#and i’ve described my symptoms and everyone thinks i have asthma but i can’t see a doctor until the 10th
Explore tagged Tumblr posts
Note
Have you caught covid ever, Pi? Are you nervous about it?
[preface that this is a long winded talk of medical problems - ignore this if that sorta stuff is upsetting to you]
Ok, so this is going to be a longer response than you probably are interested in, so the short version is that I think I got infected with Covid-19 early last year, but due to my inability to get tested until way later, I’ve been told that it’s unlikely I’ll know for certain if I was until there’s blood tests to detect trace amounts of antibodies readily available.
=====
So the long version is that I was having some bizarre breathing problems in February/March (I can’t remember the exact time) last year, and I made an appointment to get tested. When I went to get tested, I was told because I hadn’t been overseas in the past 2 weeks and I couldn’t name a direct link to a confirmed case, then I couldn’t have Covid and therefore couldn’t get tested.
This was utter bullshit because this was around the same time that Tom Hanks was vacationing here and hospitalised at the local-ish university hospital. There was Covid in the community, unless they wanted me to believe Tom and his wife didn’t visit the beach or the shops, or anywhere with people. And aside from that - how does the first person get tested for everyone to connect to later? Funny how it looks like nobody is sick when you don’t let them be tested.
Regardless, I’m not a doctor, so I wanted to believe this guy. I told him I was having breathing issues, random fever spikes, nausea from being hyper aware of my own breathing, and a weird inability to think clearly. I described my breathing problem as “like asthma, but different and in the bottom of my chest instead of the top” and mentioned that along with the bottom half of my lungs feeling constricted, it felt like any air that I breathed deep into my lungs wasn’t doing anything. I only felt like I wasn’t out of breath if I was breathing faster and at the top of my chest – this is not how I normally breathe and it was a conscious effort to change that.
But I apparently didn’t have a low blood oxygen level at the time, and it didn’t sound like my lungs were obstructed. Which I did tell him that I didn’t currently feel out of breath because I had changed my breathing pattern to not feel that way – but that was what was making me feel sick.
He told me what I was experiencing was a complication with asthma and allergies… conditions I’ve had for a long time and know what they feel like. This wasn’t that. It didn’t feel like that. But again, not a doctor, if he wants to prescribe me with more steroids and a red inhaler, then I was open to trying it and seeing if it helped.
Then as I was leaving, he gave me this weird look and told me to continue staying isolated until my symptoms were gone.
But like… in case someone catches my allergies? Or asthma? This didn’t make sense to me. That made it sound like he thought I was infected. Which I think may have been true in retrospect, and that maybe there was some regulation that meant he couldn’t test me without confirmation of a transmission point.
In any case, I got my medication and inhaler. I hadn’t ever used the red inhalers since my asthma is very mild and strictly allergic asthma that I can normally get through without a complete airway closure. And that red inhaler hurt. A lot. It was awful, it made it so much more painful to breathe. And honestly, I don’t feel like it fixed anything.
Still I persisted with the medication. And I got worse.
I couldn’t lie on my back, at all. I would wake up in the night because I had rolled onto my back and lost feeling in my lips and fingers. For some reason I was having difficulty walking properly because my knees wouldn’t “lock”. I couldn’t read because I couldn’t remember enough words in order to understand the context. I had one really weird day where everything tasted wrong. I never again want to taste a roast chicken that tastes like sour lollies.
And the thing is, we were told to not go to the hospital unless it was urgent, and I never had a symptom that I couldn’t at least manage to a degree that made me not feel like I was in danger. I would lean severely forward while sitting and I could breathe better. I would take breaks every half hour or so to lie on my stomach and breathe. I slept a lot and spent a lot of time lying down or sitting because walking was exhausting. Also had a rather long stint where I would fall asleep randomly during the day while sitting up.
And the weird thing was that as the symptoms slowly dissipated over like 3 months, I had roughly 2 weeks where I felt normal again. I thought it was over, and that maybe I’d feel weak for a while, but it was over.
Then it was like getting hit with a second wave. Breathing was weird, but not the same degree, I could not think at all, still couldn’t read properly, I was sooo tired, and now I also was having random heart palpitations and sudden blood pressure fluctuations (I started checking my own blood pressure because I could physically feel something wrong and yeah, I was dropping into low and then going higher than normal on other occasions).
So like…. It was weird.
I went to the doctor and was told I had “post-viral fatigue” … meaning those allergies and asthma, that was a virus. Funny...
And I’m not the only one in my family who got sick. I got sick after trying to take care of my Ma who got sick. She actually managed to push harder on tests because we had all the exact same symptoms (but with me being 2 weeks behind) and she was diagnosed with chronic fatigue syndrome from this – and whether that lasts forever or will dissipates is unknown in this case.
So yeah….
Does that sound like Covid to you?
Because I still don’t feel like myself. Most of the bigger symptoms are gone, but I have so little energy and had mild muscular atrophy from being sick for so long. And it really feels like the more I try to fix my muscular weakness, the more tired I get. More strength, but less stamina. And sometimes I just can’t think at all, it’s like every single thought just leaves my brain. It sucks. I am living in hope that if I keep active that maybe I can push through it…. But like, there’s good days and bad days.
The last few days have been bad days. For a few reasons, but extreme fatigue is one of them.
I do seriously hope that what has happened to me isn’t common with people who do get infected – but it is equally frustrating trying to explain these things to people who don’t seem to understand why I’m so tired. Because there is a lot of focus on how to help people in the peak symptoms (which is a good thing), but that focus is gone once you’re out of the woods (bad thing). I just want to know if what I’m going through will resolve eventually.
And to answer the second part of your question… I’m not nervous about getting Covid anymore - I’m pretty sure I had it and I am very careful around people now. But I am nervous that the lingering effects won’t go away.
5 notes
·
View notes
Text
Can’t Control Chaos
Sometimes, when life has thrown SO MUCH at you, when you feel battered and broken... sometimes all that is left are hope, love, and determination... or at least that is all I have left.
I don’t want to start the year off on a “bad note,” but this holiday season has been cruel... there’s a C word for you... Yes, of course there were good moments and I have so much to be thankful for... but the season has been cruel none the less.
I honestly have been avoiding really processing what is happening... denial of course... fear of jinxing it, hope, luck, a miracle... whatever you’d like to call it.
I think I also have just been tired... too tired to really answer when someone asks, “How are you?” Because really? I’m not so okay... I haven’t been for a long time...
***So some background***
In early 2020, my godmother, Josie (Mama Jo), had started complaining of groin pain. I advised her to consult her doctor to get it checked out. Based on what she told me and my previous knowledge in women’s health, I thought it might be an ovarian cyst. These are quite common and can cause discomfort similar to what she described. Her doctor’s first diagnosis was possible muscle strain... prescribed her some medication, rest, and sent her home...
The pain persisted and worsened over the coming weeks, so I told her to advocate for herself and have her doctor investigate further... The issues with the American healthcare system.... But lets not get into that right now...
By this time, March 2020, the COVID pandemic was hitting California and we were forced into shelter in place.
Her doctor finally ordered some tests and found an extremely large mass, about 20cm in diameter... She was immediately scheduled for surgery. You can kind of see where this is going... In surgery they removed the mass with some difficulty and we were informed...
... the big C... not COVID... Cancer...
No one could be with her in the hospital after her surgery, we couldn’t visit when she had to stay extra days to recover... but we could speak to her and see her posting on facebook. She was doing okay and surgery was “successful.”
Ovarian cancer is in the top 5 cancer deaths among women and accounts for more deaths than any other female reproductive cancer... Now the reason for this is usually because there are little to no symptoms and when it is diagnosed, it is usually a late stage... In a way, we were blessed Mama Jo was experiencing pain. Her cancer was discovered at stage IIA, meaning she had some spread within her reproductive system, but none to neighboring abdominal organs or lymph nodes... good?
So the next step was chemo. Another C... interesting...


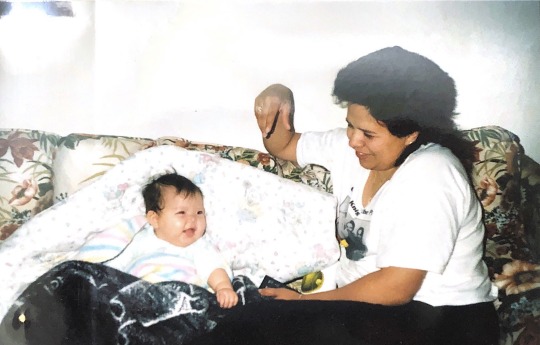
First infusion & cutting Mama Jo’s hair.
She was scheduled for a total of 6 rounds of chemo. Each round consisted of 1 appointment every Friday, for 3 weeks. 1 week of 2 drug infusions, and 2 weeks of a single. In total, 18 weeks. She handled it like a champ. Luckily she didn’t experience the extreme and awful symptoms, until her last round...
She started to feel the effects more and more as the chemo had gradually started to break her down. Finally, after about her 16th infusion, the start of the final round, her electrolytes were imbalanced, she needed a blood transfusion for low hemoglobin, and she was extremely pale, clammy, and easily fatigued.
Some STATS: currently the difference in mortality rate for ovarian cancer from 3 rounds (9 weeks) of chemo to the full 6 rounds is roughly 2-5%... Doesn’t seem like much when you consider the damage and side effects those 9 extra weeks cause... but that extra percentage is still a better chance... If patients experience more side effects after the first weeks, the doctor will stop treatment after 3 rounds...
Mama Jo made it through 5 complete rounds of chemo. Her initial scans were clear and we just needed to wait a few months for more follow-up scans.
She did it.
And in the best fashion, with THE BEST attitude. She has always been a positive person. You can always count on her to cheer for you, encourage you, and love you deeply. If anyone could make it through the big C, it was her... and she did!
So here we are... in the middle of another wave of this COVID-19 pandemic, living in the San Joaquin Valley, where hospitals are overflowing, COVID cases have rapidly increased, and COVID related deaths...
Friday, December 18th, Mama Jo, got tested for COVID-19. She had been symptomatic for a few days prior and scheduled a test to confirm. Her symptoms were very typical to COVID: upset stomach, diarrhea, cough, shortness of breath, body aches, etc. Mama Jo also has a long history of terrible asthma that is routinely exacerbated by changes in season, allergens, poor valley air quality, and illness...
She was positive... COVID-19... another C.
She was at home and on a regimen of several asthma medications, steroids, and regular breathing treatments to decrease her symptoms. Her oncologist saw her diagnosis of COVID and suggested she go to the ER if she continued to have symptoms... which she did... and finally, via ambulance, went to the hospital.
And that is where she has been... through Christmas and New years... She has run through all the treatments, transferred facilities, undergone all the tests, a slew of infections secondary to COVID... and here we are.
Part of me feels angry... part of me feels numb.... I move through the day knowing that I have to...There is nothing I can do, but trust that she is in good hands...
Hello 2021.
I’ve been tested. SHE has been relentlessly tested... we’ve all been tested in some way, shape, or form... I’m so done... and in those dark moments, sometimes all I want to do is give up... throw my hands in the air and say “FINE! You win!”
... and then... after my inner turmoil has had its opportunity to cry it out... after the water has settled... things become more clear... my inner voice... that voice deep... DEEP inside that speaks to you, keeps you going, motivates you, and sometimes kicks your ass in gear... well... she says I will be okay...
I have been through some great awfuls... but life will continue on and I will be OKAY because if there is anything I’ve learned from my Mama, from my Mama Jo, from everyone I’ve ever looked up to and been inspired by... its that I CAN do anything and I am so much stronger than I ever fathomed.
Can... another C.
So this is me... just leveling with you all. So much has been taken... but if there is anything I’m going to hold onto... its my hope for the best, my love for all those I care about, and my determination to continue... another C...
She’s the real champ... “C” what I mean? ;)

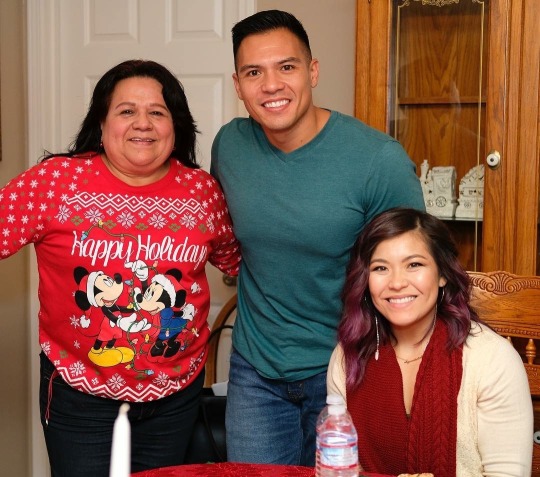
Christmas 2018?

Easter 2019?

Thanksgiving 2019

Christmas 2019

Summer 2020
Mama Jo,
I know you can’t read this just yet, but I love you so much!
Love,
Your baby girl
Nisa
3 notes
·
View notes
Note
Hi c: I remember a post, I think it was from you, about long covid and getting it? Was that you? A friend of mine is struggling and I was wondering if you had any advice about what she can do :< Thank you!!
Oh no, I hope your friend feels better soon! That might have been me, I think I posted about it here a few times and there have definitely been twitter threads.
Standard disclaimer stuff: I am not a doctor. What I found helped me might not help someone else. Long covid is kind of fucked up to deal with because it seems to hit everyone in different ways, in different areas, and months later something that wasn't a problem before can suddenly become one. The long haul groups talk about it as something that feels like it moves around the body, like a total shit gremlin.
The thing that helped me the most initially was joining the facebook groups with other people figuring shit out. This was back April/May for me but they're still very active and full of people sharing resources.
Survivor Corps is I think the big one and they've been the ones reaching out to media and doctors to try to gain some recognition with the medical community initially (as far as I know, all kind of a blur tbh). There's also a long covid group here, and if your friend searches for like, long covid + the country they're in there are usually more local/regional ones for resources closer to home too.
Because we don't really know what specific mechanism is triggering a lot of the long covid stuff yet, most of us are just treating symptoms. Some people have been diagnosed with mast cell activation syndrome (MCAS) and I don't know diddly squat about that but it might be something for your friend to look into. My whole thing has been inflammation and my immune system basically attacking itself because immune systems are both very complex and compellingly fucking stupid. Not to victim blame the immune system or anything.
What helped me depended on what was going wrong at the time, obv, but it means it's a long list.
This is just going to be a brain dump, sorry.
- I never had pneumonia. Mine started in my throat, probably damaged my vocal chords, but never turned into pneumonia. I still had shortness of breath, pressure in my chest, and my oxygen levels dropped. I could breathe but with great difficulty and described it to the EMTs as "breathing is like work." It took all of my energy and focus to breathe in enough. If you are that this point, ever, like, literally fucking ever, call an ambulance.
- Tylenol for a fever.
- Blood thinners if necessary, I never had any but we know now that a lot of problems are blood clot-related. Tbqh my blood is more thin now than anything but I always had anemia and some sort of “your blood is too small actually?” problem and we don’t know why. I just bleed a lot and bruise easier now.
- If they try to tell you it's anxiety or in your head or you're not that bed, tell them to go fuck themselves and go to the hospital. Get tested if you can. A lot of the problems long haulers ran into was that we got sick before tests were available, or we were talked into staying home by the emergency workers, and we never got tested. This opens the doors for doctors to tell you it's all in your head, psychological, anxiety, allergies, etc. Just. Go when you first feel sick if at all possible. Get tested before it turns into long covid.
- I was not sure in the beginning what "shortness of breath" or "pressure" actually felt like, and it made me delay calling for an ambulance for a few days as well. For me, it felt like there was an elastic band of pressure around my lungs. I couldn't fully inhale. My diaphragm was fucked in ways I still don't understand. My lungs also felt heavy, like there was a weight on them or like my lungs themselves were too stiff to inhale. That all counts as pressure/tightness/shortness of breath. So does air hunger, or feeling like you want to be swallowing air.
- I know I'm being super obvious but seriously shortly before I got sicker, I hit up twitter to ask what "pressure" was supposed to feel like because I couldn't tell if what I had "counted."
- Breathing: lying on my stomach with my chest propped up by pillow, in bed helped. So did pursed lip breathing: here.
- I was prescribed salbutamol initially, which did help with the worst of the wheezing and opened up some of my lungs so I could breathe easier. When I went to the ER again a couple months later, they gave me like 5x the usual dose and sent me home.
- I'm also taking Flovent/fluticasone twice a day for asthma maintenance.
- Histamines are a problem for a lot of people. Some develop a histamine intolerance, which can be helped by eating a low histamine diet.
- Antihistamines helped me the most. I was taking Allegra-D daily. Pepcid AC also helps, because it targets a different kind of histamine. There was such a run on Pepcid when this started that it was actually impossible to find in my area and I had to order some online.
- I was recently prescribed Singulair and it has been life-changing this past week or so. As far as I know it's not really an antihistamine but blocks/inhibits a particular receptor involved in inflammation that comes into play when allergies do.
- Electrolytes. I don't know why, but my electrolytes are permanently fucked and too low now. If I don't go through like a litre of gatorade a day (or whatever, pick your brand of supplements), I am even more tired and brain foggy than usual. Helps a lot.
- Inflammation is a major problem all around. Sometimes I go for the naproxen or advil and it will help any really major acute flare-up now (like, I can feel when my gallbladder is getting inflamed and about to spasm and I can cut it off sort of), but mostly it's also daily maintenance. I take cucurmin and black pepper daily.
- Other supplements: vitamins A & D, a multivitamin, NAC.
- CBD oil. This worked wonders for me for a lot of the side-effects of covid, costochondritis and shingles pain especially.
- Diet. I mentioned the low histamine one above. Other people have had some success with a low inflammation diet. Some folks also have so many GI problems that they basically ate chicken and rice and slowly reintroduced foods to see what would trigger something. I appear to get super fucked by nightshades now, e.g. Alcohol is an absolute no. I had to cut caffeine for months because of my heart. (No caffeine/alcohol/red meat was my doctor's first and best advice for heart stuff at the time.)
- Speaking of the heart stuff, if your friend is dealing with that: electrolytes again. I have pedialyte freezies that I would suck on whenever heart palpitations started and it helped calm it down some. My heart was so, so fucked for months that whenever I ate or stood up or sat down it would hit like 140bpm and I had to spend an hour moving as little as possible or I'd just about pass out. There are a LOT of long-haulers now dealing with POTS and I can't really speak to what helps that in particular but if your heart is messing up at all: call a doctor. I still don't know how damaged my heart is from all of this because doctors and wait lists, etc. Get a jump on that.
- Insomnia was absolutely the worst I’ve ever had and I’ve had lifelong, “I’m awake for three days wee” insomnia. The Singulair knocks me right out at night, so that's a bonus, but there has not been a single night since getting sick where I didn't have to take something to help me sleep. I was on Zopiclone before getting sick, at least, but seriously talk to someone about insomnia if necessary. The sleep deprivation alone was making so many things worse.
- Brain fog? Brain fog. I don't have any or many answers for this. My short-term memory is wrecked and usually I'll remember something 2 weeks later, so I live my life on a 2-week lag now.
- Related to brain fog, fatigue. Don't fuck with it. Do not. Chronic Fatigue and Myalgic encephalomyelitis are both brought up often with long covid. I am dealing with it but don't know what to say about it yet because I haven't had a single doctor give a shit thus far. I've spoken to a relative who's an occupational therapist about it and her most helpful advice was about "energy envelopes," which is basically spoon theory. If you feel tired: stop. If you don't, or if you try to push through, we relapse hard and fast and you can pay for one day of walking 10 minutes too long with weeks of being stuck in bed. It's miserable. It will take longer to get back to normal. Some of us can exercise and feel amazing after; others are exercise intolerant and it wrecks them. (I feel best after like, 10 minutes of walking and sunshine right now, which is after months and months of being bedridden.)
- Treat mental exertion the same as physical. Doctors told me to drink Gatorade after mental work because it's still work, and it has helped a lot for whatever reason. It also helps to work on one thing at a time, take a break, switch gears, take a break, etc. I can't multitask anymore anyway.
- Eliminate whatever stressors you can. Stress will make everything worse.
- It comes and goes. Every relapse was a bit shorter and a bit easier for me, so that now when I fuck up it's like 2-3 days instead of weeks, but it's a rollercoaster.
- It can be random as hell. For about two months my gallbladder just decided to up and die, basically, and we were talking about having it removed. And then it was fine. Hasn't bugged me again lately. I know I said it's symptom management, but it's also like... symptom chasing and trying to figure out what's happening every time the sun rises. This is also exhausting. Everything is exhausting.
- Brain shit. Some of us have serious trouble reading. Sentences swim together. Letters wouldn't turn into words. I took this as a Challenge and started reading children's books and then Animorphs again, like... slowly, as much as I could do without pushing it, and it's still not perfect or great but it was an okay place to start. Honestly the hardest part was the embarrassment and going from a PhD program to reading kids books, but. Do what you have to. Do what you can.
- Sticky notes and labelling things around the house so I could see them when I needed them. I am not fucking around when I say brain fog. I can open the fridge, know I have milk, know it is in the door, and literally not see it to find it. I will put the cream in the dishwasher. I will spin in circles in the kitchen remembering and forgetting and remembering why I’m there again. Sticky notes. Also: journals, index cards, write literally everything down if you need to remember something. Put it somewhere obvious. I like writing on the bathroom mirror for the important shit. (Don’t use lipstick.)
- Unsurprisingly, a lot of us are struggling with anxiety and depression. Don't let doctors get it backward: it's not anxiety making us sick, it's being sick and ignored and fighting to be helped that's making our mental health worse. So many doctors tell us it's all in our head. I did not move across the country because I was too sick to take care of myself because of ~allergies~ or ~anxiety.~ Fuck off.
- So, so many people report that they relapse whenever they menstruate so if your friend is in that group, they might want to prepare to feel like fucking trash every 4 weeks no matter what they do. I don’t have any advice on this one, I’m sorry. There are a lot of people discussing it in the FB groups, though, and those are searchable for symptoms.
- So... a tl;dr list of things that might help: anti-inflammatory diets, anti-histamine diets, pepcid AC, allegra or other allergy meds, vitamin A/D/E, multivitamins, electrolytes and gatorade, albuterol, fluticasone, zopiclone (or anything that helps with sleep), CBD oil, singulair, anti-nausea meds (buscopan), muscle relaxants (spasming gallbladder). Rest, so much rest, do not fuck with The Rest if you can help it. I also encourage just getting high and edibles as much as you can because it sure helped me chill out big time and I think was a big factor in my recovery, at least as far as helping me calm down and helping my heart were concerned.
- The actual most helpful part outside of what to take or do was other people. Friends would go out and get me things when I could not, including like, cat food deliveries and all. I had co-workers ready to step in to take over my work on days I could not. I had friends calling doctors because I was too tired to fight them or self-advocate. I don't think it's an exaggeration to say they helped save my idiot life this year. Literally. It's a lot to ask of anyone but it's also that level of support that some of us need, and there shouldn't be any shame in it. (I still feel bad about it anyway but what are you gonna do.)
Depending on where you live, some places are setting up long-haul covid clinics to help people. Reports are mixed: some demand you had a positive test even if you were sick before tests were available. Some people are getting a lot of help regardless. Some are being sent home and told not to come back anyway. It’s kind of a gamble right now but either way, there’s at least some medical recognition making headway now so my fingers are crossed.
Anyway you basically sound like a good bean and your friend is lucky to have you asking around. I have absolutely forgotten something at some point in here because, well, brain fog and no memory, but if you have any questions or want something clarified please just ask. Stay safe!
2 notes
·
View notes
Text
From Depressed to Living a Happy Life: Ciera's Story
New Post has been published on https://depression-md.com/from-depressed-to-living-a-happy-life-cieras-story/
From Depressed to Living a Happy Life: Ciera's Story

Comments: 0 | June 13th, 2019
Dr. Hotze and his special guest, Ciera Kizerian, discuss her journey from depression to living a happy life again. After her first child was born, Ciera experienced severe depression and intense self-loathing. Thanks to the staff at Hotze Health & Wellness Center, Ciera is now living a healthy, vibrant, productive life with her husband and 3 children, while helping others through her podcast called Light Through the Dark.
youtube
Podcast Transcription:
Stacey: Welcome to Dr. Hotze’s Wellness Revolution. I’m Stacey Bandfield here with Dr. Steven Hotze, founder of the Hotze Health & Wellness Center. As always, you can find our podcasts on hotzehwc.com. That’s H-O-T-Z-E-H-W-C.com.
Stacey: We have a really great inspirational story for you today. One of our guests, Ciera, is going to be talking about how she was pretty much at the very bottom and how she climbed her way back up to the top, and how she is helping other people find their way, as well. Here is Dr. Hotze and Ciera.
Dr. Hotze: Thank you, Stacey, and thank each one of you for joining us today on Dr. Hotze’s Wellness Revolution. You know, I believe that you and everybody needs a doctor and a staff of professionals who can coach you on the path of health and wellness naturally, so that you have a life-changing transforming health experience here at the Hotze Health & Wellness Center. That’s what we offer.
And the reason we do this is because we believe that as you age, you ought to be full of energy. You ought to have vitality in your life and be brimming with enthusiasm, no matter if you’re 30 or 70 or 80. You ought to have those qualities – energy, vitality, and enthusiasm. And so we do that here at the Hotze Health & Wellness Center. We help get you on that path. We coach you onto the path of health and wellness so you could have that life-changing experience, because my philosophy is this: I believe if you’re alive, you ought to feel alive, right? Why be part of the walking-wounded or half-dead? Enjoy life, be full of energy, and that’s what we help you do here at the Hotze Health & Wellness Center.
And I want to give you a great example of that. Most people think, “Well, you know, people don’t really start having problems until they get older and I don’t need to do anything about my problems. I’m young now. I’m 30 or 40 or 50, and I’ll wait until I have some problems.” An once of prevention is worth a pound of cure. That’s an old adage, thousands of years old. An ounce of prevention is worth a pound of cure.
We have with us today a guest of ours who’s been a guest since 2017, Ciera Kizerian. Ciera is a, what, 27-year-old woman?
Ciera Kizerian: How old am I? I’m 28 now.
Dr. Hotze: 8, a young…
Ciera Kizerian: I shouldn’t…
Dr. Hotze: …woman. 28-years-old, came to see us when she was 26. So, Ciera, welcome to the program. Glad to have you…
Ciera Kizerian: Thank you.
Dr. Hotze: …on board here, dear.
Ciera Kizerian: Happy to be here.
Dr. Hotze: Glad to have you here. And you have such a wonderful and remarkable story. Why don’t you start and tell us where you’re from, where you grew up? Where are you from?
Ciera Kizerian: Yeah, I grew up in Dallas, Texas, and…
Dr. Hotze: That’s near Fort Worth, isn’t it?
Ciera Kizerian: Yeah.
Dr. Hotze: I like to tell Dallas people that.
Ciera Kizerian: Yeah.
Dr. Hotze: So you grew up in Dallas. And how did you end up down here in Houston?
Ciera Kizerian: My husband’s work brought us down here a couple of years ago.
Dr. Hotze: Okay. Now did you go off to school? You go to college?
Ciera Kizerian: I did, yeah. My husband and I met at Brigham Young University.
Dr. Hotze: Oh, that’s wonderful.
Ciera Kizerian: Yeah!
Dr. Hotze: I just came back, yesterday, from Salt Lake City.
Ciera Kizerian: Oh, awesome.
Dr. Hotze: Isn’t that great?
Ciera Kizerian: It’s beautiful.
Dr. Hotze: And I went up to…we went and saw the Salt Lake Tabernacle, where the Mormon Tabernacle Choir sang.
Ciera Kizerian: Yes. They are so talented.
Dr. Hotze: Yeah, and that was built in 1868, and it is…man, the acoustics in there are just…
Ciera Kizerian: Incredible.
Dr. Hotze: …phenomenal. And of course, the temple was across the street, and it was wonderful. It was a wonderful time, and Utah’s a…
Ciera Kizerian: Oh…
Dr. Hotze: …beautiful, beautiful state, and all around Salt Lake City, the mountains that are still covered with snow…
Ciera Kizerian: Oh…
Dr. Hotze: It was wonderful.
Ciera Kizerian: Yeah, I love…
Dr. Hotze: And the flowers?
Ciera Kizerian: …Utah.
Dr. Hotze: Oh my goodness. Just incredible. So anyway, you went to Brigham Young, and then what kind of work is your husband in?
Ciera Kizerian: He is an entrepreneur. We call ourselves “serial entrepreneurs.”
Dr. Hotze: Well, what is he doing right now? What kind of work is he doing?
Ciera Kizerian: So we both, actually, are working on a project called “Light Through the Dark,” and it’s to help people that are dealing with anxiety and depression know how to come out of it and get the resources they need to get better. And then also it helps those who are the support system for those struggling to know what to do to help the person, and have it not be damaging, but to be helpful. So we’re building…I don’t know what you’d call it, an effort, right now, to try to help people dealing with that.
Dr. Hotze: That’s wonderful. And this, really, is an outshoot of what happened to you, in your life, and your coming through Hotze Health & Wellness Center. So tell us, you have three children now, right?
Ciera Kizerian: As of one month ago, I have three children, yes.
Dr. Hotze: That’s great. So tell us what your health experience was like growing up. Did you have health problems?
Ciera Kizerian: No. I mean, not any mental health problems at all. I had asthma growing up, but other than that, mentally, I’ve always been described as someone that was optimistic and happy, a go-getter. I definitely ran at a hundred-plus speed every day, and would…
Dr. Hotze: You were a live wire.
Ciera Kizerian: …be myself, yes. Live wire, exactly.
Dr. Hotze: And so when did that change?
Ciera Kizerian: So after my daughter was born in 2014, about six weeks later, I noticed that I just started feeling this oppressive heaviness. I had a really good relationship with my husband, but he said to me, “I literally can’t do anything right around you right now.” And I was like…
Dr. Hotze: Any guy ever felt that way before, huh?
Ciera Kizerian: And that keyed me in of, “Oh, you’re right, something’s off right now.” I was getting really irritable, I was starting to have a lot of brain fog. I just didn’t feel myself. And then I started having all these crazy symptoms and realized that I was developing depression really bad. And this wasn’t something I’d ever experienced beforehand. Again, these…
Dr. Hotze: And then you were how old? It was five years ago, so…
Ciera Kizerian: 24. I was 24.
Dr. Hotze: 24, okay.
Ciera Kizerian: Yeah, and…
Dr. Hotze: So what did you do about it?
Ciera Kizerian: So I went and talked to my OB at six weeks, and they put me on some antidepressants, and they said, “Oh, but it’ll take a while for it to kick in.” So that was a really hard winter. Everything was just so new to me, all these emotions, all these feelings that I never experienced before. And it was just a really, really dark and hard place for me.
It took a while for the medicine to kick in, and then I felt kind of felt up, not totally like I had before, but well enough where I was able to function. And then, a year later, it just flipped a switch, and, when I started my cycle again for the first time after having my daughter, and I hit a low that I didn’t know was possible.
And that’s when I first experienced suicidal ideation, and where I started just feeling like everyone would be better off without me. And really had intense self-loathing, which I had never, ever, ever experienced. And I couldn’t interact with anyone. If I went out, if I went to church, or wherever I was going, it was like I was watching the clock the entire time to be able to just leave, and escape, and go back to my closet where I could just get in that hole and just want to just be done with everything. It was not me at all. And it was very hard, and…
Dr. Hotze: And you were taking medication, antidepressant medication at that time, right?
Ciera Kizerian: Yup. And I saw a psychiatrist, and I got even more medication. They upped it to the highest amount that I could be on for the antidepressants. I got put on antipsychotic medication three times a day, anti-anxiety medication three times a day, and even with that, was still having these battles with…
Dr. Hotze: Does this sound familiar?
Ciera Kizerian: …fighting suicide.
Dr. Hotze: I have heard this story…if I’ve heard it once, I’ve heard it thousands of times. Now, the conventional doctors take an individual like Ciera, and I’m sure they did blood work on you before they started this, and said, “Well, your blood work’s normal,” right?
Ciera Kizerian: Yeah.
Dr. Hotze: “Your blood work’s normal, so you must be depressed.” You are, and they put her on all these antidepressant medications, anti-anxiety medication, antipsychotic medication, and you didn’t get better, and they kept bumping it up.
Ciera Kizerian: Yeah.
Dr. Hotze: Frankly, I just think that’s criminal. And these ought to be banned, and these doctors should be reported to the medical board, and their license should be removed, because they destroy people’s lives. I feel really strongly about this. I’ve seen so many people like Ciera, and we’re not going to talk about what happened.
And this is so simple to resolve. I’ve written books about it. You know, all these psychiatrists ought to read my books, and figure out what to do to help women when they start coming in…and men, too, when they begin to have these sort of problems.
So you ended up having another baby. Were you on antidepressants at the time when you did?
Ciera Kizerian: No, so that’s my miracle baby. I was on all that medication starting in two thousand and…
Dr. Hotze: Fourteen.
Ciera Kizerian: Well, the antidepressants, but then when I saw…that was what the OB put me on.
Dr. Hotze: Right.
Ciera Kizerian: Then the psychiatrist on all the other stuff in…it was three years ago, so 2016. Like, May 2016. So then I came to the Hotze Health & Wellness Center in May 2017, and did the yeast-free diet, and was feeling really good, and started coming off of the…not everything, because I wanted to have another baby, but again, there’s no way I could’ve.
Dr. Hotze: Before you come…I’m looking right here. It’s your first appointment, and we have the reasons for the appointment: “anxiety, panic attacks, low moods. Wants to be able to get off the medication, have another baby, low energy, brain fog, lightheadedness, hoarseness, severe constipation.” These are some classical features that we see in people that have hypothyroidism. Were you having difficulty with weight, too?
Ciera Kizerian: t that point, I was so depressed I just wasn’t eating, really, at all. And so my mother-…
Dr. Hotze: You did…
Ciera Kizerian: …in-law came out just to see me, ’cause she said, “Ciera, you are getting way too thin, and we’re going to lose you.”
Dr. Hotze: But you had problems, then, with brain fog, with poor sleep, and…
Ciera Kizerian: Yeah, I mean, I never had my phone on me. My grandparents were calling my parents and saying, “Can you please tell Ciera to answer her phone? They were getting offended and upset with me, and it was causing family problems ’cause I could never find my phone. And I would leave my wallet and my purse just on the driveway, and I would walk into a room be like, “Why am I here?”
And I hear my grandma telling me that, “Oh, I’m just…I forget my purse everywhere.” I’m like, “Yeah, I’m right there with you, grandma.” Except we have a big age gap, and I shouldn’t be feeling like a grandma in my mid-twenties. Nuts, and…
Dr. Hotze: So you came into the Health & Wellness Center.. How did you find out about us, by the way?
Ciera Kizerian: A friend referred me, and told me. Actually, she told me about it in the fall, but I was just too bad to really help myself, and she then told my husband about six months later, and he’s the one that got the ball…
Dr. Hotze: Encouraged you to get here, right.
Ciera Kizerian: …and helped me come here, yeah.
Dr. Hotze: So when you came in, you saw Dr. Ellsworth, and he put you on the yeast-free eating program, and he put you on some thyroid medication. He also gave you some natural female hormones, progesterone, to help you with your menstrual cycles, because it was obvious that your problems were hormonal, because it happened after childbirth.
This is not uncommon at all. A woman will feel fine, have her first baby, and then all of a sudden they crash, and their hormones don’t kick back in right. Remember, during pregnancy, the hormones that a woman has in her body are made by the placenta, which belongs to the baby. And so, when the baby’s delivered, and the placenta follows, there’s a dramatic fall in the naturally-occurring hormones of pregnancy, and her ovaries have been shut off, and they have to turn back on.
And if they don’t turn back on right, and she doesn’t have adequate amount of female hormones, and they don’t balance out, she’s going to have a host of symptoms. I mean, there are all these symptoms that we talked about. The fatigue, low body temperature, can’t think clearly, poor sleep, constipation…Oftentimes women have problems with weight gain. She didn’t because she was so depressed she didn’t even want to eat, and if you don’t eat, you’re not going to gain weight, obviously. So what happens to these women, then they end up going to see your conventional doctor, like Ciera did, and what do they do? Immediately slap them on some SSRI antidepressant. That’s a…SSRI is a selective serotonin reuptake inhibitor. It inhibits the uptake, in your brain, of a neurotransmitter called serotonin.
Well, guess what? And this was Lexapro you were on, but there are other SSRI antidepressants, like Prozac and Effexor and Paxil, just to name a few, Cymbalta and others. And these are all SSRI, or they’re reuptake inhibitors, with the idea that if we don’t let the body reuptake the serotonin in the brain, and it just floats around, you’re going to feel better, which is not the case.
The case, in your case, in fact, it made you worse, and they gave you more drugs. And you just got drugged up, and what it does is it flattens the entire affect. It takes away who you are so you don’t have any feelings anymore. You don’t feel sad, you don’t feel good, you don’t cry…
Ciera Kizerian: Apathetic.
Dr. Hotze: You’re apathetic about life.
Ciera Kizerian: Numbness, you feel this…
Dr. Hotze: Right.
Ciera Kizerian: …total numbness. Like, I would love to feel happy right now, I would love to just feel anything right now, but you just feel empty inside.
Dr. Hotze: The SSRI antidepressants are a knock off of cocaine. Cocaine is a reuptake inhibitor. It blocks the reuptake of serotonin and of dopamine. It’s a neurotransmitter reuptake inhibitor. If you look at the molecular structure of the SSRI antidepressants, they’re almost identical to cocaine. They’re highly addictive, it’s hard to get off of them, there are terrible withdrawal symptoms, and it’s a way, basically, that drug companies get people to be addicts and take the drugs the rest of their lives.
Nobody has depression because they have low levels of antidepressants or anti-anxiety medication in their body. Nobody. If you’re having problems with moods that are roller coaster moods, they’re up and down, or you’re depressed, or you’re having anxiety attacks or panic attacks, that’s not caused because you lacked some pharmaceutical drug. It is primarily going to be a result, and almost 90% of the cases, it’s going to be a result of hormone decline and imbalance, which can be easily corrected.
So I know that Dr. Ellsworth put you on some thyroid medication, right? He put you on some female hormones, natural progesterone, got you eating right, put you on some vitamins and minerals. And how long did it take you to begin to notice any difference?
Ciera Kizerian: Oh, I wanted to cry when I started feeling…it was, I think, within two weeks of taking those that I was feeling up and feeling myself. I was able to…I’m a photographer, and I was able to go on a trip by myself for a photo shoot in Greece. Just, like, in August of that year, which…
Dr. Hotze: And you came in when?
Ciera Kizerian: In May. So within…
Dr. Hotze: So within two or three months, you were…
Ciera Kizerian: I was able to…whereas before, I’m stuck in my closet, I can’t interact with anyone. Within a couple months, I’m getting on a place by myself, I’m flying across the ocean first time by myself. I’m exploring Greece. Like, wow, that’s a huge difference…
Dr. Hotze: Sure.
Ciera Kizerian: And I remember, when I was there in Greece, I was on this catamaran, and we’re snorkeling, and I was swimming, and I was in the ocean, and I remember just having the water flow through my hair, and I just thanked God that I could enjoy life again. It was a moment for me where I was like, “Wow, this is worth living. I don’t feel what I’ve felt for years of just wanting to be gone, because it was just too painful to be alive.”
Where, with depression, when you have really severe depression, you feel so low that death seems up, it seems like a welcomed option because of how horrible you feel. And for me to be there, and to just love that moment, and love how I felt, it was priceless.
Dr. Hotze: That’s wonderful.
Ciera Kizerian: Thanks.
Dr. Hotze: A wonderful story, all that. So how long did it take you to get off the antidepressants?
Ciera Kizerian: So I am…I started trying to get off November of 2017, and it took me about three months. Dr. Ellsworth was really good at helping me get off of it, and helping me to understand the withdrawal symptoms, and that whole process. And helped me find this great book that he recommended, “The Antidepressant Solution.”
Dr. Hotze: …Solution.”
Ciera Kizerian: Wow, that book is…I’m like, “This is the bible for anyone that has been on antidepressants.”
Dr. Hotze: It’s by Dr. Glenmullen, “The…
Ciera Kizerian: Incredible.
Dr. Hotze: …Antidepressant Solution.”
Ciera Kizerian: Yeah, that really helped me a lot, to just know what I was coming up against, and what to expect, and how to come down, and I had to come down really slowly. But I had this goal of, “I want to have another baby.” I just, when we first got married, I was like, “We’re having six kids. Here we go.” But once this depression kicked in, it really changed a lot of things in our life of what reality would actually look like.
But I did still want to have one more. And so we came…about three months, the withdrawal reactions were miserable, like you said, and I was coming down so slowly. It was a really rough time for our family, trying to go through that, but then I was able to get off of it in, probably March, I was totally done with them, and it had been…
Dr. Hotze: March of ’18.
Ciera Kizerian: ��some time. March, 2018.
Dr. Hotze: Right.
Ciera Kizerian: And then I got pregnant in July of 2018, which is like nothing short of a miracle. I had been looking into adoption and all these other things of how I could somehow still have this baby, knowing I might never be able to get off this medication. I might not ever be able to feel better, like way before, but then coming here and then learning about all this stuff, it made me feel like I could not only come off of it, but be able to be a good mom, which is not what I had felt beforehand, at all.
Dr. Hotze: Well, this is really, really remarkable. And wonderful. And first, I want to congratulate you for doing a 180 and taking charge of your health, and not just resigning yourself to being on drugs the rest of your life. And you can imagine what that would’ve done for your husband. I know you’re a woman of faith, and your husband is, too, and thank God, it’s to your husband’s credit that he stood by you.
Ciera Kizerian: Oh, he has said, and I have said, this could have resulted, for so many people, in divorces…
Dr. Hotze: In divorce. Oh, this happens all the time.
Ciera Kizerian: …or your kids having a lot of issues with you long-term. All these things, like…I’m so grateful that we had fought for me, because if we had just said, “This is just our new normal, this is just how things are going to be,” we never would have tried to get in that hustle and literally fight. And it was a fight every day, because you have to fight to eat the right way, you have to fight to make the changes that are needed.
And I talked to him, and now with the Light Through the Dark stuff, and talked to people now that are like, “Yeah, my kids don’t have a good relationship with me, and our family is estranged, because when they were younger I dealt with these things, and I never addressed it. And I thought that this was just my normal, and just accepted that this is my MO for life.”
Or they get divorces. I have another friend who, he’s like, “I didn’t realize I was dealing with depression and anxiety all these years.” And yet he would have these big blowups with his spouse, and she’s couldn’t…she was like, “I don’t want my kids in that environment.” Really, it was he needed more support and more help with his mental health to be able to not have these triggers set off the irritability, and the panic.
Dr. Hotze: And so this is…your new business venture is entitled what?
Ciera Kizerian: Light Through the Dark.
Dr. Hotze: Light Through the Dark. And so how can somebody look at the podcast that you’re doing, and the YouTube videos, how do they do that?
Ciera Kizerian: You can just look up “Light Through the Dark” on YouTube, or whatever. And the main goal of it is really…
Dr. Hotze: So type in YouTube, ‘light through the dark.’ And how about on podcasts, what do they do?
Ciera Kizerian: Yeah, same thing. It’s called Light Through the Dark.
Dr. Hotze: Light Through the Dark on a podcast, and you can hear Ciera, she talks about these various issues that people have with mental depression, and anxiety, and panic attacks, and these things that are affecting them…she helps individuals that are having those problems. And then she interviews other people that have had problems, and as a matter of fact, we’re going to do an interview…later today, I’m going to do a podcast for Ciera, and we’ll talk about these things. Well, Ciera, this is a wonderful story…
Ciera Kizerian: Thank you.
Dr. Hotze: Now let me ask you, on a scale of zero to ten, ten being “brimming with energy,” when you first came in, what was your energy level?
Ciera Kizerian: Oh! Zero? Like, I just…I had no energy.
Dr. Hotze: At 26 years old. No energy.
Ciera Kizerian: Yeah, no, I’d wake up and feel exhausted, and I would be so tired I needed to take a nap, but I knew that if I, for whatever reason, I’d wake up and just have gripping anxiety. So bad it felt like someone had chains and cords around me, and I would just be stuck in that anxiety for at least an hour, where I couldn’t get up, because it was so gripping and so bad. And couldn’t talk to anyone, couldn’t reach out and be like, “Help me get out of bed.” And then, it was just multiple naps during the day. Never feeling…
Dr. Hotze: So…
Ciera Kizerian: Yeah.
Dr. Hotze: How would you describe your energy level now, your overall moods, on a scale of zero to ten? Now you just had a baby, here, six weeks ago, didn’t you?
Ciera Kizerian: I just had a baby, and I mean, I need a nap a day, but sometimes…and that’s usually because I stayed up too late watching Netflix with my husband and then was up with the baby again in the night, but on the days when I’m not watching a show, it’s not anything outside of what I felt as a teenager. Or, actually, I feel like I feel better. I keep telling everyone, like, “Wow, I feel like I should be having a much harder time with having a newborn than I actually am,” but I actually do have a lot more energy right now than I did with everything before…even though I should not have as much, having a newborn.
Dr. Hotze: Right.
Ciera Kizerian: I don’t know if that’s making sense, but…
Dr. Hotze: And I know this is important, and I talked to you about it, and I asked you if you had started on progesterone, and you just started on it yesterday. This is six weeks after the birth. If I had of known about you having…that you’re pregnant, I would have made sure, like I did with my five daughters, the day after they had their baby, they were on progesterone. And none of our daughters, out of our five daughters and we have 23 grandkids, none of them even had the baby blues. They never had any depression.
But that’s because progesterone levels dropped dramatically. They’re very, very high at the end of pregnancy. The placenta makes huge amounts of progesterone, they’re many times what you would normally experience. And when the placenta’s delivered, there’s a precipitous drop in progesterone, and that’s what leads to the problems with depression.
Also, low thyroid can lead to the problem with depression, also. Thyroid can be adversely affected when the hormones fall, that puts you in a state of estrogen dominance, and that adversely affects the thyroid, so now that we have you on progesterone, you’re going to be feeling back, just on top of your game again.
Ciera Kizerian: Well, I’m really grateful that this pregnancy, I had the bioidentical hormone therapy, because as soon as I found out I was pregnant, that morning I called the nurses here, and they said, “Okay, well, let’s have you have this much progesterone, so we can protect the pregnancy.”
Dr. Hotze: Right.
Ciera Kizerian: And went through that until I was, like, 14 weeks pregnant. And that was really helpful for me, because I had had miscarriages before, and obviously had worked so hard to get pregnant…
Dr. Hotze: How many miscarriages had you had?
Ciera Kizerian: Sorry, I had had one before my daughter. And my mom had a history of miscarriages, and…
Dr. Hotze: Which is a classical feature of hypothyroidism. Infertility and miscarriages are classical features of low thyroid that doesn’t show up in your blood. It’s not how much thyroid you have in your blood, it’s how much thyroid you have in your cells, and that can only be diagnosed by a clinical history.
So I believe that everybody that has the clinical symptoms of hypothyroidism, no matter what their blood test shows, deserves a therapeutic trial of thyroid hormones to see how they do. And it usually does remarkable for them.
Well, Ciera, congratulations on your success, and I wish you every success as you work on Light Through the Dark, this effort to help individuals overcome their depression, anxiety, and panic attacks. Thank you for joining us, and…
Ciera Kizerian: Thank you.
Dr. Hotze: Thank each one of you for joining us today, on Dr. Hotze’s Wellness Revolution. You remember, this is what I believe. I believe that while liberals are getting high, conservatives should get healthy so we can make America great again. If you want to get yourself on a path to health and wellness, if you’ve experienced symptoms that Ciera has , if you’re a young woman, you don’t have to wait till you’re 50 to come in and suffer on antidepressants on 20 to 30 years in your life, you can get yourself on a path to health and wellness now, by taking charge of your life, doing a 180.
Dr. Hotze: Give us a call at Hotze Health & Wellness Center at (281) 698-8698, and we’ll be glad to set up a complimentary consultation for you, and partner with you so that you can get you on a path to health and wellness and help you have a life-changing health transformation, so you have energy, you have vitality, and you have enthusiasm again for your life.
Thanks for joining us today. God bless you.
We Can Help
Can you relate to Ciera’s experience? Take our symptom checker to find out if your symtpoms could be caused by hormone decline and imbalance.
!function(f,b,e,v,n,t,s) if(f.fbq)return;n=f.fbq=function()n.callMethod? n.callMethod.apply(n,arguments):n.queue.push(arguments); if(!f._fbq)f._fbq=n;n.push=n;n.loaded=!0;n.version='2.0'; n.queue=[];t=b.createElement(e);t.async=!0; t.src=v;s=b.getElementsByTagName(e)[0]; s.parentNode.insertBefore(t,s)(window, document,'script', 'https://connect.facebook.net/en_US/fbevents.js'); fbq('init', '391742731206178'); fbq('track', 'PageView'); Source link
0 notes
Text
Resistance is Futile

The virus is real. The virus is here. It is highly contagious and potentially deadly. I think we can debate about the severity and the origins of the virus later, or, we could debate it now, but while staying the hell away from each other and cutting off this thing's lifeline.
Okay, so, it's easy for me to have that opinion. I'm lucky. Kind of. Ish. I've kept my job. Kind of. Ish. My pay has actually been slashed pretty badly. Commission has been cancelled for April and May so I'm going to be getting base pay only. Okay, yeah, I know a lot of people only get base pay and I was one of them for a very long time, and I’m lucky to have gotten anything above and beyond that. But I have been getting paid above and beyond my base pay and I've grown accustomed to a new comfort level. The stimulus covers that for this month, so I’m not feeling it yet. But I'm lucky to have kept my job and gained the flexibility to do it from home, which is something I've been lobbying for to management for the past four years, anyway.
But the immediate lifestyle adjustments? Fuck, man. This is heaven. Sequestration is magical. I have a valid reason now for telling people to stay the fuck away from me when before I was just an asshole. I never had any desire to go anywhere anyway — and now I have the perfect excuse, and zero guilt. It's fucking fantastic.
Okay, so, I like the lockdown. It's not hard for me. I'm working from home, which is perfection. I want my commission pay back, my performance-based earnings, but aside from that, we can keep this lockdown going for everyone capable of working remotely for just as long as … well, forever. We can just keep this up forever.
I don't miss anything. I don't miss eating out. I don't miss going out. In fact, I just had to go out, and it was sheer hell. I needed a VGA cable immediately, so I ordered one from Best Buy for curbside pickup. Traffic is fucking stupid. Fucking assholes everywhere. Nobody at Best Buy was wearing a mask or gloves, and they're walking up to customers' cars handing them merchandise, talking to each other in close quarters. The guy who handed me my purchase weighed at least four hundred pounds. If he gets this virus, he's pretty likely dead. This thing isn't kind to the morbidly obese. Unfortunately, most of central Indiana is morbidly obese.
Okay, so, all cards on the table, I have ulterior motives. I like things shut down. So, of course I'm going to champion this course of action. But I also just think it's the right thing … nay, the ONLY thing to do right now. The death toll will likely be at or very near 45,000 by the time I post this, and it is climbing steeply on a daily basis. And that's with all of the extreme social distancing most of us are practicing right now. If we hadn't done this, if we hadn't shut down, we'd be over 200,000 deaths, easy, and it would be fucking chaos out there. Hospitals would be beyond capacity, mayhem would ensue. I have no proof of that, it's just what I think. I can't prove something that I think would have happened under different circumstances.
I'm not terrified of this thing. I'm being respectfully cautious. This is a formidable enemy. My goal is to not get it, to avoid it completely. That way I don't roll the immune system dice on this disease at all, and I maintain a zero fault status in the spread of the virus. If I can pull that off, that will be a perfect game, I win. But this thing is highly contagious, and it is in my city, and it is inside far more people than the daily news numbers show because hardly anyone is being tested. Also, a lot of people get it, and they are just fine. If I get it, I will likely be okay. But, that's not a guarantee. There is a risk. People say the mainstream media is collectively sensationalizing this. Well, of course they are, in their way. Of course they're playing it up for ratings, that's what they do.
But I don't think they are making it sound worse than it is. I was watching a news broadcast and they said that eighty-six percent of the people under fifty who died of COVID-19 had an underlying health condition such as an autoimmune disorder, obesity, diabetes, high-blood pressure, asthma, or being a smoker. First of all, those are all pretty common. That's a lot of at-risk people. But second, that's what they did say. Eighty-six percent of those under fifty who died had an underlying health condition. But what they didn't say, and what I heard was this: Fourteen percent of the people under fifty who died of COVID-19 did NOT have an underlying health condition. That sounds fucking scary. Yes, that is still a small number. Most of the people who die from COVID-19 are over eighty years of age. So, the percentage of people who died who are under fifty is low, and it's fourteen percent of that number … but still. That's otherwise healthy young people with no underlying health conditions who are dying. Greater risk for the elderly doesn't equal zero risk for the young. That's not how math or statistics work.
I've watched videos online from real people. Nurses on the front lines in the hardest hit cities describing chaotic and dangerous conditions in hospitals. People who got the disease pretty badly, but recovered, recounting their terrifying near-death experiences. Yes, a lot of people have a sniffle and a cough. Yes, some people remain asymptomatic throughout the life of their infection, remaining symptom free, but still allowing the virus to replicate in their bodies so they can spread it. But this thing just slaps the fuck out of some people, and sometimes kills them, for no reason. Not because they're old, or sick, or have an otherwise compromised immune system, but they’re just simply unlucky. I mean, maybe there’s something we don’t know. Perhaps they all have something in common, some underlying factor that hasn’t been identified as a risk. That’s surely possible. But still — do you have it, this factor? Do I?
But fear of getting infected isn't the main reason to distance and hunker down.
We should stay locked down and we should try our best not to spread it because it's extremely contagious, and there is a pretty large section of our society, who, for various reasons, really shouldn't be put into battle with this virus. A lot of them don't have a chance, and we, as a society, need to do the right fucking thing and keep this bug as far away from them as we can. And if caring about the sick and elderly is outside of your capacity, just know that you aren't safe, either. It could kill you, too. Fourteen percent of the people under fifty who died from COVID-19 did not have an underlying medical condition or compromised immune system. I'm sure they all thought they would be fine.
I have learned the following by reading articles written by experts in the field.
There are eight strains of SARS-CoV-2 circulating the globe right now that cause the disease COVID-19. No one strain is deadlier than another, they are all very similar to each other. SARS-CoV-2 is not likely to rapidly mutate and go airborne or get into the water supply. Its current method of transmission from human to human is so effective it has no immediate need to try to adapt or evolve. If and when it does need to evolve to try to bypass our eventual vaccine, it will take it a while. Coronavirus evolves, or mutates, at a slow rate, about four times slower than influenza.
I should be citing this stuff, but this is a blog, not a peer-reviewed paper. This isn't shit I've discovered through testing and examination, and I’m not trying to formulate my own hypothesis. I’m no expert in any of this, I'm just repeating shit I've found from articles that were well-sourced, and anyone can find them by Googling this stuff and seeing where I found it. But I digress, as I am wont to do. Anyway, more science facts.
SARS-CoV-2 spreads from human to human in both large droplets and aerosol that exit the body during a cough, sneeze, panting, heavy breathing, etc. Any method that would allow moisture to escape the mouth on the breath. The virus can hang suspended in mist for up to three hours and remain active. The virus can live on paper and cardboard for up to 24 hours, and can live for up to 72 hours on plastic, stainless steel, and other smooth shiny surfaces.
So, on a relatively humid day, and, I know, how many of those are we going to see in mid-Spring, right? On a relatively humid day, an infected person sneezes. That infected aerosol can join with the water already in the air, and just float around ready to be breathed in for up to three hours. So, sure, stay six feet away, but if you move into a space someone else was just standing, you're now breathing in what they just breathed out.
I don't care who says what about masks. I don't need someone to explain to me how and why masks work. I get that the virus is small and can pass through very small openings and to be fully effective a mask would have to be rated to work against particles as small as the virus, which in this case is N-95. But I also understand that if you're sick and you cough and you're wearing a piece of cloth over your face, you're going to greatly decrease the chances that you're going to spread the virus. Yes, small aerosols will make it through, but a lot of the germs will be caught and never enter the atmosphere. So, yeah, masks are prudent. Any of us could have it, and we should try not to spread it in case we do.
I am lucky and I get to stay in my house. I don’t know what lies I’d be telling myself if I had to go out in the world every day like nothing has changed and do a thankless job. Everyone still out in the world and not practicing social distancing will probably get this. I may get this, despite my best efforts. Most of us will be okay. Some of us won’t.
0 notes
Text
Press/Video: Jameela Jamil Is Shutting Up and Making Space in 2019
New Post has been published on https://jameelajamil.org/2019/02/01/press-video-jameela-jamil-is-shutting-up-and-making-space-in-2019/
Press/Video: Jameela Jamil Is Shutting Up and Making Space in 2019

youtube
The ‘Good Place’ actress and body positivity activist joins the #AerieREAL role model family.
If you’re familiar with Jameela Jamil’s, work you may know her for a few things: her role as the narcissistic but always well-intentioned Tahani Al-Jamil on NBC’s The Good Place; her fiercely vocal stance against photoshopping and airbrushing in advertisements and magazine covers; her news-making tweet in which she hoped certain celebrities “shit their pants in public” for hawking “detox teas” that promise to help with weight loss and bloating. In her 32 years on earth, the British actress has battled an eating disorder, hearing loss, and a car accident that broke her back. Yet she’s come out on the other side, starting a beloved life positive moment called “I, Weigh” and as of today, Jamil is one of the newest members of the #AerieREAL Role Model family for spring 2019. Ahead of the reveal, I phoned Jamil to discuss how the body positivity movement can change moving forward, why she wished Aerie existed when she was a teen, and why in 2019 she’s making space, not taking it.
When Aerie revealed you were going to join their campaign, it seemed like a match made in heaven. Why did you want to work with them?
I wanted to work with Aerie because they’re one of the only brands I’ve ever seen actually take inclusion seriously, and it’s not performative. It runs throughout the entire brand: their desire to reflect, on their website and in their stores, what we see outside in everyday life, which just never happens. Seeing people from all walks of life and all ages modeling underwear and modeling clothes was just such a breath of fresh air. When I walked into their store I realized how much I could’ve benefited from having a store like that and a company like that when I was younger, so I was very excited to be a part of it. Your body’s been through a lot, between an eating disorder and a serious car accident. How has that affected the way you treat your body now?
I treat my body with great respect now and I make sure to check in with it and thank it every so often. Because I’m aware of what it’s like to not be able to go to the toilet by myself, or to be able to breathe because I had asthma, or be able to hear, because I was deaf as a child. I also stopped menstruating when I had an eating disorder, so my body has been in jeopardy so many times that I’ve, frankly, by the age of thirty, a little bit late but better late than never, learned to treat it with lots of kindness and respect. I don’t talk shit to myself anymore. Every time it crops up I stick up for myself the way that I would for a friend or for a stranger even. The things that women say to themselves in their head, they would never tolerate being said to someone that they love. So I’ve decided to be my own best friend.
I’ve become the loudest voice that’s been allowed in body positivity and I think that has given some people the wrong idea.
How does being your best friend manifest itself?
I did EMDR therapy, which is a specific kind of therapy that removes the conditioning of irrational thought. So it goes right to the core of the problem. It’s very good for PTSD, anxiety, depression, eating disorders, and OCD—all of which I had. Within a matter of months, it just sort of extracted the root of the problem, which meant that I didn’t have to deal with the symptoms anymore. So that was a big thing that I did. I also made the decision three years ago that most of my money that I would spend on corrective or beauty items I’d save up for therapy. I started doing that when I was 29, and that was probably the biggest act of self love I’ve ever done. So no cellulite cream, no stretch mark cream, nothing anti-aging, I just put all of my money into a piggy bank that I would’ve spent on must have products. I just did therapy and then bought myself some self love.
youtube
Body image and body positivity can be super personal. How do you discuss these topics without alienating people?
I link body positivity with mental health, which makes it a much bigger and broader conversation. I think that we don’t do that enough I think I’ve kind of moved it more into a life positive movement and more into mental health discussion, and I think we can all relate to that. Body positivity is something that we have to be very conscious of not leaving women who are of minorities out of. We need to include everyone, so I just make sure to be inclusive with my language and make sure that I’m involving activists from different minorities in my work and giving them a platform in order to make sure that everyone knows it’s a conversation for all of us to have.
For example, the MeToo movement got kind of taken over by a lot of very famous, slender, predominantly white, straight women actresses. I think it’s important not to let that happen with body positivity, which it does happen. Often, in the last year I’ve become the loudest voice that’s been allowed in body positivity and I think that has given some people the wrong idea: that I think that I speak for all people, which I don’t. It’s just that I have a platform and a privilege that allows me to be listened to and heard, when other people who are actually struggling with these things are being ignored. I’m not afraid of being annoying, I’m just afraid of being complicit in a problem that is systemically destroying the mental health of most of the women around the world.
So how do you deal with the criticism?
I don’t take it personally anymore, and I think I used to get defensive and when I would be called out for not being intersectional enough or just feel frustrated that people were expecting too much of me, but now I just shut up and I listen and I realize that there are people who are going through a lot and I would like to help those people, so I just focus on the good. I also don’t receive a lot of negativity or backlash. Most people support me and my profile growing in the way that it has, has been a sign of mass support of so many people who were just done, they feel the same way as me. I’m not on the wrong side here, I’m on the right side, the feminist side of mental health of young people and their well being internally and externally, of women and people everywhere.
The hashtag is #AerieReal. When do you feel you’re most real?
I feel I’m most real when I’m cuddling my boyfriend, I do [laughs]. I feel most real when I’m spooning. There are so many great role models. Who are some of your own role models in this space?
I mean, Samira Wiley is one of them, so I was super starstruck to meet her and to be photographed alongside her. That was a big seal of approval. Janet Mock is someone that I’m very, very obsessed with, and think that what she has done for our culture is just so extraordinary and she’ll be remembered forever and go down in history as such a game changer for the trans community. Roxanne Gay, I think she’s a real hero of mine, and her books have taught me so much and called me out so brilliantly. As in, in reading them I’ve been able to find my own mistakes and learn, via her, how to do better and be better.
I think we bring a lot of ego into activism and wokeness these days.
What did you learn from her books?
I’ve learned from her books about white feminism and how much we could leave people out of the conversation and what makes you a bad feminist and how you can call yourself out, and that that can be okay to make mistakes. You know, she calls herself out on her own blind spots, and I think that’s a really important thing to do. I think we bring a lot of ego into activism these days and ego into wokeness. I think that that can sometimes make you afraid of admitting when you don’t know something, and therefore you don’t ask, and therefore you don’t learn. Even someone as brilliant and accomplished and educated as Roxanne Gay, to sometimes owning up to her weaknesses or her blind spots, has been so inspiring so many people that I know, because it makes you feel like it’s okay to just keep learning and if you’re a bad feminist now, it doesn’t mean you’ll always be a bad feminist.
We’re having a lot of conversations in the office about the kind of energy that we’re bringing into 2019. How would you describe the energy you’re bringing into this year?
It’s make space, don’t take space. That’s the thing that I’m gonna bring into 2019, is making sure that I create space for other women. I create space for people from minorities, and people who are living in experiences that I have not myself had to live through. Recently I turned down a role of a deaf woman, because even though I used to be deaf as a child, I’m no longer completely deaf. And so that role should go to someone who still currently cannot hear because there’s a brilliant deaf actress out there somewhere who we don’t know her name, but she can’t get the role. I do think it’s really important to start to make sure that we stop being greedy and we just step aside for one another, and don’t fear each other. We’ve been taught to fear each other by men, and feel like there’s only space for one, and that’s a lie. That’s so that we don’t all join together and take up loads of space and become equal. So supporting other women, making sure that I put my money where my mouth is, and pass the mic.
Source: Elle
0 notes
Text
Living with Depression

By Nancy Boutot, Manager, Financial Empowerment, National Disability Institute
“Do not confuse my bad days as a sign of weakness...those are actually the days I am fighting my hardest.”
(Quote: healthyplace.com)
Revealing at age 50 that I am a person living with clinical depression is something I have been thinking about for over a year… perhaps close to two. There was something about turning 50 that made me think enough is enough. I have advocated for people with disabilities, literally, my entire life, yet I certainly was not advocating for myself. In fact, I was diagnosed in my very early twenties and have been living with my disability for about 30 years. Hiding it from most. What kind of a hypocrite was I?
There should be no shame in having a mental illness.
I have good days, great days, wonderful days, and luckily I have a lot of them. That’s how most people know me. Friendly, cheerful and, dare I say, occasionally witty? I also have bad days, but other than those closest to me, you will not know me on those days. You will not see me when I am too depressed to get out of bed, or brush my teeth or take a shower. You will not see me when I’ve been crying excessively. You will not talk to me when I’m anxious about being depressed, when I can’t make plans because I just don’t know what the next day holds. I won’t let you see ‘me.’ Or should I say, I used to not let you see me.
Now I do. I was tailgating at a football game once and someone said “Nancy, it is always nice to see you, you have such a positive attitude!” When situations like that arose, I used to think to myself, ‘If you only knew the real me,’ but I have learned to not say that to myself because that person with a positive attitude is the real me too!
Let me share some information with you: Millions of Americans have depression. According to the Centers for Disease Control (CDC), one in 10 adults (defined as 18 and over) are depressed at any given time, and women, minorities, and those unemployed are most likely to meet the criteria of major depression. So why, with millions of Americans experiencing depression, does it still have such a negative stigma? When we hear about horrible things on the news, why does the topic of mental health immediately arise? According to a report in the Huffington Post in 2016, the news media disproportionately links mental illness and violent behavior.
Depression isn’t just being sad -- it can cause anxiety, severe mood swings, feelings of guilt (for bailing on any number of social activities), discontent, apathy, fatigue, restlessness, irritability… well, you get the point. Several years ago, I was with a small group of friends. I stated that one friend would not be attending due to her depression and not being ‘in the mood’ to socialize. A person in the group made a face and spoke up: “Really? Come on, tell her to just get over it. I don’t get it, sorry.” I was a bit taken back by this declaration, and while I could have said something, I just let it go. Well, sort of. I never got over the feeling that this friend of mine, whom I consider a wonderful friend, would never totally get me, whether I told her about my depression or not. And I never did. Partially because it is simply hard to describe.
How do I tell someone that at times I feel nothing; I have neither happy nor sad feelings, just none? That I can’t see the joy in life some days? That lying in bed feels safe? That I’m tapped, spent, as if all the energy has been sucked out of my body? That I’m not quite the best guest when I can’t concentrate on anything, especially dinner conversation. Believe me, if I could just ‘snap out of it’, I would.
And if I did tell someone, would they want to hear it? When you tell people you have the flu or you broke a bone, you hear words of concern, comfort. When you tell someone you have depression, you hear silence. If I do tell someone, I immediately follow it up with how I have it under control so they do not think I will a) harm myself or b) harm others. It seems to ease them.
Saying to someone who has depression, “What do you have to be depressed about? You have a great life!” is the same thing as saying to a person with asthma: “What do you mean you can’t breathe? There’s lots of air in here!” (#endthestigma)
I will be in recovery from clinical depression for the rest of my life, and part of my recovery is to stop being embarrassed, and to stop pretending that I am always okay. After all, are any of us 100 percent on any given day? No. Recovery can look different for everyone, and what works for me some days may not work for others. One thing that seems to improve my depression is sunlight, and I try to get outside and into the sunlight for at least 10 or 15 minutes every day… more when I feel my body needs it. I seem to do best when I stick to a scheduled routine. I also incorporate some deep breathing exercises into my daily routine. Taking a few minutes to breathe and relax, especially when I start to feel anxious, can be a proactive way to stop that spiral into deep depression. Eating healthy and exercising are good ways to manage my depression, but I’m still working on those! I seem to eat well and do light exercise for a while, but don’t keep up with it on a regular basis like I should. Also, I can’t say enough about talk therapy! Call a friend, laugh, joke, and catch-up!
It is whatever works on any given day. I know my symptoms will never totally go away. But through these techniques, and taking and regulating my medication (thankfully, I’ve been on the same one for about 11 years now), I can live a pretty great life!
So, if you know someone with depression, here are some ways you may be able to be there for them. I say ‘may,’ because everyone is different. And I can only say what works for me.
On a good day, and I must stress good, ask how you can help me on a bad day.
On a bad day, never, and I repeat never, tell me to ‘get over it.’
Ask me what you can do to help, and if I say nothing, then do nothing.
Respect me as a person living with and managing depression.
Learn more about what people with depression deal with… research it, and understand as best you can.
Don’t feel sorry for me. It doesn’t help. Just be there for me.
There are a few resources that I go to on a regular basis, whether it be to find inspiration, tips on managing my depression, or sites where I can go to simply know I’m not alone. Maybe some of these can help someone else too.
RESOURCES
The Mighty is one of my favorites! Real people sharing real stories about a variety of mental health diagnoses, as well as other disabilities and health concerns.
National Alliance on Mental Illness (NAMI): NAMI’s motto is “You Are Not Alone.” They are a great source to find local groups and resources.
1 note
·
View note
Text
Justin Gulliver - phaware interview 322
COVID-19 SPECIAL EDITION: Justin Gulliver is a pulmonary hypertension patient from New Zealand as well as a health social worker primarily working with people who have chronic and long term health conditions. Justin discusses being on both side of the health system in NZ. He also discusses the impact that social distancing is having on his practice in a time of coronavirus. #phaware #COVID19
My name is Justin Gulliver and I live in Wellington, which is in New Zealand. I was diagnosed with pulmonary hypertension in November of 2018, but I’d had some problems, probably symptoms for a lot longer than that. It all started when I was about 11 years old and I got a virus that kept me in hospital for quite a long time. That virus caused some problems to my liver, which turned into portal hypertension about 11 years later. Then over time, that's gradually developed into pulmonary hypertension. Portal hypertension is caused by problems with the liver. Most commonly, it's caused by cirrhosis of the liver, but that's not what I have. It affects the portal vein, which is one of the key veins that connects the liver and the lungs and heart all together. They're not 100% sure for me why that happened, because I actually have a really healthy liver, but it's caused damage to my lungs which is where the pulmonary hypertension comes from. So, officially they call it portal pulmonary hypertension. New Zealand is a pretty small country. There's only about 5 million people on a good day, so that means that the number of people who have pulmonary hypertension is quite low. I think it's kind of about 200 people in the whole country that are known to have it. It's not very well recognized. As with everywhere in the world, it's not easy to diagnose. People aren't automatically looking for it. We have access to most of the same treatments that are available in the rest of the world, but we have some restrictions around how much is funded. So, for the first line therapies, [sildenafil], that's the only one that's easy to access and is funded for New Zealand citizens. The other ones within that same category aren't funded at all. To get them, you have to have special sign off from the doctor and from the government to access them. So, it's quite a different system from what I'm aware of around the world. All of our healthcare is free in New Zealand, so my diagnosis happened on the back of an acute kidney problem, which then led to sepsis and then lead to heart failure. While I was getting ready to have that kidney issue sorted out, that's where they realized that there was something else going on. So, it took an acute illness for me to get diagnosed. But I'd been having tests over probably the previous three years, because I knew that something was wrong, but no one else really understood what I was talking about and the symptoms that I was describing. When I finally got the diagnosis of pulmonary hypertension, I was actually relieved. I'd probably spent three or four years going backwards and forwards to doctors telling them that I thought something was wrong. I work in the health system and I've been able to do a bit of research, so I'd actually heard of pulmonary hypertension before, so I knew about it in relation to portal hypertension. That meant that I was already thinking about pulmonary hypertension, but I couldn't get the tests. When I brought it up with the GPs and the other doctors that I was seeing, I couldn't even count how many specialists I'd seen in that time, they would just dismiss it as a cough. I put on heaps of weight because I couldn't exercise, so they said that I was unfair to overweight. They diagnosed me with asthma at one point. So, there was those kinds of things happening. Once I actually got into hospital, even though it was a really traumatic event, getting really, really sick and almost dying, when they actually said, "You've got pulmonary hypertension," I went, "Yeah, I know, and I'm really relieved to hear you say that finally and get the treatment." I mentioned that I work in the health system in New Zealand. I'm a social worker and I primarily work with people who have cancer, but I also work with people who have long-term chronic health issues. So, I was kind of aware of a lot of the things that go on for people when they get a serious and new diagnosis like this. I guess being a patient in the hospital that I work in was quite a strange experience. There was some really good things about it, that I got a private room and people knew that I was there and they kind of really went the extra mile, because they knew who I was. But there was also the whole everybody knew where I was and they assumed that I understood and knew things that maybe I didn't understand that well. Then we sort of moved into the outpatient setting, whereas going to my assessments and tests and other things, and I realized how tricky and difficult the health system can be for people to navigate without support. Because even as a staff member trying to coordinate my appointments and get information back from doctors and that kind of thing, I found it really, really tough. The doctors were really great in front of me when they were sitting in front of me, but it was those times in between where you didn't have necessarily someone to talk to. In Wellington, where I live, they don't have a nurse specialists for pulmonary hypertension. They don't even have one for respiratory illnesses. So, we didn't have anyone that I could go to directly with questions or problems that I might've been having. I found all of that really hard, especially when I was working with people in the same health environment and advocating for them to have that information. I have a better understanding of what my patients are going through now than I did before, because I've been where they are. It's different because it's a different illness and it's got a different future and trajectory and I'm not going through kind of chemotherapy treatments every week or anything like that. But I understand the limitations that an illness can cause. There's always in the back of your mind that little thing about we don't really know what's going to happen in the future and my life may be shorter than it could have been if I didn't have this illness. So, I think I have a better understanding and I'm able to empathize with my patients there are a lot more than I used to. But I have also had health problems since I was a kid that have assisted me and led me into the work that I do. I've probably become a little bit looser with some of my boundaries than I used to be in the last 18 months or so. But I don't want to give them my problems, so I don't really talk about my own health issues so much, except in my head I can kind of go, "Yeah, I understand where you're coming from." I think sometimes it actually can make it harder, because I can empathize with some of the complaints that they have. Living in New Zealand with such a small number of people with this condition, there isn't a lot of people around and a lot of opportunity to meet with them. We do have a Facebook group, Pulmonary Hypertension New Zealand, which I help to administrate. That's really been a really good connecting place, both for me to hear what other people are going through and to help them, the ones who have come after me as well. One thing that is really great, is that we have a National Center for Pulmonary Hypertension, which some people can go to which is based in Auckland. When I'm up there, I get to meet other patients when we're kind of sitting in the waiting room waiting for our six minute walk test or to see the specialist or whatever we're doing. That's really good because you get to talk to them about their experience, and people seem to want to connect. I think we've found ways of doing that across quite a big distance with quite a small number of people. I think that's really important to connect with people who are like you, because no matter how much you describe to people who aren't going through the same things, they never really understand it. COVID-19 has had a pretty big impact here. We're probably a few weeks behind where the States are at and where some of the other countries are at. But our country has gone into complete lockdown two weeks ago, nearly, and that just means that nobody is seeing anybody. I'm now working from home, which is a bit weird, because I normally would be working at the hospital in the frontlines, but I can't do that because it's not safe for me to do that. That's been quite challenging for me. The approach that our government's taken is that we're completely in lockdown and we're trying to break the chain of transmission, and it's too early to say whether that's working, but we haven't seen the full kind of force of what this could do like some of the other countries that we're watching. We're just all sort of quietly sitting in our lounges hoping that we've done the right things. I think New Zealand is or Kiwis have been pretty responsive. Our prime minister kind of sat down one day and said, "You have to go home and you have to stay there." And we all kind of have. Everyone's just gone, "Yeah, okay, sure. We'll do what you say and we'll try and get through this." Everything's really supportive and there's lots of centralized government advertising about what we're going to do and how are we going to do it and how we are going to be towards each other. We're very lucky, because we probably produce 80% of our consumable goods in New Zealand and we don't have to worry and rely on the rest of the world too much. Our biggest moneymaker is tourism, so we've been heavily affected by that. But our government have gone very much on the caring side where they want us to get through alive and to have as few deaths as possible. Our communities banding together and our supermarkets are still open and helping each other out. I was able to get a priority assistance from my supermarket, which meant they just dropped everything at my door, and I've got extra slots that I can choose from where the general public don't have those. They're looking after us, I think, and they're trying to get everybody through together. The thing that helped me the most [with my diagnosis] was finding places where I could talk to others and hear information about this condition that wasn't so scary, because a lot of the stuff that I first found online, it was all about short life expectancy and all of that sort of stuff. As you go through the process of getting onto the right therapies and working with the doctors, you realize that that's not actually the case anymore. It might've been a few years ago, but it's not so bad now. I think I found that really helpful. My advice, I guess, is seek out good information. Talk to people about what they're going through, and speak up when you're with the doctors. Tell them what you want to know. Don't wait for them to give you the information because they're probably as uncertain as you are. I think the other thing is that I found it really helpful just talking about this with my family and friends, because they don't really understand what it's like and what the physical limitations are. For me, I look fine, so they don't really fully understand all the time what I'm struggling with. Unless I tell them that, they're not going to know. My name is Justin Gulliver, and I'm aware that I'm rare.
Stay up to date with the latest on Coronavirus Disease 2019 at the CDC Website.
Click here for Important COVID-19 Information & Resources for PAH Patients & Caregivers from the phaware website.
Listen and View more on the official phaware™ podcast site
0 notes