#i might draw gradient joe as well
Explore tagged Tumblr posts
Text

bug,,,,bo,,,,,,,,,,,, dont just like my art, reblog it!! pleas!!
#lakes art#bugbo#bugbo fanart#tuxpaint#i had too much making the bg it just looks like funny bubbles to me#i might draw gradient joe as well
10 notes
·
View notes
Text
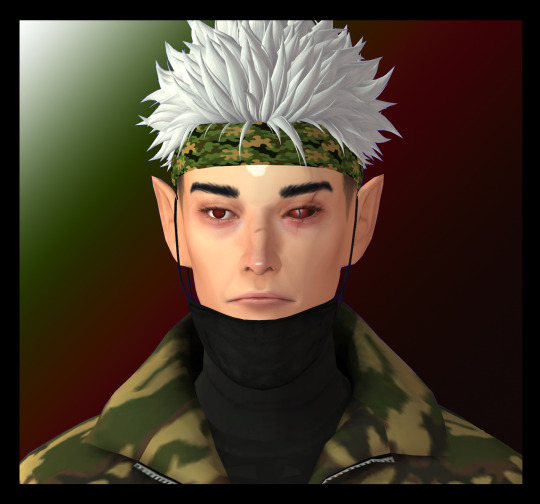
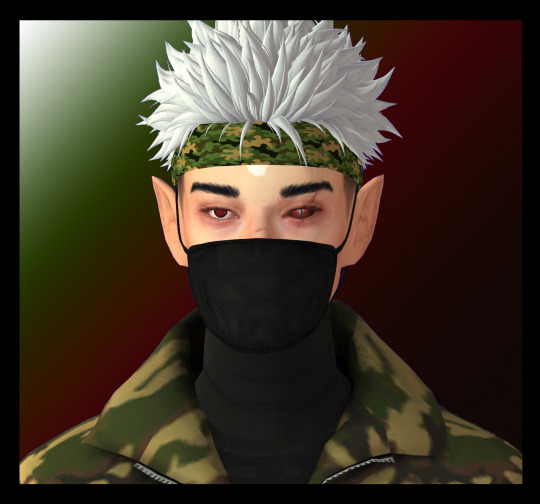


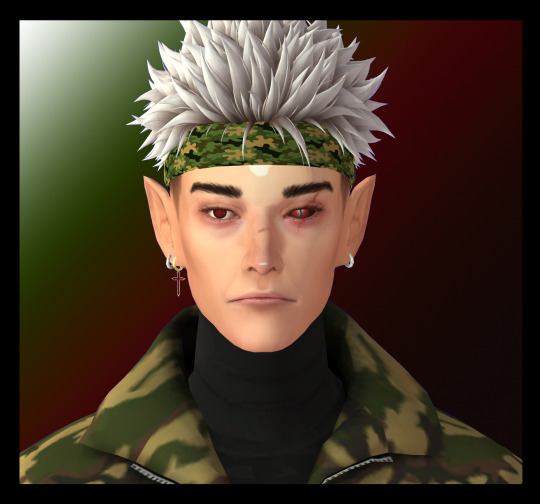
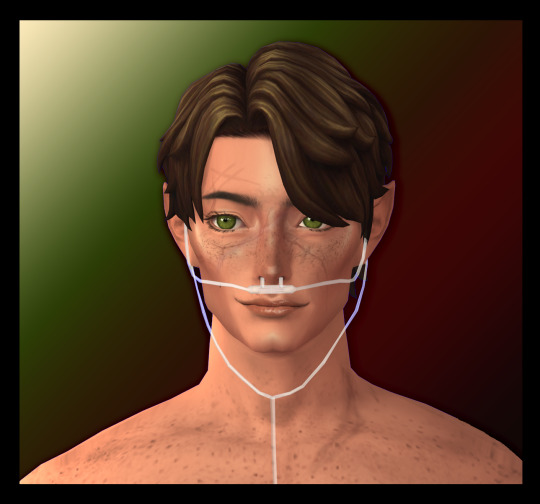
please pretend i finished this yesterday <3 i was up until 4:30am.
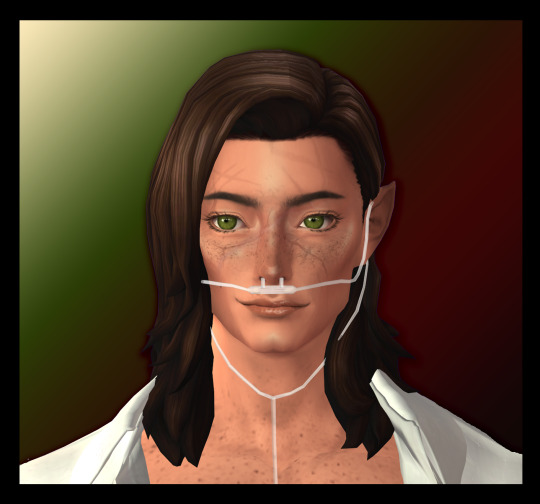
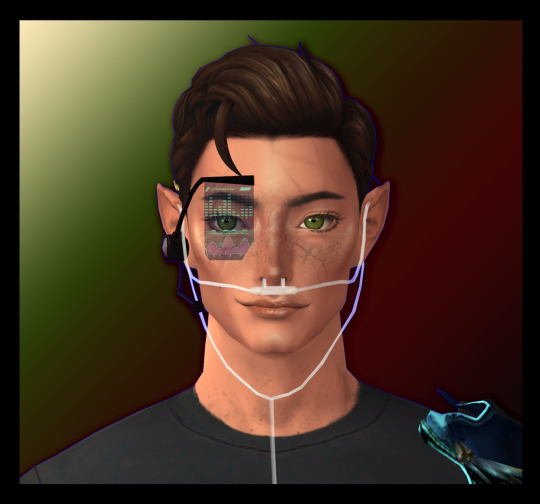
to see what he looks like (whole point of this exercise), first etho from start of s9.
raise up that mask for his modesty <3 ooh mysterious wonder what's under there (normal guy)
gas mask. he does live in an alien landscape by this point. a post limited life etho. he stole those earrings (guess who) (easy answer) (why his hair is brownish now) (don't randomly soulbond to people fellas [gn]. leaves lasting impacts on your physiology.)
a post double life etho <3 he was freely given those earrings. Retroactively they will become stolen. Time is relative <3.
maskless post secret-life Etho. <3 <3 For your full understanding of his design. (The sims are basically how I would draw the characters, for the most part. Er. Jevin is... not simmable. Nor is muppet Joe... Im working on it!!! I'm working on it. Joe was meant to be made today but I really need to finish my dissertation. This was me procrastinating. Do not follow my example.)
Anyways! Hermitaday 17 - Ethoslab!! As i am currently unable to draw for a number of reasons, I thought showing my sims of the hermits would be a cool idea. (And since i haven't done any previous days because of my university degree dissertation, have a bunch of random hermits under the readmore; s9 editions)















in order;
general application bdubs <3
king cleo, human hair (wearing a sleevless dress. just. syk.)
king cleo, gorgon hair <3
elven warrior princess gem, outfit 1* <3
general application pearl <3
dwarven imp Impulse <3
elven warrior princess gem, outfit 2* [*I had full body pics of everyone, but I lost them >-< oh well. you get to see doc at least?] <3
general application grian [he's. a bit weird looking. sorry. i try really hard but i am blind. You... don't want to see my first etho attempt
general application false <3
SCARS SO MANY SCARS. first; buttercup <3
second; shirtless. he does that a lot.
cool shirt you can't see because i lost the picture :(
park architect scar <3
elf scar <3
hotguy!!!
doc! m! 77!!
full fit of doc! m! 77!!
mr Ren Dog <3 not finial version. might change the ears?
(The gradients were randomly chosen from my pre-existing gradient collection <3 do not read into them. Except the impulse one because. easy guy to make gradient for. easy. Also you do not see colour banding. it does not exist! sRGB sucks.)
Sm bonus pics (bc i found the fullbodies!!! they're just not edited. no fun gradients. pure blue chroma
(sorry. cw eyestrain:)

fun shirt!!!!!!!!!!!!!

iconic

the guy in question. very tiny <3 because of how photosets work. clicketh the images for better visability.


gems!!!!!!!!!!!
and that's all tumblr will let me fit </3 have a good day everyone who clicked thru to this part!!! <3
#hermitaday#a day late *symbol smash*#<- /joke sorry. sorry it's late. i was up until 4:30am#simply had to crash </3#anyway: etho!!! slab!!! etho's lab!!!#hc#hcfanart#???? i guess#hc etho#these are s9 ethos#just ftr#from start of season + end of season (post secret life)#he stole the earrings. he stole them. those are stolen earrings.#guess who from (easy) (reason his hair changes shades slightly)#(i love giving characters lasting consequences of their actions) (getting soulbound to each other)#HMMMM i wonder. lol. anyway#hope you like him!!!!!!! i spent a lot of time on him!!!!!!!!!!!#and hope you like the rest of them i also spent a lot of time on the rest of them. but this is etho's moment not theirs /sorry for not#having posted theirs on their days :( ive been a busy gal#ts4#ts4edit#??? i guess#ts4 hermitcraft
1 note
·
View note
Text
The Ethics of Keeping Alfie Alive
By SAURABH JHA
Of my time arguing with doctors, 30 % is spent convincing British doctors that their American counterparts aren’t idiots, 30 % convincing American doctors that British doctors aren’t idiots, and 40 % convincing both that I’m not an idiot.
A British doctor once earnestly asked whether American physicians carry credit card reading machines inside their white coats. Myths about the NHS can be equally comical. British doctors don’t prostate every morning in deference to the NHS, like the citizens of Oceania sang to Big Brother in Orwell’s dystopia. Nor, in their daily rounds, do they calculate opportunity costs for keeping patients alive on ventilators.
Conversations such as this are vanishingly rare.
Administrator: “It’s costing an arm and leg keeping this sick baby alive – to balance the annual budget we need to stop dialyzing a granny.”
ICU doctor: “We’ll have to send poor Ethel to her grave. That’s a shame. She was beginning to grow on me.”
Health Ethicist: “Wait, let me check with National Institute of Clinical Excellence, the rationing experts, who should be relieved of intensive care first. Perhaps it should be Winston, not Ethel – because Winston is an alcoholic. We need to make rationing scientific and fair.”
For the most parts, doctors in both systems do their best for their patients – the constraints of biology play a greater role in influencing physician decisions than the economics of fee-for-service or capitation. This doesn’t mean the system is unimportant – the system sets the stage which shapes decisions systematically – and differences between systems are most evident in gray zones. For instance, British doctors don’t relish missing STEMI anymore than American physicians – but their propensity to get a triple rule out study for vague chest pain may be lower.
To wit, if American doctors do more and British doctors do less, it’s because they believe, respectively, that more and less are in their patient’s best interests. Part of the challenge analyzing physicians, ever since the Dartmouth studies on variation in physician practice, is reconciling in opposite medical decisions similar intentions.
And some differences between the two systems can be stark, and not just in how we spell (o)esophagus. The starkest differences are in the nature and intensity of care, specifically when and who decides medical intervention should be withdrawn, in end-of-life (EOL). The recent case of baby Alfie Evans illustrates these transatlantic differences.
Ventilated without hope
Known to have marked developmental delay, Alfie presented to Alder Hey Hospital, Liverpool, at seven-month age with febrile seizures and pneumonia. Alfie had severe difficulty in breathing and was intubated and transferred to pediatric intensive care unit (PICU). It turned out that fever was not causing seizures – nor were they primary seizures, i.e. seizures for no good reason. His seizures were secondary to severe encephalopathy – severe brain dysfunction.
How severe was Alfie’s encephalopathy? MRI showed substantial areas of reduced diffusion in his brain. The existential struggle of neurons is in throwing sodium out and bringing potassium into the cells by the sodium-potassium pump against their gradients, i.e. against their will – politics at a cellular level is all fascism. When the neuron gives up, meaning the pump fails, sodium builds up in the cells. Then water rushes in, but as the cell swells with water, the diffusion of water slows. Restricted diffusion meant that vast territories of Alfie’s neurons had surrendered.
Failed neurons still express themselves electrically. Afie’s EEG showed purposeless electrical activity, essentially seizures. Though the analogy is not exact, Alfie’s neuronal activity was like ventricular fibrillation – the electrical activity existed for its own sake; it was extreme anarchy without a purpose.
Alfie had infantile spasms. First described by English surgeon, James West, infantile spasms are pernicious not just because they often imply an incurable encephalopathy, but because of their nature. West described these attacks as “…. a complete heaving of the head forward towards his knees, and then immediately relaxing into the upright position, something similar to the attacks of emprosthotonos.” Seen also in tetanus infection and strychnine poisoning, in emprosthotonos the head and feet come together with the back fully arched. It’s not a pretty sight. Infantile spasms are difficult to treat.
Alfie’s repeat MRIs showed that the encephalopathy had progressed. The thalamus, the headquarters of sensation, was barely extant. Not only had the cerebellum, the fine tuner of movements, been replaced by water but so had the basal ganglia, through which commands for gross movement travel. It’s not the volume of neurons per se which is important, but what the neurons are doing. Alfie had too few neurons doing too little.
As radiologists recognize, diagnostic tests don’t stand on their own – clinical correlation is advised. Alfie’s clinical situation portended an even graver prognosis than his MRI suggested. He was in coma and depended on mechanical ventilation. Alfie’s muscle tone was too weak to even form contractures. Deep pressure above the eye – a richly innervated area – elicited no response. There was no response to loud noise. And, most portentous, his pupillary reflex was abnormal.
When light is shone in the eyes the pupils constrict. The optic nerve, via the command center in the mid brain, tells the oculomotor nerve – a doer, not thinker, nerve – to close the blinds. The absence of normal pupillary reflex, taken in context of Alfie’s MRI findings, confirmed that his midbrain was gutted.
Because of Alfie’s semi-vegetative state his physicians believed that palliation, not ventilation, was in his best interests. Alfie’s parents, devout Catholics, disagreed and sought the counsel of the Pope. Alfie was granted Italian citizenship. A military helicopter was ready to transfer Alfie to a hospital in Rome, but Alder Hey Hospital stopped the transfer. Finally, the courts were involved. The High Court sided with the hospital. The Court of Appeal sided with the High Court. After an aggressive legal battle, and after a year of being dependent on ventilation, Alfie’s ventilator was stopped. Five days later Alfie died.
Alfie’s case elicited strong responses from pro-lifers, libertarians and American conservatives, ranging from parody to disgust. Joe Walsh, with his tongue somewhere near his cheek, used Alfie’s example to underscore the importance of the Second Amendment – though how AR-15s titrate the dose of inotropes in the ICU was not explained by Walsh. Some likened stopping ventilation in Alfie to murder. Even more thoughtful observers were disturbed and saw over reach of medical paternalism, a triumph of the state over the individual, and a moral failing of the NHS.
The crux of the dispute is who has the last say in a child’s treatment decisions – parents or physicians. Many believe that in EOL the right exclusively belongs to parents, which Alder Hey violated by stopping Alfie’s transfer to Italy. However, the matter is not as ethically clear cut as it first appears.
Doctors versus Parents
Parent’s right to ignore physician’s management of their child is not absolute. For example, parents can’t stop antibiotics for acute bacterial meningitis just because they have an objection to antibiotics. But they can object to their child being immunized – even though immunization benefits their child. Medical paternalism isn’t absolute but there are zones in which it becomes absolute and zones in which it is ineffective.
Why can doctors treat a child against parent’s wishes for meningitis but not vaccinate a child against parent’s wishes? Intuitively we see the difference – meningitis has a high mortality untreated. Though, with labored reasoning, we can also create an indistinction. An unvaccinated child is also at risk of death from the infection the vaccine seeks to prevent – though the mortality risk is nowhere near that from untreated meningitis, it is not zero.
Thus risk, in and of itself, cannot be what permits medical paternalism in one but not the other. One may reason that it’s not risk per se but the degree of risk which distinguishes the two. This is an argument of degree. The trouble with arguments of degree, as scientific and logical as they sound, is that they inevitably lead to the question: where do we draw the line? By line I mean a threshold of risk – a numerical or even a descriptive threshold of mortality above which medical paternalism is permitted and below which it is not.
No such line in the sand exists though it need not exist for us to see that the risk of imminent death from meningitis vastly exceeds risk of death from an infection one doesn’t have but might have. And here is the important point: one need not have defined a precise threshold of risk over which doctors prevail over parents should a conflict arise, in order that medical paternalism prevails in the treatment of bacterial meningitis. The child is in danger – arguing where imaginary lines are drawn would be silly. Nor do we need to define “danger.” Some things are self-evident – obvious without explicit definitions.
There are situations where the diagnosis is less clear cut than acute bacterial meningitis, where doctors still prevail over parents when it comes to a child’s well-being. Take a child with fever, rigors, cough and weight loss with nodules on the chest radiograph, and the doctors make a presumptive diagnosis of military tuberculosis and ask that the child be admitted in hospital for treatment. The parents cannot transfer the child to Spain for a second opinion if that transfer interferes with the treatment and may harm the child. However, if a child has headaches and the physician decides against an MRI, believing that the headaches are tension headaches, the parents have every right to get the child checked by any physician anywhere in the world.
Let’s return to the case of parents objecting to their child being vaccinated. An unvaccinated child places other children at risk by potentially disrupting herd immunity. Vaccination is for both individual and greater good. Yet NHS doctors, doctors in socialized medicine, a system – let us remind ourselves – in which society pays for the individual, can’t vaccinate children against parent’s wishes even though vaccination increases net societal welfare by building herd immunity. Put it this way – medical paternalism can’t prevail over parents’ wishes to help other children. Doctors only prevail if a particular child’s welfare is in jeopardy. Far from being in service of utilitarianism, of greatest good for the greatest number, doctors in the NHS triumph over parents only when a specific child is in danger.
Medical Paternalism in End-of-Life
To recap, there are three points. First, neither parental wishes nor medical paternalism is absolute. Second, when doctors and parents have opposing views on medical management of a minor there is no explicit line in the sand which separates situations where doctors prevail from situations where parents prevail. Third, increasing net social welfare is not a reason for doctors to prevail over parents.
The question is should parents have the last say in end-of-life decisions about their child. Specifically, when parents wish to prolong the life of a terminally ill child with profound neurological compromise at all costs – by costs I don’t mean financial costs but medical intervention – but doctors believe palliation, not prolongation of life, is in the best interests of the child, who should prevail?
Palliative care is clearly different from the antibiotics-meningitis example in which the doctors prevail because antibiotics save the child’s life. At first it may seem odd, not just to a restless logician, that medical paternalism prevails over parental wishes both to extend a child’s longevity and not to try to extend it. Surely, there’s a distinction between starting treatment and stopping treatment.
The distinction between palliative care and antibiotics for meningitis is not a distinction of degree but a categorical distinction. Palliation seeks not so much to curtail life but to relieve it from suffering. If the appropriateness, or lack thereof, of medical paternalism in EOL decisions is to be explored, we must explore the role of doctors in palliative care.
The goal of medical care isn’t always to prolong life by any means necessary, is often just symptom relief, and sometimes to keep the terminally ill comfortable, to ensure that they’re treated with dignity. These goals aren’t always congruent, and sometimes oppositional.
There are fates worse than death. Keeping the cardiorespiratory system intact by aggressive modern medical techniques in persistent vegetative state may seem humane to some but does seem inhumane to many. End-of-life is at best an ethical gray zone – by that I mean you can understand both the stance of the family and the point of view of the doctors. As the patient, the rightful decision maker, by the very nature of their terminal and profound neurological compromise is unable to articulate their preferences, someone must make a decision.
The role of medicine in palliative care is not absolute – there is much to palliation which is metaphysical. But doctors do have an important role in determining prognosis, in ascertaining that prognosis is indeed hopeless, and establishing that palliation, whatever may comprise it, is appropriate.
The conclusion that Alfie’s neurological deficit was substantial, progressive and incurable was fundamentally a medical analysis, which Alfie’s physicians, world experts in pediatric neurology, made by their in-depth understanding of biology and careful assessment of Alfie. It would be humane including Alfie’s parents in the decision making, encouraging and indulging all the questions they have. It would be naive concluding they knew more about Alfie’s prognosis than his physicians.
Alfie’s father believed that Alfie was summoning him for help. He thought he saw Alfie yawn. It is humane respecting his beliefs. It is unwise abandoning medical judgment. When experts studied videos of Alfie’s movements they concluded that they were nothing more than seizures. Alfie’s father, a non-physician, a grieving father in understandable denial, could not possibly be expected to make the same analysis.
Some have asked how letting Alfie die can be in his best interests. The argument advanced is that stopping ventilation couldn’t possibly be in Alfie’s best interest because it hastened his death. Others have gone a step further and compared stopping ventilation in Alfie to euthanasia, or even murder.
I’m tempted to ignore the charge that stopping Alfie’s assisted ventilation is murder – but it’s worth thinking it through just to show how unfettered logic becomes fanatical. The rationale is that it’s murder stopping Alfie’s ventilation against his parent’s wishes but not murder if the parents consent to withdrawal of ventilatory support. Imagine if I said – it’s murder if you shoot a child but not murder if the parents ask you to shoot their child. You would think that I have lost the plot.
Was taking Alfie off the ventilator state-sponsored euthanasia, as former leader of UKIP, Nigel Farage, insinuated? Was this the same as a neurologically intact eighty-year-old man with untreatable pain from metastatic prostate cancer flying to Switzerland to receive a lethal dose of morphine? In our conflationary zeal we see similarities when we wish to – but the two situations are different. In the latter, a person capable of making their own decision enters a mutual agreement with a physician to end life. Are we unable to distinguish between stopping intensive care to reduce suffering in the terminally ill from administering a drug with the express purpose of ending life? Is intention irrelevant?
I can put it no better than the Catholic church which distinguishes between withdrawal of ventilatory support and euthanasia, and says eloquently in their catechisms, (2278): “here one wills not to cause death. One’s inability to impede death is merely accepted.”
Was Alfie Suffering?
How could it possibly be in Alfie’s best interest to die? This question is usually accompanied by another: who are doctors to decide that Alfie needed palliation?
The first question is a partial strawman. His doctors’ intention with palliative care wasn’t to end Alfie’s life but to give him dignity in the attenuated life he had left. This is not a distinction without a difference but a nuanced distinction which hinges on intent. Physicians must be judged, or at least judge each other, by intent, not just outcome. If a physician gives thrombolysis to a patient with acute stroke and the patient gets a brain hemorrhage and dies, the intention of the physician was to open the artery and restore function, not cause hemorrhage and end life. To ask how substituting life prolonging mechanisms with palliative care could possibly be in Alfie’s interest is to question the very essence of palliative care.
Let’s reframe the first question. In a person in a vegetative state is there something inherently inhumane about constantly changing artificial feeding and respiratory access, manipulating support lines, fighting infection, getting numerous x-rays and CT scans, and breaking ribs in attempts at cardiopulmonary resuscitation? The question isn’t whose call it is to switch the ventilator off – that’s an important question, too – the question is whether there is indignity in prolonging life of someone in a vegetative state. Science can’t help you here – it’s your moral intuitions you have to call upon.
It is the patient, not the doctor, who determines their quality of life. However, if the patient can neither feel, that is they lack consciousness, nor articulate that they can feel or not – we do not know whether they prefer palliation over prolongation of life. The second question is a paradox. However, when we do not know we must assume – there is no getting away from assuming – but no normative ethics says that we must assume that a patient in a vegetative state would wish for life to be prolonged, rather than assume that they desire palliation, instead.
The retort is that if a person in a mall has a cardiac arrest would you not assume the person wishes to live and administer CPR? The nuance is in appreciating that we do not know the neurological prognosis in a person unknown to us, which is a different kettle of fish from Alfie’s situation – where the dismal neurological prognosis was without reasonable clinical doubt.
Putting aside pain and suffering, which have some objectivity to them, let’s consider indignity. Alfie could neither feel nor express whether he was experiencing indignity which is, admittedly, a more nebulous concept, but not that nebulous. For example, it is disrespectful being casual about the body of the deceased and there is dignity in giving the deceased a decent burial. Even Osama bin Laden’s body was treated with respect. We treat the body of the deceased with respect not because of the feelings of the deceased, who can’t feel, but for ourselves. It is we, not the deceased, who decide that there is indignity in treating their body with disrespect.
Similarly, the indignity, or lack thereof, in prolonging life in a patient in a vegetative state cannot be decided by the person in a vegetative state – this ought to be so obvious that you should berate me for saying it. Though it is still disputable who has the final say when ventilator should be switched off, doctor or the family, there should be little dispute that it can be the person in the vegetative state, unless that person has an advanced directive specifying their preferences ex ante.
Stopping the Airlift to Italy
After Alfie’s father, Thomas Evans, posted about Alfie’s condition on Facebook, Christine Broesamle, a pro-life activist in Italy got in touch with him. Broesamle moved to Liverpool and began counseling the Evans – who accepted her help in sheer desperation. Also helping the Evans was a law student from Christian Legal Center, Pavel Stroilov.
Broesamle had substantial influence. She had at her beck and call a network of non-NHS doctors who she called upon to assess Alfie. The doctors, pretending to be family friends of the Evans, assessed Alfie behind the back of Alder Hey physicians. Professional courtesy was thrown to the wind. Though it is unclear whether it was because of Broesamle’s influence, the Pope met Evans. The Pope is a busy chap and can’t possibly meet every parent in the world with a dying child – there are millions dying in Africa, hundreds from snake bite, thousands from treatable malaria. But somehow the Pope found the time to meet Thomas Evans.
Thus, the Evans were surrounded by enthusiastic pro-life Christians. There’s, of course, nothing wrong with that – faith has a role in easing the pain of EOL. However, the new friends of the Evans had their own axes to grind. They were interested in Alfie not because he had a treatable condition, but precisely because his condition was untreatable – i.e. he was at the end-of-life.
Neither Broesamle nor Stroilov had kind words to say about Alder Hey Hospital. Broesamle accused Alder Hey physicians of being determined to kill him. Stroilov was described by Justice Hayden, the judge who presided over the legal dispute, as a “fanatical and deluded young man” – particularly harsh words from a usually temperate British judge. After Alfie died, Stroilov egged Thomas Evans to sue Alfie’s physicians for conspiracy to murder in private courts. Thomas Evans, wiser than his advisors, decided against it.
As the media sensationalism began, the rift between the Evans and Alder Hey physicians widened. Alfie was to be air rescued to Bambino Gesu Hospital (BGH). The Alder Hey physicians stopped the transfer. There was uproar. Mobs gathered outside the hospital.
Even thoughtful observers can’t understand why Alfie’s transfer to Italy was stopped. The dispute isn’t that Alder Hey violated the parent’s right to a second opinion. BGH were not offering a second opinion – and I’m assuming that the Pope wasn’t going to re-attempt the Raising of Lazarus miracle on Alfie. BGH was offering long term ventilation and feeding by means of a tracheostomy and gastrostomy, respectively.
The dispute is this. When the Alder Hey physicians knew that Alfie’s condition was hopeless, what was the harm in allowing Alfie to be airlifted to Italy? They were not using the public purse – the transfer and care were to funded by private money. There seems at once little moral, ethical, medical or financial reason to stop the transfer. Was this an ego battle between Alder Hey Hospital and pro-lifers?
Things spiraled very quickly out of control. The Italian government – who, once they granted Alfie Italian citizenship, threatened to hold the British government responsible for the homicide of an Italian citizen.
Were I Alfie’s neurologist I’d have allowed the transfer. I might have written a book, “Alfie and Me,” taken a selfie with Alfie and the helicopter and posted it on Twitter. I’d have invited the Pope to bless Alder Hey Hospital – and seen what would happen to the all-cause mortality. If a poor infant’s predicament was going to be made into an international circus show, I’d have milked it. But Alder Hey physicians aren’t as ostentatious as I am. And before we accuse them of being agents of the state, a particularly dishonest accusation coming from physicians, who rely heavily on the state for protectionism, it’s worth exploring their reasoning.
Their rationale cannot be strewn to one dimension. Alfie’s case was complex, and the sum of the parts shouldn’t be disrupted by attacking the individual parts. Alfie was in coma with no prospect of any motor or sensory function, with no capacity to express himself, whose only neuronal activity was seizures, which were resistant to treatment. Alfie’s neurological condition was not static, like cerebral palsy, but progressive. Though Alfie had too little thalamus to feel pain, they could not rule out that he was feeling pain – there’s a raging debate, not just of the philosophical nature, whether the brain is even necessary for consciousness.
They speculated, based on their strong clinical judgment, that there was a risk that the helicopter ride would have increased the frequency of Alfie’s intractable seizures. Indeed, the physicians in Italy made this assessment, too. This doesn’t mean that infants with epilepsy shouldn’t be air lifted. But Alfie’s situation was different, and any logic which counters the rationale of Alder Hey physicians must acknowledge Alfie’s unique case. It’s one thing flying an infant with status epilepticus when the purpose of transfer is treatment of the epilepsy, or another life-threatening condition. It’s another thing worsening the frequency of intractable seizures when the purpose of transfer isn’t cure but continuation of care. In the latter situation, it is imposing suffering – i.e. suffering from seizures – for no gain.
Alder Hey physicians were challenged –what’s the evidence the helicopter ride would have worsened Alfie’s seizures? “Show me the data” is a common refrain as it adds a patina of science but asking for data is ignoring the uniqueness of Alfie’s condition, ignoring the value of clinical judgment, of expertise in unique situations.
The irony is cute when the same physicians who laud physician expertise over journalists and economists, challenge the medical judgment of Alder Hey physicians. Why do they not extend the same professional courtesy they seek for themselves to Alfie’s physicians, who are experts in their own realm? I suspect it’s because of a lingering mistrust of NHS doctors. British doctors are believed to act for the state, society or greater good, rather than the patient. Mistrust of physicians is a transatlantic phenomenon. American physicians are thought to act for their financial interest rather than patient’s welfare. Mistrust of physicians is difficult to palliate because, as Othello discovered, once you start off with suspicion, it is difficult to be convinced otherwise.
Though it is hard seeing how Alfie’s physicians were wrong in believing that palliation, not prolongation of life, was in his best interest, the question remains: when family disagrees with doctors in EOL who should prevail? In the US, the family seems to prevail. I need not labor about the brutality of EOL in the US – and American physicians have spoken more lyrically on this topic than I ever could. Suffice to say that no normative ethics supports that the parents have the veto when the ventilator should be switched off in cases such as Alfie’s.
The Court
Britain is different but not that different. Even in Britain, doctors do not have a veto over parents in EOL decisions. Given the impasse between Alder Hey and Alfie’s parents the case went to the high court. The case was meticulously analyzed by Justice Hayden. He requested a broad range of medical opinion – from Great Ormond Street Hospital, from Rome, from Germany. The consensus supported the prognostic assessment of Alder Hey physicians.
Hayden praised Alfie’s father for his probing questions about the prognosis of Alfie but noted that he was understandably in denial about Alfie’s prognosis. Hayden was careful in not letting any histrionics enter his decision. For instance, he chided German physician, Dr. Haas, who in making the case that Alfie’s ventilator should not be switched off, alluded to his country’s legacy in treating disabled people. Hayden considered such allusions tendentious and inflammatory.
Through meticulous reasoning Hayden concluded that stopping ventilation was in Alfie’s best interest because his neurological impairment was advanced, progressive, incurable and, and this is the important addition, that there remained a possibility that Alfie was suffering.
Some see in his decision an over reach of the state. It is tempting invoking the state – but who is this nefarious entity we call the “state”? Elected members of parliament in Westminster, most of whom know little about terminal illness? Bureaucrats? Judges? The secret police? MI5? What did this nebulous, nefarious, entity gain from switching off Alfie’s ventilator?
A common sentiment is that the courts decided that Alfie’s life wasn’t worth living. In any contentious issue it’s a useful exercise re-framing the issue and seeing if you arrive at an alternative conclusion. That the courts were involved showed the limitations of medical paternalism. That Hayden solicited the opinion of pediatric neurologists showed the importance of medical expertise. That the experts agreed on Alfie’s prognosis wasn’t a medical conspiracy, but a moment of medical clarity. That Thomas Evans represented his case, and cross examined the experts, showed that extreme humanity is still possible in extreme circumstances. That Justice Hayden agreed with Alder Hey hospital showed that the hospital got it right.
Thus, far from the courts determining that Alfie’s life wasn’t worth living – by endorsing palliative care, they gave Alfie dignity, they gave his life its due worth by giving the possibility of his suffering considerable importance.
Was Alfie’s ventilator switched off because the NHS rations care?
One argument advanced was that if the issue was constrained resources, it was perfectly fine to switch Alfie’s ventilator off, so long as we all agree that it was about money. The argument, far from being exculpatory, makes the hospital seem reptilian, performing cost-benefit analyses on dying kids. Though resources are always constrained, even in the US, Alfie’s care was not subjected to the usual economic constraints in the NHS – he was in PICU for over a year. Not a dime was charged to his parents. Just imagine the medical bill if he was treated in the US.
The rationale of rationing is withholding expensive treatment which has small benefits because the benefits aren’t worth the costs – note, for rationing to even occur the intervention must have some, i.e. non-zero, benefit. By its very definition, you can’t ration an intervention which has zero benefit and may, in fact, have some harm.
Alder Hey physicians weren’t concerned about the costs of keeping Alfie alive. And costs were irrelevant precisely because Alfie’s condition was incurable. You can only do a cost-effectiveness analysis if there is effectiveness.
The slippery slope argument
A common argument made not just by pro-lifers but Burkean conservatives is the slippery slope argument, which goes like this. Once you decide that Alfie’s life is not worth living who is next? The kid with cerebral palsy? Trisomy 21? Autistic kid? Was Stephen Hawking’s life not worth it, either?
The slippery slope argument dominates public discourse these days. Many believe that Donald Trump’s election is a short step to National Socialism. And it’s not just Trump. When Obama was president, even thoughtful conservatives felt the outgrowth of government was a short step to fascism. In the slippery slope argument everyone templates their political prejudices to an imagined dystopia. It’s Orwell’s Room 101 – where you face your biggest fears.
The slippery slope rationale is first order thinking at its most primal. It is a type of Malthusian error – Malthus believed that the world would be so over populated that we’d be eating each other’s livers. His rationale assumed a linear progression of events, a sort of linear regression where everything else was held constant. It was a mark of a furtive, unchecked, imagination – aka, paranoia. Dystopians make great fiction. They are less useful as public policy.
Let’s examine the rationale because it’s worth introspecting. When history is assessed, it is assessed backwards – we see in Nazism and fascism culmination of several events which started off somewhat innocuously. This is historiography – where we see that short step which led to an evil regime. The error lies not in historiography, which is an analysis in hindsight, but in reverse historiography – which is a forward analysis – where we see in an event a short step to an evil. The trouble with reverse historiography is that many disparate events can potentially be a short step to whatever your most feared political regime happens to be.
Thus, in Alfie’s case we see a short step to the NHS deciding that kids with cerebral palsy will be deemed by the courts as “not worth living.” This is generalization writ large, a Kantian universalism, which is as disingenuous as it is wrong. It is ironic that the same people who laud individualism are so keen to generalize Alfie.
End-of-life is fertile grounds for slippery slope arguments, in part because it’s so difficult getting a grip on nuance. But EOL isn’t a spectrum; it comprises categories and each individual is their own category. You can’t compare Alfie’s predicament – a ventilator-dependent infant with progressive encephalopathy in coma, facing intractable seizures – with a conscious child with cerebral palsy. To conflate is to abandon judgment. For all the rugged individualism, nothing delivers individual nuance in medicine more than clinical acumen.
Physicians in End-of-Life
So long as life is prolonged by modern medical techniques, doctors will be involved in EOL decisions. End-of-life is an emotive area and clashes between family and physicians happen frequently. Spare a thought, though, for Alfie’s physicians who remain anonymous, who faced a mob outside the hospital, faced death threats, faced accusations of murder, faced vituperative attacks on social media. They are humans, too. Caught between doing the best for Alfie and relinquishing to populism they chose the former. You may disagree with their choice. But there’s little doubt that they were courageous physicians who stuck to their convictions. I, for one, give them a standing ovation.
About the author:
Saurabh Jha is a contributing editor to THCB and can be reached @RogueRad
The Ethics of Keeping Alfie Alive published first on https://wittooth.tumblr.com/
0 notes