#all (h)ours sceanrios
Explore tagged Tumblr posts
Text
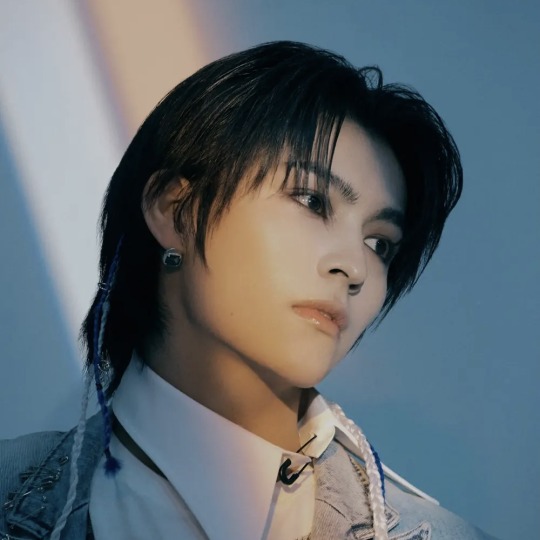


𝐩𝐡𝐨𝐭𝐨𝐬 𝐲𝐨𝐮'𝐯𝐞 𝐭𝐚𝐤𝐞𝐧 𝐨𝐟 𝐲𝐨𝐮𝐫 𝐛𝐨𝐲𝐟𝐫𝐢𝐞𝐧𝐝, 𝐚𝐥𝐥(𝐡)𝐨𝐮𝐫𝐬
will be added as posted
xayden
masami
on:n
#all hours#all (h)ours#all hours masterlist#all (h)ours masterlist#kunho#lee geonho#youmin#cho yumin#xayden#shin jeongmin#minje#kim minje#masami#akiba masami#hyunbin#lee hyunbin#on:n#kim jihwan#all hours imagines#all (h)ours imagines#all hours scenarios#all (h)ours sceanrios#all hours smau#all (h)ours smau#all hours texts#all hours fluff#all (h)ours fluff#all hours x reader#all (h)ours x reader#all hours social media au
7 notes
·
View notes
Text
Engineered Protein Adhesive Gel as an Osteo Conductive Material for Bone Healing Abstract The present study explores the bone fracture repairing efficacy of an engineered protein in detail. Engineered protein prepared using phenolic acids and gelatin demonstrated adhesive property under in-situ condition while subjected to oxidation. The experimental groups include control and sample treatment and all the experiments were conducted in Albino rats in Tibia. Followed by the fracture, the glue was applied and subjected to casting. Healing or rejoining of bone was assessed using X-ray, SEM and H&E sectioning of repaired bone tissue at zero and 30th day. Results revealed that engineered protein supports bone fracture repair at faster rate compared to control. Both SEM and H&E sections also corborates well with the repairing pattern observed. The presence of minerals and the in-situ gelation property of the engineered protein promote the repair as expected. Keywords: Bioadhesive; Hydrogel; Gelatin; Caffeic acid; Fracture bone repair Go to Introduction The current sceanrio in the development of health care materials introduced numerous biological materials [1,2]. Most of the biological materials target skin and wounds and only few materials focused the internal organs [3]. Bone, an important organ and if there is any critical injury or fracture it needs immediate attention. To fix a bone fracture surgeons use metal screws, pins, rods or plates to hold the bones in the place [4]. However, these materials needs to be removed (by another surgery) once the bone got repaired. In recent years, tissue regeneration, an important research area paves a way to have remediation through supporting materials in the form of biomaterials. Since, most of the biomaterials are from synthetic followed by natural, the biocompatibility and immunological issues restrict the benefits [5]. Our recent research on the development of tissue approximation agent for cut wounds demonstrated interested results for both external and internal tissue approximation [6,7]. The tissue approximation agent used in the present study is an engineered protein which under in- situ condition acts as a glue and fix the fracture. Since, there is no biological glue is available for fixing the bone fracture, in the present study, an attempt was made to explore the bone fracture repairing efficacy of the engineered protein glue in small animals models. Go to Experimental Methods Preparation of the PAMG and PAMG-gel Phenolic acid modified gelatin (PAMG) prepared through EDC/NHS chemistry as per the reported literature [6,7]. To prepare PAMG-gel, in brief, 2ml of 16%(w/v) PAMG solution was prepared and treated with 50-100μl of 2%(w/v) sodium meta–periodate. The transformation of PAMG solution to the gel state was termed as PAMG-gel. In-vivo bone healing studies: animal model To access the bone fracture repair efficacy, in the present study we used tibia bone fracture model [8]. All the studies were performed upon Institute ethical approval. Six male albino rats (wistar strain) were segregated into two groups: (i) untreated (Control) and (ii) PAMG-gel treated group. The animals were housed in standard animal cages and fed with pelletized feed and surplus water. The house temperature was maintained at 25 °C with a 12 hour light-dark cycle. The rat was anesthetized by the intra-peritoneal injection of ketamine: Xylazine (60:20mg/kg body weight). The left hind tibia was taken for the bone fracture study. The operative site was dehaired and sterilized with provide on iodine solution. Th bone was fractured using a side cutting diamond disk and high speed micro motor under an abundant irrigation with sterile solution. Experimental animals receiving sample treatment was indented with PAMG-gel on site to fix the fracture and the control animals are left as such by simple fixing. Both the animals groups and the injured skin site was approximated with restorable sutures and provided with orthopaedic casting. All the animals were undisturbed until the end of the experiment. Upon healing, X-ray imaging was performed to analyze the rejoining efficacy. Further, all the animals were sacrificed and the experimental bone was removed for further SEM and H&E analysis. Go to Results And Discussion In general, bone has an intrinsic healing capacity and it does not require any healing agent to rejoin upon fracture [9]. However, rejoining of bone requires proper guiding and requires additional supporting factors for the faster rejoining and strengthening of the bone. With regard to complex bone fracture repair, conventional screws and plates are not helpful and the patients undergo number of surgery. Rejoining the bone fracture with suitable adhesives of either synthetic or natural origin with high compatibility is always a welcoming idea for the orthopaedic surgeons [10]. However, till now there are no specific adhesives have been designed as per the clinical requirement. Decades before several synthetic adhesive were in the clinical markets and now excluded for its biocompatible and biodegradable properties. Though natural materials like fibrin and gelatin were taken into consideration, the inherent low mechanical property restricts its applications. Our previous report on the mussel mimicking biological adhesives for skin approximation widens the scope, for several other 3 applications [6,7]. PAMG-gel is a composition of gelatin conjugated with phenolic acid. Gelatin, the hydrolyzed form of collagen is an integral protein in bone formation. Reported literature suggests that mechanically stable hydrogel act as osteo conductive materials for bone tissue regeneration [11]. The present study exploits bone fracture repairing efficacy of the PAMG-gel as an inherent osteo conductive protein and as a bone adhesive. Preparation and characterization of the PAMG were discussed in our earlier paper. Further PAMG-gel was prepared by oxidizing the PAMG solution with mild oxidizing agents. The phenolic acids conjugated to the gelatin (From Fish scale collagen) backbone further undergoes Michael's addition reaction to form inter and intra molecular cross linking with the protein and forms a gel like material. This reaction was performed on-site to imitate the approximation the bones and tissues. In-vivo tibial fracture model was performed to access the bone healing efficacy of the PAMG-gel. During the course of the study all the animals remained healthy and observed for 30 days for the complete joining of the bone. At scheduled time interval, the walking pattern and speed of the rat was analyzed physically It has been found that from third week onwards the PAMG- gel treated group can able to give a normal walking posture, whereas for the untreated wound, the walking pattern were not the same as earlier. On, day 30 X-ray imaging was performed for all the rats, from the results (Figure 1) we can able to conclude that the PAMG-gel treated rat shows improved repair pattern on comparing with the untreated group. Though the untreated fractured bone shows the rejoined structure in the X-ray imaging, the morphology of the rejoined bone was different. Further the animals were sacrificed to excise the fractured bone. The ex-vivo images of both the untreated and PAMG-gel treated were shown as a representative image in the Figure 1. The untreated wound shows calcification in the rejoined bone area whereas the PAMG- gel treated wound was very clean and equal to that of that of the normal bone. Further, the SEM images of the ex-vivo bone show a clean repair pattern for the PAMG-gel treated bone, whereas for the untreated bone, due to calcification, the bone appears porous and minor cracks were seen. Similarly, results from the H&E section of the cross sectioned bone shows high porous structure for the untreated group were as for the PAMG-gel treated group shows dense packed bone structure. Click here to view Large Figure 1 Go to Conclusion The present studies evidently proves that in-situ gelation of phenolic acid engineered protein repair bone fracture without any calcification and thus avoid the use of metal screws and plates. For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/ for more details click on the juniper publishers material science
#Juniper Publishers#juniper publishers group#material science#composite materials#biological materials
0 notes