#heparin dosing
Explore tagged Tumblr posts
Text
Ruben Dias x Reader - Fix You Part 2/10
Part 3 and 4 are out on my Patreon for Free!
Summary - Reader is hired as Ruben's assistant nurse after receiving head trauma during a football game. He has fallen into a deep depression on his road to recovery and does not accept much help from Reader as she only reminds him of how incapable he is.
Enjoy!
Ruben's family were not joking when they said that if successful, you'd be hired immediately. You still had your flat in London with all of your belongings, however, that would be taken care of for you since Ruben's family were more than willing to set up a room for you in Ruben's apartment. There you received your own private quarters, with a joint bathroom and everything, not to mention your own walk-in closet.
"I kid you not, it's bigger than my old flat." You squealed into your phone.
"Well, what is he like, your employer?" Your friend Donna asked. She was currently in your apartment in London, collecting the immediate essentials that had to be shipped to you right away.
"Well, you know. He's kind of quiet." You said, having only known Ruben for two days. During these two days his physio, Max, had taken care of everything, only asking you to measure the proper proportion for Ruben's daily dose of Heparin, which was injected to prevent blood clots from forming.
"But he's hot, no?"
"Who, Max?"
"No, the guy you're working for, Ruben?"
"I don't know?" You muttered. Although he was tall and fairly built, there was something about not knowing the color of a man's eyes that didn't sit right with you. "It's the mirror to one's soul, you know."
"I'd rather wanna know the size of his...."
"Donna." You hissed. "Really?"
Her laughter buzzed in your ear. "What, it's the canal of life, you know."
"Ha, ha, very fun..."
"Y/N?"
A knock on the door interrupted you.
"Just a second!" You pressed the phone to your ear as you jumped down from your bed.
"It's Max."
"Yeah, just a second!"
You said goodbye to Donna and hurried up to close the suitcase that lay open on your floor. You shoved it under the bed along with other scattered items, before making your way over to the bedroom door. Max stood waiting for you in the doorway.
"Hey, I just wanted to say that I'm leaving now."
"Oh, okay, when will you be back?"
"On Monday?"
"What? But that's in three days."
"Exactly." He nodded. "I work four days and get three days off to see my girls."
"You have a family?" You said, quite disappointed by the fact. Max was really handsome for a forty-two year old.
"Anyway, If you need anything I think Ivan is stopping by tomorrow with some groceries, other than that I wrote down everything that needs to be done during the day, along with some light exercises that you can help Ruben do."
"Me, help Ruben?" You frowned. It took you two days to get comfortable living the easy life. You would've never pursued acting if you had known about being a rich man's nurse.
"Like I said," Max smiled. "If you need anything, call Ivan. He lives twenty minutes away from here."
"Alright, okay. " You nodded, accepting the situation. "Have a good weekend."
"You too."
And just like that a man's life was left in your hands. It was an odd feeling. Not scary, just odd. Nevertheless, you plotted yourself in the living room, just in case Ruben needed you he could call for help and you'd hear him. However, hours passed without a word from him. You weren't concerned at first, considering the fact that Ruben knew how to walk on his own. But after some thought, you decided to knock on his door and see if he needed anything.
"Ruben, It's me."
No answer.
"I thought that maybe I could make you a snack? Would you like that?"
Still no answer.
It hit you, what if he was bleeding out? With the trauma to his brain, perhaps he had developed some internal bleeding and now he was laying in bed, dying on your watch.
"Ruben, I'm sorry but I'm going to have to...." You burst into his room. The first thing that hit you was the breeze from the balcony with its door ajar.
"Oh, no."
Only seeing the traces of Ruben on his bed, you could only assume the worst.
"Please don't be dead, please don't be dead."
You rushed out onto the balcony, leaning over the railing, expecting to see a body laying flat on the ground. However, there was nothing, not a trace of human remains.
"You're worse than the others, you know that right?"
You gasped, hearing his low chuckle. Turning your head, you spotted Ruben, shirtless, laying on his back, arms tucked behind his neck as he bathed in the sun.
"You're....you're...."
"Not dead?" He said, raising a brow behind his bandaged eyes.
"I'm sorry, I thought...."
"That a guy with injuries like mine should consider killing himself?"
"Yes and no."
"Yes and no?" He frowned, "Care to elaborate?"
"Not should consider." You said. "But I believe some people would consider...doing it."
"Well, unfortunately I'm still alive."
"I can see that." You muttered.
Ruben sat up, and to your surprise removed the blindfold from his eyes by tugging it down to rest around his neck. He then reached for the bottle of sunscreen on a stool nearby, applying a drop of it on his nose.
"If you're planning on laying in the sun all day, you should probably apply sunscreen to your entire body."
He stopped the motion of putting on sunscreen, shifting his head your way. "I'm Portuguese, I'm pretty sure I can handle a dose of English sun."
"But can you handle a dose of skin cancer?"
He chuckled, eyelids flickering as he did. He seemed tempted to open them, his eyes. And for a moment that thought struck fear within you.
"Was there something you wanted?"
"Pardon?" You had been distracted. Your eyes falling onto the sight of his abs. They were visible even though he was sitting down. Something worth remembering for your next call with Donna.
"Was there something you wanted?" Ruben repeated, snatching you out of your daze. "I mean Max already gave me my shot and I don't need your help swallowing my pills."
"Right." You said. "I guess I just wanted to check on you."
"To see if I was still alive?" He grinned.
"Right." What an asshole, you thought. "Now that that's confirmed, I'll get started on dinner."
"Don't bother." He said, pulling the bandage to cover his eyes again.
"Why not?"
"Well, my mom left us food that should last us all year."
"Oh, okay."
"She's afraid that you can't cook, you know."
"Well I can."
"Yeah, but not as good as her."
"Right."
You left Ruben's room, embarrassed to have entered in the first place. Who does the guy think he is, speaking to you like some kind of servant? You wondered how long you'd be able to put up with it. Not for long you reckoned.
'
Part 3 and 4 are out on my Patreon for Free!
#fanfiction#football imagine#footballer x reader#ruben dias#footballer imagine#man city#football angst#manchester city#ruben dias x reader#ruben dias imagine
51 notes
·
View notes
Text

Erin is an amazing person to follow if you have long covid. The link to th article is below.
@doc4care on Twitter also has this to say about mitochondrial damage and drugs
And there are simple, effective ways to quiet TLR4 inflammation (metformin, berberine, curcuminoids, low dose naltrexone, low dose lithium). And for quieting the RAGE pathway low molec wght heparin (or if outside IS, sulodexide - essentially, oral heparin - not approved in U.S.)
38 notes
·
View notes
Text
What it took to keep me alive: February edition
Video described:
Dave, a white non-binary person with glasses, short dark brown hair, a black tank top, a wedding band and several bracelets listing out all of the things that kept them alive for the month of February, including:
160 cartons of formula
6 times my port was accessed
11 bags of IV saline
11 syringes of heparin
6 bags of lactated ringers
1 tube change with IV sedation
300 Sodium/potassium capsules
1 bottle of electrolyte chews
275 pills
116 gummy vitamins
3 nasal sprays
10 doses of albuterol
8g of plant medicine
1 container of Miralax
1 3-day hospitalization
2 bags of IV antifungals
4 therapy appointments
2 doctors appointments
1 medical haircut
The videos ends asking the audience “what did it take to keep you alive for the month of February?”
34 notes
·
View notes
Text
Recurrent Pregnancy Loss: Finding Answers and Hope with Ekam Fertility
Miscarriage is a painful experience, but when it happens more than once, the emotional weight becomes even harder to carry. Recurrent pregnancy loss (RPL)—defined as two or more consecutive pregnancy losses—affects around 1% of couples trying to conceive. While it's deeply distressing, the good news is that many causes of recurrent pregnancy loss are identifiable and treatable.
At Ekam Fertility, we understand that every loss is more than just a number. That’s why we take a holistic, evidence-based approach to investigate, support, and offer solutions—so you can move forward with clarity and renewed hope.
What is Recurrent Pregnancy Loss?
Recurrent pregnancy loss refers to the repeated loss of pregnancy, usually before the 20th week of gestation. It’s important to know that RPL is not just bad luck—it often has an underlying cause. Identifying that cause is essential in improving future pregnancy outcomes.
Couples who have experienced recurrent pregnancy loss often feel alone, but they are not. With proper diagnosis and tailored treatment, many go on to have healthy, successful pregnancies.
RPL Testing: The First Step to Clarity
At Ekam Fertility, our first priority is to uncover the root cause through comprehensive RPL testing. Our advanced diagnostic panel includes:
Genetic Testing: To identify chromosomal abnormalities in either partner.
Hormonal Evaluation: Thyroid, prolactin, and other hormone levels can affect pregnancy.
Uterine Evaluation: Imaging tests like HSG, sonohysterography, or hysteroscopy help detect anatomical issues.
Blood Clotting Disorders (Thrombophilia Workup): Certain conditions can increase miscarriage risk.
Immunological Testing: To explore autoimmune causes of recurrent pregnancy loss.
Our detailed RPL testing panel provides the foundation for a customized treatment plan that addresses your unique challenges.
Immunology Treatment for Recurrent Pregnancy Loss
Sometimes the immune system may see the developing embryo as a threat, triggering a response that leads to miscarriage. In such cases, immunology treatment can be life-changing.
Ekam Fertility offers advanced immunology treatment options including:
Intravenous Immunoglobulin (IVIG)
Steroid Therapy
Low Dose Aspirin or Heparin for clotting issues
Intralipid Infusions to modulate immune responses
Lymphocyte Immunization Therapy (LIT)
Each immunology treatment is tailored based on your RPL testing results and medical history. We closely monitor your immune profile to increase the chances of a full-term pregnancy.
Why Choose Ekam Fertility for Recurrent Pregnancy Loss Care?
We know that recurrent pregnancy loss isn’t just a medical issue—it’s an emotional journey that deserves empathy, sensitivity, and ongoing support. At Ekam Fertility, we go beyond just offering RPL testing and immunology treatment. We walk hand-in-hand with you through every step, providing emotional counseling, personalized care, and unwavering hope.
Our fertility experts are pioneers in RPL care, and our protocols are aligned with global best practices. Whether the solution lies in surgical correction, lifestyle changes, hormonal support, or advanced immunology treatment, we’ll find it—together.
Let’s turn heartbreak into hope. At Ekam Fertility, we believe every woman deserves a chance at motherhood.
📞 Schedule a consultation today and start your journey with India’s trusted fertility experts.
0 notes
Text
Medications That May Be Causing Your Hair Loss (And What to Do About It)
If you've been noticing more hair in your brush or shower drain lately, you might be wondering if something you're taking could be behind it. While stress, hormones, and health issues often take the blame, many medications can also trigger hair shedding or thinning — sometimes as a hidden side effect.
In this post, we’ll break down the most common types of medications linked to hair loss, explain why it happens, and give you steps to take if you think your prescriptions might be impacting your hair.
Why Medications Cause Hair Loss
Certain medications can interrupt the natural hair growth cycle, pushing hair prematurely into the "shedding" phase (telogen effluvium), or damaging the hair follicle directly (anagen effluvium). This type of hair loss is usually temporary, but it can still feel emotionally challenging — especially when it happens without warning.
Disclaimer: I’m not a physician. This post is for educational purposes only. Do not stop taking any medications without talking to your doctor first — especially if they are managing serious or life-saving conditions. This blog is here to support conversations with your healthcare provider, not replace them. Hair matters, but your health comes first.
Medications Commonly Linked to Hair Loss (By Category)
1. Acne & Dermatology Medications
Isotretinoin (Accutane)
Acitretin
Etretinate
2. Antibiotics & Antifungals
Penicillin derivatives
Cephalosporins
Fluconazole
Itraconazole
Griseofulvin
3. Antidepressants & Mood Stabilizers
Fluoxetine (Prozac)
Sertraline (Zoloft)
Paroxetine (Paxil)
Bupropion (Wellbutrin)
Amitriptyline, Nortriptyline, Imipramine, Clomipramine
Lithium
4. Anticoagulants (Blood Thinners)
Warfarin (Coumadin)
Heparin
Apixaban (Eliquis)
Rivaroxaban (Xarelto)
Dabigatran (Pradaxa)
5. Anticonvulsants
Valproic acid (Depakote)
Carbamazepine (Tegretol)
Phenytoin (Dilantin)
Lamotrigine (Lamictal)
Levetiracetam (Keppra)
6. Antihypertensives (Blood Pressure Medications)
Beta-blockers: Propranolol, Atenolol, Metoprolol
ACE inhibitors: Enalapril, Lisinopril
Diuretics: Furosemide, Hydrochlorothiazide
7. Cholesterol-Lowering Agents
Statins: Atorvastatin, Simvastatin
Fibrates: Gemfibrozil, Fenofibrate
8. Chemotherapy Agents
Cyclophosphamide
Doxorubicin
Methotrexate
Paclitaxel, Docetaxel
Vincristine, Etoposide
9. Hormonal Therapies
Oral contraceptives
Hormone replacement therapy
Tamoxifen
Testosterone therapy
10. Immunosuppressants
Methotrexate
Azathioprine
Cyclosporine
Tacrolimus
11. Parkinson's Disease Medications
Levodopa
Carbidopa
12. Thyroid Medications
Levothyroxine
Methimazole
Propylthiouracil
13. Weight Loss Medications
Orlistat (Alli, Xenical)
Phentermine
Semaglutide (Ozempic, Wegovy)
14. Miscellaneous
Interferons (used for hepatitis)
Allopurinol (for gout)
NSAIDs: Ibuprofen, Naproxen
Amphetamines (for ADHD)
What to Do If You Suspect Medication-Related Hair Loss
Don't stop your medication abruptly. Always consult your doctor first.
Track your symptoms. Note when the hair loss started and any new medications or dosage changes.
Ask about alternatives. Your provider may be able to adjust your dose or switch you to a similar medication with fewer side effects.
Support your hair and scalp health. Treat the symptoms while you work on the root cause — consider scalp treatments, gentle haircare, and nourishing your body with key nutrients.
Book a hair recovery consultation. Professionals trained in hair loss support (like trichologists or hair health specialists) can help guide your recovery plan.
Hair loss is more common — and more reversible — than most people realize. If you're unsure what's causing your shedding, getting curious and gathering the right info is the first step.
Need support or want a customized recovery plan? Book a hair health consultation with me today →
0 notes
Text

Jiulong: Your Premier Heparin Company for Exceptional Solutions
In the intricate landscape of the pharmaceutical industry, the role of heparin cannot be overstated. When it comes to a reliable heparin company, Jiulong has firmly established itself as a leading force, offering a comprehensive suite of products and services that meet the highest standards of quality and innovation.
Heparin, a vital anticoagulant, is widely used in various medical settings, from preventing blood clots during surgeries to treating patients with thrombotic disorders. Jiulong understands the critical nature of heparin in healthcare and has dedicated significant resources to ensure the production of top-notch heparin products.
One of the hallmarks of Jiulong as a heparin company is its unwavering commitment to quality control. Our manufacturing facilities are equipped with state-of-the-art technology and adhere to strict international pharmaceutical standards. Every step of the heparin production process, from the sourcing of raw materials to the final packaging, is meticulously monitored. We work closely with trusted suppliers to obtain the finest raw materials, ensuring that the heparin we produce is of the highest purity and potency. This attention to detail results in heparin products that healthcare providers can rely on with confidence.
Jiulong also prides itself on its diverse range of heparin offerings. Whether you are in need of unfractionated heparin for traditional anticoagulation therapies or low molecular weight heparin for more targeted treatment, we have you covered. Our team of experienced scientists and researchers is constantly exploring new formulations and delivery methods to enhance the efficacy and safety of our heparin products. For instance, we are at the forefront of developing innovative heparin-based drugs that can provide more convenient dosing regimens for patients, improving their quality of life and treatment compliance.
In addition to product excellence, Jiulong stands out for its customer-centric approach. We understand that each customer has unique requirements, and our dedicated customer support team is always ready to assist. Whether you are a hospital, a research institution, or a pharmaceutical distributor, our team will work closely with you to understand your needs and provide tailored solutions. We offer prompt responses to inquiries, efficient order processing, and reliable delivery services, ensuring that you receive your heparin products in a timely manner.
If you are searching for a heparin company that combines quality, innovation, and exceptional service, look no further than Jiulong. Our track record of excellence in the heparin industry speaks for itself. Contact us today to discover how we can meet your heparin needs and partner with you for a healthier future. Let Jiulong be your go-to heparin company for all your pharmaceutical requirements.
0 notes
Text
The Wind Beyond The Building
The content written is solely fiction. Medical scenarios are for storytelling and character development, not professional advice; inaccuracies may occur. Some topics may explore critical conditions—trigger warnings will be provided if needed. Reader discretion is advised.
Trigger Warning: Medical Trauma, Cardiac Emergency, Possible Violence, and Attempted Homicide Previously:
Shiv, arriving at the scene after just a brief sleep, watched as the trauma team worked swiftly around the patient. His injuries didn’t match a long fall—bruises across his chest, swollen eyelids, and an open wound on his femur.
“ECG is showing nonspecific ST-T changes,” Soleil, her most trusted resident, reported. “Troponins are slightly elevated.”
She frowned at the strangeness. “His heart’s under stress, but not from blunt trauma. Something else happened before he hit the ground.”
A nurse called out, “BP’s dropping—98 over 60. Tachycardic at 122.” She speculated that if his injuries weren’t consistent with trauma, then something else had led to his collapse. “Dr. Soleil, we need an aortogram and pulmonary angiography—stat.”
“Pulmonary embolism?” Soleil asked, already signaling for the scan.
“It fits,” Shiv stated. “A sudden PE could have caused syncope. If he collapsed near a window, he might not have fallen—he might have been pushed after losing consciousness.”
They rushed him to imaging, the machines whirring as contrast dye illuminated the hidden battle inside his body. There it was. A pulmonary embolism. A massive clot blocking circulation in his lungs.
Soleil swore under her breath. “That explains the collapse.”
Calmly interpreting the result, Shiv added. “It also means he never jumped. He lost consciousness before he ever hit the ground.”
Back in the trauma bay, the patient’s vitals were deteriorating. His heart was struggling, starved of oxygen, his breathing rapid but shallow. He was in danger of cardiac arrest. Fast, Shiv instructed her team. “We need immediate anticoagulation. Get a heparin drip started—low dose. We have to break down the clot before it causes a full-blown infarction.”
Soleil grabbed the medication, carefully calculating the dosage. Heparin, an anticoagulant, would help dissolve the clot, but it came with a risk—his open leg wound. If they thinned his blood too much, he could bleed out.
“We’ll titrate the dose carefully,” Soleil said, adjusting the IV pump as the anticoagulant began flowing into his bloodstream.
“Good call. Keep an eye on his BP. If it drops further, we’ll need vasopressors to support perfusion.” The team moved swiftly following her instructions. Meanwhile, a nurse secured a compression bandage over his femoral wound, monitoring for any signs of excessive bleeding.
His oxygen levels were still a concern. “Dr. Shiv, he’s desaturating,” Soleil warned. “SpO2 dropping to 91% despite high-flow oxygen.”
Responding in seconds, she called a respiratory therapist. “Increase O2 flow. If he worsens, we prepare for intubation.” His body was struggling against the clot, but they needed to do more than just slow it down. “Get alteplase ready.” They begin again. “If he doesn’t improve in the next thirty minutes, we start thrombolysis.”
Soleil hesitated. “That could worsen his bleeding.”
“And if we don’t act, his heart won’t survive,” She countered.
The minutes stretched long, filled only by the rhythmic beeping of the monitors. Then—his heart rate began to stabilize. His oxygen levels steadied.
Soleil let out a breath. “He’s responding.”
Shiv allowed herself a small relief, but she stayed cautious. The man was still unconscious, but alive. His heart had fought through a deadly clot, through trauma, and through something else—something that had happened before he ever left that building.
0 notes
Text
What Are the Best Treatments for Low INR Mean Thick Blood?
Low INR, which often signifies thick blood, is a condition that requires careful management to prevent serious health complications such as blood clots, strokes, or heart issues. If you’re searching for the best treatments for low INR mean thick blood, this blog will guide you through proven medical options, lifestyle changes, and preventive measures to keep your blood health in check.
Understanding Low INR and Its Link to Thick Blood
INR (International Normalized Ratio) is a measure used to evaluate the time it takes for blood to clot. A low INR value indicates faster clotting, which may result in thicker blood. Thick blood can increase the risk of thrombosis or blockages in blood vessels, leading to potential cardiovascular complications.
If you’ve been diagnosed with low INR mean thick blood, understanding your treatment options is the first step to managing this condition effectively.
Medical Treatments for Low INR and Thick Blood
Anticoagulant TherapyAnticoagulants, also known as blood thinners, are the most common treatment for low INR mean thick blood. Medications like warfarin, heparin, or newer alternatives such as apixaban or rivaroxaban, help slow down clot formation. These drugs are often prescribed based on your INR levels and overall health condition.
Aspirin TherapyLow-dose aspirin may be recommended to prevent blood clots, especially for individuals at high risk of heart attacks or strokes. It’s a milder option than anticoagulants but can still be effective for some cases of low INR mean thick blood.
Plasma Exchange (Plasmapheresis)In severe cases, plasma exchange is used to reduce the thickness of the blood. This procedure removes the excess proteins or cells causing blood to thicken, thereby improving blood flow and lowering risks.
Targeted Therapies for Underlying ConditionsIf the low INR mean thick blood is caused by a medical condition like polycythemia vera or a clotting disorder, specific treatments such as chemotherapy, targeted medications, or phlebotomy (removal of blood) may be required.
Lifestyle Changes to Improve Low INR and Thick Blood
While medical treatments are crucial, adopting certain lifestyle changes can enhance their effectiveness and help regulate your INR levels.
Maintain a Balanced Diet
Increase your intake of foods rich in omega-3 fatty acids, such as salmon, walnuts, and flaxseeds. These can help thin the blood naturally.
Limit foods high in vitamin K (like spinach, kale, and broccoli), which may interfere with anticoagulant medications.
Stay HydratedProper hydration plays a critical role in reducing blood viscosity. Drinking enough water throughout the day can prevent dehydration, which is a common cause of thick blood.
Exercise RegularlyPhysical activity improves circulation and reduces clotting risks. Even moderate activities such as walking, yoga, or swimming can make a significant difference.
Quit Smoking and Limit AlcoholSmoking thickens the blood and increases clotting risks, while excessive alcohol can interfere with INR levels. Cutting these habits can have a positive impact on your condition.
Monitoring Your INR Levels
For those managing low INR mean thick blood, consistent INR monitoring is essential. Regular testing ensures that your treatment plan is working effectively and helps your healthcare provider adjust medications or recommendations as needed.
At-home INR testing devices are now widely available, offering convenience and accuracy. They empower patients to take control of their health by providing real-time results without frequent hospital visits.
Natural Remedies and Supplements
In addition to medical treatments and lifestyle changes, certain natural remedies and supplements may support blood health:
Garlic and GingerBoth are known for their natural blood-thinning properties. Including them in your diet can help improve circulation.
TurmericThe active compound curcumin in turmeric has anti-inflammatory properties and may help reduce blood thickness.
Fish Oil SupplementsRich in omega-3 fatty acids, fish oil is a natural choice for improving blood flow and reducing clotting risks.
Always consult your doctor before starting any supplements to ensure they won’t interfere with prescribed medications.
Managing low INR mean thick blood requires a combination of medical treatment, lifestyle adjustments, and ongoing monitoring. From anticoagulant therapy to dietary changes, there are several effective ways to address this condition and lower the risks associated with it.
For individuals looking for convenient and accurate INR monitoring solutions, PatientSelfTesting offers reliable at-home INR testing devices. With our tools, you can stay on top of your health and manage low INR mean thick blood more effectively. Take charge of your blood health today!
0 notes
Text
Acute Coronary Syndrome (ACS) Protocol in Emergency Care: A Complete Guide
Introduction Acute coronary syndrome (ACS) refers to a group of severe heart conditions, including unstable angina, non-ST-segment elevation myocardial infarction (NSTEMI), and ST-segment elevation myocardial infarction (STEMI). These conditions require immediate medical attention to improve outcomes and prevent life-threatening complications such as heart failure or sudden cardiac death. Early identification and prompt intervention are essential in preventing further damage to the heart muscle.
1. Initial Assessment The first step in managing ACS is an early diagnosis. This involves performing an ECG and ordering laboratory tests such as Troponins and CKMB. Symptoms commonly include chest pain (often described as pressure or tightness), shortness of breath, excessive sweating, nausea, and pain radiating to the arm, jaw, or shoulder. In some cases, patients may experience only mild chest discomfort, often coupled with a sense of impending doom.
2. Immediate Interventions When ACS is suspected, initiate the following interventions immediately:
Oxygen Therapy: Administer oxygen if the patient’s saturation levels drop below 90%.
Aspirin: A dose of 300 mg to help inhibit platelet aggregation.
Clopidogrel: 300 mg to provide further antiplatelet support.
Anticoagulation: Administer Enoxaparin (1mg/kg SC) or Heparin (1cc IV) to reduce the risk of clot formation.
Nitroglycerin: Sublingual nitroglycerin (0.3-0.6 mg) can help relieve chest pain unless contraindicated by low blood pressure.
Pain Control: Morphine can be used to alleviate persistent chest pain, but it should be administered cautiously.
3. Confirmatory Diagnostics To confirm the diagnosis, conduct timely investigations:
ECG: Perform an ECG within 10 minutes to differentiate between STEMI, NSTEMI, or unstable angina.
STEMI: ST-segment elevation indicates complete coronary artery blockage, necessitating immediate reperfusion therapy.
NSTEMI/Unstable Angina: No ST-segment elevation, though T-wave changes or ST depression may be observed.
Cardiac Biomarkers: Elevated troponin levels are a hallmark of myocardial injury in cases of NSTEMI or STEMI.
4. STEMI Management In the case of STEMI:
Reperfusion Therapy: Time is of the essence. PCI should be performed within 90 minutes, or fibrinolysis within 30 minutes if PCI is unavailable.
Antiplatelet Therapy: Administer dual antiplatelet therapy (aspirin and clopidogrel).
Anticoagulation: Heparin or low-molecular-weight heparin should be initiated.
5. Management of NSTEMI/Unstable Angina For patients with NSTEMI or unstable angina, a personalized approach is critical:
Risk Stratification: Use scoring systems like the GRACE or TIMI scores to guide decision-making for invasive or conservative management.
Medical Therapy: Administer dual antiplatelet therapy, beta-blockers, and anticoagulants. Statins should be considered to stabilize lipid levels.
Angiography: For high-risk patients, coronary angiography is recommended within 24–72 hours.
6. Supportive Care Supportive measures throughout the ACS management process are essential:
Continuous Monitoring: Continuous cardiac monitoring is crucial to detect arrhythmias or other complications.
Communication: Regular updates to patients and their families are important to ensure clarity and support.
Psychological Support: Address anxiety and stress, which can worsen the condition.
7. Post-ACS Care Once the patient is stabilized, ongoing care is vital to prevent further events:
Medication Adherence: Emphasize the importance of medications like antiplatelets, statins, ACE inhibitors, and beta-blockers.
Lifestyle Changes: Encourage smoking cessation, a heart-healthy diet, and regular exercise.
Follow-Up Care: Ensure regular follow-up with a cardiologist to monitor progress and adjust treatment.
Conclusion Effective management of ACS in an emergency setting requires swift diagnosis, timely treatment, and a coordinated team effort. By adhering to clinical guidelines and providing comprehensive care, healthcare professionals can significantly reduce mortality and improve outcomes for patients facing this critical condition. -BazingaMatte source: https://providerscentralhub.com/
1 note
·
View note
Text
Heparin Injection- Uses, Side Effects, Precautions and More

Heparin Injection is a natural anticoagulant sterile solution that contains Heparin. This injection is generally used to prevent blood clots. Read this blog to the end and you will get full information about Heparin Injection uses, side effects and many more important details.
1. Uses of Heparin Injection
Heparin Injection is widely used in the healthcare sector to treat various health issues. Here are all the benefits of Heparin Injection.
Prevent and cure various thromboembolic disorders, such as deep vein thrombosis, pulmonary embolism, and arterial thrombosis.
Prevent blood clots of patients who recently had serious surgery, or other critical medical issue.
2. Know the Side Effects of Heparin Injection
Like other medication, Heparin Injection also has some common side effects. We have listed below all the side effects of Heparin Injection. Inform your doctor as soon as possible if you are facing any of these side effects or negative effects.
Abdominal or stomach pain
back pain or backaches
bleeding from the gums
blood in the urine
Blood in coughing
headaches
Pain or itching at Injection sight
3. Precautions for Heparin Injection
Now check some precautions for Heparin Injection so that you don't get any side effects of it.
Patients with bleeding disorders should consult a doctor before taking Heparin Injection.
Avoid prolonged use of Heparin Injection as long time use may lead to heavy bleeding.
Elderly patients should consult physicians before taking it.
Pregnant women also be cautious of using this injection and take doctor’s advice before taking.
4. How to Supply and Store Heparin Injection?
Heparin Injection should be supplied in vials and in sterile solution. It comes in 5000 iu/5 ml, 25000 iu/5 ml doses.
You can keep it in a dry place at a temperature between 15 to 25 degree centigrade.
Contact Leading Heparin Injection Supplier in India to Collect Heparin Injection at Affordable Price
Are you looking for a trusted Heparin injection manufacturer and supplier in India who can provide you bulk supply of genuine heparin Injection at affordable price? Then get in touch with Montage Laboratories PVT. LTD. now. We supply wholesale price Heparin injection and many more medications to pharma stores, pharma franchise and individual patients as well. No matter wherever you are, now you can easily get heparin injection and any other pharma products at your doorstep from this top Heparin injection exporter in India.
0 notes
Text
Top Heparin Injection Manufacturer and Supplier in India.
Sanjar Pharma LLP is recognized as one of the leading manufacturers and suppliers of Heparin injection in India, specializing in essential anticoagulant therapy. We pride ourselves on delivering high-quality Heparin injections nationwide, with extensive experience in both manufacturing and exporting.
Understanding Heparin Injection The Life-Saving Anticoagulant
Heparin injection, often referred to as a blood thinner, plays a vital role in the prevention and treatment of blood clots. This effective formulation, which includes heparin sodium, sodium chloride, benzyl alcohol, and purified water, helps minimize the risk of clot formation in veins, arteries, and lungs. It is frequently prescribed following major surgeries or for patients at high risk of clotting disorders, making it a reliable option for healthcare providers.
Sanjar Pharma LLP, is committed to manufacturing high-quality Heparin Injections to provide healthcare providers economical and effective anticoagulant therapy.
Why Choose Sanjar Pharma LLP’s Heparin Injection?
As a leading manufacturer and supplier of Heparin injection in India, we are committed to ensuring that our product adheres to strict quality standards, providing reliability for all users. Sanjar Pharma’s Heparin injection comes in 5000 IU/5 ml and 25000 IU/5 ml doses, giving healthcare providers the flexibility to select the right dosage for their patients' needs. Each vial is crafted with precision to support effective anticoagulant therapy, making it the preferred choice for numerous clinics, hospitals, and pharmacies throughout India.
Benefits and Applications of Heparin Injection
Prevents Deep Vein Thrombosis (DVT): Crucial for preventing blood clots in veins, particularly after surgery or in patients who are immobilized.
Pulmonary Embolism (PE) Prevention: Heparin helps lower the risk of dangerous blood clots that can travel to the lungs.
Maintains Catheter Patency: In critical care environments, Heparin ensures that IV lines and catheters remain free from clots, promoting patient safety.
Supports Hemodialysis and Cardiopulmonary Procedures: Heparin plays a vital role in specialized treatments, effectively managing anticoagulation.
Get Heparin Injection Directly from Us
For healthcare providers, pharmacies, and distributors, ordering Heparin injections in bulk from Sanjar Pharma LLP is a smart decision that can transform your operations. Starting at just Rs. 10,000, our bulk order option allows you to keep a well-stocked inventory, ensuring you are always ready to meet patient demand quickly and efficiently. Imagine the reassurance of having a dependable supply of Heparin injections on hand. With our competitive wholesale prices, you can lower your expenses while guaranteeing that your patients receive top-quality care. This translates to more resources for your practice or pharmacy, enabling you to concentrate on what truly matters: delivering outstanding service and care to your patients.
But there’s more! By partnering with Sanjar Pharma, you also benefit from:
Faster Delivery: We recognize that time is critical in healthcare. Our streamlined supply chain guarantees prompt delivery, even during emergencies.
Quality Assurance: Our Heparin injections are produced under strict quality control standards, so you can be confident you’re providing the best for your patients.
Customized Solutions: Do you require specific dosages or packaging? We are adaptable and can customize our offerings to suit your specific needs.
Get Your Heparin Injection Directly from Sanjar Pharma LLP
Sanjar Pharma LLP is your reliable partner, committed to delivering safe, effective, and high-quality Heparin injections designed to meet your healthcare requirements.
Our dedication to excellence ensures that we provide our products in bulk, ready for immediate dispatch, allowing you to keep your practice or pharmacy well-stocked and prepared for any situation. With our competitive pricing and outstanding service, you’ll see why we’re the preferred choice for Heparin injection suppliers throughout India.
Why wait? Get in touch with us today to place your bulk orders, starting at an amazing Rs. 10,000!
Join the many satisfied healthcare providers who rely on Sanjar Pharma for their medical supply needs. Enjoy seamless deliveries, unparalleled quality, and the reassurance that comes from partnering with a leader in the pharmaceutical industry.
Don’t let this opportunity pass you by—secure your supply of Heparin injection now and enhance your healthcare services! Contact us today, and let’s collaborate to ensure the best outcomes for your patients.
Who we are:
Sanjar pharma is a leading company incorporated in the year 2014, headquartered in Himatnagar (Gujarat). We are rapidly growing pharmaceutical company expertise in injection manufacturing including Dry powder injections, Liquid Vial, Ampoule Injection, PFS injection, and suspension injection as well ear and eye drops. Our products reach patients and healthcare providers in various regions, showcasing our dedication to global health.
#pharmaceutical products#heparin injection#heparin sodium#blood thinner injection#anticoagulent#injection manufacturer#injection manufacturing company
0 notes
Text

How Does Pregnancy Impact the Safety of Taking Xarelto?
Xarelto (rivaroxaban) is an anticoagulant or blood thinner widely prescribed to prevent and treat blood clots. Although it can be life-saving, Xarelto carries specific considerations when prescribed to pregnant individuals. Pregnancy impacts many physiological processes in the body, including blood clotting, which makes taking medications like Xarelto during pregnancy more complex. Here, we’ll explore how pregnancy affects the safety of taking Xarelto, the potential risks and benefits, and alternatives for expecting mothers.
Blood Clotting and Pregnancy
During pregnancy, the body undergoes a natural increase in clotting factors to prevent excessive bleeding during childbirth. However, this increase also raises the risk of developing blood clots, a condition known as pregnancy-associated venous thromboembolism (VTE). Blood clots can lead to serious complications, including deep vein thrombosis (DVT) or even pulmonary embolism (PE), which can be fatal if untreated. Pregnant individuals with a history of blood clots, certain heart conditions, or genetic clotting disorders may be at an even higher risk.
Xarelto and Pregnancy: Understanding the Risks
Xarelto works by inhibiting Factor Xa, a key protein in the clotting process, to reduce the likelihood of clots forming. However, studies on the safety of Xarelto use during pregnancy are limited, and it is generally advised against because of potential risks to both the mother and fetus.
Fetal Risks: Xarelto crosses the placenta, potentially exposing the fetus to its anticoagulant effects. There is limited human data on Xarelto’s effects on fetal development, but animal studies have shown increased risks of bleeding in offspring. The potential for teratogenic effects, or harmful impacts on fetal growth, means that Xarelto is generally avoided unless absolutely necessary.
Maternal Risks: The risk of bleeding is elevated for anyone on Xarelto, and pregnancy can further increase this risk. If a woman on Xarelto experiences complications during pregnancy, such as placenta previa (where the placenta blocks the cervix), the chances of severe bleeding could be even higher. Given that pregnancy involves regular bodily changes and often invasive procedures during delivery, the bleeding risks associated with Xarelto use can be significant.
Lack of Antidote: Although a reversal agent for Xarelto exists, it is not widely available or commonly used in obstetric emergencies. This limits the ability to quickly control bleeding if complications arise, adding to the risks involved with using Xarelto during pregnancy.
Alternatives to Xarelto for Pregnant Individuals
For women at high risk of blood clots during pregnancy, alternative anticoagulant options are generally preferred:
Low Molecular Weight Heparin (LMWH): This injectable anticoagulant is commonly prescribed because it does not cross the placenta, making it safer for the fetus. LMWH has been studied extensively in pregnant populations, showing reduced risk of blood clots without the increased risk of bleeding to the fetus.
Unfractionated Heparin (UFH): Another alternative, UFH has a shorter half-life, allowing for more flexible dosing. Like LMWH, it does not cross the placenta, but it is often considered less convenient due to its more frequent dosing schedule and need for monitoring.
Both LMWH and UFH are considered safer and more manageable in a pregnancy setting than Xarelto, particularly in cases where blood clot prevention is essential.
When Xarelto Might Be Considered During Pregnancy
In rare, high-risk cases where no alternative is available or effective, a healthcare provider might consider the continued use of Xarelto. However, this would require careful assessment and close monitoring from a specialized medical team. Xarelto’s potential benefits must significantly outweigh the risks for it to be prescribed to a pregnant individual.
Planning Pregnancy While on Xarelto
For women taking Xarelto who are considering pregnancy, it’s essential to consult a healthcare provider well in advance. Doctors typically recommend switching to a safer anticoagulant before conception. Those already on Xarelto who become pregnant should inform their healthcare provider immediately to develop a safe plan for managing blood clot risk during pregnancy.
Key Takeaways
Xarelto use during pregnancy is generally discouraged due to its potential risks to both the mother and fetus, including increased bleeding risks and lack of adequate safety data.
Alternative anticoagulants, such as LMWH or UFH, are generally safer options for pregnant women at risk of blood clots, as they do not cross the placenta and have been studied extensively in pregnancy.
Careful planning and consultation with healthcare providers are essential for those at risk of blood clots during pregnancy, especially when managing anticoagulation therapy.
While Xarelto can be life-saving for many patients, pregnancy requires additional caution and alternatives to ensure the safety of both mother and child. Each case is unique, and only a healthcare provider can determine the best approach based on an individual's health history and risk factors.
#usascripthelpers#diabetes management#diabetes care#usascriphelpersofficial#diabetes treatment#diabetes symptoms#diabetes mellitus#diabetic#weight loss diet#insulin#xarelto
0 notes
Text
Coenzyme Q10 Detection Technology
In 1957, Prof. Grane of the Institute of Enzyme Research of the University of Wisconsin isolated a new quinone compound from the lipid extract of bovine heart mitochondria [1]. The compound is an orange-yellow crystal with a melting point of 48-49 ℃, capable of reversible oxygenation and reduction, and mainly involved in mitochondrial electron transfer. The compound is coded as Q-275 (Q is the initials of quinone, and 275 is the maximum absorption at 275 nm).
In 1958, American scholar Folkers and his team synthesized a series of coenzyme Q compounds, confirmed the structure of Q-275 and named it coenzyme Q10 [2]. In 1961, Mitchell, a British chemist, proposed the theory of "chemotaxis" in the study of energy conversion in living organisms and revealed the role of coenzyme Q10 in the energy conversion system of mitochondria [3], and was awarded the Nobel Prize in Chemistry in 1978. Since then, people have gradually recognized coenzyme Q10, and its applications have been widely and deeply studied.

Coenzyme Q10 (CoQ10), also known as ubiquinone, is chemically known as 2,3-dimethoxy-5-methyl 6-deca-isopentadienylbenzoquinone and consists of a benzoquinone ring and polyisoprene side chains. The number of isoprene units in the coenzyme Q series varies by species, with humans having 10 units. Coenzyme Q10 is available in both oxidized (ubiquinone, CoQ10, Ubiquinone) and reduced (ubiquinol, CoQ10H2, Ubiquinol) forms, and its chemical structure is shown in Figure 1.
Fig. 1 Chemical structures of oxidized (a) and reduced (b) forms of coenzyme Q10
Coenzyme Q10 is an important component of the mitochondrial respiratory chain, where it acts as an electron carrier and participates in electron transfer and ATP production. Furthermore, the cellular functions of coenzyme Q10 are multifaceted: it is present in all cell membranes, it limits the toxic effects of free radicals, it is a component of low-density lipoprotein (LDL), and it is involved in the aging process. Its deficiency is associated with a variety of diseases, such as mitochondrial disease, cardiovascular disease, age-related diseases, tumors, liver disease, kidney disease, etc. Panthenol is also a powerful antioxidant. Panthenol is also a powerful antioxidant, preventing lipid peroxidation in biological membranes [4].
With the deepening of the research on coenzyme Q10, the application of coenzyme Q10 is becoming more and more extensive. In addition to its use as a drug, it also has many applications in nutraceuticals, cosmetics and dietary supplements. Coenzyme Q10 is an endogenous substance, but its concentration in living organisms is very low. The analysis and determination of CoQ10 is important for the clinical diagnosis of diseases and the quality control of drugs and health products. In recent years, many analytical methods for the determination of coenzyme Q10 have been developed, which are summarized and discussed in this paper.
1 Coenzyme Q10 extraction and sample preparation
Coenzyme Q10 is insoluble in water and methanol at room temperature, slightly soluble in ethanol, soluble in acetone, 1-propanol, and soluble in organic solvents such as hexane and chloroform. Pharmaceuticals and dietary supplements such as tablets, capsules and softgels can be dissolved in ethanol, 1-propanol and other solvents, and analyzed by ultrasonication or filtration.
The isolation and enrichment of coenzyme Q10 from complex biological matrices is a laborious process.
Conventional liquid-liquid extraction is the most commonly used extraction method. This method is simple and has a large processing capacity, but has the disadvantage of high solvent consumption and some solvents can interfere with subsequent detection. Often the solvent is evaporated under N2 protection after extraction and redissolved in a mobile phase or other solvent. Whole blood samples were immediately dosed with the anticoagulants heparin or EDTA, and the plasma was centrifuged at low temperature and stored at -80°C. The plasma was then analyzed for the presence of coenzyme Q10 in the plasma. Coenzyme Q10 was extracted from plasma as follows [5]: Methanol was added to the plasma to precipitate the proteins, and the plasma was extracted with hexane. The mixture was rotated and shaken for 15 min, then centrifuged for 5 min, and the supernatant was extracted and the solvent was evaporated. The supernatant was dissolved in acetonitrile before analysis.
Coenzyme Q10 was extracted from animal heart tissue [6]. The extraction of coenzyme Q10 from animal heart tissue [6] was performed by precise weighing, transferring to homogenization tubes containing lysis medium A (containing garnet and zirconia beads), adding 1-propanol and the antioxidant 2,6-di-tert-butyl-4-methylphenol (BHT), shaking, centrifugation, and collection of the supernatant, which was analyzed immediately. The extraction of coenzyme Q10 from muscle tissue is most often done directly using muscle homogenate, or sometimes mitochondria are extracted from the tissue under ice-cold conditions, and then the mitochondrial suspension is diluted with 1-propanol, centrifuged, and the organic layer is extracted with ethanol and hexane [7]. The one-step extraction method is to use a suitable organic solvent to extract coenzyme Q10 while precipitating proteins. Yang et al. [8] studied the one-step precipitation of plasma proteins with different organic solvents (methanol, ethanol, acetonitrile, and acetone), and found that acetone was the best precipitant, and the extraction yield ranged from 71.00% to 93.07%, and was simpler than the operation of liquid-liquid extraction.
The solid phase extraction (SPE) technique can also be used for the extraction of coenzyme Q10. On-line SPE techniques are less time-consuming, less expensive, and reduce sample loss and contamination problems. The technique is usually automated using a programmable on/off valve [9]. However, protein precipitation is required prior to extraction.
Molecularly imprinted polymers (MIPs) are specialized molecular recognition techniques that have been developed in recent years. Molecularly imprinted polymers (MIPs) are formed by mixing template molecules with functional monomers, cross-linkers and initiators. After polymerization, the template molecules are removed and binding sites and cavities complementary to the templates in size, shape and function are formed [10], allowing selective recognition and adsorption of molecules structurally similar to the templates.
Contin et al. [10] synthesized MIP using coenzyme Q0 as the template, methacrylic acid as the functional monomer, acetonitrile as the pore-forming agent, ethylene glycol dimethylacrylate as the cross-linking agent, and benzoyl peroxide as the initiator. MIP was used as an adsorbent for solid-phase extraction of coenzyme Q10 from liver samples using dispersive solid-phase extraction. In addition, MIP synthesized in the same way could be used as the filling adsorbent for solid-phase extraction of coenzyme Q10 in urine. In addition, the MIP synthesized by the same method can also be used as the filling adsorbent of polypropylene columns for solid-phase extraction of coenzyme Q10 in urine, and the columns can be reused four times [11]. Compared with the traditional solid-phase extraction, MIP as a polymer adsorbent for solid-phase extraction has the advantages of simple synthesis, low cost, good stability, porous, and high selectivity for target molecules [11].
Sometimes it is necessary to maintain the original oxygenated and reduced state of coenzyme Q10 in the samples during the extraction process, which causes great difficulties due to the oxidizability of CoQ10H2. In this case, the temperature can be controlled at a low temperature of 4 ℃ during the extraction process [6,12], shortening the extraction time and using anhydrous extract will increase the stability of CoQ10H2 [13], and the use of HCl-acidified ethanol as a diluent can also prolong the stability of CoQ10H2 and prevent the auto-oxidation of CoQ10H2 [12]. BHT is an antioxidant often added in the extraction of plasma and tissue samples, which can prevent the oxidation of CoQ10H2 [6,12,14]. However, the addition of BHT to CoQ10H2 extracts from dietary supplements and pharmaceuticals was found to increase the oxidation of CoQ10H2 [13,15]. The difference in matrix composition between plasma samples and dietary supplements may be the main reason for the loss of antioxidant capacity of BHT [13].
Biological samples for coenzyme Q10 extraction include plasma, leukocytes or platelets, muscle, fibroblasts and urine [16]. Muscle biopsy is the best choice for studying coenzyme Q10 status in mitochondrial diseases, but it is very invasive; the correlation between the levels of coenzyme Q10 and tissues in plasma, blood cells and urine has been controversial, but the determination of coenzyme Q10 in these samples has an important role in therapeutic monitoring [16]. However, the determination of coenzyme Q10 in these samples is important for therapeutic monitoring [16].
The methods used to extract coenzyme Q10 from biological samples are summarized in Table 1.
Table 1 Extraction methods of Coenzyme Q10
Simple operation, large processing capacity, high solvent consumption, some solvents may interfere with the subsequent detection.
Plasma, animal heart, muscle homogenate, mitochondria
Online Solid Phase Extraction
Less time-consuming and costly, reducing sample loss and contamination.
plasma (medicine)
Molecular Blotting Techniques
Low cost, good stability, high selectivity for target molecules, and can be combined with solid phase extraction.
Animal liver, urine
2 The main assay for Coenzyme Q10
2.1 High Performance Liquid Chromatography (HPLC)
HPLC is currently the main analytical method for analyzing coenzyme Q10 in various matrices. The main detectors coupled with HPLC are ultraviolet (UV), tandem mass spectrometry (MS/MS), electrochemistry (ECD), fluorescence (FL), chemiluminescence (CL), etc. The separation effect of HPLC is good, and each detector has its own characteristics.
2.1.1 HPLC-UV
HPLC-UV is the most commonly used method for the determination of coenzyme Q10, and has become the national standard for drugs and health foods [17, 18]. It has been widely used for the determination of coenzyme Q10 in pharmaceuticals [15, 19-22], health foods or dietary supplements [15, 20], plasma [14, 23] and tissues [10]. Conventional C18 or C8 reversed-phase chromatographic columns can separate either one form of coenzyme Q10 (usually oxidized) or both oxidized and reduced forms.
Liposomes are a new type of pharmaceutical dosage form formed by the self-assembly of lipids (mainly phospholipids and cholesterol) with a bilayer structure similar to that of a cell membrane, which can encapsulate hydrophilic or hydrophobic drugs. Ruiz-Garcia et al. [21] prepared a small monolayer of liposomes encapsulating coenzyme Q10, phosphatidylserine, and fat-soluble vitamin C (6-o-palmitoyl-L-ascorbic acid) by thin-film hydration. The prepared samples were freeze-dried, solubilized in chloroform and determined by HPLC-DAD at two analytical wavelengths.
Clementino et al. [22] prepared lecithin/chitosan nanoparticles encapsulating simvastatin and coenzyme Q10. The chitosan-modified liposomes showed higher stability and narrower particle size distribution. The content of simvastatin, simvastatin hydroxylate and coenzyme Q10 was quantified by reversed-phase HPLC-UV method to account for possible degradation products. The encapsulation rate was determined and the in vitro release of the drugs was studied. According to the study, the serious side effects of statins, such as rhabdomyolysis, were associated with the decrease of coenzyme Q10, so the co-encapsulation of these two drugs is of great significance.
Coenzyme Q10, as a fat-soluble vitamin coenzyme, is often measured in conjunction with other fat-soluble vitamins. Franke et al. [14] analyzed 25 substances including 25-OH-vitamin D3, 25-OH-vitamin D2, retinol, tocopherols, carotenoids (including their stirrup isomers), and oxidized and reduced coenzyme Q10 in plasma on a fusion-nucleated 2.6 μm particle size C18 column in tandem with a C30 column, which is good at separating carotenoid isomers, and in conjunction with a six-pass valve. D2, retinol, tocopherols, carotenoids (including their stirrup isomers), and oxidized and reduced coenzyme Q10 in plasma. The switching of the six-way valve allows coenzyme Q10 to flow from the C18 column to the detector while the carotenoid isomers are eluted on the C30 column, avoiding the difficulty of separating these two substances on the same column. In addition, if a pressure-resistant UV-Vis detector is added between the C18 and C30 columns, it is possible to separate all substances without switching the six-way valve, but special software is required to control the two detectors and to acquire and process the data. It has also been reported that retinol, six carotenoids, two tocopherols, and coenzyme Q10 (10 fat-soluble vitamins) can be measured in human plasma using a MYC30 column, and the total amount of the oxidized form of coenzyme Q10 was measured by oxidizing coenzyme Q10H2 first with FeCl3 [23].
The HPLC-UV method is highly accurate and reproducible, with LOD generally on the order of μg-mL-1 and sometimes on the order of ng-mL-1 with highly sensitive detectors [14].
2.1.2 HPLC-MS/MS: HPLC-MS/MS has been developed rapidly and applied more and more widely. This method utilizes the high separation efficiency of HPLC for complex samples combined with the high sensitivity and high selectivity of mass spectrometry, which can detect low content samples under the background of complex matrix, and is widely used in the analysis and determination of target compounds in biological samples.
The main types of tandem mass spectrometry are triple quadrupole mass spectrometry [5,7,11,25,26], quadruple linear ion trap mass spectrometry [13,24], and hybrid quadruple orbit trap mass spectrometry [12], etc. Most of them use electrospray ionization, multiple reaction monitoring (MRM), and positive ionization mode. Due to the low sensitivity of [M + H]+ analysis of coenzyme Q10, ammonium adducts, i.e., [M + NH4]+, are often used to improve the sensitivity of the mass spectrometric response. By adding a certain amount of ammonium acetate to the mobile phase, [NH4]+ forms a stable five-membered chelated ammonium cation with coenzyme Q10 [8]. The formation of Li adducts has also been reported to greatly increase the sensitivity [24].
The electrostatic field orbitrap mass spectrometry (Otbitrap) is a new type of high-resolution mass spectrometry, which has the advantages of high resolution, high mass accuracy, and wide dynamic range, etc. Pandey et al. [12] applied HPLC-hybrid quadruple orbitrap mass spectrometry (Q-Orbitrap) to rapidly determine the redox state of coenzyme Q9 and coenzyme Q10. Two scanning modes, full MS/AIF and tSIM/data-dependent secondary scanning (tSIM/ddMS/MS), were compared, and it was found that full MS/AIF had higher signal sensitivity and good peak shape. During sample preparation, coenzyme Q9 and coenzyme Q10 were extracted with BHT-containing hexane to limit the oxidation of the reduced form, and the Kinetex C18 column, with fused-core SiO2 packing and smaller particle size (2.6 μm), was found to have higher column efficiency, better resolution, and good peak shape. Oxidized and reduced forms of coenzyme Q9 and coenzyme Q10 were analyzed in brain, heart, liver, adipose tissue, and muscle of healthy mice with a small amount of sample (<5 mg) and a very short analysis time (4 min). the LOD ranged from 0.01 to 0.49 ng mL-1 .
Due to the complexity of the biological sample matrix and the low concentration of coenzyme Q10, sample pretreatment is very important. Becerra et al. [11] analyzed coenzyme Q10 in human urine by molecularly imprinted polymer solid-phase extraction (MIP-SPE) coupled with HPLC-MS/MS. The pretreatment process concentrates the coenzyme Q10 by at least 5-fold. The high degree of sample purification reduces the ion suppression caused by the matrix effect of mass spectrometry. The analytical system does not interfere with protein or white blood cell elevations, which is important in cases of coenzyme Q10 deficiency with renal impairment.
The HPLC-MS/MS method uses a lot of internal standards, and the selection of suitable internal standards is also an effective way to eliminate matrix effects. Commonly used internal standards include coenzyme Q9 [5, 11, 25], coenzyme Q4 [12], and the isotopes of coenzyme Q10, coenzyme Q10-2 H6 [7] and coenzyme Q10-2 H9 [26], which are structurally similar to coenzyme Q10. Structural analogs of coenzyme Q10, such as coenzyme Q4 and coenzyme Q9, have many advantages. They are also endogenous ubiquinones and are present in human plasma at very low concentrations, or at least at levels that do not interfere with their use in analytes at the concentrations required for analysis, and therefore do not interfere with the quantification of analytes. In addition, it separates well from coenzyme Q10 [5]. A potential source of error in mass spectrometry is ion suppression, especially in electrospray ionization mass spectrometry, where the response signal of the analyte is altered and often suppressed if an interfering substance interferes with the ionization of the analyte on the surface of the droplet, or if there is competition. The use of an isotope internal standard is a good solution to the problem of ion suppression. By co-eluting the isotope internal standard with the analyte, the effects of various effects can cancel each other out, and the matrix effect can be minimized and the sample recovery can be better [7].
2.1.3 HPLC-ECD
Electrochemical detectors (ECDs) are widely used because of their high sensitivity, good selectivity and low price. Coenzyme Q10 can undergo a reversible redox reaction and can be detected by an ECD.
The commonly used detection methods are coulometric or voltammetric analysis. Different voltages are set according to the redox potentials of the substances to be measured. For oxidized coenzyme Q10, it is usually reduced to its reduced form first, and then oxidized as the original reduced coenzyme Q10 in the sample. This method can measure both oxidized and reduced coenzyme Q10 simultaneously.
Yubero et al. [27] used HPLC-ECD to determine coenzyme Q10 in urine and gave reference values for the pediatric population. An ESA Coulochem II electrochemical detector was used, and the cell voltages were -600 mV and +600 mV. The amount of coenzyme Q10 in urine fluctuated greatly at different times of the day, and the morning urine with the smallest fluctuation was chosen as the sample. The results were expressed as the amount of coenzyme Q10 per gram of particulate protein. The reference standards for children are: 2-10 years old: 24-109 nmol; 11-17 years old: 43-139 nmol. This assay provides a noninvasive method for assessing renal coenzyme Q10 status in patients with renal disease, but it is not currently available and requires up to 30 mL of urine per sample.
Schou-Pedersen et al. [6] determined reduced and oxidized coenzyme Q10 in canine plasma and cardiac tissue by HPLC-ECD and compared it with HPLC-MS/MS. The ECD was performed by fluid dynamic voltammetry using an RS6011 ultra-analytical cell at a voltage setting of 500 mV. A guard cell at -600 mV was used prior to the analytical cell to reduce oxidized coenzyme Q10 eluting from the column. Mass spectrometry was performed using a Waters Micromass Quattro micro API triple quadrupole mass spectrometer with multiple reaction monitoring (MRM) and the internal standard CoQ10-2 H9. Both methods used the same column with slightly different mobile phase ratios and additives. The results showed that CoQ10H2 was approximately 30% lower in the HPLC-MS/MS method than in the HPLC-ECD method, which may be due to differences in the calibration stock solutions or to accelerated oxidation during storage or analysis in the LC-MS/MS system. Therefore, the two methods are not interchangeable. In terms of sensitivity, the sensitivity of the two methods was comparable for coenzyme Q10H2, whereas the sensitivity of the HPLC-ECD method was higher for coenzyme Q10.
2.1.4 HPLC-FL and HPLC-CL
HPLC with a fluorescence (FL) detector is widely used for the determination of various substances in biological samples due to its high selectivity and sensitivity. Coenzyme Q10 is not a fluorescent substance and needs to be derivatized before determination. Nohara et al. [28] measured CoQ10 and CoQ10H2 in blood by post-column derivatization using HPLC using 2-cyanoacetamide and CoQ10 and CoQ10H2 heated under alkaline conditions to produce fluorescent products. The fluorescence emission and excitation wavelengths were 442 nm and 549 nm, respectively.
HPLC coupled with a chemiluminescence (CL) detector has also been reported for the determination of coenzyme Q10.Kishikawa et al. [29] used dithiothreitol (DTT) as a reductant to reduce quinone to semiquinone radicals, and semiquinone radicals converted dissolved oxygen to superoxide anion, which reacted with luminal to form CL.Accordingly, coenzyme Q10 was determined in plasma by HPLC-CL, and other components in plasma were not interfered with. Coenzyme Q10 in plasma was determined by HPLC-CL, and other components of plasma were not interfered.
Both methods require a reaction coil between the column and the detector, and require two or three pumps to mix the various reaction reagents with the coenzyme Q10-containing eluent after the column and then into the reaction coil, which is a cumbersome operation. In recent years, the literature in this area is relatively scarce.
2.2 Spectrophotometric and fluorescent methods
The Enzyme Labeler, also known as Microplate Reader, is an instrument for reading and analyzing the results of Enzyme Linked Immunosorbent Assay (ELISA) experiments. The basic principle of ELISA is similar to that of spectrophotometer or photoelectric colorimeter, using plastic microplates instead of cuvettes, usually 48-well, 96-well, or larger, with low reagent consumption, high speed, and good repeatability. Multifunctional enzyme labeling instrument often has a variety of detection functions such as absorbance, fluorescence, chemiluminescence, etc., in the medical and health inspection has been widely used.
Fukuda et al. [30] developed a rapid microtiter plate method for the determination of coenzyme Q10 using the redox cycle of quinone. Coenzyme Q10 was reduced to ubiquinone radical by NaBH4, and then the ubiquinone radical was oxidized to ubiquinone and superoxide anion radical by dissolved oxygen. The superoxide anion radical converts 2-(4-iodophenyl)-3-(4-nitrophenyl)-5-phenyl-2H-tetrazolium chloride (INT) into a pink methanol dye. It has a strong absorbance at 510 nm, which increases with increasing concentrations of coenzyme Q10. The absorbance of Mazanine dye was measured quickly and easily by a microplate reader. As an application of this method, the content of coenzyme Q10 in cosmetics was successfully determined with an LOD of 14.8 nmol-L-1 . The proposed method can be used for the rapid high-throughput analysis of ubiquinone-containing products.
Fei et al. [31] developed a new method for the determination of coenzyme Q10 in serum and urine of Alzheimer's disease patients by fluorescence spectrophotometry, also using a microplate reader. The method is based on the fact that the chemical derivative between ethyl cyanoacetate (ECA) and coenzyme Q10 is fluorescent and can be detected by fluorescence spectrophotometer (FS-ECA) at λex/em = 450/515 nm. The results showed that serum and urine levels of coenzyme Q10 were significantly lower in Alzheimer's patients than in age-matched controls. This method has similar LOD and LOQ as the HPLC-UV method.
The FS-ECA method has some advantages over the HPLC-UV method, such as easier sample preparation, faster detection speed, and similar accuracy and specificity [31].
The important role of liposomes as a new drug dosage form for co-administration and targeted delivery was described in the literature [21,22], and liposomes can also be used as micro-containers to protect and concentrate reagents.Román-Pizarro et al. [32] prepared a new type of magnetic liposomes (MLs) containing hydrophobic magnetic gold nanoparticles (Fe3 O4 @ AuNPs) and the long-wavelength fluorophore cresyl violet for the determination of coenzyme Q10 in foodstuffs. AuNPs) and a long-wavelength fluorophore, cresyl violet, were used for the determination of coenzyme Q10 in food. First, the MLs were introduced into the flow-through system using a flow injection device and retained in front of the detector for 300 s by means of a solenoid device to achieve preconcentration. Then, a coenzyme Q10 solution containing the surfactant Triton X-100 was injected into the flow-through system. The surfactant caused the solubilization of the MLs and the release of cresyl violet, which was oxidized by coenzyme Q10, resulting in a decrease in the fluorescence signal. The concentration of coenzyme Q10 is directly proportional to the decrease in fluorescence signal. The LOD of this method is lower than that of the LC-UV method, but the equipment required is simpler and less expensive.
2.3 Electrochemical analysis
The redox properties of CoQ10/CoQ10H2 allow the determination of coenzyme Q10 by electrochemical analysis. The methods are generally voltammetric, such as cyclic voltammetry (CV) [33], differential pulse voltammetry (DPV) [34], square wave voltammetry (SWV) [35], etc. The samples can be pharmaceuticals, dietary supplements, animal and plant tissues, etc. The samples can also be used for the determination of CoQ10/CoQ10H2. Samples can be pharmaceuticals, dietary supplements, plant and animal tissues, etc.
Li et al. [34] investigated the electrochemical reduction mechanism of coenzyme Q10 at a silver electrode and developed a DPV method for the direct determination of coenzyme Q10 in plant and animal tissues. Cyclic voltammetry (CV) and electrochemical impedance spectroscopy (EIS) revealed that the reduction of coenzyme Q10 under anoxic conditions is a reversible one-electron, one-proton reduction and forms a stable semiquinone radical (coenzyme Q10H-), which is quenched by oxygen in an oxygen-filled environment. This is the reason why coenzyme Q10H2 is able to scavenge oxygen radicals due to its antioxidant function. Under the optimized experimental conditions, the DPV method can be used to determine coenzyme Q10 in complex samples, and it is rapid, sensitive, and highly selective, with an LOD of 3.33 × 10 -8 mol-L-1 .
Graphene, a single atom thick planar sheet composed of carbon atoms heterogeneously linked by sp2 in a honeycomb lattice, is a new type of sensor material [35]. Screen printing is a practical technique for manufacturing low-cost disposable sensors [35].
The new graphene sensor developed by this technology can be used for the determination of coenzyme Q10 and α-lipoic acid. The MnO2-modified screen-printed graphene electrode (MnO2/SPGE) has a larger capacitance and electrically active surface area, which facilitates electron transfer and significantly improves the oxidation performance of coenzyme Q10 and α-lipoic acid. The MnO2-modified screen-printed graphene electrode coupled with square wave dissolution voltammetry (SWV) can be used for the simultaneous determination of coenzyme Q10 and α-lipoic acid in dietary supplements with high sensitivity and practicality.
The electrochemical mechanism of coenzyme Q10 is complicated by the different electrodes and media. In a 1.1:1 methanol-ethanol solution, the electrochemical reaction of coenzyme Q10 at the glassy carbon electrode was controlled by adsorption, and the sensitivity of the determination could be improved by pre-enrichment [33]. In anaerobic ethanol solution, the cathodic process of coenzyme Q10 at the silver electrode was one-electron-single proton reduction [34], while the oxidation on MnO2/SPGE showed two-electron-single proton transfer [35]. Michalkiewicz [36] investigated the anodic oxidation of oxidized coenzyme Q10 in acetic acid solution using a glassy-carbon electrode and a carbon-fiber microelectrode coupled with voltammetry, respectively. The oxidized coenzyme Q10 in acetic acid solution was studied by
The results show clear oxidation peaks or waves in the potential range above 1.5 V. The presence of these signals cannot be linked to the well-known redox pair CoQ10/CoQ10H2, but may be attributed to the irreversible and diffusion-controlled two-electron oxidation of methoxy in coenzyme Q10 (formation of two additional quinone groups at the 2 and 3 positions of the ring). the total number of electrons involved in the CoQ10 anodic oxidation is much greater than two, suggesting that the oxidation also takes place in the unsaturated isopentadienyl side chain. The total number of electrons involved in CoQ10 anodic oxidation is much higher than two, suggesting that oxidation also occurs in the unsaturated isoprene side chain. The oxidation of the oxidized coenzyme CoQ10 has been rarely reported, is much less readily accessible than that of coenzyme Q10H2, and the mechanism of oxidation has yet to be demonstrated.
2.4 Other analytical methods
Supercritical fluids are substances whose temperature and pressure exceed the critical point, in a state of gas-liquid indistinguishability, with a density close to that of liquids, and a viscosity close to that of gases, and a high diffusion coefficient. Supercritical fluids with high diffusivity and low viscosity, very suitable for mobile phase. The supercritical fluid with more research and application is supercritical CO2. Supercritical fluid chromatography-tandem mass spectrometry (SFC-Ms/Ms) with supercritical CO2 as mobile phase can be used for the determination of coenzyme CoQ10 in rat plasma [8]. The method uses one-step acetone method to precipitate the protein and extract CoQ10 from the sample. Due to the low sensitivity of [M + H]+ of CoQ10 in mass spectrometry, methanol containing ammonium acetate was used as a post-column compensating solvent to provide [M + NH4]+ and improve the sensitivity. Supercritical CO2 is non-toxic, non-flammable, and relatively inexpensive, so it is widely used. Due to its non-polar nature, it is well suited for the analysis of fat-soluble compounds and can greatly reduce the use of organic solvents.
Other analytical methods include: high performance thin layer chromatography (HPTLC) [37], Fourier transform near infrared spectroscopy (FT-NIR) [38], nuclear magnetic resonance hydrogen spectroscopy (1 H- NMR) [39], etc. HPTLC is simple and rapid, but the sensitivity is not very high, and can be used for the analysis of coenzyme Q10 in raw materials and pharmaceutical preparations. FT-NIR does not require complex sample pretreatment, but requires a certain number of samples to establish a calibration model and obtain results through complex statistical analysis, and is generally used for the initial screening of the target analyte. 1 H- NMR also does not require complex sample pretreatment, can be both calibrated models, and obtained through complex statistical analysis, and is generally used for the initial screening of target analytes. FT-NIR does not require complex sample pretreatment, but requires a certain number of samples to establish a calibration model and obtain the results through complex statistical analysis, and is generally used for the initial screening of target analytes.1 H-NMR also does not require complex sample pretreatment, and can be used both qualitatively and quantitatively, with low sensitivity, and can be used for routine analysis of preparations. These methods can be used as a useful supplement to the quantitative analysis of coenzyme Q10.
3 Simultaneous determination of oxidized and reduced coenzyme Q10
In many methods, the total amount of coenzyme Q10 is determined by adding oxidizing agents such as FeCl3 to oxidize coenzyme Q10H2 to the oxidized form, and then the total amount of the oxidized form is determined. However, coenzyme Q10 coexists in both oxidized and reduced forms in biological matrices, and sometimes it is necessary to determine the two forms of coenzyme Q10 in biological samples, drugs and supplements separately. Commonly used methods include HPLC-UV [14, 15], HPLC-MS/MS [12, 13, 24, 25, 40], HPLC-ECD [6, 41], HPLC-FL [28], and so on.
Coenzyme Q10H2 standards are sometimes not readily available and can be obtained by reducing oxidized coenzyme Q10 with reducing agents such as NaBH4 [12-14,24,25,28,40,41]. The reduction of coenzyme Q10 at low concentrations may be incomplete, even if the amount of NaBH4 is 8800-fold excess [13], so the reduction process needs to be controlled at a certain concentration range. The reaction is usually carried out at low temperature and in the dark, and sometimes ED-TA is added to the solution after the reaction [12,13,15,25,41], which mainly binds to the metal ions that catalyze the oxidation process and acts as an antioxidant. Even if a standard of coenzyme Q10H2 is available, it may be partially oxidized and needs to be reduced before use [15], or the absorbance of the stock solution (ε = 4010) can be measured spectrophotometrically at 290 nm to determine the exact concentration [6].
Whether the quantitative results were expressed as the total amount of coenzyme Q10 or as the oxidized and reduced amounts, respectively, could affect the sample preparation. In order to maintain the reduced state of coenzyme Q10H2, in addition to the rapid operation at low temperature and the addition of antioxidants such as BHT during the preparation process, researchers have different opinions on whether the extracted solution should be re-dissolved by evaporating the solvent in the presence of N2. Some of them evaporate the solvent and re-dissolve it during sample pretreatment [12,14,15,24], while some scholars believe that there will be significant oxygenation of Coenzyme Q10H2 during solvent evaporation, so the extracted solution should be immediately dissolved in the presence of N2 [12,14,15,24].
Determination [6 ,13 ,25 ,28 ,40 ,41].
In fact, coenzyme Q10H2 is highly unstable during extraction and determination.Yamashita et al.[41] found that coenzyme Q10H2 was stable only at -78 °C, and the rate of oxidation of coenzyme Q10H2 to coenzyme Q10 increased with increasing storage time and temperature.Claessens et al.[25] found that significant oxidation of coenzyme Q10H2 to coenzyme Q10 occurred after 2 h in 1-propanol extracts of human plasma, so routine analysis was limited to 12 samples per batch in order to keep the total run time within 2 h. In addition, coenzyme Q10H2 is not stable at the same temperature as coenzyme Q1010. Claessens et al. [25] found that in 1-propanol extracts of human plasma, significant oxidation of coenzyme Q10H2 to coenzyme Q10 occurred after 2 h. Therefore, routine analyses were limited to 12 samples per batch in order to keep the total run time within 2 h. The results of this study are summarized below.
Due to the uncontrolled nature of oxidation, it has been suggested that almost all mitochondrial coenzyme Q10H2 is oxidized during sample pretreatment, and therefore quantification of total coenzyme Q10 in isolated mitochondria does not require ubiquinol oxidation [7]. Nevertheless, attempts have been made to control the rate of oxidation of coenzyme Q10H2 during analysis or to know the extent of oxidation. The choice of internal standards has helped to realize this desire. Structural analogs of coenzyme Q10 and coenzyme Q10H2, such as diethyl- or dibutyl-coenzyme Q10 [14] and dipropoxy-coenzyme Q10 [40], are sometimes used as internal standards in the analysis of coenzyme Q10 and coenzyme Q10H2. They are structurally very similar to CoQ10 and CoQ10H2 and exhibit the same chemical behavior as the analytes, especially with respect to artificial oxidation, which makes it possible to accurately back-calculate the original CoQ10H2/CoQ10 ratio [14].
The CoQ10H2/CoQ10 ratios in biological tissues varied, and Claessens et al. [25] showed that the plasma CoQ10H2/CoQ10 ratios in healthy volunteers without nutrient supplementation ranged from 22.3 to 64.4, with an average of 41.7, whereas Yamashita et al. [41] showed that the plasma CoQ10H2/CoQ10 ratio was about 95/5, suggesting that plasma coenzyme Q10 is mainly in the reduced form. These results indicate that plasma coenzyme Q10 exists mainly in the reduced form.
Changes in the CoQ10H2/CoQ10 ratio have important physiological significance and are associated with many functional disorders and diseases. Measurement of the CoQ10H2/CoQ10 ratio is useful in exploring the mechanisms of many diseases. Oxidative stress has been defined as a disturbance of the pro-oxidant-antioxidant balance in favor of the former, and is considered to be a causative factor in aging and degenerative diseases such as cardiac diseases, diabetes mellitus and cancer [41]. There is a consensus that the CoQ10H2/CoQ10 ratio is an important parameter in the assessment of oxygenation stress [24, 25, 41].
Another study showed that 2,3,7,8-tetrachlorodibenzo-p-dioxin (TC-DD) damaged mouse liver in a dose-dependent manner. Tang et al. [40] investigated the mechanism, and found that exposure of mouse liver samples to TCDD resulted in a decrease in the total amount of coenzyme Q10, a decrease in the level of coenzyme Q10H2, and an increase in the CoQ10H2/total CoQ10 ratio. This may be due to the inhibition of succinate dehydrogenase in the electron transport chain. In addition, the decrease in the total amount of CoQ10 implies that CoQ10 is degraded by external environmental influences, which was confirmed by Temova Rakua et al [42]. They found that oxidized coenzyme Q10 was degraded during storage of dietary supplements and drugs containing coenzyme Q10, and that oxidized coenzyme Q10 was converted to reduced coenzyme Q10H2, especially in the presence of antioxidants such as vitamin C.
4 Summary
Coenzyme Q10 is an important electron carrier and antioxidant component of the mitochondrial respiratory chain and is widely found in human cells. Coenzyme Q10 deficiency may be associated with a variety of diseases. Although it is an endogenous substance, it can be used as a drug or dietary supplement to treat or ameliorate certain related diseases. Therefore, the selection of efficient isolation and analytical methods is of physiological and clinical importance. Liquid-liquid extraction is the most common method for the extraction of coenzyme Q10, while the extraction of reduced coenzyme Q10H2 requires temperature control and the addition of antioxidants. Solid-phase extraction and molecular blotting techniques have also been applied in the extraction of coenzyme Q10 from biological samples, which have greatly improved the extraction efficiency and detection sensitivity.
Coenzyme Q10 can be detected by a variety of methods, and currently the most commonly used method is HPLC. In clinical and pharmaceutical analysis, miniaturization of instrumentation by reducing column diameter and length and particle size is one of the major trends in improving separations [43]. HPLC-UV is easy to use as a standard method, has good stability, is not very sensitive, but is generally sensitive enough to meet the requirements for the simultaneous analysis of a variety of components.
HPLC-MS/MS has high sensitivity and good selectivity, and has unique advantages for the analysis of coenzyme Q10 in complex matrices, such as biological samples, but the operation of the instrument is complicated and the price is expensive. The electrochemical analysis method is simple, fast and sensitive, and has certain applications in the analysis of coenzyme Q10. The HPLC-ECD method is convenient for the simultaneous determination of oxidized and reduced Coenzyme Q10. Coenzyme Q10 co-exists in both oxidized and reduced forms in almost any sample. Some analytical methods are capable of determining both the total amount of coenzyme Q10 and the oxidized and reduced forms, while others can only determine the total amount, depending on the HPLC separation. The characteristics of the various methods, their determination formats and their applications in samples are shown in Table 2.
Table 2 Comparison of different analytical methods for Coenzyme Q10
Easy and fast to use, sometimes requires color development or derivatization, matrix may be interfering
Coenzyme Q10 is mainly present in reduced form in organisms, and the ratio of CoQ10H2/CoQ10 is clinically important, with greater bioavailability of CoQ10H2 in drugs and dietary supplements. Therefore, the simultaneous determination of oxidized and reduced coenzyme Q10 is a future development. The distribution of the two forms, their interconversion and their biological significance will be a focus of future research, which also brings opportunities and challenges to the study of extraction and analytical methods for both forms of coenzyme Q10.
In order to meet the clinical needs, coenzyme Q10 can be prepared by microbial fermentation [44] or chemical synthesis in addition to extraction from biological samples. Chemical synthesis is divided into total synthesis [45] and semi-synthesis [46], and the intermediate of semi-synthesis is ganiol. Microbial fermentation can be used for large-scale industrial production.
References:
[1] Crane FL, Hatefi Y, Lester RI, et al. Isolation of a quinone from beef heart mitochondria [J].Biochim.Biophys.Acta, 1957 , 25 ( 1 ): 220-221.
[2] Wolf DE , Hoffman CH, Trenner NR, et al. Coenzyme Q. I. Structural studies on the coenzyme Q group [J]. J. Am. Chem. Soc, 1958 , 80 (17) :4752.
[3] Mitchell P. Coupling of phosphorylation to electron and hydrogen trans- fer by a chemi-osmotic type of mechanism [J].Nature,1961 ,191 :144- 148.
[4] Pallotti F,Bergamini C ,Lamperti C ,et al. The roles of coenzyme Q in disease:direct and indirect involvement in cellular functions [J]. Int.J.Mol.Sci,2022 ,23(1) :128.
[5] Visconti GL, Mazzoleni L, Rusconi C ,et al. Determination by UPLC/ MS-MS of coenzyme Q10 (CoQ10) in plasma of healthy volunteers be- fore and after oral Determination by UPLC/ MS-MS of coenzyme Q10 (CoQ10) in plasma of healthy volunteers be- fore and after oral intake of food supplements containing CoQ10[J].
J. Anal. Bioanal. Tech, 2015 ,S13 :011.
[6] Schou-Pedersen AMV,Schemeth D,Lykkesfeldt J. Determination of re- duced and oxidized coenzyme Q10 in canine plasma and heart tissue by HPLC-ECD : a comparison with LC-MS/MS quantification [J].Antioxi- dants,2019 ,8(8) :253.
[7] Itkonen O,Suomalainen A,Turpeinen U. Mitochondrial coenzyme Q10 determination by isotope-dilution liquid chromatography - tandem mass spectrometry〔J〕.Clin.Chem,2013 ,59(8) :1260-1267.
[8] Yang R,Li Y,Liu C ,et al. An improvement of separation and response applying post-column compensation and one-step acetone protein pre cipitation for the determination of coenzyme Q10 in rat plasma by SFC- MS/MS [J].J. Chromatogr.B ,2016 ,1031 :221-226.
[9] Bompadrea S,Tulipanib S,Romandini S,et al. Improved HPLC col- umn-switching determination of coenzyme Q and Vitamin E in plasma [J]. 2008 ,32(1-4) :257-262.
[10] Contin M,Flor S,Martinefski M,et al. The use of coenzyme Q0 as a template in the development of a molecularly imprinted polymer for the selective recognition of coenzyme Q10[ J].Anal.Chim.Acta,2014 ,807 :67-74.
[11] Becerra CG,Baez F,Lucangioli S,et al. Miniaturized imprinted solid phase extraction to the selective analysis of Coenzyme Q10 in urine [J]. Chromatogr.B ,2019 ,1116 :24-29.
[12] Pandey R,Riley CL,Mills EM,et al. Highly sensitive and selective determination of redox states of coenzymes Q9 and Q10 in mice tis- sues. Application of orbitrap mass spectrometry [J].Anal.Chim.Acta, 2018 ,1011 :68-76.
[13] Vass A,Deák E ,Dernovics M. Quantification of the reduced form of coenzyme Q10 , ubiquinol, in dietary supplements with HPLC-ESI- MS/MS [J]. food Anal.Methods,2015 ,8(2) :452-458.
[14] Franke AA, Morrison CM, Custer LJ, et al. Simultaneous analysis of circulating 25-hydroxy-vitamin D3 ,25-hydroxy-vitamin D2 ,retinol, to- copherols,carotenoids,and oxidized and reduced coenzyme Q10 by high performance liquid chromatography with photo diode-array detec- tion using C18 and C30 columns alone or incombination [J].J. Chromatogr A,2013 ,1301 :1-9.
[15] Temova Rakua,Kristl A,Rokar R. Quantification of reduced and oxi- dized coenzyme Q10 in supplements and medicines by HPLC-UV [J].Anal.Methods,. 2020 ,12(20) :2580-2589.
[16] Yubero D,Allen G,Artuch R,et al. The value of coenzyme Q10 de- termination in mitochondrial patients [J].J.Clin.Med,2017 ,6(4) : 1-10.
[17] National Pharmacopoeia Commission, ed. Chinese Pharmacopoeia (Part II) [S]. Beijing: China Pharmaceutical Science and Technology Publishing House ,2020 :1457.
[18] GB/T 22252-2008. Determination of Coenzyme Q10 in Health Food [S].
[19] Grace AC,Prabha T,Jagadeeswaran M,et al. Analytical method develop- ment for simultaneous determination of ubidecarenone and vitamin E ace- tate in capsule dosage form by HPLC [J].Int.J.Pharm.Pharm.Sci, 2019 ,11(1) :79-84.
[20] Rakusa ZT,Srecnik E ,Roskar R. Novel HPLC-UV method for simul- taneous determination of fat-soluble vitamins and coenzyme Q10 in medicines and supplements [J].Acta.Chim.Slov,2017 ,64(3) :523 - 529.
[21] Ruiz-Garcia M, Perez-Lozano P, Mercade-Frutos D, et al. Development and validation of a new high-performance liquid chromatography method for the simultaneous quantification of coenzyme Q10 ,phos- phatidylserine, and vitamin C from a cutting-edge liposomal vehiculi- zation [J].ACS Omega,2019 , 4(22) :19710-19715.
[22] Clementino A,Sonvico F. Development and validation of a RP-HPLC method for the simultaneous detection and quantification of simvasta- tin ′s isoforms and coenzyme Q10 in lecithin/chitosan nanoparticles [J].J.Pharm.Biomed.Anal,2018 ,155 :33-41.
[23] Boulet L,Alex B ,Clavey N,et al. Simultaneous analysis of retinol,six carotenoids,two tocopherols,and coenzyme Q10 from human plasma by HPLC [J]. J. Chromatogr.B ,2020 ,1151 :122158.
[24] Kotnik D,Jazbec-Krizman P,Krizman M,et al. Rapid and sensitive HPLC-MS/MS method for quantitative determination of CoQ10 [J]. Research on Precision Instrument and Machinery ( RPIM) ,2013 ,2 (1) :6-13.
[25] Claessens AJ,Yeung CK,Risler LJ,et al. Rapid and sensitive analysis of reduced and oxidized coenzyme Q10 in human plasma by ultra per- formance liquid chromatography-tandem mass spectrometry and appli- cation to studies in healthy human subjects [J].Ann.Clin.Biochem, 2016 ,53(2) :265-273.
[26] Mathieu RE ,Riley CP. Quantitation of ubiquinone (coenzyme Q10) in serum/plasma using liquid chromatography electrospray tandem mass spectrometry (ESI-LC-MS/MS) [J].Methods.Mol.Biol,2016 , 1378 :61-69.
[27] Yubero D,Montero R,Ramos M,et al. Determination of urinary coen- zyme Q10 by HPLC with electrochemical detection:Reference values for a paediatric population [J].Biofactors,2015 ,41(6) :424-430.
[28] Nohara Y, Suzuki J, Kubo H. Determination of ubiquinone in blood by high-performance liquid chromatography with post-column fluorescence- cence derivatization using 2-cyanoacetamide[J].J. Fluoresc,2011 ,21 (6) :2093-2100.
[29] Kishikawa N,Ohkubo N,Ohyama K et al. Selective determination of ubiquinone in human plasma by HPLC with chemiluminescence reac- tion based on the redox cycle of quinine[ J].Anal.Bioanal.Chem,2011 ,400(2) :381-385.
[30] Fukuda M, Liu Q, Kishikawa N, et al. Development of ultrafast colori- metric microplate assay method for ubiquinone utilizing the redox cy- cle of the quinine [J].Microchem.J,2019 ,150(C) :104104.
[31] Fei X, Yu Y, Di Y, et al. A rapid and non-invasive fluorescence meth- od for quantifying coenzyme Q10 in blood and urine in clinical analy- sis [J]. Clin. Lab. Anal,2020 ,34(4) :e23130.
[32] Román-Pizarro V,Fernández-Romero JM,Gómez-Hens A. Automatic determination of coenzyme Q10 in food using cresyl violet encapsula- ted into magnetoliposomes [J].Food Chemistry,2017 ,221 :864-870.
LIU Yuhong,GUO Bin,TU Yifeng [33]. Determination of coenzyme Q10 by adsorption voltammetry[J]. Journal of Analytical Testing ,2021 ,40(8) :1224-1229.
[34] Li D,Deng W,Xu H,et al. Electrochemical investigation of coenzyme Q10 on silver electrode in ethanol aqueous solution and its determina- tion using differential pulse voltammetry〔J〕.J.Lab.Autom,2016 ,21 (4) :579-589.
[35] Charoenkitamorn K, Chaiyo S, Chailapakul O, et al. Low-cost and dis- posable sensors for the simultaneous determination of coenzyme Q10 and α- Lipoic acid using manganese (IV) oxide-modified screen-prin- ted graphene [J].Anal.Chim.Acta,2018 ,1004 :22-31.
[36] Michalkiewicz S. Anodic oxidation of oxidized forms of coenzymes Q10 and Q0 on carbon electrodes in acetic acid solutions [J].Bioel- ectrochemistry,2011 ,82(2) :103-111.
[37] Kulkarni MB ,Joshi AM,Patil RV.A novel HPTLC method for simul- taneous determination of co-enzyme Q10 and α-tocopherol in bulk and pharmaceutical formulation [J].Int.J.Pharm.Pharm.Sci,2018 , 10(10) :134-141.
[38] Rácz A,Vass A,Héberger K,et al. Quantitative determination of co- enzyme Q10 from dietary supplements by FT-NIR spectroscopy and statistical analysis [J].Anal.Bioanal.Chem, 2015 , 407 ( 10 ): 2887-2898.
[39] Monakhova YB ,Ruge I,Kuballa T,et,al. Rapid determination of co- enzyme Q10 in food supplements using 1H NMR spectroscopy.Int.J.Vitam.Nutr.Res,. 2013 ,83(1) ,67-72.
[40] Tang Z,Li S,Guan X,et al.Rapid assessment of the coenzyme Q10 redox state using ultrahigh performance liquid chromatography tandem mass spectrometry[J].Analyst,2014 ,139(21) :5600-5604.
[41] Yamashita S, Yamamoto Y. Simultaneous Detection of ubiquinol and ubiquinone in human plasma as a marker of oxidative stress [J]. Anal. Biochem,1997 ,250(1) :66-73.
[42] Temova Rakua, Kristl A, Rokar R. Stability of reduced and oxidized coenzyme Q10 in finished products [J]. Antioxidants, 2021 , 10 (3) :360.
[43] Lucangioli S,Martinefski M,Tripodi V. Coenzyme Q10 analytical de- termination in biological matrices and pharmaceuticals [J]. Front.Biosci.Scholar,2016 ,8(2) :321-330.
[44] Fan JB ,Xu W,Xu Xi,et al. Production of Coenzyme Q10 by mi- crobes:an update [J].World J.Microbiol.Biotechnol,2022 ,38(11) :194.
[45] Nguyen T,Mac H,Pham P. Preparation of Key Intermediates for the Syntheses of Coenzyme Q10 and Derivatives by Cross-Metathesis Re- actions [J]. Molecules,2020 ,25 :488.
[46] Atla SR,Raja1 B ,Dontamsetti BR.A new method of synthesis of co- enzyme Q10 from isolated solanesol from tobacco waste [J]. Int.J.Pharm.Pharm.Sci,2014 ,6(8) :499-502.
#coenzymecoq10 #Coenzyme Q10 #Q10 #coq10
0 notes
Text
Understanding Clexane 60 mg Injection: Uses, Dosage, and Precautions
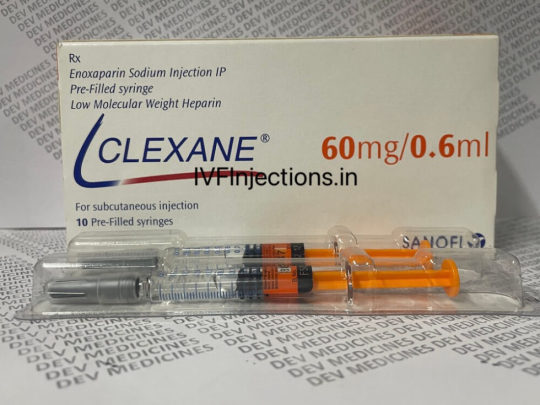
Uses:
Prophylaxis of Deep Vein Thrombosis (DVT): Clexane is often prescribed to patients undergoing surgery, particularly orthopedic or abdominal surgery, to prevent the formation of blood clots in the veins of the legs or pelvis.
Treatment of Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE): Clexane may be used in the treatment of established cases of DVT or PE, either alone or in combination with other anticoagulant medications.Prevention of Blood Clots in Certain Medical Conditions: Individuals with certain medical conditions, such as atrial fibrillation or cancer, may be at an increased risk of developing blood clots. Clexane may be prescribed as a preventive measure in these cases.
Dosage:
The dosage of Clexane 60 mg injection varies depending on the indication for which it is prescribed and the patient's individual factors, such as weight and renal function. It is typically administered subcutaneously (under the skin) once or twice daily. The injection is usually given in the abdomen, alternating sides with each dose.
For prophylaxis of DVT in patients undergoing surgery, a typical dosage regimen may involve a single injection of Clexane 40 mg administered 2 hours before surgery, followed by once-daily injections of Clexane 40 mg or 30 mg for up to 14 days post-surgery.
For the treatment of established cases of DVT or PE, the recommended dosage of Clexane is typically higher, with initial doses ranging from 1 mg/kg to 1.5 mg/kg administered subcutaneously every 12 hours. The duration of treatment may vary depending on the severity of the condition and individual patient factors.
It is important for patients to follow the dosage instructions provided by their healthcare provider and not to adjust the dosage or frequency of administration without consulting a healthcare professional.
Precautions:
Bleeding Risk: Clexane is an anticoagulant medication and can increase the risk of bleeding, particularly in patients with certain medical conditions such as gastrointestinal ulcers or bleeding disorders. Patients should be monitored closely for signs of bleeding, Endofert H 2 Mg and the medication should be used with caution in individuals at increased risk of bleeding.
Renal Impairment: Clexane is primarily eliminated from the body by the kidneys, and its clearance may be reduced in patients with renal impairment. Dosage adjustments may be necessary in patients with impaired renal function to prevent accumulation of the medication and potential adverse effects.
Heparin-Induced Thrombocytopenia (HIT): Rarely, patients treated with heparin medications such as Clexane may develop heparin-induced thrombocytopenia, a potentially serious condition characterized by a low platelet count and increased risk of blood clotting. Patients should be monitored for signs of HIT, and treatment should be discontinued if suspected.
0 notes
Text
Understanding the Role of Anticoagulants in Treating Pulmonary Embolism
Pulmonary embolism (PE) is a serious medical condition caused by the blockage of one or more arteries in the lungs, usually by a blood clot. Prompt and effective treatment is crucial to prevent complications and improve outcomes for patients. Anticoagulants play a key role in managing PE by preventing the formation and growth of blood clots. In this blog, we will delve into the importance of anticoagulants in treating pulmonary embolism.
What are Anticoagulants?
Anticoagulants are medications that inhibit blood clot formation. They work by interfering with the clotting factors in the blood, thereby preventing the formation of new clots and reducing the risk of existing clots growing larger. Commonly prescribed anticoagulants include warfarin, heparin, and direct oral anticoagulants (DOACs) such as apixaban, dabigatran, edoxaban, and rivaroxaban.
Role of Anticoagulants in Treating Pulmonary Embolism:
. Preventing Clot Growth: Anticoagulants are crucial in preventing the growth of existing blood clots in the pulmonary arteries, which can lead to severe complications such as pulmonary infarction or right heart strain.
. Reducing Recurrence Risk: Patients who have experienced a pulmonary embolism are at increased risk of recurrence. Anticoagulant therapy helps reduce this risk by maintaining blood thinness and preventing clot formation.
. Managing Symptoms: Anticoagulants can alleviate symptoms associated with pulmonary embolism, such as shortness of breath, chest pain, and fatigue, by improving blood flow through the lungs.
. Preventing Complications: By preventing new clots from forming, anticoagulants also help prevent complications like deep vein thrombosis (DVT) and stroke, which can occur if clots travel to other parts of the body.
. Long-term Management: Depending on the underlying cause of the pulmonary embolism, some patients may need long-term anticoagulant therapy to prevent future clotting events.
Types of Anticoagulants:
. Warfarin: Warfarin is a vitamin K antagonist that has been used for many years as an oral anticoagulant. It requires regular monitoring of the International Normalized Ratio (INR) to ensure therapeutic effectiveness.
. Heparin: Heparin is often used initially in the treatment of pulmonary embolism due to its rapid onset of action. It can be administered intravenously (IV) or subcutaneously (under the skin).
. Direct Oral Anticoagulants (DOACs): DOACs are newer anticoagulant medications that have gained popularity due to their convenience and predictable dosing. They include apixaban, dabigatran, edoxaban, and rivaroxaban and are taken orally.
Monitoring Anticoagulant Therapy:
Regular monitoring of anticoagulant therapy is essential to ensure therapeutic levels are maintained while minimizing the risk of bleeding complications. This may involve blood tests such as the INR for warfarin or specific tests for DOACs, depending on the medication prescribed.
In conclusion, anticoagulants play a vital role in the treatment and management of pulmonary embolism by preventing clot growth, reducing recurrence risk, managing symptoms, and preventing complications. Patients with PE require individualized treatment plans, and anticoagulant therapy is often a cornerstone of these plans. For reliable information and resources on anticoagulant therapy and self-monitoring options, visit patientselftesting.com and stay informed about managing pulmonary embolism effectively.
0 notes
Note
Hi, I want to start by saying I really enjoy your writing style but there are a couple of issues in Enouement. 1) You only give anti-heparin to when Heparin has been used, its not used on its own and never to a pregnant woman. If the bleeding was severe enough they would have other options that are safer. 2) Ibuprofen isn't a pain killer per se, its an anti-inflammatory which does help with pain by decreasing swelling, its no where near Morphine. Morphine is a highly regulated and monitored pain medication. 3) There is no studies showing that Ibuprofen causes miscarriage. It can cause problems in the first 8 weeks by decreasing blood flow to the baby's kidneys, but 1 dose isn't likely to do a ton of damage.
Normally I dont comment on these things but this could potentially lead to bad medical advice/knowledge being spread.
Keep up the writing!
henlo! thank you so much for the kind words <3 i am so glad you like my stories, i appreciate it <3
i agree with everything you said about the medical stuff because neither am i medical student nor a doctor. but hey, i am just out here writing fiction stories set in hypothetical universes. i cannot imagine anyone reading my stories and thinking what i wrote is how that aspect works.
i am a law student and in liberosis the portrayal of spousal privilege is made up. that is not how it works and again, i cannot imagine someone reading my stories and thinking ‘hey, this is how spousal privilege works!’ i take bits of information and try to bend it to the flow of my story and how i want it to go.
my main aim as a writer is to not write completely wrong things but then again, i am not trying to be correct to the last T because it is not a scientific academic paper published in a science journal. it is simply not possible: medical aspects, legal aspects, scientific aspects; they are never simply black and white and every little thing depends on the circumstances, the particular environment, the particular variables of that particular circumstances but my stories ain’t about that, the plot is about the characters not the correctness behind some aspects.
nothing in my stories is meant to be as advice and nothing written in fictional stories should be taken as advice anyways, unless the author explicitly vets that they know what they are talking about and that it is their professional opinion upon the topic.
i am not legally or medically advising anyone nor is there any vetted knowledge in my stories that a ordinary prudent person would think is legit.
5 notes
·
View notes