#telehealth app development company
Explore tagged Tumblr posts
Text
Telemedicine in 2024: What's Changing?
The future is bright for forward-thinking healthcare organizations that make strategic investments in telemedicine capabilities today. At Consagous Technologies, a leading telemedicine app development company, we are at the forefront of designing and implementing seamlessly integrated, highly intuitive telemedicine application development solutions for healthcare providers across the country. Our full-stack engineering expertise and user-centric approach help maximize clinical value and patient engagement.
#telemedicine app development#telemedicine application development#telehealth app development company
0 notes
Text
In today's world of healthcare, there's a game-changing force making waves: telemedicine. It's like a digital lifeline, linking up patients and healthcare pros in ways we couldn't have imagined a short while back.
No recent example highlights this better than the Covid-19 era, where in-person meetings have become riskier.
Now, let's take a closer look. Picture this: rural and underserved communities, often feel like islands cut off from regular healthcare.
They deal with challenges like distance, not enough resources, and a shortage of medical facilities. Imagine a simple check-up turning into a puzzle or getting vital medical advice becoming a journey. That's the reality for many in these areas.
But here's the exciting part—telemedicine steps in as a solution, breaking down these barriers and creating a new route to healthcare that includes everyone.
Telemedicine isn't just a cost-saver; it simplifies the entire hospital workflow. It acts like a GPS for keeping track of patient’s post-treatment, making recovery management straightforward.
Keep reading, as this blog briefs about telemedicine and its need in Healthcare. Significant capabilities, features, barriers, and applications are discussed briefly.
The Promise of Telemedicine
Telemedicine is more than just a tool; it’s a real way to change healthcare in places that are hard to reach. Here’s why it’s so important.
Cost-Effective Healthcare: Telemedicine helps people in rural areas save money. It cuts costs and makes healthcare cheaper. Think about getting great medical help without a big bill. That’s what telemedicine offers—good care without spending a lot.
Closing the Health Gap: In some places, getting good healthcare can be hard. Telemedicine can help with this. It removes the problem of distance, making sure everyone, whether in a busy city or a quiet village, can get good healthcare. It’s like having the doctor come to you, no matter where you are.
So, whether you’re in the middle of the countryside or in the heart of the city, telemedicine keeps its promise. It provides affordable healthcare and connects us all to quality medical help.
Benefits of Telemedicine in Rural Areas
Let’s look at the real benefits of telemedicine in rural areas—it’s not just an idea, but a real solution to real problems.
Solving Doctor Shortages: In places where there aren't many doctors, it can be hard to find healthcare. But with telemedicine, it's like having lots of doctors available on your computer. This means everyone can get good healthcare, even if there aren't many doctors nearby.
Reducing Travel Time: Sometimes, rural areas are far from the nearest hospital. It takes a long time to reach there. Telemedicine helps by bringing the doctor's office to your home. It makes healthcare easier and saves time on traveling.
Helping When Hospitals Close: If a local hospital closes, telemedicine can keep healthcare services available. It’s a safety net for communities facing hospital closures, making sure people can still get medical care.
Breaking Down Barriers to Care: Some barriers to healthcare aren’t physical—they’re about time, access, transportation, and mobility. Telemedicine breaks down these barriers. It’s like opening a door for people who live far away, are busy, or have trouble getting to a doctor’s office. With telemedicine, you can get care wherever you are, making healthcare truly for everyone.
Some Real Stories of Health Transformation
Let’s look at some real examples of how telemedicine is making a difference:
Telestroke Services
When someone has a stroke, every second counts. Telestroke services are like a fast help team for telemedicine, connecting people in rural areas with stroke experts quickly. Think about this: a person in a small town who might be having a stroke can talk to a brain doctor right away. This means they can get the care they need fast, no matter where they are.
Home-Based Cardiac Rehab
Cardiac rehab at home? With telemedicine, it’s possible. Think about a person who’s recovering from a heart problem, but lives far from the nearest rehab centre. With home-based heart rehab, it’s like the rehab team comes to your house. Through online sessions, patients get personal advice, can see how they’re doing, and can recover better. This makes heart care easier and available to everyone.
These examples show how telemedicine is really helping with important health services. From helping with strokes to heart rehab, it’s not just making healthcare available—it’s changing how healthcare can reach everyone, no matter where they live.
Implementing Telemedicine in Rural Settings: Making It Work
Setting up telemedicine in rural places can help people living there get better healthcare. Here’s a simple way to understand how to do it:
1. Figure out what people need: First, understand what health issues are common in rural areas and what challenges people face in getting healthcare.
2. Make sure there's good internet: Improve the local internet and phone connections so that telemedicine works well. This might mean working with phone companies or the government to make it happen.
3. Tell people about it: Let the community know about telemedicine and why it's helpful. Teach them how to use it and make sure they're comfortable with the idea.
4. Work with local doctors: Partner with the doctors and clinics already in the area. Train them on how to use telemedicine, so they can offer it to their patients.
5. Sort out the rules and payments: Make sure the rules and how doctors get paid for telemedicine are fair and make sense. Work with policymakers to update any outdated rules.
6. Use easy technology: Choose telemedicine tools that are easy to use, especially in places where internet might not be super-fast. Help people who might not be great with technology.
7. Help patients use it: Assist people in scheduling appointments and getting their medications. If needed, set up ways to check on their health remotely.
8. Keep an eye on how things are going: Make sure the telemedicine services are working well. Get feedback from both doctors and patients to make things better over time.
By doing these things, we can make sure that even in rural areas, people can easily get good healthcare through telemedicine.
Conclusion
Telemedicine is like a saviour for people living in remote or less-resourced areas. It removes obstacles and brings health services directly to people's homes. With telemedicine, you can consult a doctor and get the treatment you need, no matter how far you live or how few resources are available in your area. It's like a virtual bridge that connects everyone to the healthcare they need. So, in short, telemedicine ensures that everyone gets the medical help they need, regardless of their location.
#Telemedicine App Development Services#telemedicine app development solutions#telehealth app development company#telemedicine app development company#telehealth app developers
0 notes
Text
#Telehealth App Development Company#telemedicine app development company#Telemedicine App Development Services
0 notes
Text
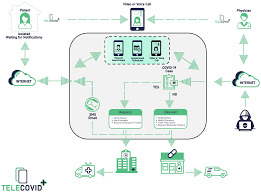
future of virtual care and its impact on the Healthcare Industry

The healthcare industry has undergone a major transformation in recent years, with the rise of telehealth technologies and virtual care. Telehealth apps and telehealth software have become increasingly popular, providing patients with access to healthcare services from the comfort of their own homes. One company that has been at the forefront of this trend is SISGAIN, a leading telehealth app development company. In this blog post, we will explore the future of virtual care and its impact on the healthcare industry, focusing on the role of telehealth software companies like SISGAIN.
Telehealth software has the potential to revolutionize the way healthcare is delivered, by providing patients with convenient access to healthcare services, regardless of their location. This can be particularly beneficial for patients who live in rural or remote areas, and who may struggle to access traditional healthcare services. Telehealth software can also help to reduce costs and improve efficiency, by enabling healthcare providers to deliver care remotely.
The COVID-19 pandemic has accelerated the adoption of telehealth technologies, as healthcare providers have had to find new ways to deliver care while minimizing the risk of infection. As a result, telehealth app development has become a top priority for many healthcare organizations. Telehealth software companies like SISGAIN have been working hard to develop new telehealth apps and software solutions that can help healthcare providers to deliver care remotely.
One of the key advantages of telehealth software is its ability to improve access to healthcare services. Patients can use telehealth apps to connect with healthcare providers from anywhere, at any time. This can be particularly beneficial for patients who live in areas with a shortage of healthcare providers, or for those who have mobility or transportation issues. Telehealth software can also help to reduce wait times for appointments, by enabling patients to see a healthcare provider more quickly.
Telehealth software can also help to reduce costs, by enabling healthcare providers to deliver care more efficiently. For example, telehealth software can be used to conduct remote consultations, reducing the need for in-person visits. This can help to reduce the cost of healthcare delivery, while also improving patient outcomes.
Telehealth software can also help to improve patient outcomes, by enabling healthcare providers to monitor patients remotely. For example, telehealth software can be used to monitor patients with chronic conditions, such as diabetes or heart disease. This can help healthcare providers to detect potential health problems early, and to intervene before they become more serious.
As the demand for telehealth services continues to grow, so too does the need for telehealth app development. Telehealth software companies like SISGAIN are playing an increasingly important role in the development of telehealth apps and software solutions. These companies are working to develop new technologies and applications that can help healthcare providers to deliver care remotely, while also improving patient outcomes.
One of the key challenges facing telehealth software companies is the need to ensure that their products are secure and compliant with regulations. Telehealth software must comply with strict privacy and security regulations, to ensure that patient data is protected at all times. Telehealth software companies must also ensure that their products are user-friendly and accessible to patients of all ages and abilities.
Despite these challenges, the future of telehealth software looks bright. As the healthcare industry continues to evolve, telehealth software will play an increasingly important role in the delivery of healthcare services. Telehealth software companies like SISGAIN will continue to develop innovative new solutions, to help healthcare providers to deliver care remotely, while also improving patient outcomes.
In conclusion, the future of virtual care is bright, thanks to the development of telehealth software and telehealth apps. These technologies have the potential to revolutionize the way healthcare is delivered, by improving access to healthcare services, reducing costs, and improving patient outcomes. Telehealth software companies like SISGAIN are playing an increasingly important role in the development
#telehealth app#telehealth software#telehealth app development#telehealth software companies#telehealth app development company
0 notes
Text
Top 10 Best Telemedicine App Development Companies In The USA
Digitization is gaining ground in every industry and is even affecting the healthcare sector. The digital revolution in the healthcare industry has driven the growth of healthcare IT companies. Let’s know the Top 10 Best Telemedicine App Development Companies in the USA.
Mobile healthcare or healthcare applications are fast becoming the preferred way for healthcare providers and insurers to increase patient satisfaction and improve health outcomes. Today, telemedicine refers to the provision of real-time clinical services via two-way communication. It works between the patient and the healthcare provider.
The growth of telemedicine will help patients receive healthcare services on their phones, including virtual doctor visits via video chat, prescription management, and health reports. The healthcare industry will also benefit from convergence with wearable technologies, which will provide 24* health checks, clinical trials, and access to emergency healthcare.
For companies looking to build mobile applications to take advantage of this growing opportunity, it is vital to find development partners with the experience and know-how to create successful applications in this highly regulated field.
What are the best mobile app development companies on the market that I should contact? For this question, you must have an answer about the platform on which you want the mobile app, and for this, you must consider various things. You must have an idea about the requirements of your app, budget, etc. As just a result, we’ve established this weblog to help you.
Here are the top ten companies in the US for mobile application development.
App Development Platforms
Years of fierce competition led to a duopoly of the mobile operating system. There are currently two major established platforms — iOS and Android OS. There is also Windows 10 Mobile, although its market share in the US is less than 1% and in all other markets less than 10%.
So, the major platforms people look for app development are iOS and Android. They prefer iOS or Android development, and if they want an application on both platforms, they prefer cross-platform app development.
Top Telemedicine App Development Companies
1. VCDoctor
2. Interexy
3. Table XI
4. Y Media Labs
5. Impekable
6. ScienceSoft
7. Intersog
8. Boston Technology Corporation
9. UpTop
10. Appstem
How to Choose the Best Telemedicine App Development Company?
Now that we have listed the top 10 telemedicine app development companies, the following questions might arise how to choose the best among the best?
A few things to consider while choosing the best telemedicine App Development company are:
Previous work or business sector experience
Reviews and recommendations
Market value
Challenges tackled and resolved
Other than these, you will have to discuss with the company about your requirements and find the complete quote.
Conclusion
The application development sector is maturing as several large international agencies have emerged. As healthcare needs grow worldwide, they regularly face the challenge of providing innovative approaches to meet these demands. Medical software companies provide solutions within a medical space by building and delivering products, services, and systems.
Original Blog source: https://www.vcdoctor.com/blog/best-telemedicine-app-development-companies
#top telemedicine app developers#telemedicine app development company#telehealth app development company#telehealth app development services#telehealth software company usa#vcdoctor
0 notes
Text

Discover why SISGAIN is the most trusted Health Care App Development Company in UAE. We deliver secure, AI-powered solutions for hospitals, clinics & telehealth.
#health care app development company#healthcare app development UAE#medical software development#telehealth solutions UAE#remote patient monitoring
0 notes
Text
How Serverless Computing and Cloud-Native Technologies Improve Telehealth Platform Scalability
In recent years, telehealth has emerged as a transformative force in the healthcare industry, revolutionizing the way patients access medical care and interact with healthcare providers. With the increasing demand for remote healthcare services, scalability has become a paramount concern for telehealth platforms. Fortunately, advancements in serverless computing and cloud-native technologies offer innovative solutions to address these scalability challenges effectively.
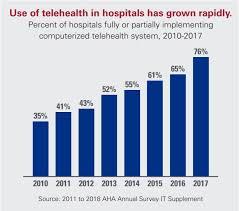
The Rise of Telehealth Platforms
Telehealth platforms have experienced unprecedented growth, fueled by factors such as technological advancements, changing patient preferences, and the need for convenient access to healthcare services. These platforms enable patients to consult with healthcare professionals remotely, whether through video calls, chat interfaces, or mobile applications. However, as the demand for telehealth services continues to soar, scalability has emerged as a critical consideration for platform developers and healthcare providers alike.
Understanding Serverless Computing
Serverless computing represents a paradigm shift in cloud computing, where developers can focus on writing code without the need to manage underlying infrastructure. In a serverless architecture, cloud providers dynamically allocate resources to execute code in response to incoming requests, eliminating the need for provisioning and managing servers. This approach offers several benefits for telehealth platforms, including:
1. Scalability on Demand: Serverless computing enables telehealth platforms to scale automatically in response to fluctuations in user demand. Whether handling a sudden surge in patient consultations or managing periods of low activity, serverless architectures can efficiently allocate resources to match workload requirements.
2. Cost Efficiency: With serverless computing, telehealth platforms only pay for the computing resources consumed during code execution, eliminating the need for idle infrastructure. This pay-as-you-go model can result in significant cost savings, particularly for platforms with unpredictable usage patterns.
3. Improved Developer Productivity: By abstracting away infrastructure management tasks, serverless computing allows developers to focus on writing code and delivering features that enhance the telehealth experience. This increased productivity can accelerate the development and deployment of new features, helping telehealth platforms stay competitive in a rapidly evolving landscape.
Leveraging Cloud-Native Technologies
Cloud-native technologies complement serverless computing by providing a comprehensive framework for building and deploying applications in the cloud. These technologies are designed to leverage the scalability, resilience, and agility of cloud environments, enabling telehealth platforms to deliver reliable and efficient services to users. Key components of cloud-native architectures include:
1. Containerization: Containerization technologies such as Docker enable developers to package applications and their dependencies into lightweight, portable containers. By encapsulating each component of the telehealth platform in a container, developers can achieve consistency and reproducibility across different environments, facilitating seamless deployment and scalability.
2. Orchestration: Container orchestration platforms like Kubernetes provide tools for automating the deployment, scaling, and management of containerized applications. By orchestrating containerized workloads across clusters of virtual or physical machines, Kubernetes ensures optimal resource utilization and high availability for telehealth platforms, even during periods of peak demand.
3. Microservices Architecture: Adopting a microservices architecture allows telehealth platforms to decompose complex systems into smaller, loosely coupled services that can be developed, deployed, and scaled independently. This modular approach enhances flexibility, resilience, and scalability, enabling telehealth platforms to evolve rapidly in response to changing requirements and user feedback.
Conclusion
As telehealth continues to gain momentum as a preferred mode of healthcare delivery, the scalability of telehealth platforms becomes increasingly crucial. Serverless computing and cloud-native technologies offer compelling solutions to address the scalability challenges faced by telehealth platforms, enabling them to deliver reliable, efficient, and scalable services to patients and healthcare providers worldwide. By embracing these innovative technologies, telehealth platforms can unlock new opportunities for growth, innovation, and impact in the evolving landscape of healthcare delivery.
0 notes
Text
Pioneering Healthcare Solutions: The Role of a Medical Software Development Company
In the rapidly evolving landscape of healthcare, technology plays an instrumental role in transforming patient care, streamlining operations, and advancing medical research. At the heart of this technological revolution lies the expertise of medical software development companies. These specialized firms are dedicated to creating innovative solutions that empower healthcare providers, improve patient outcomes, and drive efficiency across the industry.
The Crucial Intersection of Medicine and Technology
The integration of technology into healthcare has given rise to a new era of patient-centric care and data-driven decision-making. Medical software development companies are at the forefront of this movement, creating bespoke software solutions that cater to the unique needs of healthcare providers, from small clinics to large hospital systems.
**1. Tailored Electronic Health Records (EHR) Systems
Electronic Health Records (EHR) have become the backbone of modern healthcare. They provide a comprehensive digital record of a patient's medical history, diagnoses, medications, treatment plans, immunization dates, allergies, radiology images, and laboratory test results. Medical software development companies excel in crafting EHR systems that are intuitive, secure, and seamlessly integrated with existing workflows.
By customizing EHR solutions, these companies ensure that healthcare providers can access critical patient information with ease, leading to faster diagnoses, more accurate treatment plans, and improved patient safety.
2. Telehealth Platforms for Remote Care
The COVID-19 pandemic accelerated the adoption of telehealth, making it an indispensable tool for providing care remotely. Medical software development companies have been instrumental in developing user-friendly telehealth platforms that facilitate virtual consultations, enabling patients to receive timely medical advice from the comfort of their homes.
These platforms often incorporate features such as video conferencing, secure messaging, and appointment scheduling. They are designed to ensure compliance with healthcare regulations while delivering a seamless and intuitive experience for both healthcare providers and patients.
3. Medical Imaging and Diagnostic Tools
Medical imaging is a cornerstone of modern medicine, enabling accurate diagnoses and treatment planning. Medical software development companies work in tandem with radiologists and imaging experts to create sophisticated software for tasks like image reconstruction, segmentation, and analysis. These tools enhance the accuracy and speed of diagnoses, ultimately leading to better patient outcomes.
4. Clinical Decision Support Systems (CDSS)
CDSS leverage data analysis and artificial intelligence to assist healthcare providers in making informed clinical decisions. These systems integrate with EHRs and other health information systems to provide real-time recommendations based on evidence-based guidelines and patient-specific data.
By collaborating with medical experts, software development companies refine these systems to ensure they are reliable, accurate, and capable of adapting to the evolving landscape of medical knowledge.
5. Data Security and Compliance Solutions
Ensuring the confidentiality and integrity of patient data is paramount in healthcare. Medical software development companies develop robust security protocols, encryption algorithms, and compliance solutions to safeguard sensitive information. They stay abreast of evolving regulatory requirements, such as HIPAA (Health Insurance Portability and Accountability Act), and continuously update their software to maintain compliance.
The Future of Healthcare Innovation
As medical knowledge and technology continue to advance, the role of custom software development companies becomes even more pivotal. They are poised to drive innovation in areas such as artificial intelligence, genomics, personalized medicine, and the Internet of Things (IoT). By partnering with healthcare professionals and researchers, these companies are at the vanguard of pioneering solutions that will shape the future of healthcare.
In a world where every second counts and accuracy is paramount, the collaboration between healthcare providers and medical software development companies represents a beacon of hope for improved patient care, streamlined operations, and groundbreaking medical discoveries. Together, they are not only advancing healthcare, but also revolutionizing the way we approach and experience wellness.
0 notes
Text
Telehealth APIs: Building Tools for Remote Care
Telehealth APIs are instrumental in building tools for remote care, revolutionizing the delivery of healthcare services. These APIs facilitate the seamless integration of remote healthcare solutions into existing healthcare applications, enabling efficient data exchange between patients and healthcare providers. They play a vital role in the development of healthcare apps, providing access to a wide range of functionalities such as real-time communication, remote monitoring, appointment scheduling, and electronic health record integration. Additionally, APIs for Healthcare Apps empower developers to create comprehensive solutions that enhance patient care and accessibility.
Visit us:
#Telehealth API#ios app development#website development company#blockchain application development#website design services#iot development services#best iphone app development
0 notes
Text
Unlocking the Advantages of Telehealth App Development Solutions
Telehealth has emerged as a game-changer in the healthcare industry, leveraging technology to revolutionize the way medical services are delivered and accessed. With the advent of telehealth app development solutions, healthcare has transcended physical boundaries, offering patients and healthcare providers unparalleled advantages. This blog delves into the various benefits of telehealth app development solutions and how they are transforming the healthcare landscape.
Increased Access to Healthcare Services
One of the most significant advantages of telehealth apps is their ability to bridge the gap between patients and healthcare providers. Telehealth apps enable remote consultations, eliminating the need for patients to travel long distances to receive medical advice or treatment. This is especially beneficial for patients residing in rural or underserved areas, where access to healthcare facilities may be limited.
Enhanced Convenience and Flexibility
Telehealth apps empower patients to seek medical advice and support at their convenience. With 24/7 accessibility, patients can schedule virtual appointments, access medical records, and receive prescription refills without leaving the comfort of their homes. This flexibility also benefits healthcare providers, as they can efficiently manage their schedules and optimize their time.
Timely Intervention and Preventive Care
Telehealth app development solutions enable real-time patient monitoring and data tracking. Healthcare providers can remotely monitor patients with chronic conditions, allowing for timely intervention in case of any concerning changes in vital signs or health metrics. This proactive approach promotes preventive care, leading to better health outcomes and reduced hospitalizations.
Cost-Effectiveness and Efficiecy
Telehealth services offer cost-effective solutions for both patients and healthcare organizations. Patients can save on travel expenses, and healthcare facilities can reduce overhead costs associated with physical visits. Telehealth app development solutions streamline administrative tasks, appointment scheduling, and billing processes, leading to improved operational efficiency.
Increased Patient Engagement and Adherence
Telehealth apps promote active patient engagement by providing access to personalized health information and educational resources. Patients become more involved in their healthcare journey, leading to better treatment adherence and improved health management.
Improved Communication and Collaboration
Telehealth apps facilitate seamless communication and collaboration among healthcare providers. Specialists can remotely consult with primary care physicians, share medical records, and jointly develop comprehensive treatment plans. This team-based approach fosters a holistic view of patient care and ensures informed decision-making.
Privacy and Data Security
Telehealth app development solutions prioritize patient data privacy and security. Reputable telehealth apps comply with industry regulations, such as HIPAA, to safeguard patient information from unauthorized access or breaches. Robust encryption protocols ensure that patient data remains confidential and protected.
Remote Medical Training and Education
Beyond patient care, telehealth apps are instrumental in medical training and education. Telehealth platforms provide remote training sessions, webinars, and virtual conferences, empowering medical professionals to enhance their knowledge and stay up-to-date with the latest medical advancements.
Telehealth app development solutions have revolutionized the healthcare industry, unlocking a plethora of advantages for both patients and healthcare providers. From increased access to healthcare services and improved patient engagement to cost-effectiveness and streamlined workflows, telehealth apps are shaping a patient-centric, efficient, and accessible healthcare ecosystem.
As telehealth continues to evolve and integrate with advanced technologies like artificial intelligence and Internet of Things (IoT), its impact on healthcare is bound to grow exponentially. The future of healthcare is undoubtedly digital, and telehealth app development solutions will remain at the forefront of this transformation, revolutionizing the way we receive and deliver healthcare services.
Revolutionize healthcare with our cutting-edge telehealth app development solutions!
Whether you're a medical practice, hospital, or healthcare startup, our expert team of developers can create robust, user-friendly telehealth applications tailored to your needs.
Embrace the future of healthcare with our telehealth app solutions. Contact us today to schedule a demo and take the first step towards a healthier tomorrow!
Contact Information:
Contact: +91 9499501397
Email: hello@knovator.com
Website: https://knovator.com/custom-telehealth-software-solutions/
0 notes
Text

We use industry best practices to design and develop healthcare mobile apps and customized web software that are user-friendly, scalable, secure, and yet, highly cost-effective.
#telehealth website development services#custom telemedicine app#custom medtech software development#telemedicine software development company#ehr software development company#telemedicine website development company#telehealth software development
0 notes
Text
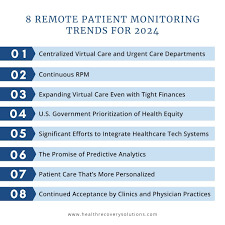
Telemedicine in 2024: What's Changing?
The COVID-19 pandemic undoubtedly propelled telemedicine application development into the healthcare mainstream. Virtual visits went from a novelty to an absolute necessity almost overnight. Now, as the initial crisis stabilizes, many wonder – was telehealth just a fleeting bandage during an unprecedented time of need? Or is it the future?

Telemedicine is no short-lived fad.
In fact, it is on the cusp of revolutionary, permanent transformation into one of the primary modalities of healthcare delivery. The genie is out of the bottle.
In this blog post, we will examine the imminent changes on the horizon that will shape the rapid evolution of telemedicine in 2024 and beyond. You will gain insight into the coming wave of innovation in virtual care access, connected health devices, remote exams, integrated data, specialty use cases, and telehealth-centric business models.
The COVID-19 crisis offered a glimpse into the digital future of healthcare. Read on to understand how telemedicine application development will fundamentally reshape medicine into a more proactive, prevention-focused and patient-centered system. The opportunities stretch far beyond just video visits.:
#Trend 1: Greater Insurance Coverage and Access
One of the most impactful shifts will be greatly expanded insurance coverage and access to telemedicine app development services across patient demographics. Up until recently, many insurers offered limited coverage for telehealth visits. Policies often restricted virtual care to specific types of appointments or limited the types of providers and platforms that could be used.
In 2023, the Centers for Medicare & Medicaid Services (CMS) implemented sweeping changes to telehealth coverage for Medicare beneficiaries. Medicare can now reimburse for over 100 additional telehealth services, including emergency department visits, therapy services, mental health counseling, and more. Importantly, Medicare has also permanently removed geographic restrictions that previously limited telehealth coverage mainly to rural areas.
Many private insurers have followed suit in expanding telehealth benefits. Over 90% of large employers expected to provide telemedicine application development access for workers on their health plans.
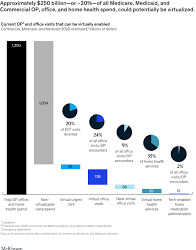
This expansion of telehealth insurance coverage will open up virtual care access for tens of millions more patients in 2024 and beyond. Older adults, lower-income patients, and those with disabilities or without easy transportation will particularly benefit. McKinsey estimates up to $250 billion of current U.S. healthcare spending could potentially be virtualized given the increased coverage.
Annual telemedicine usage growth is projected to be over 24% from 2024 to 2030. It will become the primary way many patients interact with their providers. Natural language processing (NLP), chatbots, and other emerging technologies will make telehealth interactions increasingly dynamic and smart.
#Trend 2: Connected Devices and Remote Monitoring
New connected health devices and wearable sensors have also gone mainstream, making it easier for patients to share important vitals and health data with providers during virtual visits. These include:
- Smartwatches and fitness trackers that monitor heart rate, sleep patterns, activity levels, and more. Popular models include the Apple Watch, Fitbit Sense, and Google Pixel Watch.
- Connected blood pressure cuffs that sync readings to a smartphone app, like those from Omron and Withings.
- EKG monitors that allow patients to take a mobile 30-second EKG, such as the KardiaMobile from AliveCor.
- Fingertip pulse oximeters that measure oxygen saturation levels.
- Continuous glucose monitors (CGMs) like those made by Dexcom that share real-time glucose readings with patients and providers.
- Smart inhalers, insulin pens, scales, thermometers, and other connected devices tailored to chronic conditions.
Types of Connected Health Devices
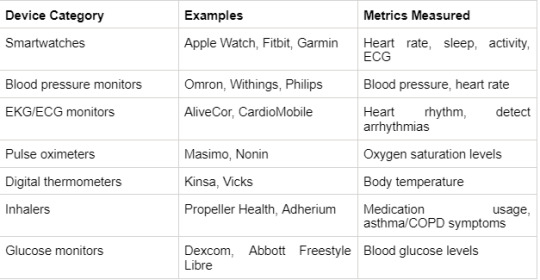
Per a survey, 65% of patients now use some type of connected health device. These devices are especially helpful for managing chronic illnesses. They allow care teams to remotely track vitals and symptoms that previously required in-person visits. Any telehealth app development company can gain deeper, real-world insights to inform diagnoses, treatment adjustments, and lifestyle recommendations.
In the future, ingestible sensors, smart contact lenses, and skin patches will collect even more advanced biometrics. Along with the growth of the “Internet of Medical Things,” telemedicine app development will increasingly happen in context, with patient-generated data seamlessly powering personalized virtual care.
# Trend 3: Advancements in Virtual Physical Exams
While telehealth platforms have enabled limited components of the physical exam, providers have been constrained in their ability to fully visualize and assess the patient virtually. Innovations in several technology areas are poised to close many of these gaps in 2024 and beyond:
Visualization
- High-resolution cameras built into smartphones and laptops continue to improve imaging and video quality to levels sufficient for many visual inspections.
- Specialized adapters like the TytoCare examine the ears, throat, lungs, heart, abdomen, and skin in high fidelity.
- Digital otoscopes and ophthalmoscopes allow detailed ear and eye exams.
- Mobile ultrasound probes can be paired with smartphones to share images in real time.
Audio
- Electronic stethoscopes like the Eko CORE can amplify heart, lung, and other body sounds for a virtual exam.
- Advanced auscultation belts use embedded sensors to pick up and transmit body sounds.
- Algorithms can process these audio signals into meaningful visual data representations.

Simulation
- Augmented reality will allow patients to project a full-sized visual of their body for the telehealth app development company to inspect, annotate, and guide the exam.
- Haptic gloves combined with AR will enable simulation of palpations, pulses, muscle strength assessments, and range of motion.
- Virtual reality can immerse providers and patients together in a simulated exam environment.
Adopting these technologies by a leading telemedicine app development company ill remove many remaining barriers to comprehensive remote exams. Physical and virtual care will become intrinsically linked to benefit patients and clinicians.
#Trend 4: Interoperability and Data Integration
A longstanding challenge with telemedicine app development adoption has been integrating data from virtual care platforms into electronic health records (EHRs) and other health IT systems. Much of the early growth of telehealth has resulted in fragmented, siloed data across disjointed tools.
True transformation of healthcare delivery will depend on seamless data sharing and making data contextually useful at the point of care.
In 2024, we are likely to see an acceleration of initiatives addressing these needs:
-EHR Integration: Major EHR vendors like Epic and Cerner are developing improved application programming interfaces (APIs) to more seamlessly integrate real-time telehealth visit data into longitudinal patient records.
- Data Standards: Health data interoperability standards like FHIR and APIs will enable telemedicine platforms to connect with external apps and systems. Data normalization frameworks will allow medical devices to share streaming data.
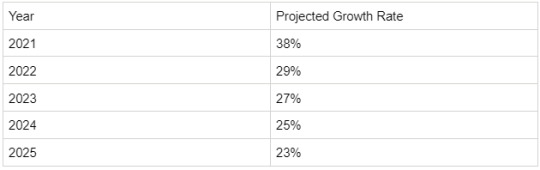
Projected Telemedicine Usage Growth Rates
-Care Coordination: Platforms will directly integrate with pharmacy, lab, benefits, health information exchanges (HIE), and other systems involved in care transitions and population health.
- Analytics: With comprehensive data, analytics will identify usage trends, gaps in care, risk factors, and other clinically meaningful insights to guide telemedicine application development strategy.
Overcoming these interoperability challenges will allow telehealth to slot in as a natural integrated component of holistic care delivery.
## Trend 5: Telemedicine Specialty Growth Areas
Until recently, telehealth was primarily leveraged for lower acuity primary care visits and mental health. That is poised to change as virtual care grows across numerous specialties:
Tele-ICU
Remote access to intensive care unit (ICU) patients enables continuous off-site monitoring by critical care specialists. This tele-ICU approach has demonstrated benefits, including:
- Reduced mortality rates
- Shorter ICU and hospital length of stay
- Faster response times for alarms and alerts
- Improved adherence to care protocols
- Access to specialist expertise for smaller and rural hospitals
Image
Telestroke
Virtual neurology consultation during emergent stroke care has become standard practice. Telestroke networks allow community hospitals quick access to neurologist expertise for time-sensitive evaluation and treatment decisions.
Outcomes data shows that telestroke significantly increases rates of life-saving interventions like intravenous thrombolysis and mechanical thrombectomy. According to a study, telestroke is now used in over 30% of U.S. hospitals.
Teledermatology
Store-and-forward teledermatology allows clinicians to acquire images or video of skin conditions, which dermatologists can asynchronously review in depth. Live video teleconsultation is also being used for real-time assessment and diagnosis.
Among the benefits shown are improved access to specialty care, reduced wait times, and avoidance of unnecessary in-person referrals. Teledermatology utilization increased double fold during the pandemic and will continue rising, given the ubiquity of smartphones with high-res cameras.
Telerehabilitation
Virtual physical therapy, occupational therapy, and speech therapy visits are practical options for many patients. Telerehab provides continuity of care after discharge, increased access for those with limited mobility, and reduced infection risks.
Digital measurement tools and wearable sensors that track patient movement, activity levels, and progress notes are enablers. Demand is being driven by recovery needs for long COVID patients as well as the aging population.
Telepsychiatry and Mental Health
Telemental Health has long been a pioneer telemedicine app development specialty. Virtual therapy and psychiatric services enable access regardless of geography. Digital tools improve engagement among high-risk populations. And care transcends episodic visits through continuous monitoring and digital therapeutics.
According to a study, telepsychiatry utilization increased 10-fold during the pandemic. Key drivers will be severe telemedicine app development company shortages and surging behavioral health needs. Integrated care models blending virtual and in-person behavioral health will emerge.
Tele-Surgery
While still nascent, virtual surgery assistance holds promise for enhancing collaboration, expanding access to experts, improving training, and guiding complex procedures. Long-distance telementoring allows experienced surgeons to advise less experienced surgeons remotely.
Augmented reality can overlay virtual guidance onto the live surgical field. Robotic surgery platforms create digital environments amenable to remote guidance. While tele-surgery has a long runway, foundations are being built.
Conclusion
Telemedicine had been incrementally gaining steam before COVID-19 due to gradual policy changes, tech improvements, and shifting consumer habits. However, the pandemic radically accelerated adoption across providers, patients, payers, and regulators. It also illuminated telehealth’s untapped potential beyond basic teleconferencing.
While telemedicine application development solutions hold great potential to transform healthcare accessibility and delivery, there are also challenges to address:
- Reimbursement still poses barriers in many states and for several specialties, restricting universal telehealth access. Continued advocacy is crucial for coverage expansion.
- Shortage of providers trained in virtual care delivery models can hinder rapid scale-up. Investments in telemedicine app development training and recruitment are vital.
- Concerns about data privacy remain a key barrier for any telemedicine app development company and patient adoption. Robust cybersecurity and HIPAA compliance are mandatory.
- User-friendly solutions and physician buy-in are equally important for successful implementation. Change management is key.
However, with continued policy reforms, technological advances, public-private partnerships, and changing care delivery models, telehealth is poised for robust mainstream growth in the coming decade.
The next few years will see the telemedicine app development industry evolve into a more seamless, integrated, and intelligent component of the overall healthcare infrastructure. While initial limitations around reimbursement, technology, culture, and perception are finally giving way to pragmatic innovation.
Rather than a temporary fad, telehealth will increasingly become the preferred and superior modality for many healthcare interactions and workflows.
The future is bright for forward-thinking healthcare organizations that make strategic investments in telemedicine capabilities today. Partnering with a leading cutting-edge telemedicine app development company will be key to building next-gen virtual care platforms tailored to their needs.
At Consagous Technologies, a leading telemedicine app development company, we are at the forefront of designing and implementing seamlessly integrated, highly intuitive telemedicine application development solutions for healthcare providers across the country. Our full-stack engineering expertise and user-centric approach help maximize clinical value and patient engagement.
To explore how Consagous can help you implement scalable telehealth app development platforms and differentiate your services, schedule a consultation with our healthcare IT specialists. You can also see the reviews from our first-hand users on Goodfirms.
Let’s discuss how we can jointly shape the future of virtual care at your organization.
#telemedicine app development#telemedicine application development#telehealth app development company
0 notes
Text

Teledocto- Market ready Telehealth app for doctors with specific features
Teledocto is a white labelled mobile app which can customized easily according to your business need of telemedicine services. It has in-build features of online scheduling file and screen sharing, remote monitoring. Let us help you with your ideas!!
#telemedicine app development services#telemedicine app development#telemedicine software development#telemedicine app development company#telehealth app development#telehealth app development company#hire telemedicine app developers
0 notes
Text
Crafting Telehealth App Development for Tomorrow
what is telehealth app development?

pidly evolving world, technology continues to reshape various industries, and the healthcare sector is no exception. The rise of telehealth app development has sparked a transformation in the way healthcare services are delivered and accessed. This article delves into the significance, challenges, and future prospects of telehealth app development, focusing on the role of a Telehealth App Development Company in shaping the future of healthcare.
Telehealth apps are paving the way for a more accessible and patient-centric healthcare experience. With the rising demand for remote medical consultations, these apps have become essential tools for both patients and healthcare providers. Through seamless video consultations, instant messaging, and remote monitoring, patients can access medical expertise regardless of their geographical location.
The Essence of Telehealth Apps
Telehealth apps are innovative digital platforms that bridge the gap between patients and healthcare professionals. They enable users to connect with doctors, therapists, and specialists in real-time, breaking down the barriers of distance and time. These apps offer an array of medical services, from primary care consultations to mental health support.
Benefits of Telehealth Apps
Enhanced Accessibility
One of the primary advantages of telehealth apps is their ability to provide healthcare services to individuals who may have limited access to medical facilities. Rural areas, for instance, can benefit greatly from telehealth services, as patients can consult with doctors without the need for extensive travel.
Convenience and Flexibility
Telehealth apps offer unparalleled convenience. Patients no longer need to take time off work or spend hours in waiting rooms. Instead, they can schedule appointments that suit their routines, fostering a more patient-centric approach to healthcare.
Cost-Effectiveness
Telemedicine App Development Services often come at a lower cost compared to traditional in-person consultations. This affordability makes quality healthcare more attainable for a wider range of individuals.
Key Features of Successful Telehealth Apps
User-Friendly Interface
An intuitive user interface is crucial for the success of telehealth apps. Patients, especially those who might not be tech-savvy, should be able to navigate the app effortlessly.
Secure Data Transmission
Privacy is paramount in healthcare. Telehealth apps must employ robust encryption techniques to ensure that sensitive patient data remains confidential during transmission.
Integration of Health Monitoring Devices
To enhance the effectiveness of telehealth consultations, many apps integrate with wearable health monitoring devices. This allows doctors to receive real-time data for more accurate diagnoses.
Telehealth App Development Process
The journey of crafting a telehealth app involves several stages:
Market Research and Idea Generation
Identifying the target audience and understanding their needs is the first step. This research informs the features and functionalities of the app.
Design and Prototype Creation
The app's user interface and experience are designed at this stage. Prototypes are created and refined based on feedback.
Development and Testing
The actual coding and development of the app take place here. Rigorous testing is essential to identify and eliminate any bugs or glitches.
Launch and User Feedback
Once the app is ready, it's launched to the public. User feedback is collected and analyzed to make necessary improvements.
Challenges in Telehealth App Development
Regulatory Compliance
Telehealth apps must adhere to strict regulatory standards to ensure patient safety and compliance with medical laws.
Data Security and Privacy Concerns
Storing and transmitting medical data safely is a significant challenge. Any breach in data security could have severe consequences.
Integration with Existing Healthcare Systems
Interoperability with existing electronic health records and healthcare systems is necessary for smooth patient care.
The Role of Telehealth App Development Companies
Expertise in Healthcare and Technology
These companies possess a blend of medical and technological knowledge, enabling them to create apps that cater to the specific needs of healthcare providers and patients.
Customized Solutions
Telehealth app development companies tailor their solutions to the unique requirements of their clients, ensuring a personalized experience.
Continuous Support and Updates
The healthcare landscape is ever-evolving. These companies provide continuous support and updates to keep the app current and effective.
Future Trends in Telehealth
Artificial Intelligence in Diagnostics
AI-driven algorithms can aid in diagnosing medical conditions accurately, revolutionizing the diagnostic process.
Remote Patient Monitoring
Wearable devices can continuously monitor patients' health, providing real-time data to healthcare professionals for timely interventions.
Virtual Reality for Telemedicine
Virtual reality can simulate medical scenarios, allowing doctors and medical students to enhance their skills in a controlled environment.
Impact on Healthcare Industry
Improved Patient Engagement
Telehealth apps empower patients to take charge of their health by providing access to medical resources and information.
Reduced Healthcare Costs
By eliminating the need for physical infrastructure, telehealth apps contribute to cost savings for both patients and healthcare institutions.
Evolving Doctor-Patient Relationship
Telehealth encourages more open and frequent communication between doctors and patients, fostering a stronger bond.
Conclusion
The dawn of telehealth app development is reshaping healthcare delivery, making it more accessible, convenient, and patient-centric. With the continuous advancement of technology, the role of Telemedicine App Development Company becomes even more critical in driving innovation and ensuring the highest standards of patient care. The future holds exciting possibilities as telehealth apps continue to evolve and transform the healthcare landscape.
#Telehealth App Development Company#Telemedicine App Development Company#Telemedicine App Development Services
0 notes
Text

Telehealth Software & Solution Development Company
#telehealth development company#telehealth Software technology#telehealth Development services#telehealth software#telehealth Development platform#custom telehealth solutions#remote monitoring telehealth software#telehealth implementation development#telehealth software systems#telehealth app developers#telehealth app development company#telehealth app
0 notes
Text
Top 10 Mobile App Consulting Trends in 2025: Expert Insights from Digiflex.ai
Introduction: The mobile app ecosystem is undergoing a seismic shift, driven by AI breakthroughs, immersive tech, and evolving user expectations. As a leader in AI-driven consulting, Digiflex.ai empowers businesses to navigate this dynamic landscape. In this blog, we unveil the top 10 mobile app consulting trends of 2025 and how our strategic expertise ensures your app stays ahead of the curve.
1. AI-First App Strategy Consulting
Why it’s trending: Apps without embedded AI risk obsolescence. Companies need advisors to integrate predictive analytics, chatbots, and autonomous decision-making. Digiflex.ai Edge: We audit your app’s AI readiness and design roadmaps for features like real-time sentiment analysis or personalized in-app journeys.
2. Hyper-Personalization via Generative AI
Why it’s trending: Users expect apps to anticipate needs. Generative AI crafts dynamic content, layouts, and offers. Our Approach: For a fitness app client, we deployed AI-generated workout plans that adapt to user moods, boosting retention by 40%.
3. Ethical AI Governance Frameworks
Why it’s trending: Regulations like the EU’s AI Act demand transparency. Digiflex.ai Solution: We help clients implement bias detection tools and ethical AI audits, ensuring compliance without sacrificing innovation.
4. Metaverse and AR/VR Integration Consulting
Why it’s trending: Brands are building virtual storefronts and 3D training apps. Case Study: We guided a retail client to launch an AR-powered “virtual try-on” app, increasing conversions by 55%.
5. Voice-First App Interfaces
Why it’s trending: 70% of Gen Z prefers voice commands over typing. Our Expertise: We design voice-optimized UX flows and NLP integrations, like our project for a telehealth app enabling voice-based symptom logging.
6. Super App Ecosystems
Why it’s trending: Users want all-in-one platforms (e.g., payments + social + shopping). Digiflex.ai Strategy: We consult on modular architectures, like our work with a Southeast Asian fintech app merging loans, e-commerce, and insurance.
7. Predictive Analytics for Churn Reduction
Why it’s trending: Retention is 5x cheaper than acquisition. Our Toolset: We deploy ML models to predict user drop-offs and prescribe interventions, slashing churn by 30% for a streaming app client.
8. Quantum-Ready App Security
Why it’s trending: Quantum computing threatens current encryption. Future-Proofing: We advise on post-quantum cryptography and quantum-safe APIs, keeping client data unhackable.
9. Blockchain-Powered Decentralized Apps (dApps)
Why it’s trending: Demand for trustless transactions and tokenized rewards is soaring. Digiflex.ai Insight: We helped a gaming app launch a dApp with NFT-based leaderboards, driving a 200% surge in DAUs.
10. Sustainability-Centric App Design
Why it’s trending: Eco-conscious users favor apps with low energy consumption. Our Green Strategy: We optimize apps for battery efficiency, reduce data bloat, and advise on carbon-offset partnerships.
Why Partner with Digiflex.ai?
Proven AI Leadership: 90% of our clients see ROI within 6 months.
End-to-End Consulting: From ideation to post-launch analytics.
Global Compliance: GDPR, CCPA, and AI ethics frameworks baked into every strategy.
Case Study Spotlight:How Digiflex.ai Revamped “FinEase”
Challenge: A fintech app struggled with high user drop-offs during KYC.
Solution: Emotion-aware AI streamlined the process by detecting frustration and simplifying steps.
Result: 50% faster onboarding, 25% higher completion rates.
SEO Tips for 2025 Mobile Apps:
Target keywords: “AI mobile app consulting 2025”, “metaverse app development services”.
Optimize for voice search with FAQ schema markup.
Repurpose blogs into (short videos) for TikTok/Reels.
Final ThoughtsIn 2025, mobile apps will be judged by their ability to blend intelligence, ethics, and immersion. At Digiflex.ai, we don’t just adapt to trends—we define them. Ready to transform your app into a future-ready powerhouse? Schedule a free strategy session today!
0 notes