#respiratory safety for healthcare workers
Explore tagged Tumblr posts
Text
"National Nurses United wrote to CDC Director Mandy Cohen on July 10 [2023] expressing concern about HICPAC’s guideline update, and nearly 900 public health experts on July 20 wrote a similar letter to Cohen, about the lack of transparency and the failure to address and protect against aerosol transmission of infectious diseases.
The CDC responded to the second letter on Friday, Aug. 19, but did not provide any indication there would be any traction to meet the requests to open up the process and involve key experts and stakeholders, according to one of the authors, Peg Seminario, an industrial hygienist who served for 30 years as the health and safety director at the AFL-CIO.
“We are deeply dismayed that the CDC response did not address any of our substantive concerns about the weakness of the guidelines,” Seminario said.
No minutes or transcripts of any HICPAC meetings so far in 2023 have been posted to the panel’s website.
Sharan said federal rules give the government three months or 90 days to post meeting minutes, and the June HICPAC minutes will be available within that time frame.
Including Wednesday, it has been 77 days since the June meeting. The deadline to post the minutes is Sept. 5.
Rachel Weintraub, executive director of the Coalition for Sensible Safeguards, urged the federal agency to immediately seek input on the rule proposals from the public, health care workers, unions, engineers with expertise in ventilation and research scientists with expertise in aerosols.
As the guidelines are being written, Weintraub also urged the CDC working group to create a public docket for the guideline’s development, including all meeting minutes, drafts, all scientific evidence used, and public comments submitted.
The Centers for Disease and Control and Prevention did not directly respond to Source NM’s question about whether they intend to create a centralized public docket specifically for the update to the Isolation Precautions Guidance.
“CDC hospital infection control measures are still failing to protect health care workers and patients,” Seminario said. “We need to do more. CDC must develop strong infection control guidelines that fully protect against aerosol transmission, and open up the development process to include necessary experts and members of the public.”"
#cdc#national nurses united#nurse union#hicpac#respiratory safety for healthcare workers#healthcare#mask#masks
3 notes
·
View notes
Text
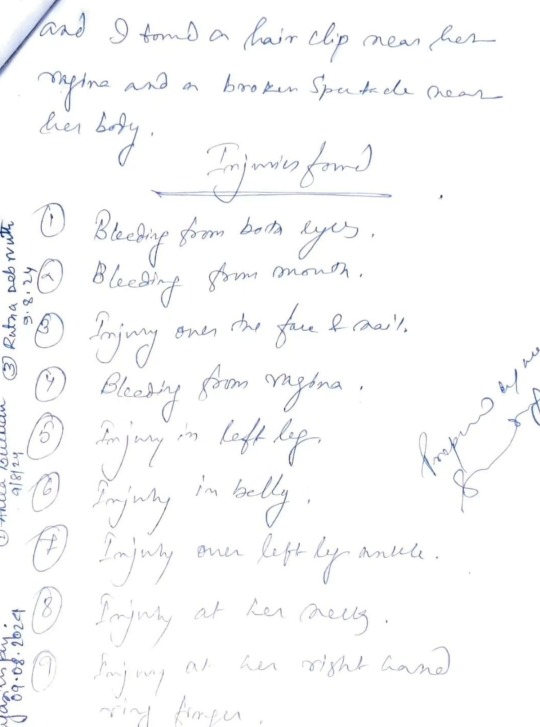
She has not just been raped and murdered, she was very much tortured and brutalized like Nirbhaya. It is all over the Bengali news. I don't understand why no one is talking about this.
A 2nd year Respiratory Medicine in a well known government medical college in Kolkata, West Bengal, India is found in a semi-naked state and the college/ hospital called it a suicide.
I'm a MBBS student in second year. After reading about her, what crossed my mind is the amount of times she would have felt this fear, before this worst fear of hers eventually materialized.
"A young resident doctor was found dead in the seminar room of her medical college in Kolkata. Initial autopsy report suggests possible rape and murder."
As all are saying,
She wasn't walking the street at odd hours. She wasn't wearing clothes that were provocative. She wasn't loitering in dangerous neighbourhoods.
She was a resident doctor, looking for a place to rest in her own hospital.
She had been on duty and had gone to rest in the early hours of Friday.
The one place which was supposed to guarantee her safety failed her, miserably.
Someone comes, rapes a female pg who is merely resting in a seminar hall because there is no proper place for her to rest, brutalized her and kills her. How did NO one know? The college and police initially call it a suicide. Excuse me? It is also being said that under pressure from local politicians, the Principal and Dean attempted to alter the post-mortem report. Autopsy confirms sexual assault.
What are the actions taken? One man arrested because his behavior seemed "shady". This is clearly not an act of one man. And this was a very well aware of and a well executed criminal act.
Also, all this happening in WB right when the situation of bangladesh is in turmoil and news of Bangladeshi Hindus being killed and tortured, seems wrong, VERY WRONG. Happening right before NEET-PG, as 24 lakh doctors prepare to write an exam on Sunday to be resident doctors, this news has wrapped us all in agony and rage,
What are they working so hard for? Why should they aspire to be in a system that ignores their basic needs? The minimum requirement of a workplace is safety. That should be non-negotiable.
This profession demands extereme hardwork, a lot of mental strength and Physical Assaults, harassment, low paying jobs with odd working hours with intense humiliation. Now its the worst of all seeing a bright mind losing her life in the most disrespectful state of all. This should never happen to any woman.
I'd also like to question why isn't any big media house covering this news, where are all the international news channels all this time.
What are the students in other medical colleges doing? This talks about their own safety and lives. What are the medical students across the world doing? It's time for us to stand for the most basic Human right, safety.
Yesterday when my roommate, an MBBS final year intern was heading for her night posting, I feared and prayed for her to come back safely. Thinking about it, in a few years I will also have night posting, I'll also return from my hospital duties late at night. I'll also have to go through the same fear, and I'll also have to keep praying that my worst fears don't turn into reality. So many female doctors, nursing staffs, other Healthcare workers, other working women, non-working women go through the same fear, probably multiple times a day.
It is a shame to be born in such a disgusting world and society, it is shame to witness such a brutal crime, and it is a shame to live in this fear daily.
Those RAPISTS need to be hunged infront of the whole natio...if needed burned alive. People should fear the idea of raping, more than getting raped.
#medicine#desi teen#desi dark academia#desi things#desi girl#desi academia#desi#kolkata#west bengal#bengali#bangla news#bangla#indian#india#indian students#indian aesthetic#desi memes#desi culture#desi life#justice#justiceformoumitadebnath#nirbhaya#rape/noncon#not incorrect quotes#junko furuta#crimes against humanity#crime against humanity#crime against women#doctor#r g kar
1K notes
·
View notes
Text
Holy Shit, Worldbuilding?
I do my worldbuilding on the fly so it's definitely shakey. So awhile ago I did a whole like blueprint thing for Digits prosthetics. I've been wanting to do something similar with Donnie but that's a lot of machine. And I was reminded I never really did XD so have a very very simple write up/summary of some of the tech stuff in Robots & Gardens so far.
Tag list: @outpost51 @nanashi23 @winterandwords @jezifster2 @aether-wasteland-s @dumbthunder @manathen @the-void-writes @livums @vacantgodling (Let me know if you want to be added or removed from the taglist!)
Reoccuring in-world tech
Teched shades/Teched glasses ->
Pretty fucking common. Some people possess modded versions. You don't buy them modded you pay someone to mod them or you figure out how to yourself. Kinda like the equivalent of jailbreaking and modding a nintendo device (side tangent fuck nintendo).
They started strictly as business/work wear before coming to the public. For example I mention a sort of equivalent Digits and other construction workers have. It's work issued and they're actually safety glasses. So less customizable quirks. But work grade at least for the construction workers (and probably a lot of other trade work but we're gonna stick with construction right now) allows them to see plans, estimated scheduling, and general blueprints or schematics if needed. All visuals can only be seen clearly by the wearer themselves. From the outside the lenses tint. So you might catch light either on their face or peeking through the lenses but that's the most. Also massive rip if you need prescription lenses to see. You're either wearing contacts, going blind, or hoping a pair of prescription glasses can fit beneath.
For everyone else they are styled more like a very standard pair of glasses. There's a couple generations of them. With the most recent generations you can actually get them with prescription lenses (but you'll have to pay a shit ton more and it can damage some other functions. Mostly cosmetic but you can view things (news, shows, shit on the internet, etc), you can talk to other people (like calls), it can play music. The speakers are kinda shit though lol.

Lenses ->
Lol so yeah this is literally just contacts. Arguably far more dangerous and a risk than glasses. These are prescription and they are teched. Really simple advancement and not very widespread. Supposed to help with seeing in darker locations as well. Valuable for Hollis since she's technically doing illegal work and does have terrible vision. They can cause extreme eye damage. Great for precision jobs. They can cause extreme eye irritation and can blind you. The tech in the lenses can cause your eyes to appear another color. (Part of the reason why Hollis' eyes appear blue/blueish sometimes. Her natural eye color is brown).
Vapes ->
Lol they function just like normal ones. No one smokes tobacco really. They want death aggressive, fast, and fruit flavored.
Prosthetics ->
Very important. And hella reoccurring. A lot of people have them. Some people do by choice. But most don't, very common to have workplace accidents. Or to just need a modification for a job which is partially how we get to Donnie. They can vary a lot and the upkeep is costly. It's a whole business at this point the healthcare part has been stripped away from this common facet of the world. As in it's not always gotten out of benefit for the patient themselves but often encouraged and required. Through health they've gotten prosthetics more mechanic. Easier to mimic original human counterparts (human mobility is a wild thing y'all).
Filters/Filtration ->
I haven't dived super deep into this. Just know it's important and necessary. So people in smog ridden places (Which is a lot of places in this story) can breathe in their homes. And minimize some air contaminants and respiratory problems. Heavy on minimize cause it doesn't completely stop those problems.
Donnie's shit in particular
My beloved cyborg got a lot of shit going on. Please know that cyborg's are a rare phenomenon, his mods and prosthetics are top of the line because he works security, and he can only maintain them because of his economic status. But even then it's still a strain. On top of this he is mute which is a whole separate thing. It's not because of the prosthetics or anything. While they have some "fixes" they could've done for this they didn't want them.
He can sign but doesn't do it often because it's kind of a dying language in this world. And screen readers struggle capturing and understanding it. Most forms of communication with other people is gesturing and body language, typing/writing, or whistling (more specific situations for that one). But there's a secret here I am actively unclear how much of Donnie is machine and how much isn't like all the time. Which I kinda am pushing onto Donnie himself as well. I still have stuff to figure out about him lol.
Keyboard and holographics/projections ->
Strictly for communication. The keyboard is built into his arm. It's not a mechanical kind of keyboard. It's more of a projection with sensors tracking pressure? Or maybe just when their fingers go through certain letters of the projection. The keyboard has adjustable heights to make room for the words being written to be visible.
Can sort of broadcast/share screen the words as he's typing them to teched glasses. Got a finicky piece of tech on his collarbone. Should work through the synthetic skin but it doesn't (something he probably won't get fixed). Pick at the synthetic skin, move it aside, slide a finger over something (didn't make it specific it's literally just exposed tech ����😅) and it'll share the words as he types.
Rando stuff that probably isn't set in stone
Since he's security and just has better/and more expensive prosthetics some of the overall force comes from hydraulics. Can produce a lot more pressure, force, and speed.
The lights you can see beneath his skin are mostly cosmetic. Some have purpose but Donnie definitely doesn't know which ones.
Donnie does in fact break their mods and prosthetics all the time. Very injury prone. (This one is set in stone as of now)
Donnie can have machine parts break in a way that damages human parts of him. Like if an insulation or hydraulic fluid line somehow breaks.
He can overheat. Maybe even a bit easier than some other people. Because he's so much machine and it's harder to regulate temperature with extremities gone. Has some resistance to colder temps though. He only sweats through places with actual skin. I haven't figured out if he has an internal cooling system. But he probably should. Just a rudimentary one cause I am not giving myself or any in world builders of Donnie benefit of the doubt.
#long post#I think that's everything I got#robots & gardens#worldbuilding#of course there's plenty of other tech when it comes to production and stuff#but all of that hasn't been completely figured out#I'll bullshit my way through when I get there if needed#lol love me only doodling one pic#didn't include the luggers cause I kinda explain them in the snippet where I made them up XD
7 notes
·
View notes
Text
Also preserved in our archive (Daily updates!)
By Stephanie Soucheray, MA
During the 2023-24 cold and flu season, healthcare workers, including nursing home personnel and staff, had low uptake of COVID-19 vaccine booster doses and seasonal flu vaccines, despite a consistent recommendation from the Advisory Committee on Immunization Practices (ACIP) to stay up to date on those vaccines.
The findings, published yesterday in Morbidity and Mortality Weekly Report, showed regional differences in uptake.
The National Healthcare Safety Network (NHSN) tracks vaccination among healthcare workers in hospitals, clinics, and nursing homes. From October 2023 to March 2024, NHSN defined up-to-date COVID-19 vaccination as receipt of a 2023-2024 COVID-19 vaccine, and up-to-date seasonal flu vaccine with that season's immunization.
Among approximately 8.8 million healthcare personnel working in more than 4,000 acute care hospitals, flu vaccine coverage was 80.7%. Among approximately 2.1 million healthcare personnel working in 14,294 nursing homes, flu vaccine coverage was 45.4%.
COVID vaccine uptake lower than for flu COVID vaccine uptake was much lower. Among the employees working in acute care hospitals, only 15.3% were vaccinated. The percentage was even lower in nursing homes, at 10.5% overall.
Uptake of COVID-19 vaccines was highest in the Pacific region for both acute care hospital staff and nursing home staff. Uptake was lowest in Mountain and Southern states, the authors said.
For the flu vaccine, uptake was highest in the Mountain region (84.5%) and lowest in the Pacific region (74.3%) for acute care hospitals. Vaccination coverage was highest in the Northeast region (58.6%) and lowest in the South region (38.1%) for nursing homes.
The authors said uptake in COVID-19 vaccines decreased sharply from the previous year.
"Coverage with COVID-19 vaccination among healthcare personnel in nursing homes decreased from 22.8% during the 2022–23 respiratory virus season to 10.5% during the 2023–24 respiratory virus season," they wrote. "Like findings in previous studies, the current findings highlight the need to further investigate barriers to vaccination among health care personnel and identify additional strategies to address these challenges.
Study link: www.cdc.gov/mmwr/volumes/73/wr/mm7343a2.htm
#mask up#covid#pandemic#public health#wear a mask#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2
19 notes
·
View notes
Text
Urgent Appeal for Funding to Support Public Health Research in Gaza🔔🍉
Dear Friends and Supporters,
My name is Abed al aziz, a public health researcher currently conducting critical research on the spread of epidemics and infectious diseases in the overcrowded shelters and refugee camps in Gaza. The escalating humanitarian crisis has left thousands of people displaced, living in extremely dire conditions without basic sanitation, clean water, or adequate medical care.
In these settings, the threat of disease outbreaks is a constant nightmare. Families are crammed into small, unsanitary spaces with no means to protect themselves from the spread of infections. Children, pregnant women, and the elderly are particularly vulnerable, facing the risk of diseases like cholera, hepatitis, and respiratory infections. Every day, I witness the fear and helplessness in the eyes of mothers who struggle to keep their children safe in these inhumane conditions. The lack of healthcare resources makes it impossible to control the spread of illness, turning what should be preventable infections into life-threatening crises.
The aim of my research is to collect crucial data that can help healthcare workers and humanitarian organizations, such as Médecins Sans Frontières (Doctors Without Borders), Action Against Hunger, and the International Medical Corps, respond more effectively to these health emergencies. By understanding the patterns of disease transmission and identifying the highest-risk areas, we can develop targeted interventions to prevent future outbreaks and save countless lives.
However, to continue this urgent work, I desperately need financial support to cover the costs of field research, laboratory analysis, and creating intervention strategies. Every dollar counts. Your contribution, no matter how small, can help ensure that this research reaches completion and delivers lifesaving recommendations to protect the most vulnerable.
Please consider donating to this vital cause. Your support will directly impact thousands of individuals who are suffering without a voice. Together, we can make a real difference in the health and safety of these communities.
Donate now and be a part of this mission to protect lives in Gaza.
GoFundMe Link
With heartfelt gratitude,
Abed al aziz
Public Health Researcher
13 notes
·
View notes
Text
From @MaskTogetherAmerica (bolding mine): "IN-N-OUT’s customer service line confirmed that masks are banned for workers in AZ, CO, TX, NV & UT, unless they have a doctor’s note. Meanwhile, if you work for @innout in CA or OR, it’s up to you but you must wear only company-provided N95s if you choose to #MaskUp! (Different masks may be allowed with a valid medical note.) “N95 masks provide the highest level of protection for C0VID-19 and other viruses and are recommended by OSHA for other respiratory protection.” – the policy stated. @Forbes contributor Dr. Judy Stone shared valuable details in her story: In-N-Out Burger’s New Masking Policy Threatens Their Employees’ Health. Puzzling, isn’t it? 🧐 See CA & OR Mask Policy: https://bit.ly/3Q2LfNJ Call 1-800-786-1000 to let IN-N-OUT know how you feel about their 😷policy. Key points from Dr. Stone’s article: https://bit.ly/3XUR5CB 👉60% of people in the U.S. have underlying conditions that put them at increased risk for severe C19. 👉Forcing employees to disclose reasons for mask exemption likely violates medical privacy. 👉It’s unfair to ask employees to get a doctor’s note which would require seeing a doctor. 👉Requiring proof of a disability might be considered a violation of the ADA. 👉“Fast food workers don’t owe anyone their smiles.” —@jessica.wildfire.writer wrote in her commentary. Fast food workers certainly don’t owe anyone their lives, considering the risk of getting #LongCovid. 👉The CA OSHA regulations state, “No employer shall prevent any employees from wearing a face covering, including a respirator, unless it would create a safety hazard.” 👉The CDC states, “People may choose to mask at any time. Layered prevention strategies — like staying up to date on vaccines and wearing masks — can help prevent severe illness and reduce the potential for strain on the healthcare system. Wear a mask with the best fit, protection, and comfort for you.” 👉HHS tweeted, “The more often you get C19, the higher your risk of complications.” 👉Masking protects you from respiratory viruses as well as pollutants & pollen." PLEASE CALL THE CUSTOMER HOTLINE (1-800-786-1000) AND MAKE YOUR VOICE HEARD THAT YOU DO NOT SUPPORT THIS POLICY AND WILL NOT PATRONIZE IN-N-OUT BURGER AS LONG AS THEY DO THIS. You don't need to be rude and keep in mind the customer service rep isn't the one responsible for putting this policy in place. ANTI-MASKERS, VIRUS-DENIERS, AND OTHER PLAGUE-RATS DO NOT INTERACT WITH THIS POST.
#masks#face masks#workers' rights#employee safety#in-N-out burger#wildfire smoke#covid-19#coronavirus#workplace safety#employee rights#mlop#medical privacy#workers' rights violations
30 notes
·
View notes
Link
2 notes
·
View notes
Text
Smart Eldercare Solutions

The landscape of senior care at home is experiencing a remarkable transformation in 2025, driven by groundbreaking artificial intelligence technology that's making it possible for millions of older adults to age in place safely and independently. With over 90% of seniors expressing a desire to remain in their own homes as they age, AI-powered eldercare solutions are bridging the gap between independence and safety like never before.
The Growing Demand for AI-Enhanced Senior Care at Home
As America's population ages rapidly, with projections showing that one in five Americans will be 65 or older by 2030, families are desperately seeking innovative solutions for senior care at home. Traditional eldercare models are struggling to meet demand, with significant shortages in healthcare workers and rising costs that can reach $11,000 monthly by 2050.
The AI in aging and elderly care market is responding to this crisis with explosive growth, expected to expand at a 21.2% compound annual growth rate through 2034, reaching $322.4 billion. This surge reflects the urgent need for technology-driven solutions that can supplement human care while keeping seniors safe and comfortable in their own homes.
Revolutionary AI Technologies Transforming Home-Based Senior Care
Smart Health Monitoring Systems
Modern AI-powered health monitoring represents a quantum leap from traditional eldercare approaches. These sophisticated systems use wearable devices and home sensors to continuously track vital signs, activity levels, and behavioral patterns. When anomalies are detected, the technology can predict potential health issues days or even weeks before they become serious problems.
Voice biomarker technology is particularly promising, with AI systems now capable of detecting early signs of depression, cognitive decline, or respiratory issues simply by analyzing changes in speech patterns during routine conversations. This non-intrusive monitoring allows seniors to maintain their privacy while ensuring their wellbeing is constantly safeguarded.
AI-Powered Personal Care Assistants
Today's AI care assistants go far beyond simple reminders. These intelligent systems learn individual preferences and routines, providing personalized medication management, scheduling healthcare appointments, and even offering emotional support through natural conversations. Unlike rigid automated systems, modern AI assistants adapt to each senior's unique needs and communication style.
These digital companions can detect falls through advanced sensor networks, automatically contacting family members or emergency services when needed. They also provide cognitive stimulation through games, memory exercises, and social interaction, helping combat the loneliness that affects many seniors aging in place.
Smart Home Integration for Aging in Place
AI-enabled smart home technology is making independent living safer and more manageable for seniors. Automated lighting systems adjust to prevent falls, smart thermostats maintain optimal comfort levels, and voice-activated controls eliminate the need for complex interfaces that can frustrate older adults.
Advanced home safety systems use computer vision to monitor for unusual activities or emergencies, while smart medication dispensers ensure proper dosing and timing. These integrated solutions work seamlessly together, creating an invisible safety net that allows seniors to maintain their independence with confidence.
Real-World Benefits of AI Senior Care Technology
Predictive Health Management
AI's ability to analyze vast amounts of health data is revolutionizing preventive care for seniors. By identifying patterns in vital signs, sleep quality, mobility, and daily activities, these systems can predict health crises before they occur. This proactive approach has shown potential to reduce hospital readmissions by up to 30% while improving overall quality of life.
Families report significant peace of mind knowing that AI monitoring provides 24/7 oversight without being intrusive. The technology can distinguish between normal variations and concerning changes, reducing false alarms while ensuring genuine emergencies receive immediate attention.
Cost-Effective Care Solutions
AI-enhanced senior care at home offers substantial cost savings compared to traditional institutional care. With average assisted living costs exceeding $4,500 monthly, AI-supported aging in place can reduce expenses by 50-70% while providing comparable or superior safety and health monitoring.
These savings come from reduced need for round-the-clock human supervision, fewer emergency interventions due to predictive monitoring, and decreased healthcare costs through early intervention and prevention.
Addressing Privacy and Implementation Concerns
While AI technology offers tremendous benefits for senior care at home, successful implementation requires careful attention to privacy and user acceptance. Modern systems prioritize data security with encrypted communications and secure local storage options that protect sensitive health information.
Equally important is ensuring that AI enhances rather than replaces human connection. The most successful implementations combine technology with regular family interaction and professional healthcare support, creating a comprehensive care network that addresses both physical and emotional needs.
The Future of AI-Powered Senior Care at Home
Looking ahead, AI technology will continue evolving to provide even more sophisticated support for aging in place. Emerging developments include advanced robotics for physical assistance, improved natural language processing for more intuitive interactions, and integration with telehealth services for comprehensive remote medical care.
As these technologies mature and become more affordable, AI-enhanced senior care at home will transform from a luxury option to a standard approach for families seeking the best possible care for their aging loved ones.
The revolution in AI-powered senior care technology is not just about keeping older adults safe – it's about empowering them to live fulfilling, independent lives in the comfort of their own homes while giving families confidence that their loved ones are receiving the best possible care.
For families considering AI-enhanced senior care solutions, consult with eldercare professionals to determine which technologies best meet your loved one's specific needs and preferences.
0 notes
Text
Why Non-Woven Face Masks Are Essential During Flu Season

With flu season on the horizon, it’s crucial to prioritize effective prevention strategies. One of the simplest and most effective tools in reducing the spread of flu viruses is the humble non woven face mask. These lightweight yet powerful masks play a vital role in personal and public health protection—especially during times when influenza viruses are highly contagious and easily spread in public spaces, workplaces, and homes.
What Makes Non-Woven Face Masks Special?
Unlike cloth masks or traditional woven alternatives, non woven face masks are made using melt-blown or spun-bonded polypropylene fabric. This material is produced through a process that bonds fibers together without weaving or knitting, resulting in a product that is more efficient in filtration and moisture resistance.
Here are some standout features of non woven face masks that make them ideal during flu season:
High Filtration Efficiency: The non-woven fabric acts as a barrier, filtering out airborne particles, including flu-causing viruses and bacteria.
Breathability: These masks allow for easy breathing while still maintaining protection, making them more comfortable for extended use.
Fluid Resistance: Non woven masks repel moisture, including droplets from coughs and sneezes—one of the primary transmission modes of flu viruses.
Hypoallergenic: The materials used are typically soft, skin-friendly, and less likely to cause irritation or allergic reactions.
Protection Beyond the Surface
During flu season, the flu virus is mainly spread through respiratory droplets when an infected person talks, coughs, or sneezes. When worn correctly, non woven face masks can significantly reduce the risk of inhaling these harmful particles. Additionally, wearing a mask helps prevent frequent face-touching, reducing the risk of transferring viruses from contaminated surfaces to your mouth or nose.
For those who are already ill, wearing a face mask is a responsible step to prevent spreading the infection to others. This is especially important in densely populated environments like schools, offices, hospitals, and public transportation.
Advantages for Daily Use
In addition to their medical-grade effectiveness, non woven masks are also affordable and disposable. They offer convenience and hygiene for daily use:
Easy to wear and remove without contamination
Disposable after a single-use, reducing infection risk
Lightweight and portable—can be carried in bags or pockets
Whether you're a healthcare professional, office worker, student, or senior citizen, having a stock of non woven face masks on hand is a smart choice during flu season.
Environmental Considerations
Today, many non woven face mask manufacturers are adopting eco-friendly production practices. Biodegradable options are now available that ensure safety without adding to environmental waste. Choosing masks from responsible producers adds another layer of ethical value to your health decisions.
Non-Woven Face Mask Manufacturer & Exporter in India - Denex International
When it comes to quality, safety, and reliability, Denex International stands out as a trusted non woven face mask manufacturer in India. With a state-of-the-art production facility and a commitment to international standards, Denex has earned its reputation as a leading non woven face mask exporter.
Whether you are a hospital, corporate buyer, retailer, or distributor, Denex International offers a wide range of non woven face masks customized to your needs. Their masks are manufactured with precision, tested for safety, and packed for hygiene—making them an essential partner in the fight against flu and airborne diseases.
Stay protected, stay safe—choose Denex International for superior non woven face mask solutions.
Contact Details
Phone- 0124 4115465
Email - [email protected]
#Non-Woven Face Masks#face masks#non woven face mask manufacturer#non woven face mask exporter#non woven face mask manufacturer in India
0 notes
Text
"...The planned HICPAC revisions would water down infection control protections, particularly for aerosol transmission and multidrug-resistant organisms.
Most immediately worrisome is its conclusion that plain surgical masks (aka “baggy blues”) are equivalent to N95s and provide adequate protection to healthcare workers and patients. There is abundant evidence to the contrary. This from the CDC:
[Graphic showing that N95s lower odds of getting covid]
It is clear that N95s offer far better protection against aerosols, such as from Covid-19 and other inhaled pathogens.
More than 900 experts in infectious disease, public health, industrial hygiene, aerosol science and ventilation engineering signed a letter to Mandy Cohen, M.D., the new CDC director, explaining how the new draft guidelines weaken protections for healthcare workers. They state, “Surgical masks cannot be recommended to protect health care personnel against inhalation of infectious aerosols.”
The experts’ letter was coauthored by Lisa Brosseau, Jane Thomason and Peg Seminario, among others. Seminario was the director of occupational safety and health for the AFL-CIO from 1990 to 2019.
The CDC responded to Seminario and the experts’ letter only now, a month later, and just before the scheduled Aug 22 meeting. The agency offered no substantive or specific rebuttal, but spoke of its dedication to “improving healthcare quality” and commitment to “to transparency, communication, and stakeholder engagement.” It also claimed that the CDC is meeting the guidelines for transparency required by the Federal Advisory Committees Act. The letter is not yet publicly available.
HICPAC’s proposals also fail to include ventilation, UV disinfection and HEPA filtration, all essential tools against an airborne pathogen.
There are many concerns regarding HICPAC’s process, as well.
Meetings did not include experts in aerosol transmission, ventilation, occupational health and worker protections, Occupational Safety and Health Administration (part of the Department of Labor), National Institute of Occupational Safety and Health (part of CDC which researches worker health and safety) or representatives of healthcare workers.
Lisa Brosseau, an expert on respiratory protection from infections at the Center for Infectious Disease Research and Policy and a retired professor, expressed outrage at HICPAC’s process: “Why are they not consulting with all the people and all the stakeholders? They are not, and that's a sort of basic expectation of a federal advisory committee.”
Brosseau was equally critical of the committee’s literature review, saying that it was “cherrypicked” and “the most ridiculous literature review I've ever seen.” She concluded, “I think they were hoping nobody would notice” how the review was manipulated.
While HICPAC suddenly (Aug 15–a week before its scheduled meeting) invited public participation, it has not provided meeting notes, minutes, transcripts or a draft policy beyond its bullet point slides.
Thomason said HICPAC is “weakening existing guidance for infection control and not following the science that has been built over the last several decades about aerosol transmission.” She added that, in their goal of providing more flexibility, “They said to employers, ‘Here are the minimal standards, and you guys figure out what you need and want to do.’” They are proposing minimal crisis standards of care.
Brosseau added, “Being in health and safety, I know where that goes. It means you get nothing, workers get nothing, no protections. You don’t leave it to the employer to make decisions about workplace hazards.”"
More in the article:
8 notes
·
View notes
Text
Workplace Safety Begins with Monitoring Health 🫁❤️
At Emerald Hills Medical Centre, we care about your workforce's health and safe working conditions. We provide professional ECG and Spirometry Testing to industries where your workers may encounter harmful airborne contaminants, dust, chemicals, and infectious agents.
Whether you’re in the business of construction, manufacturing, or chemicals, it’s important you do Spirometry testing on a regular basis to detect early signs of respiratory disease. Our team also provides ECG Testing for heart health - assisting you to ensure your team is fit for duty.
When you invest in regular health assessments, you’re not just fulfilling your legislative obligations - you’re protecting your most important resource, your people. 🛡️💼
We can assist you to arrange onsite testing based on your workplace requirements.
📞 Call us today on 02 4604 6071 to arrange testing or to find out more.

#EmeraldHillsMedical#WorkplaceHealth#SpirometryTesting#ECGTesting#OccupationalHealth#EmployeeWellbeing#ConstructionHealth#RespiratoryHealth#HealthAndSafetyFirst
0 notes
Text
Cattle and Sheep Vaccine Market Driven by Livestock Health Needs and Rising Protein Consumption Globally
The global cattle and sheep vaccine market is experiencing significant growth, driven by increasing awareness of livestock health, rising demand for animal-based products, and the economic importance of livestock in agricultural economies. As diseases such as foot-and-mouth disease, brucellosis, and clostridial infections threaten livestock populations, vaccination remains a vital tool in disease prevention and control.

Vaccines for cattle and sheep are biological preparations that provide active acquired immunity against specific pathogens. These vaccines can be live attenuated, inactivated (killed), toxoid, or subunit-based. They are administered to prevent outbreaks that can cause substantial economic losses due to decreased productivity, high mortality rates, and trade restrictions. The effectiveness of these vaccines directly impacts meat, milk, and wool production across several countries.
In recent years, the livestock sector has undergone modernization, resulting in improved animal husbandry practices, better disease diagnostics, and a growing dependence on preventive healthcare measures, especially vaccines. This transformation is particularly visible in emerging economies in Asia-Pacific, Latin America, and parts of Africa, where livestock serves as a critical source of livelihood. Consequently, these regions present strong growth opportunities for vaccine manufacturers.
North America and Europe dominate the market in terms of revenue, owing to their well-established veterinary infrastructure, strong R&D capabilities, and proactive government policies. The United States, in particular, has a well-regulated animal vaccine industry with several key players investing in innovative technologies, such as mRNA-based and recombinant vaccines, which are increasingly being explored in veterinary applications.
Among the major diseases affecting cattle and sheep, clostridial infections such as blackleg, tetanus, and enterotoxemia are widespread. Multivalent vaccines that protect against multiple strains are commonly used, offering broader protection in a single dose. Similarly, respiratory diseases, parasitic infections, and reproductive disorders like leptospirosis and brucellosis are key focus areas for vaccine development.
One of the most significant challenges in the cattle and sheep vaccine market is ensuring cold chain logistics and proper vaccine delivery, particularly in rural and remote areas. Improper handling can compromise vaccine potency, reducing effectiveness and leading to disease outbreaks. To address this, governments and private sectors are investing in cold chain infrastructure and training for veterinary workers.
The market is also shaped by regulatory frameworks. Different countries have stringent laws regarding vaccine approval, manufacturing, and distribution. The World Organisation for Animal Health (WOAH) plays a role in standardizing vaccine quality and promoting international cooperation to control transboundary diseases. Compliance with Good Manufacturing Practices (GMP) and regular surveillance further ensures product quality.
Technological advancements are accelerating market evolution. New delivery methods, such as intranasal vaccines and needle-free injectors, are improving ease of administration and safety. Furthermore, data analytics and AI are being utilized to predict outbreaks and optimize vaccination schedules based on regional risk factors, livestock density, and weather patterns.
Another emerging trend is the increased focus on combination vaccines, which reduce the number of injections needed and minimize handling stress for animals. This not only enhances animal welfare but also improves labor efficiency on farms. Companies are investing in R&D to develop broader-spectrum vaccines and address strain variation, which is particularly important for rapidly mutating pathogens.
Major players in the cattle and sheep vaccine market include Zoetis, Merck Animal Health, Boehringer Ingelheim, Elanco, and Ceva Santé Animale. These companies continue to expand their portfolios through strategic mergers, acquisitions, and collaborations with local veterinary networks. Partnerships with government agencies and NGOs are also helping in the rollout of vaccination programs in low-income regions.
Looking ahead, sustainability and food security will remain key drivers of the market. With the global population projected to exceed 9 billion by 2050, ensuring the health of livestock is crucial for stable food production. Vaccination programs that reduce the need for antibiotics also align with growing global concerns around antimicrobial resistance (AMR), making vaccines an essential component of responsible livestock management.
In conclusion, the cattle and sheep vaccine market is poised for continued growth, supported by technological innovation, increasing livestock populations, and greater emphasis on preventive veterinary care. While challenges such as distribution and regulation remain, proactive policy-making and industry collaboration are paving the way for a resilient and efficient animal healthcare ecosystem.
#LivestockHealth#AnimalVaccines#VeterinaryMedicine#CattleFarming#SheepFarming#AnimalHealth#VeterinaryScience
0 notes
Text
Also preserved in our archive
— HICPAC supports surgical masks for airborne pathogens, sick workers returning after 3 days
With Democratic administrations like these, who needs Republicans?
by Sophie Putka
Members of the Healthcare Infection Control Practices Advisory Committee (HICPAC) voted Friday to defend what some have called weak standards of infection control for healthcare settings, agreeing nearly unanimously that surgical masks provideopens in a new tab or window adequate protection against airborne pathogens, and that sick healthcare workers may return to work after 3 days of viral respiratory symptoms without testing.
The meeting centered largely on written responses to CDC questions pushing backopens in a new tab or window on draft guidelinesopens in a new tab or window to prevent transmission of pathogens in healthcare settings, and on proposed updates to a section of a separate guidelineopens in a new tab or window for infection control in healthcare personnel from 1998.
HICPAC, which advises the CDC and HHS on infection control practices, has faced an outcryopens in a new tab or window from some healthcare workers and occupational health experts since the beginningopens in a new tab or window of its guideline revision process in 2023. Critics have condemned the proposedopens in a new tab or window infection precautions as woefully inadequate for protecting healthcare workers and patients, and called for more transparent processes, along with input from those representing their concerns.
HICPAC has since made adjustments, such as adding members to its voting contingent and workgroup. This includes two leaders from a group that has been among its loudest critics, National Nurses United (NNU): Lisa Baum, MA, the lead occupational health & safety representative at the New York State Nurses Association, an NNU affiliate, and Jane Thomason, MSPH, lead industrial hygienist for NNU. Baum is one of 11 HICPAC voting members and Thomason serves on the HICPAC workgroup.
Despite the concessions, HICPAC voted to approve language that kept the recommendationsopens in a new tab or window largely the same. Though HICPAC's guidelines are not mandatory, most healthcare employers use them to guide their infection control practices.
Michelle Gutierrez Vo, RN, president of the California Nurses Association/National Nurses Organizing Committee, an affiliate of NNU, told MedPage Today, "We're not surprised, you know, it's not something that we thought was going to be easy. But it doesn't deter us." "They need to be preventing illness, and they need to be sitting at the highest level to make sure that people don't get sick," Vo added. "And if they don't do that, then they're failing."
Vo and others noted that HICPAC's members are largely administrators and managersopens in a new tab or window from institutions including academic research centers and health departments, but also hospitals and health systems with a vested interest in keeping costs down. Throughout the deliberations, Baum stood in stark contrast to the rest of the HICPAC members, arguing for stronger language, and was nearly the sole "disapprove" vote in all six of the items voted on.
Defending the Draft CDC asked four key questionsopens in a new tab or window about the isolation precautions guidance when it sent the draft back to HICPAC earlier this year. For the first question, members approved language stating that "N95 respirators should not be recommended for all pathogens that spread by air."
As for the draft's "routine air precautions," it recommended the use of "masks" -- including surgical masks -- for "common, often endemic, respiratory pathogens that spread predominantly over short distances."
To a question about voluntary use of N95 respirators by healthcare staff, the workgroup voted to respond, in part, that the guideline should not include this as a direct recommendation. Language that "clearly supports the concept of voluntary use of N95" masks should be left in the "narrative" portion of the relevant section, the group decided.
Finally, the workgroup responded that a blanket recommendation for source control -- the use of masks to prevent transmission of pathogens from the mask-wearer -- was not needed.
As for the healthcare personnel guidance, HICPAC recommended workers stay home for 3 days after the onset of a confirmed or suspected respiratory virus, returning if they are fever-free for 24 hours, have improving symptoms, and "feel well enough to return to work." After the return to work, they should wear a mask until day 7 from onset.
This decision came after reviewing data compiled from a number of studies, from which the workgroup estimated that most viral transmission occurs within the first 5 to 7 days of the primary case.
Public Pushback Noticeably frustrated public commenters called for universal masking in healthcare settings, better evidence reviews, and stronger protections for healthcare workers and immunocompromised people. "Who's going to send the memo to all the firefighters that they should start using surgical masks for wildfire smoke? [Or] to the lab workers that work with other infectious diseases like tuberculosis, bird flu, or whatever else pops up that can spread by the air?" asked Shea O'Neil, a volunteer at the World Health Network and Air Support Project. "Just let them know to put down those coppers and N95s and throw on a baggy blue surgical mask, because it probably works just as fine."
"It's a risk you all are willing to take today, and somehow you've been put in this position to decide for us. That's not the precautionary principle," O'Neil said, calling for N95 respirators or better as a standard precaution.
"If folks are symptomatic, then they should be home [until] they're not symptomatic -- 3 or 5 days does not handle the issue," said commenter Don Ford, a COVID-19 safety and long COVID advocate. "I hear the committee discussing what is best for hospital management when your role is to determine what is best healthcare practices. The group is not called 'hospital management practices.' It's Health Infection Control Practices Advisory Committee."
#HICPAC#covid#covid news#mask up#public health#wear a mask#pandemic#wear a respirator#covid 19#still coviding#coronavirus#sars cov 2#long covid#covid conscious#covid is airborne#covid pandemic#covid isn't over#covid19#covidー19
8 notes
·
View notes
Text
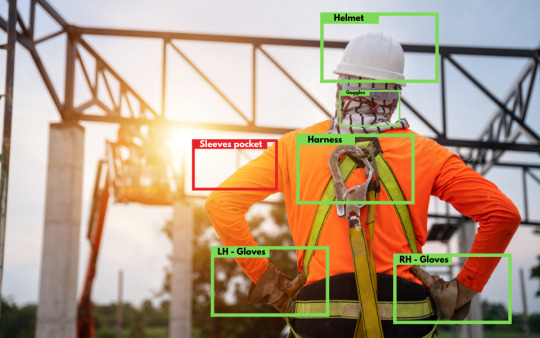
Ensuring Workplace Safety in Australia: How AI-Powered PPE Compliance is Revolutionizing Industries
Workplace safety has always been a top priority across Australia's diverse industrial sectors. From mining in Western Australia to construction projects along the east coast and large-scale manufacturing in Victoria and South Australia, ensuring employees are equipped with the right Personal Protective Equipment (PPE) is vital. Yet, manual monitoring of PPE compliance is not only resource-intensive but also prone to human error. Enter AI-powered PPE compliance solutions — a transformative approach that is reshaping how safety is enforced across Australian workplaces.
The PPE Challenge in Australia
Australia’s strict Work Health and Safety (WHS) regulations require employers to take all reasonable steps to ensure that workers are wearing PPE appropriate for their tasks. Whether it’s hard hats on a Brisbane construction site, high-visibility clothing in a Melbourne logistics hub, or respiratory protection in a Perth mining tunnel, compliance is non-negotiable. However, traditional monitoring systems — such as manual inspections or CCTV surveillance — are limited in scalability and often reactive rather than proactive.
AI-Powered PPE Compliance: An Overview
AI-powered PPE compliance systems leverage computer vision and machine learning algorithms to detect, track, and report PPE usage in real-time. These systems are typically integrated with existing CCTV or smart camera infrastructure and trained to identify whether workers are wearing required safety gear — including helmets, gloves, goggles, masks, vests, and boots — based on industry-specific requirements.
Key Statistics:
AI-driven PPE detection systems have demonstrated a sensitivity of 98.9% during doffing and 85.3% during donning, compared to traditional buddy systems, indicating high accuracy in real-world applications according to Macquarie University
Implementing AI-based PPE monitoring can lead to a significant reduction in workplace incidents. For instance, predictive models have the potential to prevent up to 4,500 injuries and 50 deaths annually in scaffold-related incidents. Reference - Occupational Health & Safety
According to HPV Health, Australia In healthcare settings, AI systems have been employed to train, audit, and improve PPE compliance, reducing reliance on limited healthcare worker resources and enhancing overall safety.
Here's a breakdown of how the system typically works:
Camera Feed Ingestion: Live video feeds are ingested by AI systems.
Object Detection and Recognition: The AI model identifies humans and checks for the presence of PPE items.
Real-Time Alerts: Non-compliance is flagged instantly, and alerts are sent to supervisors.
Data Logging and Reporting: Historical data is stored to identify trends and improve compliance over time. This automation of safety enforcement offers unmatched efficiency and consistency.
Cutting-Edge Applications Across Australian Industries

Mining Sector: Western Australia
Western Australia’s mining industry is globally recognized but also inherently dangerous. Mining operations often require PPE that includes high-grade respirators, head protection, and flame-resistant clothing. AI-powered PPE compliance systems have been deployed in several mines to automatically check if personnel entering restricted zones are adequately protected.
One notable application includes using thermal and visual cameras at entry checkpoints to verify PPE adherence before allowing access. Integrated with access control systems, the AI solution prevents gate entry unless PPE is validated — significantly reducing incidents.
Construction Industry: New South Wales and Victoria
Construction remains one of Australia’s most hazardous sectors, and PPE non-compliance can lead to serious injuries or fatalities. Several large infrastructure projects, including metro tunnel works in Melbourne and Sydney, are adopting AI-powered PPE compliance systems.
By mounting smart cameras on site cranes and mobile monitoring vehicles, contractors can receive real-time feedback on site-wide PPE usage. In some pilot programs, drones equipped with AI cameras are used to scan large sites and alert ground supervisors when non-compliance is detected in hard-to-reach areas.
Manufacturing: South Australia and Queensland
In Australia’s manufacturing hubs, high-speed machinery and chemicals make safety gear like goggles, ear protection, and gloves mandatory. AI solutions are now being used to monitor workstations and assembly lines. When the AI detects a worker missing gloves or ear muffs, it sends immediate alerts to floor managers, reducing the reliance on safety officers alone.
Some facilities are integrating these systems with wearable sensors that track biometrics along with visual PPE compliance — merging safety enforcement with health monitoring for a holistic approach.
Logistics and Warehousing: National Scope
E-commerce and retail warehousing have grown significantly in Australia, especially post-pandemic. Fulfilment centres, where heavy lifting and machinery use are common, now use AI-driven PPE verification at entry points and throughout the floor. When high-visibility vests or steel-toe boots are not detected, personnel are prompted through digital signage or wearable alerts to correct the oversight.
Technical Aspects Behind the Innovation
AI-powered PPE compliance systems are built on a stack of core technologies:
Computer Vision: Leveraging deep learning models like CNNs (Convolutional Neural Networks), the system identifies objects (helmets, vests, etc.) and human figures.
Edge Computing: Real-time processing at the edge (camera level) minimizes latency and avoids sending large video data to central servers.
Cloud Integration: For storage, advanced analytics, and reporting dashboards, cloud platforms like AWS and Azure are commonly used.
Custom Training Datasets: AI models are trained using datasets collected from specific sites to recognize unique PPE types and layouts relevant to Australian standards.
These systems are often built using frameworks such as TensorFlow or PyTorch and require continuous retraining to improve accuracy and adapt to changes in PPE designs or lighting conditions.
Addressing Privacy and Ethical Concerns
One of the primary concerns with any surveillance-based technology is privacy. In Australia, businesses must comply with the Australian Privacy Principles (APPs) under the Privacy Act 1988. When deploying AI PPE systems, organizations are required to:
Provide transparency on what data is collected and how it’s used
Securely store data and prevent unauthorized access
Ensure the AI systems do not use facial recognition without explicit consent
By designing solutions that anonymize individuals and only assess PPE presence, many companies have managed to strike a balance between safety and privacy.
The Broader Impact on Workplace Culture
AI-powered PPE compliance is not just a tool for surveillance — it’s an enabler of a proactive safety culture. With real-time feedback and analytics, organizations can:
Identify departments or shifts with high non-compliance rates
Offer targeted training and awareness sessions
Recognize teams with the best safety records
This data-driven approach encourages a more engaged and safety-conscious workforce.

AI Trends in PPE Compliance: What’s Next for Australia?
Predictive Compliance: Instead of merely detecting PPE violations, future systems will predict potential non-compliance based on historical patterns and worker behavior.
Integration with Robotics: Autonomous robots and drones will become more common on large industrial sites to monitor safety continuously.
Augmented Reality PPE Checks: Wearables like AR glasses can offer real-time safety instructions or alerts to workers who are improperly equipped.
AI + IoT Fusion: Combining AI vision with IoT sensors will create a robust safety net — for instance, ensuring not only that a helmet is worn but also if it meets current impact safety standards.
Compliance-as-a-Service Platforms: Australian tech startups are emerging in this space, offering plug-and-play PPE compliance tools as subscription models for small and mid-sized enterprises.
How We Can Help Australian Companies with AI-Powered PPE Compliance

At iProgrammer Solutions - Australia, we specialize in developing AI-powered workplace safety solutions tailored to Australian industry standards and compliance frameworks. With deep technical expertise in computer vision, machine learning, and edge computing, we build robust PPE compliance systems that seamlessly integrate with your existing infrastructure.
Whether you're managing a mining site in WA, a construction project in Sydney, or a manufacturing facility in Adelaide, our AI solutions can help you:
Achieve real-time PPE monitoring and reporting
Improve safety compliance and reduce manual inspection costs
Meet WHS regulations with confidence
Customize AI models to recognize site-specific PPE requirements
Let’s work together to create a safer, smarter workplace for your teams across Australia. Reach out to our experts today to explore how we can support your PPE compliance journey with intelligent automation.
0 notes
Text
"Face Shields: The Essential Protective Gear for Health and Safety"
Face shields have become an essential part of personal protective equipment (PPE), providing an additional layer of protection against airborne particles, droplets, and other potential contaminants. Unlike masks, face shields cover the entire face, offering visibility and comfort while serving as a barrier to protect both the wearer and those around them. This makes them particularly effective in environments where close contact is unavoidable, such as healthcare settings, public transportation, and crowded places.
The effectiveness of face shields in blocking respiratory droplets, which are the primary carriers of viruses like COVID-19, has made them a key tool in the fight against the spread of infectious diseases. While they are not a substitute for face masks, face shields can be used in combination with masks for enhanced protection. Their design allows for easy cleaning and reuse, making them a sustainable option for both individuals and businesses aiming to ensure the safety of employees and customers.
In addition to their protective features, face shields offer several practical benefits. They are comfortable to wear for extended periods, provide clear visibility, and do not cause the same breathing difficulties that can occur with face masks. This makes them ideal for professionals who need to communicate clearly, such as teachers, healthcare workers, and service industry employees. Furthermore, face shields are often preferred by individuals with medical conditions or those who struggle with wearing masks for long durations.
As the global health landscape continues to evolve, face shields are becoming a critical component of personal protection. Innovations in materials and designs are improving their durability, comfort, and efficiency. With the growing focus on health and safety across industries, face shields will continue to play an important role in preventing the transmission of diseases and protecting individuals in high-risk environments.
#FaceShields#PPEProtection#HealthAndSafety#COVID19Prevention#PersonalProtectionGear#ClearProtection#StaySafe
0 notes
Text
Safety Equipment Suppliers in Dubai, UAE - Clothing Dealers
List of best safety equipment clothing suppliers in Dubai, UAE browse top safety material suppliers in Dubai with phone numbers, locations, maps, email, website and more on dcciinfo
Safety Equipment Suppliers in Dubai, UAE – Clothing Dealers You Can Trust
Dubai, a city known for its rapid development and booming industrial sector, places a strong emphasis on safety standards across various industries. Whether it's construction, oil and gas, manufacturing, or warehousing, every business must comply with the region's strict safety regulations. That’s where safety equipment suppliers in Dubai, UAE step in – providing the necessary protective clothing and gear to keep workers safe and ensure legal compliance.
In this comprehensive guide, we’ll explore the role of safety clothing dealers, what products they offer, and how to choose the right supplier for your business needs in the UAE.
Why Safety Equipment Is Crucial in Dubai
Dubai's industrial growth has led to increased construction sites, manufacturing plants, and logistics operations – all of which present various occupational hazards. The UAE Ministry of Human Resources and Emiratisation (MOHRE) and Dubai Municipality enforce stringent safety guidelines to protect workers.
Failure to comply can lead to hefty fines, business shutdowns, or worse – serious injuries and fatalities. That’s why investing in high-quality personal protective equipment (PPE) and safety clothing isn’t just a recommendation, it’s a legal requirement.
What Products Do Safety Equipment Suppliers in Dubai Offer?
Top safety clothing dealers in Dubai provide a wide range of products designed to safeguard workers in different industries. Here are the most commonly offered items:
1. Protective Clothing
High-Visibility Jackets & Vests: Ideal for construction and roadwork environments.
Flame-Resistant Coveralls: Designed for workers in oil and gas or welding industries.
Disposable Coveralls: Used in chemical labs, cleanrooms, or medical sectors.
Waterproof & Weather-Proof Gear: For outdoor workers exposed to harsh climates.
2. Head Protection
Hard Hats & Helmets: Certified to protect from falling objects and impact.
Bump Caps: Lightweight protection for lower-risk environments.
Welding Helmets: Equipped with shading and face protection for welders.
3. Eye and Face Protection
Safety Goggles: For dust, debris, and chemical splash protection.
Face Shields: Common in grinding, metal cutting, and laboratory settings.
4. Hearing Protection
Ear Muffs: For high-noise industrial settings.
Ear Plugs: Cost-effective hearing protection used in factories and construction.
5. Hand and Arm Protection
Safety Gloves: Including cut-resistant, chemical-resistant, and insulated gloves.
Sleeve Guards: For workers handling sharp or hot materials.
6. Foot Protection
Steel-Toe Safety Boots: Mandatory in construction and industrial plants.
Anti-Slip Shoes: Used in kitchens, hospitals, and warehouses.
Electrically Insulated Footwear: For electricians and power plant workers.
7. Respiratory Protection
Dust Masks & Respirators: For environments with airborne particles or hazardous gases.
Full-Face Respirators: For chemical handling and high-risk zones.
Top Industries Served by Safety Clothing Dealers in UAE
Safety equipment suppliers in Dubai serve a variety of industries, each with its own unique requirements:
Construction & Infrastructure: Helmets, reflective vests, steel-toe boots.
Oil & Gas: Flame-resistant clothing, chemical-resistant gloves, respirators.
Healthcare & Pharmaceuticals: Disposable gowns, masks, gloves, shoe covers.
Food & Beverage: Hygiene-focused uniforms, non-slip footwear, hairnets.
Manufacturing & Logistics: Coveralls, safety glasses, ear protection.
Hospitality & Housekeeping: Lightweight gloves, uniforms, eye protection.
Key Features to Look for in a Safety Equipment Supplier in Dubai
When choosing a safety clothing dealer in UAE, consider the following factors to ensure quality and compliance:
1. Product Certifications
Ensure the PPE meets international safety standards such as ISO, CE, ANSI, or EN. Certified equipment assures compliance and worker protection.
2. Variety and Availability
The best suppliers offer a wide product range and ready stock for fast delivery. Bulk availability is essential for large-scale operations.
3. Customization Options
Some suppliers offer branded uniforms and customized sizing or specifications based on industry needs.
4. Expert Consultation
Choose suppliers who offer safety audits, training, and expert advice on suitable PPE for your specific business.
5. After-Sales Support
Post-purchase support, warranty options, and return policies indicate the supplier’s commitment to customer satisfaction.
Top Safety Equipment Suppliers in Dubai, UAE
Here are some well-known safety clothing and PPE dealers in Dubai:
1. Al Asayel Health & Safety
One of the oldest PPE suppliers in the UAE, offering everything from fire-resistant gear to safety boots and helmets. They cater to industries such as oil & gas, healthcare, and hospitality.
2. PPE Online (PPE Online UAE)
A modern, e-commerce-focused PPE supplier providing fast delivery across the UAE. Known for carrying top global brands.
3. Protec Safety LLC
A Dubai-based supplier offering industrial safety solutions including head-to-toe protection. They also provide safety signage and traffic control products.
4. Spark International
Specializes in industrial clothing and provides custom branding and embroidery options for safety gear.
5. Safety House General Trading
Offers budget-friendly PPE solutions for small businesses and startups without compromising on quality.
Tip: You can also use online directories like DCCIInfo to search and filter safety clothing dealers in Dubai based on category, rating, and location.
Benefits of Choosing Local Safety Equipment Suppliers in Dubai
✅ Fast Delivery
Local dealers can provide same-day or next-day delivery, critical for urgent PPE requirements.
✅ Compliance Knowledge
Suppliers in Dubai are well-versed with local safety regulations, ensuring the equipment meets all regional guidelines.
✅ On-Site Support
Some suppliers offer site visits for assessing risks and recommending the right gear.
✅ Local Warranty and Replacement
Easier product replacement and warranty claims compared to overseas orders.
Future Trends in Safety Equipment & Clothing
As technology evolves, so does workplace safety gear. Here are some trends to watch in Dubai’s PPE market:
Smart PPE: Safety gear equipped with sensors for temperature, heart rate, or gas detection.
Eco-Friendly PPE: Sustainable and biodegradable materials gaining traction, especially in hospitality and food industries.
Customization and Branding: Uniforms with company logos and safety colors tailored to brand identity.
Increased Use of E-Commerce Platforms: More companies are turning to digital portals for ordering safety gear efficiently.
How to Choose the Right Safety Equipment for Your Business
Here’s a quick checklist to help business owners or procurement managers:
Conduct a Risk Assessment Understand what hazards exist in your workplace to determine the PPE required.
Consult with Experts Speak with safety consultants or knowledgeable dealers for product recommendations.
Buy Certified Products Only Ensure all products meet safety regulations and are tested for their specific use case.
Train Your Employees Educate your workforce on the proper usage, storage, and disposal of PPE.
Monitor and Replace When Needed Safety gear has a lifespan. Periodic checks help ensure continued protection.
Final Thoughts
In a city as progressive as Dubai, workplace safety is non-negotiable. Whether you're in construction, logistics, healthcare, or hospitality, choosing the right safety equipment suppliers in Dubai, UAE is critical to protecting your workers and your business.
From high-visibility clothing to specialized PPE for oil and gas operations, reputable safety clothing dealers in UAE offer reliable, certified, and customized solutions tailored to your industry.
Invest in safety – because it pays off in productivity, peace of mind, and most importantly, lives saved.
0 notes