#osmoaj
Explore tagged Tumblr posts
Text
Lupine Publishers | A literature review of the treatment options for Idiopathic Adhesive Capsulitis of the Shoulder

Orthopedics and Sports Medicine Open Access Journal (OSMOAJ) Abstract
Goal: Systematic review of current therapeutic options for Idiopathic Adhesive Capsulitis of the shoulder (IAC).Materials and Methods: Research carried out in the MEDLINE / Pubmed database using MeshTerms: “adhesive capsulitis”, “frozen shoulder”, “treatment”. The articles in Portuguese or English published were selected, after which non-relevant articles were excluded based on the title, reading of the abstract and full article.Results: Physical therapy has proven to be beneficial, either isolated or concomitantly with other therapeutic approaches. Options like capsular distention, manipulation under anesthesia and arthroscopic surgery have reported good results, especially in refractory cases. No significant benefits were found with the use of oral corticosteroids, NSAIDs or acupuncture. New treatment options are currently being tested with promising results.Conclusions: There are several effective options for the treatment of Adhesive Capsulitis. In the early stages, conservative measures should be chosen, with special emphasis on physical therapy within the limits of pain associated with low-dose intraarticular injection of corticosteroids. In refractory cases, more invasive treatment options should be suggested namely capsular distension and manipulation under anesthesia.Keywords: Adhesive Capsulitis; Frozen Shoulder; Diagnosis; TreatmentIntroductionGo toAdhesive capsulitis is a pathology characterized by a spontaneous onset of insidious and diffuse pain in the shoulder associated with progressive restriction of active and passive motion of the glenohumeral joint [1]. Almost 150 years after its first description, it remains an uncertain entity. The proper terminology, used for the first time in 1945, is also controversial, since this condition is related to the contraction and thickening of the glenohumeral capsule, in particular the coracohumeral ligament in the rotator’s interval [1, 2]. The disease is classified as primary and secondary. The primary entity has an unknown etiology and will be addressed in this review [3]. Secondary adhesive capsulitis is caused by an event or triggering condition such as trauma, surgery or a systemic condition such as diabetes mellitus, thyroid abnormalities, etc. [2]. Diabetes mellitus has the most established connection, with an estimated incidence of adhesive capsulitis in 20% of this population [4]. The prevalence of this pathology in the general population is believed to be 2-5%. However, it is believed that the true prevalence is actually inferior and difficult to determine, not only because vague and insidious symptoms lead to numerous diagnostic errors, but also because most studies include specific comorbidities with a greater incidence of IAC than within the general population [2, 3, 5, 6]. This pathology occurs mainly between the 4th and 6th decade of life and is thought to be more frequent in women [7]. Some argue that it affects the non-dominant side more often and that in about 20-30% of cases it recurs on the contralateral shoulder, usually in the first 5 years after the resolution of the primary condition [1, 3, 7-10]. Although considered a benign condition, with a self-limiting pattern and resolution within 2 to 3 years, it is estimated that 20-50% of the cases continue with mild to moderate pain and restricted movement over a period of up to 10 years [4, 11]. The etiology of adhesive capsulitis also remains uncertain and theories vary. However, the evidence points to a chronic inflammatory response with subsequent capsular fibrosis that possibly involves increased deposition of cytokines such as TGF-β, PDGF, TNF-α and IL-1 [1-3, 7]. There are also studies that advocate an association with Dupuytren’s contracture that may involve the same abnormalities. The changes found include: contraction and fibrosis of the coracohumeral ligament, thickening and fibrosis of the rotator’s interval, contraction of the anterior and inferior capsule, decrease in joint volume, obliteration of the axillary recess and neovascularization [2, 3]. The evolution of this pathology can be divided into three phases. The acute initial phase (freezing phase) is characterized by the insidious appearance of diffuse pain and restriction of the range of motion of the glenohumeral joint, which lasts for about 10 to 36 weeks (Figure1). In the second phase (frozen phase), for about 4 to 12 months, the pain slightly decreases but the movement restriction continues, with almost total loss of external rotation. In the resolution phase (thawing phase) there is spontaneous progressive improvement in the range of motion and resolution of pain. This last phase has an average duration of 30 months (12 to 42 months) [3, 6-8]. Numerous studies have attempted to determine which treatment is the most effective for adhesive capsulitis. However, currently, despite the various options, there is still no consensus among the authors regarding the most advantageous treatment and at what stages of the disease it should be performed [4, 12, 13]. Most of the evidence is inconclusive due to the precarious methodology of the studies [14].
Diagnosis
There is no standard diagnostic method for this condition, which is based on clinical examination, exclusion of differential diagnosis, normal radiographic appearance and findings on ultrasound, magnetic resonance imaging (MRI) and arthrographic magnetic resonance imaging (arthroMRI) [2, 15]. The early diagnosis of adhesive capsulitis is extremely important since it allows the institution of therapy before the progression of thickening and contracture of the capsule observed in advanced stages [15]. Clinically, an insidious diffuse pain with at least four weeks that interferes with the activities of daily life should be investigated. Night pain is also common, with the patient complaining of more severe pain while sleeping on the affected side. Painful restriction of active and passive motion of the glenohumeral joint is also frequent, with special emphasis on external rotation (more than 50% of restriction) and elevation (less than 100ᴼ) [1, 3]. Radiographs do not normally show any changes, except for a slight periarticular osteopenia of the humeral head and neck, which can occasionally be found [1, 3, 7,15]. The most important role of radiography is the possibility of ruling out other pathologies such as calcifying tendinitis of the rotator cuff, osteoarthritis, avascular necrosis or fractures that can also cause painful movement restriction and be misdiagnosed as adhesive capsulitis [15, 16]. For a more accurate diagnosis, ultrasound, MRI or ArtroRM are usually necessary [15]. With the use of ultrasound, the diagnosis can be suspected by a thickening of the structures in the rotator’s interval, namely of the coracoumeral ligament, and restriction of the motion of the supraspinatus tendon during abduction. With echodoppler, synovial inflammation can be readily detected (Figure 2), which has advantages when compared with MRI and ArtroMRI since it is less expensive, faster, more dynamic and easily accessible [2, 3, 15]. MRI is an effective non-invasive diagnostic tool, not only for cases where this condition is suspected, but also provides information that can help the surgeon differentiate between the different stages of the disease [3,15,17]. Although it is not diagnostic, some argue that the degree of capsular thickening, measured in the axillary recess, can be correlated with the clinical stage of adhesive capsulitis [16]. Among other findings, several characteristics of this condition can be seen: thickening of the coracohumeral and capsular ligament in the rotator’s interval and axillary recess (greater than 4 mm) and obliteration of the subcoracoid space by the thickened capsule (Figure 3). Thus, MRI allows for early diagnosis, determining the pathophysiological stage and ruling out differential diagnosis [15]. ArtroMRI allows for visualization of basic disease characteristics, namely the thickening of the coracohumeral ligament and the capsule, possibly with greater precision than the MRI, but also to detect decreased joint volume [1,3,15]. However, some claim that both MRI and ArtroMRI, despite the useful findings, are not indicated as a means of diagnosis for adhesive capsulitis and should only be used as a method of excluding other intra-articular pathologies [3]. TreatmentA great variety of therapeutic options are available for the treatment of adhesive capsulitis. During the early stages, where pain predominates, treatment should be directed towards pain relief and patients should be advised to limit activities according to their tolerance [7]. The secondary objective is to improve the range of motion [4] and restore the ability to perform the daily activities.Conservative TreatmentConservative treatment, such as physical therapy, is recommended in the freezing phase [4, 6]. Most patients will recover with this initial management [16, 18, 63]. The conservative approach has a wide range of modalities, with well documented results.PhysiotherapyIsolated physiotherapy is a widely accepted treatment option, which can also be used as a complement to other therapeutic modalities [1, 3], with some reports considering it to be crucial for success [4]. Currently, various techniques are used, such as the application of moist heat, strengthening exercises, stretching and manual exercises [7, 19, 20]. Several studies have compared these modalities with different conclusions, making it difficult to determine which is the most beneficial [4, 9,20]. Most studies in which comparisons were made between two interventions did not detect significant differences between the techniques [21]. In several investigations, the techniques of high and low grade glenohumeral mobilization were compared, with significant improvement after 12 months for both approaches. Some authors concluded that the intensive approach was significantly more effective in restoring mobility and reducing disability [20-22]. In contrast, others argue that the amount of force applied should be adjusted to the patient’s condition, limited to their tolerance, because if excessive force is applied, it can produce extreme pain, periarticular injury or abandonment of treatment, thus, one should opt for prolonged progressive low-load stretches, a method considered safe and effective [7, 9, 23]. In a study with level I evidence, the effectiveness of three different physical therapy modalities was compared: group physiotherapy, individual physiotherapy and home exercise program. Not only was there a greater degree of symptomatic improvement in the shoulder, but also better anxiety control with group physiotherapy. There were also benefits in relation to costeffect and self-management in this group. However, standard physical therapy remains a good alternative and has been shown to be significantly better than unsupervised home exercises [6]. In another study with level II evidence in which regular physical therapy was compared with a new contraction technique, the new approach demonstrated greater recovery of the function of the glenohumeral joint when compared to the group of normal physical therapy. However, further studies are needed to validate this conclusion [24]. Some authors advise a Multimodal Care program that includes mobilization, shoulder orthoses and stretches with strengthening exercises, which appears to be beneficial for symptomatic relief, although the evidence seems limited [25, 26]. Horst, et al. compared structural-oriented (conventional) physical therapy with an activity-oriented physiotherapeutic treatment, concluding that therapy based on performing activities appears to be more effective for pain reduction and the ability to perform daily life activities than conventional treatment methods [64]. When compared to ad initium arthroscopy, physical therapy produces similar results, but without surgical aggression and with a better cost-benefit ratio [27]. Lamplot, et al. in a level III cohort study [57] found a decrease in the need of a second intra-articular injection in the patients who underwent physical therapy following the first injection, underlining the major role of physiotherapy in the treatment of IAC. Intra-Articular Injection of CorticosteroidsCorticosteroids have been administered to the glenohumeral joint in several ways, namely anterior, lateral and / or posterior approach [4, 28]. Although clinically it is common practice to use an injection via an anterior or posterior approach, studies comparing different techniques have not found significant differences in the improvement of pain or range of motion [11, 29]. Cho, et al. [60] in a randomized trial study found that the efficacy of corticosteroid injection into the subacromial space in IAC was inferior to intraarticular injection up to 12 weeks. However, a combination of injection sites had an additive effect on the benefits in the internal rotation angle There is no agreement regarding the optimal dose of intra-articular corticosteroids. Yoon et al. did not detect a significant difference between the low (20 mg) or high (40 mg) dose groups, indicating, due to its side effects, the preferential use of low dose corticosteroids for the treatment of adhesive capsulitis [30]. A limitation of the use of intra-articular corticosteroids is the fact that blind injections can be inaccurate in about 60% of cases. The current use of ultrasound or fluoroscopy-guided injection can overcome this problem [8, 16]. It has been shown in several studies that this practice improves accuracy and results compared to the “blind-technique” [3, 31]. There is evidence that the initial corticosteroid injection can reduce pain and improve range of motion in the short term and that its benefit can be increased in the short and medium term when these injections are followed by physical therapy [11, 21, 57]. Kraal et al. in a two center, randomized controlled trial, found that additional physiotherapy after corticosteroid injection improves ROM and functional limitations in early-stage IAC up to the first three months, underlining the good results of these techniques combined [61]. When compared as isolated treatments, there is strong evidence in benefit of corticosteroid injection in the short term (4-6 weeks), compared to isolated physical therapy, but not in the long term [11, 22, 30, 32, 33]. In a study that compared the injection of corticosteroids and the benefit of isolated intra-articular analgesics, significant improvements were found with the administration of corticosteroids [22]. Hettrich et al. showed that corticosteroid injections decreased fibromatosis and myofibroblasts in the shoulders with IAC [58]. On the other hand, some studies conclude that this form of treatment has results similar to isolated physical therapy or more invasive treatments such as MUA and arthroscopy [29, 32, 34], confirming the high degree of controversy surrounding this disease.Echography-Guided Capsular DistensionUltrasound-guided interventions have several strong points like the lack of radiation and the possibility of real time visualization of the needle’s trajectory. This technique has advantages when compared to fluoroscopy, CT and MRI since these are less practical, more time consuming and involve radiation or a specific needle [35]. One of the modalities of capsular distention is based on the use of hyaluronic acid. The ideal time between injections is one week and the effects are usually seen after the second injection [36]. In a study comparing this approach with the injection of corticosteroids, it was found to be more effective in favor of distension with hyaluronic acid in passive external rotation (10ᴼ) at 2 and 6 weeks, with no significant differences in pain relief or in function recovery. This study also concluded that this approach is a good alternative to intra-articular injection of corticosteroids and can be especially useful in patients with diabetes mellitus or contraindicated to the use of corticosteroids [37]. Calis et. al. also concluded that this approach is effective in the treatment of adhesive capsulitis when compared to isolated corticosteroid injection, physical therapy and exercise [36]. Ultrasound-guided capsular hydrodistension is a procedure that aims to distend the capsule contracted by increasing pressure by injecting large amounts of sodium chloride into the glenohumeral joint [9]. There is evidence that it provides relief from pain and improves range of motion, especially when it is followed by physical therapy [29, 38]. Other studies have found that saline distension with or without concomitant corticosteroids are more effective than MUA, describing better results after 6 months with this procedure, with less risk, and resulting in a higher level of satisfaction on the part of patients. However, the effects do not seem to persist beyond 6-12 weeks [9, 29, 39, 40].Artrographic Capsular DistensionThis technique can be performed with sodium chloride, local anesthetic, steroids, contrast or air. It should be reserved for patients who do not improve despite physical therapy [22]. It is also considered a good therapeutic option for rapid symptom relief. Better results were observed when followed by physical therapy [38]. There was no significant difference in the efficacy of capsular distention with or without corticosteroids in most investigations [39, 41]. However, Rysns et al. when comparing distension with corticosteroid injection with placebo saline injection to determine whether the results were due only to the increase in volume, found a significant improvement with the concomitant use of corticosteroids [32].Extracorporeal Shockwave TherapyThe use of Extracorporeal Shock Wave Therapy (ESWT) in the treatment of several shoulder diseases, namely in calcific tendinopathy of the rotators cuff, is well documented. Several studies evaluate its usefulness in IAC, with positive effects such as a quicker return to daily activities and quality-of-life improvement [66, 67], at least in the short-term. El Naggar, et al. compared the effectiveness of radial extracorporeal shock-wave therapy versus ultrasound-guided low-dose intra-articular steroid injection in in diabetic patients, concluding that in the short-term follow-up ESWT was superior to a low-dose intra-articular steroid injection in improving function and pain in diabetic patients with shoulder IAC [68], therefore validating it as an alternative to steroid injections in diabetic patients with this pathology. This particular usefulness of ESWT in diabetic patients has also been documented in other studies [69, 70]. Many prospective randomized trials are underway to further validate ESWT as a treatment option in IAC, especially in the diabetic population.OtherOral non-steroidal anti-inflammatory drugs, although widely used in the initial / inflammatory phases for pain relief in the short term, did not prove their benefit when compared with placebo [3, 7, 9]. Prednisone at a dose of 40 to 60 mg / day for two to three weeks provides faster relief of symptoms in the short term, but their effects are not significant after 6 weeks and there is no evidence that they shorten the duration of disease [28]. Some studies have concluded that there may be a moderate short-term benefit with acupuncture associated with exercise [22], however the usefulness of this therapeutic approach remains undetermined [21]. Calcitonin is a polypeptide hormone secreted from parafollicular cells of the thyroid that has been used for pain control in several pathologies. Although its pathophysiology is not totally clear, it is thought to diminish the inflammatory response and increase endorphins’ release [71, 72]. Rouhani, et al. in a double-blinded randomized controlled trial compared intranasal calcitonin versus placebo for 6 weeks and found great improvement of shoulder pain, ROM, and functional scores in the calcitonin group [71]. Currently the dose recommendation is 200 U (1 puff) daily [73]. Regarding future approaches, Badalamente, et al. [53, 54] published two papers evaluating the applicability of extra-articular collagenase injections in the anterior shoulder capsule. In a placebo controlled doubleblind RCT, they found improvements in shoulder motion, functional score and pain control in the collagenase group in their 1.8 years follow up. In a randomized pilot study comparing subcutaneous adalimumab with local corticosteroids, Schydlowsky et al. found no benefits with the anti-TNF agent in the treatment of frozen shoulder [55] These new treatment approaches for IAC must undergo further investigation, but, if developed, could also play a role in the management of other arthrofibrosis [56].Surgical TreatmentSurgical treatment of adhesive capsulitis is considered after failure of conservative treatment. It is estimated that 10% of patients do not respond to non-invasive treatment [25, 26]. There are no defined guidelines for this transition. However, regardless of the chosen conservative treatment, a surgical approach is only considered after about 6 months of non-surgical treatment without clinical improvement [3, 4, 8, 12, 16, 42]. Its benefit in refractory / severe adhesive capsulitis is proven and well documented [43], and some studies have found that in patients with high risk factors such as diabetes mellitus, and those who suffer chronic symptoms or bilaterally affected, early surgery is beneficial [65]. In a recent questionnaire to health professionals, only 3% recommended surgical treatment in the acute phase, while 47% recommended it in the second and third stages of the disease [4]. Surgical treatments should be complemented with an appropriate physical therapy scheme [63]. Some advocate the initiation of immediate postoperative physiotherapy, with light isometric exercises after 1-2 weeks and isotonic exercises in the following 2-3 weeks. Ideally the range of motion without complete restriction should be achieved in 12 to 16 weeks [4].Manipulation Under AnesthesiaThis procedure involves stabilizing the shoulder blade with flexion, abduction and adduction, followed by maximum internal and external rotation. Some studies advocate good results with this technique, mainly in terms of range of motion [44], others have not found significant differences in comparison with other treatments [45]. There is modest evidence of the benefit of MSA in relieving pain and recovering mobility when followed by physical therapy [46]. However, some authors have not found significant differences in the improvement of pain, function, disability or range of motion in the short, medium or long term between isolated MUA and exercise-associated MUA when compared to physical therapy alone [21, 45]. When compared with arthroscopy, better results were observed with arthroscopic distention at 6 months [21]. However, more recently, Schoch et al. in a study with the largest series of patients undergoing surgical treatment of adhesive capsulitis with a direct comparison between MUA, MUA/Capsular release (CR), and CR alone, found significant improvement of the ROM in all surgical modalities, however, the MUA group had the greatest external rotation, postoperatively [59]. MUA has been associated with several intra-articular iatrogenic complications such as humeral fracture, glenohumeral dislocation, brachial plexus injury rotator cuff injury and hemarthrosis [4, 46, 47]. Nonetheless, some argue that these lesions have no clinical relevance or that they can be minimized by performing the technique properly [44, 47]. Others advise that this procedure should be avoided in patients with osteoporosis, osteopenia or previous MUA recurrence [46]. Another limitation of manipulation is the fact that stretching the tissues can cause severe pain after the end of the anesthesia effect, leading to delays in recovery [8].ArthroscopyArthroscopy allows the distension of the glenohumeral joint to be combined with a series of other procedures, such as adhesions release, opening of the rotator’s interval, circular capsulotomy and section of the coracohumeral ligament. This procedure must be followed by physiotherapy [2]. Several studies have supported the role of this approach as safe and effective in the treatment of adhesive capsulitis [27, 48, 49]. Several authors support the use of arthroscopy, claiming that, in addition to the good results obtained, it makes it possible to deepen and confirm the diagnosis by a complete assessment of the shoulder joint during the procedure [4, 8]. Some, on the contrary, argue that currently the evidence does not support the use of this technique [50], underlining the prevalent controversy in the treatment of this pathology. Recent investigations have not shown greater benefits in range of motion with more extensive release of the capsule (anterior release vs. Anterior plus posterior release) [9, 62]. Sivasubramanian et al. made a systematic review and meta-analysis which suggests that less extensive releases may result in better functional and pain scores. The addition of a posterior release appears to increase early internal rotation, but doesn’t maintain that benefit over time. No benefit was found with the complete 360 release [62]. Some authors suggest that arthroscopic distension can be associated with concomitant manipulation, with improved outcomes [8]. In a study comparing arthroscopy plus manipulation against isolated intraarticular corticosteroid injection, both approaches were effective in improving pain and range of motion. However, the objectives were achieved sooner by the group that underwent arthroscopy (6 weeks vs 12 weeks) [51]. Grant, et al. compared arthroscopic distention with MUA finding a small benefit in favor of arthroscopy alone or in association with manipulation, advising this technique due to the lower number of complications [52]. On the other hand, Jerosch et al. concluded that this therapy has a greater benefit in reducing pain and improving movement, even in the long term, being a valuable, more precise, controlled option with fewer complications than manipulation [12].Open SurgerySurgical treatments have changed from open to arthroscopic procedures and, therefore, the open technique, although effective, has fallen into disuse [4]. It is rarely used nowadays, but may be beneficial in cases refractory to MUA and arthroscopy [9].ConclusionGo toIdiopathic adhesive capsulitis is an extremely painful and limiting pathology of the shoulder, which, despite the abundant published literature, remains controversial in many aspects. Its etiology is unknown, but synovial inflammation of the glenohumeral joint and subsequent progressive capsular fibrosis is believed to occur. The correct diagnosis of this condition is a crucial step in patient orientation. Although the diagnosis is mostly clinical, ultrasound, MRI and ArtroMRI have gained increasing importance, as they more accurately allow ruling out other conditions. Despite the various therapeutic options available, there is still no global consensus among authors regarding the most appropriate approach for the treatment of IAC of the shoulder and there is a need for high-level, definitive evidence to elaborate definitive approach guidelines. Initially, conservative measures should always be chosen, with the majority of patients recovering with non-surgical treatment. There is evidence that demonstrates the effectiveness of physical therapy, being considered by many authors as an essential component of treatment. Corticosteroid injection is an effective form of treatment, especially when guided by ultrasound, with evidence of its benefit in the short, but not long term (after 6 weeks). Lower dosages have been advised in order to minimize its possible adverse effects. ESWT is gaining popularity in the treatment of diabetic and refractory cases, with many studies underway to further validate its importance. Calcitonin and collagenase are two relatively new approaches to the disease, with promising results. Ultrasound-guided capsular distention with hyaluronic acid appears to be useful in the treatment of adhesive capsulitis, being mainly suitable in patients with Diabetes Mellitus or in those with contraindications to corticosteroids. Hydrodistension is an effective method, with results similar to MUA, but with a lower rate of complications, although its effect does not seem to last beyond 6-12 weeks. Arthrographic capsular distention is considered a good option for rapid pain relief, especially in cases refractory to physical therapy. Oral corticosteroids, while providing short-term pain relief, do not appear to shorten the duration of the disease. The association of corticosteroid injection guided by ultrasound with physiotherapy, demonstrated a statistically significant improvement, being advocated by many as the ideal approach for early stages.Surgical treatment should be reserved for cases with unsatisfactory results with conservative approaches, that is, after about 6 months without clinical improvement. Regardless of the surgical therapeutic option, it should be followed by rehabilitation physiotherapy.MUA and arthroscopy are effective in the treatment of idiopathic adhesive capsulitis, especially in severe and complicated cases. MUA, although very popular in the past, has recently gained some skepticism because of the frequently associated complications. For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
8 notes
·
View notes
Text
Lupine Publishers | Persistent Wound Leakage After Total Knee And Hip Arthroplasty

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
In this mini-review the pathogenesis, pathophysiology, diagnosis, treatment and course of prolonged wound leakage after total hip and knee arthroplasty are discussed. It appears there is a disconcerting lack of research and knowledge concerning this topic. Wide variations in definition, classification, diagnosis and treatment hamper patient management, early mobilisation and rehabilitation, as well as the function of the operated joint, severely.
Introduction
The diagnosis and treatment of persistent wound leakage is an important and poorly understood topic in the field of joint arthroplasty. Persistent wound leakage after total knee and hip arthroplasty is associated with a higher risk of developing periprosthetic joint infection (PJI) [1-6]. PJI is a seious complication with great impact on a patient’s physical functioning and quality of life. Moreover, PJI is a high financial burden for society. Additional medical costs of PJI are approximately € 30.000 per patient with even higher societal costs because of productivity loss,home care and informal care provided [7,8]. Unfortunately, there are no evidence-based guidelines for the diagnosis and treatment of persistent wound leakage after joint arthroplasty [6].
Numerous issues hamper the development of sound guidelines. First of all, research on wound leakage is hard, as PJI is used as the major endpoint of wound leakage treatment, which has a low incidence (1,5%)- [9]. Secondly, there is no uniformly accepted definition of wound leakage and when to call it persistent. Clinical practices in orthopedic hospitals vary widely therefore. For that reason pathogenesis, pathophysiology, treatment and course of prolonged wound leakage after arthroplasty are discussed in this mini-review.
Pathogenesis
Following Winter’s original research in 1962, it is now widely accepted that a certain amount of moisture in the wound bed is necessary for optimal healing [10]. The difficulty is determining what that certain amount is and how long it should persist. Inflammation is the body’s normal protective response to any injury (including surgery) or foreign bodies.Acute inflammation follows the early stage of the foreign body response ( protein adsorption) [11,12]. Chemotactic agents within the provisional matrix play a key role in controlling the migration of neutrophils from the vasculature. The travelling leukocytes surrounding the implant become activated in response tothe cytokines released by the platelets e.g PDGF (platelet derived growth factor) and betathromboglobulin [13].
After localization and activation of macrophages and neutrophils tothe site of injury, enzymes are released and then the neutrophils mediated phagocytosis occurs. Theoretically, the phagocytosis should include the procedures of firstly recognizing and attaching to the foreign materials, the nengulfing and degrading them. However, due to the materials size, engulfment and degradation are often not possible,although the process of recognition and attachment occurs. Instead, the implants are coated with opsonins such as complement activated fragments C3b and IgG, which aid the adhesion and activation of neutrophils and macrophages [11]. Macrophages assemble at the implant site, leading to further production of chemoattractive-signalling molecules such as PDGF, tumor necrosis factor (TNF-alpha), interleukin 6 (IL-6), granulocyte-colony-stimulating factor (G-CSF) and granulocyte macrophage colony stimulating factor (GM-CSF), leading to further recruitment of macrophages to the implant site [14]. The foreign body response to bulk implant materials is abberant and prolonged.
At the end-stage of the foreign body response,or when the chronic inflammation occurs, mononuclear cells such as monocytes, lymphocytes and macrophages can present at the implant site. These macrophages which are added by the production of IL-4, IL-13 from Th2 lymphocytes, can fuse together to form a multinucleated foreign body giant cell (FBGC) at the implant surface [15,16]. Next the infiltrated fibroblasts, macrophages and neovascularisation will present within the newly formed granuloma tissue, which is a precursor for forming a fibrous capsule [17,18]. This capsule may contnue to grow following inflammation dueto mechanical motions or chemical leaching exerted in the joint. It was thought that the host response to most bulk biomaterials used in THA was identical and followed these main stages. However, the response tothe wear particles released by different biomaterials over time differ greatly [11,18,19]. Alumnium ceramics are the most biocompatible while Cobalt-Chromium and Ultra-High Molecular Weight Polyethylene (UHMWPE) have reduced bioavailability [18].
Pathophysiology
Total hip arthroplasty is a commonly performed operation and yet little information exists about the duration of wound oozing,the factors associated with this and the implications. Wood et al. Studied 62 consecutive patients undergoing total hip arthroplasty (THA). Time to dryness was associated with wound length (p=0,01), body mass index (BMI;p=0,05) estimated volume of blood in dissected tissues (p=0,05) and length of hospital stay (p=0,02). No association was found with duration of surgery or ASA (American Society of Anaesthesiologists) physical grades [20]. Local factors compromising wound healing include extensive scarring, lymphoedema, poor vascular perfusion and excessive adipose tissue. Systemic comorbidities affecting wound healing include diabetes mellitus, rheumatoid diseases, renal or liver disease, corticosteroid medication, poor nutrition HIV and smoking.Since a history of smoking is associated with a statistically significant increased risk of PJI, many centers use formal smoking cessation programs to assist patients n giving up, preferably before surgery [21].
Patel et al. conducted a retrospective study to determine the risk factors associated with prolonged wound drainage after hip and knee arthroplasty [5]. Risk factors included a BMI>40kg/ square meter, the use of low molecular weight heparin (LMWH) prophylaxis,and a high drain output after THAs. High drain output was the only risk factor associated with prolonged wound drainage after TKAs. HIV infection is also a risk factor for prolonged wound drainage after TKAs [22]. Obesity is a risk factor associated with prolonged operation times,and a higher rate of early postoperative complications, including excessive wound drainage and infection [23]. However,optimal peri-operative glucose control is an important factor in decreasing wound complications for all patients, including those without diabetes [24]. demonstrated that non-diabetic patients were three times more likely to develop PJI if the fasting blood glucose was > 140 mg/dl on the first postoperative day [25]. Proper selection, dosing and timing of prophylactic antibiotics are critical. Most commonly, a first generation cephalosporin is administered within one hour prior to the skin incision.In patients with allergies to penicillin or cephalosporins, clindamycin is an acceptable alternative. For patients with methicillin-resistant Staphylococcus aureus (MRSA) or coagulase-negative Staphylococcus colonisation, vancomycin is used [26].
Diagnosis and Management
Wound healing problems can range from superficial incisional, to deep incisional (outside the joint space) to involving the joint space. Gaine et al. reported a 10% incidence of superficial wound problems in primary TKAs [27,28]. Patel et al. [5] found that each day of prolonged wound drainage increased the risk of deep wound infection by 25% following TKAs. Drainage from the incision one to three days after surgery should be managed by immobilisation in extension, and application of a foam or rolled gauze compressive bandage over the incision. Use of immobilisation and observation should not exceed three days. Wound drainage that persists greater than three days is considered abnormal and should be treated surgically to decrease the chance of subsequent PJI [2,5,22,29].
Aspiration of the joint is necessary if there is a high level of suspicion. The synovial fluid should be analysed for white blood cell (WBC) count and differential.Cultures should also be obtained. There is some consensus with regard to the cell count. In patients with TKAs, a synovial WBC count>1700 cells/ul or a polymorphonuclear neutrophil (PMN) percentage > 65% is rhe recommended threshold for infection [30-32]. In THAs, the recommended thresholds are a synovial WBC count of > 4200 cells/ ul or PMN percentage>80% [33]. During the acute postoperative period,within 6 weeks of surgery, the thresholds are higher with a synovial WBC count>10.000 cells/ul and PMN>89% [34].
Treatment
Prolonged wound leakage after arthroplasty is induced by an inflammatory response , as described above (1,10-16). Conversely, surgical wounds may also show prolonged leakage for other reasons (hematoma,seroma or fatty necrosis) and take longer to heal without development of a PJI. Autoimmune disorders as e.g rheumatoid arthritis and SLE are also associated with prolonged wound leakage [35]. The causes of prolonged wound leakage are poorly understood and studies are scarce and methodologically flaw [6]. However,as expected orthopedic surgeons have been focussed primarily at the association between prolonged wound leakage and PJI.
In the Netherlands,the prevalence of prolonged wound leakage at day 9 after index surgery is about 4% ,2200 patients anually of 55.000 THAs and TKAs. The Dutch Arthoplasty Register reports a total of 3809 THA and 2667 TKA revision surgeries performed in 2015. Revision surgery within 1 year of index surgery was necessary in more than 600 patients and at least 30% of these were PJI related [36]. Persistent wound leakage can be treated by non-surgical and surgical treatment modalities. Non-surgical treatment can consist of relative rest (no exercise and bed rest), pressure bandages,and wound care with sterile bandages.Hospital admission can be required.
Surgical treatment typically consists of debridement, antibiotics and implant retention (DAIR) [37-42]. A DAIR procedure is meant to clean the prosthesis and wound,including break down of the bacterial biofilm, in order to treat the infection and render further infection. Treatment of persistent wound leakage varies considerably among Dutch orthopedic surgeons, as mentioned above [6]. There was a wide variation in classification, definition, diagnosis and treatment of wound leakage. The survey had only a response rate of 18,1%, suggesting wider variations are possible. More than 30 combinations of treatment modalities were used. Remarkably, 23, 4% of responders used antibiotics in the nonsurgical treatment of wound leakage, despite the fact that the efficacy of antibiotic treatment in persistent wound leakage has never been studied. Most respondents (43,8%) convert to surgical treatment if wound leakage is present for ten days after index surgery, implying a non-surgical treatment of 3-7 days. Literature offers litlle guidance but suggests that wound leakage more than 3-5 or 5-9 days after index surgery should be managed by surgical treatment.
Several authors have investigated the effect of DAIR for treatment of wound leakage and reported various results,statements or opinions,generally in favour of early DAIR [2-6], [38-42]. The most recent PJI consensus meetings suggest 5-7 days of wound leakage as the threshold to perform DAIR,but there is no solid evidence forthis statement. As early DAiR is hypothesized tobe helpful in treating or preventing infection and salvaging the implant, the Dutch Leak study will be started soon. This is a controlled randomized study, enrolling 388 patients, with prolonged wound leakage after THA or TKA. Patients are randomized for surgical treatment (DAIR at day 9-10 from index surgery) or continued non-surgical treatment. Primary outcome is the percentage of reoperations for PJI within one year of index surgery. Secondary outcomes are self-reported questionnaires regarding quality of life etc at 3,6, and 12 months after index surgery.
Course and Outcomes
There is a lack of data on the long-term outcome of THAs [43]. Short and medium- term THA studies report substantial improvements in the generic health related quality of life (HRQol) [44-48]. Mariconda et al. conducted a follow-up study to evaluate the quality of life and functionality of 250 patients an average of 16 years (11-23 years) after THA using a validated assessment set including the SF-36 questionnaire,Harris Hip Score,WOMAC score,Functional Comorbidity Index and a study specific questionnaire. The authors report that patients who had undergone THA have impaired long-term self-reported physical quality of life and hip functionality but they still perform better than untreated patients with hip osteoarthritis. However, the level of post-surgical satisfaction is high [43].
considerable proportion of patients report long-term pain after THA or TKA for osteoarthritis.Beswick et al conducted an extensive MEDLINE and EMBASE search of articles published to 2011. Of 1308 articles 115 reported patient-centered pain outcomes. Fourteen articles describing 17 cohorts (6 with hip and 11 with knee replacement) presented appropriate data of pain intensity. The proportion of people with an unfavourable long-term pain outcome in studies ranged from 7% to 23% after hip and 10% to 34% after knee replacements. In the best quality studies,an unfavourable pain outcome was reported in 9% or more of patients after THA and about 20% after TKA [49]. There are no specific short- or long-term studies (>3 years after index surgery) concerning the effect of persistent wound leakage after THA or TKA on quality of life and joint function, whatever the cause or treatment of prolonged oozing.
Conclusion
There is a disconcerting lack of research and knowledge concerning the treatment of prolonged wound leakage after THAs and TKAs, surgeries performed in huge numbers worlwide. With an estimated prevalence of 4%, patients with prolonged wound leakage after arthroplasty also represent a lot of people. Prolonged wound leakage is induced by inflammation, caused by infection immunologic incompability to the implant, autoimmunity as in rheumatoid disorders and SLE, or decreased host defence as in e.g.HIV infection. It will be no surprise that orthopedic surgeons primarily focussed on the association between the low incidence periprosthetic joint infection (1,5%) and prolonged wound leakage after THA or TKA. Recently, a Dutch survey among orthopedic surgeons showed a wide variation in definition, classification, diagnosis and treatment of prolonged wound leakage after arthroplasty.More than 30 combinations of treatment modalities were in use. Remarkably, the unproven use of antibiotics was present in nearly 25% of non-surgical treaments of this issue.
There is no evidence favouring non-surgical treatment above surgical treatment or vice versa. N evertheless, DAIR (debridement, antibiotics and implant retention) is favoured by most orthopedic surgeons at 3-5,5-7 and 9-10 days after index surgery. This arbitrarily and hypothetical timing of DAIR will be studied in an upcoming Dutch trial, the LEAK trial, randomizing 388 patients with prolonged oozing for DAIR at day 9-10 after index surgery versus non-surgical treatment. It is clear that whatever the cause and treatment of persistent wound leakage,early mobilisation and rehabilitation of the patient as well as the function of the joint are hampered severely. There are no sttudies availabale evaluating this topic. It is evident a lot has to be learned in managing and treating prolonged wound leakage after the most common performed arthroplasties in orthopedics.
To know more about our Orthopedics and Sports Medicine click on https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php To know more about Lupine Publishers click on https://lupinepublishers.us/
To know more about Open access publishers click on Lupine Publishers
1 note
·
View note
Text
Adrenal Fatigue
New Post has been published on https://ndmedic.com/adrenal-fatigue__trashed/
Adrenal Fatigue
Adrenal Fatigue affects individuals who suffer from a long stretch of physical, mental, environmental, or emotional stress. Adrenal fatigue can affect anyone, but individuals who are more likely to suffer from Adrenal Fatigue include single parents, individuals who are drug dependent, those who have faced a life crisis, or those who have a stressful job circumstance. The term adrenal fatigue syndrome encompasses a broad spectrum of debilitating symptoms associated with chronic adaptation to stress. Nervousness, body aches, sleep disturbance, digestive problems, reduced memory, and feelings of tiredness and exhaustion are some of the common adrenal fatigue symptoms [1].
Does adrenal fatigue really exist?
Prolonged exposure to stress leads to degenerative and physiological changes that are brought up by the excessive stimulation of the sympathetic nervous system in our bodies. As of now, there is no specific medical condition that can diagnose this progression to health degeneration.
There are controversies over whether or not adrenal fatigue is an actual medical condition. Recent studies have shown that stress profoundly affects adrenal gland activities and its hormonal activities; further supporting the theory of adrenal fatigue [2]. The truth is that the labelling of the condition is irrelevant when there are simple options available that can help with the collection of symptoms and the condition. Regardless of the label, there are many people who are suffering from similar symptoms, and a personalized plan that includes counselling, medications, supplements, and lifestyle changes can help.
Then what is the real theory behind Adrenal Fatigue?
Adrenal fatigue is an actual problem that occurs when we face too much stress in our lives. Adrenal glands are two small organs that are located above our kidneys; they deal with stress through the release of hormones like cortisol [3]. When people face long term stress, adrenal glands cannot produce an appropriate amount of stress-related hormones required by our body. Symptoms of “adrenal fatigue” occur because of such conditions [4,5]. Physiological Progression of Adrenal Fatigue consists of three phases: the alarm, the resistance and the exhaustion phases [6].
Alarm Phase:
During the Alarm Phase also known as the fight-or-flight response, the body responds to the release of stress chemicals by increasing blood pressure, heart rate, increasing blood flow to the muscles. Increased cortisol hormone, then causes a reduction in dehydroepiandrosterone (DHEA) production. The high cortisol to DHEA ratio may cause high blood sugar, infections, bone demineralization, water and salt retention, muscle loss, and an inability to lose weight [6].
Resistance Phase:
During the resistance phase, the action of cortisol is most prevalent. When secreted in small amounts cortisol acts as a powerful anti-inflammatory helping with tissue repair, but in large amounts, it further suppresses the immune system. The risk of disease increases as the excessive cortisol over stimulates cells.
Exhaustion Phase:
Diminished amounts of cortisol and aldosterone during this phase cause a decrease in gluconeogenesis, rapid blood sugar fall, and sodium loss and potassium retention [6].
Adrenal Fatigue versus Adrenal Insufficiency:
It is important to note that Adrenal Fatigue is different from Adrenal Insufficiency. Adrenal insufficiency is a medical condition that occurs when our adrenal glands do not produce sufficient amounts of hormones that are required by our body. In fact, Adrenal Insufficiency occurs due to the damage in the adrenal or the pituitary glands [7] [8]. The pituitary gland is a pea-sized gland present in the brain and its primary function is to instruct the adrenal glands to produce cortisol hormone [9]. A person who has adrenal insufficiency can be confused, dehydrated, and can face weight loss. They can feel tired, weak, have blood-pressure problems, and feel dizzy. Other symptoms include nausea, diarrhoea, stomach pain, and vomiting. Adrenal fatigue is a different condition in which high-stress levels affect the optimal functioning of the adrenal glands.
Symptoms and Signs of Adrenal Fatigue [10] [11] [12]:
The most common symptoms and signs of adrenal fatigue are the following:
Decreased energy and stamina- feeling exhausted and run down most of the day Reduced resilience Decreased productivity Feeling overwhelmed Lack of a refreshed feeling even after 8 hours of sleep Hypoglycemia Mild depression Concentration problems Craving sugar and salt Digestive problems Trouble in waking up and getting sleep Tiredness Lightheadedness when standing up quickly. Inability to really wake until after 10 a.m., afternoon low between 3 and 4 p.m. and then feeling better after 6 p.m. Difficulty getting up in the morning Increased effort to do everyday tasks
Natural Treatment of Adrenal Fatigue:
let’s explore how to treat adrenal fatigue naturally:
Lifestyle Modification [13] [14]:
There are some important modifications that you can bring into your lifestyle for treating or reducing the effects of adrenal fatigue: Let’s have a look at them to learn how to treat adrenal fatigue?
Look out for ways to reduce your emotional, mental and physical stress load Reduce commitments Spend at least 2 hours of free time daily Create a chart! Make Two columns; In one column list the tasks or situations that make you feel good and in the next column list habits, situations, people or tasks that are making you feel down or stressed out. After prioritizing the items, start doing more of the things that make you feel good and try to daily eliminate things that are making you feel low or stressed out. After a few weeks, you will feel a good change in you. Have a regular sleep schedule Avoid people who drain your energy. Exercise in a moderate way daily
Dietary Changes:
Adrenal fatigue diet:
Foods to avoid:
It is recommended to limit the use of drinks and foods which are high in sugar [15].
Here are some foods which you should avoid:
White flour White sugar Caffeine Alcohol Soda Processed food Fried foods Artificial sweeteners Fast foods
Eating a meal on time is also essential to regulate your blood sugar and for the proper functioning of your adrenal glands.
Foods to eat:
Try foods that have healthy fats, a balanced amount of protein, and nutrient-dense carbohydrate. Also, increase the amount of vegetable intake in your food. Vitamins B, C, and magnesium are also good for the optimal functionality of the adrenal glands. vitamin C, in particular, is essential for the production of adrenal steroid hormones and is used in the adrenal cascade. Vitamin C is considered to be the most important vitamin in adrenal recovery.
Here is a list of foods you should include in your diet to treat adrenal fatigue [16]:
Fish Eggs Nuts Legumes Colourful vegetables Leafy greens Whole grains Olive oil Grapeseed oil Coconut oil Low sugar fruits
Herbal Supplements:
Here is the brief detail of some of the best supplements that would help you with the collection of the symptoms.
Maca root
Maca root is an adaptogenic herb; meaning that it helps our body in stress. It is full of Vitamin B, Vitamin C, zinc, magnesium, calcium, and iron. Maca is full of phytonutrients and antioxidants and plant-based proteins. It helps to relieve depression and anxiety to support mood balance and energy [17]. These herbs are best adrenal fatigue treatment.
Licorice root
Licorice root is very beneficial for those people who do not produce an adequate amount of cortisol. There are many studies conducted that proved that licorice root can increase the energy level and can regulate the cortisol level in adrenal glands [18] [19].
Siberian ginseng
Siberian ginseng is the herb that supports adrenal glands and increases body stamina. It deals with memory issues, chronic fatigue, irregularities in blood sugar level, and lowered immunity. It is the best natural treatment for adrenal fatigue [20].
Golden root
Golden root is also known as Rhodiola Rosea. If you are suffering from Adrenal Fatigue, then this root can help you to reduce your stress [21].
Outlook:
If you feel symptoms such as weakness, feelings of tiredness, or exhaustion then you should visit your naturopathic doctor for your full diagnosis. You may also have anaemia, sleep apnea, depression, fibromyalgia, or other health-related problems.
References:
[1] Lee, D., 2009. Adrenal fatigue syndrome: A project report. California State University, Long Beach.
[2] Francesca Spiga, Eder Zavala, Jamie J. Walker, Zidong Zhao, John R. Terry, Stafford L. Lightman. Dynamic responses of the adrenal steroidogenic regulatory network. Proceedings of the National Academy of Sciences, 2017; 201703779 DOI:
[3]Rosol, T.J., Yarrington, J.T., Latendresse, J. and Capen, C.C., 2001. Adrenal gland: structure, function, and mechanisms of toxicity. Toxicologic pathology, 29(1), pp.41-48.
[4] Hajare, R.A., 90 90 90 Formulas and Symptoms of Adrenal Fatigue Syndrome (AFS) of Adult Men. Orthop & Spo Med Op Acc J 1 (3)-2018. OSMOAJ. MS. ID, 111.
[5] Jameson, D., 2016. Persistent burnout theory of chronic fatigue syndrome. Neuroscience and Medicine, 7(2), pp.66-73.
[6] Martini FH. Fundamentals of Anatomy and Physiology. (6th ed.). San Francisco, CA: Pearson Education; 2004.
[7] Oelkers, W., 1996. Adrenal insufficiency. New England Journal of Medicine, 335(16), pp.1206-1212.
[8] Charmandari, E., Nicolaides, N.C. and Chrousos, G.P., 2014. Adrenal insufficiency. The Lancet, 383(9935), pp.2152-2167.
[9] Rubin, R.T., Phillips, J.J., McCracken, J.T. and Sadow, T.F., 1996. Adrenal gland volume in major depression: relationship to basal and stimulated pituitary-adrenal cortical axis function. Biological psychiatry, 40(2), pp.89-97.
[10] Patel, L., Wales, J.K., Kibirige, M.S., Massarano, A.A., Couriel, J.M. and Clayton, P.E., 2001. Symptomatic adrenal insufficiency during inhaled corticosteroid treatment. Archives of disease in childhood, 85(4), pp.330-334.
[11] McDermott, M.T., 2019. Adrenal Fatigue. In Management of Patients with Pseudo-Endocrine Disorders (pp. 127-137). Springer, Cham.
[12] Lee, D., 2009. Adrenal fatigue syndrome: A project report. California State University, Long Beach.
[13] Cope, C.L., 1972. Adrenal steroids and disease (Vol. 179, p. 275). London: Pitman medical.
[14] Wilson, J.L., 2014. A clinical perspective on stress, cortisol, and adrenal fatigue. Advances in Integrative Medicine, 1(2), pp.93-96.
[15] Kara Fitzgerald, N.D., Health Regimen for a 29-Year-Old Female Diagnosed With Adrenal Fatigue. Integrative Medicine, 10(6).
[16] Sarris, J., Moylan, S., Camfield, D.A., Pase, M.P., Mischoulon, D., Berk, M., Jacka, F.N. and Schweitzer, I., 2012. Complementary medicine, exercise, meditation, diet, and lifestyle modification for anxiety disorders: a review of current evidence. Evidence-Based Complementary and Alternative Medicine, 2012.
[17] Meissner, H.O., Mrozikiewicz, P., Bobkiewicz-Kozlowska, T., Mscisz, A., Kedzia, B., Lowicka, A., Reich-Bilinska, H., Kapczynski, W. and Barchia, I., 2006. Hormone-balancing effect of pre-gelatinized organic Maca (Lepidium peruvianum Chacon):(I) biochemical and pharmacodynamic study on Maca using clinical laboratory model on ovariectomized rats. International journal of biomedical science: IJBS, 2(3), p.260.
[18] Al-Dujaili, E.A., Kenyon, C.J., Nicol, M.R. and Mason, J.I., 2011. Liquorice and glycyrrhetinic acid increase DHEA and deoxycorticosterone levels in vivo and in vitro by inhibiting adrenal SULT2A1 activity. Molecular and cellular endocrinology, 336(1-2), pp.102-109.
[19] Imbalance, A., 2009. Nutrients and botanicals for treatment of stress: adrenal fatigue, neurotransmitter imbalance, anxiety, and restless sleep. Alternative Medicine Review, 14(2), pp.114-140.
[20] https://medlineplus.gov/druginfo/natural/985.html
[21] https://www.nccih.nih.gov/health/rhodiola
0 notes
Text
Lupine Publishers | Best Position and Duration for Immobilization in Primary Anterior Shoulder Dislocation: A Systematic Review and Meta-Analysis of Randomized Controlled Trials

Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Abstract
Background: Anterior shoulder dislocation is the most common injury of the glenohumeral joint and primarily caused by traumatic event and shoulder instability. Recurrent dislocation of anterior shoulder dislocation is a common occasion following the primary anterior shoulder dislocation. Generally, anterior shoulder dislocations are treated with closed reduction, stages of immobilization, and series of physical exercise treatment. This systematic and meta-analysis study were conducted to consider the best duration and position of immobilization after primary anterior shoulder dislocation reduction to reduce the risk of anterior shoulder dislocation recurrence.
Methods: PubMed, Cochrane, NCBI, Elsevier were used to searched randomized controlled trials. Two reviewers selected studies for inclusion, assessed methodological quality, and extracted data. The studies were peer-reviewed by two consultant, then selected based on inclusion criteria.
Study Design: Systematic review and meta-analysis; Level of evidence, I, II.
Result: A total of seven randomized controlled trials (635 patients) included in this systematic review and meta-analysis. In these studies, the recurrence rate of instability in ER group was 23.45% (76/324) versus IR group was 33.44% (104/311). Pooled data showed that ER immobilization significantly reduced the recurrence rate of instability (risk ratio, 1.83; P= 0.0001) compared to IR immobilization. Pooled data also summarized that immobilization in 3 weeks significantly reduced the risk of recurrence compared to ER immobilization in 4 weeks (risk ratio, 2.35; P=0.01). The subgroup analysis has been made and there was no significant difference between ER immobilization and IR immobilization in patient aged <30 years (P=0.29). Analysis on 3 studies showed that there was no significant difference in WOSI score between both groups (p=0.32).
Conclusion: Best position and duration for primary anterior shoulder dislocation is ER immobilization in 3 weeks. This study found it significantly reduces the risk of recurrence instability. Furthermore, more studies needed to support the result of our studies to determine best assessment for anterior shoulder dislocation and the risk of recurrence instability.
Keywords: Anterior Shoulder Dislocation; Immobilization; External Rotation; Recurrence Rate; Meta-Analysis
Introduction
The glenohumeral joint has its large arc of motion, making them prone to mild or even severe injury [6,12]. The most common injury to the glenohumeral joint is anterior shoulder dislocation [12], which possibly the cause of a traumatic event or the shoulder instability itself.9 Anterior shoulder dislocation contributes 96% of total shoulder dislocations [11, 19]. The incidence of primary anterior shoulder dislocation is between 11.2 to 26.2 per 100,000 people. Recurrent dislocation is caused by a lesion in the glenoid labrum; the primary stabilizer of the shoulder. The prevalence of primary anterior shoulder dislocation is high in athletic activities, with the mechanism of apprehension position of shoulder abduction and external rotation [29]. Traditionally, anterior shoulder dislocations are treated with closed reduction, stages of immobilization in external or internal rotation for 2-6 weeks, and a series of physical exercise treatment, perhaps reducing the risk of recurrent dislocation and enhance the soft tissue healing [12, 18, 20] Despite its protocol to treat the anterior shoulder dislocation, the most advantageous time and position of immobilization yet the best position has to be proven. Therefore, we conducted a systematic review and meta-analysis from the available literature to consider the best duration and position for immobilization after the reduction of anterior shoulder dislocation.
Materials and Methods
Literature Search
Electronic databases (PubMed, NCBI, Cochrane, and Elsevier) were searched without limit. This study was conducted strictly following the methods established in the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA). We independently reviewed the titles and abstracts and strictly followed the inclusion criteria12: [1] the patient must be diagnosed with primary anterior shoulder dislocation; [2] direct comparison between internal and external rotation immobilization with recurrence rate in result for comparison; [3] more than 1-year follow up; [4] must be randomized controlled trials (RCTs). Exclusion criteria included studies where: [1] retrospective study, case reports, reviews, observational studies; [2] the outcome data were not available; [3] follow up time less than 1 year. Publications were excluded by title review, and abstracts, of all studies that were not excluded by title were reviewed to meet the criteria mentioned above. Then publications that have been reviewed were retrieved in full text and were read in detail.
Literature Search
We reviewed and extracted independently all the studies. Especially year of publication, study design, patient demographics (age, sex, sample size), type of immobilization, duration of immobilization, mean follow-up time, loss to follow up rate, recurrences rate, and WOSI Score. We used data from the analysis of treatment from the available data from the studies. If the data were not reported, we extracted them from the accompanying graphs.
Statistical Analysis
To perform the meta-analysis, we used RevMan version 5.3 software (Cochrane Collaboration). We used the risk ratio (RR) and a 95% CI as a pooled measure for dichotomous data. Inconsistency index [I2] test which ranges from 0% to 100% was used to assess heterogeneity across studies. A value above 50% or P <0.05 indicates statistically significant heterogeneity. We used the Mantel-Haenzsel method with a fixed-effect model for meta-analysis and a random effect model was used in case of heterogeneity. All P values were 2-tailed with a statistical significance set at 0.05 or below.
Source of Funding
No external funding support was received for this study.
Results
The literature search identified 138 studies. Among these 138 studies, 41 were excluded by titles (duplicates), 36 were excluded by abstract. Leaving 61 studies to be screened, and after we reviewed all the studies, we did consult with our consultant and 54 have been excluded by peer-reviewed, leaving 7 RCT in total to be included in our study.
Description of Studies
We included 7 RCTs comparing ER and IR immobilization after primary shoulder dislocation. Overall, there were 635 patients included in this study, with a mean age of 29.2 years across the 7 included studies. The overall follow-up time for the included studies was 23.6 months. Male to female ratio was 288:68 in the ER group, and 262:65 in the IR group. Duration of immobilization ranged from 3 to 4 weeks. The characteristics, main outcomes, and patient demographics included in the studies are shown in Tables 1 to 3. Itoi, et al [1] Itoi et al. reported in a clinical trial that immobilization in ER was shown to reduce the risk of recurrence shoulder dislocation compared to the IR groups. There were 198 participants (104 were treated in ER and 94 in IR). The average patient age reported was 37 years. The inclusion criteria included [1] firsttimer dislocation, [2] within 3 days after dislocation, [3] no associated fracture based on radiograph findings. They reported that recurrent dislocation was 25% in the ER group (22/85), and 42% in the IR group (31/74). Taskoparan, et al. [2] performed a randomized clinical trial comparing 3 weeks of immobilization in 10o of external rotation and internal rotation. The inclusion criteria of this study were primary anterior shoulder dislocation, no hyperlaxity of the shoulder, and admission on the first day of reduction after a dislocation. However, the exclusion criteria were not stated in this study, but it was stated that 2 patients were excluded from the study with, respectively, brachial plexus injury and hyperlaxity of the shoulder. A total of 33 met the inclusion criteria with 20 patients who encountered the dominant side. To be noted, 1 from 16 patients (6.3%) in external rotation group and 5 from 17 patients (29.4%) in internal rotation group experience anterior shoulder dislocation recurrence (p>0.05). While patients aged between 21-30 in the ER group did not fall on anterior shoulder dislocation recurrence, 5 patients in the IR group did (p=0.035). Hence, this study showed that external rotation is an effective preference to prevent recurrence of anterior shoulder dislocation rather than traditional internal rotation sling Liavaag, et al. [3] enrolled in a multicenter clinical trial from 13 hospitals, comparing immediate 3 weeks immobilization of both internal rotation; sling and swathe; and 15o external rotation; external rotation immobilizer. The inclusion criteria were [1] patients aged 16 – 40 years old and [2] successful reduction of primary traumatic anterior glenohumeral dislocations which were documented with a conventional radiograph. Furthermore, glenoid fracture with large osseous defect, greater tuberosity fracture with malalignment after repositioning, nerve injury-prone to the dislocation or even the reduction, and the unwillingness or ineptitude to take part in the study were excluded. Afterward, the outcome of the intervention was measured with a minimum of 24 months (2 years) of follow-up after the first anterior shoulder dislocation. A total of 188 patients; 93 randomized to ER and 95 randomized to IR; were acquired in the study with the mean age of 26.8 ±7.1 years old, ranging from 16-40 years old. It was shown that the recurrence rate (primary outcome) of internal rotation immobilization was 24.7% and 30.8% for external rotation immobilization with p = 0.37. Moreover, the secondary outcome measures the Western Ontario Shoulder Instability Index (WOSI) with a median score for the ER group was 238 and 375 for the IR rotation group, the difference was not significant (p=0.32). From the study, it was concluded that immobilization in the external rotation did not reduce the rate of recurrence for patients with primary anterior shoulder dislocation Heidari, et al [4] performed a prospective, randomized, controlled, clinical trial to compare the effectiveness of immobilization in external rotation (15o abduction and 10o external rotation) and internal rotation. The subjects were picked from the ED within 6 hours after the primary unilateral anterior shoulder dislocation, ranging from 15-55 years old and inclining to be followed up. Patients with previous shoulder issues, surgical joint repair, multidirectional instability, shoulder injuries requiring surgical intervention, associated with fractures of the shoulder upon routine radiographic examination, and unwilling to be followed up for the next 24 months were excluded. Afterward, all the patients included were assigned in a ratio of 1:1, respectively, in the adduction – internal rotation (AdIR) group and abduction – external rotation (AbER) group. The primary outcome was a recurrent dislocation, measured with WOSI. From the results, it was shown that the recurrence rate was significantly higher in AdIR group (33.33%) rather than the AbER group (3.9%), with p < 0.001. Hence, the abducted and externally rotated stabilization for primary anterior shoulder dislocation has more benefit in reducing the risk of anterior shoulder dislocation recurrence Whelan, et al. [5] Prospective multicenter randomized control trial with singleblinded evaluations was a study conducted by Whelan et al to 2 study groups. They are external rotation brace (90o elbow flexion, 0o shoulder abduction and flexion, and 0o- 5o external rotation at the shoulder), and internal rotation sling (90o of elbow flexion, 0o of shoulder abduction and flexion, and 70o-80o of internal rotation at the shoulder). Both groups were obligated to wear the fixator for a total of 4 weeks. Furthermore, the exclusion criteria of this study including previous instability of the affected shoulder with significantly associated fractures of the proximal humerus, glenoid, or scapula (except Hill-Sachs lesion and/ or small bony Bankart lesions) or those who were unwilling to participate in the study. The result was 37% (10/27) of ER group experienced recurrent dislocation and subluxation, while 40% (10/25) of the IR group (p=0.41 for recurrent instability between groups). The WOSI scores were not different between the groups respectively 87% and 84% for external rotation and internal rotation (p=0.74). Hence, it was concealed from this study that there was no significant difference in the rate of recurrent dislocation or instability between the groups of external and internal rotation Chan, et al. [6] A prospective, multi-center randomized control trial was conducted by Chan, et al. between 2006 and 2010. This study looked into the better outcome between using the conventional sling/ Polysling (internally rotated shoulder) or external rotation brace (30o externally rotated shoulder and 30o abduction) in the first occurrence of anterior shoulder dislocation for 4 weeks after the incidence. Starting from September 2006, patients with primary anterior shoulder dislocation ranging from 14-45 years old were put into the study. Exclusion criteria included an associated fracture, an indication for surgery (as determined by the recruiting surgeon), inability to provide informed consent, learning difficulties, mental illness, dementia, significant co-morbidities, or if the patient was unwilling to participate. After 24 months, the follow-up data showed that 30% of subjects who were put in internal rotation sling experienced recurrence of anterior shoulder dislocation, while 24% of subjects of external rotation and abduction did come through anterior shoulder dislocation recurrence. From the study by Chan et al, it can be concluded that ER bracing is unlikely more superior to provide advantages in traumatic first-time anterior shoulder dislocation Murray, et al. [7] A report from Murray, et al found that there is no significant difference between the ER and IR groups. Fifty patients were included in the study, which 25 patients allocated in the IR group and others [25] in the ER group. One patient refused to be treated in external rotation, and three patients were lost to follow-up. This study also reported that 38.3% of the patients had recurrent shoulder dislocation within two years. The recurrence rate was 47.8% (11 of 23) in IR group and 29.2% (7 of 24) in the ER group. They also report that in the subgroup aged between 20 and 40 years, the recurrence rate was 50% (9 of 18) in the IR group and 17.6% (3 of 17) in the ER group (p=0.044). For the patient aged under 20 or over 40 years found that no significant difference was found between IR and ER groups.
Recurrence Rates
We included 6 studies for the recurrence rate at all ages. All data were pooled to make a meta-analysis. We found that ER immobilization was significantly reduce the recurrence rate at all ages (RR: 1.83 (1.35, 2.48); p=<0, 0001; I2=42%) (Figure 2). Moreover, in sub-group analysis we found no significant difference in recurrence rate based on age, <30 years (RR: 1.50 (0.70, 3.18); p= 0.29; I2=67%) (Figure 3), and >30 years (RR: 1.81 (0.45, 7.24); p=0.32; I2=59%).
Duration of Immobilization
We included 6 studies for the duration of immobilization which separated into two groups, inclusive of 3 weeks and 4 weeks. We pooled all the data to make a meta-analysis. From the forest plot, we found that 3 weeks of immobilization in ER significantly reduce the recurrence rates (RR of 2.35 (1.18, 4.67); p= 0.01; I2=53%). In contrast, 4 weeks immobilization showed no significant difference to reduce the recurrence rate of anterior shoulder dislocation (RR=1.14 (0.65, 2.01); p= 0.64; I2=0%).
The Western Ontario Shoulder Instability Index (WOSI) Scores
The WOSI scores analysis was obtained from 3 studies to value the disease-specific quality of life (QoL) deficits between both IR and ER groups. It was found that there was no significant difference in the WOSI scores between both groups (p = 0.32, I2 = 0%).
Discussion
Recently, several studies showed reports about preferences in immobilization. Yet its duration, after a primary anterior shoulder dislocation, remains questionable, controversial, and debatable [25]. In our study that includes a meta-analysis of level I and II trials, we added 2 RCTs that had not been included in the previous meta-analysis [6, 7]. We pooled recurrence rates by age (all ages, <30 years, and >30 years) to evaluate the effectiveness of immobilization for reducing the risk of recurrence rate objectively. We also pooled the duration of immobilization of primary anterior shoulder dislocation to conclude the significance duration for reducing recurrence rate, WOSI score also being pooled to evaluate the better immobilization position. The previous systematic review and meta-analysis studies reported that there was no statistically significant difference between ER and IR immobilization to reduce the risk of recurrence [21,31]. In contrast, one of the recently published systematic review and meta-analysis showed that there is a statistically significant difference in recurrence rate based on immobilization, the investigator found that ER immobilization is superior to IR immobilization based on pooled data that has been shown in their study (p = 0.007)8.
The summary of our review and meta-analysis based RCTs with the highest-level evidence (level I or II trials) found that ER immobilization is statistically significant to reduce the recurrence rate (P<0.0001) at all ages, although we did not find any statistically significant difference in group ages <30 years (P=0.29), and >30 years (P=0.40). Even though we found a significant difference between the groups, still more RCTs are needed to prove the efficacy and preferred immobilization position [21]. According to our study, ER immobilization after primary anterior shoulder dislocation was preferably superior to IR immobilization, perhaps reducing the risk of recurrence and shoulder instability [1,17]. It was found no detachable contact force when the arm placed in IR immobilization after anterior shoulder dislocation. ER immobilization has been suggested based on an MRI study which stated that external rotation would maintain the labrum and capsule in close contact to the glenoid and enhance the tension on the subscapularis muscle [19,32]. Moreover, a biomechanical study on cadaver proved that gleno-labral contact was much wider when the shoulder was externally rotated in 450. [2,19,22,32] However, 45o in the external rotation will increase the contact force and seem difficult to be tolerated by the patients, therefore, most of the studies performed 10o external rotation to increase the cooperation rate in immobilization [2,22]. A radiologic study also confirmed that immobilization in external rotation had a positive impact in decreasing the hemarthrosis and reduction of anterior capsule detachment and labral lesions [1, 2, 17, 32]. Regarding to its superiority, some studies also reported the conflicting results on patients’ acceptance to use external rotation brace [23]. In 2010, Paterson, et al made an analysis for preference duration of immobilization in primary anterior shoulder dislocation. 25 The analyst showed that duration of immobilization <1 week and >3 weeks had no statistically significant difference in reducing the risk of recurrence. Since then, no reports have been showing about preferred durations of immobilization of primary anterior shoulder dislocation. Two comparisons had been made in our study to conclude the best duration of immobilization. Pooled data from 3 weeks of immobilization showed a statistically significant difference to reduce the recurrence rate (p=0.01). Otherwise, we found no statistically significant difference in the duration of immobilization in 4 weeks (p=0.64). One of the most common complications of anterior shoulder dislocation is hemarthrosis of the glenohumeral joint which would maintain the anterior capsule detachment.21,28,33 Hemarthrosis itself would resolve and be absorbed only after 3 to 7 weeks, which why 3 weeks are considered as the minimum compliance time of immobilization 21,33.
Conclusion
This meta-analysis study summarized that ER immobilization in 3 weeks is the best position and duration for immobilization after primary shoulder dislocation based on recent RCTs (Level I; II Evidence). We suggest more meritorious and thorough prospective randomized controlled trials with long-term follow-ups to be conducted, perhaps cutting off the biases in meta-analysis study and annotate an objective outcome.
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
6 notes
·
View notes
Text
Lupine Publishers | Effectiveness of Eccentric Exercise for the Management of Rotator Cuff Tendinopathy: A Critical Review

Lupine Publishers | Orthopedics and Sports Medicine
Introduction
The rotator cuff (RC) mainly contains four muscles and their tendons: infraspinatus, supraspinatus, teres minor and the subscapularis [1]. These four muscles and their tendons surround the shoulder joint [2]. It is a group of muscles start from the scapular and attach around the humeral head, forming a cuff at the anatomical neck of the humeral head. The main function of the RC is to stabilize and activate the glenohumeral joint (ibid). The RC primarily performs three types of movement: abduction, external rotation and internal rotation. Previous studies report that there is no strong evidence that the RC contributes to glenohumeral movement (ibid). However, there are a large number of published studies that describe the link between RC and glenohumeral joint stability [3]. Hence, RC injury can result in loss of stabilization of the glenohumeral joint. RC tendinopathy (RCT) has been regarded as a kind of RC injury. RCT is a term used to describe a combination of pain and weakness in the RC tendon [4]. Also, it can be loosely described as excessive load resulting in impaired performance of the RC tendon when experienced with particular movements of the shoulder [5]. The prevalence of RCT is 14% in the general labor population [6]. In addition, a number of authors have considered the prevalence of RCT. It has been reported that prevalence is 19% among all ages (ibid). Therefore, the high prevalence of RCT cannot be underestimated. The diagnosis of RCT can be measured by ultrasound and magnetic resonance imaging (MRI). Its diagnosis also can be considered in association with pain symptoms [7-9].
Pathophysiology
There are many risk factors that can cause RC injuries. These include glenohumeral joint dynamic instability, joint abnormality and abnormal shoulder structure [10]. After a RC injury, the damaged tendon gradually develops microtears, calcification and fiber vascular proliferation [11]. The pathophysiology of RC injury can be attributed to the result of series of inflammatory reactions after soft tissue injury. However, RCT is characterized by different types of RC tendon injury. Tendinopathy is a common term used to describe pathological changes in tendons. Previous research has established that the pathology of RCT primarily contains intrinsic mechanisms, extrinsic mechanisms or combined mechanisms [2-7]. Intrinsic mechanisms can be defined as pathological changes directly affecting the tendon itself [12]. Excessive load is an important contributor to RC intrinsic tendinopathy. Healthy adult’s RC tendons consist of water, collagen, proteoglycan and glycosaminoglycan [13]. The largest proportion of RC tendon is type I collagen [14]. The collagen fibers of the tendons are confluent and form a cuff on the humeral head. It also forms a five-layer complex near the greater tuberosity. The first to fifth layers are superficial coracohumeral ligament, the main portion of tendon complex, dense fascicles, loose connective tissue and fibrocartilage, respectively. This composite structure seems to have excellent stability and elasticity. However, according to the intrinsic theory, the transformation of collagen bundles density and orientation could result in sheer forces between layers (ibid). Excessive load can cause changes and result in a strong force in the tendon. This increases with age and the impact of the disease can cause degenerative changes which can reduce adaptability in the tendon. There is an unambiguous relationship between degenerative changes and increasing age [15]. Excessive load plus degenerative changes lead to variation in biology and morphology of the RC tendon (ibid). There is a relatively small body of literature that is concerned with degenerative changes in RC tendons which contained calcification, fatty infiltration, tendon thinning and vascular proliferation [16]. Moreover, in an investigation into degenerative changes, [17] found that type III collagen has been increased that could decrease the elasticity of tendon during RC injury. Extrinsic mechanisms can broadly be defined as RC tendon injury that is potentially attributed to the friction on impact with external structures. These structures contain the humeral head and coracoacromial arch. Numerous studies have attempted to explain that 95% of RC injury was caused by impingement between the coracoacromial arch and humeral head [18]. Even in normal shoulder anatomy, a series of shoulder functions such as elevation and abduction can damage the RC tendon. There are a large number of published studies that describe the link between external impingement and RCT [19,20]. It has been thought that extrinsic impingement primarily results in pathological changes near the glenohumeral joint side of the RC tendon. The causes of intrinsic and extrinsic mechanisms are different, but both of them lead to an inflammatory response. After RCT, tendon healing is commonly divided into three parts [21, 22].
Firstly, the inflammatory phase lasts for one week. During this phase, vascular permeability increases, lymph and inflammatory cells flood into the lesion site. Secondly, in the proliferative phase, the influx of inflammatory cells produces some growth factors and cytokines which result in recruitment and proliferation of fibroblasts. Finally, in the remodeling phases, fibroblasts proliferate and begin to generate, orient, deposit and interconnect than become collagen [23] has shown that intrinsic factors or extrinsic factors alone do not increase the prevalence of RCT. In total 108 mature rats were equally divided into three groups: extrinsic compression group, overuse group and a combination of overuse and extrinsic compression group. Results from the studies indicated that no significant differences were found between separate overuse or extrinsic compression and RCT. Also, a positive correlation was found between a combination of overuse and extrinsic compression and RCT. This study suggested that a combination of intrinsic factors (overuse) and extrinsic factors could increase the possibility of RCT. However, these results came from study on animals and are difficult to directly utilize in clinical conditions. This is because human beings and animals have different anatomical and biological characteristics.
The Physiological Effects of Eccentric Exercise
Eccentric exercise is a type of muscle action characterized by contraction of a muscle during its lengthening due to an external load. To determine the effect of eccentric training, [24]. carried out an experiment. This study recruited 12 young male soccer players (mean=26 years) and implemented 3 sets of heels raising eccentric training twice a day for 12 weeks. Six participants have Achilles tendinosis and others were healthy one. To evaluate collagen synthesis and degradation, blood samples were taken 1 week before and after 12-week eccentric training programme through micro dialysis technique. Pain visual analogue scale (P-VAS) also was used to assess the level of pain before and after 12-week training. There are a large number of publish studies that describe the link between carboxyterminal propertied of type I collagen (PICP) increasing in blood and type I collagen synthesis. Also, data from several sources have identified the increasing carboxyterminal telopeptide region of type I collagen (ICTP) associated with the degeneration of type I collagen [25,26]. The findings of this study showed that PICP increased significantly in the blood after 12 weeks of training in injured tendon, but not changed in healthy tendon. ICTP have no significant difference before and after study in both health and injured. Many recent studies have shown the same findings as [23] experiment [27,28]. To eliminate bias, this study carried out the same starting time (9am) and controlled the room temperature (25︒C). In injured group, the level of pain also reduced after 12 weeks training. Combining the outcomes from blood samples and P-VAS, this study could provide strong evidence to support the effectiveness of eccentric exercise. However, although the study examined plasma concentrations of PICP and ICTP, the changes of collagen type I formation could not directly be observed. Previous studies suggested that MRI or ultrasound can observe the changes in collagen type I formation [29,30]. More medical examinations should be included in further studies. Also, the population of this study is professional athletes, instead of ordinary people. It may reduce the generalizability of this study. Further studies should focus on the ordinary population and carry out more clinical examinations.
One of the most influential accounts of eccentric training came from [31]. The findings of this study demonstrated significant neovascularization after eccentric training. 22 males and 8 females with Achilles tendinopathy participated in this investigation. Ultrasonography and colored Doppler were used to examine the neovascularization in the tendon before and after intervention. Participants were asked to complete 12 weeks of knee eccentric exercise twice per day, seven days per week. The result of this study indicated that eccentric training is likely to accelerate the neovascularization. Although this study focused on patients with Achilles tendinopathy, the benefit of eccentric exercise is likely to generalize to other tendinopathies, due to the similar anatomical, physiological and pathological feature of tendinopathies [32]. However, different gender ratios (22 males and 8 females) may result in bias of experimental outcomes. Compared to women, men are more likely to regenerate new blood vessels in the tendon area after eccentric training [33]. This is due to the difference in the physiological characteristics of men and women. In addition, there is no control group in this study. Although setting a control group is not ethically permissible, a control group could reduce cointervention bias and make the experimental results more reliable and valid. A systematic review that is often cited in research on the effect of eccentric exercise is that of [34] who found that eccentric training may promote increases in tendon stiffness. This study also reported that low intensity eccentric exercise is more effective than concentric exercise for increasing a tendon’s mechanical tension. The keywords “eccentric”, “tendon” and “performance” were used in its search strategy. 40 studies were included and total of 1150 participants (406 women and 744 men) were recruited in this study. Results of this study found that, compared to concentric exercise, muscle cross-sectional area (CSA) increases significant difference after eccentric exercise. Eccentric exercise can promote more CSA synthesis than concentric exercise [35]. also identified that increasing number of CSA were beneficial for the stiffness of tendons. In addition, this study highlighted low intensity eccentric exercise was beneficial for the maximal tendon force and stress, instead of high intensity eccentric exercise. The whole design of this study is rigorous and appropriate, given proper keywords and suitable search strategy. However, this study carried out narrative analysis which cannot provide strong evidence for the findings. In addition, the study recruits healthy participants which may not demonstrate the effect of eccentric training in clinical condition. Therefore, these findings should be translated with caution into clinical scenarios. Overall, these studies provided relevant evidence that eccentric exercise promote collagen synthesis, formation of new blood vessels and increases tendon stiffness. However, further study should focus on clinical condition and more rigorous experimental design.
The Effectiveness of Eccentric Exercise
Reported [36] positive correlation between tendon repairing and supraspinatus and infraspinatus eccentric exercise. Ten middleaged (mean age=54) patients with diagnosed RCT were recruited from two health care clinics. All the patients were provided with shoulder abduction and external rotation eccentric training which involved 90 repetitions per day. Shoulder pain was assessed by visual analogue scale (VAS) after the training programme, which was believed to be valid and reliable for evaluating level of pain. According to the result of this study, VAS significantly reduced from 57 to 29. Authors attributed this improvement to healing of tendon. This hypothesis seems to be consistent with the study of [23]. which found significantly improved collagen synthesis after eccentric training. In Susanne’ s study, ten middle-aged participants indicated small sample size and low generalizability. However, compared to middle aged people, the synthesis of young people’s collagen is significantly faster [37-39]. found that insulin-like growth factors that promote collagen synthesis increased significantly among young people (mean age =25) compared with elderly people (mean age 70 years). The design of this study is a single-subject research design which is appropriate for the study condition. Therefore, the outcomes produced by middle-aged people as research participants can be accepted. [40] investigated the effectiveness of eccentric training comparing with conventional exercise in clinical RCT. 36 patients diagnosed with RCT, were recruited and randomly divided into eccentric exercise group (20) and conventional exercise group (16).
The eccentric exercise group (mean age = 50.2) performed external rotator and abduction exercises for the shoulder. The conventional exercise group (mean age = 48.9) contained shoulder shrugs and stretching exercise for the pectoralis. Both groups completed 12 weeks of daily exercise at home. 14 weeks after the training programme (26th week), the Constant Murley Score (CMS) and Pain VAS were applied for measuring shoulder function and pain. Results of this study indicated that both eccentric and conventional exercise for the RC area improve significantly in shoulder function and pain after 26 weeks. The findings from this study also shown that there is no significant difference between eccentric training and conventional training for managing shoulder pain and function after 26 weeks. This study provided 12 weeks training and follow-up after 26 weeks, giving plenty time to examine the results. However, single-blinded instead of doubleblinded controlled trial measures were implemented in this study. This may lead to experimenter bias. In addition, although different language versions of the CMS showed good reliability and validity [41, 42], this instrument needs to have established standards [43]. Therefore, this study showed that in the long term, both eccentric and conventional exercise is beneficial for middle-aged people with RCT.
There is a published study describing the role of eccentric exercise for managing RCT [44]. A total of 11 patients with diagnosed RCT and preparing for arthroscopic subacromial decompression surgery were recruited in this study. All patients were randomly divided into 3 groups: control group, concentric RC exercise group and eccentric RC exercise group. The concentric group was asked to perform shoulder abduction exercises, 3 sets of 15 repetitions twice a day from 0° to 90°. The eccentric group was asked to perform shoulder adduction exercises, 3 sets of 15 repetitions twice a day from 90° to 0°. The control group were asked to carry out standard practice without normal treatment pathway. The Oxford shoulder Score and pain Visual Analogue Scale were used to measure shoulder function and pain at the beginning, after 4 weeks and after 8 weeks. Interestingly, results from this study did not indicate any statistically significant differences between all three groups. In addition, two individuals in the eccentric group determined to cancel the surgery and continue exercise at the end of study. Compared to [37]. study, a total of 8 weeks length of this study is relatively short. It may demonstrate that longer study could result in statistically significant differences [45-47] also found that a longer follow-up period of eccentric exercise can avoid shoulder surgery. To compare with eccentric exercise and concentric exercise, further study design should extend the length of the experiment or implement a follow-up period. However, 11 patients is a small sample size which cannot provide strong evidence to support the outcomes of the study. In addition, although individual cases show significant improvement and avoid surgery after this study, this result may not be generalizable. Overall, data from this study gave no significant differences between concentric exercise and eccentric exercise on managing RCT. Moreover, short-term eccentric exercise may not have obvious therapeutic effect. Further study should collect more samples and extend experimental time.
Conclusion
Overall, the present study was designed to determine the effect of eccentric exercise. The research findings clearly indicated that eccentric exercise can promote the synthesis of type I collagen, accelerate the neovascularization and increase the integrity of a tendons. The second aim of this study was to investigate the effectiveness of eccentric exercise on RCT. Generally, the investigations have shown that, in the long term, eccentric, concentric and conventional exercise are beneficial for patients with RCT. Compared to concentric and conventional exercise, although eccentric exercise may not have obvious therapeutic effect, evidence indicated that, in the long term, eccentric exercise should be more effective in managing RCT than other treatments. However, the findings in this assignment are subject to at least three limitations. First, different gender ratio and age stage could lead to bias. Secondly, small sample size could decrease the generalizability. Finally, single examinations method and lack of randomization show that results should be interpreted with caution. Nonetheless, therapists may still select eccentric exercise or combine them with other treatment to manage RCT in clinical condition. Further investigation should increase sample size, balance gender ratio and use diverse examination methods. Also, it is necessary to determine which level of intensity of eccentric exercise is more effective in treating RCT. In addition, accurate eccentric exercise should be investigated as the RC contains four muscles.
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
14 notes
·
View notes
Text
Lupine Publishers | Resident Investigators Excel
Lupine Publishers | Orthopedics and Sports Medicine
Introduction
On September 5, 2018, the fifth iteration of the Orthopaedic Research and Education Foundation (OREF)/Orthopaedic Research Society (ORS) Southwest Region Resident Research Symposium was held in San Diego, California. The event showcased resident researchers from University of California, San Diego, Stanford University, University of California, San Francisco, Naval Medical Center San Diego, Cedars-Sinai Medical Center, the San Francisco Orthopaedic Residency Program, the University of California, Davis the University of Arizona and Loma Linda University. Papers were judged by clinical and basic science faculty members from the University of California, San Diego; Naval Medical Center San Diego; and by OREF Visiting Professor, Nicholas M. Bernthal MD, Assistant Professor in Residence, Department of Orthopaedic Surgery, University of California, Los Angeles. Hosted by Reid A. Abrams, MD, Interim Chairman and Professor, Department of Orthopaedic Surgery, University of California, San Diego, the OREF ORS Southwest Region Resident Research Symposium has continued to grow since its inception in 2009. This year, 26 residents were selected to present at the symposium. “We were impressed by the number of excellent abstracts. The winners in both the clinical and basic science categories presented impressive, high-quality research,” according to D.C. Covey, MD, the local event coordinator.
Participating residents found the event both rewarding and thought-provoking. According to Stephanie Wong, MD, “The OREF has long been dedicated to those in orthopaedics early in their careers which is underscored by the Resident Research Symposiums. The 2018 Southwest Resident Research Symposium was a well-organized conference exhibiting excellent research with renowned faculty speakers and judges. The OREF award is an important recognition of resident research. I am grateful to the OREF for its support of my research and for advancing musculoskeletal research and innovation.” Dylan Kluck, MD added that, “Having the opportunity to present this research in front of a regional conference and field questions from an impressive guest speaker was a truly inspiring experience and highlighted the role that we, even as residents, can have in advancing the orthopedic field. In particular, winning the 2nd place Clinical Science OREF award was a true honor and one of the highlights of my career thus far.” Trevor Shelton, MD, stated that, “Winning one of the research awards meant a lot as far as validating the time invested in this project and other research projects to hopefully bring forth clinically useful research.” “This award helps to advance my goal of becoming a surgeon-scientist studying novel ways to prevent muscle degeneration and fatty infiltration following rotator cuff tears,” according to Michael Davies, MD.
Congratulations to the winners!
The judges named the following winners, each of whom received an honorarium:
Basic Science
1st Place: Michael Davies MD, University of California, San Francisco. Altering Stem Cell Fate to Decrease Muscle Degeneration After Rotator Cuff Tears. Study significance:
Our group used a mouse model of rotator cuff tear to replicate the pathology seen after cuff tears in humans and to study the muscle stem cell populations that play a role in the pathogenesis of fatty infiltration. Our recent work suggests that adipogenic differentiation of fibro-adipogenic progenitors present in muscle can be inhibited by histone deacetylase inhibitors, leading to less fat both in vitro and in vivo using our injury model.
2nd Place: Mario Vargas-Vila MD PhD, University of California, San Diego. Transcriptional Profile of Supraspinatus Muscle in Rabbit Model of Rotator Cuff Tear Over Time. Study significance:
Our study aimed to better characterize muscle degeneration in rotator cuff disease. We used a rabbit model to do this at both the cellular and molecular level.
3rd Place: Derek Ju MD, Cedars-Sinai Medical Center, Electrospun Synthetic Bone Scaffold Promotes Mesenchymal Stem Cell Function and rhBMP-2 Mediated Spinal Fusion. Study significance: My research focuses on osteoinductive synthetic bone scaffolds for spinal fusion.
Clinical Science
1st Place: Stephanie Wong MD, University of California, San Francisco. Effect of Gender on Outcomes After Reverse Total Shoulder Arthroplasty. Study significance:
In this study, we showed that males achieve significantly higher SF-12 PCS and ASES function scores postoperatively compared to females. This may be attributed to differences in ADLs, especially those that require shoulder rotation. All patients experienced improvements in forward elevation and abduction, decrease in pain, and improvement in function. However, patients should be aware that shoulder arthroplasty alone may not change their shoulder rotation. Addressing gender differences in outcomes after surgery will further our understanding of how musculoskeletal conditions affect males and females differently and would help optimize evaluation and treatment of orthopaedic conditions.
2nd Place: Dylan Kluck MD, University of California, San Diego. A Novel 3D Parameter Can Guide Concave Rod Contour for the Correction of Lost Kyphosis in Adolescent Idiopathic Scoliosis. Study significance:
“As part of my UCSD research year I was fortunate enough to work in Dr. Peter Newton’s lab at Rady Children’s Hospital where I was involved in several projects centering primarily around adolescent idiopathic scoliosis. As part of his lab I worked on a longstanding project analyzing intra-op rod contours during posterior spinal fusion to quantify the ideal amount of rod contour required to achieve a desired amount of surgical correction. During my research year, our biomechanical engineer was instrumental in identifying a new 3D parameter which we found to strongly correlate with restoration of thoracic kyphosis. Using 3D spinal reconstructions, this parameter represents an exciting step in being able to estimate a starting point for ideal rod contour.
3rd Place: Trevor Shelton MD, University of California, Davis. ACL Graft with Hamstring Tendons: Optimal Location for Pre- Operative MRI Measurement of Cross Sectional Area. Study significance:
The goal of my research project was to determine where along the hamstring tendons had the best correlation to intraoperative graft size for autograft hamstring ACL reconstruction. Using this, we created a model to predict whether hamstring autograft would be of sufficient size for ACL reconstruction.
For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin https://www.linkedin.com/company/lupinepublishers Follow on Twitter : https://twitter.com/lupine_online
#lupine publishers#Lupine indexing site#OSMOAJ#Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)#orthopedics and sports medicine open access journal
9 notes
·
View notes
Text
Lupine Publishers | Radiographic Accuracy in Scaphoid Waist Fractures

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Objectives: We compared CT scanning and radiographic imaging to determine the relationship between measurements of displacement and angulation of the fracture.
Design: X-ray review.
Methods: All patients with acute scaphoid fractures treated at our hospital in a 4-year period that had a CT scan and plain radiographs were evaluated. The maximum displacement seen on either AP or lateral X-rays was measured as well as the amount of palmar flexion through the fracture as seen on the lateral X-ray. The differences were calculated and the mean of the sum of the differences was calculated.
Results: 103 patients radiographic files were evaluated and 43 were found to have CT scans through the longitudinal axis of the scaphoid as well as AP and lateral plain radiographs taken within one week of the CT in acute fractures. The average displacement seen on the CT was 1.85mm with an average of 50.9 degrees of palmar flexion through the fracture. The average displacement and angulation on the plain radiographs were .93mm and 33.2 degrees respectively. The mean difference in displacement and angulation between the CT scan and plain radiographs was 1.39mm (p=0.003) and 17.9 degrees (p=0.013) respectively. These were statistically significant using paired t-test comparison.
Conclusion: We believe that the accurate assessment of scaphoid fractures is essential to ensure the most appropriate treatment is rendered. We feel that CT scanning should be used to evaluate all acute scaphoid fractures to ensure that the most reliable determination of displacement can be made, and the most effective treatment rendered.
Introduction
Radiographs are routinely used to diagnose and evaluate scaphoid fracture displacement and angulation [1-9]. The amount of angulation and displacement is used to determine whether or not a patient would benefit from non-operative or operative management [10-12]. The accuracy of plain radiographs is often taken for granted and has not been validated with other imaging modalities that are more accurately utilized for fracture displacement and angulation. We compared CT scanning and radiographic imaging to determine the relationship between measurements.
Materials and Methods
All patients with acute scaphoid fractures treated at our hospital over a 4-year period that had a CT scan and plain radiographs were evaluated. The maximum displacement and angulation of the scaphoid fracture was measured in the sagittal plane (Figure 1) using the dorsal cortical angle (Figure 2) [13,14]. The maximum displacement seen on either AP or lateral X-rays was measured as well as the amount of palmar flexion through the fracture as seen on the lateral X-ray. The differences were calculated and the mean of the sum of the differences was calculated.
Results
103 patients’ radiographic files were evaluated and 43 were found to have CT scans through the longitudinal axis of the scaphoid as well as AP and lateral plain radiographs taken within one week of the CT in acute fractures. The average displacement seen on the CT was 1.85mm with an average of 50.9 degrees of palmar flexion through the fracture. The average displacement and angulation on the plain radiographs were .93mm and 33.2 degrees respectively. The mean difference in displacement and angulation between the CT scan and plain radiographs was 1.39mm (p=0.003) and 17.9 degrees (p=0.013) respectively. These were statistically significant using paired t-test comparison.
Discussion
Scaphoid fractures are one of the most troublesome injuries about the wrist. The propensity for suboptimal outcomes with these injuries should make the treating physician particularly suspicious when dealing with wrist injuries that may involve the scaphoid. Radiographic determination of displacement and angulation of scaphoid fractures is quite difficult at times. Displacement and angulation of 1mm and 60-70 degrees is generally accepted as indications for operative stabilization of scaphoid fractures [15,16]. Hence, it is extremely important to evaluate the scaphoid using the most accurate modality available.
Conclusion
In our series of patients, we have found a significant discrepancy in the amount of displacement and angulation between plain X-rays and CT scanning. Based on this data we recommend CT scanning for all scaphoid fractures that have displacement and angulation. The CT scan will better delineate the fracture characteristics and facilitate pre-operative planning.
For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/ For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin https://www.linkedin.com/company/lupinepublishers Follow on Twitter : https://twitter.com/lupine_online
#Lupine indexing site#lupine publishers#Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)#OSMOAJ
6 notes
·
View notes
Text
Lupine Publishers | Addition of mannitol to hyaluronic acid enhances the inhibition of matrix metalloprotease expression in IL-1β stimulated human C-20/A4 chondrocytes Volume 4 - Issue 2

Lupine Publishers | Orthopedics and Sports Medicine
Introduction
Osteoarthritis (OA) of the knee and hip is ranked as the 11th leading raison of disability and its prevalence keeps going up over the last past decades [1]. In the United States, over 9 million people suffer from symptomatic knee OA [2]. One third of adults over the age of 60 have radiographic evidence of this condition and 12.1% experience pain and/or disability [3]. Despite the high prevalence of knee OA and the high level of disability related to the disease progression, only few patients undergo joint replacement with a mean time from symptoms onset to Total Knee Replacement (TKR) of about 19 years [3,4]. Such a long evolution explains the huge need of new non-surgical therapies, which can alleviate pain and improve the quality of life with a better effectiveness than the current therapeutic modalities. The therapeutic approach of knee OA is based on the combination of non-pharmacological and pharmacological modalities, widely described in multiple guidelines [5-7]. Among the pharmacological modalities, Intra-Articular (IA) injections of hyaluronic acid (HA), also named Viscosupplementation (VS), have been ranked as the most effective treatment for alleviating knee OA pain [8], despite some controversies remain regarding the interpretation of the meta-analyses [9-12]. Hyaluronic acid is a non sulfated High Molecular Weight (HMW) glycosaminoglycan naturally present in ECM and synovial fluid that plays a major role in cartilage lubrication [13,14]. The HA lubricating properties explain that HA injections for treatment of OA are classified by the majority of health agencies worldwide, as a medical device but not as a drug. However, it has been now well evidenced that IA HA has also multiple pharmacological effects on molecular signaling pathways and contributes to the joint homeostasis. The multiple mechanisms by which HA may act as an anti-inflammatory and a structure-modifying drug for OA have been developed in a recent review [15]. Inflammation plays a central role in the development and progression of OA. Multiple pro-inflammatory cytokines are involved in the pathogenesis of the disease, especially interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF)-α, which play key roles in the extra cellular matrix (ECM) breakdown. IL-1β and TNF-α, produced by chondrocytes, synoviocytes, mononuclear cells and even osteoblasts, stimulate matrix metalloproteinases (MMPs) and a disintegrin and metalloproteinase with thrombospondin motifs (ADAMTS) [16] synthesis and activity. Furthermore IL-1β stimulates Nitric Oxide (NO) synthesis and oxygen free radicals production that increases the damaging effects on cartilage [17]. The ECM degradation and particularly that of its two major components, aggrecan and type 2 collagen, is mainly due to MMP-1, -3, -9, and -13, and ADAMTs 4 and 5. Hyaluronidase and Reactive Oxygen Species (ROS) degrade HA macromolecules, leading to increased levels of HA fragments of low molecular weight with pro-inflammatory properties that worsen again the inflammatory cascade [15]. The important role of oxidative stress resulting from chronic overproduction of ROS is often underestimated. Oxygen free radicals damage DNA, increase cell apoptosis, contribute to degradation of the ECM and inhibit proteoglycans synthesis [18]. The NADPH oxidase enzymes constitute a large enzyme family which function is dedicated to the production of reactive oxygen species (ROS). One of our recent work showed that the NADPPH oxidase 4 (Nox4) is the major source of ROS production in human chondrocytes and in the C-20/A4 human chondrocyte cell line [19,20] in which Nox4-derived ROS regulate collagenase 1 (MMP-1) expression and chondrocyte death consecutive to IL-1β stimulation. Interestingly a number of hydroxyl rich polysaccharides, such as HA, have also antioxidant properties and are themselves inhibitors of oxygen free radical −O2* , underlining the importance of HA concentration [21]. However HA is also very sensitive to oxidative stress [22]. HA macromolecules, containing many OH groups, react with ROS, resulting in the rupture of the macromolecular chains and accelerated degradation of the highly viscous solution. The rapid depolymerisation of HA is a major reason for the short intraarticular half-life of viscosupplements made of non-cross-linked HA, cross-linking being another way to protect HA from degradation by ROS [21]. Several studies have shown that the addition of a polyol with ROS scavenging properties, such as mannitol or sorbitol, protect HA from ROS degradation [21-24]. Safety and efficacy of a mannitol-modified HA viscosupplement, HANOX-M, has been assessed in a large scale multicenter, prospective doubleblind controlled trial [25] in patients with knee OA. The study demonstrated that HANOX-M was as safe and effective than a high molecular weight HA viscosupplément not containing mannitol, but with a more rapid onset of action than that of the latter [26]. Due to the antioxidant effect of mannitol we hypothesized that, besides its better resistance to degradation, the mannitol-modified HA might have a more pronounced effect than HA alone on inflammation and MMPs related ECM degradation. The aim of the study was to compare in vitro the effect of the addition of mannitol to HA versus HA alone on the level of ROS production and the NOX-4 and MMPs expression upon IL-1β stimulation.
Materiel and Methods
Material
Human C-20/A4 chondrocyte cell line immortalized by SV40 is a generous gift from Dr M.B. Goldring (Harvard Institute of Medicine, Boston, MA, USA). HEK293 Nox4 T-Rex™ cells were kindly provided by PATIM laboratory, Pr KH. Krause (Geneva University, Switzerland). Dulbecco’s modified Eagle’s medium (DMEM), fetal bovine serum (FBS) and geneticin (G418) were purchased from life technologies (Saint Aubin, France); blasticidin was from Funakoshi Co (Tokyo, Japan); complete mini EDTA-free protease inhibitor EASYpack, Na4P2O7, Na3VO4, PMSF, luminol, Horseradish Peroxidase (HRPO), Triton X-100, were purchased from SIGMA (Saint Quentin Fallavier, France) ; leupeptin, pepstatin, trypsin inhibitor, TLCK and human interleukin-1β were purchased from Roche (Meylan, France) ; Diisopropylfluoro-phosphate (DFP) was purchased from Acros Organics (Halluin, France); Pro-MMP1 monoclonal antibody was obtained from R&D Systems (Lille, France); rabbit polyclonal antibodies directed against ADAMTS5 (RP1-ADAMTS5) were respectively from Biovalley (Illkirch, France) and Abcam (Paris, France).
Hyaluronic Acid Products
The viscosupplement to be studied was HAnox-M (HAppyVisc®, LABRHA SAS, Lyon, France), a solution made of an intermediate MW (1-1.5MDa) HA of non-animal origin, in a concentration of 1.55 mg/ml, combined with mannitol, concentrated at 35 mg/ml. The comparator was HA1% (Go On ®, Meda Pharma, Solna,Sweden), solution of an intermediate MW (1-1.5 MDa) of non-animal origin, in a 10 mg/ml concentration.
Cell culture
C-20/A4 chondrocytes and HEK293 T-Rex™ were cultured in DMEM containing 4.5 g/L glucose and 0.11 g/L sodium pyruvate, supplemented with 10% (v/v) fetal bovine serum, 100 units/ml penicillin, 100 mg/ml streptomycin and 2 mM glutamine at 37°C in atmosphere containing 5% CO2. Selecting antibiotics, blasticidin (5μg/ml) and geneticine (400μg/ml) were used for HEK293 Nox4 T-Rex™ cells. Expression of Nox4 by HEK293 Nox4 T-Rex™ cells were induced by the addition of 1 μg/ml tetracycline in the culture media [26]. All experiments were performed within cell passages 3 to 10 at 60-90% confluence. Cells were incubated in presence of HANOX-M or HA 1%e with a final concentration of 1.25 mg/ml hyaluronic acid. Cells were stimulated or not with 2ng/ml IL-1β during 48h for RT-PCR or 24h for ROS production evaluation.
Evaluation of ROS Production
Expression of Nox4 by HEK293 Nox4 T-Rex™ cells were induced by the addition of 1 μg/ml tetracycline in the culture media for 24 hours. Cells were then detached with 0.25 % (w/v) trypsin, washed twice with PBS and collected after 8 min centrifugation at 400 g at room temperature. The viability of the suspended cells was over 95%, as determined by the trypan blue exclusion method. In a 96- well plate, 5x105 living cells resuspended in 20 μl PBS were added per well. Before the start of the assay, 100 μl of a PBS solution containing 5 μM Amplex Red and 10 mUnits/ml horseradish peroxidase was added in each well. Results are expressed as the sum of Relative Fluorescent Units (RFU) recorded every two minutes during 60 min on a fluostar omega spectrofluorimeter (BMG labtech).
RNA Extraction and RT-q-PCR
Total RNA extraction was performed with NucleoSpin® RNA (Macherey Nagel, Hoerd, France) following recommendations. cDNA was reverse transcribed from 1 μg of total RNA with the SuperScriptIII First-Strand Synthesis (Life Technologies, Carlsbad, CA). As recommended an RNase H treatment was added. Real time RT-qPCR was conducted using the QuantiTect SYBR Green RT-PCR kit (Qiagen) and a Stratagene Mx3005P (La Jolla, CA). Briefly, the transcript expression levels of human IL-1β, CYBA, NOX4, HMOX1, MMP-1, MMP-13, ADAMTS4 and housekeeping genes GAPDH, RPL27 and RPL32 were determined using specific primers chosen to include intron spanning. Gene expression was quantified using the comparative threshold cycle (Ct) method. The amount of target gene, normalized to three endogenous reference genes (RPL27, RPL32 and GAPDH) was expressed relative to the control cells. The specificity of the PCR products was confirmed by gel electrophoresis migration and a by melting curve analysis.
Statistical Analysis
Data are presented as means +/- SD, significance levels were assessed using Student’s paired t test. A p-value of 0.05 or less between groups was considered to indicate a statistically significant difference.
All quantitative data were generated using biological replicates in triplicate unless stated otherwise and are expressed as the mean plus 95% confidence interval. Data normality was tested by a Shapiro-Wilk test. For each experiment, p-values were determined using a paired Student test. All analyses were conducted using StatView (SAS institute, US).
Results
Differential Impact Of HANOX-M And HA 1% On NADPH Oxidase Activity In HEK293 T-REX™ Cells
When HANOX-M or HA 1%, at a final concentration of 1.25 mg/ ml of HA, were added to the cells right before the ROS production measurement, or 24 hours before ROS measurement, no significant impact on Nox4 activity was noticeable, showing that the two viscosupplement compounds do not exert direct antioxidant properties.(Data not shown)
Effect Of HANOX-M And HA 1% On Nox4 Expression In Human Chondrocyte Cell Line C20/A4
As expected, IL-1β-stimulated C-20/A4 chondrocyte cell line increase Nox4 expression, determined by quantitative PCR. Despite a non-statistically significant difference, HANOX-M tended to better inhibit Nox4 expression than HA 1% (Figure 1).
Figure 1: NOX-4 expression in non-stimulated (NS) and IL-1β-stimulated HEK 293 Nox4™ cells, after incubation with HANOX-M or HA1%.
Effect of HANOX-M and HA 1% on MMPs expression in human chondrocyte cell line C20/A4
Figures 2, 3, 4 Quantitative RT-PCR showed that treatment with HANOX-M inhibits the effect of stimulation by IL1β on the increase in expression of MMP13 and ADAMTs4. Treatment with HA1%, on the other hand, cannot prevent the increase in transcripts encoding the two metalloproteases MMP13 and ADAMTs4.
The effect of stimulation by IL1β on the increase in expression of MMP1 was completely inhibited by the two treatments, HANOX-M and HA1% (Figure 4).
Figure 2: Collagenase MMP13 expression in non-stimulated (NS) and IL-1β-stimulated C20/A4 chondrocytes, after incubation with HANOX-M or HA1%.
Discussion
It has become increasingly apparent that HA has the capacity not only to alleviate pain but also to protect and restore the chondral matrix via multiple molecular pathways [15]. Therefore it is legitimate to consider HA not only as a pain-killer but as a background therapy for OA with structure-modifying properties. The development of novel HA viscosupplements with chondroprotective effects, especially for treating early OA, is a exciting challenge. Henrotin et al. (27) reported the results of a randomized double-blind placebo controlled trial showing that a single IA injection of HANOX-M-XL, a crosslinked HA combined with mannitol, can reduce the serum levels of Coll2-1, a marker specific of type II collagen degradation, in patients with knee OA. This finding suggests that HANOX-M-XL may have a beneficial effect on cartilage degradation.The present study compared the effects of HANOX-M, a non-crosslinked 2nd generation viscosupplement [28], containing 35 mg/ml of mannitol, to a regular HA 1% viscosupplement. It suggested that HANOX-M might have a positive therapeutic effect on the expression of the transcripts coding for the metalloproteinases MMP1, MMP13 and ADAMTs4, while HA1% exhibited a positive effect only on the expression of MMP1. HANOX-M also tended to better inhibit Nox4 expression than HA 1%, despite a non-statistically significant between-treatment difference. The mechanisms by which mannitol exerts its beneficial effect on OA are not fully understood. It has been published [29] that a combination of HA and sorbitol, a mannitol isomer, prevented IL- 1β-induced oxidative stress, p47-NADPH oxidase phosphorylation, 4-hydroxynonenal (HNE) production and HNE-metabolizing glutathione-S-transferase A4-4 expression. Furthermore, HA + sorbitol inhibited IL-1β-induced MMP-13, nitric oxide (NO) and prostaglandin E2 release and NO synthase expression, by acting on the nuclear factor-kappa B (NFKB) pathway. Obviously, our data do not allow us to extrapolate these in vitro results to claim a chondroprotective effect of HANOX-M, in vivo.
Conclusion
This in vitro study suggests that combining high concentration of mannitol with HA may have a positive therapeutic effect on the expression of the transcripts coding for the metalloproteases MMP1, MMP13 and ADAMTs4. Treatment with HA alone has a potentially therapeutic effect only on the expression of MMP1. HANOX-M might be useful as a first line treatment to treat chondropathy and early OA, thanks to its potential structure-modifying effect
For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/ For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
To Know More About Open Access Publishers Please Click on Lupine Publishers Follow on Linkedin https://www.linkedin.com/company/lupinepublishersFollow on Twitter : https://twitter.com/lupine_online
9 notes
·
View notes
Text
Lupine Publishers | Neglected Posterior Shoulder Dislocation with a Large Bone Defect in a young Active Patient Treated with Osteochondral Allograft

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Background: Posterior glenohumeral joint dislocation is a rare injury. Despite positive clinical signs is often underdiagnosed and undertreated. The presence of a large bone humeral defect could worsen the outcome.
Case Report: We report a case of 45 years-old man with a neglected posterior shoulder dislocation with a large segmental bone defect involving 40% of the articular surface of the humeral head. We decided to treat the patient with an open reduction of the shoulder dislocation and reconstruction of the articular surface with fresh-frozen humeral head allograft. Our patient showed improved shoulder mobility and ROM on all planes that positively affected the patient daily activities; no pain was registered at follow-ups.
Conclusion: Our case report demonstrates that neglected posterior shoulder dislocations with a large bone defect and viable humeral head can be treated using allograft, obtaining optimal clinical results and avoiding the need for early prosthetic replacement surgery.
Keywords: Neglected Posterior Shoulder Dislocation; Reverse Hill-Sachs Lesion; High-Demand Patient; Humeral Head Allograft; Anatomic Shoulder Restoration
Abbreviations: GHJ: Glenohumeral Joint; MRI: Magnetic Resonance Imaging; MVA: Motor Vehicle Accident; LHB: Long Head Of Biceps Brachii; XR: X-Rays
Introduction
Posterior glenohumeral joint (GHJ) dislocation is a rare injury and accounts for only 2% to 5% of all dislocations of the shoulder [1]. GHJ posterior dislocation has a prevalence of 1.1 per 100,000 inhabitants per year, with the first peak in male patients aged between 20-49 years old, and the second one in the elderly over the age of seventy [2]. Posterior shoulder dislocation is often underdiagnosed and undertreated in up to 50% of cases admitted to the E.R. [3]. A dislocation is defined chronic when left untreated for more than 3 weeks. Diagnosis of posterior GHJ dislocations is often delayed, becoming chronic and leading to a locked joint and decreased functional outcome [4]. Typically, posterior shoulder dislocation can be traumatic or atraumatic: the first might be due to direct high-energy trauma or it can also develop insidiously through a repetitive minor injury. A major trauma with a force applied to the arm with the shoulder in adduction, flexion and internal rotation is the most frequent cause (e.g. A direct blow to the anterior shoulder or by a fall on a forward-flexed upper limb)[5]. On the other hand, seizures and electrocution are the major causes of atraumatic dislocations, by contraction of the internal rotators and disruption of the joint static and dynamic posterior stabilizers [1]. Associated injuries include humeral neck or tuberosity fractures, impaction fractures of the anterior humeral head (i.e. reverse Hill–Sachs lesion), posterior labrum capsular complex lesions (i.e. reverse Bankart lesion) and rotator cuff tears [2, 6]. Reverse Hill-Sachs lesions can be associated with posterior GHJ dislocation in up to 86% of cases, requiring open or arthroscopic surgical therapy [1, 7, 8].
Missed, late or incorrect diagnosis is a significant clinical problem, as it can predispose to serious complications, such as chronic instability, osteonecrosis, post-traumatic osteoarthritis, persistent joint stiffness and functional instability [4, 8]. Treatment management of chronic posterior shoulder dislocation associated with a large articular defect is strongly debated due to lack of studies with significant clinical records: operative treatment is usually preferred based on the type and the extension of injury, age, medical history and functional demand of the patient. The patient gave consent for case report.
Case Report
A 45-year-old deaf man, involved in an MVA, sustained a direct blunt trauma to his dominant right shoulder. The patient was employed as a warehouse worker. At the time of the accident, he has been admitted to the ER of another hospital where he has been discharged with the diagnosis of “right shoulder contusion”. The patient was admitted to our clinic three months after the trauma, complaining severe pain and functional limitation of the right shoulder. At physical examination the patient showed functional limitation of the shoulder motion on all planes, in particular: abduction 30°, flexion 30°, internal rotation at the iliac spine, external rotation 0°. At palpation the shoulder was painful. The patient was neurovascular intact. X-Ray and CT scan were carried out, showing posterior GHJ dislocation with an osteocartilagineous lesion about 40% of the humeral head surface, localized on its antero-medial edge (a reverse Hill-Sachs lesion; type I according to Randelli’s classification of posterior shoulder dislocation) (Figure 1) [9]. Based on clinical (i.e. not reducible dislocation after conservative treatment) and radiological evaluation (i.e. complete dislocation of the shoulder with important bone loss of the humeral head), the patient was subsequently scheduled for surgery. Considering the young age of the patient, his high functional demand and the extension of the lesion, we decided to perform a humeral head allograft reconstruction. We requested it to the bone bank communicating the size of the humerus of the patient to obtain the best matching allograft. The procedure was performed under general anaesthesia with the patient placed in a beach-chair position. A deltopectoral approach was used with release of the pectoralis major tendon insertion to improve the exposure of the surgical field. After finding and isolating the anterior humeral circumflex artery and vein, the subscapularis tendon was exposed and cut through its insertion. After detaching the subscapularis muscle from the lesser tuberosity, as the long head of biceps brachii (LHB) tendon tended to dislocate from the bicipital groove we decided to tenotomize it. We proceeded to perform lysis of the posterior adhesions and then the posteriorly dislocated locked humeral head was gently reduced with the aid of a Schanz pin inserted in the lateral aspect of the humeral shaft used as a joystick. Subsequently a large 40% reverse Hill–Sachs lesion was exposed. With an appropriate burr, an accurate regularization of the Hill-Sachs lesion was made, obtaining a viable bony surface. The fresh-frozen humeral allograft was then carefully prepared aside to obtain an anatomic restoration of the cephalic anatomy. The size-matched osteocartilaginous allograft was press-fit into the humeral defect and fixed with 3 4.0mm lag screws reaching a stable construct – (Figure 3). The subscapularis tendon was reinserted by two anchors (JuggerKnot® SoftAnchor - 2.9 mm, Zimmer-Biomet, Jacksonville, FL, USA), (ALLthread™ Suture Anchor – 5mm Zimmer-Biomet, Jacksonville, FL, USA), on his anatomical site. The LHB was sutured on the pectoralis major tendon with non-absorbable suture. The arm was kept in a 30° of abduction and 30° of external rotation using a shoulder brace for 4 weeks post-operatively. Passive range of motion was started at 4 weeks following surgery and active range of movement was started 6 weeks post-operatively. A shoulder CT scan was performed at 1-year follow-up showing no signs of allograft bone resorption, screw loosening or avascular necrosis (Figure 4 A-B). Also 1 year after surgery the patient reported no painful symptoms showing excellent ROM on all planes (Figure 5 A-D); he was able to perform normal daily and work-related activities. A 95 points Constant- Murley Score was recorded at this time.
Discussion
The aim of this paper is to present the clinical results using a fresh-frozen osteochondral humeral head allograft in a young active patient affected by a chronic GHJ dislocation with reverse Hill-Sachs lesions about 40%. Scientific literature shows scarce consensus about the treatment of this rare injury: there is an ongoing debate about the different treatment options. Moreover there is not an agreement on the best allograft that has to be used. The reverse Hill-Sachs lesion size is the most influencing factor for choosing the type of treatment [3]. The reverse Hill-Sachs (also called McLaughlin lesion) is a wedge-shaped impaction fracture on the antero-medial aspect of the humeral head [7]. Any significant lesion should be treated operatively [8]. According to Guehring et al., for defects involving less than 25% of the articular surface closed reduction is the first choice of treatment; patients with unstable joints and bone defects >25% could benefit of operative treatment, with arthroplasty being recommended if the bone defect is >40% [9,10]. For defects between 25% and 40% a plethora of treatment modalities can be adopted including the classical or the modified McLaughlin technique, bone grafts, etc. [11.12]. In our patient, we opted for a humeral head allograft to obtain an anatomic restoration. We preferred this procedure to non-anatomic procedures as subscapularis tendon transfer (i.e. classic McLaughlin) or the lesser tuberosity transfer (i.e. modified McLaughlin) because, according to authors, a non-anatomic restoration of the humeral head sphericity can lead to a decreased internal rotation of the shoulder and can complicate a foreseeable prosthetic reconstruction [3, 4, 5]. Our patient had borderline indications for hemiarthroplasty. Considering his relatively young age and global clinical assessment, we decided to perform an allograft procedure to respect the patient’s high functional demand of the affected limb. Furthermore, we agree with authors which alert on the difficulty to manage the moderate-sized Hill Sachs lesions (i.e. sizing between 40-55%), even for experienced shoulder surgeons: young and middle-aged individuals with high functional demand can benefit of a delay in the hemiarthroplasty surgery by preserving the sphericity of the humeral head [6]. Concerning the graft type, most literature focus on cancellous allograft or autograft to treat acute posterior shoulder dislocation. These grafts are used as a void filler after lifting off the previous impacted articular surface to better stabilized the lesion gap and promote bone healing [1]. For defect between 25% and 40% some authors report reconstruction of the articular surface with fresh-frozen osteochondral allograft [1, 5, 13, 22, 23]. No specific guideline has been proposed for the choice of the allograft. Some authors used a fresh-frozen femoral head allograft. In particular, authors report good functional outcomes using a femoral head allograft for treating locked chronic posterior shoulder dislocation in patients having 25-50% articular surface bony defects [5,13]. The same good results are described in a case report by Patrizio et al. [22]. The most frequent possible complications recorded with this procedure are graft resorption, articular surface flattening and arthritis [5, 13]. Other authors. Proposed the use of a fresh-frozen talus allograft in case of limited accessibility of humeral head graft. They described a similar congruency between the radii of curvature observed with the taller dome and with the humeral head, allowing for application to broader category of patients [23]. The use of fresh-frozen humeral head allograft has been described by Martinez et al. in 5 patients affected by GHJ instability after posterior GH dislocation and in 1 patient with chronic GH dislocation. All patients had a 40% humeral defect. The study had a follow-up period of 10 years; 4 patients had satisfying outcomes while 2 suffered collapsing of the graft [1]. When comparing our case with the aforementioned paper, we obtained from the bone bank an accurate sized humerus matching the patient’s one. By doing so we were able to better fill the gap and restore the precise curvature of the humeral head of the patient, rather than with the use of femoral head, achieving an anatomical restoration. By filling the defect using a humeral head allograft we aimed at preserving both shoulder stability and function, while maintaining the integrity of anatomic soft tissue attachments and preserving the remaining articular surface. Our case report showed how operative treatment options must be patient-targeted according to each intrinsic factors (e.g. age, functional demand, comorbidities, etc.), to the type of injury (e.g. extension of bone defects) and its severity [14, 15]. Our patient had a high functional demand influencing his work-related activities and reported consistent pain for up to three months. Patients with posterior GHJ dislocation suffer a diagnosis delay and often report aspecific symptoms during healthcare evaluation [16, 17]. Our patient as well had aspecific symptoms; apart from significant pain and loss of motion, patients with chronic GHJ dislocation may show shoulder muscle atrophy and prominent acromion on the opposite side, while the dislodged humeral head can be palpated on the back of the shoulder [18]. XR findings can mislead clinicians as the AP view could show no sign of posterior GHJ dislocation: axillary-lateral or Y views (hard to obtain if consistent pain is present), CT scan and/or, as in our case, an MRI can unmask the dislocation [7, 19]. Diagnosis delay pivots the treatment: in a case series study it is highlighted how patients promptly treated for acute dislocation have a better outcome and are easier to treat [20]. During follow-up, our patient has undergone rehabilitation therapy; post-operative recovery consists of strengthening exercise neuromuscular re-education, while educating the patients to avoid flexion, adduction and internal rotation movements [19, 21]. We acknowledge the limitations of this paper due to limited follow-up.
Conclusion
Posterior GHJ dislocation greatly benefits early diagnosis. If a reverse Hill-Sachs lesion is associated, there is the need of standardized treatment protocols for management of this condition. An important limit we faced when searching the literature is the paucity of studies with a large number of cases treating GHJ dislocation with a reverse Hill-Sachs lesion: we strongly recommend for future studies to unveil possible benefits and limitations, especially involving the benefits of bone grafts. We want to emphasize the importance of preserving the GHJ anatomy in the young, active patient by delaying prosthetic replacement only once necessary. We want to point out how, even if the graft procedure fails there is still the possibility to proceed with a salvage procedure (i.e. prosthetic replacement), that will be found easier to perform over a preserved humeral head anatomy.
For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
6 notes
·
View notes
Text
Femoral Shaft Fractures in Pediatric Age: Treatment Strategies and ResultsLupine Publishers |

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Purpose: Femoral shaft fractures represent 1.4-1.7% of all fractures in the pediatric population and may be associated with significant morbidity. The purposes of this study are to verify if increasing age and weight are predictive factors of associated injuries and complications in children with femoral shaft fractures.
Methods: Retrospective study, including patients with age below 16 years old, admitted in our Department between 2011- 2015, with the diagnosis of femoral shaft fracture. Patient demographics, fracture characteristics, associated injuries, treatment methods, time to union, follow-up and complications were collected from the medical records. Statistical significance was set for level of p<0.05.
Results: Sixty patients were included. There was a male predominance [n=40]. Age at the time of injury was 6.3±4.9years old. The 61 femoral shaft fractures: observed affected different areas: 12-proximal; 43-middle; 6-distal. The most common etiology was direct trauma after a fall and traffic accident. Associated lesions were found to be significantly higher in older (p=0.01) and heavier (p=0.009) patients. Conservative treatment was the option for 62% of all fractures. The minimum age to surgery was 6 years old and rigid trochanteric entry nailing was only considered above 10 years old. Patients treated conservatively had a significant lower weight (16.4±8.4Kg) than those operated on (42.5±13.8Kg) [p<0.001]. Mean follow-up time was 50.4±56.8weeks and complications were reported in 15% of patients. We did not verify any statistically significant differences between post treatment complications and the treatment method (p=0.803).
Conclusions: The age, weight and associated lesions were considered significant factors when choosing the treatment method.
Keywords: Pediatric Femur Shaft Fracture; Age; Weight: Associated Injuries; Complications
Introduction
Fractures affect 10%-25% of children sustaining a musculoskeletal injury [1]. Different risk factors have been reported, such as age, sex, season, risk-taking behavior, bone mineral density (BMD), sports, but also violence, ethnicity and socioeconomic status [2-7]. Overweight and obesity seem to increase the fracture risk [8- 10], likely due to lower bone mass relative to body size and greater mechanical load caused by falls or reduced body balance [4-13]. Femoral shaft fractures are among the most common major injuries in pediatric age representing 1.4-1.7% of all fractures in pediatric population [14-16]. The etiology of the injury includes falls, motor vehicle accidents, sports injuries and child abuse. Non-accidental injury has been reported as the leading cause of femur fractures in children less than 1 year old [17-19] and the AAOS recommends that children younger than 36 months with a diaphyseal femur fracture should be evaluated for child abuse [20]. The ideal treatment for a pediatric diaphyseal femur fracture is highly dependent upon age and size of the child but it should also consider weight, associated injuries, fracture pattern and mechanism of lesion [14- 22]. The treatment should focus on getting the fracture to heal in an adequate alignment according to age, avoiding complications such as nonunion, delayed union, angular or rotational deformities, limb length discrepancy, infection, neurovascular injury, disruption of the growth plate, muscle weakness, and/or compartment syndrome [21]. At the same time, the treatment should also be comfortable for the patient and convenient for the family, causing the least negative psychological and socioeconomical impact [23].
Femoral shaft fractures are one of the most common pediatric orthopedic injury requiring hospitalization. Casting with or without preceding traction has been the mainstay of treatment in the past, leading to healing and remodeling with good long-term outcomes [14-25]. However, in the last decades there has been a gradual shift towards operative treatment in order to achieve a quicker recovery, shorter rehabilitation time and, simultaneously reducing the morbidity associated with prolonged immobilization [14-26]. With the development of age-adequate fixation devices, several different procedures are available for stabilization of femoral shaft fractures in children, such as external fixators, submuscular plates, rigid intramedullary nails and flexible intramedullary nails [14- 23]. Age, weight, fracture personality and skeletal maturity are key factors in guiding treatment options in our institution. Usually, with advancing age and skeletal maturity, acceptable values for angulation and shortening of the fracture decrease, as there is less potential for remodeling. For patients from birth to 2 years, up to 30° of angulation in all planes and 20mm of shortening can be accepted. In patients aged 2 to 5 years one can accept up to 15° of Varus/valgus, 20° of anterior/posterior angulation and 15mm of shortening. In patients from 6 to 10 years, it is acceptable 10° of Varus/valgus, 15° of anterior/posterior and 15mm of shortening. For patients older than 11 years of age, the surgeon can only allow 5° of Varus/valgus, 10° of anterior/posterior of angulation and up to 10mm of shortening [27].
Nonoperative treatment is mainly indicated for children under 5-6 years of age and options include Pavlik harness, early traction (skin and/or skeletal) with delayed Spica casting, and early fracture manipulation with Spica casting [14-28]. Pavlik harness use is indicated for patients less than 6 months old [20]. Early closed reduction and hip Spica cast has become the primary treatment for patients between the age of 6 months and 5 years, with less than 2cm of fracture shortening. Isolated traction is still an option for management, although less popular nowadays [20]. If, during the treatment, the fracture shortening increases beyond 2cm, a change in the treatment plan must be considered [20].
Operative treatment is usually reserved for children over the age of 5 or 6 years, but must be considered whenever there is unacceptable deformity, polytrauma, open fracture, neurovascular injury, pathologic fracture or body habitus not amenable to casting [28]. Surgical treatment should be considered when conservative treatment fails or there are associated head injury or multiple injuries [14-23]. Operative stabilization and fixation options, include flexible/elastic intramedullary nailing, rigid intramedullary nailing, internal plate fixation and external fixation. The use of flexible/elastic nails is indicated to treat children age 5 to 11 years old weighing less than 49Kg [20-29]. Flexible interlocking intramedullary nailing (FIIN) is an option for patients between 5 and 11 years of age weighing more than 45.5Kg, but too skeletally immature for rigid nailing [28-30]. Rigid intramedullary nailing and submuscular plating are options for patients older than 11 years old with diaphyseal femur fractures. Trochanteric entry point should be used in antegrade rigid nailing and piriformis or near piriformis entry should be avoided because of the risk of osteonecrosis of the femoral head or growth plate disturbances [28-31]. Indirect reduction with submuscular bridge plating is an option for comminuted fractures, particularly in patients older than 5 years [24-32]. On the other way, direct open reduction with compressive plating remains a rare option for fractures not suitable to closed or indirect reduction [14]. External fixation is useful when skin integrity is compromised and for damage control but has a high rate of malunion and pin tract infection [20-33]. Complications related to treatment include femoral head osteonecrosis (reported uncommonly, after rigid intramedullary nailing), malunion (more prevalent with external fixation and flexible/elastic intramedullary nailing in heavier children), nonunion, implant migration or prominence (mostly with flexible/ elastic intramedullary nailing), infection, neurovascular injury, refracture, venous thromboembolism and fat emboli syndrome [28]. The main aim of our study was to verify if age and weight are predictive factors of associated injuries and complications in children with femoral shaft fracture.
Methods
We performed a retrospective cohort study, including all patients age 0-16 years old, admitted to our institution, in the period 2011-2015, with a diagnosis of femoral shaft fracture. Patients with syndromic or neuromuscular pathology were excluded. Patient records were searched to collect data on age, weight, gender, side of fracture, etiology of injury, pattern and location of fracture, associated lesions, type of treatment, complications, fracture healing and result at final follow-up. Statistical analysis was performed using the IBM SPSS Statistics 23.0 software. Data were shown as mean ± standard deviation for the continuous variables, median (minimum-maximum) for ordinal variables, and frequency, with a percentage for categorical variables. Due to the small sample size and inability to assume normal data distribution, the Fisher’s exact test was selected for analysis of categorical variables and the Mann-Whitney and Kruskal-Wallis tests used to compare continuous variables. A significance level of p<0.05 was set for considering statistically significant differences.
Results
Sixty patients with 61 femoral shaft fractures were included in this study. A male predominance [n=40] was observed. Mean age at the time of injury was 6.3±4.9years. Of the 61 femoral shaft fractures identified, 13 were proximal: 42 mid-diaphyseal and 6 distal. The most common etiology of injury was direct trauma after a fall [n=25] followed by traffic accident [n=16], indirect trauma [n=12], hit-by-car [n=7] and child abuse [n=1] (Figure 1). We verified a greater number of right sided fractures [n=34] and the most common pattern of fracture was transverse [n=29], followed by spiral [n=19] and oblique [n=13]. At the time of fracture, 18% of the patients [n=11] had also other associated lesions: other fractures [n=7], severe thoracic trauma [n=3], head trauma with subdural hematoma [n=3], renal trauma [n=2], splenic trauma [n=1], hepatic trauma [n=1] and braquial plexus neuropraxia [n=1] (Table 1). The occurrence of associated lesions was significantly higher in older (p=0.01) and heavier (p=0.009) patients. The relative risk of associated lesions at the time of fracture was 1.4 times higher in patients with more than 5 years old when compared to those who were younger [RR=1,384 (IC95%: 1.058-1.812), p=0.008].
For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
4 notes
·
View notes
Text
Lupine Publishers | Vicryl or Ethibond for open Surgical Achilles Tendon Repair

Lupine Publishers | Orthopedics and Sports Medicine
Mini Review
The strongest tendon in the body is the Achilles tendon. Acute tendon rupture can occur and is found most commonly in males. Management of rupture can be conservative or surgical. Surgical management is often associated with wound complications that can occur early or later. By contrast, conservative management is associated with a higher rate of re-rapture. Various suturing open techniques have been reported [1]. Krakow, Kessler and Bunnel suture techniques are commonly used [1,2]. Cadaveric study has shown that the three techniques have no strength differences [3]. The surgeon should be aware of the risk of developing wound complications. Bruggeman et al. have reported that females, tobacco use, and steroid use are risk factors for developing wound complications following open Achilles tendon repair [4]. Nonathletic patients tend to have poor outcomes following Achilles tendon surgery because of a higher body mass index, greater calf circumference, smoking, and greater subcutaneous body fat than athletic patients[5]. The surgeon is often the one who chooses which material to use to suture the tendon. This selection could be based on experience or on how the surgeon was taught. Suture materials can be divided into absorbable and non-absorbable. The absorbable suture commonly used in orthopaedics is vicryl, while ethibond and fibre wire are non-absorbable [6]. The reasons why surgeons use a non-absorbable suture include a higher knot and suture security and holding resistance, and also a belief that this type of suture is stronger [7]. But in biochemical test, it has been found that there was no knot slippage for either type of suture [6]. Kocaoglu et al. reported comparable clinical scores for both suture types, however, the non-absorbable had higher complication rates following Achilles tendon repair. Common complications for a non-absorbable suture include delayed wound healing, wound dehiscence, and at a later stage granulation formation which can present as a chronic sinus [7, 8, 9]. Patients may then require oral antibiotics or surgical debridement that involves removal of the non-absorbable material. When surgically treating Achilles tendon rupture, the absorbable suture material can be used.
Ethical Approval
Not applicable.
Data Availability
Not applicable.
Funding
No specific funding was received for this work.
Transparency Declarations
The author declares that there is no conflict of interest.
For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/ For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php To Know More About Open Access Publishers Please Click on Lupine Publishers Follow on Linkedin https://www.linkedin.com/company/lupinepublishers
Follow on Twitter : https://twitter.com/lupine_online
6 notes
·
View notes
Text
Lupine Publishers | Haglund Syndrome – A Case of Bilateral Involvement
Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Haglund syndrome is a cause of posterior heel pain and occurs commonly in adolescent girls who wear high heels with restrictive heel counters and may occur in people with rheumatoid arthritis. Is characterized clinically by thickening of the soft tissues at the Achilles tendon insertion or a painful “pump bump” and retrocalcaneal bursitis, Achilles tendinitis, and a prominent posterosuperior calcaneal border or bursal projection. We report a case of a 59 years-old woman with bilateral Haglund syndrome which did not needed surgical treatment, being the conservative treatment enough to improve the patient’s quality of life.
Keywords: Calcaneus; Magnetic resonance imaging; Foot diseases
Introduction
Haglund syndrome is a cause of posterior heel pain and was first described by Patrick Haglund, in 1928, to occur in patients who had a prominence of the posterosuperior surface of the calcaneus [1]. It occurs commonly in adolescent girls who wear high heels with restrictive heel counters and may occur in people with rheumatoid arthritis [1]. Haglund syndrome has also been termed “pump bump,” “winter heel,” “knobby heels,” “calcaneal altus,” “highbrow heels,” and “cucumber heels” [1]. Haglund syndrome is characterized clinically by thickening of the soft tissues at the Achilles tendon insertion or a painful “pump bump” and retrocalcaneal bursitis, Achilles tendinitis, and a prominent posterosuperior calcaneal border or bursal projection [1-4].
Case Presentation
59 years-old woman with pain and swelling in both feet for four months that get worse when use slippers and when she wake up and put her feet in the floor for the first time in the day. The patient denies other complaints and surgeries. At physical examination refers pain at the palpation of in the posterior and inferior regions of the ankle. The Magnetic Resonance Imaging (MRI) demonstrates posterior and plantar calcaneal spurs, liquid in retrocalcaneal and subcutaneous calcaneous bursa, and calcaneal tendon with heterogeneous signal and thickened (1.4cm at left and 1.2cm at right), markedly in their insertion with adjacent bone edema (Figures 1 & 2). The set of findings are compatible with Haglund syndrome. The patient started conservative treatment with non-steroidal anti-inflammatories, change of footwear and physiotherapy, presenting a good response, not requiring surgery.
Discussion
Haglund syndrome is caused by mechanically induced inflammation of the Achilles tendon and its bursa, from abnormally high pressure between the bursal projection of the calcaneus, the Achilles tendon, and the bursa [1,5]. Patients with bursitis have erythema and swelling over the bursa and tenderness to direct palpation [2] besides pain with dorsiflexion of the foot [6]. Clinically, by physical examination alone, it may be difficult to distinguish Haglund’s syndrome from other causes of hindfoot pain such as Reiter’s disease, rheumatoid arthritis, or isolated local conditions such as superficial tendon Achilles bursitis secondary to poor shoe fit [7]. Plain radiograph in a lateral standing position is useful to assess the presence of a prominent bursal projection of the calcaneum, the Haglund deformity [3]. Loss of a lucent retrocalcaneal recess is an important indication of underlying retrocalcaneal bursitis [3]. The Achilles tendon is swollen, and dystrophic calcifications may also be seen [3].
MRI may be required for ambiguous or clinically equivocal cases [3]. The cardinal soft tissue abnormalities, namely Achilles tendinopathy, and retrocalcaneal and retroachilles bursitis are more easily and directly depicted by MRI [3]. The detection of marrow oedema within the prominent bursal projection is likely to support the repetitive mechanical compression and inflammation as the pathological mechanism in this condition [3]. Treatment of Haglund deformity, with or without bursitis, targets decreasing the pressure and inflammation with openheeled shoes, anti-inflammatory or analgesic medications, and corticosteroid injections [2]. Physical therapy may also help reduce pain. In recalcitrant cases, surgery to remove the Haglund deformity may be necessary [2].
The nonsurgical treatment, combined with modifications in daily shoe wear, is an appropriate initial treatment for pain relief of Haglund’s syndrome [7]. Using ultrasound guidance to inject the retrocalcaneal bursa is a simple, reliable method of ensuring accurate delivery of medication into the bursa and avoiding intratendinous injection [7].
For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/ For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ)
Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin https://www.linkedin.com/company/lupinepublishers Follow on Twitter : https://twitter.com/lupine_online
4 notes
·
View notes
Text
Lupine Publishers | Bone Marrow Edema and Joint Overuse in Athletes: a Mini-Review

Lupine Publishers | Orthopedics and Sports Medicine Abstract A marginal number of adolescents meet the recommended guidelines of 60 minutes of moderate to vigorous daily physical activity, and even fewer underrepresented minority females achieve this metric as compared to their male and white counterparts. While potential interventions exist to address these low levels of activity, which is a known risk for acute injuries and chronic disease, there is lack of consensus on the devices used to measure the intensity of daily activity levels. Wearable activity trackers such as FitbitTM have been utilized to quantify human motion and exercise intensity, but there is little precedence for these measures being assessed in adolescent wearers. Thus, our objective was to assess the feasibility of using Fitbit to assess daily physical activity levels in underrepresented minority adolescent females, who attend an economically challenged urban high school, over the course of a physical activity intervention. We also aimed to identify candidate Fitbit outcome measures for future prospective studies. A 10-week physical activity intervention was implemented in a cohort of 24 high school female athletes. From within this cohort, a sample of five students was provided FitbitTM devices, from which we obtained data sets from three students. Activity on the days of the exercise intervention was measured and compared to activity on non-intervention days. Post-hoc assessments were performed based on individual heart rate reserves, the predefined levels set by the Inspire FitbitTM device and the American College of Sports Medicine (ACSM) 2009 guidelines. The results showed that while compliance is challenging, wearable devices can be used to assess daily physical activity levels and intensities in underrepresented minority high school female athletes during an extended physical activity intervention. Of the Fitbit outcomes currently available, assessment of moderate-vigorous activity (min/day) appeared to be the best as a measure of global physical activity. Prospective research is now warranted to validate these thresholds, and to test novel interventions for their ability to transition inactive adolescents at risk of sports-related injuries and long-term chronic disease, into a more active lifestyle.Keywords: Fitbit; Physical Activity Recommendations; Physical Activity Intensity LevelsIntroductionGo toThe recommended physical activity guidelines for adolescents are 60 daily minutes of moderate to vigorous activity with at least three days a week involving vigorous activity [1]. Moderate physical activity examples include bike riding, brisk walking and dancing; examples of vigorous level activities include running, martial arts and active games like tag [1]. According to NHANES data, only 20% of young adults and adolescents meet this requirement, which is worrisome in light of the United States’ obesity epidemic [2]. Even more concerning is that a large gender and racial disparity exists within these numbers [3-7]. Females, particularly those of underrepresented racial minorities, most often do not meet these recommended levels in comparison to their male and white counterparts [5,8]. This activity gap has short-term effects, with lower activity adolescents being observed to have a higher incidence of obesity and glucose intolerance during their adolescent years, in addition to long-term effects such as increased risk for development of cardiovascular disease and associated co-morbidities such as hypertension and diabetes, all of which decrease life expectancy [9-11]. An opportune time to intercede and decrease prevalence of these diagnoses, which greatly shortens lifespans and negatively impacts quality of life, may be during the formative, teenager years [12,13]Until recently, the gold standard for daily objective physical activity assessment was accelerometers [14]. While there is a plethora of supportive evidence on the validity of these devices, drawbacks and limitations also exist [15]. Their utility, which has been demonstrated within the lab setting, is not always able to be replicated pragmatically in real life settings [16]. Although these devices have continued to diminish in size, they are relatively larger on children, leading to discomfort. They also require specific instructions in location of placement on the body, which needs to be consistent throughout the intervention [17-18]. Accelerometers can be expensive, limiting the ability of researchers to be able to study large populations [15,16]. Additionally, they may be viewed as a research implement and therefore less likely to be utilized by participants as designed in the study methodology [19,20] More recently, fitness monitors have introduced an alternative technological method to objectively quantifying activity levels. These devices offer multiple benefits over accelerometers. They can be less expensive; they are often easier to position, are lightweight and are accepted in mainstream culture as wearables. This may increase the probability that they are more consistently worn which then leads to increased quantity and improved quality and reliability of the collection of the data they generate as previous data has shown their validity for physical activity studies [14-23]. Recently, we developed and implemented a 10 week athletic performance and injury prevention program for adolescent high school students, and demonstrated the use of Patient-Reported Outcomes Measurement Information System (PROMIS) and Functional Movement System (FMS) outcomes [24]. To expand on this, we aimed to assess daily activity levels during a similar 10 week study in underrepresented minority female athletes monitored via FitbitTM wearable technology. Our hypothesis was that the wearable devices would be able to distinguish thresholds between low, moderate and vigorous activity among student participants. Longterm, these thresholds could be validated for utilization in future prospective studies.Materials and MethodsGo toThis was a prospective cohort study of adolescent athletes enrolled in an athletic performance and injury prevention program. The pilot was administered in an urban high school setting during a 10-week program led by co-investigators in fall 2019. Study participants were led through a three day a week exercise intervention that targeted all major muscle groups [24]. Out of the cohort’s 24 participants, a sample of five was given a FitbitTM (Inspire HR, United States, San Francisco, CA). Study participants were instructed by the research staff in use of the device and also to wear their assigned FitbitTM device all day, removing only to bathe or charge the device. Wear age and device charge capacity was checked during the thrice weekly intervention sessions. All human subject research was performed following informed consent from a legal guardian and assent from the study subjects, on an Institutional Review Board approved protocol. A data agreement was made with the company for data access. Data was uploaded to the FitbitTM database multiple times a day and then participant data was downloaded to an approved, secure University of Rochester database every 24 hours. Our primary goals were to demonstrate the ability to consistently track physical activity levels via the FitbitTM monitoring system in this pilot feasibility study. Daily FitbitTM output obtained included minutes of activity, resting heartrate (HR) and heartrate during activities. Maximum heartrate and heart rate reserve (HRR) were calculated using participants’ age and resting heartrate. The American College of Sports Medicine (ACSM) categorizes physical intensity levels into distinct groups [25, 26]. These levels are determined from the calculated maximum heart rate and resting heart rate of individuals’. The levels assigned for heart rate data were predetermined by FitbitTM, and so we retrospectively determined which ACSM intensity levels those categories best fit. Results Three female athletes were followed through a subsection of a 10 week physical activity intervention program (Table 2). A fourth athlete had data collected, but it was for less than 50% of the intervention timeframe and so her data was excluded. Another participant had to leave the program for personal reasons; therefore, her data was also excluded. The Fitbit results showed that Participant 1 and Participant 2 did not meet the recommended daily 60 minutes of moderate/vigorous activity throughout the intervention, on either the days of the week with the activity intervention or without (Figure1). However, participant 3 met the average daily activity recommendation on six intervention days. Appropriate device wear age varied from 41% to 97%. Discussion To the end of establishing thresholds values to characterize an individual’s activity as low, moderate, or vigorous, we performed post hoc analyses on various daily Fitbit measurements including: Steps, Minutes Sedentary, Minutes Lightly Active, Minutes Fairly Active, Minutes Very Active, Activity Calories, Resting Hours, Out of Range, Fat Burn, Cardio, and Peak. Of these, moderate-to-vigorous physical activity (MVPA) was best defined by the predefined Cardio and Peak FitbitTM categories. While various commercial wearable devices are now available to quantify daily activity in human subject research, we chose the Fitbit Inspire HR device largely due to its secure internet interfaces with the study subjects and our research database. Of note, some studies have shown that in comparison to validated accelerometers, FitbitTM devices provided comparatively accurate estimates of sedentary activity, but overestimates MVPA under free-living conditions [27]. Additionally, it has been shown that the test-rest reliability of Fitbit is dependent on activity type and has greater variation between sessions compared to other wearable devices [28]. Nonetheless, we found FitbitTM suitable for the intended purpose, and the development of threshold values to evaluate groups of people a potential solution to the device’s limitations in precision measurements. Obtaining Fitbit daily activity data on underrepresented minority high school female athletes during a 10-week training program is feasible. Fitbit MVPA thresholds for moderate and vigorously active levels can be derived and used to evaluate the efficacy of an intervention aimed at improving sedentary life-styles. For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/ For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ) Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php To Know More About Open Access Publishers Please Click on Lupine Publishers Follow on Linkedin https://www.linkedin.com/company/lupinepublishersFollow on Twitter : https://twitter.com/lupine_online
6 notes
·
View notes
Text
Lupine Publishers |A Novel Approach to Multi-Trauma Patients with Bleeding Pelvic Fractur

Lupine Publishers | Orthopedics and Sports Medicine
Introduction Bleeding from pelvic fracture, especially in patients with multiple trauma injuries, is a difficult problem facing the general practitioner working at Emergency Room (ER). Orthopedist, general surgeon, neurosurgeon, urologist and interventional radiologist are the main consultants taking care of these kind of patients. Recently, there have been many changes in practice to predict and limit hemorrhage in the patient with a pelvic fracture, and multidisciplinary approach has improved the outcome and overall survival [1]. Institutional guidelines or trauma protocols should be well-established especially in advanced trauma centers.
The first thing to do in these patients is to understand if the case is hemodynamically stable or unstable [2]. Multiple intravenous (iv) accesses should be ready in use and Foley catheter should be inserted in the monitorized patient. In hemodynamically stable patients, simple orthopedic fractures and any possible accompanying intracranial pathology can be excluded by using computerized tomography (CT) scans from cranium to the pelvis and X-rays of all suspected extremities. Then, the ER team can emphasize particularly on the pelvic fracture. The ongoing bleeding should be further interrogated. Furthermore, the accompanying intraabdominal and/or retroperitoneal pathology should also be evaluated in detail. FAST (focused assessment with sonography in trauma) can be a useful tool in the evaluation of precordial and abdominal cavities [3]. However, its dependence on the personal experience seems to be a major disadvantage in comparison with more detailed CT interpretations. Hemodynamically unstable patients with suspected intraabdominal bleeding should undergo emergent exploration.
Pelvic stabilization has been attempted for years to control bleeding by decreasing the pelvic volume and supplying tamponade effect [4]. Initially used pneumatic antishock garments have largely fallen out of favor as they lead to compartment syndrome, and they are bulky, difficult to apply and interfere with physical examination. In case of unstable pelvic injuries, the initial application of external pelvic fixation and pelvic C-clamp can be tried in an attempt to control hemorrhage associated with pelvic fracture [5]. However, an emergent pelvic angiography and embolization should be planned after nonpelvic sources of blood loss have been ruled out. A CT finding of arterial iv contrast extravasation in the pelvis is another indication for pelvic angiography and embolization regardless of the hemodynamic status. However, it only controls arterial bleeding and indicated in only up to 10 % of cases with the pelvic instability.
The exclusion of intraabdominal bleeding is vital in patients with pelvic fracture. FAST and abdominal CT are the best tools here, and replaced the historically used diagnostic peritoneal tap or lavage which are known with their high false negative or positive rates [6]. As the indications for explorative laparotomy in cases with pelvic fracture are the same for all trauma patients, the concomitant bleeding from pelvis and abdomen should be differentiated, and each should be treated. If abdominal exploration reveals a specific organ injury, repair can be tried in case of stabilization of the vitals intraoperatively. However, intraabdominal or retroperitoneal packing is currently accepted as the golden standand approach in unstable multiple trauma patients with ongoing abdominal bleeding where the major vessels are severely injured [7]. This procedure saves time till the patient gains hemodynamic stability and the physician decide what to do the next. Therefore, the procedure is also called as ‘damage control surgery’ [7,8]. In case of presacral bleeding accompanying multiple pelvic fractures, packing of the pelvic cavity can be life-saving. Pelvic packing can also be used in unstable patients without intraabdominal pathologies [9]. In these cases, exploration starts with a midline incision from umbilicus toward the pelvis, and bladder is retracted away from the fracture and three to five laparotomy pads are soaked into the retroperitoneal space on each side (toward the iliac vessels). Packing in combination with external mechanical fixation of the pelvis is reported to be successful as well. The second-look surgery can be planned in first to third postoperative days, and the laparotomy pads are removed carefully.
To know more about our Orthopedics and Sports Medicine click on https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
To know more about Lupine Publishers click on https://lupinepublishers.us/
To know more about Open access publishers click on Lupine Publishers
1 note
·
View note
Text
Lupine Publishers | Haglund Syndrome – A Case of Bilateral Involvement
Orthopedics and Sports Medicine Orthopedics and Sports Medicine
Lupine Publishers | Orthopedics and Sports Medicine
Abstract
Haglund syndrome is a cause of posterior heel pain and occurs commonly in adolescent girls who wear high heels with restrictive heel counters and may occur in people with rheumatoid arthritis. Is characterized clinically by thickening of the soft tissues at the Achilles tendon insertion or a painful “pump bump” and retrocalcaneal bursitis, Achilles tendinitis, and a prominent posterosuperior calcaneal border or bursal projection. We report a case of a 59 years-old woman with bilateral Haglund syndrome which did not needed surgical treatment, being the conservative treatment enough to improve the patient’s quality of life.
Keywords: Calcaneus; Magnetic resonance imaging; Foot diseases
Introduction
Haglund syndrome is a cause of posterior heel pain and was first described by Patrick Haglund, in 1928, to occur in patients who had a prominence of the posterosuperior surface of the calcaneus [1]. It occurs commonly in adolescent girls who wear high heels with restrictive heel counters and may occur in people with rheumatoid arthritis [1]. Haglund syndrome has also been termed “pump bump,” “winter heel,” “knobby heels,” “calcaneal altus,” “highbrow heels,” and “cucumber heels” [1]. Haglund syndrome is characterized clinically by thickening of the soft tissues at the Achilles tendon insertion or a painful “pump bump” and retrocalcaneal bursitis, Achilles tendinitis, and a prominent posterosuperior calcaneal border or bursal projection [1-4].
Figure 1: Sagittal section MRI in T1 sequence in A and T2 STIR sequence in B of the right ankle demonstrating posterior calcaneal spur (red arrow), liquid in retrocalcaneal bursa (blue arrow), liquid in subcutaneous calcaneous bursa (orange arrow), and calcaneal tendinopathy (green arrow).
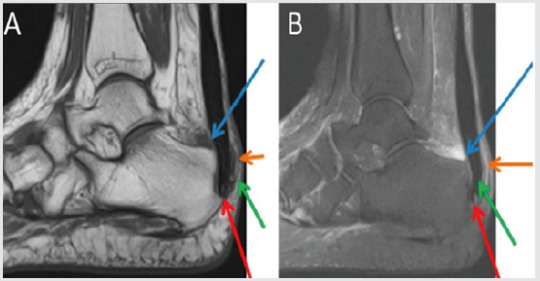
Figure 2: Sagittal section MRI in T1 sequence in A and T2 STIR sequence in B of the left ankle demonstrating posterior calcaneal spur (red arrow), liquid in retrocalcaneal bursa (blue arrow), liquid in subcutaneous calcaneous bursa (orange arrow), and calcaneal tendinopathy (green arrow).
Case Presentation
59 years-old woman with pain and swelling in both feet for four months that get worse when use slippers and when she wake up and put her feet in the floor for the first time in the day. The patient denies other complaints and surgeries. At physical examination refers pain at the palpation of in the posterior and inferior regions of the ankle. The Magnetic Resonance Imaging (MRI) demonstrates posterior and plantar calcaneal spurs, liquid in retrocalcaneal and subcutaneous calcaneous bursa, and calcaneal tendon with heterogeneous signal and thickened (1.4cm at left and 1.2cm at right), markedly in their insertion with adjacent bone edema (Figures 1 & 2). The set of findings are compatible with Haglund syndrome. The patient started conservative treatment with non-steroidal anti-inflammatories, change of footwear and physiotherapy, presenting a good response, not requiring surgery.
Discussion
Haglund syndrome is caused by mechanically induced inflammation of the Achilles tendon and its bursa, from abnormally high pressure between the bursal projection of the calcaneus, the Achilles tendon, and the bursa [1,5]. Patients with bursitis have erythema and swelling over the bursa and tenderness to direct palpation [2] besides pain with dorsiflexion of the foot [6]. Clinically, by physical examination alone, it may be difficult to distinguish Haglund’s syndrome from other causes of hindfoot pain such as Reiter’s disease, rheumatoid arthritis, or isolated local conditions such as superficial tendon Achilles bursitis secondary to poor shoe fit [7]. Plain radiograph in a lateral standing position is useful to assess the presence of a prominent bursal projection of the calcaneum, the Haglund deformity [3]. Loss of a lucent retrocalcaneal recess is an important indication of underlying retrocalcaneal bursitis [3]. The Achilles tendon is swollen, and dystrophic calcifications may also be seen [3].
MRI may be required for ambiguous or clinically equivocal cases [3]. The cardinal soft tissue abnormalities, namely Achilles tendinopathy, and retrocalcaneal and retroachilles bursitis are more easily and directly depicted by MRI [3]. The detection of marrow oedema within the prominent bursal projection is likely to support the repetitive mechanical compression and inflammation as the pathological mechanism in this condition [3]. Treatment of Haglund deformity, with or without bursitis, targets decreasing the pressure and inflammation with openheeled shoes, anti-inflammatory or analgesic medications, and corticosteroid injections [2]. Physical therapy may also help reduce pain. In recalcitrant cases, surgery to remove the Haglund deformity may be necessary [2].
The nonsurgical treatment, combined with modifications in daily shoe wear, is an appropriate initial treatment for pain relief of Haglund’s syndrome [7]. Using ultrasound guidance to inject the retrocalcaneal bursa is a simple, reliable method of ensuring accurate delivery of medication into the bursa and avoiding intratendinous injection [7].
For more Lupine Publishers Open Access Journals Please visit our website: h http://lupinepublishers.us/ For more Orthopedics and Sports Medicine Open Access Journal (OSMOAJ) Please Click Here: https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php To Know More About Open Access Publishers Please Click on Lupine Publishers
Follow on Linkedin : https://www.linkedin.com/company/lupinepublishers Follow on Twitter : https://twitter.com/lupine_online
0 notes
Text
Lupine Publishers | No Fact Check, Pharmaceutical Instituions from Reputed Pune University and Socially Situated and Socially Constituted Agency

Lupine Publishers | Orthopedics and Sports Medicine
Abstract
The behavioral view of corporate governance has derived from the behavioral view of the firm, which arguably rests on more realistic assumptions than the economics rooted positive agency theory with regard to the heuristics of managerial action. In addition to the bounded rationality condition, the principle of satisfying and the assumption on routinisation in the decision-making process, the behavioral view treats organizations as complex social systems. They constitute venues of power battles among the coalitions of corporate actors realizing often conflicting goal agendas. It is therefore probably the most explicit about the existence of phenomena of power and politics in the corporate settings among all theories of the firm.
Keywords: PAT (Positive Agency Theory)
Introduction
Recently published work, suggest enriching the under socialized agency perspective with the predictions of the behavioural theory of the firm. They refer to this cross theoretical hybridization as the behavioural theory of corporate governance. Within that framework, they distinguish two main mechanisms that impact on behaviour and actions of actors involved in governance processes in corporations, i.e. the socially situated and socially constituted agency [1,2]. PAT, as an under socialized and actor centric theory, concentrates on examining patterns, according to which individuals voluntarily, however rationally, realize their own goal agendas. They are motivated by self-interest and differential personal risk preferences, as well as are subject to informational and incentive constraints. In effect, PAT governance mechanisms tend to be formal in nature. They take a form of either incentive for managers as agents or means of monitoring/controlling them. They are construed to provide safeguards against such actions of managers, who driven by their self-interest may be potentially deviating from the desired organizational and/or societal outcomes. This unfolds by aligning managerial interests with those of shareholders or disciplining managers as agents. Infuse the agency relationships with the social context. They emphasise that corporate leaders do not operate in the social vacuum. On the contrary, they act in the socially constructed and interpreted reality. In the methodological sense, they enrich the of the individual human action in corporate governance, as posited in PAT, with the social fabric of norms, values and beliefs, and point towards the socio-cognitive processes as actual frames, within which particular board members enact their decision-making processes [3,4].
In other words, in this cross-theoretical framework and conceive the missing link between the macro-social explanations of well-functioning corporate governance practice, as offered by the economics-rooted PAT, and the micro-behaviour that is most likely to actually unfold in the boardroom reality. The term ‘socially situated’ is thought of in recognition of the fact that in any given situation individuals are enmeshed in a set of social relationships, networks, as well as institutions, which have influence on their perceived individual agency (e.g., a manager being accountable to non-executive directors directly, and to shareholders indirectly). Therefore, they represent crucial contingencies that ultimately shape the behaviour of individuals. The notion ‘socially constituted’, in turn, is conceived to capture a deeper kind of influence of the social context on the perception of the individual agency than it is the case with the socially situated agency. This concept emphasizes ways in which individuals’ socialization into performance of their particular roles (e.g., as a manager, a Chairman, a non-executive director), as well as their cumulative personal experiences to date, determine what they regard as possible or realistic in a given situation. The perceived individual agency, shaped through these processes, ultimately precipitates in a specific socio-cognitive orientation that particular board members adopt in their socially constructed boardroom reality. There have emerged entire streams of empirical research, which, even if it does not fully explain the theoretical rationale of the suggested behavioural theory of corporate governance, explicitly examines the socio-cognitive processes and behavioural tactics that are likely to unfold in the boardroom reality. They act as contingencies that shape decisionmaking processes by particular board members. For example, predicts the likely board outcomes as a result of competition and collaboration between the executive and non-executive directors in the boardroom. Research pluralistic ignorance on boards. Scrutinize favour rendering, ingratiation tactics and norms of reciprocity. Analyze the processes of symbolic and impression management, together with organizational/ institutional decoupling [4,5]. Finally, look at the social distancing tactics as a means of disciplining and/ or demonstrating ostracism towards those minority coalitions, which step out of the line dictated by the dominant board fraction.
Culturally determined agency
The notions of social situatedness and constitution fall close to concept of habitus. He coined it in elaborating on his view of power as internalized constraints. His perspective is methodologically akin to the conceptualizations of power, who regarded it as a ubiquitous abstract and subtle force that is impacting on individuals in such a way, that they actually act as their own over-seers. They discipline themselves and the existing social relationships thus arise as the natural order. These arguments suggest that the individual agency as perceived by particular social actors is de facto socially constructed, whereby this process is hugely influenced by the position of a given actor in the existing structure of social relationships. In corporate governance of domestic firms, the socio-cognitive processes that shape board members’ perception of their individual agency are described in the aforementioned contributions. However, such developments can also occur on Pharmaceutical Instituions’ boards [6-8]. There is one characteristic, though, which makes corporate governance in Pharmaceutical Instituions distinctively different from corporate governance in their domestic counterparts.
This is the phenomenon of culture and cultural differences between nation states. It is also the distinctive feature of the entire international business research, and hence we have it as a separate field of study in management science. Without drilling deeply into intricacies of accountability chains on boards within the Pharmaceutical Institutions headquarters and within its foreign subsidiaries separately, I therefore propose the view of culturally determined agency. The notion is to capture the socio-cognitive processes that particular board members in a given foreign subsidiary and their counterparts in the Pharmaceutical Institutions headquarters are exposed to, being located at the interface of Luo’s (2005a, 2005b) 1st- and 2nd-tier governance [9,10]. I suggest this view as a specific and distinctive feature of the corporate governance in Pharmaceutical Institutions. It incorporates cultural influences on the processes of social construction of the perceived individual agencies by particular board members at both governance levels and constitutes a significant portion of the overall variance of all types of impact factors on these processes [11,12].
Conclusion
Other corporate governance mechanisms typically distinguished in the academic literature comprise:
a) Minority investors’ protection rights.
b) Ownership concentratio
c) Incentive alignment (performance- related executive pay contingency).
d) Direct shareholders’ control (e.g. voting at the annual general meeting (AGM)).
e) Managerial labour market (reputation effects).
f) Market for corporate control (takeover activity).
g) Product market competition.
To know more about our Orthopedics and Sports Medicine click on https://lupinepublishers.com/orthopedics-sportsmedicine-journal/index.php
To know more about Lupine Publishers click on https://lupinepublishers.us/
To know more about Open access publishers click on Lupine Publishers
0 notes