#Global Medical Billing Market Analysis
Explore tagged Tumblr posts
Text
Global Medical Billing Market Size, Growth Outlook 2035
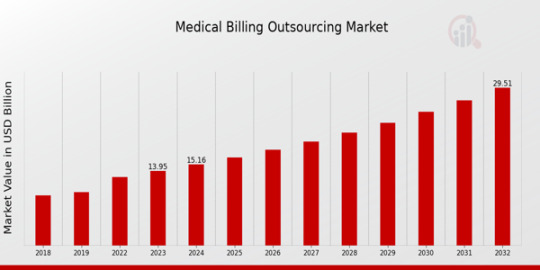
The medical billing market Size was valued at USD 15.88 billion in 2023 and is projected to grow from USD 17.76 Billion in 2024 to USD 32.79 billion by 2032
Summary
The global medical billing market is experiencing rapid expansion due to the increasing need for streamlined revenue cycle management (RCM) in healthcare. With the growing complexity of medical billing and coding procedures, hospitals, physician offices, and diagnostic centers are turning to automated and outsourced billing solutions to optimize their administrative and financial operations. The transition from traditional paper-based billing systems to cloud-based and AI-driven solutions has significantly improved efficiency, minimized billing errors, and enhanced reimbursement processes. Additionally, government initiatives promoting electronic health records (EHRs) and digital billing solutions are further accelerating market growth. However, the market faces challenges such as data security concerns, regulatory complexities, and the high cost of implementation. Despite these obstacles, advancements in AI, blockchain, and automation are expected to drive innovation in medical billing systems, ensuring sustained market growth.
Market Overview
Medical billing is a crucial component of healthcare administration, ensuring that healthcare providers receive payments for their services from insurance companies, patients, and government healthcare programs. The market has evolved significantly, integrating automated claim processing, real-time patient billing, and AI-powered coding assistance to reduce human errors and increase operational efficiency. With the increasing burden of medical debt and insurance reimbursement challenges, healthcare organizations are investing in robust billing solutions to optimize revenue cycles. The outsourcing of medical billing services is also gaining popularity, as third-party service providers offer cost-effective solutions while ensuring compliance with evolving healthcare regulations.
Market Size and Growth Analysis
The medical billing market Size was valued at USD 15.88 billion in 2023 and is projected to grow from USD 17.76 Billion in 2024 to USD 32.79 billion by 2032, exhibiting a compound annual growth rate (CAGR) of 12.14% during the forecast period (2024 - 2032). The rise in healthcare expenditure, regulatory mandates for digital healthcare solutions, and increasing adoption of cloud-based billing platforms are key contributors to this growth.
Market Dynamics
Growth Drivers
The increasing complexity of medical billing and the need for efficient revenue cycle management solutions are primary drivers of market growth. The adoption of electronic health records (EHRs) and practice management software has streamlined billing processes, reducing administrative burdens on healthcare providers. Additionally, government regulations supporting healthcare digitization, such as the Health Insurance Portability and Accountability Act (HIPAA) in the U.S., are encouraging hospitals and clinics to implement secure and compliant billing systems. The growing trend of outsourcing medical billing services is also driving market expansion, as healthcare organizations seek cost-effective and error-free billing solutions.
Challenges and Restraints
Despite the market's rapid growth, challenges such as data security risks, regulatory compliance complexities, and high initial investment costs pose significant hurdles. Medical billing systems must adhere to stringent regulations to ensure patient data privacy and avoid legal penalties. Moreover, the lack of skilled personnel and resistance to adopting new technologies in certain regions further restrains market growth.
Regional Analysis
The North American region dominates the global medical billing market, with the United States being the key contributor due to its advanced healthcare IT infrastructure and stringent regulatory mandates for digital billing. Europe follows closely, driven by government initiatives promoting digital healthcare solutions. Asia-Pacific is expected to witness the highest growth rate, with countries such as India, China, and Japan increasingly investing in healthcare IT and billing automation. The Middle East & Africa and Latin America are gradually adopting digital billing solutions, but infrastructure challenges continue to limit rapid expansion.
Market Segmentation
By Component:
Software – Includes cloud-based and AI-driven billing platforms
Services – Outsourced billing services and consulting
By Mode of Deployment:
Cloud-based solutions – Increasingly preferred due to scalability and cost-efficiency
On-premise solutions – Offers greater security and customization options
By End-User:
Hospitals & Healthcare Providers – Major adopters of automated billing software
Diagnostic Centers & Laboratories – Require streamlined claims processing solutions
Outsourced Billing Companies – Provide end-to-end revenue cycle management services
Key Market Players
Several companies are actively shaping the medical billing landscape, including:
Accenture (US)
AGS Health (India)
TCS (India),
Cognizant Technology Solutions (US)
Genpact (US)
GeBBS Healthcare (US)
INFINIT Healthcare
Recent Developments
The medical billing market has seen notable advancements in recent years, including the integration of AI-driven coding systems, blockchain-based secure billing solutions, and real-time claim adjudication technologies. Mergers and acquisitions among key market players have strengthened the industry, enhancing technological capabilities and service offerings. Governments worldwide are also introducing new policies for medical billing transparency, further shaping the market landscape.
Future Outlook and Opportunities
The future of the medical billing market looks promising, with ongoing innovations in AI, machine learning, and automation revolutionizing revenue cycle management. The adoption of predictive analytics in billing processes is expected to reduce claim denials and improve financial performance for healthcare providers. Additionally, as telehealth and remote patient monitoring services continue to rise, the demand for digital billing solutions will further expand. However, overcoming data security risks and regulatory challenges will be crucial to ensuring sustained growth in this evolving industry.
For more information, please visit @marketresearchfuture
#Global Medical Billing Market Size#Global Medical Billing Market Share#Global Medical Billing Market Growth#Global Medical Billing Market Analysis#Global Medical Billing Market Trends#Global Medical Billing Market Forecast#Global Medical Billing Market Segments
0 notes
Text
Trump Made Marijuana Legal with THCA Flower
Summary for Each Section
Part 1: Introduction
The introduction sets the stage by providing historical context for marijuana legislation, tracing its roots from early uses and legal status to eventual prohibition. It also outlines the purpose and key provisions of the Farm Bill, highlighting its relevance to agriculture and hemp.
Part 2: Understanding the Farm Bill
This section delves into the historical context and evolution of the Farm Bill, with a focus on the 2018 version. It explains the specific sections addressing hemp and cannabis, and how these differ from previous versions, laying the groundwork for understanding the legal framework established by the bill.
Part 3: Legal Framework for Hemp and THCA
Here, the report explores the legal definition of hemp under the Farm Bill and the distinction between hemp and marijuana. It provides a detailed analysis of THCA, its chemical structure, properties, and legal status, along with the federal and state regulations governing hemp cultivation and compliance requirements.
Part 4: Impact of the Farm Bill on Marijuana Industry
This part examines the economic, agricultural, and market implications of the Farm Bill, highlighting the growth of the hemp industry, changes in farming practices, and the introduction of THCA products. It also looks at consumer trends and market acceptance.
Part 5: Scientific and Medical Perspectives
A comparative analysis of THCA and THC is provided, focusing on their chemical differences, effects, and therapeutic potential. The section also explores current medical applications of Wholesale THCA, ongoing research, and potential future applications.
Part 6: Social and Cultural Impact
This section discusses the changing public perception of cannabis, cultural shifts resulting from legalization, and ongoing legal and social challenges. It examines how cannabis is becoming integrated into mainstream culture and its impact on social norms and values.
Part 7: Case Studies and Real-World Examples
Through case studies, the report illustrates state-level implementation of the Farm Bill, profiles industry leaders and innovators in the THCA market, and offers a global perspective by comparing international cannabis laws and market trends.
Part 8: Future Outlook and Conclusions
The final part of the report looks ahead to the future of cannabis legislation, economic growth projections, and social implications. It concludes with a summary of key findings, policy recommendations, and suggestions for future research.
2 notes
·
View notes
Text
Mobile Payment Market 2025 Analysis: Regional Perspectives and Global Impact
The recently released Fortune Business Insights research on the Global Mobile Payment Market survey report provides facts and statistics regarding market structure and size. Global Mobile Payment Market Size 2025 Research report presents an in-depth analysis of the Global Market size, growth, share, segments, manufacturers, and forecast, competition landscape and growth opportunity. The research’s goal is to provide market data and strategic insights to help decision-makers make educated investment decisions while also identifying potential gaps and development possibilities.
Get Sample PDF Brochure: https://www.fortunebusinessinsights.com/enquiry/request-sample-pdf/100336
Companies Profiled in the Global Mobile Payment Market:
Alipay com Co., Ltd. (China)
Amazon com, Inc. (U.S.)
American Express Co. (U.S.)
Boku Inc. (U.S.)
Google LLC (U.S.)
MasterCard International Inc. (U.S.)
Obopay (U.S.)
Fidelity National Information Services (FIS), Inc. (U.S.)
PayPal, Inc. (U.S.)
Visa, Inc. (U.S.)
Strategies for Paybacks and Rewards to Accelerate Market Growth
There is intense rivalry in the consumer market due to numerous payment service providers investing in their companies. Companies that make payment apps, including Alipay, Amazon Pay, Google Pay, and others are utilizing new strategies to keep their existing user base and attract new ones. For instance, Google Pay offers scratch cards that could be obtained with few purchases and include a specific amount. Such programs are supporting in maintaining client loyalty among those who use their smartphones to make payments. These features are expected to increase the mobile payment market share.
Most people still prefer cash and are reluctant to use online applications for payments, which may stifle the mobile payment market growth.
Ask For Customization: https://www.fortunebusinessinsights.com/enquiry/customization/100336
What exactly is included in the Report?
– Industry Trends and Developments: In this section, the authors of the research discuss the significant trends and developments that are occurring in the Mobile Payment Market place, as well as their expected impact on the overall growth.
– Analysis of the industry’s size and forecast: The industry analysts have provided information on the size of the industry from both a value and volume standpoint, including historical, present and projected figures.
– Future Prospects: In this portion of the study market participants are presented with information about the prospects that the Mobile Payment Market is likely to supply them with.
– The Competitive Landscape: This section of the study sheds light on the competitive landscape of the Mobile Payment Market by examining the important strategies implemented by vendors to strengthen their position in the global market.
– Study on Industry Segmentation: This section of the study contains a detailed overview of the important Mobile Payment Market segments, which include product type, application, and vertical, among others.
– In-Depth Regional Analysis: Vendors are provided with in-depth information about high-growth regions and their particular countries, allowing them to place their money in more profitable areas.
This Report Answers the Following Questions:
What are the Mobile Payment Market growth drivers, hindrances, and dynamics?
Which companies would lead the market by generating the largest revenue?
How will the companies surge the processes adoption amid the COVID-19 pandemic?
Which region and segment would dominate the Mobile Payment Market in the coming years?
Have Any Query? Speak to Our Analyst:
Mobile Payment Market Segments:
By Payment Type
Proximity Payment
Near Field Communication (NFC)
Quick Response (QR) Code
Remote Payment
Internet Payments
Direct Operator Billing
Digital Wallet
SMS Payments
By Industry
Media & Entertainment
Retail and E-commerce
BFSI
Automotive
Medical & Healthcare
Transportation
Consumer Electronics
Others (Education, IT & Telecom, and Others)
Table Of Content:
1. Introduction 1.1. Research Scope 1.2. Market Segmentation 1.3. Research Methodology 1.4. Definitions and Assumptions
2. Executive Summary
3. Market Dynamics 3.1. Market Drivers 3.2. Market Restraints 3.3. Market Opportunities
4. Key Insights 4.1 Global Statistics — Key Countries 4.2 New Product Launches 4.3 Pipeline Analysis 4.4 Regulatory Scenario — Key Countries 4.5 Recent Industry Developments — Partnerships, Mergers & Acquisitions
5. Global Mobile Payment Market Analysis, Insights and Forecast 5.1. Key Findings/ Summary 5.2. Market Analysis — By Product Type 5.3. Market Analysis — By Distribution Channel 5.4. Market Analysis — By Countries/Sub-regions
……………
11. Competitive Analysis 11.1. Key Industry Developments 11.2. Global Market Share Analysis 11.3. Competition Dashboard 11.4. Comparative Analysis — Major Players
12. Company Profiles
12.1 Overview 12.2 Products & Services 12.3 SWOT Analysis 12.4 Recent developments 12.5 Major Investments 12.6 Regional Market Size and Demand
13. Strategic Recommendations
TOC Continued……………….
Access Full Report at - Mobile Payment Market:
About Us:
Fortune Business Insights™ Delivers Accurate Data And Innovative Corporate Analysis, Helping Organizations Of All Sizes Make Appropriate Decisions. We Tailor Novel Solutions For Our Clients, Assisting Them To Address Various Challenges Distinct To Their Businesses. Our Aim Is To Empower Them With Holistic Market Intelligence, Providing A Granular Overview Of The Market They Are Operating In.
Contact Us:
Fortune Business Insights™ Pvt. Ltd.
US:+1 424 253 0390
UK:+44 2071 939123
APAC:+91 744 740 1245
Email:[email protected]
0 notes
Text
0 notes
Text
Real-world Evidence Solutions Market to be Worth $6.37 Billion by 2031
Meticulous Research®—a leading global market research company, published a research report titled,'Real-world Evidence Solutions Market Size, Share, Forecast, & Trends Analysis by Component (Datasets [Clinical, Claims, Pharmacy], Services) Application (Market Access, Drug Development & Approvals, PMS) End User - Global Forecast to 2031’.
The global RWE solutions market was valued at $2.62 billion in 2023. This market is expected to reach $6.37 billion by 2031 from an estimated $2.94 billion in 2024, at a CAGR of 11.7% during the forecast period of 2024-2031.
The increasing prevalence of chronic illnesses, drug development delays and the resulting rise in development costs, the growing emphasis on personalized healthcare, the move toward value-based care, and the expanding use of real-world evidence solutions in drug development and commercialization are the main factors propelling the growth of the real-world evidence solutions market. Moreover, participants in the real-world evidence solutions market could expect to see substantial development prospects due to the emergence of emerging economies and the growing emphasis on end-to-end RWE services. Many organizations use delivery methods that can offer value-based care with the goal of improving population health and achieving better results. An end-to-end strategy for utilizing a life sciences organization's data, evidence, and knowledge assets enables R&D to commercialization through insight-driven decision-making.
Download Sample Report Here @ https://www.meticulousresearch.com/download-sample-report/cp_id=4954
Key Players
The key players operating in the global real-world evidence solutions market are IQVIA Holdings Inc. (U.S.), Elevance Health, Inc. (U.S.), ICON plc (Ireland), Clinigen Group plc (U.K.), Cognizant Technology Solutions Corporation (U.S.), Revvity, Inc. (U.S.), F. Hoffmann-La Roche Ltd (Switzerland), Thermo Fisher Scientific Inc. (U.S.), Oracle Corporation (U.S.), SAS Institute Inc. (U.S.), Parexel International Corporation (U.S.), and HealthVerity, Inc. (U.S.).
Real-world Evidence Solutions Market: Future Outlook
The global RWE solutions market is segmented by Component (Datasets [Disparate Datasets {EMR/HER/Clinical Data, Claims & Billing Data, Pharmacy Data, Product/Disease Registries Data, Genomics Data, and Other Disparate Datasets}, and Integrated Datasets], and Consulting & Analytics), Application (Market Access & Reimbursement/Coverage Decisions, Drug Development & Approvals [Oncology, Neurology, Immunology, Cardiovascular Diseases, and Other Therapeutic Areas], Medical Device Development & Approvals, Post-market Surveillance, and Other Applications), End User (Pharmaceutical, Biotechnology, and Medical Device Companies, Healthcare Payers, Healthcare Providers, and Other End Users), and Geography. This study also evaluates industry competitors and analyzes the market at the global and regional levels.
Among all the components studied in this report, in 2024, the datasets segment is expected to account for the largest share of 53% of the RWE solutions market. The significant market share of this segment can be attributed to several factors, including the growing amount of medical data generated by hospitals, the growing reliance on outcome-based research on real-world data (RWD), and the growing healthcare payer, regulatory, and provider demand for drug safety information.
Among all the applications studied in this report, the drug development & approvals segment is projected to witness the highest growth rate of 13.1% during the forecast period of 2024–2031. The pharmaceutical and biopharmaceutical industries have been forced to concentrate on medication development due to the increasing prevalence of diseases, which has fueled the market's expansion. All parties involved can benefit from RWE's assistance in responding to these developments. By facilitating drug approvals, quickening the pace of development, and assisting in the analysis of the effects of novel medicines, the efficient application of RWE can propel the market's expansion.
Among all the end users studied in this report in 2024, the pharmaceutical, biotechnology, and medical device companies segment is expected to account for the largest share of 39.1% of the RWE solutions market. The largest portion of the market is accounted for by pharmaceutical and biotechnology businesses, which are using RWE more and more to gather real-time post-trial data about medications. Researchers and healthcare professionals can better comprehend and manage medication errors, side effects, and drug responses with the aid of the RWE drug information. Furthermore, the life sciences sector is utilizing RWE solutions at a quick pace to perform observational research, expedite medication development, and find qualified candidates for marketing campaigns and clinical trials.
This research report analyzes major geographies and provides a comprehensive analysis of the market in North America (U.S. and Canada), Europe (Germany, France, U.K., Italy, Spain, Switzerland, Belgium, and Rest of Europe), Asia-Pacific (China, Japan, India, South Korea, Taiwan, Singapore, Australia, and Rest of Asia-Pacific), Latin America (Brazil, Mexico, and Rest of Latin America), and Middle East & Africa.
Among all the regions studied in this report, in 2024, the North America region is expected to account for the largest share of 48.9% of the RWE solutions market. The pharmaceutical and biotechnology industries' rising R&D spending, the existence of significant market participants, government measures that are supportive, the adoption of EHR in hospitals, and strict drug approval procedures are all responsible for this region's substantial market share.
Complete Report Here : https://www.meticulousresearch.com/product/real-world-evidence-solutions-market-4954
Key questions answered in the report-
Which are the high-growth market segments in terms of component, application, end user, and region/country?
What was the historical market size for the RWE solutions market globally?
What are the market forecasts and estimates for the period 2024–2031?
What are the major drivers, restraints, challenges, opportunities, and trends in the global RWE solutions market?
Who are the major players in the global RWE solutions market?
What is the competitive landscape like, and who are the market leaders in the global RWE solutions market?
What are the recent developments in the global RWE solutions market?
What are the different strategies adopted by the key players in the global RWE solutions market?
What are the geographical trends and high-growth regions/countries?
Contact Us: Meticulous Research® Email- [email protected] Contact Sales- +1-646-781-8004 Connect with us on LinkedIn- https://www.linkedin.com/company/meticulous-research
#RWE#Real-world evidence#Real-world Data#RWE Market#RWE Platform#RWD#Real-world evidence solutions#Real-world Evidence Solutions Market
0 notes
Text
Did you know organs are being forcibly harvested from human beings?
It is shocking, but human trafficking for the purpose of organ removal and organ trafficking persist around the world, with primary victims being political prisoners, ethnic and religious minorities, and other vulnerable people. Organ trafficking hotspots include China, India, Pakistan, Turkey, Brazil, Nepal, the Philippines, Kosovo, Iran, and former Soviet states in eastern Europe.1
Alarmingly, globally only seven countries have passed legislation to combat these horrific crimes.2 Today, we demand more countries follow suit to stop forced organ harvesting and organ trafficking once and for all.
Forced organ harvesting and organ trafficking are interlinked crimes where organs are taken from victims through coercion or without informed consent and sold illegally, often making their way into the organ tourism transplant market. This means unknowing tourists undergoing organ transplants abroad are at-risk of receiving organs linked to organ trafficking and forced organ harvesting.
In many countries, impoverished people are targeted and coerced to sell an organ from which the traffickers make a significant profit. The ‘donor’ is left without medical care and with significant health risks.
In China, minorities rounded up by government crackdowns – political prisoners, ethnic Uyghurs3, and Falun Gong (Buddhist Qi Gong)4 practitioners — are known to be victims of forced organ harvesting. An international people’s tribunal in London recently found that some of China’s 1.5 million detainees in prisons camps have been killed for the state-sanctioned organ transplant trade worth over $1 billion.
“Forced organ harvesting has been committed for years throughout China on a significant scale,” said the China Tribunal,5 calling the crimes “of unmatched wickedness – on a death for death basis.”6
In 2012, China pledged to phase out harvesting organs from prisoners, but the international tribunal, researchers, and human rights activists stress that the practice continues to this day. An academic research analysis of organ donation data in China uncovered “highly compelling evidence [the numbers] are being falsified” and that tracking the sources of organs in the country remains difficult.7
Despite the clear evidence of organ trafficking and forced organ harvesting, ‘tourists�� continue to go abroad for organ transplants where the source of the organ cannot be verified. In fact, research suggests that 28% of organ transplants in China go to foreigners.8
Some governments are paying attention
But there are promising signs that governments around the world are waking up to this problem. South Korea, Belgium, Norway, Italy, Taiwan, Spain, and Israel have all passed legislation to combat forced organ harvesting, organ transplant tourism, and organ trafficking.9
Canada and the UK are now tabling similar bills that would criminalize the practice of receiving an organ transplant where informed consent was not given or recklessly obtained, prescribing harsh punishments for those who engage in the organ trafficking trade at home and abroad.1011
Organ transplants can save lives, but we believe that organs must be donated ethically and with complete transparency. Unfortunately, that is not the reality for many countries where organ trafficking occurs, and it’s high time for countries around the world to take a stand against organ transplant ‘tourism’ to these criminal hotspots.
You can take action!
Join our call, along with the International Coalition to End Transplant Abuse in China, in pushing countries around the globe to step up and tackle the often-overlooked crimes of human trafficking for the purpose of organ removal and organ trafficking.
@upontheshelfreviews
@greenwingspino
@one-time-i-dreamt
@tenaflyviper
@akron-squirrel
@ifihadaworldofmyown
@justice-for-jacob-marley
@voicetalentbrendan
@thebigdeepcheatsy
@what-is-my-aesthetic
@ravenlynclemens
@writerofweird
@bogleech
@anon-lephant
1 note
·
View note
Text
Barcode
Understanding Barcodes: The Key to Modern Inventory and Retail Management
Barcodes have become an indispensable part of our daily lives, revolutionizing how products are tracked, managed, and sold globally. From retail stores to warehouses, and healthcare facilities to logistics operations, barcodes simplify product identification, improve inventory accuracy, and enhance operational efficiency. This article dives into the fundamentals of barcodes, their types, uses, and why they remain a critical tool in modern business operations.
What is a Barcode?
A barcode is a method of representing data in a visual, machine-readable format using a combination of parallel lines, spaces, or dots. Scanners or mobile devices equipped with barcode readers decode this data and convert it into readable information, such as product details, pricing, or inventory levels.
Barcodes primarily consist of two elements:
Black Bars (or Patterns): Represent data.
White Spaces: Separate the black bars for clarity.
Each barcode contains a unique identifier that links to a database, providing details about the product, including its price, stock status, and origin.
History of Barcodes
The concept of barcoding was introduced in the 1940s by Norman Joseph Woodland and Bernard Silver. However, it wasn’t until 1974 that the first barcode was scanned on a Wrigley’s gum pack in an Ohio supermarket, marking the beginning of a technological revolution in retail and inventory management.
Types of Barcodes
There are two primary categories of barcodes: 1D (Linear Barcodes) and 2D Barcodes.
1. 1D (Linear) Barcodes:
These are the traditional barcodes with vertical black and white lines. Examples include:
UPC (Universal Product Code): Commonly used in retail stores.
EAN (European Article Number): International retail barcode.
Code 39: Used in manufacturing and military applications.
Code 128: Often found in logistics and shipping.
2. 2D Barcodes:
These barcodes store more data in both horizontal and vertical patterns. Examples include:
QR Codes (Quick Response Codes): Used in marketing, payments, and product information.
DataMatrix Codes: Common in healthcare and electronics.
PDF417: Found in shipping labels and ID cards.
How Do Barcodes Work?
Barcode Creation: A unique identification number is encoded into a barcode format.
Printing: The barcode is printed on labels or product packaging.
Scanning: A barcode scanner reads the black and white patterns.
Decoding: The scanner translates the barcode into digital data.
Database Lookup: The system retrieves product or asset details from the database.
This seamless process ensures accurate and instant information retrieval, reducing manual errors and improving efficiency.
Applications of Barcodes
Barcodes are widely used across various industries:
1. Retail:
Quick and accurate billing at checkout counters.
Improved inventory management and stock tracking.
2. Healthcare:
Tracking patient medications.
Managing medical equipment and supplies.
3. Logistics and Warehousing:
Real-time tracking of shipments.
Efficient warehouse inventory control.
4. Manufacturing:
Monitoring production lines.
Ensuring quality control through traceability.
5. Event Management:
Ticket scanning for concerts, sports events, and conferences.
Benefits of Barcodes
Accuracy: Reduces human errors in data entry.
Speed: Speeds up processes like billing, inventory checks, and shipping.
Cost-Effective: Affordable technology with significant ROI.
Inventory Control: Real-time visibility into stock levels.
Improved Traceability: Enhances product tracking across supply chains.
Data Insights: Provides accurate data for business analysis and forecasting.
Barcode Scanning Technology
Barcode scanners are devices designed to read and decode barcode information. Common types include:
Laser Scanners: Fast and accurate, commonly used in retail.
CCD Scanners (Charge-Coupled Device): Best for short-range scanning.
2D Image Scanners: Can read both 1D and 2D barcodes.
Mobile Scanners: Smartphones with barcode scanner apps for flexible use.
Barcodes vs RFID
While barcodes are widely used, RFID (Radio Frequency Identification) is emerging as an alternative technology.
Feature
Barcode
RFID
Cost
Low
Higher
Range
Short-range scanning
Long-range reading
Line of Sight
Required
Not required
Data Storage
Limited
Extensive
Both technologies have their advantages, but barcodes remain the preferred choice for cost-sensitive applications.
Challenges with Barcodes
Despite their advantages, barcodes face certain challenges:
Damage or Smudging: Barcodes may become unreadable if damaged.
Limited Data Storage: 1D barcodes can only store minimal information.
Dependency on Line of Sight: Direct scanning is necessary.
The Future of Barcodes
The future of barcoding technology is promising:
Smart Barcodes: Embedded with enhanced data storage.
Integration with IoT (Internet of Things): Enabling smarter inventory systems.
AI Integration: Improving predictive analytics for supply chains.
Blockchain Integration: Ensuring immutable traceability records.
With the rise of e-commerce and digital logistics, barcodes are evolving to meet the demands of modern supply chains.
How to Get a Barcode for Your Business
Register with GS1: GS1 is the global authority for barcode standards.
Obtain a GTIN (Global Trade Item Number): A unique identifier for your product.
Generate the Barcode: Use GS1-approved barcode creation tools.
Print and Apply: Ensure high-quality printing for accurate scanning.
Investing in barcoding systems ensures smooth operations and enhances scalability for businesses of all sizes.
Conclusion
Barcodes are far more than black lines on product packaging—they are a gateway to efficiency, accuracy, and global connectivity. From simplifying retail checkouts to ensuring supply chain transparency, barcodes have proven their value across industries.
As technology continues to advance, barcodes remain a cornerstone of effective product identification and data management, offering unparalleled benefits in a world driven by speed and precision.
0 notes
Text
Comprehensive Analysis of the Medical Terminology Software Market
The global medical terminology software market size is expected to reach USD 2.34 billion by 2030, registering a CAGR of 10.1% during the forecast period, according to a new report by Grand View Research, Inc. The increasing demand for standardization of patient data and compliance with standard vocabularies, such as SONOMED CT, RxNorm, ICD, CPT and HCPCS, and others are driving the adoption of clinical terminology solutions. The software uses a set of standard clinical terms to enable communication between different hospitals, departments, and specialties. This can be useful in situations where doctors need to collaborate in patient care or when patients need to be transferred between hospitals.
Using medical terminology software can also help improve patient safety by reducing the risk of misunderstandings caused by incorrect terms. It also saves physicians time by assisting in the documentation and thereby reducing burnout. Hospitals, health systems, and payers are all seeking innovative while manageable ways for data integration. Moreover, the government is taking active steps by launching incentive programs for patient data integration. Computer-assisted coding and accurate clinical documentation by employing Artificial Intelligence (AI), such as Natural Language Processing (NLP) technology and medical machine learning, are accelerating this process.
In addition, the growing demand for advanced healthcare data solutions is expected to create better business opportunities for clinical terminology solution providers. For instance, in September 2022, XpertDox, a Birmingham-based company specializing in automated AI-powered medical coding solutions, received funding of USD 1.5 million from TN3, LLC, a privately held company based in Arizona. The COVID-19 pandemic slowed down the industry growth. Revenue loss and financial crises, created by the pandemic, restrained hospitals to invest in the deployment of medical terminology software. Furthermore, the postponement of clinical trials resulted in a decrease in the utilization of clinical terminology software by CROs.
Medical Terminology Software Market Report Highlights
The industry will witness substantial growth post-pandemic due to the rising focus on data integration & automation in health systems
Based on application, the quality reporting segment held the largest revenue share in 2021 owing to the rising focus on the improvement of health quality outcome
The healthcare provider end-use segment held the largest revenue share in 2021 due to the high EHR adoption and demand for solutions to streamline the billing process
North America led the industry in 2021 owing to the factors, such as high demand for interoperability solutions, focus on improving care quality, and new software launches
In December 2021, CareCom and J2 Interactive formed a strategic agreement to introduce J2 Managed Terminology, a new service that offers cloud-hosted, best-in-class clinical terminology services to payers, health information exchanges, providers networks, and healthcare software companies
Medical Terminology Software Market Segmentation
Grand View Research has segmented the global medical terminology software market on the application, end-use, and region:
Medical Terminology Software Application Outlook (Revenue, USD Million, 2017 - 2030)
Data Aggregation
Reimbursement
Public Health Surveillance
Data Integration
Decision Support
Clinical Trials
Quality Reporting
Others
Medical Terminology Software End-Use Outlook (Revenue, USD Million, 2017 - 2030)
Healthcare Providers
Healthcare Payers
Healthcare IT Vendors
Others
Medical Terminology Software Regional Outlook (Revenue, USD Million, 2017 - 2030)
North America
US
Canada
Europe
Germany
UK
France
Spain
Italy
Asia Pacific
China
Japan
India
Australia
South Korea
Latin America
Brazil
Mexico
MEA
South Africa
Saudi Arabia
UAE
Order a free sample PDF of the Medical Terminology Software Market Intelligence Study, published by Grand View Research.
0 notes
Text
Unlock Your Career: BPO Jobs in the Philippines - Your Gateway to Success
The Business Process Outsourcing (BPO) industry in the Philippines continues to be a powerhouse of employment opportunities, offering attractive career paths for professionals at all levels. According to recent data from JOBYODA, the BPO sector remains one of the country's largest employers, with consistent growth projected through 2025.
Why Choose a BPO Career in the Philippines?
The Philippine BPO industry has established itself as a global leader in outsourcing services. JOBYODA's latest market analysis reveals that BPO employees in the Philippines enjoy competitive salaries, with entry-level positions offering starting salaries ranging from PHP 18,000 to PHP 22,000 per month. Team leader positions can command salaries of PHP 40,000 to PHP 60,000 monthly, while managers can earn upwards of PHP 80,000 per month.
Beyond the attractive compensation packages, BPO jobs offer comprehensive benefits including health insurance, performance bonuses, night differential pay, and various allowances. JOBYODA's employment data shows that 92% of BPO companies in the Philippines provide extensive benefits packages to their employees.
In-Demand BPO Positions
JOBYODA's current job market analysis highlights several high-demand positions within the Philippine BPO sector:
Customer Service Representatives: The backbone of the industry, these professionals handle customer inquiries across various channels. JOBYODA reports over 10,000 active openings for customer service positions across the country.
Technical Support Specialists: With the growing demand for IT services, technical support roles have seen a 25% increase in job postings over the past year, according to JOBYODA's platform data.
Healthcare Information Management: The healthcare BPO sector has experienced significant growth, with JOBYODA noting a 30% increase in medical coding and billing positions.
Back Office Processing: Data entry, claims processing, and documentation roles continue to be in high demand, with thousands of positions available across major BPO hubs.
Key Skills and Qualifications
JOBYODA's recruitment data indicates that successful BPO candidates typically possess:
Excellent English communication skills (both written and verbal)
Basic computer literacy and typing skills
Problem-solving abilities
Adaptability to different work schedules
Customer service orientation
Strong multitasking capabilities
Where to Find BPO Jobs
Major BPO hubs in the Philippines include Metro Manila, Cebu, Clark, and Davao. JOBYODA's platform features thousands of BPO job listings across these locations, with new opportunities added daily. The platform's data shows that 65% of BPO positions are concentrated in Metro Manila, followed by 20% in Cebu, and the remaining distributed across other urban centers.
Application Process and Tips
Based on JOBYODA's successful placement data, here are key steps to secure a BPO position:
1. Create a comprehensive profile on JOBYODA's platform, highlighting relevant skills and experience
2. Update your resume to emphasize customer service and communication abilities
3. Prepare for common BPO interview questions and assessments
4. Be ready for possible voice and accent evaluations
5. Research the company culture and specific role requirements
Growth Opportunities
JOBYODA's career tracking data shows that BPO professionals can expect significant career advancement opportunities. Many entry-level agents progress to senior positions within 2-3 years, with some reaching team leader positions in 3-4 years. The platform's career progression statistics indicate that 40% of BPO employees receive promotions within their first two years of employment.
Future Outlook
The Philippine BPO jobs industry continues to evolve and expand. JOBYODA's industry analysis projects a 15% annual growth rate in job opportunities, with emerging sectors like healthcare, IT, and financial services creating new positions. The platform's data suggests that artificial intelligence and automation will create more specialized roles, requiring enhanced technical skills and expertise.
For job seekers looking to start or advance their BPO careers, JOBYODA remains committed to connecting talented professionals with leading companies in the industry. With thousands of active job listings and comprehensive career resources, JOBYODA provides the tools and opportunities needed to succeed in the dynamic world of Business Process Outsourcing in the Philippines.
Remember to regularly check JOBYODA's platform for the latest BPO job opportunities and industry updates, as new positions are posted daily across various locations and specializations.
0 notes
Text
AI in Medical Coding Market 2025: Current Trends, Opportunities and Future Growth Challenges for 2037
Research Nester assesses the growth and size of the global AI in medical coding market which is anticipated to account for significant financial losses resulting from incorrect billing, false insurance claims, and misinterpretations of medical records.

Research Nester’s recent market research analysis on “AI in Medical Coding Market: Global Demand Analysis & Opportunity Outlook 2037” delivers a detailed competitor’s analysis and an overview of the global AI in medical coding market in terms of market segmentation by mode, application, end use, and by region.
Increased Emphasis on Accuracy to Promote Global Market Growth of AI in Medical Coding
Enhanced efficiency is one of the factors propelling the market for AI medical coding. AI-driven coding systems can significantly expedite diagnosis and procedure coding by automating the coding process. There are various benefits for healthcare professionals from this efficiency increase. By allowing healthcare organizations to process more claims and medical information in less time, it shortens backlogs and accelerates the revenue cycle. Moreover, greater efficiency frees up healthcare personnel's time from labor-intensive coding to patient care and complex medical tasks. Ultimately, this shift in focus results in better medical outcomes and enhanced patient care.
Request Free Sample Copy of this Report @ https://www.researchnester.com/sample-request-6493
some key factors and challenges associated with the AI in medical coding market include:
Growth Drivers:
Growing number of healthcare data
Increasing need for a coding and invoicing system
Challenges:
Due to privacy and security issues, there are major development barriers in the medical coding AI business. The healthcare industry bears the obligation to handle sensitive patient data, which includes personal information and medical history. Systems using AI that manage this data must strictly adhere to privacy regulations. Unauthorized access and data breaches are genuine issues, and even minor security lapses could have detrimental legal and financial effects on healthcare businesses. The possibility of a breach involving patient data can erode trust and harm an organization's standing.
By mode, the global AI in medical coding market is segmented into outsourced and in-house. The outsourced segment is expected to garner the highest revenue by the end of 2037. Outsourcing firms employ certified medical coders with experience who are up to date on the latest regulations and recommendations. This experience guarantees higher coding accuracy and compliance, necessary for proper billing and regulatory compliance. Furthermore, outsourcing allows healthcare firms to swiftly scale up or down their coding operations in response to demand, without being limited by staff levels.
Request for customization @ https://www.researchnester.com/customized-reports-6493
By region, Europe AI in medical coding market is expected to generate significant revenue by the end of 2037. The expansion of AI in medical coding is facilitated by Europe's heavy focus on technical innovation and healthcare research. The nation's cutting-edge healthcare IT infrastructure and investments encourage the advancement and uptake of AI technology. Furthermore, the healthcare system in Europe places a high value on effectiveness and high-quality patient care. AI in medical coding contributes to better coding and billing procedures, which is in line with the nation's goal of raising system performance and healthcare outcomes.
This report also provides the existing competitive scenario of some of the key players of the global AI in medical coding market which includes company profiling of 3M, AGS Health, Aidéo Technologies, aiHealth, Arintra, Buddi AI, Clinion, CodaMatrix, Corti HQ and others.
Access our detailed report @ https://www.researchnester.com/reports/ai-in-medical-coding-market/6493
About Research Nester-
Research Nester is a leading service provider for strategic market research and consulting. We aim to provide unbiased, unparalleled market insights and industry analysis to help industries, conglomerates, and executives make wise decisions for their future marketing strategy, expansion investment, etc. We believe every business can expand to its new horizon, provided the right guidance at the right time is available through strategic minds. Our out-of-the-box thinking helps our clients to make wise decisions to avoid future uncertainties.
Contact for more Info:
AJ Daniel
Email: [email protected]
U.S. Phone: +1 646 586 9123
U.K. Phone: +44 203 608 59
0 notes
Text
Medical Coding Market Research Consumption, Companies, Industry Report Analysis and Future Demand
Analysis of Medical Coding Market Size by Research Nester Reveals the Market to Grow with a CAGR of 9.6% During 2025-2037 and Attain ~USD 127.46 Billion by 2037
Research Nester assesses the growth and market size of the global medical coding market which is anticipated to be on account of the increasing adoption of electronic health record (EHR) systems and rising digital transformation.
Research Nester’s recent market research analysis on “Medical Coding Market: Global Demand Analysis & Opportunity Outlook 2037” delivers a detailed competitors analysis and a detailed overview of the global medical coding market in terms of market segmentation by component, classification type, end user and by region.
Surging Need for Universal Language in Healthcare to Promote Global Market Share of Medical Coding Market
The global medical coding market is estimated to grow majorly on account of the increased need for a universal language to eradicate misinterpretations and frauds related to insurance claims. Other than this, the rising prevalence of diseases, there is a rise in patient visits and admissions in hospitals. It has been estimated that almost 1 in 3 of all [R1] adults suffer from multiple chronic conditions. This will eventually lead to the widespread adoption of digital technologies to accomplish a smooth workflow in healthcare settings. Medical coding is the transformation of healthcare procedures, diagnoses, medical services, and equipment into universal medical alphanumeric codes. Medical coding helps increase revenue and eliminate errors. The demand for coding services is also growing remarkably. For instance, in the year 2022, as per the American Hospital Association, there were almost 33,356,852 admissions in all the hospitals in the United States. Thus, there is an increased demand for medical coders and billers in the market is projected to fuel the growth of the medical coding market during the forecasted period. Furthermore, there is a rising demand to divert to more convenient and streamlined billing and coding solutions. On the back of this, the global medical coding market is anticipated to garner significant revenue during the forecast period.
Some of the major growth factors and challenges that are associated with the growth of the global medical coding market are:
Growth Drivers:
Rising Need for Medical Coding and Billing Software in Healthcare Infrastructures
Increasing Number of Patients with Chronic Diseases
Challenges:
Data security & privacy concerns associated with the market, lack of standardization, and lack of skilled professionals are some of the major factors anticipated to hamper the global market size of the global medical coding market.
Access our detailed report at: https://www.researchnester.com/reports/medical-coding-market/5899
By classification type, the global medical coding market is segmented into the international classification of diseases (ICD), healthcare common procedure code system (HCPCS), current procedural terminology. Out of these, the international classification of diseases (ICD) segment is projected to garner remarkable revenue on the back of widespread utilization by clinical coders across the world for clinical coding in health databases.
By region, the Europe medical coding market is to generate the highest revenue by the end of 2037. The reason for the high growth in the region for the market is due to high patient visits and mandates of medical coding in healthcare settings.
Customized report@ https://www.researchnester.com/customized-reports-5899
This report also provides the existing competitive scenario of some of the key players of the global medical coding market which includes company profiling of 3M, Aviacode Inc., Maxim Healthcare Services, MRA Health Information Services, Oracle, Verisk Analytics, Inc. , Nuance Communications, Inc., Optum Inc., Outsource Strategies International, VertMarkets, Inc., S&P Global , AltuMED, Coding Network, PAREXEL International Corporation, Startek, GeBBS Healthcare Solutions, Fujitsu Limited, NTT and others.
Request Report Sample@ https://www.researchnester.com/sample-request-5899
Research Nester is a leading service provider for strategic market research and consulting. We aim to provide unbiased, unparalleled market insights and industry analysis to help industries, conglomerates and executives to take wise decisions for their future marketing strategy, expansion and investment etc. We believe every business can expand to its new horizon, provided a right guidance at a right time is available through strategic minds. Our out of box thinking helps our clients to take wise decision in order to avoid future uncertainties.
Contact for more Info:
AJ Daniel
Email: [email protected]
U.S. Phone: +1 646 586 9123
U.K. Phone: +44 203 608 5919
0 notes
Text
Patient Access /Front-end RCM Solutions Market 2024 : Size, Growth Rate, Business Module, Product Scope, Regional Analysis And Expansions 2033
The patient access /front-end rcm solutions global market report 2024 from The Business Research Company provides comprehensive market statistics, including global market size, regional shares, competitor market share, detailed segments, trends, and opportunities. This report offers an in-depth analysis of current and future industry scenarios, delivering a complete perspective for thriving in the industrial automation software market.
Patient Access /Front-end RCM Solutions Market, 2024 report by The Business Research Company offers comprehensive insights into the current state of the market and highlights future growth opportunities.

Market Size - The patient access /front-end RCM solutions market size has grown rapidly in recent years. It will grow from $2.26 billion in 2023 to $2.52 billion in 2024 at a compound annual growth rate (CAGR) of 11.7%. The growth in the historic period can be attributed to rising demand for patient access services, growing adoption of denials management, increasing demand for standardizing patient data, high demand for patient access/front-end RCM solutions in the medical sector.
The patient access /front-end RCM solutions market size is expected to see rapid growth in the next few years. It will grow to $3.86 billion in 2028 at a compound annual growth rate (CAGR) of 11.2%. The growth in the forecast period can be attributed to increasing demand for web and cloud-based solutions, rising demand for training, education, medical necessity, and pre-certification services, growing focus on integration platform as a service (IPAAS), increasing healthcare expenditure, and rising healthcare awareness, Major trends in the forecast period include growing importance of denials management to drive the market, increasing adoption of connected healthcare ecosystems, high deployment costs of patient access solutions, increasing adoption of patient access solutions in the healthcare industry, and changing demographics impacting the market.
Order your report now for swift delivery @ https://www.thebusinessresearchcompany.com/report/patient-access-or-front-end-rcm-solutions-global-market-report
The Business Research Company's reports encompass a wide range of information, including:
1. Market Size (Historic and Forecast): Analysis of the market's historical performance and projections for future growth.
2. Drivers: Examination of the key factors propelling market growth.
3. Trends: Identification of emerging trends and patterns shaping the market landscape.
4. Key Segments: Breakdown of the market into its primary segments and their respective performance.
5. Focus Regions and Geographies: Insight into the most critical regions and geographical areas influencing the market.
6. Macro Economic Factors: Assessment of broader economic elements impacting the market.
Market Drivers - Increasing patient engagement is expected to propel the growth of the patient access /front-end RCM solutions market going forward. Patient engagement refers to patients' active involvement, participation, and collaboration in the healthcare journey. It encompasses a range of actions, behaviors, and interactions between patients and healthcare providers designed to enhance the overall healthcare experience, improve health outcomes, and promote patient empowerment. Accurate data collection at the front end reduces billing errors, claim denials, and the need for costly corrections, contributing to the efficiency of RCM processes. For instance, in November 2022, according to Xtelligent Healthcare Media, a US-based B2B media and events focused on the healthcare industry, 61% of patients expressed a desire for enhanced patient engagement, while 83% of healthcare consumers indicated readiness to pursue health and wellness enhancements. Therefore, increasing patient engagement drives the growth of the patient access /front-end RCM solutions market.
Market Trends - Major companies operating in the patient access /front-end RCM solutions market are developing innovative technologies, such as Enabled Solutions, to improve revenue cycle outcomes. Enabled solutions use advanced technological tools and systems to enhance and optimize the various processes in managing a company's revenue cycle and implementing robust cybersecurity measures to protect sensitive financial and patient data. For instance, In October 2023, Omega Healthcare, a US-based technology company, launched the Omega Digital Platform (ODP). Utilizing cutting-edge proprietary technologies provides end-to-end revenue cycle management solutions for patient access, mid-revenue cycle, and business office functions. These solutions simplify workflows, lessen administrative burdens, and boost financial performance. Artificial intelligence, robotic process automation, machine learning, bots, and natural language processing are all incorporated into the ODP to improve accuracy and efficiency. This enables clients to reallocate resources, increase patient and employee satisfaction, and produce better financial results.
The patient access /front-end RCM solutions market covered in this report is segmented –
1) By Product And Service: Services, Software 2) By Deployment : On-Premise Solutions, Web And Cloud-Based Solutions 3) By End-User : HCIT Outsourcing Companies, Healthcare Providers
Get an inside scoop of the patient access /front-end rcm solutions market, Request now for Sample Report @ https://www.thebusinessresearchcompany.com/sample.aspx?id=14155&type=smp
Regional Insights - North America was the largest region in the patient access /front-end RCM solutions market in 2023. Asia-Pacific is expected to be the fastest-growing region in the forecast period. The regions covered in the patient access /front-end RCM solutions market report are Asia-Pacific, Western Europe, Eastern Europe, North America, South America, Middle East, Africa.
Key Companies - Major companies operating in the patient access /front-end RCM solutions market are McKesson Corporation, Optum Inc, Genentech Inc (Roche), Qway Healthcare Inc., 3M Company, Cognizant Technology Solutions Corporation, Experian PLC, Cerner Corporation, Cerner Corporation, Epic Systems Corporation, Conduent Inc, PATIENT ACCESS SOLUTIONS, INC., Conifer Health Solutions, Exela Technologies Inc, VIRTUSA CORPORATION, Waystar, Availity LLC, Craneware Inc., Allscripts Healthcare Solutions Inc., Kareo Inc, The SSI Group LLC, AccuReg Software, KYRUUS, HEALTHASYST, ACCESS ONE INC., Clearwave Inc, PLEXIS HEALTHCARE SYSTEMS, VEE TECHNOLOGIES, Cirius Group Inc., FINTHRIVE
Table of Contents 1. Executive Summary 2. Patient Access /Front-end RCM Solutions Market Report Structure 3. Patient Access /Front-end RCM Solutions Market Trends And Strategies 4. Patient Access /Front-end RCM Solutions Market – Macro Economic Scenario 5. Patient Access /Front-end RCM Solutions Market Size And Growth ….. 27. Patient Access /Front-end RCM Solutions Market Competitor Landscape And Company Profiles 28. Key Mergers And Acquisitions 29. Future Outlook and Potential Analysis 30. Appendix
Contact Us: The Business Research Company Europe: +44 207 1930 708 Asia: +91 88972 63534 Americas: +1 315 623 0293 Email: [email protected]
Follow Us On: LinkedIn: https://in.linkedin.com/company/the-business-research-company Twitter: https://twitter.com/tbrc_info Facebook: https://www.facebook.com/TheBusinessResearchCompany YouTube: https://www.youtube.com/channel/UC24_fI0rV8cR5DxlCpgmyFQ Blog: https://blog.tbrc.info/ Healthcare Blog: https://healthcareresearchreports.com/ Global Market Model: https://www.thebusinessresearchcompany.com/global-market-model
0 notes
Text
Final Expense Insurance Market Competitive landscape, Key company profile analysis and Opportunities 2032
The Final Expense Insurance market has witnessed significant growth over the years, reflecting an increasing awareness among consumers about the need to manage end-of-life expenses efficiently. As of 2022, the market size was estimated at USD 5.84 billion, and it is projected to grow from USD 6.11 billion in 2023 to a substantial USD 9.2 billion by 2032. This growth trajectory represents a Compound Annual Growth Rate (CAGR) of approximately 4.64% during the forecast period from 2024 to 2032.
Market Overview
Final Expense Insurance, also known as burial or funeral insurance, is a type of life insurance designed to cover the costs associated with an individual's funeral and other related expenses. Unlike traditional life insurance policies, which may cover a wide range of financial obligations, final expense insurance is tailored to meet the specific needs of end-of-life planning. This includes covering funeral costs, medical bills, and any other outstanding debts, ensuring that beneficiaries are not burdened with these expenses.
Get FREE Sample Report:
Drivers of Market Growth
Several factors are driving the steady growth of the Final Expense Insurance market:
Aging Population: The global population is aging rapidly, particularly in developed regions such as North America and Europe. As the elderly population grows, there is an increasing demand for insurance products that cater specifically to end-of-life expenses. Final Expense Insurance provides a cost-effective solution for individuals seeking to ensure that their final expenses are covered without placing a financial burden on their loved ones.
Rising Funeral Costs: Funeral costs have been steadily increasing, making it more challenging for families to afford these expenses out of pocket. Final Expense Insurance offers a way for individuals to preemptively manage these costs, providing peace of mind for both policyholders and their families.
Increased Awareness and Education: There has been a significant increase in awareness and education surrounding the importance of end-of-life planning. Insurance companies and financial advisors are increasingly promoting Final Expense Insurance as a practical and affordable option for managing final expenses, contributing to its growing popularity.
Simplified Underwriting Processes: Unlike traditional life insurance policies, which often require extensive medical examinations and underwriting processes, Final Expense Insurance typically offers simplified underwriting. This makes it more accessible to a broader range of individuals, including those with pre-existing health conditions.
Regional Insights
The Final Expense Insurance market is experiencing growth across various regions, with North America leading the charge. The United States, in particular, is a significant market due to its large aging population and the high cost of funeral services. In Europe, countries with aging populations, such as Germany and the United Kingdom, are also witnessing increased adoption of final expense insurance products.
In emerging markets, such as Asia-Pacific and Latin America, the market is still in its nascent stages but is expected to grow rapidly as awareness of end-of-life planning increases and the insurance industry expands.
Challenges and Opportunities
While the Final Expense Insurance market is on a growth trajectory, it is not without its challenges. One of the primary challenges is the saturation of the market in developed regions, where competition among insurance providers is intense. To stand out, companies are increasingly focusing on offering personalized products and leveraging digital platforms to reach a broader audience.
Another challenge is the need for ongoing education and awareness campaigns to reach underserved populations, particularly in emerging markets. However, these challenges also present opportunities for growth. By tapping into underserved markets and expanding product offerings to include additional benefits, insurance companies can capture a larger share of the market.
Future Outlook
The future of the Final Expense Insurance market looks promising, with steady growth expected over the coming years. As the global population continues to age and funeral costs rise, the demand for Final Expense Insurance is likely to increase. Insurance providers that can effectively address the needs of this growing market and differentiate themselves through innovative products and services will be well-positioned to succeed.
Get Related Reports:
Push Rod Sensor Market
Smart Air Conditioning Market
Atomic Force Microscope Market
Ultracapacitor Market
Trimmer Potentiometer Market
0 notes
Text
How a Knowledge Process Outsourcing (KPO) Center Can Transform Your Business Strategy

Introduction
In today’s rapidly evolving business landscape, Knowledge Process Outsourcing (KPO) has emerged as a pivotal strategy for organizations seeking to enhance their operational efficiency and gain a competitive edge. KPO involves the outsourcing of complex tasks that require specialized knowledge and expertise, making it distinct from traditional outsourcing models. As businesses increasingly recognize the value of leveraging external expertise, KPO is witnessing significant growth across various sectors.
Understanding Knowledge Process Outsourcing (KPO)
Knowledge Process Outsourcing (KPO) refers to the practice of outsourcing tasks that require specialized knowledge and expertise, often involving analysis, research, and complex decision-making. Unlike traditional Business Process Outsourcing (BPO), which typically handles routine tasks, KPO focuses on higher-level processes that add significant value to organizations.
Industries That Benefit from KPO Services
Manufacturing: KPO in manufacturing involves supply chain management, product development, and quality assurance. By outsourcing these knowledge-intensive tasks, manufacturers can optimize their processes, reduce costs, and improve product quality.
Information Technology: KPO services in IT include software development, data analysis, and IT consulting. Companies can leverage KPO expertise to enhance their technological capabilities and focus on strategic IT initiatives.
Healthcare: KPO firms provide services such as medical billing, coding, and clinical research, allowing healthcare providers to focus on patient care.
Finance: KPO services in financial modeling, risk analysis, and investment research help financial institutions make informed decisions.
Legal: Legal process outsourcing enables law firms to streamline research, documentation, and compliance processes, enhancing efficiency.
Real Estate: In the real estate industry, KPO services encompass property research, market analysis, and financial modeling. Real estate firms can make informed investment decisions and enhance property management practices.
Benefits of Establishing a KPO Center
Enhanced Global Competitiveness
KPO can significantly improve a company's competitive positioning in the global market. By leveraging specialized expertise, businesses can enhance their service offerings and differentiate themselves from competitors. This competitive edge is particularly crucial in industries characterized by rapid change and innovation.
Improved Operational Efficiency
KPO centers often implement streamlined processes and advanced technologies, leading to enhanced operational efficiency. By outsourcing complex tasks, companies can reduce turnaround times, improve accuracy, and ultimately increase productivity.
Cost-effectiveness and Scalability
KPO offers significant financial benefits, including reduced labor costs and improved resource allocation. Additionally, KPO centers provide scalability, allowing businesses to adjust their outsourcing needs based on market demands without the overhead associated with in-house operations.
Access to Specialized Expertise
KPO providers offer skilled professionals with domain-specific knowledge that may be costly to maintain in-house.
Focus on Core Competencies
Outsourcing specialized tasks allows organizations to focus on their core business activities.
Faster Decision-Making
KPO firms provide insights and data analysis that can accelerate business decisions.
Scalability and Flexibility
Businesses can scale operations without the need for significant upfront investments in staff or infrastructure.
SETTING UP A SUCCESSFUL KPO CENTER
Data Security and Confidentiality:
Ensuring robust data protection is crucial in KPO operations. Organizations must implement encryption, access controls, and compliance with regulatory standards to safeguard sensitive information.
Technology Infrastructure:
Investing in advanced software and platforms enhances data processing, communication, and project management, ensuring seamless operations.
Skilled Workforce:
Recruiting talented professionals and providing continuous training on industry trends are key to KPO success.
Target Markets and Services:
Conducting market research helps KPO centers identify potential clients and tailor services to meet specific needs, fostering strong client relationships and effectiveness.
Future of KPO Centers
Increased Focus on Customer Experience
KPO centers will prioritize enhancing the customer experience by providing personalized and responsive services. Understanding client needs and delivering tailored solutions will become crucial for maintaining long-term partnerships and driving business success.
Expansion of Specialized Services
The demand for specialized knowledge and expertise will lead KPO centers to diversify their service offerings. This could include emerging fields such as blockchain technology, cybersecurity, and sustainable business practices, allowing companies to access cutting-edge solutions tailored to their unique challenges.
Increased Automation and AI Integration
The integration of artificial intelligence (AI) and automation technologies will transform KPO services by enhancing efficiency and accuracy. Intelligent systems can streamline data analysis, automate repetitive tasks, and provide predictive insights, enabling KPO centers to deliver quicker and more precise results.
Conclusion
In conclusion, Knowledge Process Outsourcing (KPO) centers play a vital role in modern business by providing specialized expertise, improving operational efficiency, and enhancing competitiveness. As organizations navigate the complexities of the global market, KPO offers a strategic solution for driving growth and innovation.
CrosLinks, a premier knowledge process outsourcing company in the USA, delivers specialized services requiring expertise and analytical skills. Our tailored solutions drive efficiency, foster business growth, and ensure seamless communication with our clients. We encourage organizations to explore KPO solutions with CrosLinks as a means of unlocking their full potential and enhancing performance in an increasingly competitive landscape.
#knowledge process outsourcing#telemarketing#customer services#contact center#call center outsourcing#healthcare call center#finance call center
0 notes
Text
Healthcare BPO Market Industry Analysis
Market Overview
As of 2024, the global healthcare BPO market is estimated to be valued at approximately USD 371.20 billion and is projected to reach around USD 592.99 billion by 2029, growing at a CAGR of 9.82% during the forecast period. This growth is driven by several key factors:
Rising Healthcare Costs: With the escalating costs of healthcare, organizations are seeking cost-effective solutions to manage their operations more efficiently. Outsourcing helps reduce overhead costs and improve resource allocation.
Focus on Core Competencies: Healthcare providers are increasingly recognizing the importance of concentrating on their core competencies, such as patient care and clinical services. By outsourcing administrative and support functions, they can enhance their operational efficiency.
Technological Advancements: The integration of technology in healthcare outsourcing processes, such as telemedicine, electronic health records (EHR), and data analytics, is transforming the industry. These advancements enable better service delivery and improved patient outcomes.
Key Segments
The healthcare BPO market is segmented into various categories, including:
Medical Billing and Coding: This segment involves outsourcing billing and coding processes to ensure accuracy and compliance with healthcare regulations. It plays a crucial role in revenue cycle management, helping healthcare organizations maximize reimbursements.
Pharmaceutical BPO: This segment encompasses services related to drug development, clinical trials, and regulatory compliance. As the pharmaceutical industry becomes increasingly complex, outsourcing these functions allows companies to focus on innovation and product development.
Health Information Management: This includes the management of patient data, EHR maintenance, and data analytics. Outsourcing health information management ensures data security, compliance, and efficient handling of patient information.
Patient Care Services: Many healthcare organizations are outsourcing services such as telehealth, patient monitoring, and care coordination. These services enhance patient engagement and improve overall care quality.
Competitive Landscape
The healthcare BPO market is highly competitive, with a mix of large multinational companies and niche service providers. Major players such as Optum, Cognizant, and TCS dominate the market, leveraging their extensive experience and technological capabilities. However, smaller firms specializing in specific areas, like telehealth or medical billing, are gaining traction as healthcare organizations seek tailored solutions.
Future Trends
Several trends are expected to shape the healthcare BPO market in the coming years:
Increased Adoption of Telehealth: The COVID-19 pandemic accelerated the adoption of telehealth services. Healthcare organizations are increasingly outsourcing telehealth solutions to improve patient access and reduce wait times.
Focus on Data Analytics: The growing importance of data analytics in healthcare decision-making is driving the demand for BPO services that offer advanced analytics capabilities. Organizations are looking to harness data to improve patient outcomes and operational efficiency.
Regulatory Compliance: As healthcare regulations continue to evolve, organizations are increasingly outsourcing compliance management to ensure adherence to industry standards. BPO providers specializing in regulatory compliance will see increased demand.
Conclusion
The healthcare BPO market is poised for significant growth as organizations seek innovative solutions to enhance operational efficiency and patient care. With rising healthcare costs, a focus on core competencies, and advancements in technology, the demand for outsourcing solutions is expected to continue expanding. Companies that adapt to these trends and prioritize quality, compliance, and data security will thrive in this dynamic market, ultimately contributing to improved healthcare delivery and patient outcomes.
For a detailed overview and more insights, you can refer to the full market research report by Mordor Intelligence https://www.mordorintelligence.com/industry-reports/global-healthcare-bpo-market-industry
#marketing#healthcare bpo market#healthcare bpo industry#healthcare bpo market size#healthcare bpo market share#healthcare bpo market trends#healthcare bpo market growth#healthcare bpo market report
0 notes
Text
0 notes