#uterine polyp removal
Explore tagged Tumblr posts
Text
Uterine Polyp Treatment and Hysteroscopy | Dr. Neha Lalla

Uterine Polyps are growth attached to the inner wall of the uterus that extend into the uterine cavity. Overgrowth of cells in the lining of the uterus leads to the formation of uterine polyps. Mostly noncancerous, although some can be cancerous or can eventually turn into cancer.
For more information, consult Dr. Neha Lalla one of the best Gynaecologist in Dubai or you can contact us on +971 4212 2599.
#gynaecologist in dubai#best indian gynaecologist in dubai#gynecologist#dr. neha lalla#best indian gynaecologist in dubai.#health & fitness#hysteroscopy#polypectomy#uterine polyp removal#Uterine Polyp
0 notes
Text

Explore uterine polyp removal surgery at Audubon Fertility. Dive into comprehensive details on the procedure, benefits, and understand the speed of polyp regrowth. Make informed decisions about your reproductive health.
0 notes
Text
0 notes
Text
Hysterometer

Due to anatomical differences between different people, in many cases gynecologists need to measure the uterine depth. A hysterometer is a device used for this purpose. Although previously reusable hysterometers were more widely used, nowadays, due to higher hygienic standards and to prevent the transmission of contagious diseases, disposable hysterometers are more in demand.
0 notes
Text
Symptoms and Causes of Uterine Polyps
Uterine polyps are growths in the lining of the uterus. They are usually benign, but can sometimes be cancerous.

The most common symptom of uterine polyps is abnormal vaginal bleeding. Other symptoms may include pelvic pain, infertility, and heavy menstrual bleeding.
The exact cause of uterine polyps is unknown, but they are thought to be caused by a combination of factors, including
Hormonal imbalances
Inflammation
Genetic mutations
There is no specific treatment for uterine polyps, but they can often be removed with surgery or medication.
Here are some of the most common symptoms of uterine polyps:
Abnormal vaginal bleeding, such as heavy menstrual bleeding, bleeding between periods, or bleeding after menopause
Pelvic pain
Infertility
Heavy menstrual bleeding
If you experience any of these symptoms, it is important to see a doctor to get a diagnosis and treatment.
#Uterine Polyps#endometrial polyp#causes of uterine polyps#symptoms of uterine polyps#uterine polyp removal#endometrial polyp treatment#how to prevent polyps in uterus
0 notes
Text
Hey y’all! just a little life update from me and I promise after that we will continue to your regularly scheduled hot fat girl content
(for those who were not aware, I’ve been having this on and off spotting/bleeding for like a year now and today I finally had answers.)
I went to the Gyno today after getting an internal screening to find out and I have to get 2 procedures done on Tuesday. The first one they have to do is thin out my uterine lining. I was told that it’s so thick that if it doesn’t get treated in the long run it could cause uterine cancer.
The second procedure is they have to look for a polyp and if they do find one, they will proceed with removing it. It’s really nothing major but I’ll be honest I’m scared to death because I hate this kinda stuff and the Gyno but I know I gotta get it done.
Anyway that was probably too much info sorry LOL but I just wanted to let yall know what’s going on, and if u could please send good vibes that it goes well it would be greatly appreciated, love u 💙
19 notes
·
View notes
Note
Hey Spider.
Sending some love and sympathy your way. I had a similar health issue a couple of years ago, although I had a polyp rather than fibroids.
They didn't offer me the full womb-yeet option (although peri menopausal i havent had kids so they think i should keep my options open?), but I did get me uterine lining abraded at the same time as the polyp was removed, and my periods have been much better, and mega-clot free, since.
Hope everything goes well for you xxx
Thanks. :) I was offered other options, but none of the options I've so far been offered were acceptable to me. (lol no I do not want hormonal birth control???? why do you think i would want to put more estrogen in my system, dude, you write my T prescription?)
I'll talk to a surgeon towards the end of December.
15 notes
·
View notes
Text
Most common surgeries done by gynecologist surgeon
Gynecology surgery comprises any surgical procedure that involves the organs and structure of the female pelvic region: the ovaries, uterus, fallopian tubes, cervix, vulva, and vagina. There are several reasons why a woman might need to go through gynecology surgery. She might need treatment for a condition such as fibroids (benign tumors), endometriosis, cancer, ovarian cysts, pelvic inflammatory disease, chronic pelvic pain, abnormal bleeding or uterine prolapse. Gynecology surgery can also be used as permanent birth control.
The most common surgeries done by gynecologist surgeon are as follows:
Cervical Cryosurgery
Abnormal cervical cells are at times discovered during a routine Pap smear. Abnormal cells do not always indicate cancer, but your healthcare provider will likely want to do some follow-up tests or procedures. One procedure they might recommend is cervical cryosurgery. This procedure is a highly effective gynecological treatment that freezes a section of the cervix. Cryosurgery destroys these cells to stop them from developing into cancer.
Hysteroscopy
Hysteroscopy is a process that your healthcare provider may use to diagnose or treat uterine issues. This procedure might be used to:
Locate an intrauterine device
Remove adhesions (scar tissue)
Determine the cause of repeated miscarriage
During this procedure, a healthcare professional inserts a hysteroscope, a lighted, thin, telescope-like instrument, into your uterus through the vagina. Then, it sends pictures of your uterus to a screen for further test.
Pelvic Laparoscopy
Laparoscopy is a surgical procedure usually performed under general anesthesia. But it can be performed with other types of anesthesia while you are awake. It is used for:
Gallbladder removal
Tubal ligation (tying the fallopian tubes for permanent birth control)
Treating endometriosis and uterine fibroids
Hernia repair
The typical pelvic laparoscopy involves a small incision in the belly button or lower abdomen. A surgeon then pumps carbon dioxide into your abdomen to help them see your organs easily.
Dilation and Curettage
It is one of the most common gynecological procedures. During this process, a healthcare provider removes a portion of your uterine lining with a suction device or a sharp curette. The procedure can diagnose uterine conditions, including:
Uterine cancer
Endometrial hyperplasia (an abnormally thick uterine lining)
Uterine polyps (overgrowth of tissue in the uterine lining)
In addition, D&Cs are commonly used for miscarriage, abortion procedures, molar pregnancy, and retained placenta.
Common gynecological procedures by gynecologist surgeon include colposcopy, cervical cryosurgery, D&C, LEEP, hysteroscopy, and pelvic laparoscopy. Most of these procedures can help healthcare providers get a better look at the cervix, uterus, and vagina and take samples for a biopsy. Some of them can also treat specific conditions.
Understandably, you might have concerns about any process your healthcare provider or gynecologist recommends. Learning as much as you can is a good idea. In addition, it is essential to ask your doctor any questions you might have. Finally, do not forget to tell them if you may be pregnant, even though they usually do a test to check first.
3 notes
·
View notes
Text
I have had to talk my doctor multiple times about severe bleeding - turns out each time it was a uterine polyp. Symptom management (aka stop the bleeding so I can function) needs a prescription and each time I ended up in surgery to remove the polyps.
There's a post going around Tumblr about how if you're post-menopausal and have bleeding, you should get it checked by your doctor. I brought some minor bleeding I'd had up in a doctor visit earlier this year, prompted by that post, and this week, after a biopsy, I found out I have cancer. It's early stage and the survival odds at 5 years are 99%. I have an oncologist appointment and we may have caught it early enough that surgery alone will be sufficient treatment (no radiation/chemo).
So that post may have saved my life and it may have made my treatment a lot easier too.
If you get into menopause and then start bleeding again, really, get your reproductive innards checked out. The life you save may be your own.
62K notes
·
View notes
Text
Types Of Abnormal Uterine Bleeding
During a woman’s monthly menstrual cycle, the mucous membranes that line her uterus are shed. The lining, consisting of the tissues, mucus, and blood, exits your body through the vagina in the form of menstrual blood. This should normally last between 3 and 7 days. If the menstrual bleeding occurs at unpredictable times, amounts, and duration, this could indicate Abnormal Uterine Bleeding (AUB). It’s important to schedule a visit to the gynecologist in Thane West to get evaluated for abnormal bleeding, as it can indicate an underlying health issue.
Types of Abnormal Uterine Bleeding
1) Menorrhagia:
The most common type of AUB is menorrhagia. If you experience heavy bleeding that lasts longer than 7 days, results in significant blood loss (above 80 mL per menstrual cycle), and occurs with large blood clots, you could have menorrhagia. The condition can lead to anemia. Uterine fibroids, polyps, and hormonal disorders can cause menorrhagia.
2) Metrorrhagia:
Metrorrhagia refers to abnormal uterine bleeding that occurs outside your menstrual cycle. It could be spotting in between periods or heavy bleeding. Sometimes, bleeding that occurs a few days after menstruation is mistaken for another menstrual cycle in the same month. Polyps, endometriosis, and hormonal fluctuations are the common causes, but the condition could also indicate a more serious issue, like cancer of the reproductive organ.
3) Polymenorrhea:
You may have normal blood flow during your menstrual cycle, but the interval between your menstrual cycle could be shorter than normal. In women with polymenorrhea, the menstrual cycle is shorter than 21 days, which means you might get periods twice a month.
4) Oligomenorrhea:
Some women may have menstrual cycles longer than 35 days. You might go two months or more without having a period. The condition is called oligomenorrhea and is mostly caused by PCOS or thyroid disorders.
Causes and Risk Factors
a) PCOS:
Polycystic Ovarian Syndrome can be the cause of abnormal uterine bleeding or infrequent periods. It’s a hormonal disorder that may lead to a wide range of reproductive and other health issues in women.
b) Uterine Fibroids and Polyps:
These are the non-cancerous growths in your uterus, causing prolonged menstruation and heavy bleeding. You might also experience spotting between periods.
c) Endometriosis:
The tissues lining your uterus can grow outside the uterus (mainly within the pelvic region), causing heavy bleeding and painful cramps.
d) Cancer:
Although less common, abnormal uterine bleeding, specifically if it happens after menopause, can indicate malignancy.
Treatment Options
See a doctor if you have heavy bleeding (soaking a pad every hour or passing blood clots), prolonged bleeding, or infrequent menstrual cycle. AUB treatment in Thane West can include medication, home remedies, and invasive treatment options.
Usually, mild cases of abnormal uterine bleeding can be fixed with lifestyle adjustments, like practicing stress-reducing exercises, controlling your weight, living an active lifestyle, and eating a balanced diet. A gynecologist may recommend hormonal treatment, like birth control pills or progesterone therapy, to control heavy bleeding. You may consider minimally invasive treatments, like uterine fibroids embolization and endometrial ablation. If nothing works, your last resort is hysterectomy — uterus removal surgery that ends menstruation and makes pregnancy impossible.
0 notes
Text
Is the removal of a retained IUD a complex procedure?
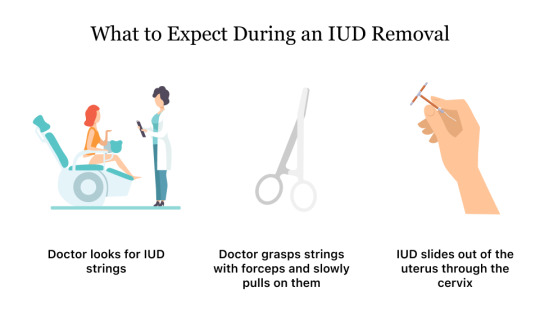
The removal of a retained Intrauterine Device (IUD) is typically a straightforward and routine procedure. However, the complexity can vary based on several factors:
1- Location of the IUD:
If the IUD is easily visible and located within the cervix, the removal is usually simple. However, if it has migrated or embedded in the uterine wall, extraction may be more challenging.
2- Time Since Insertion:
The longer the IUD has been in place, the more likely it is to become embedded. This can make removal more complex, as the device may become surrounded by tissue over time.
3- Experience of the Healthcare Provider:
A skilled and experienced healthcare provider, such as a gynecologist, is better equipped to handle challenging cases. They can employ various techniques to safely retrieve the IUD.
4- Patient Comfort:
The procedure is generally well-tolerated, and healthcare providers may use local anesthesia or recommend pain relief measures to enhance patient comfort during removal.
In most cases, the removal of a retained IUD is a quick office-based procedure. The healthcare provider may use forceps or special instruments to grasp the IUD strings and gently guide it out. If the strings are not visible, imaging studies such as ultrasound may be used to locate the device.
It's crucial for individuals experiencing difficulty with IUD removal to seek prompt medical attention. Delayed removal can lead to complications, such as infection or perforation. Healthcare providers are experienced in managing such situations and will take necessary steps to ensure a safe and effective removal process.
Experience comprehensive women's health care with Dr. Neha Lalla, your trusted Uterine Polyp removal in Dubai . Book your appointment today for expert guidance and personalized care.
#gynaecologist in dubai#dr. neha lalla#best indian gynaecologist in dubai#gynecologist#Uterine Polyp removal in Dubai#IUD removal#gynecological care
2 notes
·
View notes
Text

Explore Audubon Fertility's advanced and safe options for uterine polyp removal surgery. Learn how we restore women's health and improve fertility outcomes. Get comprehensive care with us today!
0 notes
Text

Hysteroscopy is a minimally invasive procedure that allows doctors to diagnose and treat uterine conditions such as abnormal bleeding, fibroids, polyps, and adhesions. It helps identify causes of infertility or recurrent miscarriage and can also be used for treatment, including removing growths and correcting abnormalities without open surgery.
Performed on an outpatient basis, hysteroscopy ensures minimal discomfort and faster recovery. If you have unexplained gynecological symptoms, consult our gyno surgeons in Mukundapur at Long Life Speciality Clinic for expert care and guidance.
#gyno surgeons in mukundapur#diagnostic centre in mukundapur#orthopedic doctors in mukundapur#ENT specialists in Mukundapur
0 notes
Text
What You Need to Know About Recurrent Miscarriages

Pregnancy is a journey filled with hope and anticipation. However, for some women, recurrent miscarriages can turn this joyful experience into one of distress and uncertainty. If you have experienced multiple pregnancy losses, you may be searching for answers. Understanding the causes, diagnosis, and potential treatment options can empower you to take the next steps toward a healthy pregnancy.
Meaning of Recurrent Miscarriages
Recurrent miscarriages, also known as recurrent pregnancy loss (RPL), refer to the loss of two or more consecutive pregnancies before 20 weeks of gestation. While miscarriage is common, affecting about 10–20% of pregnancies, recurrent miscarriages occur in about 1–2% of women.
Possible Causes of Recurrent Miscarriages
Several factors can contribute to recurrent miscarriages:
1. Genetic Abnormalities: Chromosomal abnormalities in the embryo, often due to genetic issues from the parents, can lead to miscarriage.
2. Hormonal Imbalances: Conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, or insufficient progesterone can affect pregnancy viability.
3. Uterine Abnormalities: Structural abnormalities such as fibroids, a septate uterus, or scar tissue can interfere with implantation and fetal development.
4. Blood Clotting Disorders: Conditions like antiphospholipid syndrome (APS) or thrombophilia can increase the risk of pregnancy loss due to clot formation in the placenta.
5. Autoimmune Disorders: The immune system may mistakenly attack the embryo, leading to miscarriage.
6. Infections: Some bacterial or viral infections can compromise pregnancy health.
7. Lifestyle Factors: Smoking, excessive alcohol intake, obesity, and unmanaged stress may contribute to pregnancy loss.
8. Unexplained Causes: In some cases, despite extensive testing, no specific cause is identified.
Diagnosing Recurrent Miscarriages
If you have had two or more miscarriages, a thorough medical evaluation is recommended. Tests may include:
Genetic Testing: Karyotyping of both parents and testing fetal tissue from previous losses.
Hormonal Assessments: Checking thyroid function, progesterone levels, and glucose metabolism.
Uterine Imaging: Ultrasound, hysteroscopy, or MRI to detect structural abnormalities.
Blood Clotting Tests: Screening for APS and other clotting disorders.
Immunological Testing: Evaluating immune system responses that may impact pregnancy.
Treatment Options for Recurrent Miscarriages
Treatment depends on the underlying cause:
Genetic Counseling: If chromosomal abnormalities are detected, options like preimplantation genetic testing (PGT) during IVF can help.
Hormonal Support: Progesterone supplementation, thyroid medication, or insulin management for PCOS-related issues.
Surgical Corrections: Procedures like hysteroscopic surgery to remove fibroids, polyps, or uterine septum.
Blood Thinners: Medications like aspirin or heparin for women with clotting disorders.
Lifestyle Modifications: Maintaining a healthy diet, managing stress, quitting smoking, and avoiding alcohol.
Emotional and Psychological Support
Experiencing multiple miscarriages can take an emotional toll. Seeking support through:
Counseling or therapy to process grief.
Support groups where women share similar experiences.
Open communication with your gynecologist and your partner.
Consult a Gynec to Avoid Miscarriages in the Future
The good news is that many women who experience recurrent miscarriages go on to have successful pregnancies with the right diagnosis and treatment. Consulting a best gynecologist or fertility specialist in Mumbai can help you create a personalized plan for a healthy pregnancy.
If you have experienced multiple pregnancy losses, you are not alone. With the right medical care, emotional support, and treatment options, you can approach this journey with hope and strength. Advances in reproductive medicine, personalized care, and lifestyle adjustments are improving outcomes, helping many women embrace the joy of motherhood. Essential Tips for a Healthy Pregnancy Journey can provide valuable insights to support you every step of the way.
0 notes
Text
Your Guide to the Best Hysterectomy Surgeon and Hysteroscopy Doctors in Surat

When it comes to women's health, timely and expert medical care is essential. Whether you need a hysterectomy or a hysteroscopy, choosing the right specialist ensures safe and effective treatment. If you’re looking for the best hysterectomy surgeon and hysteroscopy doctor in Surat, this guide will help you understand the procedures, their benefits, and where to find top-rated medical care.
What is a Hysterectomy?
A hysterectomy is a surgical procedure to remove the uterus, often recommended for conditions such as:
✔ Uterine fibroids ✔ Endometriosis ✔ Chronic pelvic pain ✔ Uterine cancer ✔ Heavy or abnormal bleeding
Types of Hysterectomy Procedures:
🔹 Total Hysterectomy – Removal of the uterus and cervix. 🔹 Partial (Subtotal) Hysterectomy – Removal of the uterus while keeping the cervix intact. 🔹 Radical Hysterectomy – Removal of the uterus, cervix, parts of the vagina, and nearby tissues (often for cancer treatment). 🔹 Minimally Invasive Hysterectomy – Laparoscopic or robotic-assisted surgery for faster recovery and minimal scarring.
What is a Hysteroscopy?
A hysteroscopy is a minimally invasive procedure that allows doctors to examine and treat the uterus using a thin, lighted tube. It is commonly performed for:
✔ Diagnosing and treating abnormal uterine bleeding ✔ Removing fibroids or polyps ✔ Evaluating infertility issues ✔ Removing adhesions or scar tissue
Finding the Best Hysterectomy & Hysteroscopy Doctors in Surat
Choosing an experienced gynecologist is crucial for safe and effective treatment. The best hysterectomy surgeons and hysteroscopy doctors in Surat offer:
✔ Expert Surgical Skills – Years of experience in performing successful procedures. ✔ Advanced Medical Technology – Minimally invasive techniques for quick recovery. ✔ Comprehensive Women’s Healthcare – From diagnosis to post-surgery support. ✔ Personalized Treatment Plans – Tailored care based on individual health conditions.
Book a Consultation with the Best Specialists in Surat
If you're facing gynecological concerns and need expert advice, consulting the top hysterectomy surgeons and hysteroscopy doctors in Surat can help you make the right choice for your health.
📞 Schedule an Appointment Today for Advanced Women’s Healthcare!
website:- https://harshhospital.in/contact-us/
#harsh hospital#Best Hysterectomy & Hysteroscopy Doctors in Surat#Hysterectomy#Hysteroscopy Doctors in Surat
0 notes
Text
Gynecologist in Jaipur: Comprehensive Women’s Healthcare with Dr. Nisha S Mangal

When it comes to women’s health, choosing the right gynecologist is crucial. Jaipur, the Pink City, is home to some of the most experienced and skilled gynecologists who provide top-notch healthcare services. Among them, Dr. Nisha S Mangal, a Gynecologist and Infertility Specialist in Malviya Nagar, Jaipur, stands out for her expertise, compassionate care, and commitment to women’s health.
Why Choose a Gynecologist in Jaipur?
Jaipur has emerged as a hub for advanced medical treatments, including gynecology and infertility care. With modern hospitals and specialized clinics, the city offers a range of services tailored to meet the diverse healthcare needs of women.
Who is Dr. Nisha S Mangal?
Dr. Nisha S Mangal is a renowned Gynecologist and Infertility Specialist in Malviya Nagar, Jaipur, known for her dedication and vast experience in women’s healthcare. With years of practice, she has helped countless women with issues related to pregnancy, infertility, gynecological disorders, and reproductive health. Her personalized approach ensures that every patient receives the best possible care.
Services Offered by Dr. Nisha S Mangal
Dr. Nisha S Mangal provides comprehensive gynecological and obstetric services, including:
1. Pregnancy and Maternity Care
Prenatal and postnatal care
High-risk pregnancy management
Normal and cesarean deliveries
2. Infertility Treatment
IVF (In-Vitro Fertilization)
IUI (Intrauterine Insemination)
Hormonal therapy for infertility
PCOS and endometriosis management
3. Gynecological Treatments
Menstrual disorders (irregular periods, heavy bleeding)
Fibroids, ovarian cysts, and polyps treatment
Menopause management
4. Laparoscopic and Hysteroscopic Surgeries
Minimally invasive gynecological surgeries
Laparoscopic removal of fibroids and cysts
Hysteroscopy for diagnosing uterine abnormalities
5. Preventive Healthcare & Wellness
Cervical cancer screening (Pap smear, HPV testing)
Breast health screenings and examinations
Family planning and contraception guidance
Why Choose Dr. Nisha S Mangal?
Extensive Experience: Years of expertise in gynecology and infertility treatments
Advanced Technology: Utilization of the latest medical techniques and equipment
Patient-Centric Approach: Individualized treatment plans tailored to each patient
Compassionate Care: A warm and understanding approach to patient concerns
Where to Find Dr. Nisha S Mangal in Jaipur?
Dr. Nisha S Mangal practices at a well-equipped facility in Malviya Nagar, Jaipur, ensuring patients receive high-quality medical care in a comfortable environment. Whether you need regular gynecological check-ups, infertility treatment, or expert pregnancy care, she is a trusted name in the city.
Final Thoughts
Women’s health is a priority, and consulting an experienced gynecologist like Dr. Nisha S Mangal | Gynecologist and Infertility Specialist in Malviya Nagar, Jaipur ensures that you receive the best medical care possible. With her expertise and patient-first approach, she continues to be a leading name in women’s healthcare in Jaipur.
For consultations and appointments, contact Dr. Nisha S Mangal today and take a step toward better health and well-being!
0 notes