#she has an injection site sarcoma
Explore tagged Tumblr posts
Text
Rosie checking the cat Internet. Every cat that passes sniffs the lower branches of the hedge to check who's been by and what's going on.
Also some seagulls stop by.
#cats#personal#cw pet death#we decided on palliative care yesterday#she has an injection site sarcoma#which is essentially untreatable#i will write more about this at some point but not yet
60 notes
·
View notes
Text
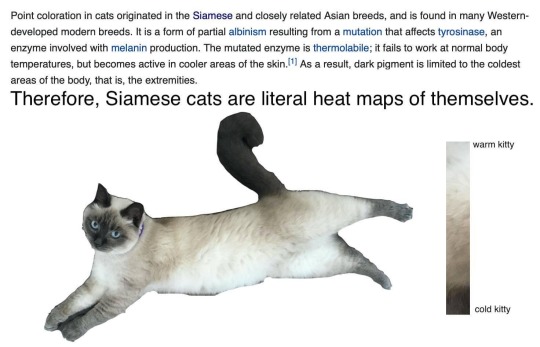
Misty had surgery to remove an injection site sarcoma earlier this year and it has been so fascinating watching the shaved patch grow back! I expect it will be darker until her next big shed.
I love how you can see the fur closer to the body is lighter and it darkens towards the end of the shaft, giving the shaved area a halo.

This is more recent. The newly grown hair is much closer to the color of her face than the rest of her back.

Be sure to take your fur babies to the vet if you notice any irregular lumps! Siamese are particularly prone to injection site sarcomas which, as the name indicates, happen where they have received any sort of injection. They can turn cancerous if ignored too long. When I first noticed the lump, it was the size of a grain of rice and I took her in the next day to make sure her microchip hadn't migrated. We did a cytology and got the results back after a week, then scheduled her for surgery the following week. In the two weeks between discovery and removal, it had grown to the size of a walnut.
Misty's prognosis is excellent because I noticed the lump early and acted so quickly. They managed to get it all and she won't receive any injections again for the rest of her life. I need to be more aware of changes to her skin and get any other lumps checked right away. But that's a very small concern and I will do whatever it takes to keep my fur baby with me for another decade if possible!

80K notes
·
View notes
Text

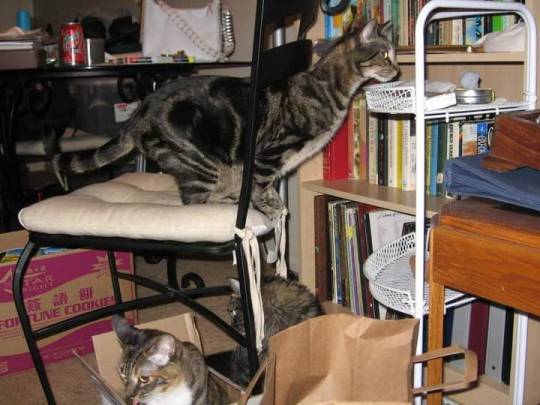
Look at that kitty face. That's my boy, Thor. In the fall of 2004, we adopted a litter of three 6-week old Halloween kittens who has been wanted out of a storm drain by an autumn storm. Because they were Halloween storm kitties, we named them accordingly. I named Thor after the little grey kitten from Number The Stars. We named his sisters Gloomdrop and Zot (partially for the sound of electricity/lightning and partially because she was the spitting image of the kitten in the webcomic Queen of Wands.

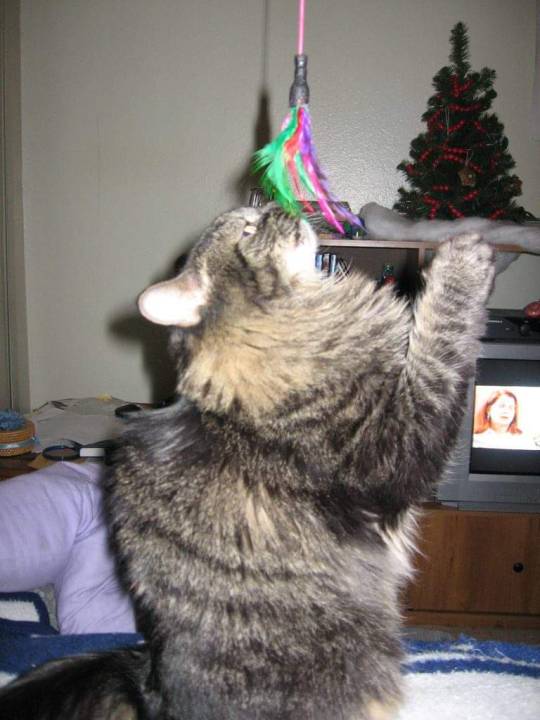
We lost Gloomdrop in February of 2019, and Zot is dealing with hind leg neuropathy as a side effect of her diabetes, but their brother, Thor, has always been the model of a healthy, active kitty.

In mid-September (2020), Thor developed a lump in his hind right leg. After multiple tests, including 2 biopsies, our vet confirmed he had a malignant tumor and referred us to a specialist. We met with the oncologist today, and he diagnosed Thor with a soft tissue sarcoma, likely from his vaccines (a rare but documented side effect that occurs at the vaccine injection site.)



Happily, we caught the tumor early enough that it hasn't yet metastasized to the rest of his body. Less happily, Thor has two treatment options open to him: radiation or leg amputation. The vet confirmed that, other than this tumor, Thor is in incredible health -- not just for a 16-year-old kitty, but "even compared to cats half his age." Thor keeps up with -- and outpaces -- our 5-year-old cat, so that sounds pretty accurate to us!
Thor's radiation treatment is estimated at $3800, with another $1350 to cover the hospitalization that will go along with it since he'll be getting a sequence of five consecutive days at a hospital in Carlsbad. (He was a very good kitty on the 4-hr round trip commute there today for his consultation.) We have to wait ten days before doing the radiation, so his stitches from the punch biopsy can be removed, but the oncologist wants to stay the treatment as soon after that as possible.
Gloomdrop's end-of-life care and Zot's autoimmune, diabetes, and mobility care has already drained our savings, but we'll do everything we can for our kitties. While the oncologist thinks Thor might be able to adjust to being an amputee, even at 16, we are doing everything we can to try to make the radiation treatment feasible in order to preserve his quality of life.
Anything you can donate -- even just a dollar or sharing this -- would be amazing, and we would be so appreciative and ever grateful. We know right now is hard for so many people for so many reasons, and it means the world to us that you would even consider helping us save our kitty. We genuinely can't imagine what our lives would be like without our cuddly boy.
Thank you so much, especially if you read all of this! We love you, and Thor would, too, if he understood what was happening.
https://fundrazr.com/campaigns/01ir0c
37 notes
·
View notes
Text

So. What she has is injection site sarcoma. In order to remove the mass they would need to remove her entire leg. They say "Yeah it's okay, cats can survive with three legs, conservatively it'll buy you six months." There's no knowing just how much she would suffer through such an ordeal. This isn't our first cancer rodeo (humans, cats, dogs... cancer sucks). She's going to keep her limbs and enjoy being extra spoiled for the rest of her days. Living it up like Queen Latifah in Last Holiday.
#cat#kitty#Tsuki#tsukimeow#cancer sucks worse that this one developed from an injection of disease preventing something
4 notes
·
View notes
Text


PLEASE READ‼️
my brother and his wife’s cat toby has been diagnosed with a very serious and rare form of cancer and will need upwards of $10,700 CAD to cover treatment. toby is a young cat with a ton of life left in him - it would be a complete and utter tragedy for his days to be cut short.
please consider donating here, and read below for more info on toby’s condition.
-
“At the beginning of the year Toby was diagnosed with cancer, specifically Injection-site Sarcoma (ISS), at only four years old. We learned without treatment my little boy would only have approximately one year left to live. ISS is a tumor caused by vaccines, injections and potentially genetics. Towards the end of 2019, we noticed a small lump on Toby's back and brought him to the vet. We were informed he would need a biopsy to identify it, which was about $800.00. As soon as we had the money we brought him in for his operation, and about an hour before I was allowed to pick him up I received a phone call from the vet technician. She called to let me know they had decided to do a lumpectomy since it had been larger than they had previously been able to see and it appeared to be more serious. Due to this, Toby's back had been almost entirely shaved and he had 25-30 stitches spanning the lower width. It hurt so much to see him like that, but he stayed strong and reminded us we needed to stay strong for him too. We spent every moment with Toby while he healed, constantly staying no further than a couple steps away. He healed so well, and had so much energy we began to feel relief and reassurance, until we received the phone call with his test results.
We were told Toby has cancer and was going to need extensive treatment in Guelph. This treatment will include: X-rays $200.00 Bloodwork $200.00 CT Scan $1,000.00 MRI $800.00 Chemotherapy & Radiation therapy $6,000.00 Follow up surgery $2,500.00
With the arrival of Covid-19, my workplace, as well as my husband's were shut down. I had no way to continue raising funds for his appointment due to bills needing to be paid. My workplace has been given the okay to re-open, however living on a single income still makes it hard to save. Any money I have leftover has been put into Toby's fund however, without receiving financial help, he might not even make it to his appointment. If you can spare any amount, Toby will be one step closer to his second chance at life. One that was jeopardized by the very vaccinations that were supposed to ensure he lived long and comfortably. Toby is fighting this with all of his strength, he just needs a helping hand. If you are able to donate even a little bit then you can help give Toby his Second Chance, so please donate today! #Toby'sSecondChance”
2 notes
·
View notes
Text

What a month
First off, Oberon is alive and kicking, sort of. It turned out that he did not have dropsy and my best guess is perhaps septicemia (water quality has been and remains pristine, so I’m still shocked either way)? He has a mass or lesion under his jaw that has gotten larger this past week and his right eye seems completely blind. However he is no longer bottom sitting as much or gasping as desperately. His is not the same happy fish as before, but I’m not longer considering euthanasia first and foremost. I just started his antibacterial treatment because he seemed to have plateaued while I was dealing with the other huge issue...

My cat has an injection site sarcoma from her rabies shot! Or rather, she had one. The vet amputated her leg yesterday and we picked her up today. She is recovering brilliantly, much better than the vets anticipated. Its still been a huge point of emotional and financial stress, and until the sutures are out, a large consumer of my time.
Poor Oberon has to take the back seat in all this kerfuffle, but thankfully healed rather well on his own. I don’t know if he is the way he is a result of permanent damage from his illness or if he is still sick, but time will tell I suppose.
#cw sick pet#fishblr#catblr#bettablr#sick fish#sick betta#oberon#oberon king of the cherries#sick cat#ISS#injection site sarcoma#sarcoma
1 note
·
View note
Photo
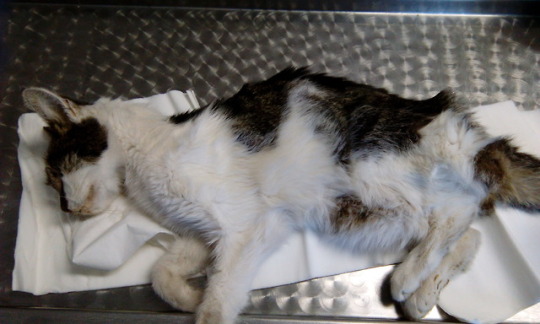
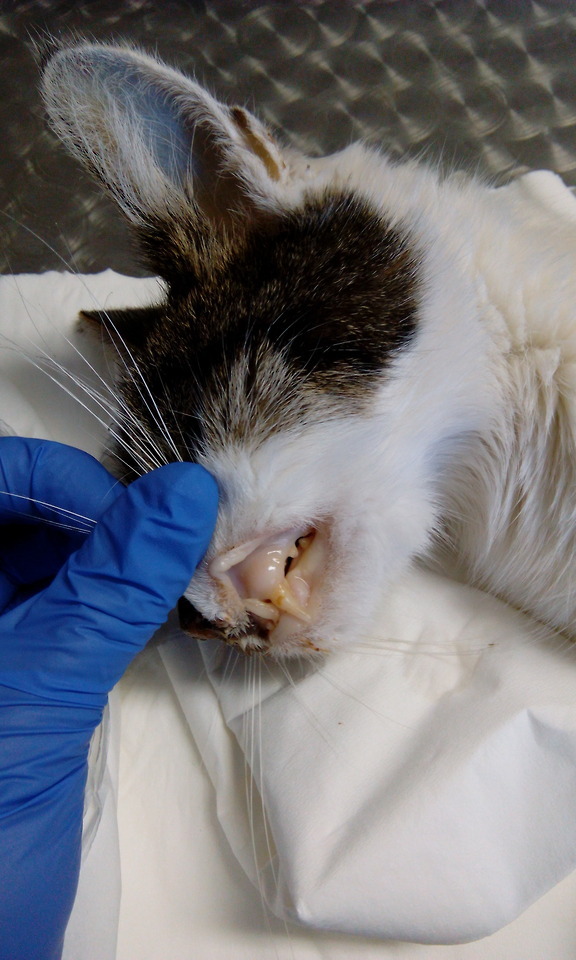
I will probably lose a lot of followers, and get anon hate again for posting something like this, but if seeing these photos will change someone’s mind about letting their cats roam freely, it is worth the effort. Pictured above is a 4-year-old (!!!), unvaccinated, intact free-roaming female cat, which was presented for inappetence. When I asked the owners for how long she has been anorexic, they shrugged and said ‘a couple of days’, although I found it hard to believe, while examining the moribund cat on the table in front of me. As you can notice, she is severely dehydrated, cachectic (loss of weight and muscle mass), anaemic and has a body condition score of 1. She also had purulent discharge coming from her eyes and nose, severe bronchitis, halitosis due to uraemia, stomatitis and lingual ulcers, diarrhoea. She tested positive for Feline Leukaemia Virus(FeLV) and the lab results suggested acute kidney failure. Needless to say there was nothing I could do, except end her suffering. FeLV is shed in the saliva and nasal secretions, urine, faeces and milk of the infected cats, and is spread especially through bite wounds, but also grooming, shared litter boxes and dishes, and from mother cats to their kittens either in utero or via nursing. At my clinic, we call FeLV ‘the chameleon’, because it manifests through a multitude of symptoms that are actually caused by secondary diseases, not the virus itself. An infected cat may be asymptomatic for weeks, months or even years, but it keeps shedding the virus. FeLV causes blood disorders that lead to the deterioration, and thus, suppression of the immune system, so the cat acquires severe forms of diseases caused by bacteria, fungi, viruses or parasites that usually do not affect an otherwise healthy cat. The sings of the disease are not very specific. Anorexia, anaemia, poor coat condition, fever, gingivitis, stomatitis, respiratory tract infections, diarrhoea, urinary infections, enlarged lymph nodes, abortion, eye diseases- these are the most commonly observed symptoms, a lot of which were present in the cat I examined. ELISA and PCR are the most commonly used methods of testing. At the moment, there is no definitive cure for FeLV, so the treatment is symptomatic. Antibiotics, blood transfusions and keeping the cats indoors is the mainstay of therapy. I cannot stress this enough: KEEP CATS INDOORS. All cats should be tested prior to introducing them to a multi-cat household. FeLV, in itself, is NOT a death sentence. An infected cat can live a long a relatively normal life, although the median survival is 2,5 years, and that can be emotionally devastating for the owner. A FeLV positive cat should be closely monitored for any of the symptoms enumerated above and any suspicion should prompt a check-up at the vet. Even though there has been some association between FeLV vaccine and injection site sarcomas in cats, the vaccine is rather safe and effective, although not 100%. Preventing exposure is the most efficient way of protecting cats against FeLV. Same goes for FIV and FIP. Keep your cats indoors.
195 notes
·
View notes
Text
Glimpses on Cystic Swellings around the Knee in in Open Access Journal of Medical and Clinical Surgery by Thulasivasudevaiah Narayan*

Abstract
The most common presenting complaints in the orthopaedic Out-patient department are knee pain due to osteoarthritis. Many patients present with swelling around the knee due to benign disorders. The majority of the swellings are cystic in nature and the differential diagnosis depends on the anatomical location of the cystic swelling and the radiological findings. We made an attempt to discuss the presenting clinical features, investigations, and operative findings among the few knee swellings presented in the surgical wards. The most common cyst in relation to the knee is Baker’s cyst, semi- membranous bursa, ganglion cysts. In our discussion we are excluding the acute inflammatory diseases of knee namely septic arthritis, cellulitis/abscess around the knee. A case of Ganglion cyst of the peroneal nerve and other cystic swellings were presented in this article.
Keywords: Ganglion cyst; Peroneal nerve; Baker’s cyst; Epidermoid, Bursa; UGAFI
Introduction
Cystic swellings around the knee are benign in nature; some of them are due to chronic inflammatory pathology. To understand the diagnostic criteria, we present different types of cysts around the knee. All patients were evaluated pre-operatively by taking detailed history and clinical findings were recorded and subjected for surgical excision. The patients were followed up for a minimum period of 4 weeks and the Biopsy findings were noted.
Case Summary-1
A 54-year-old male presented with history of swelling over the front of right knee for 6 months. He has noticed the swelling following injury over the right knee, which was gradually increased in size over a period of 6 months. He has noticed pain and skin changes (scaling) for 15 days. On admission his vitals were stable with BP-130/80 mm of Hg. Local examination of right knee showed an irregular well-defined swelling of ,8cm X 6 cm with bosselated surface and thinning of overlying skin due to stretching (Figure 1). It was tender with variable consistency. The knee joint mobility was normal.
There was free mobility over the underlying patella (Figure 1). The inguinal lymph nodes were not enlarged. A clinical diagnosis of pre patellar Implantation dermoid cyst was made. The Cystic lesion was excised through an elliptical incision under spinal anaesthesia. There was pultaceous material drained from the ruptured thin wall of the cyst. The resulting wound closed primarily. The Histopathology revealed features of chronic granulomatous lesion. The sutures were removed on 14th day, with good scar.
Case Summary-2
A 40-year-old male presented with a swelling over the right knee for 1 year duration. It was painless, with no history of trauma. On clinical examination it was 5cmX4cm in size, cystic in nature , non-tender, freely mobile over the patella (Figure 2). A clinical diagnosis of pre-patellar bursa was made. The lesion was excised under local anaesthesia. The cyst was containing gelatinous fluid. Post operatively patient was treated with oral Antibiotics and analgesics. Following suture removal on 10th day, the scar was healthy. There were no complications in the post-operative period. Histopathology was not performed as operative findings were suggestive of benign lesion (bursa).
Case Summary-3
A 50-year-old female presented with history of swelling over left lower limb for 6 weeks. She also complained of tingling sensation in the left lower limb since 1 month. She has noticed a swelling over the side of left leg insidiously, with mild pain. She was not a diabetic or hypertensive, and there was no history of trauma. Her blood investigations - Hb%-12.6 g. TC-7000cells/cumm, DC-N-57%,L-37%. Local examination of the left leg showed an elongated slightly tender cystic swelling over the lateral aspect lying about 3 cm below the left knee joint (Figure 3). There was no free mobility of the swelling. It was transilluminant. Ultra sound (surface scan) of the swelling was suggestive of Ganglion cyst of the Common peroneal nerve.Under spinal anaesthesia by a vertical incision along the cyst was dissected from surrounding structures (Figure 2). The cyst wall was very thin and it has ruptured during dissection and gelatinous fluid evacuated from cyst. The cyst wall separated from the peroneal nerve trunk and excised. Wound closed in layers. Post-operative period was uneventful. There was no neurological deficit noted during follow up period.
Case summary – 4
A male patient aged 55 years, who is agriculturist by occupation presented with a swelling over the lateral aspect of right knee for 8 months. There was history of thorn prick while working in the field, following which 2 months later he has noticed a swelling at the site of prick. The clinical examination of the swelling was suggestive of implantation dermoid cyst. It was excised successfully under local anaesthesia. Patient was followed up on OPD basis. HPE was suggestive of dermoid cyst.
Case summary-5
An adult male aged 50 years was admitted with history of swelling over the back of knee for 1 year. There was no history of pain in the swelling; patient says the swelling is more obvious on standing posture. There is no history of knee pain or knee joint swelling. On examination there was a soft cystic swelling in the right popliteal area, measuring 5X4 cm with smooth surface, ill-defined borders. It was less obvious on flexion of the knee. The movements of the right knee were normal. A clinical diagnosis of Baker’s cyst was made (Figure 4). The surface scanning was showing features of infected Baker’s Cyst . The cyst was excised under spinal anaesthesia, and patient was discharged after 3rd day with oral antibiotics. All sutures were removed on 10th day, scar was healthy.
Discussion
Clinician must be aware of differential diagnosis of the cystic swellings around the knee before requesting for a radiological investigation. The Baker’s cyst is known to all medical students as it is commonly seen in the surgical or orthopaedics OPD. But In our surgical practice many pathological conditions can occur around the knee starting from cellulitis, to osteoarthritis. Patients can present with a pain less swelling around the knee, and most of them are cystic in nature. We made an attempt to describe the cystic swellings presented to our surgical wards with different clinical features. The Clinical diagnosis depends on the anatomical location, and associated history.
The cystic swellings around the knee [1] can be Classified as:
True Cysts.
synovial cysts- Baker’s cyst, Proximal tibiofibular joint.
Ganglia- Gastrocnemius, Popliteus, Peroneal nerve ganglion (Figures 3a & 3b).
Bursa- Prepatellar, Infrapatellar,Pes anseinus,
Meniscal Cyst- Intrameniscal, parameniscal, Synovial
Lesions that mimic cysts
- Haematoma, seroma, Abscess,
-Vascular lesions- Popliteal artery Aneurysm, Varices (Figure 5), Haemangioma
Neoplasms- Synovial sarcoma, peripheral nerve sheath tumor. Myxomatous neoplasms.
The pre-patellar bursa is located anterior to the patella, deep to the subcutaneous soft tissue. Direct trauma to the patella can lead to inflammation of the bursa. This is an example of Housemaid’s knee where the patient will have repetitive injury to bursa.
Ganglion cyst of the peroneal nerve: The common peroneal nerve (CPN) arises from the L4-S1 nerve roots. It gives rise to lateral cutaneous nerve of calf. The CPN provides sensory innervations to the antero-lateral and dorsal aspect of the foot, as well as motor innervations to the anterior and lateral compartment muscles. The CPN divides into superficial and deep peroneal nerve in the fibular tunnel. It can be affected by extra neural compression from the habitual leg crossing, anorexia, previous regional limb surgery with immobilization cast, ganglion or Baker’s cyst.
Intraneural ganglion cysts are benign mucinous lesions in the peroneal nerve [2]. The cause for the development of this cyst is due to tracking of fluid from the joint through a small tear in the joint capsule (Superior tibiofibular joint). They can present with a swelling over the lateral aspect of knee with neuropathy symptoms. Patient can present with parasthesia over the dorsum of foot and foot drop due to intraneural ganglion cyst following trauma [3-6].
There may be associated muscle atrophy in the nerve distribution. Ultrasound examination of the cyst showed multiloculated fluid collection in close relation with common peroneal nerve [4]. The differential diagnosis of the peroneal nerve cyst is Neurilemmoma, Neurofibroma, neuroma. Early diagnosis and appropriate surgical treatment of this condition is a key to good outcome. Delayed diagnosis can lead to partial relief of symptoms [5]. In our case of Ganglion cyst of peroneal nerve left leg, the patient noticed improvement in the movement of foot with disappearance of numbness over the dorsum of foot in 2 weeks after the excision of the cyst.
The Popliteal (Baker’s) cyst is common cystic swelling in the popliteal region due to communication between the posterior joint capsule and the normally occurring gastrocnemius-semimembranosus bursa. They are lined by synovium, may be simple or septated and contain haemorrhage, debris or loose bodies. Many are asymptomatic, they can cause limitation of flexion of knee, and they can rupture with symptoms similar to Deep vein thrombosis of leg. UGAFI- (Ultrasound guided aspiration fenestration and injection) is an effective and safe treatment option for symptomatic popliteal cyst. This is accomplished by aspiration and fenestration by spinal needle followed by injection of 1 ml triamcinolone&2ml of 0.5% Bupivacaine into the decompressed remnant [7].
Implantation dermoid occurs most commonly in the Foot or hand among agriculturist /tailors due to thorn Prick. The swelling is cystic in consistency, fixed to skin, freely mobile over the deeper structures. In our patient the dermoid was over the pre- patellar region with thinning of skin with impending rupture. During surgical excision, the sac was ruptured at thinnest point to drain the pultaceous material. This epidermal inclusion cyst over the pre patellar area can mimic chronic pre-patellar bursitis [8]. The cystic lesions around the knee should be radiologically investigated (Ultrasound /MRI) to know the character of the content. Routine MR Imaging of the cystic swellings in the soft tissues exhibit high signal intensity on T2 –weighted images because of their high content of free water [9].
Conclusion
Acute painful conditions in the knee can be due to infective lesions like cellulitis, pyogenic abscess like in other parts of the lower limb. Cystic swellings in the soft tissues of knee can be provisionally diagnosed due to their anatomical location and clinical findings. Most of the cystic lesions are superficial and they require MRI imaging studies to know the character of contents. These cystic lesions are amenable to excision with good post-operative results. Careful dissection is necessary in case of peroneal nerve ganglion cyst.
Regarding our Journal: https://oajclinicalsurgery.com/ Know more about this article https://oajclinicalsurgery.com/oajcs.ms.id.10023/ https://oajclinicalsurgery.com/pdf/OAJCS.MS.ID.10023.pdf
#Ganglion cyst#Peroneal nerve#Baker’s cyst#Epidermoid#Bursa#UGAFI#Thulasivasudevaiah Narayan*#oajcs#clinical surgery
0 notes
Text
I’m having a little weird evening anxiety but it’s been a good - but very busy - couple of days. Today was a rest day, so step goal wasn’t met. My calories were high, but I drank all my water and took my meds. The calorie thing will even out, I just feel a little weird about it because I was hungry all freaking day.
I’m almost done reading my 20 pages of Tocqueville. And I think that’s all my accountability stuff.
Sheba goes back to the vet tomorrow for her booster shots. The probiotics have helped, though she still has some soft stools. But she’s not having such major stomach issues that she can’t make it to the litterbox and honestly, she’s had stomach upsets off and on ever since she’s lived here, so it’s kind of normal. But she did develop a lump on her leg where they give one of the vaccines. :( Frown emoticon because I’m a massive worrywort and I lost a cat a couple of years ago to vaccine induced sarcoma. I know those are very rare - I think I read that it’s between 1 in 10k to 1 in 30k cats that get it, so the odds of my having a second one are pretty slim. The lump hasn’t changed size since it came up, so I am currently taking that as a good sign, but I will have the vet look at it, also.
I know cats sometimes develop injection site lumps like this one, and they go away on their own.
I’m also getting a little out of sorts because mice are starting to come into the house again. It happens out here - the time of year is right, and since I live in the middle of a forest, mice are abundant. This is why I don’t discourage snakes around the yard (except rattlers) and have plans to make owl nesting boxes. My organic indoor pest control measures are kind of lazy, though.
1 note
·
View note
Text
High Risk HPV, HSIL and Primary Diffuse Large B Cell Lymphoma of Cervix: An Unsual Case- Juniper Publishers

Abstract
Primary malignant non-Hodgkin’s lymphomas in the female genital tract are rare, accounting for less than 1% of all extranodal non-Hodgkin’s lymphomas. HPV infection has well been documented as the causative factor for Carcinoma cervix; not malignant lymphoma of cervix. Here we report an interesting case of primary non-Hodgkin’s lymphomas of uterine cervix with proven HPV 16 infection and High grade squamous intraepithelial lesion with co-existing diffuse large B-cell lymphomas (DLBCL) on histopathological examination and immunohistochemical study. The patient was successfully treated with chemotherapy after Cervical Conisation for HSIL and is now in complete remission with follow up period of 11 months. Gynecological lymphomas can be a diagnostic challenge due to nonspecific symptoms. However, when diagnosed and treated they have a good prognosis. Clinicians should therefore include lymphoma in their differential diagnosis when investigating gynecological symptoms.
Case report
28-year-old lady went for a routine gynecological checkup where a Pap smear was taken. The report came as Low grade squamous intra-epithelial lesion (LSIL). HPV test was done; it came as positive for genotype 16 which is consistent with high risk HPV, which is a proven carcinogenic virus for cervical cancer. Colposcopic biopsy soon followed and it showed (Figure 1) High grade squamous intraepithelial lesion (HSIL) (CIN III). Cervical LEEP excision was done to cure the disease. The specimen measured 4.5x3x1cm and was oriented at 12 o’ clock. It was inked and serially sliced. The sections showed foci of epithelial dysplasia involving the entire thickness with loss of maturation and presence of hyperchromatic pleomorphic nuclei with involvement of the endocervical glands. The features were in keeping with High grade squamous intraepithelial lesion (HSIL) (CIN III) (Figure 2a). No histological evidence of stromal invasion was seen.
The sub epithelial region showed (Figure 2b) sheets of neoplastic lymphoid cells with irregular nuclear contours, vesicular nuclei, occasional prominent nucleoli and moderate amount of eosinophilic cytoplasm. Mitosis was frequent. Spindling of tumour cells was evident in areas. Immunohistochemical work up showed the tumour cells were positive for CD20 (Figure 2c) while negative for CD3, CD10, Bcl-6 and Cyclin D1. The neoplasm extended up to the deep resection margin. The final diagnosis was given as High grade squamous intraepithelial lesion (HSIL) (Cervical intraepithelial Neoplasia III/ CIN III) with Non-Hodgkin’s Lymphoma B-cell type; Diffuse Large B Cell (DLBCL) Further staging work up and imaging was done (Figure 3) which showed extension of neoplasm to the vaginal fornices, the anterior vaginal wall and the parametrium with involvement of the left ureteric wall and subsequent mild hydronephrosis.
CT neck, chest and abdomen showed no evidence of metastasis. In chest and abdomen; no significant abnormality noted. No significant lymphadenopathy or metastasis in chest. In abdomen, liver was displaying multiple hepatic focal lesions with progressive fill in the contrast likely hemangiomatous left hydroureteronephrosis, left ovarian cyst, retained fluid within the uterine cavity. PET CT scan impression came as hypermetabolic lesions involving the cervix with vaginal and parametrial involvement in keeping with biopsy proven metabolically active lymphoma. The remainder of the study shows no evidence of FDG avid lymphoma. Mild left hydronephrosis was noted. Since Lymphoma of cervix is a very uncommon lymphoma type and surgery has removed most of the disease, in the tumour board it was planned to consider chemotherapy followed by radiotherapy based on available data; measures that could be used in treating lymphoma of cervix. Different options of treatment was discussed and finally planned to give her 6 Cycles of R-CHOP followed by PET- CT and involved field Radiotherapy.
Since the patient was just engaged only and with no children, fertility issue had been discussed with her. Patient decided not to do any fertility preservation procedure. So prophylactic Goserelin injections to increase the chance of being fertile was also planned; once every 4th week up to 6 months after last chemotherapy. After 6 cycles of R- CHOP the patient was sent for PET- CT and impression showed a complete response to therapy. Hence a follow up PET- CT was planned after 3 months. This also showed complete response. The case was rediscussed in the tumour board and since the patient being young, unmarried and with no children and had a complete metabolic response to treatment, it was decided not to give her any Radiotherapy; but to follow up with 6 monthly PET- CT and bloods. To date 13 months after the diagnosis, she is healthy and disease free.
Discussion
Primary cervical lymphoma is rare and involvement of the cervix by a lymphoproliferative disorder is more commonly seen in the setting of systemic disease [1]. It affects adult women over a wide age range. Vaginal bleeding is the most common symptom. Lymphomas are often bulky tumours, sometimes with circumferential enlargement of the cervix (“barrel-shaped” cervix) [1,2]. Cervical diffuse large B-cell lymphomas, which is the predominant type are are often associated with prominent sclerosis and may be associated with a cord-like arrangement or spindle-shaped tumor cells (“spindle cell variant”) [3]. Rare cervical marginal zone lymphomas (MALT lymphomas), Burkitt lymphomas [4] and extranodal NK/Tcell lymphomas, nasaltype, have been described. Differential diagnoses of cervical lymphomas include sarcoma, poorly differentiated carcinoma, neuroendocrine tumours, Malignant Mixed Mullerian tumour, Melanoma, extraosseous Ewing’s sarcoma, and chronic cervicitis. Most cases of NHL involving uterine cervix presents at stage I or II. The optimal treatment of such tumours is not clear. These tumours have been managed with chemotherapy, [5] radiotherapy, and surgery, alone or in combination [6]. Heredia et al. demonstrate the use of combination of CHOP × 3 plus involved field radiotherapy as therapy for this malignancy [7]. The association of HPV infection with cervical cancer is well known; though literature on HPV association to cervical lymphoma is scanty. A Danish study [8] noted that HPV infection is associated with an increased risk of Lymphoma. This association may be attributable to a chronic immune activation induced by persistent HPV infection and/or failure of the immune system both to clear HPV infection and to control lymphoma development.
Conclusion
In our patient the rare combination of High-risk HPV, Lymphoma and High grade squamous intraepithelial lesion was quite interesting. But the efficient interdisciplinary discussions gave her a wonderful outcome.
https://juniperpublishers.com/ijcsmb/IJCSMB.MS.ID.555666.php
https://juniperpublishers.business.site/
For more Open access journals please visit our site: Juniper Publishers
For more articles please click on Journal of Cell Science & Molecular Biology
0 notes
Text
A tale of two pandemics: AIDS and COVID-19While AIDS and COVID-19 have both left marks on the world, they are very different beasts
André Picard, The Globe and Mail
Friday, June 04, 2021
On June 5, 1981, a short article titled “Pneumocystis Pneumonia – Los Angeles” appeared in Morbidity and Mortality Weekly Report, a journal published by the U.S. Centers for Disease Control.
Little did the authors know that the dry case report about a cluster of “5 young men, all active homosexuals” with PCP, a rare form of pneumonia, would herald the arrival of HIV-AIDS, one of the worst pandemics in human history.
Similarly, the moderator who posted chatter on the Chinese social-media site Weibo about an “urgent notice on the treatment of pneumonia of unknown cause“ in Wuhan on Dec. 30, 2019, on the ProMed (Program for Monitoring Emerging Diseases) listserv likely had no idea that it was a harbinger of an earth-shaking pandemic. (China did not formally notify the World Health Organization about the spread of a novel coronavirus until Jan. 8, 2020.)
Today, on its unofficial 40th anniversary, AIDS almost feels like yesterday’s news, overshadowed by COVID-19, an in-your-face pandemic of the digital age.
While AIDS and COVID-19 have both scarred the world, they are very different beasts.
Human immunodeficiency virus, which is spread in bodily fluids like semen and blood, has infected an estimated 76 million people, 33 million of whom have died.
SARS-CoV-2, the airborne virus that causes COVID-19, has infected almost 175 million people and caused more than 3.7 million deaths, making it more easily spread but far less deadly than HIV.
And, of course, no one yet knows how long COVID-19 will be around, or what the long-term health consequences will be, especially for the significant minority of the infected who seem to be developing chronic symptoms.
Still, there are many parallels, many common lessons unheeded, and much to learn about bolstering public health in this tale of two pandemics.
If anything, AIDS should remind us that, for all the havoc COVID-19 has caused, it could have been much, much worse in the short term, and we should not make too many assumptions about how it will play out in years to come.
Dr. Catherine Hankins, a professor of public and population health at McGill University in Montreal, distinctly remembers reading the now-iconic MMWR report 40 years ago. “It was one of those ‘where were you when…’moments,” she said.
In pre-internet days, medical journals came in the mail and infectious disease experts such as herself read MMWR religiously. An unusual pneumonia in five otherwise healthy men hinted at something new and worrisome. One month later, on July 3, 1981, MMWR published a second report that sealed the deal.
Titled “Kaposi’s Sarcoma and Pneumocystis Pneumonia Among Homosexual Men – New York City and California,” the study reported the cases of 26 gay men who had an unusual combination of a rare pneumonia, PCP, and even rarer form of cancer, KS.
That same day, The New York Times published an article titled “Rare Cancer Seen in 41 Homosexuals,” which is often described as the first coverage of AIDS in the mainstream media. (Gay publications such as the New York Native had already been reporting on rumours of a “gay cancer.”)
“It took a few weeks to realize it was an infectious disease, but it was clearly something new and important,” Dr. Hankins said. All over the world, public-health officials and clinicians began to understand why they were seeing gay men falling ill and dying in large numbers.
The new virus changed the course of Dr. Hankins’s career. She went from working on preventing hepatitis B in babies to studying what was initially dubbed GRID (gay-related immune deficiency), including early work on the spread in prisons and among injection drug users.
Dr. Hankins is still at it four decades later. She is also a key member of the COVID-19 Immunity Task Force, and that’s not a coincidence.
A year prior to the emergence of HIV-AIDS, in 1980, the World Health Organization declared the end of smallpox, the first disease to be eradicated in human history, thanks to vaccination.
It was a heady time. Many scientists believed that the end of infectious diseases was nigh – a rather pompous conviction that there were likely no new pathogens to be found, and if they did emerge, they could be quickly quashed.
AIDS was a brutal wake-up call.
It also spurred a resurgence of interest in epidemiology and immunology, which has paid great dividends since, and especially during COVID-19.
Today, the spread of the novel coronavirus is being tracked around the world virtually in real time and we know more about its immunology than any pathogen in history. Not to mention that the genome of the virus was decoded in mere weeks.
More importantly, there is a COVID-19 vaccine. Several actually, and more than 150 others in development.
On April 23, 1984, Margaret Heckler, the U.S. Secretary of Health and Human Services, told a packed news conference that a team led by American scientist Robert Gallo had discovered HIV, the virus that causes AIDS. (It turned out that a team of French scientists had actually discovered the virus in May, 1983, and shared samples with the Americans. After years of acrimonious legal battles, they are officially co-discoverers, although only Dr. Luc Montagnier, and his colleague Françoise Barré-Sinoussi, were awarded the Nobel Prize.)
What is also memorable about Ms. Heckler’s announcement is that she vowed that an AIDS vaccine would be available within two years, a prediction that turned out to be spectacularly wrong. In 1997, U.S. president Bill Clinton made a similar pledge, but said it would take 10 more years. That goal went unaccomplished, too.
So why have scientists been able to develop COVID-19 vaccines so quickly, but failed repeatedly do to so for AIDS?
The problem is principally the virus itself. HIV is far more complex and wily than SARS-CoV-2. HIV is good at hiding and moves slowly and stealthily. (It can often take a decade before an infected person develops serious symptoms.) Worse yet, HIV infects the very cells a vaccine would need to trigger an immune response, and it can hide undetected in viral reservoirs and resurface again. The coronavirus, by contrast, is easy to detect, stymie and eliminate from the body.
There is also a question of political will. There have been many AIDS vaccine initiatives but never one with the urgency or breadth and financing of Operation Warp Speed, a U.S. initiative to develop COVID-19 vaccines quickly.
Governments around the world signed advance purchase agreements for billions of doses even before COVID-19 vaccines were developed, providing both funding and tremendous incentive for companies to succeed. Canada alone committed to buying 400 million shots.
In contrast, HIV vaccine development remains stalled – but it could be reinvigorated by the success of mRNA vaccines for COVID-19.
“The big and last Holy Grail we have to develop is a safe and effective vaccine,” Dr. Anthony Fauci, director of the U.S. National Institute of Allergy and Infectious Diseases, said in an interview with HIV Unmuted, a podcast of the International AIDS Society.
While he has become a household figure during COVID-19, Dr. Fauci is also a lodestar of AIDS, having started researching the disease just weeks after the first MMWR publication. The U.S. National Institutes of Health are, by far, the biggest funders of AIDS research in the world.
The closest thing HIV has to a vaccine is antiretrovirals, cocktails of drugs that are used to keep the virus from replicating. That suppression makes it virtually impossible to transmit the virus and unlikely that infected people will fall sick.
It is a major improvement from the early days of the pandemic: Treatments have gone from non-existent, to complex and brutal, to incredibly effective. Some people now take only a single pill daily to control HIV. Given the aging demographic of those infected, and the damage caused by long-time treatments, however, many take a myriad of pills for conditions such as heart disease and diabetes.
Despite the lack of vaccines, both HIV infections, which peaked at 3.3 million in 1997, and AIDS deaths, which hit almost two million in 2006, have come down tremendously over the years. In 2019, there were “only” 1.7 million people newly infected with HIV, and 690,000 AIDS deaths. Treatment as prevention (TAsP), an approach developed in Canada, has contributed to the steep decline in cases. The concept is illustrated in the slogan U = U (undetectable = untransmittable).
In wealthy countries, HIV cases have largely disappeared outside of marginalized groups such as intravenous drug users and sex workers. The vast majority now occur in southern Africa.
This illustrates one of the many parallels Dr. Fauci sees between the pandemics, both in the scientific and political response. Infectious diseases always prey on vulnerable populations, and there are always groups who are harder hit, whether it’s gay men for AIDS or elders for COVID-19.
Dr. Fauci said on the podcast his greatest fear is that, as with AIDS, Western countries will control the initial surge and then move on, leaving the developing world to cope with the burden of COVID-19 for years to come.
In the 2020s, just as in the 1980s, it is well-off countries and individuals who are benefiting disproportionately from both new prevention programs and treatments.
As effective as HIV treatments are, it remains a struggle to get them to those who can most benefit. Of the 37.6 million people in the world living with HIV, 27.4 million have access to antiretrovirals, a vast improvement over the 7.8 million a decade ago, but still leaving many to suffer and die. Even in wealthy countries such as Canada, ARVs can be too costly, and are not covered by public-health plans in all provinces.
A similarly cruel pandemic math is playing out with COVID-19. Countries such as India and Nepal are experiencing deadly shortages of basic medical supplies, including oxygen.
Of the almost two billion vaccine doses administered worldwide, only a tiny fraction of shots have gone to those living in the developing world. The recovery is being enjoyed by the haves, not the have-nots.
Ron Rosenes, a long-time AIDS activist, was diagnosed with HIV in 1987, but is sure he was infected in the late 1970s when, like many of his generation, he revelled in the sexual liberation movement and was a frequent visitor to some of the over-the-top discos of New York.
Today, he says: “I’m a survivor, witness and pioneer – among the first generation to age with HIV.”
Echoing Dr. Fauci, Mr. Rosenes said his greatest frustration with COVID-19 is seeing the same prejudices and inequities surface 40 years after the advent of AIDS.
The scapegoating language, from “gay plague” to “China virus,” is similar. The tendency to blame “others” for the spreading of disease remains strong. With AIDS, it was gay men, and even individuals such as Gaétan Dugas. (The Canadian flight attendant was long described as Patient Zero, or the first case, when in fact he was patient O, the letter, for “out of California.”) Now, the COVID-19 finger-pointing is aimed at workers like those at the Wuhan seafood market (or, more recently, at a Wuhan microbiology lab).
The political unwillingness to invest adequately to protect those at greatest risk of newly emerging viruses – whether it’s gay men and hemophiliacs, or essential workers and elders – remains problematic. So too does the eagerness to move on when it’s only the marginalized who are still suffering.
Mr. Rosenes, at 73, was among the first to get the COVID-19 vaccine, and he hopes to see another world-changing scientific breakthrough. “I’m cautiously optimistic that I will still be around to see an HIV vaccine.”
He is only slightly less optimistic that he will be a witness to both the beginning, and beginning of the end, of two of the worst pandemics in history.
0 notes
Text
I hate that I have to give so many disclaimers when I bring up the subject of cat vaccines. I never want to inadvertently give any ammunition to the anti-vax movement. That said, here we go...
I’m currently trying to explain to my sister what to ask for when she gets her cats vaccinated. There ARE risks with feline vaccines that are NOT present for humans. Cats can develop injection-site sarcomas (humans don’t), so non-adjuvanted versions of vaccines are a lower-risk option. Cats can also develop kidney problems because distemper vaccines are cultivated in feline kidney cell culture (human vaccines tend to be grown in chicken eggs), and loose kidney proteins can inadvertently induce an immune response against a cat’s kidney cells.
Yes, sarcomas are still rare, and the amount of damage distemper shots cause kidneys is hard to determine, but these are still risks that can be reduced through thoughtful vaccinations. Distemper and rabies vaccines are absolutely so important!
But, the distemper shot (which is included in the FVRCP formulation) confers essentially lifelong immunity against distemper when given to a cat over 4 months old. Check titers if you want to confirm, but yearly vaccinations are not needed after that. That shot helps build immunity against a couple other viruses too, but not completely, and they are not dangerous and unlikely to reach an indoor-only cat with no exposure to outside cats, so it’s not worth risking kidney damage for those alone with excessive shots in my opinion. And, you can ask for the modified-live, non-adjuvanted version to reduce the risk of an injection site sarcoma.
With the rabies shot, you should get the 3 year one if your state will allow it. It’s hard to do multi-decade studies on cats, but what little research is out there does show that cats still have immunity against rabies for many years from a single shot, even from the 1 year formulation. Definitely specifically request the PureVax, non-adjuvanted rabies vaccine in either case, because this will also reduce the chance of sarcomas.
Anyway, I’m trying to get my sister to ask for these types, and she is SO resistant to the idea of bringing ANYTHING up to the vet that the vet doesn’t bring up first. She really doesn’t want to...potentially offend? And I guess I get it on some level because I’ve had that instinct too (I have outgrown it), but it’s really important to remember that 1) you absolutely SHOULD feel comfortable having a discussion with your vet about plans for your animal and decide together what is the best option for your cat’s specific situation. Even if you bring it up yourself, your vet should be happy to jump in and clarify things for you or be willing to find reasonable alternatives if you’re not comfortable with an option.
And 2) the reason, I suspect, that most vets don’t always bring up the “best” option themselves and default to the more popular option is because they get so much abuse all day long about how much clients have to pay, and if there’s an option that makes things cheaper, they assume that’s what you want. If a vet doesn’t bring up a treatment option that is objectively better, it’s usually not because they don’t know about it, but because it’s more expensive and they assume most people wouldn’t consider it. It’s amazing how many pet owners who love their animals start to say things like, “that much for a DOG?” when they see the bills. Hearing that all the time has an effect and a compassionate vet is always trying to find the line of offering the right treatment for the pet’s health but also at a reasonable enough cost that the owner will actually pay for it.
Anyway, the moral of this story is, take a deep breath, get up the courage, and talk to your vet about things! I’ve gotten over my “fear” because my vet is amazing and on the rare occasion when I bring up a concern she hasn’t already addressed (because she can read my mind), she is extremely open to a discussion and willing to educate me. You have a right to understand what’s going on with your pet’s health, and a good vet will want you to!
#my vet is so amazing#when I finally graduate (could be a while) I really want to leave#ideally...the country#and I would have no trouble giving up pretty much everything#but there is ONE thing that makes me go...oh#maybe that's worth staying here for#and that's my vet#She's so wonderful!!!!#my mom who is normally such a self-advocate is afraid of the vet too#she won't discuss anything with them!#is this a family thing or is this larger social thing that I don't understand
0 notes
Link
Our previous cat had to be put down about a year and a half ago after a horrible fight with cancer that left our entire family distraught and my Dad heartbroken. After coming back home for the summer, I was surprised that my parents had gotten another cat, about to be a year old now. However, when I asked my Dad about taking her to the vet, he grew uneasy and told me he hasn't taken her to the vet for anything yet aside from some vaccines she got as a kitten as well as getting fixed. Honestly, the thought of another cat of ours getting cancer terrifies me as well, but I know that even as an indoor cat she should probably be getting her vaccines and such.Is there anything I can do to try and convince my Dad to take her? via /r/cats
0 notes