#fibromatosis
Explore tagged Tumblr posts
Text
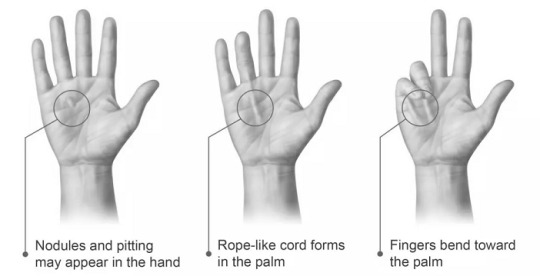
Dupuytren's Disease Market Dynamics: A Comprehensive Report
The global dupuytren’s disease market size is expected to reach USD 5.87 billion by 2030. Dupuytren’s disease is a debilitating condition characterized by the abnormal thickening and shortening of palm tissue, leading to the formation of claw-like finger deformities. This projected market expansion highlights the growing recognition of the importance of effectively addressing and treating this condition. The industry presents lucrative prospects for stakeholders, such as pharmaceutical companies, medical device manufacturers, and healthcare providers to develop innovative therapies and interventions. As the prevalence of the condition continues to rise, there is an escalating demand for effective treatments that can improve symptoms and enhance patients' quality of life.
Dupuytren’s Disease Market Report Highlights
The type II disease segment dominated the market in 2022 due to its higher prevalence, more severe symptoms, and greater demand for treatment options
In addition, advancements in medical technology have focused on addressing challenges specific to type II Dupuytren's disease, leading to a wider range of effective treatments available for patients
By type, the treatment segment held a dominant revenue share in 2022 due to the increasing demand for effective treatment options to alleviate symptoms and improve the quality of life for individuals
The hospitals end-use segment held the largest market share in 2022 due to advanced infrastructure, specialized care, and referral networks
Europe established a strong regional position in the market in 2022. This can be attributed to factors, such as advanced healthcare infrastructure, increasing prevalence of the disease, and presence of key players driving innovation and access to treatment options in the region
Gain deeper insights on the market and receive your free copy with TOC now @: Dupuytren's Disease Market Report
Consequently, intensified research and development efforts are anticipated in the near future, leading to advancements in treatment options and potential breakthroughs in managing Dupuytren's disease. In a recent study, adalimumab emerged as a potentially cost-effective treatment choice during the early stages of Dupuytren’s disease. The research findings suggest that this medication holds promise in effectively managing the condition while providing value for the investment. These results underscore the potential advantages of adalimumab as a practical and economically viable treatment option specifically for individuals in the early stages of Dupuytren’s disease. The growing awareness and understanding of the disease among healthcare professionals and patients, along with advancements in medical research and diagnostics, are driving the market expansion.
Improved detection rates and timely intervention have increased the demand for effective treatments. Endo Pharmaceuticals’ “Watching Education Unfold” campaign, featuring real patients, aims to raise awareness about Dupuytren’s contracture and educate the public and healthcare community about the condition and available treatment options. This initiative is expected to contribute to heightened awareness, early diagnosis, and improved management of contractures. In addition, significant advancements in medical technology and therapeutic approaches, such as injectable collagenase and minimally invasive surgical techniques, have played a crucial role in driving the market forward. Injectable collagenase treatment like Xiaflex has gained approval for Dupuytren's contracture in multiple countries, offering a less invasive alternative to traditional surgical procedures and leading to improved patient outcomes and shorter recovery times. These advancements in medical technology and therapeutics are significant contributors to the overall growth of the market.
#Dupuytrens Disease#Hand Health#Connective Tissue Disorders#Dupuytrens Awareness#Hand Contracture#Finger Deformity#Dupuytrens Treatment#Hand Surgery#Fibromatosis#Hand Therapy#Disease Awareness#Hand Rehabilitation#Collagen Disorders#Hand Function#Medical Research#Orthopedics#Patient Support#Healthcare#Chronic Illness#Hand Care
0 notes
Text
Effective Cryoablation Treatment for fibromatosis - Picture This Imaging
Cryoablation for fibromatosis is a cutting-edge treatment option offered by Picture This Imaging. This procedure uses extreme cold to target and destroy fibromatosis, which are benign but potentially troublesome tumors. By applying a precisely controlled freezing process, cryoablation effectively reduces or eliminates these growths while minimizing damage to surrounding healthy tissue. Picture This Imaging provides advanced imaging technology to ensure accurate placement and monitoring during the procedure. If you or a loved one is dealing with fibromatosis, cryoablation at Picture This Imaging offers a promising solution for effective management and relief.
0 notes
Text
Fibromatosis Cryoablation at Picture This Clinic
Picture This offers advanced Fibromatosis Cryoablation, a non-invasive treatment that uses extreme cold to destroy fibrous tumours. This innovative therapy offers numerous benefits, including minimal scarring and a shorter recovery time, making it an excellent alternative to traditional surgery for patients seeking effective and minimally invasive treatment options.
0 notes
Text
A rare case of bilateral plantar fibromatosis (Ledderhose’s disease): A case report by Amrutha Viswanath in Journal of Clinical and Medical Images, Case Reports
Abstract
Ledderhose’s disease, also known as plantar fibromatosis is a rare, benign hyperproliferative disorder affecting plantar fascia with unknown etiology. Clinical presentation of the disease varies according to the stage of the disease and individual characteristics. Diagnosis of the disease is usually based on clinical findings. Histopathological examination, Ultrasound or MRI can be used to rule out other conditions and for confirmation of the disease. Plantar fibromatosis can mimic the features of plantar fasciitis especially in early stages of the disease, hence it should be considered as a differential diagnosis in patients with pain and nodules in plantar aspect of foot. In this case report, we present a case of 24-year-old male with bilateral plantar fibromatosis, which was managed by surgical excision of the nodules due to unresponsive conservative management.
Keywords: Plantar fibromatosis; ledderhose’s disease; heel pain; nodular swelling; plantar fasciitis.
Introduction
Plantar fibromatosis or Ledderhose disease, is a rare benign pathology of the plantar aponeurosis, first described by Dr. George Ledderhose. It is characterised by disordered fibrous tissue proliferation and the subsequent formation of lump or nodules over the plantar aspect of the foot. The Office of Rare Diseases of the National Institutes of Health listed it as a rare disease with frequency about 1–1.75/100,000 [1]. Although etiology of plantar fibromatosis is unknown, it is associated with Dupuytren’s disease (palmar fibromatosis), Peyronie’s disease (penile fibromatosis) [2]. Increased risk of its occurrence is associated with alcoholism, chronic liver disease, diabetes mellitus, long term anticonvulsive treatment for epilepsy and genetic factors [3]. Males are more commonly affected than females. 25% of cases with plantar fibromatosis present with bilateral disease [4]. Diagnosis of Ledderhose’s disease is usually established clinically. Initially the nodule is asymptomatic and it becomes symptomatic as it enlarges in size. Direct pressure on the nodule while walking barefoot, standing for long periods of time and use of restrictive shoes may exacerbate pain and walking disability. Over time, multiple nodules may develop and can cause exacerbation of symptoms, contractures and deformities [5]. Given the benign nature, initial phase of the disease can be managed conservatively and if symptoms persist, definitive management of surgical excision of nodule gives complete relief of symptoms. The nodular swellings affecting the plantar fascia is of greater significance in population with poor socioeconomic status as people prefer to walk barefoot in developing countries.
The similarities of plantar fibromatosis to Dupuytren's disease affecting palmar fascia support the theory that, two conditions are different expressions of the same disorder [6]. Even though much has been discussed about Dupuytren's contracture in the literature; only very few literatures are available regarding plantar fibromatosis. In this case report, we present a case of 24-year-old male with bilateral plantar fibromatosis and aims to discuss the clinical presentation and various management options in plantar fibromatosis.
Case Report
A 24-year-old male presented to our department with dull aching type of pain over the plantar aspect of both feet of 1-year duration. Pain prevented the patient from weight-bearing for long time and walking for small distances. There was no significant familial history of the disease or history of any associated trauma. No associated medical history in the patient. Patient gives history of treatment in another hospital as bilateral plantar fasciitis. Conservative management was given there in the form of analgesics, anti-inflammatory drugs, advice to use footwear with soft insole and gives a history of 3 steroid injections administered 4-6 weeks apart. With persistence of symptoms patient came to our department. On physical examination small, well circumscribed, palpable, firm, nodular, single swelling was present over the medial plantar aspect of his both feet. The swellings measured about 2 x 1.5 cm on the right foot and 1 x 1 cm on the left foot. The skin over the swellings appeared normal and there were no neurovascular deficits or deformities. Ankle joint and foot range of movements were within normal range. On further examination, we found a similar swelling of size 0.5 x 0.5 cm on the palmar aspect of right hand with no restriction of movements and clinical signs. FNAC report showed mild to moderately cellular oval to plumb spindle shaped fibroblastic cells with elongated nuclei arranged in clusters and dispersed pattern associated with myxoid matrix. Cytology findings were suggestive of benign fibroblastic lesion. A provisional diagnosis of bilateral plantar fibromatosis was made, based on clinical and cytological findings. Since conservative management was tried earlier and there was persistence of symptoms and limitation in function surgical excision of the nodules was planned. Surgery was performed under spinal anesthesia. Nodules on both sides were palpated and skin over it was marked for surgical incision. The dissection of skin and soft tissue exposed the nodules on both sides, which were greyish white in colour, firm in consistency and attached to plantar fascia (Figure 3).
Figure 1: Nodular swelling on right foot (dot circle).
Figure 2: Dot circle indicating the nodular swelling on right palm.
Figure 3: Exposed nodule ( Right foot ) intraoperative image.
Figure 4: Excised nodule from right foot (greyish white, measuring 1x0.8x0.2 cm).
Figure 5: Excised nodule from left foot (greyish white to greyish brown, measuring 1.7x1.5x0.4 cm).
Excision of the nodules were done in both feet and primary wound closure was done. The patient was advised for non-weight bearing for 2 weeks and use of soft insole footwear thereafter for 2 weeks. Postoperative period was uneventful and sutures were removed after 2 weeks of surgery.
Figure 6: Postoperative wound before suture removal.
The histopathological examination of the excised nodules revealed spindle-shaped cells with abundant collagen in a fibrous stroma background and features were consistent with the diagnosis of bilateral plantar fibromatosis. On follow up of 6 months, patient reported complete relief of symptoms and improvement in function.
Figure 7: Photomicrograph of HPE slide showing nodular lesion composed of spindle shaped cells in a fibrous stroma background. (H&E staining, x40).
Figure 8: Photomicrograph of HPE slide showing spindle shaped cells with abundant collagen in fibrous stroma(H & E staining , x100).
Discussion
Ledderhose’s disease (Plantar fibromatosis) is a fibrous hyperproliferative pathology affecting the plantar fascia characterised by formation of nodules [7, 8]. The diagnosis of Ledderhose’s disease is usually established clinically and rarely require further investigations for confirmation [9]. Histopathological analysis and diagnostic imaging helps to differentiate between other lesions that can present with similar symptoms such as plantar fasciitis ( The most common disorder of plantar fascia), lipoma , ganglion cyst, leiomyoma, epithelioid sarcoma, rhabdomyosarcoma and liposarcoma [10, 11]. According to the clinical and pathological studies, plantar fibromatosis can be classified into three stages. The first (proliferative) stage of the disease is characterised by cellular proliferation and increased fibroblastic activity. The second stage of the disease which is the active phase is characterised by formation of nodules. It is followed by the third (residual) stage where collagen maturation and tissue contractures occur [11, 12]. Therefore the normal plantar fascia is replaced progressively by abnormal collagen fibres and can present at any stage of the disease with pain, nodule, walking difficulty, contractures or deformities of toes and the treatment is planned accordingly.
Patients presenting in the early stage of the disease with no or mild pain can be conservatively managed with padded shoes with soft insoles or custom offloading to redistribute the weight from the nodules, analgesics, anti-inflammatory drugs and intralesional steroid injections[10,13]. If left untreated, nodules may gradually increase in size and number which in rare cases may result in deformities of the toes due to contractures in later stages. In cases with persistence of symptoms after conservative management, lesions which are progressive, severe limitation of function and in advanced stages of the disease surgical management is considered as the last resort of treatment [14, 15].
The nodular swellings affecting the plantar fascia is of greater significance in developing countries with poor socioeconomic status as people prefer to walk barefoot. For the same reason, early surgical management is indicated for symptomatic cases in the developing countries.
Conclusion
The diagnosis of Ledderhose’s disease can be done clinically alone. Diagnostic imaging such as Ultrasound or MRI and histopathological examination may be used, to exclude other conditions and to rule out malignancies [16]. The treatment of the disorder is planned accordingly. Even though plantar fasciitis is the commonest disorder affecting plantar fascia, plantar fibromatosis should be considered as a differential diagnosis in patients presenting with pain and nodules in plantar aspect of foot as it can mimic the features of plantar fasciitis. The recommended treatment approach is to start with conservative management in early stages of the disease and perform surgical excision in unresponsive cases and advanced stages. But the best treatment plan is to establish a personalised approach depending on the individual characteristics, type of symptoms, stage of the disease and recurrence.
Authors Disclosures:
Funding / Grants: Nil.
In this study, there was no competing interests or financial benefits to the authors.
Details of any previous presentation of the research, manuscript, or abstract in any form: Not presented anywhere.
Acknowledgement:
Authors declare no conflict of interest.
In this case report, there is no financial benefits to the authors.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Plantar fibromatosis#ledderhose’s disease#heel pain#nodular swelling#plantar fasciitis#characterised#FNAC#Cytology#hyperproliferative#pathology#Amrutha Viswanath#jcmicr
0 notes
Text
The night of the July 28th election, hundreds of thousands of people saw the actas, and not only the opposition’s witnesses who kept copies.
What follows are three stories that break the silence: two from PSUV electoral witnesses and one from a community leader from the chavista grassroots. We’ll call them Karla, Daria, and María Eugenia.
María Eugenia
The streets of the rural settlement where María Eugenia lives haven’t seen asphalt. There’s no public transport, and cell phone service is very spotty. She has lived there, on the outskirts of Ciudad Bolívar, in southern Venezuela, for 26 years except for the six she spent in Barinas, the birthplace of Hugo Chávez, where her connection with chavismo began.
María Eugenia always enjoyed community work: giving talks to the elderly, helping with health campaigns, protecting animals, anything where she could lend a hand. When she arrived in Barinas, she completed high school through the Misión Ribas program. She became a chavista and remains one at 48. However, she quickly clarifies that she’s not a Maduro supporter—she’s certain there’s a distinction between him and Chavez.
After returning to Ciudad Bolívar, she felt grateful once more when, through the Ministry of Women’s Affairs, she was able to have surgery for fibromatosis. She coped with the depression of feeling unwell by throwing herself into more community work. She joined the Misión Ribas program in her parish, gave talks, and tried to help the most vulnerable students. She fought for resources to build houses for them. She regained strength by feeling useful.
In time, her community began seeing her differently. She wasn’t just another neighbor; she was a leader committed to social work. She was nominated as community leader, a role in the chavista grassroots structure that bridges the political efforts led by the head of the UBCh (whose mission is to defend the revolution) and community leaders. She became part of what she calls the “grassroots chavismo.”
As the presidential election approached, María Eugenia was given the task of securing a minimum of 90 votes for PSUV. Her community had about 300 residents, a little more than half were eligible to vote. She encouraged them in her own way: “Don’t let someone else vote for you,” “If you want things to improve, you need to vote…”
She didn’t tell them to vote for Maduro. She knew it wasn’t easy to convince everyone. For the construction of 20 houses, they were given MDF boards -wood waste- for roofing, which didn’t last through two rainy days. It took two years to replace them with zinc sheets. At political events, they were barely given water. She knew that her community, being so small, was among the most forgotten in the parish. Without work, the young men had to risk their lives in the gold mines in the south of the state. Her nephews had left for the mines or Brazil. She herself survived on a government salary of 220 bolivars a month and 1,390 bolivars in bonuses (around $39 in total). Even with the “economic war bonus” of 3,288 bolivars ($79), it wasn’t enough.
No, she didn’t tell them to vote for Maduro, only to vote according to their conscience.
“But people moved on their own,” she says, as if it’s a revelation. “We didn’t have to go fetch them from their homes like in all the other elections. People went to vote because they wanted to. It was like they knew who to vote for.”
And that wasn’t the only unusual thing about Sunday, July 28.
It was a traumatic election. All day there was tension. On the chat, they told us to stay alert, that there might be trouble, that the opposition would send motorcycles to scare us, that they could cut the power. I felt like they were terrorizing us for no reason. In our community, we’ve never fought over politics. We joke about it instead.
That day, she was responsible for providing food for her 17 street leaders and writing down the name of every neighbor who voted in her center. She was one of the first to vote.
And as dusk fell, the most unusual thing happened: the chat exploded with messages saying they had lost in almost all the centers in the parish. The UBCh heads were furious, demanding explanations, hysterical.
A parish where they had never, ever lost. A community where they had always won by a landslide.
In her voting center, with only one voting table, in a school that had started under a mango tree and gradually gained walls and a roof, Maduro won by just a tiny margin.
One of only 74 stations where the opposition lost, according to the tally sheets gathered by its witnesses from 1,129 stations across Bolívar state.
She didn’t get to see the tally sheet from her table because she went home, because she left before it was printed. She hasn’t been interested in seeing it either. In the community, they say Maduro won by very little votes. She doesn’t know, but according to the tally sheets collected and published by the opposition, the margin was a bit larger. But it makes no difference, winning by so little is unimaginable. Something María Eugenia never would have thought possible but somehow sensed.
“That’s why we didn’t have to fetch them from their homes like in all the other elections. People knew what they wanted… I knew what I wanted: so I have to confess, I voted for Edmundo González. And I haven’t lost hope, like many in my community, that justice will be served.
9 notes
·
View notes
Text
i worked an “honest” job standing 10 hours a day getting screamed at by customers who were intent on making me feel stupid and lower than them just because i was wearing an uniform, and was regularly punished by making me take both opening AND closing shifts because i didn’t seem to put in enough effort (i suffer from Plantar fibromatosis and regularly had to sit down, my feet were killing me.)
sold my nudes for a few months and not only did i make more money than what my “honest” job paid me, but i was routinely told that i was beautiful and that i was a wonderful person for allowing them to see me, lol. most were respectful of my availability and didn’t ask more than what i could give them, which is way more than what my previous employers have done for me lol.
157K notes
·
View notes
Text
Gingival And Periodontal Diseases Question And Answers
#OralMedicine#DentalHealth#OralHealthMatters#SmileCare#Gingival And Periodontal Diseases Question And Answers
0 notes
Text
Complicazioni dopo un intervento ginecologico: risarcita con 30mila euro
Una donna ha ottenuto un risarcimento dopo aver riportato complicazioni mediche a seguito di un intervento chirurgico eseguito presso una struttura ospedaliera in provincia di Agrigento
Una donna ha ottenuto un risarcimento dopo aver riportato complicazioni mediche a seguito di un intervento chirurgico eseguito presso una struttura ospedaliera in provincia di Agrigento. La vicenda risale all’estate del 2016, quando la paziente, affetta da fibromatosi uterina, una patologia caratterizzata dalla presenza di fibromi benigni ma fastidiosi, era stata ricoverata per un’operazione di…
0 notes
Text
“Hereditary Gingival Fibromatosis”, Victor McKusick, Mendelian Inheritance in Man, 1966. 牙龈纤维瘤病。(HGF).
Here I present: “Gingival Fibromatosis”, Victor McKusick, Mendelian Inheritance in Man’, 1966. 牙龈纤维瘤病。(HGF). INTRODUCTION. Hereditary gingival fibromatosis (HGF) is a condition of gingiva (gum) overgrowth. The gingival (gums) consist of the mucosal tissue that lies over the mandible and maxilla inside the mouth. Gingiva (gums) health and disease can have an effect on general health. HGF is a…

View On WordPress
0 notes
Text
Gingival And Periodontal Diseases Question And Answers
0 notes
Text
Gingival And Periodontal Diseases Question And Answers
0 notes
Text
Advanced Cryoablation Treatment for Fibromatosis - Picture This Imaging
Picture This Imaging is offering Best Cryoablation for fibromatosis in Mumbai. Our innovative approach uses Cryoablation technology to target and eliminate affected tissues, offering swift relief. Imagine a life without the discomfort of fibromatosis as our non-invasive procedure ensures minimal downtime and optimal results. Picture This Imaging as your partner in restoring well-being, with state-of-the-art cryoablation paving the way for a brighter, healthier tomorrow. Embrace comfort and vitality with Picture This Cryoablation
0 notes
Text
Cryoablation for Pelvic Fibromatosis Treatment- Picture This
Cryoablation involves using extreme cold to eliminate cancer cells. This is achieved by inserting a cryoprobe, which is a thin needle-like wand, through the skin and into the tumour. PictureThis offers expert cryoablation for the treatment of Pelvic Fibromatosis. To learn more about the treatment, visit Picture This today.
0 notes
Text
Happy Dupuytren Day! Guillaume Dupuytren, the famous surgeon, was born on 5 October 1777. He would have been 246 years old today. If he were alive now, there's a good chance he'd have the disease named after himself. Why is it called Dupuytren disease or Dupuytren contracture? Most medical disorders are named in one of three ways. Dupuytren has all three. Many names are eponyms - the name of someone linked to the disease, usually the doctor who first described it. For example, surgeon James Parkinson first described "paralysis agitans", which came to be known as Parkinson disease. Dupuytren described the condition and operated on his patient in front of a live medical audience. He believed it came from mechanical stresses: his patient held horse reins as a coachman. He didn't name it himself, but at the time, he was the most famous surgeon in Europe, so his name stuck. Another way to name conditions is by describing what they look like, often in Latin, so it sounds official. For example, a vesicle is a small blister and a bulla is a large blister. Dupuytren has been described as palmar fascial fibromatosis, contraction of palmar fascia, and similar terms. Lay names are the third source of medical names, usually simple explanations or descriptions. For example, tennis elbow (lateral epicondylitis), athlete's foot (fungal dermatosis), and lockjaw (tetanus). Dupuytren has many lay names, including Viking disease, Celtic hand, and "the curse of the MacCrimmons". In Denmark, it's been called kuskefingre - Danish for "Coachman's finger", from Dupuytren's original theory. Catchy, but medically inaccurate. Dupuytren contracture was described by Felix Plater in 1610, and by others long before Dupuytren's time. Before Dupuytren, it was called "crispatura tendinum" by Boyer, and "permanent retraction of the fingers" by Cooper. Dupuytren won the naming competition. Guillaume Dupuytren's most significant contribution to Dupuytren contracture is not his surgical operation. It's not his theory of what causes it. It's not his description of the anatomy. It's that it became the standard name for this condition. Why is that a big deal? Because a standard name allows doctors and scientists in different countries speaking different languages to collaborate. When you say or write "Dupuytren disease", people know exactly what you're talking about, regardless of location or language. For example, this image is from a 1997 publication in The Journal of the Korean Rheumatism Association: For English speakers, Dupuytren is hard to spell and its pronunciation doesn't make sense. Should we rename it? No! It's a way for patients to talk about what they are dealing with. It's the rallying cry of those working on a cure, like the Dupuytren Research Group. So even though he had no role in choosing either his birthdate (Happy Birthday!) or his name (Thanks for the eponym!), today is the right day to celebrate both. Happy Dupuytren Day! - Charles Eaton MD
0 notes
Link
Desmoid Tumor: Unraveling Its Enigmatic Nature Desmoid tumors, though rare, hold a perplexing place in the world of medical conditions. Understanding their intricacies is vital, as they can significantly impact those affected. In this comprehensive guide, we will delve into the depths of desmoid tumors, shedding light on their causes, symptoms, and treatment options. What is a Desmoid Tumor? A desmoid tumor, also known as aggressive fibromatosis, is an uncommon type of tumor that arises from connective tissue. Unlike traditional tumors, desmoid tumors don't spread to distant organs, but they can infiltrate nearby tissues and structures. These tumors typically grow slowly and, while benign, can be locally aggressive, causing significant health issues. [caption id="attachment_50569" align="aligncenter" width="732"] desmoid tumor[/caption] Causes and Risk Factors The exact cause of desmoid tumors remains elusive. However, researchers have identified several potential factors and risk factors that may contribute to their development. These include: Genetic Predisposition: Some individuals may have a genetic predisposition to desmoid tumors, with a family history of the condition. Previous Surgeries or Trauma: In some cases, desmoid tumors have been linked to previous surgical procedures or trauma to the affected area. Hormonal Influence: Hormonal changes, such as those occurring during pregnancy, may play a role in the growth of desmoid tumors. Genetic Mutations: Certain genetic mutations, such as mutations in the APC gene, have been associated with an increased risk of desmoid tumors, particularly in individuals with familial adenomatous polyposis (FAP). Signs and Symptoms: Deciphering Desmoid Tumor Indicators Recognizing the signs and symptoms of a desmoid tumor is paramount, as early detection can lead to more effective treatment and improved outcomes. While desmoid tumors can manifest differently in each individual, some common indicators include: Persistent Pain and Discomfort Desmoid tumors often cause persistent, localized pain and discomfort at the site of the tumor. This pain may gradually intensify and become more pronounced over time. Palpable Mass or Swelling Many individuals with desmoid tumors notice the presence of a palpable mass or swelling beneath the skin. This mass may feel firm or rubbery to the touch. Limited Range of Motion Depending on the tumor's location, it can restrict the affected area's range of motion. Individuals may experience difficulty moving joints or performing regular activities. Pressure on Nearby Organs In some cases, larger desmoid tumors may exert pressure on nearby organs or structures, causing issues such as bowel or bladder problems. Visible Changes in the Skin Desmoid tumors beneath the skin may lead to visible changes, such as dimpling or reddening of the overlying skin. It's important to note that desmoid tumors can mimic other medical conditions, which can complicate diagnosis. Therefore, if you or someone you know experiences any of these symptoms or has unexplained pain or swelling, it's crucial to seek medical evaluation promptly. Diagnosis: Shedding Light on Desmoid Tumor Detection Diagnosing a desmoid tumor often involves a series of medical evaluations and tests to confirm its presence and assess its characteristics. Healthcare professionals typically follow these steps: Medical History and Physical Examination The process begins with a thorough medical history review, including any family history of desmoid tumors or related conditions. A physical examination helps locate and assess the tumor's size and location. Imaging Tests Imaging tests like ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) scans provide detailed images of the tumor. These tests help determine the tumor's size, shape, and proximity to surrounding structures. Biopsy A biopsy involves the removal of a small tissue sample from the tumor for laboratory analysis. This confirms whether the tumor is desmoid and rules out other potential conditions. Genetic Testing In cases where a genetic predisposition is suspected, genetic testing may be recommended to identify relevant mutations. Treatment Options: Navigating the Path to Desmoid Tumor Management The management of desmoid tumors requires a tailored approach, as treatment plans are influenced by various factors, including the tumor's location, size, growth rate, and the individual's overall health. Several treatment options are available: Watchful Waiting In cases where the desmoid tumor is small, slow-growing, or not causing significant symptoms, healthcare providers may recommend watchful waiting. Regular monitoring through imaging tests allows them to track the tumor's progression. Surgery Surgical removal of the desmoid tumor is an option when it's feasible without causing significant functional impairment. Surgeons aim to completely remove the tumor while preserving surrounding structures. Radiation Therapy Radiation therapy involves the use of high-energy X-rays to target and shrink desmoid tumors. It is often considered when surgery is not possible, or when tumors recur after surgery. Medications Non-surgical treatments may include medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), hormonal therapies, or targeted therapies. These medications can help slow tumor growth and alleviate symptoms. Physical Therapy Physical therapy may be recommended to improve mobility and reduce discomfort in individuals with desmoid tumors that affect joint or muscle function. Supportive Care Supportive care measures focus on managing pain and improving the individual's overall quality of life. This may include pain management strategies and psychosocial support. The choice of treatment depends on the specific circumstances of each case. Healthcare providers work closely with individuals diagnosed with desmoid tumors to develop a personalized treatment plan that addresses their unique needs and goals. Living with Desmoid Tumors: Strategies for Coping and Support A diagnosis of desmoid tumors can be challenging, but several strategies can help individuals and their families cope: Seek Supportive Communities Connecting with support groups or online communities can provide valuable emotional support and a platform to share experiences. Communicate with Healthcare Providers Maintaining open and honest communication with healthcare providers ensures that treatment plans are aligned with individual preferences and goals. Prioritize Self-Care Practicing self-care through relaxation techniques, exercise, and a healthy diet can enhance overall well-being. Explore Complementary Therapies Some individuals find relief from complementary therapies such as acupuncture, massage, or meditation. Stay Informed Educating oneself about desmoid tumors and staying up-to-date on the latest advancements can empower individuals in their healthcare journey. Frequently Asked Questions (FAQs) About Desmoid Tumors 1. What is a desmoid tumor? A desmoid tumor, also known as aggressive fibromatosis, is a rare, non-cancerous growth that arises from connective tissue. Although benign, these tumors can be locally aggressive. 2. Are desmoid tumors cancerous? No, desmoid tumors are not cancerous. They do not spread to other parts of the body like cancerous tumors, but they can grow and invade nearby tissues. 3. What causes desmoid tumors? The exact cause is unclear, but genetic factors, previous surgeries, trauma, and hormonal influences may contribute to their development. 4. How are desmoid tumors diagnosed? Diagnosis typically involves a medical history review, physical examination, imaging tests (ultrasound, MRI, CT scans), and a biopsy to confirm the presence of a desmoid tumor. 5. Are desmoid tumors hereditary? While most desmoid tumors are sporadic, some individuals may have a genetic predisposition due to mutations in certain genes, such as APC, often associated with familial adenomatous polyposis (FAP). 6. What are the treatment options for desmoid tumors? Treatment options include watchful waiting, surgery, radiation therapy, medications (NSAIDs, hormonal therapies), and physical therapy, depending on the tumor's characteristics. 7. Are desmoid tumors painful? Yes, desmoid tumors can cause persistent pain and discomfort at the tumor site, which may intensify over time. 8. Can desmoid tumors come back after treatment? Yes, desmoid tumors can recur even after treatment. Regular monitoring is essential to detect and manage recurrences. 9. Do all desmoid tumors require treatment? No, smaller and slow-growing desmoid tumors may be monitored without immediate treatment, following a "watchful waiting" approach. 10. Where can I find support for dealing with desmoid tumors? Support groups, online communities, and organizations dedicated to rare diseases can provide valuable emotional support and information for individuals and families coping with desmoid tumors. Conclusion Desmoid tumors may be enigmatic, but with knowledge, support, and the right medical care, individuals can face this condition with resilience. Understanding the signs, seeking timely diagnosis, and exploring the available treatment options are essential steps in managing desmoid tumors.
0 notes