#ASXL1
Explore tagged Tumblr posts
Text
Updated Screening Guidelines
A new publication was recently published by Patel et al. 2024 on two children with Bohring-Opitz Syndrome, who are diagnosed with liver cancer. These two, together with a previously known case, are now three individuals diagnosed with hepatoblastoma described in the medical literature. Hepatoblastoma is a very rare malignant liver cancer occurring in infants and children and can spread to other…
View On WordPress
#ASXL1#Bohring-Opitz and Cancer#Bohring-Opitz Syndrome#Hepatoblastoma#Screening Guidelines#Wilms tumor
0 notes
Text
SRSF2 mutation cooperates with ASXL1 truncated alteration to accelerate leukemogenesis
http://dlvr.it/SzS4JT
0 notes
Text
What Is Clonal Haematopoiesis, What To Know?
In the intricate landscape of the human body, the circulatory system, powered by blood, stands as a crucial lifeline. However, beneath the surface of this vital fluid lies a fascinating phenomenon known as clonal haematopoiesis. Recently discovered and still under extensive research, clonal haematopoiesis has piqued the curiosity of scientists and medical professionals alike. In this blog, we will delve into the world of clonal haematopoiesis, exploring its definition, implications, and what we need to know about this enigmatic process.
Understanding Clonal Haematopoiesis
Clonal hematopoiesis is a relatively new term in the realm of medicine, first gaining recognition in the early 2010s. It refers to a condition where a single mutated stem cell or a group of mutated stem cells give rise to identical copies of themselves, leading to the production of a large number of identical blood cells. These cells can carry specific genetic mutations that confer a competitive advantage to them, allowing them to outgrow and outnumber their normal counterparts in the blood.
Normally, the genetic material of our cells is susceptible to random mutations due to environmental factors or errors in DNA replication. However, our body has a robust system to repair these mutations and maintain the integrity of our genetic code. Clonal haematopoiesis arises when this repair mechanism fails, leading to the accumulation of mutations in a small population of blood stem cells.
Implications and Significance
While clonal haematopoiesis was initially considered a benign age-related phenomenon, recent research has revealed its potential connection to serious health conditions. Studies have shown that individuals with clonal haematopoiesis have a higher risk of developing various hematologic malignancies, such as leukemia, myelodysplastic syndromes (MDS), and myeloproliferative neoplasms (MPNs). Additionally, it has been linked to an increased risk of cardiovascular diseases, including heart attacks and strokes.
The most common mutation observed in clonal haematopoiesis involves a gene called DNMT3A. Other frequently mutated genes include TET2, ASXL1, and JAK2. Interestingly, some of these mutations are shared with certain blood cancers, further highlighting the complexity of this phenomenon.
Diagnostic Challenges
Detecting clonal haematopoiesis poses a challenge in clinical settings. It is often asymptomatic, and its presence may go unnoticed without thorough genetic testing of blood samples. As such, researchers are working to develop more accurate and sensitive tests to identify individuals at risk.
Potential Therapeutic Avenues
Despite the potential risks associated with clonal haematopoiesis, researchers are optimistic about uncovering therapeutic avenues. By understanding the molecular and cellular mechanisms underlying this phenomenon, they hope to develop targeted treatments to prevent the progression of clonal haematopoiesis into full-blown blood disorders.
Moreover, ongoing research is focused on identifying factors that contribute to the development of clonal haematopoiesis. Genetic predisposition, lifestyle choices, and environmental factors are all areas of investigation.
Conclusion
Clonal hematopoiesis may still be a relatively new concept, but its implications for health and disease have caught the attention of the medical community. Understanding the mysteries of this phenomenon holds the potential to revolutionize the diagnosis and treatment of blood disorders and cardiovascular diseases. As research continues, we can hope for a future where early detection and intervention will minimize the impact of clonal hematopoiesis on our health, leading to improved outcomes and quality of life for affected individuals.
0 notes
Text
Oncotarget: Hispanic Chronic myelomonocytic leukemia patients
Oncotarget: Hispanic Chronic myelomonocytic leukemia patients
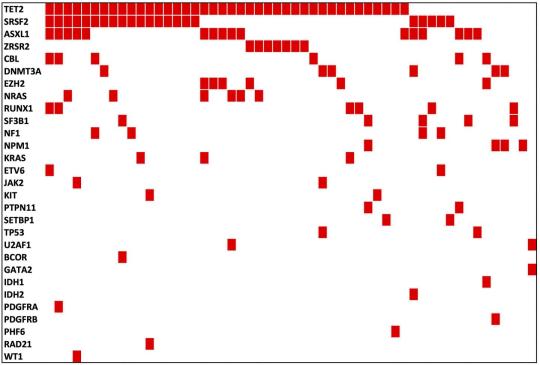
This Oncotarget study had significantly lower mutation rates in ASXL1 and SETBP1, and a higher rate of muTET2/wtASXL1 Credit: Correspondence to – Jie-Gen Jiang – [email protected] Oncotarget published “Cytogenetic and molecular landscape and its potential clinical significance in Hispanic CMML patients from Puerto Rico” which reported that one hundred and eleven Hispanic CMML patients from…
View On WordPress
1 note
·
View note
Text
Myelodysplastic Syndrome: Epidemiology Forecast to 2028 published on
https://www.sandlerresearch.org/myelodysplastic-syndrome-epidemiology-forecast-to-2028.html
Myelodysplastic Syndrome: Epidemiology Forecast to 2028
Myelodysplastic Syndrome: Epidemiology Forecast to 2028
Summary
MDS are rare and a diverse group of clonal hematopoietic malignancies characterized by cytogenetic and molecular abnormalities, causing bone marrow failure and risk of progression to AML. MDS can affect people of any age but usually is most common in the 70 years and older population, with approximately 86% of newly diagnosed cases in older population over the age of 60 years. MDS patients present with symptoms related to peripheral cytopenias, though they may also be asymptomatic and routine laboratory findings might not detect anything significant except abnormal blood counts.
GlobalData epidemiologists used age- and sex-specific diagnosed incidence and prevalence rates to forecast the diagnosed incident and prevalent cases, taking into account the significant relationship between age and MDS incidence and prevalence. GlobalData epidemiologists applied country-specific incidence and prevalence rates of MDS, wherever available, to each country’s population to obtain the number of estimated diagnosed incident and prevalent cases.
The following data describes epidemiology of MDS cases. In 2018, the 8MM had 90,332 diagnosed incident cases of MDS. This is expected to increase to 111,861 diagnosed incident cases by 2028, at an Annual Growth Rate (AGR) of 2.38%. This increase is partly attributed to the moderately rising trend in incidence in the 8MM, combined with underlying demographic changes in the respective markets. The 8MM will also see an increase in five-year diagnosed prevalent cases of MDS throughout the forecast period at an AGR of 2.35%, with 236,076 cases in 2018 and 291,581 in 2028. The development of more effective therapies, particularly for elderly patients, would improve survival from MDS.
Scope
– Myelodysplastic syndrome (MDS) Epidemiology Report provides an overview of the risk factors and global trends of MDS in the eight major markets (8MM: US, France, Germany, Italy, Spain, UK, Japan, and Canada). – This report also includes a 10-year epidemiological forecast for the following segmentations in ages 18 years and older across the 8MM: diagnosed incident cases and five-year diagnosed prevalent cases of MDS, and diagnosed incident cases of MDS/myeloproliferative neoplasms (MDS/MPN); diagnosed incident cases of MDS by subtypes (MDS with single lineage dysplasia, MDS with ring sideroblasts, MDS with multilineage dysplasia, MDS excess blasts, MDS with isolated del(5q), and MDS, unclassifiable), risk groups (very low risk, low risk, intermediate risk, high risk, and very high risk), primary/secondary, and mutations (IDH1, IDH2, SF3B1, ASXL1, TET2, RUNX1, JAK2, and TP53). – The MDS Epidemiology Report is written and developed by Masters- and PhD-level epidemiologists. – The Epidemiology Report is in-depth, high quality, transparent and market-driven, providing expert analysis of disease trends in the 8MM.
Reasons to Buy
The MDS Epidemiology series will allow you to – – Develop business strategies by understanding the trends shaping and driving the global MDS market. – Quantify patient populations in the global MDS market to improve product design, pricing, and launch plans. – Organize sales and marketing efforts by identifying the cancer subtypes that present the best opportunities for MDS therapeutics in each of the markets covered. – Understand magnitude of MDS market by biomarkers, risk group, and mutations.
0 notes
Text
ASXL1 mutations, previous vascular complications and age at diagnosis predict survival in 85 WHO-defined polycythaemia vera patients.
Pubmed: http://dlvr.it/RQJ6Kp
0 notes
Text
Anti-cancer effects of curcumin on myelodysplastic syndrome through the inhibition of enhancer of zeste homolog-2 (EZH2).
Anti-cancer effects of curcumin on myelodysplastic syndrome through the inhibition of enhancer of zeste homolog-2 (EZH2).
Curr Cancer Drug Targets. 2019 Feb 12;:
Authors: Ma L, Zhang X, Wang Z, Huang L, Meng F, Hu L, Chen Y, Wei J
Abstract Enhancer of zeste homolog-2 (EZH2), a histone methyltransferase that regulates histone H3 methylation of lysine27 (H3K27me3), is involved in the pathogenesis of myelodysplastic syndrome (MDS). Targeting epigenetic regulators has been identified as a potential treatment target in MDS chemotherapy. Curcumin, a natural compound extracted from turmeric, was found to possess a wide range of anticancer activities in various tumors. This study was designed to investigate the inhibitory effect and action mechanism of curcumin in myelodysplastic syndrome (MDS) in vitro and in vivo. Our results showed that curcumin can significantly suppress cell proliferation and induce cell apoptosis and cell cycle arrest in human MDS-derived cell lines. It reduced EZH2, DNA methyltransferase 3A(DNMT3a), ASXL1 and downstream H3K4me3, H3K27me3 and HOXA9 expression and inhibited EZH2 and H3K27me3 nuclear translocation. Curcumin also showed anti-cancer effects in a xenograft mouse model and reduced EZH2, H3K4me3 and H3K27me3 in vivo. EZH2 knockdown can reduce the H3K27me3 levels and induce curcumin resistance in vitro but attenuates leukemic transformation in vivo. These findings provide the potential molecular mechanism of curcumin as a therapeutic agent for MDS.
PMID: 30747066 [PubMed - as supplied by publisher]
http://bit.ly/2BAw5Ig
0 notes
Text
Interactive Visual Aid
Interactive Visual Aid on symptoms, concerns, and treatment options for ASXL1/Bohring-Opitz Syndrome.
It’s Bohring-Opitz Syndrome Awareness Day! This year we present Your Interactive Visual Aid (IVA) on the most common symptoms of Bohring-Opitz Syndrome (BOS), which have been described in the medical literature and case studies in recent years between 2006 – 2023. We also highlight treatment options noted in the important “Bohring-Opitz Syndrome” research. Although children with Bohring-Opitz…

View On WordPress
0 notes
Text
CRISPR/Cas9-mediated ASXL1 mutations in U937 cells disrupt myeloid differentiation.
CMLHope.Com http://dlvr.it/QhRVG3
0 notes
Text
Genetic Leukemia Detection Testing Market Forecast and Opportunity Assessment by Future Market Insights 2017-2027
Out of general types of blood cancers (Lymphoma, Leukemia, and Lymphoma), leukemia accounts for 36 % of the cases according to the American Cancer Society. Leukemia is the cancer of the blood forming tissues, which includes the bone marrow and the lymphatic system in the body. There are many types of leukemia, some are more common in children and others are more common in men. The white blood cells are the second line of defense in the human body that grow normally and divide in an orderly way, as per the requirements of the body. But in people with leukemia, there is an abnormal growth of white blood cells, which do not function properly. No fixed explanation of the cause of leukemia exists. It is believed to be developed from a combination of genetic and environmental factors.
There are changes in the cells which are yet to be understood to contribute to leukemia. Based on the speed of progression and the type of cells involved, leukemia can be classified into, namely acute leukemia (abnormal cells are immature blood cells) and chronic leukemia (abnormal cells are mature blood cells). Based on the type of white blood cells affected, leukemia can be classified into lymphocytic Leukemia and myelogenous. The major types of leukemia are acute lymphocytic leukemia (ALL), acute myelogenous leukemia (AML), chronic lymphocytic leukemia (CLL), and chronic myelogenous leukemia (CML).
Request for sample Report:https://www.futuremarketinsights.com/reports/sample/rep-gb-6733
Genetic Testing For Leukemia Detection
Leukemia is a genetic disease, but it isn’t hereditary. It is caused by mutations in the genes caused by lifestyle risk factors such as smoking, exposure to certain radiations or chemicals. There are various genetic testing kits available for genetic testing of leukemia. These tests are done to identify mutations in some of the following genes, namely FLT3, CEBPA, KIT, N-RAS, MLL, WT1, IDH/2, TET2, DNMT3A and ASXL1. These tests are done using fluorescence in-situ hybridization test kits, PCR test kits, and ELISA test kits. The tests are done in hospitals, diagnostic centers, clinics, research centers and some of these kits can be availed by the customers without a doctor’s prescription. Out of the various genetic testing methodologies for leukemia, fluorescence in-situ hybridization and PCR take only a couple of days to identify the mutations whereas cytogenetic testing takes around 2-3 weeks, because it takes time for the cells to start dividing. Hence FISH and PCR are the most lucrative segments under the Genetic Leukemia Detection Testing market.
Drivers and Restraints for the Genetic Leukemia Detection Testing Market
Leukemia is the most common form of cancer in children. It accounts for approximately 35% of all cancers diagnosed in children under the age of 15. The urgency to identify any prospects of leukemia, and hospitals shifting towards tests which are advanced and less time consuming are the important factors driving the genetic leukemia detection testing market. The growing awareness about various early genetic detection tests drives the Genetic Leukemia Detection market. However, the costs of the tests and lack of awareness in the emerging regions might restrain the growth of genetic leukemia detection testing market.
Regional Outlook for Genetic Leukemia Detection Testing Market
Though leukemia accounts for approximately 3 % of all the cancers, the prevalence for Leukemia is highest in North America, Latin America, Eastern Europe and Western Europe. China and Asia Pacific excluding Japan follow the list in terms of prevalence. Japan and Middle East and Africa stand last in the list as the prevalence is less compared to other regions of the world.
Genetic Leukemia Detection Testing: Key Players
Examples of some of the key players identified in the genetic leukemia detection testing market are Thermofisher Scientific, Creative Diagnostics, Vector Labs, TCS Biosciences Ltd., Alchem Diagnostics, Vela Diagnostics, Beckman Coulter, ELItechGroup.
Request for Brows-Full Report:https://www.futuremarketinsights.com/reports/genetic-leukemia-detection-testing-market
0 notes
Text
Blindsided
New Story has been published on https://enzaime.com/blindsided/
Blindsided
An American tourist visiting London tries to cross the street. Instinctively, he looks to the left first. Finding it clear, he steps off the curb, looks to the right, and is immediately flattened by one of those double-decker buses they have over there. Whoops!
I’ve been feeling a little bit like that lately. For a long time now, my multiple myeloma journey has been sailing along on cruise control. My numbers have been fine with no evidence of monoclonal gammopathy. I am now on Cycle 54 of my Revlimid maintenance therapy. The only glitch was a reduced iron level in 2014 causing some anemia. I received an iron infusion which remedied the problem. Then this happened again this year, which I mentioned in my last post. I received another iron infusion in September, which has again boosted my red blood cell counts back up to normal. So all is good, right?
As I metaphorically look to the left, I see an undisturbed 4 plus years of my MM in complete remission. The road is clear. However, as I step off the curb and look to the right, Bam! The double-decker bus turns out to be the spectre of Myelodysplastic Syndrome (MDS). MDS is a form of blood cancer where the bone marrow doesn’t produce enough healthy blood cells. This is a serious blood disorder which has a high risk of becoming Acute Myeloid Leukemia (AML), an even more serious blood cancer. It has long been known that MM patients are at a heightened risk for developing MDS/AML, possibly due to treatment-related effects of the chemotherapy (such as the melphalin I had for my ASCT).
In August, Paul informed me that he had ordered a blood test genetic profile for me, which revealed that I have some genetic mutations that predispose me to develop MDS. While my numbers show that I don’t (yet) have MDS, he put me on Vitamin B1 and folic acid as a precaution. He also referred me for a consult with Dr. David Steensma at the Farber, who specializes in MDS.
I started to do some research (surprise) and was a bit nonplussed to discover from the gene profiling pathology report that one of the genetic mutations I have is ASXL1. For patients with MDS, the ASXL1 oncogene is associated with high-risk aggressive disease with poor clinical outcomes. Gulp! I also learned that one of the first signs of MDS is often anemia. Could my iron deficiency have something to do with this?
So I was understandably a bit nervous when I met with Dr Steensma today. He was great! He immediately put me at ease and allayed some of my concerns. For one thing, he assured me that my recent history of iron deficiency is completely unrelated to MDS. MDS-related anemia is an entirely different mechanism. That’s good! Also, since my CBC blood test results are almost completely normal, there is no sign of impending MDS. He likened my condition to MGUS, a precursor asymptomatic condition to MM, which has a small (about 1%) annual chance of progressing to full MM. In my case, since I have two oncogenes identified (the second one is SH2B3, another MDS predisposition gene), I may have a somewhat greater chance of progressing to MDS, but he thinks it is still pretty small.
I told him that with my bad genetics, if I do contract MDS, I’m fucked. Is there anything available to forestall getting MDS with my predisposition oncogenes? He said there is some recent research being done on this, and that there will soon be a clinical trial to see if administering some chemo to at-risk patients who have been pretreated for another blood disease could prevent the onset of MDS. I intend to follow up on this research.
This was a great relief! All I have to do is continue to monitor my blood counts. If I become anemic again due to iron deficiency, it’s not MDS. If it’s not due to iron deficiency, then I need to explore further. In the meantime, I plan to look both ways before stepping off the curb!
I’ve scheduled a colonoscopy/endoscopy for next month to see if there might be a reason I’m losing iron. I sure hope it’s not colon cancer!
As for the other patient in our household, Gretchen is slowly recovering from her recent esophagectomy. It has not been an easy recovery. She has had to go back to Dr. Kent twice to have her esophagus dilated. While this definitely improved things, she is still having trouble eating solid foods, so she may have to go back again for another dilation. She also has a lot of nausea and is really tired, but she was told that this is all pretty normal. We just hope that she gets through this phase sooner rather than later.
#ASCT#chemo#clinical trial#colonoscopy#esophagectomy.#MDS.#Myelodysplastic Syndrome#pretreated#Cancer
0 notes
Text
ASXL1 frameshift mutations drive inferior outcomes in CMML without negative impact in MDS
http://dlvr.it/Q30fkJ
0 notes
Text
#cancers, Vol. 11, Pages 1600: Mutational Landscape of the BAP1 Locus Reveals an Intrinsic Control to Regulate the #miRNA Network and the Binding of Protein Complexes in Uveal Melanoma
The BAP1 (BRCA1-associated protein 1) gene is associated with a variety of human #cancers. With its gene product being a nuclear ubiquitin carboxy-terminal hydrolase with deubiquitinase activity, BAP1 acts as a tumor suppressor gene with potential pleiotropic effects in multiple tumor types. Herein, we focused specifically on uveal melanoma (UM) in which BAP1 mutations are associated with a metastasizing phenotype and decreased survival rates. We identified the ubiquitin carboxyl hydrolase (UCH) domain as a major hotspot region for the pathogenic mutations with a high #evolutionary action (EA) score. This also includes the mutations at conserved catalytic sites and the ones overlapping with the phosphorylation residues. Computational protein interaction studies revealed that distant BAP1-associated protein complexes (FOXK2, ASXL1, BARD1, BRCA1) could be directly impacted by this mutation paradigm. We also described the conformational transition related to BAP1-BRCA-BARD1 complex, which may pose critical implications for mutations, especially at the docking interfaces of these three proteins. The mutations affect - independent of being somatic or germline - the binding affinity of #miRNAs embedded within the BAP1 locus, thereby altering the unique regulatory network. Apart from UM, BAP1 gene expression and survival associations were found to be predictive for the prognosis in several (n = 29) other #cancer types. Herein, we suggest that although BAP1 is conceptually a driver gene in UM, it might contribute through its interaction partners and its regulatory #miRNA network to various aspects of #cancer. Taken together, these findings will pave the way to evaluate BAP1 in a variety of other human #cancers with a shared mutational spectrum. http://bit.ly/31uMbNZ
0 notes
Text
RASSF1A hypermethylation is associated with ASXL1 mutation and indicates an adverse outcome in non-M3 acute myeloid leukemia
from # All Medicine by Alexandros G. Sfakianakis via alkiviadis.1961 on Inoreader http://ift.tt/2veFc0a
from OtoRhinoLaryngology - Alexandros G. Sfakianakis via Alexandros G.Sfakianakis on Inoreader http://ift.tt/2vpIauZ
0 notes
Text
ASXL1 impairs osteoclast formation by epigenetic regulation of NFATc1.
Pubmed: http://dlvr.it/QlrRJt
0 notes
Text
MiR-10a and HOXB4 are overexpressed in atypical myeloproliferative neoplasms
Abstract
Background
Atypical Myeloproliferative Neoplasms (aMPN) share characteristics of MPN and Myelodysplastic Syndromes. Although abnormalities in cytokine signaling are common in MPN, the pathophysiology of atypical MPN still remains elusive. Since deregulation of microRNAs is involved in the biology of various cancers, we studied the miRNome of aMPN patients.
Methods
MiRNome and mutations in epigenetic regulator genes ASXL1, TET2, DNMT3A, EZH2 and IDH1/2 were explored in aMPN patients. Epigenetic regulation of miR-10a and HOXB4 expression was investigated by treating hematopoietic cell lines with 5-aza-2’deoxycytidine, valproic acid and retinoic acid. Functional effects of miR-10a overexpression on cell proliferation, differentiation and self-renewal were studied by transducing CD34+ cells with lentiviral vectors encoding the pri-miR-10a precursor.
Results
MiR-10a was identified as the most significantly up-regulated microRNA in aMPN. MiR-10a expression correlated with that of HOXB4, sitting in the same genomic locus. The transcription of these two genes was increased by DNA demethylation and histone acetylation, both necessary for optimal expression induction by retinoic acid. Moreover, miR-10a and HOXB4 overexpression seemed associated with DNMT3A mutation in hematological malignancies. However, overexpression of miR-10a had no effect on proliferation, differentiation or self-renewal of normal hematopoietic progenitors.
Conclusions
MiR-10a and HOXB4 are overexpressed in aMPN. This overexpression seems to be the result of abnormalities in epigenetic regulation mechanisms. Our data suggest that miR-10a could represent a simple marker of transcription at this genomic locus including HOXB4, widely recognized as involved in stem cell expansion.
https://ift.tt/2qKr7CR
0 notes