#microdeletion
Explore tagged Tumblr posts
Text
Trisomy 18 and Microdeletion 18p Mosaicism: A case report and literature review by Chao-Chun ZOU in Journal of Clinical Case Reports Medical Images and Health Sciences
ABSTRACT
The trisomy 18 syndrome is a common chromosomal disorder due to the presence of an extra chromosome 18, either complete, mosaic trisomy or partial trisomy 18q. The mosaic trisomy 18 patients’ phenotype was extremely variable, from the absence of dysmorphic features to complete trisomy 18 syndrome. The phenotype of 18p deletion syndrome is variable and almost all survived. A 2-year-old girl was referred to our hospital due to growth delay. Mild dysmorphy including thin hair, frontal bossing, low set ears, broad-flat nose, nostrils slightly upward, downturned corners of the mouth, dysplasia teeth, small hands and fingers bilaterally was observed. The karyotype of peripheral leukocyte showed 46,XX, psu idic (18)(p11.2)[55]/46,XX, del (18)(p11.2)[45]. We report this case to add to our knowledge of the trisomy 18 and microdeletion 18p mosaicism.
Keywords: Trisomy 18, mosaic;18p microdeletion; Psychomotor retardation; Karyotype
INTRODUCTION
The trisomy 18 syndrome was first reported by Edwards et al in 1960, also known as Edwards syndrome. It is the second most common autosomal chromosomal disorder after trisomy 21(Down’s syndrome)due to the presence of an extra chromosome 18, which has three basic types: complete, mosaic and partial type (Edwards et al., 1960, Cereda and Carey, 2012,Mudaliyar and Mudaliyar, 2017). The syndrome presents a recognizable pattern of major and minor anomalies, significant psychomotor and cognitive disability are associated with high neonatal and infant morbidity and mortality. The estimated overall prevalence of trisomy 18 in live born is approximately 1/6, 000 to 1/8, 000 while the incidence in fetus is much higher, the difference is caused by fetal loss and pregnancy termination after prenatal diagnosis (Cereda and Carey, 2012, Rasmussen et al., 2003). The mosaic trisomy 18 usually means having more than one cell line in the individual, and it occurs in approximately 5 percent in all trisomy 18 patients (Fitas et al., 2013). The phenotypic manifestations are highly variable, from the absence of dysmorphic features to the complete trisomy 18 syndrome (Tucker et al., 2007). Since the clinical outcomes of complete and mosaic trisomy 18 can be different, it is of vital importance to achieve a correct diagnosis because of implications in medical management and genetic counselling. 18p deletion was first described by de Grouchy and colleagues in 1963 and was estimated to occur in approximately 1/50, 000 live born, which results from deletion of a part or full of the short arm of chromosome 18(Turleau, 2008). The mostly reported clinical features include cognitive impairment, congenital heart defects, small stature, minor facial dysmorphy, and skeletal deformities(Turleau, 2008, Xiao et al., 2019, Hasi-Zogaj et al., 2015, Yi et al., 2014)
Typical facial features include hypertelorism, ptosis, strabismus, broad–flat nose, micrognathia, and low-set big ears. Holoprosencephaly may be seen in approximately 10–15% of patients(Turleau, 2008). In addition, speech and language difficulties, pituitary abnormalities, generalized seizures, dystonia, and autoimmune diseases have also been described(Turleau, 2008, Rao et al., 2001, Graziadio et al., 2009, McGoey et al., 2011). However, these non-specific features are easily overlooked clinically. The clinical phenotype severity is related to the size and location of deletion region. In this report, we present a 2-year-old girl of mosaic trisomy 18 and 18p microdeletion with mild psychomotor retardation, cognitive impairment and language developmental disability.
Clinical description
A 2-year-old female second child of non-consanguineous parents was admitted to our hospital due to growth delay. Her mother and father were 34 years old and 38 years old when giving birth to her. She was born at full-term with uncomplicated gestation, her birth weight was 3.35 kg and the length was about 50 cm. No feeding difficulty and complications were referred in the neonatal period. She had a motor retardation of autonomous walking until 22-months old and intelligence disability and language disability. She only knew a few simple words like ”mama“, not ”baba“, and she cannot communicate clearly with others though she was willing to speak to strangers. Gesell Developmental Schedules performed in local hospital indicated mental developmental delay in motor behavior, language behavior, adaptive behavior and personal-social behavior at age of one year and 8 months old. The height of her father, mother and 15
years old sister were 165cm, 161cm, and 155cm, respectively. No similar history was noted in her family.
On physical examination, she had a height of 81.4 cm below -3SD and a weigh of 11.6 kg below -1SD. Mild craniofacial dysmorphy was present, including thin hair, frontal bossing, low set ears, broad-flat nose, nostrils slightly upward, and downturned corners of the mouth while other craniofacial anomalies were not obvious (Fig.1A). Her hands were small especially her fingers, but the fingernails are normal (Fig.1B). Her teeth were dysplasia (Fig.1C). The echocardiography revealed patent foramen ovale (ϕ 2.96 mm) while no murmur was present. The muscle tension was normal and no other organ abnormality was detected in our patient.
Laboratory examinations (urine, liver, kidney, thyroid hormone, GS/MS and blood glucose analyses) were all normal. Insulin-like growth factor-1 was 72.5 ng/ml (normal range, 55-327 ng/ml).
Management and outcome
Ten months ago, the child was brought to a local hospital with developmental delay, the peripheral leukocyte karyotype was taken and revealed two abnormal cell lines, the result was 46,XX, psu idic (18)(p11.2)[55]/46, XX, del (18)(p11.2)[45] . She was then referred to another hospital to take the whole-exome sequencing demonstrating a deletion at 18p11.32-p11.22 (GRch37/hg19, chr18:158679 9708482del) and a duplication at
18p11.21-q23(GRch37/hg19, chr18:12012132 78005255dup). She was diagnosed mosaic trisomy 18 syndrome.
Discussion
The first reported patients with trisomy 18 syndrome were initially described by Edwards et al and Smith et al in 1960s, while the first case of mosaic trisomy 18 was reported in 1965. Less than 5% portion of patients have mosaicism of trisomy 18, and Banka et al reminded that routine karyotype from lymphocyte culture may not be sufficient to diagnose mosaicism if practitioners suspect a diagnosis of mosaic trisomy 18, karyotype from skin fibroblasts should be considered. Since then over 40 cases of mosaic trisomy 18 have been described, Tucker et al reviewed 33 reported individuals of mosaic trisomy 18 and added 2 more cases in 2007. Their clinical manifestations are extremely variable from complete trisomy 18 syndrome with early death to near totally normal. Some physical features are relatively more common and included brachydactyly, high arched palate, microcephaly, delayed bone age, frequent respiratory infections and otitis media, heart defect, 5th finger clinodactyly, micrognathia, and hypotonia. The most common heart defect is ventricular septal defect in mosaic trisomy 18. Our case has mild craniofacial dysmorphy and patent foramen ovale, and no other physical anomalies were observed.
Trisomy 18 mosaicism usually indicates the existence of more than one cell line in the individual. The peripheral leukocyte karyotype demonstrates pseudodicentric chromosome substituting a normal chromosome 18 in 55 cells and chromosome 18 missing the end of the short arm in 45 cells. The skin fibroblasts karyotype was not taken. Furthermore, there is no correlation between the physical and intellectual findings and the percentage of trisomy 18 cells in either peripheral leukocytes or skin fibroblasts. Besides, there is no correlation between the percentage of trisomic cells in peripheral leukocytes and brain, gonads, or other key organs. The variety of mosaic trisomy 18 may be related to the percentage of trisomic cells in different key organs of the body.
For complete trisomy 18 patients, approximately 50% of infants live longer than one week and about 5-10% of children survive beyond the first year. In overall, trisomy 18 mosaicism patients usually survive longer when compared to complete trisomy 18. This does not mean that all the mosaic trisomy 18 patients have a longer survival, some died a few hours after birth. For normal or mild phenotypical mosaic trisomy 18 cases, some were diagnosed due to recurrent miscarriages or giving birth to a child with trisomy 18 while others may never be identified. 18p deletion syndrome, also called monosomy 18p and De Grouchy syndrome type Ⅰ, which means a deletion of full short arm of chromosome 18 or a microdeletion of the short arm of chromosome 18. Some researches showed that nearly half of patients have breakpoints in the centromeric region and the rest scatter in the short arm, and approximately half of the deletions occur on the maternal chromosome 18 no matter where the breakpoint locations are. Our case’s breakpoint is at the 18p11.32-p11.22. Approximately two thirds of patients’18p deletion are de novo; the rest may be due to a de novo unbalanced translocation or malsegregation of parental chromosome rearrangement or a ring chromosome. The patient’s height and weight is 81.4 cm below -3SD, 11.6 kg below -1SD, respectively. It may be a prodrome of small stature, but her insulin-like growth factor-1 was normal. It also could be contributed to feeding problem. More follow-up work needs to be done to figure it out. Some reported cases show that growth hormone replacement treatment is efficient in growth hormone deficiency patients.
Our case has trisomy 18 and microdeletion 18p mosaicism simultaneously. The possibility of meiotic chromosomal nondisjunction of the ovogonia/spermatocyte was increased because of her parents’ advanced maternal age, some women may have higher a risk for nondisjunction. More possible mechanism may be a de novo unequal recombination occurring in early embryonic mitosis. Some deletions are from the parents, there is no way to figure her mutation mechanism out since we can not get her parents’ consent to analysis. The phenotype of our case combines two syndromes’ typical features, including common psychomotor retardation, cognitive impairment and congenital heart defect, characteristic small stature and language impairment of 18p deletion syndrome. Our case’s uncharacteristic craniofacial features also combine two syndromes.
In a conclusion, mosaic trisomy 18 and 18p deletion syndrome both are chromosomal disorders which has a variety of clinical manifestations. If an individual has untypical phenotypical anomalies and psychomotor and cognitive disability, chromosome disorder should be considered and cytogenic analysis is needed.
Acknowledgements: We thank the patient and his parents for permitting us to use the data.
#Trisomy 18#mosaic#jcrmhs#Research Article in Journal of Clinical Case Reports Medical Images and Health Sciences#18p microdeletion#Psychomotor retardation#Karyotype
4 notes
·
View notes
Text
Everyone around me, my relative, my neighbour and also my teacher from school ALL OF THEM gave birth to babygirls like the microdeletion of Y chromosome is so real and we fucking cheer.
38 notes
·
View notes
Text
intro!!!!!
I’m Sam aka Mr Holzark.
I’m 19 years old.
I have autism, ADHD, 4q35.2 Microdeletion and insomnia.
I’m a bit weird.
I’m apagender and aroace.
I make ocs
my interests:
.pokemon
.guts and blackpowder
.transformers
.gemstones and crystals
.parrots
.memes
.Severed Heads (the band)
.J-fashion
.the 80s
.kandi making
.roller skating
.sci fi
.horror
.fashion
.dark comedy
.the napoleonic wars
.art
.magical girls
.sushi
.jewellery
.science-fantasy
.obscure 80s music
.carnivals and theme parks
.robots and animatronics
.making headcannons
.ghosts
.aliens
.magic
.slime
.FNAF
.scene fashion
.merfolk
my mutuals: @kr9vorebeazt @autisticfoxgirl333 @sundove88 @m00nb04rd5 @ask-tfone-megatron @ask-tfone-optimus @decepticonjusticedivisonrevival @your-artificial-god @your-favs-as-birds
I hope y’all enjoy my stuff
#mr holzark#intro post#introduction#pokemon#guts and blackpowder#headcannons#80s#memes#transformers#parrots#magical girl#decora#decora fashion#decora kei#alien#ghosts#horror#black comedy#jewellery#fashion#napoleonic era#napoleonic wars#kandi bracelet#kandi kid#kandi#roller skating#robots#animatronics#scenecore
14 notes
·
View notes
Text
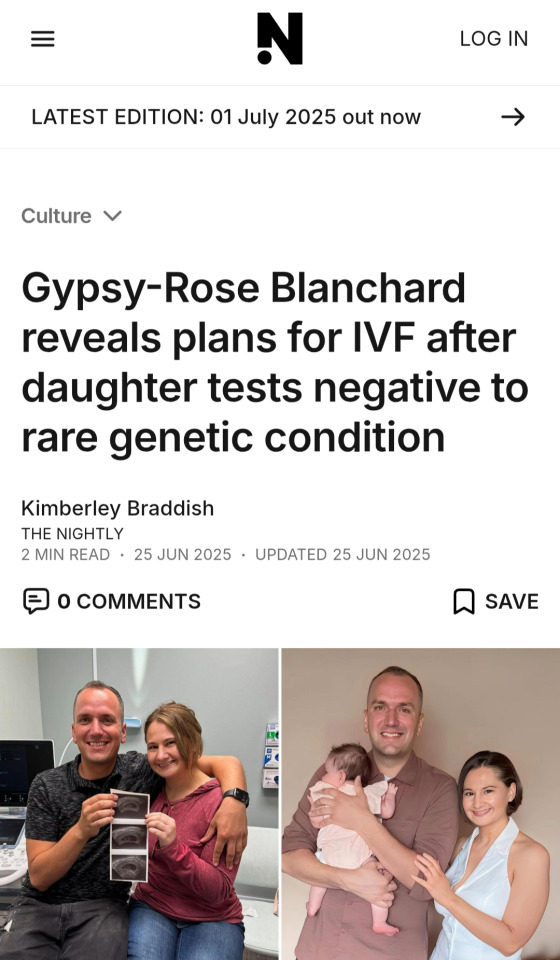
This woman got away with murdering her mother by claiming she was being abused due to Munchausen's by proxy but then it TURNS OUT she ACTUALLY HAS a rare genetic chromosomal deletion disorder that significantly impacted her health when she was younger and caused pretty much every issue she received medical treatment for. Deedee was a scam/con artist, and maybe even controlling or psychologically abusive, but Gypsy Rose was and is someone who was born with microdeletion 1Q21.1!!! AND SHE ALSO KNEW HER REAL AGE AND HAD BEEN TOLD BY MEDICAL/LEGAL PROFESSIONALS THAT SHE WAS A COMPETENT LEGAL ADULT.
And we're all just like "oh, yeah, it's cool, we're going to report on her second kid is going to be IVF so that child isn't born with the same chromosomal deletion that made her sick! The sickness we all were told was MADE UP by the mother she had murdered. Because she was "perfectly healthy."
GenreReview and Medline Plus Genetics:
1q21.1 recurrent deletion itself does not lead to a clinically recognizable syndrome, as some persons with the deletion have no obvious clinical findings. Others have variable findings that most commonly include mildly dysmorphic but nonspecific facial features (>75%), mild intellectual disability or learning disabilities (25%), microcephaly (43%), and eye abnormalities (26%). Other findings can include cardiac defects, genitourinary anomalies, skeletal malformations, joint laxity, and seizures (~23%). Psychiatric and behavioral abnormalities can include autism spectrum disorder, attention-deficit/hyperactivity disorder, and sleep disturbances. Sensorineural hearing loss and recurrent infections /otitis media are rare.
Distinctive facial features can also be associated with 1q21.1 microdeletions. The changes are usually subtle and can include a prominent forehead; a large, rounded nasal tip; a long space between the nose and upper lip (philtrum); and a high, arched roof of the mouth (palate). Other common signs and symptoms of 1q21.1 microdeletions include an unusually small head (microcephaly), short stature, and eye problems such as clouding of the lenses (cataracts). Less frequently, 1q21.1 microdeletions are associated with heart defects, abnormalities of the genitalia or urinary system, bone abnormalities (particularly in the hands and feet), and hearing loss.
Neurological problems that have been reported in people with a 1q21.1 microdeletion include seizures and weak muscle tone (hypotonia). Psychiatric or behavioral problems affect a small percentage of people with this genetic change. These include developmental conditions called autism spectrum disorders that affect communication and social interaction, attention-deficit/hyperactivity disorder (ADHD), and sleep disturbances. Studies suggest that deletions of genetic material from the 1q21.1 region may also be risk factors for schizophrenia.
Some people with a 1q21.1 microdeletion do not have any of the intellectual, physical, or psychiatric features described above. In these individuals, the microdeletion is often detected when they undergo genetic testing because they have a relative with the chromosomal change. It is unknown why 1q21.1 microdeletions cause cognitive and physical changes in some individuals but few or no health problems in others, even within the same family.
And she manipulated and egged on Nicholas Godejohn to murder on her behalf and it's so upsetting.
#this case makes me so insane lol#like shout out to her defense team for fucking burying this i guess
2 notes
·
View notes
Note
Let's talk abt genetics!! You start!
OOOOH ok this may be a little niche but i actually have a doc w multiple tabs on stuff but i made a shrine on chromosome 17 because chromosome 17 is my personal lord and savior.. i love researching deletions and i was looking at 17q1.31 microdeletion syndrome and it deletes like up to 6 different genes like as FLJ25168, SPPL 2c, CRHR1,MAPT, annnnd KIAA1267. it happens usually de novo cuz an inversion in a parents chromosome causes it w a non allelic recombination mechanism…AND i read about one specific lady who has it and shes the oldest know to have it at 63 and she has moderate intellectual disability (moderate is typical for this deletion). she also has the very very typical characteristic of the deletion — extremely friendliness and amiable personality, amongst other stuff but with her and the other patients, facial dysmorphism is almost always present which isnt uncommon for deletions but some of the features like upward slanting palpebral fissures and a brodening chin we’re interesting to me and every time i look at a deletion with distinct features (like 1p36 deletion🥸) i wonder what about the specific genes and dna being gone affects that specifically… if that makes sense. do u look at deletions too or are you more into hereditary or something else (sorry long ass text☠️)
4 notes
·
View notes
Text
Best sexologist in delhi - Best Ayurvedic Doctors for Male Infertility Treatment in Delhi NCR India
Best Doctor For Male Infertility Treatment In Delhi Male infertility is when the male partner cannot cause pregnancy in a fertile female partner. It is one of the most common conditions in males, affecting almost 7% of the male population, although much less talked about. TYPES OF MALE INFERTILITY Based on recovery of the condition, male infertility is divided into the following two types: • Complete infertility: This condition is present in the sterile male, and there are rare chances of getting fertile. Complete infertility is due to a genetic mutation that causes an inability to produce healthy sperm in sufficient concentration. Assisted reproductive technology is also of no use in such patients. The options generally available to these people are donor sperm. • Subfertility: This type of infertility is caused due to some underlying conditions that can be treated with the help of medications or surgery. Treatment for underlying diseases can restore fertility. CAUSES OF MALE INFERTILITY Various causes are involved in the development of male infertility. However, some of the common causes of male infertility are: • Genetics: Genetics is one of the most dominating factors for male infertility. It covers almost 15% of all male infertility problems. One of the most common genetic conditions for male infertility is Klinefelter’s syndrome which affects around 1 in 500 newborns. The condition is caused due to the problem in gamete formation leading to small testes, low levels of male hormones and poor sperm count. Another genetic cause of male infertility is the microdeletions in the Y chromosomes. In this condition, the deletions in Y chromosomes lead to either absent or poor sperm count or sperms produced with altered morphology. • Spermatogenesis-altering causes Various factors affecting spermatogenesis, resulting in reduced production of sperms or poor quality sperms. Varicocele is a condition affecting almost 40% of males with infertility. This condition results in the production of excess heat in the scrotum and oxidative stress that affects spermatogenesis. Celiac disease, bicycle riding, drug addiction, excessive alcohol, and medications such as chemotherapy and steroids also involve forming sperm. Hypogonadism also results in low sperm production.
• Anatomical causes: Despite producing healthy sperm in the optimum quantity, various anatomical abnormalities prevent the sperm from reaching the site through which they are ejaculated. These causes include problems in the Vas deferens, a tube which forms from the passage for sperm to travel. The Vas deferens may either be blocked or utterly absent, as seen in some cases of cystic fibrosis. Other anatomical abnormalities include infection, hypospadias, retrograde ejaculation and blockage of the ejaculatory duct. • Other causes: Other causes that contribute to male infertility include age, poor lifestyle, infection, trauma or injury to the testes and age. In almost 25% to 30% of the cases, no known cause of infertility is found, and the condition is known as idiopathic male infertility. MALE INFERTILITY SYMPTOMS The following are the symptoms of male infertility: • Swelling and pain in testes. • Low libido or Low Sexual Desire • Low volume of semen • Ejaculatory problems • Erectile dysfunction • Low sperm count in semen analysis • Reduced body hair due to hormonal imbalance • Smaller than normal testes MALE INFERTILITY TESTS Both partners should be fertile to achieve pregnancy. Thus in cases of infertility, various tests are performed to identify the exact cause. In some instances, male infertility tests cannot identify the cause. Following are the different diagnostic techniques used for diagnosing male infertility: • Physical evaluation: The doctor will physically evaluate the reproductive organ and try to ascertain any swelling in the testes. The doctor may ask various queries related to lifestyle habits, medical history or family history. • Sperm analysis: This is one of the essential tools for diagnosing male infertility. The semen of the patient is collected, and the number of sperms, morphology, and mobility are analyzed. The semen is also tested for the presence of any infection. Sperm analysis is done through a series of tests to arrive at an accurate conclusion, as the sperm in different samples may vary. • Other tests: The doctor advises various other tests to precisely diagnose the cause of infertility in a particular patient. These tests include a genetic test, a biopsy of the testes, an ultrasound of the scrotum, the level of reproductive hormones, and pre-ejaculation urinalysis • Avoid smoking • Limit the quantity of alcohol • Refrain from taking addictive drugs • Manage Obesity • Do not keep the laptop on the lap for an extended period • Manage stress • Take a sound sleep • Exercise regularly • Avoid exposure to harmful chemicals and toxic substances • Avoid mobile phone radiation near testes • Do not supplement yourself with sexual vigour-improving drugs without consulting a physician • Keep yourself on a healthy diet WHEN TO VISIT DOCTOR Book an appointment with your doctor if: • You are unable to cause pregnancy in the fertile female partner despite one year of unprotected sex • You have a problem with ejaculation • You have reduced libido • The volume of semen is too low • You are suffering from erectile dysfunction • You have pain or swelling in the testes • You have undergone any testicle or scrotum surgery • You had trauma or injury in your reproductive organs AYURVEDIC TREATMENT OF MALE INFERTILITY Unlike the allopathic treatment, which does not provide a comprehensive management strategy for various causes of male infertility, ayurvedic therapy, from time immemorial, has been considered the best treatment for sexual problems, including male infertility. Best Doctor for Male Infertility in Delhi, Best STI Doctor and STD Specialist in Delhi, Best Doctor for Low Sex Desire in Delhi, Best Doctor for Nightfall in Delhi, Best Doctor for HIV Counselling in Delhi, Best Doctor for Candidiasis in Delhi, Best Doctor for Balanitis in Delhi, Best Doctor for Genital Warts Treatment in India, Best Doctor for Penis Yeast Infection in Delhi, best GONORRHEA TREATMENT IN DELHI, Best Doctors For Chlamydia Treatment In Delhi
#bestperformanceanxietyandayurvedictreatmentindelhi#BestDoctorforPenisYeastInfectioninDelhi#BestSexologistinindia#TOPSEXOLOGISTFORPARAPHIMOSISTREATMENTINDELHI#BESTNIGHTFALLTREATMENTDOCTORSINDELHI#bestdoctorforPARAPHIMOSISINIndia#BestDoctorforLowSpermCountTreatment
1 note
·
View note
Note
Hi! I'm Kayla, and I'm very shy irl, plus I have a disorder called: 2q23.1 microdeletion of a chromosome plus a duplication called 16p.13.11, I rp as sans, Toriel, frisk, plus sometimes I rp as horror sans.
Greetings Kayla!! It’s nice to meet you! ^^
In Narra, but, since everyone calls me that sometimes, you can call me Chara -v-
3 notes
·
View notes
Text
Understanding the Importance of NIPT Test in Pregnancy
Pregnancy is a crucial and exciting phase in a woman’s life, and ensuring the health and wellbeing of the unborn child is every parent’s top priority. With the advancements in prenatal screening, the NIPT Test in pregnancy has emerged as a revolutionary, non-invasive, and highly accurate method for detecting genetic abnormalities in the fetus. At MedGenome Labs, we offer cutting-edge NIPT testing services that empower parents with vital genetic insights early in the pregnancy journey.
What is the NIPT Test in Pregnancy? The Non-Invasive Prenatal Test (NIPT) is a blood test performed during pregnancy that analyzes fetal DNA circulating in the mother’s blood. The test screens for common chromosomal abnormalities such as:
Trisomy 21 (Down syndrome)
Trisomy 18 (Edwards syndrome)
Trisomy 13 (Patau syndrome)
[removed] chromosome conditions like Turner syndrome and Klinefelter syndrome
Unlike traditional screening methods, NIPT is safe, poses no risk of miscarriage, and can be done as early as the 10th week of pregnancy.
Why Choose the NIPT Test in Pregnancy?
High Accuracy: NIPT offers over 99% accuracy in detecting Down syndrome and other chromosomal anomalies.
Early Detection: Allows parents to receive critical genetic information early in the pregnancy, enabling better planning and medical support if needed.
Non-Invasive and Safe: As it requires only a maternal blood sample, it eliminates the risks associated with invasive procedures like amniocentesis.
Peace of Mind: Provides reassurance and reduces anxiety during pregnancy by giving a clear picture of the baby’s genetic health.
Who Should Consider NIPT? Although NIPT is available to all pregnant women, it is especially recommended for those who:
Are aged 35 or older
Have a family history of genetic disorders
Had abnormal results in prior ultrasound or screening tests
Have experienced previous pregnancies with chromosomal abnormalities
Consulting with your gynecologist or genetic counselor can help determine if NIPT is the right choice for you.
The NIPT Process at MedGenome Labs At MedGenome Labs, we ensure a smooth, accurate, and confidential experience. Here’s how the process works:
Sample Collection: A small amount of blood is drawn from the mother.
DNA Analysis: Fetal DNA is extracted and analyzed in our state-of-the-art genomic labs.
Results and Counseling: Within 7–10 days, the results are shared with your healthcare provider, and genetic counseling is offered to explain the findings.
Our NIPT panels also offer optional screening for microdeletions and fetal [removed] determination (as permitted by law), providing a more comprehensive genetic insight.
Why MedGenome Labs? As a leader in genetic diagnostics and genomics research, MedGenome Labs is committed to delivering accurate, timely, and ethical genetic testing services. Our NIPT solutions stand out because of:
Advanced technology and globally recognized platforms
Accredited laboratories with a proven track record
Expert genetic counseling for result interpretation and support
End-to-end care from sample collection to post-test guidance
Conclusion The NIPT Test in pregnancy is a modern, reliable way to screen for chromosomal conditions in the fetus with minimal risk and maximum accuracy. At MedGenome Labs, we bring the power of genomics to prenatal care, helping expectant parents make informed decisions with confidence and peace of mind.
Talk to your doctor today about how NIPT from MedGenome can support your journey to a healthy pregnancy.
0 notes
Text
How to Identify Hereditary Fertility Issues: Tests and Solutions
Introduction: Might Your Family History Be Impacting Your Fertility?
Trying to conceive can be puzzling, emotionally charged, and overwhelming. For others and couples, the explanations are not to be found in lifestyle habits or medical conditions but in genetically inherited characteristics that span generations. If you have a history of reproductive difficulties in your family, you might ask yourself: Is fertility a hereditary condition? More importantly, how can they be detected and treated?
In this blog, we discuss how to identify hereditary fertility problems, the newest diagnostic tests on the market, and the treatments that can provide hope. Whether you’re trying to conceive or experiencing unexplained infertility, this guide will give you insight into how genetics may be affecting your journey.
What Are Hereditary Fertility Problems?
Hereditary fertility disorders are reproductive problems resulting from genetic mutations or chromosomal defects that can be inherited from parents to offspring. Such genetic disorders can influence ovulation, sperm development, hormonal balance, or reproductive organ structure.
Prevalent Hereditary Fertility Disorders
Klinefelter Syndrome (additional X chromosome in males)
Turner Syndrome (absent X chromosome in females)
Fragile X Premutation (associated with premature ovarian failure)
Polycystic Ovary Syndrome (PCOS) with familial patterns
Y Chromosome Microdeletions (which impact sperm production)
Mutations in Cystic Fibrosis Gene (associated with missing vas deferens in men)
If these diseases are in your family, early testing and intervention can really increase your odds of a successful pregnancy.
Signs You Might Have an Inherited Fertility Problem
Although not every fertility issue is inherited, some patterns can suggest a genetic connection.
Watch Out For:
A history of early menopause or ovarian failure in your family
Male relatives with low sperm count or azoospermia
Recurrent miscarriages within the family
Known chromosomal disorders in close relatives
Delayed or absent puberty in family members
Discussing your family’s reproductive health history with your doctor can be an essential first step. Ayuh Fertility Centre offers in-depth consultation services to guide you through the process.
0 notes
Text
Understanding the Causes of Male Infertility

Infertility is often thought of as a women’s health issue, but in reality, male infertility contributes to nearly 40-50% of all infertility cases. Understanding the underlying causes is the first step toward finding effective treatment and building the family you desire.
As a specialist in reproductive health, Dr. Swapnil Langde highlights the key causes of male infertility that every couple should be aware of.
⚠️ Common Causes of Male Infertility
1. Low Sperm Count (Oligospermia)
A low sperm count means fewer than 15 million sperm per milliliter of semen. This reduces the chances of fertilizing an egg naturally.
2. Poor Sperm Motility
Sperm motility refers to the ability of sperm to swim efficiently. If sperm cannot move properly, they cannot reach and fertilize the egg.
3. Abnormal Sperm Shape (Teratospermia)
Sperm with abnormal shape or structure often struggle to penetrate the egg, affecting fertility.
4. Hormonal Imbalances
Imbalances in hormones such as testosterone, FSH, and LH can negatively impact sperm production and overall reproductive health.
5. Varicocele (Swollen Veins in the Scrotum)
This is one of the most common, treatable causes of male infertility. Varicocele affects sperm quality and production by increasing the temperature in the testicles.
6. Infections
Sexually transmitted infections (STIs) like chlamydia or gonorrhea, as well as other infections, can damage sperm health or cause blockages.
7. Lifestyle Factors
Unhealthy habits such as smoking, excessive alcohol consumption, drug use, obesity, and poor diet can all contribute to reduced fertility.
8. Exposure to Environmental Toxins
Prolonged exposure to harmful chemicals, radiation, heavy metals, or excessive heat (like hot baths or saunas) can lower sperm count and quality.
9. Genetic Factors
In some cases, genetic conditions such as Klinefelter syndrome or Y chromosome microdeletions can impair sperm production.
10. Ejaculation Disorders
Issues such as retrograde ejaculation (semen entering the bladder instead of exiting the penis) can interfere with conception.
🩺 When to Seek Help?
If you and your partner have been trying to conceive for 12 months or more without success, it’s essential to consult a specialist. Dr. Swapnil Langde offers advanced diagnostic tests and personalized treatment plans to help overcome male infertility challenges.
🌟 Expert Care for Male Fertility
Early diagnosis and the right approach can significantly improve the chances of conception. Don’t hesitate to seek professional guidance.
Schedule a consultation with Dr. Swapnil Langde today and take a step toward parenthood.
0 notes
Text
Best Azoospermia Treatment In Hyderabad | Gachibowli - Dr Sravya Buggana
Best Azoospermia Treatment In Hyderabad, Gachibowli – Dr. Sravya Buggana | Expert Fertility Specialist
If you are seeking the Best Azoospermia Treatment In Hyderabad, Gachibowli, Dr. Sravya Buggana offers expert diagnosis, advanced medical solutions, and compassionate support to help you or your partner overcome male infertility and move forward on the journey to parenthood.
Understanding Azoospermia
Azoospermia is a medical condition characterized by the complete absence of sperm in the ejaculate. It affects about 1% of the male population and 10–15% of infertile men. While it may sound alarming, modern medicine offers hope. With the right specialist, even men diagnosed with azoospermia can father biological children.
This is where Dr. Sravya Buggana, known for offering the Best Azoospermia Treatment In Hyderabad, Gachibowli, steps in. She brings advanced diagnostics, targeted treatments, and personalized care to help couples address male-factor infertility effectively.
Meet Dr. Sravya Buggana
Dr. Sravya Buggana is a highly respected fertility and reproductive health expert based in Gachibowli, Hyderabad. With years of experience and a specialized focus on male and female infertility, she provides evidence-based solutions to even the most complex fertility challenges.
As the go-to choice for the Best Azoospermia Treatment In Hyderabad, Gachibowli, Dr. Sravya has helped countless couples understand their diagnosis and take actionable steps toward achieving pregnancy.
Causes of Azoospermia
Azoospermia can be classified into two main types:
Obstructive Azoospermia – Caused by a blockage or obstruction in the reproductive tract, preventing sperm from entering the ejaculate.
Non-Obstructive Azoospermia – Caused by decreased or absent sperm production due to hormonal imbalance, genetic conditions, or testicular failure.
Identifying the type of azoospermia is critical to choosing the correct treatment path, which is why getting the Best Azoospermia Treatment In Hyderabad, Gachibowli is so important. Dr. Sravya uses a comprehensive diagnostic process, including hormonal testing, scrotal ultrasound, and sometimes testicular biopsy, to identify the underlying cause.
Treatment Options for Azoospermia
Dr. Sravya offers tailored treatments based on the type and cause of azoospermia. Options may include:
Hormonal Therapy – For cases related to hormone imbalances such as low FSH, LH, or testosterone.
Surgical Procedures – Such as varicocelectomy or reconstructive surgery for obstructive azoospermia.
Sperm Retrieval Techniques – Including TESE (Testicular Sperm Extraction), PESA (Percutaneous Epididymal Sperm Aspiration), and micro-TESE, which are often used in conjunction with IVF/ICSI.
Genetic Counseling – For cases involving chromosomal abnormalities or Y-chromosome microdeletions.
As the Best Azoospermia Treatment In Hyderabad, Gachibowli, Dr. Sravya ensures that every patient receives a customized plan that maximizes the potential for conception—whether through natural means or assisted reproductive techniques.
Why Choose Dr. Sravya Buggana?
Here’s why Dr. Sravya is widely regarded as offering the Best Azoospermia Treatment In Hyderabad, Gachibowli:
Advanced Diagnostics: Accurate identification of the root cause using cutting-edge technology.
Personalized Treatment Plans: Every case is unique, and so are the treatment strategies.
High Success Rates: Proven outcomes in male-factor infertility and successful pregnancies.
Transparent Communication: Patients are educated and involved in decision-making at every step.
Modern Clinic in Gachibowli: Convenient, private, and fully equipped with the latest tools.
Patient Testimonials
Many couples who previously struggled with unexplained male infertility found hope and success under Dr. Sravya’s care. Here’s what one patient had to say:
"We were devastated after learning about my azoospermia diagnosis, but Dr. Sravya guided us with care and expertise. She explained every step and gave us the confidence to try sperm retrieval with ICSI. We are now expecting our first child thanks to her. She truly provides the Best Azoospermia Treatment In Hyderabad, Gachibowli."
Convenient Location and Supportive Environment
Located in the heart of Gachibowli, Dr. Sravya’s clinic is easily accessible to patients from Madhapur, Kondapur, Hitech City, and the Financial District. The clinic maintains high standards of hygiene, privacy, and professionalism—ideal for patients seeking sensitive care.
Her friendly staff, efficient appointment scheduling, and optional teleconsultations further make the experience comfortable and stress-free. It’s not just the treatment—it’s the journey that makes Dr. Sravya’s practice the Best Azoospermia Treatment In Hyderabad, Gachibowli.
Book a Consultation Today
If you or your partner has been diagnosed with azoospermia, don’t lose hope. Early intervention, the right diagnostic tools, and personalized treatment make all the difference.
Take the first step toward parenthood with confidence—book an appointment with Dr. Sravya Buggana today and experience the Best Azoospermia Treatment In Hyderabad, Gachibowli.
Conclusion
Azoospermia may sound like a roadblock, but with the right guidance and treatment, many couples go on to achieve successful pregnancies. Dr. Sravya Buggana, known for offering the Best Azoospermia Treatment In Hyderabad, Gachibowli, is your trusted partner in overcoming male infertility with expertise, empathy, and excellence.
0 notes
Text
0 notes
Text
What genetic tests are available to detect inherited fertility issues?
There are several genetic tests that can help find out if fertility problems are caused by something inherited from your family. These tests can help both men and women understand the root cause of infertility — especially when other tests are normal.
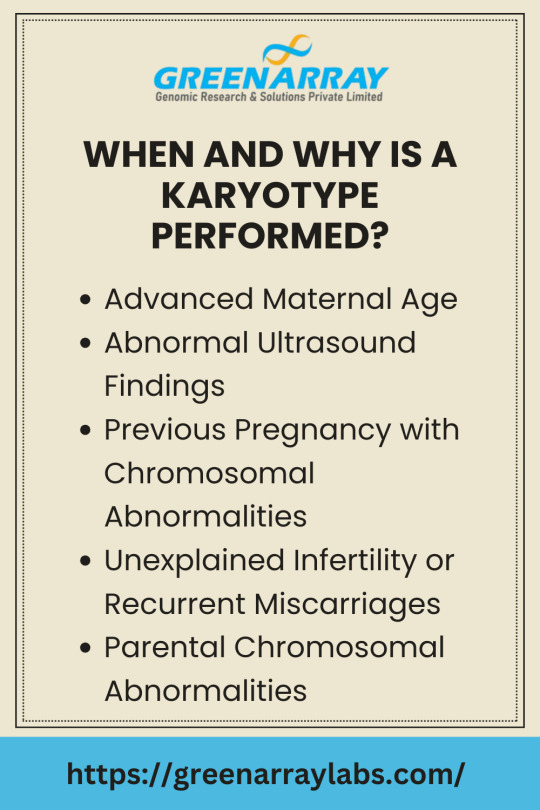
🔹 Karyotyping (Chromosome Analysis): This test checks the number and structure of chromosomes in your cells. It can detect problems like missing or extra chromosomes, which may lead to infertility or repeated miscarriages.
🔹 Carrier Screening: This test shows if you or your partner carry any hidden genetic diseases (like cystic fibrosis or thalassemia) that could be passed to your child. It’s useful even if you don’t have symptoms.
🔹 Y Chromosome Microdeletion Test (for men): This is done for men with very low or no sperm count. It checks for missing pieces in the Y chromosome that are linked to sperm production problems.
🔹 Fragile X Testing (for women): This test helps check for premature ovarian failure or early menopause risk caused by a change in the FMR1 gene.
🔹 Preimplantation Genetic Testing (PGT): Used during IVF, this test checks embryos for genetic problems before they are transferred to the uterus. It increases the chance of a healthy pregnancy.
If you have a family history of infertility, or if you’ve had IVF failures or miscarriages, these tests can help. A fertility doctor or genetic counselor can guide you on which test is best.
0 notes
Text
Understanding Karyotyping and Its Uses in Cytogenetics
Introduction
Cytogenetics is a branch of genetics that focuses on the study of chromosomes—the thread-like structures within our cells that carry DNA. Through specialized laboratory techniques, cytogenetic testing allows scientists and physicians to analyze the number, structure, and behavior of chromosomes, providing essential information for diagnosing genetic disorders, congenital abnormalities, and certain types of cancer.
This powerful diagnostic tool bridges the gap between molecular genetics and clinical medicine, helping uncover the root causes of health conditions that often remain hidden.
What Is Cytogenetics?
Cytogenetics refers to the study of chromosomes and their relation to disease. It involves examining:
Chromosome number
Chromosome structure
Chromosomal abnormalities like deletions, duplications, translocations, inversions, or rings
Cytogenetic analysis can be performed on a variety of sample types, including blood, bone marrow, amniotic fluid, placenta, and even tumor tissue.
Key Techniques in Cytogenetics
1. Karyotyping
A karyotype is a visual representation of all 46 chromosomes, arranged in pairs. This method detects large-scale changes like:
Trisomy (e.g., Down syndrome with an extra chromosome 21)
Monosomy (e.g., Turner syndrome, where one X chromosome is missing)
Translocations (rearrangement of genetic material)
2. Fluorescence In Situ Hybridization (FISH)
FISH uses fluorescent probes to detect and locate specific DNA sequences on chromosomes. It's especially useful for:
Rapid prenatal diagnosis
Identifying gene fusions in leukemias and lymphomas
Detecting microdeletions or duplications too small for karyotyping
3. Comparative Genomic Hybridization (CGH)
CGH allows for genome-wide screening of DNA copy number changes. It is often used when there's suspicion of subtle chromosomal imbalances involved in developmental disorders or congenital anomalies.
Applications of Cytogenetics
1. Diagnosing Genetic Disorders
One of the most common uses of chromosome analysis is identifying genetic syndromes. Conditions such as:
Down syndrome
Edward syndrome
Patau syndrome
Klinefelter syndrome
are all diagnosed through cytogenetic techniques. Early detection allows for better medical management and genetic counseling.
2. Prenatal Testing
Cytogenetics plays a crucial role in prenatal diagnostics via:
Amniocentesis
Chorionic villus sampling (CVS)
These tests identify chromosomal abnormalities in a fetus, helping expectant parents make informed decisions.
3. Cancer Cytogenetics
In oncology, cytogenetic analysis of bone marrow or tumor samples is essential in diagnosing:
Leukemias (e.g., Philadelphia chromosome in CML)
Lymphomas
Solid tumors (e.g., Ewing sarcoma)
Certain chromosomal abnormalities help predict disease progression, treatment response, and prognosis.
4. Infertility and Reproductive Health
Cytogenetics is used in evaluating:
Recurrent miscarriages
Infertility
Preimplantation genetic diagnosis (PGD) during IVF
Abnormal chromosomal patterns in either parent may be the cause of conception challenges.
Cytogenetics vs Molecular Genetics
While cytogenetics focuses on large chromosomal changes, molecular genetics dives deeper into mutations at the DNA sequence level. Increasingly, both disciplines are integrated for a comprehensive diagnostic picture.
For example:
Cytogenetics may detect a chromosomal deletion.
Molecular testing (like PCR or sequencing) can pinpoint which gene within that region is disrupted.
Limitations of Cytogenetics
Cannot detect single-nucleotide changes (point mutations)
Some subtle rearrangements may escape detection on conventional karyotyping
Requires live, dividing cells, which may not always be obtainable
For more precise or smaller-scale changes, next-generation sequencing (NGS) or whole exome/genome sequencing may be recommended.
The Future of Cytogenetics
The field is rapidly evolving. Advances such as chromosomal microarray analysis (CMA) and digital karyotyping are making cytogenetic evaluations more accurate and automated. Additionally, integrating cytogenetics with AI-powered image analysis and big data genomics is expected to revolutionize personalized medicine.
Why Cytogenetics Still Matters
Despite the rise of molecular testing, cytogenetics remains:
The gold standard for detecting many chromosomal abnormalities
Indispensable in hematologic malignancies
A cost-effective method for initial genetic screening in many cases
For clinicians and genetic counselors, it provides a crucial starting point in the diagnostic process.
Conclusion
Cytogenetics offers a window into the very blueprint of life—our chromosomes. By detecting chromosomal abnormalities that underlie a wide range of medical conditions, cytogenetic testing continues to be an essential part of modern diagnostics. From birth defects and developmental delays to cancer and infertility, cytogenetics helps uncover the genetic story behind each condition, guiding more accurate diagnoses and targeted treatments.
0 notes
Text
Understanding Male Infertility Causes: Insights from Dr. ALKA IVF
Infertility affects millions of couples worldwide, and while female fertility issues often receive significant attention, male infertility is an equally critical part of the equation. At Dr. ALKA IVF, we understand the emotional and physical toll infertility can take on individuals and couples. That’s why we offer a compassionate, science-driven approach to diagnosing and treating male infertility. In this article, we will explore the various male infertility causes, their impact, and the modern treatment options available.
What is Male Infertility?
Male infertility refers to a man's inability to cause pregnancy in a fertile female partner. It typically relates to issues with the quantity or quality of sperm. A thorough evaluation is necessary to determine the root cause, and at Dr. ALKA IVF, we employ advanced diagnostic tools and expertise to offer accurate assessments.
Common Male Infertility Causes
There are several potential male infertility causes, ranging from lifestyle factors to medical conditions. Understanding these causes is crucial to finding the right treatment path. The most common causes include:
1. Low Sperm Count (Oligospermia)
One of the most common male infertility causes is a low sperm count. A healthy sperm count should be at least 15 million sperm per milliliter of semen. When the count is significantly lower, it reduces the likelihood of fertilization.
2. Poor Sperm Motility
Sperm motility refers to the sperm's ability to move effectively. If the sperm cannot swim through the female reproductive tract to reach the egg, conception becomes unlikely. Poor motility can result from structural defects or underlying health conditions.
3. Abnormal Sperm Morphology
The shape and structure of sperm are also important for fertility. Abnormally shaped sperm may struggle to penetrate and fertilize the egg. Genetic factors, lifestyle habits, and health problems can all lead to poor sperm morphology.
4. Varicocele
A varicocele is a swelling of the veins that drain the testicle and is one of the leading male infertility causes. It can increase the temperature of the testicles, which may impair sperm production and quality. Fortunately, this condition is treatable through minimally invasive surgery or assisted reproductive technologies.
5. Hormonal Imbalances
Hormones like testosterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) play a vital role in sperm production. Any imbalance in these hormones can lead to decreased sperm count and motility. Hormonal issues may result from thyroid disorders, pituitary gland problems, or certain medications.
6. Infections and STIs
Sexually transmitted infections (STIs), such as chlamydia or gonorrhea, can cause inflammation and blockages in the male reproductive tract. Other infections like mumps (if it affects the testicles) can also impact fertility. At Dr. ALKA IVF, infection screening is a standard part of male fertility assessments.
7. Ejaculation Issues
Problems such as retrograde ejaculation, where semen enters the bladder instead of exiting the penis, can hinder fertility. Erectile dysfunction or premature ejaculation may also contribute to difficulty in achieving conception.
8. Genetic Disorders
Some male infertility causes are genetic in nature. Conditions like Klinefelter syndrome or Y chromosome microdeletions can impair sperm production. Genetic testing can identify these issues and guide appropriate treatments.
9. Environmental and Occupational Factors
Prolonged exposure to toxins, such as pesticides, heavy metals, or radiation, can negatively affect sperm production. Certain professions involving high heat exposure or sedentary work may also be contributing factors.
10. Lifestyle Factors
Smoking, excessive alcohol consumption, use of recreational drugs, obesity, and chronic stress are significant male infertility causes. At Dr. ALKA IVF, we encourage lifestyle modifications as a first step toward improving fertility outcomes.
Diagnosis at Dr. ALKA IVF
A comprehensive evaluation is essential to pinpoint the specific male infertility causes. At Dr. ALKA IVF, we offer a full range of diagnostic tests, including:
Semen analysis
Hormonal profiling
Scrotal ultrasound
Genetic testing
Post-ejaculation urinalysis
Our experienced team ensures a thorough and respectful evaluation process, designed to help you understand the underlying causes and available solutions.
Treatment Options
Once we determine the cause, treatment can begin. Depending on the diagnosis, treatment may include:
Medication for hormonal imbalances or infections
Surgical interventions for varicocele or blockages
Assisted reproductive technologies (ART) such as IUI, IVF, or ICSI
Lifestyle counseling to address smoking, weight, or substance use
Dr. ALKA IVF also offers sperm retrieval techniques and donor sperm options when necessary. Our personalized treatment plans aim to maximize the chances of success while minimizing emotional stress.
Emotional Support and Counseling
Male infertility can take a psychological toll. Feelings of guilt, shame, and frustration are common. That’s why we offer counseling and support services alongside medical treatment. Our goal at Dr. ALKA IVF is to support every aspect of your fertility journey.
Conclusion
Understanding the various male infertility causes is the first step toward addressing and overcoming them. With advancements in diagnostics and treatments, many men who once faced significant fertility challenges now have the opportunity to become fathers. At Dr. ALKA IVF, we are committed to delivering compassionate care, cutting-edge treatments, and unwavering support.
If you or your partner are struggling with fertility, don’t hesitate to consult the specialists at Dr. ALKA IVF. Together, we can explore your options and take the next step toward building your family.
0 notes
Text
Pregnancy is an exciting journey, but it also comes with concerns about the health of the unborn baby
Introduction
Pregnancy is an exciting journey, but it also comes with concerns about the health of the unborn baby. Thanks to advancements in medical technology, expecting parents can now get accurate and early insights into their baby’s genetic health through NIPT test in Dubai. Non-Invasive Prenatal Testing (NIPT) is a revolutionary screening method that detects chromosomal abnormalities with high accuracy, without posing any risk to the mother or the fetus.
If you're considering prenatal genetic testing in Dubai, this comprehensive guide will cover everything you need to know about NIPT Dubai, including its benefits, how it works, where to get it, and why it’s a preferred choice for many parents.
What is the NIPT Test?
The NIPT test (Non-Invasive Prenatal Testing) is a cutting-edge blood test that analyzes fetal DNA present in the mother’s bloodstream to screen for genetic conditions such as Down syndrome (Trisomy 21), Edwards syndrome (Trisomy 18), and Patau syndrome (Trisomy 13). Unlike invasive tests like amniocentesis, NIPT in Dubai is completely safe and carries no risk of miscarriage.
How Does the NIPT Test Work?
Simple Blood Draw – The mother’s blood is drawn, usually after the 10th week of pregnancy.
DNA Analysis – The lab examines cell-free fetal DNA (cffDNA) circulating in the mother’s blood.
Chromosomal Screening – The test checks for extra or missing chromosomes linked to genetic disorders.
Results Delivery – Reports are typically available within 7-14 days, providing a risk assessment for genetic conditions.
Why Choose NIPT Test in Dubai?
Dubai is home to world-class medical facilities offering advanced prenatal genetic testing Dubai. Here’s why expecting parents opt for NIPT Dubai:
High Accuracy – Detects chromosomal abnormalities with over 99% accuracy.
Non-Invasive & Safe – No risk to the baby, unlike amniocentesis or CVS.
Early Detection – Can be done as early as 10 weeks into pregnancy.
Gender Reveal – Some tests also determine the baby’s gender with high precision.
Reduces Need for Invasive Tests – Helps avoid unnecessary invasive procedures.
Conditions Detected by NIPT in Dubai
The NIPT test screens for several genetic conditions, including:
Down Syndrome (Trisomy 21)
Edwards Syndrome (Trisomy 18)
Patau Syndrome (Trisomy 13)
Sex Chromosome Abnormalities (Turner syndrome, Klinefelter syndrome)
Microdeletion Syndromes (Optional in some advanced tests)
Who Should Consider NIPT Testing?
While NIPT Dubai is available to all pregnant women, it is especially recommended for:
Women over 35 (Higher risk of chromosomal abnormalities)
Previous pregnancy with genetic disorders
Abnormal ultrasound findings
Family history of genetic conditions
Those seeking early and accurate screening
NIPT Test Cost in Dubai
The NIPT test cost in Dubai varies depending on the clinic and the extent of screening. Basic NIPT tests start from AED 3,500, while more comprehensive panels can go up to AED 6,000. Many insurance providers now cover NIPT in Dubai, so it’s best to check with your provider.
Best Clinics for NIPT Test in Dubai
Dubai has several leading healthcare providers offering prenatal genetic testing Dubai, including:
Feto Maternal & GenetYX Center
Mediclinic City Hospital
American Hospital Dubai
King’s College Hospital Dubai
HealthBay Polyclinic
These clinics use state-of-the-art technology and provide expert genetic counseling to ensure accurate results.
NIPT vs. Traditional Prenatal Screening
Feature
NIPT Test
Traditional Screening (e.g., Triple Test)
Accuracy
>99%
80-90%
Risk
Non-invasive
Low risk, but less accurate
Timing
From 10 weeks
11-13 weeks (combined test)
Detection
Multiple conditions
Limited conditions
Frequently Asked Questions About NIPT in Dubai
1. Is NIPT Test in Dubai Safe?
Yes, NIPT Dubai is completely safe as it only requires a blood sample from the mother.
2. How Accurate is the NIPT Test?
The NIPT test has an accuracy rate of over 99% for detecting major chromosomal abnormalities.
3. Can NIPT Replace Diagnostic Tests Like Amniocentesis?
While highly accurate, NIPT in Dubai is a screening test, not diagnostic. In case of high-risk results, doctors may recommend confirmatory tests.
4. Does Insurance Cover NIPT in Dubai?
Some insurance plans cover NIPT test cost in Dubai, especially for high-risk pregnancies. Check with your provider.
5. When Should I Get the NIPT Test Done?
The best time for prenatal genetic testing Dubai is between 10 to 22 weeks, with optimal results at 10+ weeks.
Conclusion
The NIPT test in Dubai is a game-changer in prenatal care, offering expecting parents peace of mind with its high accuracy and safety. Whether you’re at high risk or simply want the best screening available, NIPT Dubai provides reliable insights into your baby’s genetic health.
If you’re considering prenatal genetic testing Dubai, consult with a specialist to determine if NIPT is right for you. With world-class medical facilities and expert care, Dubai remains a top destination for advanced pregnancy screenings.
0 notes