#Nursing Interventions to Prevent Falls In Older Adults
Explore tagged Tumblr posts
Text
#Ligament Doctor in Patna#Knee Replacement Doctor Patna#Common Fracture in Old Age#Complications of Broken Bones in the Elderly#How to Prevent Falls In Elderly#How to Prevent Fractures in the Elderly#Frequent Falls in Middle-Aged Woman#Nursing Interventions to Prevent Falls In Older Adults#Causes of Recurrent Falls In Elderly
0 notes
Text
old age patient care
Old age patient care is a complicated and multidimensional approach that calls for the use of full strategies in addressing the needs of elderly people in terms of health. The care of older adults requires specialized medical attention, holistic support, and individualized interventions in order to provide them with care and quality life. Healthcare Issues in Geriatric Patients Older adults have numerous health problems that require medical attention. Some of the common health issues related to aging include: Hearing impairment Cataracts and vision impairment Chronic pain (back and neck) Osteoarthritis Chronic obstructive pulmonary disease Diabetes Depression Dementia Geriatric Syndromes are highly complex health conditions which characterize older age, often originating from multiple underlying causes. Among them are: Frailty Urinary incontinence Falls Delirium Pressure ulcers Comprehensive Hospital Care Approach Hospitals have developed particular strategies to meet the distinct needs of older patients: Specialized Emergency Department Care Development of geriatric emergency departments with: Geriatric-trained medical staff Specialized equipment Pressure-reducing mattresses Improved lighting and acoustics Interdisciplinary Care Strategies Key elements of good elderly patient care are: Geriatric Interdisciplinary Team Identifies complex patient needs Prevents potential complications Provides comprehensive care Primary Care Nursing Continuous patient monitoring Personalized care planning Patient and family education Communication and Documentation Effective communication among healthcare professionals Detailed medication documentation Prevention of diagnostic and treatment errors Discharge and Continued Care Discharge planning for elderly patients is very complex1: Critical Discharge Planning Components Functional status assessment Management of identified health problems Medication adherence evaluation Caregiver capability assessment Comprehensive follow-up care planning Holistic Care Approaches Preventive and Promotional Strategies The NPHCE in India lists strategic care approaches2: Critical Care Approaches Preventive and promotive care Nutrition management Illness surveillance Medical rehabilitation Healthcare human resource development Interventions at community levels Psychological and social support Effective care of elderly people is not merely medicare: Counseling support Dementia awareness Improvement in skills of caregivers Inter-generational bonding programs Support to mental health Technology and Policy Interventions Government support Pension plans Healthcare policies Welfare schemes Elderly protection Technological intervention Guidance at doorstep level Specific geriatric health-care technologies Comprehensive Rehabilitation Centers Care Principles Suggested Care customized to person Care plan designed individually Patient's unique needs Holistic health management Preventive Approach Health check-ups Early treatment Lifestyle management Comprehensive Care Medical care Psychological care Social interaction Family participation Old age patient care is a multidimensional approach that deals with the physical, psychological, and social aspects of elderly health. With comprehensive approaches, healthcare systems can ensure that older adults are cared for in a dignified manner and with quality.
0 notes
Text
The Importance Of Allied Health Services In Disability And Aged Care

Allied health services play a crucial role in improving the quality of life for individuals with disabilities and the elderly. These services encompass a wide range of health professionals who work in collaboration to provide holistic care, ensuring the physical, mental, and emotional well-being of clients. Whether you or a loved one requires support, understanding the impact of allied health can lead to better health outcomes and enhanced day-to-day living.
What Are Allied Health Services?
Allied health refers to a group of healthcare professionals other than doctors and nurses who provide specialized support. These include, but are not limited to:
Physiotherapists: Assist with mobility, strength, and balance for improved physical function.
Occupational Therapists: Help individuals regain independence in daily tasks through adaptive techniques and equipment.
Speech Pathologists: Aid in communication difficulties, including speech, swallowing, and language issues.
Dietitians: Focus on nutrition and diet to improve overall health, particularly for those with special dietary needs.
Psychologists: Provide mental health support and coping strategies for managing stress, anxiety, and other emotional concerns.
Each of these professionals contributes to a coordinated approach in disability and aged care settings, working together to ensure comprehensive care.
The Role of Allied Health in Disability Support
For individuals living with disabilities, allied health services are invaluable. Physiotherapists can help manage mobility issues, ensuring that individuals can navigate their environment safely. Occupational therapists provide adaptive solutions that enhance independence, allowing clients to perform daily tasks like cooking or dressing with minimal assistance.
Speech pathologists are essential for those with communication barriers, offering tools and techniques to improve interaction with others. Meanwhile, psychologists address the emotional challenges that can arise, such as anxiety or depression, fostering mental well-being through therapeutic intervention.
Allied Health for Aged Care
As we age, our health needs change and allied health professionals play a pivotal role in managing these transitions. Physiotherapy can aid in reducing the risk of falls, maintaining strength, and improving mobility in the elderly. Occupational therapists ensure that homes are adapted for safety, providing modifications that make it easier for seniors to move around and live independently.
For seniors facing communication issues, speech therapy offers solutions for both speech and swallowing difficulties, enhancing the ability to engage with loved ones. Dietitians ensure that seniors maintain proper nutrition, especially when managing chronic health conditions like diabetes or heart disease. Psychologists offer essential support for mental health, helping older adults cope with feelings of loneliness or loss that may accompany aging.
Benefits of Allied Health Services
The integration of allied health services in disability and aged care results in:
Improved independence and mobility.
Enhanced communication and emotional well-being.
Greater confidence in managing daily activities.
Comprehensive care tailored to individual needs.
Whether it’s through rehabilitation, therapy, or preventive care, allied health professionals are integral to fostering long-term health outcomes in both the disabled and aged populations.
Conclusion
Allied health services are an essential component of quality care for both individuals with disabilities and the elderly. By providing specialized support, allied health professionals ensure that clients can lead fulfilling and independent lives. At Disability and Aged Care Services, we are committed to delivering personalized allied health services to meet the unique needs of each client. Explore our range of allied health services and see how we can support your journey toward improved health and well-being.
0 notes
Text
Comprehensive Guide to Elderly Care Therapy Equipment
Caring for the elderly requires a multifaceted approach, combining medical care, emotional support, and therapeutic interventions. One example of the critical components of effective elderly care is the use of specialized therapy equipment. In this blog post, we will explore various types of elderly care therapy equipment, their benefits, and how they can enhance the quality of life for seniors.
Understanding Elderly Care Therapy EquipmentElderly care therapy equipment market encompasses a wide range of devices and tools designed to support the physical, mental, and emotional well-being of older adults. This equipment is used in various settings, including homes, nursing homes, and rehabilitation centers, to aid in mobility, improve cognitive functions, and provide comfort and safety.
Types of Elderly Care Therapy Equipment
1. Mobility AidsMobility aids are essential for seniors who have difficulty walking or maintaining balance. These aids help prevent falls and allow seniors to stand and move around more independently.
Walkers and Rollators: These provide support for walking and often come with seats and storage compartments.
Wheelchairs and Scooters: For those with limited mobility, these aids offer an excellent way to maintain independence.
Canes and Crutches: Lightweight and easy to use, they provide extra stability for those who need minimal support.
2. Physical Therapy EquipmentPhysical therapy equipment helps seniors maintain or improve their physical strength, flexibility, and coordination.
Exercise Bands and Tubes: Used for strength training and resistance exercises, they are versatile and effective.
Balance Boards and Pads: These tools help improve balance and coordination, reducing the risk of falls.
Pedal Exercisers: Compact and easy to use, they help improve cardiovascular health and leg strength.
3. Cognitive Therapy ToolsCognitive therapy tools are designed to stimulate the brain and improve mental functions such as memory, attention, and problem-solving skills.
Puzzles and Brain Games: Engaging activities that help keep the mind sharp.
Memory Aids: Devices such as digital clocks with large displays and reminder alarms can help seniors keep track of their daily schedules.
Interactive Apps and Tablets: Specially designed for seniors, these can offer cognitive exercises and entertainment.
4. Comfort and Safety EquipmentComfort and safety equipment ensures that seniors can live in their homes safely and comfortably.
Adjustable Beds: These beds can be adjusted to different positions, providing comfort and aiding in mobility.
Grab Bars and Handrails: Installed in bathrooms and other areas, they help prevent falls.
Lift Chairs: These chairs can help seniors transition from sitting to standing with ease.
Benefits of Using Elderly Care Therapy Equipment
The use of elderly care therapy equipment offers numerous benefits:
Enhanced Independence: Mobility aids and physical therapy equipment help seniors perform daily tasks independently.
Improved Physical Health: Regular use of exercise equipment can lead to better physical health and reduced risk of chronic diseases.
Mental Stimulation: Cognitive therapy tools keep the brain active and reduce the risk of cognitive decline.
Increased Safety: Safety equipment reduces the risk of falls and injuries, allowing seniors to live safely in their homes.

0 notes
Text
Unlocking Potential: The Role and Impact of Occupational Therapy
In the realm of healthcare, one often hears about doctors, nurses, and physical therapists. However, there's a crucial profession that often flies under the radar but plays an essential role in improving people's lives: occupational therapy. Occupational therapy for children in kondapur is a dynamic field dedicated to helping individuals overcome challenges, regain independence, and live life to the fullest. Let's delve into what occupational therapy entails, its significance, and the profound impact it has on individuals across various walks of life.
Understanding Occupational Therapy:
Occupational therapy focuses on enabling people to engage in the activities that are meaningful and necessary for their daily lives, known as occupational therapy for toddlers in kondapur. These activities can range from simple self-care tasks like dressing and grooming to complex skills required for work, leisure, and social interaction.
The Role of Occupational Therapists:
Occupational therapists (OTs) are highly trained professionals who assess a person's physical, cognitive, emotional, and environmental factors that may occupational therapy center for kids in kondapur hinder their ability to participate in daily activities. Through personalized interventions, OTs help individuals develop or regain essential skills, adapt to their environment, and modify tasks as needed to enhance independence and quality of life.
Key Areas of Practice:
Rehabilitation: OTs assist individuals recovering from injuries, surgeries, or illnesses to regain strength, mobility, and functional abilities. They may provide exercises, teach adaptive techniques, and recommend assistive devices to facilitate the rehabilitation process.
Pediatrics: In pediatric occupational therapy, the focus is on helping children develop the skills necessary for school, play, and social interaction. OTs work with children occupational therapist for kids in kondapur with developmental delays, sensory processing disorders, autism spectrum disorders, and other challenges to promote their overall development and independence.
Mental Health: OTs play a vital role in mental health settings by addressing the functional impairments associated with psychiatric conditions such as depression, anxiety, schizophrenia, and bipolar disorder. They assist individuals in managing daily routines, coping with stressors, and improving social skills to enhance their well-being and participation in society.
Geriatrics: With the aging population, there's a growing need for occupational therapy services for older adults. OTs help seniors maintain independence pediatric occupational therapists in kondapur and age in place by addressing issues related to mobility, falls prevention, home modifications, and cognitive decline.
The Impact of Occupational Therapy:
The impact of occupational therapy extends far beyond improving physical functioning. By addressing barriers to participation in meaningful activities, OTs empower individuals to lead fulfilling lives and achieve their goals. Here are some ways occupational therapy makes a difference:
Enhancing Independence: Whether it's learning to perform daily tasks after a stroke or adapting to life with a disability, occupational therapy equips individuals with the skills and confidence to live independently and maintain their dignity.
Improving Quality of Life: OT interventions focus on promoting well-being and a sense of purpose by enabling individuals to engage in activities that bring them joy, fulfillment, and a sense of accomplishment.
Conclusion:
Occupational therapy is a profession driven by compassion, innovation, and a commitment to helping individuals live life to its fullest potential. Whether it's supporting a child with developmental delays, assisting a stroke survivor in regaining independence, or advocating for workplace accommodations, occupational therapists play a pivotal role in transforming lives and building inclusive communities. As the demand for holistic, client-centered healthcare continues to grow, the importance of occupational therapy in promoting health, well-being, and participation in society cannot be overstated
0 notes
Text
How Technology is Revolutionizing Nursing Homecare in Kuwait
Technology is revolutionizing nursing home care in Kuwait by enhancing efficiency, improving quality of care, and promoting the well-being of residents. Here are some ways technology is making a difference:
Electronic Health Records (EHR):
EHR systems streamline documentation, enabling nurses and caregivers to access residents' medical records, treatment plans, and medication histories electronically. EHRs promote accuracy, efficiency, and communication among healthcare providers, ensuring continuity of care and reducing the risk of medication errors or duplications. Remote Monitoring Devices:
Remote monitoring devices, such as wearable sensors, smart beds, and motion detectors, allow nurses to track residents' vital signs, activity levels, and sleep patterns in real-time. These devices provide early detection of health issues, falls, or emergencies, enabling timely interventions and preventive care strategies. Telehealth Services:
Telehealth platforms enable remote consultations between residents and healthcare providers, including physicians, nurses, and specialists, without the need for in-person visits. Telehealth services facilitate access to medical care, monitoring, and follow-up appointments, especially for residents with mobility limitations or chronic conditions. Medication Management Systems:
Automated medication dispensing systems and electronic pill reminders help nurses administer medications accurately and on schedule. These systems reduce medication errors, improve adherence to treatment regimens, and enhance medication safety for residents. Fall Detection and Prevention Technology:
Fall detection devices and alarm systems alert caregivers in real-time when a resident experiences a fall or is at risk of falling. Integrated fall prevention programs utilize predictive analytics and risk assessment tools to identify residents at higher risk of falls and implement personalized interventions to reduce fall incidence. Electronic Communication Tools:
Electronic communication platforms, such as secure messaging apps or video conferencing software, facilitate communication and collaboration among nursing home staff, residents, and family members. These tools enhance communication, coordination of care, and family engagement, fostering a supportive and connected care environment. Robotic Assistance and Automation:
Robotics and automation technologies assist caregivers with tasks such as lifting, transferring, and mobilizing residents, reducing physical strain and injury risk. Robotic companions and assistive devices provide social interaction, cognitive stimulation, and entertainment for residents, promoting emotional well-being and quality of life. Data Analytics and Predictive Modeling:
Data analytics tools analyze large datasets to identify trends, patterns, and predictors of health outcomes among nursing home residents. Predictive modeling algorithms help forecast healthcare needs, anticipate adverse events, and optimize resource allocation for proactive and personalized care delivery. Smart Home Technology:
Smart home systems integrate environmental sensors, smart appliances, and home automation devices to create safe, comfortable, and accessible living environments for residents. These technologies enhance security, energy efficiency, and convenience while promoting independence and autonomy for older adults. By leveraging technology in nursing home care, Kuwait can improve efficiency, quality, and safety while enhancing the overall experience and well-being of residents and caregivers. Ongoing innovation and investment in healthcare technology are essential to address the evolving needs of an aging population and ensure sustainable, person-centered care delivery.
0 notes
Text
Understanding Lip Tie: What You Need to Know

Lip tie, a condition where the upper or lower lip is tightly connected to the gums by a thick or improperly positioned tissue called the frenulum, can lead to various challenges for newborns and adults alike. Despite being less recognized than tongue tie, lip tie affects approximately 11% of newborns. Here's a comprehensive overview of lip tie and its implications.
Defining Lip Tie:
Lip tie refers to the abnormal attachment of the upper or lower lip to the gums due to a shorter or thicker frenulum. This condition is categorized into four levels based on the severity of attachment:
1. Mucosal type (Level 1)
2. Gingival type (Level 2)
3. Papillary type (Level 3)
4. Papilla Penetrating type (Level 4)
Causes of Lip Tie:
Lip tie can occur as a result of various genetic conditions affecting bone and muscle development, such as Oro-facial-digital Syndrome, Ellis-van Creveld Syndrome, and Ehlers-Danlos Syndrome.
Impact of Lip Tie:
The restricted movement of the lips due to lip tie can result in difficulties with breastfeeding, eating, speaking, and oral hygiene. Infants with lip tie may struggle to latch onto the breast and experience challenges in obtaining sufficient nutrition, leading to weight gain issues. Additionally, lip tie can contribute to dental problems like teeth misalignment and cavities.
Signs and Symptoms:
Signs of lip tie in infants include difficulties latching onto the breast, breathing while nursing, making clicking sounds during feeding, and falling asleep during feeding sessions. In older children and adults, symptoms may manifest as gum recession, gaps between front teeth, loss of gum tissue, and crooked or crowded teeth.
Treatment Options:
Pediatric dentists can diagnose lip tie through physical examination and recommend appropriate treatment based on the severity of the condition. Treatment options may include manual therapy techniques, such as lip tie revision for infants, or minimally invasive surgical procedures like frenectomy for severe cases.
In Conclusion:
Recognizing the signs and symptoms of lip tie is crucial for timely intervention and preventing potential complications. Whether it's addressing breastfeeding difficulties in newborns or correcting dental issues in older individuals, seeking professional guidance from a dentist can help manage lip tie effectively and improve overall oral health.
To know more, visit: https://www.sendhildental.com/what-everyone-should-know-about-lip-tie/
0 notes
Text
EBP Nursing Project Ideas: Transforming Healthcare, One Idea at a Time

In the fast-evolving world of nursing, Evidence-Based Practice (EBP) has emerged as a beacon of light, guiding healthcare professionals toward better patient outcomes. It's the practice of integrating clinical expertise with the best available evidence, and it's reshaping healthcare. If you want to embark on an EBP journey, you're in the right place. In this article, we'll explore 49+ innovative EBP nursing project ideas tailored to various niches, ensuring that you not only understand the concepts but also find inspiration for your next big project.
What Is EBP, and Why Does It Matter?
Before we dive into the myriad project ideas, let's clarify what EBP is and why it's essential. Evidence-Based Practice, in essence, is a process that integrates the most relevant research evidence with clinical expertise and patient values and preferences. It's a driving force behind improved patient outcomes, increased patient satisfaction, and more efficient healthcare delivery. EBP ensures that the care provided is not just routine but tailored to each patient's unique needs, backed by the latest scientific evidence.
Now, let's explore EBP nursing project ideas tailored to various niches in simpler and more human terms.
Pediatrics
Child-Friendly Medication Administration: Investigate and implement ways to make medication administration less daunting for children in healthcare settings.
Pediatric Immunization Outreach: Develop evidence-based strategies to increase pediatric immunization rates, ensuring children receive the necessary vaccines for their well-being.
Pediatric Pain Management: Create guidelines for evidence-based pediatric pain management, allowing young patients to cope better with discomfort.
Geriatrics
Falls Prevention in the Elderly: Design and implement a program to prevent falls in elderly patients, enhancing their quality of life.
Dementia Care Excellence: Discover and apply evidence-based practices to improve the care and well-being of elderly patients living with dementia.
Polypharmacy Solutions: Address the challenges of polypharmacy in older adults, suggesting evidence-based methods to reduce medication-related complications.
Mental Health
Suicide Prevention Strategies: Create a mental health program rooted in evidence-based interventions to help prevent suicides and support individuals at risk.
Anxiety Management in Adolescents: Explore proven methods for managing anxiety in teenagers and provide healthcare professionals with tools to assist.
Telepsychiatry Adoption: Investigate the benefits and obstacles of integrating telepsychiatry services into mental health care, making it more accessible.
Maternal Health
Reducing Maternal Mortality: Scrutinize the causes of maternal mortality and suggest EBP solutions to enhance maternal health.
Breastfeeding Support: Provide healthcare professionals with an evidence-based guide on how to support new mothers in their breastfeeding journey.
Postpartum Depression Screening: Develop a protocol for screening postpartum depression, ensuring mothers receive timely support.
Chronic Illness Management
Empowering Diabetes Patients: Create an evidence-based self-management program for diabetes patients, improving their quality of life and minimizing complications.
Controlling Hypertension: Investigate the latest evidence-based strategies for hypertension management and suggest a hypertension control plan.
Chronic Pain Relief: Develop a toolkit for healthcare professionals to navigate evidence-based strategies for chronic pain management, reducing reliance on opioids.
Nursing Education
EBP in Nursing Curriculum: Innovate ways to effectively integrate EBP into nursing education, shaping the nurses of tomorrow into evidence-based practitioners.
Online Learning for Nurses: Explore the effectiveness of online platforms in delivering EBP education and highlight best practices.
Simulated Learning: Discover how simulation can improve EBP skills in nursing students, preparing them for real-world decision-making.
Quality Improvement
Reducing Hospital Readmissions: Develop an evidence-based program to lower hospital readmission rates by enhancing discharge planning and post-discharge care.
Enhancing Patient Safety: Apply EBP to improve patient safety, especially in areas such as medication safety and infection control.
Streamlining Hospital Workflow: Investigate the role of EBP in making hospital workflows more efficient, benefitting both patients and staff.
Infection Control
Hand Hygiene Compliance: Examine methods to enhance hand hygiene compliance among healthcare workers, reducing healthcare-associated infections.
Managing Resistant Pathogens: Develop guidelines for the management of antibiotic-resistant pathogens in healthcare settings, using evidence-based strategies.
Pandemic Preparedness: Create a pandemic preparedness plan based on EBP, ensuring healthcare facilities are well-prepared during crises.
End-of-Life Care
Advance Care Planning: Develop a comprehensive guide on evidence-based advance care planning, ensuring patients' wishes are respected in critical situations.
Palliative Care Best Practices: Explore the latest evidence-based practices in palliative care, enhancing the quality of life for patients at the end of life.
Family-Centered Care at the End of Life: Investigate and recommend evidence-based strategies for involving families in end-of-life care decision-making.
Rural Healthcare
Telehealth in Rural Areas: Explore the role of telehealth in providing evidence-based healthcare services to underserved rural populations.
Community Health Worker Programs: Develop an evidence-based program to train and support community health workers in rural areas, improving healthcare access.
Transportation Solutions: Investigate evidence-based transportation solutions to overcome the barriers rural residents face in accessing healthcare services.
Nursing Leadership
Transformational Leadership: Explore how evidence-based leadership strategies can transform healthcare organizations and enhance patient outcomes.
Conflict Resolution for Nurse Leaders: Develop a guide for nurse leaders on resolving conflicts within healthcare teams using evidence-based techniques.
Nurse Retention Strategies: Investigate and propose evidence-based approaches to retain and motivate nursing staff in healthcare institutions.
Telemedicine and EBP
Telemedicine EBP Guidelines: Create a set of guidelines for healthcare providers to deliver telemedicine services that align with evidence-based practices.
Data Security in Telemedicine: Investigate best practices for securing patient data during telemedicine consultations, ensuring privacy and compliance.
Telemedicine for Specialized Care: Explore the potential of evidence-based telemedicine solutions for delivering specialized care in remote areas.
Cultural Competence in Nursing
Culturally Competent Care: Develop a training program for nurses to provide culturally competent care by incorporating evidence-based cultural sensitivity.
Addressing Language Barriers: Investigate the impact of language barriers in healthcare and propose evidence-based language assistance solutions.
Promoting Inclusive Policies: Examine and recommend evidence-based policies to promote inclusivity in healthcare settings.
Patient Advocacy
Patient Advocacy Training: Create a training program for healthcare professionals to advocate for patients' rights and needs using evidence-based approaches.
Navigating Healthcare Systems: Develop a guide to help patients and their families navigate complex healthcare systems using evidence-based strategies.
End-of-Life Decision Advocacy: Investigate and suggest evidence-based approaches for healthcare professionals to support patients and families in making end-of-life decisions.
Technology and EBP
Optimizing Electronic Health Records (EHR): Explore ways to optimize EHR systems using evidence-based customization for improved efficiency and accuracy.
Wearable Health Technology: Investigate the role of wearable technology in evidence-based health monitoring and patient engagement.
Artificial Intelligence in Healthcare: Examine how AI can be integrated with EBP to enhance diagnostic accuracy and treatment planning.
Ethical Dilemmas in EBP
Informed Consent Challenges: Investigate ethical challenges related to informed consent in EBP research and propose solutions to ensure patient autonomy.
Resource Allocation Dilemmas: Examine the ethical implications of resource allocation in healthcare and how EBP can guide fair decisions.
Conflict of Interest in Research: Explore the impact of conflicts of interest on EBP research and recommend safeguards for research integrity.
Implementing EBP in Small Hospitals
Scaling Down EBP in Smaller Settings: Develop a framework to implement EBP in smaller healthcare facilities with limited resources and staff.
Overcoming Barriers to EBP Adoption: Investigate the common barriers small hospitals face when embracing EBP and propose practical solutions.
Measuring EBP Outcomes: Explore methods for assessing and demonstrating the positive impact of EBP initiatives in smaller healthcare settings.
Conclusion
In this exploration of EBP nursing project ideas, we've covered an array of topics that cater to diverse niches within the healthcare field. EBP isn't just a concept; it's a practice that can elevate the quality of healthcare worldwide. By choosing a project that resonates with your passion, you can make a significant difference in patient care and healthcare outcomes. Whether you're a seasoned healthcare professional or a budding nurse, there's an EBP project idea waiting for you. The future of healthcare is evidence-based, and you can be a part of it.
So, pick an idea, gather your evidence, and start your journey to transform nursing practice. Make a lasting impact on healthcare, one evidence-based project at a time.
1 note
·
View note
Text
Approaching a Patient with Altered Mental Status: The Three D's
Dementia is a chronic confusional state that develops slowly, over months to years.
Delirium is an acute disturbance in consciousness and perception with an underlying medical etiology.
Depression is primarily a mood disorder but can present as confusion in older adults.
More about delirium
Delirium affects approximately 30% of hospitalized older adults who normally live in the community. This number rises to 65% among hospitalized older adults who are admitted from nursing homes. The incidence of delirium in patients admitted to the ICU is even higher.
The incidence of delirium in the hospital depends on both the baseline vulnerabilities of the patient and precipitating factors that occur during the hospitalization. For example, a patient who is highly functional and living independently in the community is much less likely to develop delirium than a patient who resides in a nursing home with dementia, even if the patient experiences the same acute changes, such as infection or new medications.
Risk Factors for Delirium
Baseline vulnerabilities that predispose an older adult to develop delirium during hospitalization can be categorized as follows:
Functional status prior to hospitalization:
-Advanced age (>65 years)
-Diminished activities of daily living
-Immobility
-Pain
-Sensory impairment (visual or hearing)
Cognitive impairment:
-Dementia
-Psychiatric disorder
-Sleep deprivation
Substance use disorders
Nutrition:
-Malnutrition
-Dehydration (which may present as a high BUN:creatinine ratio)
Other medical comorbidities:
-Co-morbid illness (e.g. chronic kidney disease, end stage liver disease)
-"High-risk" medication use
-Admission to the ICU
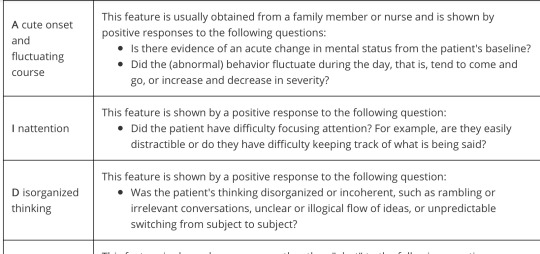
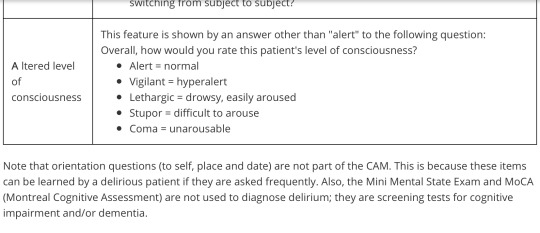
The Confusion Assessment Method (CAM) is a simple tool developed for hospitalized older adults to diagnose delirium and differentiate it from dementia and depression. For a diagnosis of delirium, the first two items and either the third or fourth item must be present. You can remember the four items of CAM by their first letters (A-I-D-A).
Assess item 1 with information from others. Nurses and family members are a good resource for this as they often spend more time at the bedside than we do.
Assess items 2, 3, and 4 when taking history.
Medications that act on the central nervous system (either directly or as a side effect) commonly cause delirium in older adults. These include:
-benzodiazepines (e.g. lorazepam)
-zolpidem
-opioids (e.g. morphine or hydrocodone)
-anticholinergics (e.g. promethazine, diphenhydramine, a.k.a. Benadryl)
-corticosteroids
Antihypertensives which act centrally, such as the alpha-2-agonist clonidine, can also cause sedation and delirium.
Some antibiotics, especially the fluoroquinolones (e.g. ciprofloxacin), cause delirium.
Hypoactive delirium, where patients tend to sleep more, tends to be overlooked, as opposed to hyperactive delirium, where patients are often disruptive.
Sequelae of Delirium
Patients who develop delirium in the hospital have a two-fold increase in their one-year mortality, independent of their underlying medical problems. They also require longer hospitalizations and are more likely to require institutionalization on discharge.
Although delirium often improves with treatment of the underlying cause, observational studies have found that a significant proportion (up to 31.6% in the study by McCusker, et al. cited below) of patients with hospital-acquired delirium have persistent symptoms at 6-12 months after discharge. These patients have also been found to be at higher risk for persistent cognitive impairment and development of dementia than similar hospitalized patients who do not develop delirium.
Patients with a hypoactive (decreased level of alertness) delirium are at increased risk for developing pressure ulcers, pulmonary emboli and aspiration pneumonia.
Patients with a hyperactive delirium may try to get out of bed unassisted, and barriers such as IV poles and urinary catheters may cause them to fall. This may result in injury, further lengthening their hospitalization and increasing the level of assistance they require on discharge. Multifaceted interventions can reduce the number of falls in hospitals. In a cluster randomized trial of over 10,000 patients, a fall prevention tool kit consisting of fall risk assessment, fall prevention plan, bed poster alert, and patient and family education resulted in a fall rate of 1.7% in the control group vs 1.3% in the intervention group (p=0.02, NNT 250).
Patients who are confused may not be able to reliably report their symptoms. Patients who are somnolent with their delirium may not eat properly or take their oral medications. Patients may remember their confusion and be frightened by it, causing symptoms of post-traumatic stress disorder. Family members may also become anxious when they perceive that their relative is "acting crazy."
A chemistry panel with electrolytes, glucose, and BUN/creatinine should be included when evaluating any patient with delirium because they will identify most electrolyte abnormalities (including hyper- and hyponatremia and hypercalcemia), renal failure, and hyper- or hypoglycemia. A CBC is also indicated to evaluate for inflammation, infection, or post-operative anemia, although it is important to recognize that older patients may have a normal white blood cell counts during an infection.
1 note
·
View note
Text
Quantum Leap - Season Two Review

"He works in mysterious ways."
While still formulaic, season two is much better than the brief leap-of-the-week season one. Scott Bakula and Dean Stockwell are a lot more comfortable with their roles, and many of the leaps are more interesting and complicated. There are also some intriguing additions to what we know about our main characters and some progress with the arc story — particularly in the premiere and the finale.
What works
Sam is enjoying leaping around and helping people. He doesn't seem to mind that he left his own life behind, although the continuing partial amnesia could be responsible for that.
Another issue they begin to address in season two is what became of Sam's physical body. In season one, the saga sell says that Sam "stepped into the quantum accelerator and vanished." In season two, we're told that Sam's physical body is in a "waiting room" back at the project, and that when he leaps, Al questions whoever just leaped into Sam's body so that he can locate where and when Sam went.
The best episodes of season two are the premiere and the finale.
2.1 "Honeymoon Express (April 27, 1960): I love this episode, mostly because of the cleverness of the twist ending. Al, whom we learn here is an admiral, is testifying before a hostile senate subcommittee responsible for further funding of the Quantum Leap Project, while Sam leaps into a cop who is on his honeymoon. Sam's bride, Diane, is a law student who is preparing for her bar exam.
Although it was mentioned in the season one pilot that God might be responsible for what is happening to Sam, here it is confirmed. Because Sam virtuously avoids hitting the sheets with Diane even though he is attracted to her, he keeps trying to help her study for the bar instead. At the very moment when Sam is ready to give in and make love with Diane, she has a breakthrough, finally grasping a key legal concept that would have made her fail the exam, and Sam leaps out. At that moment, the grumpy male head of the senate subcommittee turns into Diane, thirty years older, and she tells Al that the Quantum Leap funding has been approved. Only Al is aware that anything has changed.
Two of my other favorite shows had finales that centered on the existence of God, which didn't make me happy because it felt like a cop out. Not Quantum Leap though, because honestly, the only possible explanation for what is happening to Sam is divine intervention.
The only problem I have with this episode is the multitude of smoochfests. I did like that Sam and Al discussed the moral implications of Sam having sex with Diane, even though she wouldn't have known because she believed Sam was her husband. I also like the implied feminist message that Diane is no one's possession, and that she was destined for great things.
2.22 "M.I.A. (April 1, 1969)": Sam leaps into a San Diego cop. Al tells Sam that the purpose of the leap is to convince a Navy nurse named Beth Calavicci to not give up on her M.I.A. husband, who has been imprisoned in Vietnam for two years. But as it turns out, Sam is there to save the life of another cop, his partner, Roger Skaggs (Jason Beghe).
This episode features an exceptional and moving performance by Dean Stockwell, who ripped my heart out in the last ten minutes. Al is clearly signaling confusion and distress throughout the episode; he describes to Sam the torturous confinement that Beth's husband is experiencing without revealing that it is himself who is enduring it. When Sam guesses correctly that Skaggs is the reason for the leap, not Beth, Al confesses that Beth is his first wife and the love of his life, and when she had him declared dead and remarried, Al never recovered, and his other marriages never worked.
"God" allows Sam a few extra minutes before leaping so that Al can say goodbye to Beth, even though, of course, she can't see or hear him. He tells her how much he loves her, begs her to wait for him when we know she won't, and then they dance to Beth's favorite song. The thing is, what happens with Beth explains everything we need to know about Al, and it turns him from Sam's supportive friend and occasional comic relief into a tragic figure. Susan Diol as Beth Calavicci also does a wonderful job. We can believe she is the love of Al's life, that she is incredibly special to him, and her conflict is so well done. Sam's gentle treatment of Al, even though Al misled him and nearly caused Skaggs' death, is also touching. This episode never fails to make me cry.
The music replacement controversy, particularly regarding the episode "M.I.A."
As I mentioned in my review of season one, when Quantum Leap was initially released on DVD way back when, Universal had neglected to get the rights to a number of the songs featured on the series, simply because it was prohibitively expensive. Changing the music changes the series, and the fans were, to put it mildly, livid about it. Although the music replacement had a serious detrimental effect on "Good Morning, Peoria," the worst offender was "M.I.A." because that final scene where Al says goodbye to Beth is framed by the Righteous Brothers' "Unchained Melody" and Ray Charles' "Georgia," two memorable songs that truly cannot be replaced.
Netflix and Amazon have the original version of "M.I.A." Hulu does not. For what it's worth.
Other episodes of note
2.2 "Disco Inferno (April 1, 1976)": Not really notable, but if you're watching Quantum Leap on Hulu or Netflix, you've probably noticed that this episode is missing. I went to the trouble of buying it on Amazon because I'm hung up on that completion thing, and it's not worth it. "Disco Inferno" is about a stuntman who helps his younger brother defy their stuntman father and become a musician. The only important piece of it is that Sam remembers that he has an older brother named Tom who died fighting in Vietnam.
2.4 "What Price Gloria? (October 16, 1961)": This episode is notable because it is the first time that Sam leaps into a woman, so of course it goes the preachy route and is all about sexism. Al is hot for Sam in a woman's body, which I just found uncomfortable. What I liked most was Scott Bakula wearing women's clothing without making too much of a thing about it. It feels like for Bakula, it's just another costume and he's such a good actor that playing a woman doesn't throw him.
2.6 "Good Morning, Peoria (September 9, 1959)": I loved this episode; it was a lot of fun. Maybe it because the stakes were less life and death and more personal. Patricia Richardson does such a great job as Sam's love interest, and the romance actually works this time. It also features a lot of great old music, and Sam pretty much channeling Robin Williams in Good Morning, Vietnam.

Like "Honeymoon Express," the question of Sam having a physical relationship while he is in someone else's body is again addressed. Sam is uncomfortable about romancing Patricia Richardson's character, but he does it anyway and it turns out that it was the right thing to do.
2.8 "Jimmy (October 14, 1964)": Sam leaps into a young, developmentally disabled man who is trying to hold down his first job while encountering bullying and prejudice. The most interesting thing about this one is Sam starts acting differently, clumsily, because he is being treated that way. Possibly a little preachy, but very well done.
2.10 "Catch a Falling Star (May 21, 1979)": Quantum Leap does Man of La Mancha, with the great actor and singer John Cullum as a guest star. This episode is pretty much an excuse to have Scott Bakula sing show tunes onstage and romance his teenage crush music teacher, but there's nothing wrong with that. There was also a deeper meaning when you think about it, because Sam really is like Don Quixote, spending his life rescuing others. Wonderful episode.

2.18 "Pool Hall Blues (September 4, 1954)": Loved this one. Maybe because Sam is so convincing as an adult woman's grandfather (loved the costume). I also loved the laser lines that allowed Sam to be a brilliant pool player.
What doesn't work
I don't usually point out the badness of bad episodes, but these three are truly awful.
2.11 "A Portrait for Troian (February 7, 1971)": We have a haunting, a mysterious lake full of bodies, a vanishing housekeeper and a pointless romance, none of which work. Which is too bad, since it stars Deborah Pratt, who was a writer/producer of the series, the saga sell narrator, and later the voice of Ziggy.
2.16 "Freedom (November 22, 1970)": Another poorly written stinker about an elderly Native American who wants to go home to die. See rule five.
2.17 "Good Night, Dear Heart (November 9, 1957)": This time Sam is a mortician who solves a murder instead of preventing one, which makes absolutely no sense to me. The circumstances of the victim's life and demise are depressing, and it all seems incredibly pointless.
Bits and pieces:
-- "Sea Bride" featured the Queen Mary, which is a tourist attraction in Long Beach, California. I toured it twice and I always enjoy stumbling over stuff that was filmed there.
-- I particularly liked that his second leap into a woman's body ("Another Mother") had nothing to do with sexism; he was there to save his host's son.
-- Famous people: The Beatles and Chubby Checker. In fact, it's the real Chubby Checker, who did a cameo in "Good Morning, Peoria."
-- Notable actors: Lorne Greene (Bonanza), a teenage Kelli Williams (Lie to Me), Robert Duncan MacNeill, Marcia Cross, and Troian Bellisario when she was still a very little girl in "Another Mother."
-- Sam's hair is way too long at first, and is later a good bit shorter. But if he's in someone else's body, can he even get his hair cut? Maybe someone cut Sam's hair in the Waiting Room.
-- Small children and animals can see Al, and genuine psychics can sense his presence. Al's presence affects EMF.
-- Sam creates the Heimlich maneuver.
-- More about Sam: he was a child prodigy, not a surprise, and a concert pianist.
-- More about Al: he was an astronaut. His mother abandoned him when he was a child and his sister was disabled. Al also looks better in red than in green.
-- The cliffhanger endings referencing Sam's next leap still bother me. Especially when we get one that relates to a rerun.
To conclude
I haven't finished my rewatch yet, but "M.I.A." and the two-parter that starts season three are my favorite episodes of the series,
Billie Doux loves good television and spends way too much time writing about it.
#Quantum Leap#Sam Beckett#Al Calavicci#Scott Bakula#Dean Stockwell#Quantum Leap Reviews#Doux Reviews#TV Reviews#something from the archive
7 notes
·
View notes
Text
Prevention of falls, malnutrition, and pressure ulcers in older adults

Prevention of falls, malnutrition and pressure ulcers is important among frail older persons. Assessment scales are suggested to be useful tools when screening for risks. A systematic way to perform preventive work can improve quality of care. The assessment scales do not fully reflect the reality of residents in nursing homes.There is no structure for learning from the results of the assessments and the performed interventions. Older persons who receive home help could benefit from a more comprehensive and structured preventive work. Abstract A structured and systematic care process for preventive work, aimed to reduce falls, pressure ulcers and malnutrition among older people, has been developed in Sweden. The process involves risk assessment, teambased interventions and evaluation of results. Since development, this structured work process has become web-based and has been implemented in a national quality registry called ‘Senior Alert’ and used countrywide. The aim of this study was to describe nursing staff’s experience of preventive work by using the structured preventive care process as outlined by Senior Alert. Eight focus group interviews were conducted during 2015 including staff from nursing homes and homebased nursing care in three municipalities. The interview material was subjected to qualitative content analysis. In this study, both positive and negative opinions were expressed about the process. The systematic and structured work flow seemed to only partly facilitate care providers to improve care quality by making better clinical assessments, performing team-based planned interventions and learning from results. Participants described lack of reliability in the assessments and varying opinions about the structure. Furthermore, organisational structures limited the preventive work. Keywords: falls prevention, home care, nursing care of older people, nursing homes, nutrition, risk assessment
References
Lannering, C., Ernsth Bravell, M., & Johansson, L. (2017). Prevention of falls, malnutrition and pressure ulcers among older persons - nursing staff’s experiences of a structured preventive care process. Health & Social Care in the Community, 25(3), 1011–1020. https://doi.org/10.1111/hsc.12400
1 note
·
View note
Text
Nutrients with Malnutrition-Sarcopenia- Juniper Publishers
Abstract
Prevention of age-related losses in muscle mass and strength is key to protecting physical capability in older age and enabling independent living. To develop preventive strategies, a better understanding is needed of the lifestyle factors that influence sarcopenia and the mechanisms involved. Existing evidence indicates the potential importance of diets of adequate quality, to ensure sufficient intakes of protein, vitamin D, and antioxidant nutrients. Although much of this evidence is observational, the prevalence of low nutrient intakes and poor status among older adults make this a current concern. However, as muscle mass and strength in later life are a reflection of both the rate of muscle loss and the peak attained in early life, efforts to prevent sarcopenia also need to consider diet across the lifetime and the potential effectiveness of early interventions. Optimizing diet and nutrition throughout life may be key to preventing sarcopenia and promoting physical capability in older age.
Introduction
Sarcopenia is a syndrome characterized by progressive and generalized loss of skeletal mass and strength with a risk for adverse outcomes such as physical disability, poor quality of life, and death [1-4]. It is a multifactorial process where nutrition, hormonal factors, lifestyle, and diseases exert an important role [5]. Apart from that, age-related loss of muscle mass is characterized by a 3% to 8% decline per decade after the age of 30y, with a further decline in adult’s >60y of age [6]. Epidemiologic data suggest that the prevalence of sarcopenia varies widely, depending on the population studied, sex, age, settings, and the diagnostic criteria used [4]. The prevalence of sarcopenia in nursing homes, according to the European Working Group on Sarcopenia in Older People (EWGSOP) criteria [7], is between 17 and 40.2% [5,8-12].
Sarcopenia and malnutrition are both commonly happening conditions in older adults. Both entities result in numerous and substantial negative outcomes to the patients and the health care system, including decreased quality of life and functionality, and increased health care costs, hospitalization rates, morbidity and mortality [13]. Their clinical affect and the high direct and indirect costs input the need for health care systems to focus on these syndromes [14,15].
Food intake falls by around 25% between 40 and 70 years of age [16]. In comparison with younger ages, older adults eat more slowly, they are less hungry and thirsty, consume smaller meals, and they snack less [16]. The mechanisms for the "anorexia of ageing” are not fully understood but there may be a person of physiological, psychological, and social factors that influence appetite and food consumption, including loss of taste and olfaction, increased sensitivity to the satiating effects of meals, chewing difficulties, and impaired gut function [16,17]. These changes are compounded by the effects of functional impairments that impact on the ability to access and prepare food, psychological problems such as depression and dementia, as well as the social effects of living and eating alone. Low food intakes and lacking in variety and interest diets put older people at risk of having inadequate nutrient intakes [18]. Thus in a serious of cause and effect , declining muscle strength and physical capability in older age may increase the risk of poor nutrition, and poor nutrition may contribute to further declines in physical capability.
In the ageing and sick population malnutrition that has been seen in hospitals, residential care and in the community [19-21]. Prevalence rates have been estimated for the general hospital population to be between 11% to 44%, but this rises in elderly groups to 29%-61% [19]. Malnutrition is not an inevitable side effect of ageing, but many changes associated with the process of ageing can promote malnutrition [22]. For example, ageing is frequently associated with decreases in taste acuity and smell, deteriorating dental health, and decreases in physical activity, which may all affect nutrient intake [23]. Any change in nutrient intake can lead to malnutrition with its potentially serious consequences. Many studies have found a direct relation between the degree of malnutrition and increased length of stay, treatment costs, and re-admission to hospital rates [24-26]. Therefore the treatment and prevention of malnutrition, which is most common in the older age group, is an important challenge for the health care system.
Nutrients Influence on Sarcopenia and Malnutrition
There are two consequences of cause older age for muscle mass and strength. Firstly, lower energy intakes, if not matched by lower levels of energy expenditure, lead to weight loss, including a loss of muscle mass [4]. Secondly, as older people consume smaller amounts of food, it may become more difficulty for them to meet their nutrient as they needs-particularly for micronutrients. For older people with low food intakes, this highlights the importance of having diets of adequate quality. Although the importance of adequate nutrition has been recommend for a long time, its contribution to muscle mass and strength has not been studied extensively and much of the research in this area is relatively new [27]. A number of interventions have been researched,people can be provided of nutritional supplementation with specific nutrients [28-30]. The nutrients that have been most consistently linked to sarcopenia and frailty in older adults are vitamin D, protein, and a number of antioxidant nutrients, that include carotenoids, selenium, and vitamins E and C [27]. However, there is also some evidence that variations in long-chain polyunsaturated fatty acid status may have important effects on muscle strength in older people [30].
Protein and Vitamin D
Protein is considered a key nutrient in older age [31]. Dietary protein provides amino acids that are needed for the synthesis of muscle protein, and importantly, absorbed amino acids have a stimulatory effect on muscle protein synthesis after feeding [32]. There is some evidence that the synthetic response to amino acid intake may be less in older people, particularly at low intakes [31], and when protein is consumed together with carbohydrate [33]. Recommended protein intakes may, therefore, need to be raised in older people in order to maintain nitrogen balance and to protect them from sarcopenia muscle loss [31].
There is currently no consensus on the level to which dietary protein requirements change in older age, there is an insufficient protein intake may be an important contributor to impaired physical function. Aging and Body Composition Study, a greater loss of lean mass over 3 years, assessed using dual-energy X-ray absorptiometry, was found among older community-dwelling men and women who had low energy-adjusted protein intakes at baseline [34]. Protein and/or amino acid supplementation should, therefore, have the potential to slow sarcopenia muscle loss. However, the amino acid supplementation has been shown to increase lean mass and improve physical function [35], other trials have not been successful [33,36]. Further need to work, including longer-term trials, is needed to define optimal protein intakes in older age [33].
An association between vitamin-D-deficient osteomalacia and myopathy has been identified for many years [37], but the role of vitamin D, and the extent to which it has direct effects on normal muscle strength and physical function remains controversial [38]. The potential mechanisms that link vitamin D status to muscle function are complex and include both genomic and no genomic roles [37,39]. The vitamin D receptor (VDR) has been isolated from skeletal muscle, indicating that it is a target organ [37], and polymorphisms of the VDR have been shown to be related to differences in muscle strength [40]. At the genomic level, binding of the biologically active form of the vitamin (1, 25-dihydroxyvitamin D) results in enhanced transcription of a range of proteins, including those involved in calcium metabolism [37]. The no genomic actions of vitamin D are currently less well understood [39].
Much of the epidemiological literature is consistent with the possibility that there are direct effects of vitamin D on muscle strength. For example, among men and women aged 60 years and older, low vitamin D status (serum 25-hydroxyvitamin D <15ngmL-1) was associated with a fourfold increase in risk of frailty [24,41], and in a meta-analysis of supplementation studies of older adults have showed that supplemental vitamin D (700-1000IU per day) reduced the risk of falling by 19%. However, the evidence is not always consistent as some research studies find no association between vitamin D status and physical function, and supplementation studies have not always resulted in measurable improvements in function [12,21]. In a review of published studies, discuss the reasons for due to methodological differences, including a lack of consideration of confounding influences in some studies. Further evidence is needed, particularly as vitamin D insufficiency is common among older adults [38,41].
Antioxidant Nutrients and Polyunsaturated Fatty Acids (PUFAs)
There is increasing interest in the role of oxidative stress in a etiology of sarcopenia, and markers of oxidative damage have been shown to predict impairments in physical function in older adults [42]. Damage to biomolecules such as DNA, lipid, and proteins may occur when reactive oxygen species (ROS) are present in cells in excess. The actions of ROS are opposite effect to musicaldamaged by antioxidant defense mechanisms that include the enzymes superoxide dismutase and glutathione peroxidase, as well exogenous antioxidants derived from the diet, such as selenium, carotenoids, tocopherols, flavonoids, and other plant polyphenols [32-42]. In older age, an accumulation of ROS may lead to oxidative damage and contribute to losses of muscle mass and strength [32].
A number of observational studies have shown positive associations between higher antioxidant status and measures of physical function [27]. Importantly these associations are seen both in cross-sectional analyses and in longitudinal studies, such that poor status is predictive of decline in function. There are higher plasma carotenoid concentrations were associated with a lower risk of developing a severe walking disability over a follow-up period of 6 years among older men and women, after taking substances of antioxidant nutrients that included level of physical activity and other morbidity, the odds ratio was 0.44 (95% CI 0.27-0.74)[43]. Inverse associations have also been described for vitamin E and selenium status and risk of impaired physical function [27]. There have been few studies of older adults to determine how antioxidant supplementation affects muscle strength, and the benefits of supplementation remain uncertain [44]. Since ROS have both physiological and pathological roles, interventions based on simple suppression of their activities may be unlikely to improve age-related declines in muscle mass and function [45]. However, low antioxidant intakes and status are common [46], and this remains an important question to be addressed.
Sarcopenia is increasingly identified as an inflammatory state driven by cytokines and oxidative stress [47]. Since eicosanoids derived from 20-carbon polyunsaturated fatty acids are among the mediators and regulators of inflammation [30], this raises the possibility that many of different types oils in intake of n-3 and n-6 PUFAs, and their balance in the diet, could be of importance. In particular, n-3 PUFAs have the potential to be potent anti-inflammatory agents [30]. There is some observational evidence to support an effect of n-3 LCPUFA status on muscle function, as higher grip strength was found in older men and women who had greater consumption of oily fish [48]. Consistent with this finding, a number of studies of patients with rheumatoid arthritis have shown that supplementation with fish oil resulted in improved grip strength [30]. In a recent randomized controlled trial, supplementation of older adults with n-3 PUFA (eicosapentaenoic and docosahexaenoic acids) resulted in an enhanced anabolic response to amino acid and insulin infusion. These novel data suggest that the stimulation of muscle protein synthesis by n-3 LCPUFA supplementation could be useful for the prevention and treatment of sarcopenia [49], further evidence is needed to establish the nutrition care process for potential of n-3 PUFAs in inflammatory conditions [30].
Foods and Dietary Patterns
One problem with the existing evidence base is that dietary components are often highly correlated with each other. This may help to explain why the effects of supplementation with single nutrients may be less than that predicted by the research evidence. It also means that from researchable data it may be difficult to understand the relative importance of the influences of different nutrients on sarcopenia. For example, with an antioxidant nutrient such as p-carotene may be causally related to variations in physical function, it may also be acting as a marker of other components of fruit and vegetables. Since diets are patterned, high fruit and vegetable consumption may be indicators of other dietary differences which could be important for muscle function, such as greater consumption of oily fish and higher intakes of vitamin D and n-3 LCPUFAs [50]. Having a result that increases in effects of nutrient deficiencies have been identified. To estimated that each additional nutrient deficiency raised the risk of frailty in older women by almost 10% [51]. This emphasizes the importance of the quality of diets of older adults, as well as the quantity of food consumed, to ensure that intakes of a variety of nutrients are sufficient.
Compared with the evidence that links variations in nutrient intake and status to physical function, much less is known about the influence of dietary patterns and dietary quality in older age. "Goodbalance” diets, characterized by greater fruit and vegetable consumption, whole meal cereals, and oily fish, have been shown to be associated with greater muscle strength in older adults [48]. Data from studies of younger adults appear to be consistent with this finding. For example, among women aged 42-52 years, “unhealthy” diets, defined by higher saturated fat intakes and lower fruit and vegetable consumption, were associated with greater functional limitations over a 4-year follow-up period [52]. Benefits of healthier diets and greater fruit and vegetable consumption on physical function in midlife have also been described in women and men study [53,54]. Intervention studies that take a food-based or "balance diet” approach are likely to change intakes of a variety of nutrients and, therefore, have the potential to be more effective than single nutrient supplementation studies in preventing age-related losses in muscle mass and strength.
Diet and Physical Activity
Resistance exercise training interventions have been shown to be effective in increasing muscle strength and improving physical function in older adults [55]. A further issue in understanding a possible protective role for diet in sarcopenia is, therefore, the potential for interactions between diet and exercise, and the extent to which interventions that combine supplementation and exercise training may be more effective than changing nutrient intake alone. The interactive effects of diet and exercise on physical function have been studied most extensively in relation to protein/amino acid supplementation. For example, in consumption of a high protein meal has been shown to increase muscle protein synthesis in older adults by ~50%, combining a high protein meal with resistance exercise increases synthesis more than 100% [56]. However, a number of studies of older adults have failed to show additional benefits of protein/amino acid supplementation on the skeletal muscle response to prolonged resistance exercise training [32,57], and the implications for long-term effects of combined exercise training and high protein intakes are, therefore, not clear [33]. The need for further research-particularly to address the effects of differing quantity and timing of supplementation [56,57]. At present we have limited information into the combined effects of vitamin D supplementation and resistance exercise on muscle strength and function [58].
Lifelong Nutrition and Sarcopenia
Firstly, the health of older people is depend on lifelong experience to a healthy diet and lifestyle [27]. Although there is evidence that healthier eating behaviors are reasonably stable in adult life [59]. The influence of lifelong nutrition on age-related changes in muscle mass and strength has been little studied, but in terms of interventions to delay or prevent sarcopenia in older age, there may be key factors earlier in the lifetime that need to be identified. A second consideration is that muscle mass and strength achieved in later life are not only determined by the rate of muscle loss, but also reflect the peak attained in early life. Thus, factors that influence growth, such as variations in early nutrition, may contribute to muscle mass and strength in older age.
It is importance of life time influences, is that low weight at birth predicts lower muscle mass and strength in adult life. This is a consistent finding by a number of studies. Although little is currently known about the influence of diet in early life on sarcopenia, recent studies of adolescents have provided evidence of nutrient effects on muscle mass and function earlier in the lifetimes. Consistent with studies of older adults, low vitamin D status has been shown to be associated with lower grip strength and with poorer muscle power and velocity. However, randomized controlled trials of vitamin D supplementation of adolescents have had mixed results. Among premenarcheal girls who were supplemented with vitamin D over 1 year, there were rank increases in lean mass, although supplementation did not result in measurable differences in grip strength( 64 ) In contrast, vitamin D supplementation of adolescent boys and postmenarcheal girls has not been shown to be effective in increasing lean mass or muscle strength or power. There are concluded that earlier interventions, before the period of peak muscle mass increased, may be needed to improve muscle function and physical performance.
To date, few studies have examined the role of diet in early childhood in the act of getting of muscle mass and effects on later function, although there is some evidence that it could be important. For example, the risk of frailty has been shown to be greater in older adults who grew up poor in quality conditions, and who experienced hunger in childhood. However, animal models suggest that nutrition even earlier in life may be key, as muscle growth in the neonatal period is highly sensitive to variations in nutrient intake. Among children, duration of breastfeeding was not associated with physical work capacity assessed at the age 9 years, in adolescents studied, longer duration of breastfeeding was associated with measurable differences in physical performance-particularly in lower body explosive strength. Consistent with longer duration of breastfeeding and greater compliance with infant feeding guidance has been shown to be associated with greater lean mass in later childhood. Dietary patterns marks across childhood, and this may simply reflect continuing benefits of healthier diets. However, it does suggest that variations in early postnatal diet could have implications for muscle function in later life.
We currently know little about the contribution of nutrition throughout the lifetimes to muscle mass and strength in adult life, and further work is needed to understand how early nutrition influences the act of getting of peak muscle mass, and the role played by nutrition of age-related losses in muscle function. Taking a life time approach to understanding the links between nutrition and muscle mass and function in older age could change dietary strategies to prevent sarcopenia in the future.
Conclusion
To develop strategies to prevent or delay sarcopenia, a better understanding is needed of the lifestyle factors that influence the rate of decline of muscle mass and strength in older age, and the mechanisms involved. Existing evidence indicates the potential importance of diets of adequate quantity and quality, to ensure sufficient intakes of protein, vitamin D, and antioxidant nutrients. Although much of this evidence is observational and the mechanisms are not fully understood, the high prevalence of low nutrient intakes and poor status among older adults make this a current concern. However, muscle mass and strength achieved in later life are not only determined by the rate of muscle loss, but also reflect to reach the peak earlier in life, and efforts to prevent sarcopenia also need to identify the potential effectiveness of interventions earlier in the life course. Optimizing diet and nutrition throughout life may be key to preventing sarcopenia and promoting physical capability in older age.
For more about Juniper Publishers please click on: https://twitter.com/Juniper_publish
For more about Journal of Thyroid Research please click on: https://juniperpublishers.com/jetr/index.php
#Endocrinology Research#hormones#Hypothyroidism#Juniper Publishers e-pub#Juniper Publishers Plagiarism policy
0 notes
Text
Juniper Publishers- Open Access Journal of Case Studies

Dynamics of Frailty as a Geriatric Syndrome
Authored by Esra ATES BULUT
Abstract
Frailty and sarcopenia are new geriatric syndromes which lead to poor outcomes including functional decline, falls, morbidity, hospitalization and mortality. Frailty is a distinctive health state related to the ageing process in which multiple body systems gradually lose their reservation capacity. It is a multidimensional state with interrelated factors in the physical, psychological, social, and environmental domains. It is also associated with other geriatric syndromes in the mood, cognition areas and physical performance. Clinically, diagnosis is based on weight loss, slow walking speed, low muscle strength and physical activity. Due to high frequency among seniors and being a reason of poor health outcomes, accurate diagnosis, and appropriate prevention and treatment strategies should be established.
Keywords: Ageing; Geriatric syndromes; Sarcopenia; Physical dependence
Introduction
Ageing process, frailty and death concepts belong to the mysterious subjects of medicine. Frailty is used currently different clinical meanings: easily broken, damaged, rapidly dying, diminished resistance and strength. It is a gradual process that develops slowly, and the rate of decline accelerates with acute events. Once a person becomes frail, a progressive process proceeds until death [1]. Many health care providers focus on diseases when they evaluate patients. However, frailty does not fit to this approach, and it is not the chief complaint. Patients are usually asymptomatic, or the findings are subtle [2]. Frailty is defined difficulty in restoring the homeostatic balance against stressors with ageing. Frailty has multidimensional state with interrelated factors in the physical, psychological, social, and environmental domains that affect the physiologic reserve of the systems. Furthermore, it is also indicated as a geriatric syndrome characterized by reduced physical function, which may lead to decreased strength, endurance, and increased dependence or mortality [3]. Because of the reduced capacity of the organism, the risk of developing poor health outcomes such as falls, hospitalization, disability, discharge to nursing home and mortality increases [4,5].
Although ageing is considered as frailty in society, every elder is not frail. Prevalence of frailty in subjects aged 65-75 years ranges from 3% to 7% [6]. This rate rises to 32% over the age of 90 years [7]. The prevalence of frailty differs from various ethnic groups and increases with age.
Frailty can be primary or secondary diagnosis. 7% of frail older adults do not have a systemic disease. Moreover, 25% have only one disease [8]. However, an acute event, atherosclerosis, infection, malignancy, depression or the last period of a chronic process may cause frailty. It has been reported increased age, history of cancer, chronic obstructive pulmonary disease, cerebrovascular disease, physiological impairments of inflammatory processes and coagulation are risk factors for frailty [9].
Discussion
Frailty characteristics are associated with overt changes in the four main title: body composition, homoeostatic dysregulation, energetic failure and neurodegeneration. In addition, impaired glucose metabolism, inflammatory biomarkers, and some physiological variables such as markers in clotting pathway contribute the pathophysiologic pathway [7]. Many physiological systems including the central nervous system, the sympathetic nervous system, the endocrine system, the skeletal-muscular system and the immune system are affected. Which system is affected first and what threshold level is needed to develop the clinical situation are the key questions to be answered at the moment.
Age-related skeletal muscle loss or sarcopenia is the main feature of frailty. Preservation of skeletal muscle function requires the interaction of many factors, such as hormones, neurological functions, inflammatory markers, and nutrients [10]. Recent studies showed infiltration of the muscle by fat tissue causes decrease in the muscle strength and mass. It was reported adipose tissue especially visceral fat tissue, can cause some hormonal and inflammatory changes which contribute release of inflammatory cytokines and hormones [7]. Interleukin-6 (IL-6), Tumor Necrosis Factor-α (TNF-α) and other inflammatory mediators cause muscle destruction for energy production [11]. Increasing evidence indicates these markers may cause skeletal muscle loss by inducing apoptotic mechanisms [12]. As a result, metabolically active fat stores establish chronic inflammatory state and increase sarcopenia. Many studies have shown inflammatory markers such as IL-6, CRP, white cells, and macrophage counts are related to frailty [13]. These findings suggest that chronic, low level of inflammatory activity induce frailty. Increased IL-6 causes reduction in bone mineral density, muscle loss, anemia, insulin resistance, hypothalamo-pitiuter-adrenal axis stimulation and impaired immune system regulation [14]. Recent studies reported hyperinsulinemia and hypertriglyceridemia lead to suppression of appetite and nutritional intake. Besides, they may also be associated with cognitive impairment, physical decline and leptin resistance [15].
It was hypothesized cognitive impairment, physical inactivity, visual-hearing loss and incontinence were related to frailty in women [16]. The coexistence of cognitive and physical impairment may be explained by the role of proinflammatory cytokines in the pathophysiology of both conditions [17].
Three main hormones decrease with ageing: growth hormone, sex steroids and adrenocorticoid hormones [18]. Sex steroids and growth hormone affect age-related changes in body composition. IGF-1 plays major role in the development of skeletal muscle cells, however inflammatory cytokines suppress IGF-1 release [19]. Furthermore, dehydroepiandrostenodion sulfate (DHEAS) suppresses inflammation induced by nuclear factor kappa B. Reduced DHEAS and testosterone levels were thought to related to frailty [20,21]. In addition, impaired cortisol diurnal rhythm is associated with increased catabolism, muscle loss, anorexia, and decreased energy expenditure, which are the main building blocks of frailty [22]. Changes in cellular ageing pathways, disruption of telomeric structures, mitochondrial dysfunction, increased free radical production, decreased DNA repair capacity with ageing may explain reduction of multisystem physiological regeneration capacity. Figure 1 summarizes pathophysiology of frailty [23].
Because of the increase the number of older adults who need medical support, and cost of these patients to the healthcare system, it has great importance to determine the biological older patients. In the last two decades, it is desirable to develop biomarkers and scales to distinguish the biological age of older individuals [24]. Therefore, patients should be evaluated not only disease-oriented but also function-oriented.
Fried and his colleagues composed the most frequently used criterion to assess vulnerability. The Fried Physical Frailty Scale is shown in Table 1 [25]. Frailty is defined in this phenotype model as presence of 3 or more of the following: exhaustion, weight loss, low muscle strength, low walking speed, and of low physical activity. The presence of one or two criteria was considered as pre-fail state. The walking speed, muscle strength and physical activity are evaluated by 4-meter walking test, hand grip test (dynamometer) and Minesota Leisure Time Activity questionnaire, respectively. This model successfully predicts poor health outcomes such as falls, disability, hospitalization, and mortality [25].
Due to the difficulty of application the phenotype model in daily clinical practice, various other scales were developed. The FRAIL scale has 5 criteria: fatigue, resistance, ambulation, systemic diseases (ilness) and weight loss [26]. Presence of 1-2 criteria is considered as pre-frail state and 3 or more criteria indicates frailty
The cumulative deficit model was then established by the Canadian Health and Ageing Study. Total 92 basal variables were included in this study, including various findings (e.g. tremor), symptoms (e.g. low mood), disease states, abnormal laboratory values, and disabilities. Vulnerability was assessed by the accumulation of deficiencies in patients. The more deficiencies patients have, the worse frailty status they have [27]. In addition to these scales, other indexes with wider psychosocial contents such as the Groningen and Tilburg Frailty Indicators were also developed [28,29].
A meta-analysis which was conducted between 2009-2015, assessed 29 frailty scales, according to this meta-analysis [30], the Fried physical scale and the deficit index are the most commonly used scales. Fried phenotype model, frailty deficit index, Edmonton frailty scale and clinical frailty scale were found both reliable and well predict clinical results.
Because frailty is more common with increasing age, it is important to apply protective approaches from middle ages. Early recognition and effective treatment strategies have great importance in order to prevent frailty in later life.
Optimal treatment of patients’ systemic medical diseases and stable management of intervening acute conditions constitute the basic principles of frailty treatment [31]. Currently, there is strong evidence that exercise is more beneficial than other interventions in frail patients. Multi-component exercises such as resistance, flexibility, aerobic and balance exercises are useful in the prevention and treatment of frailty. In addition, it is also considered to be the best strategy to prevent the development of disability in the frail patients [32,33]. However, the most effective type, duration and frequency of exercise intervention is uncertain.
Vitamin D support is known to reduce falls, hip fracture and mortality in older adults [34-36]. Vitamin D is also effective on neuromuscular functions [37]. Although, there are no large scale studies, replacement of vitamin D deficiency seems to be effective for the treatment of frailty.
In 2013, consensus for frailty was determined treatment of physical frailty under 4 main headings: [3]
a) Exercise
b) Calorie and protein supplement
c) Vitamin D
d) Prevention of polypharmacy
Conclusion
Prevention of frailty should not only be considered as a necessary intervention for the elderly. Effective prevention of systemic diseases starts at early ages. Promoting healthy lifestyle and improving health services should be considered as main targets for successful ageing. However, primary care practitioners should be aware of frailty and risky individuals should be referred to necessary higher levels of health care service. Furthermore, clinicians should keep frailty on mind in individuals over 70 years with unintentional weight loss. Recognition of frailty identify high risk patients for medical interventions and reduce risk of adverse outcomes. In the future, universal, valid diagnostic criteria should be established, and more detailed studies are needed to clarify the pathophysiology of frailty.
For more articles in Juniper Publishers | Open Access Journal of Case Studies please click on: https://juniperpublishers.com/jojcs/index.php
#Juniper Publishers Contact#Juniper Publishers#Critical Care Medicine#Gastrointestinal Surgery#Obstetrics and Gynaecology#Pharmacology
0 notes
Link
Pregnant Women Get Conflicting Advice on Covid-19 Vaccines Pregnant women looking for guidance on Covid-19 vaccines are facing the kind of confusion that has dogged the pandemic from the start: The world’s leading public health organizations — the U.S. Centers for Disease Control and Prevention, and the World Health Organization — are offering contradictory advice. Neither organization explicitly forbids or encourages immunizing pregnant women. But weighing the same limited studies, they provide different recommendations. The C.D.C.’s advisory committee urged pregnant women to consult with their doctors before rolling up their sleeves — a decision applauded by several women’s health organizations because it kept decision making in the hands of the expectant mothers. The W.H.O. recommended that pregnant women not receive the vaccine, unless they were at high risk for Covid because of work exposures or chronic conditions. It issued guidance on the Moderna vaccine on Tuesday, stirring uncertainty among women and doctors on social media. (Earlier this month, it published similar guidance on the Pfizer-BioNTech vaccine.) Several experts expressed dismay at the W.H.O.’s stance, saying the risks to pregnant women from Covid were far greater than any theoretical harm from the vaccines. “There are no documented risks to the fetus, there’s no theoretical risks, there’s no risk in animal studies,” from the vaccines, said Dr. Anne Lyerly, a bioethicist at the University of North Carolina, Chapel Hill. “The more that I think about it, the more disappointed and sad I feel about it.” The difference of opinion between the C.D.C. and the W.H.O. is not rooted in scientific evidence, but the lack of it: Pregnant women have been barred from participating in clinical trials of the vaccines, a decision in line with a long tradition of excluding pregnant women from biomedical research, but one that is now being challenged. While the rationale is ostensibly to protect women and their unborn children, barring pregnant women from studies pushes the risk out of the carefully controlled environment of a clinical trial and into the real world. The practice has forced patients and providers to weigh sensitive, worrisome issues with little hard data about safety or effectiveness. Vaccines are generally considered to be safe, and pregnant women have been urged to be immunized for influenza and other diseases since the 1960s, even in the absence of rigorous clinical trials to test them. “As obstetricians we are often faced with difficult decisions about using interventions in pregnancy that have not been properly tested in pregnancy,” said Dr. Denise Jamieson, an obstetrician at Emory University in Atlanta and a member of the Covid expert group at the American College of Obstetrics and Gynecologists. The college strongly advocated including pregnant and breastfeeding women in the vaccine trials. “What many people miss is that there are risks to doing nothing,” Dr. Jamieson said. “Not offering pregnant women the opportunity to be vaccinated and protect themselves, where there are known and severe risks of Covid amplified by pregnancy, is not a wise strategy.” The uncertainty isn’t limited to Covid vaccines: Many if not most medications, including widely used drugs, have never been tested in pregnant women. It can take years or decades for adverse side effects to come to light in the absence of a study with a control group for comparison. “This isn’t a story about the W.H.O. or other people advising against vaccination in pregnancy,” said Carleigh Krubiner, a policy fellow at the Center for Global Development and a principal investigator for the Pregnancy Research Ethics for Vaccines, Epidemics and New Technologies project (PREVENT). “It’s a story about the failure to timely and appropriately include pregnant women in vaccination studies.” Saying she understood the commitment of the W.H.O. and other advisory bodies to rely on scientific studies, Dr. Krubiner added: “The reality is that we don’t yet have the data on these vaccinations in pregnancy, and it’s very difficult without that data to come out and give a full-throated recommendation in support.” The C.D.C. and the W.H.O. have offered dissonant advice many times over the course of the pandemic — most notably on the usefulness of masks and the possibility of the virus traveling by air indoors. In a statement, the C.D.C. said on Thursday that based on how the Pfizer-BioNTech and Moderna vaccines work, “they are unlikely to pose a specific risk for pregnant women.” The C.D.C.’s recommendation may make sense for the United States, where women may easily be able to consult with their health care providers, said Joachim Hombach, a health adviser to the W.H.O. on immunizations. But the W.H.O. provides guidance to many low- and middle-income countries where women do not have access to doctors or nurses, he said. The W.H.O.’s recommendation was also made “in the context of limited supply” of the vaccines, Dr. Hombach said. “I don’t think the language is discouraging, but the language is stating the facts.” Pfizer did not include pregnant women in its initial clinical trials because it followed the policies outlined by the Food and Drug Administration to first conduct developmental and reproductive toxicity studies, said Jerica Pitts, a spokeswoman for the company. Pfizer and Moderna both provided results from toxicity studies in pregnant rats to the F.D.A. in December. Pfizer plans to begin a clinical study in pregnant women in the first half of 2021, Ms. Pitts said. Moderna is establishing a registry to record outcomes in pregnant women who receive its vaccine, according to Colleen Hussey, a spokeswoman for the company. Critics of the companies’ decisions to exclude pregnant women from trials say the reproductive toxicity studies could have been carried out much earlier — as soon as promising vaccine candidates were identified. The companies should have added a protocol to enroll pregnant women once it was clear the vaccines’ benefits outweighed potential harm, Dr. Krubiner said. “It’s hard to understand why that delay is happening and why it wasn’t initiated sooner,” she said. “The bigger issue is, we’re going to have lost months by the time they start them.” Akiko Iwasaki, an immunologist at Yale University who has advocated immunizations for pregnant women questioned the underlying issue that prompted the W.H.O.’s decision. “Whatever it is, I wish the W.H.O. would be more transparent in their reasons behind this recommendation,” she said. “Women’s lives depend on it.” Covid-19 Vaccines › Answers to Your Vaccine Questions Am I eligible for the Covid vaccine in my state? Currently more than 150 million people — almost half the population — are eligible to be vaccinated. But each state makes the final decision about who goes first. The nation’s 21 million health care workers and three million residents of long-term care facilities were the first to qualify. In mid-January, federal officials urged all states to open up eligibility to everyone 65 and older and to adults of any age with medical conditions that put them at high risk of becoming seriously ill or dying from Covid-19. Adults in the general population are at the back of the line. If federal and state health officials can clear up bottlenecks in vaccine distribution, everyone 16 and older will become eligible as early as this spring or early summer. The vaccine hasn’t been approved in children, although studies are underway. It may be months before a vaccine is available for anyone under the age of 16. Go to your state health website for up-to-date information on vaccination policies in your area Is the vaccine free? You should not have to pay anything out of pocket to get the vaccine, although you will be asked for insurance information. If you don’t have insurance, you should still be given the vaccine at no charge. Congress passed legislation this spring that bars insurers from applying any cost sharing, such as a co-payment or deductible. It layered on additional protections barring pharmacies, doctors and hospitals from billing patients, including those who are uninsured. Even so, health experts do worry that patients might stumble into loopholes that leave them vulnerable to surprise bills. This could happen to those who are charged a doctor visit fee along with their vaccine, or Americans who have certain types of health coverage that do not fall under the new rules. If you get your vaccine from a doctor’s office or urgent care clinic, talk to them about potential hidden charges. To be sure you won’t get a surprise bill, the best bet is to get your vaccine at a health department vaccination site or a local pharmacy once the shots become more widely available. Can I choose which vaccine I get? How long will the vaccine last? Will I need another one next year? That is to be determined. It’s possible that Covid-19 vaccinations will become an annual event, just like the flu shot. Or it may be that the benefits of the vaccine last longer than a year. We have to wait to see how durable the protection from the vaccines is. To determine this, researchers are going to be tracking vaccinated people to look for “breakthrough cases” — those people who get sick with Covid-19 despite vaccination. That is a sign of weakening protection and will give researchers clues about how long the vaccine lasts. They will also be monitoring levels of antibodies and T cells in the blood of vaccinated people to determine whether and when a booster shot might be needed. It’s conceivable that people may need boosters every few months, once a year or only every few years. It’s just a matter of waiting for the data. Will my employer require vaccinations? Where can I find out more? The toxicity data released by Pfizer and Moderna in December found no harmful effects from the vaccines to pregnant rats — evidence cited by the W.H.O. in its guidance. One extreme consequence of a conservative approach to vaccines played out during the Ebola epidemic in the Democratic Republic of Congo, when health workers offered a vaccine for the disease to all frontline workers and contacts of people confirmed to have it — except if they were pregnant or breastfeeding. Without the vaccine, 98 percent of pregnant women who were infected with the Ebola virus died. The rules were changed following a public outcry but, by then, many pregnant women had died, Dr. Lyerly said. Covid-19 has also proved to be dangerous to pregnant women. A large C.D.C. study published in November found that pregnant women with Covid who were symptomatic were significantly more likely to be hospitalized or to die when compared with nonpregnant women who also had Covid symptoms. The evidence prompted agency officials to add pregnancy to the list of conditions that heighten the risk of severe disease and death from Covid. The C.D.C. has set up a smartphone application called v-safe to solicit reports of side effects from immunized people. About 15,000 pregnant women have enrolled in the registry so far, the agency’s immunization committee reported on Wednesday. “I think that’s our best chance of getting safety data rapidly,” Dr. Jamieson said. Britain initially starkly recommended against Covid vaccines for pregnant women, but has since revised its guidance to authorize inoculating pregnant women who are frontline workers or otherwise at high risk. “I’m hoping the W.H.O. will reconsider as well,” Dr. Jamieson said. Some experts said the recommendations are not as divergent as they may appear at first glance. “The C.D.C. is more inclined to say that pregnant women should have access to the vaccine, but should discuss their circumstances with their providers,” said Dr. Ana Langer, a reproductive health expert who leads the Women and Health Initiative at Harvard’s T.H. Chan School of Public Health. “The W.H.O.’s interim recommendation says that women who are at particularly high risk of exposure or getting Covid should get the vaccine. So where’s the big difference here?” Denise Grady contributed reporting. Source link Orbem News #Advice #conflicting #Covid19 #Pregnant #Vaccines #Women
0 notes
Text
Facts about Alcohol Abuse in Elderly – Dr. Sandy Sanbar

Youth To Elderly & Alzheimer’s: Sex, Intimacy, Love, and Romance in Elderly & Alzheimer’s Patients is the third edition of Dr. Sandy Sanbar’s book in which he has compiled stories about the lives of the elderly and Alzheimer’s patients. Stories about love, relationships, sex, gambling, and drug abuse in the elderly. Dr. Sanbar provides an unseen insight into their lives. Topics that are almost always stigmatized in society are discussed in this book. It’s a must-read for adults, caregivers of elderly and Alzheimer’s patients, and their families. He also discusses the benefits of the Mediterranean-DASH Intervention for Neurodegenerative Delay diet and the impact of COVID-19 on the elderly and patients.
In the book, Dr. Sanbar writes about how common alcohol addiction is becoming among older adults. This crisis is growing every year but somehow is still unnoticed by many. That is because most people associate alcohol abuse with younger adults. In reality, the highest rate of alcoholism is found among widowers over the age of 75. According to the Alcohol Addiction Center, here are a few more surprising facts about alcohol abuse among the elderly:
· Alcohol contributes to 60 percent of falls.
Because seniors often lose their dexterity and flexibility they may have balance problems that are made worse after a few drinks. The National Council on Aging states that one in four people over the age of 65 has a serious fall each year and it is the leading cause of fatal injuries among the elderly, so you can see why fall prevention is vital for older Americans.
Falls are the culprit in over 2.8 million emergency room visits each year, and although they may be non-fatal they can seriously compromise the mobility of seniors. Healing slows as we age, and an elderly person who faces an extended recovery from a fall injury is more prone to depression as they may be more isolated from social activities.
· Increased sensitivity
The elderly may not realize they have an increased sensitivity to alcohol. Typically as we age our tolerance for alcohol decreases as our metabolism slows down. According to the National Institute on Alcohol Abuse and Alcoholism, this is primarily because as we age our body's water content is reduced, which means the same amount of alcohol consumption gives a higher blood alcohol level.
Because of the increased sensitivity, an elderly drinker might think they're okay to drive because they consumed the same amount of alcohol as they did for years when in fact their tolerance is lower. Lower tolerance for alcohol can lead to a higher rate of car crashes, falls, and other injuries.
· There is a 65 percent rise in high-risk drinking in the elderly
Researchers define high-risk drinking in seniors as five or more drinks a day for men and four for women at least once a week during a year. This rate of drinking has skyrocketed 65 percent in the past decade and now stands at 3.8 percent of the elderly population, or about 2.5 million seniors.
High-risk drinking isn't confined to those who live alone, either. The National Council on Alcoholism and Drug Dependence states that almost half of nursing home residents have an alcohol-related problem. In addition, high-risk drinking is responsible for 20 percent of elderly admissions to psychiatric hospitals and 14 percent of senior emergency room admissions.
0 notes
Text
July 2020 Learning Network Resources
Tuesday, July 28th at 4:00PM EST
Join usfor a webinar on our latest tool. Dr. Lisa Letourneau and Kelly Rand will share a look at our patient engagement toolkit, discuss the research behind it and provide a few examples on how to apply the tools to COVID-19. Click here to join.
Blogs, Issue Briefs, Opinion Pieces and More…
Measurement and Evaluation Approaches to Improve Outpatient Antibiotic Prescribing. Center for Healthcare Strategies. July 2020 “A key consideration for jurisdictions seeking to improve outpatient antibiotic prescribing is how to measure and evaluate baseline performance and progress over time and how to identify goals for antibiotic stewardship initiatives. This technical assistance tool describes metrics that state Medicaid and public health agency partners can use to evaluate and target opportunities to improve antibiotic prescribing practices. It also provides a summary of data sources that can be used to evaluate efforts focused on improving antibiotic stewardship.”
Pandemic guidance for health professionals. Choosing Wisely Australia. Retrieved July 2020 “The Choosing Wisely principles have been a pillar during Australia’s COVID-19 pandemic response. Our health system has come together for a common goal and purpose to manage the pandemic. Health professionals have had to be stewards of our finite health resources. Multidisciplinary teams have united to adopt an evidence-based, patient-centered approach. As a result, our health system has adapted in ways and with urgency unseen before. To assist clinicians and consumers to access reliable information about the pandemic we’ve developed specific pandemic guidance, which is based on current evidence and will continue to be update as evidence evolves over time.”
Covid-19: an opportunity to reduce unnecessary healthcare. BMJ. July 2020 “This pandemic has provoked the best of human compassion and solidarity, but those who manage our health systems still face extraordinary challenges responding to covid-19 and preparing for the second wave. Looking beyond the crisis, our collective learning about the effects of the large falls in healthcare use can help inform and intensify efforts to reduce unnecessary care. This in turn can prevent avoidable harm to patients, enhance healthcare equity, and improve the sustainability of health systems everywhere.”
Journals
Salzman B, et alt. Breast Cancer Screening Shared Decision-Making in Older African-American Women. Journal of the National Medical Association. July 2020 “This study explored African American women’s knowledge of breast cancer screening guidelines in older adults, prior conversations with providers regarding continuation of screening, and their understanding/willingness to engage in discussions about individualized breast cancer screening decision-making using two versions of tested decision aids.”
Vieira ER. Perspectives on Research and Health Practice in Physical and Occupational Therapy in Geriatrics during and Post COVID-19. Physical & Occupational Therapy in Geriatrics. July 2020 “COVID-19 has revealed the susceptibilities and gaps in the P&OT delivery models to the public in general and especially to older adults with chronic conditions. The effects will continue to be felt long until effective COVID-19 treatments and a vaccine is available, but these vulnerabilities need to be addressed before the next pandemic.”
Boone S, et alt. Management of Nonpregnant Women Presenting to the Emergency Department With Iron Deficiency Anemia Caused by Uterine Blood Loss: A Retrospective Cohort Study. The Journal of Emergency Medicine. June 2020 “In this cohort of adult females with moderate to severe IDA caused by uterine bleeding, blood transfusion was often administered in the absence of hemodynamic instability or active hemorrhage, iron deficiency was inadequately treated, and a high rate of subsequent transfusions occurred. Future studies should investigate optimal indications for transfusion and emphasize adequate iron supplementation.”
Poor Cost Awareness Among Anesthesia Providers for Medications, Supplies, and Blood Products. The Joint Commission Journal on Quality and Patient Safety. June 2020 “The majority of anesthesia providers have poor knowledge of cost. These findings suggest that cost awareness interventions may be necessary for promoting high-value health care.”
Sun JY. Implementing Electronic Health Record–Based Clinical Decision Support for Head CT Ordering in Minor Pediatric Head Trauma. Journal of the American College of Radiology. June 2020 “Traumatic brain injury (TBI) is an important and increasingly common reason for pediatric emergency department (ED) visits, resulting in 812,000 ED visits by children in the United States in 2014. Although head CT is a cornerstone for the diagnosis of clinically significant TBI requiring acute intervention, the large majority of presentations for minor pediatric head trauma have negative imaging findings. Clinical providers must make rapid decisions that balance the need to identify clinically significant TBI with the economic costs and radiation risks of CT overuse.”
Neuner-Jehle S, et alt. What interventions do general practitioners recommend avoiding? A nationwide survey from Switzerland. Swiss Medical Weekly. June 2020 “Most RIA suggestions from GPs were concordant with previously published RIAs, independently of GPs knowledge of these and reflecting their high clinical relevance. In addition, our study revealed some more relevant topics and may help to develop future “Choosing Wisely” recommendations, with the final goal to reduce low-value care.”
Graham K, et alt. Challenges of Implementing the Choosing Wisely Guideline to Promote Sleep and Rest at Night for Hospitalized Patients. Nursing Care Quality. June 2020 “A pilot intervention to support the initiative, “Don’t wake the patient for routine care unless the patient’s condition or care specifically requires it,” was implemented on 3 units in 3 hospitals. All the 3 units had experienced patient concerns about lack of sleep at night. There was multidisciplinary support to promote a better patient experience of nighttime sleep. The experiences across the 3 hospital units were positive for providers, patients, and patients’ families.”
Media Coverage
The Dentist Will See You Now. But Should You Go? NPR. July 2020 “Remember, infectious disease specialists note, that we all have important responsibilities as patients, too, to let the dentist know before or on the day of the appointment if we’re feeling sick in any way. We’re all in this together — if you’re sick, stay home.”
“Why People Are Still Avoiding the Doctor (It’s Not the Virus).” The New York Times. June 2020 “At first, people delayed medical care for fear of catching Covid. But as the pandemic caused staggering unemployment, medical care has become unaffordable for many.”
Should you take a dietary supplement to prevent disease? CNN Health. June 2020 “If you’ve been more concerned about your health lately, you might be wondering if taking a nutrition supplement containing vitamins, minerals or a combination is worthwhile. It’s estimated that more than half of Americans take one or more dietary supplements daily or on occasion. The pills are popular in Europe, too: According to one estimate, the dietary supplement market was worth over $14 billion in 2018, although research has suggested that usage varies widely according to each country. But are you wasting your money on vitamins and minerals you don’t need or possibly harming yourself by taking high doses? Here’s the lowdown.”






https://feeds.feedblitz.com/~/631237550/0/catherinemccracken~July-Learning-Network-Resources/
0 notes