#congenital hydrocephalus
Explore tagged Tumblr posts
Text
Find Me Friday: Theo, Phil, Vincent, & Eddie!
Logo that says Reece’s Rainbow Special Needs Adoption Support in blue, below a blue & yellow paint stroke rainbow graphic with a yellow Ukrainian trident symbol on the right half. In this series, each Friday I’m able, I want to share a different child or group of children who are available for adoption and listed through the adoption advocacy website Reece’s Rainbow. Please note, names used on…

View On WordPress
#accessible post#adoption advocacy#asthma#available for adoption#available to large families#available to married couples#available to older parents#available to single parents#bronchopulmonary dysplasia#cognitive delay#congenital STD#cortical blindness#Eastern Europe adoption#education#Edwards syndrome#esophogeal atresia#Find Me Friday#FSP#g-tube#gastric reflux#heart defect#hydrocephalus#low birth weight#medical history#Phil#photo descriptions#polymalformative syndrome#premature birth#psychomotor delay#Reece&039;s Rainbow
0 notes
Text
I have personally witnessed so many instances of pet owners forcing beloved animals to continue living far beyond the point of their quality of life hitting zero that the whole "Deux Face" situation was absolutely nothing new to me, except for the wave of genuine nausea I experienced at the social media reaction to her existence.
I can honestly say that I feel a palpable sense of relief, knowing that that calf is no longer being forced to live in that condition, and there's no amount of "well, she had vet care!" or "it doesn't seem like she's in pain!" that would have mollified me. I have been in hundreds of QoL consults with clients who parrot the exact same sentiments while their animal lies, completely recumbent and unresponsive, on the examination table. It's the exact same thing, except compounded by the ghoulish addition of the calf's value as a sideshow act.
Any normal presenting newborn calf that failed to thrive as she did would have been euthanized on welfare grounds long before the 26 day mark. A dairy calf is literally supposed to be able to walk away from its birthing site, a calf whose only developmental milestone was that it "can kinda lift its head" is a calf that has something inherently wrong with it. If Deux Face wasn't deformed in a way that makes well-meaning assholes spout that stupid poem, then she probably would have been put out of her misery ages ago. I keep thinking of the grotesque congenital deformities that domestic cattle can present with, twisted spines and fused joints and extreme hydrocephalus and cleft palates, and how, if Deux Face had presented with QoL reducing examples of any of those conditions, people wouldn't have even batted an eye at her euthanasia. She was literally forced to keep on living, just so people could keep "consuming" her continued existence. She was forced to live, not because it was to her benefit, but for the benefit of the farm, who romanticised and profited from her, and the benefit of idiots who think a goddamn newborn calf should be a source of inspiration in their own lives.
The people on this site who mourned that we didn't get to gawk at this animal a little longer disgust me. The only difference between you and the woman who keeps her 19 year old constant DKA, cushingoid, and severely arthritic Shih Tzu alive is that she, at least, has the excuse that this is an animal she has loved and cared for for decades. She's blinded by love, and needs to be counselled towards the realisation that the dog's existence is now more for her benefit than his. You're just upset that there are no more juicy pics of a recumbent, half-dead calf that you can caption with "TWice aS MaNY STArs As UsuaL!!!!!" in goofy ass fonts.
The only sad thing about Deux Face's death is that it took so long. Fight me on it, I don't care. Your gross parasocial relationship with a dying farm animal you've never met was not worth that animal's enforced suffering.
#vet stuff#i guess#dunno if i should tag this as deux face#bc im pretty sure if the people in complaining about find this post#theyll take my skin
367 notes
·
View notes
Text
September is Chiari Malformation Awareness Month!
Hi yes hello! Since many people probably aren't aware of it, I wanted to bring attention to something we ourselves have called chairi malformation at the start of its awareness month! Its recognized with a purple ribbon usually with a zipper on it (for the zipper scars of those who've had Chiari surgery)
What is Chiari Malformation?
Chiari (key-arr-ee) Malformation is a brain malformation in which the brain is too large, skull is too small, or some combination on the both, causing the cerebellar tonsils (and in some instances the brain stem) to slip through the skull and into the spinal chord.
Chiari is most typically a congenital effect. There are two main types (though they aren't the only ones). The most common of the two us Chiari 1, in which only the cerebellar tonsils are descended through the skull. The second most common, Chiari 2 (also known as Arnold-Chiari malformation) has more tissue herniation in the cerebellar tonsils and even the cerebellum, as well as brain stem herniation as well.
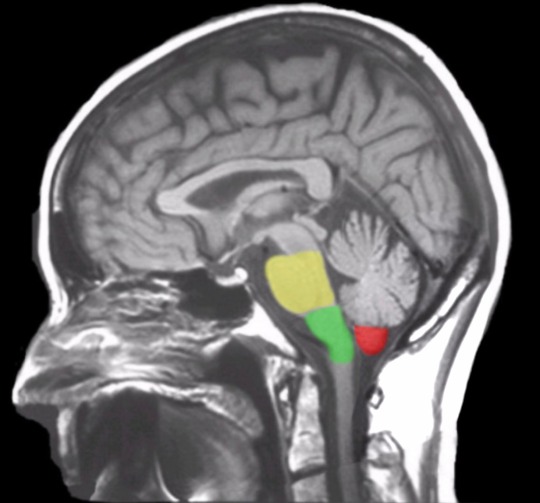
(See Below, the Cerebellar tonsils are marked in red while the brainstem is marked in green and yellow. This is considered a normal MRI)
Chiari malformation is likely to occur in 1 in 1,000 people, making it uncommon but not rare. The statistics are likely to be slightly higher than that for Chiari 1, as many people don't present symptomatically (and many incidents are only found in cases where the person was receiving radiological imaging for other instances such as head injury, so many people are unaware they had Chiari to begin with).
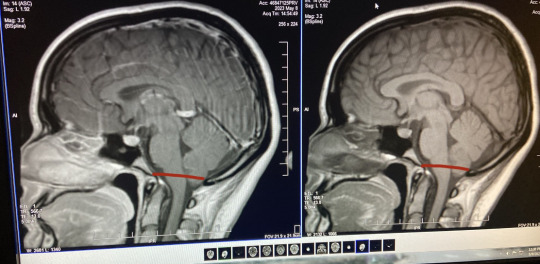
The only way to diagnose Chiari is through radiological imaging (many arguing upright MRI specifically is the only proper way to view the real level pf herniation). Herniation is measured down from the McRae line to the lowest point on the cerebellar tonsils. Depending on the accuracy of the machine (and which imaging tool is used) herniation can appear at different levels at different times. (See below, my first MRI looks markedly less in comparison to my second MRI, which features a roughly drawn on McRae line. In the second image I was noted to have a 7-8mm herniation.)

Symptoms
Chiari is marked by a number of symptoms and commorbidities, even moreso depending on the type you have. Symptoms can occur at any level of herniation. Some people with Chiari can have a 3mm descent and have debilitating symptoms, while some may have a 15 mm descent and be completely asymptomatic. The most common of these is occipital headaches & migraines, ranging from mild to severe, but many more are possible. These range from...
Balance Issues
Dizziness & Vertigo
Neck & Shoulder Pain
Difficulty Swallowing
Sore Throat
Sleep Apnea
Nausea & Vomitting
Tinnitus & Hearing Loss
Blurred Vision, Visual Snow, & Vision Loss
Muscle Weakness
Numbness or Pins & Needles (Caused by Nerve Damage)
Poor Motor Skills
Fatigue
Cognitive Difficulties (including but not limited to Brain Fog, Memory Problems, Confusion, & Difficulty Speaking)
Insomnia
Photophobia/Light Sensitivity
Syncope, Fainting, & Drop Attacks
Seizures
Dysautonomia
Since the cerebellar tonsils block the opening to the base of the skull, Chiari can halt the proper flow of CSF (Cerebral Spinal Fluid) between the brain and the spinal chord. Because of this, Syringomylia (cysts filled with CSF formed on the spine called Syrinxs) is considered common with Chiari. Other common disorders with Chiari are Scoliosis, EDS & Cervicocranial Instability, POTS, Tethered Spinal Chord Syndrome, Spina bifida, & Hydrocephalus.
So What's the Solution?
Well, the only known solution for Chiari as of right now is surgery. This surgery is called posterior fossa decompression-- in which a small portion of the base of the skull is removed from the Chiari patient to relieve pressure and give more room for the brain. The surgeon can then do for sone patients a duraplasty, in which the dura (or opening of the brain) is cut open and a patch of tissue is sewed into the incision to make the dura bigger and give even more room for the brain. Surgery can also be done as a preventative measure against syrinxes for those without them. In the case the patient also has a syrinx, more surgical procedure can be done to drain the cyst. In patients with EDS, special procedures must be made to avoid surgical complications and making things worse.
Surgery is not guaranteed to completely alleviate symptoms, but typically helps with some. However, due to large misunderstanding and disagreement on proper diagnostic traits of Chiari from doctors (most typically neurologists and neurosurgeons) many may be denied surgery for a number of years, and Chiari Diagnosis can take on an average of 4 years to officially receive.
Some go years experiencing symptoms and having "low lying cerebellar tonsils" (or similar language, such as incidental tonsillar ectopia) noted on their radiology reports without doctors officially recognizing it as Chiari. In this time many are misdiagnosed with other disorders such as chronic headaches, multiple sclerosis, fibromyalgia, and more before finally finding a doctor who will listen. Many will brush off the radiological findings as just a difference in your brain being formed at birth before admitting the symptoms can be due to Chiari. It can take years of your own patient advocacy before someone finally listens.
This is why awareness to it is so important, in hopes of reaching other people and doctors and forming a stronger understanding of the condition from information found by experts on it and those with Chiari themselves. With more awareness comes more accessibility to treatment and surgery so those who are symptomatic can hopefully find some relief. So this month send a little love & luck to those with Chiari!

#chiari#chiari malformation#chiari awareness#neurological disability#disabled#disability#disability awareness
36 notes
·
View notes
Text

Restless Foot Syndrome
Central Processing Unit Syndrome
Asperger Syndrome
Chronic Intestinal Pseudo Obstruction
Mowat Wilson Syndrome
Pitt Hopkins Syndrome
Charge Syndrome
Oppositional Defiant Disorder
Progressive Disease
Trisomy
Shortened Achilles Tendon
Arterial Venous Malformation
Schizophrenia
Anxiety
Stormme Syndrome
Panhypopituitarism
Adrenal Insufficiency
Bicuspid Aortic Valve
Chiari Malformation
Sensorineural Hearing Loss
Unknown Genetic Syndrome
Congenital Cytomegalovirus Infection
Catastrophic Epilepsy
Chromosomal Condition
Arthogryposis
Charcot Marie Tooth Disease
Disease Tuberose Sclerosis
End Stage Heart and Lung Disease
Spina Bifida
Hydrocephalus
Shaken Baby Syndrome
Cornelia De Lange Syndrome
Parry Romberg Syndrome
3 notes
·
View notes
Text
Pediatric neurological surgery in Lahore
Prof. Dr. Naveed Ashraf is a renowned surgeon of Pakistan and specializes in pediatric neurosurgery. Through years in practice, he has conducted many intricate neurosurgical operations among children with congenital disability, brain tumor, seizures, hydrocephalus, spina bifida, and other neurological conditions. His insurance while performing operations also makes sure that his patients get the best treatment to meet their pediatric needs.
0 notes
Text
Clinical Case Reports – 1970 by P. Syamasundar Rao in Journal of Clinical Case Reports Medical Images and Health Sciences
Abstract
In this paper five case reports were presented and include congenital pulmonary cyst, Wilson-Mikity syndrome, diaphragmatic eventration; foreign body in the bronchus, and cor pulmonale that developed after implantation of a ventriculo-atrial shunt with a Pudenz-Heyer valve for treatment of hydrocephalus. For each case report, clinical, chest x-ray, electrocardiogram and other pertinent findings were presented. This was followed by discussion of etiology, diagnosis, and treatment options, as appropriate.
Keywords: congenital pulmonary cyst; diaphragmatic eventration; Wilson-Mikity syndrome; foreign body in the bronchus; cor pulmonale
Introduction
During the academic clinical practice for over five decades, the author had the unique opportunity to observe and document many interesting clinical case scenarios. The purpose of this review is to revisit these interesting cases. Because of the voluminous amount of this material, the material may be divided into a five-part series. Each of these case reports, while rare and important clinical observations, do demonstrate a clinical point that is useful to the pediatricians, pediatric cardiologists and/or other physicians.
Congenital Pulmonary Cyst
Case Report
A female infant with a birth weight of 6 lb 7 oz, born after a full-term, normal pregnancy and delivery with an Apgar score of 9 presented at three weeks of age with a two-week history of tachypnea. There were no other symptoms and the infant’s physical examination was normal except for tachypnea (respiratory rate of 50 per minute) and mild inter-costal and sub costal retractions. A chest roentgenogram was obtained (Figure 1) which was interpreted as pulmonary cyst. The heart was pushed to the right by the cyst (dextroposition of the heart). At thoracotomy, a huge lung cyst, involving the lower lobe of the left lung, was found, and was resected and the patient made an uneventful recovery.
Discussion
Congenital pulmonary cysts in the neonate are uncommon and are considered as errors in embryological development. They are of several categories namely, bronchogenic cell, alveolar cell, and combined cell types, based on the cellular component of the cell wall of the cyst. The symptoms depend largely upon the size of the cyst. These patients may not be discovered until a chest x-ray is performed for other reasons or may present with symptoms of tachypnea, dyspnea, and cyanosis in the neonatal period secondary to compression of lung tissue. The findings depend upon the size and location of the cyst. Dextroposition of the heart or tracheal shift and hyper-resonance, diminished breath sounds, and rales may be detected on physical examination. The chest x-ray findings may demonstrate a cyst, as in our case (Figure 1) or may be misinterpreted as pneumothorax. Other conditions simulating the cyst are staphylococcal pneumonia, diaphragmatic hernia, congenital lobar emphysema, sequestrated lobe, and hydro-pneumothorax or pyo-pneumothorax. In symptomatic cases, cystectomy, segmentectomy, lobectomy, or pneumonectomy, depending upon the size and location of the cyst is suggested. Percutaneous aspiration of the cyst is not recommended except as an emergency measure to relieve the tension. Some authorities advocate no surgical intervention because of the possibility of spontaneous regression of the pulmonary cysts, but most authorities recommend surgical excision of the cysts [1].
Late Respiratory Distress in a Premature Infant
Case Report
A premature male infant was born at 25 weeks of gestation and weighed 2 lb 12 oz at birth. Abruptio placenta and prolapse of the umbilical cord complicated the delivery and required resuscitation with oxygen. The chest x-ray was normal at that time. The baby was placed in an incubator in 35 percent oxygen, which was discontinued within 24 hours. At the age of 31 days, tachypnea and recurrent apnea with cyanosis developed. Auscultation revealed bilateral rales in the chest, again necessitating resuscitation with O2, administered by bag and mask. Chest x-ray revealed a diffuse parenchymal reticular pattern with multifocal areas of radiolucency. This roentgenographic pattern, along with the clinical findings, is essentially diagnostic of the Wilson-Mikity syndrome.
Figure 2: Chest x-ray in posterio-anterior view demonstrating a diffuse parenchymal reticular pattern with multifocal areas of radiolucency. This roentgenographic pattern, along with the clinical findings, is essentially diagnostic of the Wilson-Mikity syndrome. Reproduced from Rao PS. Chest 1970; 57:495-6.
Discussion
Wilson an Mikity originally described this condition in 1960, and is now called Wilson-Mikity syndrome.2 The etiology is not clearly understood but is considered to be due to pulmonary dysmaturity with uneven postnatal development of pulmonary alveoli in the premature infants.2 No consistent relationship with O2 therapy has been established. Bronchopulmonary dysplasia is another condition seen in the neonatal period and should be distinguished from Wilson-Mikity syndrome. The cystic appearance on the chest x-ray in the third stage of bronchopulmonary dysplasia resemble those of Wilson-Mikity syndrome; however, it follows treatment of severe hyaline membrane disease with high concentrations of O2 and artificial ventilation.2 The clinical presentation of Wilson-Mikity syndrome is characteristic in that the infant is premature with minimal or no respiratory distress at birth but, develops progressive respiratory distress, with dyspnea, tachypnea, cough, cyanosis, and rales in a few days to weeks. Diffuse reticular pattern of both lungs with areas of multifocal radiolucency are usually seen, similar to those seen in figure 2. Progressive pulmonary insufficiency with signs of right heart failure develop in patients with fatal outcome. But, about half of the patients eventually recover from their pulmonary disease. Pulmonary function studies are abnormal with decreased lung compliance, increased expiratory flow resistance, and increased breathing effort. Respiratory acidosis develops in spite of increased minute volume. Arterial O2 desaturation is thought to be secondary to intrapulmonary right-to-left shunting.2 The treatment is largely supportive [2].
Fever, Vomiting and Dome-Shaped Density in Right Thorax
Case Report
A four-month-old boy presented with a history of fever, poor feeding, vomiting, and slight cough for two days. Past history is essentially normal except for an Apgar score of 6 at birth. Breath sounds were diminished at the right base. Laboratory studies were normal. Chest x-ray (Figure 3) was performed which revealed a dome-shaped density in the right thorax which did not coincide with any pulmonary lobe or segment. The elevation of the inferior liver margin in the abdomen indicated that the abnormal shadow was liver. Based on these findings eventration of the right hemi-diaphragm was suspected. To confirm the diagnosis, a diagnostic pneumoperitonium was performed which confirmed the diagnosis.
Discussion
Eventration of the diaphragm is classified into adult and infantile types [3]. It is generally thought to be the result of congenital mal-development of the diaphragmatic musculature. However, such an abnormality may occasionally be caused by phrenic nerve injury during birth. The true incidence of eventration is not known, but in mass x-ray surveys of adults, it was found to be one in 10,000 [3]. Total eventration is thought to be more common on the left side and partial eventration on the right [3].
Clinical findings largely depend on the extent of eventration. There may be no symptoms or the patient may present with dyspnea, tachypnea, and cyanosis in the newborn period, requiring immediate treatment. Seesaw cyclic motions of the epigastrium with respiration and Hoover's sign (uninhibited divergence of costal margin from midline on inspiration), if present, are helpful in making the diagnosis. Percussion on the affected side may be dull or tympanic depending on the organs migrated under the diaphragm.
Fluoroscopy and chest x-rays are generally useful in arriving at the diagnosis. In right-sided eventrations, the lesser amount of liver shadow in the abdomen, i.e., elevation of the inferior margin of the liver helps to distinguish eventration from the other conditions [3]. Diagnostic pneumoperitonium is likely to establish the diagnosis, but the current availability of ultrasound technology, diagnostic pneumoperitoneum may not be necessary at the present time.
Symptomatic newborns with diaphragmatic eventration should be treated surgically; plication of the eventrated diaphragm is successful in relieving the symptoms with good long-term results. Some authorities suggest that asymptomatic patients also should be addressed surgically [3].
Foreign Body (Peanut) in The Left Main Stem Bronchus
Case Report
A 13-month-old girl with a history of poor appetite, loss of weight, cough, and intermittent low grade fever was admitted to the hospital for evaluation and treatment. No history of choking episodes was elicited. History revealed that a relative who had active pulmonary tuberculosis lived with the infant's family for a short period of time four months prior to the current admission. Because of this reason, the local health department performed tuberculin skin test which was positive and treatment with isoniazid was initiated. On examination her weight and height were between the third and tenth percentile. Decreased breath sounds on auscultation and hyper tympanic note on percussion were noted over the left side of the chest.
Intermediate strength purified protein derivative (PPD) was positive. Chest roentgenograms were obtained . Based on the history, physical examination, and chest x-ray findings, a diagnosis of endobronchial tuberculosis was entertained. However, prior to beginning treatment, bronchoscopy was performed to appraise the extent of airway encroachment.
Discussion
Autoimmune encephalitis is a condition that can be easily missed as it is not commonly considered in the differential diagnosis of various medical presentations. However, such diagnosis should be always taken into consideration when a person, particularly a child, presents with a new onset of refractory status epilepticus (NORSE) and/or new behavioral or psychiatric conditions. An early diagnosis of AE is essential, as the treatment is different from other conditions. With correct timely interventions the outcome is frequently favorable.
Though SARS-Cov-2 virus rarely invades the nervous system, Covid-19 infection frequently causes neurological symptoms like headache, delirium, anosmia, and dysgeusia [14]. One of the mechanisms of indirect nervous system involvement is through inflammatory response and immune dysregulation. There are few recorded cases of indirect involvement of CNS by auto-antibodies that are directed against the surface and synaptic protein. This case is one of the rare cases of Anti NMDA antibody autoimmune encephalitis that is associated with Covid-19 infection [15]. It indicates that in the era of COVID-19, high vigilance is required as a possible association may increase AE incidence.
A recent systemic review that analyzed 16 studies, including a total of 161 patients with NORSE [16], showed that the most frequent cause was AE. In addition to the well-known association with teratoma and cancer, AE, and specifically Anti-NMDA receptor Ab encephalitis, could be associated with a SARS‑CoV‑2 infection, either concomitantly or as post-infection manifestation. In this reported case, immunotherapy, in addition to anti-seizure medication, showed to be effective.
The main limitation of this report is the relatively short follow-up period. Observation of the child is ongoing to detect possible medium- or long-term consequences.
Positive PPD in an infant with poor appetite, loss of weight, and fever is suggestive of primary tuberculosis. This is particularly so given the patient's exposure to a subject with active pulmonary tuberculosis. The x-rays show hyper aeration of the left lung with a shift of the heart and mediastinum to the right. The left leaf of the diaphragm is also flattened. While there are no areas of infiltration or consolidation were seen, prominent shadows suggesting enlarged lymph nodes were seen . Endobronchial tuberculosis with compression of the bronchus by adenopathy may produce changes seen figure 5.
Discussion
Even though there was no history of choking or aspiration, the possibility of foreign body aspiration should be considered in this age group. Consequently, bronchoscopy was performed which revealed a peanut in the left main stem bronchus and was extracted during bronchoscopy. The peanut and the adjacent edema of the bronchus caused partial bronchial obstruction and acted as a check valve, so the air entered the left lung but, unable to leave the left lung since the bronchus becomes smaller during expiration, producing the roentgenographic appearance shown in figure 5. The baby improved and the treatment with isoniazid was continued because of the positive PPD.
Cor Pulmonale as a Complication of Ventriculoatrial Shunts
Introduction
Cerebral ventricle-to-right atrial shunts with Pudenz-Heyer or Spitz-Holter valves were widely used to treat hydrocephalus in the 1960s. Development of pulmonary hypertension with chronic cor pulmonale is rare with these shunts. We reported a patient who developed such a complication along with description of specialized pulmonary function studies in the early detection of such complication [5].
Case Report
An 11-year-old white boy was hospitalized in April 1969 with a history of progressive weakness, dyspnea, and pedal edema. He was diagnosed to have hydrocephalus and had a ventriculo-atrial shunt with a Pudenz-Heyer valve implanted at the age of 6 months. The shunt was thought to be functioning well when he was evaluated at the age of 2 years. He was asymptomatic until he was 9.5 years old, when he developed signs of congestive heart failure (CHF) and was treated at another hospital with digitalis and diuretics with some improvement. Right heart catheterization at the same institution revealed a mean right atrial pressure of 35 mmHg and right atrial angiography revealed slow emptying of the contrast, filling defects on the right lateral atrial wall and in the right and left pulmonary arteries. The ventriculo-atrial shunt was removed shortly thereafter. The patient was referred to our group for further evaluation and management [5].
Pertinent findings on examination included height and weight below the third percentile, head circumference above the 97th percentile, pretibial edema, prominent “a” wave in the left side of the neck, no venous pulsations on the right side, palpable right ventricular heave, markedly accentuated single second heart sound, an audible fourth heart sound at left lower sternal border, a Grade I/VI ejection systolic murmur at the mid-left sternal border, liver edge palpable 5 cm below the right costal margin, clear lung fields on auscultation, and normal neurological examination.
Electrocardiogram (ECG) and the vectorcardiogram (not shown) revealed right atrial and ventricular hypertrophy. Chest roentgenogram showed moderate cardiomegaly and prominent main pulmonary artery (PA) segment and clear lung fields. Lung scan with 131I-labeled macro-aggregated albumin was suggestive of multiple pulmonary emboli. Blood gas analysis showed pH 7.56; PaO2 80 mmHg, PaCO2 23 mmHg and bicarbonate 24 mEq/liter. Routine pulmonary function studies revealed restrictive lung disease. The ratio of wasted ventilatory volume (physiological dead space) to tidal volume (VD:VT) using Bohr's equation was 0.58 (normal 0.3 or less).
Vigorous treatment with digitalis and diuretics resulted in only temporary relief. During the next year, he continued to deteriorate and died of intractable right ventricular failure. Postmortem revealed right atrial thrombosis, severe right ventricular hypertrophy, multiple thrombo-emboli in the large and medium-sized pulmonary arteries, and intimal proliferation of the pulmonary arterioles.
Discussion
The case presented demonstrated development of cor pulmonale secondary to pulmonary thrombo-embolism which was produced by thrombi that arose following a ventriculo-atrial shunt with a Pudenz-Heyer valve for treatment of hydrocephalus. The causes of thrombo-embolic complications were not well understood, but the hypotheses, as reviewed by us [5], include infection, periarteritis due to autoimmune reaction of the pulmonary vessels to protein of cerebrospinal fluid, release of brain thromboplastin resulting in thrombosis at the point of contact with plasma coagulation factors, and simply the presence of a foreign body in the cardiovascular system for prolonged periods of time.
Early detection of pulmonary hypertension by periodic (every six months) evaluation by chest x-ray and ECG studies was suggested by some investigators, but early detection of pulmonary hypertension is of limited value since obstruction of 60% of the pulmonary vascular bed occurs by the time pulmonary hypertension develops [5]. Detection of multiple filling defects on radioisotope scanning in a child with a ventriculo-atrial shunt would be suggestive of pulmonary embolization and might be useful in early identification. Based on the observations of Nadel and associates [6] and those of ours [5], we suggested that specialized pulmonary function studies such as VD:VT, pulmonary diffusing capacity, pulmonary capillary blood volume, blood gas, and pH be performed periodically to detect obstruction of pulmonary vasculature prior to the development of pulmonary hypertension and cor pulmonale [5]. However, it should be noted that ventriculo-atrial shunts are no longer performed to treat hydrocephalus, but instead ventriculo-peritoneal shunts are used at the present time.
In summary, a rare case of pulmonary thrombo-embolism with resultant pulmonary hypertension and cor pulmonale following ventriculo-atrial shunt for hydrocephalus was presented with the recommendation to use of special pulmonary function studies for early detection and if found to be positive, immediate removal of the shunt system may eliminate further embolization into the lungs and prevent irreversible pulmonary vascular disease.
#congenital pulmonary cyst#diaphragmatic eventration#Wilson-Mikity syndrome#foreign body in the bronchus#cor pulmonale#Clinical Case Reports and Studies.
1 note
·
View note
Text
Advancements in Treatment and Care for Spina Bifida: What You Need to Know
Spina Bifida, a congenital condition that affects the spine, has long posed significant challenges for those living with it. However, advancements in medical technology and care have transformed the landscape for individuals with Spina Bifida, providing them with better opportunities to lead active, fulfilling lives. Let’s take a look at the key advancements in treatment and care that are shaping the future for people with this condition.
Fetal Surgery: A Groundbreaking Option One of the most significant advancements in recent years is fetal surgery, a procedure performed on the fetus while still in the womb. This surgery involves closing the opening in the spine before birth to prevent further damage to the spinal cord and nerves.
Improved Mobility Outcomes Studies have shown that children who undergo fetal surgery for Spina Bifida have better mobility outcomes compared to those who undergo surgery after birth.
Reduced Risk of Hydrocephalus The surgery has also been linked to a decreased need for shunt placement to manage hydrocephalus (fluid buildup in the brain), a common complication of Spina Bifida.
While fetal surgery is a complex procedure, it offers hope for better quality of life and long-term health outcomes for children born with Spina Bifida.
Advances in Neurosurgery and Spine Care Traditional neurosurgical procedures continue to evolve, offering better outcomes for patients with Spina Bifida. Modern neurosurgery techniques have become less invasive and more effective in managing symptoms and complications associated with the condition.
Shunt Systems for Hydrocephalus Innovations in shunt technology have improved the management of hydrocephalus, reducing the risks of infection and malfunction.
Tethered Cord Surgery Many individuals with Spina Bifida develop tethered cord syndrome, where the spinal cord is abnormally attached to surrounding tissues. Advances in tethered cord release surgery now provide safer and more effective solutions to alleviate pain and prevent further neurological damage.
These advances ensure that individuals with Spina Bifida can maintain greater mobility and experience fewer complications as they grow older.
Enhanced Mobility Solutions and Assistive Devices Modern mobility equipment has greatly improved the independence and quality of life for people with Spina Bifida.
Custom Wheelchairs Advanced wheelchair designs, such as lightweight models with better maneuverability, offer greater comfort and freedom for people with limited mobility.
Exoskeletons Although still in early stages of development, wearable robotic exoskeletons hold promise for providing mobility assistance, allowing people with Spina Bifida to walk with mechanical support.
These technological advancements make daily tasks easier and give individuals greater autonomy, both at home and in public spaces.
Multidisciplinary Care Approaches The complexity of Spina Bifida requires a multidisciplinary approach to care, involving a team of specialists such as neurologists, orthopedic surgeons, urologists, and physical therapists. Advances in this model of care have led to better coordination between healthcare providers, ensuring comprehensive treatment for the physical and emotional needs of individuals with Spina Bifida.
Coordinated Care Patients now benefit from integrated care plans, where all aspects of their health are addressed, from mobility and bladder management to mental health support.
Telemedicine With the rise of telemedicine, individuals with Spina Bifida have greater access to expert care, even if they live far from specialized healthcare facilities. Telehealth services allow for regular check-ups and consultations without the need for frequent travel.
This holistic approach not only improves medical outcomes but also enhances overall well-being.
Stem Cell Research and Regenerative Medicine One of the most exciting areas of advancement is stem cell research. Scientists are exploring the potential of stem cells to repair spinal damage caused by Spina Bifida.
Spinal Cord Regeneration Early studies suggest that stem cell therapy could help regenerate damaged spinal tissues, offering a potential breakthrough in treating Spina Bifida at the cellular level.
Long-Term Potential While still in experimental stages, stem cell therapies could one day become a routine part of Spina Bifida treatment, improving mobility and reducing complications.
These developments represent a significant step forward in understanding how to repair the nervous system and offer hope for more effective treatments in the future.
Improved Urological and Bowel Management Many individuals with Spina Bifida face challenges related to bladder and bowel function. Recent advancements in medical devices and treatments are providing better control and comfort.
Bladder Augmentation Surgery New techniques in bladder augmentation help improve urinary continence and reduce the risk of infection.
Intermittent Catheterization Innovative catheters and better training have made bladder management easier and more hygienic for individuals with Spina Bifida.
These advancements allow for better management of one of the most common complications of Spina Bifida, improving quality of life and reducing health risks.
Rehabilitation and Physical Therapy Rehabilitation plays a key role in helping individuals with Spina Bifida maximize their physical abilities. Modern approaches to physical therapy focus on improving mobility, strength, and overall fitness.
Adaptive Physical Therapy Tailored exercises and therapies help individuals develop strength, balance, and flexibility, even with limited mobility.
Assistive Technology in Therapy Devices like robotic-assisted gait trainers and virtual reality systems are being integrated into rehabilitation programs to enhance therapeutic outcomes.
By continuing physical therapy, people with Spina Bifida can maintain their independence and improve their functional abilities over time.
Advancements in treatment and care for Spina Bifida have opened new doors for those living with the condition. From fetal surgery and mobility aids to stem cell research and coordinated care, these developments are helping individuals with Spina Bifida lead healthier, more independent lives. With ongoing research and innovation, the future looks bright for improving the quality of life for people with Spina Bifida.
Source:
0 notes
Text
Make the Horoscope of your Child by the NT Scan

A good radiologist or a foetal medicine specialist can be an expert horoscope maker most of time better than an astrologer because he or she has a better proved scientific approach.
HOW it is done you may wonder?
NT scan
NT scan is the key for him or her to make the horoscope. NT means Nuchael Translucency. It is the thickness of fluid behind the neck in the subcutaneous plane. NT scan is done between 11 weeks and 13 + 6 weeks (not 10 weeks 6 days or at 14 weeks) when the CRI- (total length from crown to rump) is between 45mm and 84mm.
The astrologer needs the correct time of birth and the child’s gender. Here the Doctor needs 5 things to make the horoscope chart.
The CRL
NT measurement
Nasal bone present or absent — all these obtained from scanning the fetus
From the maternal blood, he or she collects the levels of PAPP-A and
Free Beta HCG
He or she feeds all these to a computer which is loaded with special software which gives the result as follows
(a)Low risk (b) Intermediate risk (c) High risk
If the result is low risk, we will give a pass mark and allow the pregnancy to continue. No need to worry. This baby will have a more or less a normal life and will live up to death like any of us with all the pangs and happiness of life.
If the result is intermediate risk, we will give one more chance to the pregnancy by advising NIPT – a blood test for mother. If NIPT is negative, they are like the group mentioned above but if it is positive they fall into high risk category.
The high risk category— It is in this group, unfortunately the horoscope predictions will be bad for these children.
What to do with the high risk group?
To draw a “Thalakury” and predict the future instead of “Star Positions” we make it with four main factors.
Adenini
Quaninei
Cystinom and
Thyminym which the scientist call nucleotides
For more accurate reading of the Grahanila position we add three components of the nucleotides
(a) Phosphate group (b) A sugar molecule and (c) A nitrogen base
How is this data collected for the horoscope?
We do CVS (chorionic villus Sampling) before 14 weeks of pregnancy or amniocentesis after 16 weeks of pregnancy. These samples contain fetal cells. We culture it outside and multiply the cells. Then we analyse the chromosome and DNA by which we get all the data to draw the Grahanila.
Predictions
Will the parent get a full term baby or will the pregnancy end up in intra uterine fetal death?
If the DNA test comes as Edwards syndrome — trisomy 18 (Extra chromosome 18); PATAVU Syndrome (Trisomy 13); TURNER Syndrome (Monosomy X) ; TRIPLOIDY Hydatid mole ; Osteogenesis imperfect type Il, severe case of congenital diaphragmatic hernia; SMITH LEMLI — OPITS Syndrome
In the above conditions one can predict that most probably the pregnancy will end up in IUD.
By scanning you can decide whether it is a male or female child (We do not reveal this to the patient, as this is against Indian law)
If it is a male child will it have IUD?
X linked recessive disorders (DUCHENNE MUSCULAR DYSTOPHY; Haemophilia A and B ; X linked Hydrocephalus ; X linked severe combined immino deficiency ( SCID); X linked ICHTHYOSIS (severe form of a skin disease), X linked lympho proliferative syndrome ; Menkes disease; X linked MYOTUBULAR MYOPATHY; HUNTER SYNDROME; ORNITHINE TRANSCARBAMYLASE Deficiency – All usually will lead to IUD.
If it is a female fetus will it live up to term?
TURNER SYNDROME (MONOSOMY X); REIT Syndrome; Congenital adrenal hyperplasia; LEIGH syndrome; GOLTS Syndrome, severe form of cystic fibrosis etc. may end up in IUD
In the horoscope we can predict this “BOY” may not reach adulthood — like the story of MARKENDAYAN in Hindu mythology or we can predict the “GIRL” may not reach adulthood.
Also like “SARPADOSHAM” we can indicate this female child will potentially pass the disease to their offsprings.
0 notes
Text
Brain Aneurysm: Causes, Symptoms, Risk Factors, and Treatment Options

A brain aneurysm, also known as an intracranial or cerebral aneurysm, occurs when a weak spot in the wall of a blood vessel in the brain bulges and fills with blood. It resembles a small, berry-shaped sac hanging from the artery. When a brain aneurysm ruptures or leaks, it can cause a life-threatening condition known as a hemorrhagic stroke, which requires immediate medical attention.
Causes of Brain Aneurysm
Brain aneurysms often develop in the arteries located at the base of the brain, especially at branching points where arterial walls are weakest. These weak areas are more susceptible to rupture.
Signs and Symptoms of a Brain Aneurysm
Common signs and symptoms include:
Severe headache
Nausea and vomiting
Stiff neck
Double or blurred vision
Sensitivity to light
Seizures
Drooping eyelids
Loss of consciousness
Confusion
A leaking aneurysm may cause a sudden, severe headache, while an unruptured aneurysm can cause localized pain, double vision, and facial numbness.
Risk Factors for Brain Aneurysm
Certain factors can increase the likelihood of developing a brain aneurysm, including:
Age (more common in adults)
Gender (women are more susceptible)
Smoking
High blood pressure (hypertension)
Drug use (e.g., cocaine)
Excessive alcohol consumption
Genetic conditions like Ehlers-Danlos syndrome
Polycystic kidney disease
Congenital conditions, such as brain AVM (arteriovenous malformation)
Family history of aneurysms
Complications from a Brain Aneurysm
When a brain aneurysm ruptures, it causes bleeding that can damage or destroy surrounding brain cells, increasing pressure inside the skull. This disruption of blood and oxygen flow can result in unconsciousness or even death. Other complications may include:
Rebleeding
Vasospasm (narrowing of blood vessels)
Hydrocephalus (fluid buildup in the brain)
Hyponatremia (low sodium levels)
Diagnosis of Brain Aneurysm
At Yashoda Hospital and Research Centre, Ghaziabad, various diagnostic tools are used to detect brain aneurysms, especially in patients with a family history of the condition. These may include:
CT Scan: Produces 3D images of the brain.
MRI: Uses radio waves and magnetic fields to capture brain images.
Cerebrospinal Fluid Test: Checks for blood in the fluid surrounding the brain and spine.
Cerebral Angiogram: Detects aneurysms by imaging the brain's blood vessels.
Treatment for Brain Aneurysm
Treatment options depend on factors like the size, location, and whether the aneurysm has ruptured. Urgent treatment is required for ruptured aneurysms, with several surgical options available:
Surgical Clipping: A metal clip is applied at the base of the aneurysm to halt blood flow.
Endovascular Coiling: A catheter is inserted into the artery, and tiny platinum coils are placed inside the aneurysm to block blood flow.
Flow Diverter Surgery: A stent is placed in the artery to redirect blood flow away from the aneurysm.
Symptom Management and Preventive Care
To manage symptoms and prevent complications, doctors may recommend:
Pain relief medications (e.g., acetaminophen) for headaches
Calcium channel blockers to prevent blood vessel narrowing
Anti-seizure medications for seizures
Drainage procedures (ventricular or lumbar catheters) to reduce pressure on the brain
Shunt surgery for fluid drainage
Rehabilitative therapy to help regain lost skills due to brain damage
By recognizing the signs and symptoms early, and understanding the risk factors, timely intervention can prevent life-threatening complications from a brain aneurysm.
Conclusion:
Early diagnosis is key to effectively treating a brain aneurysm. Being vigilant and recognizing the warning signs can make a significant difference. Immediate medical attention and timely intervention for a ruptured aneurysm greatly improve survival rates and recovery outcomes. While recovery from an unruptured aneurysm is typically fast, a ruptured aneurysm may require multiple surgeries, and the recovery period can vary based on the extent of damage. Prompt action is crucial for better long-term prognosis.
Dr. (Brig.) Yadvendra Singh Sirohi is a highly distinguished neurologist with over 24 years of experience, having trained and excelled at leading national institutions. Known for his clinical expertise, compassion, and commitment, he serves as a Senior Consultant in Neurology at Yashoda Hospital & Research Centre, Ghaziabad. Dr. Sirohi is adept at managing a wide range of neurological conditions with exceptional skill and care.
Dr. Shishir Kumar is a highly skilled neurosurgeon, neuro interventionist, and endoscopic spine surgeon with over 9 years of experience in the Delhi/NCR region. He has completed fellowships in neuro intervention, endovascular surgery, and minimally invasive spine surgery. With his extensive training, Dr. Kumar provides comprehensive neurosurgical care, focusing on patient education and a collaborative treatment approach. He currently practices at Yashoda Hospital & Research Centre, Nehru Nagar, Ghaziabad.
Dr. Atul Gupta is a highly experienced neurosurgeon with 29 years of expertise. He specializes in complex procedures, including brain tumor surgeries, cerebrovascular surgeries, epilepsy treatments, and spine surgeries.
Dr. Puneet Malik is a skilled neurosurgeon specializing in complex brain and spinal cord surgeries, particularly for patients experiencing severe numbness. He is adept at procedures such as clot removal, tumor excision, and halting brain bleeding, all performed with exceptional precision and care.
0 notes
Text
Neurosurgeon in Gaya and Bihar — Arsh Hospital Expertise in Neurosurgery

Arsh Hospital Neurosurgery Department
Located in Gaya, Arsh Hospital is renowned for providing specialized neurosurgical care that is both accessible and effective. The hospital’s Neurosurgery Department is equipped with state-of-the-art diagnostic and surgical equipment, allowing doctors to perform intricate procedures with precision. From routine brain surgeries to emergency trauma care, Arsh Hospital covers all aspects of neurosurgical treatment under one roof, setting it apart as a leading center for neurosurgery in Bihar.
Top Neurosurgeons at Arsh Hospital, Gaya
Arsh Hospital is home to some of the best neurosurgeons in Bihar, each with years of experience and specialized training.
Dr. Ranjan Kumar Jena is one of the most respected neurosurgeons in the region, with expertise in treating complex brain and spinal conditions. His meticulous surgical skills and deep knowledge have earned him a stellar reputation.
Dr. Ashish Kumar Jha, another leading neurosurgeon at Arsh Hospital, specializes in minimally invasive neurosurgical procedures and has successfully treated numerous patients suffering from spinal and brain disorders.
Both of these specialists, along with other qualified neurosurgeons, work together to provide a comprehensive range of services aimed at improving patient outcomes.
Common Neurosurgical Conditions Treated
At Arsh Hospital, the neurosurgery team handles a variety of neurological conditions, including:
Brain Tumors and Cranial Injuries: From benign tumors to malignant brain cancers, Arsh Hospital’s neurosurgeons are skilled in performing delicate brain surgeries.
Spinal Cord Disorders and Injuries: Patients suffering from herniated discs, spinal fractures, or degenerative spinal diseases are treated using the latest surgical techniques.
Cerebrovascular Diseases and Stroke Management: The hospital offers advanced treatment for stroke patients, including emergency intervention and post-stroke care.
Pediatric Neurosurgery: Children with congenital neurological disorders, such as hydrocephalus, receive specialized care from the pediatric neurosurgery team.
Advanced Neurosurgical Procedures Offered
Arsh Hospital is known for its ability to perform advanced neurosurgical procedures, some of which include:
Minimally Invasive Brain Surgery: Using cutting-edge techniques, surgeons at Arsh Hospital can operate on brain tumors and other conditions with minimal incisions, leading to quicker recovery times.
Spinal Fusion and Decompression Surgery: These surgeries are commonly performed on patients with chronic spinal issues, offering long-term pain relief and improved mobility.
Aneurysm Clipping and Endovascular Procedures: For patients with aneurysms or vascular malformations, the hospital provides both surgical and non-surgical interventions.
Neurotrauma Care at Arsh Hospital
Emergencies such as traumatic brain injuries require immediate attention, and Arsh Hospital’s 24/7 emergency neurotrauma services are designed to handle these critical situations. The hospital is equipped with a state-of-the-art Intensive Care Unit (ICU) that offers round-the-clock monitoring and care for patients recovering from neurotrauma.
Post-Surgical Care and Rehabilitation
Recovery after neurosurgery is a critical phase, and Arsh Hospital takes a holistic approach to post-surgical care. Patients are provided with personalized rehabilitation programs, including physical therapy and occupational therapy, to help them regain strength and function. The goal is to offer a smooth and steady recovery that allows patients to return to their normal lives.
Technology and Infrastructure Supporting Neurosurgery
At Arsh Hospital, neurosurgeons are supported by advanced imaging and diagnostic tools such as MRI, CT scans, and intraoperative monitoring systems. These technologies enable precise diagnosis and guide surgeons during complex procedures. In addition, the hospital’s surgical suites are equipped with the latest medical devices, ensuring high success rates and minimal complications during surgery.
Why Choose Arsh Hospital for Neurosurgery in Bihar?
There are several reasons why patients choose Arsh Hospital for Neurosurgeon in Bihar:
Multidisciplinary Approach: The hospital takes a team-based approach to patient care, with neurosurgeons working closely with neurologists, radiologists, and other specialists.
Expertise and Experience: With renowned neurosurgeons like Dr. Ranjan Kumar Jena and Dr. Ashish Kumar Jha leading the department, patients are in the hands of experts.
Compassionate Care: Beyond technical expertise, the hospital is known for its compassionate approach to patient care, ensuring that each patient feels supported throughout their treatment.
Success Stories and Patient Testimonials
Patients treated at Arsh Hospital have shared heartwarming stories of recovery and success. Many have praised the hospital’s expertise, state-of-the-art facilities, and the dedication of its medical staff. These testimonials reflect the hospital’s commitment to providing high-quality neurosurgical care.
Future of Neurosurgery at Arsh Hospital
As the demand for neurosurgical services continues to grow in Bihar, Arsh Hospital plans to expand its neurosurgery department further. By investing in research, training, and the latest technology, the hospital aims to remain at the forefront of neurosurgical innovation in the region.
How to Book a Consultation with a Neurosurgeon
Booking a consultation at Arsh Hospital is straightforward. You can contact the hospital directly through their helpline or schedule an appointment online via their website. The hospital’s team will assist you in getting a consultation with the best available neurosurgeon based on your needs.
Conclusion
For anyone in Gaya or Bihar seeking specialized neurosurgical care, Arsh Hospital offers an unmatched level of expertise, cutting-edge treatments, and compassionate care. Whether you need emergency neurotrauma care or complex brain surgery, the hospital’s team of experienced neurosurgeons is equipped to handle it all.
0 notes
Text
Find Me Friday: Erik & Liam!
Logo that says Reece’s Rainbow Special Needs Adoption Support in blue, below a blue & yellow paint stroke rainbow graphic with a yellow Ukrainian trident symbol on the right half. In this series, each Friday, I want to share a different child or group of children with you who are available for adoption and listed through the adoption advocacy website Reece’s Rainbow. All the kids who are listed…

View On WordPress
#accessible post#adoption advocacy#arthrogryposis#available to large families#available to married couples#available to older parents#available to single dads#available to single moms#CHD#congenital heart defect#craniofacial disability#disability adoption#education#Erik#Find Me Friday#FSP#hydrocephalus#Liam3#medical history#Noonan syndrome#photo descriptions#physiotherapy#pulmonary stenosis#Reece&039;s Rainbow#short stature#waiting children
0 notes
Text
Pediatric Neurosurgeon in Pimpri Chinchwad: Expert Care at Neuronest Clinic
When it comes to the health and well-being of children, specialized medical care is crucial. Pediatric neurosurgery, which focuses on diagnosing and treating neurological disorders in children, requires a high level of expertise and compassion. Neuronest Clinic in Pimpri Chinchwad is a leading healthcare provider in this field, offering world-class pediatric neurosurgical care. This blog explores the importance of pediatric neurosurgery and why Neuronest Clinic is the top choice for parents seeking the best care for their children.
Understanding Pediatric Neurosurgery
Pediatric neurosurgery involves the surgical treatment of neurological disorders in children, from newborns to adolescents. These conditions can range from congenital anomalies and brain tumors to epilepsy and spinal disorders. The complexity of these cases requires a specialized approach, tailored to the unique needs of young patients whose bodies and brains are still developing.
Why Choose Neuronest Clinic for Pediatric Neurosurgery?
Neuronest Clinic is dedicated to providing exceptional care for children with neurological conditions. Here are the key reasons why it stands out as the premier choice for pediatric neurosurgery in Pimpri Chinchwad:
1. Expert Pediatric Neurosurgeons
Neuronest Clinic boasts a team of highly skilled and experienced pediatric neurosurgeons. These specialists have undergone extensive training in both neurosurgery and pediatrics, equipping them with the knowledge and skills needed to address the unique challenges of treating children. Their expertise ensures that young patients receive the best possible surgical care.
2. State-of-the-Art Facilities
The clinic is equipped with cutting-edge technology and advanced surgical tools, essential for performing precise and effective neurosurgical procedures. The state-of-the-art facilities at Neuronest Clinic enable the medical team to diagnose and treat complex neurological conditions with the highest level of accuracy and safety.
3. Comprehensive Multidisciplinary Care
Pediatric neurosurgery often requires a multidisciplinary approach. At Neuronest Clinic, a team of specialists, including neurologists, pediatricians, anesthesiologists, and rehabilitation therapists, work together to provide comprehensive care. This collaborative approach ensures that every aspect of the child’s health is addressed, from diagnosis to recovery.
4. Child-Friendly Environment
Understanding the emotional and psychological needs of young patients is crucial in pediatric care. Neuronest Clinic is designed to be a child-friendly environment, aiming to reduce anxiety and make children feel comfortable. The compassionate staff at the clinic are trained to handle pediatric patients with care and empathy, making the experience as stress-free as possible for both the children and their parents.
5. Focus on Family Support
Neuronest Clinic recognizes the importance of involving families in the treatment process. Parents are provided with detailed information about their child’s condition, the proposed surgical procedure, and the expected outcomes. The clinic also offers support services to help families cope with the challenges of dealing with a child’s neurological disorder.

Conditions Treated by Pediatric Neurosurgeons at Neuronest Clinic
Neuronest Clinic’s pediatric neurosurgeons are equipped to treat a wide range of neurological conditions in children, including:
Congenital Anomalies: Conditions such as spina bifida, encephalocele, and craniosynostosis, which are present at birth and require surgical intervention.
Brain and Spinal Tumors: Removal of benign and malignant tumors affecting the brain and spinal cord.
Hydrocephalus: Treatment of excessive accumulation of cerebrospinal fluid in the brain.
Epilepsy: Surgical options for children with drug-resistant epilepsy.
Traumatic Brain Injuries: Management of head injuries resulting from accidents or falls.
Chiari Malformations: Treatment of structural defects in the brain and spinal cord.
The Surgical Process: What to Expect
The surgical process at Neuronest Clinic begins with a thorough evaluation and diagnosis, using advanced imaging techniques to pinpoint the issue. The pediatric neurosurgeon will then discuss the recommended surgical plan with the family, explaining the procedure, potential risks, and benefits. On the day of surgery, the child will be cared for by a team of specialists, ensuring their safety and comfort throughout the process. Post-operative care includes monitoring, pain management, and rehabilitation to support the child’s recovery and long-term well-being.
Conclusion
For families in Pimpri Chinchwad seeking expert care for their children’s neurological conditions, Neuronest Clinic offers unparalleled pediatric neurosurgical services. With a team of dedicated specialists, state-of-the-art facilities, and a compassionate approach, the clinic ensures that young patients receive the best possible care. Trust Neuronest Clinic to provide the expertise and support needed to navigate the challenges of pediatric neurosurgery and help your child achieve a healthier future.
0 notes
Text
Advancing Brain Health: Neurosurgery Excellence
1. The Brain: Our Command Center
Understanding Neurosurgery
The brain—the epicenter of our thoughts, emotions, and bodily functions—requires specialized care. At Orthomed Multispeciality Hospital, their neurosurgery team combines expertise, precision, and compassion to address a wide range of brain-related conditions.
2. Comprehensive Brain Services
From Diagnostics to Treatment
Orthomed’s neurosurgeons offer a holistic approach:
Brain Tumor Surgery: Precise removal of brain tumors, whether benign or malignant.
Cerebrovascular Surgery: Treating aneurysms, arteriovenous malformations (AVMs), and strokes.
Functional Neurosurgery: Addressing movement disorders like Parkinson’s disease.
3. Minimally Invasive Techniques
Navigating Brain Pathways
Orthomed’s neurosurgery team employs minimally invasive approaches:
Endoscopic Brain Surgery: Using tiny incisions and specialized tools for tumor removal.
Stereotactic Radiosurgery: Precise radiation targeting for brain tumors.
4. Spinal Cord Surgery
Brain-Body Connection
Orthomed’s neurosurgeons specialize in spinal cord procedures:
Spinal Tumor Resection: Safely removing tumors affecting the spinal cord.
Spinal Fusion: Stabilizing the spine to alleviate pain and improve function.
5. Traumatic Brain Injury Care
Urgent Interventions
Orthomed’s neurosurgery team responds swiftly to head injuries:
Craniotomy: Surgical repair of skull fractures.
Intracranial Pressure Monitoring: Vital for severe head trauma cases.
6. Pediatric Neurosurgery
Nurturing Young Minds
Orthomed’s pediatric neurosurgeons address congenital brain conditions:
Hydrocephalus: Managing excess cerebrospinal fluid.
Spina Bifida Repair: Correcting neural tube defects.
7. Rehabilitation and Support
Beyond Surgery
Orthomed’s neurosurgery care extends to rehabilitation:
Neurorehabilitation: Tailored programs for brain injury recovery.
Pain Management Clinics: Addressing chronic pain.
8. Patient-Centric Approach
Compassion and Expertise
Orthomed Multispeciality Hospital’s neurosurgery team understands the impact of brain health on overall well-being. They collaborate with patients, families, and other specialists to provide personalized care.
Conclusion: Navigating Brain Health with Orthomed
Orthomed Multispeciality Hospital ensures that Chennai residents receive advanced neurosurgical care, empowering them to lead healthier lives—one neuron at a time.
Remember, Orthomed Multispeciality Hospital is your partner in health. Explore their services on their website here. Feel free to delve deeper into any of these topics or ask for more information! 🌟
0 notes
Text
What is Hydrocephalus? What is the Main Cause of Hydrocephalus
Medical science is complex, it includes studying topics like diseases, causes, and treatments to help people live healthy lives. One such topic that is crucial to understand in detail is Hydrocephalus.
So, let’s understand the basics about the subject and then we will discuss how you can grab in-depth information and study resources about the subject.
What is Hydrocephalus?
Hydrocephalus is a chronic neurological disorder where the fluid (Cerebrospinal fluid) builds inside the brain.
Though the Cerebrospinal fluid is already present inside the brain and acts as a caution, the excess can permanently damage the brain. It puts pressure on the skull and squashes surrounding brain tissue, which causes problems with physical and mental development. If untreated, it is usually fatal.
The condition is primarily common in infants or people older than 60. The common symptoms of hydrocephalus in infants include:
Increase in the size of an infant's head
A bulge or tense soft spot on the top of the head
Nausea and vomiting
Sleepiness or sluggishness
Poor eating
Seizures
Eyes fixed downward
Problems with muscle tone and strength.
The following are the more common symptoms of hydrocephalus among adults 60 and older:
Loss of bladder control
Memory loss
Progressive loss of reasoning skills.
Trouble walking
Poor coordination or balance.
Remember: The systems among toddlers, children, and middle-aged adults can differ.
Types of Hydrocephalus
The following are the different types of Hydrocephalus:
Congenital hydrocephalus: It is caused by a brain malformation or birth defect that causes excessive cerebrospinal fluid (CSF) to accumulate in brain cavities, called subarachnoid space.
Acquired hydrocephalus: Usually resulting from a stroke, brain tumour, meningitis, or a severe head injury.
Communicating hydrocephalus: A condition when the flow of CSF is blocked after leaving the ventricles. Because CSF can still flow between the brain’s ventricles, it is also called “communicating.”
Non-communicating hydrocephalus: Also known as obstructive hydrocephalus, this type occurs when the narrow pathways connecting the ventricles become blocked.
Normal pressure hydrocephalus: NPH affects primarily those aged 60 and up. It can arise following a stroke, injury, infection, surgery, or hemorrhage.
Hydrocephalus ex-vacuo: Occurs after a stroke, traumatic brain injury, or degenerative disease. In this type, as brain tissue shrinks, the brain's ventricles become larger.
Now that we know the symptoms and types of hydrocephalus, let's dive in to learn about the causes so we can understand the problem better.
What is the Main Cause of Hydrocephalus
There are two distinct cause categories into which hydrocephalus can be classified:
Congenital
Acquired
Congenital hydrocephalus is the result of both genetic and environmental factors working together during foetal development. The following are the main reasons for congenital hydrocephalus:
Spina bifida and other brain and spinal cord (neural tube) defects.
A narrowing of the small passage between the third and fourth ventricles of the brain (aqueductal stenosis).
Complications of premature birth, such as bleeding within ventricles.
Mom has an infection during pregnancy.
On the other hand, Acquired hydrocephalus develops after birth and can affect people of all ages. Below, we have listed the most common causes of acquired hydrocephalus:
Brain or spinal cord tumours
Head trauma
Stroke
Meningitis or other infections of your brain or spinal cord.
After gaining a basic understanding of the subject, let us give you a solution that will help you get more details of the topic: Pediatrics MD Course!

Enroll in an online pediatrics course.
Without the assistance of a professional, it can be challenging to find the study material and understand the basics of the subject.
That is why Dr. Piyush Gupta designed this course for students preparing for an MD in pediatrics.
The course includes pediatrics video lectures along with other crucial resources.
So start your journey toward a good hold on the subject, and enroll in the course now!
#pediatrics md#md in pediatrics#Dr. Piyush Gupta#online pediatrics course#pediatrics video lectures#neurological disorder#cerebrospinal fluid#obstructive#communicating#hypersecretory#NPH
1 note
·
View note
Text
Ultrasound Scans in Pediatrics: Ensuring Healthy Growth and Development
At Ovum Hospital, we prioritize the health and well-being of children, understanding that early detection and monitoring of medical conditions are crucial for ensuring healthy growth and development. One of the most valuable diagnostic tools in pediatric medicine is the ultrasound scan. This non-invasive imaging technique is essential for diagnosing a range of conditions and monitoring various aspects of a child's health. Here’s an in-depth look at the importance of ultrasound scans in pediatrics.
What is an Ultrasound Scan?
An ultrasound scan, also known as sonography, uses high-frequency sound waves to create images of structures within the body. Unlike X-rays or CT scans, ultrasounds do not use ionizing radiation, making them a safer option for imaging, especially in children. Ultrasound scans are performed using a device called a transducer, which emits sound waves and captures the echoes as they bounce back from internal tissues and organs. These echoes are then converted into real-time images.
Common Pediatric Conditions Diagnosed with Ultrasound
Ultrasound scans are incredibly versatile and can be used to diagnose a wide range of conditions in children, including:
Abdominal Issues: Ultrasounds can detect problems in the abdominal organs such as the liver, kidneys, spleen, and intestines. Conditions like appendicitis, gallstones, kidney stones, and liver disease can be accurately diagnosed with an ultrasound scan.
Congenital Anomalies: Prenatal ultrasounds are crucial for detecting congenital anomalies before birth. Postnatal ultrasounds continue to monitor these conditions, such as congenital heart defects or kidney malformations, ensuring early intervention.
Head and Brain Issues: In infants, ultrasounds can evaluate the brain's structure and check for conditions like hydrocephalus, where there is an accumulation of cerebrospinal fluid, or any other brain abnormalities.
Musculoskeletal Disorders: Ultrasounds can assess soft tissue injuries, joint problems, and developmental dysplasia of the hip in infants, helping to ensure proper growth and mobility.
Thyroid Problems: Ultrasound scans are used to examine the thyroid gland, checking for abnormalities such as goiters, nodules, or other thyroid-related issues.
The Benefits of Ultrasound Scans in Pediatrics
Safety: One of the most significant advantages of ultrasound scans is their safety profile. Since they do not use ionizing radiation, they are safe for repeated use, making them ideal for monitoring chronic conditions or performing follow-up exams.
Non-Invasive: Ultrasounds are non-invasive, which means they do not require any incisions or injections. This aspect is particularly beneficial for children, who may be more sensitive to invasive procedures.
Real-Time Imaging: Ultrasound scans provide real-time images, allowing for immediate assessment and diagnosis. This real-time capability is especially useful in emergency situations where quick decision-making is required.
Versatility: Ultrasounds can be used to examine almost any part of the body. From the abdomen to the brain, and from muscles to joints, the versatility of ultrasound scans makes them indispensable in pediatric care.
Cost-Effective: Compared to other imaging modalities like MRI or CT scans, ultrasound scans are generally more affordable. This cost-effectiveness makes them accessible and a preferred first-line diagnostic tool in many cases.
How Ultrasound Scans Contribute to Healthy Growth and Development
Early Detection and Intervention: Early detection of abnormalities or conditions through ultrasound scans can lead to timely intervention and treatment. For example, identifying a congenital heart defect early on can allow for surgical correction before it causes significant health issues.
Monitoring Growth and Development: Regular ultrasound scans can monitor a child’s growth and development, ensuring that organs are developing correctly and identifying any potential issues early.
Guiding Treatment Plans: Ultrasound scans provide detailed information that can guide treatment plans. Whether it's determining the exact location of a kidney stone or assessing the extent of an abdominal infection, the information gathered from an ultrasound scan is invaluable for creating effective treatment strategies.
Reassurance for Parents: For parents, having access to a safe and reliable diagnostic tool like ultrasound provides reassurance. Knowing that any potential health issue can be detected and monitored without exposing their child to harmful radiation offers peace of mind.
Choosing the Right Facility for Pediatric Ultrasound Scans
When it comes to ensuring the best care for your child, choosing the right medical facility is crucial. At Ovum Hospital, we pride ourselves on being a leading provider of pediatric healthcare services, including ultrasound scans. Our state-of-the-art equipment and experienced team of pediatric specialists ensure that every ultrasound scan is performed with the highest level of precision and care.
If you are looking for a reliable place for an ultrasound scan Bangalore, Ovum Hospital is your best choice. Our commitment to providing comprehensive and compassionate care makes us a trusted name in pediatric healthcare.
Conclusion
Ultrasound scans are a cornerstone of pediatric diagnostics, offering a safe, non-invasive, and effective way to monitor and ensure healthy growth and development in children. At Ovum Hospital, we utilize advanced ultrasound technology to provide accurate diagnoses and guide treatment plans, reinforcing our reputation as a top gynecologist hospital Bangalore residents trust. If you need an ultrasound scan Bangalore for your child, trust Ovum Hospital to deliver the highest standard of care.
0 notes
Text
Pediatric Neurosurgery in Borivali West: Expert Care for Your Child's Neurological Needs

When it comes to your child’s health, especially concerning neurological issues, you want the best care available. Pediatric neurosurgery in Borivali West is a highly specialized field focusing on diagnosing and treating neurological conditions in children. In Borivali West, Dr. Bhavesh Doshi offers unparalleled expertise and compassionate care for young patients facing these complex challenges.
Understanding Pediatric Neurosurgery
Pediatric neurosurgery involves surgical procedures to address neurological disorders in children, ranging from newborns to teenagers. These conditions may include congenital anomalies, brain tumors, spinal cord problems, and traumatic injuries. The primary goal is to restore normal function or improve the quality of life for the affected child.
Why Choose Dr. Bhavesh Doshi in Borivali West?
1. Expertise and Experience: Dr. Bhavesh Doshi is a leading pediatric neurosurgeon in Borivali West, known for his extensive experience and successful outcomes. With a deep understanding of the delicate and intricate nature of pediatric neurosurgery, he ensures that each child receives the best possible care tailored to their unique needs.
2. Comprehensive Care: At Dr. Doshi’s clinic, the focus is on comprehensive care that addresses the physical, emotional, and developmental needs of young patients. From the initial diagnosis to post-surgical recovery, every step is carefully planned and executed to ensure the best results.
3. State-of-the-Art Facilities: The clinic is equipped with advanced technology and state-of-the-art facilities, ensuring that all procedures are performed with the highest standards of safety and precision. This commitment to excellence ensures that children receive the best possible care in a comfortable and supportive environment.
Common Pediatric Neurosurgical Procedures
1. Brain Tumor Surgery: Brain tumors in children can be benign or malignant. Early diagnosis and surgical intervention are crucial for successful treatment. Dr. Doshi uses advanced imaging techniques and minimally invasive surgical methods to remove tumors with precision.
2. Hydrocephalus Treatment: Hydrocephalus, characterized by an accumulation of cerebrospinal fluid in the brain, requires timely intervention to prevent brain damage. Shunt systems and endoscopic third ventriculostomy (ETV) are commonly used procedures to treat this condition.
3. Spinal Cord Surgery: Conditions such as tethered spinal cord, spina bifida, and scoliosis may require surgical correction. Dr. Doshi’s expertise ensures that these delicate procedures are performed with utmost care to minimize risks and promote recovery.
4. Trauma Surgery: Accidents and injuries can lead to severe neurological damage. Prompt surgical intervention can significantly improve outcomes for children suffering from traumatic brain or spinal cord injuries.
Holistic Approach to Pediatric Care
At Dr. Bhavesh Doshi’s clinic, the approach to pediatric neurosurgery is holistic. This means considering not just the immediate surgical needs but also the long-term developmental and psychological well-being of the child. The team works closely with pediatricians, neurologists, physiotherapists, and psychologists to provide integrated care that supports overall recovery and development.
Support for Families
Navigating a child’s neurological condition can be overwhelming for families. Dr. Doshi and his team offer extensive support and guidance, ensuring that parents are well-informed and involved in every decision-making process. Educational resources, counseling, and follow-up care are integral parts of the patient journey, providing families with the tools they need to support their child’s recovery and well-being.
Book an Appointment
If your child is experiencing neurological issues, don’t wait to seek expert care. Dr. Bhavesh Doshi is here to help. With a proven track record and a compassionate approach, he is dedicated to improving the lives of young patients through exceptional pediatric neurosurgery in Borivali West.
Ensure your child receives the best possible care for their neurological needs with Dr. Bhavesh Doshi. Contact us at 9820565205 today to learn more and take the first step towards a healthier future for your child or click here for Direction to reach Clinic.
#gynecologist in borivali#maternity hospital in borivali#pediatric surgeon in mumbai#gynecologist in mira road#best gynecologist in borivali#pediatric surgeon in mumbai.#gynecologist in mumbai#dr. bhavesh doshi#dhanvantari hospital#abortion clinic in mumbai
0 notes