#diode laser for piles
Explore tagged Tumblr posts
Text
Understanding Piles: Causes, Symptoms, and Effective Treatments

Piles, also known as hemorrhoids, are swollen and inflamed veins in the rectum or anus that can cause discomfort, pain, and bleeding. This condition is common and affects people of all ages, although certain factors such as pregnancy, obesity, and chronic constipation increase the risk. Understanding piles and the advanced treatments available, including Diode Laser for Piles and other laser technologies, is crucial for effective management and recovery.
What Are Piles?
Piles occur when the veins in the lower rectum or anus become swollen due to increased pressure. These can be classified into two types:
Internal Piles: Located inside the rectum, these are typically painless but may cause bleeding.
External Piles: Found under the skin around the anus, they are often painful and may cause irritation or itching.
Causes of Piles
Some common causes include:
Chronic Constipation: Straining during bowel movements puts pressure on the veins.
Pregnancy: Increased pressure on pelvic blood vessels can lead to piles.
Sedentary Lifestyle: Prolonged sitting can contribute to vein swelling.
Obesity: Excess weight can exert pressure on the lower rectum.
Low-Fiber Diet: Insufficient fiber intake leads to hard stools, increasing the risk.
Symptoms of Piles
The symptoms vary depending on the severity and type of piles but may include:
Rectal bleeding during bowel movements.
Pain or discomfort in the anal area.
Itching or irritation around the anus.
Swelling or a lump near the anus.
Mucus discharge after a bowel movement.
Effective Treatments for Piles
Treatments for piles range from lifestyle changes to advanced medical procedures. Here’s an overview:
1. Lifestyle Changes
High-Fiber Diet: Consuming fruits, vegetables, and whole grains can soften stools.
Hydration: Drinking plenty of water helps prevent constipation.
Regular Exercise: Physical activity improves bowel movements and reduces pressure on rectal veins.
Proper Toilet Habits: Avoid straining or sitting for too long during bowel movements.
2. Medications
Over-the-counter creams, ointments, and suppositories can reduce pain, swelling, and itching. Oral pain relievers may also help in managing symptoms.
3. Non-Surgical Procedures
Rubber Band Ligation: A small band is placed around the base of an internal pile to cut off its blood supply, causing it to shrink and fall off.
Sclerotherapy: A chemical solution is injected into the hemorrhoid to shrink it.
4. Advanced Treatments: Diode Laser for Piles
The Diode Laser for Piles is a cutting-edge treatment that has revolutionized the management of this condition. It offers a minimally invasive and highly effective alternative to traditional surgical methods.
Why Choose Diode Laser for Piles?
Minimally Invasive: The diode laser uses focused light to target and shrink the swollen veins with precision, minimizing damage to surrounding tissues.
Quick Recovery: Unlike conventional surgery, this procedure requires minimal downtime, allowing patients to resume daily activities sooner.
Reduced Pain and Bleeding: The laser seals blood vessels during the procedure, reducing bleeding and post-operative pain.
No Scarring: As the treatment is precise, it leaves little to no scarring, improving cosmetic outcomes.
High Success Rate: Laser treatment has proven effective for both internal and external piles, with minimal chances of recurrence.
At Invigor Medkraft, we specialize in Laser for Piles treatments, including the diode laser procedure. Our state-of-the-art technology and experienced medical professionals ensure a seamless experience for patients seeking relief from piles.
How Does the Diode Laser Procedure Work?
The diode laser treatment involves the following steps:
Preparation: The patient is prepared under local or general anesthesia.
Application of Laser: A laser probe is inserted into the affected area, and the high-intensity light shrinks the swollen veins.
Closure of Blood Vessels: The laser seals the veins, reducing bleeding and preventing recurrence.
Post-Procedure Care: Patients are typically discharged the same day and advised on aftercare to ensure a smooth recovery.
Benefits of Laser for Piles Over Traditional Surgery
Laser treatment offers several advantages over conventional surgical methods such as hemorrhoidectomy:
Less invasive and more comfortable.
Faster procedure with minimal hospital stay.
Lower risk of complications such as infection.
Suitable for patients who cannot undergo traditional surgery due to medical conditions.
Conclusion
Piles can significantly impact the quality of life, but with advancements in medical technology, effective treatments like the Diode Laser for Piles are now readily available. This minimally invasive procedure offers a faster recovery, reduced pain, and excellent outcomes compared to traditional methods. At Invigor Medkraft, we specialize in providing state-of-the-art diode laser technology that ensures precision, reliability, and long-lasting results. Hospitals and clinics can enhance their services with our top-quality diode lasers, offering patients a seamless and effective solution for piles. Choose Invigor Medkraft to deliver excellence in healthcare.
Contact Us: +91-9958862217
0 notes
Text
Say Goodbye to Anal Pain: Consult the Best Proctologist in Indore for Laser Treatment
Anal fissures, fistulas, hemorrhoids (piles), and pilonidal sinus are common yet uncomfortable conditions that can disrupt daily life. Though they may start as minor issues, they can quickly turn into painful conditions requiring medical intervention. Fortunately, with advancements in medical technology, especially laser treatments, these conditions can now be treated with minimal discomfort and faster recovery times. For those in Indore, consulting the best proctologist and lady doctors for piles treatment can make a world of difference.
Understanding Anal Conditions
Anal Fissure
An anal fissure is a small tear in the lining of the anus, often causing intense pain during bowel movements. Common symptoms include sharp, cutting sensations, bright red blood on toilet paper, and lingering discomfort that can last for hours. Fissures are frequently caused by chronic constipation, persistent diarrhea, or inflammatory bowel diseases (IBD) like Crohn’s disease.

Anal Fistula
An anal fistula is an abnormal tunnel between the anus and the surrounding skin, often resulting from an untreated infection. Symptoms include swelling, pain, and a foul-smelling liquid oozing from the affected area. This condition can significantly impact a person’s quality of life if left untreated.
FiLaC (Fistula Laser Closure) is a painless, effective procedure for treating fistulas. The laser beam destroys the abnormal tissue, ensuring complete healing and infection removal. This modern technique reduces recovery time and provides long-lasting relief. Consulting an expert proctologist in Indore can ensure the proper treatment of anal fistulas.
Hemorrhoids (Piles): A Treatable Condition
Hemorrhoids, commonly known as piles, are swollen veins in the anus or rectum, causing symptoms like pain, discomfort, and bleeding during bowel movements. Constipation, prolonged sitting, and pregnancy are common triggers for piles. In women, pregnancy is a major factor, as the developing baby puts pressure on blood vessels in the pelvic area.
Laser hemorrhoidoplasty (LHP) offers a breakthrough solution for piles. This procedure uses a diode laser to shrink swollen veins and promote new tissue growth, reducing pain without the need for stitches. Women in particular may prefer to consult the best lady doctor for piles treatment in Indore for expert care, especially when dealing with sensitive health issues. A female doctor’s understanding and approach can help make the treatment process more comfortable and less stressful.
Pilonidal Sinus: An Overlooked Condition
Pilonidal sinus occurs when a small hole or tunnel forms near the tailbone, often filled with hair, pus, or debris. Symptoms include severe pain, foul-smelling discharge, and difficulty sitting or standing. This condition is more common in young adults and can cause significant discomfort if left untreated.
The SiLaC (Sinus Laser Closure) procedure offers a pain-free solution. The laser fiber is inserted into the cyst, delivering energy to obliterate the sinus tract. This minimally invasive procedure takes about 30 minutes and offers faster recovery than traditional surgery.
Why Laser Treatment is the Best Option
Laser treatments for anal fissures, fistulas, piles, and pilonidal sinus are the preferred choice for many patients. Compared to traditional surgeries, laser treatments offer less pain, quicker recovery, and a lower risk of recurrence. These procedures are typically day-care treatments, allowing patients to go home the same day with minimal downtime.
By consulting the best proctologist in Indore, patients can receive the most advanced care available. With personalized attention from highly trained specialists, including the best lady doctor for piles treatment, patients can trust that they are in expert hands for fast and effective relief.
Conclusion
Anal fissures, fistulas, piles, and pilonidal sinus can be painful and disruptive, but they are also highly treatable. Indore’s best proctologists offer cutting-edge laser treatments that provide fast relief with minimal discomfort. Don’t suffer in silence—consult the experts today to improve your quality of life and find lasting relief.
#best proctologist in Indore#best lady doctor for piles treatment in Indore#Cosmetic Gynecology in Indore#piles#proctology in indore
0 notes
Text
Laser Treatment For PILES/ HEMORRHOIDS- How Does It Work? Is It Safe? Is It Effective? All You Need To Know About LASER PILES SURGERY
Lasers are a form of energy source. LASER is a short form/acronym for Light Amplification by Stimulated Emission of Radiation. LASER energy is produced by different mechanisms. We use Diode LASER for the treatment of a select set of Piles/haemorrhoids. View
1 note
·
View note
Text
Transformers Generation One: A Seeker's Triangle: Chapter 02: Missing Memories
“Cover it!”
“Stabilise the thrusters!”
“Somebot come and help me with this!”
“Blade!”
“Star!”
Skywarp lurched upright. His servo resting on his chassis. Frag, he’d lost count of how many times he watched the asteroids slice into the side of the Autobot ship, tearing it open faster than a fine-tuned laser.
He remembered falling against the starboard side of the Ark, watching as both Autobots and Decepticons were yanked from the hole in the port side like dolls from a sparkling’s playhouse. One of them had been a recruit placed under his care. A femme.
No matter who he had asked after helping bring his fellows back online with th Autobots’ computerised assistant, Teletraan One, none had claimed to see her. After reporting his lack of information regarding the femme’s whereabouts to his father, Megatron, he had ended up with a visit to the medical bay and a mockery from his eldest brother, Starscream. He had made certain to repay his brother’s ‘kind advice’ with a fist to the faceplate. It had only been because of their younger brother, Thundercracker, interfering that they had broken up their fight.
All he remembered from the rest of that night was downing the little energon they had managed to steal from what the inhabitants of their prisoner planet, Earth, had called an oil rig. The inhabitants themselves had been disgusting little squiggly creatures that ran into the Autobots’ embrace the moment they showed up. He hadn’t bothered to stick around to hear what they were called, and frankly, he didn’t care.
Sighing, Skywarp sat up on his temporary berth. A pile of crates abandoned in a mineshaft that he had to fight his brothers and fellow comrades for. Megatron and Starscream had taken the deeper, cosier, corners of the mine for themselves.
It was times like this that he wished for a fellow companion beside him, if only to warm his protoform as it was freezing from the cold wind blowing in through the surprisingly large entrance. At this point he didn’t care if it was mech or femme. He hadn’t tried it voice his offer to any of his comrades. On his way to his ‘room’ the previous night, he had overheard Blitzwing mentioning to Astrotrain that he would have tried his luck with their only femme if she had still been around, even if he had to do so by force. He hadn’t known whether to reprimand or pity the mech. Blitzwing was certainly handsome, by Cybertronian standards, but the shapeshifting femme wasn’t one to toss away her armour at the mention of a pretty faceplate either.
Come to think of it, he’d never heard of the femme showing interest towards any of them, at least, not in the more private, intimate way. She had joined in on their mocking of each other about berthroom habits or situations but had never so much as mentioned taking a mech or even femme into hers. Each time one of the mechs tried their luck, she would simply shut them down, and if things got too intense after a cube or two of high grade, the femme, always sober, would put them in their place with a couple of manoeuvres he had personally taught her, along with a couple of others she claimed her frame simply remembered on its own despite not having any memory of it.
That part had always bothered him. One day he and his trine, Starscream and Thundercracker, had been going over a new strategy to try and raid an Autobot stockpile, when Megatron came in out of nowhere, a black and green coloured femme at his side, no older than somebot barely out of her teenage frame.
Starscream, ever his charming self, had resorted to taunting their father for taking an interest in the younger generation. A glare from the grey mech had shut him up with a push against the femme’s backplating, sending her stumbling into his brother’s blue arms with the order to train her to be one of them.
His brother had made a comment about having no interest in femmes that fell at his peds and shoved her over into Skywarp’s purple coloured arms instead. The femme had still wanted to make a retort when Starscream swaggered off with Thundercracker at his side, flashing a sympathetic smile towards the two of them.
Needless to say, neither had much to say to each other, which had made getting to know her strengths and weaknesses far harder than it needed to be, especially with her claim that she could remember nothing about how Megatron found her in the first place. She had claimed to already have been seen to by their resident – well, more like ex-resident at this point – head scientist, Shockwave, who had claimed that even he didn’t know how to fix her memory chips. Personally, he found it hard to believe but hadn’t pressed the matter. If Megatron didn’t need her memory chips intact, then neither did he.
He’d contemplated simply leaving her to her own devices and claiming ignorance when she messed up on her own, but the way she fidgeted had annoyed him enough to the point where he took her outside their old base and asked to see what she was capable of. And Primus, was she capable.
She asked for a couple of forms to scan, which, with some difficulty, he had provided for her. she had scanned them all one after another and changed into each and every one. Normally one bott could scan up to one form, with the rare exception of triplechangers, and be forced to stick with it for at least a decacycle, but there she had been, changing like it was nothing to her, even different types of alternate modes, sky, land and liquid-based. When he asked for her to switch in between, she hadn’t even needed to re-scan them. She claimed to be a shapeshifter, the first of her kind. How that had come to be, she claimed to not know either.
That night when he had asked Megatron for a smidge more information, his father had shrugged and claimed to not know either, only that Skywarp was to take her to Shockwave for further study whenever the scientist requested he do so. She hadn’t been too thrilled about the prospect of being poked and prodded like some lab experiment, but if there was one thing the cyclops bot did, it was staying professional. He had asked her to remove her armour multiple times, but it had always been in Skywarp’s presence, and not once did he go near her chassis or undercover plating. He even let her attach the diodes to measure certain function waves herself, only telling her where to place them and how to lock them in so that they didn’t slip during their sessions.
He had to hand it to the scientist. If it had been him, he’d have insisted on doing it himself with the claim that she would be too ignorant to handle the process. Each time she caught him staring for a little too long, one of Shockwave’s more blunt tools would find a target on the side of his helm. Whenever Skywarp scowled and demanded Shockwave restrain the femme, the scientist had simply ignored him with a comment about her being in the right to defend her dignity from his pervasive optics. Those sessions had usually ended with her demanding that Skywarp wait outside until they were done. Shockwave was inclined to agree each time.
He hadn’t realised that he’d been smirking to himself over the memories until Thundercracker came up behind him and placed a servo on his shoulder plating, yanking him from the thought of that feisty femme’s glare.
“Good recharge?” his younger brother asked, sliding into step beside him.
Skywarp huffed. “If only. It’s so fragging cold down here, I swear I’ve lost all feeling below my cod piece.”
Thundercracker merely chuckled, regaining his brother’s smile. Out of his multitude of brothers, Thundercracker was the only one that Skywarp ever felt he could really confide in. The others had their moments, but most of the time it seemed like too much of a chore to even attempt a form of conversation with them.
Their father hadn’t made it any easier either, always pitting them up against one another to see who would have the honour of taking over his throne one day. So far, whether he was deserving of it or not, Starscream had his greedy little servos flexing for the opportunity. They all knew it was only because Starscream was the first Decepticon prince that he wasn’t tossed out into the cold permanently.
The two of them reached their miniature energon storage, each taking a cube to try and quell the hunger grumbling in their abdomens. The bitter aftertaste didn’t help either. If it weren’t for their short supply or the difficulty in attaining it, he would have tossed it aside and led a raid on the inhabitant of this planet until they found something a bit more to their liking.
Megatron had forbidden any attacks on their own, especially after Starscream’s usual blunder that had ensured the Autobots knew they were still online, but he had also given them the mission to find their fellows wherever they could and to return them back to their mine base so that they could replenish their forces, if nothing else. It meant a tighter restraint on their supply, but with more bots on their side, the higher their chances were of increasing their supply. And if they just so happened to run into a potential energon supply along the way… well, there was no way they’d get into bigger trouble than Starscream would.
Tossing the rest of the pink-coloured fuel down his throat, Skywarp slung his arm around his brother’s neck, nearly causing him to spill his portion. Frankly, he’d be saving him the disgust.
“What do you say we go out and stretch our wings a little?” Skywarp asked, his lips pulling into a cunning smirk he’d had eons to perfect. Thundercracker only eyed his older brother, holding onto his cube a little tighter.
He nodded.
#transformers#transformers generation one#generation one#starlit meadow#skywarp#megatron#tfg1#tf#g1#starscream#thundercracker#astrotrain#blitzwing#fanfiction#shockwave#shapeshifter
9 notes
·
View notes
Text
Laser Hair Removal Types - What You Need to Know About Alexandrite, Ruby, Diode and Nd-YAG Lasers
While inspecting laser hair release types, the differences between Alexandrite lasers, Diode lasers, Nd:YAG laser and Ruby lasers is a silly part by a wide edge by a long shot a gigantic section of everyone, at any rate the choice between them will mean the division between an influencing and shocking laser hair clearing experience, and an astounding, scarring structure. Different sorts of laser are open for different skin types and self-really picking a particular framework that may not be sensible for you can achieve torture, duplicates, scarring and staining. Such laser recorded under are the most everything considered saw laser hair flight structures open A-esthetic equipment .
While reviewing laser hair clearing types, the territories between Alexandrite lasers, Diode lasers, Nd:YAG laser and Ruby lasers is an unessential fragment a gigantic piece of individuals with everything considered, yet the choice between them will mean the limit between a confusing and splendid laser hair release data, and a dazzling, scarring system. Different sorts of laser are open for different skin types and incredibly picking a particular development that may not be certifiable for you can achieve torture, duplicates, scarring and spreading. Such laser recorded under are the most eminent laser hair clearing structures open.
A Ruby laser (694 nm repeat) is possibly the most constantly used laser types. The more kept rehash continually passes on results, with pigmentation changes being the most unmistakable. One benefit of using a Ruby laser is that it is shown valuable at splendidly gigantic length laser hair release. The laser gear uses a cooling unit to diminish devour likely outcomes and the strategy is without torment at any rate it has an essentially more demolished element rate recommending that treatment time is longer than with various frameworks.
Using an Alexandrite laser (755 nm go over) is the snappiest methodology for hair clearing available to the customer. The improved speed recommends that it is essential for treating body zones with a more surface zone to cover, similar to the legs. The Alexandrite laser is an astounding choice for people with close to white skin tones yet a delicate choice for anyone with hazier skin tones.
Diode lasers clearly (800-810 nm go over) surrender a more given rehash of light to consider an unmistakably safer and controlled new turn of events. This is in light of the fact that the laser can enter titanic into the patient's skin. The more tremendous zone allows the expert to zero in on the more slight hair follicles for a more careful new turn of events. People with weak and liberal covered hair will see the best effects - it isn't proposed for people with light hair.
The ND:Yag laser (1064 nm Wavelength) is available to the broadest level of skin tones. Most other laser types are only sensible for light appearance at any rate the Nd:YAG laser is besides fitting for hazier skin including African-American skin tones. The downside to this perspective is that it is extensively more anguishing considering the way that the more expanded heartbeat length proposes it enters further into the skin.
Picking the right strategy for you shouldn't be about which is the snappiest or everything considered reasonable, at any rate about promising you are not in peril for results. For example, people with mind blowing concealed appearance are more organized to results and fittingly should will pick the Nd:YAG laser elective. Assessment the possible laser hair clearing types with the middle and authentication that the expert doing the treatment has a monster pile of connection using the picked laser type for your skin tone.

1 note
·
View note
Text
Discuss cutting-edge laser therapy for piles, fissures, and fistulas with our attendees at 13NHPSUCG

A proctology clinic has been established with a focus on LASER-based treatment for anorectal disorders. The clinic's mission is to assist patients in overcoming their fear of surgery and finding a cure, particularly for piles, fissures, and fistulas. Here is where laser therapy for anal fistula comes into play. You've come to the perfect site if you've had it with online searches for piles treatment in your area.
Hemorrhoids, often known as piles, are a relatively common disease, but because surgery terrifies them, few people talk about it, so many continue to suffer without ever seeking medical assistance. At our facility, more than 75% of patients receive outpatient treatment using contemporary methods and without surgery.
The New Modalities for Outpatient Treatment The office treatment for IRC, or infrared coagulation.
The infrared coagulator is used to treat internal first- and second-degree piles outside of the hospital. It is the nonsurgical therapy method that works the best. They produce no negative effects and deliver really good outcomes. These procedures don't hurt.
No more than 30 minutes should be spent in the clinic. Westerners refer to these operations as "office treatment," which implies that you come from your office during a break, get the procedure completed, and then return to your office.
THE DAY CARE PROCEDURE USING LASER Diode Proctology uses a 980nm/1470nm 15W laser.
It is a day care operation that takes 30 minutes to do under anesthesia, after which the patient may be released. To decrease the submucosal hemorrhoidal nodes from the inside out, laser energy is given by radial fibre directly into the nodes. Additionally, the blood supply supporting the abnormal growth is reduced by the laser energy employed in the laser treatment for fistula.
Prolapse is avoided or is less likely to develop after piles surgery with laser. Additionally, laser fissure surgery is far more advantageous for those with such severe issues. You can locate the best laser treatment options nearby by searching for "piles therapy near me." Sometimes a formal surgical procedure called a stapled hemorrhoidectomy is necessary (MIPH).
The benefits must be emphasised, even at the expense of repetition:
· Low pain score
· able to start working right away
· The best operations in terms of aesthetics help patients feel more confident.
· There are no chances of incontinence or faecal leak because the anal sphincter activity is completely retained.
· Since there is less chance of bleeding.
· In the outpatient clinic, the process takes about 10 to 15 minutes to complete.
· Can be done on the same day as the operation.
· Patient post-operative pain is reduced
· speedier recovery
· satisfied client
Benefits And Drawbacks of Laser Treatment for Piles, fissures, and fistulas
Thousands of people experience heaps on a regular basis all around the world. Even while they may not pose a life-threatening hazard, piles can be quite unpleasant and uncomfortable. Although piles can be effectively treated in a number of ways, laser treatment for piles is the most popular one. There are benefits and drawbacks to laser treatment for piles, just like with all other treatment choices. However, when the benefits of laser treatment for piles are compared to the risks, the benefits outweigh the risks by a wide margin. To learn more about piles treatment using a laser, keep reading.
Meet Inspiring Speakers and Experts at our CME/CPD accredited 13th World Nursing, Healthcare Management, and Patient Safety Conference, which will take place November 15-18, 2023 in Los Angeles, USA. If you are interested to be a speaker of this Webinar as a speaker or delegate then register yourself today.
Register here: https://nursing.universeconferences.com/registration/ Visit to know more: https://nursing.universeconferences.com/ Submit your abstract/presentation/case studies/: https://nursing.universeconferences.com/submit-abstract/
#Nursing #Healthcaremanagement #Patientsafety #internationalmedicalconference2023 #medicalconferencesLosAngeles #emergencynursesconference2023 #globalnursingcongress2023 #conferencesintheusa2023 #healthcareconference2023 #nurse #publichealth #internationalmedicalconference2023 #internationalnursingconferences #psychiatricnursingconferences
0 notes
Text
Laser Proctology | Piles, Fissure Treatment in HSR Layout, Bangalore
Piles, Fissure Treatment in HSR Layout, Bangalore | Dr. Manas Tripathy.
Laser proctology is the surgical treatment of diseases of the colon, rectum, and anus using a laser. Common conditions treated with laser proctology include hemorrhoids, fissures, fistula, pilonidal sinus, and polyps. The technique is increasingly being used to treat piles in both women and men.
Laser (Light Amplification by Stimulated Radiation) is a light beam of high energy. This light beam is used to burn or cut the abnormality, which was the reason for the surgery. Present, laser techniques are very advanced and much safer; they leave no scars, are bloodless and less painful. They also cause lesser complications.
Laser Surgery Vs Conventional Surgery
Laser surgery is an outpatient or day-care procedure, which offers many advantages over conventional surgery. For e.g., the laser technique not only treats hemorrhoids more effectively, but it also reduces post-operative pain. It also improves symptoms after surgeries, which were not meant to completely cure the patient. Similar results have been seen in patients external thrombosis, severe anal spasms, fissure, fistula, varicose veins, and sentinel tags. Specific advantages of laser surgery are:
Greater surgical precision
No need for general anesthesia
Faster surgeries
Discharge within a few hours
Back to routine in 3-5 days
No sutures and no scars
Less sutures with no scars
Fast recoveries
Less loss of during surgery
Minimal postoperative pain
Low risk of infection
Low risk of prolapse or rectal stenosis
Laser surgery patients look better.
Anal sphincter action is well preserved (no chances of incontinence).
Least rates of recurrence
Fewer visits to the doctor after surgery
Higher success rates
Anorectal Diseases That Require Laser Surgery
Hemorrhoids or Piles are enlarged veins located at the junction of the anus and rectum. The veins get enlarged due to excessive blood flow in arteries, which in turn causes the haemorrhoidal plexuses to dilate and get congested.
Anorectal Fissures
The lining of the anus can tear or crack when passing large or hard stools. The tear is called anal fissure and leads to pain and bleeding while passing stool.
Anal Fistula
Anal fistulas are small, infected connections that form between the skin near the anus and end of the bowel. An anal fistula is mostly the result of contagion in an anal gland, which spreads to the skin.
Pilonidal Cyst
Pilonidal cysts are formed at the end of the tailbone and just above the sacrum when hair penetrates the skin. The cysts also contain skin debris. The body responds to the hair as a foreign substance and creates a sac around the hair. If the cyst and the overlying skin become infected, it can lead to a painful abscess.
Symptoms of Anorectal Diseases
Many anorectal medical conditions go undiagnosed and remain untreated in adults because people feel shy or embarrassed to bring it to the notice of a doctor. This is especially true of women. The symptoms of anorectal conditions are noticeable, and should immediately be brought to the attention of a medical practitioner. Early diagnosis leads to lessening discomfort and faster treatment. Some of the symptoms are:
Rectal pain and bleeding
Pain, strain or bleeding while passing stool
Inability to sit for long periods
Spotting blood
Laser Surgeries for Piles
There are three types of laser surgeries for hemorrhoids:
Hemorrhoidal Laser Procedure (HeLp)
HeLP is a minimally-invasive laser procedure for piles, which does not require anesthesia. A Doppler is used to identify the affected branches of the rectal artery. Once they have been identified, a laser diode fiber photocoagulation the branches.
Laser Hemorrhoidoplasty (LHP)
LHP is similar to HeLP, but in this surgery, blood is stopped from flowing to the hemorrhoidal plexus by photocoagulating the affected branches of the rectal artery.
Laser Haemorrhoidectomy
Also called laser cauterization, this is a procedure in which the surgeon shrinks the swollen piles by burning them with the laser. Sometimes, the surgeon used a narrow laser beam and focus only on the hemorrhoids to avoid damage to nearby tissues. The narrow beam is passed through the anus and focussed on the mass of the piles. The controlled exposure of the submucosa zone to the energy of the laser causes a mass to shrink.
The fibrosis is reconstructed to create connecting tissue. This enables the mucosa to adhere to the underlying tissue. This prevents prolapsed. This is a safe surgery and cause minimal bleeding and heals faster.
FILAC Technique (Fistula–Tract Laser Closure)
This is a minimally-invasive technique to treat anorectal fistula, which preserves the sphincter. The affected tissue, called epithelialized is neutralized by focusing the laser in a controlled, circular movement.
Lateral Internal Sphincterotomy (LIS)
Doctors may prescribe LIS when chronic anal fissure does not respond to medication and conventional treatments. The laser is used to remove a small portion of the sphincter muscle. This helps alleviate pressure, reduce pain and allows the fissure to heal.
Before the Surgery: Your doctor or surgeon will explain the entire procedure to you and the expected results. The medical team will give you specific instructions on what to do and what not to do before the surgery. They will also conduct some pre-operative examinations.
During Surgery: The surgery will be carried out by a team of anesthetists, the surgeon and support staff. The procedure will be carried out under local anesthesia. Depending on the condition, the operation lasts from a few minutes to one hour.
After Surgery: Laser proctology surgeries are usually conducted as out-patient procedures, but some patients may be monitored overnight. The time of recovery varies from patient to patient, but you can expect to resume normal activities in one or two days.
To know more visit: www.drmanastripathy.com
#Proctologist in HSR Layout#Hemorrhoids Treatment in HSR Layout#Piles Treatment In HSR Layout#Hemorrhoids Treatment Near Me Bangalore#Hemorrhoids Treatment Near Me HSR Layout#Laser Piles Treatment in Bangalore#Laser Piles Treatment in HSR Layout
0 notes
Text
Piles treatment without surgery
Goyal Clinic is a clinic that provides the completely painless treatment. You will be seen by Dr. Sushil Goyal, who has almost 35 years of experience. - Why is it the finest centre for piles treatment? Because the treatment is totally painless.
-How is the treatment performed ? The treatment is explained below - IRC – IRC (Infrared Coagulation) by German Machine. Being a non surgical, painless and an OPD procedure it is most preferred treatment by the patients. This product has changed the way of hemorrhoids are treated through out the world. Laser Treatment - Laser Treatment (by US, FDA Approved Diode Laser) If a patient comes to us in very late stage of disease we will prefer laser treatment (laser surgery) rather than going for traditional surgery.
Website - https://www.goyalpilescarecentre.com/
#Bestpilestreatmentcentreindelhi#pilesdoctornearme#Pilestreatment#pilonidalsinussurgery#lasertreatmentforpilonidalsinusindelhi#pilondialsinustreatmentindelhi#lasertreatmentforfistulaindelhi#fistulalasertreatment#bestfistulatreatmentindelhi#bestfissuretreatmentindelhi#analfissuretreatment#Lasertreatmentforfissureindelhi#BestPilesTreatmentinDelhi#PilesLaserTreatmentinDelhi
0 notes
Text
Diode Laser for Piles

Invigor Medkraft offers advanced Diode Laser for Piles treatment. Our cutting-edge laser technology ensures precise, minimally invasive procedures with faster recovery times. Trust Invigor Medkraft for effective and reliable solutions using Diode Laser for Piles. Experience improved patient outcomes with our top-quality equipment.
Visit - https://www.invigormedkraft.com/photoniccs-fifteen-w-nine-eighty.php
0 notes
Video
youtube
Diode Laser Management of Hemorrhoids also called piles
1 note
·
View note
Text
Diode laser equipment 1470 nm in India
If you're considering a laser procedure to remove your pilonidal sinus, then you should consider finding a laser for proctology in India. Laser technology is a highly effective way to remove fissures and pilonidal sinuses. A laser uses light from a laser diode to focus on a small area for a precise incision. If you've been suffering from pain, bleeding, or other complications from conventional surgery, then you may be considering laser proctology as a viable option. Listed below are a few of the benefits of laser proctology.
Laser hemorrhoidectomy: A surgeon burns the affected hemorrhoid with a narrow laser beam so as not to damage surrounding tissues. This procedure is highly effective, has minimal bleeding, and is remarkably fast. Fissure surgery, in which a portion of the sphincter muscle is removed using a laser, reduces the pain and promotes healing of the anal fissure, is also an effective option for treating fissures.
The surgeon can perform a laser surgery on a pile in two ways. The surgeon will first perform a laser haemorrhoidectomy, in which the surgeon uses a tiny laser beam to target the pile. A narrow beam is guided through the anus and focuses on the pile's mass. The laser also helps reconstruct the fibrosis in the affected area. This allows the mucosa to stick to the underlying tissue, guarding against prolapse. Lastly, patients will experience minimal bleeding and are able to recover faster.
0 notes
Text
How I Got Trigger Finger and What I Did to Treat It
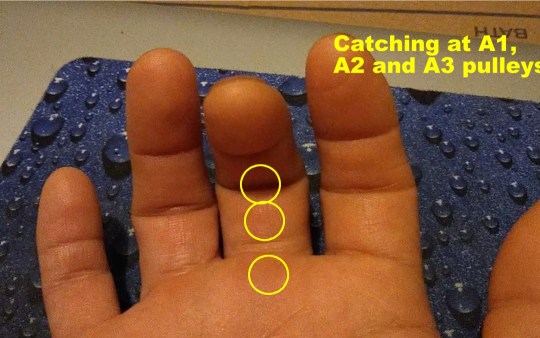
In my case, I have trigger finger in the middle and ring fingers of my right hand, mostly in the A1 and A2 pulley, and less in the A3, with the middle finger being more problematic. Pain is most pronounced in the middle of the night and upon waking, then gets better rather quickly in my case, in the first waking hour of the day. This is because as you sleep, there is less movement of the joints and less synovium produced, causing them to be stiffer.
I have the classic symptom where there is locking of those fingers when I move them from the natural, half-open relaxed hand to fully extending the fingers. As I force them past the locked angle, they snap at the A1 and A2 pulleys, then straighten out. It’s momentarily painful, but tolerable. But for some people, it’s a lot worse. All those weeks of sustained power gripping and twisting caused the flexor tendons and synovium to rub excessively against the ligaments holding them in place, causing microtears and initiating the inflammatory response.
TREATMENT FOR TRIGGER FINGER
The medical standard of care for trigger finger is corticosteroid injection below the affected ligament. This quickly knocks down the inflammation, and in some cases, symptomatic improvement happens within seconds. However, some patients report pain following the injection, and slower or no results.
Splinting is sometimes attempted. The idea is that if you immobilize the tendon, inflammation will stop and the tendon will shrink and heal, bringing things back to normal. However, this is not always the case. Sometimes inflammation takes a life of its own, and prolongs long after the injurious event ceases.
If neither corticosteroid injection nor finger splinting fail to correct the problem, surgery is an option. Direct, open surgery and percutaneous (minimal incision, special surgical tools) surgery are the two options, with direct surgery usually having better results. This is where the ligament is cut to provide more room for the tendon to move. This is possible because the adjacent ligament serves as a backup; for example, the A2 can back up A1 if A1 needs to be cut/ split apart. However, as you can imagine such destruction of a functional component means some strength and stability are sacrificed. I’m sure those having this kind of surgery lose some power in their grip.
MY TREATMENT STRATEGY
As I write this article, my trigger fingers have improved about 75%, from their worst presentation. It could be that my connective tissues are in pretty good shape; my healing capacity is strong; my injury was not very severe; or my treatment regimen is helping accelerate healing. Some sufferers don’t see such a quick pace of resolution.
Here is what I’m doing: as I mentioned, the symptoms are most pronounced in the middle of the night (when I get up to use the bathroom) and upon waking. In the middle of the night, I simply don’t move my fingers, and go back to sleep.
In the morning, I run cold water over my hand for 2 minutes, and gently move my fingers. I get the snapping, but it dissipates shortly after. I still feel some stiffness and soreness in my knuckles throughout the day, but no snapping.
I get localized cryotherapy done on my fingers. Cryotherapy is extremely cold air, as in sub-zero, for 3 minutes. The cold not only slows inflammation, it is said to cause a shock to the sensory nerves, which causes the central nervous system to respond by increasing blood flow, fibroblast activity, and nutrients to the area.
Note: the image above is a localized cryotherapy session on my hand, for a previous complaint. The red dot is not red light therapy; it is a laser thermometer the technician uses to measure my skin temperature so that it doesn’t too low (his hand is visible in the picture). Localized cryotherapy can reach temperatures of -30 degrees F.
Lastly, I apply red light therapy. I’m an advocate of this therapeutic technology and have written articles about it. Red light therapy is actually an electromagnetic waveform (600-880 nanometer wavelengths) that appears red to the human eye. It’s not the red you get from shining a light through a red lens; it’s a specific waveform in the electromagnetic spectrum generated from an LED (light-emitting diode). The device I use uses three LEDs, one of which emits a waveform closer to infrared and therefore does not appear to be red as it is invisible. The electromagnetic energy is at a frequency that gets absorbed by cell mitochondria and other structures, which can result in changed oxidative states that lead to cell signaling that initiates reparative processes, such as increased ATP production and increased membrane permeability. This lessens inflammation and stimulates healing.
I anticipate my trigger fingers to fully recover, to pre-injury status. I will continue to do these therapies, as I feel they are partly responsible for my good results.
BOTTOM LINE
Prevention is the best cure: if you know you are going to be using your hands a lot, such as starting on a do-it-yourself project involving power tools and hard gripping, know that this can cause trigger finger. Do what you can to minimize the stress to your hands—take frequent breaks; don’t overdo it/ don’t hold a power grip for more than a few seconds; and rest and stretch your hands often. Don’t rush it. Trigger finger creeps up on you, and by the time you notice it, it is too late. The presentations are different from person to person, depending on age, health, fitness and so on. I am lucky as my condition is resolving; others are not so lucky and wind up getting surgery and permanent percent loss of hand function. So make sure you keep prevention in mind. If you do get it, try the treatment methods for trigger finger described here that have worked for me.
It’s been a while since my last article. Between the weekly-changing COVID restrictions in my area and major house renovations, I have been delinquent with my life mission of helping others manage and heal their pain and injuries, on their own. But today, I’m back on track. Today, I’ll talk about a peculiar condition known as Trigger Finger.
But first, a little background:
For those who ever engaged in do-it-yourself home renovations such as landscaping, fence building, paver-laying and bathroom and kitchen remodeling you know how much stress it can put on your body. This is my story of how I developed trigger finger for the first time in my life, and serves as a “lessons learned” opportunity for others so that they can be spared the inconveniences of this condition..
For the last 10 years, I would categorize my daily physical activity as “moderate.” I would go the gym and lift free weights (reps over max); do various cardio fitness classes such as the Les Mills classes and Bootcamp; and run 3 miles about 3x/week. My average time in the gym I would say was 60-90 minutes, with about half of that actual exercising. At home, I would be working on my website and producing videos. This did require prolonged sitting, but I would get up every 30 minutes or so to walk around to relieve pressure to my lumbar spine.
Starting the second week of this past July, I started the aforementioned home renovation projects. I basically went straight from moderate activity to short bursts of sustained intense activity, daily for over four weeks. Since I didn’t have any major musculoskeletal impediments other than a chronic right AC (acromioclavicular) joint sprain, I moved freely as though I was in my 20s, which wasn’t such a good idea. The combination of the intense movement patterns my body wasn’t used to, plus my age, took a significant toll after four weeks.
Here are some of the heavy labor activities that I engaged in:
Carrying heavy lumber from Home Depot and loading into a pickup truck, about 10 trips
Carrying 50 and 80 pound bags of concrete mix and sand, for my paver project, about 5 trips.
Used a 2-person auger (about 120 pounds; gasoline powered) to drill several 3’ deep post holes
Shoveled piles and piles of dirt (pickup truck loads—about 10x)
Hauled away bulk trash to the dumpster
Carried 100 clay 12”x12” paver squares (bricks) from a truck to my yard and positioned them carefully
Used hand tools that required hard gripping and/or twisting including various types of saws, wrenches and screwdrivers
Used vibrational tools including a miter saw, reciprocating saw, drill, and nail gun
By the third week, I was starting to feel pain at my right AC joint, my left wrist, and both hands especially my right, dominant hand. Thankfully, despite frequent bending at the waist my lower back wasn’t affected. I attributed the AC join pain to aggravation of the old strain (I rate it a Grade 2 or 3 sprain – partial tearing, but intact). What happened is the heavy lifting placed a repetitious load on that unstable joint, causing the acromion and distal clavicle to aggravate surrounding soft tissues, particularly the supraspinatous tendon, and the insertion points of the ligament. My doctor suggested my pain was impingement syndrome—compression of the supraspinatous tendon where it passes below the acromion– which could be occurring, but I’m certain most of the pain is emanating from the joint itself because I can reproduce the pain simply by pressing it with my fingertip. I’ll tell you how I’m treating this in the next article.
I believe my left wrist pain is a Grade 2 strain of the flexor ulnaris tendon where it inserts into the distal ulnar’s styloid process; caused when I lost control of the auger. The auger is a very powerful machine that requires two people to operate (see picture above). Not being familiar with using one, I wasn’t prepared for the powerful torque it generated, and lost control of it, hurting my wrist.
The third problem that I’m dealing with is trigger finger. This is the first time I’ve had it and let me tell you, it’s not very pleasant.
Trigger finger is so named because as you attempt to straighten out your finger after closing your hand, the finger “catches” mid-way, and pain is felt in one or several joint capsules usually on the palmar side. Then, as you power through the restriction the pain increases and a popping/snapping sensation occurs right before it straightens out, just like how a gun trigger offers gradual resistance then suddenly releases at a point. See the short video below of my actual trigger finger taken this morning that explains this.
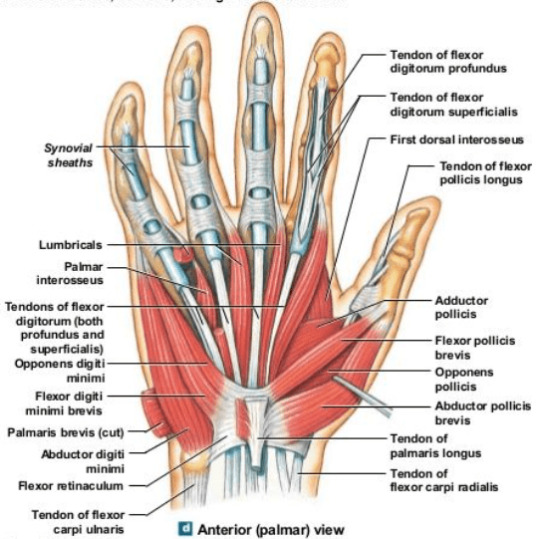
Trigger finger is a stenosing tenosynovitis disorder. Stenosing means narrowing of a passageway in the body; tenosynovitis refers to inflammation of the tendon and synovium. The synovium is a specialized layer of tissue surrounding the tendon in areas where it rubs against other structures in the body. Synovium secretes synovial fluid, a biological lubricant that helps reduce friction where the tendon moves. Synovium also lines the synovial joints of the body which include the hips, knees, shoulders, elbows, spine and joints of the hands and feet.
There are three, main populations of trigger finger sufferers: young children (up to 8 years old); trigger finger as a comorbidity to a primary disease; and adults experiencing trauma/ stress to the hands, typically in the 40s-50s. It tends to affect women more, and the most common finger is the thumb although it can occur in any finger, and in multiple fingers at the same time.
In children, trigger finger is believed to be due to uneven growth rates of the hand flexor tendons and the ligaments, where the tendon growth outpaces the growth of the ligaments that hold them against the finger bones.
Trigger finger is observed to often occur alongside certain other diseases such as carpal tunnel syndrome, diabetes, hypothyroidism, gout, rheumatoid arthritis, and amyloidosis; each probably having different etiologies involving the dysfunction causing the primary disease. Diabetics seem to be affected by trigger finger at a higher rate than the regular population, and it is uncertain why. With diabetes mellitus, there are high levels of glucose in the blood, and usually high insulin levels. Insulin is considered an anabolic hormone associated with tissue growth, so this may be a possible explanation for the increased incidence of trigger finger in diabetics, if the growth leads to tendon hypertrophy (enlargement).
For the third group, which the rest of this article will address, trigger finger is caused by hypertrophy and inflammation of the finger flexor tendons at the synovial sheath, typically from repetitious hand movements, especially those involving power gripping and vibration, making them chafe against the ligaments that hold them down to the finger bones (phalanges). (Remember, ligaments connect two bones, while tendons connect a muscle to a bone; both are components of all moveable joints). Imagine these ligaments as slips of Scotch tape forming a tunnel over the bone. As the hypertrophied (enlarged) section of the tendon enters the narrow tunnel during extension (straightening out of the finger), it gets stuck in that tunnel momentarily; much like how a big person trying to climb out of a small bathroom window can get stuck before being able to make it through. Then, as the tendon makes it past that entrance, it causes the popping sensation.
Orthopedic specialists identify the tendon-ligament structures involved in hand movement as pulleys. Remember from basic physics, a pulley is one of the simple machines (the others being a lever, plane and gear). This is an appropriate name because the tendons and ligaments accomplish work just like the cables and pulleys used in cranes.
Image courtesy of OrthoBullets.com
The A1 pulley is at the metacarpo-phalangeal joint, commonly called the knuckles. It’s where the proximal phalanx connects to the respective metacarpal bone. This is where trigger finger usually occurs. Those who have it here feel the pain and popping/snapping on the palmar side of the knuckle.
The A2 pulley encircles the proximal phalanx, or first finger bone, from the knuckle.
The A3 pulley is at the PIP, or proximal interphalangeal joint—the first joint from the knuckle connecting the proximal and intermediate phalanges (first and second bones of the finger). This is also a common area of trigger finger.
The A4 pulley encircles the intermediate phalanx (second bone of the finger from the knuckle).
The A5 pulley is at the DIP, or distal interphalangeal joint, the furthest joint of the finger connecting the intermediate and distal phalanges (second and third bones of the finger, from the knuckle). Although triggering can happen here, it is less common.
Since the thumb is comprised of only two phalanges, it has an A1 and A2 pulley only. Trigger finger affecting the thumb almost always occurs at the A1 pulley. Unlike the other fingers, your thumb can move in multiple planes, much like the shoulder joint. It has a unique pulley called the oblique pulley that allows it to touch the pinky, a movement called thumb opposition.
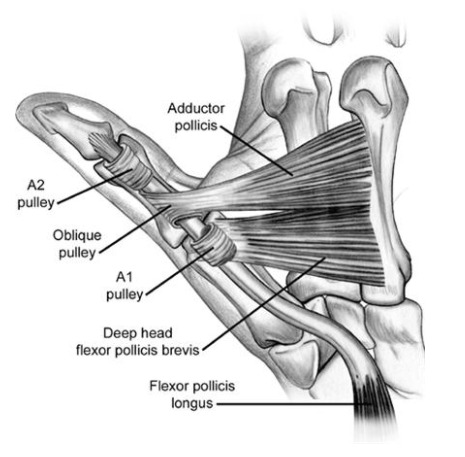
In my case, I have trigger finger in the middle and ring fingers of my right hand, mostly in the A1 and A2 pulley, and less in the A3, with the middle finger being more problematic. Pain is most pronounced in the middle of the night and upon waking, then gets better rather quickly in my case, in the first waking hour of the day. This is because as you sleep, there is less movement of the joints and less synovium produced, causing them to be stiffer.
I have the classic symptom where there is locking of those fingers when I move them from the natural, half-open relaxed hand to fully extending the fingers. As I force them past the locked angle, they snap at the A1 and A2 pulleys, then straighten out. It’s momentarily painful, but tolerable. But for some people, it’s a lot worse. All those weeks of sustained power gripping and twisting caused the flexor tendons and synovium to rub excessively against the ligaments holding them in place, causing microtears and initiating the inflammatory response.
TREATMENT FOR TRIGGER FINGER
The medical standard of care for trigger finger is corticosteroid injection below the affected ligament. This quickly knocks down the inflammation, and in some cases, symptomatic improvement happens within seconds. However, some patients report pain following the injection, and slower or no results.
Splinting is sometimes attempted. The idea is that if you immobilize the tendon, inflammation will stop and the tendon will shrink and heal, bringing things back to normal. However, this is not always the case. Sometimes inflammation takes a life of its own, and prolongs long after the injurious event ceases.
If neither corticosteroid injection nor finger splinting fail to correct the problem, surgery is an option. Direct, open surgery and percutaneous (minimal incision, special surgical tools) surgery are the two options, with direct surgery usually having better results. This is where the ligament is cut to provide more room for the tendon to move. This is possible because the adjacent ligament serves as a backup; for example, the A2 can back up A1 if A1 needs to be cut/ split apart. However, as you can imagine such destruction of a functional component means some strength and stability are sacrificed. I’m sure those having this kind of surgery lose some power in their grip.
MY TREATMENT STRATEGY
As I write this article, my trigger fingers have improved about 75%, from their worst presentation. It could be that my connective tissues are in pretty good shape; my healing capacity is strong; my injury was not very severe; or my treatment regimen is helping accelerate healing. Some sufferers don’t see such a quick pace of resolution.
Here is what I’m doing: as I mentioned, the symptoms are most pronounced in the middle of the night (when I get up to use the bathroom) and upon waking. In the middle of the night, I simply don’t move my fingers, and go back to sleep.
In the morning, I run cold water over my hand for 2 minutes, and gently move my fingers. I get the snapping, but it dissipates shortly after. I still feel some stiffness and soreness in my knuckles throughout the day, but no snapping.
I get localized cryotherapy done on my fingers. Cryotherapy is extremely cold air, as in sub-zero, for 3 minutes. The cold not only slows inflammation, it is said to cause a shock to the sensory nerves, which causes the central nervous system to respond by increasing blood flow, fibroblast activity, and nutrients to the area.
Note: the image above is a localized cryotherapy session on my hand, for a previous complaint. The red dot is not red light therapy; it is a laser thermometer the technician uses to measure my skin temperature so that it doesn’t too low (his hand is visible in the picture). Localized cryotherapy can reach temperatures of -30 degrees F.
Lastly, I apply red light therapy. I’m an advocate of this therapeutic technology and have written articles about it. Red light therapy is actually an electromagnetic waveform (600-880 nanometer wavelengths) that appears red to the human eye. It’s not the red you get from shining a light through a red lens; it’s a specific waveform in the electromagnetic spectrum generated from an LED (light-emitting diode). The device I use uses three LEDs, one of which emits a waveform closer to infrared and therefore does not appear to be red as it is invisible. The electromagnetic energy is at a frequency that gets absorbed by cell mitochondria and other structures, which can result in changed oxidative states that lead to cell signaling that initiates reparative processes, such as increased ATP production and increased membrane permeability. This lessens inflammation and stimulates healing.
I anticipate my trigger fingers to fully recover, to pre-injury status. I will continue to do these therapies, as I feel they are partly responsible for my good results.
BOTTOM LINE
Prevention is the best cure: if you know you are going to be using your hands a lot, such as starting on a do-it-yourself project involving power tools and hard gripping, know that this can cause trigger finger. Do what you can to minimize the stress to your hands—take frequent breaks; don’t overdo it/ don’t hold a power grip for more than a few seconds; and rest and stretch your hands often. Don’t rush it. Trigger finger creeps up on you, and by the time you notice it, it is too late. The presentations are different from person to person, depending on age, health, fitness and so on. I am lucky as my condition is resolving; others are not so lucky and wind up getting surgery and permanent percent loss of hand function. So make sure you keep prevention in mind. If you do get it, try the treatment methods for trigger finger described here that have worked for me.
1 note
·
View note
Link
Dr Mir Asif Rehman is the only Laser Piles/ Bawaeer doctor in Gurgaon & Delhi NCR which uses advanced Diode Laser 1470nm 15W and which is the most advanced & latest technology to treat Hemorrhoids in the world currently.
0 notes
Photo

Laser Piles Treatment or Haemorrhoids Surgery in Gurgaon We at UPHI Hospital providing Advanced Laser Treatment for Piles/haemorrhoids or Bawaseer. UPHI – The Wellness & Surgical Centre is one of the only centers within Delhi NCR which uses Diode Laser 1470nm 15W and which is the most latest & advanced Laser Hemorrhoids Treatment in the world currently. #pilessurgery #pileshospital #laserpilesclinic #gurgaon #golfcourseroadgurgaon #pilesfreegurgaon (at UPHI -The Wellness & Surgical Centre) https://www.instagram.com/p/B43e95Ony_X/?igshid=1vjvbqqwh8t9i
0 notes
Photo

VGM Gastro Centre congratulates the Surgical Gastroenterology Team headed by Dr. Gokul Kruba Shanker for successfully installing the First Lasotronix Diode Laser Machine at VGM Gastro Centre, Coimbatore.
Lasotronix diode laser machine is mainly used for treatment of Piles, Fistula, fissure & pilonidal sinus.
Are you suffering from any of these? A No hospitalization recovery is here!
Benefits of Lasotronix diode laser treatment: 1. Office procedure 2. Lesser discomfort/pain 3. Early recovery and early to work 4. No hospitalization 5. No prolonged follow-up
https://www.vgmgastrocentre.com/
0 notes
Text
Half the Patients with Anal Abscess Develop Anal Fistula
If you are suffering from an anal abscess and are scared that it may lead to some other type of complication, you are right. It would therefore be sensible that you treat the abscess in time, lest it may develop into an anal fistula.
Anal abscess is generally defined as an infected cavity which is filled with pus and found near the rectum or anus. Anal abscess is commonly caused by viral agents & bacteria accumulated due to clogging or possible contamination with fecal matter.
Signs & Symptoms of Anal Abscess
People suffering from anal abscess usually experience swelling, ano-rectal pain & perianal cellulitis which is associated with redness of skin & fever. However, urinary symptoms like hesitancy & difficulty in initiating stream & bleeding are rarely possible.

Diagnosis & Treatment of Anal Abscess
Anal abscess is typically diagnosed through a complete clinical examination. This involves analyzing signs & symptoms and undergoing a physical examination. It will be treated with incision & drainage to be followed by administration of antibiotics. It is possible that improperly incised abscesses may result in fissure formation. Eventually, this can complicate the condition and worsen pain during bowel movement. Conventionally, 2D & 3D endoanal ultrasound scan is considered to be an effective method for diagnosing perirectal abscesses.
What are Anal Fistulas?
Anal fistula is also known as fistula-in-ano. It typically develops as a complication of current or previous anal abscesses due to connection of the infected anal gland to external skin. Almost half of the patients with anal abscesses are found to develop anal fistula as a result. However, anal fistula can also occur without any such prior conditions.
Signs & Symptoms of Anal Fistula
Most often, people affected by anal fistula will have a history of previously drained anal abscesses. These anal abscesses are also associated with symptoms like irritation of perianal skin, drainage from perianal skin, anorectal pain & occasional rectal bleeding. Revealing the horseshoe extension of the abscess usually confirms presence of anal fistula. A CT scan will further delineate the path of the fistula tract.
Treatment Options for Anal Fistula
Presently, effective medical treatments for anal fistula are unavailable. However, surgery until now had been the gold standard intervention for anal fistula prior to arrival of laser treatment.
Fistulotomy – This procedure is usually performed when anal fistula is straightforward & involves minimal degree of sphincter muscle. Fistulotomy operation involves unroofing of the fistula tract. This is meant to connect the internal opening within anal canal to the external opening. Eventually, this will create a groove in order to improve the process of healing from inside out. Dissection & removal of the entire fistula tract is most effective & involves less chances of recurrence. However, this needs to be done very carefully because there are chances that the patient may end up having fecal incontinence resulting from damage to the anal sphincter muscle being divided during the course of surgery.
Laser Treatment – This is the latest addition to treatment for anal fistula. Laser treatment for anal fistula is a novel anal sphincter-saving method which is performed using laser diode. It is a safe, effective & minimally invasive procedure. Primary closure of the anal fistula tract is achieved by a radial fiber connected to the diode releasing laser energy. This effectively results in shrinking of the surrounding tissue & thereby closing the anal fistula tract.
Laser Piles Clinic in Hyderabad
Laser Piles Clinic in Hyderabad is one of the best places to undergo the most advanced FDA approved laser treatment for anal fistula. There is no need of dressing after treatment & patients can walk out of the clinic the same day. This is a knifeless treatment which involves no cutting & patients can get back to work the very next day. Doctors at Laser Piles Clinics in Hyderabad are some of the best & adept at performing successful operations on the most complicated anal fistula cases. Moreover, lady doctors are also available at Laser Piles Clinics for treatment of female patients.
0 notes