#trichodynia
Explore tagged Tumblr posts
Photo

Get the right hair treatment for Trichodynia. It is a painful sensation in the skin of the scalp or the hair without an underlying cutaneous disease.
0 notes
Photo

Ladies It is a big myth that dirty hair grows faster than clean hair. Having dirty hair can cause bacteria growth and scalp irritation. The bacteria growth can cause scalp diseases which can in turn cause your hair to fall out or not grow properly. . These are some scalp conditions you can get if you don't wash your hair often enough: * Trichodynia (Scalp Dysesthesia): A painful sensation on the skin of the scalp or the hair itself and becomes more intense when hairs are touched. . Malassezia (Yeast Overgrowth): This is a monophyletic genus of fungi found on the skin and associated with a variety of conditions, including dandruff, atopic eczema/dermatitis, seborrheic dermatitis, and folliculitis. . Continue to read more by following the link below: 🔗 https://www.byrdie.com/does-dirty-hair-grow-faster-than-clean-hair-400053#does-dirty-hair-grow-faster-than-clean-hair (at West Park, Hollywood, Florida) https://www.instagram.com/p/CTndocsL9en/?utm_medium=tumblr
1 note
·
View note
Photo
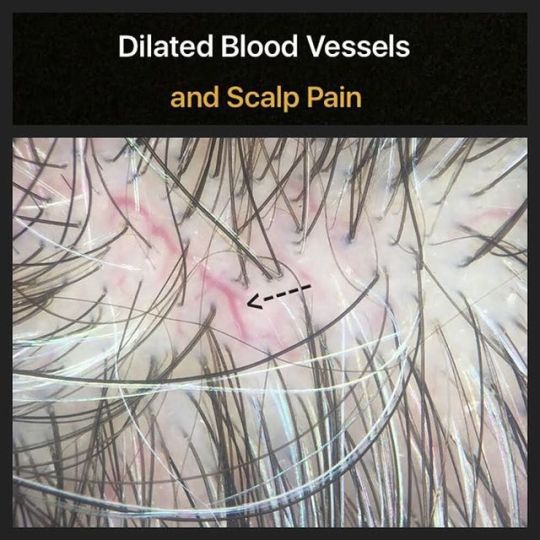
Trichodynia refers to hair pain. There are many potential causes. A study by Willimann and Trueb (in 2002) showed that dilated blood vessels seen in the scalp were strongly associated with trichodynia. Reference Willimann B, et al. Hair pain (trichodynia): frequency and relationship to hair loss and patient gender. Dermatology. 2002. #hair #trichodynia
0 notes
Link
Trichodynia Nedir? | Bilgi almak için tıklayın: https://ift.tt/2B8TmR5
0 notes
Photo

Get the right hair treatment for Trichodynia. It is a painful sensation in the skin of the scalp or the hair without an underlying cutaneous disease.
0 notes
Text
Bimatoprost for Make Balding
BIMATOPROST FOR ANDROGENETIC ALOPECIA: AN INTENSELY RESEARCHED AREA
November 22, 2017
Bimatoprost for Male Balding
Bimatoprost is a prostaglandin F2 alpha analogue that stimulates hair growth. Bimatoprost at 0.03 % is a well known eyelash growth stimulatory compound and marketed under the name Latisse.
Bimatoprost has been studied for use in androgenetic alopecia. At low concentrations, it is not particularly effective. Allergan is currently studying higher concentrations (1 and 3%). Data released by Allergan and available to the public online suggest that these higher concentrations may be beneficial in treating hair loss. This is an exciting area to watch out for in the near future.
The graph shows how bimatoprost compares to minoxidil in these Allergan led studies. In their preliminary results, higher concentrations of bimatoprost was similarly or even slightly more effective that minoxidil (the gold standard FDA approved topical treatment for androgenetic alopecia).
SHARE THIS
No Comments
SCARRING ALOPECIA: LOSS OF THE FOLLICULAR OPENING IS A HALLMARK
November 22, 2017
Scarring Alopecias Cause Scarring
Scarring alopecias are hair loss conditions that are associated with the development of permanent hair loss. There are dozens of different types of scarring alopecia. Some scarring alopecias itch. Some don't. Some are associated with increased shedding. Some aren't. Some are red. Some aren't. Some bleed. Most don't.
However what is common to all scarring alopecias is the disappearance of the follicular opening or "pore." The development of scar tissue beneath the skin leads to the destruction of the follicular pore opening.
The arrows point to an area of scarring in a subtle early scarring alopecia
SHARE THIS
No Comments
DENSITY CHANGES IN CTE VS AGA OVER TIME
November 22, 2017
Chronic Telogen Effluvium: How does density change over time?
Chronic Telogen Effluvium (CTE) and Androgenetic alopecia (AGA) are both commonly encountered diagnoses in women age 40-70 years. They are however, very different conditions.
AGA: Androgenetic Alopecia
AGA presents with hair thinning and sometimes increased daily shedding as well. The loss of hair is sometimes just frontal in location or the crown but can be diffuse (all over). A key to the diagnosis is recognition of the progressive reduction in the caliber (diameter) of hairs.
CTE: Chronic Telogen Efflvuium
Patients with CTE can appear to have a similar story. Many have a sudden onset of shedding. The shedding is diffuse. The temples may be particularly affected with reduced density to a much more significant degree than seen in AGA. Reduced hair caliber (miniaturization) is not a feature of CTE. CTE has periods where shedding appears to slow considerably or even stop. When one follows these conditions for many years there is a realization of another important difference: Density in CTE reduces initially but then plateaus and does not reduce further. Density in AGA continues to drop off over time. These points are illustrated in the graph.
SHARE THIS
No Comments
MINOXIDIL AND SHEDDING: WHY DOES MINOXIDIL CAUSE SHEDDING?
November 21, 2017
Why does minoxidil cause shedding?
Minoxidil commonly causes increased hair shedding in the first 6-8 weeks of use (and sometimes a bit longer).
Every human has hairs on their scalp that are destined to come out next week, the week after and the week after that. When minxodil is applied to the scalp, many of those hairs simply come out earlier than they are supposed to. This is termed "immediate telogen release" and is the main mechanism by which minoxidil causes shedding in the first 2 months of use.
SHARE THIS
No Comments
HAIR BREAKAGE IN ALOPECIA AREATA
November 18, 2017
Why do hairs break in alopecia areata?
Hair breakage is a common finding in active alopecia areata (an autoimmune hair loss condition). Inflammation occurring deep down in the scalp at the level of the bulb prevents strong hairs from being produced. The result is hair breakage. Some of hairs that are shed are of course full length hairs. But in patients with very active AA, a close examination of shed hairs will reveal that many are broken.
SHARE THIS
No Comments
VIBRATIONAL ANESTHESIA: A KEY TOOL FOR THE HAIR SPECIALIST
November 18, 2017
Vibration and Pain Sensation:
Injections are a key part of being a hair loss specialist. I perform steroid injections, PRP injections and use a variety of local anesthetics to freeze (numb) the scalp (ie biopsies, hair transplants). One should strive to perform injections in as pain-free manner as possible. There are several ways to limit the pain of injections including going slowly with administration, using small gauge needles, adjusting pH, and warming solutions to be injected. I also use variety of vibration devices to distract pain during injections.
Vibration helps block the perception of pain. According to the Melzack & Wall's "gate control" theory of pain, nerve fibers known as A-β nerve fibers (which transmit information from vibration & touch receptors in the skin) stimulate inhibitory interneurons in the spinal cord, which in turn decrease the amount of pain signals generated from A-δ and C fibers to the brain. This photo shows two vibration devices I use at present. Other helpful methods of vibration include scratching the skin in the area where one is injecting.
SHARE THIS
No Comments
TAPERED AND EXCLAMATION MARK HAIRS IN ALOPECIA AREATA
November 18, 2017
Tapered & Exclamation Hairs in AA indicate Activity
Tapered Hairs
Tapered hairs are frequently seen in patients with small circular patches of alopecia areata. In contrast to 4-5 mm exclamation mark hairs (see next post), tapered hairs are long and typically as long as neighboring hairs. As the hair enters into the skin it becomes much thinner. At the bottom of the tapered hair (deep under the skin) is inflammation.
Tapered are important findings in patients with patchy stage alopecia areata as they tell us that the condition is active and that anti-inflammatory type treatments (such as cortisone injections) are likely to help. The above photo shows several tapered hairs (TH).
Exclamation Hairs
Exclamation mark hairs are frequently seen in patients with small circular patches of alopecia areata. These hairs a short 4-5 mm hairs and represent broken hairs. The top is thick and the end is often frayed. As the hair enters into the skin it becomes much thinner. At the bottom of the exclamation mark hair (deep under the skin) is inflammation. Exclamation mark hairs are important findings in patients with patchy stage alopecia areata as they tell us that the condition is active and that anti-inflammatory type treatments (such as cortisone injections) are likely to help. The photo shows several exclamation mark hairs (EMH).
SHARE THIS
No Comments
CHRONIC TELOGEN EFFLUVIUM (CTE)
November 18, 2017
Misdiagnoses common with CTE
Chronic telogen effluvium (CTE) is an interesting and frequently misdiagnosed hair shedding condition. Many patients with androgenetic alopecia, acute telogen effluvium and even alopecia areata are diagnosed as having chronic telogen effluvium.
How does CTE present?
Most patients with true CTE are 40-65 and present with sudden onset of increased hair shedding that fluctuates in intensity. Some days there is alot of shedding. Some days very little. Many patients have scalp pain (trichodynia) which may correlate with the shedding episodes. Patients with CTE often appear to have good hair density to an outsider which makes the condition frustrating for the patient. A careful history and exam can confirm the diagnosis in many cases. Follicular miniaturization is not a feature unless genetic hair loss is present too. A hair collection or scalp biopsy is useful in more challenging cases.
SHARE THIS
No Comments
ANDROGEN BLOCKADE FOR FPHL: CAN I USE MORE THAN I MEDICATION?
November 16, 2017
Androgen blockade has the potential to be help female pattern hair loss. Caution is needed with any hormone blocker due to significant harm that can come to a developing baby were a woman to become pregnant on any hormone blocker. For this reason they are frequently used with various strict contraceptive methods.
Hormone Blocking Medications for FPHL
Female Pattern Hair Loss (also called female androgenetic alopecia) affects 40 % of women by age 50. There are a variety of treatment options including minxodil, anti-androgens, laser and PRP.
Anti-androgens can help some women with female pattern hair loss. A long list of anti-androgens exist including spironolactone, finasteride, cyproterone acetate, flutamide, dutasteride. The combination of anti-androgens can sometimes work even better than one alone provided the patient actually has a truly androgen responsive hair loss condition. Most men do. But not all women have a form of FPHL that is truly responsive to anti-androgens.
Anti-androgen Side Effects
The decision to use two or more anti-androgens must always be weighed against potential side effects. The combination of androgen blocking pills has the potential to be associated with side effects such as depression, worsening fatigue, breast tenderness, breast enlargement, weight gain, decreased libido.
SHARE THIS
No Comments
TREATING FEMALE PATTERN HAIR LOSS: OPTIONS FOR WOMEN OVER 60
November 16, 2017
Treatments for AGA in Women over 60
I'm often asked about treatment options for women over 60 who present with a diagnosis of androgenetic alopecia (female pattern hair loss). There is some degree of confusion as well as misconceptions which exist in this subject area.
My approach in this situation is to first confirm the diagnosis and then base treatment decisions according to the patient's medical history. The importance of the first step can not be overemphasized.
1: Confirming the Diagnosis
It is extremely important to confirm the diagnosis and ensure that a) another diagnosis is not more appropriate and b) to determine whether other diagnoses are also present. A patient need not have only one diagnosis.
A. Senescent Alopecia
Women who present with hair thinning in their 60s and 70s with no evidence whatsoever of thinning in the 30s, 40s or 50s may have senescent alopecia (age related hair loss) rather than true androgenetic alopecia. This distinction is important as senescent alopecia is less likely to be androgen-driven and therefore responds less to antiandrogens such as finasteride. The main treatment for senescent alopecia is minoxidil although agents such as low level laser and less commonly finasteride can be considered.
I typically ask patients if their hair density on their 50th birthday was more or less the same as their 30th birthday. If that answer is yes one should at least consider the possibility that senescent alopecia or even another diagnosis other than androgenetic alopecia is present.
B. Scarring Alopecia
Scarring alopecias are far more common than we currently diagnose. They range from subtle asymptomatic scarring alopecia to fibrosing alopecia in a pattern distribution to markedly symptomatic lichen planopilaris. Scarring alopecias are easy to miss but need to be considered in all patients with sudden onset of itchy hair loss or a more rapid decline in density from what they may have experienced in the past. A biopsy can help better evaluate these conditions.
C. Hair shedding issues
Both acute and chronic telogen effluvium (CTE) need to be considered in women with hair concerns. Stress, thyroid problems, new illnesses and newly prescribed medications can all contribute to increased hair shedding and hair loss. Anyone with new shedding needs a very detailed examination and workup not only by the dermatologist but by the family physician. Blood tests are especially as is a full medical examination. One must also ensure that routine mammograms and colonoscopies are up to date.
Chronic telogen effluvium (CTE) is among the more challenging to diagnose conditions. Patients present with increased shedding that waxes and wanes. To an outsider it generally appears that the person has fairly good density. A hair collection or biopsy can help with the diagnosis.
Treatment Options
The main treatment options for patients with confirmed androgenetic alopecia is minoxidil, finasteride and low level laser. If the pattern of hair loss is localized frontal loss, and donor density in the occipital scalp is good, a hair transplant can be considered as well.
Minoxidil is formally approved for women 18-65. It may, of course, be used off label for women over 65 with proper evaluation by a physician. Women with heart disease, heart failure or previous heart attacks for example may or may not be good candidates for minoxidil. One is not obligated to use the full recommended dose of minoxidil. Starting with one-quarter or one-half the recommended amount is often a good way to ease in to the treatment in patients with underlying medical issues.
Finasteride may also be a good option. Studies support the notion that higher doses of 2.5 mg and 5 mg are needed for post-menopausal women and doses of 1 mg are ineffective. Finasteride is relatively contraindicated in women with previous history of breast, ovarian or gynaecological cancer. Given the rare effects of finasteride on mood, this medication is also relatively contraindicated in women with depression.
Low level laser therapies are safe but may be less effective than minoxidil or finasteride. A number of laser devices are available in the market for use by patients in their home. None have proven superior to another and so one must balance cost with ease of use. A helmet based device may be easier for some compared to the hand-held devices.
Scalp Inflammation. Scalp inflammation must be attended to fully when caring for patients with AGA. Many women with AGA have seborrheic dermatitis and this is best controlled with periodic use of an anti-dandruff shampoo. I frequently prescribe a trial of a mild cortisone lotion if there is scalp redness if the redness does not respond to anti-dandruff therapies.
SHARE THIS
No Comments
7 HAIR TRANSPLANT MYTHS
November 12, 2017
7 Common Myths in Hair Transplantation
Hair transplantation is among the mostly consistently successful and life-changing of all the hair loss therapies. Hair transplants nowadays can look extremely natural (when performed by skilled teams). However, there are a number of myths that are infrequently talked about when it comes to hair transplantation. These can sometimes be overlooked.
1. Transplanted hair lasts forever
It’s a common myth that transplanted hair moved during a hair transplant last forever. Fortunately, most hairs that are transplanted do generally remain in their new location forever. However, anyone is has followed a hair transplant patient for 10, 20 or 30 years will tell you that the same number of hairs that were put in are not always remaining over time. Most will stay - but not all
There are many reasons why hairs transplanted hairs don’t always last forever. For one, donor hair is not always completely resistant to balding in all men. In fact, it’s a spectrum, from some men who have very little to no balding in their "donor area" (at the back of the scalp) to men who have considerable thinning in the donor area over time (ie. men with DUPA are the extreme). In addition, the medical community has not rigorously studied long term the immunological and physiological changes that happen to transplanted hairs over extended periods of time.
Nevertheless, there is no arguing that transplanted hairs last forever. It holds true for a high proportion of men and women but not all. We hope they last forever are and they seem to be in many men. However, a proportion of transplanted hairs slowly disappear over decades in some men.
2. Only one hair transplant surgery session is needed
From the time male balding and female thinning announces its presence in any patient, it always progresses. While it is true that androgenetic alopecia can stop or slow for periods of months to a year or two, androgenetic alopecia by definition never stops. Anyone who gets a hair transplant must assume that existing hair in an area will slowly thin over time. If a patient is under 30 years of age, he (or she) must assume that another hair transplant will likely be needed if he wishes to maintain his current look into his 50s and 60s.
3. A hair transplant procedure is always a great success
Hair transplants are generally quite successful. That's why they are popular! With the right patient, and a skilled team, the chances of success are high. Unfortunately, hair transplant don’t always work out as successfully as one might hope. There is not an experienced hair transplant surgeon in the world who can state that he or she has never had a patient who did not grow as much hair as they hoped. The reasons why this occurs is quite varied - but ranges from "patient factors" (post op care, smoking, unrecognized scalp diseases), to "surgeon-related" factors (surgeon skill, skill of the technicians handling the grafts). Sometimes one never knows the exact reason why things don’t turn out. In the hair transplant field, this is called the ‘X factor.’
4. A hair transplant is a one-day event
A hair transplant procedure itself is a one day event, but the actual procedure when one considers the time from the surgery to the time where the patient feels back to normal ranges from a few days to a few months. The actual recovery time varies from patient to patient and varies based on the size of the surgery.
In general, the post op recovery period is longer for FUT procedures than FUE and longer for patients that require more grafts. Patients who don’t require shaving for FUE procedures and have limited baldness, may find that 2-3 days is sufficient to feel back to their usual self. However, a patient whose scalp is shaved completely for a large 3000-4000 FUE procedures may find that it takes just a few days to “feel good” but takes 3-4 weeks before he feel confident to go to work. Depending on his occupation, he may or may not feel comfortable at work for an extended period. A patient who sees clients on a daily basis at work may not feel completely comfortable seeing his clients even after 2 weeks post op from a 4000 graft FUE. This needs to be taken into account. A hair transplant is not always a ‘one day thing.’
5. A hair transplant is always an option for treating hair loss
It’s a myth that a hair transplant is always an option for an individual with hair loss. Some patients may be too young, some have medical issues that preclude surgery, and some have a type of hair loss that also will not be successful if a hair transplant were performed. Hair transplants aren't for everyone.
6. There are no complications to a hair transplant
Hair transplants are quite safe. But it’s a bit of a stretch to say that they are without complication. Patients may have have redness, swelling and crusting post operatively. In general, the recovery in FUE procedures is much easier than FUT procedures. But there are rare complications in hair transplant surgery that include long lasting nerve pain (more in FUT than FUE procedures) and persistent scalp redness. Unless a physician is carefully monitoring the procedure, a patient can even get sick. The hair transplant community tends to shy away from calling hair transplant procedures a 'surgery' in order to make the procedure more patient friendly - but make no mistake a hair transplant is a surgery.
7. You will regain the hair density of your youth
A hair transplant is a surgical procedure which involved moving anywhere from 10 to 10,000 hairs into an area of balding. If an area of hair loss is small, it may be possible to build some very nice density in the area – but the density is generally less than it once was. For example, in a patient who is very bald, a density of 35-40 follicular units per square centimeter will typically be created. This area likely had a density of 90 or more follicular units per square centimeter at one time years earlier. Therefore, it is generally the norm for a hair transplant to create results that are less dense than the original density. A skilled surgeon can often help make 35-40 follicular units look like the original density. However, photos and videos of patients with amazingly thick and dense hair following their procedure may not always be accurate.
SHARE THIS
No Comments
NAAF VANCOUVER
November 12, 2017
The NAAF Vancouver Support Group
Alopecia areata is an autoimmune condition that affects about 50,000 Canadians. The condition affects males and females of all ages and can have a tremendous impact on the lives of both patients and their families. Support groups play an important role in imparting accurate information to patients and families with new diagnoses as well as those who have had the condition for many years. These groups connect people at different stages of coping and provides a network of support.
The National Alopecia Areata Foundation (NAAF) was founded 25 years ago and has a number of patient support groups throughout the United States and Canada. I’m honored to join the NAAF Vancouver Support Group in 2018 as Medical Advisor. Four meetings are planned for the year in Spring, Summer, Fall and Winter in Vancouver. Individuals with alopecia areata interested in attending these sessions may contact the NAAF for information on dates, times and location or contact our office.
SHARE THIS
No Comments
AGE 50: AN IMPORTANT CUT OFF FOR DIAGNOSING HAIR LOSS
November 12, 2017
The Cut off of 50: Why it matters in the diagnosis of hair loss in Older Individuals ?
Any birthday is special. The 50th birthday is an important cut off in the diagnosis of many hair diseases. An important principle of diagnosing hair loss in men and women over 60 comes from understanding what density of hair a patient had at age 50.
A true or false question
For anyone over 60, I always ask patients to help me with a true or false question. I generally ask it in the following way “Is this statement true or false: My hair density at age 50 was about the same as it was at age 30.”
This is such an important question - especially if the patient replies “TRUE”. Men and women who develop hair loss in their 60s and 70s but who report that their density age 50 was quite good have a high likelihood of having another diagnosis besides simply genetic hair loss. Of course genetic hair loss is a possibility and it’s possible the patient does not really have a good recall of their hair density at age 50. Nevertheless, there are several conditions that need to be considered in somwone with good thick hair at age 50 and hair loss in the 60s”
1. Scarring Alopecia (especially Lichen Planopilaris)
2. Senescent Hair Loss
3. Diffuse Alopecia Areata
4. Hair Shedding Disorders
Final Comment:
Patients in their 60s and 70s who tell me they had thick hair at age 50 and that it was the same thickness as age 30 often have an interesting array of hair loss conditions. One should not default to diagnosing genetic hair loss in these situations because that diagnosis may be relatively unlikely in this unique situation.
SHARE THIS
No Comments
CASE REPORTS IN THE RESEARCH WORLD: ARE THEY HELPFUL?
November 12, 2017
Case Reports in Hair Loss: Cautiously Optimistic.
A Case Report is a published medical study which presents a particular finding as it relates to a single patient. Common Examples of Case Reports are:
1. Reports of a New Diagnostic Finding
For example, a new feature that clinicians might consider to improve their ability to diagnose a particular condition
2. Reports of a New Treatment
For example, a new treatment or revised method of using a currently available treatment that improves the way we treat hair loss
3. Reports of a New Prognostic Finding
For example, a new finding either clinical or through blood tests/biopsy that helps predict the course of a patient’s hair loss
Interpreting the Value of Case Reports: Time is the Best Judge.
Case Reports are wonderful in many ways because they have the potential to stimulate additional research and thinking around the world on a particular subject. Case Reports can sometimes be the key fuel that triggered additional studies in a particular subject area.
However, case reports need to be interpreted cautiously because the results only apply to a single patient. One can not conclude that the finding will be applicable to all patients. In order to conclude that a case report has widespread applicability, further large scale studies are needed.
Take for example, the case report of sexual dysfunction from use of topical minoxidil. The study is very interesting. I can not conclude based on this study that topical minoxidil is associated with sexual dysfunction in men. However, it sets us up for further studies in this area and keep me alert to monitor these side effects in patients who use topical minoxidil. In my mind the study is extremely valuable.
Conclusion
Time will tell how any case report will go down in history as a valid or not valid contribution to the medical literature. Time is ultimately the best judge of case reports.
SHARE THIS
No Comments
CAN YOU DIAGNOSE HAIR LOSS FROM A PHOTO?
November 12, 2017
Photos: Can you diagnose hair loss from a photo?
With the widespread availability of smartphones, it’s remarkably easy nowadays to take photos. It’s also remarkably easy to post these on various forums and remarkably easily to send these via email. For these reasons, photo use is widespread among patients with hair loss. Despite this, there is a common assumption that is being made that is not correct. Many people wrongly assume that one can properly diagnose hair loss with use of a photo.
Photographs for Hair Loss: Helpful but not the entire story
There are many hair loss conditions that mimic each other. For example, I can show you a photo of androgenetic alopecia, diffuse alopecia areata, and lichen planopilaris that look identical. Can one be confident from the photo alone as to what the diagnosis is? No.
Because genetic hair loss is common, one will often be correct by guessing genetic hair loss in many photographs of hair loss. Nearly 1 out of every 2 women will have genetic hair loss by age 50 compared to approximately 1 out of 7,000 who will have (0.01%) have lichen planopilaris. Clearly, guessing that a photo is showing genetic hair loss is more likely to be the correct answer.
PRINCIPLES OF USING PHOTOS
Here are some important principles of photographs in the diagnosis of hair loss
1. One can never be 100 % confident of any diagnosis with a photo alone.
2. The lighting and background must ideally be the same if photos are to be compared.
3. The length of the hair must also be the same.
4. With a very detailed clinical history about the patient’s hair loss and medical history, one can move from being "uncertain" about the diagnosis to "somewhat confident." But that's about the maximum one can be. One can never be 100 % certain. There are many conditions that can mimic each other.
Conclusion
Photographs are wonderful to document the degree and pattern of hair loss. However, one must not assume that one can confidently determine the diagnosis of hair loss with photographs alone.
SHARE THIS
No Comments
SIDE EFFECTS FROM HAIR LOSS MEDICATIONS:
November 12, 2017
Side Effects from Hair Loss Medications: What is the Chance?
Today, I’d like to review my personal view on medication and treatment-related side effects.
1. Every single treatment has ‘potential’ adverse effects. (No treatment is risk-free).
Every treatment for hair loss has potential side effects. There is no treatment on the planet that is side effect free. How do I know that? Well, studies have shown that even patients using “placebo” treatments for their hair loss report side effects. This teaches us that any time a patient uses a treatment they have a chance to experience a side effect. Whether it’s a true side effect or not is sometimes challenging to decipher but a topic for another article.
2. No medication or treatment for hair loss should ever be prescribed or used without patients understanding the “most common" adverse events
It is critically important for patients to understand the "most common" side effects of a treatment. The purpose of delivering such information to patients is to help them with informed consent. A patient should only use a mediation if they feel that the benefits of using the medication are greater than the potential risks. It is the responsibility of the physician to transfer information about both the benefits and the risks to the patient so that the patient can offer their informed consent.
3. It is not possible to explain all the potential side effects of a medication.
Despite the important role that we as physicians have in telling our patients about the side effects of medications, it is important for patients to be aware that a given presciber can not communicate the entire list of side effects that have ever been reported. However, it is imperative for the prescriber to advice on the most common ones.
Take for example, the oral medication doxycycline. In the hair clinic, doxycycline is used for the treatment of scarring alopecia, folliculitis and a variety of other inflammatory and infectious conditions. A patient who is deciding on whether to use doxycycline or not should be made aware of the most common side effects including gastrointestinal upset, nausea, headaches, increased chance of yeast infections in women.
However, rare side effects are possible as well. For example, every year a small number of users of doxycycline around the world develop serious allergic skin reactions. It would be highly unusual for any prescriber or pharmacist to counsel a patient on this particular side effect.
4. There may be side effects that are discovered years down the road.
One must also be aware that some side effects of a medication may not be apparent during clinical trials or even during the first few years that the medication is on the market. In some cases it may take 10, 15 or even 20 years to come to understand that rarest of side effects. “Post marketing surveillance” is a term used to describe the monitoring that goes on after a medication is released on to the market. Post marketing surveillance has lead to some medications being removed from the market. One must always be aware that additional side effects of a medication may be revealed in the future through such post marketing surveillance.
5. For any potential adverse effect, one must ask “how common” that side effect is.
For some medications, the chance of adverse effects may be very low, whereas for other medications, the chance of an adverse effect may be quite high. Let’s take topical minoxidil as an example. The most common side effects and headaches, dizziness, hair shedding (in the first few months), hair growth on the face and heart palpitations. However, in deciding whether to use the medication or not, patients need to understand the overall chance of these side effects. For example, many women are extremely concerned to learn that hair growth on the face (hypertrichosis) is a potential side effect of minoxidil. it is very important from women to note that 19 out of 20 women who use minoxidil will not have any problems with hair growth on face. However, 1 out of 20 users will. This information is helpful as it encourages many women to move forward with considering the medication with knowledge that their chance of hair growth on the face is quiet low.
Conclusion
Hair loss medications have the potential to dramatically improve hair density or stop hair loss and may improve quality of life. However, anyone using a treatment, no matter what the treatment actually is, needs to be aware that every treatment has potential side effects. It is imperative that patients, together with their doctors, spend time understand how common the various side effects actually are.
SHARE THIS
No Comments
ANDROGENETIC ALOPECIA: SHOULD I START TWO TREATMENTS AT ONCE?
November 12, 2017
Androgenetic Alopecia: Should I start two treatments at once?
There are many treatments available for any particular hair loss condition. Let’s take androgenetic alopecia as an example. Individuals with androgenetic alopecia might consider topical minoxidil, oral hormone blocking medications, low level laser or even platelet rich plasma. For some types of hair loss there may be an even greater array of choices.
I’m often asked if patients should start more than one treatment at the same time. My personal view is not necessarily the right answer or the only view on the subject. However, my personal view is my view. My personal view is that whenever possible medications should not be started at the same times but rather staggered. The intervals of staggering the treatments will depend on the specific situation and the urgency of treatment.
Example
Consider the 34 year old female patient with androgenetic alopecia who is considering topical minoxidil and oral spironolactone. After a careful review of the patient’s medical history, blood tests, and examining the scalp, it is determined that both are good options for the patient. I am faced with two options: Start both or start one at a time (stagger the treatments). Let’s look at the implications of both.
Treatment Option 1: Start Minoxidil and Spironolactone at the Same Time
Both Spironolactone and Minoxidil are recommended for the patient in this situation. What needs to be considered is that minoxidil has about a 30 % chance of helping the patient. It has a 70 % chance of not being all that helpful. Spironolactone has a 40 % chance of improving hair growth. If both are started at the same time and the patient experiences and improvement it will be difficult if not impossible to know which treatment was responsible for the improvement.
Was it the minoxidil?
Was it the spironolactone?
Was it both?
Treatment Option 2: Start Minoxidil First and Introduce Spironolactone in 6-9 months.
My personal preference in this situation was to start minoxidil first. After 6-9 months of treatment (once I determine if the minoxidil is working or not), I can make a decision to add spironolactone. In this case I can have a clear sense for the entire lifetime of the patient what helps and what does not.
Comment and Conclusions
Treatments for some hair loss conditions (such as androgenetic alopecia) are life-long. A 33 year old woman who lives to 93 could potentially have 60 years of use of a given medication. From a cost perspective alone, once can potentially save a patient $ 36,000 over their lifetime by confirming that a medication does not work and should be abandoned.
SHARE THIS
No Comments
TREATMENT LADDER FOR HAIR LOSS: LOGICAL AND EVIDENCE BASED
November 12, 2017
Treatment Ladders: What is a treatment ladder?
For any type of hair loss, there are many potential treatments. Some types of hair loss may actually have 10-15 different treatments available. How does one choose which to start with? How does once decide which treatment to use if the first treatment does not work? In short, decisions on treatment are often make with use of a ‘treatment ladder.” A treatment ladder is a term that describes a logical approach to how one should progress onto different treatments if a previous one proves ineffective. In essence, a treatment ladder refers to a guide to how one should move “step by step” to additional treatments. If one treatment does not work one moves up to the next treatment on the treatment ladder. Treatment ladders helps clinicians balance effectiveness of treatment with safety.
Treatment Ladders for All Hair Loss
In my view, every hair loss condition has a treatment ladder. If there are 15 treatments for hair loss, one does not simply reach into a hat and decide on treatment based on the name that is pulled out of the hat. Also, one does not decide on treatment based on what was reported on the news, or what a neighbour or friend had benefit from. If there are 15 treatments available for a given hair loss condition, one arranges those 15 treatments on a treatment ladder for the given condition and severity of condition and moves forward with decisions on treatments based on that treatment ladder.
Treatment Ladders: Alopecia Areata as an Example.
Let’s consider a 33 year old female with 5-6 patches of alopecia areata. She comes in with a clip from the newspaper on the oral medication “tofacitinib” and wants to start it. It is true that oral tofacitinib can help alopecia areata, but is this a good option?
Well, an appropriate ladder for a 27 year old with 5-6 patches with alopecia areata could include:
TIER 1: Topical steroids and/or steroid Injections (with minoxidil)
TIER 2: Topical Immunotherapy (DPCP or Anthralin) or Prednisone Taper (with minoxidil)
TIER 3: Oral Methotrexate or Sulfasalazine or Platelet Rich Plasma (PRP)
TIER 4: Oral Tofacitinib
This is an example. The order of the ladder (or choices for treatment) will differ from physician to physician. But this would be ‘my’ ladder for a 33 year old female with alopecia areata totalling 5-6 patches. You can see that oral tofacitinib is on the list but not at the top of the list.
Conclusion
Without a treatment ladder one needs to guess if a treatment should be used or not. Treatment ladders are important in any practice and essential in my practice to ensure that evidence based principles are used wherever possible in the treatment of hair loss.
SHARE THIS
No Comments
MY HAIR WAS RIPPED OFF: WILL IT GROW BACK?
November 11, 2017
Traumatic Hair Pulling: Full Regrowth May or May Not Occur
I am often asked if hair that is pulled out forcefully will regrow. Examples of this are the pulling of hair by children on the playground, hair getting caught in doors, machines etc or cases of hair pulling during assault or abuse-related situations (for example domestic abuse).
Without actually seeing the scalp, and knowing details of the patient's story, it is impossible to determine if hair will or will not grow back in any particular case. This requires an in person examination so that the scalp can be properly examined.
Hair regrowth is not a guarantee
There is no guarantee that hair regrowth will occur. One will know in 6-9 months if they will acheive full regrowth or not because that is how long it takes for hair to grow back following any type of injury.
It is certainly possible for repeated pulling to give permanent hair loss. However, in the vast majority of cases where hair is pulled from the scalp, hair grows back. If you or I were to reach up a pluck a hair, it will grow back. However, if pulling is repeated many times or is excessive with bleeding a greater chance exists for scarring to develop. Hair pulling that is accompanied by injury to the skin layers (i.e. that creates an actual wound) has a markedly increased chance of being associated with permanent scarring. It is such scarring that blocks the regrowth of hair. Scar tissue is permanent and, if present, generally destroys stems cells.
Anyone with concerns about incomplete growth after episodes of hair pulling should see a physician who specializes in hair loss for consideration of a scalp biopsy.
0 notes
Text
Scarring Alopecia
SCARRING ALOPECIA: LOSS OF THE FOLLICULAR OPENING IS A HALLMARK
November 22, 2017
Scarring Alopecias Cause Scarring
Scarring alopecias are hair loss conditions that are associated with the development of permanent hair loss. There are dozens of different types of scarring alopecia. Some scarring alopecias itch. Some don't. Some are associated with increased shedding. Some aren't. Some are red. Some aren't. Some bleed. Most don't.
However what is common to all scarring alopecias is the disappearance of the follicular opening or "pore." The development of scar tissue beneath the skin leads to the destruction of the follicular pore opening.
The arrows point to an area of scarring in a subtle early scarring alopecia
SHARE THIS
No Comments
DENSITY CHANGES IN CTE VS AGA OVER TIME
November 22, 2017
Chronic Telogen Effluvium: How does density change over time?
Chronic Telogen Effluvium (CTE) and Androgenetic alopecia (AGA) are both commonly encountered diagnoses in women age 40-70 years. They are however, very different conditions.
AGA: Androgenetic Alopecia
AGA presents with hair thinning and sometimes increased daily shedding as well. The loss of hair is sometimes just frontal in location or the crown but can be diffuse (all over). A key to the diagnosis is recognition of the progressive reduction in the caliber (diameter) of hairs.
CTE: Chronic Telogen Efflvuium
Patients with CTE can appear to have a similar story. Many have a sudden onset of shedding. The shedding is diffuse. The temples may be particularly affected with reduced density to a much more significant degree than seen in AGA. Reduced hair caliber (miniaturization) is not a feature of CTE. CTE has periods where shedding appears to slow considerably or even stop. When one follows these conditions for many years there is a realization of another important difference: Density in CTE reduces initially but then plateaus and does not reduce further. Density in AGA continues to drop off over time. These points are illustrated in the graph.
SHARE THIS
No Comments
MINOXIDIL AND SHEDDING: WHY DOES MINOXIDIL CAUSE SHEDDING?
November 21, 2017
Why does minoxidil cause shedding?
Minoxidil commonly causes increased hair shedding in the first 6-8 weeks of use (and sometimes a bit longer).
Every human has hairs on their scalp that are destined to come out next week, the week after and the week after that. When minxodil is applied to the scalp, many of those hairs simply come out earlier than they are supposed to. This is termed "immediate telogen release" and is the main mechanism by which minoxidil causes shedding in the first 2 months of use.
SHARE THIS
No Comments
HAIR BREAKAGE IN ALOPECIA AREATA
November 18, 2017
Why do hairs break in alopecia areata?
Hair breakage is a common finding in active alopecia areata (an autoimmune hair loss condition). Inflammation occurring deep down in the scalp at the level of the bulb prevents strong hairs from being produced. The result is hair breakage. Some of hairs that are shed are of course full length hairs. But in patients with very active AA, a close examination of shed hairs will reveal that many are broken.
SHARE THIS
No Comments
VIBRATIONAL ANESTHESIA: A KEY TOOL FOR THE HAIR SPECIALIST
November 18, 2017
Vibration and Pain Sensation:
Injections are a key part of being a hair loss specialist. I perform steroid injections, PRP injections and use a variety of local anesthetics to freeze (numb) the scalp (ie biopsies, hair transplants). One should strive to perform injections in as pain-free manner as possible. There are several ways to limit the pain of injections including going slowly with administration, using small gauge needles, adjusting pH, and warming solutions to be injected. I also use variety of vibration devices to distract pain during injections.
Vibration helps block the perception of pain. According to the Melzack & Wall's "gate control" theory of pain, nerve fibers known as A-β nerve fibers (which transmit information from vibration & touch receptors in the skin) stimulate inhibitory interneurons in the spinal cord, which in turn decrease the amount of pain signals generated from A-δ and C fibers to the brain. This photo shows two vibration devices I use at present. Other helpful methods of vibration include scratching the skin in the area where one is injecting.
SHARE THIS
No Comments
TAPERED AND EXCLAMATION MARK HAIRS IN ALOPECIA AREATA
November 18, 2017
Tapered & Exclamation Hairs in AA indicate Activity
Tapered Hairs
Tapered hairs are frequently seen in patients with small circular patches of alopecia areata. In contrast to 4-5 mm exclamation mark hairs (see next post), tapered hairs are long and typically as long as neighboring hairs. As the hair enters into the skin it becomes much thinner. At the bottom of the tapered hair (deep under the skin) is inflammation.
Tapered are important findings in patients with patchy stage alopecia areata as they tell us that the condition is active and that anti-inflammatory type treatments (such as cortisone injections) are likely to help. The above photo shows several tapered hairs (TH).
Exclamation Hairs
Exclamation mark hairs are frequently seen in patients with small circular patches of alopecia areata. These hairs a short 4-5 mm hairs and represent broken hairs. The top is thick and the end is often frayed. As the hair enters into the skin it becomes much thinner. At the bottom of the exclamation mark hair (deep under the skin) is inflammation. Exclamation mark hairs are important findings in patients with patchy stage alopecia areata as they tell us that the condition is active and that anti-inflammatory type treatments (such as cortisone injections) are likely to help. The photo shows several exclamation mark hairs (EMH).
SHARE THIS
No Comments
CHRONIC TELOGEN EFFLUVIUM (CTE)
November 18, 2017
Misdiagnoses common with CTE
Chronic telogen effluvium (CTE) is an interesting and frequently misdiagnosed hair shedding condition. Many patients with androgenetic alopecia, acute telogen effluvium and even alopecia areata are diagnosed as having chronic telogen effluvium.
How does CTE present?
Most patients with true CTE are 40-65 and present with sudden onset of increased hair shedding that fluctuates in intensity. Some days there is alot of shedding. Some days very little. Many patients have scalp pain (trichodynia) which may correlate with the shedding episodes. Patients with CTE often appear to have good hair density to an outsider which makes the condition frustrating for the patient. A careful history and exam can confirm the diagnosis in many cases. Follicular miniaturization is not a feature unless genetic hair loss is present too. A hair collection or scalp biopsy is useful in more challenging cases.
SHARE THIS
No Comments
ANDROGEN BLOCKADE FOR FPHL: CAN I USE MORE THAN I MEDICATION?
November 16, 2017
Androgen blockade has the potential to be help female pattern hair loss. Caution is needed with any hormone blocker due to significant harm that can come to a developing baby were a woman to become pregnant on any hormone blocker. For this reason they are frequently used with various strict contraceptive methods.
Hormone Blocking Medications for FPHL
Female Pattern Hair Loss (also called female androgenetic alopecia) affects 40 % of women by age 50. There are a variety of treatment options including minxodil, anti-androgens, laser and PRP.
Anti-androgens can help some women with female pattern hair loss. A long list of anti-androgens exist including spironolactone, finasteride, cyproterone acetate, flutamide, dutasteride. The combination of anti-androgens can sometimes work even better than one alone provided the patient actually has a truly androgen responsive hair loss condition. Most men do. But not all women have a form of FPHL that is truly responsive to anti-androgens.
Anti-androgen Side Effects
The decision to use two or more anti-androgens must always be weighed against potential side effects. The combination of androgen blocking pills has the potential to be associated with side effects such as depression, worsening fatigue, breast tenderness, breast enlargement, weight gain, decreased libido.
SHARE THIS
No Comments
TREATING FEMALE PATTERN HAIR LOSS: OPTIONS FOR WOMEN OVER 60
November 16, 2017
Treatments for AGA in Women over 60
I'm often asked about treatment options for women over 60 who present with a diagnosis of androgenetic alopecia (female pattern hair loss). There is some degree of confusion as well as misconceptions which exist in this subject area.
My approach in this situation is to first confirm the diagnosis and then base treatment decisions according to the patient's medical history. The importance of the first step can not be overemphasized.
1: Confirming the Diagnosis
It is extremely important to confirm the diagnosis and ensure that a) another diagnosis is not more appropriate and b) to determine whether other diagnoses are also present. A patient need not have only one diagnosis.
A. Senescent Alopecia
Women who present with hair thinning in their 60s and 70s with no evidence whatsoever of thinning in the 30s, 40s or 50s may have senescent alopecia (age related hair loss) rather than true androgenetic alopecia. This distinction is important as senescent alopecia is less likely to be androgen-driven and therefore responds less to antiandrogens such as finasteride. The main treatment for senescent alopecia is minoxidil although agents such as low level laser and less commonly finasteride can be considered.
I typically ask patients if their hair density on their 50th birthday was more or less the same as their 30th birthday. If that answer is yes one should at least consider the possibility that senescent alopecia or even another diagnosis other than androgenetic alopecia is present.
B. Scarring Alopecia
Scarring alopecias are far more common than we currently diagnose. They range from subtle asymptomatic scarring alopecia to fibrosing alopecia in a pattern distribution to markedly symptomatic lichen planopilaris. Scarring alopecias are easy to miss but need to be considered in all patients with sudden onset of itchy hair loss or a more rapid decline in density from what they may have experienced in the past. A biopsy can help better evaluate these conditions.
C. Hair shedding issues
Both acute and chronic telogen effluvium (CTE) need to be considered in women with hair concerns. Stress, thyroid problems, new illnesses and newly prescribed medications can all contribute to increased hair shedding and hair loss. Anyone with new shedding needs a very detailed examination and workup not only by the dermatologist but by the family physician. Blood tests are especially as is a full medical examination. One must also ensure that routine mammograms and colonoscopies are up to date.
Chronic telogen effluvium (CTE) is among the more challenging to diagnose conditions. Patients present with increased shedding that waxes and wanes. To an outsider it generally appears that the person has fairly good density. A hair collection or biopsy can help with the diagnosis.
Treatment Options
The main treatment options for patients with confirmed androgenetic alopecia is minoxidil, finasteride and low level laser. If the pattern of hair loss is localized frontal loss, and donor density in the occipital scalp is good, a hair transplant can be considered as well.
Minoxidil is formally approved for women 18-65. It may, of course, be used off label for women over 65 with proper evaluation by a physician. Women with heart disease, heart failure or previous heart attacks for example may or may not be good candidates for minoxidil. One is not obligated to use the full recommended dose of minoxidil. Starting with one-quarter or one-half the recommended amount is often a good way to ease in to the treatment in patients with underlying medical issues.
Finasteride may also be a good option. Studies support the notion that higher doses of 2.5 mg and 5 mg are needed for post-menopausal women and doses of 1 mg are ineffective. Finasteride is relatively contraindicated in women with previous history of breast, ovarian or gynaecological cancer. Given the rare effects of finasteride on mood, this medication is also relatively contraindicated in women with depression.
Low level laser therapies are safe but may be less effective than minoxidil or finasteride. A number of laser devices are available in the market for use by patients in their home. None have proven superior to another and so one must balance cost with ease of use. A helmet based device may be easier for some compared to the hand-held devices.
Scalp Inflammation. Scalp inflammation must be attended to fully when caring for patients with AGA. Many women with AGA have seborrheic dermatitis and this is best controlled with periodic use of an anti-dandruff shampoo. I frequently prescribe a trial of a mild cortisone lotion if there is scalp redness if the redness does not respond to anti-dandruff therapies.
SHARE THIS
No Comments
7 HAIR TRANSPLANT MYTHS
November 12, 2017
7 Common Myths in Hair Transplantation
Hair transplantation is among the mostly consistently successful and life-changing of all the hair loss therapies. Hair transplants nowadays can look extremely natural (when performed by skilled teams). However, there are a number of myths that are infrequently talked about when it comes to hair transplantation. These can sometimes be overlooked.
1. Transplanted hair lasts forever
It’s a common myth that transplanted hair moved during a hair transplant last forever. Fortunately, most hairs that are transplanted do generally remain in their new location forever. However, anyone is has followed a hair transplant patient for 10, 20 or 30 years will tell you that the same number of hairs that were put in are not always remaining over time. Most will stay - but not all
There are many reasons why hairs transplanted hairs don’t always last forever. For one, donor hair is not always completely resistant to balding in all men. In fact, it’s a spectrum, from some men who have very little to no balding in their "donor area" (at the back of the scalp) to men who have considerable thinning in the donor area over time (ie. men with DUPA are the extreme). In addition, the medical community has not rigorously studied long term the immunological and physiological changes that happen to transplanted hairs over extended periods of time.
Nevertheless, there is no arguing that transplanted hairs last forever. It holds true for a high proportion of men and women but not all. We hope they last forever are and they seem to be in many men. However, a proportion of transplanted hairs slowly disappear over decades in some men.
2. Only one hair transplant surgery session is needed
From the time male balding and female thinning announces its presence in any patient, it always progresses. While it is true that androgenetic alopecia can stop or slow for periods of months to a year or two, androgenetic alopecia by definition never stops. Anyone who gets a hair transplant must assume that existing hair in an area will slowly thin over time. If a patient is under 30 years of age, he (or she) must assume that another hair transplant will likely be needed if he wishes to maintain his current look into his 50s and 60s.
3. A hair transplant procedure is always a great success
Hair transplants are generally quite successful. That's why they are popular! With the right patient, and a skilled team, the chances of success are high. Unfortunately, hair transplant don’t always work out as successfully as one might hope. There is not an experienced hair transplant surgeon in the world who can state that he or she has never had a patient who did not grow as much hair as they hoped. The reasons why this occurs is quite varied - but ranges from "patient factors" (post op care, smoking, unrecognized scalp diseases), to "surgeon-related" factors (surgeon skill, skill of the technicians handling the grafts). Sometimes one never knows the exact reason why things don’t turn out. In the hair transplant field, this is called the ‘X factor.’
4. A hair transplant is a one-day event
A hair transplant procedure itself is a one day event, but the actual procedure when one considers the time from the surgery to the time where the patient feels back to normal ranges from a few days to a few months. The actual recovery time varies from patient to patient and varies based on the size of the surgery.
In general, the post op recovery period is longer for FUT procedures than FUE and longer for patients that require more grafts. Patients who don’t require shaving for FUE procedures and have limited baldness, may find that 2-3 days is sufficient to feel back to their usual self. However, a patient whose scalp is shaved completely for a large 3000-4000 FUE procedures may find that it takes just a few days to “feel good” but takes 3-4 weeks before he feel confident to go to work. Depending on his occupation, he may or may not feel comfortable at work for an extended period. A patient who sees clients on a daily basis at work may not feel completely comfortable seeing his clients even after 2 weeks post op from a 4000 graft FUE. This needs to be taken into account. A hair transplant is not always a ‘one day thing.’
5. A hair transplant is always an option for treating hair loss
It’s a myth that a hair transplant is always an option for an individual with hair loss. Some patients may be too young, some have medical issues that preclude surgery, and some have a type of hair loss that also will not be successful if a hair transplant were performed. Hair transplants aren't for everyone.
6. There are no complications to a hair transplant
Hair transplants are quite safe. But it’s a bit of a stretch to say that they are without complication. Patients may have have redness, swelling and crusting post operatively. In general, the recovery in FUE procedures is much easier than FUT procedures. But there are rare complications in hair transplant surgery that include long lasting nerve pain (more in FUT than FUE procedures) and persistent scalp redness. Unless a physician is carefully monitoring the procedure, a patient can even get sick. The hair transplant community tends to shy away from calling hair transplant procedures a 'surgery' in order to make the procedure more patient friendly - but make no mistake a hair transplant is a surgery.
7. You will regain the hair density of your youth
A hair transplant is a surgical procedure which involved moving anywhere from 10 to 10,000 hairs into an area of balding. If an area of hair loss is small, it may be possible to build some very nice density in the area – but the density is generally less than it once was. For example, in a patient who is very bald, a density of 35-40 follicular units per square centimeter will typically be created. This area likely had a density of 90 or more follicular units per square centimeter at one time years earlier. Therefore, it is generally the norm for a hair transplant to create results that are less dense than the original density. A skilled surgeon can often help make 35-40 follicular units look like the original density. However, photos and videos of patients with amazingly thick and dense hair following their procedure may not always be accurate.
SHARE THIS
No Comments
NAAF VANCOUVER
November 12, 2017
The NAAF Vancouver Support Group
Alopecia areata is an autoimmune condition that affects about 50,000 Canadians. The condition affects males and females of all ages and can have a tremendous impact on the lives of both patients and their families. Support groups play an important role in imparting accurate information to patients and families with new diagnoses as well as those who have had the condition for many years. These groups connect people at different stages of coping and provides a network of support.
The National Alopecia Areata Foundation (NAAF) was founded 25 years ago and has a number of patient support groups throughout the United States and Canada. I’m honored to join the NAAF Vancouver Support Group in 2018 as Medical Advisor. Four meetings are planned for the year in Spring, Summer, Fall and Winter in Vancouver. Individuals with alopecia areata interested in attending these sessions may contact the NAAF for information on dates, times and location or contact our office.
SHARE THIS
No Comments
AGE 50: AN IMPORTANT CUT OFF FOR DIAGNOSING HAIR LOSS
November 12, 2017
The Cut off of 50: Why it matters in the diagnosis of hair loss in Older Individuals ?
Any birthday is special. The 50th birthday is an important cut off in the diagnosis of many hair diseases. An important principle of diagnosing hair loss in men and women over 60 comes from understanding what density of hair a patient had at age 50.
A true or false question
For anyone over 60, I always ask patients to help me with a true or false question. I generally ask it in the following way “Is this statement true or false: My hair density at age 50 was about the same as it was at age 30.”
This is such an important question - especially if the patient replies “TRUE”. Men and women who develop hair loss in their 60s and 70s but who report that their density age 50 was quite good have a high likelihood of having another diagnosis besides simply genetic hair loss. Of course genetic hair loss is a possibility and it’s possible the patient does not really have a good recall of their hair density at age 50. Nevertheless, there are several conditions that need to be considered in somwone with good thick hair at age 50 and hair loss in the 60s”
1. Scarring Alopecia (especially Lichen Planopilaris)
2. Senescent Hair Loss
3. Diffuse Alopecia Areata
4. Hair Shedding Disorders
Final Comment:
Patients in their 60s and 70s who tell me they had thick hair at age 50 and that it was the same thickness as age 30 often have an interesting array of hair loss conditions. One should not default to diagnosing genetic hair loss in these situations because that diagnosis may be relatively unlikely in this unique situation.
SHARE THIS
No Comments
CASE REPORTS IN THE RESEARCH WORLD: ARE THEY HELPFUL?
November 12, 2017
Case Reports in Hair Loss: Cautiously Optimistic.
A Case Report is a published medical study which presents a particular finding as it relates to a single patient. Common Examples of Case Reports are:
1. Reports of a New Diagnostic Finding
For example, a new feature that clinicians might consider to improve their ability to diagnose a particular condition
2. Reports of a New Treatment
For example, a new treatment or revised method of using a currently available treatment that improves the way we treat hair loss
3. Reports of a New Prognostic Finding
For example, a new finding either clinical or through blood tests/biopsy that helps predict the course of a patient’s hair loss
Interpreting the Value of Case Reports: Time is the Best Judge.
Case Reports are wonderful in many ways because they have the potential to stimulate additional research and thinking around the world on a particular subject. Case Reports can sometimes be the key fuel that triggered additional studies in a particular subject area.
However, case reports need to be interpreted cautiously because the results only apply to a single patient. One can not conclude that the finding will be applicable to all patients. In order to conclude that a case report has widespread applicability, further large scale studies are needed.
Take for example, the case report of sexual dysfunction from use of topical minoxidil. The study is very interesting. I can not conclude based on this study that topical minoxidil is associated with sexual dysfunction in men. However, it sets us up for further studies in this area and keep me alert to monitor these side effects in patients who use topical minoxidil. In my mind the study is extremely valuable.
Conclusion
Time will tell how any case report will go down in history as a valid or not valid contribution to the medical literature. Time is ultimately the best judge of case reports.
SHARE THIS
No Comments
CAN YOU DIAGNOSE HAIR LOSS FROM A PHOTO?
November 12, 2017
Photos: Can you diagnose hair loss from a photo?
With the widespread availability of smartphones, it’s remarkably easy nowadays to take photos. It’s also remarkably easy to post these on various forums and remarkably easily to send these via email. For these reasons, photo use is widespread among patients with hair loss. Despite this, there is a common assumption that is being made that is not correct. Many people wrongly assume that one can properly diagnose hair loss with use of a photo.
Photographs for Hair Loss: Helpful but not the entire story
There are many hair loss conditions that mimic each other. For example, I can show you a photo of androgenetic alopecia, diffuse alopecia areata, and lichen planopilaris that look identical. Can one be confident from the photo alone as to what the diagnosis is? No.
Because genetic hair loss is common, one will often be correct by guessing genetic hair loss in many photographs of hair loss. Nearly 1 out of every 2 women will have genetic hair loss by age 50 compared to approximately 1 out of 7,000 who will have (0.01%) have lichen planopilaris. Clearly, guessing that a photo is showing genetic hair loss is more likely to be the correct answer.
PRINCIPLES OF USING PHOTOS
Here are some important principles of photographs in the diagnosis of hair loss
1. One can never be 100 % confident of any diagnosis with a photo alone.
2. The lighting and background must ideally be the same if photos are to be compared.
3. The length of the hair must also be the same.
4. With a very detailed clinical history about the patient’s hair loss and medical history, one can move from being "uncertain" about the diagnosis to "somewhat confident." But that's about the maximum one can be. One can never be 100 % certain. There are many conditions that can mimic each other.
Conclusion
Photographs are wonderful to document the degree and pattern of hair loss. However, one must not assume that one can confidently determine the diagnosis of hair loss with photographs alone.
SHARE THIS
No Comments
SIDE EFFECTS FROM HAIR LOSS MEDICATIONS:
November 12, 2017
Side Effects from Hair Loss Medications: What is the Chance?
Today, I’d like to review my personal view on medication and treatment-related side effects.
1. Every single treatment has ‘potential’ adverse effects. (No treatment is risk-free).
Every treatment for hair loss has potential side effects. There is no treatment on the planet that is side effect free. How do I know that? Well, studies have shown that even patients using “placebo” treatments for their hair loss report side effects. This teaches us that any time a patient uses a treatment they have a chance to experience a side effect. Whether it’s a true side effect or not is sometimes challenging to decipher but a topic for another article.
2. No medication or treatment for hair loss should ever be prescribed or used without patients understanding the “most common" adverse events
It is critically important for patients to understand the "most common" side effects of a treatment. The purpose of delivering such information to patients is to help them with informed consent. A patient should only use a mediation if they feel that the benefits of using the medication are greater than the potential risks. It is the responsibility of the physician to transfer information about both the benefits and the risks to the patient so that the patient can offer their informed consent.
3. It is not possible to explain all the potential side effects of a medication.
Despite the important role that we as physicians have in telling our patients about the side effects of medications, it is important for patients to be aware that a given presciber can not communicate the entire list of side effects that have ever been reported. However, it is imperative for the prescriber to advice on the most common ones.
Take for example, the oral medication doxycycline. In the hair clinic, doxycycline is used for the treatment of scarring alopecia, folliculitis and a variety of other inflammatory and infectious conditions. A patient who is deciding on whether to use doxycycline or not should be made aware of the most common side effects including gastrointestinal upset, nausea, headaches, increased chance of yeast infections in women.
However, rare side effects are possible as well. For example, every year a small number of users of doxycycline around the world develop serious allergic skin reactions. It would be highly unusual for any prescriber or pharmacist to counsel a patient on this particular side effect.
4. There may be side effects that are discovered years down the road.
One must also be aware that some side effects of a medication may not be apparent during clinical trials or even during the first few years that the medication is on the market. In some cases it may take 10, 15 or even 20 years to come to understand that rarest of side effects. “Post marketing surveillance” is a term used to describe the monitoring that goes on after a medication is released on to the market. Post marketing surveillance has lead to some medications being removed from the market. One must always be aware that additional side effects of a medication may be revealed in the future through such post marketing surveillance.
5. For any potential adverse effect, one must ask “how common” that side effect is.
For some medications, the chance of adverse effects may be very low, whereas for other medications, the chance of an adverse effect may be quite high. Let’s take topical minoxidil as an example. The most common side effects and headaches, dizziness, hair shedding (in the first few months), hair growth on the face and heart palpitations. However, in deciding whether to use the medication or not, patients need to understand the overall chance of these side effects. For example, many women are extremely concerned to learn that hair growth on the face (hypertrichosis) is a potential side effect of minoxidil. it is very important from women to note that 19 out of 20 women who use minoxidil will not have any problems with hair growth on face. However, 1 out of 20 users will. This information is helpful as it encourages many women to move forward with considering the medication with knowledge that their chance of hair growth on the face is quiet low.
Conclusion
Hair loss medications have the potential to dramatically improve hair density or stop hair loss and may improve quality of life. However, anyone using a treatment, no matter what the treatment actually is, needs to be aware that every treatment has potential side effects. It is imperative that patients, together with their doctors, spend time understand how common the various side effects actually are.
SHARE THIS
No Comments
ANDROGENETIC ALOPECIA: SHOULD I START TWO TREATMENTS AT ONCE?
November 12, 2017
Androgenetic Alopecia: Should I start two treatments at once?
There are many treatments available for any particular hair loss condition. Let’s take androgenetic alopecia as an example. Individuals with androgenetic alopecia might consider topical minoxidil, oral hormone blocking medications, low level laser or even platelet rich plasma. For some types of hair loss there may be an even greater array of choices.
I’m often asked if patients should start more than one treatment at the same time. My personal view is not necessarily the right answer or the only view on the subject. However, my personal view is my view. My personal view is that whenever possible medications should not be started at the same times but rather staggered. The intervals of staggering the treatments will depend on the specific situation and the urgency of treatment.
Example
Consider the 34 year old female patient with androgenetic alopecia who is considering topical minoxidil and oral spironolactone. After a careful review of the patient’s medical history, blood tests, and examining the scalp, it is determined that both are good options for the patient. I am faced with two options: Start both or start one at a time (stagger the treatments). Let’s look at the implications of both.
Treatment Option 1: Start Minoxidil and Spironolactone at the Same Time
Both Spironolactone and Minoxidil are recommended for the patient in this situation. What needs to be considered is that minoxidil has about a 30 % chance of helping the patient. It has a 70 % chance of not being all that helpful. Spironolactone has a 40 % chance of improving hair growth. If both are started at the same time and the patient experiences and improvement it will be difficult if not impossible to know which treatment was responsible for the improvement.
Was it the minoxidil?
Was it the spironolactone?
Was it both?
Treatment Option 2: Start Minoxidil First and Introduce Spironolactone in 6-9 months.
My personal preference in this situation was to start minoxidil first. After 6-9 months of treatment (once I determine if the minoxidil is working or not), I can make a decision to add spironolactone. In this case I can have a clear sense for the entire lifetime of the patient what helps and what does not.
Comment and Conclusions
Treatments for some hair loss conditions (such as androgenetic alopecia) are life-long. A 33 year old woman who lives to 93 could potentially have 60 years of use of a given medication. From a cost perspective alone, once can potentially save a patient $ 36,000 over their lifetime by confirming that a medication does not work and should be abandoned.
SHARE THIS
No Comments
TREATMENT LADDER FOR HAIR LOSS: LOGICAL AND EVIDENCE BASED
November 12, 2017
Treatment Ladders: What is a treatment ladder?
For any type of hair loss, there are many potential treatments. Some types of hair loss may actually have 10-15 different treatments available. How does one choose which to start with? How does once decide which treatment to use if the first treatment does not work? In short, decisions on treatment are often make with use of a ‘treatment ladder.” A treatment ladder is a term that describes a logical approach to how one should progress onto different treatments if a previous one proves ineffective. In essence, a treatment ladder refers to a guide to how one should move “step by step” to additional treatments. If one treatment does not work one moves up to the next treatment on the treatment ladder. Treatment ladders helps clinicians balance effectiveness of treatment with safety.
Treatment Ladders for All Hair Loss
In my view, every hair loss condition has a treatment ladder. If there are 15 treatments for hair loss, one does not simply reach into a hat and decide on treatment based on the name that is pulled out of the hat. Also, one does not decide on treatment based on what was reported on the news, or what a neighbour or friend had benefit from. If there are 15 treatments available for a given hair loss condition, one arranges those 15 treatments on a treatment ladder for the given condition and severity of condition and moves forward with decisions on treatments based on that treatment ladder.
Treatment Ladders: Alopecia Areata as an Example.
Let’s consider a 33 year old female with 5-6 patches of alopecia areata. She comes in with a clip from the newspaper on the oral medication “tofacitinib” and wants to start it. It is true that oral tofacitinib can help alopecia areata, but is this a good option?
Well, an appropriate ladder for a 27 year old with 5-6 patches with alopecia areata could include:
TIER 1: Topical steroids and/or steroid Injections (with minoxidil)
TIER 2: Topical Immunotherapy (DPCP or Anthralin) or Prednisone Taper (with minoxidil)
TIER 3: Oral Methotrexate or Sulfasalazine or Platelet Rich Plasma (PRP)
TIER 4: Oral Tofacitinib
This is an example. The order of the ladder (or choices for treatment) will differ from physician to physician. But this would be ‘my’ ladder for a 33 year old female with alopecia areata totalling 5-6 patches. You can see that oral tofacitinib is on the list but not at the top of the list.
Conclusion
Without a treatment ladder one needs to guess if a treatment should be used or not. Treatment ladders are important in any practice and essential in my practice to ensure that evidence based principles are used wherever possible in the treatment of hair loss.
SHARE THIS
No Comments
MY HAIR WAS RIPPED OFF: WILL IT GROW BACK?
November 11, 2017
Traumatic Hair Pulling: Full Regrowth May or May Not Occur
I am often asked if hair that is pulled out forcefully will regrow. Examples of this are the pulling of hair by children on the playground, hair getting caught in doors, machines etc or cases of hair pulling during assault or abuse-related situations (for example domestic abuse).
Without actually seeing the scalp, and knowing details of the patient's story, it is impossible to determine if hair will or will not grow back in any particular case. This requires an in person examination so that the scalp can be properly examined.
Hair regrowth is not a guarantee
There is no guarantee that hair regrowth will occur. One will know in 6-9 months if they will acheive full regrowth or not because that is how long it takes for hair to grow back following any type of injury.
It is certainly possible for repeated pulling to give permanent hair loss. However, in the vast majority of cases where hair is pulled from the scalp, hair grows back. If you or I were to reach up a pluck a hair, it will grow back. However, if pulling is repeated many times or is excessive with bleeding a greater chance exists for scarring to develop. Hair pulling that is accompanied by injury to the skin layers (i.e. that creates an actual wound) has a markedly increased chance of being associated with permanent scarring. It is such scarring that blocks the regrowth of hair. Scar tissue is permanent and, if present, generally destroys stems cells.
Anyone with concerns about incomplete growth after episodes of hair pulling should see a physician who specializes in hair loss for consideration of a scalp biopsy.
SHARE THIS
No Comments
Newer
Older
SUBSCRIBE TO RECEIVE NEW BLOGS BY EMAIL
SIGN UP
We respect your privacy. Your information is not shared.
BLOGS BY TOPIC
ACell (1)
ARTAS Robotic FUE (2)
Age Considerations (3)
Age-related hair loss (17)
Alopecia Areata (32)
Bimatoprost (Latisse) (2)
Biopsies (2)
Body Hair Transplants (1)
Breakage (2)
Camouflage (1)
Causes of Hair Loss (40)
Children's Hair Loss (6)
Cloning (1)
Crown Hair Loss (8)
Density (5)
Diagnostic Tests (12)
Diet (6)
Donor Area (7)
Drugs (3)
Drugs (Medications) (39)
Emotions/Impact Hair Loss (6)
Ethics (2)
Ethnic Hair Loss (6)
Eyebrow Hair Loss (5)
FUE (7)
FUE vs FUT (5)
Facial Hair Loss (1)
Female Hair Loss (8)
Finasteride (7)
Frontal Hair Line (9)
Genetics of hair loss (17)
Grey Hair (1)
Hair Dye (2)
Hair Growth (14)
Itching (1)
Male pattern balding (30)
Men (28)
Minoxidil (6)
Myths (Hair Loss Myths) (5)
New Treatments (2)
Platelet rich plasma (PRP (2)
Platelet rich plasma -PRP (2)
Pre-op (2)
Recipient Area (2)
Research (56)
Robotic FUE (2)
Scalp issues (5)
Scalp micro pigmentation (1)
Scarring (5)
Scarring Alopecia (29)
Seborrheic dermatitis (1)
Shampoos (4)
Shedding (16)
Supplements (1)
Surgical Techniques (7)
Systemic Conditions (7)
Terms (28)
Trends in Hair Transplant (2)
Videos (12)
Vitamins (1)
Wigs & Camouflage (2)
Women (41)
- See more at: https://donovanmedical.com/hair-blog/#sthash.fLXlC8sL.dpuf
0 notes
Text
DENSITY CHANGES IN CTE VS AGA OVER TIME
November 22, 2017
Chronic Telogen Effluvium: How does density change over time?
Chronic Telogen Effluvium (CTE) and Androgenetic alopecia (AGA) are both commonly encountered diagnoses in women age 40-70 years. They are however, very different conditions.
AGA: Androgenetic Alopecia
AGA presents with hair thinning and sometimes increased daily shedding as well. The loss of hair is sometimes just frontal in location or the crown but can be diffuse (all over). A key to the diagnosis is recognition of the progressive reduction in the caliber (diameter) of hairs.
CTE: Chronic Telogen Efflvuium
Patients with CTE can appear to have a similar story. Many have a sudden onset of shedding. The shedding is diffuse. The temples may be particularly affected with reduced density to a much more significant degree than seen in AGA. Reduced hair caliber (miniaturization) is not a feature of CTE. CTE has periods where shedding appears to slow considerably or even stop. When one follows these conditions for many years there is a realization of another important difference: Density in CTE reduces initially but then plateaus and does not reduce further. Density in AGA continues to drop off over time. These points are illustrated in the graph.
SHARE THIS
No Comments
MINOXIDIL AND SHEDDING: WHY DOES MINOXIDIL CAUSE SHEDDING?
November 21, 2017
Why does minoxidil cause shedding?
Minoxidil commonly causes increased hair shedding in the first 6-8 weeks of use (and sometimes a bit longer).
Every human has hairs on their scalp that are destined to come out next week, the week after and the week after that. When minxodil is applied to the scalp, many of those hairs simply come out earlier than they are supposed to. This is termed "immediate telogen release" and is the main mechanism by which minoxidil causes shedding in the first 2 months of use.
SHARE THIS
No Comments
HAIR BREAKAGE IN ALOPECIA AREATA
November 18, 2017
Why do hairs break in alopecia areata?
Hair breakage is a common finding in active alopecia areata (an autoimmune hair loss condition). Inflammation occurring deep down in the scalp at the level of the bulb prevents strong hairs from being produced. The result is hair breakage. Some of hairs that are shed are of course full length hairs. But in patients with very active AA, a close examination of shed hairs will reveal that many are broken.
SHARE THIS
No Comments
VIBRATIONAL ANESTHESIA: A KEY TOOL FOR THE HAIR SPECIALIST
November 18, 2017
Vibration and Pain Sensation:
Injections are a key part of being a hair loss specialist. I perform steroid injections, PRP injections and use a variety of local anesthetics to freeze (numb) the scalp (ie biopsies, hair transplants). One should strive to perform injections in as pain-free manner as possible. There are several ways to limit the pain of injections including going slowly with administration, using small gauge needles, adjusting pH, and warming solutions to be injected. I also use variety of vibration devices to distract pain during injections.
Vibration helps block the perception of pain. According to the Melzack & Wall's "gate control" theory of pain, nerve fibers known as A-β nerve fibers (which transmit information from vibration & touch receptors in the skin) stimulate inhibitory interneurons in the spinal cord, which in turn decrease the amount of pain signals generated from A-δ and C fibers to the brain. This photo shows two vibration devices I use at present. Other helpful methods of vibration include scratching the skin in the area where one is injecting.
SHARE THIS
No Comments
TAPERED AND EXCLAMATION MARK HAIRS IN ALOPECIA AREATA
November 18, 2017
Tapered & Exclamation Hairs in AA indicate Activity
Tapered Hairs
Tapered hairs are frequently seen in patients with small circular patches of alopecia areata. In contrast to 4-5 mm exclamation mark hairs (see next post), tapered hairs are long and typically as long as neighboring hairs. As the hair enters into the skin it becomes much thinner. At the bottom of the tapered hair (deep under the skin) is inflammation.
Tapered are important findings in patients with patchy stage alopecia areata as they tell us that the condition is active and that anti-inflammatory type treatments (such as cortisone injections) are likely to help. The above photo shows several tapered hairs (TH).
Exclamation Hairs
Exclamation mark hairs are frequently seen in patients with small circular patches of alopecia areata. These hairs a short 4-5 mm hairs and represent broken hairs. The top is thick and the end is often frayed. As the hair enters into the skin it becomes much thinner. At the bottom of the exclamation mark hair (deep under the skin) is inflammation. Exclamation mark hairs are important findings in patients with patchy stage alopecia areata as they tell us that the condition is active and that anti-inflammatory type treatments (such as cortisone injections) are likely to help. The photo shows several exclamation mark hairs (EMH).
SHARE THIS
No Comments
CHRONIC TELOGEN EFFLUVIUM (CTE)
November 18, 2017
Misdiagnoses common with CTE
Chronic telogen effluvium (CTE) is an interesting and frequently misdiagnosed hair shedding condition. Many patients with androgenetic alopecia, acute telogen effluvium and even alopecia areata are diagnosed as having chronic telogen effluvium.
How does CTE present?
Most patients with true CTE are 40-65 and present with sudden onset of increased hair shedding that fluctuates in intensity. Some days there is alot of shedding. Some days very little. Many patients have scalp pain (trichodynia) which may correlate with the shedding episodes. Patients with CTE often appear to have good hair density to an outsider which makes the condition frustrating for the patient. A careful history and exam can confirm the diagnosis in many cases. Follicular miniaturization is not a feature unless genetic hair loss is present too. A hair collection or scalp biopsy is useful in more challenging cases.
SHARE THIS
No Comments
ANDROGEN BLOCKADE FOR FPHL: CAN I USE MORE THAN I MEDICATION?
November 16, 2017
Androgen blockade has the potential to be help female pattern hair loss. Caution is needed with any hormone blocker due to significant harm that can come to a developing baby were a woman to become pregnant on any hormone blocker. For this reason they are frequently used with various strict contraceptive methods.
Hormone Blocking Medications for FPHL
Female Pattern Hair Loss (also called female androgenetic alopecia) affects 40 % of women by age 50. There are a variety of treatment options including minxodil, anti-androgens, laser and PRP.
Anti-androgens can help some women with female pattern hair loss. A long list of anti-androgens exist including spironolactone, finasteride, cyproterone acetate, flutamide, dutasteride. The combination of anti-androgens can sometimes work even better than one alone provided the patient actually has a truly androgen responsive hair loss condition. Most men do. But not all women have a form of FPHL that is truly responsive to anti-androgens.
Anti-androgen Side Effects
The decision to use two or more anti-androgens must always be weighed against potential side effects. The combination of androgen blocking pills has the potential to be associated with side effects such as depression, worsening fatigue, breast tenderness, breast enlargement, weight gain, decreased libido.
SHARE THIS
No Comments
TREATING FEMALE PATTERN HAIR LOSS: OPTIONS FOR WOMEN OVER 60
November 16, 2017
Treatments for AGA in Women over 60
I'm often asked about treatment options for women over 60 who present with a diagnosis of androgenetic alopecia (female pattern hair loss). There is some degree of confusion as well as misconceptions which exist in this subject area.
My approach in this situation is to first confirm the diagnosis and then base treatment decisions according to the patient's medical history. The importance of the first step can not be overemphasized.
1: Confirming the Diagnosis
It is extremely important to confirm the diagnosis and ensure that a) another diagnosis is not more appropriate and b) to determine whether other diagnoses are also present. A patient need not have only one diagnosis.
A. Senescent Alopecia
Women who present with hair thinning in their 60s and 70s with no evidence whatsoever of thinning in the 30s, 40s or 50s may have senescent alopecia (age related hair loss) rather than true androgenetic alopecia. This distinction is important as senescent alopecia is less likely to be androgen-driven and therefore responds less to antiandrogens such as finasteride. The main treatment for senescent alopecia is minoxidil although agents such as low level laser and less commonly finasteride can be considered.
I typically ask patients if their hair density on their 50th birthday was more or less the same as their 30th birthday. If that answer is yes one should at least consider the possibility that senescent alopecia or even another diagnosis other than androgenetic alopecia is present.
B. Scarring Alopecia
Scarring alopecias are far more common than we currently diagnose. They range from subtle asymptomatic scarring alopecia to fibrosing alopecia in a pattern distribution to markedly symptomatic lichen planopilaris. Scarring alopecias are easy to miss but need to be considered in all patients with sudden onset of itchy hair loss or a more rapid decline in density from what they may have experienced in the past. A biopsy can help better evaluate these conditions.
C. Hair shedding issues
Both acute and chronic telogen effluvium (CTE) need to be considered in women with hair concerns. Stress, thyroid problems, new illnesses and newly prescribed medications can all contribute to increased hair shedding and hair loss. Anyone with new shedding needs a very detailed examination and workup not only by the dermatologist but by the family physician. Blood tests are especially as is a full medical examination. One must also ensure that routine mammograms and colonoscopies are up to date.
Chronic telogen effluvium (CTE) is among the more challenging to diagnose conditions. Patients present with increased shedding that waxes and wanes. To an outsider it generally appears that the person has fairly good density. A hair collection or biopsy can help with the diagnosis.
Treatment Options
The main treatment options for patients with confirmed androgenetic alopecia is minoxidil, finasteride and low level laser. If the pattern of hair loss is localized frontal loss, and donor density in the occipital scalp is good, a hair transplant can be considered as well.
Minoxidil is formally approved for women 18-65. It may, of course, be used off label for women over 65 with proper evaluation by a physician. Women with heart disease, heart failure or previous heart attacks for example may or may not be good candidates for minoxidil. One is not obligated to use the full recommended dose of minoxidil. Starting with one-quarter or one-half the recommended amount is often a good way to ease in to the treatment in patients with underlying medical issues.
Finasteride may also be a good option. Studies support the notion that higher doses of 2.5 mg and 5 mg are needed for post-menopausal women and doses of 1 mg are ineffective. Finasteride is relatively contraindicated in women with previous history of breast, ovarian or gynaecological cancer. Given the rare effects of finasteride on mood, this medication is also relatively contraindicated in women with depression.
Low level laser therapies are safe but may be less effective than minoxidil or finasteride. A number of laser devices are available in the market for use by patients in their home. None have proven superior to another and so one must balance cost with ease of use. A helmet based device may be easier for some compared to the hand-held devices.
Scalp Inflammation. Scalp inflammation must be attended to fully when caring for patients with AGA. Many women with AGA have seborrheic dermatitis and this is best controlled with periodic use of an anti-dandruff shampoo. I frequently prescribe a trial of a mild cortisone lotion if there is scalp redness if the redness does not respond to anti-dandruff therapies.
SHARE THIS
No Comments
7 HAIR TRANSPLANT MYTHS
November 12, 2017
7 Common Myths in Hair Transplantation
Hair transplantation is among the mostly consistently successful and life-changing of all the hair loss therapies. Hair transplants nowadays can look extremely natural (when performed by skilled teams). However, there are a number of myths that are infrequently talked about when it comes to hair transplantation. These can sometimes be overlooked.
1. Transplanted hair lasts forever
It’s a common myth that transplanted hair moved during a hair transplant last forever. Fortunately, most hairs that are transplanted do generally remain in their new location forever. However, anyone is has followed a hair transplant patient for 10, 20 or 30 years will tell you that the same number of hairs that were put in are not always remaining over time. Most will stay - but not all
There are many reasons why hairs transplanted hairs don’t always last forever. For one, donor hair is not always completely resistant to balding in all men. In fact, it’s a spectrum, from some men who have very little to no balding in their "donor area" (at the back of the scalp) to men who have considerable thinning in the donor area over time (ie. men with DUPA are the extreme). In addition, the medical community has not rigorously studied long term the immunological and physiological changes that happen to transplanted hairs over extended periods of time.
Nevertheless, there is no arguing that transplanted hairs last forever. It holds true for a high proportion of men and women but not all. We hope they last forever are and they seem to be in many men. However, a proportion of transplanted hairs slowly disappear over decades in some men.
2. Only one hair transplant surgery session is needed
From the time male balding and female thinning announces its presence in any patient, it always progresses. While it is true that androgenetic alopecia can stop or slow for periods of months to a year or two, androgenetic alopecia by definition never stops. Anyone who gets a hair transplant must assume that existing hair in an area will slowly thin over time. If a patient is under 30 years of age, he (or she) must assume that another hair transplant will likely be needed if he wishes to maintain his current look into his 50s and 60s.
3. A hair transplant procedure is always a great success
Hair transplants are generally quite successful. That's why they are popular! With the right patient, and a skilled team, the chances of success are high. Unfortunately, hair transplant don’t always work out as successfully as one might hope. There is not an experienced hair transplant surgeon in the world who can state that he or she has never had a patient who did not grow as much hair as they hoped. The reasons why this occurs is quite varied - but ranges from "patient factors" (post op care, smoking, unrecognized scalp diseases), to "surgeon-related" factors (surgeon skill, skill of the technicians handling the grafts). Sometimes one never knows the exact reason why things don’t turn out. In the hair transplant field, this is called the ‘X factor.’
4. A hair transplant is a one-day event
A hair transplant procedure itself is a one day event, but the actual procedure when one considers the time from the surgery to the time where the patient feels back to normal ranges from a few days to a few months. The actual recovery time varies from patient to patient and varies based on the size of the surgery.
In general, the post op recovery period is longer for FUT procedures than FUE and longer for patients that require more grafts. Patients who don’t require shaving for FUE procedures and have limited baldness, may find that 2-3 days is sufficient to feel back to their usual self. However, a patient whose scalp is shaved completely for a large 3000-4000 FUE procedures may find that it takes just a few days to “feel good” but takes 3-4 weeks before he feel confident to go to work. Depending on his occupation, he may or may not feel comfortable at work for an extended period. A patient who sees clients on a daily basis at work may not feel completely comfortable seeing his clients even after 2 weeks post op from a 4000 graft FUE. This needs to be taken into account. A hair transplant is not always a ‘one day thing.’
5. A hair transplant is always an option for treating hair loss
It’s a myth that a hair transplant is always an option for an individual with hair loss. Some patients may be too young, some have medical issues that preclude surgery, and some have a type of hair loss that also will not be successful if a hair transplant were performed. Hair transplants aren't for everyone.
6. There are no complications to a hair transplant
Hair transplants are quite safe. But it’s a bit of a stretch to say that they are without complication. Patients may have have redness, swelling and crusting post operatively. In general, the recovery in FUE procedures is much easier than FUT procedures. But there are rare complications in hair transplant surgery that include long lasting nerve pain (more in FUT than FUE procedures) and persistent scalp redness. Unless a physician is carefully monitoring the procedure, a patient can even get sick. The hair transplant community tends to shy away from calling hair transplant procedures a 'surgery' in order to make the procedure more patient friendly - but make no mistake a hair transplant is a surgery.
7. You will regain the hair density of your youth
A hair transplant is a surgical procedure which involved moving anywhere from 10 to 10,000 hairs into an area of balding. If an area of hair loss is small, it may be possible to build some very nice density in the area – but the density is generally less than it once was. For example, in a patient who is very bald, a density of 35-40 follicular units per square centimeter will typically be created. This area likely had a density of 90 or more follicular units per square centimeter at one time years earlier. Therefore, it is generally the norm for a hair transplant to create results that are less dense than the original density. A skilled surgeon can often help make 35-40 follicular units look like the original density. However, photos and videos of patients with amazingly thick and dense hair following their procedure may not always be accurate.
SHARE THIS
No Comments
NAAF VANCOUVER
November 12, 2017
The NAAF Vancouver Support Group
Alopecia areata is an autoimmune condition that affects about 50,000 Canadians. The condition affects males and females of all ages and can have a tremendous impact on the lives of both patients and their families. Support groups play an important role in imparting accurate information to patients and families with new diagnoses as well as those who have had the condition for many years. These groups connect people at different stages of coping and provides a network of support.
The National Alopecia Areata Foundation (NAAF) was founded 25 years ago and has a number of patient support groups throughout the United States and Canada. I’m honored to join the NAAF Vancouver Support Group in 2018 as Medical Advisor. Four meetings are planned for the year in Spring, Summer, Fall and Winter in Vancouver. Individuals with alopecia areata interested in attending these sessions may contact the NAAF for information on dates, times and location or contact our office.
SHARE THIS
No Comments
AGE 50: AN IMPORTANT CUT OFF FOR DIAGNOSING HAIR LOSS
November 12, 2017
The Cut off of 50: Why it matters in the diagnosis of hair loss in Older Individuals ?
Any birthday is special. The 50th birthday is an important cut off in the diagnosis of many hair diseases. An important principle of diagnosing hair loss in men and women over 60 comes from understanding what density of hair a patient had at age 50.
A true or false question
For anyone over 60, I always ask patients to help me with a true or false question. I generally ask it in the following way “Is this statement true or false: My hair density at age 50 was about the same as it was at age 30.”
This is such an important question - especially if the patient replies “TRUE”. Men and women who develop hair loss in their 60s and 70s but who report that their density age 50 was quite good have a high likelihood of having another diagnosis besides simply genetic hair loss. Of course genetic hair loss is a possibility and it’s possible the patient does not really have a good recall of their hair density at age 50. Nevertheless, there are several conditions that need to be considered in somwone with good thick hair at age 50 and hair loss in the 60s”
1. Scarring Alopecia (especially Lichen Planopilaris)
2. Senescent Hair Loss
3. Diffuse Alopecia Areata
4. Hair Shedding Disorders
Final Comment:
Patients in their 60s and 70s who tell me they had thick hair at age 50 and that it was the same thickness as age 30 often have an interesting array of hair loss conditions. One should not default to diagnosing genetic hair loss in these situations because that diagnosis may be relatively unlikely in this unique situation.
SHARE THIS
No Comments
CASE REPORTS IN THE RESEARCH WORLD: ARE THEY HELPFUL?
November 12, 2017
Case Reports in Hair Loss: Cautiously Optimistic.
A Case Report is a published medical study which presents a particular finding as it relates to a single patient. Common Examples of Case Reports are:
1. Reports of a New Diagnostic Finding
For example, a new feature that clinicians might consider to improve their ability to diagnose a particular condition
2. Reports of a New Treatment
For example, a new treatment or revised method of using a currently available treatment that improves the way we treat hair loss
3. Reports of a New Prognostic Finding
For example, a new finding either clinical or through blood tests/biopsy that helps predict the course of a patient’s hair loss
Interpreting the Value of Case Reports: Time is the Best Judge.
Case Reports are wonderful in many ways because they have the potential to stimulate additional research and thinking around the world on a particular subject. Case Reports can sometimes be the key fuel that triggered additional studies in a particular subject area.
However, case reports need to be interpreted cautiously because the results only apply to a single patient. One can not conclude that the finding will be applicable to all patients. In order to conclude that a case report has widespread applicability, further large scale studies are needed.
Take for example, the case report of sexual dysfunction from use of topical minoxidil. The study is very interesting. I can not conclude based on this study that topical minoxidil is associated with sexual dysfunction in men. However, it sets us up for further studies in this area and keep me alert to monitor these side effects in patients who use topical minoxidil. In my mind the study is extremely valuable.
Conclusion
Time will tell how any case report will go down in history as a valid or not valid contribution to the medical literature. Time is ultimately the best judge of case reports.
SHARE THIS
No Comments
CAN YOU DIAGNOSE HAIR LOSS FROM A PHOTO?
November 12, 2017
Photos: Can you diagnose hair loss from a photo?
With the widespread availability of smartphones, it’s remarkably easy nowadays to take photos. It’s also remarkably easy to post these on various forums and remarkably easily to send these via email. For these reasons, photo use is widespread among patients with hair loss. Despite this, there is a common assumption that is being made that is not correct. Many people wrongly assume that one can properly diagnose hair loss with use of a photo.
Photographs for Hair Loss: Helpful but not the entire story
There are many hair loss conditions that mimic each other. For example, I can show you a photo of androgenetic alopecia, diffuse alopecia areata, and lichen planopilaris that look identical. Can one be confident from the photo alone as to what the diagnosis is? No.
Because genetic hair loss is common, one will often be correct by guessing genetic hair loss in many photographs of hair loss. Nearly 1 out of every 2 women will have genetic hair loss by age 50 compared to approximately 1 out of 7,000 who will have (0.01%) have lichen planopilaris. Clearly, guessing that a photo is showing genetic hair loss is more likely to be the correct answer.
PRINCIPLES OF USING PHOTOS
Here are some important principles of photographs in the diagnosis of hair loss
1. One can never be 100 % confident of any diagnosis with a photo alone.
2. The lighting and background must ideally be the same if photos are to be compared.
3. The length of the hair must also be the same.
4. With a very detailed clinical history about the patient’s hair loss and medical history, one can move from being "uncertain" about the diagnosis to "somewhat confident." But that's about the maximum one can be. One can never be 100 % certain. There are many conditions that can mimic each other.
Conclusion
Photographs are wonderful to document the degree and pattern of hair loss. However, one must not assume that one can confidently determine the diagnosis of hair loss with photographs alone.
SHARE THIS
No Comments
SIDE EFFECTS FROM HAIR LOSS MEDICATIONS:
November 12, 2017
Side Effects from Hair Loss Medications: What is the Chance?
Today, I’d like to review my personal view on medication and treatment-related side effects.
1. Every single treatment has ‘potential’ adverse effects. (No treatment is risk-free).
Every treatment for hair loss has potential side effects. There is no treatment on the planet that is side effect free. How do I know that? Well, studies have shown that even patients using “placebo” treatments for their hair loss report side effects. This teaches us that any time a patient uses a treatment they have a chance to experience a side effect. Whether it’s a true side effect or not is sometimes challenging to decipher but a topic for another article.
2. No medication or treatment for hair loss should ever be prescribed or used without patients understanding the “most common" adverse events
It is critically important for patients to understand the "most common" side effects of a treatment. The purpose of delivering such information to patients is to help them with informed consent. A patient should only use a mediation if they feel that the benefits of using the medication are greater than the potential risks. It is the responsibility of the physician to transfer information about both the benefits and the risks to the patient so that the patient can offer their informed consent.
3. It is not possible to explain all the potential side effects of a medication.
Despite the important role that we as physicians have in telling our patients about the side effects of medications, it is important for patients to be aware that a given presciber can not communicate the entire list of side effects that have ever been reported. However, it is imperative for the prescriber to advice on the most common ones.
Take for example, the oral medication doxycycline. In the hair clinic, doxycycline is used for the treatment of scarring alopecia, folliculitis and a variety of other inflammatory and infectious conditions. A patient who is deciding on whether to use doxycycline or not should be made aware of the most common side effects including gastrointestinal upset, nausea, headaches, increased chance of yeast infections in women.
However, rare side effects are possible as well. For example, every year a small number of users of doxycycline around the world develop serious allergic skin reactions. It would be highly unusual for any prescriber or pharmacist to counsel a patient on this particular side effect.
4. There may be side effects that are discovered years down the road.
One must also be aware that some side effects of a medication may not be apparent during clinical trials or even during the first few years that the medication is on the market. In some cases it may take 10, 15 or even 20 years to come to understand that rarest of side effects. “Post marketing surveillance” is a term used to describe the monitoring that goes on after a medication is released on to the market. Post marketing surveillance has lead to some medications being removed from the market. One must always be aware that additional side effects of a medication may be revealed in the future through such post marketing surveillance.
5. For any potential adverse effect, one must ask “how common” that side effect is.
For some medications, the chance of adverse effects may be very low, whereas for other medications, the chance of an adverse effect may be quite high. Let’s take topical minoxidil as an example. The most common side effects and headaches, dizziness, hair shedding (in the first few months), hair growth on the face and heart palpitations. However, in deciding whether to use the medication or not, patients need to understand the overall chance of these side effects. For example, many women are extremely concerned to learn that hair growth on the face (hypertrichosis) is a potential side effect of minoxidil. it is very important from women to note that 19 out of 20 women who use minoxidil will not have any problems with hair growth on face. However, 1 out of 20 users will. This information is helpful as it encourages many women to move forward with considering the medication with knowledge that their chance of hair growth on the face is quiet low.
Conclusion
Hair loss medications have the potential to dramatically improve hair density or stop hair loss and may improve quality of life. However, anyone using a treatment, no matter what the treatment actually is, needs to be aware that every treatment has potential side effects. It is imperative that patients, together with their doctors, spend time understand how common the various side effects actually are.
SHARE THIS
No Comments
ANDROGENETIC ALOPECIA: SHOULD I START TWO TREATMENTS AT ONCE?
November 12, 2017
Androgenetic Alopecia: Should I start two treatments at once?
There are many treatments available for any particular hair loss condition. Let’s take androgenetic alopecia as an example. Individuals with androgenetic alopecia might consider topical minoxidil, oral hormone blocking medications, low level laser or even platelet rich plasma. For some types of hair loss there may be an even greater array of choices.
I’m often asked if patients should start more than one treatment at the same time. My personal view is not necessarily the right answer or the only view on the subject. However, my personal view is my view. My personal view is that whenever possible medications should not be started at the same times but rather staggered. The intervals of staggering the treatments will depend on the specific situation and the urgency of treatment.
Example
Consider the 34 year old female patient with androgenetic alopecia who is considering topical minoxidil and oral spironolactone. After a careful review of the patient’s medical history, blood tests, and examining the scalp, it is determined that both are good options for the patient. I am faced with two options: Start both or start one at a time (stagger the treatments). Let’s look at the implications of both.
Treatment Option 1: Start Minoxidil and Spironolactone at the Same Time
Both Spironolactone and Minoxidil are recommended for the patient in this situation. What needs to be considered is that minoxidil has about a 30 % chance of helping the patient. It has a 70 % chance of not being all that helpful. Spironolactone has a 40 % chance of improving hair growth. If both are started at the same time and the patient experiences and improvement it will be difficult if not impossible to know which treatment was responsible for the improvement.
Was it the minoxidil?
Was it the spironolactone?
Was it both?
Treatment Option 2: Start Minoxidil First and Introduce Spironolactone in 6-9 months.
My personal preference in this situation was to start minoxidil first. After 6-9 months of treatment (once I determine if the minoxidil is working or not), I can make a decision to add spironolactone. In this case I can have a clear sense for the entire lifetime of the patient what helps and what does not.
Comment and Conclusions
Treatments for some hair loss conditions (such as androgenetic alopecia) are life-long. A 33 year old woman who lives to 93 could potentially have 60 years of use of a given medication. From a cost perspective alone, once can potentially save a patient $ 36,000 over their lifetime by confirming that a medication does not work and should be abandoned.
SHARE THIS
No Comments
TREATMENT LADDER FOR HAIR LOSS: LOGICAL AND EVIDENCE BASED
November 12, 2017
Treatment Ladders: What is a treatment ladder?
For any type of hair loss, there are many potential treatments. Some types of hair loss may actually have 10-15 different treatments available. How does one choose which to start with? How does once decide which treatment to use if the first treatment does not work? In short, decisions on treatment are often make with use of a ‘treatment ladder.” A treatment ladder is a term that describes a logical approach to how one should progress onto different treatments if a previous one proves ineffective. In essence, a treatment ladder refers to a guide to how one should move “step by step” to additional treatments. If one treatment does not work one moves up to the next treatment on the treatment ladder. Treatment ladders helps clinicians balance effectiveness of treatment with safety.
Treatment Ladders for All Hair Loss
In my view, every hair loss condition has a treatment ladder. If there are 15 treatments for hair loss, one does not simply reach into a hat and decide on treatment based on the name that is pulled out of the hat. Also, one does not decide on treatment based on what was reported on the news, or what a neighbour or friend had benefit from. If there are 15 treatments available for a given hair loss condition, one arranges those 15 treatments on a treatment ladder for the given condition and severity of condition and moves forward with decisions on treatments based on that treatment ladder.
Treatment Ladders: Alopecia Areata as an Example.
Let’s consider a 33 year old female with 5-6 patches of alopecia areata. She comes in with a clip from the newspaper on the oral medication “tofacitinib” and wants to start it. It is true that oral tofacitinib can help alopecia areata, but is this a good option?
Well, an appropriate ladder for a 27 year old with 5-6 patches with alopecia areata could include:
TIER 1: Topical steroids and/or steroid Injections (with minoxidil)
TIER 2: Topical Immunotherapy (DPCP or Anthralin) or Prednisone Taper (with minoxidil)
TIER 3: Oral Methotrexate or Sulfasalazine or Platelet Rich Plasma (PRP)
TIER 4: Oral Tofacitinib
This is an example. The order of the ladder (or choices for treatment) will differ from physician to physician. But this would be ‘my’ ladder for a 33 year old female with alopecia areata totalling 5-6 patches. You can see that oral tofacitinib is on the list but not at the top of the list.
Conclusion
Without a treatment ladder one needs to guess if a treatment should be used or not. Treatment ladders are important in any practice and essential in my practice to ensure that evidence based principles are used wherever possible in the treatment of hair loss.
SHARE THIS
No Comments
MY HAIR WAS RIPPED OFF: WILL IT GROW BACK?
November 11, 2017
Traumatic Hair Pulling: Full Regrowth May or May Not Occur
I am often asked if hair that is pulled out forcefully will regrow. Examples of this are the pulling of hair by children on the playground, hair getting caught in doors, machines etc or cases of hair pulling during assault or abuse-related situations (for example domestic abuse).
Without actually seeing the scalp, and knowing details of the patient's story, it is impossible to determine if hair will or will not grow back in any particular case. This requires an in person examination so that the scalp can be properly examined.
Hair regrowth is not a guarantee
There is no guarantee that hair regrowth will occur. One will know in 6-9 months if they will acheive full regrowth or not because that is how long it takes for hair to grow back following any type of injury.
It is certainly possible for repeated pulling to give permanent hair loss. However, in the vast majority of cases where hair is pulled from the scalp, hair grows back. If you or I were to reach up a pluck a hair, it will grow back. However, if pulling is repeated many times or is excessive with bleeding a greater chance exists for scarring to develop. Hair pulling that is accompanied by injury to the skin layers (i.e. that creates an actual wound) has a markedly increased chance of being associated with permanent scarring. It is such scarring that blocks the regrowth of hair. Scar tissue is permanent and, if present, generally destroys stems cells.
Anyone with concerns about incomplete growth after episodes of hair pulling should see a physician who specializes in hair loss for consideration of a scalp biopsy.
SHARE THIS
No Comments
Newer
Older
SUBSCRIBE TO RECEIVE NEW BLOGS BY EMAIL
SIGN UP
We respect your privacy. Your information is not shared.
BLOGS BY TOPIC
ACell (1)
ARTAS Robotic FUE (2)
Age Considerations (3)
Age-related hair loss (17)
Alopecia Areata (32)
Bimatoprost (Latisse) (2)
Biopsies (2)
Body Hair Transplants (1)
Breakage (2)
Camouflage (1)
Causes of Hair Loss (40)
Children's Hair Loss (6)
Cloning (1)
Crown Hair Loss (8)
Density (5)
Diagnostic Tests (12)
Diet (6)
Donor Area (7)
Drugs (3)
Drugs (Medications) (39)
Emotions/Impact Hair Loss (6)
Ethics (2)
Ethnic Hair Loss (6)
Eyebrow Hair Loss (5)
FUE (7)
FUE vs FUT (5)
Facial Hair Loss (1)
Female Hair Loss (8)
Finasteride (7)
Frontal Hair Line (9)
Genetics of hair loss (17)
Grey Hair (1)
Hair Dye (2)
Hair Growth (14)
Itching (1)
Male pattern balding (30)
Men (28)
Minoxidil (6)
Myths (Hair Loss Myths) (5)
New Treatments (2)
Platelet rich plasma (PRP (2)
Platelet rich plasma -PRP (2)
Pre-op (2)
Recipient Area (2)
Research (56)
Robotic FUE (2)
Scalp issues (5)
Scalp micro pigmentation (1)
Scarring (5)
Scarring Alopecia (29)
Seborrheic dermatitis (1)
Shampoos (4)
Shedding (16)
Supplements (1)
Surgical Techniques (7)
Systemic Conditions (7)
Terms (28)
Trends in Hair Transplant (2)
Videos (12)
Vitamins (1)
Wigs & Camouflage (2)
Women (41)
- See more at: https://donovanmedical.com/hair-blog/#sthash.56PYXZOc.dpuf
0 notes
Photo

Chronic telogen effluvium (CTE) is an interesting and frequently misdiagnosed hair shedding condition. Many patients with androgenetic alopecia, acute telogen effluvium and even alopecia areata are diagnosed as having chronic telogen effluvium. Most patients with true CTE are 40-65 and present with sudden onset of increased hair shedding that fluctuates in intensity. Some days there is alot of shedding. Some days very little. Many patients have scalp pain (trichodynia) which may correlate with the shedding episodes. Patients with CTE often appear to have good hair density to an outsider which makes the condition frustrating for the patient. A careful history and exam can confirm the diagnosis in many cases. Follicular miniaturization is not a feature unless genetic hair loss is present too. A hair collection or scalp biopsy is useful in more challenging cases. #hair
0 notes