#MD Pulmonary Medicine
Explore tagged Tumblr posts
Text

Heart Doctor With Heart: Bernard Lown
Pioneering Physician And Peace Activist
Dr. Bernard Lown was a Jewish immigrant from Lithuania who invented the heart defibrillator, transforming the field of cardiology and saving countless lives. He was a passionate peace activist who won the Nobel Prize for co-founding Physicians for the Prevention of Nuclear War.
Born to an erudite Jewish family in Lithuania in 1921, Bernard and his father, a rabbi, emigrated to Maine soon after his bar mitzvah to escape Nazi persecution. He attended the University of Maine, where he earned a bachelor’s degree in zoology, and then went to medical school at Johns Hopkins. As someone who’d fled his country because of ethnic hatred, he was especially sensitive to racism, and caused controversy in medical school for inviting a black doctor to speak on public health issues in the African-American community. Bernard was briefly expelled from school for protesting the segregation of blood in the hospital’s blood bank.
After receiving his MD in 1945, Bernard married his cousin Louise Lown. Their marriage would last 73 years. He said, “When you ask about my heroes, clearly I have many – my wife Louise foremost.” In the 1950��s, Bernard became a physician and researcher at Harvard Medical School, specializing in cardiology. He also taught at the Harvard Chan School of Public Health, where he was among the first to emphasize the crucial role of nutrition in treating and preventing many illnesses including heart disease.
As a young cardiologist, Bernard’s mentor was Dr. Samuel Levine, who encouraged him to study the common practice of putting heart attack patients on bed rest for 4-6 weeks, which often led to pulmonary embolisms. In what became known as the “Levine Chair study,” Bernard found that having patients sit in a comfortable chair improved outcomes significantly. This simple discovery changed the standard of practice for heart patient care.
Bernard was determined to find a way to prevent the most common cause of death: cardiac arrest. After hearing about cases where patients were resuscitated with an AC electric shock, which was very dangerous, Bernard wanted to find a safer type of electric current. He worked with fellow Eastern European refugee Baruch Berkovitz, an electrical engineer, and after a year of intensive research, in 1961 Bernard developed a new defibrillator that used a DC current. It was so safe and effective that the DC defibrillator soon became the universally accepted treatment for cardiac arrest.
Bernard pioneered the use of the drug lidocaine to treat heart disorders. In 1965 at Brigham Hospital in Boston, Bernard organized one of the first coronary care units focused on the prevention of heart rhythm disorders. He proved that continuous EKG monitoring and well-trained nurses could identify arrhythmias early and save lives. Bernard founded the Lown Cardiovascular Research Foundation in 1973 to promote heart health through research and global education.
His research had an extraordinary impact on the practice of clinical medicine around the world. “The physician is not a glorified repairman of a broken-down machine; being treated is a human being with a mind and a soul.” He listened to his patients and considered them his partners in healing. Bernard wrote many bestselling books including “The Lost Art of Healing” and “Practicing the Art While Mastering the Science.”
In addition to his enormous contributions to the medical field, Bernard was a lifelong peace activist. He founded Physicians for Social Responsibility in 1961 because “you cannot be committed to health without being engaged in social struggle for health.” As the Vietnam War ramped up, Bernard organized the Committee of Responsibility to Save War Burned and War Injured Children, and brought about 100 seriously injured Vietnamese children to the United States for medical treatment.
In 1980 Bernard and Soviet cardiologist Dr. Eugene Chazov co-founded International Physicians for the Prevention of Nuclear War. Bernard said, “This was the greatest political issue of our time, because it didn’t just mean the death of an individual, but the death of multitudes. Why would doctors not get involved?” The doctors lobbied their countries for a moratorium on nuclear testing and building nuclear weapons, and held the first IPPNW World Congress, which attracted 80 medical leaders from twelve countries. In the next few years the group opened chapters in more than 60 countries and had over 200,000 physician members. For alerting people to the very real danger of nuclear war, IPPNW won the 1985 Nobel Peace Prize.
In his acceptance speech, “A Prescription for Hope,” Bernard said, “The ‘myth of the other,’ the stereotyping and demonizing of human beings beyond recognition, is still pervasive and now exacts inordinate economic, psychological and moral costs.” Incredibly, at the awards ceremony, a Russian journalist collapsed from cardiac arrest. Bernard and his Russian counterpart Dr. Chazov rushed to resuscitate the reporter and save his life. “When crisis comes, Soviet and American cardiologists cooperate,” Bernard said. His book “Prescription for Survival,” focusing on his anti-war activism, came out in 2008. That year, the Bernard Lown Peace Bridge was dedicated in Lewiston Maine.
Bernard was concerned about overtreating patients – ordering tests and procedures that often did more harm than good – and in 2012 he helped organize “Avoiding Avoidable Care,” the first global conference dedicated to the issue of overtreatment. He said, “Do as much as possible for the patient, and as little as possible to the patient.”
Dr. Bernard Lown died on February 16, 2021 at 99 years old. He is survived by three children, five grandchildren, and one great-grandchild. His wife Louise died in 2019.
41 notes
·
View notes
Text
Also preserved on our archive
Some interesting science analyzed
BY BROOKS LEITNER
Imagine lying back in an enclosed chamber where you bask for 90 minutes in a sea of pure oxygen at pressures two to three times that felt at sea level. This is the world of hyperbaric oxygen therapy (HBOT), a technology that’s been around for decades and is now being explored as a possible treatment for Long COVID.
"The silence on the inside is deafening at first,” says John M.,* who has undergone dozens of HBOT treatments for his persistent Long COVID symptoms. Fortunately, there is a television outside the chamber in view, and it is easy to communicate with the provider if needed. While the potential protocol is still being refined, patients may undergo up to 40 HBOT sessions to address some of the most problematic, lingering symptoms of this complex condition.
HBOT is a therapeutic process that has been widely used to treat such conditions as decompression sickness in scuba divers, carbon monoxide poisoning, and diabetic foot ulcers. In HBOT, the body is exposed to 100% oxygen, a significant increase from the 21% oxygen concentration we typically breathe. The therapy takes place in an enclosed chamber where the air pressure is elevated above normal levels. The combination of high-pressure and high-oxygen conditions enhances the amount of oxygen that can reach the body's tissues. The hope is that this therapy can provide the same relief and healing to people with Long COVID that it does for those with other conditions.
According to John M., HBOT was the first treatment that helped with his sleep and reduced his heart palpitations. “At one point after hospitalization, my Long COVID symptoms were so bad that I could barely walk or talk. HBOT was a great tool that really assisted with my recovery,” he said. John added that he hopes the medical community will achieve a better understanding of how HBOT can help relieve suffering for patients with Long COVID and that more research will increase access to this innovative therapy.
Does HBOT improve Long COVID symptoms? One key observation from the work of Inderjit Singh, MBChB, an assistant professor at Yale School of Medicine (YSM) specializing in pulmonary, critical care, and sleep medicine, is that Long COVID patients often experience debilitating fatigue. Based on Dr. Singh’s previous Long COVID research, the exhaustion is thought to be linked to the muscles’ inability to efficiently extract and utilize oxygen.
To picture how HBOT might work, you can think of your muscles as engines sputtering, struggling to get the fuel they need. If oxygen is the gas that fuels the muscles, it’s as if you are trying to complete your daily routine while the gas tank is running on “empty.” By aiming to directly address this oxygen utilization impairment, HBOT may be a potential solution.
A systematic review by researchers at the China Medical University Hospital noted that HBOT could tackle another major factor in the Long COVID puzzle: oxidative stress. This relates to the body's struggle to maintain balance when harmful molecules, known as free radicals, run amok, causing chronic inflammation.
Research co-authored by Sandra K. Wainwright, MD, medical director of the Center for Hyperbaric Medicine and Wound Healing at Greenwich Hospital in Connecticut, suggests that HBOT, with its high-oxygen environment, might dampen this chronic inflammation by improving mitochondrial activity and decreasing production of harmful molecules. Other potential benefits of HBOT in the treatment of Long COVID may include restoration of oxygen to oxygen-starved tissues, reduced production of inflammatory cytokines, and increased mobilization of hematopoietic stem cells—primary cells that transform into red blood cells, white blood cells, and platelets.
HBOT for Long COVID: Current and ongoing research Several small-scale reports have indicated that HBOT is safe for patients with Long COVID.
To address this question, a trial that followed the gold standard of modern medical research—a randomized, placebo-controlled, double-blind design—assigned 73 Long COVID patients to either receive 40 sessions of HBOT or a placebo of only 21% oxygen. The study observed positive changes in attention, sleep quality, pain symptoms, and energy levels among participants receiving HBOT. In a longitudinal follow-up study published in Scientific Reports, the authors at the Tel Aviv University found that clinical improvements persisted even one year after the last HBOT session was concluded. In a second study, the same authors focused on heart function, measured by an echocardiogram, and found a significant reduction in heart strain, known as global longitudinal strain, in patients who received HBOT.
In another study, 10 patients with Long COVID underwent 10 HBOT treatments over 12 consecutive days. Testing showed statistically significant improvement in fatigue and cognitive function. Meanwhile, an ongoing trial at the Karolinska Institute in Sweden has reported interim safety results wherein almost half of the Long COVID patients in the trial reported cough or chest discomfort during treatment. However, it was unclear whether HBOT exacerbated this symptom or if this adverse effect was due to the effort of participation by patients suffering from more severe Long COVID symptoms.
Is HBOT currently available as a treatment for Long COVID? For HBOT to become a mainstream treatment option for Long COVID, several critical priorities must be addressed. First, there is currently no established method for tailoring HBOT dosages to individual patients, so researchers must learn more about the specific features or symptoms that indicate potential benefits from HBOT. At the same time, we need to identify factors that may be associated with any adverse outcomes of HBOT. And finally, it’s important to determine how long these potentially beneficial effects last in a larger cohort. Will just a few HBOT trials be enough to restore patients to their baseline health, or will HBOT become a recurring component of their annual treatment regimen?
For now, HBOT remains an experimental therapy—and as such is not covered by insurance. This is a huge issue for patients because the therapy is expensive. According to Dr. Wainwright, a six-week course of therapy can run around $60,000. That’s a lot to pay for a therapy that’s still being studied. In the current completed studies, different treatment frequencies and intensities have been used, but it’s unclear how the treatment conditions affect the patient’s outcome.
“I have had some patients notice improvements after only 10 or 15 treatments, whereas some others need up to 45 treatments before they notice a difference,” notes Dr. Wainwright. “I think that HBOT is offering some promising results in many patients, but it is probably a strong adjunctive treatment to the other spectrum of things Long COVID patients should be doing, like participating in an exercise, rehab, and nutritional program.”
Dr. Singh notes that “a major challenge for research is the heterogeneity of Long COVID. It is hard to determine which symptoms to treat and enroll patients into trials based on them.”
Perhaps treatments that target multiple issues caused by Long COVID, like HBOT, may help overcome this challenge.
*Not his real name.
Brooks Leitner is an MD/PhD candidate at Yale School of Medicine.
The last word from Lisa Sanders, MD: Hyperbaric oxygen therapy (HBOT) is just one of the many existing treatments that are being looked at to treat Long COVID. We see this with many new diseases—trying to use a treatment that is effective in one set of diseases to treat another. And there is reason for optimism: We know that HBOT can deliver high levels of oxygen to tissues in need of oxygen. That’s why it’s used to treat soft tissue wounds. If reduced oxygen uptake is the cause of the devastating fatigue caused by Long COVID, as is suggested by many studies, then perhaps a better delivery system will help at least some patients.
Studies referenced:
bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-023-08002-8
www.ncbi.nlm.nih.gov/pmc/articles/PMC8806311/
www.nature.com/articles/s41598-024-53091-3
www.nature.com/articles/s41598-022-15565-0
www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1354088/full
www.ncbi.nlm.nih.gov/pmc/articles/PMC11051078/#:~:text=Proposed%20Mechanism%20of%20HBOT%20o
#long covid#hbottherapy#HBOT#hyperbaric oxygen therapy#mask up#covid#pandemic#wear a mask#public health#covid 19#still coviding#wear a respirator#coronavirus#sars cov 2
65 notes
·
View notes
Text
youtube
How to diagnose TB? What are the tests for it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad :
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
2 notes
·
View notes
Text
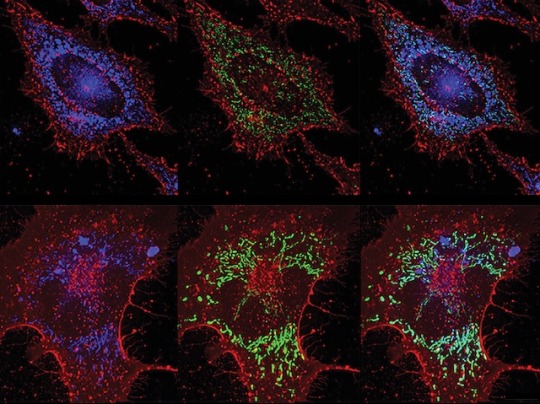
ROS vs Bacteria
Inducing lung lining cells to produce bacteria-killing reactive oxygen species (highly reactive chemicals that can cause oxidative damage) protects against pneumonia without reliance on antibiotics
Read the published research paper here
Image from work by Yongxing Wang and colleagues
Department of Pulmonary Medicine, University of Texas MD Anderson Cancer Center, Houston, TX, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY 4.0)
Published in PLOS Pathogens, September 2023
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#biology#reactive oxygen species#ROS#sci art#pulmonary#lungs#pneumonia#antibiotics#antibiotic resistance
10 notes
·
View notes
Text
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes
Text
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes
Text
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes
Text
Pneumonia Specialist Doctor in Hyderabad – Trusted Care at TX Hospitals

Pneumonia is a serious respiratory infection that can quickly escalate without timely diagnosis and proper treatment. Whether it’s caused by bacteria, viruses, or fungi, pneumonia affects the lungs and can lead to complications like respiratory failure, especially in children, older adults, and individuals with weakened immune systems. If you're searching for a pneumonia specialist doctor in Hyderabad, TX Hospitals offers expert care from some of the city's top pulmonologists, dedicated to delivering accurate diagnosis, effective treatment, and compassionate support.
At TX Hospitals, located in Banjara Hills and Uppal, we have a team of experienced chest specialists and pulmonologists who are well-versed in handling even the most complex cases of pneumonia. Our state-of-the-art facilities, advanced diagnostic tools, and 24/7 critical care services ensure that every patient receives the highest standard of care.
Why Choose TX Hospitals for Pneumonia Treatment?
✅ Experienced Pneumonia Specialists: Our doctors have extensive experience in treating all types of pneumonia, including community-acquired, hospital-acquired, and ventilator-associated pneumonia.
✅ Advanced Diagnostic Tools: With facilities like chest X-rays, CT scans, sputum cultures, and blood tests, we ensure quick and accurate diagnosis for prompt treatment.
✅ Critical Care Expertise: We offer intensive care and ventilator support for patients with severe respiratory distress, managed by trained specialists.
✅ Comprehensive Recovery Plans: Beyond treatment, we provide rehabilitation and follow-up care to restore lung health and prevent relapses.
Our Leading Pneumonia Specialist Doctors in Hyderabad
🔹 Dr. B Vijay Bhaskar – Sr. Consultant, Pulmonologist MBBS, MD (General Medicine), DM (Pulmonary Medicine) With vast expertise in pulmonary medicine, Dr. Bhaskar specializes in managing pneumonia and other severe respiratory infections. He practices at our Banjara Hills facility and is known for his clinical precision and patient-first approach.
🔹 Dr. Naresh Dude – Sr. Consultant, Pulmonologist MBBS, DNB (Pulmonary Medicine), FCCN Dr. Naresh Dude has over 12 years of experience in treating lung infections, including pneumonia in high-risk patients. His knowledge of intensive care makes him one of the most reliable pneumonia experts in Hyderabad.
🔹 Dr. Rohith Reddy Pathuri – Sr. Consultant, Pulmonologist MBBS, MD (Pulmonary Medicine) Based at Banjara Hills, Dr. Rohith Reddy is known for his efficient management of pneumonia cases, especially those complicated by asthma or bronchitis. His patient-friendly nature makes him a preferred doctor for long-term care.
🔹 Dr. Sathish Pogula – Consultant, Pulmonologist MBBS, MD (Pulmonary Medicine), IDCCM At our Uppal branch, Dr. Sathish Pogula handles both inpatient and outpatient pneumonia cases with a special focus on critical care and ventilator support. He brings over 8 years of experience and is a member of ISCCM.
🔹 Dr. M.V. Sree Keerthi – Sr. Consultant, Interventional Pulmonologist MBBS, DTCD (Gold Medalist), DNB, FABIP (AIIMS) With 12+ years of experience, Dr. Sree Keerthi is an expert in advanced lung infections and pneumonia-related complications. She uses bronchoscopy and other interventional techniques for accurate diagnosis and treatment.
🔹 Dr. M. Sai Sashank – Consultant, Pulmonologist MBBS, MD Dr. Sai Sashank has 9+ years of experience treating infectious lung diseases, including viral and bacterial pneumonia. He combines modern medicine with personalized care to ensure holistic healing.
Symptoms of Pneumonia to Watch Out For:
Persistent cough with mucus or phlegm
Fever, chills, and sweating
Difficulty breathing or chest pain while breathing
Fatigue and muscle aches
Confusion (especially in older adults)
If you or a loved one is showing signs of pneumonia, don’t wait. Timely intervention can save lives and prevent long-term lung damage.
📞 Call 9089 48 9089 to Consult the Best Pneumonia Specialist Doctor in Hyderabad 📍 Visit TX Hospitals at Banjara Hills or Uppal
When it comes to expert pneumonia care, trust only the best. At TX Hospitals, your health is in the hands of Hyderabad’s leading chest and lung specialists. Let us help you breathe better and heal faster.
#best lungs specialist in hyderabad#best chest specialist in hyderabad#pneumonia specialist doctor in hyderabad#pulmonologist in hyderabad
0 notes
Text
Best pulmonologist in chennai
Lung health is crucial to your overall well-being, yet many people tend to overlook symptoms like chronic cough, shortness of breath, or recurring respiratory infections. These symptoms might indicate underlying conditions that require specialist care. That’s where a pulmonologist steps in. If you're in Chennai and dealing with respiratory concerns, finding the best pulmonologist in Chennai can make all the difference. This guide will walk you through what pulmonologists do, when to see one, common conditions they treat, diagnostic methods, and a curated list of Chennai’s top lung specialists.

Who is a Pulmonologist?
A pulmonologist is a medical doctor specializing in the diagnosis and treatment of diseases affecting the lungs and respiratory system. These specialists manage everything from mild conditions like asthma and chronic bronchitis to more complex illnesses such as interstitial lung disease, sleep apnea, and even lung cancer. Pulmonologists undergo rigorous training, including general medical education, specialized residency, and fellowship training in pulmonary medicine.
If you’re experiencing ongoing breathing issues or respiratory discomfort, consulting a pulmonologist is essential. In a city like Chennai known for its leading medical infrastructure you have access to some of the country’s top pulmonary experts.
When Should You See a Pulmonologist?
It can sometimes be challenging to determine when it’s time to see a lung specialist. However, early intervention is key. You should consider visiting a lung specialist in Chennai if you:
Have a chronic cough lasting more than three weeks
Struggle with shortness of breath or wheezing
Experience frequent respiratory infections
Have been diagnosed with asthma, COPD, or other lung conditions
Snore loudly or have irregular breathing during sleep (possible sleep apnea)
Have a history of smoking or occupational exposure to pollutants
Notice chest tightness or unexplained fatigue
Timely consultation ensures that symptoms are managed effectively, preventing complications and improving your quality of life.
Top Pulmonologists in Chennai
Here are some of the most reputable and experienced pulmonologists in Chennai, each with a proven track record of clinical excellence:
Dr. Supraja K (MBBS, DNB – Respiratory Medicine)
Dr. Supraja K is known for her methodical and patient-centric approach. With over 17 years of experience, she has established a strong reputation in managing chronic conditions like asthma and COPD. Her practice focuses on evidence-based treatment and she actively participates in medical conferences to stay updated on emerging therapies.
Special interest in long-term asthma and allergy management
Offers customized treatment plans based on current guidelines
Highly regarded for her empathetic communication style
Dr. Elakiya M (MBBS, MD – Respiratory Medicine)
Dr. Elakiya M brings over 6 years of experience to the table. Her commitment to patient education and empowerment stands out, especially in managing COPD and interstitial lung disease.
Focuses on individualized treatment strategies
Employs advanced diagnostic tools for accurate assessments
Strong advocate for preventive care and early intervention
Dr. Krishnaveni R (MBBS, MD, DNB, DAA, FISM)
Renowned for her specialization in allergic asthma, Dr. Krishnaveni R is widely respected in the Chennai medical community. With her research-oriented practice, she is actively involved in clinical studies and the development of innovative treatments.
Expertise in managing sleep apnea and complex allergy-related conditions
Integrates holistic approaches for comprehensive respiratory care
Regularly recognized for excellence in pulmonary medicine
Dr. Subhashini (MBBS, DTCD)
With a focus on chronic asthma and long-term lung conditions, Dr. Subhashini emphasizes a hands-on, patient-first approach. With over 5 years of experience, she has become a reliable figure in community respiratory care.
Known for detailed follow-ups and continuity of care
Educates patients on home-based management techniques
Regularly updates her practice with the latest clinical guidelines
Dr. K Prithvi Boggavarapu (MBBS, MD – Pulmonology)
Dr. Prithvi specializes in complex and severe respiratory disorders, including interstitial lung disease. His technologically advanced diagnostic methods make him a sought-after name in Chennai’s pulmonology space.
Utilizes cutting-edge imaging and functional testing tools
Combines emotional support with clinical expertise
Active contributor to research in lung disease management
Dr. G. Thilagavathy (MBBS, DTCD, MD – Chest, FCCP – USA)
With over 55 years of experience, Dr. Thilagavathy is among the most senior and respected pulmonologists in Chennai. Trained both in India and the USA, her global exposure allows her to incorporate international standards into her practice.
Expert in managing severe respiratory illnesses and geriatric pulmonary care
Focuses on holistic treatment models that combine medication with lifestyle modifications
Actively mentors the next generation of pulmonologists
Conditions Treated by Pulmonologists
Pulmonologists in Chennai are equipped to manage a broad range of respiratory illnesses, including but not limited to:
Asthma: A chronic condition where airways become inflamed and narrow
COPD (Chronic Obstructive Pulmonary Disease): Includes chronic bronchitis and emphysema
Lung Infections: Pneumonia, tuberculosis, and other bacterial or viral infections
Sleep Apnea: Sleep disorder characterized by interrupted breathing
Lung Cancer: Diagnosis, staging, and treatment planning
Bronchiectasis: Damaged and widened airways prone to infections
Interstitial Lung Diseases (ILDs): Group of disorders causing lung tissue scarring
Primary Ciliary Dyskinesia: A rare condition affecting mucus clearance in the lungs
Pulmonary complications of autoimmune disorders like lupus and rheumatoid arthritis
Common Diagnostic Tools and Procedures
An accurate diagnosis is essential for creating an effective treatment plan. Pulmonologists in Chennai utilize various tools, including:
Basic Tests:
Pulmonary Function Test (PFT): Measures how well the lungs work
Chest X-ray: Helps detect infections, fluid, or tumors
CT Scan: Offers detailed imaging for precise diagnosis
Advanced Procedures:
Bronchoscopy: Visual inspection of airways using a camera
Sputum Culture: Identifies bacteria or fungi in lung secretions
Lung Biopsy: Examines tissue for diseases like cancer or ILDs
Pleural Tap (Thoracentesis): Removes fluid from lungs to test for infection or cancer
Arterial Blood Gas (ABG): Analyzes oxygen and carbon dioxide levels in the blood
These diagnostics allow pulmonologists to detect issues early and tailor the most effective treatment strategy.
Conclusion
Your lungs are vital to your health, and symptoms should never be ignored. Chennai offers some of the most skilled pulmonologists in India experts who combine clinical excellence with compassionate care. Whether you're dealing with chronic asthma, recovering from pneumonia, or simply need a thorough respiratory evaluation, consulting the best pulmonologist in Chennai can significantly enhance your quality of life.
From veteran experts like Dr. G. Thilagavathy to rising stars like Dr. Elakiya M and Dr. Prithvi, you have access to world-class respiratory care right in your city. Don’t delay seeking medical attention if you’re experiencing breathing difficulties. Prioritize your lung health it’s the foundation of your overall well-being.
For appointments or more details, reach out to their respective hospitals or clinics. Your lungs deserve the best. Read Also : https://medwayhospitals.com/best-foods-for-liver-health/
0 notes
Text
ICU-Level Care Not Definitive Indicator for Sepsis, New Study Shows
A majority (57%) of septic patients did not meet criteria for ICU level of care
30% of sepsis-associated deaths occurred in patients who did not meet the criteria of ICU level of care
Cytovale’s IntelliSep® host-response test was shown to be superior in both sepsis detection and prognosis when compared to a measurement of ICU level of care
SAN FRANCISCO and LAS VEGAS – A retrospective analysis of an observational study being presented this week at the Society of Hospital Medicine (SHM) Converge conference reveals that the need for intensive care unit (ICU)-level care in patients with suspected infection is not a definitive indicator for sepsis. “Prognostic Ability of Cellular Host Response Test in Diagnosis and Risk Stratification of Patients with Suspected Infection in Need of ICU-Level Care” details a five-year analysis of suspected infection patients at Our Lady of the Lake Regional Medical Center (OLOLRMC) in Baton Rouge, La. In comparing ICU level of care (LOC) to results of a cellular host-response test to stratify septic patients, researchers found that ruling out sepsis based on ICU level of care would have missed 57% of the patients who were ultimately diagnosed as sepsis.
“Sepsis is a fast-progressing condition that mimics other diseases and can be deadly if not addressed quickly and properly,” said pulmonary and critical care physician Robert Scoggins, MD, PhD at Kootenai Health. “Simply knowing that a patient is in need of ICU resources – such as ventilation, renal replacement therapy or vasopressors – tells you nothing about the cause of their condition. In fact, using emerging tools that correlate with ICU level of care likely provides limited value beyond measuring patients’ lactate level. There are more accurate ways to determine risk of sepsis. Specifically, there is a U.S. Food and Drug Administration (FDA)-cleared cellular host-response test that enables clinicians to more accurately risk-stratify patients, ensuring they get the proper disease-specific treatments and ultimately improving outcomes.”
Accurate and timely detection requires a specific test for sepsis
Sepsis is a dysregulated host immune response to infection that leads to life-threatening organ dysfunction and is the leading cause of in-hospital death. Most cases present initially to emergency departments (EDs), but symptoms, including fever, rapid heart rate and breathing, and low blood pressure, are not specific to sepsis. This makes diagnosis difficult, particularly in the early stages, which can impact patient outcomes. The risk of death increases by up to 8% for each hour that septic shock treatment is delayed, while treating non-septic patients for sepsis can result in further medical complications and death.
This retrospective study compared the accuracy of ICU LOC and a cellular host-response test (IntelliSep®) to determine which risk stratification approach is most accurate in predicting sepsis using data from 730 adult patients with suspected infection who presented to the ED. Researchers demonstrated in this study that:
If a provider used “no need for ICU LOC” as an indicator to rule out sepsis, 57% of patients who went on to develop sepsis would have been missed and 30% of sepsis deaths were in this subpopulation.
If a provider used IntelliSep Band 1 as an indicator to rule out sepsis, only 5% of patients who went on to develop sepsis would have been missed and 0 sepsis deaths were in this subpopulation.
“Doctors on the front lines need tests to aid in rapid decision making. We have these for stroke and heart attack, allowing us to quickly determine what’s wrong and put patients on the right path,” said Hollis “Bud” O’Neal, MD, MSc, associate professor of Medicine at Louisiana State University Health Sciences Center and medical director of research for OLOLRMC, who was one of the authors of the study. “Cellular host-response tests are filling this void for determination of sepsis, helping us accurately assess both the potential risk and severity of sepsis for patients in critical condition and determine the proper course of treatment.”
OLOLRMC is leveraging Cytovale®’s IntelliSep, the first and only U.S. Food and Drug Administration (FDA)-cleared cellular host response diagnostic indicated for use as an aid in the early detection of sepsis within the Emergency Department (ED). Within the first year of IntelliSep use, OLORMC reported significant clinical improvements, including improved patient outcomes with lower mortality rate for sepsis patients, faster treatment and shorter hospital stays.
“Because IntelliSep provides a metric of immune dysregulation, it may provide superior and more actionable risk-stratification information for the management of potentially septic patients than using ICU LOC,” said Dr. O’Neal.
This study (Abstract 278) will be presented during SHM Converge on Wednesday, April 23 at 12:10 p.m., Screen F, Converge Central (Oceanside A) at the Mandalay Bay Resort and Casino in Las Vegas.
#healthcare industry events 2025#hospital and healthcare magazine#healthcare industry trends#ICU care for sepsis#SHM Converge conference 2025
1 note
·
View note
Text
Patients With Long-COVID Show Abnormal Lung Perfusion Despite Normal CT Scans - Published Sept 12, 2024
VIENNA — Some patients who had mild COVID-19 infection during the first wave of the pandemic and continued to experience postinfection symptoms for at least 12 months after infection present abnormal perfusion despite showing normal CT scans. Researchers at the European Respiratory Society (ERS) 2024 International Congress called for more research to be done in this space to understand the underlying mechanism of the abnormalities observed and to find possible treatment options for this cohort of patients.
Laura Price, MD, PhD, a consultant respiratory physician at Royal Brompton Hospital and an honorary clinical senior lecturer at Imperial College London, London, told Medscape Medical News that this cohort of patients shows symptoms that seem to correlate with a pulmonary microangiopathy phenotype.
"Our clinics in the UK and around the world are full of people with long-COVID, persisting breathlessness, and fatigue. But it has been hard for people to put the finger on why patients experience these symptoms still," Timothy Hinks, associate professor and Wellcome Trust Career Development fellow at the Nuffield Department of Medicine, NIHR Oxford Biomedical Research Centre senior research fellow, and honorary consultant at Oxford Special Airway Service at Oxford University Hospitals, England, who was not involved in the study, told Medscape Medical News.
The Study Researchers at Imperial College London recruited 41 patients who experienced persistent post-COVID-19 infection symptoms, such as breathlessness and fatigue, but normal CT scans after a mild COVID-19 infection that did not require hospitalization. Those with pulmonary emboli or interstitial lung disease were excluded. The cohort was predominantly female (87.8%) and nonsmokers (85%), with a mean age of 44.7 years. They were assessed over 1 year after the initial infection.
Exercise intolerance was the predominant symptom, affecting 95.1% of the group. A significant proportion (46.3%) presented with myopericarditis, while a smaller subset (n = 5) exhibited dysautonomia. Echocardiography did not reveal pulmonary hypertension. Laboratory findings showed elevated angiotensin-converting enzyme and antiphospholipid antibodies. "These patients are young, female, nonsmokers, and previously healthy. This is not what you would expect to see," Price said. Baseline pulmonary function tests showed preserved spirometry with forced expiratory volume in 1 second and forced vital capacity above 100% predicted. However, diffusion capacity was impaired, with a mean diffusing capacity of the lungs for carbon monoxide (DLCO) of 74.7%. The carbon monoxide transfer coefficient (KCO) and alveolar volume were also mildly reduced. Oxygen saturation was within normal limits.
These abnormalities were through advanced imaging techniques like dual-energy CT scans and ventilation-perfusion scans. These tests revealed a non-segmental and "patchy" perfusion abnormality in the upper lungs, suggesting that the problem was vascular, Price explained.
Cardiopulmonary exercise testing revealed further abnormalities in 41% of patients. Peak oxygen uptake was slightly reduced, and a significant proportion of patients showed elevated alveolar-arterial gradient and dead space ventilation during peak exercise, suggesting a ventilation-perfusion mismatch.
Over time, there was a statistically significant improvement in DLCO, from 70.4% to 74.4%, suggesting some degree of recovery in lung function. However, DLCO values did not return to normal. The KCO also improved from 71.9% to 74.4%, though this change did not reach statistical significance. Most patients (n = 26) were treated with apixaban, potentially contributing to the observed improvement in gas transfer parameters, Price said.
The researchers identified a distinct phenotype of patients with persistent post-COVID-19 infection symptoms characterized by abnormal lung perfusion and reduced gas diffusion capacity, even when CT scans appear normal. Price explains that this pulmonary microangiopathy may explain the persistent symptoms. However, questions remain about the underlying mechanisms, potential treatments, and long-term outcomes for this patient population.
Causes and Treatments Remain a Mystery Previous studies have suggested that COVID-19 causes endothelial dysfunction, which could affect the small blood vessels in the lungs. Other viral infections, such as HIV, have also been shown to cause endothelial dysfunction. However, researchers don't fully understand how this process plays out in patients with COVID-19.
"It is possible these patients have had inflammation insults that have damaged the pulmonary vascular endothelium, which predisposes them to either clotting at a microscopic level or ongoing inflammation," said Hinks.
Some patients (10 out of 41) in the cohort studied by the Imperial College London's researchers presented with Raynaud syndrome, which might suggest a physiological link, Hinks explains. "Raynaud's is a condition of vascular control or dysregulation, and potentially, there could be a common factor contributing to both breathlessness and Raynaud's."
He said there is an encouraging signal that these patients improve over time, but their recovery might be more complex and lengthy than for other patients. "This cohort will gradually get better. But it raises questions and gives a point that there is a true physiological deficit in some people with long-COVID."
Price encouraged physicians to look beyond conventional diagnostic tools when visiting a patient whose CT scan looks normal yet experiences fatigue and breathlessness. Not knowing what causes the abnormalities observed in this group of patients makes treatment extremely challenging. "We need more research to understand the treatment implications and long-term impact of these pulmonary vascular abnormalities in patients with long-COVID," Price concluded.
#long covid#covid#covid news#mask up#pandemic#covid 19#wear a mask#public health#sars cov 2#still coviding#coronavirus#wear a respirator#covid conscious#covid is airborne#covid isn't over#covid pandemic#covid19#covidー19
99 notes
·
View notes
Text
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes
Text
youtube
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes
Text
youtube
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes
Text
youtube
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes
Text
youtube
Many doctors use injections, is it really needed? How effective is it?
In public interest, we are bringing you a video series on Tuberculosis, featuring expert Dr. Rajendra Prasad, addressing all your questions and breaking the stigma surrounding TB.
Brief About Dr. Rajendra Prasad:
Professor (Dr.) Rajendra Prasad is a distinguished member of the Internal Advisory Committee of the Help U Educational and Charitable Trust.
A towering figure in the field of Pulmonary Medicine in India, Prof. Rajendra Prasad currently serves as the Director of Medical Education and Professor in the Department of Respiratory Medicine at Era’s Lucknow Medical College and Hospital. He also holds the esteemed position of Emeritus Professor at the National Academy of Medical Sciences, India. His pioneering work has left an indelible mark on medical education, research, and patient care in the country.
With an illustrious career spanning nearly five decades, Prof. Prasad has held several prestigious positions, including:
Director, Vallabhbhai Patel Chest Institute (VPCI), Delhi
Head of Pulmonary Medicine, King George’s Medical University (KGMU), Lucknow
Director, U.P. Rural Institute of Medical Sciences and Research, Saifai
His academic journey began at KGMU, Lucknow, where he completed his MBBS in 1974 and MD in 1979, later advancing his expertise in Pulmonary Medicine, Fiberoptic Bronchoscopy, and Lung Cancer with further training in Japan.
A pioneer in Tuberculosis research and control, Prof. Prasad played a key role in shaping the Revised National Tuberculosis Control Programme (RNTCP), now known as the National Tuberculosis Elimination Programme (NTEP). He was instrumental in establishing the DOTS Center at KGMU, one of the first medical college-based centers in India. A leading advocate for integrating both government and private medical colleges in the TB elimination effort, he currently serves as:
Vice Chairman, National Task Force for Medical Colleges in NTEP
Chairman, Uttar Pradesh Tuberculosis Association
Prof. Prasad's influence extends globally. He has served as the International Governor of the American College of Chest Physicians (USA) and is recognized worldwide as an authority in Pulmonary Medicine. He holds the unique distinction of having presided over all major Indian scientific bodies in the field, including:
National College of Chest Physicians, India
Indian Chest Society
Indian College of Allergy, Asthma & Applied Immunology
Indian Association for Bronchology
Tuberculosis Association of India
His academic and research contributions are prolific. Prof. Prasad has supervised over 215 research studies and authored more than 600 original articles, reviews, and book chapters. He has written 12 books, including four on Tuberculosis, an Atlas on Fiberoptic Bronchoscopy, and a Manual of Chest X-rays based on Indian patients. His work has been globally recognized—Stanford University ranked him among the top 2% of scientists worldwide, both in career-long and recent-year rankings. His academic metrics include:
7,632 citations
H-index: 45
i10-index: 182+
Under his leadership at KGMU, he established several pioneering services in Uttar Pradesh, including:
Video Bronchoscopy (First in the state)
Medical Thoracoscopy
Thoracic Oncology Unit
Air Pollution-Related Disease Diagnostic Center
Sleep Lab
These contributions earned him the title of “Father of Pulmonary Medicine” in Uttar Pradesh, and his former students—now leading pulmonologists across India—regard him as a deeply inspiring mentor.
Prof. Prasad’s relentless dedication to medicine and public health has been honored with over 75 prestigious awards, such as:
Dr. B.C. Roy National Award
Lifetime Achievement Awards from multiple national organizations
Vigyan Gaurav Award, Council of Science & Technology, Government of Uttar Pradesh
UP Ratna Award
O.A. Sarma Oration Award
M. Santosham Oration Award
Dr. Reddy’s Lung Cancer Oration Award
Dr. R.V. Rajam Academic Oration Award, National Academy of Medical Sciences, India
Prof. Rajendra Prasad’s journey is a testament to excellence, perseverance, and an unwavering commitment to medical science. His legacy continues to shape the future of Pulmonary Medicine and serves as an inspiration to generations of doctors, researchers, and healthcare leaders across the world.
#DrRajendraPrasad #टीबीमुक्तभारत #TBMuktBharat #EndTB #StopTB #FightAgainstTB #TuberculosisFreeIndia #TBFreeIndia #StepTowardsTBMuktBharat #TBElimination #NTEP #HealthForAll
#TBHaregaDeshJeetega #PulmonaryMedicine #MedicalEducation #TuberculosisControl
#narendramodi #PMOIndia
#YogiAdityanath #UPCM
#IACM #InternalAdvisoryCommitteeMember
#helputrust #HelpUEducationalandCharitableTrust
#KiranAgarwal #DrRupalAgarwal #harshvardhanagarwal
www.helputrust.org
0 notes