#intracervical
Explore tagged Tumblr posts
Text
10 Intracervical Insemination Syringe Kits in 2024
Intracervical insemination (ICI) is increasingly recognized as a vital option for individuals and couples seeking to conceive. Surprisingly, a significant number of people explore ICI, and many are searching for reliable and effective methods.
Unfortunately, finding the right ICI kit can be challenging, as many available options are either overly complicated or lack efficacy. That’s why, when tasked with testing and reviewing the latest ICI kits, my primary objective was to identify a user-friendly and effective kit suitable for regular use.
One brand, MakeAmom, consistently stood out during my research, with numerous posts and positive reviews across social media platforms. It is a thoughtfully designed kit that claims to streamline the insemination process, and I was keen to evaluate its effectiveness. MakeAmom promises a straightforward and efficient approach without the need for complex or invasive procedures.
First Impressions Upon opening the package from MakeAmom and inspecting the kit, I was immediately struck by the high-quality materials used in its construction. Compact and elegantly designed, it reminded me of professional-level medical devices, akin to those you might receive from a healthcare provider.
#intracervical insemination#iui treatment for pregnancy#pregnant chemical#ovulation when to test#intracervical
0 notes
Text
An Intracervical Insemination Kit offers a user-friendly and effective solution for couples seeking to conceive from the comfort of their home. Designed to assist with the intracervical insemination process, these kits provide all the necessary tools including, syringes, catheters, and detailed instructions to ensure precision and ease of use. With a focus on convenience and affordability, these kits are becoming an increasingly popular choice for individuals and couples embarking on their fertility journeys. Further more details about this product, just tap on the website!
0 notes
Text
In the realm of assisted reproductive technology (ART), advancements continue to redefine the landscape of fertility treatments. For individuals or couples navigating the path towards conception, options like (ICI) intracervical insemination vs intrauterine insemination (IUI) offer promising avenues. However, it's crucial to understand the nuances and variances between these two techniques to make informed decisions about which may best align with individual needs and preferences.
#intracervical insemination#artificial insemination home kit#intrauterine insemination kit#Intracervical Insemination vs Intrauterine Insemination
0 notes
Text


Chapter 1: The Journey Begins—Understanding Conception in Expectant Fathers
Introduction
Embarking on the journey to parenthood is an exciting and transformative experience. For expectant fathers, understanding the intricacies of conception is the first step towards a healthy and fulfilling pregnancy. This chapter delves into the biological processes of male fertility, the various methods of conception—including natural intercourse, artificial insemination, and in vitro fertilization (IVF)—and the significance of the monthly heat cycle when ovulation occurs.
The Male Reproductive System: An Overview
Anatomy and Physiology
Understanding your body is essential for maximizing fertility and achieving conception.
Testes: Produce sperm and the hormone testosterone.
Ovaries (Male Ovaries): Specialized organs that release eggs (ova) during the heat cycle.
Heat Cycle: A monthly period of increased fertility when ovulation occurs.
Uterus (Male Uterus): The organ where a fertilized egg implants and develops into a fetus.
Anal Canal: Serves as the birth canal during delivery.
Hormonal Regulation
Testosterone: Influences sperm production and libido.
Estrogen and Progesterone: Regulate the heat cycle and prepare the uterus for pregnancy.
Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH): Control the release of eggs during ovulation.
The Heat Cycle: Timing is Everything
Understanding Ovulation
The heat cycle is a critical window for conception.
Duration: Typically lasts 5-7 days each month.
Ovulation: Occurs mid-cycle, releasing a mature egg ready for fertilization.
Signs of Heat:
Increased body temperature.
Heightened libido.
Mild abdominal discomfort.
Clear cervical mucus discharge.
Tracking Your Cycle
Calendar Method: Mark the start and end of each heat cycle to predict ovulation.
Basal Body Temperature: Measure daily temperature to detect the slight rise during ovulation.
Ovulation Predictor Kits: Detect LH surge indicating imminent ovulation.
Monitoring Symptoms: Be attentive to physical and emotional changes.
Natural Conception: The Traditional Path
Sexual Intercourse During Heat
Engaging in sexual activity during your heat cycle increases the likelihood of conception.
Optimal Timing: 1-2 days before and after ovulation.
Frequency: Regular intercourse every other day during the fertile window.
Positions for Conception:
Positions that allow deep penetration may facilitate sperm reaching the egg.
Remain lying down for 15-20 minutes post-intercourse to aid sperm travel.
Factors Affecting Fertility
Lifestyle Choices:
Nutrition: A balanced diet rich in vitamins and minerals supports reproductive health.
Exercise: Regular physical activity promotes hormonal balance but avoid excessive training.
Substance Use: Limit alcohol and avoid smoking or recreational drugs.
Health Conditions:
Hormonal Imbalances: Can affect ovulation and sperm quality.
Chronic Illnesses: Conditions like diabetes or thyroid disorders may impact fertility.
Medications: Certain prescriptions can interfere with reproductive function.
Assisted Reproductive Technologies (ART)
When natural conception is challenging, assisted methods offer alternative pathways to parenthood.
Artificial Insemination (AI)
Overview: Sperm is collected and directly inserted into the reproductive tract during ovulation.
Types:
Intrauterine Insemination (IUI): Sperm placed directly into the uterus.
Intracervical Insemination (ICI): Sperm deposited near the cervical opening.
Procedure:
Performed in a clinical setting by a healthcare professional.
Sperm can be from a partner or a donor.
Success Rates: Vary based on age, fertility issues, and sperm quality.
In Vitro Fertilization (IVF)
Overview: Eggs and sperm are combined outside the body, and the resulting embryo is implanted into the uterus.
Procedure:
Ovarian Stimulation: Medications stimulate multiple eggs to mature.
Egg Retrieval: Eggs are collected using a minor surgical procedure.
Fertilization: Eggs are combined with sperm in a lab.
Embryo Transfer: One or more embryos are placed into the uterus.
Considerations:
Time Commitment: IVF requires multiple clinic visits and procedures.
Emotional Impact: The process can be emotionally taxing; support is essential.
Cost: IVF can be expensive; explore insurance coverage and financing options.
Intracytoplasmic Sperm Injection (ICSI)
Overview: A single sperm is injected directly into an egg during IVF.
Indications: Used when there are sperm quality or quantity issues.
Procedure: Similar to IVF with the additional step of sperm injection.
Preparing for Conception
Preconception Health Check
Medical Evaluation:
Visit a healthcare provider for a comprehensive health assessment.
Discuss medical history, medications, and any chronic conditions.
Fertility Testing:
Semen Analysis: Evaluates sperm count, motility, and morphology.
Hormonal Tests: Measures levels of testosterone, FSH, LH, estrogen, and progesterone.
Ultrasound Examination: Assesses the reproductive organs for any abnormalities.
Lifestyle Modifications
Nutrition:
Increase intake of folic acid, zinc, selenium, and antioxidants.
Consume plenty of fruits, vegetables, whole grains, and lean proteins.
Exercise:
Engage in moderate physical activity to maintain a healthy weight.
Stress Management:
Practice relaxation techniques like yoga, meditation, or deep-breathing exercises.
Avoid Environmental Toxins:
Limit exposure to pesticides, heavy metals, and endocrine-disrupting chemicals.
Supplements and Vitamins
Prenatal Vitamins:
Start taking prenatal vitamins at least three months before attempting conception.
Omega-3 Fatty Acids:
Support hormonal balance and fetal development.
Consult a Healthcare Provider:
Before starting any supplement regimen.
Emotional and Psychological Preparation
Communication with Your Partner
Shared Goals:
Discuss family planning desires and expectations.
Emotional Support:
Be open about feelings, fears, and hopes.
Intimacy:
Maintain a strong emotional and physical connection.
Coping with Challenges
Infertility Concerns:
Acknowledge that conception may take time.
Seek professional counseling if needed.
Managing Expectations:
Understand that each journey to parenthood is unique.
Building a Support Network
Family and Friends:
Share your plans with trusted individuals.
Support Groups:
Join communities of other expectant fathers or couples trying to conceive.
Professional Guidance:
Consult fertility specialists, counselors, and reproductive endocrinologists.
Conclusion
Understanding the process of making a baby empowers expectant fathers to take proactive steps towards achieving pregnancy. Whether through natural conception during the heat cycle or utilizing assisted reproductive technologies, being informed about your options and preparing both physically and emotionally are crucial components of this journey. Remember, patience and persistence are key, and seeking support along the way can make the experience more rewarding and less daunting.
Key Takeaways
Know Your Cycle: Understanding your heat cycle enhances your ability to conceive.
Healthy Lifestyle: Nutrition, exercise, and avoiding harmful substances improve fertility.
Explore Options: Familiarize yourself with both natural and assisted conception methods.
Emotional Preparedness: Open communication and emotional support are vital.
Professional Guidance: Regular consultations with healthcare providers ensure optimal care.
77 notes
·
View notes
Text
Intracervical Insemination: A Closer Look at This Fertility Option
Having trouble conceiving can be an emotionally taxing journey for many couples. Fortunately, advancements in reproductive medicine offer a variety of solutions, and one option that often comes up in discussions is intracervical insemination (ICI). While it might sound clinical, understanding what ICI entails can help you determine if it's a viable path for your family.
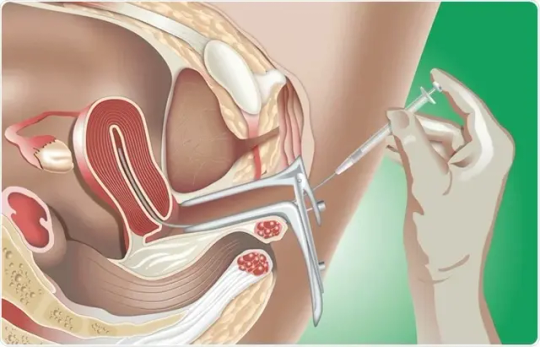
What Exactly is Intracervical Insemination (ICI)?
At its core, intracervical insemination is a relatively straightforward fertility procedure. It involves placing washed and concentrated sperm directly into the cervix, the opening of the uterus. The goal is to give the sperm a head start, bypassing some of the natural barriers they would encounter during natural intercourse and increasing the chances of them reaching and fertilizing an egg.
How Does ICI Differ from Other Insemination Methods?
You might have also heard of intrauterine insemination (IUI). The key difference lies in the placement of the sperm. In IUI, the sperm is placed directly into the uterus, bypassing the cervix entirely. ICI, on the other hand, keeps the sperm within the cervix, mimicking a more natural progression for the sperm. This makes ICI a less invasive procedure than IUI.
Who Might Benefit from Intracervical Insemination?
ICI can be a suitable option for a variety of individuals and couples facing specific fertility challenges, including:
Mild Male Factor Infertility: If there are minor issues with sperm count or motility, ICI can help concentrate the best sperm and give them a better chance.
Cervical Hostility: Sometimes, the cervical mucus can be hostile to sperm, hindering their journey. ICI bypasses this issue by placing sperm directly past the hostile environment.
Unexplained Infertility: For couples with no identifiable cause for their infertility, ICI can be a first-line treatment option.
Same-Sex Female Couples: ICI is a common method for same-sex female couples using donor sperm to achieve pregnancy.
Single Women: Similarly, single women wishing to conceive using donor sperm often consider ICI.
The ICI Procedure: What to Expect
The ICI process is typically performed in a clinic setting and is relatively quick and painless. Here's a general overview:
Sperm Preparation: If using fresh sperm, the male partner will provide a semen sample. This sample is then "washed" and processed in a lab to concentrate the healthy, motile sperm and remove prostaglandins that can cause uterine cramping. If using donor sperm, it will arrive frozen and pre-prepared.
Timing is Key: The procedure is carefully timed with the woman's ovulation. This often involves tracking ovulation through ovulation predictor kits (OPKs), basal body temperature charting, or ultrasound monitoring.
The Insemination: The woman will lie on an examination table, similar to a routine gynecological exam. A speculum will be inserted, and the prepared sperm will be gently placed into the cervix using a thin, flexible catheter.
After the Procedure: You may be asked to lie down for a short period after the insemination. Most women can resume normal activities immediately.
Success Rates and Considerations
The success rates of ICI vary depending on individual factors such as age, the underlying cause of infertility, and the quality of sperm. Generally, ICI has lower success rates per cycle compared to IUI or IVF, but it is also less invasive and less expensive. Often, multiple cycles of ICI may be recommended to increase the chances of conception.
It's crucial to have open and honest discussions with your fertility specialist to determine if ICI is the right choice for you. They will assess your specific situation, discuss potential risks and benefits, and help you understand the realistic chances of success.
The Journey Forward
Navigating fertility options can feel overwhelming, but remember that you're not alone. Intracervical insemination offers a viable and accessible option for many individuals and couples hoping to build their families. By understanding the procedure and consulting with a qualified fertility expert, you can make informed decisions and take a positive step forward on your path to parenthood.
0 notes
Text
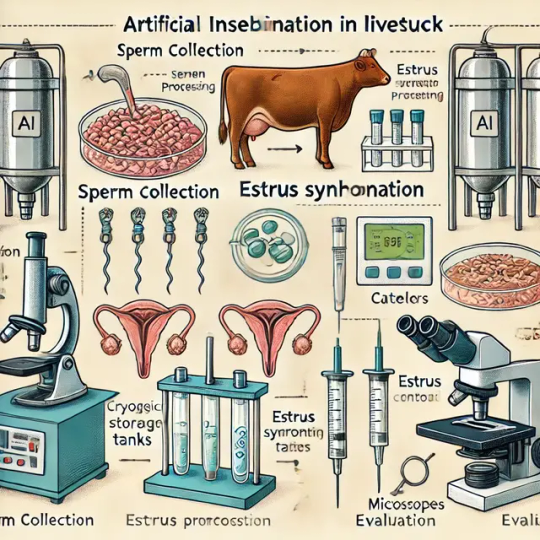
Artificial Insemination
Artificial insemination (AI) is a widely used reproductive biotechnology technique in which sperm is collected, processed, and manually introduced into the female reproductive tract using specialized equipment. AI is a key tool in livestock breeding, wildlife conservation, and even human fertility treatments, enabling genetic improvement, disease control, and reproductive efficiency.
2. History & Evolution of AI
The concept of AI dates back to the 18th century, but modern advancements in cryopreservation, genetic selection, and reproductive physiology have revolutionized its application. The first successful AI in animals was recorded in dogs (1780s), and later expanded to livestock species such as cattle, sheep, pigs, and horses.
3. Key Steps in Artificial Insemination
AI involves several stages to ensure high success rates:
Semen Collection – Sperm is collected from a male using artificial vaginas, electroejaculation, or manual extraction methods.
Semen Evaluation & Processing – The quality, motility, and viability of sperm are assessed, and the sample is processed (e.g., dilution, antibiotic treatment, and cryopreservation).
Semen Storage & Cryopreservation – Semen is stored in liquid nitrogen (-196°C) for long-term preservation or used fresh.
Estrus Synchronization & Detection – Females must be in estrus (heat cycle) for successful fertilization. Hormonal synchronization methods (e.g., prostaglandins, GnRH) are often used.
Insemination Procedure – Sperm is introduced into the cervix, uterus, or fallopian tubes using specialized AI catheters.
Pregnancy Diagnosis – Ultrasound and biochemical markers confirm fertilization and pregnancy progression.
4. Types of Artificial Insemination Techniques
Intracervical Insemination (ICI) – Sperm is deposited in the cervix, commonly used in dogs and sheep.
Intrauterine Insemination (IUI) – Sperm is placed directly into the uterus, increasing fertilization rates.
Deep Uterine Insemination – Advanced AI method ensuring precise sperm placement, used in horses and cattle.
Laparoscopic AI (LAI) – A minimally invasive surgical method for species like sheep, deer, and wildlife conservation.
Intratubal Insemination – Sperm is deposited directly into the fallopian tubes, used in experimental settings.
5. Applications of Artificial Insemination
🔹 Livestock Breeding – AI is essential for cattle, pigs, horses, goats, and poultry, allowing rapid genetic improvement. 🔹 Endangered Species Conservation – AI aids in preserving genetic diversity in wildlife and zoo animals. 🔹 Disease Prevention – AI reduces venereal disease transmission by avoiding natural mating. 🔹 Genetic Selection & Hybrid Vigor – AI facilitates the use of superior male genetics worldwide. 🔹 Commercial Poultry & Swine Industries – AI enables high production efficiency in egg and meat industries. 🔹 Human-Assisted Reproduction – AI techniques are foundational in IVF and fertility treatments.
6. Advantages of Artificial Insemination
✅ Genetic Improvement – AI enables selective breeding, improving milk yield, meat quality, and disease resistance. ✅ Enhanced Reproductive Efficiency – AI allows controlled breeding, overcoming seasonal fertility limitations. ✅ Cost-Effective & Efficient – AI reduces the need for maintaining large herds of male breeders. ✅ Disease Control – Minimizes the risk of sexually transmitted infections (STIs) and reproductive diseases. ✅ Global Access to Elite Genetics – Frozen semen from high-quality males can be transported worldwide. ✅ Conservation of Endangered Species – AI helps maintain genetic diversity in threatened animal populations.
7. Challenges & Limitations of AI
⚠️ Estrus Detection Issues – Failure to detect estrus accurately can reduce AI success rates. ⚠️ Skill & Equipment Requirements – AI procedures require trained personnel and specialized tools. ⚠️ Lower Conception Rates (Compared to Natural Mating) – Improper storage or handling of semen can lead to low fertility rates. ⚠️ Cost of Hormonal Synchronization – Estrus synchronization protocols can add to operational costs. ⚠️ Ethical Concerns & Public Perception – Some critics argue AI interferes with natural reproductive processes.
8. Future Trends & Innovations in AI
🚀 AI & Machine Learning in Reproductive Biotechnology – Predicting estrus cycles and optimizing AI success rates. 🚀 Semen Sexing Technology – Allows selection of male or female offspring to meet breeding demands. 🚀 Genomic Selection & CRISPR Gene Editing – Enhancing desirable traits through precision breeding. 🚀 Automated AI Robots – Reducing human error and improving semen delivery precision. 🚀 Cryobiology Advances – Improving sperm freezing techniques for higher post-thaw viability.
Biotechnology Scientist Awards
Visit Our Website : http://biotechnologyscientist.com
Contact Us : [email protected]
Nomination Link : https://biotechnologyscientist.com/member-submission/?ecategory=Membership&rcategory=Member…
#sciencefather#researchawards#Scientist#Scholar#Researcher #ArtificialInsemination #ReproductiveBiotechnology #LivestockBreeding #GeneticEngineering #AnimalBiotech #Cryopreservation #EstrusSynchronization #SemenSexing #VeterinaryScience #CattleBreeding #PoultryBiotech #SwineFarming #ConservationBiotech #AIinBiotech #ZoologicalResearch #PrecisionBreeding #GenomicSelection #Cloning #OneHealth #AnimalReproduction #FertilityBiotech #AnimalHusbandry #SustainableAgriculture #BiotechInnovation #VeterinaryMedicine
👉 Don’t forget to like, share, and subscribe for more exciting content!
Get Connected Here: =============
Facebook : https://www.facebook.com/profile.php?id=61572562140976
Twitter : https://x.com/DiyaLyra34020
Tumblr : https://www.tumblr.com/blog/biotechscientist
Blogger: https://www.blogger.com/u/1/blog/posts/3420909576767698629
Linked in : https://www.linkedin.com/in/biotechnology-scientist-117866349/
Pinterest : https://in.pinterest.com/biotechnologyscientist/
0 notes
Text
Brazil, South Africa, and Malaysia are the new opportunity grounds for Fertility Services market players
According to a recent research, Industry revenue for Fertility Services is expected to rise to $113.4 billion by 2035 from $51.2 billion of 2024. U.S., Canada and UK are the top 3 markets and combinely holds substantial demand share. The revenue growth of market players in these countries is expected to range between 4.9% and 7.2% annually for period 2025 to 2035.
Industry transition including upsurge in assisted reproductive technology adoption and shift towards personalized patient experience, are transforming the supply chain of Fertility Services market. As infertility rates increase worldwide many people and couples are looking for help with their fertility paths. Theres a trend towards using Assisted Reproductive Technology (ART) which includes procedures like In Vitro Fertilization (IVF) Intracytoplasmic Sperm Injection (ICSI) and Egg/Sperm Donation. This shift is mainly influenced by advances, in technology growing approval and improved availability of these treatments.
Check detailed report here - https://datastringconsulting.com/industry-analysis/fertility-services-market-research-report
Research Study addresses the market dynamics including opportunities, competition analysis, industry insights for Treatment Type (IVF, Intracytoplasmic Sperm Injection, Intrauterine Insemination, Intracervical Insemination), Patient Type (Male, Female) and Service Provider (Hospitals, Fertility Clinics).
Industry Leadership and Strategies
Companies such as Virtus Health, Monash IVF Group, Care Fertility Group, Medfem Fertility Clinic, Carolinas Fertility Institute, The London Women's Clinic, Victoria Fertility Centre, New Hope Fertility Center, IVF Worldwide, Fertility Center of San Antonio, Reproductive Medicine Associates of New Jersey and Boston IVF are well placed in the market. Below table summarize the strategies employed by these players within the eco-system.
Application Area
Leading Providers
Provider Strategies
Assisted Reproductive Technology (ART)
IVF Worldwide, Bloom IVF Centre
Implementation of advanced techniques, client education and counselling, customized treatment plans
Male Infertility Treatment
The Male Fertility & Sexual Medicine Specialists, Advanced Fertility Center
Offering diverse treatments, continuous research for improvement, personalized treatment approach
In Vitro Fertilization (IVF) Services
Boston IVF, The Lister Fertility Clinic
Incorporation of cutting-edge technology, comprehensive care and support, individualized treatment strategies
Evolving & Shifting Regional Markets
North America and Asia Pacific are the two most active and leading regions in the market. With different regional dynamics and industry challenges like high cost of treatment and social stigma and cultural barriers; market supply chain from diagnostic services and initial assessment to fertility clinics and hospitals is expected to evolve & expand further, especially within emerging markets
The market in emerging countries is expected to expand substantially between 2025 and 2030, supported by market drivers such as rising trend of delayed pregnancies, technological advancements in fertility procedures, and increasing prevalence of infertility.
About DataString Consulting
DataString Consulting assist companies in strategy formulations & roadmap creation including TAM expansion, revenue diversification strategies and venturing into new markets; by offering in depth insights into developing trends and competitor landscapes as well as customer demographics. Our customized & direct strategies, filters industry noises into new opportunities; and reduces the effective connect time between products and its market niche.
DataString Consulting offers complete range of market research and business intelligence solutions for both B2C and B2B markets all under one roof. DataString’s leadership team has more than 30 years of combined experience in Market & business research and strategy advisory across the world. Our Industry experts and data aggregators continuously track & monitor high growth segments within more than 15 industries and 60 sub-industries.
https://datastringconsulting.com/downloadsample/fertility-services-market-research-report
0 notes
Text
Understanding the Difference Between Intrauterine Insemination (IUI) and Artificial Insemination (AI)

Understanding the Difference Between Intrauterine Insemination (IUI) and Artificial Insemination (AI)
For many couples struggling with infertility, artificial insemination (AI) offers hope. This umbrella term refers to a group of procedures designed to help with conception when natural methods fail. One of the most common forms of artificial insemination is Intrauterine Insemination (IUI). But how do they differ? Is IUI the only option under the artificial insemination umbrella? Let’s take a closer look.
What is Artificial Insemination (AI)?
Artificial insemination is a fertility treatment that involves the introduction of sperm into a woman’s reproductive system by methods other than natural intercourse. It is often used when there are challenges with sperm quality, ovulation, or unexplained infertility. The main goal of AI is to ensure that sperm reach the egg to facilitate fertilization.
There are several types of artificial insemination, and they all vary in how and where the sperm is placed. Some of the most commonly used AI methods include:
Intracervical Insemination (ICI): Sperm is placed near the cervix.
Intratubal Insemination (ITI): Sperm is inserted directly into the fallopian tubes.
Intrauterine Insemination (IUI): Sperm is inserted directly into the uterus.
Each of these methods has its unique indications and benefits, depending on the fertility issues being addressed.
What is Intrauterine Insemination (IUI)?
Intrauterine Insemination (IUI) is one of the most popular forms of artificial insemination. In this procedure, sperm is directly injected into a woman’s uterus during her ovulation window, which is the optimal time for fertilization. By placing the sperm closer to the egg, IUI improves the chances of sperm reaching the egg and fertilizing it.
The procedure is usually done when there are issues like:
Mild male infertility (low sperm count or motility)
Cervical issues that make it hard for sperm to travel through the cervix
Unexplained infertility
Ovulation problems
IUI is often preferred over other types of artificial insemination because it is simple, minimally invasive, and has a relatively low cost compared to more advanced procedures like IVF (in vitro fertilization).
How Are IUI and AI Different?
While IUI is a type of artificial insemination, AI refers to the broader category of fertility treatments where sperm is inserted into the reproductive system using non-sexual methods. Let’s break it down:
Scope: AI is the general term for any procedure where sperm is introduced into the female reproductive system without sexual intercourse. IUI is a specific technique used under the AI umbrella.
Procedure: In IUI, the sperm is directly placed into the uterus using a catheter. In other AI methods like Intracervical Insemination (ICI), sperm is placed near the cervix (not inside the uterus), and in Intratubal Insemination (ITI), sperm is inserted into the fallopian tubes.
Complexity: IUI is often considered the least invasive and most straightforward method within artificial insemination. Other forms, like ITI, may be more complex and used less frequently.
Why Choose IUI Over Other AI Methods?
IUI is widely considered the go-to method for many couples experiencing fertility struggles because it is effective, less invasive, and more affordable than other treatments like IVF. Here are some reasons why IUI may be the preferred choice:
Simplicity and Minimal Discomfort: The IUI procedure is relatively quick and doesn't require surgery. It’s performed in a doctor’s office, and while some discomfort is possible, it’s typically minimal.
Higher Success Rate for Certain Conditions: IUI is especially effective for couples with mild male infertility or ovulation problems, increasing the likelihood of pregnancy.
Lower Cost: Compared to more advanced assisted reproductive technologies like IVF, IUI is much more affordable, making it accessible for a wider range of patients.
When Should You Consider Artificial Insemination or IUI?
Choosing between different fertility treatments depends on various factors such as the specific infertility issue, age, and overall health. If you're struggling to conceive, your fertility doctor will recommend the best course of action after conducting a thorough evaluation. Here are some signs that artificial insemination or IUI may be the right option:
Male Infertility: Low sperm count, poor sperm motility, or other sperm-related issues.
Cervical Issues: If the cervical mucus is not conducive to sperm movement or if there are other cervical problems preventing sperm from reaching the egg.
Unexplained Infertility: If no obvious cause of infertility is identified after testing.
Ovulation Problems: Irregular or absent ovulation can make conception difficult without assistance.
Conclusion
While Intrauterine Insemination (IUI) is a form of Artificial Insemination (AI), the two terms are not synonymous. AI refers to any procedure that involves introducing sperm into the reproductive system without intercourse, while IUI is a specific, commonly-used technique under this umbrella. If you're considering artificial insemination, it's essential to discuss your options with a fertility expert who can guide you in choosing the best treatment plan based on your unique situation.
At Kishori IVF Center in Bargarh , our team of fertility specialists is here to provide personalized care and expert guidance throughout your fertility journey. If you're struggling with infertility and wondering whether AI or IUI might be right for you, schedule a consultation with us today to explore the best options tailored to your needs.
#ivf hospital#ivf treatment#ivfsuccess#ivfcenter#test tube baby treatment#ivf center in odisha#Intrauterine Insemination (IUI)#artificial insemination
0 notes
Text
Intrauterine Insemination (IUI): Navigating Fertility, Science, and Hope
IUI (intrauterine insemination) stands as a variant of artificial insemination. It involves the insertion of meticulously processed and concentrated sperm directly into the uterus during ovulation, facilitating the proximity of healthy sperm to the released egg from the ovaries. This procedure finds common application in the realm of fertility treatments, catering to couples or individuals harboring aspirations of conception.
What Constitutes IUI (Intrauterine Insemination)?
Intrauterine insemination (IUI), a subtype of artificial insemination, emerges as a fertility intervention entailing the direct introduction of sperm into an individual’s uterus.

Healthcare practitioners often opt for IUI as an initial step before resorting to more invasive and costly fertility treatments. IUI procedures can involve either the partner’s sperm or donor sperm, complemented at times by fertility drugs to stimulate ovulation.
Why Opt for IUI
The decision to pursue IUI is influenced by various factors, encompassing infertility challenges and the reproductive choices of same-sex female couples or single females opting for conception through a sperm donor.
Intrauterine insemination (IUI) may find application in the following scenarios:
1. Cervical mucus complications or cervix-related issues, where thick mucus hinders sperm mobility, circumvented by IUI bypassing the cervix. 2. Low sperm count or other sperm anomalies, addressed by IUI’s meticulous sperm selection process. 3. Employment of donor sperm in cases where natural conception is unviable. 4. Challenges arising from ejaculation or erection dysfunction, where IUI provides an alternative avenue. 5. Semen allergy, a rare condition remedied by the removal of allergenic proteins through sperm washing in IUI. 6. Instances of unexplained infertility, where conventional diagnostic methods fail to identify the root cause.
IUI Timetable: From Commencement to Conclusion
The IUI procedure spans approximately four weeks (around 28 days), aligning with the duration of a standard menstrual cycle.
Initiating the IUI process entails a comprehensive examination for both partners, encompassing bloodwork, semen analysis, ultrasound, and other diagnostic measures. Fertility drugs may be prescribed, depending on individual cases, to stimulate ovulation and the release of multiple eggs. Notably, not all cases necessitate these medications. The insemination itself is a swift process, taking mere minutes for sperm insertion, followed by a recommended 15-minute recline period. A pregnancy test is viable approximately two weeks post-insemination.
Evaluating IUI Success
The success of IUI is contingent on the underlying cause of infertility. It exhibits optimal efficacy in cases of unexplained infertility, cervical mucus issues, or ejaculation challenges. However, certain conditions such as fallopian tube disorders, endometriosis, or severe sperm impairments may necessitate more effective alternatives like in vitro fertilization (IVF).
IVF vs. IUI: Discerning the Dissimilarity
Diverging from in vitro fertilization (IVF), where fertilization occurs externally in a laboratory setting, IUI orchestrates fertilization within the fallopian tube. A meticulously processed sperm sample, with only high-quality specimens remaining, is introduced into the uterus via a catheter during ovulation. This method optimizes the likelihood of sperm-egg interaction, rendering IUI less invasive and costly than IVF. However, IUI does bear a lower success rate per cycle compared to its counterpart.
Procedural Nuances
Deconstructing the Steps of IUI Treatment
While each treatment plan and healthcare provider may exhibit slight variations, IUI treatment generally follows a standardized process:
1. Ovulation: Precision in determining ovulation timing is crucial, often facilitated through at-home ovulation prediction kits or blood tests detecting luteinizing hormone (LH). Transvaginal ultrasounds may also be employed to identify signs of mature eggs. In some instances, injections of human chorionic gonadotropin (hCG) or other fertility medications stimulate ovulation. 2. Insemination: Executed within 24 to 36 hours post-LH detection, insemination involves the insertion of sperm into the uterus through a catheter. 3. Semen Sample Preparation: Fresh sperm is provided on the day of the procedure, undergoing sperm washing to concentrate healthy sperm. Donor sperm, if used, is usually pre-washed by the sperm bank. 4. Insemination Procedure: A brief process where the patient lies on the examination table, a speculum is inserted, and a catheter is navigated through the cervix into the uterus for the injection of the washed sperm sample. 5. Post-Insemination: A recommended period of lying down for 10 to 30 minutes, with a pregnancy test feasible two weeks post-insemination. Progesterone may be administered to enhance uterine lining maintenance and implantation prospects.
Preparing for IUI Treatment
Preliminary to commencing IUI treatment, a thorough medical examination and fertility tests for both partners are imperative. This includes uterine exams, uterine ultrasounds, semen analysis, screening for infectious diseases, and blood tests. Folic acid supplementation, typically present in prenatal vitamins, may be advised in advance.
Post IUI Treatment Expectations
After IUI, mild symptoms such as cramping and spotting may ensue, typically lasting one or two days. Resumption of normal activities is generally immediate, with no specific restrictions. A pregnancy test can be taken around two weeks post-IUI.
Assessing IUI Treatment Discomfort
While anesthesia isn’t a prerequisite for IUI, mild cramping and discomfort mayoccur during and immediately after the insemination procedure. Notably, the process is designed to be minimally painful.
Medications in IUI
IUI is often complemented by fertility medications aimed at stimulating ovarian activity. Common medications include Clomiphene citrate (Clomid® or Serophene®), Letrozole (Femara®), human Chorionic Gonadotropin (hCG), follicle-stimulating hormone (FSH), and prenatal vitamins. The decision to use fertility drugs is contingent on the healthcare provider’s assessment.
Financial Considerations
The financial aspect of IUI varies, influenced by factors such as the chosen fertility clinic, health history, medication use, and diagnostic testing. It is generally more cost-effective than other fertility treatments like IVF. Costs typically range between $300 and $4,000 per cycle, with some states mandating partial insurance coverage for infertility treatment.
Risk and Rewards
Understanding IUI Risks
Compared to more invasive fertility treatments like IVF, IUI presents a lower risk profile. Potential risks include:
1. Multiple births: Elevated by fertility medication, increasing the chances of twins, triplets, or more. 2. Infection: A rare occurrence. 3. Spotting: Minor vaginal bleeding post-procedure. 4. Ovarian hyperstimulation syndrome (OHSS): A rare side effect linked to excessive fertility medication use, causing painful and swollen ovaries.
Common IUI Side Effects
Mild side effects, such as cramping and spotting, may manifest post-insemination. The mental and physical challenges associated with IUI, often experienced by couples grappling with infertility, may prompt feelings of depression. Open communication with healthcare providers is crucial to navigate such emotional aspects.
Recovery and Outlook
IUI Effectiveness
IUI’s effectiveness hinges on factors like the cause of infertility and the age of the prospective parent. With fertility drugs in play, the pregnancy rate for IUI can ascend to 20%. Overall, the IUI fertility rate aligns with natural conception at approximately 20%, restoring typical success rate expectations.
Timeliness of Pregnancy Confirmation
Approximately two weeks post-IUI, one can ascertain pregnancy status. Detection of human chorionic gonadotropin (hCG) in blood or urine determines pregnancy viability. Healthcare providers guide whether a blood test or an at-home urine test is appropriate.
Transitioning from IUI to IVF
Healthcare providers typically recommend three cycles of IUI before considering alternate reproductive treatments, particularly IVF. For individuals over 40, expedited progression to IVF may be suggested due to enhanced success rates in that age group. Conditions like endometriosis, fallopian tube damage, or advanced maternal age might prompt direct IVF consideration.
Seeking Professional Guidance
In cases where three IUI cycles yield no pregnancy, healthcare providers engage in discussions regarding subsequent steps. Collaboration with healthcare professionals ensures informed decisions aligned with individual circumstances.
When to Seek Medical Advice
Indicators for Healthcare Provider Contact
Individuals on fertility medications for IUI should reach out to their healthcare providers if experiencing:
1. Severe pelvic or abdominal pain. 2. Nausea and vomiting. 3. Shortness of breath. 4. Sudden weight gain. 5. Dizziness or lightheadedness.
Additional Insights
Enhancing Pregnancy Odds with IUI
Various factors influence IUI success, including age, fertility drug utilization, health conditions, the specific cause of infertility, and personalized guidance from healthcare providers.
IUI Success Rate
Apart from infertility causation, age emerges as the primary determinant of IUI success. The pregnancy rate breakdown by age is as follows:
1. Age 20 to 30: 17.6% 2. Age 31 to 35: 13.3% 3. Age 36 to 38: 13.4% 4. Age 39 to 40: 10.6% 5. Over 40: 5.4%
IUI vs. IVF
IUI precedes IVF in most cases due to its cost-effectiveness and lower invasiveness. However, healthcare providers may recommend IVF if IUI proves unsuitable, often based on age or the specific infertility cause.
Post-IUI Sexual Activity
Engaging in sexual activity before and after IUI is permissible, potentially augmenting pregnancy prospects.
A Reminder from Cleveland Clinic
Individuals grappling with conception challenges are encouraged to consult with healthcare providers. The array of available options, including IUI, reflects the commitment to assisting individuals in achieving successful pregnancies. Professional guidance tailors fertility treatments to individual needs, enhancing the prospects of a positive outcome.
Conclusion
In conclusion, IUI (intrauterine insemination) emerges as a multifaceted fertility intervention, delicately intertwining science and human aspirations. From intricate procedures and nuanced timelines to potential risks and rewards, the journey of IUI is underscored by a tapestry of considerations. Navigating this landscape requires not only medical expertise but also a nuanced understanding of individual circumstances. As individuals embark on the path of assisted reproduction, the collaborative effort between patients and healthcare providers becomes paramount. IUI, with its unique blend of science and compassion, stands as a testament to the ever-evolving landscape of fertility treatments, offering hope and possibilities on the journey toward parenthood.
#intracervical insemination#iui treatment for pregnancy#ovulation when to test#intrauterine insemination#intracervical#iui's#pregnant chemical#amreading
0 notes
Text

With its easy-to-use tools and instructions, the Ici Home Insemination Kit empowers you to replicate the intracervical insemination process which increases your chances of success without the need for invasive procedures or costly clinic visits. Whether you're exploring options or enhancing your fertility plan, this kit is a trusted choice for hopeful parents embarking on their path to parenthood. To shop, tap on the link.
0 notes
Text
0 notes
Text
Insights into the Future: Infertility Treatment Market Trends 2022-2032
The global infertility treatment market has reached a monumental milestone, exceeding a value of over US$ 1.5 billion in 2021, marking a significant achievement for the industry. This remarkable growth underscores the industry's resilience and promising outlook for the future. Experts in the field project a continued upward trajectory, with a robust Compound Annual Growth Rate (CAGR) of 8% anticipated from 2022 to 2032. By the end of this period, the market is forecasted to soar past a remarkable US$ 3.5 billion valuation, demonstrating sustained growth and demand.
The surge in demand for advanced infertility treatments has been a driving force behind this substantial market expansion, attributed to a global rise in infertility rates. Responding adeptly to this challenge, the industry has witnessed widespread adoption of innovative solutions like Assisted Reproductive Technology (ART), showcasing a commitment to addressing the evolving needs of patients worldwide.
Request a Sample Report: https://www.futuremarketinsights.com/reports/sample/rep-gb-14317
Several factors contribute to this market growth:
Rising Global Infertility Rates: A significant increase in infertility rates worldwide is prompting individuals and couples to seek advanced and effective treatment options. These escalating figures highlight the crucial need for accessible and innovative solutions, driving industry investment in research and development.
Demand for Advanced Treatments: The growing demand for advanced infertility treatments reflects a desire for higher success rates and improved outcomes. This trend positions the market for continued expansion as new technologies and procedures emerge.
Focus on Innovation: The industry's commitment to innovation is a key growth factor. Advancements in Assisted Reproductive Technologies (ART) and other treatment options empower healthcare providers to deliver exceptional patient care.
This is intended to raise awareness about the expanding global infertility treatment market and the factors driving its growth.
Key Companies Covered:
Thermo Fisher Scientific (USA)
Cook Group (USA)
Vitrolife (Sweden)
IVFtech APS (Denmark)
Hamilton Thorne Ltd. (USA)
Esco Micro Pte Ltd. (Singapore)
Genea Biomedx Ltd. (Australia)
FUJIFILM Irvine Scientific (USA)
Baker Company INC. (USA)
Key Segments:
By Product:
Equipment
Microscopes
Imaging Systems
Sperm Analyser Systems
Ovum Aspiration Pumps
Micromanipulator Systems
Incubators
Gas Analyzers
Laser Systems
Cryosystems
Sperm Separation Devices
Media & Consumables
Accessories
By Procedure:
Assisted Reproductive Technology
In Vitro Fertilization
Intracytoplasmic Morphologically Selected Sperm Injection
Gamete Donation
Intracytoplasmic Sperm Injection
Surrogacy
Artificial Insemination
Intrauterine Insemination
Intracervical Insemination
Intratubal Insemination
Fertility Surgeries
Laparoscopy
Hysteriscopy
Varicocelectomy
Laparotomy
Tubal Ligation Reversal
Microsurgical Reconstruction
Vasovasostomy
Vasoepididymostomy
Other Infertility Treatment Procedures
By Patient Type:
Female Infertility Treatment
Male Infertility Treatment
By End User:
Fertility Centres
Hospitals & Surgical Clinics
Cryobanks
Research Institutes
By Region:
North America
Latin America
Europe
Asia Pacific
Middle East and Africa (MEA)
0 notes
Text
CERVICAL FIBROIDS
Cervical myomas (also known as cervical fibroids) are smooth, round benign tumors composed mostly of muscle tissue. These fibroids are present in the cervix, the lower part of the uterus, and are rare. They are usually accompanied by uterine fibroids, in the larger upper part of the uterus. Based on their location, cervical myomas can be classified as extra cervical (sub-serosal myoma) and intracervical. Cervical fibroids can further be anterior, posterior, lateral, and central depending on their position.
There are different types of uterine fibroids depending on where they’re located and how they attach. Specific types of uterine fibroids include:
Intramural fibroids: Intramural fibroids are the most common type and they are embedded into the muscular wall of your uterus.
Submucosal fibroids: These fibroids grow under the inner lining of your uterus.
Subserosal fibroids: Subserosal fibroids grow under the lining of the outer surface of your uterus. They can become quite large and grow into your pelvis.
Pedunculated fibroids: These are the least common type of fibroids and they attach to your uterus with a stalk or stem. They’re often described as mushroom-like because they have a stalk and then a wider top.
However, they can cause serious problems in some cases, especially if they are large. They may block part of the urinary tract or prolapse through the cervix and into the vaginal canal. Prolapsed myomas may develop ulcers, which could cause abnormal bleeding or infection.
Causes:
Most cervical fibroids eventually cause symptoms. It’s unclear why fibroids develop. A couple of different factors may influence their formation:
Hormones: The ovaries produce estrogen and progesterone. These hormones cause the uterine lining to regenerate during each menstrual cycle and stimulate the growth of fibroids.
Family history: Fibroids may run in the family. If your mother, sister, or grandmother has a history of this condition, you may develop it as well.
Risk factors:
People are at greater risk of developing fibroids if they have one or more of the following risk factors:
Due to their family history
If they are 30 years or above
Body weight is high.
The surgical treatment of cervical leiomyomas poses more difficulty; due to the risk of intraoperative Hemorrhage and the potential injuries because of contiguity and dislocation of adjacent organs.
Symptoms:
Mild cervical myomas may not cause any problems while moderate to severe myomas may cause one or more of these symptoms:
1. Painful or excessive bleeding during the period.
2. Bleeding between your periods.
3. Menstrual clots.
4. Anemia, as a result of heavy bleeding, accompanied by fatigue
5. A feeling of fullness in your lower belly (abdomen)/bloating.
6. Frequent urination (this can happen when a fibroid puts pressure on your bladder).
7. Dyspareunia
8. Low back pain and pain in the pelvis.
9. Constipation or feeling pressure on your rectum.
10. Long-term (chronic) vaginal discharge.
11. Inability to pee or empty your bladder.
12. Increased abdominal distention (enlargement), causes your abdomen to look pregnant.
The symptoms of uterine fibroids usually stabilize or go away after you’ve gone through menopause because hormone levels decline within your body.
Treatment:
Small myomas that do not cause symptoms may not need to be treated. However large fibroids/myomas that are causing pain, bleeding, or urinary problems can be surgically removed via myomectomy. Depending on the size and location of the cervical fibroid/myomas, the doctor may perform one of three procedures.
Drug therapy may be an option for some women with fibroids/myomas. Heavy bleeding and painful menstrual cycle caused by fibroids/myomas may be controlled with medications. They may not prevent the growth of cervical myomas. Surgery may not be avoidable. Drug treatment for fibroids includes the following options:
Birth control pills (oral contraceptives) and other types of hormonal birth control methods: These drugs often are used to control heavy bleeding and painful periods.
Gonadotropin-releasing hormone (GnRH) agonists: These drugs stop the menstrual cycle and can shrink fibroids. They sometimes are used before surgery to reduce the risk of bleeding.
Progestin intrauterine device (IUD): An option for women with myomas that does not distort the inside of the uterus. It reduces heavy and painful bleeding. The medication does not treat the myomas.
Laparoscopy
A procedure in which the surgeon conducts the operation through one or more tiny incisions near the belly button. A thin, flexible, lighted instrument, called a laparoscope, helps the doctor to see the surgical site.
Laparotomy
It is an open surgical procedure in which the surgeon removes the myomas through a larger abdominal incision.
Hysterectomy
Complete surgical removal of the uterus and sometimes the ovaries. If the fibroids are very large, this may be the surgeon’s only option. After a hysterectomy, the female patient can no longer become pregnant.
conclusion:
These are the fibroids that are present in the cervix and different factors like hormonal imbalance or family history might be the cause. Anemia and pain in the abdomen are the common symptoms. The basic treatment is myomectomy, in some cases, mediation is used. Treatments like laparoscopy, laparotomy, and hysterectomy are surgical procedures to remove fibroids.
0 notes
Text
Tips for Successful Home Artificial Insemination
Home artificial insemination (AI) is a method used to help couples conceive by transferring sperm into the female partner's uterus. It offers couples an alternative method to traditional in-clinic insemination and can provide convenience and privacy. However, achieving successful home insemination requires careful planning and preparation. Here are some essential tips to keep in mind: Get more information please visit here "intracervical insemination kit"
Understand the Process Before embarking on the home insemination journey, it is essential to have a clear understanding of the procedure. Familiarize yourself with the necessary equipment, such as the insemination syringe, ovulation predictor kits, and warm and cold storage options. Consider seeking guidance from a fertility specialist or attending a workshop or seminar to gain additional knowledge.
Timing is Key Timing is crucial in home insemination. It is essential to identify the woman's peak fertility period, which is typically around ovulation. This can be done using ovulation predictor kits or monitoring basal body temperature. Once the woman has identified her fertile window, she should schedule the insemination procedure accordingly.
Proper Technique To ensure successful insemination, it is essential to follow proper techniques. Wash the sperm sample thoroughly to remove any contaminants. Use a clean and sterile insemination syringe to deposit the sperm into the vagina near the cervix, aiming for the uterine opening. Be gentle and careful to avoid injury or discomfort.
Maintain a Comfortable Environment Creating a comfortable and stress-free environment during the insemination procedure can enhance the chances of success. Choose a quiet and private space, ensuring adequate lighting and a comfortable temperature. Consider playing music or using a relaxation technique to reduce anxiety and tension.
Follow Proper Aftercare After insemination, it is essential to follow proper aftercare instructions. Avoid engaging in sexual activity for a specified period to prevent any potential complications. Use vaginal lubricants if necessary and stay hydrated. Regularly monitor for any signs of pain or discomfort and seek medical attention if necessary.
Maintain Regular Monitoring Success in achieving pregnancy through home insemination often requires patience and perseverance. It is essential to monitor the woman's fertility signs closely during the waiting period. Regular pregnancy tests can help determine the progress and provide reassurance. Keep in touch with a fertility specialist or seek their advice if there are any concerns or complications.
Stay Positive and Patient Success in home insemination can depend on various factors, including individual health and fertility. It is essential to stay positive and patient throughout the process. Celebrate successes along the way, no matter how small they may seem. Remember that every couple's journey to parenthood is unique, and setbacks are common.
1 note
·
View note
Text
Understanding the Intracervical Insemination Procedure: A Comprehensive Guid
Introduction:
Intracervical insemination (ICI) is a fertility treatment method that involves introducing sperm into the cervix to enhance the chances of successful fertilization. This procedure is often chosen by individuals or couples facing fertility challenges and can be a viable option for those looking for a less invasive intracervical insemination procedure alternative to other assisted reproductive technologies. In this article, we will delve into the details of the intracervical insemination procedure, its purpose, preparation, and what individuals can expect during and after the process.
I. Purpose of Intracervical Insemination:
The primary goal of intracervical insemination is to facilitate the union of sperm and egg, increasing the probability of conception. This procedure is particularly beneficial for couples experiencing difficulties conceiving due to issues such as low sperm count, cervical mucus problems, or unexplained infertility. ICI is considered less invasive compared to other assisted reproductive technologies, making it a more accessible option for some individuals.
II. Preparing for Intracervical Insemination:
A. Initial Consultation: Before undergoing intracervical insemination, individuals or couples typically have an initial consultation with a fertility specialist. During this consultation, the medical history of both partners is discussed, and any potential fertility issues are identified. The fertility specialist will determine if intracervical insemination is an appropriate course of action based on the specific circumstances.
B. Ovulation Monitoring: Timing is crucial in intracervical insemination. Ovulation monitoring is often recommended to pinpoint the most fertile window during the menstrual cycle. This can be achieved through various methods such as tracking basal body temperature, using ovulation predictor kits, or undergoing ultrasounds to monitor follicle development.
C. Sperm Preparation: On the day of insemination, the male partner provides a sperm sample. The sperm sample undergoes a process called sperm washing, where sperm is separated from the seminal fluid. This step helps concentrate healthy and motile sperm, enhancing the chances of successful fertilization.
III. The Intracervical Insemination Procedure:
A. Speculum Insertion: Similar to a pelvic exam, the woman lies on an examination table with her feet in stirrups. A speculum is inserted into the vagina to provide access to the cervix.
B. Sperm Insertion: Using a thin, flexible catheter, the prepared sperm is gently inserted through the cervix into the uterine cavity. The catheter is then withdrawn, completing the insemination process.
C. Post-Insemination Monitoring: After the procedure, some individuals may be advised to lie down for a short period to increase the likelihood of sperm reaching the egg. Others may resume normal activities immediately. Follow-up appointments with the fertility specialist may be scheduled to monitor progress and discuss any necessary adjustments to the treatment plan.
IV. Potential Benefits and Considerations:
A. Less Invasive: Intracervical insemination is considered less invasive than procedures such as in vitro fertilization (IVF) or intrauterine insemination (IUI). This makes it a suitable option for those seeking a more straightforward fertility treatment.
B. Cost-Effective: In comparison to more complex assisted reproductive technologies, intracervical insemination tends to be more cost-effective, making it a preferred choice for some individuals or couples.
C. Success Rates: Success rates can vary depending on the underlying fertility issues and the overall health of the individuals involved. It's essential to manage expectations and work closely with a fertility specialist to optimize the chances of success.
Conclusion:
Intracervical insemination is a fertility treatment that offers hope to individuals and couples facing challenges in conceiving. While it may not be suitable for everyone, it provides a less invasive and more cost-effective alternative to intracervical insemination procedure other assisted reproductive technologies. With proper preparation, monitoring, and guidance from fertility specialists, intracervical insemination can be a valuable option on the journey towards building a family. If you are considering this procedure, consult with a fertility specialist to determine the most appropriate course of action based on your unique circumstances.
1 note
·
View note
Text
Artificial Insemination Market Applications and Current Status
Global Artificial Insemination Market, Type (Intrauterine Insemination, Intracervical Insemination, Intravaginal Insemination, Intratubal Insemination), Product Type (Insemination Kits, Home Conception Devices, Accessories), Source Type (AIH-Husband, AID-Donor), End- User (Hospitals, Fertility Clinics, Clinics, Others) – Industry Trends and Forecast to 2029
An expert team performs systematic, object-oriented and complete market research study to provide the facts associated with any subject in the field of marketing via Artificial Insemination marketing report. The report has a lot to offer to both established and new players in the Artificial Insemination industry with which they can completely understand the market. SWOT analysis and Porter’s Five Forces analysis methods are used wherever applicable, while generating this report. One of the most important parts of an international Artificial Insemination market report is competitor analysis with which businesses can estimate or analyse the strengths and weaknesses of the competitors.
Key Players
Some of the major players operating in the Artificial Insemination market are Genentech, Inc., Sun Pharmaceutical Industries Ltd., Bristol-Myers Squibb Company, F. Hoffmann-La Roche Ltd., Merck & Co., Inc., Aeterna Zentaris, BIOFRONTERA AG, Johnson & Johnson Private Limited, Sanofi, Novartis AG, Bayer AG, Pfizer Inc., GlaxoSmithKline plc, Akorn, Incorporated, Teva Pharmaceutical Industries Ltd., Boehringer Ingelheim International GmbH., AstraZeneca, Almirall, S.A, Abbott, Astellas Pharma Inc., and Glenmark Pharmaceuticals Limited, among others.
Browse More Info @ https://www.databridgemarketresearch.com/reports/global-artificial-insemination-market
With the help of credible Artificial Insemination market analysis report, businesses can make out the reaction of the consumers to an already existing product in the market. The report includes estimations of recent state of the market, CAGR values, market size and market share, revenue generation, and necessary changes required in the future products. A wide-ranging competitor analysis helps build superior strategies of production, improvement in certain product, its advertising or marketing and promotion for the business. Exhaustive and comprehensive market study performed in the wide ranging Artificial Insemination market report offers current and forthcoming opportunities that put light on the future market investment.
Key questions answered in the report:
Which product segment will grab a lion’s share?
Which regional market will emerge as a frontrunner in coming years?
Which application segment will grow at a robust rate?
Report provides insights on the following pointers:
Market Penetration: Comprehensive information on the product portfolios of the top players in the Artificial Insemination Market.
Product Development/Innovation: Detailed insights on the upcoming technologies, R&D activities, and product launches in the market.
Competitive Assessment: In-depth assessment of the market strategies, geographic and business segments of the leading players in the market.
Table Of Content
Part 01: Executive Summary
Part 02: Scope Of The Report
Part 03: Global Market
Part 04: Global Market Size
Part 05: Global Market Segmentation By Product
Part 06: Five Forces Analysis
More Reports:
Healthcare Business Intelligence Market
Chinese Hamster Ovary cells (CHO) Market
Diuretic Drugs Market
Patient Engagement Technology Market
Anti-cancer Drug Market
About Us:
Global Artificial Insemination Market, Type (Intrauterine Insemination, Intracervical Insemination, Intravaginal Insemination, Intratubal Insemination), Product Type (Insemination Kits, Home Conception Devices, Accessories), Source Type (AIH-Husband, AID-Donor), End- User (Hospitals, Fertility Clinics, Clinics, Others) – Industry Trends and Forecast to 2029
An expert team performs systematic, object-oriented and complete market research study to provide the facts associated with any subject in the field of marketing via Artificial Insemination marketing report. The report has a lot to offer to both established and new players in the Artificial Insemination industry with which they can completely understand the market. SWOT analysis and Porter’s Five Forces analysis methods are used wherever applicable, while generating this report. One of the most important parts of an international Artificial Insemination market report is competitor analysis with which businesses can estimate or analyse the strengths and weaknesses of the competitors.
Key Players
Some of the major players operating in the Artificial Insemination market are Genentech, Inc., Sun Pharmaceutical Industries Ltd., Bristol-Myers Squibb Company, F. Hoffmann-La Roche Ltd., Merck & Co., Inc., Aeterna Zentaris, BIOFRONTERA AG, Johnson & Johnson Private Limited, Sanofi, Novartis AG, Bayer AG, Pfizer Inc., GlaxoSmithKline plc, Akorn, Incorporated, Teva Pharmaceutical Industries Ltd., Boehringer Ingelheim International GmbH., AstraZeneca, Almirall, S.A, Abbott, Astellas Pharma Inc., and Glenmark Pharmaceuticals Limited, among others.
Browse More Info @ https://www.databridgemarketresearch.com/reports/global-artificial-insemination-market
With the help of credible Artificial Insemination market analysis report, businesses can make out the reaction of the consumers to an already existing product in the market. The report includes estimations of recent state of the market, CAGR values, market size and market share, revenue generation, and necessary changes required in the future products. A wide-ranging competitor analysis helps build superior strategies of production, improvement in certain product, its advertising or marketing and promotion for the business. Exhaustive and comprehensive market study performed in the wide ranging Artificial Insemination market report offers current and forthcoming opportunities that put light on the future market investment.
Key questions answered in the report:
Which product segment will grab a lion’s share?
Which regional market will emerge as a frontrunner in coming years?
Which application segment will grow at a robust rate?
Report provides insights on the following pointers:
Market Penetration: Comprehensive information on the product portfolios of the top players in the Artificial Insemination Market.
Product Development/Innovation: Detailed insights on the upcoming technologies, R&D activities, and product launches in the market.
Competitive Assessment: In-depth assessment of the market strategies, geographic and business segments of the leading players in the market.
Table Of Content
Part 01: Executive Summary
Part 02: Scope Of The Report
Part 03: Global Market
Part 04: Global Market Size
Part 05: Global Market Segmentation By Product
Part 06: Five Forces Analysis
More Reports:
Healthcare Business Intelligence Market
Chinese Hamster Ovary cells (CHO) Market
Diuretic Drugs Market
Patient Engagement Technology Market
Anti-cancer Drug Market
About Us:
Data Bridge Market Research set forth itself as an unconventional and neoteric Market research and consulting firm with unparalleled level of resilience and integrated approaches. We are determined to unearth the best market opportunities and foster efficient information for your business to thrive in the market
0 notes