#ConcussioninSport
Explore tagged Tumblr posts
Text
New Days Could be Dawning
A 13-part series to illuminate the way forward in the grip of suicide, drug overdose, diabetic amputations, and mental health epidemics. Readers in this space are all familiar with the headlines: Football leads to brain damage and CTE. Suicides continue to increase no matter how much more money DoD and the VA spend on Suicide Prevention strategies. Veterans are being subjected to BLAST injuries from their own weapons. Parents should avoid letting their children bang their heads in sports until they’re 14 years old. Society is experiencing increasing numbers of neurogenerative diseases at younger ages. More and more money is being spent on research to use psychoactive and hallucinogenic drugs to cope with mental health problems. 988 Suicide Crisis Line counselors are burned out, quitting, undertrained and understaffed. From football fields to battlefields to America’s classrooms and assisted living facilities, citizens and policymakers and the medical profession are wondering what can be done about suicides, “mental health” and the growing sense that daily life is causing damage to our brains. Whether it’s sports, or legal and illegal drugs, or violence, or online abuse and bullying and shaming, or mass casualty events, or the suicide and opioid epidemics, increasing numbers of young and old have “mental health problems.” We seem to be losing our minds. To a certain extent, what may seem like increased mental health challenges may be due to increased diagnoses stemming from better awareness and understanding. Increased media attention, social media, economic pressures, and isolation may contribute to higher awareness. Increased longevity and improved diagnoses may be behind seemingly larger numbers of age-related dementias. But doesn’t it just seem that there’s an abnormal number of people suffering from diminished capacity? And that no matter how much we spend, we keep getting more pleas from victims, survivors, care givers, politicians, medical staff and social media for solutions? Congressional hearings, Foundation Annual reports, investigative reporting, government fact-finding, and personal experience make it obvious that we’re falling behind while the suicide and drug overdose and mental health epidemics worsen. You’ve heard the adage: “Better to light a candle than to curse the darkness.” The TreatNOW Coalition has been taking steps for over 15 years to light candles, to educate, to end Veteran suicides, and to change medicine. Thus, the start of this 13-part series to light several candles. Not only to point out problems, but much more importantly to offer solutions that already exist. The choice is between politics and progress, between cursing “wicked complex problems” and applying proven solutions. This series will bring you some central truths and, importantly, lay out solutions to the challenges posed by a perhaps misnamed “mental health crisis” in our military and across the country. Ensuing chapters will discuss the estimated $600 Billion per year mental health costs that are only projected to consume more of our national wealth. And the World Economic Forum projects that the cost of mental health conditions and their related consequences will rise to $6 trillion globally by 2030. Together with the GruntStyle Foundation, TreatNOW and multiple other organizations aim to arrest and reverse the suicide and prescribed drug overdose death epidemics afflicting our Veterans, Armed Forces, and society. Both the VA and DoD have declared that suicide prevention is their #1 clinical priority. Based on budget choices, it would seem we’re serious about finding and applying, quickly, some methods that will work against suicidal ideation almost the way penicillin works against bacterial infections like pneumonia, meningitis, and syphilis. Part 1. Just how big is the “problem?” This series intends to tackle a range of subjects that afflict Veterans, especially suicide and drug overdoses which, along with diabetic lower limb amputations, are at epidemic levels. Across military medicine and traditional approaches to “mental health,” there is a wide gap between the palliative care model – control symptoms – and root cause analysis that gets at the physical damage and whole body wellness called for. This includes proper diagnoses and a shift to an appreciation of polytrauma and brain wound healing. Part 2. Modern War is just so damned dangerous: BLAST Injury, Burn Pits, and the nature of whole body damage/polytrauma. Includes a primer on brain wounding. Part 3. The VA/DoD Approach: Intrepid Center, DVBIC, Intrepid Spirit Centers, WRIICs, PREP, Care Coalitions, and Independent Wellness Centers. Part 4. VSOs and the Growth of 66,000 Veteran Help Organizations since 9/11 Part 5. The insidious Service Member Epidemics: Suicide, Drug Overdosing, and diabetic foot ulcers, lower limb amputations, and the hundreds of thousands of deaths directly attributable to lack of informed consent. Part 6. The Sports Industry: Making contact sports and life in general safer while engaging in a real scientific dialogue about brain wounding, the concussion cascade, "The Concussion Protocol,” and “the new normal” after brain wounding. Part 7. Eisenhower didn’t even get it half right: The Military, Industrial, Contractor, Research, Academic, Lobbyist, Insurance, and Pharmaceutical Complex. Lessons in Bureaucratic Politics and how to sort out a path to success. Part 8. Integrative/Functional/Wholistic/Complementary and Alternative Medicine. You don’t have to throw away institutions or current practices to make them better. Part 9. Alternative Therapies: Hyperbaric Oxygen Therapy (HBOT) and a new paradigm in whole body healing. Part 10. Alternative Therapies: Devices, Processes, Computers, and Artificial Intelligence. Part 11. Alternative Therapies: Non-Prescription Drugs/ Psychedelics/Supplementation/Nutrition/Diet/Lifestyle. Part 12. How to hold the Congress, White House, VA and DoD, and sports industry accountable for the Epidemics and lack of brain wound healing protocols. Part 13. SUMMARY: The Shortest Paths to Success. How to change the language around “mental health,” arrest and reverse upward trends in deaths through suicides, prescription drug overdoses, lower limb amputations, and restore Quality of Life to brain wounded Veterans and citizens. We welcome your comments. The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#blastinjury#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#HBOTTreatment#HealingwithHyperbarics#HyperbaricOxygentherapy#mentalhealth#MilitarySuicide#opioidepidemic#posttraumaticstressdisorder#PTSD#SuicidePrevention#TBI#traumaticbraininjury#VeteranSuicide#VeteranSuicidePrevention
0 notes
Photo

Regrann from @nicolawhite201 - Really insightful @rawtalkpodcast @spotify to understand more about concussion & it's hollistic management. • • Amazing how misunderstood it still is to a lot of people, but thankful that it is now becoming widely recognised in the medical world as a serious injury 👍 • • Check it out if you're interested in this area or if you're an athlete going through concussion too. The more you understand what is going on, the more you can minimise stress & anxiety around the injury! I've found it very helpful recently plus I love science & knowing why things happen so its been good for me to research. • • Happy listening 👍🎧 • #concussion #concussioninsport #braininjuryawareness #alwayslearning #everevolving #podcast #education #sports #athletes #ifindoubtsititout #hockey #Repost #HockeyFamily #HockeyVibe #StrongerTogether - #regrann https://ift.tt/2oZqPqS
0 notes
Photo

#recognisingconcussion - Taking risks is an inherent part of riding mountain bikes, but it is important to recognise when a rider has suffered a #concussion. Loss of consciousness only occurs in 10% of concussions! Make sure you know when to spot it and treat your head right! Link in bio for the full post. * * * * * #mountains #mountainbiking #mtb #downhillmtb #instamtb #mountainbikeguide #mtblife #mtbcoach #neurology #mentalhealth #loveyourbrain #concussioninsport #concussionaware #sportsinjuries 📸 @mike_jra
#instamtb#mountains#mentalhealth#mountainbiking#concussioninsport#concussion#downhillmtb#neurology#sportsinjuries#mtblife#mtbcoach#mtb#loveyourbrain#mountainbikeguide#concussionaware#recognisingconcussion
0 notes
Text
What the world knows that the VA does not: Hyperbaric Oxygen Therapy is safe, effective and can restore health

Athletes are waking up to the Use of Hyperbaric Oxygen Therapy for brain wound healing, health, endurance, peak performance, and the competitive edge. Game Changer for Football Teams? A high-profile college football program began using HBOT to manage player injuries and fatigue. The therapy quickly became a key factor in their injury management and prevention strategy. The team noted shorter recovery periods after injuries, and players were able to return to play faster than before, demonstrating HBOT's efficacy in a high-contact sports environment. Numerous professional athletes use HBOT. 100 Yards of Wellness Will Offer HBOT to Clemson Athletes Nov 22, 2022 100 Yards of Wellness, Clemson’s new $4.9-million wellness space at Allen N. Reeves Football Complex that spans roughly 300 feet in length that has become a central hub of activity and major point of pride for Tiger football. The treatment and training room area includes all requisite athletic training resources, including a diagnostic office with a full digital X-ray space and diagnostic ultrasound, general medical exam room, 30 yards of turf and hydrotherapy areas, including two underwater treadmills. Among the many features of the recovery center are: • A hyperbaric chamber to create a pressurized environment for concentrated oxygen intake. • A cryotherapy chamber for muscle recovery through extreme cold temperature exposure. • A sensory deprivation float tank that houses 1,200 pounds of Epsom salt dissolved in water at skin temperature to remove athletes from light, sound and some gravitational force. • Infrared hyperthermic Cocoon pods for Far-Infrared light therapy and vibrational massage. • Photobiomodulation therapy beds that leverage multiple wavelengths of infrared light to reduce oxidative stress. • Numerous massage chairs, including both percussive massage and hydromassage options. • Percussive Hypervolt massage guns. • Dedicated tables and space for practitioner-assisted stretching, percussive massage gun therapy and Normatec compressive sleeves provided to each player prior to the season. • Functional testing equipment to obtain objective information on student-athlete muscle and joint function that can be used for injury prevention and return-to-play purposes. The Rise of Hyperbaric Oxygen Therapy in Professional Football: A Game-Changer for Recovery and Performance Sep 5, 2023 By Mudassir Sajad In the fast-paced world of professional football, where every second counts, players are constantly seeking ways to gain a competitive edge. One such method that has been gaining traction is Hyperbaric Oxygen Therapy (HBOT). This innovative treatment has been endorsed by top-tier athletes like Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar, who have all been spotted on social media using hyperbaric chambers Hyperbaric Oxygen Therapy is proving to be a revolutionary treatment in the realm of professional football. Mo Salah, Marcus Rashford, Vinicius Junior, and Neymar endorsing its benefits, it's clear that HBOT is more than just a passing trend. Moreover as science continues to validate its efficacy, we can expect to see more football clubs adopting this cutting-edge technology to give their players the competitive edge they need. Dr. Joe Maroon on Hyperbaric Oxygen Dr Joe Maroon Joseph Maroon is an American neurosurgeon, author, and triathlon athlete. He is the professor and vice chairman of the Department of Neurological Surgery at the University of Pittsburgh Medical Center and is the current medical director of WWE. For over 20 years he has served as the neurosurgical consultant to professional and college athletes in football, baseball, golf, hockey and soccer and was team neurosurgeon to the Pittsburgh Steelers for over 40 years. As early as 2011, Dr Maroon and Dr Bost wrote: "Alternative nonpharmaceutical treatments appear to be gaining acceptance for the treatment of common neurodegenerative conditions, memory decline, and reduced cognitive function. Substantial animal and human research now suggests that these same natural dietary supplements, vitamins and minerals, and the use of hyperbaric oxygen may be a better first-line choice for the treatment of PCS, which has generally been underreported by both athletes and the military." Maroon and Bost, Concussion Management at the NFL, College, High School, and Youth Sports Levels. Clinical Neurosurgery. Volume 58, 2011, Chapter. 7. The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help end symptoms of PTSD, and heal brain wounds to end the effects of BLAST injury, mild TBI Persistent Post Concussive Syndrome, and polytrauma. www.treatnow.org Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
CTE Plagues Heisman Trophy Winners and Families
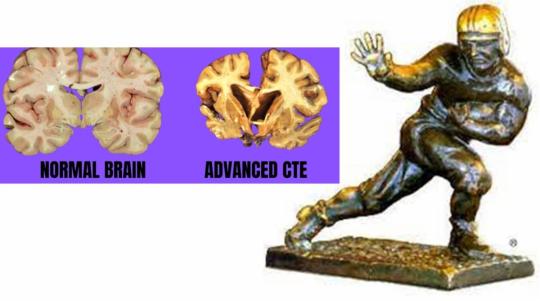
Three-quarters of 1,035 brains of football players -- over 700 --examined at Boston University had CTE The "taboo topic" is the centerpiece of "The Other Heisman Club" in the Washington Post, Dec 9, D1, by Kent Babb: the number of former Heisman winners with diagnosed or suspected Chronic Traumatic Encephalopathy (CTE). The degenerative brain disease is increasingly in the news for a number of reasons. Four Heisman winners have been posthumously diagnosed with the disease: Howard Cassady, Pat Sullivan, Paul Hornung and Charles White. The implication in the article is that more winners already exhibit symptoms of CTE but whose families can't "know" until after death. But the families know. Something is wrong. Sadly, silence is the preferred approach. And the unwillingness of our society to confront the obvious doesn't make it any easier. And the "whistling through the graveyard" approaches to concussions and the Concussion Protocols used worldwide don't provide much guidance about an alternative approach to Brain wounding. Facts matter: - Four percent of Heisman trophy winners died of CTE, and the list of their wounded fellow winners is growing. If you extrapolate those numbers to the 25,000 former NFL players, over 1,000 of them are probably carrying the CTE markers. - Three-quarters of 1,035 brains of football players, 0ver 700, examined at Boston University had CTE. - Researchers at Boston University found CTE in 92 percent of former NFL players who were analyzed: they analyzed the brains of 376 deceased former NFL players and diagnosed 345 of them with chronic traumatic encephalopathy. - More than half of the homeless have experienced traumatic brain injury and 1 in 4 have had moderate to severe brain injuries. - Approximately 876,450 post-9/11 veterans suffer from untreated brain wounds. - Researchers estimate that as many as 60% of incarcerated individuals are living with TBI, significantly higher than the 8.5% reported in the general population. - Studies on prison and jail populations have reported a range of 25-87% of inmates reporting head injuries or TBI. Of course, it is traditional to attack these numbers. Nay-sayers will demand more research. Hand-wringing by stake-holders on both sides will, like protests after mass-shootings, last a while and then subside. If anything, more dollars will go into researching how to make contact sports more safe. And treatments that are non-pharmaceutical will be ignored. Since "everyone knows there's no treatment for brain injuries," the best we can hope for from the medical profession is contained in the latest proceedings out of Boston. The Robert C. Cantu Concussion Summit was held on December 8, 2023, at the Cantu Concussion Center at Emerson Hospital in Concord, MA. The theme of the conference was "Prevention of Concussion and Long-Term Effects of Repetitive Traumatic Brain Injury (RTBI)." In what is becoming a repetitive list of findings, the conference summarized: - Eliminate intentional or avoidable head impact in contact and collision sports in both practices and games. - Encourage policies and rules that limit the number, duration, and intensity of contact sport practices. - Reinforce proper and safer techniques that avoid head contact at all levels of play. - Implement rules of play that reduce and penalize intentional or avoidable contact to the head and neck. - Correlating specific clinical symptoms with CTE neuropathology remains an important area for further investigation. - Improve the criteria for Traumatic Encephalopathy Syndrome (TES) through further research. Feel better? More importantly, if you are the parent of someone with a brain wound, what actionable intelligence can you take from that list? How will that list help you and yours deal with the here-and-now of a TBI/Concussion-suffering loved-one? If you'd like to learn more about what is happening, and what you can do, view this earlier Blog. Additional information is here. Below is an insightful film about brain wounds https://youtu.be/Zzbxrnm7jXc?si=IPKC5InadR0Eho52 https://treatnow.org/brain-wound-update-5-concussion-blast-tbi-cte/ The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can end suicidal ideation, help heal the effects of BLAST injury, TBI/PTSD, and acute concussion. Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts

August 28, 2023 Ann C. McKee, MD1,2,3,4,5,6,7; Jesse Mez, MD, MS2,3; Bobak Abdolmohammadi, BA2; et alMorgane Butler, BSc2,8; Bertrand Russell Huber, MD, PhD1,2,3,5,6; Madeline Uretsky, MS2; Katharine Babcock, PhD2,8; Jonathan D. Cherry, PhD1,2,4; Victor E. Alvarez, MD1,2,3,5; Brett Martin, MS2,9; Yorghos Tripodis, PhD2,7,9; Joseph N. Palmisano, MS2,9; Kerry A. Cormier, BA1,2,5; Caroline A. Kubilus, BA2,5; Raymond Nicks, MS1,2,3,5; Daniel Kirsch, BA2,4; Ian Mahar, PhD2; Lisa McHale, EdS2,10; Christopher Nowinski, PhD2,10; Robert C. Cantu, MD2,10,11,12; Robert A. Stern, PhD2,3,12; Daniel Daneshvar, MD, PhD2,13; Lee E. Goldstein, MD, PhD2,14,15; Douglas I. Katz, MD3,16; Neil W. Kowall, MD2,3; Brigid Dwyer, MD3,16; Thor D. Stein, MD, PhD1,2,4,5; Michael L. Alosco, PhD2,3 Author Affiliations Article Information JAMA Neurol. Published online August 28, 2023. doi:10.1001/jamaneurol.2023.2907 Audio (16:39) Neuropathologic and Clinical Findings in Athletes With Repetitive Head Impacts
Key Points
Question What are the neuropathologic and clinical findings in a convenience sample of young, deceased, symptomatic contact sport athletes? Findings In this case series of 152 contact sport athletes younger than 30 years at the time of death, chronic traumatic encephalopathy (CTE) was found in 63 (41.4%), with nearly all having mild CTE (stages I and II). Neuropathologic abnormalities associated with CTE included ventricular enlargement, cavum septum pellucidum, thalamic notching, and perivascular pigment–laden macrophage deposition in the frontal white matter. Meaning These findings confirm that CTE and other brain pathologies can be found in young, symptomatic contact sport athletes, but the clinical correlates of these pathologic conditions are uncertain.
Abstract
Importance Young contact sport athletes may be at risk for long-term neuropathologic disorders, including chronic traumatic encephalopathy (CTE). Objective To characterize the neuropathologic and clinical symptoms of young brain donors who were contact sport athletes. Design, Setting, and Participants This case series analyzes findings from 152 of 156 brain donors younger than 30 years identified through the Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Brain Bank who donated their brains from February 1, 2008, to September 31, 2022. Neuropathologic evaluations, retrospective telephone clinical assessments, and online questionnaires with informants were performed blinded. Data analysis was conducted between August 2021 and June 2023. Exposures Repetitive head impacts from contact sports. Main Outcomes and Measures Gross and microscopic neuropathologic assessment, including diagnosis of CTE, based on defined diagnostic criteria; and informant-reported athletic history and informant-completed scales that assess cognitive symptoms, mood disturbances, and neurobehavioral dysregulation. Results Among the 152 deceased contact sports participants (mean age, 22.97 years; 141 male) included in the study, CTE was diagnosed in 63 (41.4%; median age, 26 years). Of the 63 brain donors diagnosed with CTE, 60 (95.2%) were diagnosed with mild CTE (stages I or II). Brain donors who had CTE were more likely to be older (mean difference, 3.92 years; 95% CI, 2.74-5.10 years) Of the 63 athletes with CTE, 45 (71.4%) were men who played amateur sports, including American football, ice hockey, soccer, rugby, and wrestling; 1 woman with CTE played collegiate soccer. For those who played football, duration of playing career was significantly longer in those with vs without CTE (mean difference, 2.81 years; 95% CI, 1.15-4.48 years). Athletes with CTE had more ventricular dilatation, cavum septum pellucidum, thalamic notching, and perivascular pigment-laden macrophages in the frontal white matter than those without CTE. Cognitive and neurobehavioral symptoms were frequent among all brain donors. Suicide was the most common cause of death, followed by unintentional overdose; there were no differences in cause of death or clinical symptoms based on CTE status. Conclusions and Relevance This case series found that young brain donors exposed to repetitive head impacts were highly symptomatic regardless of CTE status, and the causes of symptoms in this sample are likely multifactorial. Future studies that include young brain donors unexposed to repetitive head impacts are needed to clarify the association among exposure, white matter and microvascular pathologic findings, CTE, and clinical symptoms.
Introduction
Across the world, millions of people are exposed to repetitive head impacts (RHIs) through participation in contact and collision sports, military service, physical violence, and many other activities.1-6 Repetitive head impacts can result in symptomatic concussions and the much more frequent, nonconcussive injuries that are asymptomatic.7 Sustained exposure to RHIs can produce persistent cognitive and neuropsychiatric symptoms8-11 and a progressive, tau-based neurodegenerative disease, chronic traumatic encephalopathy (CTE).12-21 Multiple studies13,15,22 link a longer duration of RHI exposure in US football players with increased odds for the presence of CTE and increased severity of CTE. In older American football players with pathologically diagnosed CTE, RHI exposure is also associated with white matter rarefaction,23-25 loss of myelin associated proteins,26 and oligodendrocyte loss.27 Emerging data show structural white matter alterations on magnetic resonance imaging (MRI) in young, active, and recently retired contact sport players exposed to RHI,1,2,28-30 although the pathologic condition underlying these changes is unclear. A definitive diagnosis of CTE requires neuropathologic evidence of perivascular hyperphosphorylated tau (p-tau) aggregates in neurons, with or without astrocytes, typically at the depths of the sulci in the cerebral cortex.31,32 The clinical syndrome associated with CTE is known as traumatic encephalopathy syndrome (TES).8,33 On the basis of the National Institute of Neurological Disorders and Stroke (NINDS) consensus diagnostic criteria for TES,8 the core clinical features of TES include cognitive impairment, especially episodic memory and executive dysfunction, and neurobehavioral dysregulation, such as impulsivity, explosivity, and emotional dysregulation.8 Supportive features include delayed onset (ie, core clinical features starting years after RHI exposure ends), parkinsonism, other motor signs (including amyotrophic lateral sclerosis), depression, anxiety, apathy, and paranoia. The Understanding Neurologic Injury and Traumatic Encephalopathy (UNITE) Brain Bank1 has harvested brains from more than 1350 donors exposed to RHIs who are considered at risk for CTE. Brain donors in the UNITE bank vary widely in age at death and include teenagers and young adults. Chronic traumatic encephalopathy has been reported in individuals as young as 17 years,13 yet, to date, there have been no large-scale neuropathologic and clinical studies of young individuals exposed to RHIs. Attention to this age group has several important implications. The study of young athletes allows insight into the earliest features of RHI-induced neuropathologic injury and CTE. Furthermore, it allows analysis in the absence of common age-associated comorbidities. Moreover, most of these young contact sport athletes played only at amateur levels, as part of teams affiliated with educational institutions; consequently, the study of young athletes adds to our understanding of the long-term consequences of amateur contact sports participation. In this report, we describe the neuropathologic and clinical features of 152 brain donors from the UNITE brain bank who were younger than 30 years at the time of death.
Methods
Brain Donors and Study Design The initial sample for this case series included 156 deceased individuals with a history of exposure to RHIs from contact sports participation who donated their brain to the UNITE Brain Bank from February 1, 2008, to September 31, 2022, and were younger than 30 years at the time of death. Race was determined by next-of-kin report and was included to understand the representativeness of the sample and the associated generalizability of the results. Procedures of brain donation have been previously described.14,34 The inclusion criterion was based on the presence of a history of exposure to RHIs without regard to symptom status. The restriction to brain donors younger than 30 years was selected to minimize any contribution from age-related conditions. Donors were excluded for poor tissue quality. Four donors were excluded because of incomplete brain fragments or prolonged premortem hypoxia, resulting in a final sample size of 152. Institutional review board approval for brain donation, postmortem clinical record review, interviews with informants, and neuropathologic evaluation was obtained through the Boston University Medical Campus and the Veterans Affairs Bedford Institutional Review Board. The next of kin or legally authorized representative of each brain donor provided written informed consent. The methods for this report followed the appropriate use and reporting of uncontrolled case series in the medical literature reporting guidelines.35
Neuropathologic Evaluation
Neuropathologic evaluation occurred blinded to the clinical evaluation by neuropathologists (A.C.M., B.R.H., V.E.A., and T.D.S.). Pathologic processing and evaluation were conducted using previously published methods and as described in the eAppendix in Supplement 1.12-14,34,36 Neuropathologic diagnoses were made using NINDS National Institute of Biomedical Imaging and Bioengineering criteria for CTE31,32 and well-established criteria for other neurodegenerative diseases.37-40 The CTE p-tau pathologic findings were classified into 4 stages using the McKee staging scheme for CTE. Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#CTE#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
BRAIN WOUND UPDATE #9 - But is a Concussion a "Wound"?
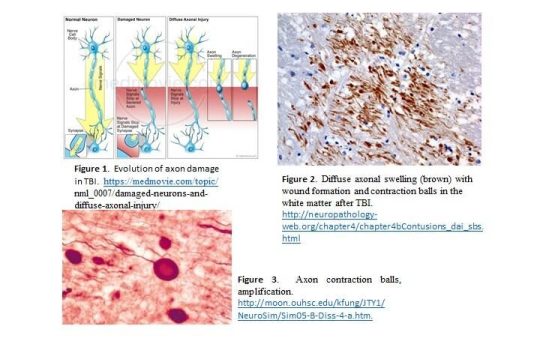
Proper Imaging Reveals the Physical Damage from Concussion and TBI
BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD Advanced imaging is outpacing medicine's ability to keep up with implications of the "new" brain science, and the nature of brain wounding. Medical textbooks are out-of-date with respect both to the nature of brain wounds and treatments to heal those wounds. Drs. Carol Henricks and Paul Harch have put forward current scientific understandings.
Concussion: Not Just a Brain Bruise
Jun 30, 2022 08:00AM ● By Carol L. Henricks Awareness of concussion injury exploded with the movie Concussion in 2015. The correlation between multiple concussions and neurodegenerative conditions was brought to the big screen. The common analogy of concussion being a “brain bruise” suggests that it is a minor injury that should recover in a few days without any permanent consequences. However, this is not true. Our brains are uniquely designed and complex, more sophisticated than any computer. Every activity is a function of networks in the brain. The brain tissue injury that occurs as the result of concussion is complex and disruptive. Concussion is the result of many kinds of trauma that cause the brain to be shaken around inside the skull, causing diffuse axonal injury (DAI). DAI creates lesions all throughout the brain, damaging the myelin (the fatty coating around axons), and may cause damage to deeper axonal structures. Diffuse injury disturbs network communication in the brain. Synapses—where one brain cell or neuron uses neurotransmitters to communicate with another brain cell—can be pulled apart, therefore disrupting cell-to-cell communication. The microenvironment of electrolytes and other brain-specific chemicals around the brain cells, glia and other support cells is disrupted and may effect electrical conductivity and functioning of cells. Even a minor concussion may cause breaches in the blood brain barrier (BBB). A breach in the BBB allows chemicals, toxins and infections access to the brain when they would otherwise be blocked. The microtubular structure that internally organizes the neuron and allows transport of neurotransmitters to the synapse may be disrupted and disable cellular function. Brain cells that are damaged and not restored to function begin a process of degeneration; this dying back of the cell leads to cell death and brain atrophy. This is the definition of a neurodegenerative process. Neurodegenerative processes include dementia, Parkinson’s disease and ALS. Functional recovery—restoring the ability to read, sleep and balance, visual function and depth perception, cognitive activities and more—can be addressed by therapy, where some re-wiring and re-networking of the brain may occur. However, decline may still occur because functional recovery is different from biologically and physiologically healing the brain. Military veterans, first responders and athletes in contact sports are at great risk for concussion and recurrent concussion, which causes cumulative injury and a high risk for neurodegenerative conditions. Traditional Brain MRI sequences, even with contrast, do not aid in diagnosing concussion because they do not highlight the disconnections. Brain MRI – DTI (diffusion tensor imaging) sequencing and/or Brain Quality SPECT scanning are the imaging tools of choice. Objective computer-based functional testing, including the RightEyeQ test (a standardized objective test of visual fixation and follow), reaction time testing and formalized balance testing, are objective and predictive, which is a good way to establish a baseline. Take brain health seriously and pursue meaningful testing and active treatment for concussion. Carol L. Henricks, M.D. is a neurologist specializing in the use of hyperbaric oxygen therapy (HBOT) and PEMF at NorthStar Hyperbaric, in Tucson. (HBOT) saturates the body with oxygen, reducing inflammation and enhancing recovery from central nervous system injury. Connect at 520-229-1238 or NorthStarHBOT.com. ########## Dr. Paul Harch has cleared up the confusion In a seminal Meta Analysis: Systematic Review and Dosage Analysis: Hyperbaric Oxygen Therapy Efficacy in Mild Traumatic Brain Injury Persistent Postconcussion Syndrome. TBI (5, 6) is a heterogeneous (7–27) diffuse physical injury to the brain that causes mechanical (7, 8, 28, 29) disruption of gray (22–24, 30, 31) and white (10, 15, 22, 23, 30, 32–35) matter, ischemia (36), hypoxia (29, 37, 38), edema (29, 39, 40), vasospasm (41, 42), release of neurochemicals (43, 44), and reperfusion injury (39, 45) and affects over 4.1 million people annually in the U.S. alone ( Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#PostconcussionSyndrome#TBI#TBItreatment#traumaticbraininjury
0 notes
Text
BRAIN WOUND UPDATE #8: "New" Discoveries but Old News to Scientists Studying Brain Wounds

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD - Military suicide rate rose 25% in first quarter, Pentagon reveals JULY 05, 2023 TIMOTHY FRUDD In an alarming update from the Pentagon, suicide rates among active-duty military personnel saw a 25% rise in the first quarter of 2023 compared to the same period last year. The suicide rate data was revealed in the recent quarterly report by the Defense Suicide Prevention Office, which found the total number of active-duty suicides was recorded at 94, up from 75 during the first quarter of 2022. “Every death by suicide is a tragedy,” the report said. “Data includes all known or suspected suicides (both confirmed and pending) as of March 31, 2023.” According to Stars and Stripes, the Army suffered the most significant surge in suicide deaths, with an increase from 37 to 49. Meanwhile, the Marine Corps saw an increase from eight to 14. The Air Force had one more suicide compared to 2022, and there was no change in the suicide rates within either the Navy or Space Force. The Pentagon’s data shows a rising trend in military suicides over the past decade, including a pronounced spike in 2020 amid the coronavirus pandemic. Beth Foster, executive director of the Pentagon’s Force Resiliency Office, spoke to this growing concern, saying, “There is still a gradual increasing trend for suicide in the military over a 10-year period, and we need to see a sustained long-term reduction in suicide rates to know if we’re really making progress.” The Defense Suicide Prevention Office noted that the numbers in the report are preliminary and are subject to change upon further investigations and reports of previously unknown suicide cases. The Pentagon’s comprehensive yearly study on military suicides, set to analyze the data from 2022, is due for release in October. ********** - Redefining Depression: TBI Affective Syndrome Discovered - Neuroscience News https://neurosciencenews.com/tbi-affective-syndrome-23580/ Summary: A new study suggests that depression post-traumatic brain injury (TBI) may be a distinct disease separate from traditional major depressive disorder. This revelation, arising from unique patterns observed in brain maps of TBI patients, could revolutionize the treatment for such individuals. The study proposes a new term for this variant of depression – “TBI affective syndrome”. Fundamentally, this research marks a significant step toward personalized treatment strategies for TBI patients. Key Facts: • Depression post-TBI might be a distinct disorder separate from traditional major depressive disorder. • The study suggests the term “TBI affective syndrome” for this variant of depression. • Personalized brain mapping revealed unique patterns in TBI patients, leading to the theory of this distinct depressive disorder. Source: Brigham and Women’s Hospital A new study led by Shan Siddiqi, MD, from Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, suggests that depression after traumatic brain injury (TBI) could be a clinically distinct disorder rather than traditional major depressive disorder, with implications for patient treatment. The findings are published in Science Translational Medicine. ********** - Researchers identify first case of CTE found in a female athlete The HILL BY NICK ROBERTSON - 07/05/23 Australian researchers have identified the first case of chronic traumatic encephalopathy (CTE) in a female athlete. The brain injury has been commonly found in American football players and other contact sport athletes, but the discovery of the condition in a female athlete is a first. Heather Anderson was an Australian rules football player who died by suicide last year at 28. An analysis of her brain found she had early-stage CTE caused by repeated head trauma. “There were multiple CTE lesions as well as abnormalities nearly everywhere I looked in her cortex,” researcher Michael Buckland, director of the Australian Brain Sports Bank, told The Washington Post. “It was indistinguishable from the dozens of male cases I’ve seen.” Her family donated her brain to researchers to learn more about her death. Scientific literature is inconclusive on the relationship between CTE and suicidality, but the condition is known to cause memory issues, personality changes and erratic behavior. Anderson retired from Australian rules football, a contact sport similar to rugby, after a career-ending shoulder injury in 2017. Her father described the CTE diagnosis as “a surprise but not a surprise,” in an interview with the Australian Broadcasting Corporation. Rhw research, published Tuesday in the journal Springer, notes that a few women have been diagnosed with CTE before, but never an athlete. The research says the low number of female diagnoses is likely because the sports where CTE is most common, American football and boxing, are male-dominated. CTE worsens as athletes suffer more head injuries and in longer careers. The condition can only be diagnosed posthumously via an autopsy. Researchers said athletes who start playing contact sports young are at the greatest risk of CTE. Anderson began playing Australian rules football at 5 years old, her family said. Women are also more susceptible to concussions than men, raising their risk for the condition, researchers said. “There has been a significant increase in women’s participation in contact sports over the past decade. … This report may, thus, represent a sentinel case: as the representation of women in professional contact sports is growing, it seems likely that more CTE cases will be identified in female athletes,” the study states. Nearly 350 American football players, 90 percent of those studied, have been posthumously diagnosed with CTE. ########## The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the symptoms and effects of acute concussion/TBI/PTSD by helping heal the brain. Heal Brains. Stop Suicides. Restore Lives. TreatNOW Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#MilitarySuicide#sportsinjury#SportsRelatedConcussions#suicide#suicideepidemic#SuicidePrevention#TBI#TBItreatment#traumaticbraininjury#VeteranSuicide
0 notes
Text
BRAIN WOUND UPDATE #7: More Shortcomings in Concussion Consensus Protocol

BRINGING YOU CURRENT INFORMATION ABOUT HOW TO HELP TREAT AND HEAL BRAIN WOUNDS: CONCUSSIONS, TBI, PTSD This report brings you information about the Consensus Statement on Concussion in Sport: the 6th International Conference on Concussion in Sport–Amsterdam, October 2022. For the sixth time, an international assemblage of specialists have come together to refine a document, purportedly to keep interested parties aware of the best information available concerning Concussion in Sport. And for the sixth time, the Conference has failed to talk about or recommend treating and healing brain wounds/TBI/Concussion. Backup papers to the Conference last year also fail to address healing brain wounds. Nowhere in the documents can you find mention of "brain wound" or a fundamental component of wound healing: OXYGEN. In fact, there is precious little medical advice, much less a protocol or even mention of the latest research and clinical evidence describing the work done worldwide to treat and heal brain wounds, including Concussion, using Hyperbaric Oxygen Therapy (HBOT) and scientifically validated alternative therapies. The group of over 300 specialists met to refine detection and assessment of Sports Related Concussions (SRC). Much was made of refining the definition of concussion and clarification and expansion of "the 13 Rs" guiding what could be considered a "Concussion Conference Cascade" of guiding principles published in the British Journal of Sports Medicine. Ancillary papers are also available. The ‘13 Rs’ of Sport Related Concussion now include: RECOGNISE, REDUCE, REMOVE, REFER, RE-EVALUATE, REST, REHABILITATE, RECOVER, RETURN-TO-LEARN/RETURN-TO-SPORT, RECONSIDER, RESIDUAL EFFECTS, RETIRE, and REFINE. What about REPAIR? To not be talking about the latest science concerning healing brain wounds -- most Concussions are mild Traumatic Brain Injuries (TBI) -- is a form of collective inattention. A dozen years of worldwide research have produced peer-reviewed science and over 21,000 success stories using HBOT to treat and help heal brain wounds. Even YouTube has a record of the stories recorded in over 135 TreatNOW Coalition clinics. Dr Joe Maroon, the Pittsburgh Steelers Medical Director for decades, should be part of any discussions about the use of HBOT for Concussions, along with Drs. Daphne Denham and Paul Harch. Here's a downpayment on a REPAIR Section in any Concussion Consensus document worthy of conscientious science and medical accuracy. REPAIR. The science and practice of wound healing is as applicable to repairing brain wounds/Concussion as it is to repairing diabetic foot ulcers and non-healing wounds, flaps, grafts, crush injuries, and burns. The FDA has already approved Hyperbaric Oxygen Therapy for 14 Indications, many of which are nearly identical to the Invisible Wound of Concussion. Most often, concussed victims will hear that most concussions get better in time. The Cleveland Clinic states: "Concussions stretch and bruise nerves and blood vessels and cause chemical changes in your brain that result in a temporary loss of normal brain function. A single concussion usually doesn’t cause permanent damage to your brain. Multiple concussions over a lifetime may result in structural changes in your brain. Concussions are not usually life-threatening. However, the effects from a concussion can be serious and last for days, weeks or even longer." They continue: "What’s the difference between a concussion and a traumatic brain injury? Really there is no difference. Both are considered injuries to the brain. These are virtually the same terms." Try this exercise: just Google "concussion treatment." You'll find that huge industries have grown up around Concussion Management and Rehabilitation, not Successful Treatment and Healing. Current, generic "treatment" includes: - Over-the-counter pain relievers. - Drinking plenty of water. - Getting enough rest. - Taking a break from sports and other strenuous activities. - Not driving a vehicle right away. - Avoiding alcohol while recovering. - Brain rest. Minimize use of electronics (including TV, cell phone, computer) to allow your brain time to heal. - Avoid bright lights and noises Note that "treatment" always includes observation, rest, and gradual progression through steps or stages to ensure the patient does not get another concussion. Yet nowhere in any Concussion Protocol or Consensus document -- whether the NFL/NBA/MLB, FIFA, NHL, NCAA or the myriad other sports -- will you find mention of the need for root cause analysis of the brain wound and accompanyin g symptoms, and how to use "alternative" medicine to heal that wound. "Oxygen" is not discussed, the fundamental natural drug demanded by the brain for healing. Further, huge arguments are ongoing about how fast a patient should start exercising after a concussion, but this is no mention of the role of exercise in delivering increased blood flow and oxygen to the brain wound. No surprise that patients heal faster with HBOT since it deliver 8-12 times more O2, reduces inflammation, repairs damage by growing more stem cells, blood vessels, and neurons. So here's a primer for patients and parents and caregivers and coaches and trainers. - A concussion is a brain wound. Some "heal" on their own; a sizeable percentage cause lingering symptoms. - Over 3.5 million ER visits a year are due to concussions. it is estimated that there are 3-5 million citizens negatively afflicted with life-long symptoms of varying severity due to unhealed brain wounds. - Hyperbaric Oxygen therapy is virtually unknown to medicine as a healing modality to treat brain wounds/Concussion/TBI. It is seldom taught in medical school. Mothers and fathers and athletes are not told they can seek healing help. - HBOT is not insured for Concussion. Average cost of one dive is $250-300. Consider that against 6 weeks - 6 months or longer of life altering symptoms like headaches, nausea, loss of memory, sleeplessness, anxiety, inability to focus, lack of energy, depression, etc. - Untreated brain wounds/Concussion/TBI can lead to degenerative brain damage and Chronic Traumatic Encephalopathy (CTE) - CTE can only be diagnosed after death. The Boston University CTE Center announced in 2023 that they have now diagnosed 345 former NFL players (out of 376) with CTE. - Current Concussion Protocols have nothing to do with healing the brain wound. Worldwide, the "standard" treatment is rest and exercise and hoping the injury gets better. Not one intervention for Concussion/TBI is approved by the FDA and there is no discussion from trainers or doctors about brain wound healing. - Hyperbaric Oxygen Therapy has been shown to heal Acute Concussions after five, one-hour sessions. It eliminates suicidal ideation, alleviates symptoms, and allows patients to get back to work, school, and play symptom-free. No two concussions are alike and multiple brain wounds exacerbate the damage and time to heal. - Don't expect anyone to tell you that HBOT is available and has been proved safe and effective. You may hear it is unproven, dangerous, or too costly; most won't know. Follow doctor's orders, but go further. Do your own research. Talk to someone who actually knows and has read the latest research. View some success stories. The TreatNOW Mission is ending service member suicides. Along the way, we have learned that we can help heal the effects of acute concussion while healing the brain.
Heal Brains. Stop Suicides. Restore Lives. TreatNOW
Information provided by TreatNOW.org does not constitute a medical recommendation. It is intended for informational purposes only, and no claims, either real or implied, are being made. Read the full article
#brainhealth#braininjured#braininjury#brainwound#concussion#ConcussioninSport#concussionprotocol#ConcussionSymptoms#concussiontreatment#HBOT#HBOTTreatment#HeadImpact#HealingwithHyperbarics#hyperbaric#HyperbaricOxygentherapy#sportsinjury#SportsRelatedConcussions#TBI#TBItreatment#traumaticbraininjury
0 notes