#lumbar stress fracture
Text
🛁Body & Health🧼
🛁6th house is also about your health. How you can get sick or which part of the body may be most vulnerable. Of course, there are other factors as to why and how. But the 6th house is connected to your body, which means that there are things here that can have the greatest impact on your body.
☀️Sun in 6th house you can be prone to exertion. Many times your heart and hair can suffer. Back, spine and immune system -They can many times be affected. It is good if you eat a lot of vitamins. Exercise is also very important. The more you move, the more energy you will have. Heart disease is often confirmed in men due to excessive strain. Herbs good for you: sunflower, calendula, mistletoe, juniper, laurel, chamomile, cinnamon, rosemary.
🌙Moon in 6th house you can be prone to depression. Emotional stress can greatly affect health. You must not be emotionally burdened with work. Your body can recover quickly even after a serious illness if you are emotionally stable. Parts of the body you have to be careful are: breasts, mammary glands, esophagus, stomach, intestines, salivary gland, liver, gallbladder, intestine. Herbs good for you: anise, cabbage, camphor, cucumber, iris, jasmine, lettuce, lily, poppy, violet, willow, lotus, moonwort, mugwort, pumpkin.
🍀Mercury in 6th house-you can be prone to stress. The nervous system is weak and sometimes they are threatened by tension and stress due to the fast pace of life. You have to remind yourself that it is necessary calm down and relax every now and then and try to eat regularly. The brain, lungs, respiratory system and nervous system can be affected the most. With mercury here The lungs are a potential weak point because it's a common cold may develop a persistent cough. Also shoulders, arms and hands. These can be susceptible to injuries such as sprains or fractures. Herbs good for you: lilies of the valley, marjoram, fern, lavender, fennel, anise, mint, thyme, dill, lemon grass.
🍒Venus in 6th house- you can be prone to prone to unpleasantness. Many times it can be something that affects your appearance, your beauty. People with this placement can fluctuate a lot with their body weight. They also tend to tighten in the neck, which is usually the result of tension that has accumulated over time. Because they want to remain calm, most of the time feelings of anger and stress. Parts of the body that may be most prone to damage: throat, kidneys, lumbar region. Herbs good for you: birch, walnut, almond, violet, narcissus, elder, poppy, passion fruit, fig, peach, apricot, olive.
🦋Mars in 6th house- you are prone to irritation. Many times you can get injured during sports or activities. It is not recommended to do things that are dangerous. Many times you can burden yourself too much by being able to finish or do something. You can often be prone to migraines and headaches. Even to a hot temperature, which otherwise quickly disappears. It is not recommended that they be active when they are tired. It can mean that you have too fast a pace of life, which can mean that you skip the main meals (which can lead to digestive problems). Parts of the body that may be most prone to damage: head, muscles, adrenal glands, fetuses. Herbs good for you: pine, pepper, hot pepper, nettle, cherry, radish, horseradish, onion, garlic, ginger, tobacco.
🫧Jupiter in 6th house-Jupiter is usually good in this house because it represents happiness luck abundance. So most likely you will be very blessed with your health. However, you may be inclined to react too impulsively or optimistically to certain health problems. Even if they get sick, they recover quickly. The thinness of the stems is rich food and wine, which can lead to obesity, especially in middle age. They tend to overeat, which can overload the liver. In later years, arthritis and rheumatism affects the hips. Parts of the body that may be most prone to damage: thighs, liver. Herbs good for you: oak, pine, maple, birch, willow, cherry, pear, licorice, moss, wheat, nutmeg, saffron, clover.
🪐Saturn in 6th house-you can be prone to burdnes. Sometimes you can have too much stuff. You are stressing too much and giving yourself too much stress and limitations. When they're exhausted, their weakened immune systems can't cope with minor ailments as easily, and unrelieved tension can prevent a good night's sleep. The main body parts associated with it signs are knees, teeth and bones. Over the years, joints can become stiff. Meticulous dental care is required. They are prone to strong melancholy and can gradually begin to sink into depression. Parts of the body that may also be prone to damage : gall bladder, spleen. Herbs good for you: cypress, hemp, wolf cherry, moss, cumin, ivy, sage.
🪼Neptune in 6th house- you may be prone to self-inflicted diseases. Things can be confusing and not clear. They can get diseases from computers, phones and other modern technology and pollutants. Mysterious health problems that modern medicine cannot define or explain. Complementary therapies may help you more. Since Neptune and Pisces are associated with the feet, this part can be the most affected. Pisces often under severe stress they seek solace in alcohol and drugs. A foot massage will be good for you. Parts of the body that may be most prone to damage : nervous system, feet. Herbs good for you: water lily, mushrooms
🧃Uranus in 6th house- You may be more sensitive to the cold. Diseases that can appear are often related to unknown or strange things. They have an intense mind that needs plenty of stimulation, but they are not always in tune with their body's needs. Daily lack of movement causes a decline in energy and circulation. During the winter months, numb fingers and feet can swell if nothing else take action. Uranus is also associated with the ankles so people can be prone to sprains. They can exercise caution and must wear appropriate footwear. They are also subjected sudden illnesses that then disappear without a trace. Parts of the body that may be most prone to damage: ankles, blood circulation. Herbs good for you:orchid
🐚Pluto in 6th house- They are extremely durable and resistant, which means that they are generally healthy. Some diseases that may be related to them are of a more psychosomatic origin. They may also be prone to nervous tension, which can affect the muscles of the shoulders, neck, and back. A massage is good. The main parts of the body are the bladder and large intestine. It is important that they excrete toxins. It is also good to do a detox diet every now and then. Parts of the body that may be most prone to damage: miscarried, gave birth, bowels. Herbs good for you:eggplant, beetroot, pomegranate, daffodil.
🎸For personal readings u can sign up here: https://snipfeed.co/bekylibra 🎸
-Rebekah🧚🏼♀️💕🌙
399 notes
·
View notes
Note
hiya! so basically, in my story Whumper forces Whumpee to walk for hours across fields in summer. what could this lead to? (worse the better thx!)
There's plenty of damage to be done there!
Chronic fatigue
Sore, stiff, strained muscles and joints
Old injuries flaring up
Loss of weight and appetite
Sunburns
Dehydration
Neuroma
Shin splints
Lumbar strain
Stress fractures
Blisters, bunions and sores
Plantar fasciitis, bursitis, tendinitis
Bug bites/stings and prickers
Heat exhaustion or heat stroke
#whump#overworking#summer#dehydration#heat exhaustion#heat stroke#soreness#stress#chronic pain#answered ask#anonymous
102 notes
·
View notes
Text
Here's the diagnoses on my rehab transfer paperwork:
Anxiety disorder, unspecified
Acute stress reaction
Hypo-osmolality and hyponatremia (this is why I was in the ICU getting blood drawn every 2 hours, low sodium can kill you or cause all kinds of permanent damage)
Other specified post-procedural states (???)
Constipation, unspecified
Dietary zinc deficiency
Insomnia, unspecified
Pedestrian injured in traffic accident involving unspecified motor vehicles
Pneumothorax, unspecified
Multiple fractures of pelvis with stable disruption of pelvic ring
Displaced fracture of body of left calcaneous
Other fracture of second thoracic vertebra
Unspecified fracture of fifth lumbar vertebra
Unspecified fracture of sacrum
Unsteadiness on feet
Other symptoms and signs involving the musculoskeletal system (???)
Muscle weakness (generalized)
Weakness
6 notes
·
View notes
Text
About that chronic pain...
Doc ordered X-rays of my lower back, because we're seriously considering that I may have ankylosing spondylitis. We were honestly expecting the x-rays to come back with nothing remarkable, because you have to have the disease for about 10 years before it starts to show up on the x-rays.
Got the x-rays today. Report just showed up.
Findings: Vertebral body heights are maintained. Lumbar alignment is anatomic. No acute displaced fractures. Mild disc height loss noted at L3-L4 and L4-L5. Multilevel facet degeneration is noted, most significantly in the lower lumbar segments. Soft tissues are grossly unremarkable, with surgical clips in the right upper abdominal quadrant.
Conclusion: Relatively mild multilevel lumbar spondylosis, most significantly involving the lower lumbar segments. If symptoms persist, consider CT or MRI for further characterization.
So ummm... I guess all those years of my "back going out" and subsequently being unable to walk for days after the incident (I would discover after years that if I aggressively treated with around the clock ibuprofen, and did massage to loosen my muscles, I could keep myself walking... barely), was probably not connected to the "injury" I sustained at 19 years old? Might even be that the "injury" I got at 19 was actually a flare triggered by placing too much stress on my spine.
Go. Fucking. Figure.
I'm laughing at the frustration, at being right, AGAIN, at what is wrong with me. Can I please shove this in the face of every doctor that ever doubted me and blamed my pain on my weight?
Also, newsflash, assholes. Chronic inflammation makes people gain weight.
I'm pissed that I'm right. Again. And grateful someone finally listened.
Anyway. End rant. At least until the official diagnosis comes back, but all signs point to ankylosing spondylitis.
3 notes
·
View notes
Text
OOC
Thought I’d give you all an update. My sister had to have a hysterectomy as well, but it was successful and she is currently in remission. I also have a new dog, or rather an old one, as I rescued a ten year-old Boston terrier a few moths ago. He’s a goofball, but so adorable! My back has gotten worse though. Turns out I have a stress fracture on my pelvis, in addition to arthritis, degenerative disc disease, and mild scoliosis, with spina bifida occulta further aggravating my lumbar pain. Anyway, I’m still on the fence about returning to tumblr. My mental state does seem better away from it.
6 notes
·
View notes
Text
The Jewett Brace is an orthopedic device used to manage spinal conditions by limiting forward flexion and supporting the thoracic and lumbar spine. It is typically prescribed for patients with stable spinal fractures, osteoporosis, or post-surgical stabilization. The brace consists of a metal frame with padded sternal and pubic pads connected by lateral bars and an abdominal pad. It helps in maintaining spinal alignment and promoting healing by reducing movement and stress on the spine. For more information, you can visit Tabeeb Medical.
0 notes
Text
Finding a Spondylolisthesis Specialist in Navi Mumbai, Mumbai

Effective Spondylolisthesis Treatment in Navi Mumbai, Mumbai
Spondylolisthesis is a spinal disorder in which one vertebra slips out of place relative to the vertebra below it. This slippage can cause pain, numbness, and weakness in the lower back and legs. While spondylolisthesis can occur at any level of the spine, it most commonly affects the lower back (lumbar spine).
This article will provide a comprehensive overview of spondylolisthesis treatment in Navi Mumbai, Mumbai. We will discuss the causes, symptoms, diagnosis, and various treatment options available, including both non-surgical and surgical approaches.
Causes of Spondylolisthesis
There are several factors that can contribute to the development of spondylolisthesis. These include:
Degenerative changes: Over time, the discs between the vertebrae can wear down, which can lead to instability and slippage.
Spondylolysis: This is a stress fracture in the pars interarticularis, a small portion of bone that connects the facet joints of the vertebrae. Spondylolysis can weaken the spine and make it more susceptible to slippage.
Congenital defects: Some people are born with malformations in the spine that make them more likely to develop spondylolisthesis.
Trauma: A sudden impact or injury to the spine can cause a vertebra to slip out of place.
Repetitive stress: Activities that put repeated stress on the spine, such as gymnastics or weightlifting, can increase the risk of spondylolisthesis.
Symptoms of Spondylolisthesis
The most common symptom of spondylolisthesis is lower back pain. The pain may be worse with activity and improve with rest. Other symptoms can include:
Radiating pain down the legs (sciatica)
Muscle stiffness and tightness
Weakness in the legs
Numbness or tingling in the legs
Changes in bowel or bladder function (in severe cases)
Diagnosis of Spondylolisthesis
If you are experiencing any of the symptoms of spondylolisthesis, it is important to see a doctor for diagnosis. The doctor will ask about your medical history and symptoms, and perform a physical examination. They may also order imaging tests, such as X-rays, MRIs, or CT scans, to get a better look at your spine.
Spondylolisthesis Treatment in Navi Mumbai, Mumbai
The treatment for spondylolisthesis will depend on the severity of your condition and your individual needs. In most cases, non-surgical treatment is effective in managing the pain and preventing the slippage from worsening. Non-surgical treatment options include:
Rest: Taking a break from activities that aggravate your pain can allow the inflammation to subside and promote healing.
Physical therapy: A physical therapist can teach you exercises to strengthen the muscles that support your spine and improve your flexibility.
Medication: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help to relieve pain and inflammation. In some cases, your doctor may prescribe stronger pain medication or muscle relaxants.
Activity modification: Avoiding activities that put a strain on your spine can help to prevent further slippage.
Bracing: A back brace can help to support your spine and reduce pain.
Surgical Treatment for Spondylolisthesis
If non-surgical treatment is not effective in managing your pain or if the slippage is severe, surgery may be an option. There are a variety of surgical procedures that can be used to treat spondylolisthesis, depending on the specific location and severity of the condition. Some common surgical procedures include:
Pars repair: This procedure is used to repair a stress fracture in the pars interarticularis.
Spondylodesis: This procedure involves fusing together two or more vertebrae to prevent them from slipping.
Laminectomy: This procedure involves removing a portion of the lamina, the back part of the vertebra, to create more space for the spinal cord and nerves.
If you are considering surgery for spondylolisthesis, it is important to find an experienced and qualified surgeon. Look for a surgeon who is board-certified in orthopedic surgery or neurosurgery and who has experience treating spondylolisthesis.
Conclusion
Spondylolisthesis is a spinal disorder that can cause pain, numbness, and weakness in the lower back and legs. There are a variety of treatment options available, including both non-surgical and surgical approaches. If you are experiencing symptoms
Schedule regular appointments to monitor treatment response, watch for complications, and adjust the treatment plan accordingly. Call��93726 71858 | 93211 24611 to schedule an appointment with Synapse Spine for Spondylolisthesis Treatment in Navi Mumbai, Mumbai.
0 notes
Text
CONSIDERING LUMBAR FUSION | DR. DILIP KIYAWAT
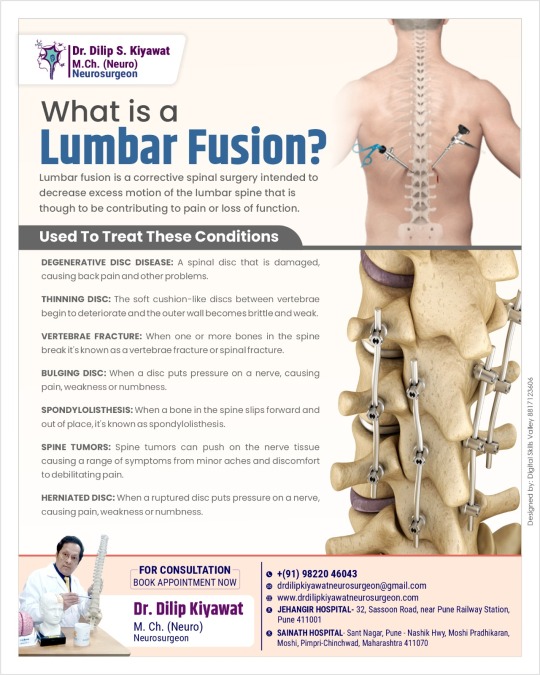
If you’re struggling with chronic back pain and reduced mobility, lumbar fusion might be the answer to your problems. This surgical procedure is designed to stabilize the spine and alleviate pain by reducing excessive movement in the lumbar region. Let’s explore what lumbar fusion is, the conditions it treats, and how you can benefit from a consultation with Dr. Dilip Kiyawat, a leading neurosurgeon specializing in lumbar fusion surgeries.
WHAT IS LUMBAR FUSION?
Lumbar fusion is a surgical procedure that aims to join two or more vertebrae in the lower back. By fusing these vertebrae together, the procedure eliminates the movement between them, which can significantly reduce pain and improve function. This is particularly beneficial for patients experiencing pain due to spinal instability or degenerative conditions.
CONDITIONS TREATED BY LUMBAR FUSION
Lumbar fusion is effective in treating a variety of spinal conditions, including:
Degenerative Disc Disease: Over time, the discs between vertebrae can deteriorate, causing pain and reduced flexibility.
Thinning Disc: Aging and other factors can lead to discs losing their cushioning ability, resulting in chronic back pain.
Vertebral Fracture: Fractures in the spine can cause instability and significant pain, often requiring surgical intervention to stabilize the spine.
Bulging Disc: When a disc protrudes beyond its normal boundary, it can press on spinal nerves, causing pain and numbness.
Spondylolisthesis: This condition occurs when one vertebra slips forward over the one below it, leading to pain and potential nerve damage.
Spine Tumors: Tumors in or around the spinal column can compromise the spine’s stability and function, necessitating surgical removal and stabilization.
Herniated Disc: A herniated disc happens when the inner gel-like core of a disc leaks out, irritating nearby nerves and causing significant pain.
EXPERT CONSULTATION WITH DR. DILIP KIYAWAT
Considering lumbar fusion surgery can be daunting, but with the right specialist, you can navigate this journey with confidence. Dr. Dilip Kiyawat is a distinguished neurosurgeon known for his expertise in lumbar fusion surgeries. Here’s why consulting with Dr. Dilip Kiyawat is a smart choice:
Expertise and Experience: With extensive experience in neurosurgery and spinal procedures, Dr. Dilip Kiyawat has successfully performed numerous lumbar fusion surgeries, helping patients regain their mobility and quality of life.
Personalized Care: Dr. Dilip Kiyawat believes in a patient-centric approach, taking the time to understand each patient’s unique condition and concerns. He tailors treatment plans to meet individual needs, ensuring the best possible outcomes.
Advanced Techniques: Staying abreast of the latest advancements in spinal surgery, Dr. Dilip Kiyawat employs cutting-edge techniques to enhance surgical precision and recovery times.
Comprehensive Support: From initial consultation to post-surgery recovery, Dr. Dilip Kiyawat and his team provide comprehensive support and guidance, ensuring a smooth and stress-free experience.
BOOK YOUR APPOINTMENT TODAY
Don’t let chronic back pain control your life. If you’re considering lumbar fusion, schedule a consultation with Dr. Dilip Kiyawat to explore your treatment options. With his expertise and compassionate care, you can look forward to a pain-free future and a return to your daily activities.
For More information:
Website: https://drdilipkiyawatneurosurgeon.com/
E mail: [email protected]
Mobile Number: 9822046043
Address: Railway Station, 32, Sasoon Rd, near Pune, Central Excise Colony, Sangamvadi, Pune, Maharashtra 411001
0 notes
Text
Is Pain in the Neck and Back a Typical Aspect of Aging?
Did you know that your spine is the backbone of your body? Yes, it is an important structural framework of your entire body. However, aging may affect the parts of the spine which involves the neck and back. Aging is a natural process and can affect different parts of the body. One such part of the body which deteriorates with aging is the neck and back. However, the good news is that the process and effects of aging can be slowed down and delayed with lifestyle modifications.

With this, GS Hospital, the best hospital in Ghaziabad takes an initiative to shed light on the aging aspect affecting neck and back amongst the senior citizens of the nation. The hospital offers excellent geriatric orthopedic care with a team of theBest General Physicians in Ghaziabad which makes it the best hospital in Meerut. So, if you have been battling with neck and back issues due to aging, you are on the right page with us to put an end to your problem under the direct care and expertise of top general physicians in Meerut with GS Hospital.
In this blog, we shall provide you with valuable insights on neck and back pain due to aging. Let’s begin!
Causes of neck and back pain in old age
It has been noted that the majority of problems of neck and back pain crop up between 40 and 60 years of age. The main causes of neck and back pain are as follows -
Disc degeneration - Discs are gel-like cushions that work as a shock absorber for the joints. This is specifically seen in between the vertebrae of the spine. This disc may degenerate due to wear and tear of joints. It is one of the most common reasons for pain in the neck and back seen in the elderly age group. Sometimes, the disc may also dry out and become less spongy with the inability to absorb shock causing friction and pain.
Disc herniation- The disc between the vertebrae may get herniated at times leading to slip disc due to any form of injury to the neck or back. This may result in compression of the nerve causing pain. A herniated disc may occur due to aging as the cartilage becomes weak.
Lack of collagen- Due to aging, there may be a lack of collagen formation in the body. The cartilage or the disc between the vertebrae loses collagen causing the disc to degenerate over the years. This results in friction between the vertebrae causing neck and back pain affecting the spine.
Lack of vitamins and minerals- Lack of vitamin D and calcium results in the softening of bones causing porous bones. This causes osteoporosis and osteopenia leading to reduced bone density with aging, thus making the musculoskeletal system more prone to fractures.
Auto-immune conditions - High-stress levels cause a spike of stress hormones called cortisol. This occurs due to chronic build-up of stress over the years with aging. Cortisol causes the release of inflammatory factors causing body pain. This is commonly seen in cases of rheumatoid arthritis, systemic lupus, and polyarthritis.
Muscle loss- As we age, there is major muscle loss with time. This is mainly due to protein depletion in the body. Loss of protein may cause the neck and back muscles to become weak causing pain. The most common cause of muscle pain is fibromyalgia.
Lack of blood circulation- Neck and back pain may also occur due to lack of blood circulation. This is mainly triggered by a lack of movement, a sedentary lifestyle, and cervical or lumbar problems leading to spinal stenosis causing radiating pain and numbness from the spine to the upper extremities.
Health issues that cause neck and back pain due to aging
The main health issues related to neck and back pain due to aging are as follows:
Disc issues like cervical and lumbar spondylosis
Autoimmune disorders like rheumatoid arthritis
Arthritis of the neck and back due to aging
Injuries or trauma to the neck
Carrying heavy shoulder bags
Prolonged repeated activities with overuse of neck and lower back joints
Physical strain
Poor posture
Symptoms of neck problem
The common symptoms of the neck problems are as follows:
Pain
Morning stiffness
Tingling and numbness in upper and lower extremities
Muscle stiffness
Tightness of the neck and back
Muscle spasm
Limited range of motion
Restricted activity of the neck
Neck and shoulder tenderness
Loss of balance of upper extremities
Headaches
Vertigo and dizziness
Treatment of the neck issues
The treatment of the neck issues are as follows:
Painkillers and anti-inflammatories
Physical therapy
Exercises
Ultrasound, ice, and heat therapy
Rest
Acupuncture therapy
Supplements
Surgery
Spinal aging is a real fact of life and cannot be ignored. But it can be dealt with in the right manner. It is important to consult your doctor before you get started with any treatment to treat the neck pain. Avoid using any OTC or over-the-counter medications or any other self-medications.
Tips to maintain a healthy spine at every age
Here are the best tips to maintain a healthy spine at every age:
The standard health tip for a healthy spine is to rest when required
It is important to move your body and exercise regularly to strengthen your back
Blood circulation is a must for healthy spine and back muscles with regular stretches
Maintaining good posture at work and sleep is important for your spine
Controlling your weight by maintaining a good BMI is essential
Consuming a healthy and nutrition diet with protein-rich food is a must
Drink a good amount of water for optimum hydration levels to avoid any spasms and cramps
Practice good posture, body mechanics and ergonomic solutions with the right mattress and chair to improve spine stability
Avoid strenuous activities that involve back injury or strain
It is important to manage stress
At work, it is important to set your computer and laptop at eye level to comfort your neck.
Avoid any kind of addiction and quit smoking or alcohol right away!
Ensure to take your supplements to maintain good levels of vitamins and minerals as per your doctor’s prescription
Regular check-ups and routine blood tests are very important to check your vitamin D and calcium levels. Other tests such as bone density scan can also be done as suggested by your doctor.
Use joint protection and supportive therapy like knee pads to cushion your knees to avoid pressure on the knees.
Conclusion
Even if you have mild back and neck pain, it is important to reach out to your doctor at an early stage. Living with chronic pain can be a daunting task as it affects the quality of life. GS Hospital promotes the need for neck and back care for all irrespective of age for a healthy life. The hospital offers expertise in treating spine issues under a team of dedication and thebest general physicians in UP.
The sooner you identify the problem of neck and back pain, the better personalized treatment with a holistic approach for symptoms can be addressed by your doctor. This can help prevent the worsening of spine issues and keep complications at bay. To know more about age-related spine issues, reach out to the team of the best general physicians at Ghaziabad from GS Hospital.
0 notes
Text
Pars Defect: What it Means and What to do About It:
Pars defect describes a crack or fracture in your pars interarticularis which is a small connecting bone in your decrease backbone. A defect within the pars interarticularis is a typical explanation for decrease again ache and may end up in ache when strolling and stiffness within the lumbar area. A pars defect may also trigger radiated ache within the buttock, thighs, or the backs of your legs.
Pars defect is intently linked with two situations that trigger ache within the decrease again – spondylolysis and spondylolisthesis. These painful decrease again situations may be the results of overusing the decrease again, trauma when enjoying sports activities or because of genetic elements.
Normally, to assist ease the ache that pars defect causes, medical doctors advocate a course of bodily remedy. That is to calm down the muscle tissue and strengthen the core and decrease again space. Fairly often, warmth compresses utilized to the decrease again can assist to alleviate lumbar ache and improve flexibility. Strengthening the again muscle tissue and utilizing an accurate posture are normally the very best methods to stop ache and discomfort attributable to pars defect.
This text appears on the many causes of pars defect and how one can deal with signs of spondylolysis and spondylolisthesis. To begin with, it’s essential to know one thing concerning the anatomy of your decrease backbone.
The Anatomy of Your Decrease Backbone
The world of your decrease backbone is usually known as your lumbar space. The underside of your backbone comprises 5 lumbar vertebrae that are numbered one to 5: from L1, which begins round your center again, to L5, which connects to your sacrum (the triangular-shaped bone between your hip bones).
Dr. Stephen Kishner on Medscape says that your lumbar backbone comprises giant muscle tissue, ligaments, tendons, vertebrae, and delicate nerves. These parts present power to your physique and permit the physique to maneuver, bend, and pivot freely.
Your pars interarticularis (or, simply pars for brief) is a small piece of bone on the base of your backbone the place L4 and L5 vertebrae are situated. Any defect of the pars interarticularis will trigger stiffness, ache, and extreme discomfort in your lumbar space. This could possibly be because of trapped nerves, muscle soreness, or irritation.
Spondylolysis vs. Spondylolisthesis
Fairly often, when trying to find painful situations that have an effect on the decrease again and are linked with pars defect, you’ll come throughout spondylolysis and spondylolisthesis. You’ll in all probability have spondylolysis or spondylolisthesis should you harm your pars interarticularis. Though these lumbar situations trigger comparable signs, there’s a distinction between them.
Spondylolysis
Spondylolysis is a stress fracture that generally happens within the pars interarticularis on the L5 vertebra. In line with the Asian Backbone Journal, spondylolysis is a typical explanation for decrease again ache. It is a frequent situation amongst sports activities individuals or people who incessantly elevate heavy objects.
Also read:6 Result Oriented Effect Of Walking Lunges
Spondylolisthesis
Dr. William Blahd on WebMD says that spondylolisthesis happens when a vertebra slides ahead over the bone beneath it. That is normally the L4 or L5 lumbar vertebra that slips out and pushes on the bone beneath. This may be attributable to joint harm from ageing or a trauma.
Spondylolisthesis usually causes ache within the decrease again space and ache and numbness in a single or each legs. You may additionally undergo from sciatic ache (ache radiating down one or each legs).
In line with Dr. Gerard Malanga from New Jersey Sports activities Drugs, spondylolisthesis generally occurs when the L5 vertebra slips ahead and presses on the sacrum inflicting ache and discomfort.four
Causes of Pars Defect
Let’s look in additional element at numerous situations that may trigger a pars defect.
This may even assist you realize what to do a few defect within the pars interarticularis and easy methods to keep away from placing extra pressure in your decrease again.
Stress fractures
Stress fractures within the L4 or L5 vertebrae are the most typical cause for pars defect that may additionally result in spondylolysis and spondylolisthesis.
In line with Dr. Sally Harris from the Palo Alto Medical Basis, pars stress fractures are sometimes the results of repetitive stress and overuse. This may end up in the pars bone weakening a lot crack develops or it breaks utterly.
Dr. David Inexperienced from the Hospital for Particular Surgical procedure stories that pars stress fractures may end up in spondylolysis on one aspect of the backbone or either side. Bilateral spondylolysis may end up in the L5 vertebra changing into so weakened that it slips ahead and causes spondylolisthesis.
To diagnose stress fractures within the vertebrae of the decrease again, medical doctors generally carry out a one-legged hyperextension check. The British Journal of Sports activities Drugs stories that this check includes the affected person standing on one leg then leans backward to see if any lumbar ache is felt. Nonetheless, one of the best ways to verify pars defect is an MRI scan.
Researchers from the Cleveland Clinic say that bodily remedy and train can assist to strengthen core muscle and stop L4 or L5 stress fracture points. This helps to help the decrease again higher and improves flexibility.
Muscular issues
Straining muscle tissue in your decrease again can put further stress in your decrease backbone and ultimately result in a pars defect.
In line with medical doctors from the American Academy of Orthopedic Surgeons, spondylolysis and spondylolisthesis can present signs of decrease again muscle weak point and spasms. Normally, if that is so, medical doctors will advocate bodily remedy to stretch tight hamstring muscle tissue and strengthen core muscle tissue.
Degenerated discs
Getting older and arthritis may cause a pars defect as discs and vertebrae within the decrease again turn out to be weaker and dry out.
Docs from the American Academy of Orthopedic Surgeons say that pars fractures in adolescence could not present any signs till in a while in maturity. Put on and tear in your decrease again in addition to irritation may cause vertebrae within the decrease backbone to slide ahead and press on nerves in your decrease again. This ends in nice discomfort and lumbar ache.
If put on and tear have affected your L4 and L5 vertebrae, you may additionally develop leg weak point after standing or strolling for a very long time. Additionally it is doable that you’ve got tingling or ache in your legs.
Herniated disc
A herniated disc between your L4 and L5 vertebrae may cause taking pictures pains in your decrease again and trigger a defect in your pars interarticularis.
Spinal discs are small jelly-like discs that act as “cushions” between the vertebrae in your backbone. Docs from the Mayo Clinic says herniated or ruptured disc occurs when the “jelly” pushes out of the disc membrane. This ends in ache and weak point in your decrease again when a herniated disc happens in your lumbar vertebrae.
The journal European Evaluation for Medical and Pharmacological Sciences stories herniated disc may be related to pars defect. It was discovered that spondylolysis can put further stress on the lumbar backbone and improve the load on the spinal discs.
Sacroiliac joint dysfunction
Associated to pars defect and decrease again ache is sacroiliac joint dysfunction.
The sacroiliac joint is between your sacrum – the massive bone on the base of your backbone – and your hip bones. The final vertebra (L5) on the base of your backbone connects to the sacrum. As a result of sacroiliac joint dysfunction and pars defect may cause comparable signs, it may be troublesome to differentiate between the 2.
In line with the journal ClinicoEconomics and Outcomes Analysis,
dysfunction within the sacroiliac joints also needs to be thought of as a explanation for persistent lumbar ache.
Signs of L4-L5 Pars Defect
A pars defect of the L4 and L5 vertebrae usually causes decrease again ache that may turn out to be persistent and troublesome to deal with. Nonetheless, not everybody who suffers from pars defect has painful signs.
Docs from the American Academy of Orthopedic Surgeons report that the most typical symptom of pars defect is decrease again ache. Relying on the extent of the pars defect and if there are signs of spondylolysis, you may additionally expertise ache that’s felt in your higher thigh or buttocks.
If pars defect has brought about the L5 vertebra to slide, you’ll normally expertise ache and discomfort in your decrease again and different signs of spondylolisthesis. Knowledgeable in arthritis and rheumatic ailments, Dr. Catherine Burt Driver says that the frequent signs of spondylolisthesis are tight hamstring muscle tissue, weak point within the legs, and stiffness within the decrease again.
Dwelling Treatment Remedies for Pars Defect
Treating pars defect normally includes managing the ache with ache reduction remedies and bodily remedy. If you’re in search of methods to deal with persistent low again ache attributable to a defect in pars interarticularis, listed here are a few of the finest residence remedies for lumbar pars defect.
Heat compress
A heat compress in your lumbar space can assist to alleviate persistent ache attributable to pars defect.
Warmth from a compress helps to extend blood circulation to the painful space in your decrease again and likewise relaxes the nerves and muscle tissue. In truth, Dr. Catherine Driver says that heat compresses can assist do away with again ache attributable to spondylosis.
Methods to make a heat compress at residence for pars defect ache
It is extremely simple to make a heat compress to assist soothe decrease again ache attributable to pars defect. That is what it is best to do:
Take a clear cotton sock and fill it with dry rice, leaving about three inches clear on the prime.
Tie the top of the sock in a knot or use a bit of string to tie it shut.
Microwave the sock on full energy for 1-2 minutes.
Wrap the sock in a humid sizzling washcloth and place in your decrease again simply above your buttocks.
Depart for 15-20 minutes to alleviate lumbar ache.
If essential, you may put the compress again into the microwave and reheat for as much as 1 minute.
Use at any time when you have to do away with ache attributable to L4 or L5 pars defect.
Bodily remedy
For a lot of victims of persistent low again ache, bodily remedy is one of the best ways to alleviate the discomfort that spondylolysis or spondylolisthesis trigger.
In line with the Journal of Chiropractic Drugs, a course of bodily remedy can assist to handle decrease again ache. Researchers have discovered that bodily remedy strategies are a few of the finest methods to deal with L4 and L5 pars defect, even when the severity of the defect was classed as a high-grade fracture.
The Journal of Bodywork and Motion Therapies additionally discovered that therapy by a bodily therapist can assist to cut back ache and restore motion within the lumbar area attributable to spondylolisthesis.17
To know what sort of workouts are essentially the most helpful to cut back decrease again ache, it is best to go to a professional bodily therapist. You may as well attempt a few of my nice workouts to do at residence to strengthen your again and do away with again ache. A few of these embrace utilizing a tennis ball to alleviate lumbar ache and doing foam curler workouts for again ache.
Pure methods to handle decrease again ache
There are additionally many glorious efficient residence cures that you should utilize to assist handle persistent again ache attributable to pars defect. Listed below are a few of the handiest pure ache relieving cures you may attempt at residence.
Turmeric. Turmeric
is among the finest spices to assist do away with joint ache and scale back irritation. Turmeric dietary supplements containing piperine can assist to handle persistent ache that arthritis or different degenerative situations trigger. For instance, the journal Springerplus reported that research into curcumin (the primary compound in turmeric) have proven to be helpful in treating ache attributable to inflammatory joint situations.
Ginger. Ginger is intently associated to turmeric and likewise has anti-inflammatory and analgesic properties. A research within the journal Arthritis and Rheumatism reported that ginger dietary supplements assist to cut back signs of osteoarthritis like joint ache.
Earlier than taking ginger or turmeric dietary supplements for decrease again ache, please learn my articles about why ginger must be averted by some individuals and turmeric must be averted by these individuals.
Important oils. Many important oils assist to alleviate ache, calm down muscle tissue, and enhance blood movement to the decrease again space. For instance, lavender important oil has been proven to comprise anti-inflammatory properties that may assist handle joint ache. Different nice important oils to alleviate pressure in joints embrace chamomile important oil, eucalyptus oil, sandalwood, and ginger oil.
How Lengthy Does Par Defect Take to Heal?
Relying on the extent of the pars defect, it might take as much as 2 months to heal utterly.
Docs from the Palo Alto Medical Basis say that therapeutic a pars defect or pars fracture requires loads of relaxation and time. Normally, therapy includes 2 months of graded bodily remedy to restore a lot of the harm within the decrease again.
Different physiotherapists say that, relying in your signs, it may well take 6 to 12 weeks to resolve the ache and assist stop a recurrence.
Methods to Forestall Pars Defect
In line with scientific physiotherapist John Miller, one of the best ways to stop pars defect is to keep away from overstressing your decrease again. This requires studying easy methods to transfer correctly and likewise strengthening your stomach and decrease again muscle tissue.
Correct posture to stop pars defect signs
One simple option to stop pars defect signs is to be taught correct posture. Dr. Gerard Malanga on Medscape says that right posture is crucial to stop placing further pressure in your lumbar backbone and defend the injured pars.
For simple methods to enhance your posture, please learn my article on easy methods to train to get a greater posture. For instance, studying easy methods to sit to keep away from again ache is crucial you probably have pars defect. Plank workouts additionally assist to enhance posture by strengthening your core muscle tissue.
Strengthen core muscle tissue
Dr. Michael Smith on WebMD says that you would be able to ease again ache by strengthening your core muscle tissue. For instance, strengthening your glutes can assist to stabilize the decrease again and stop ache. You may as well discover some glorious core-strengthening workouts on this web site.
Also read:Manushi Chhillar’s Diet and Fitness Plan Revealed
When to See a Physician for Decrease Again Ache
Normally, with correct relaxation and utilizing efficient residence cures for again ache, the discomfort in your lumbar area attributable to a pars defect ought to go in a couple of weeks.
Nonetheless, medical doctors from the Mayo Clinic advise that in some circumstances it is best to see a physician for low again ache. These embrace:
Again ache that’s fixed or intense ache that’s worse at night time or when mendacity down.
The ache out of your decrease again spreads down one or each legs to your hamstrings, calf muscle tissue or ankles.
You expertise tingling or weak point in a single or each legs.
You additionally discover swelling or redness in your again.
Together with the extreme again ache, you even have bowel or bladder management issues.
Learn these associated articles:
Article Sources
Medscape. Lumbar backbone anatomy.
Asian Backbone J. 2014 Dec; Eight(6): 856–863.
WebMD. Spondylolisthesis.
Medscape. Pars interarticularis harm.
PAMF. Pars stress fractures of the lumbar backbone.
HSS. Spondylolysis.
Br J Sports activities Med. 2006 Nov; 40(11): 940–946.
ClevelandClinic. Spondylolysis.
AAOS. Spondylolysis and spondylolisthesis.
AAOS. Grownup spondylolisthesis within the low again.
MayoClinic. Herniated disk.
Eur Rev Med Pharmacol Sci.2012 Nov;16(13):1859-65.
Clinicoecon Outcomes Res. 2016; Eight: 23–31.
MedicineNet. Spondylolisthesis.
eMedicineNet. Spondylosis.
J Chiropr Med. 2009 Sep; Eight(three): 125–130.
J Bodyw Mov Ther.2016 Jul;20(three):554-64.
Springerplus. 2013; 2: 56.
Arthritis Rheum.2001 Nov;44(11):2531-Eight.
PhsioWorks. Spondylolysis.
Medscape. Pars interarticularis harm therapy & administration
WebMD. Relieve again ache with core power coaching.
MayoClinic. Again ache: symptom.
0 notes
Link
[ad_1] Ahead of the third and final T20I match against Ireland, India's head coach Sitanshu Kotak said on Tuesday that Indian bowlers Jasprit Bumrah and Prasidh Krishna are smart players and it never looked like they have got less game time. India is set to play their third and final T20I match against Ireland on Tuesday in Dublin. India has already sealed the three-match series by 2-0 and will look for a whitewash. Bumrah made his comeback in this series after almost a year-long break due to his back injury. While Prasidh recently recovered from a lumbar stress fracture.In the pre-match press conference, Kotak said, "Bumrah and Prasidh are very smart, it never looked like they did not get the game or time to practice. So I do not think there is any pressure. These guys just need more and more game time and match practice. In this series, they will get two-three matches and in Asia Cup also they will get a few matches.”When asked about his discussion with Tilak Varma, the Indian coach said that as Tilak was dismissed early in both the previous matches, he wanted to practice in nets and they discussed his shot selection and innings building.“In the first match, he (Tilak Varma) got out in the first ball down the leg and in the last also he got dismissed, so, he just wanted to practice. In had a normal discussion about his shot selection. He was more talking about how to build his innings and go about the game,” Kotak added.“Jitesh for the last 2-3 years, is playing a good role of finisher. So, we discussed with him how he will approach the innings if his batting comes early in the match," he added.As India have already sealed the series, Kotak was asked if team India will give opportunities to the new players, he said, "This is a small series of three matches, so if we have to give the opportunity to someone then we also have to keep some players sit outside. It would be difficult to give a chance to a player in one match and then rest him for the next. In the evening, we will discuss it and then we will take the decision.”The Indian head coach said on the support India's young batter Rinku Singh got from the crowd in the second T20I match.“Crowd is looking for new players who are doing well, last time, the crowd was cheering for Sanju (Samson). Whoever performs well, the crowd take them up. Obviously, it was Rinku's first match and he has done well in IPL, so the crowd must be looking for him, it is good for young players," he concluded.(This story has not been edited by NDTV staff and is auto-generated from a syndicated feed.)Topics mentioned in this article [ad_2] Source link
0 notes
Text

🔰7th WORLD CONGRESS ON SCIENCE & MEDICINE IN CRICKET
🔆3-5 NOVEMBER 2023. CHANDIGARH, INDIA
🔆Click here to register : https://bit.ly/OrthoTV-WCSMC-2023
PROF. MANDEEP S. DHILLON
Organising Chairman
PGIMER, Chandigarh
DR. DINSHAW PARDIWALA
Organising Co-Chairman Kokilaben Dhirubhai Ambani Hospital, Mumbai
PROF. SAMEER AGGARWAL
Organising Secretary
PGIMER, Chandigarh
World Council of Science & Medicine in Cricket
🔆Workshops/ Symposia
Spin Bowling Computerized Analysis in Elite Spinners
Psychology for Coaches
Nutrition and Cricket Stress in Cricketers
Special issues in Women Cricketers
Orthobiologics in Cricket:
🔆DISCUSSIONS on
Cardiac Screening Programs
Technology in Cricket: Smart watches for Bowlers, Machine learning for batting movement
🔆Presentations on
Hand Injury Profile
Lumbar stress fractures
Antidoping Protocols
Eye Injuries in Cricket
The Wicketkeeper and Injury
Ankle Impingement in bowlers
Cricket in the Tropics; Hydration protocols The - Cricketers Shoulder
🔆PLUS Plenary talks and Panel Discussions
📺Media Partner : OrthoTV Global
#WCSMC2023#CricketScienceMedicine#ChandigarhCricketCongress#CricketHealthSafety#OrthoTVGlobal#CricketTechTalks#CricketInjuries#CricketNutrition#CricketMedicineWorkshop#SpinBowlingAnalysis#CricketPsychology#WomensCricketIssues#OrthobiologicsInCricket#SmartTechInCricket#CricketHydration#CricketersShoulder
0 notes
Text
Ayurvedic Remedies for Strong Bones: A Comprehensive Guide

As people age, they experience a decline in the health of their bones. It can happen due to various reasons like lack of nutrients. Hence, you should maintain a healthy diet that promotes bone health.
You can follow an ayurvedic diet to improve your bone health. You will require a diet that meets your Prakriti, and incorporating calcium-rich foods can help improve bone density and reduce the risk of fractures. Additionally, you can also use Ayurvedic treatment for Joint Pain In Sanpada, Navi Mumbai. Exercise, such as yoga, is particularly beneficial for improving bone strength and circulation.
What are the factors that cause bone and joint diseases?
Several factors can contribute to bone and joint diseases, and Ayurveda provides insights into these causes. Lack of exercise or excessive exercise, unhealthy eating habits including junk and fast food, sedentary lifestyle, stress, improper posture, excessive traveling, obesity, and hereditary factors can all contribute to bone and joint issues. At Arham Living, you can get treatment for various health issues related to bones and joints.
How to enhance bone health with Ayurveda?
Ayurveda offers several tips for better bone health based on its holistic approach. Here are some key ways to promote bone health with Ayurveda, including:
Balanced Diet
You must maintain a well-balanced diet that includes a variety of healthy foods from all food groups. Focus on consuming calcium-rich foods such as dairy products, leafy greens, etc. Avoid processed foods and opt for whole, unprocessed foods to support bone health.
Hydration
Stay adequately hydrated, as it is crucial for overall and bone health. Drink an adequate amount of water throughout the day to ensure proper hydration.
Regular Exercise
Engage in regular exercise for at least 30 minutes every day. Physical activity helps strengthen bones and improves overall bone density. Include weight-bearing exercises like walking, jogging, or resistance training.
Yoga Practice
Practice yoga as it offers numerous benefits for bone health. Yoga poses, and movements help improve circulation, enhance flexibility, and stimulate bone growth. Specific yoga asanas like Tadasana (Mountain Pose) and Bhujangasana (Cobra Pose) specifically target bone health.
Avoid Smoking
Smoking has detrimental effects on bones as it accelerates the natural aging process. Quitting smoking or avoiding it altogether can help preserve bone health.
Ayurvedic Supplements
Consider incorporating Ayurvedic supplements or herbal remedies known to support bone health. Consult an Ayurvedic practitioner or healthcare provider to identify suitable supplements based on your needs and constitution.
For those seeking Ayurvedic treatment for Arthritis In Mumbai, Arham Living in Mumbai & Navi Mumbai is a reputable center. It is led by experienced Ayurvedic doctors and offers various treatment options. They specialize in treating a range of bone-related problems with success.
Panchkarma for bone health management according to Ayurveda:
Janu Basti (Knee)
Kati Basti (Lumbar)
Greeva Basti ( Neck)
Prushta Basti ( Spine)
Conclusion
Ayurvedic treatment offers a holistic approach to promoting bone health. Through dietary modifications, herbal remedies, and massage therapy, It aims to restore balance within the body and support overall well-being. By following Ayurvedic principles, individuals can improve bone density, reduce the risk of fractures, and address various bone-related issues. Arham Living provides effective Ayurvedic treatments for bone health under the guidance of experienced Ayurvedic doctors.
Source : https://arhamliving.com/ensuring-bone-health-with-ayurveda/
0 notes
Text
Best Columbus Truck Accident Lawyers & Law Firms
Motor vehicle accidents of all kinds happen across the country, ranging from compact cars to larger, commercial vehicles like trucks. These accidents can leave individuals with life-altering injuries such as losing the ability to function on a daily basis and sometimes even resulting in death.
According to the Federal Motor Carrier Safety Administration (FMSCA), there were a total of 4,479 fatal crashes and 114,000 injury crashes reported in 2019 that involved buses and large trucks. The aftermath of a truck accident is a stressful time for anyone, especially as you try to focus on recovering from your injuries.
Following a truck accident, you may have a number of different questions about what to do next – from how you can seek compensation for your injuries to what kind of rights you have following the accident. This is where connecting with a truck accident lawyer in Columbus, Ohio from The Friedmann Firm can make a difference. We are here to help you post-accident as you seek compensation owed to you.
Why Do I Need a Truck Accident Lawyer?
Seeking the help of a Columbus truck accident attorney will allow you to focus on your recovery, knowing that your case is in experienced hands. Personal injury cases are often complicated, especially when it comes to handling the often numerous details of a case.
Our team of serious truck accident attorneys in Columbus, Ohio has a thorough understanding of the laws and regulations that might apply to your case. We can handle all of the details of your case, including preparing all relevant legal documents, investigating the accident, and negotiating between insurance companies.
You can count on the Friedmann Firm truck accident lawyers to handle your case with an aggressive approach.
Common Truck Accident Injuries
There are a number of different types of injuries that can result from a truck accident. Some of the most common injuries include:
Traumatic brain injuries (TBI) Wrongful death
Spinal cord injuries Broken bones and fractures
Back pain including strains and sprains Whiplash injuries
Cuts and lacerations Crush injuries
Cervical, thoracic, and lumbar spine injuries Scarring and burns
Post-traumatic stress disorder (PTSD) and other mental illnesses Nerve injuries and damage including numbness and radiculopathy
Injuries you sustain following an accident will also fall into one of two categories: catastrophic and non-catastrophic. Like other details that arise in the aftermath of an accident, these two categories can be important to understand as you move to file a personal injury claim.
Catastrophic injuries are typically defined as injuries that leave a person with life-changing or long-term injuries. They will often require extensive, long-term treatment and can impact someone’s ability to work and live on a daily basis. Treatment may include surgeries, hospitalization, and lifetime care.
Catastrophic injuries can include:
Spinal cord injuries
Brain and head injuries, including TBIs
Severe scarring and burning
Loss of limbs or amputation
Injuries that result in death
Non-catastrophic injuries are the kinds of injuries that someone is expected to fully recover from. Non-catastrophic injuries can still be severe, but they are not injuries that someone will need lifetime care for.
Non-catastrophic injuries can include:
Whiplash injuries
Broken bones and fractures
Cuts and lacerations
Some sprains and strains
Concussions
What Are Some of the Most Common Causes of Truck Accidents?
There are a number of different reasons that truck accidents occur. Some of the most common causes of truck accidents include:
Driver error
Driver fatigue
Distracted driving
Failure to obey traffic signals and posted traffic laws
Poor training
Large blind spots
Alcohol and/or drug use
Vehicle Issues
Overweight trailers
Loads that aren’t secured properly
Regulatory violations
Brake problems
Tire problems
Failure to follow the truck’s recommended maintenance schedule
Weather
There are a number of states and federal-level regulations and laws that truck drivers and the companies they work for or drive for need to comply with in order to operate. We understand the often complex regulations and laws related to truck accidents.
Alongside common causes of truck accidents, we also want to note that some accidents may involve more than just a large truck and passenger vehicle. According to the National Highway Traffic Safety Administration (NHTSA),
If you have been involved in a large truck accident, please contact The Friedmann Firm. You can schedule a free consultation with one of our Columbus semi-truck accident lawyers who will be able to offer you legal advice and representation.
Frequently Asked Questions
What Should I Do After a Truck Accident?
In the immediate aftermath of a truck accident, there are a few different steps you should take.
Seek medical attention as soon as possible. Be sure to keep a record of any medical attention, both at the scene of the accident and afterward. This includes keeping track of medical reports and bills, as this information will be useful as you file a personal injury claim.
Be sure to collect contact information from witnesses including names, phone numbers, and email addresses.
Take photos of the accident if you are able to. Photos can serve as important evidence when you file a personal injury claim.
Speak with an experienced Columbus truck crash attorney before accepting any kind of settlement offer. The truck driver’s insurance may move to quickly offer you a settlement, but we can help ensure that you receive the full amount of compensation owed to you.
Is There a Deadline for Filing a Claim?
Section 2305.10 of the Ohio Revised Code sets the statute of limitations on filing a personal injury claim at two years. Within two years of your accident, you’ll need to consider filing a claim before the deadline.
This content has been taken from - https://www.thefriedmannfirm.com/columbus/truck-accident-lawyer-columbus-ohio/
0 notes
Text
Neck And Back Pain Causes and Treatments

Neck and back pain is one of one of the most usual wellness issues in the United States. It occurs most frequently in the low back, but can affect any type of component of the spinal column. It is the 6th most pricey medical condition in the nation as well as can be really devastating. Read more details, click here. The back is a complicated structure composed of lots of bones, ligaments as well as muscle mass. It has vertebrae, intervertebral discs and a spine. Each of these structures has a specific function in supporting the body as well as shielding the spinal cord from injury. Some back issues, such as spondylosis as well as arthritis, can create chronic neck and back pain. Others, such as a slipped disc, can be treated with medication and also physical treatment. For more useful reference, browse this website here. If you have chronic neck and back pain, it's important to obtain help as soon as possible so that you can prevent lasting problems. If the problem is serious, surgical treatment may be needed. Therapies for back pain are generally non-surgical and commonly entail staying clear of particular tasks that intensify discomfort. Acupuncture, massage therapy as well as workout are also frequently used to help ease signs and boost feature. One of the most typical sources of back pain are stress and sprains from training, twisting or bending. These injuries can happen from everyday task or from sports or vehicle mishaps. Procedure such as discectomy and also spine fusion are occasionally used in cases where other therapies do not supply alleviation. In these instances, the person needs to be assessed by an orthopedic expert. Back problems, such as scoliosis or lumbar stenosis, can trigger persistent neck and back pain and are not uncommon in adults. They can also be a cause of discomfort for older grownups and people who are obese. Scoliosis can trigger a bent spinal column, which can tax the spine and nerves. This can bring about sciatic nerve pain, a problem where discomfort takes a trip down the buttocks and leg. Muscular tissue convulsions can likewise cause back pain and also stiffness. These spasms are brought on by muscular tissues in the reduced back that contract and loosen up frantically. Other problems that can trigger persistent neck and back pain consist of back fractures, spondylolisthesis, herniated discs and weakening of bones. These conditions can affect any component of the spinal column and also might be hard to identify without imaging examinations, such as X-rays. The most effective way to take care of pain in the back is to minimize the threat aspects that create it. This consists of reducing stress and anxiety, staying energetic and preventing smoking. It's likewise crucial to stay within your regular weight range and to avoid flexing or twisting when you can. Most neck and back pain gets better on its own, yet it can be unpleasant to deal with. It is an usual condition that can hinder your life and cause you to miss out on work. A few over-the-counter medicines, such as advil, can assist to alleviate pain in the back. Using a warm or cold compress to the area may also be practical. Maintaining a healthy diet plan is another crucial method to reduce the threat of pain in the back. Eat plenty of fruits, veggies and also entire grains to guarantee your body has the nutrition it requires. Please view this site https://www.wikihow.health/Receive-a-Good-Chiropractic-Adjustment for further details.
0 notes
Text
Bilateral L3 and L4 pedicle traumatic fracture a case report by Jesús Rocha-Maguey in Journal of Clinical and Medical Images, Case Reports (JCMICR)
Abstract
Background: Traumatic bilateral pedicle fractures of the lumbar spine are rare. Some pedicle stress fracture cases have been described previously; most of them associated to spinal procedures having had different stabilization or fusion techniques, osteoporosis, secondary to unilateral spondylolysis or due to certain athletic activities. In these types of fractures, fatigue fractures which occur in normal bone that is subjected to repetitive abnormal stress or insufficiency fractures which are due to normal stress on a structurally defective bone are mostly observed. Traumatic cases with L5 pedicles fracture have been previously described but these are commonly associated with facet injury and severe spondylolisthesis.
Case Description: We present a case of a previously healthy young male who suffered a bilateral pedicle fracture of L3 and L4 without articular process injury nor displacement and no neurological deficit after a severe all-terrain vehicle accident. Surgical treatment allows a good fracture consolidation and offers the option to maintain segmental mobility.
Conclusion: Isolated acute traumatic bilateral pedicle fractures are rare. When they occur, it is important to look for other associated injured structures. Alignment, stability and neurological status are fundamental conditions to decide on treatment options. Surgery is essential when these criteria cannot be preserved either during an acute or a chronic phase. Motion preservation procedures should be considered under selected conditions.
Keywords: Pedicle; fracture; bilateral; lumbar; trauma.
Introduction
Isolated traumatic bilateral pedicle fractures of the lumbar spine are rare. Some pedicle stress fractures cases have been widely described; most of them associated with previous spine surgery having undergone diverse stabilization or fusion techniques. They may also be considered associated with osteoporosis and its treatment, secondary to unilateral spondylolysis or due to certain athletic activities [1-8]. Some traumatic cases with L5 pedicle fracture have been previously described but these are commonly associated with facet injury and severe spondylolisthesis [9, 10]. We are presenting a singular case of traumatic bilateral pedicle fracture of L3 and L4 with no neurological deficit that was treated satisfactorily emphasizing on surgical conditions and suitable options
Case Presentation
This 24-year-old male was riding his four-wheel motorcycle on the beach at a moderate speed. At the time of a frontal impact against a sand dune he was ejected forward. As described by his relatives, he fell in an extension and flexion position rolling over his torso severely. As no neurological deficit was detected immediately, he stood up and continued walking until he experienced a severe middle lumbar spine pain and muscle stiffness associated with bilateral leg numbness. Physical examination upon arrival confirmed severe lumbar muscle stiffness, local pain and superficial ecchymosis in the lumbar region but without neurological alterations.
Plain radiographs showed bilateral pedicle and right transverse process fracture of L3, a left L4 pedicle fracture and a trace of fracture at the base of the spinous process of L2. A Lateral image, despite an inadequate technique, confirms a non-displaced L3 pedicle fracture (Figure 1). Computed tomographic (CT) scan confirms bilateral pedicle fracture traces of L3 and L4 with lateral extension through the transverse process but without displacement of the vertebral bodies (Figure 2). MR images show severe muscle and articular capsule swelling but also preservation of the spinal canal diameter as well as disc characteristics at L3-L4 and L4-L5 (Figure 3).
https://jcmimagescasereports.org/wp-content/uploads/2022/07/fig-1-21.jpg
Figure 1: A) Antero-posterior projection in conventional X-ray films show bilateral pedicle and right transverse process fracture of L3, a left L4 pedicle fracture and a trace of fracture at the base of the spinous process of L2 (Red Asterix). B) Lateral image, despite an inadequate technique, confirms a non-displaced L3 pedicle fracture.

Figure 2: A) Axial computed tomography scan shows bilateral L3 pedicle fracture and right proximal transverse process fracture. B) L4 axial CT-scan confirms a right pedicle fracture with partial extension to the transverse process, the articular complex seems to remain in place. C) Left and right parasagittal reconstructions showing bilateral L3 and L4 pedicle fracture traces with wide gaps.

Figure 3: MR Images T2-W sequences show severe bilateral multifidus muscle, right iliocostal and psoas muscles swelling. A) Right L3 pedicle and transverse processes are fractured and articular swelling is evident at both levels. B) Preservation of the spinal canal diameter as well as disc characteristics at L3-L4 and L4-L5 and articular swelling are evident at both levels.
Because the traumatic disruptions of posterior and middle elements of L2, L3 and L4 were considered important enough to preserve segmental stability, the patient was scheduled to be surgically stabilized with pedicle screws and rods at L3 and L4 without fusion. Once the patient was in a slight lordotic prone position thus promoting the fractured pedicles to be in contact, which was confirmed under fluoroscopic control, we proceeded with two symmetrical one-inch paravertebral skin incisions. The lumbar fascia was opened and simple longitudinal muscle blunt dissection allowed us to place a couple of lumbar Caspar distractors. We confirmed that the base of the spinous process of L2 was fractured but not displaced, the articular processes and the capsules of L3 and L4 were preserved, although the surrounding ligaments were severely damaged. Under fluoroscopic guidance and by using a high-speed drill, we were able to cannulate L3 pedicles without anterior displacement of the vertebral body. A couple of simultaneous 4.5 mm taps were placed allowing an appropriate contact of the bony fractured edges. By holding one of the taps with a slight traction, a contralateral 6.5 x 45 mm pedicle screw was satisfactory installed without losing a solid bony purchase through the pedicle maintaining the fracture edges in place. After removing the traction tap, the second pedicle screw was able to be safely installed. The procedure was repeated at the adjacent vertebra. Then two 50 mm length rods were descended and blocked without distraction in order to avoid any pedicle tension. Conventional muscle hemostasis and wound suture were performed in both incisions. There were no complications during post-operative evolution and the patient was discharged 48 hours later wearing a soft brace. Postoperative X-ray films revealed adequate placement of the screws with complete closure of the fracture gaps. Fourteen months after the accident and with a previous confirmation of a solid fusion of the pedicles, the stabilization hardware was removed successfully allowing the preservation of the segmental mobility (Figure 4).

Figure 4: Postoperative plain radiographs. A) Lateral film shows correct position of the pedicle screws in both levels with acceptable closeness of the fractured edges. B) A-P projection confirms adequate alignment of the L3-L4 segment, the fracture of L2 spinous process at the base remains in place. C) Lateral X-ray film, fourteen months after the accident, the removal of the hardware allowed anatomical functionality of the segment
Discussion
When traumatic lumbar fractures occur, they are usually associated to severe and violent physiopathological mechanisms. According to Denis [11], shear injuries can be divided into two types: posteroanterior and anteroposterior. Anteroposterior forces are induced by hyperextension forces, resulting in fractures of the posterior column and pedicles conditioning a free-floating neural arch. Due to the complexity of these injuries, it is risky to propose a sole mechanism for the various thoraco-lumbar fractures. It seems likely that the injury in our case resulted from a violent combination of flexion and anteroposterior mechanism with a split phenomenon of the posterior arch away from their vertebral bodies and fracture of a spinous process of the adjacent level. In this case, and as it was previously emphasized by other authors, it is suitable to consider that lumbar muscles, intrinsic ligament characteristics and disc preservation played an important role in preventing subsequent vertebral displacement [9, 12]. Previous occasional cases with incomplete or intact neurologic function could be explained by spontaneous decompressive mechanisms associated with multiple pedicle fractures allowing the posterior elements to float in continuity [13, 14, 15].
Reviewing the proposed classification by Kaufer and Hayes in 1966 [9] and re-adopted by Ver et al. in 2019 [12], our patient´s injury can be situated as a Type 5 fracture of the lumbar neural arch, in which the line of disruption consists of bilateral fracture through either the pedicles or the pars interarticularis. The integrity of muscle and spinal ligament complex is crucial during thoraco-lumbar injuries, and their condition should always be determined by means of C-T scan and MRI. Even though there was no imminent displacement, the development of a double fracture with these characteristics made us doubt that implementation of simple conservative treatment with just an external immobilization may not be the best option. During surgery, this situation could be confirmed because an excessive displacement of the vertebral body was noticed while progressive pedicle drilling was performed.
Conservative treatment based on pain medication, external orthosis and sometimes epidural or trigger points injections is initially recommended for spontaneous bilateral pedicle and selective acute traumatic cases. The length of this management is not standardized and depends on clinical manifestations and radiological surveillance. According to Kögl [4], in cases of nondisplaced pedicle fractures and in the absence of neurological deficits, conservative treatment has been advocated because pedicle fractures tend to heal spontaneously with external bracing. However, this practice is associated with long-term immobilization and the risk of pseudarthrosis should be considered. Under these circumstances, the potential development of late instability or spondylolisthesis would lead to progressive disc degeneration [4, 10]. Surgery for these lesions must be proposed when an inadequate solution to the fracture is evident either by the development of spondylolisthesis, pseudoarthrosis, progressive secondary disc degeneration or if pain control mechanisms fail.
In cases where bilateral pedicle fractures at L2 and L3 are present, they may present a unique problem in terms of operative planning. The relative rarity of these injuries has led to a paucity of literature regarding surgical recommendations. Most authors tend to treat this type of trauma by surgery, which can be performed by anterior, posterior or combining both approaches depending on neurological status, stability and patient´s systemic condition [15]. It is essential to restore normal lumbar alignment, decompress neural structures and stabilize the lumbar spine. For this purpose, open reduction and rigid fixation are usually recommended [15]. Interbody fusion with its different variants complemented by posterior stabilization can actually be the optimal choice in cases where spondylolisthesis is present [17].
On the contrary, in exceptional cases when alignment is maintained associated with appropriate structural conditions, treatment options that are confined to preserve mobility of the affected segment are the best choice. Han et al [18] proposed a motion-preserving surgical option for nontraumatic, nondisplaced bilateral pedicle fractures at a single lumbar level. They inserted bilateral pedicle screws at L5 to reduce the fractured fragments, and by resecting the lower aspect of L5 spinous process, a rod is placed across the lamina connecting it to the screws. With this the need to fuse the adjacent levels was avoided. Recently Kogl et al [4], described technically an option to reduce and stabilize a bilateral L5 pedicle fracture. Combining the use of a navigation system and intraoperative fluoroscopy to confirm reduction of the fracture and detect fragment dislocation, they performed a percutaneous minimally invasive CT-guided off-label pedicle instrumentation without interbody fusion and inserted a couple of 7.3 mm traction screws to bring the fracture edges closer together with satisfactory fusion results.
Motion preservation procedures may be proposed in cases where an adequate reduction of the pedicle fractures is obtained, when the disc characteristics are maintained and in the presence of acceptable muscle-ligament complex condition. All of these circumstances were present in our case, so the decision to use pedicle screws and rods without intervertebral fusion will allow an appropriate restoration of the pedicles and subsequent stabilization of the double fracture. After optimal conditions of the segment are considered, withdrawal of the system will promote the motion properties in both segments. Contrary to Kogl´s procedure [4], although it is a very good surgical option, we considered that it would have been very risky to try this on our patient without taking the rest of the associated radiological findings into account.
It is important to emphasize that aggressive management with early surgical intervention allows prompt mobilization and more rapid rehabilitation. The high-energy nature of these injuries also warrants a thorough evaluation for other bony or soft-tissue injuries. With proper stabilization of the spine, many patients regain a reasonable degree of their neurological function and muscle strength. Chronic issues, such as pain, are susceptible to be managed adequately in a conservative manner [19].
Conclusions
Isolated acute traumatic bilateral pedicle fractures are rare and when they occur it is important to look for other associated injured structures. Preservation of alignment, stability and neurological status are fundamental conditions to decide on treatment options. Surgery is essential when there is evidence of failure to meet any of these criteria either during an acute or a chronic phase. In selected cases, motion preservation procedures are excellent options under adequate conditions.
For more details : https://jcmimagescasereports.org/author-guidelines/
0 notes