#decubitus
Explore tagged Tumblr posts
Text
Pressure sores are a well-known complication of decubitus, but they are not the only⚡!
Bedsores are a well-known complication of decubitus, but they're not the only one. Decubitus can affect many systems in the body, including the urinary and digestive systems.
Bedsores, or pressure sores, are skin lesions that appear in bedridden or immobilized people. They can lead to serious complications if not treated promptly.
What are the complications?
- Local and generalized infections: Pressure sores are ideal breeding grounds for bacteria, which can lead to serious infection or even septicemia.
- Intense pain: Pressure sores are often very painful, with a considerable impact on quality of life.
- Slower healing: Certain medical conditions, such as diabetes or malnutrition, can slow the healing of pressure sores.
- Risk of tissue necrosis: In the most severe cases, tissue can die, requiring complex care and sometimes surgery.
- Systemic complications: Pressure sores can lead to more general problems such as fever, dehydration and nutritional disorders.
How to prevent bedsores?
- Change position regularly: Every 2 hours or so to relieve pressure on at-risk areas.
- Skin care: Moisturize the skin, avoid rubbing and irritation.
- Use preventive devices: Anti-bedsore mattresses, cushions, etc.
- Good nutrition: A balanced diet promotes healing.
Other decubitus-related complications in addition to pressure sores:
- Urinary disorders
o Urinary tract infections: Immobility promotes urine stagnation, increasing the risk of infection.
o Incontinence: Difficulty getting up to go to the bathroom can lead to urinary incontinence.
o Urinary retention: Urinary retention may occur, particularly in people with difficulty urinating.
- Digestive disorders
o Constipation: Lack of physical activity and an inadequate diet can cause constipation.
o Fecal incontinence: Bedridden patients may lose control of their anal sphincters.
o Swallowing disorders: Difficulty swallowing may occur, increasing the risk of pneumonia.
- Other complications
o Venous thrombosis: Immobility promotes the formation of blood clots in the veins, increasing the risk of pulmonary embolism.
o Muscular atrophy: Lack of physical activity leads to loss of muscle mass.
o o Bone disorders: Osteoporosis and fractures are more common in bedridden people.
o Psychological disorders: Isolation, pain and dependence can lead to depression and anxiety.
Why do these complications arise?
Prolonged immobility leads to reduced blood circulation, impaired tissue nutrition and lowered immune defenses. These factors favor the onset of complications.
How can these complications be prevented? In addition to preventing pressure sores (regular changes of position, skin care, etc.), it is important to :
- Maintain good hydration.
- Eat a balanced diet rich in fiber.
- Encourage passive and active patient mobilization wherever possible.
- Implement urinary tract infection prevention programs.
- Regularly monitor the patient's nutritional and fluid status.
In conclusion, decubitus is a complex problem requiring comprehensive patient management. Careful prevention and monitoring can limit complications and improve quality of life.
Go further
0 notes
Text
What is a bedsores?
A decubitus, also known as a bedsore or pressure ulcer, is an injury that affects the skin and underlying tissues. It usually develops over bony areas due to prolonged pressure, friction, or shear forces. Here are some key points regarding decubitus: Causes of decubitus: Prolonged pressure: Continuous pressure on the skin compresses the blood vessels and reduces blood flow, causing tissue…
View On WordPress
0 notes
Text
opened the page on bedsores on wikipedia and. deeply regret
0 notes
Text
https://sparktv.net/read-blog/39447_decubitus-ulcer-treatment-products-market-analysis-size-share-and-forecast-2031.html
The Decubitus Ulcer Treatment Products Market in 2023 is US$ 4.9 billion, and is expected to reach US$ 7.65 billion by 2031 at a CAGR of 5.72%.
#Decubitus Ulcer Treatment Products Market#Decubitus Ulcer Treatment Products Market Analysis#Decubitus Ulcer Treatment Products Market Forecast
0 notes
Text
Meeting the Needs of a Growing Population: The Evolving Global Decubitus Ulcer Treatment Products
Global decubitus ulcer treatment products market is anticipated to reach US$ 4,989.4 million globally in 2023 and is predicted to expand at a compound yearly growth rate of 5.5% to reach US$ 8,503.4 million in 2033. The market for decubitus ulcer treatment solutions is believed to be growing due to a rise in the senior population with disabilities. Decubitus ulcers are sometimes known as bed sores or pressure sores. Decubitus ulcers are open sores on the skin covering the bone areas of the body. They are brought on by chronic pressure that is unrelievable due to inadequate blood circulation and flow. Moreover, it may be exacerbated by fecal or urine incontinence, friction between the skin and another surface, and excessive moisture from sweating.
Unlock Advanced Analysis With Your Report Sample: https://www.futuremarketinsights.com/reports/sample/rep-gb-1438
Combating Pressure Injuries: Decubitus Ulcer Treatment Offers Relief and Improved Care
The global decubitus ulcer treatment product market is experiencing steady growth, driven by the rising need for effective solutions to manage pressure injuries. Decubitus ulcers, also known as bed sores or pressure sores, are open wounds caused by prolonged pressure on the skin. These can develop in individuals with limited mobility or those who spend extended periods lying down.
Understanding Decubitus Ulcers and Treatment Options
Decubitus ulcers can be caused by various factors, including:
Constant Pressure: Unrelieved pressure on bony areas like the heels, tailbone, and hips can restrict blood flow and damage skin tissue.
Friction: Friction between the skin and bedsheets or other surfaces can contribute to ulcer formation.
Moisture: Excessive sweat, urine, or fecal incontinence can create a moist environment that weakens the skin.
The decubitus ulcer treatment market offers a variety of products to help prevent and manage these wounds, including:
Support Surfaces: Specialty mattresses and cushions designed to redistribute pressure.
Dressings: Advanced wound dressings to promote healing and manage moisture.
Skin Care Products: Lotions and cleansers to protect the skin from breakdown.
Key Takeaways:
The global decubitus ulcer treatment products market is expected to reach US$8,503.4 million by 2033, reflecting a rise from US$4,989.4 million in 2023.
This growth is projected at a consistent compound annual growth rate (CAGR) of 5.5% throughout the forecast period.
The aging population and increasing focus on pressure injury prevention are key drivers for market expansion.
Market Competition:
Some of the key participants present in the global Decubitus Ulcer Treatment Products market include Mölnlycke Health Care AB, ConvaTec Group Plc., B. Braun Melsungen AG, Coloplast Corp., Smith & Nephew, 3M, Integra LifeSciences Corporation, Cardinal Health, and Tissue Regenix, among others.
Due to the presence of such a high number of participants, the market is highly competitive. While global players such as Mölnlycke Health Care AB, ConvaTec Group Plc., B. Braun Melsungen AG, Coloplast Corp., and Smith & Nephew account for a considerable market size, several regional-level players are also operating across key growth regions, particularly in North America.
Recent Developments
In June 2020, MBET Health announced the launch of a proactive solution, the Miracle Dressing Wound Care System (MDS), specially developed for the strong surge of pressure injuries, such as pressure ulcers, due to the enforced confinements caused by the COVID-19 lockdowns. The product is the first and only 21-day stay-in-place dressing and prevents pressure sores.
In April 2020, AxioBiosolutions announced the launch of MaxioCel, a next-generation wound care dressing made of chitosan to treat pressure ulcers. The product imparts 360-degree care with pain management, hemostatic, pain, and scar improvement properties.
In March 2020, Smith & Nephew announced the United States. Launch of their new offering of the PICO 14 Single Use Negative Pressure Wound Therapy System (sNPWT), which has a pump duration of up to 14 days. The new pump enhances the features and benefits of the previous generations of PICO sNPWT products and comes with an enhanced pump that requires less user intervention.
Key Companies Profiled:
Hill-Rom Company Inc.
Graham Field Health Products Inc.
Invacare Corporation
Sunrise Medical Inc.
ROHO Inc.
Kinetic Concepts Inc.
Span-America Medical Systems Inc.
Spenco Medical Corp
Cardinal Health
Smith & Nephew
Key Segments Profiled in the Decubitus Ulcer Treatment Products Industry Survey:
By Depth of Soft Tissue Damage:
Stage I
Stage II
Stage III
Stage IV
By Distribution Channel:
Hospitals Clinics
Public Hospitals
Private Clinics
Retail Pharmacies and Drug Stores
E-commerce
By Region:
North America
Europe
Latin America
Asia Pacific
Middle East & Africa
0 notes
Text
The Wish Clinic is a leading center for diabetic wound healing, providing state-of-the-art treatments and compassionate care. Our expert team is dedicated to helping patients with diabetes achieve faster wound healing, preventing complications, and enhancing their overall well-being. Choose The Wish Clinic for exceptional diabetic wound care and a path to a healthier, more comfortable life. Trust The Wish Clinic for effective pressure ulcer treatments and a path to recovery.
#diabetes and wound healing#decubitus pressure ulcer#pressure ulcer treatment#diabetic wound#diabetic wound treatment#diabetic foot care
0 notes
Text
OPTIMAL FREQUENCIES FOR COMMON HEALTH CONDITIONS
Condition / Symptom / Disease w.
Optimal Frequency / Range listed alphabetically.
Acne: 10 – 15 Hz
Allergies: 5 - 10 Hz
Alzheimer’s Disease: 2 - 8 Hz
Arrhythmia: 7 - 8 Hz
Angina: 2 - 8 Hz
Arteriosclerosis: 7 - 10 Hz
Asthma: 7 - 10 or 12 - 15 Hz
Anxiety: 2 – 8 Hz
Bronchitis... Acute - 4 Hz, Chronic - 12 Hz
Bruises: 10- 14 Hz
Carpal tunnel syndrome: 6 or 20 Hz
Cervical Vertebra Pain: 15 – 20 Hz
Chronic blepharitis: 1 - 2 Hz
Chronic pelvic pain: 5 - 7 Hz
Circulatory dysfunction: 7 - 10 Hz
Constipation: 5 Hz
Crohn’s Disease: 12 - 22 Hz
Cystitis: 5 - 8 Hz
Dental and oral diseases: 30 Hz
Depression: 3 or 20 Hz
Diabetes: 12 - 22 Hz
Dizziness: 10 – 15 Hz
Eczema: 10 – 15 Hz
Erectile Dysfunction: 6 Hz
Fibromyalgia: 18 Hz
Fractures: 10 or 20 Hz
Frozen shoulder: 7 - 8 Hz
Glaucoma, atrophy of the optic nerve: 12 - 22 Hz
Headache: 3 or 6 - 10 Hz
Hepatitis: 12 - 22 Hz
Herniated disc: 16 - 20 or 30 Hz
Hyperactivity: 20 Hz
High blood pressure: 1 - 5 Hz
Immune system enhancement: 24 Hz
Joint dislocations and sprains: 10 Hz
Ligament injuries: 10 - 15 Hz
Low blood pressure: 20 – 24 Hz
Lumbago: 10 or 20 Hz
Lymphatic disorders: 12 - 22 Hz
Menopause: 5 – 8 Hz
Menstrual pain: 5 - 7 Hz
Migraines: 4 – 10 Hz
Multiple Sclerosis: 5, 13 or 20 Hz
Muscles strains: 11 - 15 Hz
Musculoskeletal pain: 10 Hz
Nerve pain or neuropathy: 6 Hz
Neuralgia Trigemini: 15 – 20 Hz
Neurodermatitis: 10 – 15 Hz
Nonunion fractures: 10 or 20 Hz
Osteoarthritis: 8 - 12 or 18 Hz
Osteonecrosis/osteochondrosis: 10 or 19 - 20 Hz
Osteoporosis: 8 - 10 or 15 - 19 Hz
Pain from wound healing: 11 - 15 or 17 Hz
Parkinson’s Disease: 20 Hz
Periostitis: 6 Hz
Phantom pain: 16 - 19 Hz
Poor circulation: 2 - 6 or 20 Hz
Prostatitis: 3 - 8 Hz
Psoriasis: 12 - 22 Hz
Psoriatic arthritis: 12 - 22 Hz
Psychosomatic Syndrome: 22 Hz
Raynaud’s Syndrome: 15 Hz
Respiratory diseases: 12 - 22 Hz
Rheumatoid Arthritis: 10 or 20 Hz
Sciatica: 16 - 20 Hz
Skin Allergies, Decubitus, Ulcus Cruris: 10 – 15 Hz
Sleep disorders: 1 - 5 Hz
Spinal injuries: 12 - 22 Hz
Stomach aches: 10 Hz
Stress: 3 or 5 Hz
Stroke: 7 - 10 or 20 Hz
Swelling (Edema): 10 Hz
Systemic Lupus Erythemasosus (SLE): 12 - 22 Hz
Tendinitis: 8 Hz
Tinnitus: 10 Hz
Tuberculosis (TB): 4 Hz
Wound healing: 1 - 5 Hz
What have you got to lose to try it? ����
#pay attention#educate yourselves#educate yourself#reeducate yourselves#knowledge is power#reeducate yourself#think about it#think for yourselves#think for yourself#do your homework#do your research#do your own research#do some research#ask yourself questions#question everything#frequencies#healing frequencies#government lies#government secrets#government corruption#hidden history#hidden secrets#history lesson#history#spiritual healing#self improvement#news#you decide
179 notes
·
View notes
Text
The Rhythm of the Night
This one was recorded a few weeks ago. I was sharing with a special close friend as I fell asleep. I drifted in and out of consciousness over this rec, occasionally waking up to comments about her starting to speed up or pound. I don’t know what it is, but there’s something so comforting about knowing someone on the other side of the world is listening my heart beating… especially when I trust them enough when I’m not conscious.
Apologies for any background sound - I was listening to a podcast as I fell asleep so that might have come through. I also used the cardio instead of the classic which oddly isn’t the best for sleep beats.
Steth - Cardio IV
Location - Erbs / Tri / somewhere there
Position - Left Lateral Decubitus (laying on my side)
#cardiophile#cardiophilia#female heartbeat#heartbeat#beating heart#self stething#pounding heart#stethoscope#heartbeats#sleep beats#heart beating#female cardiophile
64 notes
·
View notes
Text
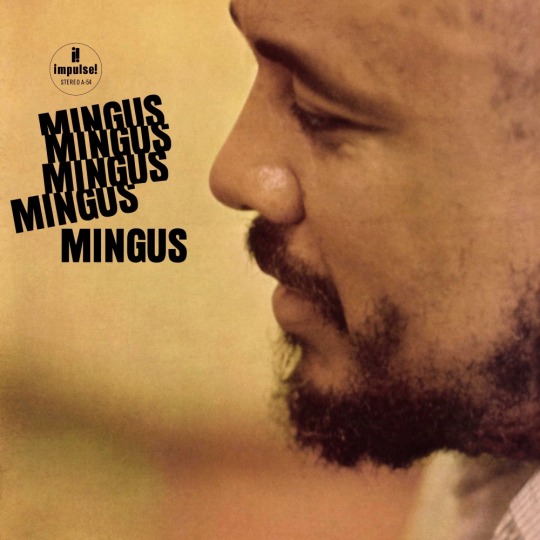
Tracklist:
II B.S. • I X Love • Celia • Mood Indigo • Better Get Hit In Yo' Soul • Theme For Lester Young • Hora Decubitus
Spotify ♪ YouTube
#hyltta-polls#polls#artist: charles mingus#language: instrumental#language: english#decade: 1960s#Post-Bop#Hard Bop#Third Stream
23 notes
·
View notes
Text
Les escarres sont une complication bien connue du décubitus, mais elles ne sont pas les seules⚡ !
Les escarres sont une complication bien connue du décubitus, mais elles ne sont pas les seules. Le décubitus peut avoir des répercussions sur de nombreux systèmes de l'organisme, notamment l'appareil urinaire et digestif.
Les escarres, ou plaies de pression, sont des lésions cutanées qui apparaissent chez les personnes alitées ou immobilisées. Elles peuvent entraîner de graves complications si elles ne sont pas prises en charge rapidement.
Quelles sont les complications ?
Infections locales et généralisées : Les escarres sont des portes d'entrée pour les bactéries, pouvant mener à des infections graves, voire à une septicémie.
Douleurs intenses : Les escarres sont souvent très douloureuses, impactant considérablement la qualité de vie des personnes concernées.
Ralentissement de la cicatrisation : Certaines conditions médicales, comme le diabète ou la malnutrition, peuvent ralentir la guérison des escarres.
Risque de nécrose tissulaire : Dans les cas les plus graves, les tissus peuvent mourir, nécessitant des soins complexes et parfois la chirurgie.
Complications systémiques : Les escarres peuvent entraîner des problèmes plus généraux comme la fièvre, la déshydratation, et des troubles nutritionnels.
Comment prévenir les escarres ?
Changer régulièrement de position : Tous les 2h environ pour soulager la pression sur les zones à risque.
Soigner la peau : Hydrater la peau, éviter les frottements et les irritations.
Utiliser des dispositifs de prévention : Matelas anti-escarres, coussins, etc.
Une bonne nutrition : Une alimentation équilibrée favorise la cicatrisation.
Les autres complications liées au décubitus, en plus des escarres :
Troubles urinaires :
Infections urinaires: L'immobilité favorise la stagnation de l'urine, augmentant ainsi le risque d'infections.
Incontinence: La difficulté à se lever pour aller aux toilettes peut entraîner de l'incontinence urinaire.
Rétention urinaire: Une rétention urinaire peut survenir, notamment chez les personnes ayant des difficultés à uriner.
Troubles digestifs:
Constipation: Le manque d'activité physique et une alimentation inadaptée peuvent provoquer de la constipation.
Incontinence fécale: Les personnes alitées peuvent perdre le contrôle de leurs sphincters anaux.
Troubles de la déglutition: Des difficultés à avaler peuvent apparaître, augmentant le risque de pneumonie.
Autres complications:
Thromboses veineuses: L'immobilité favorise la formation de caillots sanguins dans les veines, augmentant le risque d'embolie pulmonaire.
Atrophie musculaire: Le manque d'activité physique entraîne une perte de masse musculaire.
Troubles osseux: L'ostéoporose et les fractures sont plus fréquentes chez les personnes alitées.
Troubles psychologiques: L'isolement, la douleur et la dépendance peuvent entraîner de la dépression et de l'anxiété.
Pourquoi ces complications surviennent-elles ?
L'immobilité prolongée entraîne une diminution de la circulation sanguine, une altération de la nutrition des tissus et une diminution des défenses immunitaires. Ces facteurs favorisent l'apparition de complications.
Comment prévenir ces complications ? Outre la prévention des escarres (changements de position réguliers, soins de la peau, etc.), il est important de :
Maintenir une bonne hydratation.
Avoir une alimentation équilibrée et riche en fibres.
Encourager la mobilisation passive et active du patient dans la mesure du possible.
Mettre en place des programmes de prévention des infections urinaires.
Surveiller régulièrement l'état nutritionnel et hydrique du patient.
En conclusion, le décubitus est une problématique complexe qui nécessite une prise en charge globale du patient. Une prévention rigoureuse et une surveillance attentive permettent de limiter les complications et d'améliorer la qualité de vie des personnes concernées.
Aller plus loin
0 notes
Note
Hello hello, your New fic really got me ...its a super interesting Idea.
Luci in the first chapter ... I love how i hate him , its really canon typical behavior and it's great!
The second chapter leaves me so damn uncomfortable and I love that !
As I worked as a qualified nurse I have a really vivid Images of Alastor being in coma and hope Dr. White is knowing what He is doing ...and I am wondering who is taking Care of Al and all the medical devices, for example emptying the catheter bag and changing diapers , as Well as changing the positioning to avoid the risk of decubitus .
Or does He have any inhuman Powers left in His Body ? In any Case Alastor will feel humiliatied ...
I am so looking forward what will happen!
Again : you are indeed an admirable soul!!!
I haven't decided how detailed I want to get in reference to Al's coma. I have a tendency to go down rabbit holes and get carried away, and I don't want to wind up concentrating too much on medical details instead of the characters themselves. For example, I went to start some research on bed sores and suddenly it was 5 hours later and I was surrounded by case studies and brutal photos of the aftermath of poor medical care. (You can see clear through to some people's spines!) Anyway, I have to be careful where I aim my focus because I get carried away pretty easily, lol. In The Metamorphosis, Luci is handling Al's medical requirements with the support of in-home visits from Dr. White. There is still some residual Hell magic at play, or else Al wouldn't have survived at all; so that does help his recovery also.
I won't keep him in the coma for too long. I just needed to emphasize how much his situation has changed, and I wanted the rest of the hotel crew to understand the severity of it *first*, because we all know Al would downplay it for as long as possible :)
2 notes
·
View notes
Text
Blog 22 MediReva day
Hello everyone,
Today I (Sarah) like to tell you about a Healthcare Technology Day organised by MediReva. MediReva is a medical specialty store, which supplies medical devices and care materials for diabetes, wounds, stoma, incontinence, nutrition and rehabilitation care. MediReva was founded in 1979 by the couple Pierre and Tineke Gubbels, with the ambition to make the lives of (chronically) ill people more pleasant. They where a small company in the south of the Netherlands and now they are a well known company. The MediReva day is a day for the different health care professionals that use the services of MediReva and the advicers. On the day their where different guest speakers that provided new information about important subjects. Than there were also different companies that presented there (new) health care technologies. You could test out the different products and ask questions.
Van Raam is a company that makes unique adapted bicycles for people with disabilities. The different bicycles are tricycles, mobility scooter bicycles, wheelchair bicycles, tandems, side-by-side tandems, wheelchair transport bicycles and low entry bicycles or comfort bicycles.
Invacare is a company that makes different wheelchairs with or without elektric auxiliary driving. You could test out all these wheelchairs and get information about the different options.
There was also a companies that had different Anti-decubitus cushions that help to prevent sores. One cushion is called the ROHO and it has different cells that get filled with air by a hand pump. Another is called Vicair and is filled with tiny triangles filled with air.
It was fun and interesting to test all the products and learn more about how they work. With the information I got I can help my future clients.
I hope you found my story of the Medireva day interesting.
Till next time!
Sarah
4 notes
·
View notes
Text
Pathogen assigned: Porphyromonas uenonis
Cause of sacral decubitus ulcer, type of gram negative bacteria

(Image from here)
Spread via: Found in human micro biome? (Unclear)
#shrimpblr#human pathogens#gimmick blog#bacteria#cells#biology#microbiology#These guys are also obligate anaerobes#I just think that's cool
12K notes
·
View notes
Text
https://twikkers.nl/blogs/265748/Decubitus-Ulcer-Treatment-Products-Market-Analysis-Size-Share-and-Forecast
The Decubitus Ulcer Treatment Products Market in 2023 is US$ 4.9 billion, and is expected to reach US$ 7.65 billion by 2031 at a CAGR of 5.72%.
#Decubitus Ulcer Treatment Products Market#Decubitus Ulcer Treatment Products Market Forecast#Decubitus Ulcer Treatment Products Market Analysis
0 notes
Text
Technology in Nursing History of technology and its influence on nursing There is now a great influence on the impact of technology on the practice of nursing and if the well-known behavior scientists like Abraham Maslow had been around and invited to give his opinions regarding influence of technology on human life, he may not have considered technology as being essential for the existence of human lives. This is clear from the fact that humans lived prior to the discovery of cell phones, e-mail, fax machines or even the Internet. The important point for us to consider is whether there is such a high importance for these technology for human existence. The use of technology is often made so that we are able to get new and innovative strategies so that patient care delivery is improved. The attempt is now often to seek technological solutions for the nurses to be able to operate more effectively and continue with their jobs. (Richard, 2004) This can be seen in many areas and if the medication is not being delivered in the system of the patient properly, there is use of bar coding of the medicine to ensure that medicines reach the patient properly. When we notice some other problems like the patients falling off from the beds, then there are bed alarms that are installed so that the quality of nursing improves. In other diseases like decubitus ulcer, the solution that is sought most often is to get high-tech patient beds to reduce the chances of skin breakdown of the patients. These sorts of examples may certainly be considered to be the correct uses of technology so that the patients can be helped in the best possible way. At the same time, these changes should not be viewed as some sort of a magic to solve the problems of patients, but should be treated as methods to solve the problems of patients. (Richard, 2004) The use of technology is very useful even in solving the problems of shortage for nurses that we have now. The president of American Hospital Association, Dick Davidson has states that America needs another 126,000 nurses right now apart from a large number of pharmacists, lab technicians, support staff and other individuals. He has also invited for immediate action to be taken to solve these problems. The problems can be solved to some extent through the use of clinical information systems and provide a lot more confidence to the nurses. These systems will stop medical errors, streamline workflow and communications, reduce unnecessary entry of data and the total effect can be thus lasting and positive. We have a shortage of trained manpower and certainly these machines can help in that regard. (Meadows, 2002) The development and usage of technology for nurses has started from the middle of their courses and they have computer assisted instruction along with the knowledge of development of humans, knowledge about Internet, and learning about development of program development. (Siktberg; Dillard, 1999) At the same time, there seems to be a lot of interest in the study of development of nursing through the impacts of scientific influences. One study was to know about the result of phenomenon so that one could find out the qualitatively various methods by which technology is understood and experienced by nurses of the present period. (Barnard; Gerber, 1999) There have also been qualitative studies which examined ways of understanding technology in surgical nursing and examine the implications that this technology has for nursing and health care practices. (Barnard, 2000) There have also been online surveys of the technological capacities of U.S. undergraduate programs and the results were that most of the nurses were using Microsoft Windows-based computers and Microsoft Office software for their use. (Wells; Wilkie; Brown; Corless; Farber; Judge K; Shannon, 2003) Some of these studies are probably studies for the sake of studies as they are not likely to lead to any benefits for the patients or nurses. After all it is well-known today that almost everybody is compelled to use Microsoft programs for computers as nothing else practically exists. At the same time, there is no doubt that some types of technology are helping the development of nursing techniques and storages. One of them is the improvement of mobile technology and this is on the way to create mobile health systems. The changes are due to increases of availability, miniaturization, performance and cost effective bandwidth. These developments are likely to deliver cost effective technologies which will in the end improve the delivery of care by the health care organizations. Some other changes have already taken place through picture archiving and communication systems and these have practically made the radiological film practically out of date. (Simpson, 2003) The new system permits users to acquire, store, transmit and display images digitally and the end result is a clinical environment where there are no films. Another important system is the computerized provider order entry and these are designed to find out and stop medical errors during the process of treatment at the earliest possible point. When this system is installed, the person providing the medicines enter the orders into a computer and then the computer itself checks the order. It is able to find out incorrect dosages and drugs, drug allergy interactions, interactions between different drugs, and many other possible errors. The system is able to improve the process of treatment through ensuring that the right drug is administered, at the right time and also inform others if the condition of the patient changes. (Simpson, 2003) It is most important that tools of technology are used to increase interactions between different human elements in the process of treatment. The impact of technology is on the way that care is delivered to the patients, and also that the correct treatment is given at the correct time. Technology is not a substitute for care but only a supplement that will improve the quality of care. Remember it is the patient who is the most important in the entire issue for the use of correct technology. (Richard, 2004) How have the values and beliefs of nurses and other healthcare providers influenced the evolution and usage technology in nursing? It is difficult to judge the acceptance of new technology among any group except through their reactions to the change that it causes. As we know very well, the change that is caused through any change in technology will cause changes in work schedules and other matters for nurses. Let us look at the studies of an individual who had been studying the employment mobility among nurses and find out the reasons for it. The important point is not only to find out how often they change jobs, but also their individual reasons for changing of jobs. The important matter of this study was that there was a study which considered not only a shift from one institution to another institution as a nurse, but also within the same organization as a nurse in different areas. (Nursing profession studied) What this means is the shift of a nurse from the operating room to a palliative care nurse. The jobs are different and the initial study did not indicate a high degree of shifts within the nursing profession, but when studies the total data comprehensively, it is seen that there is quite a rapid shift of nurses. The latest available data available in this study is for 1991-92 and it shows that within a one year period, there were shifts in the employment status of 12 to 15% of the nurses. The change could have been for any reason like status of employment, place or setting or even the type or position. This makes it clear that during a period of one year, roughly about a third of the nurses change their job, at least in terms of characteristics. (Nursing profession studied) Thus there is a fairly rapid turnover of nurses and the net important question is to find out the reasons for change. In more than 90% of the cases, the nurses clearly stated that they had left their jobs voluntarily, and the proportion is more than 90%. Only in about three percent of the cases, the reasons for change was mutual between the nurse and the employer and in two percent of the cases, the nurse had been dismissed from their jobs. Clearly there is no desire among employers to dismiss nurses, since costs are involved in recruiting nurses, training the nursing staff and these costs are substantial for a hospital. Thus in spite of all the technical changes that have been going on, the reactions among the nursing staff is not very aggressive. There are some reasons for changing jobs that the nurse cannot avoid - like the shift of the spouse to another city on a job. This sort of a case also cannot be influenced by the hospital administrators. It is only when the nurses leave due to working conditions, it is clear that either the nurses are not able to match up to the changes, or the behavior of the hospital is not suitable. (Nursing profession studied) This is clearly not very high, and there does not seem to be a high impact of the change in technology on nurses and their employment. This leads to a dichotomy in the view about nurses - they are viewed as targets of change rather than the force which leads to changes through proposals, leadership and implementation. This often causes them difficulty in carrying on with their jobs when there are rapid changes within the organization. To save their own position, it is important that nurses learn about change theory, change strategies and methods of anticipation and managing change. This may take place in organizations which wants to change its staff mix so that it can save on costs through inclusion of more unlicensed assistive personnel. These personnel will generally try to maintain their position through direct assertion, but there have to be an analysis of the driving and restraining forces before any decision is finally taken. (The Power of Change) The driving reasons for the proposed change may be an increase in patient care hours that the hospital has to face, decreased charges that can be levied, elimination of non-professional tasks that are carried out by the registered nurses and additional time that has to be spent by them for teaching patients and their families. On the other side, there may be restrictions due to the lack of control over care for patients, concerns and worries about the supervision of unlicensed staff, the desire of maintaining the present situation and getting into any changes, and the conflict between the new staff and the old. Their may be conflicts in many cases between the new group and the old group, and the group planning the change may have their own views. These generally lead to a halt to the entire process till the conflicts are resolved. This is also the situation when the process of education and usage of technology among nurses start in any organization. In general the policy adopted is to have a strategy of re-education so that creativity is stimulated and resistance is reduced. At the same time, the process involves more time for the change and a resultant higher cost. In a certain instance this situation was faced by two nurse managers. One of them adopted a policy of directly telling the staff about the change and the positive effects the change will bring within the organization. The feelings of the staff were not taken care of and this resulted in a near rebellion of the staff when the implementation dates and new staffing plans were put up. The entire group wanted to resign. Another manager had the same problem and selected a normative re-educative strategy. When the changes were introduced, he wanted to know from the staff their reactions. The opinions of the staff were listened to and further suggestions were made by the manager so that the problems of the staff were attended to. (The Power of Change) The problems of the staff are quite easy to understand. A nurse may have developed competence with an existing documentation system, but have to start again when a computerized documentation system is introduced. There are many reasons for resistance to change - poor timing of the change, fear of loss of control, lack of trust, comfort with the existing situation, less certainty about the effects of change and the feeling that there will be extra efforts required to meet the change. At the same time, the nurse are capable of solving problems of changes and in a hospital in Wisconsin a nurse changed the frequency and timing of activated clotting time for patients with a particular type of coronary intervention. The result was a savings to the hospital of $5,000 in nursing time. (The Power of Change) Thus the introduction of changes based on technology has to be introduced in collaboration with the group which is going to implement the concept. References Barnard, Alan; Gerber, Rod. (September 1999) "Understanding Technology in Contemporary Surgical Nursing: A Phenomenographic Examination" Nursing Inquiry. Vol: 6; No: 3; p. 157. Barnard, Alan. (May 2000) "Alteration to Will as an Experience of Technology and Nursing" Journal of Advanced Nursing. Vol: 31, No: 5; pp. 1136-1144 Habel, Maureen. "The Power of Change" Retrieved at http://www2.nursingspectrum.com/ce/self-study_modules/course.html?ID=544&PageNum=3&Begin=11184. Accessed 10 September, 2005 Meadows, G. (Jan-Feb, 2002) "The Nursing Shortage: Can Information Technology Help?" Nursing Economics. Vol: 20; No: 1; pp: 46-48. Nursing Profession Studied" Retrieved at http://www.newsrelease.uwaterloo.ca/archive/news.php?id=142. Accessed 10 September, 2005 Richard, Hader. (December, 2004) "Technology Useful only with Human Touch" Nursing Management. Vol: 18; No: 1; pp: 73-77 Siktberg, L. L; Dillard, N.L. (May-June 1999) "Technology in the Nursing Classroom" Nurse Health Care Perspective. Vol: 20; No: 3; pp: 128-133. Simpson, Roy. L. (December, 2003) "Today's Challenges Shape Tomorrow's Technology, Part 2" Nursing Management. Vol: 16; No: 1; pp: 52-55. Wells, M. J; Wilkie, D. J; Brown, M. A; Corless, I. B; Farber, S. J; Judge, M. K; Shannon, S. E. (Jan-Feb, 2003) "Technology Survey of Nursing Programs: Implications for Electronic end-of-life Teaching Tool Development" Computer Information Nursing. Vol: 21; No: 1; pp: 29-36 Read the full article
0 notes