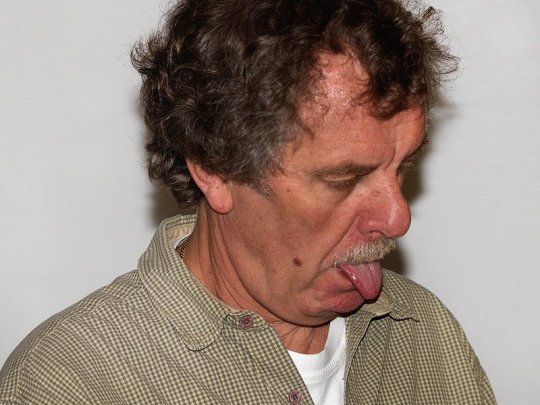
There is no cure for schizophrenia. But there is treatment. These treatments save lives, but the side effects can be hell. Last week we talked about what schizophrenia looks like when all of the symptoms are present. This week I’m going to talk about what a person with schizophrenia’s life looks like during the day-to-day. For a person with schizophrenia, taking medications every day is of utmost importance. The delusions from schizophrenia can be traced back to an over-release of the chemical dopamine in the brain. Anti-psychotics merely plug the leaky dopamine pipe. Once the leaking pipe is stopped, however, the person starts feeling much better and may decide they do not need their medications after all. Bad idea. The hallucinations and delusions come back with a vengeance (Lewis). But there’s another problem with the dopamine suppressing drugs: they don’t target just the areas where the delusions originate, but also the rest of the brain. And what’s another disease associated with low dopamine? Parkinson’s Disease. A person taking these anti-psychotic medications can not develop actual Parkinson’s Disease from the drugs, but may have pseudoparkinsonism with similar symptoms such as a hand tremor, issues with balance, and difficulty walking. They develop a shuffling gait, mask-like face (a decrease in ability to show expressions on their face due to paralyzed facial muscles), muscle stiffness, drooling, slowness in starting movement. The person taking the medications may experience dystonic reactions where spasms occur in discrete muscle groups such as the eyes and neck (the patient will have chronically raised shoulders like a tortoise shell). They might have a protruding tongue, difficulty swallowing, and spasms around their throat which, if bad enough, might lead to a compromised airway. This is obviously terrifying. Most of these side effects develop shortly after starting or increasing the dose of medications. A more long-term side effect, however, is tardive dyskinesia. It’s characterized by “abnormal, involuntary movements such as lip smacking, tongue protusion, chewing, blinking, grimacing, and strange movements of the limbs and feet” (Videbeck). Keep in mind the person is fully aware of the strange movements and are probably embarrassed. This bizarre, uncontrollable behavior may lead to further social isolation. Is it really a wonder they want to come off their meds?
And in all this, the anti-psychotics are only treating half of the problem. In the previous post, I mentioned positive and negative symptoms. Positive symptoms are those symptoms that are added experiences to a ‘normal person’: hallucinations, delusions, etc. Negative symptoms are things such as depression, withdrawal, loss of joy, etc. Anti-psychotics do not treat the negative symptoms. The struggle of day-to-day living for a person with schizophrenia is enormous. Because of this, pharmacology is just one part of the treatment. Individual and group therapy is key. There, things such as family dilemmas and medication management can be addressed. Clients can undergo social skills training where complex social behavior is broken down into easier to manage parts. Some very creative people have put together environmental supports such as signs, calendars, hygiene supplies, and pill containers to cue clients to perform various tasks. If a schizophrenic person has a good support system, they have a better shot than most. Family education and therapy are known to diminish the negative effects of schizophrenia and reduce the relapse rate. Unfortunately, good support systems are hard to build and even harder to sustain. It’s hard to take care of someone who believes everyone is out to get them. Or to be patient with someone who offers very little in return: no smiles, flat expressions, lack of joy. Unfortunately, this is a part of the therapy that is forgotten about the most. So take all that together for a moment and imagine life as someone with schizophrenia or a caregiver of someone with this disease. I’m going to give you a quick example from the perspective of a writer: Hunter moved into the apartment down the hall from his parents. He’s super excited to be independent and have a place of his own. For the past several years since his diagnosis, Hunter’s routine has been the same: get up, get dressed, brush teeth, etc. all in the same order every day. Unfortunately, just as he is about to take his medications, someone knocks on the door. It’s the maintenance guy just stopping by to let Hunter know the power might go out for a few minutes later that day. But it’s enough to distract Hunter and he forgets the meds. He goes on, grabs his bus pass, and goes to work at the deli. While he’s at the bus stop, people keep staring at Hunter. He tries to ignore it, as he leans back in his seat smacking his lips and wipes a bit of drool from the corner of his mouth. Hunter gets to work on time, but finds Ricky working that day. Ricky laughs aloud at Hunter’s slippers. Apparently, he forgot to change his shoes too. All day, Ricky mocks Hunter’s slow movements, his shaky hands—just whatever he can to get under Hunter’s skin. But that’s not the worst of it. Hunter is used to Ricky, but the customers start whispering about him behind his back too. And then there’s one guy that’s watching Hunter just a little too closely. Later on that day, Hunter sees the guy across the street, watching him through the window. Hunter takes the bus home, and all the people are watching him now, talking about him. He sees the guys again outside the bus window. Now Hunter knows he’s being followed.

When Hunter gets home, he locks the door and goes to kitchen. He grabs a meat hammer and sits by the window where he’s sure he hears the man outside, talking about him. The man says he’s going to get Hunter. He’s going to burn the apartment complex down and kill him and his parents. Hunter runs out of the apartment, not wanting to be trapped inside a burning building. Later, his mom stops by and can’t find Hunter although his coat and wallet are inside. She searches the apartment complex and finally finds Hunter barefooted and hiding behind a dumpster. By now the voices have grown too loud. Hunter doesn’t recognize his mother and charges her with the meat hammer. A neighbor stops Hunter and restrains him until the ambulance can arrive, but Hunter is institutionalized until they can get his delusions under control. Unfortunately, this is the third hospitalization this year, and Hunter loses his job at the deli. Without the extra income, he has to move back into his parent’s apartment and start over. All because the maintenance guy stopped by. People with schizophrenia are just that: people. I hope this information has helped you gain a better understanding of the condition so that we can portray those effected by mental illness accurately. Sources: Psychiatric-Mental Health Nursing, by Sheila L. Videbeck, fifth ed., Wolters Kluwer/Lippincott Williams & Wilkins, 2011. Lewis, J. (2011, March 6). The Future of Schizophrenia. Dr. Jack Lewis. http://www.drjack.co.uk/the-future-of-schizophrenia-by-dr-jack-lewis
#writersblog#writingadvice#writingtips#writer#write#author#authorblog#authortips#authoradvice#schizophrenia#mentalhealth#mentalillness#mentalhealthawareness#writingaboutmentalhealth#writingaboutschizophrenia#gettingitright
12 notes
·
View notes