#Group B Strep risks
Explore tagged Tumblr posts
Text
Group B Strep in Pregnancy: Testing, Risks, and Treatment Options
Group B Strep in PregnancyUnderstanding Group B StrepKey Facts about GBS:Testing for Group B StrepThe Testing Process:Rapid Testing Options:Risks Associated with Group B StrepPotential Risks to Newborns:Early-Onset vs. Late-Onset GBS Disease:Treatment Options for GBS in PregnancyAntibiotic Treatment:Alternative Approaches:Living with GBS: Beyond PregnancySymptoms and Signs of GBS Infection in…
#Group B Strep infection#Group B Strep prevention#Group B Strep risks#Group B Strep testing#Group B Strep treatment#maternal health#newborn health#pregnancy health
0 notes
Text
36+5
Hi there. We set up the crib yesterday and I just got a diaper pail for $5. I am spending a lot of time in the kitchen these days, craving fresh/homemade food, also getting the hang of sourdough. Knitting a hat for mei mei. Physically, I'm struggling a little. Achey belly, cervix pain, nausea, pain under my ribs. Not able to carry p for very long, not able to bend over or even wash dishes very comfortably.
I am SO happy to not be working anymore.
Quite stormy/rage-y and hormonally emotionally all over the place. Driving is hard. Really hoping I give birth just a little early, but I know that in the end everything will be just as it should be. I think I spent the last few weeks getting a second wind of energy (transitioning from total hibernation/exhaustion at around 32w), executing & planning etc. And once I've done most of my tasks I will probably transition into a sort of surrender state of waiting and being present. Sometime in the next few weeks.
Not much remains to be done. I mean, there's a lot I COULD do (reorganize the whole pantry & kitchen, for example). But strictly speaking, I only really need to pack my bag for the birth center, and even that I probably will only do partially, because most of the items I'm bringing are clothes, and I still need to wear them these next few weeks, BECAUSE SO FEW CLOTHES FEEL OK ANYMORE. I have some nice-to-dos, like give myself a haircut, or make granola bars and bone broth, but oddly I am not feeling too motivated to prep food in advance. Mostly because my parents will be here cooking/cleaning for a month and after that I feel fairly confident that I'll be able to cook and will have a better idea of what I want to eat. I probably will mostly prep bone broth & baked goods instead of proper meals, stuff I don't expect my mom to make. Essentially, I'm giving myself permission to do/not do a whole bunch of stuff depending on my motivation level.
Some things I *am* trying to prioritize are remaining fairly social / having people over quite regularly, walking my 5k steps at minimum every day, just taking this season of life in. Enjoying my firstborn. I am weirdly not worried at all about labor or birth, maybe slightly freaking out about postpartum life and how karl and I will do relationship-wise.
Feelings/thoughts about meimei....I am trusting that my relationship will develop and become its own thing in its own time. It's so hard to have many coherent thoughts about someone you've never "met". I have not very much information about her. I can think about what she represents...Phillipa becoming a big sister, a season of joy and life following a season of death and grief, the end of our very long ttc journey. Another car seat, another addition to our insurance policy, another childcare cost, the user of all the stuff we have sitting around the house. We're really happy with her English name and sort of giving up on her Chinese name.
In any case, I feel that she will come before the end of the month. The countdown is on. I don't feel like I look 9 months pregnant, same thing kinda happened with Phillipa. But my fundal height is tracking beautifully, so I am not concerned. Also, something totally unanticipated happened and I am NEGATIVE for group b strep! So no saline lock or antibiotics for me during labor, and I can go home as early as 6hours after birth! And it's just one less risk to worry about.
0 notes
Text
Diet and Lifestyle to Reduce Group B Strep Risk

Expectant mothers often seek ways to ensure a healthy pregnancy and safe delivery. One significant aspect of prenatal care involves reducing the risk of infections that can affect both the mother and the baby. Among these, Group B Streptococcus (GBS) poses a noteworthy risk. Taking precautionary measures to lower the risk of GBS is essential. By adopting a healthy diet and making specific lifestyle changes, pregnant women can strengthen their immune systems and reduce the likelihood of GBS colonization. This blog explores effective dietary and lifestyle strategies to help you minimize Group B Strep risk during pregnancy and promote a healthy pregnancy in the UK.
Importance of a Healthy Diet
A nutritious diet can strengthen the immune system and reduce the likelihood of GBS colonization. Here are some dietary tips for expectant mothers: Increase probiotic intake. Including probiotic-rich foods like yogurt, kefir, sauerkraut, and kimchi can support gut health and potentially reduce GBS colonization. Boost vitamin C consumption. Vitamin C enhances immune function and may help prevent infections. Include garlic in your diet. Garlic has natural antimicrobial properties. Adding raw or cooked garlic to meals can help combat harmful bacteria, including GBS. Stay Hydrated. Proper hydration is essential for overall health.
Lifestyle Changes for GBS Prevention
In addition to dietary adjustments, certain lifestyle changes can also help reduce the risk of GBS:
Practice good hygiene. Regular handwashing, especially before meals and after using the restroom, is crucial. Stay physically active. Regular physical activity boosts the immune system and promotes overall well-being. Gentle exercises like walking, swimming, and prenatal yoga can be beneficial for expectant mothers. Manage stress levels. Chronic stress can weaken the immune system. Practicing stress-reduction techniques such as meditation, deep breathing exercises, and adequate sleep can help maintain a strong immune response. Seeking professional guidance. While diet and lifestyle changes are beneficial, it is essential to seek professional medical advice for comprehensive GBS prevention. Regular check-ups and prenatal screening tests in the UK can help monitor and manage GBS risk effectively.
Conclusion
Reducing the risk of Group B Strep during pregnancy involves a combination of dietary and lifestyle changes. By including probiotics, vitamin C, and garlic, and staying hydrated, expectant mothers can strengthen their immune systems. Additionally, practicing good hygiene, staying physically active, managing stress, and avoiding harmful substances are crucial steps in GBS prevention. For more information on Group B Strep during pregnancy in the UK, contact the healthcare professionals at Concepto Diagnostics. They can provide expert guidance and support for a healthy and safe pregnancy journey in the UK.
Also Read: Comparing Different Methods of Group B Strep Testing
0 notes
Text
Which Tests Could Save Your Baby In The Third Trimester Of Pregnancy?

A normal pregnancy generally lasts for around 40 weeks. These weeks are divided into three trimesters where the weeks from 28-40 are considered the third trimester. This is one of the most emotionally and physically challenging periods due to constant Braxton-Hicks contractions, lots of baby movement, and breast tenderness. The fetus is in a head-down position during this trimester and most of its organs are now fully formed. In this stage, it is pivotal to increase the frequency of prenatal screenings by contacting a gynae doctor in Siliguri to ensure you and your baby’s health.
To prepare you for the baby’s arrival, the doctor will recommend you various screenings, blood tests, and urine tests to maintain your overall well-being. The third-trimester prenatal screening is also essential to select the best delivery procedure and make you ready for it. You must know that stable physical health during the third trimester is crucial for a complication-free delivery experience.
H2- Effective Tests Conducted During The Third Trimester Of Pregnancy
1. Routine screenings
The first thing that the doctor will recommend is to undergo a comprehensive routine screening. This screening will include a physical exam, blood tests, and urine tests. Some of the disorders that can be detected through these tests are hepatitis B, anemia, HIV, cystic fibrosis, chickenpox, and Rh factor of blood. Until the delivery, your glucose levels, blood pressure, and weight will also be continuously monitored.
2. Group B strep test
During the 35-37th week of pregnancy, Group B streptococcus screening is done. In this test, rectal and vaginal swabs are collected to check the presence of this bacteria. This test is important because group B strep is considered the main cause of serious infections in the newborn baby. Proper treatment of this health issue is essential to save your baby from hearing loss, intellectual disability, and impaired vision.
3. Contraction stress test
To check the impact of contractions on the heartbeat of the fetus, you can be advised to undergo a contraction stress test during the third trimester. In this test, the gynecologist in Siliguri will stimulate the uterus with the help of Pitocin. This earlier contraction test is done to see whether the heartbeat of the baby will be stable during real contractions or not. Certain heart problems can also be detected effectively during this test.
4. Nonstress test
The non-stress test is mainly recommended when the woman is experiencing a high-risk pregnancy. You must know that this is an effective test to evaluate the health status of the fetus. The main role of this test is to check whether the baby is getting enough oxygen or not. If the baby doesn’t respond properly during this test then the doctor might recommend additional screenings to determine the underlying issues.
5. Ultrasound
One of the most common tests that you will be experiencing from the beginning of the pregnancy till the end is ultrasound. This is the most effective and painless screening test which is conducted during the third trimester to look at the position and shape of the baby inside the uterus. Herein, multiple ultrasounds and biophysical profile (BPP) are done during this stage in case of high-risk pregnancy.
6. Electronic fetal heart monitoring
Another important test conducted during the third trimester is electronic fetal heart monitoring. This test is not only done during the 3rd trimester but also during labor and delivery to continuously monitor the heartbeat of the fetus. If a normal heartbeat is seen during the trimester then it is considered that the baby is doing well. Not all of these tests are done during the third trimester and to decide the best test for your pregnancy, you must consult the best gynae doctor in Siliguri. The doctor will inform you about the procedure, benefits, and risks of all the tests so that you can be comfortable while undergoing it.
0 notes
Text
NIPT and the Risk of Miscarriage: What You Need to Know

In recent years, non-invasive prenatal testing (NIPT) has revolutionized prenatal care by offering a safer and more accurate method for detecting genetic abnormalities in unborn babies. However, alongside its benefits, NIPT has raised concerns regarding the potential risk of miscarriage associated with the procedure. Understanding this risk is crucial for expectant parents as they navigate their prenatal care journey.
Therefore, in this blog post, we will look into the complexities of the nipt test in the UK and explore the real risks of miscarriage associated with this screening method.
All about NIPT
NIPT is a non-invasive prenatal screening test that analyzes cell-free DNA (cfDNA) from the mother's bloodstream to assess the risk of chromosomal abnormalities such as Down syndrome (Trisomy 21), Edwards syndrome (Trisomy 18), and Patau syndrome (Trisomy 13) in the fetus. Unlike traditional methods like amniocentesis or chorionic villus sampling (CVS), NIPT does not pose a risk of miscarriage because it involves a simple blood draw from the mother.

Understanding the risk
It's essential to distinguish between correlation and causation when examining the relationship between NIPT and miscarriage. While some studies have reported higher rates of miscarriage following NIPT, it's crucial to consider confounding factors such as maternal age, pre-existing medical conditions, and the indication for undergoing NIPT.
In cases where the nipt test identifies a high risk of chromosomal abnormalities, expectant parents may opt for invasive diagnostic procedures such as amniocentesis or CVS, which carry a small but inherent risk of miscarriage.

Role of health providers
Despite the lasting concerns, expectant parents need to make informed decisions about prenatal screening based on accurate information and professional guidance. Healthcare providers play a crucial role in educating expectant parents about the nuances of the NIPT test and helping them navigate the decision-making process. By providing comprehensive counselling and support, healthcare professionals can empower expectant parents to make choices that align with their values and preferences.

Summing Up,
NIPT represents a significant advancement in prenatal care, offering expectant parents a safer and more accurate method for detecting genetic abnormalities in their unborn babies. While concerns regarding the risk of miscarriage are valid, it's important to understand that the NIPT test in the UK itself does not pose this risk. Rather, it's the follow-up diagnostic procedures that carry a minimal but notable risk, which must be carefully considered in the context of each individual's situation. However, it's crucial to understand its limitations and interpret the results in consultation with a healthcare provider experienced in prenatal genetics. So now only get in touch with the genomics consultant at Concepto Diagnostics.
Also Read: What happens if you test positive for group B strep?
#nipt test uk#nipt london#illumina test uk#genetic test during pregnancy uk#nipt test accuracy#nipt test during pregnancy uk#downs syndrome test uk#group b strep during pregnancy uk
1 note
·
View note
Text
Due Dates & Induction Dates
I am currently due September 26th. As I have said before, my pregnancy was 100% healthy and smooth. I did not develop Gestational Diabetes, did not have/was not a carrier for Group Strep B, or did not have any signs of preeclampsia or blood pressure issues & gained an appropriate level of weight during my pregnancy.
So many people are asking me, why are they choosing to induce you if you had such a healthy pregnancy? New medicine/research.
The American College of Obstetricians and Gynecologists recommends that elective inductions in healthy pregnancies can be offered as early as 39 weeks pregnant. (Source: https://www.acog.org/womens-health/faqs/labor-induction)
When I was around 37 weeks pregnancy, my doctor checked by cervix for the first time and offered me the option of elective induction closer to my due date. At the time I wasn't really thinking about it ACTUALLY being a possibility. I told her I was open to it and from there she told me a scheduling representative will reach out to schedule.
Fast forward to now, September 20th, 2023. I am technically due in just 6 days; HOWEVER, I have shown absolutely no signs of labor. This Induction Date is seemingly becoming more real. I cannot explain the amount of research I personally have done on this topic in addition to reaching out to friends, colleagues and other OB/GYNs about this.
Of course, when I first heard the word "induction" I was absolutely terrified. My husband, family, and friends were all concerned for me. Most of which told me to deny the induction as it is my right as a patient to be able to. But once I dove a little deeper and found out my OWN personal benefits outweighs my risks of going over my due date I was more convinced.
My physician & the research I've done on my own suggested elective induction at 40 weeks due to my healthy pregnancy and to reduce the risk of placental issues and stillborn.
I thought I was going to be robbed of the experience of having myself spontaneously/chaotically go into labor at first. After some thought, I told my husband that I am more than okay with showing up to the hospital checking in as if it's a 5 star hotel, relaxed & my mind ready.
Of course, I do want to point out that I'm still hoping to go into labor naturally as this is "better for your body" or "the way God intended". But in moments like these, you start to forget about what it is that YOU want, and what it will take to ensure that your baby will be safe and healthy.
Please reach out/comment/message and tell me about your induction experience.
#mommy blogs#parenthood#parenting#parenting tips#babies#labor and delivery#labor#child birth#induction#birthstory#birth story#birth experience
1 note
·
View note
Text
Strep Throat (Streptococcal Pharyngitis)

I. Introduction to Strep Throat
A. Definition and overview
A bacterial infection called streptococcal pharyngitis, which affects the tonsils and throat, is brought on by Streptococcus pyogenes. Common in children and adolescents, it spreads through respiratory droplets or contact with infected surfaces. Severe painful throat, fever, and swollen tonsils are symptoms. Swabs taken from the throat can detect infections early, which enables quick antibiotic treatment and lowers the risk of sequelae like rheumatic fever. Practicing good hygiene and avoiding contact with infected individuals aid in prevention. Strep throat is treatable with antibiotics, ensuring a speedy recovery when the full course is completed.
B. Prevalence and common age groups affected

Strep throat is prevalent worldwide, with millions of cases reported annually. Children and teenagers between the ages of 5 and 15 are the ones that are most frequently affected. But it can also affect adults of any age, particularly those who are in close proximity to infected people or are in crowded places like daycare centers and schools.
II. Causes and Transmission

A. bacteria belonging to the group A streptococcus
A form of bacteria called Group A Streptococcus (GAS), commonly referred to as Streptococcus pyogenes, is to blame for a number of illnesses that affect people. It is one of the most prevalent organisms connected to strep throat (streptococcal pharyngitis), as well as other conditions like impetigo, cellulitis, and skin infections. GAS can spread through respiratory droplets or direct contact with infected individuals or contaminated surfaces. To stop the spread of the bacteria and associated side effects from GAS infections, prompt identification and adequate antibiotic treatment are crucial.
B. Modes of transmission
When an infected individual coughs, sneezes, or talks, respiratory droplets of Group A Streptococcus (GAS) are released into the air. It can also transmit through direct contact with infected saliva or nasal secretions, and by touching contaminated surfaces. Good hygiene practices, such as covering the mouth while coughing and frequent handwashing, can help prevent transmission.
III. Signs and Symptoms

A. A sour throat and difficulty swallowing: A sore throat and trouble swallowing are symptoms of strep throat, which is brought on by inflammation and infection of the tonsils and throat lining by the streptococcus bacterium.
B. Tonsils that are red and swollen: The inflammatory response to the Streptococcus bacterium that causes strep throat frequently results in tonsils that are red and swollen. The tonsils may look swollen and their surface may have white or yellow spots or patches.
C. Fever and chills: These symptoms typically accompany strep throat when the body’s immune system responds to the bacterial infection. Even though the body frequently experiences chills when attempting to regulate its temperature, the rise in body temperature helps the body fight the illness.
D. Body aches: Body aches and headaches are typical signs of strep throat. Inflammation brought on by the bacterial infection results in the release of certain chemicals, which can induce headache and broad bodily discomfort.
E. Rash (scarlet fever), occasionally: Strep throat can occasionally progress to scarlet fever, which is distinguished by a characteristic rash. The rash often begins on the chest and belly before spreading to other locations. It looks like little red dots and gives the skin a rough texture.
III. Diagnosis

A combination of clinical examination and laboratory tests are used to diagnose strep throat. The medical professional looks for typical signs such a sore throat, red and swollen tonsils, and swollen lymph nodes during a physical examination. They may also look for the presence of a scarlet fever rash.
In order to obtain a sample from the back of the throat, a throat swab is frequently used. This sample is then tested using a rapid strep test, which provides quick results within minutes. Even though a throat culture takes longer to complete (about 24–48 hours), it is sometimes used to confirm the diagnosis.
It is crucial to diagnose strep throat accurately to differentiate it from other throat infections and viral illnesses that may have similar symptoms. Early identification guarantees the administration of the proper medications to treat symptoms, shorten the course of the illness, and avoid problems related to streptococcal infections.
V. Complications

Strep throat, if left untreated or inadequately treated, can lead to several potential complications. The most serious complications include:
1. Rheumatic fever: An inflammatory condition that can damage the heart valves and other tissues, leading to long-term heart problems.
2. A kidney disease that produces inflammation and impairs the kidneys’ capacity to remove waste from the blood is post-streptococcal glomerulonephritis.
Peritonsillar abscess, otitis media (ear infection), sinusitis, and other less frequent side effects are also possible.
To prevent complications, early diagnosis and proper treatment with antibiotics are essential. To guarantee the elimination of the bacteria and lower the risk of problems, it is essential to finish the entire course of antibiotics as directed by the healthcare professional. Seeking medical attention for persistent or worsening symptoms is important to address any potential complications promptly.
VI. Treatment

Antibiotics are typically used to treat strep throat in order to get rid of the Streptococcus bacteria and reduce symptoms. Antibiotics including penicillin, amoxicillin, and cephalosporins are frequently administered. To ensure complete eradication of the germs and lower the risk of problems, patients are encouraged to finish the entire course of antibiotics.
In addition to antibiotics, over-the-counter painkillers such acetaminophen or ibuprofen for fever, sore throat, and body pains can be used to relieve symptoms. Throat lozenges or warm saltwater gargles may also help soothe the throat.
Regarding the role of Qme Healthcare Software System, it can streamline the diagnosis and treatment process for strep throat. Qme software may provide clinical decision support tools to aid healthcare providers in accurately diagnosing strep throat, interpreting test results, and determining appropriate antibiotic treatment. Additionally, the software system can help manage patient data, treatment plans, and follow-up care efficiently, improving overall patient outcomes and healthcare provider workflow.
A. Penicillin and amoxicillin are popular antibiotics recommended to treat strep throat. Other antibiotics include amoxicillin and erythromycin.
They target and eliminate the Group A Streptococcus bacterium responsible for the infection, helping to relieve symptoms and prevent complications when taken as prescribed.
B. Symptomatic relief (painkillers, throat lozenges, etc.): To treat the symptoms of strep throat, you can use over-the-counter painkillers like acetaminophen or ibuprofen to lower your temperature, soothe your sore throat, and ease body pains. Throat lozenges and warm saltwater gargles can help soothe the throat and provide temporary relief from discomfort.
VII. Prevention

Preventing strep throat involves several measures. Transmission can be reduced by following good hygiene habits such routine hand washing, covering the mouth and nose while coughing or sneezing, and avoiding close contact with infected people. Cleaning up after yourself on a regular basis and sanitizing frequently touched surfaces can help lessen the chance of contamination. Furthermore, receiving a vaccination against specific streptococcal diseases may add to your protection. People can be informed about the value of early diagnosis and treatment, which can result in fast management and stop the bacteria’s spread. The prevalence of strep throat and its possible consequences can be considerably decreased by a combination of preventive actions.
VIII. Prognosis and Recovery

With prompt and effective treatment, the prognosis for strep throat is typically very good. After beginning antibiotics, the majority of patients begin to feel better within a few days, and the infection is typically completely gone within a week. However, complications including rheumatic fever and kidney problems could develop in the absence of appropriate therapy. Completing the full course of antibiotics is crucial to prevent relapse and further spread of the bacteria. People can totally recover and go back to their regular activities with rest, water, and obedience to medical recommendations. Seeking medical attention for persistent or worsening symptoms is essential for a smooth recovery and to prevent potential complications.
IX. Conclusion

In conclusion, Group A Streptococcus, which causes strep throat, is a common and curable bacterial infection of the tonsils and throat. Timely diagnosis through tools like Qme Healthcare Software System can lead to appropriate treatment with antibiotics, providing effective symptom relief and preventing complications. Additionally, symptomatic relief with pain relievers and throat lozenges aids in easing discomfort during recovery. The prevalence of strep throat can be significantly decreased by taking preventive steps, such as maintaining excellent hygiene and getting vaccinated. Overall, early detection, proper treatment, and adherence to medical advice contribute to a positive prognosis and successful recovery, ensuring individuals can swiftly resume their daily activities with minimal disruption.
0 notes
Text
5 Tips for a Healthy Pregnancy: How to Reduce the Risk of Birth Defects
Structural or functional abnormalities that occur during gestation and are present at birth can lead to birth defects that can have a life-long impact on the health and well-being of a new-born baby. Birth defects can occur for various reasons, such as genetics, environmental factors, or a combination of both. According to the World Health Organization, in India, more than 1.7 million children are born with birth defects every year.
Reducing the risk of birth defects is crucial for promoting the health and well-being of both mothers and babies. There are several steps that expectant parents can take to reduce the risk of birth defects, and in this blog post, we will outline five tips that can help.
1. Get early and regular prenatal care
Benefits of early and regular prenatal care
Getting early and regular prenatal care is crucial for promoting a healthy pregnancy and reducing the risk of birth defects. Prenatal care involves regular medical check-ups, screenings, and tests to monitor the health of the mother and the developing foetus. Early prenatal care can help healthcare providers detect and manage any potential health issues before they become more serious. Early prenatal care can also help prevent complications and ensure that any existing medical conditions are managed appropriately.
Regular prenatal care throughout pregnancy helps to identify potential health issues that may arise and take action to address them. During prenatal visits, healthcare providers can monitor the growth and development of the baby, identify, and manage any medical conditions that the mother may have, and screen for potential genetic disorders.
Potential health issues that can be detected and treated through prenatal care
Prenatal care can detect and manage a range of health issues that may arise during pregnancy. Some potential health issues that can be detected and treated through prenatal care include:
High blood pressure: Prenatal care can monitor blood pressure levels and manage hypertension to reduce the risk of complications such as preeclampsia.
Gestational diabetes: Prenatal care can screen for gestational diabetes and manage blood sugar levels to reduce the risk of complications such as macrosomia and preterm birth.
Infections: Prenatal care can screen for and manage infections such as group B strep and sexually transmitted infections (STIs) to reduce the risk of complications such as preterm labour and neonatal infections.
Foetal growth and development: Prenatal care can monitor foetal growth and development to identify any potential issues and take action to address them. This can include screening for foetal abnormalities and genetic disorders.
Preterm labour: Prenatal care can monitor for signs of preterm labour and take action to prevent it or manage it if it occurs.
Getting early and regular prenatal care is essential for promoting a healthy pregnancy and reducing the risk of birth defects. Prenatal care can detect and manage a range of health issues that may arise during pregnancy and can help prevent complications and ensure that any existing medical conditions are managed appropriately. It's important for pregnant women to work closely with their healthcare providers and seek guidance and support throughout their pregnancy journey.
2. Lead a healthy lifestyle prior to and during pregnancy
Significance of adopting a healthy lifestyle for both parents
Maintaining a healthy lifestyle before and during pregnancy is important for both parents. A healthy lifestyle can reduce the risk of birth defects, promote a healthy pregnancy, and improve the health of the mother and baby. It's important to note that the father's health and lifestyle can also affect the health of the baby. Therefore, it's recommended that both parents adopt healthy habits before and during pregnancy.
Healthy diet and exercise recommendations
A healthy diet and regular exercise are important components of a healthy lifestyle before and during pregnancy. A healthy diet can provide the necessary nutrients for a developing baby and can reduce the risk of complications such as gestational diabetes and preterm birth. It is recommended that pregnant women eat a variety of foods, including fruits, vegetables, whole grains, lean protein sources, and low-fat dairy products. It's also recommended to avoid foods that may be harmful to the developing baby, such as certain types of fish that contain high levels of mercury.
Regular exercise can help promote a healthy pregnancy and reduce the risk of complications such as gestational diabetes, high blood pressure, and preterm birth. The ACOG recommends that pregnant women engage in at least 150 minutes of moderate-intensity aerobic activity per week, such as brisk walking, swimming, or cycling. But before starting an exercise program during pregnancy, it is crucial to seek advice from a healthcare provider.
Avoid alcohol, tobacco, and illicit drugs
Avoiding alcohol, tobacco, and illicit drugs is crucial for reducing the risk of birth defects and promoting a healthy pregnancy. Consuming alcohol during pregnancy can result in various birth defects, such as foetal alcohol syndrome. Tobacco uses during pregnancy can increase the risk of complications such as low birth weight, preterm birth, and sudden infant death syndrome (SIDS). Illicit drug use during pregnancy can cause a range of birth defects and can also increase the risk of complications such as preterm birth and low birth weight.
3. Take Prenatal Multivitamins for a Healthy Pregnancy
Proper nutrition during pregnancy is crucial for the healthy development of the foetus. Prenatal multivitamins are essential in ensuring that pregnant women get the necessary nutrients for foetal development. These prenatal supplements can also reduce the risk of birth defects and improve pregnancy outcomes.
Recommended prenatal vitamin supplements
There are several essential nutrients that should be included in prenatal multivitamins, including:
Folic acid: Folic acid is a B vitamin that is important for the development of the neural tube. Neural tube defects can cause serious birth defects such as spina bifida and anencephaly. Reducing the risk of birth defects is possible by taking folic acid before and during the early stages of pregnancy.
Iron: Iron is necessary to produce haemoglobin, which carries oxygen in the blood. Pregnant women need extra iron to support the growth of the foetus and the placenta.
Vitamin D: Vitamin D is important for the absorption of calcium and the development of strong bones. It is also important for immune function and can reduce the risk of preeclampsia and preterm birth.
Calcium: Calcium is necessary for the development of strong bones and teeth. It also supports the development of the nervous system and muscles.
Trimacare™ Prenatal Multivitamins: A Comprehensive Solution for a Healthy Pregnancy
Trimacare™ Prenatal Multivitamins are a comprehensive prenatal vitamin supplement designed to support the health of both mother and baby. The formula includes all the recommended prenatal vitamins and minerals, including folic acid, iron, vitamin D, and calcium. In addition, it contains other important nutrients such as omega-3 fatty acids and antioxidants.
Trimacare™ Prenatal Multivitamins help reduce the risk of birth defects by providing the necessary nutrients for foetal development. Folic acid is crucial for the development of the neural tube, and iron supports the growth of the foetus and placenta. Vitamin D and calcium are important for the development of strong bones and teeth. The antioxidants in Trimacare™ Prenatal Multivitamins also help reduce the risk of birth defects by protecting against oxidative stress.
Taking prenatal multivitamins is essential for the healthy development of the foetus and can reduce the risk of birth defects. Trimacare™ Prenatal Multivitamins provide all the essential nutrients for foetal development, including folic acid, iron, vitamin D, and calcium. The addition of antioxidants and omega-3 fatty acids make it an excellent choice for pregnant women looking to support the health of both them and their babies.
4. Manage chronic health conditions
Managing chronic health conditions before pregnancy is important for reducing the risk of birth defects and promoting a healthy pregnancy. Chronic health conditions, such as diabetes, hypertension, and thyroid disorders, can increase the risk of complications during pregnancy, such as preterm labour, preeclampsia, and foetal growth restriction. It's important to manage these conditions before becoming pregnant to optimize maternal and foetal outcomes.
There are several chronic health conditions that can impact pregnancy, including:
Diabetes: Uncontrolled diabetes during pregnancy can lead to complications such as preterm labour, preeclampsia, and macrosomia (large baby).
Hypertension: High blood pressure during pregnancy can increase the risk of complications such as preterm labour, preeclampsia, and placental abruption.
Thyroid disorders: Thyroid disorders, such as hypothyroidism and hyperthyroidism, can increase the risk of complications such as preterm labour, preeclampsia, and foetal growth restriction.
Asthma: Poorly controlled asthma during pregnancy can increase the risk of complications such as preterm labour and low birth weight.
Epilepsy: Women with epilepsy who take antiepileptic drugs during pregnancy may be at an increased risk of having a baby with birth defects.
It's important to discuss any medications with a healthcare provider before becoming pregnant, as some medications may be harmful to the developing baby. However, stopping certain medications abruptly can also be harmful, so it's important to work with a healthcare provider to manage chronic health conditions and any necessary medications. In some cases, it may be necessary to switch to a different medication or adjust the dosage during pregnancy.
5. Get genetic counselling and testing
Genetic counselling and testing can help identify the risk of certain genetic disorders and birth defects. This information can be used to make informed decisions about family planning, prenatal testing, and pregnancy management. Genetic counselling is recommended for individuals with a family history of genetic disorders, couples with a history of multiple miscarriages or stillbirths, and women over the age of 35.
Types of genetic tests
There are several types of genetic tests that can be done, including:
Carrier screening: This test can identify if an individual carries a gene for a genetic disorder. If both parents are carriers for the same genetic disorder, they have a 25% chance of having a child with the disorder.
Prenatal testing: Prenatal testing can identify certain genetic disorders and birth defects in a developing foetus. This can be done through non-invasive tests, such as ultrasound or blood tests, or invasive tests, such as amniocentesis or chorionic villus sampling.
New-born screening: New-born screening is a routine test done shortly after birth to identify certain genetic disorders that may not be apparent at birth. Early identification and treatment of these disorders can prevent serious health problems and developmental delays.
Benefits of genetic testing and counselling
Genetic testing and counselling can provide several benefits, including:
Early detection and treatment of genetic disorders: Identifying genetic disorders early can allow for early intervention and treatment to prevent serious health problems and developmental delays.
Informed decision-making: Genetic counselling can provide individuals and couples with information about their risk of having a child with a genetic disorder, allowing for informed decision-making about family planning and pregnancy management.
Peace of mind: For individuals with a family history of genetic disorders, genetic counselling can provide peace of mind by identifying their risk and allowing for early intervention if necessary.
Birth defects can cause lifelong health problems for the baby and can have a significant emotional and financial impact on the family. By taking steps to reduce the risk of birth defects, parents can give their baby the best possible start in life and reduce the risk of long-term health problems.
We encourage all expectant parents to take the necessary steps to reduce the risk of birth defects. By getting early and regular prenatal care, maintaining a healthy lifestyle, managing chronic health conditions, taking prenatal multivitamins, and getting genetic counselling and testing, parents can improve their own health and the health of their baby. Talk to your healthcare provider to learn more about how you can reduce the risk of birth defects and have a healthy pregnancy.
Soucre url - https://medium.com/@sharmavk0312/5-tips-for-a-healthy-pregnancy-how-to-reduce-the-risk-of-birth-defects-b100e2beea98
#pregnancy symptoms#prenatal multivitamin#prenatal multivitamins#prenatal tablets#multivitamins for women
1 note
·
View note
Text
Influenza Persists by Uday Jain in Journal of Clinical and Medical Images, Case Reports (JCMICR)
Introduction
In the US, influenza (flu) causes 9 to 45 million illnesses, leading to 12,000 to 61,000 deaths annually (10.1001/jama.2020.14772). World Health Organization estimates that worldwide annually there are about one billion infections, 3-5 million severe illnesses, and 300,000-500,000 deaths (10.1038/s41572-018-0002-y). Influenza is caused primarily by influenza A and influenza B viruses. Influenza A is the cause of pandemics. A schematic diagram of influenza A virus is presented in (Figure 1). Influenza will continue to be prevalent because its current vaccines are safe but only 30-60% efficacious. In contradistinction, COVID-19 vaccines have an efficacy of about 90%. Additionally, new zoonotic influenza strains intermittently migrate to humans. Influenza is a major part of “The New Normal
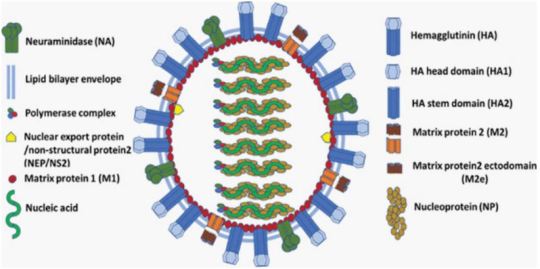
Figure 1: A schematic diagram of influenza A virus.
Coinfection
Since the start of COVID-19 pandemic, influenza is of greater concern. Overlapping spread of both diseases is a major strain on the health care system. Their coinfection is not common but may cause more severe disease. Influenza vaccination and therapy are important in addition to COVID-19 vaccination and therapy, especially in persons at increased risk.
Incubation
Influenza’s median incubation period is 2 days. Patients are infectious for a day before and 5 to 7 days after symptoms. COVID-19 has an incubation period of 4-12 days, a median of about 5 days. Patients are most infectious from 2 days before symptom onset. Influenza symptoms peak in 3-7 days. COVID-19 symptoms peak in second or third week. The spread of both viruses is facilitated by transmission by asymptomatic patients.
Transmission
About one-half of influenza A cases are due to aerosol transmission (10.1038/s41598-019-38825-y). Adequate ventilation can reduce it. Precautions utilized during the COVID-19 pandemic reduced the incidence of influenza in 2020. Used appropriately, surgical masks reduce the concentration of aerosolized influenza virus by about ten-fold and are adequate for prophylaxis against influenza (10.1016/j.jhin.2013.02.007; 10.7326/M20-3213). Transmission by respiratory droplets can also be reduced by masking. Transmission by direct contact can be reduced by hand and general hygiene. COVID-19 is transmitted in a similar manner. Social distancing reduces transmission by all the mechanisms. Influenza is less contagious and causes less severe disease than COVID-19. Quarantine recommended for COVID-19 patients is not necessary for those with influenza. Children play an important role in transmitting influenza. Healthcare providers should take precautions to avoid infecting themselves and others.
Influenza-Like Illness (ILI)
The Centers for Disease Control define ILI as fever 100°F (38°C) or greater and cough or sour throat that is not due to another known cause including streptococcal pharyngitis (strep throat). ILI’s causes can be benign such as common cold (nasopharyngitis caused by rhinovirus or other viruses) or severe including sepsis, meningitis, COVID-19, and SARS. Often there is an abrupt onset. SARS leads to severe disease in most of the infected. Influenza and COVID-19 cause mild disease in most of the infected (10.1016/S1473-3099(20)30484-9). SARS is currently not prevalent. Severe disease due to COVID-19 and SARS occurs primarily in the elderly. Influenza is more evenly distributed across the age groups. ILI can cause immunosuppression, leading to bacterial pneumonia, necessitating antibiotics (10.1097/QCO.0000000000000347).
After general anesthesia, children with influenza have a longer hospital length of stay and increased risk of requiring intensive care (10.1186/1471-2253-11-16). Routine surgery should be postponed for about four weeks in a patient with ILI. Unvaccinated patient should be offered influenza vaccination after the acute phase of ILI has passed and before the surgery. Before performing urgent surgery, severe causes of ILI should be excluded
Upper Respiratory Tract Infection (URI) Excluding ILI
In cold weather URI is common, especially in children. Often it is due to common cold, or noninfectious allergic or vasomotor rhinitis. Less commonly, it can be early presentation of more serious illness including ILI, COVID-19, strep throat, and herpes simplex. Early in infection it is difficult to distinguish between different etiologies of URI.
URI may cause sneezing, coughing, headache, malaise, rhinorrhea, sore throat, sinusitis, and bronchitis. Subsequently, bronchi may be hyperreactive for about six weeks. Pulmonary complications associated with surgery in a patient with URI are bronchospasm, laryngospasm, coughing, breath holding, postintubation croup, episodes of desaturation, atelectasis, and pneumonia. Anticholinergics and bronchodilators may not be beneficial. Perioperatively, adequate hydration and humidification should be maintained. There are no pediatric or adult anesthesia closed claims that implicate URIs including influenza with serious adverse events. There is a very small incidence of viral myocarditis in patients with URI including ILI. It may lead to serious arrhythmias and refractory heart failure (10.1016/j.jcrc.2018.06.001; 10.1038/s41569-020-00435-x).
Diagnostics Tests
These include nucleic acid amplification via polymerase chain reaction (PCR) and antigen-based immunological assays. A PCR test can be performed even at the point-of-care with results available within an hour (10.1016/S2213-2600(20)30469-0). This can facilitate infection control and utilization of antiviral therapeutics. It is especially useful for patients who have severe symptoms or are hospitalized. Test for COVID-19 may also be performed if indicated.
Influenza Vaccine
It is the best preventive measure. Although not very efficacious, it substantially reduces morbidity and mortality because of high prevalence of influenza. It is recommended for anyone over 6 months of age. It is especially beneficial in the presence of age <2 years or >65 years, pregnancy, and pre-existing conditions (10.1001/jama.2020.14772). Lack of vaccination in pregnancy not only increases the risk to mother but also increases the risk of preterm birth, fetal death, infant respiratory infection and hospital admission. The T cell response vaccines elicit is substantially weaker than the antibody response. Children may need two doses of vaccine, at least four weeks apart. The vaccine should be administered at least one week before surgery. It takes two weeks to develop full effect. As the protection wanes over time, mid-September to mid-October is preferred for vaccination. Influenza and COVID-19 vaccines may be administered together. The vaccine may be administered to surgical inpatients (10.7326/M15-1667).
Available Vaccines
The influenza virus mutates frequently. Quadrivalent vaccines protect against four of the currently most prevalent strains of influenza. The vaccines are altered every year for the predicted prevalent strains. Nine vaccines from four manufacturers are available in the US. Inactivated influenza vaccine is most commonly used. It is approved for persons above 6 months of age. As older individuals have a reduced response, vaccines that have a higher dose or are adjuvanted are recommended for persons above 65 years of age. The vaccine is usually administered intramuscular, but a lower dose intradermal vaccine is non-inferior (10.1001/jamanetworkopen.2020.35693).
Live-attenuated influenza vaccine is administered via nasal spray. It is approved for ages 2-49 years. It may be preferable in some situations such as vaccinating many persons in a community. It should be avoided if the patient or someone nearby has a suppressed immune system. Hence, it is not suitable for inpatients.
Recombinant vaccine and cell culture vaccine do not contain egg products. They are especially suitable for persons who need to avoid eggs because of allergy or dietary preferences.
Available Vaccines
Universal vaccines that provide durable response against all influenza strains are in human trials (10.1038/s41591-020-1118-7). These vaccines generate antibodies against the viral hemagglutinin protein stem (stalk) domain (HA2). Current vaccines generate antibodies against the immunodominant globular head domain (HA1), which is variable and mutates much more frequently. Vaccines utilizing mRNA are also in human trials. They are likely to have greater efficacy but more side effects than current vaccines. A major advantage of the mRNA vaccines is that they can be readily modified to match mutations in the virus.
Benefits of Vaccination for Adults
Influenza vaccine reduces the risk of respiratory and cardiovascular adverse outcomes and mortality among adults, especially in the presence of pre-existing conditions and advanced age. This was confirmed in a meta-analysis of studies on all adults (10.1016/j.arr.2020.101124). Another meta-analysis found that vaccine reduced the risk of adverse cardiac outcomes, especially in sicker patients (10.1001/jama.2013.279206). Preoperative vaccination is beneficial. A large study of elderly patients who had major surgery found preoperative vaccination reduced by about one-half the risk of pneumonia, intensive care admission, and death (10.1093/infdis/jix616). Patients also had shorter hospital stays and reduced resource utilization.
Influenza Therapeutics
These include neuraminidase inhibitors oseltamivir, zanamivir, peramivir, and laninamivir; cap-dependent endonuclease inhibitor baloxavir; and matrix protein M2 ion channel blockers (10.1001/jamanetworkopen.2021.19151). They attenuate viral replication. They provide postexposure prophylaxis. When started within 2 days of symptom onset, they reduce duration and severity of the disease, and complications. They also reduce transmission of influenza virus. However, their efficacy is limited, especially in patients with serious illness. They are expensive and not widely utilized. Although influenza and COVID-19 have similar initial symptoms, their therapeutics are different. Thus, dexamethasone reduces mortality for hospitalized COVID-19 patients on respiratory support but may increase mortality for hospitalized influenza patients (10.1001/jama.2020.15260).
Influenza Pandemics
They are usually caused by zoonotic influenza A virus strains migrating to humans. The 1918 “Spanish flu” pandemic caused by influenza A H1N1 virus led to more than 40 million deaths worldwide. H1 denotes haemagglutinin subtype 1 and N1 denotes neuraminidase subtype 1. The pandemics of 1957, 1968 and 2009 were caused by influenza A H2N2, H3N2, and H1N1 viruses, respectively. The 2009 “swine flu” influenza A H1N1 virus that originated from pigs was antigenically different from previously dominant influenza A H1N1 viruses. It caused 150,000-600,000 deaths worldwide. Avian influenza “bird flu” caused by H5N1 and H7N9 is not prevalent. Overlapping occurrence of influenza pandemic and COVID-19 will be devastating. Vigilance and prompt action are essential to prevent zoonotic influenza A virus strains from migrating to humans.
Conclusion
Influenza is a prevalent respiratory disease that will continue to affect anesthesia practice in the foreseeable future. With appropriate management, the risk of adverse outcomes is low. Vaccination is highly recommended, especially preoperatively.
For more details : https://jcmimagescasereports.org/author-guidelines/
#US#COVID-19#humans#therapy#appropriately#influenza#prophylaxis#ILI#SARS#anesthesia#laryngospasm#arrhythmias#Uday Jain#jcmicr
1 note
·
View note
Photo

What is the fastest way to cure tonsillitis? Tonsils are lumps of tissue at the back of the throat. There are two of them, one on each side. Along with the adenoids, tonsils are part of the lymphatic system. The lymphatic system clears away infection and keeps body fluids in balance. Tonsils and adenoids work by trapping the germs coming in through the mouth and nose. Both acute and chronic tonsillitis respond well to this treatment. Immunity plays an important role in infections and individuals with low immunity are easily susceptible to infections. And so homeopathy serves as the best medicine to boost immunity and treat infections properly. The majority of homeopathy treatment for tonsillitis is based on the symptoms of the condition, such as a sore throat, thirst, perspiration, shivering, mental restlessness, changes in appetite, etc. Homeopathy cures the youngster by removing the infection's weaknesses and restoring their health. Common Tonsil Conditions: • Acute tonsillitis: Acute condition of tonsil infection caused either by bacteria or virus called the acute tonsillitis. In this condition tonsils are swelled, inflamed, pain during deglutition and develop a grey or white coating of exudates. • Chronic tonsillitis: Persistent infection of the tonsils at slightest exposure develop the condition of chronic tonsillitis. Here the tonsils are always in large size due to the repeated episode of acute infection. • Peritonsillar abscess: An infection creates a pocket of pus next to the tonsil, pushing it toward the opposite side. It is called the peritonsilar abscess • Acute mononucleosis: Usually caused by the Epstein-Barr virus. Mononucleosis causes severe swelling in the tonsils, fever, sore throat, rash, and fatigue. • Strep throat: Streptococcus, a bacteria when infects the tonsils and throat is called as Strep throat. • Tonsilloliths (tonsil stones): Tonsil stones, or tonsilloliths, are formed when the trapped debris in the tonsilar crypts get hardens, or calcifies.
What are plus point of homeopathy treatment in tonsillitis?
• It gives rapid relief to the acute condition of tonsillitis in compare to other therapy • It not only cure the tonsillitis, but cures the allergic sensitivity of the person’s immune system so he/she leads a healthy life for life long • Homeopathy medicines are very safe and without any side effects. So it cures the disease in a very smooth and holistic way • It is given to all age group from 1 day infant to 80 years old person. • It is very palatable and thus favorite for small children. The little kids are very fond of taking these round sugar pills. • Homeopathy offers a long term cure to the tonsillitis condition as it modify the hypersensitive nature of person’ immune system to a healthy functioning immune system. Does Homeopathy Work for (Tonsillitis) Throat Infections? Homeopathy medicines for tonsillitis are selected based on signs and symptoms; each case is taken after a thorough history, extracting the causative factors, modalities as well as characteristic symptoms. Homeopathy treatments are very safe and side effect free. So it cures the disease in a very smooth and holistic way. It is given to all age groups from 1-day infant to 80 years old person. Homeopathy offers a long-term cure to the tonsillitis condition as it modifies the hypersensitive nature of a person's immune system to a healthy functioning immune system. It boosts the body’s immune system and restores the body’s defenses to normal. Proper homeopathy treatment can be able to check the repeated infection of tonsils and adenoids. Tonsillitis is highly contagious. To decrease your risk of getting tonsillitis, stay away from people who have active infections. Wash your hands often, especially after coming into contact with someone who has a sore throat, or is coughing or sneezing. If you have tonsillitis, try to stay away from others until you are no longer contagious. Know more: https://www.multicarehomeopathy.com/diseases/6-best-homeopathic-medicines-for-tonsillitis-treatment
#homeopathy treatment for Tonsillitis#homeopathy medicines for Tonsillitis#homeopathic medicines for Tonsillitis#homeopathic treatment for Tonsillitis#homeopathy for Tonsillitis#treatment for Tonsillitis
0 notes
Text
Third Trimester Tests In Pregnancy
Overview
The third trimester is the final stage of pregnancy and starts from week 27 and extends till delivery. The third trimester can be both physically and emotionally challenging for a pregnant woman. As a woman may face some major complications during this period, the doctor may recommend more frequent prenatal visits to keep a closer watch on the mother and baby’s health.
Let us go over different types of third trimester prenatal tests recommended by the doctor in the next sections.
What happens during the Third Trimester?
The third trimester marks the home stretch, as a woman gets ready for the birth of her baby. The fetus also continues to grow in weight and size. Some of the physical symptoms during this period include shortness of breath, hemorrhoids, urinary incontinence, varicose veins, and sleeping problems. Many of these symptoms arise from the increase in the size of the uterus.
It is highly important to get checked and tested regularly along with maintaining a healthy weight, eating a balanced diet, and even exercising mildly to stay fit for the upcoming delivery.
What are the important Third Trimester Tests?
Some of the important tests that may be recommended in the third trimester are as below.
● Glucose Screening - This test is used to detect diabetes in a pregnant woman. Pregnancy can lead to induced diabetes which if not controlled, can result in overly large babies, a broad range of health problems for the mother and the baby, and even difficulty at the time of delivery.
● Urine Examination Routine: This test is used to detect a range of medical conditions such as kidney infection, diabetes, and urinary tract infection. It also detects protein, which could indicate the presence of preeclampsia, a pregnancy-induced disease that is accompanied by high blood pressure.
● Group B Streptococcus Screening: Group B Strep test, also known as Group B Streptococcus test or GBS is one of the routine antenatal tests which diagnoses infection with the Group B streptococcus bacteria during pregnancy. Group B Streptococcus bacteria is usually found in the intestines, rectum, urethra, or vagina and can lead to complications in the mother and may cause sepsis, pneumonia,
meningitis, seizures, or at times death in the newborn if the infection is transmitted to the baby, during the process of delivery.
● CBC (Complete Blood Count): This blood test is done to determine any health issues a woman may have developed. It monitors the red blood cells that carry oxygen throughout the body and also determines the count of red blood cells, white blood cells, and platelets.
● Electronic Fetal Heart Monitoring: This test is done during the course of pregnancy, at the time of labor, and once during delivery to monitor the heart rate of the fetus, and ensure everything is absolutely fine.
● Non-Stress Test: This test is usually performed on a regular basis in high-risk pregnancy cases, such as when a woman is carrying twins or has diabetes, or has high blood pressure. The test aids in monitoring the baby’s heart rate as it moves in the womb.
● Contraction Stress Test: This test is also recommended in high-risk pregnancy cases. During the test, a fetal monitor measures the baby’s heart rate when the womb is contracted either by oxytocin or nipple stimulation. Gynecologists use this technique for predicting the baby’s response to labor stress.
● Ultrasound: Third trimester ultrasounds are used to examine the placenta and check the baby’s position and growth. Biophysical profile can also be done with an ultrasound to see whether the baby is getting enough oxygen.
0 notes
Text
How’s pregnancy going so far..
Found out I was pregnant around 8 weeks after thinking I had food poisoning.
1st trimester - diagnosed with hyperemesis gravidon, spent every second of the day throwing up/retching to the point I couldn’t keep liquid or solids down. Felt like I was going to die (no joke) and ended up in hospital after multiple visits and on a drip for fluids. ended up on sick leave for work.
This ended at around 12 weeks which saw me into the second trimester.
2ns trimester, amazing! However from around 18 weeks I started having pains and I was worried due to my hips not being right before I was pregnant. Diagnosed with pelvic girdle pain which unbeknownst to myself which get worse the more the pregnancy continues. Found out also my blood type was rare Onegative which meant that if I had a knock or fell I’d needed an injection to make sure that mine and babies blood didn’t mix.
3rd trimester so from 28 weeks onwards this is when all hell broke loose. I was given the diagnoses of gestational diabetes which has honestly ruled my life from 30 weeks till now. Baby is growing on the larger side for his age so there are concerns with that. He also has fluid in both of kidneys meaning that when he’s born he’ll have to for a scan and be on antibiotics. The pelvic girdle pain and gotten so bad for me I’m unable to walk. I’m unable to bend/pick anything up/ walk for more than 2/3 minutes, I have to wear a support band over my hips to help minimise the pain which isn’t a lot, I have to have help getting up when sitting down, I’m suffering really bad from oedema, my ankles, legs and feet feel like they’re going to snap, this has led to a diagnoses of pre eclampsia due to high blood pressure and the normal symptoms. I’ve also been diagnoses with group strep b, I’m on insulin daily and nightly for my diabetes as unable to manage it, my blood count is low so having to take iron tablets, to top it off... I’ve been newly diagnosed with bipolar and complex PTSD and have a high risk after birth of post partum psychosis, I have to take meds to make sure I don’t suffer an outbreak during birth, I’m not going the full 40 weeks, in fact I’m being on the 5th January instead of going to the 19th and having natural labour... honestly I love my little gem with all my heart but this pregnancy has been so tough mentally and no one even knows. I’m constantly in agony 24/7 and unable to do anything myself which is affecting me mentally. Constantly having to go to appointments on my own without Airon there to support me is scary as every time I go to hospital I’m leaving with a new diagnoses..
Sigh just a little rant anyway.. I can’t wait to meet my little boy soon tho.. it’ll all be worth it in the end 💙
1 note
·
View note
Text
Understanding The Facts About Group B Strep Test in the UK

Group B Streptococcus (GBS) is a bacterium often found in the digestive and lower reproductive tracts. Though it is harmless to adults, it can cause serious complications for newborns. Expecting mothers in the UK need to understand the importance of the Group B Strep test. This simple, routine test can make a significant difference in ensuring the health and safety of your baby. By familiarizing yourself with the facts about GBS testing, you can take proactive steps to protect your newborn from potential infections.
Fact 1: The Group B strep test identifies the presence of GBS in pregnant women. This test is typically done between the 35th and 37th weeks of pregnancy. Early detection helps in planning the right care to prevent transmission to the baby.
Fact 2: It is a simple and painless test. The test is simple and painless. A swab is taken from the vagina and rectum. This sample is then sent to a lab for analysis and the results are usually available within a few days. If GBS is detected, antibiotics can be administered during labor to prevent infection in the baby.
Fact 3: There are risks if GBS is left untreated. If GBS is not treated, it can be passed to the baby during delivery. This can lead to serious health issues, such as pneumonia, meningitis, and sepsis. Early testing and treatment significantly reduce these risks.
Fact 4: Testing positive for GBS is common. About 20–30% of pregnant women in the UK test positive. If you test positive, you will be given antibiotics during labor. This greatly reduces the chance of your baby getting infected.
Fact 5: All pregnant women should get tested for GBS. The test is a standard part of prenatal care in many countries, including the UK. Group B Strep testing is available through your NHS healthcare provider. Additionally, private clinics like Concepto Diagnostics offer reliable testing services. Early testing ensures you and your baby receive the best care.
To summarize, Understanding the importance of the Group B Strep test is vital for expecting mothers. This simple test can prevent severe health issues in newborns. Early detection and treatment are key to ensuring a safe delivery and a healthy baby. The peace of mind that comes from knowing you've taken every precaution is invaluable. Expecting mothers in the UK should prioritize the health and safety of their newborns. Visit Concepto Diagnostics for a reliable Group B Strep test in the UK.
Also Read: The effective ways to prevent early GBS in the UK
#Group B Strep during pregnancy UK#Group B Strep Test UK#Prenatal screening test UK#Pregnancy Scan UK
0 notes
Text
This week has ended a lot better than how it began. I decided to stick with my original plan of birthing at the hospital. I think I just took in too much of the fear and panic which made me want to look into other options. But my husband and I really couldn’t afford other options, and making a last minute switch was really stressing me out. I think I also just needed time to grieve the loss of having my doula with me at the hospital and not have the original birth I had planned. I talked about my concerns thoroughly with my OB and I feel better. I also tested positive for Group B Strep, so that tipped the scales in favor of hospital birth. Also like...there’s really no 100% safe place to have a baby, and even if I did birth at a birthing center or at home, I’m still risking exposure in some way, shape or form. I’ll still be around other people. And the number of confirmed cases in my city is growing, but not at an amount to where it would overwhelm hospitals by the time I give birth.
The other frustrating thing that has made me just want to check out entirely of following anything covid-19 related is the conflicting sources of information I’m getting. My OB says the hospital is taking every possible measure to keep the L&D ward separate from the rest of the hospital and that the L&D nurses are staying on the L&D floor, that there are only two confirmed cases of the virus at the hospital I’m delivering at, etc. The midwife I was talking to said my hospital had the most cases of the virus, that the nurses would be everywhere, that it was good I felt secure in my birth plan but that I should try and go to a different hospital. It just makes me angry, and this is honestly the most frustrating thing about this virus, that it’s almost impossible to get accurate information, because no one knows for sure how many cases there are, and how many people are really infected or the real death toll.
So, I’m trying to offer it up to God. At this point, I just want to have my baby and go home in peace.
Please pray though that my husband, baby and myself stay healthy. Let me know how I can pray for you!
3 notes
·
View notes
Text
I'm triggered today. I just saw a post from the hospital saying it's International Midwives day. While I am sure there are a lot of great midwives out there, ours was NOT. None of them on the team where in fact. From missing appointments, not telling me I had gestational diabetes, not telling me I had a severe bladder infection, not scheduling a NST the day I said I was worried our baby wasn't moving to telling me that in less I was bleeding not to worry about her. There was always something with them, and I wasn't happy from day one. The main midwife was not a nice person, very stone cold, made comments rudely about my weight,. She in fact blamed me and ONLY me for Leia dying.. She said we turned down the NST and ultrasound which was a lie. We weren't offered one that day. In her notes she said that Leia died because I was obese, had gestational diabetes. We later found out from an autopsy that I had Group B strep. So in fact in a way I did kill my baby. I will never know if I went in that Friday if she was showing signs of distress or not. I don't get to know if she could have been saved. What I do know is that I called her 3 times in 2 days after that appointment (that they showed up for 45 mins late) on Friday Sept 30th. That I said I'm not feeling well, I am now 36 weeks pregnant and am worried my baby is going to die. Fast forward to Monday when I managed to get an Ultrasound since Sat I called her again and she told me that "if you aren't bleeding stop worrying". There was a lot of time she would tell me that I needed to stop reading books looking up info. I requested to see and OB week 12 of my pregnancy and was told that a midwife was better for me. If I was high risk, obese and in danger of killing my baby then WHY agree to take me on as a patient? After I found out at the ultrasound that likely Saturday was the last time Leia's heart beated I just knew it was my fault. I knew I should have went to the hospital and demanded to be seen after I left the office. Or Sat when I felt ill. The midwife tried to come see me, but I wouldn't let her. If she couldn't come to see me when I needed her to, then no way I was letting her now. I screamed threw the door, that I wasn't bleeding and my baby was fucking dead. She heard me. I could hear her telling the dr's to let her in. I never got a condolence card, follow up phone call, or anything from her after this. NOTHING. I mean I wouldn't have opened it anyways but it should have been periodical. I filed a complaint against her and the other midwife that I saw regularly. I got all their notes and read all the lies. When I would talk to people about my story, they would ask who I had and every single time they would tell me they had her too. Many said they never went on with her. More than 20. If I had to do a poll right now about her, I bet everyone would agree with me that she was a bitch. I'm a pretty easy going person, and generally as a rule love and respect people. But I knew from the moment she saw me that she wasn't a good fit. I have so many regrets. So many what if's. Things I thought I was 'over' by now. Because I won. She was suspended without pay. She went back to her country I was told. Guess she's back. I seen her face just now and all I can do is cry. I still blame myself after all this time. It will be 9 years this October and all I can do is cry. Does she have regrets? Does she think of me? I've read the paperwork many many times and all I know is that it was not my fault. I know this, but I also know that without her taking blame, than it still feels like it's on me.
1 note
·
View note