DocTube is an enriching patient-engagement and patient-centric platform. Here thousands of doctors from across the country share valuable health-related information to raise awareness among the public.
Don't wanna be here? Send us removal request.
Text
Diagnosis and Treatment of Epilepsy

Epilepsy is a neurological disorder where a patient suffers from recurrent and unpredictable seizures. Seizures occur due to abnormal electrical activity in the brain, resulting in a temporary disruption of normal brain function. Epilepsy can affect people of all ages and can be caused by various factors, including genetic predisposition, brain injury, tumors, infections or developmental disorders. Seizures in epilepsy can manifest in different ways, depending on the area of the brain affected. They can range from brief lapses in awareness or staring spells to convulsions and loss of consciousness. Some seizures may be preceded by warning signs called auras, which can include visual disturbances, unusual sensations or emotional changes. The diagnosis of epilepsy is typically made after a person has experienced at least two unprovoked seizures. Medical professionals use a combination of clinical history, neurological exams and diagnostic tests such as electroencephalogram (EEG) to evaluate and diagnose epilepsy. It is important for people with epilepsy to work closely with healthcare professionals to develop an individualized epilepsy treatment plan and to take necessary precautions to minimize the risk of injury during seizures. With proper management and treatment of epilepsy, many individuals with epilepsy are able to lead active and fulfilling lives.
Diagnosis of Epilepsy
The diagnosis of epilepsy typically involves a comprehensive evaluation process conducted by medical professionals. Before initiating the treatment of epilepsy, the following methods are used to diagnose it effectively:
Medical history: The healthcare provider will begin by collecting a detailed medical history of the individual before starting relevant epilepsy treatment (Watanabe, E., Nagahori, Y. and Mayanagi, Y., 2002. Focus diagnosis of epilepsy using near‐infrared spectroscopy. Epilepsia, 43, pp.50-55). This includes information about the patient’s symptoms, the frequency and duration of seizures, any potential triggers, family history of seizures or epilepsy and any other relevant medical conditions.
Physical examination: A thorough physical examination will be conducted to look for any signs or symptoms that may be associated with epilepsy or other underlying medical conditions.
EEG: An EEG test is a crucial tool in diagnosing epilepsy. It involves placing electrodes on the scalp to record the electrical activity of the brain (Pillai, J. and Sperling, M.R., 2006. Interictal EEG and the diagnosis of epilepsy. Epilepsia, 47, pp.14-22). Abnormal patterns of brain waves known as epileptiform discharges can indicate the presence of epilepsy or seizure activity.
Additional tests: In some cases, additional tests may be ordered to gather more information and assist in the diagnosis. These can include brain imaging scans such as MRI or CT scans. These scans can help identify any structural abnormalities or lesions in the brain that may be causing the seizures.
Depending on the complexity of the case, individuals may be referred to a neurologist or an epileptologist, who are doctors specialized in the diagnosis and treatment of epilepsy.
Treatment of Epilepsy
The treatment of epilepsy aims to control seizures, reduce their frequency and severity, and improve the individual's quality of life. The specific treatment approach depends on various factors, including the type of seizures, the underlying cause of epilepsy, the individual's age, overall health, and their response to previous treatments. Here are some common treatment options for epilepsy:
Medications: Anti-epileptic drugs are usually the initial treatment of epilepsy. There are numerous AEDs available, and the recommended medication depends on the seizure type and individual factors. These medications work by stabilizing the electrical activity in the brain and reducing the likelihood of seizures. It is important to take the prescribed medication consistently and as directed by the healthcare provider.
Ketogenic Diet: This high-fat, low-carbohydrate and adequate-protein diet is known to be effective in reducing seizures, particularly in children suffering from epilepsy. It is typically supervised by a dietitian and requires careful monitoring.
Vagus Nerve Stimulation: VNS is a surgical treatment option that involves implanting a device under the skin of the chest that stimulates the vagus nerve (Binnie, C.D., 2000. Vagus nerve stimulation for epilepsy: a review. Seizure, 9(3), pp.161-169). This stimulation can help reduce the frequency and intensity of seizures in some individuals.
Responsive Neurostimulation: RNS is a newer treatment approach that involves the implantation of a device into the brain. The device detects abnormal brain activity and delivers electrical stimulation to prevent seizures from occurring.
Epilepsy Surgery: In cases where seizures are localized to a specific area of the brain, surgery may be the only option related to epilepsy treatment. The goal of epilepsy surgery is to remove or disconnect the brain tissue responsible for triggering seizures.
Lifestyle Modifications: Certain lifestyle changes may help manage epilepsy and reduce the risk of seizures. This comprises managing stress, following a good sleep schedule and avoiding seizure triggers like specific foods or alcohol and following medication schedules effectively.
#Treatment of Epilepsy#epilepsy treatment#epilepsy#health and wellness#healthcare information#health#doctube#healthcare
0 notes
Text
Symptoms and Management of Vocal Cord Paralysis

Vocal cord paralysis, also known as vocal fold paralysis is a medical condition characterized by the inability of one or both vocal cords to move or function properly. The vocal cords are located in the larynx or the voice box and play a crucial role in producing sound and enabling speech. In vocal cord paralysis, one or both of the vocal cords may become partially or completely paralyzed (Toutounchi, S.J.S., Eydi, M., Golzari, S.E., Ghaffari, M.R. and Parvizian, N., 2014. Vocal cord paralysis and its etiologies: a prospective study. Journal of cardiovascular and thoracic research, 6(1), p.47). This can result in a variety of symptoms, some of which may include including:
Symptoms of Vocal Cord Paralysis
Hoarseness or raspy voice: The voice may sound breathy, weak or strained due to the impaired movement of the affected vocal cord.
Voice fatigue: Speaking for extended periods can be tiring and may lead to a loss of voice or increased effort to produce sound.
Difficulty swallowing: The paralyzed vocal cord or cords may interfere with the normal closure of the larynx during swallowing, leading to swallowing difficulties or choking sensations.
Breathing difficulties: If the vocal cord fails to close properly during inhalation, it can cause breathing problems, especially during exercise or sleep.
Aspiration: If the vocal cord cannot close adequately during swallowing, food, liquids or saliva may enter the airway, leading to coughing, choking or recurrent respiratory infections.
Management of Vocal Cord Paralysis
Management and treatment of vocal cord paralysis usually depend on the underlying cause as well as the severity of the condition. In some cases, the paralysis may resolve on its own without any intervention. However, if the symptoms persist or cause significant functional impairment, treatment options may include voice therapy to improve vocal cord function, surgical procedures to reposition or reshape the vocal cords, or injections into the vocal cords to improve their movement. These may further be discussed as the following:
Voice therapy: Voice therapy can be beneficial for individuals with vocal cord paralysis. A speech-language pathologist can teach techniques to improve vocal cord function, breath control and voice projection (Walton, C., Carding, P. and Flanagan, K., 2018. Perspectives on voice treatment for unilateral vocal fold paralysis. Current Opinion in Otolaryngology & Head and Neck Surgery, 26(3), pp.157-161). These exercises help maximize vocal efficiency and reduce strain on the vocal cords.

Surgical interventions: Surgery may be recommended in cases where vocal cord paralysis significantly affects voice quality or breathing. The type of surgery will depend on the specific needs and conditions of the individual. Some surgical options may comprise of the following:
Vocal cord injection: This procedure involves injecting a filler substance, such as collagen or hyaluronic acid into the affected vocal cord to improve its movement and voice quality.
Vocal cord medialization: In this procedure, a small implant or suture is placed to reposition the paralyzed vocal cord, allowing it to meet the unaffected vocal cord more effectively during speech and swallowing.
Thyroplasty: Thyroplasty involves reshaping the thyroid cartilage to adjust the position and tension of the vocal cords, improving voice quality and control.
Treatment of the underlying cause: If vocal cord paralysis is caused by an underlying medical condition or injury, treating that condition may help resolve or improve the paralysis. This may include medication, therapy or addressing any structural issues or nerve damage.
Breathing and swallowing management: For individuals with breathing difficulties or swallowing problems due to vocal cord paralysis, strategies such as postural adjustments, diet modifications and swallowing therapy may be recommended to improve safety and quality of life.
Supportive measures
In addition to specific treatments, certain supportive measures can help manage vocal cord paralysis. These may include:
Vocal rest: Limiting voice use and avoiding excessive speaking or shouting can help prevent further strain on the vocal cords (Ryu, C.H., Kwon, T.K., Kim, H., Kim, H.S., Park, I.S., Woo, J.H., Lee, S.H., Lee, S.W., Lim, J.Y., Kim, S.T. and Jin, S.M., 2020. Guidelines for the management of unilateral vocal fold paralysis from the Korean society of laryngology, phoniatrics and logopedics. Clinical and experimental otorhinolaryngology, 13(4), pp.340-360).
Hydration: Staying hydrated by drinking enough fluids can help keep the vocal cords lubricated and reduce vocal fatigue.
Reflux management: If gastroesophageal reflux disease contributes to vocal cord paralysis, managing reflux symptoms through lifestyle changes and medications can be beneficial.
0 notes
Text
What is the normal thyroid level in female?
Thyroid function is measured by several hormones, including thyroid-stimulating hormone (TSH), free thyroxine (FT4) and triiodothyronine (T3). Normal thyroid levels can vary slightly depending on the laboratory reference ranges and individual factors. However, the generally accepted normal thyroid level in female may be identified as the following:
TSH (Thyroid-Stimulating Hormone): The normal range for TSH is typically between 0.4 and 4.0 mIU/L (milli-international units per liter). However, some experts suggest that a narrower range of 0.4 to 2.5 mIU/L may be more optimal.
FT4 (Free Thyroxine): The normal range for FT4 is generally between 0.8 and 1.8 ng/dL (nanograms per deciliter).
T3 (Triiodothyronine): The normal range for T3 is usually between 80 and 200 ng/dL.
It's important to note that these ranges are general guidelines, and individual factors and specific circumstances may require a more personalized approach (Alam Khan, V., Khan, M.A. and Akhtar, S., 2002. Thyroid disorders, etiology and prevalence. J Med Sci, 2(2), pp.89-94). If a patient has concerns about his thyroid levels, it is always recommended to consult with a healthcare professional who can evaluate his specific situation and provide appropriate guidance.
Thyroid issues have become widely common in both males and females. Thyroid symptoms for male and female patients may often vary although there are also many similarities. Read along to know the potential differences in thyroid symptoms that may occur in males:
Fatigue and weakness: Both males and females with thyroid issues may experience fatigue and weakness (Sawicka-Gutaj, N., Ziółkowska, P., Wojciechowska, K., Shawkat, S., Czarnywojtek, A., Warchoł, W., Sowiński, J., Szczepanek-Parulska, E. and Ruchała, M., 2021. Eye symptoms in patients with benign thyroid diseases. Scientific Reports, 11(1), p.18706). However, males may be more likely to attribute these symptoms to other factors, such as stress or aging, rather than considering thyroid dysfunction.
Muscle mass and weight changes: Thyroid disorders can affect body composition and weight. In males, an underactive thyroid or hypothyroidism may lead to a decrease in muscle mass, weight gain and difficulty losing weight. On the other hand, an overactive thyroid or hyperthyroidism can cause weight loss and a decrease in muscle mass.
Sexual and reproductive symptoms: Males with thyroid dysfunction may experience changes in libido, erectile dysfunction or decreased fertility. These thyroid symptoms for male patients can be related to hormonal imbalances caused by thyroid disorders.
Emotional changes: While both genders can experience emotional changes due to thyroid problems, males may be more likely to exhibit irritability or anger rather than depression or anxiety commonly seen in females.
Cardiovascular symptoms: Hyperthyroidism in males may be associated with different kinds of cardiovascular symptoms like an increased heart rate, palpitations and high blood pressure.
It is important to know that these differences are not definitive and thyroid symptoms can vary widely among individuals, regardless of gender. Additionally, many symptoms of thyroid disorders can overlap between males and females. If a person suspects having a thyroid issue, it is essential to consult a healthcare professional for proper evaluation and diagnosis.
Management of thyroid symptoms for male and female patients
Managing thyroid problems typically involves a combination of medical treatments, lifestyle modifications and regular monitoring. Some general strategies for managing thyroid problems may include the following:
Medical treatment: Thyroid disorders such as hypothyroidism or hyperthyroidism are often treated with medications. These medications aim to restore thyroid hormone levels to a balanced state. It is important to follow your healthcare professional's prescribed treatment plan, take medications as directed and attend regular check-ups.
Regular monitoring: Thyroid function should be regularly monitored through blood tests to assess hormone levels and adjust medication dosages as needed (Shaha, A.R., 2000. Controversies in the management of thyroid nodule. The laryngoscope, 110(2), pp.183-183). Follow-up appointments with your healthcare professional are crucial for ongoing management.
Healthy diet: A well-balanced diet that includes adequate amounts of iodine, selenium and other essential nutrients can support thyroid health. Consult with a registered dietitian or healthcare professional to develop a personalized diet plan that meets your specific needs.
Stress management: Stress can have an impact on thyroid function. It is beneficial to engage in stress-reducing activities such as exercise, meditation, deep breathing exercises or hobbies to help manage stress levels.
Regular exercise: Regular physical activity can help boost metabolism, maintain a healthy weight and improve overall well-being. Thyroid patients are often recommended to follow a combination of cardiovascular exercise, strength training and flexibility exercises. However, it is important to consult a healthcare professional before starting any exercise program.
Adequate sleep: Patients must prioritize getting enough restful sleep each night. They must strive to establish a consistent sleep routine, create a sleep-friendly environment and practice good sleep hygiene habits.
Avoid smoking and limit alcohol: Smoking can negatively affect thyroid function, so quitting smoking is always advisable (Knudsen, N., Bulow, I., Laurberg, P., Perrild, H., Ovesen, L. and Jorgensen, T., 2002. High occurrence of thyroid multinodularity and low occurrence of subclinical hypothyroidism among tobacco smokers in a large population study. Journal of Endocrinology, 175(3), pp.571-576). Additionally, excessive alcohol consumption can interfere with thyroid hormone production, so it is best to consume alcohol in moderation or avoid it altogether.
Self-awareness and education: It is important for patients to learn about their specific thyroid condition and its management. They must stay informed about any new research, treatment options or lifestyle recommendations related to thyroid health.
Managing thyroid problems is an individualized process and it is important to work closely with your healthcare professional to develop a personalized treatment plan that meets your specific needs. Healthcare professionals can provide guidance, monitor your progress and make any necessary adjustments to optimize your thyroid health.
#normal thyroid level in female#health#healthcare#doctube#healthcare information#health and wellness#thyroid symptoms for male#thyroid symptoms#thyroid
0 notes
Text
Causes and Treatment of Vocal Cord Paralysis
Vocal cord paralysis is a condition where a person is not able to control muscle movements that control his voice. It usually happens due to disruptions in the nerve impulses to a person’s larynx. This leads to paralysis of the muscles present in the vocal cord. This condition makes it difficult for the patient to speak or even breathe. This is because the vocal cords have more roles than merely producing sound. They protect a person’s airways by preventing food objects from entering the windpipe thereby helping a person to prevent choking (Toutounchi, S.J.S., Eydi, M., Golzari, S.E., Ghaffari, M.R. and Parvizian, N., 2014. Vocal cord paralysis and its etiologies: a prospective study. Journal of cardiovascular and thoracic research, 6(1), p.47). Usually, in the case of vocal cord paralysis, one vocal cord is paralyzed. However, in a few severe cases, a person may also suffer from paralysis of both vocal cords. This is a serious condition that may lead to speech difficulties as well as problems in swallowing and breathing. For more information and insights on this condition, follow DocTube.
Symptoms of Vocal Cord Paralysis
The common signs and symptoms of vocal cord paralysis are diverse and may include the following:
Hoarseness
Noisy breathing
Loss of vocal pitch
Shortness of breath
Coughing or choking while drinking or swallowing food
Inability to speak loudly
A need to take frequent breaths while speaking
Ineffective coughing
Loss of the gag reflex
Frequent throat clearing
Whenever a person experiences unexplained voice hoarseness that does not go away even after 2-4 weeks or if there are unexplained voice changes and discomfort, it is crucial for him to make a prompt consultation with a healthcare provider.
Causes of Vocal Cord Paralysis
In the case of vocal cord paralysis, a person’s nerve impulses to his larynx are disrupted which causes paralysis of the muscle. It often becomes difficult for healthcare providers to determine the main cause of this vocal cord paralysis. However, some of the commonly known causes may often comprise the following:
Chest or neck injury: Often trauma to the chest or neck can injure nerves that serve the vocal cords or the larynx.
Vocal cord injury during surgery: Surgery on or near the upper chest or neck may lead to some damage to the nerves that serve the larynx (Gupta, J., Varshney, S., Bist, S.S. and Bhagat, S., 2013. Clinico-etiolological study of vocal cord paralysis. Indian Journal of Otolaryngology and Head & Neck Surgery, 65, pp.16-19). Some of the common surgeries that involve a certain degree of risk of damage are surgeries to the parathyroid or thyroid glands, chest, neck and esophagus.
Stroke: Strokes interrupt the flow of blood in the brain and this may damage the part of our brain that is responsible for sending messages to the larynx.
Tumors: Cancerous as well as non-cancerous tumors may grow in and around the nerves, muscles and cartilage that control the functioning of the larynx and this may lead to vocal cord paralysis in patients.
Infections: Some infections like herpes and Lyme disease may lead to inflammation and damage of the nerves in the voice box. It has also been found that COVID-19 infection may cause vocal cord paralysis in individuals.
Neurological conditions: Vocal cord paralysis may also be caused by certain neurological conditions like Parkinson’s disease and multiple sclerosis.
People who undergo surgery on their throat, upper chest or thyroid have a higher risk of damaging their vocal cord nerve. In some cases, the breathing tubes used during surgery or for helping a patient to breathe if he has severe respiratory trouble may damage his vocal cord nerves. On the other hand, as stated above, patients with certain neurological conditions like multiple sclerosis and Parkinson’s disease are more prone to suffer from weakness or paralysis of their vocal cords.
Complications of Vocal Cord Paralysis
Breathing issues linked to vocal cord paralysis may be mild enough to be causing just a hoarse voice. However, in severe cases, they may also be life-threatening. As vocal cord paralysis prevents the opening of the airway from closing and opening completely, other complications may also be faced. These may include inhaling or choking on food or liquid. Aspiration can result in severe pneumonia and this condition needs immediate medical care.
Treatment of Vocal Cord Paralysis
Surgery and voice therapy are the most common treatments done for vocal cord paralysis. In some patients, their voices will recover naturally during the first year following diagnosis and it is because of this reason that doctors may often delay surgery for a year. During this time, doctors usually refer patients to speech-language pathologists. Voice therapy is recommended for such patients. This involves exercises for strengthening the vocal cords and improving breath control while talking. These therapists may teach patients how to use their voices differently. For example, this may include opening the mouth wider when you speak or speaking slowly. On the other hand, different surgical procedures are also available and this usually depends on whether one or both the vocal cords are paralyzed.
In these surgeries, efforts are made to change the position of the vocal fold. It can include inserting structural implants and stitches for repositioning the laryngeal cartilage and for bringing the vocal folds closer (Dankbaar, J.W. and Pameijer, F.A., 2014. Vocal cord paralysis: anatomy, imaging and pathology. Insights into imaging, 5(6), pp.743-751). This leads to a stronger voice in patients. Surgery is often followed by additional voice therapy as this helps in fine-tuning the voice. In case both the vocal folds are paralyzed, a tracheotomy may be needed to help patients with breathing. In this surgery, an incision is made on the front portion of the neck and a breathing tube is thereafter inserted into the trachea. Due to this surgery, breathing happens through the tube rather than the mouth and nose. After the surgery, patients are again referred to speech-language pathologists wherein they learn how to use the voice well and how to take care of the breathing tube.
#Vocal Cord Paralysis#doctube#healthcare#health#health and wellness#healthcare information#treatment#doctors#health articles
0 notes
Text
Know About Atrial Septal Defect

An atrial septal defect is a birth defect wherein there is a hole in the wall that divides the atria or the upper chambers of the heart. This hole may differ in size and in many cases may close on its own. However, in some cases, it may require surgery. An atrial septal defect is one of the common kinds of congenital heart defects or those defects that are present at birth. A baby’s heart develops during pregnancy and thus there are several openings in the wall that divides the upper chambers of the heart. These holes generally close during pregnancy or within a short span of time after birth. However, if one of these openings do not close, a hole is left and this is termed an atrial septal defect (Geva, T., Martins, J.D. and Wald, R.M., 2014. Atrial septal defects. The Lancet, 383(9932), pp.1921-1932). This hole increases the amount of blood flowing through the baby’s lungs and with time, it causes damage to the blood vessels in the lungs. On the other hand, damage to the blood vessels in the lungs can lead to complications as the child grows and enters adulthood and some of these problems may include high blood pressure and heart failure. In addition to these, other complications may include an increased risk of stroke and abnormal heartbeat.
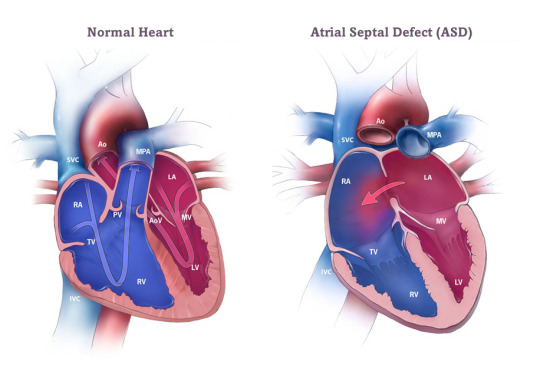
Diagnosis of an Atrial Septal Defect
An atrial septal defect can be diagnosed during pregnancy and may also be detected after the child is born. However, in several cases, it may be left undetected until the child reaches adulthood. During pregnancy, a woman may go for different kinds of screening tests or prenatal tests to diagnose birth defects as well as other conditions. An atrial septal defect can be seen by an ultrasound (Webb, G. and Gatzoulis, M.A., 2006. Atrial septal defects in the adult: recent progress and overview. Circulation, 114(15), pp.1645-1653). However, this is usually dependent on the location and the size of the hole. Whenever an atrial septal defect is suspected, specialists are required to confirm the diagnosis. On the other hand, genetic testing may also be helpful if the patients or any of their biological family members have congenital heart disease. An atrial septal defect is usually present at birth. However, many babies may not have any signs and symptoms. For the best insights on this condition, follow DocTube.
Symptoms of an Atrial Septal Defect
Some of the most common signs of untreated atrial septal defect may comprise the following:
Difficulty breathing
Frequent lung or respiratory infections
Tiring when feeding the baby
Shortness of breath while exercising or being active
Skipped heartbeat
Swelling of the stomach area, feet or legs
A whooshing sound or a heart murmur that is heard with a stethoscope.
As stated above, in many cases, atrial septal defects are not diagnosed until a child reaches adulthood. One of the best and commonest ways this condition is diagnosed is by detecting murmurs when listening to the patient’s heart with a stethoscope. The healthcare professional usually requests some other tests to confirm the diagnosis if a murmur is heard or if other symptoms are present in the patient. Echocardiogram is the most common test which includes conducting an ultrasound of the heart.
Treatment of an Atrial Septal Defect
Atrial septal defects may be closed through percutaneous or non-surgical repair or through surgical methods. The kind of treatment usually depends on diverse factors such as the size and the type of defect and how the condition is affecting the patient’s heart (Liava’a, M. and Kalfa, D., 2018. Surgical closure of atrial septal defects. Journal of thoracic disease, 10(Suppl 24), p.S2931). It also depends on other conditions that the patient may have like coronary artery disease, valve disease or pulmonary hypertension. Small atrial septal defects usually do not need any repair. On the other hand, larger atrial septal defects must be treated and repaired even if they are not causing any problems. This is important as this helps to prevent many different kinds of serious complications in the future. Repair becomes essential whenever a person exhibits any signs of lung or heart damage. Healthcare professionals recommend prompt treatment if the right side of the heart is larger than normal or if there is a significant amount of shunting or flow of blood through the ASD.
Medications may be prescribed for treating some symptoms of atrial septal defect. However, it is important to note that there are no medications that can close this hole. In addition, if the person suffers from pulmonary hypertension, he must take relevant medications before the repair procedure is done. This is important as such medication helps to treat pulmonary hypertension while making the procedure safer for the patient. Closure of the hole is commonly recommended for adults who have many and severe symptoms. This closure may be done during open-heart surgery or cardiac catheterization. After such procedures are done, follow-up care depends on the patient’s age, the size of the defect and the presence of any other birth defects.
Prevention of an Atrial Septal Defect
It is important to note that there is no particular way to prevent this defect. They may develop when the fetus is still present in the uterus. However, proper prenatal care can have a substantial impact on the fetus’s chance of developing congenital heart disease. So if you are planning a pregnancy, it is important for you to consider the following factors:
Avoid drinking alcohol
Quit smoking and using all kinds of tobacco products
Avoid secondhand smoke as much as possible
Avoid all forms of recreational drugs
Talk to your doctor about the common prescription medications that you are taking and if they are prone to affect your pregnancy in any manner.
1 note
·
View note
Text
Beware! Smoking Causes These Problems In Your Body

There is no way around it, smoking is incredibly bad for your health and it affects nearly every organ of the body. Cigarettes, cigars, pipes and various forms of smokeless tobacco such as chewing tobacco or snuff are common examples of smoking products. Each of these is equally harmful and is in no way better than the other. Nicotine is the addictive drug present in tobacco smoke that makes smokers continue smoking. Smoking causes diverse kinds of complications and problems in the human body. Along with nicotine, smokers are prone to inhale around 7000 other chemicals present in cigarette smoke. Some of these compounds are known to be chemically active and trigger damaging and profound changes in the body.
Tobacco smoke contains more than 70 cancer-causing chemicals. Smoking causes harm to almost all organs of the body and affects your overall health in general. Indeed all of us are aware of how smoking causes health problems. Yet, people do smoke, despite knowing the risks. Let us first see why. The causes of smoking are diverse and must be understood well. For example, social factors play a significant role in smoking initiation and maintenance. In addition, peer pressure, cultural norms and social acceptance of smoking can influence an individual's decision to start smoking. If someone grows up in an environment where smoking is prevalent or if they have friends or family members who smoke, they may be more likely to start smoking themselves. Causes of smoking may also include other factors like stress. Some individuals turn to smoking as a way to cope with stress, anxiety or other emotional issues. Smoking is often perceived as a way to relax or relieve tension. However, while it may provide temporary relief, smoking actually increases stress levels in the long run and can create a cycle of dependence. Smoking tobacco introduces various harmful chemicals into the body, including nicotine, tar, carbon monoxide and numerous carcinogens. These substances can have detrimental effects on the health of individuals who smoke, as well as those who are exposed to secondhand smoke. Let us now identify how smoking causes different kinds of health hazards and problems.
Increased risk of cancer: Smoking is the leading cause of preventable cancer worldwide. It is strongly linked to lung cancer as well as cancers of the mouth, throat, esophagus, pancreas, bladder, kidney and cervix.
Respiratory problems: Smoking causes widespread damage to the lungs and respiratory system, leading to chronic conditions such as chronic obstructive pulmonary disease, emphysema and chronic bronchitis. These conditions can cause breathing difficulties, coughing, wheezing and reduced lung function.
Cardiovascular diseases: Smoking is a significant risk factor for heart disease and stroke. It damages blood vessels, increases blood pressure, contributes to the formation of blood clots and reduces the oxygen-carrying capacity of the blood.
Reduced fertility and pregnancy complications: Smoking can impair fertility in both men and women. Pregnant women who smoke are at a higher risk of complications such as miscarriage, premature birth, low birth weight, and developmental issues in their babies. It is also commonly linked to infertility in males. For the best insights on how smoking causes male infertility, follow DocTube.
Skin and oral health problems: Smoking accelerates the aging process, leading to premature wrinkling and skin damage. It also contributes to gum disease, tooth loss, bad breath and oral cancers.
Increased risk of other diseases: Smoking is associated with an increased risk of various other health problems including diabetes, osteoporosis, rheumatoid arthritis and vision-related issues.
Quitting smoking at any age can provide significant health benefits. If you are a smoker and want to quit, there are various resources available, such as counseling, medications, support groups and helplines that can assist you in your journey to become smoke-free.
#smoking causes#causes of Smoking#health#smoking#health and wellness#healthcare information#healthcare#doctube
0 notes
Text
Learn the Best Way to Manage Asthma

Asthma is a chronic respiratory condition that affects the airways, which are the tubes that carry air in and out of the lungs. It is characterized by inflammation and narrowing of the airways, leading to symptoms such as wheezing, shortness of breath, chest tightness, and coughing. When a person with asthma is exposed to certain triggers, such as allergens like pollen, dust and mites or irritants like smoke, air pollution and strong odors or other conditions like respiratory infections, exercise or emotional stress, the airways become inflamed and constricted. This inflammation causes the muscles around the airways to tighten and produce excess mucus, thereby further obstructing the airflow. For the best insights on asthma and its management, follow DocTube.
Common symptoms of asthma:
Wheezing: A high-pitched whistling sound when breathing, especially during exhalation.
Shortness of Breath: Difficulty breathing, wherein a person feels that he cannot get enough air or has to catch his breath.
Chest Tightness: A sensation of tightness or pressure in the chest.
Coughing: A persistent cough, especially at night or in response to triggers.
The severity and frequency of asthma symptoms can vary from person to person. Some individuals may experience occasional mild symptoms, while others may have more frequent and severe episodes that significantly impact their daily activities and quality of life. The best way to manage asthma involves a combination of medical treatment and self-care strategies. Here are some of the best ways to manage asthma effectively:
Taking Prescribed Medications: Use prescribed asthma medications as directed by your healthcare provider. This may include long-term controller medications to manage inflammation and prevent symptoms, as well as quick-relief medications to relieve acute symptoms during an asthma attack. It is also important to understand how to properly use inhalers or other devices and adhere to the prescribed dosage schedule to manage asthma well.
Identifying and Avoiding Triggers: Patients must determine the specific triggers that worsen their asthma symptoms and take steps to avoid or minimize exposure to them. These may include exposure to pollen, smoke, dust mites, strong odors and different kinds of infections. Therefore creating a trigger-free or low-trigger environment can significantly reduce asthma symptoms.
Maintaining a Healthy Environment: To manage asthma effectively, it is important to keep your home clean and free of dust, mold and other allergens. Vacuum the rooms regularly and maintain proper ventilation. Avoid smoking and secondhand smoke exposure, as it can worsen asthma symptoms. If you have pets and are allergic to them, consider minimizing exposure or finding alternative arrangements.
Staying Active and Exercising Safely: Regular physical activity can benefit overall health, including lung function. It is crucial for asthma patients to consult their healthcare provider about the most suitable exercises for them and if there are any precautions they should take. Warm up adequately and avoid exercising in cold or dry environments when symptoms tend to worsen.
Managing Stress: Emotional stress can trigger or worsen asthma symptoms. Patients must practice different kinds of stress management techniques like deep breathing exercises, yoga, meditation or engaging in activities they enjoy to help reduce stress levels and promote overall well-being.
Monitoring Lung Function: Use a peak flow meter or a spirometer to regularly monitor your lung function. This can help you track changes in airflow and detect early signs of worsening asthma. It is crucial to follow instructions given by healthcare providers on how to use these devices and when to seek medical attention based on the results.
Regular Check-ups: To manage asthma well, patients must attend scheduled check-ups with their healthcare provider to assess their asthma control. They have to adjust medication if needed and address concerns or questions that they may have. Regular monitoring is crucial for optimizing asthma management.
Educating Yourself: Patients must learn as much as possible about asthma, its triggers and management strategies. They must also understand how to recognize and respond to worsening symptoms or an impending asthma attack. Education empowers a person to take control of his health condition and make informed decisions regarding his health.
Thus, remember to consult your healthcare provider for personalized advice and guidance specific to your asthma management. Following these strategies and working closely with your healthcare provider can help you to manage asthma well while minimizing its impact on your daily life.
0 notes
Text
Are You Experiencing These Symptoms of Abdominal Wall Hernia?

An abdominal wall hernia occurs when an organ or tissue protrudes through a weak spot or opening in the abdominal wall. The abdominal wall is composed of several layers of muscle and tissue that help protect the organs in the abdominal cavity. However, certain factors can weaken the abdominal wall, allowing a hernia to develop. Inguinal hernias occur in the groin area and are more common in men. They can develop due to a weakness in the inguinal canal, which allows a portion of the intestine or fatty tissue to protrude.
Similar to inguinal hernias, femoral hernias also occur in the groin area. However, they are more common in women and tend to protrude through the femoral canal. Incisional hernias develop at the site of a previous surgical incision. They occur when the surgical incision does not heal properly, leading to a weakness in the abdominal wall. Hiatal hernias involve the upper part of the stomach pushing up through the diaphragm into the chest cavity. They are associated with the hiatus, a small opening in the diaphragm through which the esophagus passes.
Causes and Risk Factors of Abdominal Wall Hernia
Age: The risk of developing an abdominal wall hernia tends to increase with age. This is because the abdominal muscles may weaken over time, making them more susceptible to herniation.
Gender: Some types of hernias are more common in one gender than the other. For example, inguinal hernias are more prevalent in males, while femoral hernias are more common in females.
Family history: There may be a genetic component to hernia development. If a person has a close family member who has had a hernia, he may be at a higher risk of developing one.
Obesity: Being overweight or obese puts additional strain on the abdominal muscles and can weaken the abdominal wall, making hernias more likely to occur.
Chronic coughing or sneezing: Conditions that involve frequent and forceful coughing or sneezing, such as chronic bronchitis or allergies, can strain the abdominal muscles and increase the risk of abdominal wall hernia development.
Heavy lifting: Engaging in activities that involve heavy lifting or straining can put excessive pressure on the abdominal muscles. This can weaken the abdominal wall and contribute to herniation.
Chronic constipation: Regularly straining during bowel movements due to chronic constipation can also put a strain on the abdominal muscles and increase the risk of hernia development.
Symptoms and Complications
The symptoms of an abdominal wall hernia may vary depending on the type and size of the hernia. Common symptoms include a visible or palpable bulge or lump in the affected area, discomfort or pain at the hernia site, aching or heaviness, and possible gastrointestinal symptoms like nausea, vomiting, or difficulty passing stool or gas. If left untreated, abdominal wall hernias can lead to complications such as strangulation or incarceration. Strangulation occurs when the herniated tissue becomes trapped and its blood supply is compromised. This can be a medical emergency and requires immediate attention.
Diagnosis and Treatment
Abdominal wall hernias are typically diagnosed through a physical examination. Imaging tests like ultrasound, CT scan or MRI may be done to confirm the diagnosis or assess the extent of the hernia. Treatment options include lifestyle modifications to manage symptoms and surgical repair. Surgery is the most common treatment for symptomatic or large hernias. If anyone suspects to have an abdominal wall hernia or is experiencing symptoms related to it, it is important to consult a healthcare professional for proper evaluation, diagnosis and treatment recommendations. These professionals can provide guidance based on the specific type and severity of the hernia.
#abdominal wall hernia#hernia#healthcare information#healthcare#health#health and wellness#wellness#treatment#doctube
0 notes
Text
Essential Guide: Foods to Avoid During Pregnancy

Pregnancy is an extraordinary journey filled with joy, anticipation, and responsibility. During this time, it is crucial for expectant mothers to prioritize their health and well-being, as they are nurturing a new life within. One significant aspect of a healthy pregnancy is consuming a balanced and nutritious diet. While there are numerous foods that provide essential nutrients for both mother and baby, it is equally important to be aware of foods to avoid during pregnancy. Some of these foods are as follows:
Raw or Undercooked Meats:
Raw or undercooked meats, such as poultry, beef, and seafood, pose a significant risk of bacterial or parasitic infections. These infections can lead to severe complications such as miscarriage, preterm labour, or developmental issues in the unborn baby. Therefore, it is crucial to ensure that the meats are thoroughly cooked to kill any harmful bacteria or parasites before consumption.
Raw or Unpasteurized Dairy Products:
Raw milk, unpasteurized cheese, and other dairy products can harbour harmful bacteria like Listeria, Salmonella, or E. coli1. These bacteria can cause foodborne illnesses that can be detrimental to both the mother and the developing baby. Thus, it is advisable to choose pasteurized dairy products to eliminate the risk of bacterial contamination.
Certain Seafood:
Undoubtedly, seafood is an excellent source of omega-3 fatty acids and other essential nutrients. However, some varieties contain high levels of mercury, which can be harmful to the developing nervous system of the fetus2. Avoid consuming shark, swordfish, king mackerel, and tilefish, as they tend to have higher mercury content. Instead, opt for low-mercury fish like salmon, shrimp, and catfish, and limit your consumption to two to three servings per week.
Raw or Undercooked Eggs:
One of the foods to avoid during pregnancy is raw or undercooked eggs as they may contain Salmonella, which can cause food poisoning. Additionally, it is also advised to avoid foods containing raw or partially cooked eggs, like homemade mayonnaise, Caesar salad dressing, and certain desserts like mousse or tiramisu. However, eggs can be consumed, but it needs to be ensured that they are thoroughly cooked until both the white and yolk are firm.
Unwashed Fruits and Vegetables:
Fresh fruits and vegetables are an essential part of a healthy diet. However, unwashed ones may contain potential bacteria, pesticides, or dirt. Thus, the consumption of unwashed produce can lead to foodborne illnesses. Hence, it is one of the crucial foods to avoid during pregnancy.
Caffeine:
While a moderate intake of caffeine is generally considered safe during pregnancy, excessive consumption should be avoided. High levels of caffeine have been linked to an increased risk of miscarriage and preterm birth. It is recommended to limit caffeine intake to no more than 200 milligrams per day, which is roughly equivalent to one 12-ounce cup of coffee3.
Alcohol:
The consumption of alcohol during pregnancy is strongly discouraged. It can lead to fetal alcohol spectrum disorders (FASDs), which can cause physical, behavioural, and cognitive abnormalities in the baby. Hence, it is best to abstain entirely for the duration of pregnancy. Knowledge of food to avoid during pregnancy can significantly ease your journey to pregnancy.
Reference list
Pal, M., Mulu, S., Tekle, M., Pintoo, S.V. and Prajapati, J., 2016. Bacterial contamination of dairy products. Beverage and food world, 43(9), pp.40-43.
Kim, E.H., Kim, I.K., Kwon, J.Y., Kim, S.W. and Park, Y.W., 2006. The effect of fish consumption on blood mercury levels of pregnant women. Yonsei Medical Journal, 47(5), pp.626-633.Keegan, J., Parva, M., Finnegan, M., Gerson, A. and Belden, M., 2010. Addiction in pregnancy. Journal of addictive diseases, 29(2), pp.175-191.
#Foods to Avoid During Pregnancy#food to avoid during pregnancy#during pregnancy#pregnancy#healthcare information#healthcare#health and wellness#health
0 notes
Text
Preseptal Cellulitis Causes and Management

Preseptal cellulitis is also known as periorbital cellulitis, an infection that affects the tissues surrounding the eyes. Preseptal cellulitis causes mainly include insect bites or other kinds of minor trauma or the spread of sinus and other infections. It causes swelling and redness of the eyelid and the skin around the eyes. Preseptal cellulitis can be treated effectively with close monitoring and antibiotics. However, it may be serious if ignored and left untreated. It may lead to permanent vision problems as well as blindness if the infection spreads to the eye socket. Therefore to prevent complications, prompt diagnosis and treatment are crucial.
Symptoms of Preseptal Cellulitis
Eye pain
Redness around the eyelid
Swelling of the eyelid and the area surrounding the eye
Low-grade fever
Primary Causes of Preseptal Cellulitis
Viruses
Bacteria
Fungi
Helminths, also known as parasitic worms
Most of the preseptal cellulitis causes are due to infection caused by bacteria. These bacterial infections can spread from sinus infections or from other parts of the eye. In addition, it can also occur due to minor trauma to a person’s eyelids such as scratches or bug bites. After minor injuries, bacteria can enter this wound and cause infections. Streptococcus, Staphylococcus and Haemophilus influenzae are the most common bacteria that cause this condition. Preseptal cellulitis is more commonly seen in children as they are at a higher risk for infection. The primary treatment includes antibiotics that may be given intravenously or orally. The kind of antibiotics given usually depend on a person’s age and whether the type of bacteria causing the infection has been identified.
Diagnosis of Preseptal Cellulitis
Optometrists or ophthalmologists are likely to conduct a physical examination of the eye. After checking for any potential signs of infection such as pain, swelling and redness, other tests may be ordered. It may include taking a sample of blood or discharge from the eye. These samples are thereafter analyzed in the laboratory to find out which kind of bacterium has caused the infection. Other tests like CT scans and MRIs may be suggested to understand how far this infection has spread. Thus, preseptal cellulitis is not usually a serious condition if treated right away and may clear up quite quickly with the right antibiotics. However, it may lead to further complications and severe vision difficulties if left untreated.
#preseptal cellulitis causes#causes of preseptal cellulitis#preseptal cellulitis#doctube#healthcare#health#healthcare information#health and wellness
0 notes
Text
Causes of Preseptal Cellulitis and its Management

Preseptal cellulitis is an infection that occurs in the tissues surrounding the eyes. It is also commonly known as periorbital cellulitis and may be caused by minor trauma to a person’s eyelid. This may include insect bites or the spreading of other infections such as sinus infections. It causes redness as well as swelling of the eyelid and the skin around the eyes. Preseptal cellulitis can be treated successfully with close monitoring and antibiotics. However, it can be serious if ignored and left untreated. It can lead to permanent vision problems and even blindness if the infection spreads to the eye socket. Prompt treatment is therefore crucial to prevent such complications.
Common Symptoms of Preseptal Cellulitis
Redness around the eyelid
Eye pain
Swelling of the eyelid and the area surrounding the eye
Low-grade fever
Causes of Preseptal Cellulitis
It is important to know the different causes of preseptal cellulitis so that this condition can be managed effectively. It can be caused by:
Bacteria
Fungi
Viruses
Parasitic worms
However, the majority of preseptal cellulitis infections are caused by bacteria. Bacterial infections can spread from sinus infections or from other parts of the eye. In addition, it can also occur due to minor trauma to the eyelids such as from a cat scratch or bug bite. After these minor injuries, bacteria can cause infections by entering the wound.
Some of the most common bacteria that cause preseptal cellulitis are Streptococcus, Staphylococcus and Haemophilus influenzae. This condition is usually more commonly seen in children than adults as children remain at a higher risk of these infections.
When to consult a doctor?
It is important to consult a healthcare provider immediately if any of the symptoms of preseptal cellulitis are experienced such as swelling and redness of the eye. Early diagnosis and treatment prove crucial in preventing further complications.
Diagnosis and Management of Preseptal Cellulitis
Prompt diagnosis of preseptal cellulitis is crucial and this is usually done by an optometrist or ophthalmologist who conducts a physical examination of the affected eye. After examining for signs of infections like swelling, pain and redness, further tests may be recommended. These tests comprise taking a blood sample or a sample of eye discharge. They are then analyzed in the laboratory for finding out what kind of bacteria has been causing the infection. In addition, eye doctors may recommend imaging tests like CT Scans and MRIs to understand how far the infection has spread. Thus, it is evident that preseptal cellulitis is not generally very serious when prompt diagnosis and treatment are done. Antibiotics may help in clearing up the infection quickly. However, in case it is left untreated, preseptal cellulitis can lead to more serious conditions which may also lead to permanent vision problems and even blindness.
0 notes
Text
Know why heart failure in young people has become so common today

Over the years, the incidence of heart failure in young people has increased alarmingly. Heart failure occurs when a person’s heart muscle does not pump blood as effectively as it should. In this case, blood backs up and there is a build-up of fluid in the lungs which gives rise to shortness of breath. Certain inherent heart conditions make the heart stiff and weak to pump blood properly. Such conditions may include high blood pressure and narrowed arteries in the heart. It is important for the youth today to adopt different kinds of lifestyle changes that may help in improving their quality of life. For example, one must manage stress, consume less salt and try to lose some weight.
Common symptoms of heart failure in young people
Shortness of breath while lying down or while undertaking any activity
Weakness and fatigue
Swelling in the ankles, feet and legs
Irregular or rapid heartbeat
Inability to exercise
Wheezing
Cough that brings up pink or white mucus
Swelling in the belly area
Lack of appetite
Nausea
Chest pain
Risk Factors and Causes of Heart Failure in Young People
Some of the most common risk factors and causes of heart failure in young people may be identified as the following:
Excessive alcohol use or substance abuse: Young people who drink heavily develop a high level of inflammation in their bodies. This is linked to diverse health conditions which may include cardiovascular diseases.
Stress: The youth today often face massive stress in their personal and professional lives. Consistent high stress can cause different kinds of heart diseases like heart attack, heart failure, sudden cardiac death and arrhythmia.
Smoking: Smoking has numerous adverse health impacts and heart disease is one of them. It causes different kinds of heart diseases and is one of the common risk factors for heart failure.

High cholesterol and blood pressure levels: It is crucial to monitor and manage blood pressure and cholesterol levels as these may also lead to heart failure in patients. Heart failure in young people can be prevented if they are proactive in monitoring and managing their blood pressure and cholesterol levels.
Sedentary lifestyle: The youth today are often found to lead a sedentary lifestyle without any kind of physical activity. It increases the risks of developing different kinds of heart diseases and also may lead to high blood cholesterol, high blood pressure, obesity and Type 2 diabetes. These conditions make a person more prone to developing heart failure.
A poor diet: A poor diet that lacks nutritional value is another cause that makes a person more prone to developing heart failure. For example, eating a diet that is high in trans fat and saturated fats is linked to heart disease and other related conditions.

Prevention
Prevention of heart failure includes taking proactive steps towards leading a healthier and more active lifestyle. Some of the best ways in which a person can reduce his risk of developing heart failure may include:
Managing stress as much as is possible
Taking effective steps to manage common conditions that increase the risks of heart failure such as obesity, diabetes and high blood pressure
Avoiding consumption of alcohol, tobacco and all kinds of recreational drugs
Moving away from a sedentary lifestyle by exercising regularly and by taking part in different kinds of physical activities
Eating a healthy and nutritious diet that is full of lean protein, vegetables, fruits and whole grains.
#heart failure in young people#causes of heart failure in young people#causes of heart failure#heart failure#heart
1 note
·
View note
Text
Your Thirst for Alcohol Could Push You Towards Oral Cancer, Know How?

Have been ignoring the cancer warning labels on cigarette packs?
Be aware! In your temporary happiness, you are inviting an unwanted and dangerous guest, ‘ORAL CANCER’. Yes, studies have found that alcohol intake coupled with tobacco consumption increases the risk of mouth cancer. One of the studies published in 2016 linked alcohol consumption with four types of oral cancer:
Oesophageal cancer,
Larynx cancer,
Lip and oral cavity cancer and
Pharynx and nasopharynx cancer
At the global level, the incidence of new cases of oral cancer was estimated to be 3,77,713 in 2020. Additionally, 177,757 deaths were also registered due to oral cancer. This cancer is more deadly in men in comparison to women. Along with this, the prevalence of this cancer has been found to strongly vary by socio-economic circumstances. Among all other countries, India contributes to almost one-third of the total burden of the disease and ranks second in having the highest number of oral cancer cases.
Why is India a hot zone for oral cancer?
No part of India is free from oral cancer. The reason behind this is the excessive consumption of tobacco in different forms, alcohol and betel quid. People irrespective of their gender and age group can become prey to this disease. Additionally, Indian men are more at risk than women as per the data retrieved from Figure.

In India, it would be completely wrong to blame only tobacco and alcohol for the rising incidence of oral cancer in the country. Lack of awareness is also a major reason that increases the incidence of diseases. Awareness equips people with the ability to detect any disease at an early stage, which is crucial for the proper diagnosis and treatment of the conditions. Thus, by spreading awareness about oral cancer signs, it will be possible for India to climb down the ladder of oral cancer.
What are the signs of oral cancer?
A lip or mouth sore that takes time to heal.
A lump or thick patch in the mouth, lip, or throat.
A white or red patch in the mouth.
A sore throat
Difficulty moving jaw or tongue
Difficulty chewing, swallowing, or speaking
Numbness either in the tongue or other areas of the mouth.
Swelling in the jaw
Ear pain
It’s not only tobacco but also alcohol responsible for oral cancer, know how?
A decade ago the International Agency for Research on Cancer classified alcohol as a Group 1 carcinogen. One of the crucial components of alcohol is ethanol, which itself is not a carcinogen unlike its first metabolite, acetaldehyde (ACH). A major part of the ethanol is metabolised in the liver by alcohol dehydrogenase. However, when alcohol intake is high then it is catalysed by microsomal cytochrome P450 (CYP2E1). This not only increases acetaldehyde level but produces reactive oxygen species4. Further, this acetaldehyde is converted to a harmless acetate molecule by the enzyme aldehyde dehydrogenase. However, the situation reverses if a point mutation occurs in the enzyme or there is a deficiency of the enzyme. In such a situation, carcinogenic acetaldehyde keeps on accumulating in the cell. Furthermore, oral mucosa can also metabolise alcohol and as it lacks acetaldehyde enzyme, an accumulation of mutagenic ACH takes place in the saliva5. Thus, exposure to carcinogenic ACH is mainly responsible for increasing the risk factor of oral cancer. Henceforth, if an individual observes the sign of alcohol abuse among their friends and relatives, they should take action to lower their alcohol consumption. This will help to protect them from the deadly oral cancer.
Can the risk of oral cancer start from the first drop?
Over the years, scientists have systematically evaluated the risks and harms associated with alcohol. At the commercial level, it is always stated that a certain amount of alcohol is safe for human health, but how much is it true? As per the latest WHO statement, yet there is no evidence of the existence of a specific threshold at which the carcinogenic effect of alcohol switches on or off. So, it is wrong to claim anything about the safe level of alcohol use. Thus, the risk can start even from a single drop. Further, the more an individual drinks, the higher the risk. Thus, rather than debating on how much amount of alcohol is safe, it is vital to encourage the population to get rid of this habit. This will not only help to prevent oral cancer but also many other diseases like CVD, liver-related diseases and others. It would be hard, but abstain from alcohol, especially on observing signs of alcohol abuse! This is the only way by which you won’t experience oral cancer signs.
References
Griswold, M.G., Fullman, N., Hawley, C., Arian, N., Zimsen, S.R., Tymeson, H.D., Venkateswaran, V., Tapp, A.D., Forouzanfar, M.H., Salama, J.S. and Abate, K.H., 2018. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 392(10152), pp.1015-1035.
WHO, 2023. Oral health. Available at: https://www.who.int/news-room/fact-sheets/detail/oral-health#:~:text=The%20global%20incidence%20of%20cancers,strongly%20by%20socio%2Deconomic%20circumstances. (Accessed: 12 April 2023).
Borse, V., Konwar, A.N. and Buragohain, P., 2020. Oral cancer diagnosis and perspectives in India. Sensors International, 1, p.100046.
Ratna, A. and Mandrekar, P., 2017. Alcohol and cancer: mechanisms and therapies. Biomolecules, 7(3), p.61.
Ogden, G.R., 2018. Alcohol and mouth cancer. British dental journal, 225(9), pp.880-883.
#oral cancer across India#oral cancer#oral cancer signs#signs of alcohol#healthcare information#healthcare#health and wellness#healthy lifestyle#cancer
1 note
·
View note