#birthindiaorg
Explore tagged Tumblr posts
Text
The rights of the newborn, to it's own blood - Your baby needs it's blood and stem cell infusion, with all it's benefits, at the time of birth, as nature intended it.
We admire the local and global work that Ibu Robin Lim has been carrying out for decades for the rights of women and especially babies. Have you considered that it's a newborn's right to have it's own blood?
Midwife Lina Duncan states: “There is also work across the globe to ensure babies get their own blood. One of the ways we can help is by our language. It's not ‘cord blood.’ The blood belongs to the baby- it’s ‘baby’s blood.’“
Please read on and comment in response to Ibu Robin Lim's thoughtful and compassionate article.
[NOTE: Unfortunately she is unable to attend the conference to speak as we had all hoped. Regardless, we propose change to the practices across Asia to better serve our babies. May everyone be inspired through her research, writing and compassionate work.]
The Necessary Question of Infants’ Human Rights at Birth…Are there Vampires in the Birth Rooms?
Parents, grandparents, aunts, uncles, siblings, families, midwives, doulas, doctors, nurses, hospital administrators and legislators…we are BirthKeepers. It is our responsibility to ask the next question concerning human rights in childbirth. As BirthKeepers, it is we who are given the sacred responsibility to protect the mothers and our incoming humans, the newborns, at birth and as they grow, for they are the future EarthKeepers. My question now is: “Are we allowing our health providers to rob our babies of their full potential of health, intelligence, immunity and longevity, at birth?��
In Germany, children under the age of 18 are not eligible to donate blood. Blood donations are generally no more than 500 ml, which is 1/10th of the average adult blood volume. Blood donors must weigh at least 50 kg.
Yet, all over the world, in nearly every single medical institution where babies are born, newborns (usually weighing only between 2 and 5 kilograms (4.4 to 11 lbs.) are being denied up to 1/3 of their blood volume. This happens when the umbilical cord is immediately clamped and cut, by the doctor or midwife, just moments after the baby is born.
At the moment of birth, newborn infants have a blood volume of approximately 78 ml/kg, which means about 273 ml, at an average weight of 3.5 kg. This is what the newborn is left with when the umbilical cord is immediately clamped and cut.
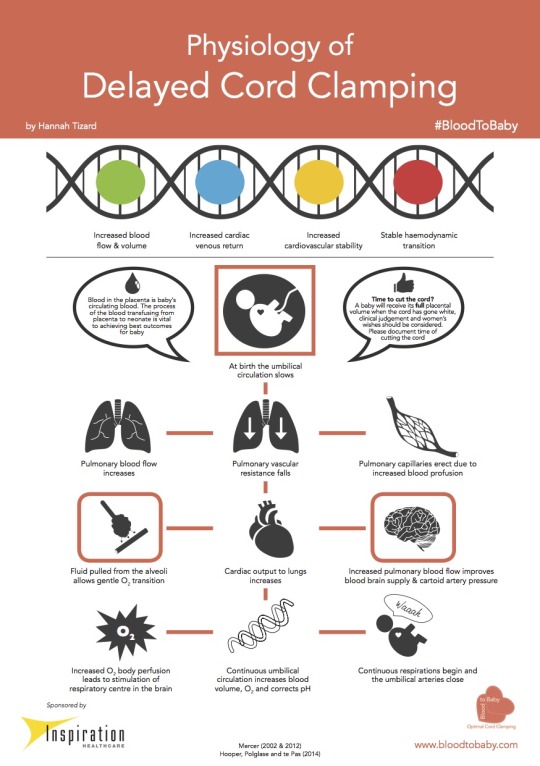
Research has shown that when umbilical cord-clamping is delayed for 5 minutes, a newborn’s blood volume increases by 61% to 126 ml/kg, for an average total of 441 ml. This placental transfusion amounts to 168 ml for an average 3.5 kg (7.7 lb.) infant. One-quarter of this transfusion occurs in the first 15 seconds, and one-half within 60 seconds of birth.

Is taking 1/3 of a mammal’s blood supply harmful?
How then can it be legal for hospital protocols and practices to harm newborns, by robbing them at birth of so much of their blood? I have reviewed the extensive research and the evidence, and found absolutely NO benefits for newborn babies, when their umbilical cords are immediately clamped and cut at the time of birth. In fact, the studies prove this to be a harmful practice.
At the time of birth up to 1/3 of each baby’s blood supply is traveling from the placenta via the umbilical cord to the baby. Calling this blood “cord blood” is doublespeak, intentionally ambiguous language, meant to fool parents into misunderstanding. The fact is, the blood present in the umbilical cord at the time of birth is truly the BABY’S blood.
No parent would sign a waiver (often presented in fine print as part of a long informed consent, given to mother when she arrives at a hospital in labor) giving away 1/3 or any amount of the baby’s blood. Yet, thousands of times, every day and night, parents are deluded into giving away a significant part of their baby’s precious blood supply! The majority of parents in the world are not even asked if the baby’s umbilical cord may be immediately severed.
I am quite sure that if I were to remove 1/3 of even one adult patient’s blood, without his or her consent, it would be considered a crime. There would be media outcry against me, and I would be prosecuted. How then is it that people tolerate the same unfair treatment of human neonates?
A mountain of research shows that by simply delaying the clamping and cutting of babies’ umbilical cords, our newborn children suffer less trauma, fewer inner cranial hemorrhages, and have higher stores of iron at 4 months of age, and even up to 8 months after birth (1) (2) (3). The nutrients, oxygen and stem cells present in the blood transfused into babies by the placenta, when cord severance is delayed, ensures that the body’s tissues and organs are properly vitalized, supplied with energy, and nourished. This translates into improved health, heightened immunity, increased intelligence and potential longevity.
In addition, keeping the umbilical cord intact for some time at birth means that the baby must stay skin to skin with mother. This eliminates or greatly reduces the potential for birth trauma. Research has proven that babies born without trauma enjoy an intact capacity to love and trust. (Michel Odent OBGYN “The Scientification of Love, see entire book)
The simple, natural, common-sense practice of giving the placenta time to do its job, of delivering to the baby his or her full blood supply, has been criticized and NOT implemented by the very doctors and hospitals who have taken an oath, to “Never Do Harm.”
The origins of immediate premature cord cutting
The imposed medical habit of immediately clamping and cutting babies’ umbilical cords has not been with us so long (just over 200 years) and yet, in the minds of many healthcare providers it is erroneously considered “normal” and “necessary.” Clearly the research proves it is not necessary, nor is it evidenced based practice.
“Another thing very injurious to the child, is the tying and cutting of the navel string too soon; which should always be left till the child has not only repeatedly breathed but till all pulsation in the cord ceases. As otherwise the child is much weaker than it ought to be, a portion of the blood being left in the placenta, which ought to have been in the child.”
~Erasmus Darwin, Zoonomia, 1801
The habitual practice of immediate umbilical cord clamping and cutting began in the 1960s when an unproved hypothesis or theory arose among physicians thinking that immediate cord severance would prevent jaundice. If this is true, why do so many babies who have had their cords immediately clamped and cut need phototherapy for pathological jaundice? Research has proven that there is no greater risk of pathological jaundice for newborns whose cord clamping and cutting is delayed.
Another theory was that early cord clamping would prevent Polycythemia, or too much hemoglobin. Some research does show an increased concentration of hemoglobin in the delayed cord clamping group, but it has not harmed babies, nor is it a significant argument for immediate cord severance. (4)
When immediate umbilical cord clamping and cutting was introduced, it was never questioned. NO research was conducted to determine if it was a safe practice. It was just done for convenience. Doctors, nurses and midwives began to follow the trend, like sheep wearing blinders. Later, they justified it with myths about delayed cord severance causing jaundice. Few asked the questions I am asking today; “What about the Baby?” “What are the Babies’ human rights?” “Is the practice and protocol of immediate umbilical cord severance harming our children?” “Is it sabotaging breastfeeding and bonding?” “Is it impairing our children’s birthright to their full potential of health and intelligence?” At this junction of herstory and history, many BirthKeepers are asking these very questions. (5)
Research proves that immediate or early umbilical cord severance is detrimental to our newborn children, but no one seems alarmed. Are we hypnotized? Why are we trusting medical professionals, who profits from denying our offspring their very blood? Stealing blood is what vampires do!
Thinking, caring parents and grandparents have concluded that OBGYNs and midwives who insist on routine, immediate umbilical cord cutting are simply protecting their right to practice with impatience, and what they deem ‘efficiency,’ with no regard for the rights of the baby, who cannot protest.
Another issue is financial profit. Stem cells are valuable, blood is valuable, and hospitals sell babies’ blood for transfusions and for research. (6) Many parents are asked to donate their babies cord blood to science or to help others. Did you know umbilical cords are marketed for transplants? Placentas have also been sold to cosmetic companies to be used in beauty supplies, though this is now much less common.
In some countries (especially the US), fear of litigation has been used to justify early cord-cutting. In 1995 the American Academy of Obstetricians and Gynecologists (ACOG) released an Educational Bulletin (#216) recommending immediate cord clamping in order to obtain cord blood for blood gas studies in case of a future lawsuit. They did this because deviations in blood gas values at birth can reflect asphyxia, or lack of. Lack of asphyxia at birth is viewed as proof in a court of law that a baby was healthy at birth.
Following an unpublished letter sent to ACOG by Dr. Morley, ACOG withdrew this Educational Bulletin in the February 2002 issue of Obstetrics and Gynecology, the ACOG journal. (7) This action released them of liability resulting from their previous bulletin #216 of 1995. Parents and all BirthKeepers must ask; WHY, if ACOG has withdrawn its erroneous instruction to doctors, to immediately clamp and cut babies’ umbilical cords, is it still universally and dangerously practiced?
Midwives and doctors who propose the healthy process of placental transfusion at birth by delaying umbilical cord clamping and cutting are criticized and charged with the burden of proving that letting nature take her course is safe!

The difference between a cord at the time of birth versus at the time of the cessation of pulsation (Photo credit: Kate Emerson, www.cord-clamping.com)
Cord Baby blood banking
The question of cord blood banking arises. First of all, remember that it is actually baby blood, not cord blood. That said, there are two directions parents are encouraged to choose from: banking their baby’s stem-cell-rich blood for donation, presumably to help someone in the future, an altruistic idea; or, banking baby’s blood for future personal use, should the child develop a disease perhaps treatable by blood transfusion. The most touted of the presumably treatable diseases is leukemia. The probability that a person in the course of his or her life will ever need a stem cell transplant (whether from umbilical cord blood or bone marrow) has been estimated by the University Hospital in Heidelberg at 0.06% to 0.46%, depending on age. Correspondingly low, the probability that one's own cord blood would be used in a transplant is between 1: 1400 and 1: 200,000. (8) The technology to properly store this baby blood is still not adequate to insure that the blood will be useable in the future.
Parents are driven by fear and love for their baby to pay between 1,500 and 2,000 euros or more, for the initial “harvesting” of their baby’s blood at birth. Storage programs, for between ten and twenty-five years cost between 90 and 120 euro per year. Parents are asked to gamble that technology will advance enough to make their investment useful, should the worst case scenario for their child’s health arise.
But it must be said out loud and precisely: YOUR BABY NEEDS THAT BLOOD AND STEM CELL INFUSION, WITH ALL ITS BENEFITS, AT THE TIME OF BIRTH, AS NATURE INTENDED IT.
With that in mind, there is a third option for parents who are convinced of the need for blood banking: to harvest the baby’s blood for collection and storage AFTER delaying the clamping and cutting of baby’s umbilical cord, allowing for some of the essential transfusion to take place. immediately after birth.

This baby is not being deprived of the transfusion of it’s own blood from the placenta. Because his cord was not cut early, he will enjoy improved health, heightened immunity, increased intelligence and potential longevity. (Photo credit: Neha Chopra, Out of Focus Photography)
At least 7,000 babies got their blood
At Bumi Sehat in Indonesia and the Philippines, we have received nearly 7,000 babies safely into the world, in high-risk, low resource settings. All of these babies enjoyed delayed umbilical cord clamping and cutting. Normally we wait 3 hours before doing anything with babies’ umbilical cords, and many parents choose keeping the cord and placenta connected to the baby until the cord naturally dries and falls away, or “Full Lotus Birth.” Both of my grandsons enjoyed this non-violent practice.
At Bumi Sehat we have experienced NO ill effects to babies through delaying umbilical cord cutting. A small study was done which compared a sample of 30 babies from Bumi Sehat (greatly delayed cord severance) and 30 babies from a local hospital with immediate cord severance. There was NO increased rate of jaundice in the Bumi Sehat babies, and they enjoyed higher hemoglobin.
Our MotherBabies enjoy a breastfeeding rate of 100% upon discharge from all three of our childbirth centers in Indonesia and the Philippines. We attribute this success of breastfeeding to the bright, enthusiastic way in which babies, born at our birth centers, bond wide-eyed and go directly to the breast to self-attach and feed. Delayed umbilical cord clamping and cutting makes it possible for babies to be bright and energetic. Babies subjected to immediate cord severance suffer from newborn anemia and all of their bonding and breastfeeding activities are impaired.
Severe anemia makes any and all newborn activities, such as gazing, crawling toward the breast, nuzzling, staying awake, latching and suckling, nearly impossible. I sing praises to the determined mothers who manage to bond and breastfeed their infants, in spite of immediate cord severance. Humans are super resilient, but that is no reason to abuse them at birth.

Just Say No
No other mammal, except humans, routinely interferes with bonding and breastfeeding by quickly severing the umbilical cords of their offspring.
No matter if you are rich or poor; educated or not; brown, black, white, red, yellow or of mixed race, Muslim, Christian, Buddhist, Hindu, Pagan, Catholic, Jewish or Agnostic, very young or quite mature, if you go to a medical institution for childbirth, your baby will be robbed of up to 1/3 or 33% of his or her/his natural blood supply.
Just say “NO, I will not allow anyone to abuse my newborn by immediately clamping and cutting my Baby’s umbilical cord!”
If you were born in a hospital or clinic, it happened to you. If you plan to give birth in nearly any medical institution on Earth, it will happen to your baby, unless YOU demand time for your baby to receive all of the blood he or she is meant to have. (9)
Immediate or early clamping and cutting of babies’ umbilical cords is the biggest most widespread, medically sanctioned Human Rights issue on Earth! Together, we can make this a thing of the past. May our babies all be blessed by our patience.

This is the non-violent practice of “Lotus Birth” in which the baby and placenta and left in-tact until the cord dries up and comes off. Obviously, this baby wasn’t shy any of his blood! (Photo credit: Lina Duncan, midwife)
REFERENCES
(1) BMJ. 2011 Nov 15;343:d7157. doi: 10.1136/bmj.d7157.
(2) Indian Pediatr. 2002 Feb;39(2):130-5.
(3) JOURNAL OF TROPICAL PEDIATRICS, VOL. 58, NO. 6, 2012
(4) Judith S. Mercer, PhD, CNM, FACNM, Debra A. Erickson-Owens, PhD, CNM J Perinat Neonat Nurs r Vo 2012Rethinking Placental Transfusion and Cord Clamping Issues
(5) http://midwifethinking.com/2011/02/10/cord-blood-collection-confessions-of-a-vampire-midwife/
(6) http://midwifethinking.com/2011/02/10/cord-blood-collection-confessions-of-a-vampire-midwife/
(7) http://www.whale.to/a/morley17.html
(8) Die Wahrscheinlichkeit, dass ein Mensch im Laufe seines Lebens überhaupt eine Stammzelltransplantation (egal ob ausNabelschnurblut oder Knochenmark) braucht, schätzt die Uniklinik in Heidelberg auf 0,06% bis 0,46% abhängig vom Lebensalter, das erreicht wird. Entsprechend gering ist die Wahrscheinlichkeit, dass bei einer Transplantion das eigene Nabelschnurblut verwendet wird: Die Schätzungen reichen von einer Wahrscheinlichkeit von 1:1400 bis 1:200.000. http://www.babycenter.de/a36661/warum-ist-nabelschnurbluteinlagerung-umstritten#ixzz3EKUNPq4X
(9) Late umbilical cord-clamping as an intervention for reducing iron deficiency anemia in term infants in developing and industrialized countries: a systematic review. http://www.epistemonikos.org/de/documents/e068abb1a37d6f4c343068377945144da56c483f?doc_lang=en

Ibu Robin Lim, CPM, is a midwife practicing in Indonesia. She, along with midwife Deborah Flowers, co-created the online resource Awakening Birth in an effort to call attention to the care of mothers, babies and their families, and the sanctity of birth as a basic human right. She is the founder of Bumi Sehat, a free clinic and birth center in Bali, Indonesia.
In 2011 she was recognized as the CNN Hero of the Year, and has received many other honors and awards.
She is the author of several books, including After the Baby’s Birth…A Woman’s Way to Wellness, and The Geometry of Splitting Souls. Her newest book, The Ecology of Gentle Birth has just been released in 2016.
See Ibu Robin's books and articles, NICE Guidelines UK, and Hannah Tizard’s www.bloodtobaby.com #WaitForWhite #WaitForWeight
Don’t miss the action at Human Rights in Childbirth Conference in Mumbai India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
4 notes
·
View notes
Text
Why Human Rights in Childbirth Matters? Rebecca Schiller can tell you.
Rebecca Schiller is the author of Why Human Rights in Childbirth Matters and chief executive of Birthrights in England. This is the perfect book to introduce you to framing maternity care within the lens of human rights. And guess what, there will be copies available at the Human Rights in Childbirth Conference in Mumbai!
...um, what?
To be honest, though I am studying to be a midwife and am keenly interested in the experience of childbirth, the concept of human rights in childbirth was new for me. Even at the time of starting to volunteer for this conference I wasn't fully aware of what human rights in childbirth meant or implicated. But along came Rebecca Schiller's book and my jaw dropped, my heart almost burst, and something shifted inside me.
So I thought it would be appropriate to interview her on Skype to further discuss the book, and it's implications in a place like India. But, what a struggle it was for me to write this blog. No matter what I wrote, it fell short of what is conveyed in this book and by Rebecca herself. Rebecca Schiller does an unprecedented job of conveying just what the title says- why human rights in childbirth matter.
But first, a little about the book...
The book (is a whole lot better than this blog)
Schiller does a wonderful job of blending together the voices of women from across the world, the words of experts, legal cases, laws, ideologies, concepts and debates and whips it all up into a comprehensive look at human rights in childbirth. According to her, the core issue in childbirth is not what type (vaginally, natural, or c-section) or where (home, hospital or birth center) women give birth, but really women's autonomy in birth (how was her birth experienced?). She points out that trauma suffered from a birth experience isn't necessarily related to what type of birth a women had, but how it was conducted. A woman may have a “normal, vaginal” birth but if in the process she feels out of control, disrespected and doesn't have enough information, she is likely to feel traumatized from her birth.
She asserts that to truly uphold human rights in childbirth, then everyone needs to recognize that when a woman is pregnant or giving birth, she is no less of a human and is entitled to the basic human rights we are all born with. These rights include the right to autonomy, dignity, choice, informed consent (and refusal) and being free from coercion. To uphold all these rights, maternity systems, healthcare practitioners, policy makers and advocates should shift their focus from pondering how to reduce intervention rates, increase rates of “normal” delivery or promote any one kind of birth, to how to implement the right models of care so that women's authority and choice is maintained. Consequently, providing maternity models that promote individualized care, are likely to reduce c-section and interventions rates that have health officials so alarmed, without degrading a woman's status as an autonomous human being in the process.
It may seem matter-of-fact that a pregnant/birthing woman is still human, but this fact is actually all too often dismissed, in the seemingly legitimate belief of making birth “safer” or a “healthy baby.” Women can be forced or coerced into c-sections, have episiotomies without consent, forcibly held down while unwanted interventions are performed, have police show up at their door for attempting a homebirth or even be denied elective c-sections because someone feels it is better for the baby. Women traumatized from birth beg the question, “Is it really all that matters is a healthy baby?” Schiller resolutely will answer NO! Of course it matters that we have healthy babies, but it is certainly not all that matters.
Right now, almost the whole world prioritizes getting a “healthy baby” out of the mother, at any cost- even at the cost of women losing their dignity, being treated with disrespect or abuse and without autonomy or self-determination. This translates into treating women like vessels or containers where things can be done to them, even without meaningful consent. She asserts that a true good outcome in birth is when both mother and baby turn out to be physically and psychologically healthy after birth.
One interesting point Schiller makes throughout the book is that maternity care systems shaped to maintain human rights will implicitly view mothers as the decision-makers. This can bring up a lot of questions, like, “Can a mother really be fit to make decisions, what about a ‘bad mother?’” But just like the dogma that “all that matters is a healthy baby” needs to be done away with, so does the idea the a mother is in conflict with her unborn child. She explains that mothers are typically exceedingly cautious and concerned about their pregnancies and births- rightfully so as it is their baby and their body that they will carry after the birth. So while they may not be a trained expert, they are the person with the highest stake in the outcomes of birth and with the objective input (not coercion or bullying) from healthcare providers, can know what is right for themselves individually (which can even be finding a trusted careprovider and dutifully doing everything he or she says!)
Schiller calls for all birth activists to unite forces and start fighting for human rights in childbirth so we can recognize the true potential of humanity in maternity care. I urge you to get a copy of her book to be fully convinced of why human rights in childbirth matters. But first read a little more from her in this interview...
The interview
Q. If there is one thing the Indian crowd should take away from this book, what would it be?
A. It's quite simple: women MATTER during childbirth. If we design a system where women matter during childbirth, it will be better for women, it will be better for babies, it will be better for healthcare professionals and it will be better for the family. Actually, it shouldn’t be too hard to do.
Q. So, why isn't that, “All that matters is a healthy baby?”
A. It’s become such a common sentence, it’s easy to let it slide. But when you look at it, what it also says is that 'women don't matter' because the opposite of that sentence is that ‘nothing else matters.’ So it gets used to excuse a lot of behavior (and treatment of women), it’s used to stop women from being able to talk about their experiences and to process their experiences.
But, on a broader level, it can be part of a quite worrying desire to reduce women to reproductive vessels. There are a lot of parallels that happen in other corners of reproductive rights, particularly in the US where there is a real intersection between human rights in childbirth and rights to abortion. So if all that matters is a healthy baby, there is a discomforting and dis-topian lens to that where women don’t matter unless that are the producers of healthy babies.
Q. What's the difference between advocating for human rights in childbirth versus advocating for “natural birth,” “homebirths” or lowering c-section rates?
A. I was a person who previously advocated for a particular kind of birth and a particular way of feeding babies but I found, when we advocate for a specific way of doing things, we can alienate some women and policy makers and health care professionals. And you risk also putting a layer of pressure on women to do things in a certain way. If all of us who are promoting different things in birth, different things in feeding, different things in reproductive rights, focused simply on ensuring that basic human dignity, autonomy, choice and non-discrimination was upheld, then things would sort of follow suite. So if a woman wants a homebirth and since we maintain that women have a choice of birth, she can. And the same with elective cesarean section. Same with infant feeding.
We don’t want to be another pressurizing force in the system, adding a layer of pressure to women. [Human rights in childbirth] brings us all together, so we are not polarized or counterbalancing our arguments by arguing amongst ourselves. We are just focusing on getting all women the respect and dignity and choice that they should have and everything else sort of follows on from there.
Q. So, can a positive birth experience be significant in woman's life?
A. I come to this from a place where I know, from my own birth experiences, that birth can be very positive...I work with a midwife who says ‘get something out of this other than a baby.’ I think what she means is that this is an opportunity to learn about yourself, to learn about your partner, and to feel very powerful and strong. And, that doesn’t mean you won’t feel vulnerable and scared.
Birth can be very healing. I have worked with women who have had trauamtising first births and go on to have very healing births. Not necessarily because it was some magical experience, but it was because she felt like she was in control, a big thing happened to them and they did it! Women can gain a sense of self that becomes stronger rather than weaker.
Birthrights did a survey where we found that women who characterized their births as negative were much more likely to have a negative view of themselves, their partners, and their babies after birth. And on the flipside, women who had positive experiences felt positively about themselves, their babies and their partners. It can be profound. A lot of women [who have had positive experiences] can take it foreward into the rest of their lives, into their careers, their mothering, illness and take on a sense of strength and pass that on into the next generation.” Her mother had a very positive view of birth, so she wasn’t frightened.
Q. How could childbirth and maternity care systems change in India, worldwide, if Human Rights were held up in the process?
A. It’s hard to see that in isolation for a general respect of women’s human rights. The first caveat is that globally, there would have to be a shift towards women and girls….
But (if human rights where upheld in childbirth) we would see many more women having births they planned. And for those whose birth don’t go to plan, there will be less trauma.
I’d imagine it would have an impact on the intervention rates, because most woman aren’t desperate to have loads of interventions [during childbirth]. It would also have an impact on mental health- overall perinatal outcomes.
It seems like India needs human rights in childbirth, not to just decrease the almost rampant intervention rates, including c-section, but to bring back women into birth- to remind women of India that they matter, too.
Join the conference to see how we can go about doing that!
**Interviewed and written by Zoe Quinn, Birth India

Rebecca Schiller is the Director of the human rights in childbirth charity Birthrights, which provides legal advice, training for midwives and doctors and campaigns to improve women’s experiences of pregnancy and birth. She is a freelance writer, occasional doula and wrote the must read book Why Human Rights in Childbirth Matters.
Come grab a copy of Rebecca Schiller’s book at the Human Rights in Childbirth Conference in Mumbai, India!!
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Just a tease...
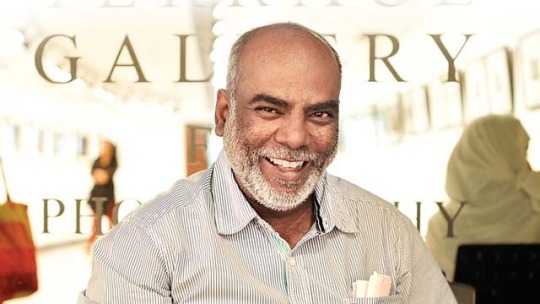
At the upcoming Human Rights in Childbirth Conference in Mumbai, in addition to hearing from and collaborating with experts from across India and the world, we can see stories of care, childbirth and babies through Padmashree Sudharak Olwe’s stunning photo exhibition. In this blog we give you a sneak peak of the raw beauty captured in Sudharak’s photographs.
The Exhibition
Stories of birth; glimpses of mums and their suckling newborns; the caring touch of the age-old ‘dais’ or midwives; a bar of soap and a blue plastic as equipment; thatched huts not measuring more than 12 feet by 12 feet; intoxicating home-made ‘handiya’ or rice beer as ritual and muddy roads nestled between the tall ‘sal’ trees that lead to a village still awaiting electricity.
We bring you real-life snapshots from lives of women belonging to the Ho tribe from Jharkhand, the mining heartland of India. Internationally celebrated photo-journalist Padmashree Sudharak Olwe travelled deep into the tribal belt of eastern India, along with the NGO Ekjut, and documented how small changes can help in the battle against maternal mortality.
With an aim of crossing divides and recognizing the unique intersectional identities of women across the world, the Human Rights in Childbirth conference in India will host this stunning exhibition of true-life photography.


About Sudharak
Sudharak Olwe has been a Mumbai-based photojournalist since 1988 and has worked as a press photographer with some of the leading newspapers in India. Sudharak has travelled the length and breadth of this nation and seen first hand some incredible stories of resilience, courage and change. He has worked in tandem with many NGOs presenting their extraordinary work with both rural and urban communities.
In 2016, Sudharak was conferred the Padma Shri, India’s 4th Highest Civilian Award by the President of India.
Sudharak's photography is that of empathy. It is a journey into the unseen perspective of the human condition. His photography cuts across all barriers and presents to you a moving story of individuals and communities.
Learn some more about him from his website.
Connect with him on Facebook.
Come see Subharak’s stunning photo exhibition at the Human Rights in Childbirth Conference in Mumbai, India!!
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
When children have children
Priyanka Idicula of BirthVillage writes to us about the abused, pregnant teenage girls at Tejus Home who receive care and give birth at BirthVillage under the care of highly sensitive midwives. BirthVillage is a sponsor of the upcoming Human Rights in Childbirth conference here in Mumbai.

When child abuse leads to child pregnancy
“I couldn’t call out as he had stuffed a towel in my mouth and pinned me down though my mother was in the yard.”-S. aged 14.
“He had a sickle in his hand while he approached me.”-R. aged 13.
“I will kill your mother and brother should you even whisper about this.”-T. aged 15.
In 2007, the Ministry of Women and Child Development (MWCD) released a study report on child abuse. The report discusses incidence of child abuse nationwide. It is estimated that 150 million girls and 73 million boys under 18 have been subjected to forced sexual intercourse or other forms of sexual violence. In 2002 there were 53,000 reported cases of child homicide.
Teen pregnancy in India has a different hue and colour than other countries as the majority of them are pregnant through violence and abuse as opposed to from a boy friend through choice. This often leaves physical mental and emotional scars on their young minds with the added burden of social stigma and abandonment by their families. They are often vulnerable and alone. Teenage pregnancies are on the rise in India possibly due to lack of comprehensive sex education and also through perpetrated violence on young children. Though hard to grapple with, child marriage continues to prevail in modern India with statistics putting it at a good 47% in India.
“My husband (aged 45) was a good man. He brought me chocolates, milk and fruits every day and compared to living in the streets it seemed to be a better life,” says this twelve year old.
The abusers are often well into their forties, fifties and even their sixties and most often come from within their families- fathers, step fathers, cousins and uncles or simply someone the child trusted. They would often play on the submissive nature of a child who often return favours for being a ‘good child’ or it would simply be repeated acts of violence for no rhyme or reason.
Busting myths
One of the biggest myths that we understood during our various rounds with many medical practioners is the belief that young women below the age of 18 are incapable of birthing children vaginally. The most common reason stated, that the pelvis would be either be too small/contracted/or wouldn’t have developed enough.
We seem to have forgotten that most of our grandmothers from this part of the world have birthed our parents pretty much in their teens and have had large families too...
But, it became quite clear to us that after 4 years of running the Tejus home and caring for these young women, that if one girl can carry a child to term with a healthy pregnancy, then by all means the others deserve at least a good trial of labour- often to be met with nothing other than excellent outcomes.
The other sad fact that came out in the open was the unkind treatment that was meted to these young girls during checkups at medical institutions with incessant questioning. It was like they would be raped verbally over and over again.

Priyanka Idicula, CPM, weighs a healthy baby born naturally from a 13 y/o girl in BirthVillage
Filling in the gap with love & sensitivity
Tejus Home opened through a chance encounter with a pregnant thirteen year old girl, Gayathri, placed at a destitute home whom we followed through pregnancy. Unfortunately these homes are often filled with women from streets, they would tell tales to young girls about horror stories of births. She was often filled with fear with mere mention of birth. She went into labour by 38 weeks only to have c section performed within 3 hours of entry to a medical institution.
After meeting and followinf Gayathri, it became clear to us there was a definite need for:
A safe space for young pregnant teenagers which would offer good nutrition,
A space where they could laugh,
A space where they could nourish their babies,
A space where they could be free,
A space which they could call their home.
And that’s how Tejus Home was born in November 2012. It is named after Gayathri’s son, the first girl who was sheltered at the home. We work in collaboration with the child welfare committee and receive girls from all across the state. It is also mandatory that all girls would have registered FIR against the abuser.
A separate home which catered exclusively to pregnant teens did not exist in India at the time of the inception of the Home. Hence, we had no mentors or prototype to model our home on which lended us a fair share of challenges.
By virtue of running a birth centre we were also able to offer free medical care and midwifery led support for births for the girls.
They attended childbirth education classes that were tailored especially for them, keeping in mind their maturity, education level and social status and with strong emphasis on eating healthy and exercise. Theses girls went on to have very healthy pregnancies, healthy births and very healthy outcomes.
TEJUS HOME is a caring environment where abused, pregnant teenagers are given a safe and nurturing place to live; it is located in Kerala, India. It is a pilot project in partnership between two NGOs, Dil Se and Birth For Change and is recognized by the Child Welfare Committee.
Here is some of what we offer in the home:
Information and resources to help the girls make choices about their pregnancy, their baby and their future.
Counselling for the young mothers and for their family
Encouragement to continue education during pregnancy and after birth.
Free birth preparation and education classes
Free Individualized health care: prenatal, birth and postnatal care with a midwife
Sexual education
Life-skills training: self-confidence and self-esteem, assertiveness, finances, home management, gardening etc.

Baby born to a girl at the Tejus Home with the care of midwives.
A model of CARE for those who need special care
Often a simple vaginal exam can trigger the abuse that these children went through. Knowing this, throughout the entire pregnancy and birth, we strived hard to do without a single one. If absolutely required, we would do one, only if she consented.
It has been often recounted to us at our clinic that many of these young girls have still been subjected to the Two-Finger test, [what is this?] despite the clear clamp down on this procedure by the Supreme Court of India. This degrading procedure, done on a cold table by a stranger in a white coat, does nothing but to relive her trauma again.
Girls who come to the Home often tend to hide their pregnancies and have no one to confide in. They starve themselves during the initial months of the pregnancy by having just one meal a day, hoping that their bellies wouldn’t show.
They are often silenced by their abuser with threats wielded against her and her loved ones. Afraid of revealing what happened, they continue to hide under over sized clothes until it is beyond limits to cover up until the pregnancy is brought to the fore by teachers and neighbours and sometimes by their own family members.
Social osctracization is very high for these girls. One of our girls recounted how the neighbourhood threw their entire family out, which included her mother who was mentally ill, her younger sister and brother, on to the streets despite the abuser being her own father.
On arrival to the home they do take a few days to settle down, they do go through a lot of ups and downs during these days, grappling with what happened in their life. But soon after they bond so well with the other girls at the home and form friendships that often last beyond their stay at the home.
Long consults with information, love and care transforms them tremendously and they blossom well.
They motivate each other when it comes to prepping up for labor. They try hard to eat their vegetables, easily climb up to 200 steps a day, walk for over an hour and very naturally committed to a natural labour default.
Meeting challenges with determination and support
One of the biggest challenges at the home would be how late in the pregnancy these girls come to us. On average, girls come when they are around 6 months pregnant and often barely weigh around 40 kilos.
Another battle would be anaemia. These girls often have be haemoglobin levels as low as 8g/dl. We even have had reports of young girls who have not eaten anything beyond rice, potato and beetroot during their entire childhood.
Both of the above mentioned state of affairs requires a lot of work, close monitoring and encouragement from our side to get them going, especially in the face of teen rebellions.
We have been amazed at the resilience and strength of the girls when labour starts at Tejus Home. They wait it out as long as possible, go about their daily tasks with the other girls often massaging their backs and placing hot water bags. As one girl put it, “I said felt like rolling on the floor- that’s when I decided it’s time for me to go to meet my Chechis.”
These young girls have often blown us away with their shining grit and strong nerves. Rarely do we hear them say they can’t do it or let alone struggled at all in active labour or when they were pushing their babies into the world.
What was needed the most was love, support and a good pair arms to hold them in their hour of need.
We can easily say that 100 percent of the girls who have birthed at BirthVillage have birthed with gravity, in the position of their choices either using the birth rope or on the birth stool or by simply squatting on the floor.
How far love, support and belief in the efficacy of birth goes- see for yourself
Updated Tejus Home statistics currently available from 2013:
80 percent of the girls had a natural birth
5 percent were transferred for assisted delivery
15 percent were transferred for c section
(Reasons for transfer include: signs of preeclampsia and obstructed labour)
95 % of the babies born full term were above 2.5 kg
4% of the babies born passed away at three months owing to respiratory complications
80 % of them do go back to school within 6-12 weeks after having birthed their babies
The youngest girl to have had a natural birth from tejus home was 12, and the average age 15 years.

This 14 y/o received exceptionally sensitive care from midwives and gave birth naturally to a healthy baby
When birth heals
An empowering birth experience strengthens these young girls and offers them courage and hope for their lives ahead. As one of the girls put it, “A window of calm in the most trying period of their lives.”
Another remarkable common feature we observe at the Tejus Home is that after the birth, they often fall into a deep slumber for a good couple of hours as if a big weight has been lifted off their shoulders.
A good 97% of them do give up babies for adoption and as midwives it is one of the hardest things to do when the girl requests the baby not to be shown after birth or when she weeps inconsolably when she gives up her child for adoption. We have been humble witnesses as a few of them cradle their child, stroke them and even feed them even if it’s for one night.
We were also blessed as we have had quite of few of our staff who were nursing mothers themselves who offer skin to skin and have breastfed many of these babies. In addition, many of the BirthVillage mothers offer pumped milk.
Postnatal time is an equally valuable time at Tejus. The girls have to process, once again, the grief and heal both mentally and physically. They often request pictures of their babies. They draw, paint or write their emotions down in diaries and create keepsakes and often take a piece of us when it’s time to say goodbye to us, albeit to a bright future forward.
We are equally proud to say that some of our girls are currently A plus grade students at school/college and continue to win laurels, and other girls who continue shine at their vocational training.

Priyanka Idicula is certified professional midwife (U.S.A.) and is Lamaze certified childbirth educator. She is currently the director of BirthVillage, The Natural Birthing Centre in Kochin, Kerala and is the managing trustee for Birth for Change (NGO). She also carries with her bachelors and masters in microbiology and has had long stints with various MNC, the last being Johnson and Johnson where she worked as regional head for application support in the diagnostic division. She strongly advocates for evidence based maternity care and works for rights for women who are from the underprivileged sections of society.
Visit BirthVillage on the web or Facebook.
Checkout Tejus Home on Facebook and watch this beautiful short film.
Also see what Birth for Change has going on on Facebook!
Come get involved at the Human Rights in Childbirth Conference in Mumbai, India!!
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
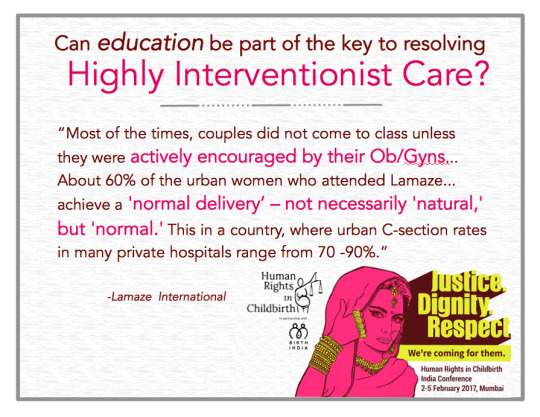
Lamaze In India – As it stands today
In our last post about Lamaze International, they told us about how they advocate for healthy birth practices and work to empower women’s birth experiences through education. But in this blog, we learn about the experiences of the childbirth educators working in India. Lamaze is sponsoring the upcoming Human Rights in Childbirth Conference in Mumbai.
When I was asked by Lamaze International to write this blog as a part of a series for the Human Rights in Childbirth India Conference 2017, I wondered what I could write that would show the depth of need for childbirth education in India. I realized that Healthy Mother’s former students who are now LCCE Educators teaching Lamaze classes in various parts of the country are the best source of information regarding this need. Healthy Mother is the only accredited childbirth education organization in South Asia that helps train childbirth educators to become certified with Lamaze International. So I set out to interview some of our former students.
First, an important note:
In a country of 1.2 billion people, we currently have only 19 Lamaze Certified Childbirth Educators. This number needs to go up exponentially if we are to provide scientific, evidence-based information to a whole generation of pregnant women! The trouble is, as I found out very quickly in my interviews, this potential is limited by medical professionals, many of whom are very reluctant to refer mothers to childbirth education classes.
What I found out:
I found the following information about the current LCCEs here in India:
1
Lamaze International is very new to India and as such, there is quite a range of educator experience from as little as two months to as many as nine years.
2
Six of the LCCE Educators taught hospital based classes. The rest taught independent classes. Some of them started teaching hospital classes, but left to teach independently because of overwhelming pressure in most hospitals to teach a class which was mainly exercise and breathing based, and barely addressed interventions in childbirth.
3
There is a wide range of couples that these educators have worked with spanning from 8 to 1000 couples, depending on how long the educators had been teaching.
4
Most educators noted that couples learned about their classes by word of mouth. Some have active marketing and social media pages to promote their Lamaze programs. One childbirth educator, who has been teaching for a while, also gets some referrals from local OB/GYNs. Only four childbirth educators, who are employed in big hospitals, get referred clients consistently. Usually couples do not come to class unless they are actively encouraged by their OB/GYNs.
5
90% of couples who attended these classes initially thought it would be an exercise/breathing/Yoga class. Lamaze is still viewed as a technique, as opposed to a way to be empowered and informed about the birth experience! The exceptions are Birth Center-based classes like ours at The Sanctum, Natural Birth Center, and BirthVillage in Cochin, where most couples come expecting childbirth education to help them labor and give birth with confidence.
6
The feedback that our educators receive from parents is incredibly positive, 95% report leaving incredibly informed. They leave feeling equipped to talk to their doctors and ready to make informed birth decisions. However, after the birth experience, many couples report that their doctors were not receptive to the desire for a natural birth, and mother’s found it difficult to control their birth experience.
7
There is currently a wide gap between the medical community and childbirth educators. Most independent educators feel that the medical community is not so receptive of Lamaze classes and childbirth education in general. Many OB/GYNs encourage educators to limit themselves to teaching exercises and positions, comfort measures and breathing techniques. The medical community in India still appears to view childbirth as a form of suffering, from which women need to be saved, as opposed to an opportunity for women to be empowered.
8
About 60% of the urban women who attended Lamaze classes gave feedback that they had managed to achieve a “normal delivery” – not necessarily “natural,” but “normal.” This in a country where urban C-section rates in many private hospitals range from 70 -90%. The mothers also felt that taking the classes had made them better prepared to manage the challenges of labor and birth. However, during labor, many of them felt helpless when their birth plan or preferences were not respected.
In short, they felt empowered when they attended Lamaze classes, but felt that they had no say during the process of labor and birth. Yet, about 70% of them viewed the Lamaze classes (post-birth) as contributing to a decent birth experience.
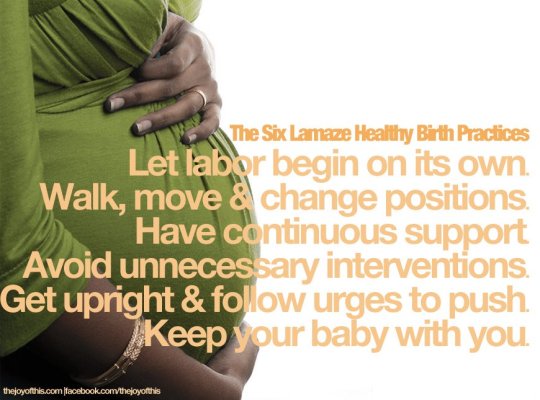
Lamaze works
Today, Lamaze childbirth classes provide the knowledge, skills, and support that help women give birth with confidence and joy as they have done for centuries. Lamaze is for everyone!!
As I wrote this blog about Lamaze Childbirth Educators’ experiences in teaching classes in India, I realized it was crucial to share that Lamaze works!
Lamaze that “works” has nothing to do with feeling pain, taking or avoiding medication, or developing complications that necessitate medical interventions. Rather, Lamaze teaches women that nature has a simple design for birth, and that women already know how to give birth. Lamaze “works” if women trust their bodies to give birth, have the freedom to work with their bodies as labor progresses, and are supported by health care providers, family and friends who wait patiently for nature to do its incredible work. Lamaze “works” if birth is allowed to work!
**written by Dr. Vijaya Krishnan, CPM, DPT, LCCE, FACCE

Connect with others, develop professional opportunities, and get high quality resources to support expectant families to have a natural, safe, and healthy birth with Lamaze International. As a part of their commitment to promoting the improvement of birth, they are sponsoring the upcoming Human Rights in Childbirth Conference in Mumbai this February.
Come see why Lamaze is supporting the Human Rights in Childbirth Conference in Mumbai, India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
The Disparities in Care- women’s voices and solutions
What matters? Why does it matter? As a birth worker, Lina Duncan has a few non-negotiable values: Dignity, Kindness, Respect, and a blanket of Compassion. Here she shares with us her training and experiences as a midwife, which took her all over the world. Lina will be speaking at the Human Rights in Childbirth conference in Mumbai.
The start of a colourful journey
My journey as a midwife has been an interesting one. As a British citizen, I found myself on a midwifery training course in El Paso, Texas with the New Mexico College of Midwifery. The first birth I observed was in a large, and very busy Mexican hospital, just across the border in Juarez. I will never forget the baby’s hand and arm appearing before its head! That’s where my compassion for this wonderful life-work begun.
My college fees funded a brilliant initiative in the Philippines, providing simple, safe, clean and respectful clinics for women to birth their babies. This was the place I put all my learned knowledge into action. Learning and growing in the Philippines was substantial. Each family I met there in the simple clinic in the middle of a notorious slum where we lived, and served, taught me something different. Women chose to birth at our clinic for many reasons. Many could not afford the time to leave their families to admit into hospital, didn’t have money to pay for the medicines at the government hospitals, or were afraid of the overcrowded wards that you can get a taste of here.
The taxi drivers would regularly refuse to drive in because of the area’s bad reputation. I learned the language, fell in love with the people, facilitated hundreds of births, often in the quiet of the night.
Fast forward – another chapter begins, in Mumbai, India, the “city of dreams”
In India I have seen many aspects of life, and I still consider myself on a learning journey about this diverse and colourful culture. Along with my colleagues, I set up a private limited business, Mumbai Midwife in 2008 which was the maternity section of a company called Justlink Health Services.
The vision behind “Justlink” was to provide just and respectful services for all, to bridge links between national and international people, to create a richer experience for all. To some extent it was successful, but without a #MidwifeModelOfCare across India it was a challenge to maintain a successful business model.
I met some beautiful people, whom I now call my friends and whom I had the honour of attending those precious times surrounding pregnancy, birth, and beyond. I have stepped over the threshold into mansions and my feet have walked barefoot into the most basic of shelters by the railway, or the roadside. Both, and all were a privilege. I believe we experienced ripples of change in the culture of childbirth.

(Photo by Lina from a high rise flat after a home visit to a pregnant woman)

(Photo: Lina Duncan in Mumbai)
You can see the disparities of habitat in these pictures. Strangely, the enormous gaps in wealth did not necessarily contribute to a different birth experience. I saw a lot of similarities and will share some women’s stories here, and at the conference next week. Some of the families I met on the street or in government housing requested me to accompany them to the local government hospitals. Most of the families were already vulnerable with complexities such as domestic violence, substance abuse, temporary shelter as a “home.” Their daily lives are a struggle for survival in all aspects. I have written a birth story of a dear friend for Birthrights UK here.
On several occassions I made SOS phone calls to Doctor Armida Fernandez, who will also be speaking at the HRiC Mumbai Conference when I was with women or babies with particularly complex needs and care was not being provided. Because of her kind and prompt assistance through the decades of her work as a neonatologist, we were able to facilitate life-saving care and solutions to the issues. I don’t know what I would have done without her help!

(photo by Lina of a community of Government housing where a high percentage of women access local government facilities for perinatal care)
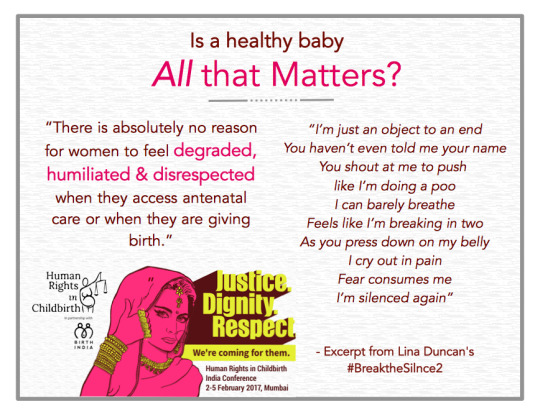
One of the ways I tell my own stories and those of others is in poetry. This one represents hundreds of women that I witnessed in Asia. It broke my heart to see people I know, and also complete strangers experiencing care like this. I wrote it for the women who have suffered in silence, for the ones that don’t know how or what to say. It’s not exaggerated. If anything, it’s tamed down a little. I have witnessed worse than this. Globally women are often told “A healthy baby is all that matters”.
How can we say this and ignore her emotions, physical and spiritual experience?
#BreakTheSilence2
Look at my face
Please tell me your name
I'm all uncovered and feeling ashamed
I want to move, to squat, to stand
Yet mobility is forbidden in this lonely “labour land”
I can't describe the pain
Of lying flat on my back here
Worse my shame of nakedness
I learned to swallow my tears
I've closed my eyes and closed my brain
I'm not involved in this birthing game
I'm just an object to an end
You haven’t even told me your name
You shout at me to push like I'm doing a poo
I can barely breathe
Feels like I'm breaking in two
As you press down on my belly
I cry out in pain
Fear consumes me
I’m silenced again
You cut me below
I heard the scissors snip
It’s like I'm watching from above
The pain and trauma makes me drift
To survive this hour
I've gone somewhere else in my head
Yet when I hear her sweet cry I'm back on earth instead
Childbirth is a life-changing event and a pinnacle one for each mother, baby, family member involved. It costs very little, financially to be able to incorporate kind and dignified models of care. Often some creative thinking and input is required, especially in busy, urban, institutional settings. In this day and age there is absolutely no reason for women to feel degraded, humiliated and disrespected when they access antenatal care or when they are giving birth.
How can we bring compassion to the birthplace? Surely that's how we would all want to be treated and how we would want our daughters and granddaughters to be cared for?
#BetterBirths for all
One of the important lessons I learned during my midwifery training was to be kind, be kind, be kind. To provide the best care I needed to learn to listen more, and not just to the spoken words. I find as a care provider, it starts with me. My well-being, my language, my attitude, my responses (including any physical touch)
How are birthing (delivery) rooms designed?
Is the set up for comfort and benefit of the woman or the care provider?
Where are the doors?
Who comes in and out?
Does each woman have privacy?
Does the woman have a companion she knows?
Does she feel safe?
Can she be mobile if she chooses and adopt positions as per her instinct and choice?
Are procedures explained?
Is there informed consent and informed refusal?
Is the baby kept with its mother?
Is breastfeeding support offered?
Is data recorded and statistics transparent?
(Photo: Lina Duncan, Mumbai)
Why it matters
Welcoming a new life is a memorable and special occasion
It may only happen once for the mother and it only happens once for each baby.
She will remember it forever.
It affects how she will start her journey as a new parent.
It can affect her relationship with her partner and her new start for each new parenting journey.
Our planet is in trouble. There are many things we can't change but there are ways in which we can make a difference, in the way we treat women, their partners and their baby/babies in their care surrounding pregnancy, childbirth and the first 1000 days.
As in any sort of “service” it's a healthy partnership that facilitates a good outcome. I recently attended #Womensvoices16, an even set up by Michelle Quashie in London. Women were on the stage speaking of their child birthing experiences, the effect of their experiences on them personally and on their family, etc. We also heard from an obstetrician and the pressures on her, her typical day and the demands from all sides on her time, professional opinion and skills. Speaking and listening to each other, on a regular basis, it's possible to build an infrastructure of services that benefits everyone.
Michelle Obama recently said “Diversity is not a threat – It makes us who we are.” One of the hopes I have for this Human Rights in Childbirth conference is that as we listen to the presentations and in the conversations, in-between, we share our stories, our failures, our learning tools, our diversity and bring a collaborative change to childbirth, both nationally and globally.
The disparities in wealth do not necessarily mean that a woman and her baby have a better or worse experience giving birth to their babies. How is this happening?
Here is an example from a private, expensive hospital:
She came from Asia and was fit and healthy. She chose a doctor and a hospital closest to home for convenience despite knowing that she probably would not get what she wanted on her birth plan. She started the process physiologically (no induction). She had many internal examinations without much discussion/ consent and eventually her waters were ruptured during one of those exams to “speed the process.” She didn’t give consent for this. Her eyes pleaded with me for them to stop but she spoke no words. During the birth, she was told “You will never be able to push this baby out. It's too big. We are going to have to help you.” A ventouse was applied. Her doctor pulled on that whilst the anaesthetist gave fundal pressure from above, which was so strong it left a bruise. A healthy baby is presented. Again, it was stated, “You would not have been able to do this yourself.”
Job done.
Everyone smiled and carried on as usual. I felt sick and put on a brave face and voice for the sake of the parents. How do you think women feel after an experience like this? Does it affect their breastfeeding and early parenting attachment and confidence? When women are told, or given the message that their bodies don’t work, it can create anxiety, lack of confidence, an inability to breastfeed or care for their newborn. Some women and their birthing partners have symptoms of PTSD such as flashbacks of the traumatic birth experience.
This is not okay.
This is one reason that there is a cry for midwifery care in India. Women are searching for what they want and choosing their own journey, albeit a challenge. It’s always worth going the extra mile for this major, life-changing event. Even if the plans and dreams don’t work out as expected, when the woman and her partner / family are in the centre of the picture, making the decisions and agreeing to, asking for, or refusing treatment.
That’s what matters.
Woman/family-centered care & midwives
I was honoured to welcome this little girl as her mother Kanika birthed her in the presence of her husband, brother, sister and mother in her own home. You can ask her yourself if you attend the conference. She is the event manager from the Birth India team.

(Photo credit: Neha Chopra for Out Of Focus pictures, Twitter: #oofpictures @oofpictures @foreverjugni)
I believe there are solutions. Similar issues and creative ideas for improvement are also being shared around the world.
Rethinking the role of midwives in the region and forming an independent Midwifery unit in India would benefit everyone. Autonomous midwives provide quality of care, continuity of care when possible, have lower caesarean rates and less interventions such as instrumental birth. Midwives are trained to facilitate “normal” birth and to refer complex issues to a doctor.
I have worked alongside many doctors in India and have used the collaborative model that works so well for all concerned. I’m looking forward to the Asia launch of the Maternal Lancet Series and to the inspiring conversations that are going to begin/ carry on from experts who have travelled across India and the globe to share hope for Midwifery in India and better births for all, for generations to come.

Lina Duncan is returning to India from London, UK where she is pursuing further education in Midwifery, to speak at Human Rights in Childbirth Conference, Mumbai. She loves to wear saris, eat Pani Puri, watch Bollywood films, visit her friends on the street and catch up with the families she was a midwife or a doula for, in Mumbai, Pune and Nashik. Lina is also part of the Conference Planning Team as an active member of Birth India for the last 9 years.
Lina’s website: mumbaimidwife.com
Don’t miss Lina at the Human Rights in Childbirth Conference in Mumbai, India!!
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Bloom Healthcare is listening to women and trying to bring the “natural” back to birth
Bloom Healthcare in Chennai is another Indian maternity hospital taking efforts to offer woman-centred, respectful maternity care. They are sponsoring the upcoming Human Rights in Childbirth conference in Mumbai as part of that effort. Read on to know more about their services and come meet some of the valuable staff at the conference.
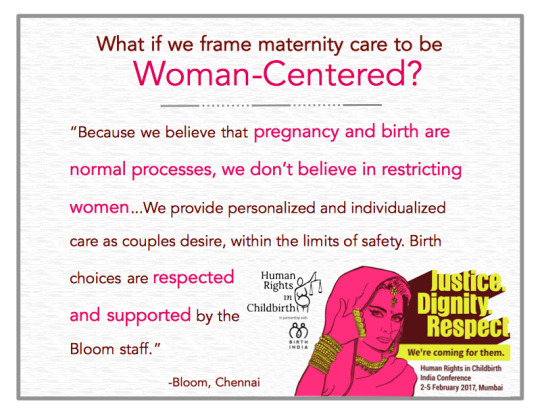
Bloom is a “Natural Birth Boutique,” unit attached to Bloom Healthcare hospital. We provide a home-like environment, rather than the hospital labor ward. Because we believe that pregnancy and birth are normal processes, we don’t believe in restricting women; this is why we generally allow food/drink, music, and the attendance of family and spouse/partner.
Women are free to act more spontaneously during their birth, such as finding comfortable postures that assist in labor. Active birth, rather than lying down in bed, is encouraged!
Childbirth choices
We provide personalized and individualized care as couples desire, within the limits of safety. Birth choices are respected and supported by the Bloom staff. For example, any birth position that is comfortable for the mother is acceptable.
Water birth
The Bloom is pleased to be able to offer water birth for women who have a low risk of developing complications. We know the use of warm water can bring great relief to laboring and birthing moms. We have spacious tubs and showers that can accommodate both the mother and the father. Bloom Birthing Centre is fully equipped, to cater for your needs during labor and birth.

This couple travelled a long way to birth in one of our tubs! [photo credit: Bloom Healthcare]
Vaginal Birth After Cesarean
There is a common misconception that if a woman has had a cesarean delivery, a c-section, then any subsequent birth must also be a c-section. However there is a possibility to deliver her next baby vaginally. This is called vaginal birth after cesarean, or VBAC, which we support for eligible candidates.
Hypno Birth
Bloom provides Hypno Birth sessions to prepare women for natural labor and birth. Through the use as self-hypnosis, the mind can be reprogrammed to expect relaxation and pleasure rather than fear and pain. This process reduces the amount of adrenaline that is produced, addressing one of the primary causes of dysfunction in labor. A hypno-birth also reduces the need for interventions including caesarean sections.
Delayed Cord Clamping
Because we are committed to providing evidence-based care, we make sure babies have delayed cord clamping. Contrary to what is routinely practised throughout India (immediate cord clamping), this is a a birth practice where the umbilical cord is not clamped or cut until after pulsations have ceased, or until after the placenta is delivered. This way, the baby receives as much of it’s blood as possible and therefore is more likely to have a healthy start. Many of parents are choosing delayed cord clamping for their baby. We have even had parents who had delayed cord clamping for 2 hours and more.
Placental Encapsulation
We also offer the service of placental encapsulation. This where the placenta is steamed, dehydrated, ground, and placed into pills for the mother to consume. Tradition and holistic medical customs embrace a number of potential advantages which come from ingesting the placenta. Possible benefits are: increased release of the hormone oxytocin, which helps the uterus return to normal size and encourages bonding with the infant, increase in CRH, a stress-reducing hormone, decrease in post-partum depression levels and Increase in milk production.

The placenta in it’s raw stage ready to be dried [photo credit: Bloom Healthcare]

The placenta that has been dehydrated and powdered, ready to be put into capsules for the mom to swallow! [photo credit: Bloom Healthcare]
Aqua-natal Session
Aqua-natal is a wonderful form of safe exercise during pregnancy. This session will help a mother in Positions, breathing, and comfort techniques. The benefits of buoyancy and hydrostatic pressure makes the participation of Aqua-natal not only enjoyable, but also advantageous to women both during and after their pregnancy.

A fun aqua-natal session! [photo credit: Bloom Healthcare]
Centre Facilities include:
Private suite rooms with nursing staff
Neonatal Intensive Care Unit
Birth rooms
Bedrooms comfortably furnished
Large birth pool
Moms Kitchen provides healthy home like food in Birth Centre
Family room with dining facilities
All of the specialist support services
Obstetrician, Gynaecologist, Neonatologist, Pediatrician, Childbirth Educator, HypnoBirth Practitioner, Aquanatal Instructor, Pregnancy Massage, Labor support services, Lactation Consultant, Physiotherapist, Occupational Therapist,Post Pregnancy Massage, Ayurvedic Massage, Speech Therapist, Neurodevelopment Therapist, Psychiatrist, Integrated child development centre are available if required.
Birthing Services
Health assessment and care throughout the antenatal, birth and postnatal experience (regular visits are required).
Personalised attention to each woman’s individual needs and choices.
Information and support to individuals choice.
Antenatal education covering
Physical and emotional changes
Changing family roles
Maintaining health through exercise and nutrition
Aquanatal Classes
Mom's Library to get to know more about pre and postnatal care
Active birthing including coping strategies for labour and pain relief options
Breastfeeding Support
Familiarization of the Birth centre
Expectant mom and her support person and family are encouraged to get to know the consultants, experts, support staff and environment where the baby will be born via:
A tour of the Birth Centre facilities
Regular antenatal visits
Attendance at Childbirth education classes
Hypno Birth Sessions
Aqua natal Classes
Specialized Pelvic/Prenatal Massage
Foot Reflexology
Birth Room visits
Postnatal care
Full Pediatric examination, newborn screening and newborn hearing screening will be offered.
Post Natal Shape Up Class
Mother's Club from 3 months to 15 months

Bloom Healthcare is an ISO 9001:2008 certified super-specialty hospital. To establish Bloom Fertility and Healthcare as a ‘Centre of Excellence’ in Health Care in India. We at Bloom Healthcare provide quality healthcare services to meet the patients’ requirements through continual improvement by applying quality management system of the process. Boom Healthcare will follow the highest possible quality standards and ethical practices in all treatment procedures to ensure positive clinical outcomes. Commercial considerations will not influence the decision making process in any treatment. The patients right to ‘Privacy, Confidentiality & Dignity’ will be respected and adhered to at all times. The patients will be involved at every stage of the treatment process and ‘Informed Consent’ will be paramount in decision making
Please connect or visit us at: No-32, Taramani Link Road, Velachery, Chennai - 600 042, India
Phone: 044 - 40000009 / Cell: 7299911102 / 7299911104 / Email: [email protected]
Facebook: https://www.facebook.com/BloomHealthCare.in
Don’t miss the action at and meet some of the Bloom staff at the Human Rights in Childbirth Conference in Mumbai India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
A letter from the President of HRiC

Dear Stakeholders in Childbirth,
Nearly five years ago in response to the landmark Ternovszky vs. Hungary decision in the European Court of Human Rights, founder Hermine Hayes-Klein convened the first Human Rights in Childbirth conference in The Hague, Netherlands. A small organization formed soon after the inaugural conference, and then incorporated in 2014 as a non-profit in the United States with a board of directors.
Our collective vision: to put women at the center of maternity care everywhere.
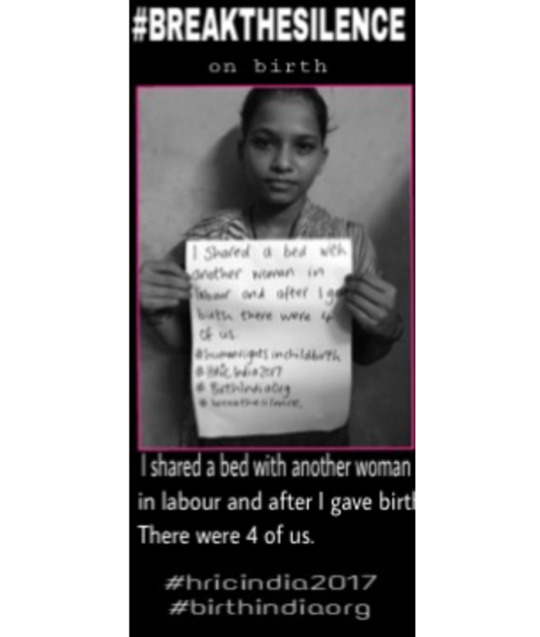
Since our founding, the global awareness around the violations of women’s human rights in childbirth has increased exponentially, with professional statements from the largest multi-lateral organizations, emerging research paradigms, and most importantly, more women coming together to share experiences of injustice. Evidence is mounting in India, from studies to the voices of women, that too many woman are going through childbirth without dignity, respect, or with their basic human rights.
We at HRiC have become ever more emboldened to achieve our mission: to connect grassroots activism with legal advocacy to make human rights in childbirth a reality for women around the world.
We have done this by convening multi-stakeholder meetings in Johannesburg, Zagreb, Los Angeles, and now Mumbai. At our conferences all participants—speakers and audience--have engaged in productive conversation to define the contours of abuse in different regions and to map out solutions. Women, have shared their stories of mistreatment; providers and lawyers have discussed the challenges of supporting women’s full realization of their human rights in maternity care. By facilitating these discussions HRiC uniquely merges grassroots activists and legal advocates on the path toward developing regional strategies, and we build vertical connections to international stakeholders.
This is why we have specifically allocated the last half day of the India conference for the collaboration of speakers and attendees to brainstorm the needs and the remedies to facilitate improvements within Indian maternity system.
In the coming years we will pursue regionally coordinated legal strategies and build an international network of lawyers to develop and publish argumentation that can be used to educate and advocate about human rights in childbirth.
We intend to create a “Know Your Rights” documents in multiple languages so that women, lawyers, and providers can make more informed choices and take purposeful action.
We plan to build the capacity of women’s rights organizations to report to UN bodies, creating international pressure to uphold human rights in childbirth.
Thank you to the incredible team at Birth India, our speakers, and our attendees. We could not be more excited to work with you to make cost-effective, universally accessible, routine or emergency, woman-centered maternity care a reality for all women, on their terms, regardless of race, cast, language spoken, or socio-economic status.
Have a great conference,
Nicholas Rubashkin, MD
President of the Board Human Rights in Childbirth

HRiC is an international network of some of the most influential thought leaders who work to address global maternal and newborn health issues through the lens human rights in interdisciplinary and innovative ways. HRiC integrates the professional and political segmentation of women’s and children’s health, and advocates for recognition of the full range of human rights at stake in pregnancy, childbirth, and postpartum.

Birth India was initially founded in 2007 by five women in Mumbai from various nationalities. These women were looking to make a positive difference in the way women in India are cared for during pregnancy, childbirth, and postpartum. Since inception, we have seen an increase in the presence of international childbirth education, birthing options, doulas, midwives, and lactation institutions within India. Our mission is to promote the benefits of best practices for childbirth in India by advocating for women’s reproductive rights and spreading awareness on mother-baby-friendly care.

Our partners include: Human Rights Law Network, The White Ribbon Alliance, United Nations Family Planning Association, The Tata Institute of Social Science, The Lancet and IdeaHive
Come be apart of this incredible work at the Human Rights in Childbirth Conference in Mumbai India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
The HRiC India Conference Lineup!!!
If you don’t already know about the upcoming Human Rights in Childbirth Conference in Mumbai, here’s a chance to get a deeper look at the happenings of the event. Check out this blog to see the amazing speaker lineup and topics to be covered. Please come to be apart of this much needed discussion, advocacy and change!!

SYNOPSIS OF THE CONFERENCE - Women have a right to survive childbirth, but it is not their only human right.
The Human Rights in Childbirth Global Conference in India will be held at the Tata Institute of Social Sciences in Mumbai from 2-5 February to 2017.
The event addresses how maternity care can optimize maternal and infant health outcomes in a respectful, culturally sensitive, human rights framework.
The Conference will convene a vibrant and interdisciplinary group of maternity care providers, public health professionals, lawyers, activists, policy makers and reproductive justice advocates and others interested in advancing respectful and evidence-based care.
Collaborators and participants will join the front edge of global efforts to eliminate disrespect and abuse in maternity care and ensure non-discriminatory access to care for every woman and baby.
This Conference will help evolve global maternity care policies and practices from the critical recognition that preventable maternal mortality is a human rights issue, toward recognition of the full spectrum of human rights at stake in childbirth.
Together, attendees will envision maternity care systems that attend to the healthcare needs and human rights of mothers, babies, families, and communities worldwide.
DAY 1 - VOICES OF WOMEN - 4, FEB 2017
Keynote Address
Aparajita Gogoi (WRAI)
Plenary Panel: Indian Maternity Care Development and Human Rights - is there a connection?
Dr. Kirti Iyengar (UNFPA)
Dr. Prakassama (ANSWERS)
Dr. David Osrin (Paediatrician)
Kerry McBroom (ICRC Rapporteur)
Panel 1 - Women’s Experience of Care - too little too late?
Unnimaya Kurup (IIT Madras)
Sohini Chattophadya (FreelanceJournalist)
Asha Kilaru (BBN) & Pushpalatha M.
Sarita Barpanda (HRLN)
Panel 2 - Non-Discriminatory Access to Maternity Healthcare Services
Manju Kamarcharya
Sushma Shende (SNEHA)
Nalini Visvanatham
Regina Tames (GIRE)
Panel 3 - Womens' Experience of Care - too much too soon?
Ibu Eka Maya, Midwife Indonesia (video)
Subarna Ghosh (Birth India)
Vijaya Krishnan (Healthy Mother)
Lina Duncan (Mumbai Midwives)
DAY 2 - SYSTEMS OF CARE - 3, FEB 2017
Lancet: Maternal Health Series (Asia Launch)
Prof. Suellen Miller, Ob/Gyn (London School of Hygiene and Tropical Medicine)
Prof. Lynn Freedman (ADMM)
Panel 1 - Organizing healthcare for Improving Quality and Respect
Prof. Neel Shah (Ariadne Labs)
Dr. Jishnu Das (Worldbank)
Prof. Lesley Page (RCOM)
Panel 2 - Supporting Healthy Birth
Dr. Armida Fernandez (SNEHA)
Stella Mpanda (Childbirth Survival International Tanzania)
Maha Al-Musa (EmbodyBirth)
Amelia Christmas (PRONTO)
Panel 3 - Evidence and Human Rights in Indian Obstetric Medicine
Dr. Evita Fernandez & Indie Kaur (Fernandez Hospital)
Dr. Arun Gadhre (SAATHI)
Dr. Rinku Sengupta (Sitaram Bhartia)
DAY 3 - ACCOUNTABILITY & CHANGE - 4, FEB 2017
Keynote Address - Human Rights in Childbirth - the legal framework in India
Prof. Asha Bajpai (UNCRC)
Panel 1 - Rethinking the Role of Midwives in the Region
Frances McConville (WHO)
Frances Day-Stirk (ICM)
Lancet Midwifery Series
Prof. Saraswati Vedam (University of British Columbia)
Panel 2 - Accountability & Advocacy for Change
Payal Shah (CRR)
Anubha Rastogi (Advocate, Maharashtra)
Sarah Malkani (Lawyer, Pakistan)
Purna Shrestha (Center for Reproductive Rights)
Sabin Shrestha (FWLD)
Panel 3 - Quality, Progress and Vision in Maternity Care
Dr. Aruna Uprety (Nepal)
Prof. Hannah Dahlen (University of Sydney)
Dr. M S Kamath
Closing Keynote - For Richer and for Poorer - changing the landscape of Indian Maternity Healthcare, one woman at a time
Bashi Hazard (HRiC)
DAY 4 - COLLABORATION DAY - 5, FEB 2017
This is a day to for attendees and speakers to work together to discuss the most valuable actions to take to ensure we put back the Human Rights in childbirth.
The questions we will be discussing are:
(a) What are the 5 priority areas that need immediate attention in maternity healthcare in the region?
(b) How will those identified priorities support and/or protect women's human rights in pregnancy and childbirth?
(c) If you were in charge, what steps would you take to make these priority areas a reality?
HRiC is an international network of some of the most influential thought leaders who work to address global maternal and newborn health issues through the lens human rights in interdisciplinary and innovative ways. HRiC integrates the professional and political segmentation of women’s and children’s health, and advocates for recognition of the full range of human rights at stake in pregnancy, childbirth, and postpartum.

Birth India was initially founded in 2007 by five women in Mumbai from various nationalities. These women were looking to make a positive difference in the way women in India are cared for during pregnancy, childbirth, and postpartum. Since inception, we have seen an increase in the presence of international childbirth education, birthing options, doulas, midwives, and lactation institutions within India. Our mission is to promote the benefits of best practices for childbirth in India by advocating for women’s reproductive rights and spreading awareness on mother-baby-friendly care.

Our partners include: Human Rights Law Network, The White Ribbon Alliance, United Nations Family Planning Association, The Tata Institute of Social Science, The Lancet and IdeaHive
Come be apart of this incredible work at the Human Rights in Childbirth Conference in Mumbai India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Empowering the mother—First step to safe motherhood
In this account from Dr. Rinku Sengupta of Sitaram Bhartia, we see the implications of confident, prepared mothers versus the potential effects of unnecessary interventions in maternity care. Dr. Rinku will be speaking at the HRiC Conference in Mumbai this February and telling us more about the substantial and sustained changes she and Sitaram Bhartia made to bring back the normalcy of childbirth in their hospital. And if you missed it, get the full scoop about Sitaram Bhartia’s revealing research and informed institutional changes in this blog.
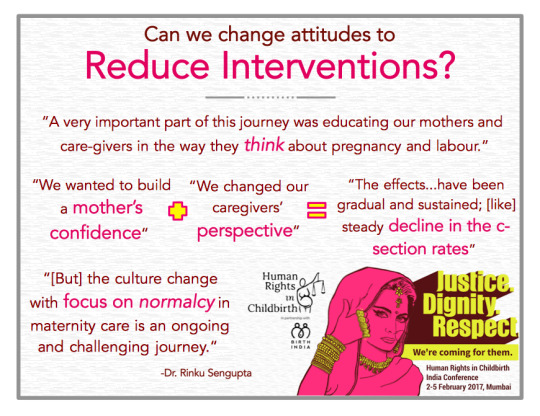
A mother can know best
Betty,* a Brazilian lady and a fourth time expectant mother, came to my antenatal clinic a couple of years back. She was now in the second trimester and was looking for a place which could wholeheartedly support her desire for natural birth.
From what she told me, I felt her personal birth experiences and innate confidence in her body would tremendously simplify her current pregnancy and labour. After all she was a fourth gravida with an uncomplicated pregnancy after three previous normal deliveries and was healthy and active herself.
After chatting with her for some time I realized that she had a difficult first labour in Brazil. Her first baby was 4 kg at birth and she had an instrumental birth. In a country like Brazil where national c-section rates are close to 80% she had a tremendously tough time finding an obstetrician to support her for a vaginal birth.
Although her second stage was prolonged and she was exhausted, she only remembered the positive aspects of the birth, i.e., the immediate skin to skin contact, her baby ready to latch on her breast immediately after birth and the fact that she felt fit to look after the baby soon after.
Her next two deliveries were in China which is also known for its high caesarean rates. She told me she had to accept the care provided there and although it was very professional and prompt, it lacked the human element of maternity care without much scope of discussion and dialogue. She was induced both times and distinctly felt that induced labours were more painful.
I felt her knowledge of pregnancy and birth was profound and she probably did not need my help at all.
Unfortunately she developed gestational diabetes in this pregnancy and at 40 weeks we had to counsel her for induction. She patiently heard me out but was very clear that she would wait till 41 weeks despite understanding the inherent risks of diabetes at term. She asked me not to worry and would report to me in case there was a need. Her exemplary confidence in her body, instinct and the natural process of childbirth overwhelmed me.
Doctors don’t deliver babies, mothers do
The mothers we are caring for most of the time ask us “Doctor, will you deliver my baby?” We find it hard to convince them that they deliver their own babies and we have a limited part to play most of the time as birth is a natural process.
A large, almost obsessive, dependence of expectant mothers on doctors to make everything right in pregnancy and labour along with the obstetrician’s deep seated belief in the need of medicalization of births is a fairly recent phenomenon seen in the last 40 years.
This complicated set of circumstances could be an offshoot of the advances in medical technology like the CTG (a device used to monitor the fetal heart rate) but it is also related to our zero tolerance to any minor or major complications in maternity care.
In our drive to prevent some rare complications we sometimes cause more common iatrogenic complications. If we have to modify this situation, I think we have to first change the expectations that an expectant mother has from her care-givers in general and obstetrician in particular. Doctors should not have to justify doing nothing in face of normality but should have to justify prophylactic interventions.
We have to educate the mothers to understand that in most clinical situations care-givers need not do anything active and need to only support the natural processes of birth and pregnancy.
Only in some situations interventions are required to prevent adverse outcomes. Also important to understand is that some clinical adverse outcomes are not preventable. Uncertainty of bad outcomes must not drive us to medical interventions which may themselves lead to short or long term complications.
The Journey at Sitaram Bhartia
My own journey at Sitaram Bhartia Institute of Science and Research towards the goal of reducing medical interventions in general and reducing caesarean sections in particular has been a rollercoaster ride with its ups and downs, failure and successes. In the year 2001 the overall caesarean rate was 79% in our hospital. Fifteen years back, when we started this project, we realized that one of the many reasons of this high surgical intervention was elective non-medical induction and pre-labour cesarean section (40%) due to patient demand and also lack of continuous trained labour support.
The risk of interventions hit me sharply in 2008 when Sucharita*, a booked expectant mother, came to me in emergency at 37 weeks with vague abdominal pain and spotting per vaginum. Her CTG was non-reassuring.
She’d had a previous non-medical pre-labour CS at 36 weeks in Calcutta. We found a silent rupture uterus – a condition that rarely happens without a previous caesarean - and we could just save the baby in the nick of time.
As an obstetrician I am aware of the rampant, almost epidemic, problem of non-medical interventions especially in the private sector. But how seriously this can affect future pregnancies and how urgently we need to address this problem was reemphasized by Sucharita’s case.
We started our second innings to transform maternity care in our organization in 2011 after a series of trial and errors in the preceding 8 years. A very important part of this journey was educating our mothers and care-givers in the way they think about pregnancy and labour.
We wanted to build a mother’s confidence in her innate ability to deliver naturally, so we developed an education model. Education began from the early antenatal period in the OPD and antenatal workshops. We gave out educational handouts and talked about the benefits of healthy eating habits and exercise; we prepared mothers for a normal delivery on a physical, psychological and spiritual level; we encouraged families, especially husbands, to participate in maternal care and in promoting the concept of normal deliveries.
We changed our care-givers’ perspective by encouraging our nurses and doctors to focus on our outcomes and improvement measures. We also asked our neonatologists to participate in the meetings. The multidisciplinary meetings amongst our nurses and doctors reemphasized the common philosophy and goal of improving our care.
They supported each other and the mother to promote natural birthing. The culture change with focus on normalcy in maternity care is an ongoing and challenging journey.
The effects of these interventions have been gradual and sustained; and over the last 4 years, there has been a steady decline in the caesarean section rates (CSR) at our institute. In the year 2015 our c-section rate was 28%. We have realized that preventing the primary caesarean sections in low risk mothers at present will be the most effective method to reduce caesarean section rates (CSR) in future. Our c-section rate in low risk primigravidas is below 20% in the first half of 2016, our VBAC rates have also gone up and 70% of our mothers who opt for trial of labour after one caesarean are successful.
The Next Steps for Moving Forward
Betty visited us in 2014 when these transformative changes in maternity care were in full swing in our hospital. We supported her to our best ability. She had a latent phase of labour at 4cm for 10 hours and finally had an active labour for only half an hour. She did not let anybody interfere with her birthing and finally delivered a 4.68 kg healthy baby with no tear and no shoulder dystocia.
Skin to skin contact and immediate breast feeding was initiated. While we were thrilled for her, we realized that supporting the Betty’s in their quest for a natural birthing experience is not enough. We also have to create more Betty’s by educating girls in the community, encouraging women to conceive at an earlier age, empowering them through antenatal education and involving the larger family to re-inculcate the innate confidence in birthing.
On the professional side, we need to encourage obstetricians to closely look at their practices and move towards a more evidence-based approach. This may require not only continuing education on recognizing the limits of normal variations in labour but also work on evolving practice structures where obstetricians move away from solo practice that puts them on call 24 x 7.
Lastly, India needs to develop midwifery as way of ensuring that women with uncomplicated pregnancies receive supportive care without medicalization of a natural and spiritual life event.
*Names have been changed to protect mothers’ identities.

Dr. Rinku Sengupta has been a practising Obstetrician-Gynaecologist since 1994 and has been at Sitaram Bhartia Institute of Science and Research since 2002. Her work at the Institute has majorly revolved around stabilizing and reducing the caesarean section rates and developing a holistic, evidence-based care model for expecting mothers. Her interests also include teaching and training medical and paramedical professionals in natural birth. Dr. Rinku specializes in high-risk pregnancies, and VBAC deliveries.
Come meet Dr. Rinku at the Human Rights in Childbirth Conference in Mumbai India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Widespread departure from evidence-based maternity care across Delhi
Sitaram Bhartia gives us a forthright look into the reality of maternity care in Delhi and their process of improving maternity care within their hospital. They are sponsoring the Human Rights in Childbirth Conference in India because they are committed to getting India back on track with evidence-based maternity practices. Read on and you are guaranteed to be shocked, and inspired.
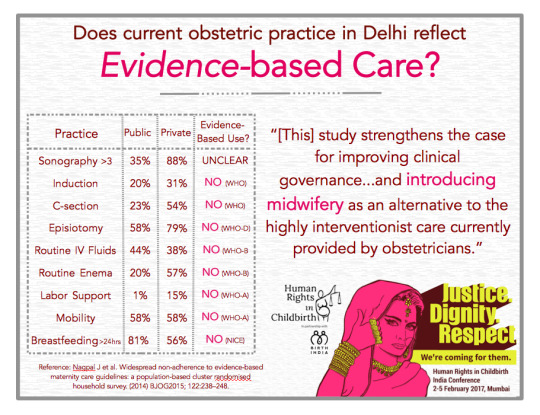
The honest introspection of maternity practices
“What is the quality of maternity care across Delhi?” asked Abhishek Bhartia, director of Sitaram Bhartia Institute of Science and Research.
This was 2005, but the question had its genesis three years ago in an initiative to deliver evidence-based maternity care.
This initiative had been prompted by a 79% caesarean rate in our nonprofit hospital.
When we looked closer, we found high use of enemas, shaving, cannulation, augmentation (drugs that start or increase labor contractions), episiotomy (surgical cut through woman’s perineum), and lithotomy position (woman lying on her back with feet up in stirrups to give birth).
Furthermore, babies were being routinely moved to the nursery post-delivery and rates of breastfeeding were low. And all this was happening in a reputed South Delhi hospital with leading consultants, many of whom were former professors at leading teaching hospitals.
Somehow, things didn’t add up and we decided to attempt a city-wide survey to understand the extent of the problem of over-intervention in maternity care.
We also wanted to understand how the maternity care differed between government and private facilities. Unlike previous surveys in India, we decided to focus not just on compliance with minimal care standards, but explored a wider adherence to evidence-based guidelines covering antenatal, intrapartum and postpartum care.
Findings from the Research
A grant from the Indian Council of Medical Research allowed us to conduct an extensive survey covering over 100,000 households from the low, middle and high socio-economic strata in Delhi.
Below are some of our findings:
We found that about a third of women from the lower socio-economic strata delivered at home, while >90% of women from middle and high socio-economic strata were delivered in institutions by obstetricians.
Minimal antenatal care guidelines - such as 3 antenatal visits, iron supplementation and tetanus vaccine – were met in >80% of women. High use of ultrasounds was widely prevalent in the private sector (mean 4.2).
The caesarean-section rate was higher in the private than public sector (54% vs 24%) and about 30% of women in the private sector had a planned caesarean.
Episiotomies were given to a majority of the women across the board and reached a high of 79% in private facilities. Only ~1% of women received labour support and pain relief in labour in public hospitals and rates were low (10-15%) even in private facilities.
Antiquated practices such as routine enemas, urinary catherisation and shaving of pubic hair were widely prevalent.
Only half of the women were allowed mobility during labour and consumed oral fluids.
The lithotomy rate was 70% in private hospitals.
The colostrum continued to be discarded (traditional Indian practice) in 8-12 % of hospital deliveries.
Breastfeeding was not initiated even by 24 hours of birth in ~20 % of mother delivered at public hospitals compared with 48% in private hospitals.
Picking ourselves up
Overall the study found widespread departure from evidence-based maternity care across government and private facilities – despite most care being provided by qualified obstetricians.
We believe that findings of this study strengthen the case for improving clinical governance of maternity care in all institutions and introducing midwifery as an alternative to the highly interventionist care currently provided by obstetricians.
There is a great opportunity for progressive clinicians and hospitals to lead the way towards de-medicalising childbirth and providing the woman-centered care that all mothers deserve. In our own unit, we have made substantial progress in reducing our caesarean rate (Sep-2016 YTD 19%, low-risk first-birth rate 14%), eliminating practices such as shaving and enemas, empowering families through childbirth education, and providing one-on-one support during labour.
These changes have taken close to 15 years – with long periods spent in “failure to progress.”
But our experience shows that with perseverance, organizational commitment and leadership from clinicians change is very much possible.
REFERENCE:
Nagpal J, Sachdeva A, Sengupta Dhar R, Bhargava VL, Bhartia A. Widespread non-adherence to evidence-based maternity care guidelines: a population-based cluster randomised household survey. BJOG2015; 122:238–248.
Sitaram Bhartia Institute of Science & Research is a leading, non-profit maternity hospital in New Delhi, India. The Institute works to empower women to take better, more informed childbirth decisions.
Learn about and support evidence-based care by attending the Human Rights in Childbirth Conference in Mumbai, India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Inspired by birth, Midwife Ibu Maya will probably inspire you.
Ibu Maya is a young activist midwife in her country who will be speaking at the upcoming Human Rights in Childbirth Conference. She is passionate for all women to choose their way to birth, and with whom, using evidence based research. Read her own experiences here, both as a mother, and as a midwife.
27 years ago I was born in a small town called Pemalang, Central Java. When I was in 4th grade I represented the school to participate in a small midwife activity where I was trained and accompanied a village midwife named Ibu Janatun. Since then I was determined to be a midwife in order to assist the women give birth.
Armed with knowledge as a young midwife participant, at the age of 11 years I accompanied my mother who gave birth to my youngest brother. I accompanied my mother to walk to the grocery shop and to buy rice when the latent phase of labour had started. I gave her food and drink whenever she asked, until finally I saw my youngest brother cry loudly when he was just born. My mother gave birth normally at that age, usually classified as “high risk”, aged 42 years old. That's the first time I accompanied a birth.

Indonesian Midwives Association; Ibu Maya second from right.
Labor culture in my village in that time was a midwife coming for homebirth. I saw my village midwife, Ibu Janatun assist breech deliveries, PROM (premature rupture of membranes) without infection, childbirth in multigravida, and also babies that were overdue. She was helping mothers and babies survive. There were rarely cases of cesarean delivery, cesarean delivery happened only with a proper and needed indication.
In 2007, I continued education to midwifery college and finished it in 2010. After finishing midwifery college in 2010, I started working in a private hospital and also became a member of the Indonesian Midwives Association (IBI). In 1 decade since I became a new midwife, the paradigm of midwifery and birthing women saw too many changes. In the Private Hospital where I work, from 10 birthing women, two of them gave birth vaginally and 8 were cesarean birth. Natural childbirth became a very rare event while caesarean birth be common. Many medical interventions "should not" happen and eventually the woman did not have a choice, birthing women were no longer a subject but became the object of midwives, doctors and hospitals.
In early 2012 I got married and moved away to the densely populated metropolitan city of Bogor regency, West Java. I automatically moved Membership Indonesian Midwives Association (IBI). In this city was the start of my start fighting for my rights as a midwife in obtaining a license for an Independent Midwife Practice. Soon a midwife practice license for independent practice came out and I was the youngest licensed midwife there.
Shortly after getting married I became pregnant. In the 24-week gestational week my doctor diagnosed placenta totallis placenta Previa with baby in transverse position. At 28 weeks gestation, the placenta shifted upward into the marginalis position, but the baby turned into a breech position. Breech position of the baby settled for up to 32 weeks so then the doctor-gynecologist planned cesarean delivery for my first child, if the baby remained breech until the next scheduled antenatal consultation. Then my husband and I did a lot of research on breech deliveries, there I found that cesarean delivery is riskier than breech deliveries. My husband went around looking for midwives and doctors to help breech deliveries, but they were not willing. Finally, near the end of pregnancy, I met a midwife who is willing to accompany my breech delivery. In the New Year's, 2013, I gave birth vaginally to my first daughter who was in a footling breech position.
From the experience of my first child in footling breech position, I got the idea to make an observational documentary about a mother who fights for her rights during pregnancy. In 2013 we conducted research on cesarean delivery. Based on data Riskesdes in 2012, the rate of cesarean deliveries in cities - big cities in Indonesia reached 64%, while the WHO recommends that the rate of cesarean delivery in a country should not be more than 5-15%. The high rate of cesarean is apparently caused by a cesarean delivery which is done, not because of medical indications. This is now commonly known as an “unnecessarean.” Once the first birth is a cesarean, doctors always recommend cesarean for the next delivery, Mom no longer has a choice of mode of delivery.

Screening of “All About my Pregnancy” at Sumbawa Technology University
In 2014 I accompanied Mrs. Susilawati’s pregnancy journey. It was her third pregnancy after Susilawati had two children by cesarean. The trauma to the previous delivery process was still being felt until this day. Coupled with the incidence of death of three close friends of Susilawati, after cesarean delivery, it made her determined to give birth vaginally even stronger. She took a stand in her pregnancy from the start taking prenatal classes, doula visits, keep the intake of nutrients, acupuncture, acupressure, yoga and exercise as well as finding doctors and hospitals that want to help VBA2C (Vaginal Birth After 2 Cesareans).
In our country, the applicable Standard Operating Procedure (SOP) in hospitals states that pregnant women with 2 times cesarean section must give birth to their third child by caesarean. VBA2C labor is considered highly risky because it can cause uterine rupture, can cause maternal and infant mortality. On the other hand, recent research published in the British Journal of Obstetrics & Gynecology (BJOG), a systematic review and meta-analysis of the medical research on vaginal birth after two cesareans (VBA2C) found that there is no statistically significant difference in key maternal and infant outcomes between VBA2C and repeat cesarean section (RCS). Susilawati was experiencing difficulties. Yet, the dozens of doctors whom she met one by one were not willing to help to give birth vaginally.
Towards the end of pregnancy, Susilawati asked me help her labor. I felt a dilemma. As a woman I feel the same instinct to give birth normally, my heart was moved to help Susilawati to birth. But as a midwife, I collided with the SOP (hospital guidelines) that Susilawati must have a cesarean. The day of delivery arrived, finally Susilawati successfully gave birth vaginally in water at home with a midwife. VBA2C, water birth, homebirth is illegal in Indonesia.

Ibu Susilawati, the mother documented in “All About my Pregnancy” in latent phase of labor at home.
Susilawati’s pregnancy struggle was summarized in an observational documentary film with the theme of human rights in childbirth entitled "All About My Pregnancy." The film invites women to empower themselves before and during pregnancy. Knowledge is a key and power, the more knowledge we have, the more opportunities to have a choice. The birthing mother will have a choice which they are entitled to.
Then I founded the "Rumah Sehat Bunda." Midwives team at Home Healthy Mother consisted of 3 young midwives, Myself (27 yo), midwife Vivi (24 yo) and midwife Firly (24 yo). In the Obstetrics clinic, we have a vision of natural birth and women being supported in holistic care. We have a joint mission to fight for what is the choice of mother in pregnancy and childbirth.

The Rumah Sehat Bunda Team: from right- Midwife Firly, Midwife Vivi, Midwife Ibu Maya and new Mom and Dad.
I also found a Thinker Moms Community, whose members are midwives, expectant mothers and mothers who want to empower and educate themselves about the latest evidence based birth. The goal is to support mothers to decide independently, to choose and be responsible for the selected health care during pregnancy and childbirth.

The Thinker Mom’s Community, founded by Ibu Maya
In Indonesia, the community and the profession of the midwife thought that the knowledge and skills of a senior midwife is true, enviable and does not need to be changed. Senior midwives often do not give an opportunity to younger midwives to develop updates in obstetrics based on evidence based. As a young midwife, facilitating more updated and scientific research, I struggled to practice midwifery using the latest evidence.
For that I felt called to join the international Human Rights in Childbirth to build networks in the international arena. As a mother as well as a midwife, I will represent Indonesia’s voice and women's rights in selecting the mode of childbirth for the world to hear and understand what we feel, for the world to respect our choice. Only we who know the consideration of everything, we know the extent of our strength and we who live it, not doctors or others.
- Ibu Eka Maya Febriana, Str. Keb (Midwife, Producer, CBE)
(Founder Rumah Sehat Bunda, Founder Community Thinker Moms)

Come meet Ibu Maya by attending the Human Rights in Childbirth Conference in Mumbai, India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
An interview with Dr. Vijaya Krishnan, Certified Professional Midwife, on her journey, her Birth Center, & her passion for Human Rights in childbirth.
If you read our article about the Right to Privacy, you should be knowing the function of an autonomous midwife (check it out if you haven’t!). While adequately trained midwives are wholly lacking in India, there are some independent midwives, mostly trained abroad, who provide high-quality midwifery care to pregnant women. One of those midwives is Vijaya Krishnan, CPM, who runs The Sanctum, Natural Birth Center in Hyderabad. In a free-flowing interview with Zoe Quinn, she talks about the current status of maternity care in India, her journey, her Birth Center, and her passion for Human Rights in Childbirth. She will also be speaking at the HRiC India Conference, so you can meet her there as well.
Q: Can you tell me a little bit about your journey?
I started out my professional life years ago as a Physical Therapist, went on to get my Doctorate, and practiced in the US, where I lived with my husband. Then, my first pregnancy happened.
I was completely healthy, working until the very end of my pregnancy. But then, as sometimes life does, things went a bit awry. My first born came into this world in a hurry, by Emergency Cesarean Section, at a little less than 36 weeks. It was on a Sunday afternoon at 4:30 pm when I could feel the knife go through me, before the anesthesia took effect. It was scary as I could hear his heart tones dropping into the 40s. But we both made it, albeit with some struggles.
By the time I got around to having my second son, researching alternatives and having a good care-provider meant that I had the VBAC (Vaginal Birth After Cesarean) of my dreams. At the time, VBAC restrictions and bans hadn’t taken hold of hospitals in the US. I never had a second thought about having a VBAC and I never felt like there was a barrier preventing me from achieving one! My mind was free, my doctor was supportive.
I read up about Lamaze practices and gathered information the old-fashioned way because, back then, there was not much information available online. My VBAC Moment - I can never forget it. It was the most empowering moment of my life. I can clearly remember the expression of my newborn’s face, even today!
That moment also pulled me closer to becoming a midwife. It just seemed like a natural process. I started by informally talking to pregnant women, and then naturally accompanying them while they were in labor.
In 2003, we moved back to India. The first few years were spent settling down afresh. But when I started to venture back into the field of maternity care I was in for a shock. While in the midst of a research project I got to see the care that pregnant women received, and soon became acquainted with the challenges in present day maternity care in India. That was the beginning of my journey to supporting women give birth.
I became a Lamaze Certified Childbirth Educator, a doula and then a midwife. I found one thing singularly lacking, and that was good information given to the pregnant woman and her family in a way that could support good decision making for themselves. Procedures and C-sections seemed to be everywhere, and birth, well, nothing seemed natural about it! Lamaze childbirth education was virtually unheard of, and so the first step for me was to start Lamaze classes.
However, the moms from the classes would go back into the same “system” and land up with the same interventions and C-sections during birth. The women in these big hospitals were totally unacknowledged in terms of their rights. There was such a fear of pregnancy and this hierarchical dynamic between the women and doctors. No one was telling the women that most of the tests and scans were optional. Nor were they being told that there were pros and cons to every choice or decision.
Women became totally passive recipients of care.
Here is the current scenario in the private sector -
The mother is told (and hospital hoardings exhort) to go to a doctor the moment she conceives. There she waits in a line for sometimes up to 4 or 5 hours to get “seen” by the doctor, who really does not “see” her at all. She is seen as a pregnant belly which needs to be scanned! But, that early at four or five weeks there may be very little to “see” even on the scan, and if the gestational age by LMP and what is seen on the scan does not match, the mother is told to take medications to “strengthen” her pregnancy. These medications are oral or vaginal progesterone, B-HcG injections and then to get a repeat scan in a week to 10 days. From here on, the mother has now outsourced her body to her doctor, and thinks that her pregnancy can only be carried forward with medications, rest and the doctor’s instructions. She is so far removed from connecting with her body and her baby that the same mind-set then carries on into the birth of her baby, with the doctor directing the whole process. Even when women in India say that they had “normal delivery” it had very often involved induction/augmentation with Syntocinon drip (most times without informed consent). She is told "Amma (mummy) I am going to run ‘glucose,’” and then the whole cascade of interventions including Syntocinon, epidural, episiotomy, fundal pressure (Kristeller manoever), and sometimes instrumental delivery may occur.
Routine practice means there is no ‘care’ in maternity care, it’s just an assembly line. The system favors the medical model of care and does not allow any one-on-one personalization. Women get 2-3 minutes with their doctor and often the mother is too scared to even ask any questions. She may not even get any privacy. And then, when it comes to labor and birth, she has no real information.
When I started teaching Lamaze classes in Hyderabad, I was hoping I could get women the information and preparation they needed to have a good birth experience. Often the women were taken aback by my classes, they expected exercises not information! But despite my best efforts, 90% of my clients, in those first years, ended up with c-sections. They would call me up saying, ‘We did XYZ! but the doctor didn’t allow us to do ABC!’
So I started attending births.
I hoped that by attending births it would make a difference, but the gains were small. The women never had the locus of control, so I was often fighting a losing battle. One birth was so traumatizing to witness, that I was emotionally and physically drained, and I left all things birth-related, for months.
This particular mother had an absolutely amazing pregnancy and the labor was going really well but she unnecessarily ended up getting a large episiotomy which extended, and did not heal. The mom was in pain for the better part of 2 months, and it took 6 months for the woman to heal completely. The grandmother, after it was all over asked me, ‘How is this better than a c-section?’ I had no answer to that, and decided I would not be a doula anymore.
My husband, seeing my anguish, asked me if we would like to have a birth center of our own. God bless his heart. So we landed up talking and planning ahead for months with our current back-up OB, found a space inside her hospital, converted it to a Natural Birth Center and started offering midwifery care.

[Lamaze classes in the Sanctum]
Q: How did your Birth Center come into being?
In 2009, we started providing midwifery services in our first Birth Center, in a small space which we leased in one corner of an existing hospital. Initially we provided one-to-one autonomous midwifery care to low-risk women and consulted with our back-up OB (obstetrician) if any conditions arose which were outside of the range of normal.
But there were definitely struggles. For one, my back-up OB in the hospital, while very supportive and respectful of my practice, still had a very high c-section rate. This translated into more c-sections than was probably necessary for some of our clients in the first 1.5 years of practice. Also, when my usual back-up OB was unavailable I had problems getting back-up support that I needed from someone who understood the midwife model of care. Again, this translated into more medical management than was probably needed.
I found that sometimes doctors in the hospital were so ignorant of what we did that they didn’t even use my name. I would hear, ‘The lady from Healthy Mother is on the phone!’”
Also, operating a natural birth center from inside a hospital sent some mixed messages to our clients. Natural birth and hospitals in India don’t normally equate. This was a big first in early 2009!! The opening of a midwife-owned and run birth center where professional midwives could provide independent, autonomous midwifery care, where low-risk women could access normal birth and have access to OB support and infrastructure inside the same premises. All this provided in a timely and safe way in the case of complex needs or complications. As time went along, both the doctors and the families who came to us for care understood the importance of the Collaborative Care that we were providing.

[Vijaya (orange) with babies born in the Sanctum]
Q: Collaborative Care: Can you explain a bit more about this model of care?
Recently my husband and I opened our free-standing Birth Center, The Sanctum, Natural Birth Center. It is not attached to any hospital, but has all the emergency infrastructure like a fully equipped operating theater, a small level 1 NICU, a Lab and a pharmacy built into it. My husband, Mr. Krishnan Sakotai, who is the Co-founder and Partner at Healthy Mother, also looks after all strategic planning and the innumerable details that are needed to run a Birth Center with optimal qualitative and quantitative outcomes. After 8 years of having provided collaborative back-up partnership, our main Obstetrician, Dr. Jayanthi Reddy, has also come on board as a full time partner at our Birth Center.
The Sanctum, Natural Birth Center, can be regarded as a gold standard of collaborative midwifery care.
What makes the Sanctum different from the average free-standing birth centers one might see in other developed countries is that though midwives run birth centers, they are restricted to taking on low-risk clients because they do not have the skills, facilities or backup required to manage clients with complex needs or complications. Obstetricians in hospitals do. At our Birth Center we can take on and assist clients with more complex needs. This includes women with twins, Gestational Diabetes, Gestational Hypertension, breech babies, etc. because we have full support of backup Obstetricians, Physicians, and Pediatricians if the help is required, all available on site.
This collaborative model of care has led to some pretty amazing, safely assisted, and satisfying natural births. However, if there are any red flags during pregnancy or labor, we have a number of backup OBs nearby whom we can consult with or have come and perform a c-section if necessary, in The Sanctum itself. By now, we have won the credibility of the local medical profession and backup care is easy to come by.
{You can read some birth stories on the Sanctum’s Facebook page to see what she means}
Our collaborative model of care works. We have an amazing team of Nurses (who we have cross-trained to provide excellent labor support), Midwives who have education, training and experience in providing excellent maternity care with the Midwifery Model of care, Ayammas who provide MotherBaby Care from the heart, as much as with their hands, Physiotherapist, Prenatal Yoga Instructor, and Lamaze Certified Childbirth Educators who teach with unparalleled passion and energy, to help women have a safe and healthy childbirth experience. Of course, our team of back-up OB/Gyns , On Call Anesthetists, Physician, and Pediatrician excel in their respective roles, to provide well-rounded comprehensive care for both the Mother and her Baby, as per their individual needs.
Our statistics speaks for themselves. Of the 613 births so far (15 January 2017), we have an 8% C-section rate, 4 vacuum births, and only one forceps birth. These statistics span over 8 years. We currently have a 98% VBAC (vaginal birth after a previous C-Section) success rate, and have successfully helped 6 women have a successful VBA2C (a vaginal birth after 2 previous C-sections) - this in a country where VBACs are almost non-existent.
All of this of course happens because mothers and their families want access to good evidence-based, respectful, informed, transparent maternity care.
I am really thankful for excellent back-up obstetrical care though, not that we often need it. It is funny when I call up one of our anesthetists on call and he says “It’s good we haven’t met [for so long]!”

[Vijaya to Mother: “You did so well mamma, you did perfect.”]
Q: What else contributes to the success of the Midwifery and Collaborative Model of Care that is provided at your Birth Center?
It is the mother who has to birth the baby after all. We expect mothers to take equal responsibility during pregnancy and birth.
I expect my clients to become responsible partners in care.
I expect them to take Lamaze classes, and encourage their partners and even grandmothers to attend, so that the whole family can now encourage the mother to give birth without fear.
I expect the women to put in some effort to maintain their health.
I want them to be inspired to have a better birth for themselves. Whoever comes here should give it 100% so that [the mother] gets to the point where she can go into labor confidently...She must walk out of the birth center stronger than when she came in.
I know it makes a difference when women take charge of their pregnancy, rather than hand it off to an “expert.” Most women come to our [Lamaze] classes with some fear. But if parents have skipped the classes - those births tend to not go as well. Hence, [in our classes] we stress the significance of labor support, the importance of managing early labor at home, how to remain calm, how to use the many tools available to manage the challenges of labor.
Also, our dedication to informed consent and informed refusal empowers mothers to make good choices for herself. I am an advocate for her and her baby, but I do not make choices for her. I am here to empower her with good knowledge and skills and help her feel confident so that she can make decisions for herself. This is the hallmark of respectful maternity care: the woman is treated like an individual and her personal circumstance, preferences and choices are integrated into the care.
Another aspect of the success of this model of care is attributed to integrating the positive aspects of a birth center with the positive aspects of centering the care on the woman throughout her lifetime, knowing that women bond with their midwives and feel comfortable receiving care from them. We are now able to provide everything from preconception counseling, to care during pregnancy, labor and birth, pediatric services on the premises, postpartum care, lactation counseling and support, contraception/family planning services, and well-woman check-ups. We also run a Healthy Mother Breastfeeding Support Network.
This holistically comes together so beautifully to support the woman in all aspects of her reproductive health and in her childbearing years. Similarly, taking care of the wellness aspect of women’s care is so important. Hence we also have a Pediatric clinic, Prenatal yoga, Lamaze childbirth education, Postnatal fitness programs, Pre- and Post-natal massage services, Lactation clinic, Gynecological Services (with our back-up OBs), as well as Women’s Physiotherapy services. We have therefore developed a model where the entire family can access care that is Midwife-led and driven, but which has integrated complementary and medical care, as well as Wellness services that are focused on preventative care.
Ultimately this model thrives on excellent continuity of care which differentiates “The Sanctum, Natural Birth Center” from the standard care in India.
Q: Do you see Midwifery Care becoming mainstream in India?
I got my midwifery certification from the US because presently India doesn’t have the equivalent training. Here, the General Nurse Midwives (GNM) and the Auxiliary Nurse Midwives (ANM) in India are not given enough training to provide true, autonomous and professional midwifery care.
We have a very long way to go. The word ‘midwife’ is finally coming to the lexicon of the common man, so I hope it spreads faster. But, since there aren’t enough qualified midwives, trained in scientific, evidence-based midwifery, we need autonomous midwifery training programs. In training autonomous midwives who provide independent care to women wherever they are, in urban, semi-rural or rural areas, we can actually look at reducing maternal and infant mortality and morbidity. This is the need of the hour. Another need of the hour, is the recognition of collaborations between midwives and obstetricians. Without this collaborative care, optimal maternity care will always be missing.
We also need to capitalize on the care providers we already have. All the necessary midwifery training and education will not happen in one go. So, we can’t afford to lose anyone. The present GNMs and ANMs need some extra skills, which can be taught. Plus, there needs to be a separate Program to educate, train, certify and license independent midwives. The Dais who are India’s Indigenous Birth Attendants have so much experience and they have provided decades of care. We don’t want to lose them! But we can enhance their skills, introduce them to basic aspects of clean/sterile care of the woman and her newborn, teach her skills to revive newborns in the golden minute, give her some training with respect to controlling postpartum hemorrhage, etc. She is an asset in her community. We must not lose the cultural aspects and needs of a woman giving birth in her own community.
Two issues are concurrently evident: One, there is a need to improve the skills and training of midwives, and introduction of Professional Midwifery with the Midwives Model of Care that is of a worldwide Gold Standard. Secondly, there is a need to document the safety of midwifery-led care in a state and country where this has never been done. This will be the 2 major things that will improve the delivery of maternity care in India. I am optimistic that if public, private and Government organizations take this as a priority, it can be done!

[Midwifery care during labor.]
Q: The HRiC Conference: What are your hopes for this conference?
I see the conference as a wonderful platform to raise the consciousness of people on a level that has never been done before in India. Hopefully, it will reach out to more people and we will really start looking at what are human rights in childbirth and what are the needs of women and their babies? Looking at birth through the lens of human rights is so critical because birthing women are so vulnerable.
My hope is that the HRiC Conference brings together practitioners, parents, concerned citizens and authorities from the Birth community worldwide to highlight access to good evidence-based birthing practices, and respectful maternity care as major human rights issues so that it can translate into better MotherBaby care, both here in India and worldwide. The conference is a part of a crescendo building to raise the agenda and to get the Indian government involved and notice us. I will be at the conference representing the small, but growing presence of professional, autonomous midwives. I am also expecting to learn so much from all the amazing speakers at the Conference!
I will also be presenting on a subject that I am passionate about - the fact that childbirth is not just about the mother and baby surviving it, it is also about how the mother experiences it. It is also about how the newborn in its most vulnerable state experiences the first minute in it’s world. It is about making a woman confident about herself and her body. This can leave a lasting impact for a lifetime, either positive or negative. I will be presenting about how women view their childbirth experiences, and what we as care-providers can learn from it.


Dr. Vijaya Krishnan practices at The Sanctum, Natural Birth Center in Hyderabad. She is a registered Certified Professional Midwife (CPM) from North American Registry of Midwives (NARM), and is an Official Certified Lamaze Childbirth Educator (LCCE). She also has a doctorate in Physical Therapy. She will be speaking at the upcoming Human Rights in Childbirth Conference this February in Mumbai.
You can learn more about Vijaya, midwifery, the collaborative model of care and the births that occur in The Sactum, Natural Birth Center both on Facebook and YouTube. The website is presently under construction.
Zoe Quinn is an American living outside of Pune, India for over 4 years. She s a volunteer with Birth India and has been working on producing blogs for the upcoming Human Rights in Childbirth Conference. After a profound and amazing birth experience with the care of midwives, she is pursuing becoming an autonomous midwife herself.
Learn more from Vijaya Krishnan by attending the Human Rights in Childbirth Conference in Mumbai, India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Lamaze is a wealth of information.
Lamaze International is a not-for-profit organization composed of parents, childbirth educators, healthcare practitioners and other health professionals whose mission is to advance safe and healthy pregnancy, birth and early parenting through evidence-based education and advocacy. Lamaze is sponsoring the upcoming Human Rights in Childbirth Conference in Mumbai.
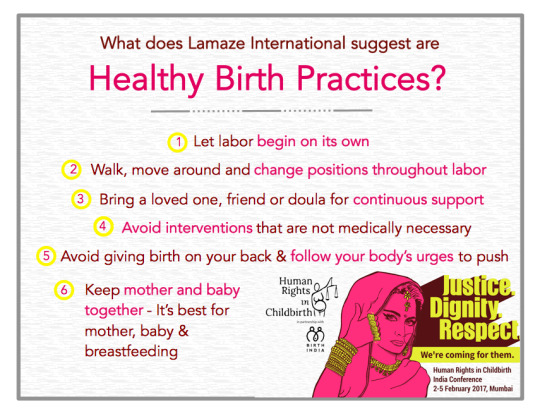
Knowing that access to credible information and research is key to a healthy pregnancy, childbirth and a good start to parenting, Lamaze works to educate women and provide support so they are equipped to effectively partner with their care provider, navigate their options in care and push for the safest, healthiest birth possible.
Lamaze education and practices are based on the best and most current medical evidence available. The Lamaze Six Healthy Birth Practices are tried and true ways to teach parents how to have a safe and healthy birth. Our vision is “knowledgeable parents making informed decisions.”
The Lamaze Healthy Birth Practices help simplify the birth process with a natural approach that helps alleviate fears and manage pain. Regardless of the baby’s size, labor’s length and complexity, or the mother's confidence level, these care practices will help keep labor and birth as safe and healthy as possible.
Healthy Birth Practice 1: Let labor begin on its own
Healthy Birth Practice 2: Walk, move around and change positions throughout labor
Healthy Birth Practice 3: Bring a loved one, friend or doula for continuous support
Healthy Birth Practice 4: Avoid interventions that are not medically necessary
Healthy Birth Practice 5: Avoid giving birth on your back and follow your body's urges to push
Healthy Birth Practice 6: Keep mother and baby together - It's best for mother, baby and breastfeeding
Lamaze Certified Childbirth Educator (LCCE) certification is internationally respected and the only childbirth educator program that has passed rigorous standards set by the National Commission for Certifying Agencies (NCCA). Lamaze childbirth education professional training and continuing education programs meet the highest professional standards as an American Nurses Credentialing Center (ANCC) Accredited Provider.
The LCCE Educator promotes, supports and protects every woman’s right to give birth, to be confident in her own ability, to be free to find comfort in a wide variety of ways, and to be supported by her family and all members of the health care team.
Lamaze Education focuses on seven competencies designed to give families the most empowering birth experience possible.
Competency 1: Promotes the childbearing experience as a normal, natural, and healthy process which profoundly affects women and their families.
Competency 2: Assists women and their families to discover and to use strategies to facilitate normal, natural, and healthy pregnancy, birth, breastfeeding, and early parenting.
Competency 3: Helps women and their families to understand how complications and interventions influence the normal course of pregnancy, birth, breastfeeding and early postpartum.
Competency 4: Provides information and support that encourages attachment between babies and their families.
Competency 5: Assists women and their families to make informed decisions for childbearing.
Competency 6: Acts as an advocate to promote, support, and protect natural, safe and healthy birth.
Competency 7: Designs, teaches, and evaluates a course in Lamaze preparation that increases a woman’s confidence and ability to give birth.
Lamaze International seeks to empower families to have informed birth experiences, and to celebrate the beautiful process that is birth.
Lamaze International was established in 1960. Learning from years of research and observing women’s experience of normal, natural birth has provided evidence that gradually but dramatically changed Lamaze from being a method for giving birth to an evidence-based approach that provides the foundation and direction for women as they prepare to give birth and become mothers.
The 2001 position paper, Lamaze for the 21st Century, outlined the evidence-based rationale for the evolution of Lamaze preparation for birth with the Lamaze Philosophy of Birth as the centerpiece. Today the Lamaze Fundamentals for Pregnancy, Birth and Parenting capture the core tenets and continuum of Lamaze education. The Lamaze Six Healthy Birth Practices, adapted from the World Health Organization, translate evidence-based practices into concrete, understandable concepts that form the basis of Lamaze education today.

Connect with others, develop professional opportunities, and get high quality resources to support expectant families to have a natural, safe, and healthy birth with Lamaze International. As a part of their commitment to promoting the improvement of birth, they are sponsoring the upcoming Human Rights in Childbirth Conference in Mumbai this February.
Lamaze International is doing their part, you can do yours at the Human Rights in Childbirth Conference in Mumbai, India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Dr. Evita Fernandez: “India needs to wake up.”
Dr. Evita Fernandez, sponsor and speaker of the Human Rights in Childbirth conference in Mumbai this February, is a part the growing global movement to bring human rights back into Birth. Read her message on why India’s maternity care needs a wake-up call.
Over the past seven years, my views on childbirth practices have taken a 180 degree turn. Today, I am convinced we obstetricians in India need to UNLEARN a lot of what we have been taught, and we need to LISTEN more to the women we are privileged to serve.
I realized, to my horror and shame, that we have indeed been violating a woman’s human right with regard to childbirth. Every time we fail to share/offer honest evidence based information, fail to give her the freedom to make a choice, prevent her from having a birth companion, refuse to let her birth in the position she finds most comfortable, we are violating her rights.
With a birth rate of 22 million a year, India has an overwhelming volume of laboring mothers, in overcrowded, poorly staffed hospitals.
With institutional deliveries being made mandatory, the majority of our women are subjected to “obstetric violence,” which translates into physical and verbal abuse by healthcare workers, who are ignorant and insensitive to woman-centered care. I admit to being that myself (ignorant and insensitive) particularly in my early years of training and as a young obstetrician. Compounding all of this is the utter lack of privacy, loss of dignity and respect. Our women, especially the voiceless poor, birth in appalling environments.
Human rights in childbirth has today become a global movement which is gaining strength, and rightly so. Women, doctors, lawyers, midwives and activists are coming together to offer solutions to help protect the basic human rights of birthing women.
We in India need to wake up.
All levels of health care workers involved in maternity services, need to wake up. We need to reflect, rethink, and change our attitude and understanding of childbirth practices.
Rebecca Schiller, in her well researched and well written book “Why Human Rights in Childbirth Matter” (Pinter & Martin Why It Matters 9), says:
“Looking at how a society approaches childbirth, how it constructs a system around it, the rituals, the rites and the way it treats the key protagonist - the birthing woman - is akin to taking the temperature of that society. Nothing says more about the communities we live in than how they treat their most vulnerable at this extraordinary time.”
India is hosting the International Human Rights in Childbirth Conference in February (2 - 5th) in Mumbai. I hope, it will help bring about the much needed change in attitude, practices, and more importantly, help build a network of support for women birthing in our country.


Evita Fernandez FRCOG, is sponsoring and will be speaking at the upcoming Human Rights in Childbirth Conference in Mumbai. She is an obstetrician who a decade ago began to soul-search on the medicalisation of childbirth. She launched an in-house Professional Midwifery Education and Training Programme in August 2011, supported by British midwives. She is a strong advocate of professional midwifery and natural birth.
Come meet Dr. Evita Fernandez and make birth better by attending the Human Rights in Childbirth Conference in Mumbai, India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes
Text
Soul searching obstetrician shares her thoughts.
This week we introduce Dr Evita Fernandez, from Fernandez hospital in Hyderabad. First we'll read her response to the recently published article "Midwives back: Women opt for intimate home settings to give birth.” She is both sponsoring and speaking at the Human Rights in Childbirth Conference in Mumbai this February. Watch this space for more on Human rights in Childbirth from Dr Evita.
In response to this article I agree that women should be given the opportunity to choose and have control in their birth journeys. There are several studies supporting continuity of care by midwives, which result in better outcomes for both mother and her newborn.
While home births offer women the much-wanted privacy, intimacy and comfort of personalized care, I strongly support the collaborative hospital model (especially for India) where midwives and obstetricians work together as a team – respecting each other’s roles. C-section if required can be performed without wasting time driving the laboring mother through narrow roads and horrendous traffic.
I am convinced of the vital role professional midwives play in a woman’s journey through pregnancy, labour, birthing of her baby and in the care of her newborn. It is time India promotes and supports Professional Midwifery.
All pregnant women who do not have medical/obstetric complications (otherwise termed as low risk) should be offered midwifery care. The midwife is trained for normality and works within a strict safety framework of rules. Stand alone birthing units in the UK is a good example where clear guidelines and defined protocols exist for midwifery led units. It is important that we in India focus on the quality of training to help produce a cadre of competent and confident midwives. It is equally important to define her role and responsibilities. Most importantly, is the attitude of the obstetric community – to accept, understand, respect and take delight in working with midwives as professional colleagues.
My own epiphany happened only a few years ago. Today, as an enlightened obstetrician, I champion the cause of Professional Midwifery.
I am convinced that we obstetricians need to step back and stop interfering. We have medicalized and dehumanized birth. Our training focuses on making pregnancy a journey of complications and emergencies. Our own fears are often transferred to the woman. Most of us have a very poor understanding of “natural” birth and unfortunately an even poorer understanding of a woman’s needs during her labour and birth of her baby. We obstetricians need to get involved only when there is a medical or an obstetric complication, which demands our expertise.
At Fernandez Hospital we launched a two year in-house Professional Midwifery Education and Training Programme in August 2011. More than 5000 mothers have been supported through their labours and have enjoyed our professional midwives assisting them with their births. This journey has changed our own understanding of birthing issues and woman centered care. Our team of 40 ObsGyn doctors has had to unlearn a lot while simultaneously opening our minds to new thinking. It has been an enriching learning experience. PROMISE (Professional Midwifery Services) is the campaign we launched – out of conviction and belief that professional midwives are urgently needed. The campaign has four objectives.
To make pregnancy safe
Humanize birthing
Train a workforce
Promote midwifery by raising awareness among women and obstetricians
In India, where role models for professional midwifery exist, it is even more important that we encourage professional midwives (ensuring they are certified and have impeccable credentials) from countries that produce them i.e. UK, Australia, Sweden, Netherlands (to mention a few) to register with the Indian Nursing Council. This will give them the license and medico legal protection to offer their services without fear. Besides, they could also partner with local hospitals/state Governments in teaching and training a similar workforce for our country. The Indian Government and the Indian Nursing Council should open its doors to such well trained and competent professionals from other countries.
So while I STRONGLY support woman centered care, work towards reducing our interventions, help train a professional midwifery workforce, I do not (presently) support home births especially in a climate where there is no medico-legal protection for the professional midwife and with the Indian Government mandating institutional births.
I reiterate the fact that Professional Midwifery is the most urgent need of the hour. ALL laboring women MUST be offered midwifery support and care.


Evita Fernandez FRCOG, is sponsoring and will be speaking at the upcoming Human Rights in Childbirth Conference in Mumbai, which is also being sponsored by the Fernandez Hospital. She is an obstetrician who a decade ago began to soul-search on the medicalisation of childbirth. She launched an in-house Professional Midwifery Education and Training Programme in August 2011, supported by British midwives. She is a strong advocate of professional midwifery and natural birth.
Come meet Dr. Evita Fernandez and make birth better by attending the Human Rights in Childbirth Conference in Mumbai, India.
Sign this petition to make it mandatory that Indian hospitals declare their c-section rates!
Check out Human Rights in Childbirth on Facebook.
Ask questions, find support and information at Birth India’s Facebook Support Group.
0 notes