#Dermatology billing services
Explore tagged Tumblr posts
Text
Dermatology billing services will optimize your revenue cycle management efficiently. From documentation to reimbursement, improve your practice's revenue while reducing administrative hassles.
0 notes
Text
#dermatology Billing Services in US#dermatology billing Specialist#dermatology billing services#dermatology billing#dermatology billing company#dermatology medical billing#medical billing for dermatology#dermatology medical billing and coding
0 notes
Text
Overcoming Revenue Cycle Management Challenges in Dermatology Billing
Dermatology, the branch of medicine that deals with the skin and its diseases, encompasses a wide range of diagnostic and therapeutic services. As with any medical specialty, dermatology practices face unique challenges in managing their revenue cycle effectively. Revenue cycle management (RCM) in dermatology billing involves the entire process of identifying, capturing, and collecting revenue for services provided.
However, this process is often fraught with complexities, including coding errors, claim denials, and reimbursement discrepancies. Understanding and overcoming these challenges is essential for dermatology practices to maintain financial stability and optimize revenue streams.

Understanding Revenue Cycle Management in Dermatology
Dermatology Revenue Cycle encompasses a series of interconnected processes, including patient scheduling, insurance verification, coding and documentation, claims submission, reimbursement, and accounts receivable management. Each of these processes plays a crucial role in ensuring that dermatology practices receive timely and accurate reimbursement for the services they provide.
1. Patient Scheduling: Efficient scheduling practices are essential to optimize revenue in dermatology billing. Practices must ensure appointments are scheduled appropriately, maximizing provider productivity and minimizing patient wait times. Over- or under-booking appointments can lead to lost revenue opportunities or patient dissatisfaction.
2. Insurance Verification: Verifying patient insurance coverage is a critical step in the revenue cycle management process. Practices must confirm patient eligibility and benefits before each visit to avoid denial of claims and ensure services are reimbursed.
3. Coding and documentation: Accurate coding and documentation are essential for proper reimbursement in dermatology billing. Dermatologic procedures often involve complex coding requirements, including evaluation and management (E/M) services, surgical procedures, and diagnostic testing. Appropriate documentation of the patient's medical history, examination results, and treatment plan is necessary to support billed codes and demonstrate medical necessity.
4. Claim Submission: Submitting clean claims is crucial for timely reimbursement in dermatology billing. Practices should ensure that claims are accurately coded, appropriately formatted, and include all necessary documentation to support the services provided. Electronic claims submission is preferred for its efficiency and speed, but practices must meet specific payer requirements to avoid claim denials or delays.
5. Reimbursement: Dermatology practices may receive reimbursement from several sources, including private insurance, Medicare, Medicaid, and patient payments. Understanding payer policies, fee schedules, and reimbursement rates is essential to optimizing revenue streams and maximizing collections. Practices should also monitor reimbursement trends and identify opportunities to improve revenue or reduce costs.
6. Accounts Receivable Management: Accounts receivable management is critical to maintaining financial stability in dermatology billing. Practices should track outstanding claims, follow up on unpaid invoices, and address claim denials or rejections promptly. Implementing effective accounts receivable processes, such as aging reporting, payment plans, and collection strategies, can help practices minimize bad debt and improve cash flow.
Challenges in Dermatology Billing
Dermatology practices face several challenges when it comes to managing their revenue cycle effectively. Some common challenges include:
Complex coding requirements: Dermatologic procedures often involve complex coding requirements, including multiple diagnosis codes, use of modifiers, and procedure grouping rules. Navigating these complexities can lead to coding errors, claim denials, and lost revenue.
Claim Denials and Rejections: Claim denials and rejections are common in dermatology billing, often due to coding errors, incomplete documentation, or payment policies. Resolving denied claims takes time and resources, delaying reimbursement and impacting cash flow.
Payer policies and reimbursement rates: Payer policies and reimbursement rates vary widely in dermatology billing, leading to inconsistencies in reimbursements between different payers. Practices must understand payer requirements and negotiate favorable contracts to maximize reimbursement and minimize revenue loss.
Compliance and Regulatory Changes: Dermatology practices must comply with numerous regulations and guidelines governing billing and reimbursement, including the Health Insurance Portability and Accountability Act (HIPAA), the Affordable Care Act (ACA), and the of Medicare Access and CHIP Reauthorization (MACRA). . Keeping up with regulatory changes and ensuring compliance can be challenging and time-consuming.
Patient Financial Responsibility: Rising healthcare costs and high-deductible health plans have increased patient financial responsibility in dermatology billing. Practices should educate patients about their financial obligations, offer transparent pricing, and establish payment plans to facilitate timely payment and reduce bad debt.
Strategies to Overcome Revenue Cycle Management Challenges
To overcome revenue cycle management challenges in dermatology medical billing and coding, practices can implement the following strategies:
Invest in staff training: Provide comprehensive training to staff members involved in the revenue cycle management process, including front-office staff, coders, billers, and collections specialists. Ensure staff members are knowledgeable about coding guidelines, payer policies, and regulatory requirements.
Use technology solutions: Implement electronic health records (EHR) systems, practice management software, and revenue cycle management tools to streamline billing processes, reduce errors, and improve efficiency. Use features like automated claims purging, electronic claim submission, and denial management to improve productivity and accuracy.
Conduct regular audits: Conduct regular audits of coding and documentation practices to identify coding errors, compliance issues, and areas for improvement. Address any deficiencies promptly through staff training, process improvements, or corrective action plans.
Establish clear policies and procedures: Develop clear policies and procedures for billing, coding, documentation, and accounts receivable management. Ensure staff members understand their roles and responsibilities and consistently follow established protocols.
Monitor Key Performance Indicators: Track key performance indicators (KPIs) such as clean claims rate, days in accounts receivable, denial rate, and collection rate to assess the health of the customer service cycle. revenue and identify areas for improvement. Use data analysis and reporting tools to gain insight into revenue trends and performance metrics.
Foster Payer Relationships: Build strong relationships with payers through regular communication, negotiation, and collaboration. Advocate for fair reimbursement rates and contractual terms that support the financial viability of the practice.
Conclusion
Effective revenue cycle management is essential to the financial success and sustainability of dermatology practices. By understanding the revenue cycle management process, identifying common challenges, and implementing strategies to overcome them, practices can optimize revenue streams, minimize revenue loss, and improve overall financial performance.
Investing in staff training, leveraging technology solutions, establishing clear policies and procedures, monitoring key performance indicators, and fostering relationships with payers are key strategies to overcome revenue cycle management challenges in dermatology billing. By proactively addressing these challenges, dermatology practices can improve their operational efficiency, maximize collections, and provide high-quality care to patients.
#dermatology billing services#dermatology billing#dermatology billing company#dermatology medical billing#dermatology billing and coding#medical billing for dermatology#dermatology medical billing company#dermatology medical billing and coding
0 notes
Text
Simplifying Billing for Dermatology Practices

In the ever-evolving healthcare industry, medical billing services are indispensable for ensuring providers are reimbursed for their expertise and care. Dermatology, a specialized field focusing on skin, hair, and nail disorders, requires precise billing practices to manage its diverse and intricate procedures. From routine consultations to advanced treatments like laser therapy or Mohs surgery, accurate billing ensures smooth revenue flow and compliance with regulatory standards. Dermatology Billing Services streamline these processes, allowing providers to focus on enhancing patient care.
What Are Dermatology Billing Services?
Dermatology Billing Services form an essential part of Revenue Cycle Management (RCM) services tailored specifically to dermatology practices. These services handle all aspects of the billing process, from verifying insurance and coding procedures to submitting claims and following up on payments. Given the diverse range of dermatological treatments, RCM services ensure that each procedure is accurately coded and compliant with insurance guidelines. By managing the entire revenue cycle efficiently, Dermatology Billing Services minimize errors and delays, ensuring timely reimbursements for practices.
The Importance of Dermatology Billing Services
The significance of medical billing and coding in dermatology lies in its ability to ensure financial stability and compliance. Dermatology involves a wide array of treatments, each requiring precise documentation and coding to avoid claim denials or underpayments. Accurate medical billing and coding help capture the full value of services provided, optimizing revenue while reducing the risk of audits or penalties. Effective billing practices also enable dermatology practices to maintain a strong financial foundation, supporting investments in advanced equipment and patient care innovations.
Benefits of Dermatology Billing Services
Incorporating Healthcare IT services into dermatology billing processes offers numerous advantages. Automated systems streamline administrative tasks, reduce manual errors, and accelerate the claims process. Healthcare IT services also provide analytics tools that help dermatology practices monitor financial performance, identify trends, and make data-driven decisions. Furthermore, these systems ensure compliance with regulatory changes, safeguarding practices from potential liabilities. By leveraging technology, dermatology providers can achieve operational efficiency and focus more on delivering quality care to their patients.
How Mediclaim Management Supports Dermatology Practices
Mediclaim Management specializes in providing tailored Dermatology Billing Services designed to meet the unique challenges of dermatology practices. Their experienced team ensures accurate documentation, coding, and claims submission, helping providers minimize denials and maximize reimbursements. Mediclaim Management also uses advanced technology to streamline billing workflows and ensure compliance with industry standards. From insurance verification to tracking unpaid claims, their comprehensive services allow dermatology providers to focus on patient care without the burden of managing complex billing processes.
In conclusion, Dermatology Billing Services are essential for the financial and operational success of dermatology practices. With Mediclaim Management’s specialized solutions, providers can streamline their billing processes, enhance revenue cycles, and ensure compliance with healthcare regulations. By partnering with an expert billing service, dermatology practices can achieve financial stability while continuing to provide exceptional care to their patients.
0 notes
Text
Key Dermatological Billing Trends to Watch for
Providers of dermatology medical billing services will carefully evaluate the documentation and pull out everything related to the procedures to apply the right codes and modifiers. This post highlights the latest updates in dermatology codes that have an impact on dermatology billing and coding. Check out the details here. https://www.outsourcestrategies.com/blog/dermatology-medical-billing-and-coding-key-considerations-for-success/
#dermatology medical billing company#medical billing services#medical billing outsourcing#medical billing companies
0 notes
Text

Know About Dermatology Medical Billing Services
Know About Dermatology Medical Billing Services
Are you struggling as a dermatologist to keep up with your medical billing, or experiencing denied claims? Outsourcing your dermatology medical billing is the way to go.
Unlike some other healthcare providers, dermatologists provide various procedures that need detailed information to be covered by insurance and some are not. There are also constant changes in insurance reimbursement policies, making their medical billing process overwhelming and time-consuming.
So, partnering with seasoned dermatology medical billing services gives you access to a team of professional billers and coders trained to process medical billing for dermatologists. Continue reading as Unify Medcraft takes us through the process of dermatology medical billing and its benefits for healthcare providers.
What is Dermatology Medical Billing Services?
Dermatology medical billing services are companies that help dermatologist process and submit their billing claims to their patients' insurance companies. Dermatologists are healthcare professionals who specialize in the diagnosis and treatment of skin disorders.
Medical billing is an essential part of a dermatologist's revenue cycle and financial growth. Also, during the dermatology billing process, the coder must change the treatment into industry-recognized codes.

Common Medical Codes Used in Dermatology Billing
ICD-10 diagnosis codes for urticaria
L50.0 Allergic urticaria
L50.2 Urticaria due to cold and heat
L50.3 Dermatographic urticaria
L50.5 Cholinergic urticaria
L50.6 Contact urticaria
L50.8 Other urticaria
ICD-10 codes for Acne
L70.0 Acne vulgaris
L70.1 Acne conglobata
L70.4 Infantile acne
L70.5 Acne excoriée
L70.8 Other acne
L70.9 Acne, unspecified
Benefits of Dermatology Medical Billing Service
Choosing to use billing software for your medical billing is a smart move as it makes operations smoother and boosts revenue. It also allows healthcare providers to concentrate more on taking care of their patients.

Here are some of the benefits of outsourcing medical billing services for dermatologists
Promote Focus on Patient Care
Using them to handle their medical billing process reduces their administrative burden and gives healthcare providers the privilege to spend more time with their patients while providing great services.
Precision in Billing Process
The process of dermatology medical billing is often complicated, and any slight errors can lead to claim denials, delayed payments, and compliance issues. Leaving the process to professionals ensures precision and reduces billing errors.
Best for Effective Reimbursement
Eliminating your administrative burdens and continuous staff training by using billing software is a cost-effective solution for healthcare practices that also boosts fast reimbursement.
Improve Cash Flow
When insurance payments are delayed there is an increase in claim denial, it will affect the cash flow of every dermatologist. Using dermatology medical billing services accelerates revenue cycles, ensuring timely payments and consistent cash flow.
Ensures Patient Satisfaction
A nicely organized billing process cannot be overemphasized when it comes to a patient's experience when they visit their dermatologist. Every patient wants clear and accurate billing. When they receive this type of service, they are satisfied and trust the healthcare provider.
Provides Billing Compliance
Healthcare providers must keep up with healthcare regulations which change from time to time. With a billing service, healthcare providers will not have to worry about all that as the companies ensure that their billing process aligns with the latest industry standards.

Increase Revenue Growth
With patient satisfaction, frequent claim acceptance, and faster reimbursement, healthcare providers experience a significant increase in their revenue.
Final Thoughts
Working with a medical billing service provider is very important if you want to succeed as a dermatologist and Unify Medicarft stands out as a reliable choice among others. With Unify Medicraft, you lower the risk of denials on claims submitted and your billing process aligns with the requirements of the healthcare industry.
#dermatology medical billing services#dermatology#medical billing#healthcare#united states#billing software
1 note
·
View note
Text
#revenue cycle management#health#health & fitness#medical billing#medical billing services#medical#healthcare#billing and coding#dermatology#skin health
0 notes
Text
MGSI streamlines Dermatology billing for smoother reimbursements

Automated coding & claim creation frees your team for patient care Stay compliant with ever-changing regulations in dermatology The dedicated support team understands your unique needs Focus on what matters most - healthy patients & a healthy bottom line. Partner with MGSI (Dermatology Medical Billing Services ) today!
0 notes
Text

Benefits of using a dermatology billing service
Discover the advantages of utilizing a dermatology billing services. Streamline your practice's financial processes and enhance revenue management with specialized dermatology billing expertise.
0 notes
Text
#“dermatology Billing Services in US”#“dermatology billing services”#“dermatology billing”#“dermatology billing company”#“dermatology medical billing”#“medical billing for dermatology”#“dermatology medical billing and coding”#“dermatology billing specialist”
0 notes
Text
When the coworker who has been there 15+ years throws their work on you and tells you to figure it out so you try your best and get hit with 2 emails demanding more information that you couldn’t possibly have.


Basically: New doctor wants to use our lab, but they only do cosmetic procedures so that means no insurance is involved. The new doctor requested that all patient bills be sent to their office so the patient can pay in 1 go instead of making an account with us. Ok.
To do this we have to make an account for that doctor. I have no idea how to do this so I ask.
Coworker says “Just email them”
Email who? Why do I have to ask if it’s my first time doing this? It ended up being a specific section of the IT department I needed to email.
Anyway I get the email and IDK wtf I’m supposed to say so I’m just like “Good morning, please create a billing account for a new doctor who will be utilizing our lab. We need to be able to send the patients’ bills to the doctor’s office. Heres the doctor’s information to create the account.”
They ask me to clarify the nature of the services we provide, what is being billed, etc.
Fairly simple questions. It’s a dermatology lab. The doctor sending samples owns a hair transplant clinic. They want our doctors to look at the samples to determine whether a transplant or medication is needed. Straight forward, right?
I get a reply back asking me about billing cycles, procedures being done, billing codes, and what specific requirements the doctors need. They are asking for specifics because apparently these outside doctors owe us a lot of money.
This. Is. Not. My. Job. My job is to verify insurance and keep patient accounts up to date. That’s it.
You know whose job it is to set things up for new doctors? My boss. You know who does the coding for billing? My coworkers. Not me. You know who does the actual billing? The billing department for the whole company, it’s got nothing to do with us.
It just pisses me off that my coworkers can’t be bothered to lift a finger and expect me to figure everything out. And when I can’t because I don’t have access to that information, they call me useless. Getting set up to fail so they can take it out on me. It’s exhausting.
#I just can’t get over asking how do I create the account and being told ‘email them’ who the fuck is ‘them’#genuinely the most useless people ever. then they get mad I’m not super friendly. lol. lmao.
8 notes
·
View notes
Text
The Essential Role of Medical Billing Services in Healthcare

In today’s healthcare landscape, medical billing services are essential to the smooth functioning of healthcare providers. These services ensure that healthcare facilities receive timely and accurate payments from insurance companies for the care they provide. Medical billing services help in converting the work done by healthcare providers into billable claims, allowing for efficient reimbursement. Without these services, healthcare providers would face delays and challenges in securing payments, which could impact their operations and financial stability. In this blog, we’ll discuss what medical services entail, their importance, their benefits, and how Mediclaim Management supports healthcare providers through its expert medical billing services.
What Are Medical Services?
Medical services encompass a wide range of healthcare-related activities, including patient diagnosis, treatment, consultation, and follow-up care. For healthcare providers to maintain effective Revenue Cycle Management (RCM) services, it is essential that each of these activities is accurately recorded, billed, and processed for payment. Medical services also involve routine check-ups, laboratory tests, surgeries, and specialty care, each with unique billing requirements. RCM services play a crucial role in this by managing and optimizing the flow of revenue from patient engagement to final payment collection. By streamlining these processes, RCM services ensure that healthcare providers can focus on patient care while maintaining a steady financial flow.
The Importance of Medical Services
The importance of medical billing and coding cannot be overstated when it comes to processing medical services accurately and efficiently. Medical billing and coding translate every medical service provided into standardized codes, which insurance companies use to process claims. Without accurate coding, healthcare providers risk claim denials, payment delays, or potential revenue loss. Medical billing and coding are crucial for compliance with healthcare regulations, preventing costly errors and ensuring that healthcare providers are paid for the care they deliver. In this way, accurate coding helps bridge the gap between healthcare providers and insurers, ensuring a seamless revenue flow and reducing administrative burden.
Benefits of Medical Services
One of the significant benefits of medical services, particularly with the support of Healthcare IT, is the improvement in operational efficiency. Healthcare IT has transformed the billing and coding process by introducing automation and digital record-keeping, which reduce human error and expedite claims processing. Through automated systems, healthcare providers can track payments, monitor claims, and access valuable data on revenue trends. This technological integration not only helps in reducing claim rejection rates but also allows for better patient data management, reducing redundancies and optimizing staff workload. Additionally, Healthcare IT provides data analytics tools that help healthcare providers make informed decisions to improve overall financial performance and patient care.
How Mediclaim Management Supports Medical Billing Services
Mediclaim Management offers a comprehensive suite of Medical Billing Services designed to support healthcare providers in navigating the complexities of the billing process. With expertise in both medical billing and coding, Mediclaim Management ensures that claims are submitted accurately and on time, minimizing delays and denials. Their team of professionals uses advanced tools and technologies to optimize the billing process, providing healthcare providers with faster reimbursements and more reliable revenue management. Mediclaim Management’s Medical Billing Services include everything from initial patient billing to follow-up on claims, ensuring that providers receive consistent payments for their services.
In conclusion, medical billing services are a crucial aspect of healthcare operations, enabling providers to secure timely payments and focus on quality patient care. With Mediclaim Management’s dedicated Medical Billing Services, healthcare providers can streamline their revenue processes, reduce administrative burdens, and enhance their financial stability.
#medical billing agency#medical billing company#medical billing and coding#medical billing outsourcing#medical billing and credentialing services#medical billing for dermatology
0 notes
Text
ICD-10 Codes to Report Dermatitis
Our post discusses dermatitis – a common inflammatory skin condition and the related ICD-10 codes used to report this condition. Dermatology medical coding involves using the specific ICD-10 diagnosis codes for reporting dermatitis (eczema) on your medical claims. https://www.outsourcestrategies.com/blog/coding-dermatitis-overview-symptoms-icd-10-codes/

#dermatology medical billing#insurance authorization and verification services#general surgery medical billing company#orthopedics medical coding company
0 notes
Text
Not just cats, dogs can be too.
I work at a vet office. One of my coworkers raises seeing eye dog puppies. She has her own personal pets too, one of which is a German shepherd named Bill who flunked the service dog program. He passed his behavior and training exams like a pro but he has bad allergies which forced them to reject him. One of the vets at our work specializes in dermatology and is helping get his itchiness under control. They ran an allergy panel on poor Bill, which came back positive for a whole list of things. The allergen that most caught my attention was listed at the bottom: human dander. Damn tragic.
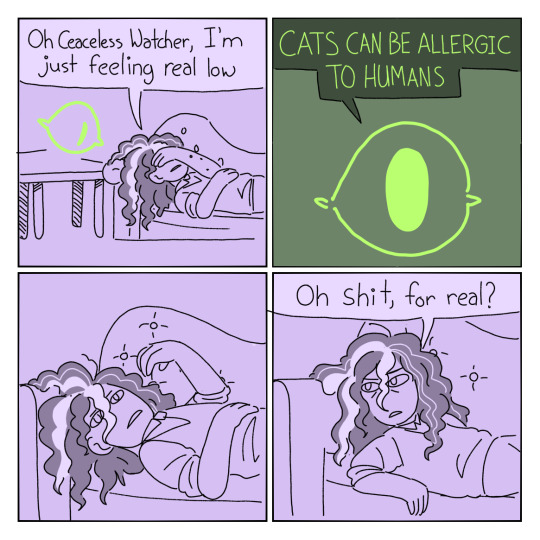
My favorite part of tma is that the eye just airdrops random info into jon's head at random times
Description under cut
[A four panel comic featuring the main character of the Magnus Archives, Jonathan Sims. The comic parodies oniongalic comic about Spinach sending emails. Three of the four panels have purple backgrounds. The second panel is green.
Panel 1- Jon lays on a couch covering his face with his hand. A giant eye floats above the table beside him
Jon: oh ceasless watcher,I'm just feeling real low
Panel 2- the eye is centered in panel. The background is now green and the text box is dark with neon green text.
Eye: CATS CAN BE ALLERGIC TO HUMANS
Panel 3- Jon holds his hand in the air staring into nothing.
Panel 4- Jon leans over to look at eye off panel.
Jon: Oh shit, for real?
Caption: My favorite part of tma is that the eye just airdrops random info into jon's head at random times
End Description]
#Bill is a very good boy and his itch is doing better#he gets to help raise other guide puppies now#be a good example
16K notes
·
View notes
Text
Top EHR EMR Solutions for Telemedicine in 2024 Telemedicine revolutionized health care, such that each and every patient in the world can access services more efficiently. At the core of this telemedicine revolution is EHR EMR software; it brings virtual consultations to a more streamlined management and smooth care for the patients involved.
We came up with this guide—the top 10 EHR EMR software for telemedicine in 2024—an analysis of features, benefits, and, more importantly, the role of each EHR EMR in transforming the landscape of health care.
Understanding EHR EMR Software in Telemedicine EHR (Electronic Health Record) and EMR (Electronic Medical Record) software are the digital backbones of telemedicine.
This service provides access to, manages, and shares patient data with healthcare providers in the course of consultations carried out over virtual space, which would, as such, ensure a smooth flow of communication and continuity of care.
As such, the systems complement in-person and online healthcare delivery, ensuring patients receive the same quality of care regardless of their location.
Why EHR EMR Software Is Important for Telemedicine:
1. Access to patient records simultaneously A telemedicine provider has to have immediate access to patient records. EHR EMR software gathers this information, creating real-time, integrated views of medical histories, lab results, and treatment plans.
2. Better coordination between the care providers EHRs facilitate better collaboration between specialists, primary care providers, and telemedicine platforms to preserve continuity and consistency in patient care.
3. Seamless virtual integration Today, modern EHR solutions are built to integrate telehealth tools such as video consultations, prescriptions, and far-field monitoring from one interface.
4. Compliance with Regulations Telemedicine is regulated strictly under HIPAA. EHR EMR ensures encrypted data and complies with legal standards.
Top 10 EHR EMR Software Solutions for Telemedicine in 2024 1. clinthora As a leading clinic management software provider, clinthora succeeds in delivering telemedicine with EHR EMR support. Their solutions suit the specific needs of today's healthcare practices.
Key Features:
Seamless integration with telehealth Personalized EHR workflows Advanced data security and compliance
Main Features:
Telemedicine scheduling and billing Mobile access for providers Real-time updates on patient care
2. Cerner Millennium Cerner provides cloud-based EHR software that allows for seamless integration of telehealth. This supports patient monitoring, allows for appointment scheduling, and has assured data exchange.
Key Features:
Customizable dashboards AI-powered decision support HIPAA-compliant security
3. Athenahealth Athenahealth is clinic management software with advanced telemedicine solutions added. It simplifies workflows for small to medium-sized practices with its intuitive interface.
4. Allscripts Allscripts is a robust EHR platform all about the world of telemedicine. This ensures connectivity between providers and patients. Interoperability is key for multispecialty practices, and this makes it an excellent choice.
Key Features:
Integrated virtual consultation tools Data-sharing across platforms Advanced analytics for patient trends
5. Kareo Kareo is aimed at small practices and solo physicians. Its telemedicine features are friendly and can be easily set up to allow for efficient remote management of patients.
Key Features:
Telehealth-enabled patient portals Easy to navigate and affordable for start-ups
6. DrChrono DrChrono is an all-in-one solution that brings together electronic health records, practice management, and telemedicine into one application. It is highly versatile and would support various specialties such as dermatology and pediatrics.
Key Features:
Schedule virtual visits E-prescribe with billing tools Wearables compatibility
7. NextGen Healthcare NextGen features an advanced EHR EMR system with strong telemedicine functionalities. It is known for being a patient engagement-cummer business-oriented orientation, deeply emphasizing analytics.
Important Features:
Secure Video Conferencing Automated appointment reminders Voice Recognition Documentation
8. eClnicWorks eClinicWorks comes with a fully featured EHR platform that comes with full telemedicine capabilities. The cloud-based network ensures scalability and timely access for the providers and patients.
Core Features:
Integrated Telehealth Patient Self-Scheduling Population Health Management
9. Greenway Health Prime Suite Greenway Health is pretty powerful in interoperability, where very different healthcare technologies are used by the practice. It supports powerful telemedicine tools for efficient patient-provider interactions.
Core Features:
Cloud-based flexibility Multi-specialty adaptability Advanced charting and documentation
10. Epic Systems Epic Systems continues to be at the forefront in the EHR EMR market, with a strong integration of telemedicine. Its user-friendly system encompasses video appointment capabilities, patient portals, and real-time data exchange.
Key Features:
Patient Record Management Telehealth Tools Integrated Clinics and clinic scale-up
Benefits of EHR EMR Software for Telemedicine: 1. Higher Engagement of Patients Patient portals allow patients to take over the management of their healthcare by accessing their records, scheduling appointments, and more-to-see and talk to providers through the telemedicine system.
2. Reduced Administrative Burden EHR EMR software helps health care providers devote more time to patient care by automating scheduling, billing, and documentation.
3. Scalability for All Practices EHR EMR software can accommodate both small clinics and big clinics, as telemedicine demands vary.
4. Data-driven insights Advanced analytics may share actionable insights about patient trends, helping providers provide proactive and personalized care based on insights.
5. Increased Access Patients in rural or underprivileged locations enjoy the service of telemedicine, whereby EHR EMR software is robust, ensuring timely attention.
Telemedicine EHR EMR Solution Implementation Challenges
1. Integration Complexity EHRs may not integrate well with telehealth devices. Therefore, the complexity of integrating might be the operational inefficiencies.
2. High Start-Up Cost Even though telemedicine ensures long-term cost-saving practices, a high upfront cost might be challenging, including software and training costs.
3. Threat of Cyberattacks The electronic storage of sensitive patient data puts health systems at risk of breaches and cyberattacks.
4. Technical Obstacles for Patients Some patients, especially older patients, may not be able to operate successfully through digital channels.
5. Inflexibility to Change Health care providers who are used to traditional approaches have an avoidance of adopting telemedicine technologies.
Future Telemedicine Trends: EHR EMR Software
1. AI-Based Analysis Artificial intelligence will be highly focused on automating diagnostic and predictive analytics, as well as treatment prescriptions.
2. Blockchain for Data Security Blockchain will help build trust through trusted and unalterable data-sharing platforms for telemedicine web pages. 3. Integration of Wearable DevicesFitness tracking devices, full health monitors, as well as smartwatches, will be linked with EHRs to give real-time data interpretation.
4. Global Collaboration EHR's feature is cross-border telemedicine, therefore opening up new opportunities for partners in global healthcare practices and joint research initiatives.
5. Personalized Telehealth Experience Future systems using machine learning technology will navigate virtual visits based on the needs of patients, thus improving the quality of care and satisfaction.
Conclusion The top 10 EHR EMR software solutions in 2024 represent the pinnacle of what can be defined as innovation in health care. Through their more efficient and patient-centered services, these platforms bridge the gap between physical care and its virtual counterpart. Telemedicine, with the right EHR EMR solution, ensures staying ahead in this digital healthcare revolution.
For clinics wishing to upgrade their telemedicine offerings, clinthora is always available as a trusted and all-inclusive solution that ensures smooth integration and delivery with other interventions.
0 notes
Text
Top Medical Billing Companies in NY: Streamline Your Revenue Cycle Today!
Top Medical Billing Companies in NY: Streamline Your Revenue Cycle Today!
In the healthcare industry, efficient medical billing is crucial for ensuring that healthcare providers receive timely payments for their services.As the demands of billing adn coding evolve, healthcare providers in New York are increasingly turning to specialized medical billing companies to manage their revenue cycles. This article will provide a comprehensive overview of the top medical billing companies in New York,along with practical tips for selecting the best fit for your practice.
Understanding Medical Billing and Its Importance
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for services rendered. A streamlined revenue cycle not only increases cash flow but also minimizes errors that can lead to delays in payments. Here are some key reasons why medical billing is essential:
Improved Cash flow
Reduced Administrative Costs
Enhanced Focus on Patient Care
Minimized Billing Errors
Benefits of Outsourcing Medical Billing
Outsourcing medical billing to professional companies can offer several advantages:
Expertise: Medical billing companies have expertise in the latest coding standards and reimbursement processes.
Cost-Effective: Businesses save money by avoiding hiring, training, and maintaining an in-house billing team.
Scalability: Medical billing companies can handle fluctuations in volume, ensuring that practices can focus on growth.
Technology: These companies often use advanced software solutions to streamline processes and enhance accuracy.
Top Medical Billing companies in New York
Here is a list of some of the top medical billing companies in New York that can definitely help streamline your revenue cycle:
Company name
Services Offered
Website
AdvancedMD
Medical Billing, RCM, EHR
advancedmd.com
Optimum Billing
Claims Processing, Denial Management
optimumbilling.com
MedBillingExperts
Billing Services, Coding, consulting
medbillingexperts.com
CareCloud
Revenue Cycle Management, EHR
carecloud.com
eCatalyst Healthcare Solutions
billing, Coding, Consulting
ecatalysths.com
Case Studies: Prosperous Implementation of Medical Billing Services
To understand the impact of outsourcing medical billing,let’s take a look at two case studies.
Case Study 1: A Growing Dermatology Practice
A dermatology practice in New York was struggling with billing delays, resulting in cash flow issues. By outsourcing its medical billing to a specialized firm, the practice saw a 30% increase in collections within the first six months. The billing company’s expertise in handling dermatological codes increased the accuracy of claims.
Case Study 2: Multi-Specialty Medical Group
A multi-specialty medical group was facing challenges with claim denials and slow reimbursements. After partnering with a leading medical billing company,the group experienced a 25% reduction in denial rates within three months. The company’s effective denial management strategies played a crucial role in this success.
Practical tips for Choosing a Medical Billing Company
Choosing the right medical billing company can be daunting. Here are some practical tips to help you make an informed decision:
Evaluate Experience: Look for companies with experience in your specialty to ensure they understand the specific billing codes and requirements.
check Reviews and Testimonials: Research online reviews and case studies to gauge the company’s reputation and performance.
Assess Technology: Inquire about the technology and software they use, as an efficient system can substantially impact billing accuracy.
Understand Fee Structures: Be clear on how the company charges for services; some may charge a percentage of collections, while others may have a flat fee.
Seek Communication: Ensure that the company communicates effectively and provides regular updates on your practice’s revenue cycle.
Conclusion
Streamlining your revenue cycle is essential for the financial health of any healthcare practice. By partnering with one of the top medical billing companies in NY, you can alleviate the challenges associated with billing and coding, improve your cash flow, and ultimately enhance patient care.
Remember to assess your specific needs, conduct thorough research, and choose a medical billing partner that aligns with your practice’s vision. The right company can transform your billing process and significantly boost your practiceS profitability. Start your journey towards a more efficient revenue cycle today!
youtube
https://medicalbillingcertificationprograms.org/top-medical-billing-companies-in-ny-streamline-your-revenue-cycle-today/
0 notes