#5 Stages of IVF
Explore tagged Tumblr posts
Text
#5 Stages of IVF#5 Stages of IVF Treatment#Understanding the IVF Process Step by Step#Starting with Fertility Tests and Consultation#Ovarian Stimulation and Monitoring#Egg Retrieval Procedure#Fertilization and Embryo Development#Embryo Transfer and Waiting for Results#How Long Does Each IVF Stage Take?#Tips to Prepare for IVF at Every Stage
0 notes
Text

So Elon has decided to skip the imminent disaster of global climate change and just move on to a calamity 5 billion years in the future.
If you ever need to understand Elon's motivations, it's all this.
Okay and a little bit the woke mind virus.
But mostly this.
He wants to get to Mars more than anything. It's why the only thing he can speak intelligently about is his rockets. He has put in the time and effort to learn about them because this is his singular passion.
A lovely Youtube physicist did a video about SpaceX and she said half of the rockets blow up and Elon just wants more money. And it was disappointing to hear her say that because she is a scientist and both things are inaccurate.
SpaceX would be an amazing company without Elon. His leadership is the only thing really holding it back. They have put lots of cool shit into space. Their Falcon program is the most productive and cheapest rocket program in history. They put more stuff into space than everyone else combined.
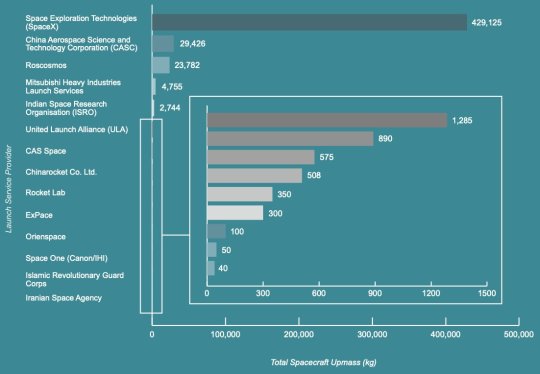
They had to blow up part of the graph just so you could see the competition. Half of the SpaceX rockets are *not* blowing up.
Starship is a specific prototype. It has nothing to do with their main rocket business. Starship is Elon wanting to go to Mars. It is basically him trying to send a 3 story building into space. And he keeps blowing it up because that is the fastest way to develop a rocket. He's wasting a lot of money by trying to speedrun a trip to Mars in his lifetime. And these tests are bit more like crash test data than expecting the rocket and Starship to actually function properly. It's a process and they have goals for each launch, and for the most part, they reach those goals. Any success after those goals is gravy to them. But they are pretty certain it is going to end in fireworks at this stage of development.
I don't know if they will get it to work. It would be nice because a functional spaceship that size could do a lot of cool science. But Elon's goals and NASA's goals are going to conflict in a major way at some point in the future. And I'm worried that may damage space exploration.
Starship is very different than their Falcon program. It's a science experiment. Falcons rarely blow up. They get shit to space like the James Webb telescope.
And as far as Elon just wanting more money... sort of.
His personal wealth has not been a huge concern of his for a while. Otherwise he wouldn't have let Tesla fall apart like it has. The wealth he is actually concerned about is not his own. Going to Mars is a trillion-dollar-plus endeavor. Even the richest man in the world cannot raise that much money.
Only a government could fund that.
Elon knows this. He figured it out a while ago. And when he saw an opportunity to get his hands on the government purse strings, he jumped at the chance.
He jumped in the shape of an X like a giant loser.

I'm *positive* Elon thought, "If I could save the government a trillion dollars, they'll give it to me so I can go to Mars."
But it is probably breaking his brain right now after learning he isn't this super genius who can figure out government bureaucracy in a weekend with a bunch of coding dorks.
He got depressed and realized his cool plan to get to Mars was falling apart.

Whoops.
Elon will say anything to get to Mars. He will lie about anything to get to Mars. He will consort with anyone to get to Mars. If you are ever unsure why Elon is doing something, it's to get to Mars. His moral calculus is based on this. In his delusional mind, everything is justifiable to save the human race.
He does have side quests. He wants to repopulate the Earth with his seed. And he uses IVF because you can drastically increase the odds of getting a boy if you pay extra. And he is angry at his trans daughter because he wants boys to continue his mission to spread Musk seed. He spends $50,000 extra to make sure he gets boys and she is messing with the plan.
Oh, and he really really wants people to think he is good at video games. And he wants people to like him. And he wants to kill the woke mind virus because he didn't get the boy he paid for.
But Mars is *almost* all he cares about.
Elon thinks Earth is doomed and he wants immortality from being the man who saved human civilization. He truly believes our existence is dependent on being "multiplanetary." It might be the only thing he believes.
Saving the human race is supposed to be his legacy.
And it is killing us.
359 notes
·
View notes
Note
Could you rate Marina scenes but only.from s7.
Ik it wasnt perfect and kinda rushed but we had so many cute stuff
Sorry for the delay! This took some time and I'm still not sure of my ranking because some of these were tough. We did get some great scenes despite them ultimately doing Marina dirty in Season 7 IMO. A lot of stuff brushed under the rug/put in wordless montages that was really frustrating after waiting so long for certain storylines to wrap up and come to fruition but this is how I would rank them.
This would be my top 5 and then the rest under the cut:
7x04: truth or scared scene. so good. finally got to hear them express their fears to one another. (crazy how they all ended up becoming reality during the season) and then of course the cuddling scene at the end and carina sleeping in maya’s neck like we all knew she did <3 lovely to see and bonus that it was directed by Stefania.
2. 7x05: in maya’s bunk. top tier. everything about this scene is perfect. carina waiting for maya while wearing her sfd clothes. liam there. maya freaking out when she sees carina’s bloody shirt. carina having to tell maya she can’t get pregnant and maya immediately wanting to fix it and suggesting her eggs. maya finally speaking italian to her wife. i’m so glad we got this and in the 100th episode makes it even more meaningful <3
3. 7x10: we’re pregnant. two babies. i love this scene even if i wish we got more of an initial reaction to them finally seeing each other after all the wildfire stress. but the payoff of carina finally getting to tell maya she’s pregnant was beautiful and so special. the spinning kiss parallel to their proposal scene felt meaningful also. they finally had their moment <3
4. 7x09: i’d rather focus on my hot wife. 10/10 great scene. the foreshadowing of this is definitely evil but it's probably the sexiest thing we got of the season and didn't disappoint. Danielle and Stefania truly delivered as they always do when getting the material.
5. 7x01: Hi little Liam. We’d like to be your moms. I love this scene. Maya being the one to suggest adoption, saying they can still have their plans to get pregnant, listing all the reasons it makes sense for them. Carina being so happy and the way Maya looks at her at the end as Carina is looking at Liam and Liam looking up at both of them. I’ll always wish we got more of the beginning stages of Marina bringing Liam home from the hospital/introducing him to the team etc. but this scene was really good. The start of them finally becoming moms <3
Now the rest. I don't know if the 7x09 cliffhanger technically counts because they don't interact in it but I have to shout it out/put it close to the top because it's still so beautifully done and intertwined both of them together in such an amazing way. Just such a shame that they didn't pay it off that well.
6. 7x09: scene in kitchen. mutual i love you’s finally, the ultrasound picture on the fridge, maya wearing the jacket she wore when they first met. another great scene that gave us so many good things.
7. 7x05: FaceTime maya carina liam. super cute. we got probie and babe and maya in her class A’s.
8. 7x08: opening montage scene of ivf process/embryo transfer. loved this scene, glad we got to see some of it on tv for once that just involved the two of them. i think out of all their wordless montage scenes in the season, this is the one that actually made sense to be a montage but some of us were so frustrated with them already having a lot of those scenes already that we wished there was dialogue. but i think it was nice seeing the process being done, the way they were looking at each other with complete heart eyes, maya holding carina’s hand every step of the way and then carina explaining things to maya on the ultrasound photo. and i love that it was the first scene of the episode. and then the transition to them at the clinic and maya being all protective of carina moving heavy things? 10/10
9. 7x07: scene in the beginning with liam is adorable. maya testing carina for her meeting about the lawsuit, maya and liam both crying and carina comforting them both. all it was missing was a kiss of some sort, don’t know why they didn’t add that. also carina calling herself mommy felt wrong
10. 7x04: getting locked out of the house. peak comedy. carina saying she wants to fight. love seeing them bicker like an old married couple lol "i’m married to maya bishop, of course my car is locked"
11. 7x06: at the clinic. maya being all smitten at the idea of carina being pregnant. i’m so glad we at least got this since we never got to see maya around a pregnant carina…we were so robbed of that
12. 7x08: over protective maya about the embryo transfer at the clinic and wanting carina to take it easy…adorable. the little bits we got of her being that way since we didn’t get to see it while carina was actually pregnant but i love that carina also reassures her she’s fine and still capable of doing things.
13. 7x09: in the tent, worried wives and ‘see you at home’ short but sweet
14. 7x09: texting scene. lasagna mention. super cute and bonus carina/liam cuteness
15. 7x06: joe’s bar. annoyed they cut the kiss which was a theme this season but i really liked this scene. maya being a cute yapper while carina amusingly listens to her wife and them talking about mason and their parents and bringing it back to them having their own kids. carina telling maya she’s going to be a good mom…it was just a cute married domestic scene at their place.
16. 7x01: talking about getting house. Carina saying ‘your apartment’ stings even if I get she’s saying it because of the bad memories. seeing Carina with Liam in the beginning and Maya saying she did everything she could to save his bio mom was cute. our house. our home. this scene is cute but the fact that they didn’t just let them kiss properly is annoying and then we got the awkward angle instead.
17. 7x08: in the lounge talking about liam and the bio dad. love how carina leans into maya’s chest and maya kisses the top of her head. wish it wasn’t so quick but it was a nice scene
18. 7x02: Carina getting sued: Maya being supportive of Carina from the jump was cute and the little touches throughout the scene was so them. and Maya basically making sure everything was taken care of and leading the way once they got the call to get Liam? my heart
19. 7x04: discussing attachment parenting and their different styles. i found this scene to be very interesting and to hear maya's POV of why she felt the way she did and it made sense for her stance to be what it was while carina felt the opposite. thought it was nice to hear them talk about it in a healthy way despite them disagreeing.
20. 7x04: the fight in liam’s room. lots of mixed feelings with this scene. i know people think Carina always pushes Maya too hard but i also think she should be able to talk about the tough things with her wife at times. it shouldn’t just be a ‘therapy’ thing when Carina is just trying to figure out where Maya is coming from. it’s also interesting to me how Maya always goes to bring up Carina’s father whenever she gets confronted with something by Carina, i wish that was something that was addressed. i also understand Maya is still working on herself and so getting defensive and walking out is still something she does and i don’t blame her for that. but part of me does wish we would have gotten to see them grow from this as it was already a step in the right direction after the fighting in season 3 (and we all know how maya handled that) but to finally get to see them ‘fight’ and discuss something without Maya walking away.
21. 7x08: marina walking into the engagement party and telling the team about being on track to adopt liam. glad we got this moment and the team being happy for them.
22. 7x02: Marina Clinic Scenes (I’m just grouping them altogether as one since they weren’t technically alone for any of them but still had some moments) love the look Carina gives Maya when she says “That’s what I said” about never having kids. Carina helping Maya with her gown, seeing them work together to figure out the illness the woman had, it was nice seeing them work together in that element like that (though i still think it was a missed opportunity for them to deal with a contagious situation and one of them catching something/worrying about liam but there was already a lot going on plus the suing situation at the end)
23. 7x04: Maya with the drill in the beginning. Carina with liam was adorable but it felt a little forced that Carina just couldn’t get a diaper herself lol
24. 7x07: end scene. having the box hit Maya’s boobs so they can’t kiss? stupid and unnecessary. only good things were the hand holding and amore mio. the double standards between all the couples sex scenes were trash as we’ve all said.
25. 7x10: the flash forwards. idk if these count but they were fine. Maya’s showing them both giving birth was unexpected but i am glad we got the vision of carina giving birth to their baby. Carina’s only showing some weirdly placed photoshoot was underwhelming though.
26. 7x02: bringing Liam to the station…the fact that this was just a wordless montage really upsets me. I think this moment deserved way more. I get that it was Jack’s moment/episode but Marina had been waiting for this for so long and we deserved to see them excited and having the team excited with dialogue that they were finally bringing their baby home with them.
27. 7x03: montage scene(s) - if these even count…I think we all know how ridiculous it was that this it the only content they got in the Pride episode and while it was sweet seeing the three of them in their new home and getting to dance and have their moment as a family…they deserved so much better and so much more.
#asks#anon#carina x maya#station 19#this makes it seem like they had so much in the season lol#but they really kinda didn't 😔 always going to be sad for what we missed out on and lost#thanks to those who asked these it was fun to go through
16 notes
·
View notes
Text
Walter Einenkel at Daily Kos:
Illinois Sen. Tammy Duckworth took Donald Trump to the cleaners during her speech at Tuesday night’s Democratic National Convention. Duckworth, a veteran who lost both legs in the Iraq War, went straight at Donald Trump for nearly five minutes straight.
[...]
“So let me say to every would-be parent: I see you. I'm with you,” Duckworth said. “And together in November, we'll send a message to old cadet bone spurs: Stay out of our doctors offices! And while you're at it, out of the Oval Office too!” The crowd loved that. “My struggle with infertility was more painful than any wound I earned on the battlefield,” Duckworth continued. “So how dare a convicted felon like Donald Trump treat women! Seeking health care like they're the ones breaking the law? How dare JD Vance criticize childless women on cable news, then vote against legislation that would have actually helped Americans to start families? “How dare the GOP endanger the dreams of countless veterans whose combat wounds prevent them from having kids without IVF? Punishing our heroes for their willingness to serve. It's simple, every American deserves the right to be called Mommy or Daddy without being treated like a criminal. Kamala Harris believes that. So let's make some history.”
Illinois Senator Tammy Duckworth delivered a blistering rebuke to Cadet Bone Spurs and gave a robust defense of IVF last night on the DNC stage in Chicago. #DNC2024 #DemConvention
9 notes
·
View notes
Text
Repost from @bristololdvic1766 - Louise Brown, the world’s first IVF baby, popped into rehearsals to visit the cast of #AChildofScience.
Louise (@louisejoybrown), a proud Bristolian, spoke with the cast and shared her excitement for the show in her hometown ahead of its world premiere.
The production tells the incredible story of the creation of IVF by pioneers Patrick Steptoe (played by #JamieGlover), Robert Edwards (played by @t22felton), and Jean Purdy (played by @megkbellamy), along with the brave women who made it possible.
Don’t miss Louise at the Stage Talk on Wed 26 Jun when she will be joined by writer Gareth Farr. Head to our website to book your spot.
📸 @joncraig_photos
📆 5 Jun – 6 Jul
📍 Bristol Old Vic Theatre
🎟️ Tickets from £10 (plus concessions)
#IVF #BristolOldVic #AChildOfScience #WorldPremiere
12 notes
·
View notes
Text
Hey, I just want to talk about the Alabama ruling that frozen embryos are children, and why this shows a distinct lack of science education and why the ruling is bullshit. (and also how the ruling is designed to harm women/"keep women in line.")
Frozen embryos are not children. Blastocysts (the stage at which an embryo is frozen) has about 100 cells and is about 5 days old at the time of freezing. The cells are undifferentiated, which are also called "stem cells." This means that the cells CAN (and if implanted, will differentiate) into the systems that will eventually lead to a full organism. Right now, the blastocyst does not have a heart, lungs, brain, or any other organ. It's alive in the sense that individual cells are alive, but there is no consciousness. It's not human. The cells will rapidly divide, but so do epithelial cells. So do cancer cells. If you wouldn't consider a liver tumor a child, you cannot consider a blastocyst a child.
This ruling is designed to "keep women in line." Currently, anyone with a uterus can have an IVF procedure in order to have a child without having heterosexual sex. Anyone capable can undergo an IVF procedure to be a surrogate for a gay relationship, or a relationship in which neither person can undergo "natural" pregnancy. A single cis woman, or even a trans man, who has no desire to be in a relationship can also undergo IVF to become a single parent. The ruling that blastocysts are children means that clinics will close (because if blastocysts in cold storage die, the clinic then becomes responsible) and these categories of people will no longer be able to have children. This forces heterosexual relationships in which an AFAB woman is beholden (or at least attached) to a cis man to have children.
The only argument being made is solely religious, and solely based on bad interpretation of scripture. The bible says nothing about terminating pregnancy, and the entire abortion debate is about control.
19 notes
·
View notes
Text
How IVF Experts Can Increase Success Rates: Key Factors to Consider
In-vitro fertilization (IVF) has revolutionized the field of reproductive medicine, offering hope to millions of couples struggling with infertility. While the IVF process is highly effective, the success rates can vary based on a number of factors. Fortunately, the expertise of IVF specialists can significantly enhance the chances of a successful pregnancy. In this blog, we’ll explore how IVF experts can increase success rates and provide guidance on optimizing treatment for the best possible outcome.
1. Personalized Treatment Plans
One of the most crucial ways IVF experts can increase success rates is by developing a personalized treatment plan. Every patient’s fertility journey is unique, and a one-size-fits-all approach may not work for everyone. By assessing factors such as age, medical history, hormone levels, and the underlying cause of infertility, IVF specialists can tailor the treatment to meet the specific needs of the patient.
Customized medication protocols: Experts adjust the type, dose, and timing of fertility medications to stimulate egg production in the most effective way.
Individualized embryo selection: With a personalized approach, the best embryos can be selected for transfer, increasing the likelihood of successful implantation.
2. Advanced Diagnostic Tools and Testing
IVF success is often greatly influenced by the accuracy of diagnostic testing. IVF experts use advanced diagnostic tools to assess both male and female fertility. By identifying any underlying issues early on, specialists can recommend the most effective treatment strategies.
Genetic screening: Preimplantation genetic testing (PGT) allows experts to screen embryos for genetic disorders, ensuring only the healthiest embryos are transferred.
Hormonal profiling: Hormonal tests help IVF specialists understand the reproductive health of the patient and identify any imbalances that might impact treatment.
3. Optimizing Egg and Sperm Quality
The quality of the eggs and sperm used in IVF plays a significant role in the success of the treatment. IVF experts can help improve the quality of both through various strategies:
Egg retrieval timing: By carefully timing egg retrieval, specialists ensure that eggs are harvested at the optimal moment for fertilization, increasing the chances of success.
Sperm selection techniques: Advanced sperm selection methods, such as Intracytoplasmic Sperm Injection (ICSI), can be used when sperm quality is a concern, ensuring the best sperm is used for fertilization.
4. Embryo Culture and Monitoring
The embryo culture stage is critical in determining the success of IVF. IVF specialists use advanced technology and expertise to monitor embryo development closely. Embryos are cultured in controlled environments, with temperature and pH levels optimized for growth.
Embryo monitoring: Regular assessments of embryo growth help identify the most viable embryos for transfer. The use of time-lapse imaging and embryo grading ensures that the best embryos are chosen.
Blastocyst culture: Transferring embryos that have reached the blastocyst stage (5–6 days old) often increases success rates. This is because blastocysts are more likely to implant successfully compared to earlier-stage embryos.
5. Embryo Transfer Techniques
The embryo transfer process is a delicate procedure, and expert handling is essential to increase the likelihood of successful implantation. IVF specialists use highly refined techniques to transfer embryos into the uterus with precision.
Catheter selection: IVF specialists use the smallest catheter possible to ensure the embryo is transferred gently and accurately into the uterine lining.
Endometrial preparation: Proper preparation of the uterine lining is crucial for embryo implantation. Experts can optimize endometrial receptivity through medications such as progesterone to create the best environment for the embryo.
6. Attention to Patient Health and Wellness
The overall health of the patient is a critical factor in IVF success. IVF experts emphasize the importance of maintaining a healthy lifestyle to support fertility and increase the chances of a successful pregnancy.
Diet and exercise: IVF specialists may recommend dietary changes and exercise routines to improve fertility health, manage weight, and reduce stress.
Stress management: The emotional and psychological aspects of IVF can affect the success of treatment. Experts often suggest counseling, relaxation techniques, or mindfulness practices to help patients manage stress throughout the IVF process.
7. Use of Cutting-Edge Technologies
Advancements in technology have significantly improved the chances of success in IVF. IVF experts stay updated on the latest techniques and innovations in reproductive medicine to provide the best treatment options available.
Cryopreservation: Freezing embryos and eggs for future use can help increase the chances of success in later IVF cycles.
Stem cell research: Experts are exploring the potential of stem cells to enhance fertility and improve IVF outcomes, although this technology is still in its early stages.
8. Managing Multiple IVF Cycles
For some patients, multiple IVF cycles may be required to achieve pregnancy. IVF specialists know when to make adjustments to the treatment plan after each cycle and can help manage the process effectively.
Cycle monitoring: Regular monitoring of hormone levels, egg quality, and embryo development can guide adjustments in the next cycle to improve outcomes.
Optimizing the next attempt: If the first IVF cycle is unsuccessful, experts review the results to make necessary changes, such as altering medications, improving embryo culture, or using genetic testing.
9. Emotional Support and Counseling
The IVF journey can be emotionally challenging, and IVF experts understand the importance of providing emotional support. Offering counseling services and a strong support system helps patients manage the psychological stress of the process and can improve overall well-being.
Counseling sessions: Many IVF centers provide counseling services to help patients cope with the emotional rollercoaster of IVF.
Support groups: Connecting with other couples going through IVF can provide encouragement and reassurance during the process.
Conclusion
The success of IVF is influenced by various factors, but the expertise of IVF specialists plays a pivotal role in increasing the chances of success. From personalized treatment plans and advanced diagnostic tools to optimizing egg and sperm quality, IVF experts use their knowledge and experience to provide the best possible care for each patient. By staying up to date with the latest advancements in fertility technology and offering emotional support, they help couples navigate the IVF journey with confidence and hope.
Take the First Step Toward Your Parenthood Journey
If you’re considering IVF and want expert guidance, don’t wait any longer. Our experienced IVF specialists are here to provide personalized treatment plans and offer the support you need every step of the way. Schedule a consultation today and let us help you increase your chances of success with the latest advancements in fertility care.
Contact us now to learn more about how we can make your dream of parenthood a reality
2 notes
·
View notes
Text
This is so totally not to do with fallout but I wanted to talk about this personal thing and maybe i dunno? See if anyone can provide advice? Vent??? (under the cut, CW: prescription drug dependency, opiates, ketamine, drug rehab and detox, pregnancy, IVF, infertility, family planning, reproductive health.)
Right so getting personal here but I've hit a point where I cannot afford to put off having kids anymore. I have always, always wanted to be a parent, but I have the triple whammy of PCOS, adenomyosis and endometriosis and my husband and I have been trying to get pregnant since... I've lost track, but it was before we even got married. I'd say we're closing in on around 4 or 5 years now and we've been together for 8 years.
We've been to several fertility specialists and my issue is that I just don't ovulate like I should. Everything else is fine -- thankfully my uterine tissue is fine despite the adeno, and we've surgically got my endo under control, but PCOS means I just don't drop eggs like I'm meant to. (Although, recently, I've like, shed weight thanks to my new ADHD medication which has overcome my insulin resistance and I ovulated last month! So who knows?)
Anyway, all this to say that I'm running out of time now and we're going to start the IVF process next year. Thankfully my odds are extremely good and (touch wood) we're likely to get lucky quickly. IVF is invasive and expensive and I am terrified but I figure I'm gonna go through birth eventually, right? May as well get scared early and get used to it. (When I say IVF is invasive I mean we went through a cycle once before and it was so traumatising to me despite everything going fine that it inspired me to write Embryology, which is a body-horror fic lmao.)
However,
These medical conditions also cause me a lot of pain. Like, a lot, chronically. I have been in pain since I was 12 and started getting periods and I've been on opiates (legally and under medical supervision) for well, well over a decade. They're awesome, they have improved my quality of life drastically. I'm able to walk my dog, go to the grocery store, hold down a job and go to the gym every second day -- which I couldn't without them.
I don't abuse my opiates. I see my doctor once a month and see a pain management specialist annually to evaluate my pain and the best way to treat it and how I'm going, which is required before you can get the kind of prescription I have in my country (this is also overseen by the government, who provide my doctor with a permit after assessments that allow them to prescribe me) I have never had a dose increase and they're totally happy with my use. I am 100% aware that opiates are scary and dangerous and cause a lot of heartache for people but I assure you that in my case it is responsibly managed and safe.
The issue, though, is that I'm getting pregnant (hopefully) next year. This means that before I undergo my first IVF cycle, I have to go off opiates. Psychologically, I'm fine with this. I want a baby more than I want opiates, and thankfully, it's almost guaranteed that pregnancy will actually stop my pain as endo and adeno pain has, as we've seen in studies, always responded well to pregnancy for the duration of it.
But physically? I have an opiate dependency. This is the physical response to withdrawal of a drug, and it happens with any drug. (There's a lot of things that your body with develop a chemical reliance on in some way that aren't drugs, too!) It's nothing to be ashamed of and I'm not ashamed of it at all.
There's no way around it, even if I am not psychologically dependant on opiates and have no history of abuse or misuse, my body is a different story and I am going to have to go through a detox stage. In a lot of parts of the world including the western world, this is done through a weening process or by swapping whatever opiate a person is using to a more controlled substance like Suboxone (which I am avoiding) and then weening off the 'safer,' controlled, replacement opiate instead.
This would suck. If you've never had opiate withdrawls, imagine you have the worst flu ever -- no cough or fever, but you feel like you have a fever. You get a runny nose and sore throat, you get congested, your eyes start to burn, your skin starts to sting, your joints hurt. You sweat through your clothes and sheets at night and during the day you feel like you have a fever even if you don't have one. Oh, and the shitting. You don't stop shitting. It starts as run of the mill diahhoreah and then turns into water. You eat, get debilitating stomach and digestive tract pain as the food works its way through you and then it comes out two hours later as water. It's never ending. You shit oil after a while. If you didn't have TMJ beforehand, withdrawals will give you TMJ. Your teeth will hurt and, to top it off, opiate withdrawals cause insomnia. Even once you pass out from exhaustion from shitting for 8 hours straight, you will wake up every five minutes and go into a cycle of 'wake up,' 'stay awake for give minutes,' 'pass out from exhaustion again,' 'wake up five minutes later.' You cannot sit still. It is pure agony.
This would take months. I would be physically unwell the whole time, being that sick for that long would probably fuck with my mental health, and even once it's out of my system -- a lot of the time, your brain matter never forgets opiates. You can be fine for years and then see something and your neurons will involuntarily fire off and your opioid receptors will start SCREAMING for opiates.
However, I'm really, extremely lucky and ketamine treatment is being offered in my country for detox and rehabilitation from opiates!
This means that instead of the agonizing weening process that can take months and even years in cases worse than mine, I spend a week in hospital under medical supervision with a constant drip of ketamine until I've fully detoxed. Ketamine is actually a really incredible drug when it comes to medical uses (I already have a prescription for something called a troche, which is a microdose that you dissolve in your mouth. I use it for when I have a cyst burst and need immediate pain relief while my other medication kicks in.) It's not just used as an analgesic or anaesthetic anymore and you've probably read about it being used to treat PTSD or treatment resistant depression. (I can definitely attest that my mood as someone with bipolar disorder and PTSD has been the most stable it's ever been since starting to use it, which is a side bonus.)
There's a lot of studies and evidence that ketamine actually re-sets or re-wires your brain's pathways, which is why opioid infusions are used for chronic neuropathic pain a lot. The idea is that a long and low dose of ketamine is delivered with a pump at regular intervals around the clock so you basically spend a full week or so having your brain's pathways re-programmed and your opiate receptors renovated.
This means that I'll both be made comfortable during withdrawal (ketamine is shown to lessen the neuropathic and painful withdrawal symptoms, but as I'm in a hospital with nurses who are specifically trained to handle withdrawal cases, I'll also be given supporting medication for the diarrhea, restlessness etc) but it'll give my brain somewhat of a clean slate, meaning I should (fingers crossed) be able to live the rest of my life without feeling random cravings.
The biggest benefit to this is that it should re-wire my brain's pain pathways (which are worn the fuck out from feeling pain for decades -- think of it like having an ass groove in a couch and picking up the cushion and beating the shit out of it until the groove is gone,) meaning that my body may feel my usual pain as lesser and that regular pain medication like ibuprofen or tylenol (panadol for us Australians) will have a far better chance of working as well on my brain as opiates do, just without the buzz.
So it's a slam dunk win and I'm absolutely taking it, but a week on ketamine is still scary. During infusions, they start you on a microdose and then work your dosage up until they work out what your limit is before you venture into a k-hole and then reduce it to the highest level they can give you without sending you to space, but it's still going to be enough that I will experience some psychedelic effects and hallucinations.
I'll be safe and cared for but given that I do have some trauma I'm a little frightened. My specialist has warned me that it might bring that up in ways I won't expect and I might get a bit distressed at times and even feel a little mentally freaked out -- which is all normal because I'm on fucking ketamine duh -- but that's still a terrifying prospect, to have to do that for an entire week.
My long term plan is that once I have this baby, I'm getting a hysterectomy as we're pretty confident that most of my pain comes from my adenomyosis, which should make it manageable afterwards, even without opiates. I have something of a light at the end of the tunnel and it's, hopefully opiate free, and that sounds nice. Not that I have a problem with opiates -- honestly, if I could stay on them forever I would because they let me live a life and I love that peace of mind knowing it's there if I get hit with debilitating pain again. But the stigma and judgement around it and the way unfamiliar doctors and nurses treat me when they find out I take opiates (even with a prescription and all that supervision and all those safety checks!) is just awful, and the way people choose to see me because of legal medication I take -- I'm refused treatment for unrelated things so often because doctors see that on my medication list and assume I'm drug seeking. HUGE CN HERE for pregnancy loss - I miscarried in a hospital waiting room once after waiting in there for 6 hours without being seen because the triage nurse decided that I was trying to get more opiates and didn't even put my details in the system, meaning that no one was ever going to come see me anyway! I want to get off them and be free of that judgement and be treated like a human being again!
But I dunno. I guess I'm just scared that I'm gonna go through like, a trauma trip for a week and then just wind up back on opiates in two years and have to keep living a life where I'm treated as less deserving of respect or dignity because of something that's just... well, it's wrong to treat people like that, even if they do abuse their medication or use street opiates, anyway. The medical system is just callous and cruel.
Anyway, the reading I've done suggests bringing comforting things to do or watch during your stay, and I know I'm looking 12 months ahead (which is the plan at the moment) but I'm trying to figure out what that is in case I want to save for something like a new laptop or even a steam deck to play comfort games (simple stuff like stardew valley, easy, calm things) and watch easy viewing stuff?? idk. This is weird.
3 notes
·
View notes
Note
HC’s of how your LIs would react to finding out she’s pregnant? For the girls let’s say they’ve been trying for ages through IVF/donors.
LOVE LOVE LOVEEEE
thanks for the question!! from your ask I gathered you mean MC and LI have been trying to have a baby, right?!
with that in mind, I'll be doing my favourite LIs that I think would love to have a child 💕 if you have any specific LI in mind, pls send me an ask.
as always, please look under the cut 👇
☆ SEASON 1
JAKE
when you finally get that positive result you're not only overflowing with happiness but also are planning to make a special announcement for daddy. there's tiny little baby shoes in a surprise box, there's cameras recording and there's MOST DEFINITELY tears. Jake can't contain his happiness and he's crying as soon as he spots the tiny shoes. then, he's swirling you around. it's just a very very happy moment.
TIM
when he sees the test and looks at you searching for confirmation — because let's face it, Tim doesn't know how a pregnancy test works — he is screaming and kissing you. also, he IMMEDIATELY calls his mom to share the news. maybe even facetiming her while he cries like a baby. he's the happiest man in the world and is already thinking of names.
TALIA
I'm a little torn between whether or not she wants to have children and I don't have any recollection if that's talked about during S1 but I'm doing it anyway.
she just can't believe it. she looks at you, then she looks at the test and then she looks at you again in complete shock. not too long after, she's crying and hugging you and just keeping you close. it's been a long time coming and she's just so, so, happy. the moment isn't loud, it's intimate. just between the two of you.
☆ SEASON 2
BOBBY
oh, man. I believe Bobby is a very family centred guy, that's why the perfect announcement would be when your families are reunited. picture the whole fam in the living room! you get up, everyone is paying attention and you announce it. Bobby gasps, then grabs you, then twirls you and then gets all worried because can he do that if you're pregnant? you're laughing all the time, even when he starts crying. the fam is looking at you guys adoringly and I can see a lot of pictures being taken (and a lot of questions being asked as well)
NOAH
you sit Noah down on the bed, grabs his hands and tells him the news. the big smile on his face and the twinkle in his eyes leave you with no doubt: he IS the one. he waste no time on touching your belly and kissing you tenderly. the moment is simple but it's also private, intimate and very special. it gets you so emotional that you can't help but cry and he also sheds a tear.
☆ SEASON 3
AJ
she's immediately jumping around, hugging you, screaming, kissing you. it's a big party as soon as she hears the word 'pregnant', there's no need to see the test. she's calling everyone, the news are spreading like wildfire and you don't even try to stop her because you don't remember ever seeing AJ that happy. the same night, she's following every baby related profile she can find.
NICKY
this man is on his knees kissing your belly from the moment you show him the test. of course, he still wants to be 100% sure and take a blood test, but when I say he is absolutely BEYOND HAPPY when he sees the lines. talks directly to the baby about how he just can't wait to see them 💕
☆ SEASON 4
BRUNO
DEAR GOD. this man will go through every stage of happiness in 5 seconds. he'll be sooooo shocked at first, asking you a BILLION times if you're sure. once you confirm to him that YES you're fucking sure, he will then cry, hug you, kiss you, repeat his wedding vows, call his mama, talk to the baby, then proceed to act like you're 8 months pregnant even though you're barely a month. already thinking of a bunch of dad jokes.
YOUCEF
I really think Youcef would be soooooo emotional. he's crying in a way you've never seen him cry before and suddenly the feeling of his touch is way more soft and tender. It's a vere honest moment between you, and he demonstrates soooo much love. I really think that being a dad is a major thing for him and he couldn't be happier to share this moment with you.
📌 headcanons masterlist.
24 notes
·
View notes
Text
Faith, Hope, Love
16th August 2023
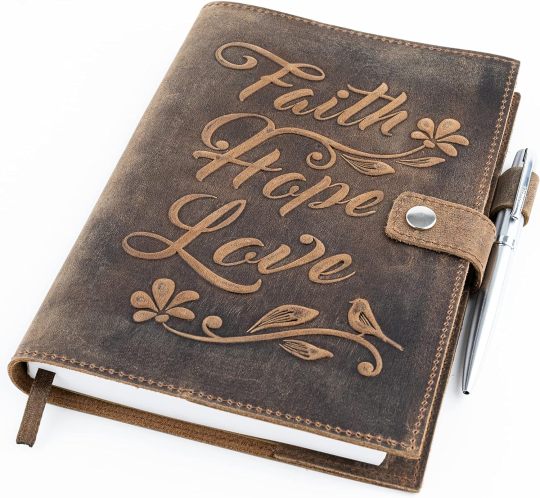
I bought this new leather-bound refillable notebook for my new job when I started working with the Scottish Bible Society in June. Never did I think how much I would look at the three simple words on its cover and for it to be a daily reminder of God’s grace – the need to be reminded of his ultimate control over our world.
Faith – I have plenty of that.
Hope – I can find plenty of that too.
Love – I definitely have plenty of that, receiving it and giving it.
We have finally navigated through all of the bureaucracy associated with the pre-IVF process, where you haven’t quite started but you technically have and still don’t know what’s ahead of you.
I have written previously about my ups and downs relating to this process. I may have even mentioned my religion in relation to my anxiety about even starting this process. Well, we are well passed that stage now. We were referred, we waited, we have been tested and further tested, waited, and waited some more and now we have consented and have been given our start month – September. Now, all that means is that with the start of my September period, I go in for a scan on Day 3 to see if my body will allow them to start intervening on my behalf. In other words, checking to see that I don’t have any unwanted cysts lying around anywhere, that my endometrial layer is thick enough and that I am healthy enough to start pumping myself full of chemicals to get my ovaries working in full-blown Hulk mode 💚 It also means we will then be signing a child welfare form which is basically a contract between us and the HFEA to check/agree that we will be suitable parents. Kevin will have to be formally identified as "himself", in person, so that they can go ahead to use his fresh or frozen swimmers to be combined with whatever eggs they harvest out of me weeks later. I will also be taught how to self-inject subcutaneously for up to 10-12 days – oh the joys! I certainly can’t wait for that fun! They will also test me for blood-borne viruses.
So, what I meant by all of that was, we’ve been given a start month but that still doesn’t guarantee anything. It’s a bit like when Kevin is due home on crew change day. It is never certain that he will definitely be making his way home that day, until he’s physically off the ship and on dry land. Until that moment, absolutely anything can happen, and it has in the past. So, until that Day 3 appointment when all papers are signed and my body is given the all-clear to start being manipulated, your guess is as good as mine as to what the preceding month will look like 😉 However, I do now have a clearer picture of what it POTENTIALLY might look like. I am on a short (antagonist) protocol as I have a 5% risk of developing OHSS.
Day 1 – First day of period
Day 3 – Baseline scan & Ovaleap injections start (Follicle Stimulating Hormone)
Day 8 – Ganirelex injections start (ovarian down regulation)
Day 10 – Follicle scan to determine size of follicles – looking to find 3 follicles or more that are 17mm in size. If not, I continue hormone injection protocol and have a repeat scan in another 2 days’ time. Repeat scan every 2 days until follicles have grown enough.
From here on in, everything is dependent on how I am responding to the hormones to determine the next steps. Basically you can only go from one appointment to the next.
So, essentially from Day 10, you take each day as it comes.
Once I take the trigger injection (for eggs to reach final level of maturity), egg retrieval happens 36hrs later. So this could be as early as Day 12 or Day 14, basically around the usual time you’d expect to ovulate. So my plan is to be down at my Mum’s in Edinburgh from Day 10 of my cycle onwards as its from then when I’m either going to be back & forth to Dundee for scans every couple of days or preparing for egg collection straight away, depending on how I respond to the hormones. It’s worth noting here that the number of follicles growing does not equal the number of eggs collected. Sometimes there are no eggs within the follicles, sometimes there are several. IT IS SO MUCH TO TAKE IN! Pardon me if I repeat myself several times but I’m using this writing opportunity to process all that I have been told over the phone, over video consults and written down in letters, gathering together all the info to make it clear and concise for me to understand – you’d be surprised how unclear the whole process actually is! You have to figure out their wording for everything. I’ve been so “caught out” by expressions in the past. Like reading “Day 5 of Gonadotrophin injections” and working out that that means Day 8 of your cycle (because you start the injections on Day 3) and that having scans on Day 8 and Day 10 of your Ovarian stimulation (stims) means Day 10 and Day 12 of your cycle – one can see how it can all be confusing and that the way they measure everything is a new language to us. I perhaps need to get on board with their way of measuring, and I’m sure I will, but for now, my way to understand it is to compare it to my usual way of measuring my cycle, from Day 1 of my first bleed, as I’m used to.
It’s nothing I’m going to worry about though. I have been doing that and have had some very dark days about it all (ones where, if anyone had been around, they’d have been quite literally picking me up off the floor to hold me in the messy state I was in). Those days are, for the moment, being kept in check. We’ve been given a treatment diary where every important date will be filled in as we go along but knowing ahead of time that there’s a high probability of back & forth every couple of days from Day 10 onwards goes a long way to help us plan that I need to leave the island around Day 9 and expect not to be returning for a fortnight at least.
Initially, after my AMH test found I had a high egg reserve, I was told in an early document to expect a frozen transfer, that a fresh transfer would be unlikely as my body would be overloaded and needing a rest, so in my head I was only considering the time required to get from the baseline scan to egg collection. Beyond that would’ve been a couple months later when my body was then ready for an embryo transfer. However, I now know from my consultant that there’s only a 5% risk of OHSS and therefore I need to be preparing for a FRESH embryo transfer as standard, so that means that I need to account for another 5-day waiting window after the egg collection day to expect to be back in for a fresh transfer under sedation, possibly as soon as Day 17 onwards and then allow a number of days rest afterwards. But, if my ovaries become swollen to 8-9cm or blood estroegan is high or I’m symptomatic or collection retrieves more then 25 eggs – all eggs will be frozen. So, in theory the whole process could be as short as 3wks or up to 4wks long and this is the window that I am working to when I am working out whether or not it is advisable to go ahead to start in September, in the month leading up to the biggest week of the Gaelic calendar – the Royal National Mòd 😂
We started trying when we were 29 & I’m now about to turn 36. Time is not on our side, only God is in control of that, but time is not to be wasted as we only have 4 years left before our NHS funding and our own personal clock runs out – once we turn 40, we’ve agreed to let it all go and live our life in the fate that God has given us. Until then, we’re prepared to fight with all the energy we are blessed with.
We’re of course focusing on doing everything we can to help, but more importantly we’re focusing on our relationship & being us in a broken world where we are forced down this rabbit hole in search of the family we so desperately want. I lost myself in the past 7yrs and I will never get those moments back again. They haven’t been wasted, no. I found meaning in the pandemic where I finally got the chance to focus on my health. We’ve been back & forth with ideas of adoption, fostering and facing a child-less life.
I’ve realised that for 12yrs since being told I may never have children, it’s ruled my life. All I ever wanted was to be a mum. I always talked about being a mum & having my own children, as many would at a young age, never possibly thinking that it might not be an option. To me, the innocent version of me, not being a mum wasn’t an option and to some extent I must regain that level of Faith & Hope. How I wish I could erase the information that I know and be that innocent girl who believes wholeheartedly that she WILL be a mum. No ifs, just no question about it. But above it all, above the waiting, the hoping, the letting go and letting God take over, or as I now have to think about it in some respects, letting the scientists take over (all the while praying that God’s will works within them to the best of their ability, whether they’re God-fearing or not – this is something I am requesting people to pray for - for the staff who’s care we will be under, who’s mortal hands will be guided by Him, to carry out his will) above all of that, is Love. Love that no matter what happens, is ever present and unconditional between us. We have spent years fighting our case, pleading our cause, kicking ourselves, being at our lowest and reaching the height and the depths we never thought we’d reach. But still, we love each other, no matter what, with or without a child. We used to dream of a house filled with children’s laughter but now, and we have not downgraded our dream, we dream only of 2 little lines on a pregnancy test. That is the step 1 we dream about. To us, that would be a dream come true, even just to get to that step. If I’ve learnt nothing from my health journey, of trying to regulate my menstrual cycles and get my weight down, it’s that yes you must have a long-term ultimate goal BUT in order to get there, you must have the tiny, achievable goals. We are well aware that my PCOS makes me 40% more likely to miscarry so we are fully aware that a positive pregnancy test does not equal a baby, or as the ACU unit call it, a live birth. Our NHS funding lasts until there is a “live birth”. As morbid as it sounds, that could even mean a baby born that dies of complications only hours after birth, complications which are even higher because of it being an IVF pregnancy. But to get back to the point, we pray for each tiny milestone along the way. At each and every stage, complications can arise but we can use them as a stepping stone to be grateful for.
Day 3 scan – get green light to start.
Hormone injections (stims) – at home in Lewis hopefully.
Day 8 & Day 10 of stims scans.
Trigger injection – at Mum’s in Edinburgh
Egg collection - under sedation & recovery period
Fertilisation - 70% success rate is normal expectation.
Blastocyst stage (125 cell-stage fertilised egg)
Best quality blastocyst identified for fresh transfer & any remaining good quality embryos sent into cryopreservation.
Embryo transfer - under sedation & recovery period
Pregnancy test - either it is a positive test, and we pray for the next stage for a viable pregnancy to continue (scan 2-3wks after test) or we’re back to square one again…..
Possible complications of each stage:
Headaches
Mood changes
Hot flushes
Night sweats
Nausea
Tiredness
Allergic reactions
Localised tenderness or injection site reactions
Weight gain
Abdominal pain
Diarrhoea
Breast tenderness
Ovarian cyst formation
Vaginal spotting
Vaginal irritation
Skin rashes
Shortness of breath
Risk of reduced response to drugs – cycle abandoned.
Risk of no eggs being collected – cycle abandoned.
Negative pregnancy test – move on to frozen transfers (if embryos are available) or next cycle.
Just remember, while this is an exciting prospect to finally be starting, the process itself is not exciting and there are no guarantees about a positive outcome, in fact, we have been given the stats of a 25% chance of success. While many people remind me, in a positive way, that 25% is still a good chance, try to think of it from the other way around as if you were dealing with the risk factors of agreeing to a surgery. If you were being told you only had a 25% chance of surviving that surgery, would you feel just as excited? Of course you’d hold on to the hope of that chance but you’d put your affairs in order because experience tells you that the number 75 is much bigger than 25 🤷🏻♀️
Being open, honest, raw & just plain & simply Me is the only way I know how to navigate this cruel journey. Kevin and I are very grateful for your support and understanding as we delve into a new world of anxiety & hormonal mood swings where he may fear for his life 😂😂😂😂😂
Faith, Hope & Love are important elements in this rollercoaster ride we’re on. Please pray that our Faith is deepened by progressing with treatment. Please pray that the Hope we have now remains strong throughout and doesn’t falter. Please also pray that the Love we have for each other develops our bond as a couple; supports us as we fall and need help; guides us to deal with each situation as we face it, wraps us up in everlasting trust and most of all, Love the God who is putting us through this pain.
Only he knows why we are going through this.
Only he knows how to get us safely to the other side.
Only he has the power to grant us a miracle, in his name, Amen.
3 notes
·
View notes
Text
Is Your Body Sending You Signals? 7 Signs Your Hormones May Be Out of Balance
Is Your Body Sending You Signals? 7 Signs Your Hormones May Be Out of Balance
Hormones may be tiny messengers in your body, but their role is anything but small. From regulating your mood and metabolism to managing your reproductive health and sleep patterns, hormones are essential to your overall well-being. When they’re in balance, you feel energized, emotionally stable, and healthy. But when they’re out of sync—even slightly—your body can react in ways you might not expect.
At Srishti Hospital and IVF Centre, we specialize in identifying and treating hormonal imbalances that affect women at every life stage. If you've been feeling "off" lately, your hormones might be trying to tell you something.
7 Common Signs of Hormonal Imbalance
Here are seven symptoms that may indicate your hormones are not functioning as they should:
1. Irregular Periods
Changes in your menstrual cycle—like missed periods, spotting, or unusually heavy flows—are often one of the first indicators of a hormonal imbalance.
2. Mood Swings and Anxiety
Feeling more emotional, irritable, or anxious than usual? Fluctuations in estrogen, progesterone, and cortisol levels can impact your mood and mental well-being.
3. Unexplained Weight Gain or Loss
If your weight changes significantly without a change in diet or exercise, it could be due to hormonal shifts affecting metabolism or fat storage.
4. Fatigue
Persistent tiredness, even after a full night’s sleep, may be a sign of low thyroid function or adrenal fatigue.
5. Skin and Hair Changes
Hormonal imbalances can trigger acne, dryness, and even sudden hair thinning or loss.
6. Sleep Disruptions
Trouble falling asleep or staying asleep may be linked to imbalanced melatonin or elevated nighttime cortisol.
7. Low Libido
A reduced interest in sex or vaginal dryness could be caused by declining estrogen or testosterone levels.
7 Common Signs Your Hormones Might Be Out of Balance
Hormones are the body’s chemical messengers—tiny yet powerful substances that control everything from your energy levels and sleep to your mood, metabolism, and reproductive health. When your hormones are in balance, your body functions like a well-oiled machine. But when they’re not, even small imbalances can throw off your physical and emotional well-being.
At Srishti Hospital and IVF Centre, we understand how crucial hormonal balance is, especially for women at every life stage. Let’s explore the common signs of hormonal imbalance, what causes hormonal imbalance, and how to cure hormonal imbalance in females naturally and medically.
What Causes Hormonal Imbalance?
Several internal and external factors may lead to hormonal disturbances, including:
Chronic stress
Poor diet and nutritional deficiencies
Thyroid disorders
PCOS (Polycystic Ovary Syndrome)
Pregnancy and menopause
Sedentary lifestyle
Exposure to endocrine disruptors in food or the environment
How to Restore Hormonal Balance
Whether you're seeking natural remedies or medical treatments, the right strategy depends on identifying the root cause. Here are some general approaches to balance your hormones:
✔ Eat a Hormone-Friendly Diet
Focus on whole foods, healthy fats, lean proteins, and leafy greens. Avoid processed items and excess sugar.
✔ Manage Stress
Incorporate yoga, meditation, or deep breathing into your daily routine.
✔ Stay Active
Regular physical activity—especially strength training and cardio—can support hormone regulation.
✔ Sleep Smart
Quality sleep is vital for hormone production and repair. Aim for 7–9 hours each night.
✔ Consider Supplements
Nutrients like magnesium, vitamin D, and omega-3s may help, but always consult a healthcare provider first.
✔ Seek Medical Treatment
In some cases, hormone therapy or medication may be necessary and should be prescribed under medical supervision.
Take the Hormone Health Quiz
Not sure if your symptoms are hormone-related? Ask yourself:
Do you feel constantly tired despite adequate sleep?
Are your periods irregular or more painful?
Do you frequently experience mood swings or anxiety?
Have you noticed weight fluctuations or skin issues?
If you answered “Yes” to two or more, it might be time to consult a specialist.
Trust Your Body, Take Action
Hormones are powerful—and when they’re out of balance, your body feels the impact. Whether you’re going through puberty, trying to conceive, or navigating menopause, maintaining hormonal health is essential to feeling your best.
At Srishti Hospital and IVF Centre, we offer compassionate, personalized care to help women achieve hormonal harmony. Don’t ignore the signs—your well-being is worth it.
📞 Ready to regain control of your health? Book your hormone consultation with Srishti Hospital and IVF Centre today.
Let me know if you'd like a version optimized for Instagram captions, email marketing, or print brochures as well!
0 notes
Text
How Many Injections For IVF Treatment In India

Originally Posted on:-https://worldfertilityservices.com/blog/injections-for-ivf-treatment-in-india/
Alert from everything whenever infertility couples or individuals is necessary in India. As a reputed IVF Hospital, its doctors or specialists are responsible for guiding you about medical circumstances such as how many injections are required for IVF treatment in India. Albeit, IVF consisting several stages each requiring medications, and injections. Now, take a survey of the whole article in which we have been discussing how Indian IVF hospitals are performed meantime of IVF treatment.
In India, an IVF cycle typically consists of 20 to 40 shots. The precise amount will be determined by the patient’s unique needs, the particular treatment plan, and how they react to the stimulation regimen. Fertility professionals offer direction and support throughout the procedure to guarantee the greatest possible outcome, even though the frequency of injections can make the process daunting.
Does IVF Treatment Require Daily Injections? – Shots Of Injection In A Day
Indeed, daily injections are usually necessary for IVF (In Vitro Fertilization) treatment, especially during the luteal and ovarian stimulation phases. Daily injections are used to stimulate the ovaries to generate many eggs rather than the single egg normally produced in a natural cycle during the ovarian stimulation phase, the first stage of the IVF cycle.
These injections, which are given every day for eight to fourteen days, often comprise FSH (follicle-stimulating hormone) or HMG (human menopausal gonadotropin). To enhance the quantity of eggs that may be extracted for fertilization, these injections are intended to stimulate the ovaries.
Stimulation of the Ovaries (FSH and/or HMG)
Duration: At the beginning of the IVF cycle, typically 8–14 days.
The hormones in these injections, such as human menopausal gonadotropin (HMG) and follicle-stimulating hormone (FSH), encourage the ovaries to generate more eggs.
Frequency: During this stage, it is usually given every day.
Antagonists or Agonists of GnRH
Duration: During the ovarian stimulation period, usually 5–10 days.
The goal of these drugs, which include GnRH agonists like Buserelin and GnRH antagonists like Cetrorelix, is to stop early ovulation.
Depending on the particular medicine being taken, they are often injected either daily or every other day.
Injections of Progesterone
Duration: Progesterone injections are usually administered for 10–14 days following the embryo transfer, or until the results of a pregnancy test are confirmed.
Progesterone serves the dual purpose of promoting early pregnancy in the event of conception and preparing the uterine lining for implantation.
Frequency: These injections are typically administered subcutaneously or intramuscularly once a day.
Injection of Trigger Shot (HCG)
Frequency: This is not a daily injection; it is usually administered 34–36 hours before egg retrieval.
Now, in the upper case of paragraphs, we have shared all the steps that will assist you in understanding how many rounds are there, and how many injections are taken during IVF treatment.
What Happens If You Stop IVF Injections During Treatment? – IVF Injections For Conception
If you think stopping injections during IVF treatment can have critical consequences, as these medications such as injections play a crucial role in making IVF treatment successful in India whether IVF occurs in private or government hospitals.
Every injection type used in IVF has a distinct function, and stopping them too soon might have a detrimental effect on the procedure or possibly result in the cycle failing. If you discontinue IVF injections at any point during treatment, the following outcomes may occur.
How Many Rounds Of IVF Is Normal? – IVF Cycles Of IVF Treatment
Injections For IVF Treatment In India
Especially, the main three rounds are present in IVF treatment in India, Numerous factors, including age, health, the cause of infertility, the quality of eggs and sperm, and how well the body reacts to the treatment, can affect how many IVF (In Vitro Fertilization) cycles a person may require. While some couples may require more IVF cycles, many couples consider 1 to 3 rounds to be typical for a successful pregnancy. If your infertility issues are bigger than, your thoughts, then it may take longer to get conceived in the first cycle.
What Are The Possible Alternatives To Injections In IVF Treatment? – Alternatives Of Injections In IVF Treatment
Altruistic posibility may be an alternative to injections in IVF treatment, but it could be dangerous for infertility partner who suffers from their sterile issues. In contrast, injections are a cornerstone of In Vitro Fertilization treatment due to their role in ovarian stimulation, hormone regulation, embryo implantation support, and maintaining reproductive balance in the body.
However, it is necessary to ensure that these alternatives are no longer used as universally applicable. In some cases, often it depends on the patient’s health, and daily lifestyle, for instance, health, fertility issues, and if your IVF specialists prefer to take IVF injection alternatives.
Is There Any Side Effects Of Injections In IVF Treatment? – Drawbacks Of Injection Stimulation
Of course, if we intake anything in a huge amount, then it feels like an overdose. As usual, injections also left an engram on a patient or its inner body. Furthermore, in the afore section are the potential side effects associated with kinds of IVF injections.
Through injections meantime IVF treatment, then it looks or feels like soreness and bruising from the sake of injections.
Mood Swings normally happen due to many causes in a woman, but if it shows by injection treatment.
Allergic reactions mean the heavy dose of injections may be a reason for any type of allergic reaction in the body.
Pain in internal organs or lower body parts is known as pelvic or abdominal to a woman during impregnation after childbirth.
These are the main reasons that every parent can feel or see the changes during IVF treatment. Often, all the keys depend on the patient’s health or inner body power.
Final Verdict – Injections For IVF Treatment
Whenever we reach the article, then we make sure all the headings or points have been covered or not. The conclusion is a medium to express the right answer in the short term. In this article, we discussed how many injections for IVF treatment in India. If you’re a blogger, and interested in reading more articles, then search World Fertility Services official website to get new or latest articles.
0 notes
Text
Best IVF Specialist In India
IHR Kolkata, a well-respected fertility clinic in Kolkata, offers a wide range of fertility treatments including best ivf centre in india. In vitro fertilization (IVF), one of the world’s premier assisted reproductive technologies, offers couples suffering from infertility an effective solution. In the IVF procedure, the eggs from the ovaries of the woman are taken and fertilized in a lab dish with sperm. The embryos that are created will then be transferred into the uterus of the woman in order to achieve a successful pregnancy. IHR Kolkata offers IVF treatments by highly experienced doctors and embryologists who collaborate to offer customized care and assistance to couples undergoing IVF in Kolkata. With the help of IVF, couples experiencing infertility have an opportunity to conceive and begin building their family.
IVF treatment in Kolkata��involves multiple stages such as ovarian stimulator, egg retrieval and fertilization, culture of embryos, and transfer. Our fertility specialists closely monitor every step of the process to create a customized treatment plan to meet the needs of each patient and enhance their chances of success.
When is IVF Treatment Recommended?
IVF treatment should generally be considered by women under 43 who have tried for two years to conceive with unprotected sexual relations without success. These treatments can help treat infertility caused by blocked fallopian tubes, genetic issues or male infertility factors. In some cases, less invasive procedures such as fertility drugs or intrauterine insemination may be tried first. However, IVF treatment in Kolkata may be recommended to women in their mid-30s when other options have failed or when other health conditions such as fallopian tube damage, ovulation disorders, endometriosis, uterine fibroids, previous tubal sterilization or removal, impaired sperm function, unexplained infertility, genetic disorders, or for fertility preservation due to cancer or other health conditions. Therefore it is wise to discuss all available treatments with a fertility specialist prior to embarking upon IVF therapy treatment plan In Kolkata. It is important to discuss all available options with a fertility specialist to determine the best course of IVF treatment In Kolkata.
Why Choose IHR India For IVF treatment in Kolkata?
At IHR Kolkata, we offer the best ivf specialist in india, providing couples struggling with infertility the opportunity to achieve their dream of having a child. We use advanced medical technologies and modern infrastructure to offer personalized treatment plans tailored to the unique needs of each patient. Our team of experienced and caring medical staff works closely with patients at every step, providing support and guidance throughout their fertility journey. With a high success rate of 70%, we are a leading choice for both domestic and international patients that are seeking for ivf specialist in kolkata. We are committed to making superior infertility treatments that are affordable and accessible to a larger population, helping more couples fulfill their dream of parenthood.
Our team of experts, fertility breakthrough results and a 70% success rate made us a unique option for desired couples. We are trying our best to make superior infertility treatments inexpensive to a larger population.
Reasons To Choose Us:
1. We are passionate about helping infertile couples with our definite solutions.
2. All our methods are well-tested and tried.
3. We always focus on reducing the mental and physical stress of our patient so that they go successfully in their IVF treatment.
4. Our medical staff is supportive and help you in every step of your IVF fertility journey.
5. We deliver supreme services for male and female infertility that results in better outcomes for both mothers and babies.
Do you have difficulty conceiving a child? Couples who have failed to conceive using other methods often consider IVF treatment in Kolkata. Here are some reasons why couples consider IVF treatment:
1. Tubal Factor: When the fallopian tubes become blocked or damaged, IVF may be the only viable way to achieve pregnancy. Since the fallopian tubes connect ovaries to womb, and an egg cannot travel down them without impediments, pregnancy cannot occur naturally.
2. Male Infertility: It is a common reason for infertility in couples. If the male partner has low sperm count or abnormalities that hinder fertilization of the egg, IVF with ICSI is frequently recommended for a successful pregnancy and biological baby.
3. Age-related Infertility: As women age, their ovarian function decreases and they may find it increasingly difficult to get pregnant. Some women’s ovarian function decreases earlier, making it necessary to consider IVF treatment sooner.
4. PCOS: Patients living with Polycystic Ovary Syndrome (PCOS) frequently have difficulty becoming pregnant. IVF treatment may be beneficial and help lower some risk factors.
5. Undetermined Infertility: Approximately 20% of couples experience unexplained infertility, without any identifiable reason. IVF treatment has proven to be successful in such cases.
6. Genetic Disease: Couples suffering from genetic disorders who experience repeated miscarriages should consider IVF treatment as the only option for a successful pregnancy.
0 notes
Text
The Emotional Impact of IVF: Coping Strategies for Couples
Introduction
In vitro fertilization (IVF) has brought hope to millions of couples facing infertility. While the advancements in medical science and the availability of top clinics like the Best IVF Centre in Delhi have made it possible to achieve parenthood, the journey is far from easy. IVF is not just a medical process—it’s an emotional marathon filled with highs and lows. As couples navigate this complex path, the emotional toll often becomes as significant as the physical or financial challenges.
Whether you're looking into the IVF cost and success rate, or searching for the Best IVF Clinic in Delhi, it’s equally crucial to understand the emotional side of the journey. This blog delves into the psychological challenges IVF presents and offers realistic, supportive coping strategies that help couples stay resilient.
Overview of IVF as a Physically and Emotionally Intense Journey
IVF is a multi-step process involving hormone injections, egg retrieval, fertilization in a lab, and embryo transfer. At every stage, hopeful parents encounter not just physical discomfort but emotional intensity.
For many, this journey begins with disappointment and desperation after months or years of unsuccessful conception. Couples turn to IVF as a beacon of hope. However, while clinics like the Best IVF Centre in South Delhi offer cutting-edge technologies and treatments, they can’t eliminate the emotional upheaval involved.
Adding to the emotional weight is the IVF cost breakdown, which often includes expenses for medications, consultations, lab work, and procedures—none of which guarantee success. The financial stress, especially for those comparing IVF costs by state or trying to calculate the IVF total cost in Delhi, adds another layer to an already demanding process.
Importance of Recognizing and Addressing Emotional Challenges
Emotional well-being during IVF is often overlooked. Many couples focus so much on the logistics, treatment protocols, and financial aspects that they forget to care for their mental health.
Ignoring emotional stress can lead to burnout, relationship strain, or even abandonment of treatment. Recognizing these emotional challenges early on and addressing them through communication, support, and professional help can make a world of difference.
A Message of Empathy and Support for Couples Navigating IVF
To every couple going through IVF: you are not alone. The path you're on is courageous, no matter the outcome. Whether you're researching the Top 5 IVF Centre in Delhi or trying to figure out how much IVF is with insurance, your feelings are valid, your fears are real, and your hope is powerful.
This blog is here to offer not just information, but understanding—to walk beside you in your emotional journey and provide practical tools for healing and resilience.
Understanding the Emotional Rollercoaster of IVF
Common Emotions During IVF
IVF often brings a whirlwind of conflicting emotions:
Hope – the driving force behind every appointment and injection.
Anxiety – stemming from medical procedures and uncertainty.
Fear – of failure, pain, or what the future holds.
Frustration – due to delays, costs, or the physical toll.
Grief – especially if cycles fail or losses occur.
Couples can feel all these emotions within a single day or even a single hour.
Emotional Impact of Failed Cycles or Uncertain Outcomes
One of the harshest realities of IVF is that success isn't guaranteed. Even after spending time and money at the Best IVF Centre in Greater Kailash Delhi, some cycles fail. The heartbreak of a negative pregnancy test can feel like mourning a loss.
Failed cycles can lead to self-doubt and guilt, even when the causes are out of your control. Add to this the pressure of IVF injections cost in Delhi and other financial considerations, and couples may feel like they’re investing emotionally in a black hole.
Pressure from Family, Society, and Self
In cultures where parenthood is expected after marriage, couples face additional emotional strain. Family members may ask invasive questions, friends may announce pregnancies, and societal timelines may add pressure.
Many couples internalize this pressure, feeling like they’ve failed as partners or adults. This self-imposed burden can be more damaging than external factors.
Emotional Stages Couples May Experience
Pre-Treatment Anxiety and Decision-Making Stress
Before the first appointment, couples often feel overwhelmed by questions:
Is this the right decision?
Can we afford the IVF total cost in Delhi?
What are our chances?
The fear of the unknown can paralyze decision-making.
Emotional Ups and Downs During Hormone Treatments and Procedures
Hormonal medications can cause mood swings, physical discomfort, and fatigue. These symptoms, combined with constant monitoring and invasive procedures, can erode emotional strength.
Even when attending a Top 5 IVF Centre in Delhi, the process is rarely smooth. Unexpected setbacks—such as fewer eggs retrieved or fertilization issues—can be emotionally jarring.
Waiting Period After Embryo Transfer
The "two-week wait" after embryo transfer is one of the most emotionally intense periods. Couples oscillate between hope and dread. Every cramp, every change in mood is overanalyzed.
This phase is mentally exhausting, yet couples are often expected to go about life normally.
Dealing with Positive or Negative Pregnancy Results
A positive result brings joy but also fear—especially of miscarriage. A negative result, on the other hand, leads to devastation.
Either outcome can deeply affect emotional well-being and strain relationships.
Differences in Coping Styles Between Partners
How Men and Women May Experience and Express Emotions Differently
Men and women often process IVF stress differently. Women, bearing the physical burden of treatment, may feel more emotionally raw. Men might internalize emotions, focusing on being supportive or practical.
This difference can lead to misunderstanding unless acknowledged openly.
Importance of Mutual Understanding and Support
A strong emotional partnership requires:
Active listening
Compassion for each other’s unique experience
Joint decision-making
Understanding that both partners are affected—even if in different ways—is key.
Avoiding Blame and Strengthening Emotional Connection
It’s crucial to avoid the blame game. Infertility is a medical condition, not a moral failure. Partners should remind each other: “We’re in this together.”
Celebrate small victories. Offer comfort without judgment. These are the building blocks of emotional strength.
Coping Strategies for IVF-Related Stress
Open Communication: Creating a Safe Space for Sharing Feelings
Honest conversations help couples stay emotionally aligned. Don’t just talk about logistics—discuss fears, dreams, and disappointments. Make it a daily practice to check in with each other.
Mental Health Support: Counseling, Therapy, and Support Groups
Seeing a therapist—especially one experienced in infertility—is not a sign of weakness. It’s proactive self-care.
Many clinics, including the Best IVF Centre in Delhi, now offer in-house counselors or referrals. Joining a support group, online or offline, can also ease the isolation.
Mindfulness Practices: Meditation, Yoga, and Breathing Exercises
Mindfulness can reduce stress hormones and bring calm. Yoga, especially fertility-focused routines, helps both body and mind. Breathing techniques can be life-changing during high-stress moments—like blood tests or procedure days.
Healthy Lifestyle: Exercise, Balanced Diet, and Sleep for Emotional Balance
Physical wellness affects emotional health. Light exercise improves mood. A balanced diet supports hormone regulation. Quality sleep is crucial for emotional stability.
Ask your clinic—like the Best IVF Centre in South Delhi—about wellness programs tailored to IVF patients.
Limiting Social Pressure: Setting Boundaries with Family and Friends
It’s okay to say, “We’re not ready to talk about it.” Set clear boundaries. Choose who to confide in. Don’t feel obligated to explain your journey to everyone.
Staying Informed: Understanding the Process to Reduce Fear of the Unknown
Knowledge reduces fear. Use trusted resources to learn about Advanced IVF techniques, stages of treatment, and what to expect.
Use an IVF cost calculator to plan realistically. Ask your doctor for success rate data, especially if you're comparing the IVF cost and success rate at different clinics.
When to Seek Professional Help
Recognizing Signs of Anxiety, Depression, or Burnout
Emotional red flags include:
Constant fatigue or sadness
Losing interest in daily activities
Sleep disruptions
Relationship conflicts
If you or your partner experience these, seek help immediately.
Role of Fertility Counselors and Mental Health Professionals
Fertility counselors offer coping tools and emotional support tailored to your journey. They can help both partners understand and support each other better.
Don’t hesitate to reach out—especially if your clinic, such as a Best IVF Clinic in Delhi, offers integrated mental health care.
Importance of Early Intervention and Ongoing Support
Getting support early can prevent emotional crises. Don’t wait until breaking point. Regular counseling, even just once a month, can provide stability.
Inspiring Stories of Resilience
Short Real-Life Anecdotes
Aditi and Raj, patients at the Best IVF Centre in Greater Kailash Delhi, faced two failed cycles. The grief nearly broke them, but therapy helped them reconnect. Their third cycle brought success, but more importantly, they felt emotionally prepared.
Meena and Ravi joined a support group while navigating IVF costs and decisions. Connecting with others helped them feel less isolated and more hopeful—even before their successful pregnancy.
Building a Support Network
Connecting with Others Going Through Similar Experiences
Joining IVF forums or support groups can provide comfort. You’re not the only one questioning if this path is right, or how to afford IVF with insurance.
Shared experiences build solidarity and reduce shame.
Online Forums, Local Support Groups, and Therapy Options
Search for support groups through your clinic or community centers. Some Top 5 IVF Centre in Delhi even host monthly peer sessions.
Online forums like Reddit, BabyCenter, or FertilityNetwork can also be helpful.
Encouragement to Reach Out and Not Go Through It Alone
You don’t have to suffer in silence. Reaching out is an act of strength—not weakness.
Encouragement & Hope for the Journey Ahead
Reinforcing That All Emotions Are Valid
It’s okay to cry. It’s okay to be angry, hopeful, or confused. Every emotion is valid and worthy of space.
IVF is not just a physical treatment—it’s an emotional journey, and your heart deserves care.
Staying Hopeful, Regardless of Outcomes
Hope isn’t just about success. It’s about perseverance. Even if IVF doesn’t lead to pregnancy, many couples find peace, strength, and new paths forward.
IVF is a Journey—Success Isn’t Only Defined by Pregnancy But Also by Courage
Your courage to face infertility, to try, to keep going—that is a success in itself.
You’ve shown love, determination, and emotional bravery. No matter the outcome, you’ve already triumphed in a way that deserves recognition.
Final Words
The emotional impact of IVF is real, deep, and often unspoken. But by recognizing these challenges, leaning on your partner, accessing support, and staying informed, you can navigate this journey with resilience and hope.If you’re just beginning your journey or are deep into your treatment, know that the right clinic, like the Best IVF Center in Delhi, will support both your physical and emotional needs.
1 note
·
View note
Text
Dr. Alka IVF: The Best Infertility Specialist in Udaipur
When it comes to starting a family, many couples encounter challenges along the way. Infertility is a common issue faced by both men and women, and it can cause a great deal of emotional and physical strain. Thankfully, advancements in medical science have made it possible for couples to overcome these challenges with the help of experienced specialists. Dr. Alka, widely recognized as one of the best infertility specialists in Udaipur, offers comprehensive services in infertility treatments.
Her clinic, Dr. Alka IVF, is known for providing world-class care, expert guidance, and successful treatment options for couples looking to conceive. In this article, we’ll delve into why Dr. Alka IVF is the go-to place for infertility treatments in Udaipur.
Why Choose Dr. Alka IVF?
There are numerous reasons why Dr. Alka is considered the best infertility specialist in Udaipur. These reasons revolve around her expertise, personalized care, and the use of the latest technologies. Here's a closer look at why so many couples trust her clinic with their fertility treatment needs:
1. Expertise and Experience
Dr. Alka’s vast experience in the field of infertility treatment sets her apart from others. With years of training and practical experience, she is highly skilled in diagnosing and treating a wide range of fertility issues. Whether the problem lies with male or female infertility, Dr. Alka provides accurate diagnoses and effective treatment plans. She specializes in various advanced techniques, including In Vitro Fertilization (IVF), IUI (Intrauterine Insemination), egg freezing, and more. Her expertise extends to handling complex infertility cases, making her the best infertility specialist in Udaipur for couples with difficult fertility issues.
2. Personalized Treatment Plans
One of the hallmarks of Dr. Alka IVF is her personalized approach to infertility treatment. She understands that every patient is unique, and their needs, preferences, and medical histories vary. Therefore, Dr. Alka takes the time to carefully assess each individual or couple’s situation and craft a treatment plan tailored specifically to them. Whether it’s recommending specific lifestyle changes or choosing the best fertility treatment, Dr. Alka ensures that every patient receives a plan that offers the best chance of success.
3. State-of-the-Art Facilities
At Dr. Alka IVF, the clinic is equipped with state-of-the-art medical equipment and the latest technology to support infertility treatments. From advanced diagnostic tools to cutting-edge fertility treatments, the clinic is well-equipped to provide a comprehensive range of services. These facilities ensure that patients receive the highest standard of care, increasing the chances of successful pregnancies.
4. High Success Rates
Success rates are a critical factor when choosing an infertility specialist, and Dr. Alka IVF has consistently high success rates. This success can be attributed to Dr. Alka’s in-depth understanding of fertility issues, her use of advanced treatments, and her hands-on care. She is committed to providing the best possible outcomes for her patients and works tirelessly to ensure that couples have the best chance of achieving their dreams of parenthood. Her clinic's track record speaks for itself, and many patients have shared their success stories, attributing their journey to becoming parents to Dr. Alka’s expertise.
5. Compassionate and Supportive Care
Dealing with infertility can be a deeply emotional experience. Dr. Alka and her team provide not only excellent medical care but also compassionate and supportive care to their patients. They understand the emotional toll that infertility can take, and they offer counseling and guidance throughout the treatment process. From the first consultation to the final stages of treatment, patients can expect a warm and supportive environment at Dr. Alka IVF. This level of care helps ease the stress and anxiety that many couples face during their fertility journey.
Services Offered at Dr. Alka IVF
Dr. Alka IVF provides a wide range of infertility services designed to meet the needs of couples at various stages of their fertility journey. Some of the key treatments and services available include:
In Vitro Fertilization (IVF)
IVF is one of the most advanced and effective treatments for infertility. Dr. Alka is highly experienced in IVF procedures, where the egg and sperm are combined outside the body in a laboratory setting, and the fertilized embryo is then transferred to the woman’s uterus. IVF has helped countless couples achieve their dream of parenthood, and Dr. Alka’s expertise ensures the highest chances of success.
Intrauterine Insemination (IUI)
IUI is a less invasive fertility treatment where sperm is directly injected into the uterus around the time of ovulation. This procedure is ideal for couples with mild infertility issues. Dr. Alka is known for providing personalized IUI treatments based on each couple’s needs.
Egg and Sperm Donation
For some couples, egg or sperm donation is necessary to conceive. Dr. Alka IVF offers both egg and sperm donation services, helping couples who may be dealing with male or female infertility issues. The clinic ensures that donated eggs and sperm are from carefully screened donors to ensure the best chances of a successful pregnancy.
Egg Freezing
For women who wish to delay childbearing for personal or medical reasons, egg freezing is an excellent option. Dr. Alka offers egg freezing services, allowing women to preserve their fertility for the future. This is particularly beneficial for women who may face a medical condition such as cancer, which could affect their fertility.
Fertility Preservation for Cancer Patients
Dr. Alka IVF also provides fertility preservation services for cancer patients who are undergoing treatments like chemotherapy that could affect their reproductive system. The clinic helps women and men preserve their fertility through egg, sperm, and embryo freezing, giving them the opportunity to have children in the future.
Patient Testimonials
The patients who have visited Dr. Alka IVF share glowing reviews about their experiences. Many have praised Dr. Alka for her professionalism, expertise, and the emotional support she provides. Couples have expressed their gratitude for the compassionate care they received, with many citing the clinic as a turning point in their journey toward parenthood.
Conclusion
For those seeking the best infertility specialist in Udaipur, Dr. Alka IVF is the clear choice. With her extensive experience, advanced treatment options, high success rates, and compassionate care, Dr. Alka has earned a reputation as one of the leading fertility specialists in the region. If you and your partner are struggling with infertility, Dr. Alka IVF offers the support and expertise you need to turn your dreams of parenthood into a reality.
0 notes
Text
Understanding IVF Treatment Procedure in Andhra Pradesh
Parenthood is a dream cherished by many, and thanks to advances in medical science, it is now possible to fulfill that dream even in the face of infertility. One of the most trusted methods to overcome fertility issues is In Vitro Fertilization (IVF). At Srujana Hospital, we offer a safe, personalized, and effective IVF Treatment Procedure in Andhra Pradesh, giving countless couples new hope.
Whether you're just starting your fertility journey or seeking expert care after years of trying, understanding the IVF Treatment Process in Andhra Pradesh can help you make informed and confident decisions.
The IVF Treatment Process in Andhra Pradesh – Step by Step
At Srujana Hospital, we follow a systematic and transparent IVF Treatment Process in Andhra Pradesh that includes
1. Initial Consultation and Fertility Testing: We begin with a detailed discussion and evaluation, including hormone tests, pelvic ultrasound, and semen analysis.
2. Ovarian Stimulation: The woman is given hormone injections for about 10–12 days to stimulate her ovaries to produce multiple eggs. We monitor follicle growth through ultrasound and blood tests.
3. Egg Retrieval: Once the follicles mature, we perform a minor procedure to collect the eggs. It is done under anesthesia and takes about 20–30 minutes.
4. Fertilization and Embryo Culture: The collected eggs are fertilized with sperm in our lab. The embryos are cultured for 3–5 days under expert supervision.
5. Embryo Transfer: A healthy embryo is selected and transferred into the woman’s uterus using a thin catheter. This step is quick and usually painless.
6. Pregnancy Test: Around 10–14 days after the transfer, a blood test is done to check for pregnancy.
This step-by-step IVF Treatment Procedure in Andhra Pradesh is designed to maximize the chances of a healthy pregnancy while ensuring patient safety and comfort.
Understanding IVF: A Proven Fertility Solution
In Vitro Fertilization (IVF) is an assisted reproductive technology (ART) where eggs are retrieved from the ovaries, fertilized with sperm in a laboratory, and then transferred back into the uterus. IVF is widely used to treat a range of fertility problems in both men and women.
At Srujana Hospital, we specialize in the complete IVF Treatment Procedure in Andhra Pradesh, using modern techniques, experienced specialists, and a caring approach.
Who Needs IVF?
IVF may be recommended in the following cases:
Blocked or damaged fallopian tubes
Ovulation disorders or low ovarian reserve
Endometriosis
Male infertility (low sperm count or motility)
Unexplained infertility
Failed previous fertility treatments
Advanced maternal age
We assess every couple thoroughly before recommending the appropriate treatment plan tailored to their needs
Why Choose Srujana Hospital?
Srujana Hospital has emerged as a leading center for IVF Treatment Process in Andhra Pradesh due to:
Experienced IVF specialists
Advanced embryology lab
Personalized treatment protocols
Transparent communication and affordable packages
High success rates and emotional support throughout the journey
We understand that infertility can be emotionally and physically challenging, which is why we prioritize compassionate care at every stage.
Preparing for IVF Emotionally and Physically
While undergoing the IVF Treatment Procedure in Andhra Pradesh, it’s essential to stay healthy and stress-free. Some tips include:
Maintain a balanced diet and exercise regularly
Avoid alcohol, smoking, and caffeine
Stay positive and manage anxiety through meditation or counseling
Have open communication with your partner and medical team
Our team also provides guidance and counseling for emotional well-being throughout the IVF Treatment Process in Andhra Pradesh.
Success Rates and Expectations
Success in IVF depends on several factors, like age, egg quality, and overall health. While not all cycles may be successful on the first attempt, many couples succeed in subsequent cycles. Our doctors keep you well-informed about realistic outcomes and provide all the support you need.
When Should You Consider IVF?
If you’ve been trying to conceive for more than a year (or six months if you're over 35), it’s time to consult a fertility specialist. Early diagnosis and timely treatment greatly increase your chances of success.
At Srujana Hospital, our comprehensive and compassionate approach to the IVF Treatment Process in Andhra Pradesh ensures that you receive the care and hope you deserve.
Final Thoughts
The road to parenthood may be challenging, but it doesn’t have to be lonely or confusing. With expert support, advanced technology, and a personalized approach, Srujana Hospital proudly offers one of the most trusted IVF Treatment Procedures in Andhra Pradesh.
Take the first step towards building your family — book a consultation today.
0 notes