#Gutdysbiosis
Explore tagged Tumblr posts
Text
Exercise Effects on Gutdysbiosis, Intestinal Permeability and Systemic Inflammation in Patients with Type 2 Diabetes: A Pilot Study

Authored by Evasio Pasini
Abstract
Exercise plays a significant role in the prevention of the diabetes. Recent data propose that dysbiosis of intestinal microbiota composition contributes to development of Type 2 diabetes (T2D). Moreover, dysbiosis alters intestinal endothelium permeability causing the “Leaky gut syndrome” (LGS). We measured in 15 selected patients with standard medical cures for sable T2D the effects of 6 months of endurance, resistance and flexibility training on the gut microbiota composition and intestinal permeability. At baseline, T2D patients had high biochemical parameters (glycaemia, HOMA index, HbA1c, C-Reactive Protein [CRP]) with dysbiosis (elevated concentration of Mycetes) and altered intestinal impermeability (Measured by faecal Zonulin). Alter chronic exercise, glycaemia, HOMA index, HbA1c and CPR were reduced as well as faecal presence of Mycetesspp and Zonulin. This pilot study showed that selected patients with T2D had intestinal dysbiosis with overgrow of Mycetes, presence of LGS and low grade inflammation. Interestingly, chronic exercise significantly reduced all these parameters.
Keywords: Exercise; Diabetes; Microbiota; Dysbiosis; Zonulin; Leaky gut syndrome
Go to
Introduction
Evidences show that exercise plays a significant role in the prevention of the diabetes and control of glycaemia as well as in the diabetes-related organ complications [1]. Furthermore, recent data propose microbiota composition as possible potential environmental contributor to development of T2D [2]. Indeed, gut dysbiosis influences fundamental intestinal functions as epithelium permeability, causing the “Leaky gut syndrome” (LGS) [3]. As consequence, LGS heavily influences gut functions including digestive, absorptive and endocrine activities that, in turns, may influence glucose metabolism. Moreover, LGS activates inflammation allowing translocation of microorganisms from the intestinal lumen to the blood circulation. Interestingly, recent papers show that physical activities could modify gut microbiota [4,5]. Recent evidences suggest that a useful method for assessing the alteration of intestinal permeability is the dosage of Zonulin in the patient’s stools [6]. Thus, the aim of this study was to evaluate the role of chronic exercise on the gut flora composition and intestinal permeability in patients with stable T2D.
Go to
Materials and Methods
This research was a controlled open-label trial. Research protocol was approved by the Ethics Committee of Spedali Civili di Brescia, and performed in accordance with the Declaration of Helsinki. We selected non-smokers 15 males patients with mean age of 69±1.3 years with a controlled diet of 7949kJ (1900 kcal) derived from 40-60% carbohydrates, 30% fat and 10-20% protein. About 20g/1000kcal of fibre were present.
Patients had diagnosis of T2D for at least 2 years, no need for insulin therapy, arterial hypertension and dyslipidemia controlled by statins and either ACE-inhibitors or angiotensin receptor blockers, absence of diabetes-specific complications and/or ischemic heart disease and ability to perform physical activities. Patients with endocrine disorders and inflammatory or malabsoptive intestinal diseases were not included in the study. Patients studied did not used antibiotic, steroid, laxative, antidiarrheal and/or probiotic treatment over the previous 3 months and during the study. Biochemical measurements and gut flora was determined as we described before [7]. Measurements of biochemical variables, including C-reactive protein (CRP) as marker of systemic inflammation, were performed in peripheral venous sample after 12-h overnight fast.
Gut Flora were determined in stool sample collected with strikers and inserted in a hermetic vials with a specific medium. Then, microbiota were counted after 48h of incubation at proper condition with a selective agar. A further proof of the isolation was performed with bacterial metabolic tests performed on isolated organisms through “BBL Crystal Identification System” (Becton Dickinson NJ USA). The results are expressed in CFU (Colony Forming Units)/ml of stool. The test was performed by laboratory of clinical and virology Functional Point (Bergamo. Italy) which follows international standard of quality control and it is accredited with the national health system. The tests reproducibly was <9%. LIS was measured as faecal Zonulin concentration (ng/ml) using a commercial ELISA kits (Immunodiagnostic AG, Bensheim, Germany).
T2D patients were treated with standard medical care. They have optimal glycaemic, lipid, blood pressure and body weight targets according to the international guidelines. The training program was of six months of endurance, resistance and flexibility training, following the most recent guidelines of the Italian Society of Diabetology and Medical Diabetology Association as described in details elsewhere [8]. Breathy, endurance training involved cycling on mechanically braked cycle ergometers while wearing heart rate monitors, at the intensity individually prescribed according to the baseline results of the exercise test. Time of exercise has been increased progressively in the first 3 months, starting from 15 minutes and reaching the target of 35 minutes.
Resistance training was of 40 to 50 minutes of different exercises which involved the major muscle groups (upper limb, lower limb, chest, back and core). Exercises included both calisthenics and repetitions with ankle weights, dumbbells and elastic bands. Patients started with 3 sets of 8 repetitions, then progressively improved to 3 sets of 12-15 repetitions. Flexibility training was of static stretching exercises that involved upper and lower body, performed before and after the resistance training exercise. All training sessions were performed in a hospital-based setting and under the supervision of specialized personal. Exercises was performed 3-time a week of about 90 minutes each section. To assess the statistical significance of differences between the variables measured before starting the excise programs (baseline =T0) and after 6 months of exercise training (T1), we used Student’s t-test for paired samples. A value of p <0.05 was considered statistically significant.
Go to
Results
As expected, at baseline (TO), T2D patients showed altered biochemical parameters (glycaemia, HOMA index, HbA1c, CRP) (Table 1). In addition, these patients had dysbiosis with little reduction of Lactobacillus and presence of pathogenic gut flora as documented by the high concentration of Mycetes spp. In addition, T2D patients showed higher Zonulin concentration in the stool suggesting altered intestinal impermeability (Table 2). Six mounts of exercise training (T1) improved glycaemia, HOMA index and HbA1c in T2D patients. Interestingly, exercise attenuated systemic inflammation measured as CRP also (Table 1). Furthermore, chronic exercise increased the intestinal concentration of Lactobacillus and significantly reduced Mycetesspp and Zonulin concentration (Table 2).
nv= Normal Value
nv = Normal Value
Go to
Discussion
This pilot study showed that selected patients with T2D had intestinal dysbiosis with overgrow of mycetes, presence of “Leaky gut syndrome” and chronic inflammation. Interestingly, chronic exercise significantly reduced all these parameters. Previous studies show that dysbiosis is present in T2D patients [9,10]. In line with these data, we found a massive presence of mycetes and candida in T2D patients, and inflammatory index. It is well known that gut mycetes stimulate systemic inflammation. Indeed, mycetes activates the innate immune receptor C-Type Lection Dectin-1. In detail, Dectin-1 is a cell receptor which reacts with B-1,3-glucans which is presents in the fungi wall. In turns, Dection-1 stimulates intracellular caspase recruitments domain-containing protein 9 with consequent local and generalised activation of inflammation due to inflammatory cytokine production and consequent stimulation of T helper 17 [11]. Notably, systemic inflammation is present in diabetic patients and it is consider one of the possible pathophysiological cause of this metabolic syndrome [2]. In addition, local intestinal inflammation could induce altered intestinal importability with consequent loss of gut fundamental functions. Indeed, for the first time in these patients, we found increased Zonulin’s faecal concentration suggesting the presence of “Leak gut syndrome”. Indeed, Zonilin is the proteins that physiologically modulates the intracellular intestinal cells tight junctions [6]. Traditionally, the functions of intestinal tract is the digestion and abortions of the ingested nutrients. However, recent evidences show that intestine regulates the immune and endocrine system by producing specific inflammatory molecules and/or hormones. In addition, it regulates the trafficking of macromolecules and/or microorganism between intestinal lumen and blood influencing systemic inflammation. It is intuitive that maintenance of intestinal impermeability and functions is crucial to maintain global metabolic body homeostasis avoiding the presence of “Leak gut syndrome” and the consequence malfunction.
It is known that exercise controls glycaemia and inflammation but here, for the first time, we showed that exercise decreases gut mycetes colonisation and the presence of “Leak gut syndrome” in T2D patients, likely improving important intestinal functions. The mechanisms by which exercise modified gut flora and reduced is not known yet. Recent data shows that exercise influences microbiota by several mechanisms. Indeed, exercise may modify bile acids profiles [12] and/or faecal short chain fatty acids (SCFAs) as butyrate [13]. Exercise may also interact with gut immunological function increasing intestinal immunoglobulin A (IgA), decreasing number of lymphocytes-B and CD4+T cells, and influencing gene expression of cytokines as IL-6, Il-4, IL-10 and TGF-B [14]. Exercise can also modify microbiota because is able to reduce intestinal transit time [15].
We think that our data, although preliminary, could have important clinical implications. Indeed, for the first time, we showed that patients with T2D have heavy intestinal mycetes colonisation and LIS, and chronic exercise can reduced these alteration. This likely could improving intestinal function which influence nutrients metabolism, hormonal production and absorption of oral drug-administered. So, exercise, with or without a specific therapies able to cure of intestinal microbiota, could be an important step for tailored therapy allowing traditional therapy and patients metabolism to function more properly.
This study has some limitations. We used a selective culture medium to identify bacteria and mycetes instead of molecular biology techniques. Indeed, we don’t want to provide a “faecal finger print” of patients. We won’t identify saprophytes and some minor intestinal pathological and mycetes species capable of stimulating inflammation without gastrointestinal symptoms [7]. This is a pilot study with a limited number of selected patients. We have in progress a large scale study to confirm these results.
For More articles in Current Research in Diabetes & Obesity Journal Please click on: https://juniperpublishers.com/crdoj/index.php
For more about Juniper Publishers please click on: https://juniperpublishers.com/video-articles.php
0 notes
Text
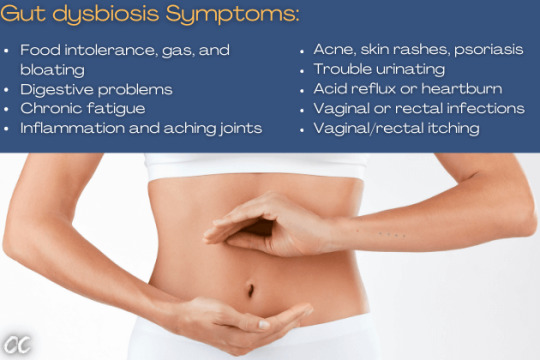
Gut dysbiosis
a symptoms of gut problems. Symptoms of gut dysbiosis include food intolerance, gas, and bloating, and other digestive problems.
Gut disbiosys not only disturbs our mood, metabolism, libido, immunity, and even causes mental fog, but it also affects our ability to process the carbohydrates.
Read more at: https://obesity.coach/weight-loss-diet/
#Gutdysbiosis#gutproblems#gutissues#foodintolerance#bloating#obesityresearch#obesitynomore#obesitycenter#obesitydoctor#overweightpeople#overweightproblem#overweightdating#overweighted#weightlossthatworks#weightlossblogger#weightlossproblems#type2diabetesawareness#type2diabetesdiet#type2diabetesremission#bloodsugarrecipe#bloodsugarrecipes#bloodsugarcontrol#bloodsugars#complexcarbsandproteins#complexcarbsaregoodforyou#ObesityCoach'#NourishingKAKA#obesediabetesmantra#ObeseDiabetesMantra
0 notes
Photo

How’s this for a testimonial??? #Repost @dctrgrmln with @make_repost ・・・ One of the best probiotics on the market along with Elixa. Start off slow with this one. I recommend a third of the dose and titrate up. Most people have gut dysbiosis so this can lead to a lot of issues. Really good for balancing fungal issues as well. @teraganix knocks it out of the park with this one. #probiotics #proem1 #teraganix #digestive #digestivehealth #labs #photosynthetic #ibs #crohnsdisease #intestinalhealth #shelfstable #nongmo #organicprobiotics #organicsupplements #candidaovergrowth #gutdysbiosis https://www.instagram.com/p/CEDADJNBCEN/?igshid=1ox9fcu4muc3c
#repost#probiotics#proem1#teraganix#digestive#digestivehealth#labs#photosynthetic#ibs#crohnsdisease#intestinalhealth#shelfstable#nongmo#organicprobiotics#organicsupplements#candidaovergrowth#gutdysbiosis
0 notes
Text
Leaky Gut Syndrome
Leaky Gut Syndrome occurs when you have increased intestinal permeability. Now, what is meant by increased intestinal permeability? It is either a genetic or acquired condition when the intestinal linings of our body become faulty or ‘leaky.’ [caption id="attachment_2174" align="aligncenter" width="700"]

Leaky Gut Syndrome occurs when you have increased intestinal permeability[/caption] Leaky gut, in recent years, has been related to gut dysbiosis. In healthy subjects, the intestinal wall of the GI tract shows a tight barrier. It hinders the passage of toxins, undigested food particles, and other potentially harmful products into the blood. Therefore, these particles migrate to various parts of the body. Due to increased intestinal permeability, the junctions in between the cells of the linings get porous. Which results in sensitive substances passing through it and cause various health problems. These toxins are identified by our immune system as foreign invaders and results in inflammation.
Leaky Gut Syndrome: Causes, Symptoms and How to heal it?
The leaky gut syndrome typically causes bloating, cramps, gas, stomach pain and aches and food sensitivities. Though this is not a medically approved disease or health problems it is an area undergoing extensive research and is of much importance considering modern lifestyles. What are the Causes? Certain foods may trigger digestive imbalance. Gluten is a primary cause of Leaky Gut syndrome Dairy products and excessive sugars may lead to inflammation Infections like an overgrowth of the harmful yeast Candida in the gut and deplete the natural microflora of the gut and cause the digestive disorder Stressful lifestyle with unhealthy food habits Environmental toxins like mercury, pesticides, BPA from plastic that enters our body through food Medications like steroids, Motrin, antibiotics, acidity reducing medicines, Anvil, aspirin can prove to be toxic Genetics, certain people are more sensitive to environmental and other food allergies that cause autoimmune inflammation Alcohol abuse [caption id="attachment_2183" align="aligncenter" width="731"]

Certain foods may trigger digestive imbalance which causes Leaky Gut syndrome[/caption] Symptoms of Leaky Gut Syndrome Though not proven medically, studies show that leaky gut syndrome may be the root of various digestive and other diseases. The symptoms that may be diagnosed as a Leaky Gut are as follows. Development of SIBO (small intestine bacterial outgrowth). Gastric ulcers. Bloating, cramps and stomach pain. Infectious diarrhea. Irritable bowel syndrome or IBS. Chronic fatigue leading to fibromyalgia. Asthma. Skin problems like psoriasis, eczema. Diabetes problems both Type I and Type II. Mental problems like anxiety, ADD, ADHD, depression. Arthritis and joint pain. Esophageal and colorectal cancer. Obesity and obesity-related diseases like fatty liver, cardiovascular disease. People with celiac and Crohn’s disease. There are controversies about the role of Leaky Gut Syndrome in causing various disease outside the GI tract. But evidence shows otherwise. Autoimmune diseases like Lupus, Multiple Sclerosis, rheumatoid arthritis is triggered by Leaky Gut Syndrome. The protein behind this is called ‘Zonulin.’ This protein breaks down the intestinal cellular joints to cause intestinal hyperpermeability. Gluten is a chief container of zonulin. Autism may also be associated with cases of Leaky Gut Syndrome. Thyroid disorders like Hashimoto’s disease which causes hypothyroidism, metabolic disbalance, obesity, depression, and fatigue. Nutritional deficiencies like Vit B12, digestive enzymes, magnesium may be caused by a Leaky Gut. Diets for Leaky Gut Syndrome The primary treatment for curing a leaky gut is to change your diet to a healthier one. This can be achieved in the following ways. Cutting down the sugar intake to deplete the Candida overgrowth. Apple cider vinegar. It creates an acidic environment and hence kills harmful bacteria. Coconut contains many antimicrobial agents that help to cure a leaky gut. L-glutamine supplement that helps to repair a faulty gut lining. Lots of vegetables like broccoli, Brussels sprouts, carrots, kale, zucchini, mushroom, eggplant, beetroots. Roots and tubers like yams, potatoes, and turnips. Sprouted seeds like chia seeds, flax-seed, sunflower seeds, pumpkin seeds, and others. Fresh fishes. Gluten-free foods like brown rice, buckwheat, sorghum, gluten-free oats, teff, and amaranth. Fruits like berries, kiwi, pineapple, orange, citrus fruits, passion fruit, papaya, and mandarin. Avocado, extra virgin olive oil, coconut oil all contain healthy fats. Raw nuts like almonds, peanuts, and pistachios. Healthy beverages like bone broth, tea, kombucha are helpful. Licorice roots an important herb that reinforce the intestinal linings. Collagen supplements may help in building new tissue within the intestine. [caption id="attachment_2184" align="aligncenter" width="500"]

Having raw nuts keeps you healthy and fit[/caption] Foods to Avoid? Products and Foods that should be avoided to prevent the occurrence of Leaky Gut Syndrome are listed below: Alcohol intake should be lowered. Restaurant sauces and salad dressings and fast foods like pizza, burger, and potato chips should be avoided as most of them contain gluten. Baked foods like muffins, cakes, pies, pastries contain an overload of sugar. Processed meats like cold cuts and deli meats, bacon, hot dogs contain saturated fats and are harmful. Various wheat products like bread, sugary cereals, couscous, wheat flour contains gluten. Refined oils like canola and sunflower oils. Carbonated drinks and sugary drinks should be avoided. Dairy products like milk, cheese, ice cream. Artificial sweeteners like aspartame, saccharin, and sucralose. Unhealthy snacks like crackers, popcorns, pretzels, muesli bars, etc. Glutinous cereals like barley, seitan, oats, rye, and bulgur. Read the full article
0 notes
Text
Mood Imbalances in Children
Suzanne Sparrow, Nutritionist & Naturopath; 20th August, 2019

We know, as adults, we often experience mood swings; highs and lows that may be exacerbated by our environment eg. stress at work, fighting with a spouse, a messy house. But most of us have “tools” to deal with these highs and lows, whether that’s seeking counselling, talking to a friend, going for a walk, taking a bath, or doing some meditation. Kids, on the other hand, are often not equipped with these “tools”. That, coupled with their underdeveloped emotional regulation and maturity, and their inability to express how they’re feeling, can mean that the mood imbalances they experience can be even more intense and harder for them to regulate. Add in external factors, such as poor nutrition and sleep quality, and things can spiral out of hand pretty quickly.
So what can we, as parents, teachers, minders and friends, do to help our kids regulate their moods?
* Focus on good nutrition: When I see kids with suspected mood disorders in clinic, the first thing I do is examine what they’re eating and drinking. And more specifically, what they’re NOT. Children with diets high in processed carbohydrates and refined sugars are more likely to suffer from anxiety and depression. Those who are fed a diet rich in complex carbohydrates, good quality protein, and a variety of healthy fats are less likely to suffer from depressive episodes, and the energy (and emotional) highs and lows that accompany the Standard Australian Diet (SAD, how apt!).
* Avoid problematic foods: Foods that cause an allergic response (eg. loose stools, skin rashes, runny nose) raise histamine levels in the body. And high histamine levels have been linked to brain inflammation and mood disturbances. Avoiding foods that cause such responses in your children, and supporting histamine metabolism with nutrients such as vitamin C and quercetin, can improve mood balance.
* Address infections: Gut dysbiosis (when the balance of bad bacteria in the gut outweighs the good) and underlying infections, such as streptoccus, can have a negative impact on mood. Antimicrobial / antiparasitic herbs, such as garlic, thyme, oregano and clove, can be an effective way to eliminate pathogenic bacteria and parasites - always work with a Naturopath or Herbalist to address gut dysbiosis in children using herbs.
* Good gut health: You’ll notice children often complain of having a “sore tummy”, even if what they’re feeling is a headache, low mood or anxiety. And we’ve all heard of the gut-brain axis by now, and how the two are intrinsically linked. Ensuring good gut health is a vital component of addressing childrens’ moods - make sure they are getting plenty of fibre and water so that they are having a bowel movement at least once a day, and eating probiotic foods (eg. yoghurt, apple cider vinegar, kombucha) or supplementing with a broad-spectrum probiotic.
* Sleep quality: Lack of sleep duration, and poor sleep quality, contribute to low mood in children, and are also linked to poor digestion and a variety of nutrient deficiencies. It is important that children have a bedtime routine that involves a wind-down period well before they are expected to go to sleep, which may involve turning off electronic devices, having a bath, reading a book, and “unloading” their day to mum or dad while having a cuddle in bed. Beautiful gentle herbs such as Passionflower and Chamomile may also be conducive to better quality sleep, as can magnesium.
* Stress: Being exposed to stress, or having a long history of stressful situations (eg. parents divorcing, the death of a close family member, being bullied at school), can cause low mood. It is important to understand what a child’s understanding of such situations is eg. whether they blame themselves, if they’ve received counselling as a result, what impact such events have had on their social interactions with other, their nutritional intake, etc.
* Exposure to toxins: Heavy metals, such as lead and mercury, can cause mood imbalances due to their accumulation in the brain. Conducting a hair tissue mineral analysis (HTMA) can give your practitioner a greater understanding of the toxic burden the child is carrying, and what can be done to support his/her detoxification from such toxins.
* Genetic considerations: Nutritional deficiencies coupled with certain genetic mutations (or “SNPs”) are also linked with mood imbalances in children, as they can result in altered production of neurotransmitters. It may be worthwhile having a genetic screening (a simple salivary test) done if you suspect this applies to your child.
In terms of specific nutrients, my top priority considerations are always zinc (especially for fussy eaters or children with behavioural disorders) and omega-3 fatty acids (for brain function and cognition). Other important nutrients to consider include magnesium, vitamin B6, vitamin B12 and vitamin D.
Think your child could benefit from a Naturopathic consult? Book online via my website, or call The Natural Health and Wellness Clinic in Somerville, VIC on (03) 5977-7342 to find a time that suits you - after-school consults available on Tuesdays and Wednesdays!
#mooddisorders#lowmood#moodhealth#childrenshealth#gutdysbiosis#sleepquality#moodimbalance#depression#anxiety#behaviouraldisorders#nutritionist#naturopath
0 notes
Text
Could gut health affect the way our immune system responds to COVID-19? Science says, yep, very likely! (Source below).

Keep an eye out for our upcoming workshops, as one will focus on gut health and how it affects even more than just our physical immunity!
#NaturAli #NaturAliHolistic #holisticliving #gutdysbiosis #gutimbalance #fixyourgut
0 notes
Photo

New on my Pinterest: New Studies @SurveyCircle http://bit.ly/2De7Qh7 : Participants needed for online survey! Topic: "Exploring the Potential Link Between Gut Dysbiosis and Human Behavior" http://bit.ly/2ULRUfG via @SurveyCircle #Microbiota #Microbiome #GutDysbiosis #Nutrition #BraingutAxis #GiDisease #Survey http://bit.ly/2CrC2ru #SurveyCircle #Research #Survey #Study #CallForParticipants #Participants #Respondents | Participate now: http://bit.ly/2UMu5EB
0 notes
Text
Past and Present
In the second half of 2015, I ended a multi-year relationship and for a time afterward went through a high-stress adjustment period which ultimately resulted in the development of persistent severe nodulocystic acne and some troubling digestive and cognitive issues, which I am actively working to solve.
Acne has been a presence in my life since I was a teenager, though it had always been fairly mild until more recently. As a younger person (I’m 29 now) I was prone to small, “normal” acne break outs and the occasional painful cyst on my face, scalp, back, or shoulders. As I have gotten older and began to experience higher levels of stress both in my job and personal life, there was a decrease in “normal” breakouts and a noticeable increase in the cystic variety, particularly on my jaw, lower cheeks, and chin. I am also prone to smaller pimples on either side of my forehead, though rarely in the middle, and deal with some pretty stubborn blackheads, clogged pores, and sebaceous filaments on a couple different areas of my face.
In terms of digestion, I had been having some trouble for 4-5 years prior to the aforementioned relationship’s end. Specifically I would become measurably bloated for several days after consuming certain foods and mysteriously began putting on extra weight even though I was eating a mostly healthful diet compared to most people. Certain things would give me terrible stomach aches, and others seemed to worsen my acne which was really nothing to write home about at that stage in my life, but seemed bad to me at the time. At the beginning of my experimentation, I decided that I was going to avoid wheat, dairy, tomatoes, and cinnamon, most of which were problem foods at some point in my earlier years and are known to be inflammatory. This seemed to work well for a time, and the mysteriously-gained weight came off within a few months of following those dietary restrictions with no other extra effort on my part. My skin was also not too bad at this point, and when I would break out a bit, I could pretty easily cover it with makeup.
Time passed, I dated a couple of different people, and spent more time than I probably should have drinking in bars, having a really wonderful time and rarely washing my makeup off before stumbling to bed. Eventually the stomach aches and bloating came back and the acne became a little more aggressive, but I still felt that I could handle it on my own. In response, I began limiting my diet even further, ultimately ending up on a Paleo diet with some additional restrictions based on my own observations about what I felt that I was “reacting” to. A “reaction” could be anything negative from getting a new pimple to brain fog to gaining a couple of pounds overnight that would persist for a few days afterward. I also started trying a lot of different facial care methods and products without much success.
To name a few things that I have tried over the years that did not “work” for me: the oil cleansing method (I have tried many different oils and combinations of them), Lush UltraBland Cleanser, Purity Made Simple Facial Cleanser, washing with water only, St. Ives Green Tea Scrub, Yes To Carrots Cream Cleanser, and more moisturizers than I can even begin to recall. None of these things really made my skin noticeably worse, but they were definitely not helping anything. I would also occasionally use Queen Helene Mint Julep mask as well as Aztec Secret Indian Clay Mask. Again, they did not seem to make my skin worse, and at times seemed to be helping somewhat, but ultimately neither led to the clear skin I was looking for. I have always been into more natural, higher quality products and so I mostly avoided the things aimed at acne that could be bought at a drug store as I felt that they would be drying or damaging to my skin in some way. Though I still prefer natural products whenever possible, I am much more focused on results at this point in the game.
In terms of mental and other symptoms, I have battled depression and anxiety to varying degrees on and off since middle school. I also experience transient brain fog, lack of motivation, fatigue, racing heart, cold hands/feet, irritability, poor concentration, pruritus, eczema, irregular menstruation, and difficulty retaining information. Probably to my own detriment, I have also always avoided doctors and preferred to sort things out on my own as much as possible.
The acne has gotten to the point that it is considered to be severe, and I am somewhat sad to say I have begun the process to get started on the controversial drug Isotretinoin (or Accutane) after a failed course of antibiotics which is something I would have avoided at all costs before, but have become desperate as I observe my face being overtaken with blemishes and scarring. Though I think that this will help get my skin clear, I do not think it addresses the root of the problem and it may not keep it from returning. It is my understanding that acne is typically an outward manifestation of internal issues such as gut dysbiosis or hormone imbalance. I have spent untold amounts of time researching acne, nutrition, health, etc. but am at a point where I can no longer proceed without additional testing and diagnosing which I can only get by working with health professionals. I also recognize that these issues have, in essence, taken over my life and stripped it of almost everything pleasurable, as well as jacked up my stress levels, which is detrimental to both my mental and physical well-being.
Needless to say, I am tired of living like this and intend to do everything I can to reclaim my health. Not only do I want to experience a higher quality of life, but I want my daughter to have a positive role model to look up to.
I will be writing here periodically about my journey back to health.
0 notes
Text
Participants needed for online survey! Topic: "Exploring the Potential Link Between Gut Dysbiosis and Human Behavior" https://t.co/giCCzHAsJB via @SurveyCircle #Microbiota #Microbiome #GutDysbiosis #Nutrition #BraingutAxis #GiDisease #Survey pic.twitter.com/IOztfi4rLv
— Daily Research (@daily_research) March 21, 2019
0 notes