#carfilzomib generic
Explore tagged Tumblr posts
Text
Insider Insights: Understanding Multiple Myeloma
Multiple Myeloma is a type of cancer that explicitly affects plasma cells essential components of our immune system. These plasma cells go rogue, multiplying uncontrollably and crowding out healthy cells, leading to various health challenges. It might not be a household name, but its impact is significant. In this section, we'll unravel the basics, from what Multiple Myeloma is to why it's essential to comprehend it.
Multiple Myeloma: Incidence and Prevalence
Multiple Myeloma, a form of blood cancer might be relatively rare, accounting for just 1.8% of all new cancer cases in the United States. However, its impact is profound. According to the American Cancer Society, approximately 34,920 new cases were diagnosed in 2021, highlighting the importance of understanding its various aspects.
Multiple Myeloma: Symptoms & Signs
Multiple Myeloma is often tricky to detect in its early stages. It usually manifests through symptoms such as
Bone pain (especially in the spine, chest, or hips)
Recurrent infections
Fatigue
Weight loss
Mental fogginess or confusion
Constipation
It is essential to identify these signs early as it helps take timely action and address the issue. Medicines like Carfilnat 60mg Carfilzomib Injection, are used to treat Multiple Myeloma.
Diagnostic Tests for Multiple Myeloma
Getting to the bottom of Multiple Myeloma involves a series of diagnostic tests.
Blood and Urine Analyses
These tests play a crucial role in detecting abnormalities associated with Multiple Myeloma. Blood tests may reveal elevated levels of specific proteins (M proteins made by myeloma cells) or abnormalities (beta-2-microglobulin) in blood cell counts. Urine tests can detect abnormal proteins (Bence Jones proteins) that may indicate the presence of the disease.
Imaging Tests like X-rays
X-rays provide a visual insight into the bones, helping identify any lesions or fractures caused by Multiple Myeloma. This diagnostic tool aids in assessing the extent of bone involvement and contributes to the staging of the disease.
Bone Marrow Tests
Bone marrow tests such as Bone marrow biopsies & aspirations involve extracting a small sample of bone marrow for examination. This procedure helps determine the presence and activity of myeloma cells. It's a crucial step in diagnosing Multiple Myeloma and provides valuable information for planning an effective treatment strategy.
Each piece of this diagnostic puzzle contributes to a clearer picture of the condition.
Staging System
Understanding the staging system helps map out the extent of the disease.
Stage I
Smoldering or asymptomatic myeloma.
M protein in the blood or urine but no symptoms or evidence of organ damage.
Lower levels of abnormal plasma cells in the bone marrow.
Stage II
Calcium levels may be normal or slightly elevated.
Moderate levels of abnormal plasma cells in the bone marrow.
Stage III
Multiple Myeloma has spread extensively.
There are signs of kidney problems.
Calcium levels might be elevated.
Higher levels of abnormal plasma cells in the bone marrow.
This knowledge guides healthcare professionals in tailoring each individual's most effective treatment plan.
Treatment Options:-
Chemotherapy
Chemotherapy, a reliable cancer treatment, is a critical player in battling Multiple Myeloma. This treatment involves using powerful drugs to target and control the abnormal plasma cells responsible for the disease. It targets and controls abnormal plasma cell multiplication and growth to restore balance to the body's blood cell production.
Stem Cell Transplantation
Stem cell transplantation, a sophisticated approach, rejuvenates the bone marrow. In this procedure, the patient's stem cells are harvested and reintroduced into the body after being enhanced in a controlled environment. This process acts like a reset button for the immune system, enhancing its ability to combat Multiple Myeloma.
Targeted Therapy
Enter the era of targeted therapy with Carfilnat 60mg Carfilzomib Injection, containing the potent carfilzomib. This modern approach disrupts the growth mechanisms of Multiple Myeloma cells with precision, offering a more tailored and effective treatment.
Carfilnat 60mg Carfilzomib Injection
Carfilnat 60mg is a form of targeted therapy, meaning it focuses explicitly on the growth mechanisms of Multiple Myeloma cells with precision.
This Carfilzomib injection disrupts the intricate processes fueling cancerous cells, halting their uncontrolled growth. It's like sending a highly specialized task force to dismantle the essential components driving the disease. This targeted approach is designed to minimize the damage to healthy cells, making the treatment more tolerable for patients with relapsed multiple Myeloma (when the cancer returns) and refractory multiple Myeloma (when the cancer no longer responds to treatment).
Benefits of Carfilnat 60mg Carfilzomib Injection
Precision Targeting
Carfilnat 60mg injection, containing carfilzomib, offers a precision-targeted approach to treating Multiple Myeloma. It blocks or turns off signals that encourage cancer cells to grow or multiply and Modify proteins within cancer cells that cause those cells to die.
Improved Disease Control
Carfilnat 60mg Carfilzomib injection's ability to disrupt the abnormal growth of myeloma cells plays a crucial role in controlling the progression of Multiple Myeloma by preventing new blood vessels from forming, which cuts off blood supply to the tumor.
Minimized Side Effects
By honing in on cancer cells precisely, Carfilnat 60mg Carfilzomib injection reduces the impact on healthy cells, leading to a lower incidence of side effects. It delivers the toxins that kill cancer cells without harming healthy cells. This targeted approach enhances the treatment's overall tolerability, improving patients' quality of life.
Conclusion:-
Multiple Myeloma is more than statistics or treatments; it's about individuals facing it. Each story is acknowledged as unique, and each journey is seen as a testament to strength and hope. The collective goal is highlighted – striding towards a future where Multiple Myeloma is understood and conquered.
Carfilnat 60mg Carfilzomib Injection brings many benefits, ranging from precision targeting and enhanced treatment efficacy to minimized side effects and improved disease control. As a modern advancement in Multiple Myeloma treatment, it represents hope and progress in the ongoing battle against this complex condition.
#carfilnat injection#carfilnat 60mg#carfilnat price#carfilzomib brand name#carfilzomib cost#carfilzomib generic#carfilzomib injection#carfilzomib price#buy carfilzomib#carfilzomib injection price"
0 notes
Text
Multiple Myeloma: An Incurable B-cell Malignancy and the Challenge of Recurrence
Multiple myeloma is a complex and incurable B-cell malignancy characterized by the uncontrolled proliferation of plasma cells within the bone marrow. Despite significant progress in multiple myeloma treatment, the disease remains chronic, with cycles of remission and relapse.
Understanding Multiple Myeloma Diagnosis and Prognosis
Early multiple myeloma diagnosis is crucial for managing disease progression. Diagnostic methods include blood markers, bone marrow biopsies, and imaging techniques. Despite aggressive treatments, the multiple myeloma cure rate remains low, and relapse occurs due to the persistence of resistant cancer cells.
Current Treatment Options for Multiple Myeloma
The multiple myeloma treatment landscape includes chemotherapy drugs for multiple myeloma, targeted therapies, and immunotherapies. One of the most effective approaches involves stem cell transplantation, which can prolong remission. Key treatments include Revlimid and proteasome inhibitors like Carfilzomib. Immunotherapy is also emerging as a promising approach, with ongoing clinical trials exploring new possibilities.
Challenges in Managing Multiple Myeloma Recurrence
One of the most significant challenges is disease relapse. The continuous evolution of multiple myeloma drugs has led to new therapeutic developments to combat resistance. The newest treatment for multiple myeloma includes monoclonal antibodies, CAR-T cell therapy, and next-generation proteasome inhibitors. However, no therapy has yet provided a definitive cure, emphasizing the need for ongoing research and innovation in multiple myeloma therapeutics.
Nutrition and Future Outlook
A comprehensive approach, including proper nutrition and adherence to multiple myeloma treatment guidelines, can significantly improve patients’ quality of life. As research advances, novel targeted therapies and evolving treatment protocols continue to enhance patient outcomes.
While multiple myeloma remains incurable, continuous advancements in treatments and clinical trials provide hope for better disease management and extended survival.
While multiple myeloma remains incurable, advancements in treatments and ongoing multiple myeloma clinical trials provide hope for better disease management and prolonged survival.
Latest Blogs Offered By DelveInsight:
Insights Into The Cutaneous T-cell Lymphoma Treatment Market
Roche’s HEMLIBRA: A Game Changer in Hemophilia A Treatment Landscape
Emerging Role of Digital Health in the Field of Oncology
How Will Emerging Therapies Drift the Amyotrophic Lateral Sclerosis (ALS) Treatment Landscape
How are Technological Trends and Innovations Reshaping the Dementia Care
Latest Blogs Offered By DelveInsight:
Medtronic Secures FDA Green Light for Affera™ Mapping and Ablation System Alongside Sphere-9™ Catheter; Precision Optics Gets FDA 510(k) Clearance; Abbott Launches New Clinical Trial Aimed at Enhancing Care for Advanced Heart Failure Patients; Fresenius Medical Care’s Study Confirms Efficacy of New Anemia Therapy Software in Enhancing Outcomes for Hemodialysis Patients; Inspira™ Announces New Distribution Center to Support INSPIRA™ ART100’s U.S. Introduction; WellSky Expands Home Care Offerings with Acquisition of Bonafide
7 Key Technologies Pioneering Cybersecurity in the Healthcare Sector
FDA Grants Orphan Status to MDL-101 for LAMA2-CMD; Pfizer’s ABRYSVO Approved for High-Risk Adults (18-59); KIND’s AND017 Gains Orphan Designation for Sickle Cell Disease; HiberCell’s HC-7366 Fast-Tracked for AML; ORLYNVAH Approved for Uncomplicated UTIs
Pfizer’s ABRYSVO Outpaces GSK’s AREXVY with Expanded FDA Approval – But Can It Sustain the Momentum?
CAR-T Cells vs. CAR-Exosome Agents: Exploring the Future of Cancer Immunotherapy
Another Reports Offered By Delveinsight
cmo contract manufacturing organization | keynote-a18 | generic for stelara | mucodyne | uromune usa | drugs for hyperkalemia | electronic devices that help the heart maintain normal rhythm | camoteskimab | artificial intelligence app iphone | msa p disease | gilead adc | what meds are used for ptsd | lack of interoperability in healthcare | d&d pharmatech | emicizumab kxwh | nxstage crrt | neuropathic ocular pain | chemo induced diarrhea | nf type 1 treatment | whats mrd | whats bci | eular 2024 abstract | does pritelivir cure herpes | ml-004 | copd statistics in the united states | bms earnings call transcript | history of breast cancer awareness month | what are some cardiac diseases
About DelveInsight
DelveInsight is a premier market research and consulting firm specializing in life sciences and healthcare. We provide in-depth insights to help pharmaceutical, biotechnology, and medical device companies navigate a dynamic and competitive industry
Contact Information
Kanishk
0 notes
Text
Encorafenib in Specialty Clinics: A Rising Trend in Cancer Treatment

Encorafenib Market: Analyzing Growth, Trends, and Future Potential
Introduction
The Encorafenib Market is witnessing significant growth as the demand for targeted cancer therapies rises globally. Encorafenib, a BRAF kinase inhibitor, has gained prominence in the pharmaceutical sector due to its effectiveness in treating melanoma and colorectal cancer. With increasing research and development activities, the Encorafenib Market Size is expected to expand, driven by rising cancer prevalence and advancements in precision medicine.
Request Sample Copy:
https://wemarketresearch.com/reports/request-free-sample-pdf/encorafenib-market/1496
Encorafenib Market Size and Share
The Encorafenib Market Share is dominated by leading pharmaceutical companies investing in innovative therapies and clinical trials. North America holds a substantial portion of the market due to strong healthcare infrastructure, government initiatives, and higher adoption rates of advanced oncology treatments. Europe and the Asia-Pacific region are also emerging as key players, with a growing emphasis on personalized medicine and improved healthcare access.
Market Value and Growth Trends
The Encorafenib Market Value is projected to rise steadily, with increased awareness about targeted therapies and a surge in regulatory approvals. Key factors fueling Encorafenib Market Growth include:
Rising Incidence of Cancer: The growing prevalence of melanoma and colorectal cancer is a major driver.
Technological Advancements: Innovations in drug formulations and combination therapies enhance treatment efficacy.
Government Support: Regulatory approvals and research funding are boosting market expansion.
Strategic Collaborations: Partnerships among biotech firms and pharmaceutical giants are fostering research and development efforts.
Market Trends and Potential
Key Encorafenib Market Trends shaping the industry include:
Combination Therapies: Encorafenib is often combined with other inhibitors, such as binimetinib, to improve treatment outcomes.
Increasing Clinical Trials: Ongoing studies are exploring expanded applications for Encorafenib in different cancer types.
Expanding Healthcare Infrastructure: Emerging economies are investing in advanced cancer treatment options, providing lucrative opportunities for market players.
The Encorafenib Market Potential remains high, especially with growing research on expanding its indications beyond melanoma and colorectal cancer. The pharmaceutical industry is focusing on optimizing dosage regimens and minimizing side effects, which could further drive adoption rates.
Encorafenib Market Forecast and Analysis
The Encorafenib Market Forecast suggests a steady upward trajectory, with a compounded annual growth rate (CAGR) expected to rise significantly over the next decade. Analysts predict that continuous investment in oncology research, coupled with increasing patient awareness, will contribute to sustained market expansion.
A thorough Encorafenib Market Analysis indicates that challenges such as high treatment costs and regulatory hurdles may slightly hinder growth. However, ongoing efforts to improve drug accessibility and reduce prices through generic alternatives and insurance coverage may counterbalance these challenges.
Related Report:
Carfilzomib Market
Ibrutinib Market
Optical Imaging Systems Market
Conclusion
The Encorafenib Market is poised for robust growth, fueled by increasing cancer cases, technological advancements, and a strong pipeline of clinical trials. As industry players continue to invest in research and development, the market is expected to witness remarkable advancements, offering improved treatment options for patients worldwide. By leveraging the latest trends and addressing market challenges, stakeholders can unlock the full potential of this dynamic industry.
#Encorafenib Market#Encorafenib Market Trends#Encorafenib Market Size#Encorafenib Market Analysis#Encorafenib Market Growth#Encorafenib Market Segmentation#Avelumab Market Forecast
0 notes
Text
Comprehensive Overview of Multiple Myeloma Treatment Methods: A Doctor's Perspective
Multiple myeloma is a challenging cancer that affects plasma cells in the bone marrow. Early detection and treatment are critical to managing the disease. With various multiple myeloma treatment methods available today, we can significantly improve patient outcomes. This post will explore the most common treatments, including chemotherapy, targeted therapy, immunotherapy, and drugs like lenalidomide.

Standard Treatment Methods for Multiple Myeloma
Chemotherapy
Chemotherapy is a cornerstone of multiple myeloma treatment. It works by killing fast-growing cells, including cancerous plasma cells. Common chemotherapy drugs used include melphalan and cyclophosphamide.
Chemotherapy is often combined with other treatments to increase effectiveness. For example, it can be used before a stem cell transplant or in cases of aggressive disease. Despite its benefits, chemotherapy can cause side effects such as fatigue, nausea, and infections due to a weakened immune system.
Targeted Therapy
Targeted therapy specifically attacks proteins or genes that are key to cancer cell growth. Unlike chemotherapy, which affects both healthy and cancerous cells, targeted therapy is more precise.
Drugs like bortezomib (Velcade), carfilzomib (Kyprolis), and ixazomib (Ninlaro) are common targeted treatments for multiple myeloma. They work by inhibiting proteasomes, causing cancer cells to die.
Targeted therapies are often combined with other drugs, such as lenalidomide, to boost their effectiveness. These drugs generally have fewer side effects than traditional chemotherapy, although they can cause neuropathy or gastrointestinal issues.
Immunotherapy
Immunotherapy is one of the most promising advancements in multiple myeloma treatment. This therapy uses the body's immune system to target and destroy cancer cells.
Lenalidomide (Revlimid) and pomalidomide (Pomalyst) are immunomodulatory drugs widely used in newly diagnosed and relapsed cases of multiple myeloma. Lenalidomide enhances the immune system’s ability to kill cancer cells and prevents the formation of blood vessels that feed tumors.
Lenalidomide is often combined with dexamethasone, a corticosteroid that enhances its anti-cancer effects. However, side effects such as low blood counts, fatigue, and an increased risk of blood clots need to be managed closely.
Stem Cell Transplantation: A Curative Option
For some patients, stem cell transplantation offers a more curative approach. Two types of transplants are used: autologous (using the patient’s own stem cells) and allogeneic (using donor stem cells).
In many cases, patients undergo autologous stem cell transplantation after high-dose chemotherapy to reduce cancer cells. Although it can lead to long-term remission, there are risks, including infection and relapse.
Lenalidomide: A Pillar in Multiple Myeloma Therapy
Lenalidomide is a central drug in the treatment of multiple myeloma. It is used in both newly diagnosed and relapsed patients, often combined with other treatments like bortezomib and dexamethasone.
One of the biggest challenges with lenalidomide is its cost. The price of lenalidomide can range from $10,000 to $20,000 per month, making it difficult for many patients to afford. Despite its cost, lenalidomide is highly effective at prolonging progression-free survival and improving quality of life.
The Cost of Multiple Myeloma Treatment
The cost of multiple myeloma treatments can be significant. Beyond lenalidomide, other drugs like bortezomib and carfilzomib are also expensive, especially when used in combination therapy.
In addition to drug costs, patients often incur expenses related to stem cell transplants, hospital stays, and supportive care like blood transfusions or bone-strengthening medications. Navigating insurance coverage and patient assistance programs is crucial for many patients to manage these costs effectively.
Conclusion: The Future of Multiple Myeloma Treatment
The treatment landscape for multiple myeloma is evolving rapidly, with exciting new therapies like CAR-T cell therapy and bispecific antibodies showing promise in clinical trials. As a doctor, I am hopeful that these advancements will lead to even better outcomes for my patients.
For now, the key to successful treatment lies in a personalized approach that balances the effectiveness of therapies like chemotherapy, immunotherapy, and targeted therapy with their side effects and costs. Despite the high cost of medications like lenalidomide, their benefits make them invaluable tools in the fight against multiple myeloma.
Frequently Asked Questions (FAQ)
1. What is the most common treatment for multiple myeloma?
The most common treatment for multiple myeloma typically includes chemotherapy, targeted therapy, and immunotherapy. A combination of these treatments is often used depending on the patient’s stage and health. Stem cell transplants are also considered for patients eligible for more aggressive treatments.
2. How does lenalidomide help in treating multiple myeloma?
Lenalidomide (Revlimid) is an immunomodulatory drug that helps enhance the immune system’s ability to attack cancer cells. It also prevents the growth of blood vessels that tumors need to survive. Lenalidomide is often combined with other medications like dexamethasone and is used in both newly diagnosed and relapsed patients.
3. Why is the cost of multiple myeloma treatment so high?
The cost of multiple myeloma treatments can be high due to the expense of newer therapies like lenalidomide, bortezomib, and carfilzomib. Additionally, stem cell transplants, hospital stays, and supportive care add to the overall cost. Many patients rely on insurance and assistance programs to help cover these expenses.
1 note
·
View note
Text
Substantially Pure Carfilzomib Amorphous for Generic Launch
We manufacture Carfilzomib amorphous API at our cGMP API manufacturing facility, successfully inspected by international regulatory authorities.
0 notes
Text
0 notes
Text
The Evolving Landscape of Multiple Myeloma Therapies

Current Treatments for Multiple Myeloma The treatment of multiple myeloma has advanced significantly, providing patients with a range of options that enhance prognosis. Diagnosis relies on blood tests, imaging, and bone marrow examination. Current therapies include chemotherapy drugs, targeted treatments, and stem cell transplants for eligible patients. Key medications include Revlimid, Carfilzomib (a proteasome inhibitor), and various immunotherapies, which all work to manage the disease and improve survival rates.
Leading Companies in Multiple Myeloma Treatment The market for multiple myeloma drugs Market is largely dominated by major pharmaceutical companies investing in groundbreaking therapies. These companies are focused on developing medications that improve patient outcomes. The therapeutic landscape includes proteasome inhibitors, monoclonal antibodies, and immune-modulating agents. New entrants are making valuable contributions by expanding clinical trials, paving the way for novel treatments and improving existing therapies.
Trends and Future Outlook in the Multiple Myeloma Market The multiple myeloma treatment market is expanding rapidly, driven by progress in research and drug development. The focus is shifting toward personalized medicine, combining multiple therapies with direct treatment and nutrition strategies. While a cure for multiple myeloma remains elusive, emerging treatments, such as CAR-T cell therapy and gene editing, are gaining momentum. There is also a heightened focus on managing recurrence, with companies working on next-generation drugs to address treatment resistance. Additionally, advancements in treatment guidelines are improving patient care.
Conclusion The multiple myeloma treatment landscape is evolving, offering promising new options for patients. The introduction of drugs like cartizomib and other cutting-edge treatments is shaping the future of the market. Although challenges remain, ongoing research, clinical trials, and advancements in the drug market are paving the way for better patient outcomes and extended survival rates.
Latest Blogs Offered By DelveInsight:
Medtronic Secures FDA Green Light for Affera™ Mapping and Ablation System Alongside Sphere-9™ Catheter; Precision Optics Gets FDA 510(k) Clearance; Abbott Launches New Clinical Trial Aimed at Enhancing Care for Advanced Heart Failure Patients; Fresenius Medical Care’s Study Confirms Efficacy of New Anemia Therapy Software in Enhancing Outcomes for Hemodialysis Patients; Inspira™ Announces New Distribution Center to Support INSPIRA™ ART100’s U.S. Introduction; WellSky Expands Home Care Offerings with Acquisition of Bonafide
7 Key Technologies Pioneering Cybersecurity in the Healthcare Sector
FDA Grants Orphan Status to MDL-101 for LAMA2-CMD; Pfizer’s ABRYSVO Approved for High-Risk Adults (18-59); KIND’s AND017 Gains Orphan Designation for Sickle Cell Disease; HiberCell’s HC-7366 Fast-Tracked for AML; ORLYNVAH Approved for Uncomplicated UTIs
Pfizer’s ABRYSVO Outpaces GSK’s AREXVY with Expanded FDA Approval – But Can It Sustain the Momentum?
CAR-T Cells vs. CAR-Exosome Agents: Exploring the Future of Cancer Immunotherapy
Another Reports Offered By Delveinsight
radicava mechanism of action | how many people have cidp | therapy light benefits | internet of things in medical | health monitoring apps | cardiac monitoring devices | immunomodulatory drugs | izervay reviews | adenovirus stages | what is hemoglobinuria | peripheral artery disease prevalence | arteriotomy | orthopedic implant companies | ropressa | oceanic af | cervical dysplasia stages | tev-48574 | welireg fda approval | nevro hfx programs | axillary hidrosis | lentiginous definition | voquezna gerd | visiox pharma | fluid management systems | cln1 disease | can achondroplasia be treated
Contact Information
Kanishk
0 notes
Text
Avelumab in Hospital Pharmacies and Retail Pharmacies: Market Growth Trends

Avelumab Market: Growth, Trends, and Future Prospects
Introduction
The Avelumab Market has been experiencing steady growth due to increasing adoption of immunotherapy in cancer treatment. Avelumab, a PD-L1 inhibitor, has shown significant promise in treating various malignancies, including Merkel cell carcinoma and urothelial carcinoma. With growing investments in oncology research, the Avelumab Market Size is projected to expand, driven by rising cancer prevalence and enhanced healthcare infrastructure.
Request Sample Copy:
https://wemarketresearch.com/reports/request-free-sample-pdf/avelumab-market/1495
Avelumab Market Size and Share
The Avelumab Market Share is primarily held by leading pharmaceutical companies that focus on research and development to improve immunotherapeutic outcomes. North America dominates the market due to advanced medical research facilities, while Europe and Asia-Pacific are witnessing increasing demand due to improved healthcare policies and growing patient awareness.
Market Price and Growth Trends
The Avelumab Market Price is influenced by factors such as drug development costs, regulatory approvals, and market competition. The Avelumab Market Growth is supported by:
Rising Cancer Incidences: The increasing burden of cancer worldwide is a key driver.
Innovative Treatment Approaches: Advancements in combination therapies enhance efficacy and patient outcomes.
Regulatory Support: Favorable policies and approvals are accelerating market expansion.
Strategic Collaborations: Partnerships between biotech firms and pharmaceutical giants are fostering innovation.
Market Trends and Potential
Key Avelumab Market Trends include:
Increased Use in Combination Therapies: Avelumab is often combined with other immunotherapies to boost treatment success rates.
Expanding Clinical Trials: Ongoing research is exploring its efficacy in additional cancer types.
Improved Access to Immunotherapy: Growing healthcare investments are making Avelumab more accessible in developing regions.
The Avelumab Market Potential remains high, with expanding applications in oncology and immunotherapy advancements. Pharmaceutical firms are focusing on optimizing treatment protocols and reducing side effects to enhance patient compliance.
Avelumab Market Forecast and Analysis
The Avelumab Market Forecast predicts sustained growth, with a promising compound annual growth rate (CAGR) over the next decade. Analysts expect continued investments in immuno-oncology to drive market expansion.
A detailed Avelumab Market Analysis highlights potential challenges such as high treatment costs and stringent regulatory requirements. However, increasing efforts to improve affordability and accessibility through insurance coverage and generic alternatives may help mitigate these challenges.
Related Report:
Carfilzomib Market
Ibrutinib Market
Optical Imaging Systems Market
Conclusion
The Avelumab Market is poised for substantial growth, driven by rising cancer cases, technological innovations, and expanding clinical applications. With increasing research efforts and industry collaborations, the market is expected to witness significant advancements, offering improved treatment options for patients worldwide. By capitalizing on emerging trends and addressing key challenges, stakeholders can unlock the full potential of this rapidly evolving industry.
#Avelumab Market#Avelumab Market trends#Avelumab Market Size#Avelumab Market Analysis#Avelumab Market Growth#Avelumab Market Segmentation#Avelumab Market Development
0 notes
Text
0 notes
Text
0 notes
Text
Carfilzomib Market Statistics, Segment, Trends and Forecast to 2034

TheCarfilzomib Market: Trends, Opportunities, and Future Outlook
Introduction
In recent years, the pharmaceutical industry has seen significant advancements in the treatment of multiple myeloma, a type of cancer that affects plasma cells in the bone marrow. Among these advancements, Carfilzomib has emerged as a critical player. This proteasome inhibitor, marketed under the brand name Kyprolis, has made substantial impacts in the management of multiple myeloma. In this blog, we will explore the current state of theCarfilzomib market, its growth drivers, opportunities, and future outlook.
Free Sample pdf copy:
What is Carfilzomib?
Carfilzomib is a next-generation proteasome inhibitor used in the treatment of multiple myeloma, especially in patients who have relapsed or are refractory to other therapies. Unlike its predecessor, bortezomib, Carfilzomib is known for its more selective action on the proteasome, potentially leading to fewer side effects and enhanced efficacy. Approved by the FDA in 2012, it has since become an integral part of combination therapies for multiple myeloma.
Carfilzomib Market Landscape
Growth Drivers
Rising Incidence of Multiple Myeloma: The increasing number of multiple myeloma cases globally is a significant driver for the Carfilzomib market. As the global population ages, the prevalence of multiple myeloma is expected to rise, leading to a higher demand for effective treatments.
Advancements in Treatment Protocols: Carfilzomib is often used in combination with other drugs like lenalidomide and dexamethasone, enhancing its effectiveness. This combination therapy approach has shown promising results, making Carfilzomib a preferred choice in advanced treatment regimens.
Increasing Awareness and Diagnosis: Improved diagnostic techniques and greater awareness about multiple myeloma have led to earlier detection and treatment. This trend is likely to boost the demand for Carfilzomib as part of first-line and subsequent lines of treatment.
Ongoing Clinical Trials: Continuous research and clinical trials exploring new indications and combination therapies for Carfilzomib are expanding its potential market. Studies focusing on different stages of multiple myeloma and other cancers could open new avenues for Carfilzomib use.
Carfilzomib Market Challenges
High Cost of Treatment: Carfilzomib is a high-cost drug, and its price can be a barrier to access, particularly in developing countries. The high cost of treatment may limit its market potential and lead to a preference for alternative therapies.
Side Effects and Resistance: Although Carfilzomib is well-tolerated, some patients may experience side effects such as cardiovascular issues or renal complications. Additionally, resistance to the drug can develop, leading to the need for alternative therapies.
Competition from Other Therapies: The multiple myeloma treatment landscape is competitive, with several other proteasome inhibitors and novel therapies in development. This competition can impact Carfilzomib’s market share and pricing strategies.
Market Opportunities
Expanding Indications: Research into expanding the use of Carfilzomib to other types of cancer or earlier stages of multiple myeloma could provide significant market opportunities. Successful clinical trials in these areas could lead to new indications and broaden its market.
Developing Markets: As healthcare infrastructure improves in developing regions, there ispotential for growth in these Carfilzomib Market Strategic partnerships and pricing strategies could enhance Carfilzomib’s reach in these areas.
Combination Therapies: Exploring new combination therapies and optimizing treatment regimens can improve patient outcomes and increase the demand for Carfilzomib. Collaborations with other pharmaceutical companies and research institutions could drive innovation in this space.
Carfilzomib Market Future Outlook
The Carfilzomib market is poised for continued growth driven by advancements in treatment protocols and increasing prevalence of multiple myeloma. However, challenges such as high treatment costs and competition from alternative therapies will require strategic planning and innovation.
The future of Carfilzomib will likely involve ongoing research and development to expand its therapeutic indications and improve patient outcomes. As the market evolves, stakeholders will need to navigate these dynamics to maximize the potential of Carfilzomib in the treatment of multiple myeloma and beyond.
Conclusion
Carfilzomib Market has made asignificant impact in the management of multiple myeloma, and its market prospects remain strong. With ongoing advancements in treatment protocols, increasing awareness, and expanding indications, Carfilzomib is set to continue playing a crucial role in cancer therapy. However, addressing market challenges and seizing emerging opportunities will be essential for stakeholders to fully realize the potential of this innovative drug.
#Carfilzomib Market Share#Carfilzomib Market Demand#Carfilzomib Market Scope#Carfilzomib Market Analysis#Carfilzomib Market Trend
0 notes
Text
Blood Cancer Drugs Market to Generate Exciting Opportunities in the Industry by 2027
The global blood cancer drugs market is anticipated to reach USD 55.6 billion by 2025 according to a new report published by Polaris Market Research. The report ‘Blood Cancer Drugs Market [By Blood Cancer Type (Leukemia (Acute Myeloid Leukemia, Chronic Myeloid Leukemia, Acute Lymphoblastic Leukemia, Chronic Lymphocytic Leukemia), Lymphoma (Hodgkin Lymphoma, Non-Hodgkin Lymphoma (B-Cell Lymphoma, T-Cell Lymphoma)), and Myeloma; By Drugs (Rituaxan/Mabthera (Rituximab), Gleevac/Glivec (Imatinib), Revlimid (Lenalidomide), Velcade (Bortezomib), Tasigna (Nilotinib), Pomalyst (Pomalidomide), Vidaza (Azacitidine), Kyprolis (Carfilzomib), Adcetris (Brentuximab Vedotin), and Others); By Treatment Approaches (Chemotherapeutic, mAbs/Targeted Therapies, and Immunotherapeutic); By Region]: Market Size & Forecast, 2017 – 2025’ provides insights on the current market scenario and the future prospects.
The demand for blood cancer drug is primarily driven by growing death incidences by blood cancer, and continuous innovation for developing novel treatments with the help of several ongoing clinical trials. Moreover, increasing research and development of biological and targeted therapies as treatment will spur the blood cancer drugs market during the upcoming period. However, the high price of drugs and the stringent government policies will limit the growth of blood cancer drugs market during the forecast period.
Get Sample copy of this report: https://www.polarismarketresearch.com/industry-analysis/global-blood-cancer-drugs-market/request-for-sample
Most of the blood cancers start in the bone marrow, where blood is produced. In blood cancer the growth of normal blood cells is dislodged by the uncontrollable growth of abnormal blood cells. These cancerous cells prevent the blood from performing many of its functions. Hence, the existing treatments of blood cancer are being the foundation for developing the new drugs. The steady flow of the blood cancer drugs has created opportunity for research and development in the existing market. For instance, Amgen Inc. received approval for BLINCYTO in July 2017, which is used in treating B-cell precursor Acute Lymphoblastic leukemia. Similarly, European blood cancer drugs market witnessed the approvals of Gazyvaro, by Roche AG that is used in treating advanced follicular lymphoma. Also, novel technologies like CAR-T are likely to be launched this year.
The global blood cancer drugs market is segmented into blood cancer type, drugs and treatment approaches. On the basis of blood cancer type, the global blood cancer drugs market is segmented into leukemia, lymphoma and myeloma. The lymphoma segment is expected to drive the majority market of blood cancer drugs followed by leukemia. The global market of this segment is primarily driven by the increasing prevalence of lymphoma, and presence of effective treatments in the market. On the basis of drugs, the global blood cancer drugs market is further categorized into Rituaxan/Mabthera (Rituximab), Gleevac/Glivec (Imatinib), Revlimid (Lenalidomide), Velcade (Bortezomib), Tasigna (Nilotinib), Pomalyst (Pomalidomide), Vidaza (Azacitidine), Kyprolis (Carfilzomib), Adcetris (Brentuximab Vedotin), and Others. This continuous innovation for treating various sub-types of blood cancers has led to the development of novel types of treatments. For instance, the combination of Revlimid and Velcade has emerged as the preferential drugs in trials for treating multiple myeloma.
The leading companies operating in this industry include Johnson & Johnson Inc., Amgen Inc., Bayer AG., Pfizer, Inc., AbbVie Inc., Roche Holding AG., Celgene Corporation, AstraZeneca, Novartis AG, GlaxoSmithKline PLC, Merck & Co., Inc., and Eli Lily & Co. among others.
Request For Discount: https://www.polarismarketresearch.com/industry-analysis/global-blood-cancer-drugs-market/request-for-discount-pricing
About Polaris Market Research
Polaris Market Research is a global market research and consulting company. The company specializes in providing exceptional market intelligence and in-depth business research services for our clientele spread across different enterprises. We at Polaris are obliged to serve our diverse customer base present across the industries of healthcare, technology, semi-conductors and chemicals among various other industries present around the world
Contact us
Polaris Market Research
Phone: 1-646-568-9980
Email: [email protected]
Web: www.polarismarketresearch.com
0 notes
Text
Best multiple myeloma treatment in India
Multiple myeloma is cancer of the plasma cells (a type of white blood cells) of the bone marrow. Plasma cells are protein-making cells that generally produce the different kinds of antibodies for our immune system. In multiple myeloma, the plasma cells become malicious and cancerous. These myeloma cells stop making different forms of protein in response to the immune system's needs and instead start to produce a single abnormal type of protein sometimes termed a monoclonal or M protein. Multiple myeloma plasma cell populations accumulate in the bone marrow, and these collections of cells called plasmacytomas can erode the hard outer shell or cortex of the bone that normally surrounds the marrow. These weakened bones show thinning of the bone, as seen in nonmalignant osteoporosis or what appear to be punched out or lytic bone lesions. People often refer to multiple myeloma simply as myeloma (also termed Kahler's disease after the physician who first described this cancer). The disease usually occurs in people past middle age.
In India, there are large number of options available for Best multiple myeloma treatment in India.
However, rarely it can occur in a child. One type of myeloma-related plasma cell neoplasm is called a monoclonal gammopathy of undetermined significance (MGUS). In MGUS, medical professionals only find low levels of M protein and people have no symptoms; MGUS infrequently develops into multiple myeloma.
Plasma cell neoplasm is another name for multiple myeloma. Causes of multiple myeloma What triggers plasma cells into malicious multiple myeloma is unknown. The cancerous myeloma plasma cells proliferate and crowd out normal plasma cells and can corrode areas of bones. The proteins produced in large amounts can cause many of the symptoms of the disease by making the blood more viscous and depositing the proteins in organs that can interfere with the functions of the kidneys, nerves, and immune system.
Causes of multiple myeloma are not known exactly. But patients more likely to get affected • older than 65 years • people of African-American origin • overweight or obese people • family member with it
Stages of multiple myeloma
There are four stages of multiple myeloma. While many health care professionals use different staging, these are various stages cited by many clinicians:
• Smoldering: multiple myeloma with no symptoms • Stage I: early disease with little anemia, relatively small amount of M protein and no • bone damage • Stage II: more anemia and M protein as well as bone damage • Stage III: still more M protein, anemia, as well as signs of kidney damage Because staging criteria differ according to different groups, some clinicians simply define the individual's multiple myeloma without assigning a stage and simply estimate a prognosis for their patient.
Symptoms of multiple myeloma
Patients with myeloma may be asymptomatic with an unexplained increase in protein in the blood. With more advanced disease, some myeloma patients may have weakness due to anemia caused by inadequate production of red blood cells, with bone pain due to the bone damage, and as the abnormal M protein can accumulate and damage the kidneys resulting in patient’s unexplained kidney damage and decreased kidney function. Multiple myeloma cancer cells may be in or outside the bone marrow.
The following symptoms and signs of multiple myeloma -
• Anemia • Bleeding • Nerve damage • Bone tenderness or pain, including back pain • Enlarged tongue • Skin lesions (rash) • Infections Weakness, fatigue or tiredness • Kidney failure and/or other end-organ damage• Spinal cord compression • • Loss of appetite and weight loss • Leg swelling • Hypocalcaemia • Diagnosis of multiple myeloma • First sign of multiple myeloma is found when a routine blood test shows an abnormal amount of protein in the bloodstream or an unusual stickiness of red blood cells causing them to stack up almost like coins, an unusual formation for red blood cells. The health care professional will do a history and physical exam, looking for signs and symptoms of multiple myeloma. If multiple myeloma is suspected, several studies help confirm the diagnosis.
They include a bone marrow aspiration and biopsy most commonly from the large bones of the pelvis. Cells obtained from the marrow are studied by a pathologist to determine if there is one (plasmacytoma) or more (multiple myeloma) abnormal types or numbers of cells • Medical professionals also study a sample of the bone marrow aspirate for more detailed • Characteristics such as the presence or absence of abnormal numbers or types of chromosomes (DNA) by what is called cytogenetic testing.
Bone marrow biopsy can assess the concentrations of cells in the marrow and the presence of abnormal invasive growth of cellular elements. • Blood testing and urine testing by several methods can determine levels and types of National Comprehensive Cancer Network (NCCN) recommended that health care professionals use a serum free light chain assay and fluorescence in situ hybridization (FISH) test to further • Monoclonal protein produced and if there is kidney damage.
Identify multiple myeloma in patients
X-ray studies to identify skeletal lesions and MRI for spinal cord lesions in multiple myeloma.
Medical treatment for multiple myeloma
The therapy is decided based upon the patient's condition and the cancer management team, made with the patient's input. The choices for treatment(s) often include combinations of drugs, some of which medical professionals give as pills and others by intravenous injection.
These include drugs that affect or modulate the immune system, steroids, and some oral or injectable chemotherapy drugs. These are usually used in combinations. There may be a role for high-dose chemotherapy followed by the administration of bone marrow called a stem cell transplant. Numerous factors come into play in determining whether to do such a transplant. Other medical treatments may include steroids, bisphosphonate therapy, blood or platelet transfusions, plasmapheresis, and other combination therapy depending on the individual patient's disease stage.
Radiation therapy may treat painful areas of bone damage. Surgeons can surgically repair broken bones in many cases.
There are many drugs used to treat multiple myeloma. Medical professionals often use the following drugs in combination with dexamethasone,
• Bortezomib Velcade -- protease inhibitor • Lenalidomide (Revlimid) -- immune cell modulation • Melphalan (Alkeran) -- alkylating agent that is toxic to myeloma cells • Carfilzomib (Kyprolis) -- protease inhibitor that is FDA approved usually for patients • who have failed a previous treatment • Daratumumab (Darzalex) -- monoclonal antibody that may damage or kill multiple • Myeloma cells (and others) that have CD38 protein on their surface • Elotuzumab (Empliciti) -- a compound that activates the body's natural killer cells to • Destroy multiple myeloma cells, usually in combination with Revlimid and Decadron • Ninlaro (Ixazomib) -- This proteasome inhibitor, in combination with Revlimid and • Dexamethasone, improves the survival rates of some patients with multiple myeloma.
Hospitals offer best multiple myeloma treatment in India, the charges for autologous stem cell transplant ranges between USD 15000 to USD 21000 depending on the status of the disease and individual's response to the treatment provided at the hospitals.
Related Articles -
Best multiple myeloma treatment hospitals in India
Best Sickle cell disease treatment in India
Best Bone marrow transplant hospitals in India
Are you looking for Lymphoma treatment in India
About GHN Healthcare -
GHN Healthcare Services is a leading Medical treatment Assistance Company based in New Delhi (National Capital region), India. The Organization actively engaged in providing Medical assistance to foreign Patients who choose to travel to India for quality medical care at a reasonable cost. GHN Healthcare Services is associated with 25+ Top-Notch Hospitals and has a network of 500+ Super Specialists to offer world-class medical care at a reasonable cost.
For any enquiries related to Multiple myeloma treatment in India. Click here...
0 notes
Text
Multiple Myeloma Market Size Forecast, Epidemiology Analysis, Emerging Drug Uptake and Key Companies Assessment by DelveInsight
(LAS VEGAS, US) The Multiple Myeloma Market size across the 8MM i.e. the United States, Eu5(the UK, Germany, France, Italy, Spain), China and Japan, was $16.27bn in 2019 and is increasing with a modest CAGR during the study period (2017-2030), according to DelveInsight, a leading company in healthcare analytics and consulting.
The market size for Multiple Myeloma therapies will increase dramatically by 2030 due to the arrival of upcoming therapies that will carve out niche roles in the drug landscape. DelveInsight's latest report on Multiple Myeloma Epidemiology and Market indicates that the impressive growth in market size is due to the rise in incident cases of Multiple Myeloma in 8MM, incorporation of immune-therapies in treatment landscape increased patient adherence and adoption of newer therapies. Also, rich emerging pipeline, better diagnosis, rising awareness and expected increase in investment in the R&D activities are some additional factors that are going to fuel the market.
Some key highlights from the report:
The total incident cases of Multiple Myeloma are expected to reach 91,520 in 2020 in the 8MM
Higher usage of bortezomib based regimen observed across the US, EU5 and JP; Bortezomib + Lenalidomide + dex regimen is the preferred treatment choice in the US and Japan in the first-line compared to Bortezomib + Melphalan ± Prednisone and Bortezomib + dex regimen in EU5. In the case of China, higher usage of thalidomide based regimen found in the first-line setting
Among emerging therapies, Bristol Myers Squibb and Bluebird Bio's anti-BCMA CAR T Cell Therapy Idecabtagene Vicleucel (Ide-cel, bb2121) is expected to result in significant revenues owing to promising results, one-time dosing and premium pricing in heavily pretreated patients
Key Companies fuelling the Multiple Myeloma market size growth are GlaxoSmithKline, Bristol-Myers Squibb, AbbVie, Roche, Janssen Research & Development, Merck Sharp & Dohme Corp., Pfizer, Takeda, Amgen, AstraZeneca etc.
Patent expiry of multiple blockbuster drugs like Revlimid, Pomalyst, Darzalex and Kyprolis is on the lines to expire from 2026 onwards, and this will erode the sales value significantly and the market is expected to decline from 2028 onwards due to cumulative impacts of patent expiry.
Download Multiple Myeloma Sample: https://www.delveinsight.com/sample-request/multiple-myeloma-market
Though Multiple Myeloma is not common cancer; still, it is the second most diagnosed blood cancer in the United States. It is worth highlighting that it is a heterogeneous haematological malignancy in which epidemiology plays an increasingly important role. Over the past years, intensive clinical and molecular epidemiological research has extended the information about its pathogenesis, risk factors, and prognostic components which aided the approval of new drugs. Despite arduous research endeavors, the etiology remains enigmatic. The untimely or prolonged diagnosis has a severe impact on the clinical course of Multiple myeloma and a negative impact on disease-free survival. It's an unfortunate fact that approximately 95% of all the Multiple Myeloma cases are diagnosed at distant stages. The report reviews the changing epidemiology and provides the forecasts upto 2030, highlights treatment patterns, and the health disparity observed in important subgroups of Multiple Myeloma.
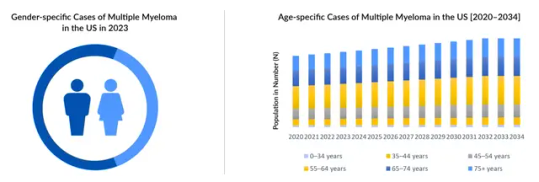
Multiple myeloma report contains epidemiological analysis segmented as the following:
Total Multiple Myeloma Incident Cases
Total Multiple Myeloma Incident cases by Age Distribution
Total Symptomatic Multiple Myeloma Cases
Cases of Multiple Myeloma by Treatment Line
Gender-specific cases of Multiple Myeloma
Multiple Myeloma Market Scenario
The current standard of care of Multiple myeloma treatment includes stem cell transplant, conventional chemotherapy, targeted therapy, surgery, and radiation therapy. Chemotherapies can be given alone or in conjunction with other drugs including corticosteroids, proteasome inhibitors, immune-modulators, and monoclonal antibodies, anti-resorptive agents such as bisphosphonates and NSAIDs, or narcotics. Currently, Lenalidomide is the market leader in multiple myeloma treatment landscape, and usage as monotherapy and also in combination with other therapies can be found across all the settings. Darzalex is also being used by the healthcare experts in combination as doublet, triplet, and quadruplet with existing therapies for the good treatment strategies and better result outcomes and has impacted the MM treatment landscape significantly. Label expansion along with higher usage of Darzalex has translated into higher revenues and expected to generate maximum revenue by 2025 before the competition and expected patent expiry would erode the sales value. At present, among the IMid's agents, Revlimid dominates the Multiple Myeloma market in the 8MM, where it is included in all lines of Multiple Myeloma therapy either as monotherapy or in combination with other drugs. In 2017, Revlimid generated a revenue of USD 7,140 million in the 8MM. Despite the loss of patent exclusivity among the major markets and approval of other potential pipeline candidates, it will continue to maintain a strong presence during the forecast period as a molecule. The novel emerging therapies are expected to bring a paradigm shift in the Multiple Myeloma treatment landscape by catering to larger unmet needs.
Report includes exhaustive analysis of Multiple Myeloma Pipeline Therapies
Idecabtagene vicleucel (ide-cel): Bristol Myers Squibb and bluebird bio
Venetoclax (Venclexta, Venclyxto): AbbVie
JNJ-68284528 LCAR-B38M/JNJ-4528): Janssen Research and Development
Keytruda (pembrolizumab): Novartis
Melflufen (melphalan flufenamide): Oncopeptides
Cetrelimab (JNJ-63723283): Janssen Research and Development
REGN5458: Regeneron Pharmaceuticals
Iberdomide: Celgene
NY-ESO-1 C259 T Cells: GlaxoSmithKline
Braftovi (encorafenib): Pfizer
JCARH125: Celgene Corporation
Felzartamab (MOR202): I-Mab Biopharma
Chidamide (Epidaza): Shenzhen Chipscreen Bioscience
The past couple of decades have shown vast changes in the treatment landscape of Multiple Myeloma, starting with the use of stem cells trailed by the availability of novel treatments such as immunomodulators and proteasome inhibitors that have transformed the natural history of the indication, leading to increased survival times. Ongoing advancements in emerging Novel therapies such as CAR-T cell and monoclonal antibodies are showing promising results in treating multiple myeloma patients and are also expected to drive the growth of the market. Recent years have witnessed an influx of several pharma companies exploring the Multiple Myeloma market through novel targets and therapies. Although the emerging pipeline candidates will reduce the gaps however, the opportunities will still remain. As a ray of hope, the launch of new drugs have extended the median overall survival of Multiple Myeloma patients to 4-6 years; however the stark reality is that the ten year survival rate is 3%. The long term burden of the therapies makes life pretty difficult for the patients. There is a dire need for a permanent cure. Another hurdle is the existing expensive treatment options that create a barrier for the aged uninsured population to get hold of costly therapies. The factors like drug-induced toxicities, differences in clinical care, access to the therapies in real-world settings are the observed gaps between trial-based and real-world outcomes. DelveInsight believes that the Multiple Myeloma market is an attractive prospect for the companies due to the high unmet needs and low regulatory hurdles.
Key Trends of Multiple Myeloma Market Report: https://www.delveinsight.com/report-store/multiple-myeloma-market
Scope of the Report
Geography Covered: 8MM - The United States, EU5 (Germany, France, Italy, Spain, and the United Kingdom), Japan, and Chine.
Study Period: 3-year historical and 11-year forecasted analysis (2017-2030).
Markets Segmentation: By Geographies, By Therapies (Forecasted + Historical).
Companies Covered: GlaxoSmithKline, Bristol-Myers Squibb, AbbVie, Roche, Janssen Research & Development, Merck Sharp & Dohme Corp., Pfizer, Takeda, Amgen, AstraZeneca, and several others.
Analysis: Comparative and conjoint analysis of emerging therapies, Attribute Analysis,
Case Studies
KOL's Views
Analyst's View
The Multiple Myeloma Marketed drugs covered report are:
Sarclisa (Isatuximab): Sanofi
Darzalex (Daratumumab): Janssen Research and Development
Empliciti (Elotuzumab): Bristol-Myers Squibb and AbbVie
Velcade (bortezomib): Takeda
Pomalyst (Pomalidomide): Celgene Corporation
Revlimid (Lenalidomide): Celgene Corporation
Farydak (panobinostat): Novartis Pharmaceuticals
Kyprolis (Carfilzomib): Amgen
Ninlaro (ixazomib): Takeda Pharmaceuticals
Blenrep (Belantamab Mafodotin): GlaxoSmithKline
Table of Contents
1
Key Insights
2
Executive Summary of Multiple Myeloma
3
KOL Views
4
SWOT Analysis of Multiple Myeloma
5
Multiple Myeloma Market Overview at a Glance
6
Disease Background and Overview: Multiple Myeloma
7
Diagnosis of Multiple Myeloma
8
Multiple Myeloma Epidemiology and Patient Population
9
The United States Multiple Myeloma Epidemiology
10
EU-5 Multiple Myeloma Epidemiology
11
Japan Multiple Myeloma Epidemiology
12
China Multiple Myeloma Epidemiology
13
Multiple Myeloma Treatment
14
Unmet Needs in the Multiple Myeloma Market
15
Patient Journey of Multiple Myeloma
16
Key Endpoints of Multiple Myeloma Clinical Trials
17
Multiple Myeloma Marketed Therapies
18
Multiple Myeloma Emerging Therapies
19
Multiple Myeloma 8 Major Market Analysis
20
8MM Multiple Myeloma Market Size
21
The United States Multiple Myeloma Market Size
22
EU-5 Multiple Myeloma Market Size
23
Japan Multiple Myeloma Market Size
24
China Multiple Myeloma Market Size
25
Market Access and Reimbursement of Multiple Myeloma (MM) Therapies
26
Multiple Myeloma Market Drivers
27
Multiple Myeloma Market Barriers
28
Appendix
29
DelveInsight Capabilities
30
Disclaimer
31
About DelveInsight
Request a WebEx Walkthrough of the Report: https://www.delveinsight.com/report-store/multiple-myeloma-market
Related Report:
CAR T-Cell Therapy for Multiple Myeloma-Market Insights and Market Forecast-2030 : This report delivers an in-depth understanding of the CAR T-Cell Therapy use for Multiple Myeloma as well as the CAR T-Cell Therapy market trends for Multiple Myeloma. It provides current treatment practices, emerging drugs, CAR T-Cell Therapy market share of the various CAR T-Cell Therapies for Multiple Myeloma, the individual therapies, current and forecasted Multiple Myeloma CAR T-Cell Therapy market Size from 2017 to 2030.
About DelveInsight
DelveInsight is a leading Business Consultant, and Market Research firm focused exclusively on life sciences. It supports Pharma companies by providing end to end comprehensive solutions to improve their performance. Get hassle-free access to all the healthcare and pharma market research reports through our subscription-based platform PharmDelve.
Contact Us: Shruti Thakur [email protected] +1(919)321-6187 www.delveinsight.com
SOURCE DelveInsight Business Research, LLP
0 notes
Text
Scotland backs Merck/Pfizer’s Bavencio combo for kidney cancer

The Scottish Medicines Consortium (SMC) backed NHS use of nine new medicines at its meeting this week, including Merck KGaA and Pfizer’s Bavencio as a first-line treatment for advanced kidney cancer.
The decision means that PD-1 inhibitor Bavencio (avelumab) can be given to previously-untreated adults diagnosed with advanced renal cell carcinoma – the most common form of kidney cancer – as a combination regimen with Pfizer’s targeted cancer drug Inlyta (axitinib).
Kidney cancer is the seventh most common cancer in Scotland, with approximately 1,200 new cases diagnosed every year.
Pfizer said that Bavencio/Inlyta had previously been available to patients in the UK as part of the Early Access to Medicines Scheme (EAMS), and is the first immunotherapy combination therapy for RCC to be cleared for use in both Scotland and England.
NICE cleared first-line use of the dual regimen in first-line RCC patients in July, but opted to make it available with interim funding via the Cancer Drugs Fund (CDF), which kicks in when upcoming trial evidence is expected to confirm whether the drug will be cost-effective.
The SMC decision came after a PACE (Patient and Clinician Engagement) meeting which heard that RCC is a devastating and incurable disease that is generally diagnosed at an advanced stage with a five-year survival rate of approximately 12%.
It is based on the results of the JAVELIN Renal 101 study, which showed that Bavencio/Inlyta extended progression-free survival for an average of five months compared with Pfizer’s older targeted drug Sutent (sunitinib).
Bavencio/Inlyta isn’t however the first immunotherapy-based regimen to be recommended by the SMC for first-line RCC use.
Last month the panel gave a green light in that setting to Merck & Co/MSD’s PD-1 inhibitor Keytruda (pembrolizumab) plus Inlyta, and last year also backed Bristol-Myers Squibb’s PD-1 drug Opdivo (nivolumab) with CTLA4 inhibitor Yervoy (ipilimumab).
The SMC also backed the following drugs for NHS Scotland use:
Bristol Myers Squibb’s Revlimid (lenalidomide) as monotherapy for the maintenance treatment of adult patients with newly diagnosed multiple myeloma who have undergone autologous stem cell transplantation (ASCT). And in combination with rituximab for adults with previously treated follicular lymphoma;
BioMarin’s Brineura (cerliponase alfa) for neuronal ceroid lipofuscinosis type 2 (CLN2), a life limiting, inherited condition in children that leads to progressive brain damage;
Janssen’s Imbruvica (ibrutinib) for the treatment of rare blood cancer Waldenstrom’s macroglobulinemia (WM) in combination with rituximab;
Amgen’s Kyprolis (carfilzomib) for blood cancer multiple myeloma in patients who have received at least one prior therapy;
Novartis’ Mayzent (siponimod) as a treatment for people with active secondary progressive multiple sclerosis (SPMS);
Menarini Pharma’s Vaborem (meropenem/vaborbactam), an antibiotic for the treatment of a number of multidrug-resistant serious infections; and
Dr Falk Pharma’s orodispersible Jorveza (budesonide) for eosinophilic esophagitis (EoE) a chronic, allergic inflammatory disease of the oesophagus.
The post Scotland backs Merck/Pfizer’s Bavencio combo for kidney cancer appeared first on .
from https://pharmaphorum.com/news/scotland-backs-merck-pfizers-bavencio-combo-for-kidney-cancer/
0 notes