Don't wanna be here? Send us removal request.
Text
What is an Anal Fissure and Its Remedies?

Introduction
Some health problems, such as anal fissures, hurt and interfere with the quality of your life. Tiny cracks in the lining of the anus may lead to stinging pain, bleeding, and soreness. Individuals suffer from this, more specifically, while having a bowel movement. Neglecting the issues can intensify the pain and cause difficulties while sitting or walking. Let us discuss the various remedies that are available to alleviate the pain and cure anal fissures successfully.
What is an Anal Fissure?
An anal fissure is a small tear in the lining of the anus. It causes pain, bleeding, and discomfort, particularly during bowel movements. The tear leaves exposed sensitive nerve endings that cause sharp pain and irritation. When the fissure occurs, the muscles in the anus can tighten, preventing healing.
Acute fissures (of less than six weeks duration) heal more quickly, whereas chronic fissures last longer than six weeks and may need medical intervention. Chronic fissures can become even more painful if left unmanaged and can prolong the healing process.
Are Anal Fissures Common?
Anal fissures are common in children and adults. It can also happen in babies. Some research indicates that one in five individuals have anal fissures during their lifetime.
Anal fissures usually occur because of constipation, straining or passing hard stools.
Dehydration, chronic diarrhoea, and low-fibre diets can also make you predisposed to get frequent anal fissures.
Pregnant women and postpartum women are also at higher risk because the anal area is under pressure.
Individuals with inflammatory bowel disease or reduced blood flow to the rectum also have a higher risk.
What are the Signs of an Anal Fissure?
Anal fissures result in several uncomfortable signs, including:
Pain: Pain may occur during or after a bowel movement and usually lasts minutes to hours.
Bleeding: You may find bright red smears on toilet tissue or in the stool.
Irritation and swelling: The skin may become swollen, sore, or tender.
Visible tear or crack: In some instances, a small cut can be seen around the anus.
Itching or burning: Discomfort can build up when sitting for extended periods.
What Does an Anal Fissure Feel Like?
An anal fissure is a sharp, burning pain that you may experience during and after bowel movements. The pain can persist for minutes or hours, depending on the severity.
Less severe fissures cause transient pain and minor irritation, while bad cases bring intense, persistent pain that worsens with movement or pressure.
Some may have a persistent ache and cannot sit easily. The bare nerve endings in the tear increase sensitivity so that every bowel movement causes pain. The pain may become continuous and unbearable if nothing is done about it or if there is an infection underneath.
Conclusion
Anal fissures hurt, but with proper care, they can heal quickly. Proper fibre intake, hydration, and regular bowel habits prevent straining of the anal muscles to prevent fissures. Sitz baths, topical care, Ayurvedic therapies, comfort symptoms, and surgeries help healing in severe cases. Gentle exercise increases circulation and muscle tone, helping recovery. Strict adherence to anal fissure treatment and lifestyle changes prevents recurrence and keeps the anus healthy in the long run. We encourage you to schedule a consultation for Anal fissure , where we offer personalised, effective care based on your unique needs.
Continue reading here learn more about: Anal Fissures and remedies
0 notes
Text
9 Best Home Remedies to Reduce Constipation by Expert Doctors
Constipation is a common digestive issue affecting millions worldwide, characterised by infrequent bowel movements or difficulty passing stools. At Chirag Global Hospitals, we advocate a holistic approach to digestive health. Below, we present nine powerful, doctor-approved home remedies for constipation relief — designed to be practical, accessible, and effective.
1. Hydration: The First Line of Defence Against Constipation
Adequate water intake is vital for softening stools and maintaining bowel regularity. When the body is dehydrated, the colon absorbs more water from the food waste, resulting in hard, dry stools.
Action Plan:
Drink 2.5 to 3 litres of water daily.
Include warm water with lemon every morning to stimulate digestion.
Add coconut water and herbal teas like chamomile or peppermint to your hydration routine.
2. Fibre-Rich Diet: The Natural Broom for Your Digestive Tract
Fibre adds bulk and softness to stools, promoting smooth bowel movements. There are two types of fibre: soluble (retains water) and insoluble (adds bulk).
Top High-Fibre Foods:
Soluble Fibre: Oats, apples, carrots, flaxseeds, psyllium husk
Insoluble Fibre: Whole wheat bread, brown rice, leafy greens, cucumbers
Aim for 25–30 grams of dietary fibre daily.
3. Prunes and Figs: Natural Laxatives That Work Fast
Prunes and figs are packed with fibre and sorbitol — a natural sugar alcohol that draws water into the intestines.
How to Use:
Soak 5–6 prunes or figs overnight, and consume them in the morning.
Drink the soaking water for added benefit.
They act as a mild laxative without disrupting the gut microbiome.
4. Psyllium Husk (Isabgol): The Ayurvedic Powerhouse for Bowel Regulation
Psyllium is a form of soluble fibre derived from the Plantago ovata plant. It absorbs water in the intestines, swelling and forming a gel-like substance that eases stool passage.
Recommended Dosage:
1–2 teaspoons mixed in warm water or milk, taken at bedtime.
For those with chronic constipation, psyllium is both safe and sustainable.
5. Olive Oil and Castor Oil: Lubricate and Stimulate
Both oils offer unique constipation-relieving benefits:
Olive Oil helps soften the stool naturally.
Castor Oil stimulates the bowel muscles through its active compound, ricinoleic acid.
Usage Guidelines:
Olive Oil: 1 tablespoon on an empty stomach
Castor Oil: 1 teaspoon mixed with warm milk once or twice a week (short-term use only)
6. Regular Physical Activity: Movement Supports Movement
Exercise enhances gut motility by increasing blood flow to the digestive organs.
Best Activities for Constipation Relief:
Brisk walking (20–30 mins/day)
Yoga poses: Pawanmuktasana, Bhujangasana, Malasana
Gentle abdominal massages to stimulate bowel movement
Staying sedentary worsens constipation — move to improve.
7. Probiotic-Rich Foods: Strengthen Your Gut Flora
An imbalanced gut microbiome can lead to sluggish digestion. Probiotics restore healthy bacteria levels in the intestines.
Effective Probiotic Sources:
Curd and yogurt with live cultures
Fermented foods: Sauerkraut, kimchi, kefir
Buttermilk with roasted cumin seeds post-lunch
For chronic cases, consider probiotic supplements after consulting a physician.
8. Herbal Teas and Natural Laxatives
Certain herbs stimulate digestive enzymes and bowel activity.
Most Effective Herbal Remedies:
Senna tea (short-term use only)
Licorice root tea
Triphala churna: 1 teaspoon at bedtime with warm water
These traditional remedies are clinically supported and widely used in integrative medicine.
9. Establish a Toilet Routine: Train Your Bowel
Ignoring the urge to pass stools weakens the natural reflex over time. Consistency is key.
How to Build a Healthy Routine:
Sit on the toilet at the same time every morning, preferably after waking.
Elevate your feet using a small stool (mimics a squatting position).
Avoid straining — take your time and breathe deeply.
At Chirag Global Hospitals, we have developed a comprehensive approach that involves providing the Best Constipation Treatment in Bangalore, exclusively. After a detailed analysis of the patient’s condition, we undertake a suitable procedure to aid the medical problem.
Continue reading to know more: Home remedies for Constipation
0 notes
Text
Effective Home Remedies to Prevent and Manage Anal Fissures
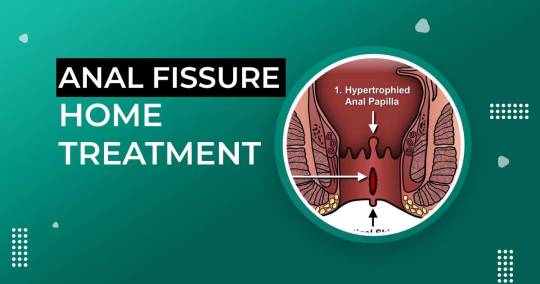
Anal fissures are small tears in the lining of the anus that can cause pain, discomfort, and bleeding during bowel movements. While medical treatments are available, natural remedies can play a crucial role in preventing and managing fissures. By making simple lifestyle and dietary changes, you can reduce the risk of developing anal fissures and promote faster healing. Below are the best home remedies to prevent and relieve fissures effectively.
1. Stay Hydrated to Keep Stools Soft
Drinking plenty of fluids is essential for maintaining soft stools and preventing constipation, one of the leading causes of anal fissures. Hard stools can cause strain during bowel movements, increasing the risk of developing fissures. Aim to drink at least 8–10 glasses of water daily, and consider hydrating with natural fruit juices and herbal teas to support digestion.
2. Increase Dietary Fiber Intake
A high-fiber diet can help regulate bowel movements and prevent constipation. Fiber adds bulk to stools, making them easier to pass. Foods rich in fiber include:
Whole grains (oats, brown rice, quinoa)
Fresh fruits (apples, pears, oranges)
Vegetables (broccoli, carrots, spinach)
Legumes (lentils, beans, chickpeas)
Health experts recommend consuming at least 25–30 grams of fiber daily. Gradually increasing fiber intake can prevent bloating and discomfort while improving digestive health.
3. Take Warm Baths (Sitz Baths) for Relief
Soaking in a warm bath for 15–20 minutes, especially after bowel movements, can help relax the anal muscles and promote healing. Warm water improves blood circulation in the affected area, reducing pain, irritation, and inflammation. Adding Epsom salt to the water can provide additional soothing effects.
4. Use Natural Stool Softeners or Mild Laxatives
If you experience frequent constipation, using a stool softener can help ease bowel movements. Natural options like psyllium husk, flaxseeds, and prunes can act as gentle laxatives. Over-the-counter stool softeners should only be used after consulting a doctor to avoid dependency.
5. Avoid Straining During Bowel Movements
Straining while passing stools can put excessive pressure on the anal canal, worsening existing fissures or creating new ones. To prevent straining:
Establish a regular bowel routine
Avoid delaying the urge to pass stools
Use a small footstool to elevate your feet while sitting on the toilet, mimicking a natural squatting position
Practicing these habits can reduce pressure on the anal region and support smooth bowel movements.
6. Apply Soothing Ointments and Natural Remedies
Topical creams and ointments with ingredients like aloe vera, coconut oil, or petroleum jelly can provide relief by keeping the affected area moisturized and reducing irritation. Some over-the-counter creams contain lidocaine for pain relief, but always consult a healthcare professional before using any medication.
7. Avoid Spicy and Acidic Foods
Certain foods can irritate the anal region and worsen discomfort associated with fissures. To prevent irritation:
Limit spicy foods, hot peppers, and curries
Reduce intake of acidic foods like citrus fruits and tomatoes
Avoid processed foods high in artificial additives
Opting for a balanced diet rich in fiber and healthy fats can improve digestion and prevent aggravation of anal fissures.
8. Exercise Regularly for Better Digestion
Physical activity helps stimulate bowel movements and reduces the risk of constipation. Engaging in at least 30 minutes of moderate exercise, such as walking, yoga, or swimming, can promote healthy digestion. Yoga poses that support gut health, such as child’s pose and seated twists, may also be beneficial.
9. Maintain Proper Hygiene to Prevent Infection
Keeping the anal area clean and dry is crucial in preventing infections and further irritation. Use soft, unscented toilet paper or cleansing wipes instead of harsh soaps. After a bowel movement, gently clean the area with lukewarm water and pat it dry instead of rubbing.
10. Consider Herbal Remedies for Healing
Certain natural remedies have anti-inflammatory and healing properties that can aid in fissure recovery. Some effective options include:
Aloe Vera Gel: Helps soothe irritation and promotes tissue healing.
Coconut Oil: Acts as a natural lubricant and has antimicrobial properties.
Witch Hazel: Reduces swelling and relieves itching.
Turmeric Paste: Contains curcumin, which has anti-inflammatory effects.
Applying these natural remedies regularly can speed up the healing process and reduce discomfort.
11. Follow a Regular Bowel Routine
Establishing a consistent bowel routine can help prevent constipation and reduce the risk of fissures. Try to use the bathroom at the same time each day and avoid holding in stools for long periods. This habit trains your body to pass stools more efficiently.
12. When to Seek Medical Attention
While home remedies can be highly effective, some cases require medical intervention. Seek professional advice if:
The fissure does not heal within 6 weeks
You experience severe pain, bleeding, or infection
Symptoms persist despite lifestyle changes
Early medical evaluation can prevent complications and ensure proper treatment.
Conclusion
Preventing and managing anal fissures naturally involves a combination of hydration, a high-fiber diet, good hygiene, and lifestyle modifications. By following these home remedies, you can significantly reduce the risk of fissures and promote faster healing. However, if symptoms persist or worsen, consulting a healthcare professional is crucial for further treatment.
At Chirag Global Hospitals, we offer specialized treatment for fissures and other anorectal conditions. Our expert team is dedicated to providing comprehensive care and effective solutions. Contact us today to learn more about how we can help you achieve optimal digestive health.
Continue reading here: Home remedies to prevent fissures
0 notes
Text
Effective Ways to Manage and Heal Anal Fissures

Anal fissures are a common yet painful condition caused by a small tear or cut in the anal lining. This condition can result in discomfort, itching, bleeding, and severe pain during bowel movements. While anal fissures can be distressing, adopting the right habits can significantly ease symptoms and promote healing. This guide outlines the best practices to relieve pain, support healing, and prevent recurrence.
Chirag Global Hospitals is a renowned hospital that offers anal fissures treatment for a range of medical conditions, including anal fissures. Our team of experienced professionals uses the latest techniques and technologies to diagnose and treat anal fissures effectively.
Essential Do’s for Healing Anal Fissures
1. Stay Hydrated
Drinking sufficient water keeps stools soft, reducing the strain on the anal area. Health professionals recommend consuming at least 6–8 glasses of water daily to prevent constipation and promote smooth bowel movements.
2. Follow a High-Fiber Diet
Fiber-rich foods, including fruits, vegetables, whole grains, and legumes, help regulate digestion and soften stools. A diet high in fiber minimizes straining during bowel movements, allowing anal fissures to heal faster.
3. Take Sitz Baths
Soaking the anal area in warm water for 10–15 minutes multiple times a day can provide relief from pain and inflammation. Sitz baths improve circulation, relax the anal muscles, and accelerate the healing process.
4. Maintain Proper Hygiene
Keeping the anal area clean and dry is essential to prevent infections and promote healing. After each bowel movement, gently cleanse the area with warm water and unscented soap. Avoid harsh chemical-based or perfumed products, as they can cause irritation.
5. Use Lubrication
Applying a water-based lubricant before bowel movements can minimize friction, making the process less painful. This practice prevents further damage to the delicate anal tissue.
6. Take Over-the-Counter Medications
Pain relievers such as ibuprofen and acetaminophen help manage discomfort and reduce inflammation. Additionally, using topical ointments recommended by a healthcare provider can accelerate healing.
7. Seek Medical Attention When Necessary
If symptoms persist or worsen despite home remedies, consulting a doctor is crucial. Severe anal fissures may require medical intervention, including prescription medications or minor surgical procedures to facilitate healing.
Critical Don’ts to Avoid Further Complications
1. Avoid Straining During Bowel Movements
Forcing bowel movements can worsen an existing fissure and prolong the healing process. To prevent this, consume fiber-rich foods, stay hydrated, and establish a regular bowel routine.
2. Steer Clear of Spicy and Acidic Foods
Foods high in spice and acidity can irritate the anal area, leading to increased pain and discomfort. Avoiding such foods while recovering from an anal fissure is essential for faster healing.
3. Do Not Use Harsh Cleansing Products
Soaps or personal care products containing alcohol, fragrance, or strong chemicals can aggravate the sensitive anal area. Stick to mild, fragrance-free cleansing solutions to maintain hygiene without irritation.
4. Avoid Holding in Bowel Movements
Delaying bowel movements can lead to constipation, which hardens stools and increases the risk of further tearing. It is important to listen to your body’s natural urges and pass stools regularly.
5. Stop Using Rough Tissue Paper
Dry toilet paper can cause irritation and discomfort. Instead, opt for soft, unscented baby wipes or rinse the area with warm water to maintain cleanliness while avoiding further injury.
6. Reduce Prolonged Sitting
Sitting for extended periods exerts unnecessary pressure on the anal region, leading to discomfort and slower healing. Take breaks, walk around periodically, or use a cushioned seat to reduce strain.
Conclusion
Healing anal fissures requires a combination of proper diet, hydration, hygiene, and lifestyle adjustments. By following these dos and don’ts, individuals can minimize pain, encourage healing, and prevent future occurrences.
At Chirag Global Hospitals our team of specialists offers advanced treatments for anal fissures and related conditions. Using the latest medical techniques, we ensure effective diagnosis and personalized treatment plans for optimal recovery.
If you or someone you know is struggling with persistent anal fissures, seeking expert medical care can lead to faster and lasting relief.
Continue reading here: Do’s and Dont’s While Managing Anal Fissures
0 notes
Text
Ten Best Home Remedies to Provide Relief from Piles During Pregnancy

Piles during pregnancy is a common problem that can cause considerable discomfort and distress. The extra weight and pressure on the abdomen can cause veins in the anus and rectum to swell. Fortunately, some simple home remedies can help relieve the symptoms of piles in pregnancy.
As explained by Piles treatment experts at Chirag Global Hospitals, one of the best piles treatment hospitals in Bangalore, here are the 10 best home remedies to reduce piles pregnancy:
1. Drink plenty of water
Drinking lots of water is essential for keeping your body hydrated and helps to reduce the risk of developing piles. This is especially important during pregnancy when your body needs more water to support the growing baby.
2. Eat a high-fiber diet
Eating foods high in fiber can help keep your digestive system regular and reduce constipation, one of the leading causes of piles. Foods like oats and whole grains, fruits, vegetables, beans, and legumes are all good sources of fiber.
3. Exercise regularly
Regular exercise helps to promote regular movement in the bowels, which can help reduce constipation and associated symptoms of piles. Aim for 30 minutes of moderate physical activity each day, such as walking or swimming.
4. Avoid lifting heavy objects
Heavy lifting can strain your abdomen, aggravating piles. Avoid lifting heavy items and use the correct techniques to reduce the risk of straining your body. Also, avoid standing or sitting in one position for too long.
5. Use a supportive pillow
Lying down with a supportive pillow under your bottom can help relieve piles by keeping your rectum and perineum elevated. This helps reduce the pressure on the area, providing temporary relief.
Following these above simple home remedies and taking necessary precautions can help reduce the risk of developing piles during pregnancy and relieve the associated discomfort. We are committed to providing comprehensive and compassionate care for pregnant women suffering from piles at Chirag Global Hospitals.
Our experienced team of medical professionals can provide you with the support, advice, and treatments you need to manage your symptoms effectively. Contact us today to find out more about how we can help you.
Continue reading here to know more: Home Remedies to Provide Relief from Piles during Pregnancy
0 notes
Text
Top High-Fibre Foods to Relieve Constipation

High-fibre foods for constipation are essential in our quest for healthier living. Do you know? According to an Indian survey, nearly 22% of India’s adult population suffers from constipation, and Kolkata tops the charts with 28%.
A common digestive problem that can interfere with day-to-day living is constipation, which can be effectively relieved by including certain foods in your diet, along with sufficient fluid intake with the food.
Since maintaining digestive health is essential, we at Chirag Global Hospitals have compiled a thorough list of the top high-fibre foods for constipation.
Commonly Available High-Fibre Foods for Constipation Relief
Horse Gram:
Horse gram, a lesser-known but highly nutritious legume, is rich in fibre, which makes it an excellent choice for aiding digestion. A single serving can provide a significant portion of the daily recommended fibre intake.
This legume bulks up stool and promotes smoother bowel movements, reducing the symptoms of constipation. To incorporate horse gram into your diet, consider adding it to soups or salads or cooking it as a side dish seasoned with herbs and spices.
Ragi:
Ragi, or finger millet, is another fantastic source of dietary fibre. Available primarily in malt or porridge, ragi can be a soothing, fibrous addition to any diet. Regular consumption helps maintain digestive health and prevent constipation.
Ragi porridge for breakfast can kickstart the digestive process for the day, while ragi malt is a refreshing, nutritious drink to include in your diet.
Incorporate Ghee in a Regular Diet:
While ghee is a form of fat, it also aids digestion. Adding a moderate amount of ghee to a regular diet can help lubricate the intestines and facilitate the easier passage of stools.
This can be particularly beneficial for those suffering from constipation. Ghee can be added to hot cooked dishes or even to warm beverages like milk to enhance absorption and ease constipation.
Barley:
Barley is a wholesome grain packed with soluble and insoluble fibre, making it an excellent choice for digestive health. It helps with regular bowel movement and balances the gut flora, supporting overall gastrointestinal health.
Barley can be enjoyed in many forms, from barley water, a popular digestive aid, to being incorporated into bread, soups, and stews.
Whole Wheat:
Whole wheat is superior to refined grains because it retains all parts of the grain kernel, including the fibre-rich bran. Regular intake of whole wheat products can significantly improve bowel regularity and prevent constipation.
For a simple dietary shift, substitute white bread and pasta with whole wheat alternatives to increase your fibre intake effortlessly.
Karjura (Dates):
Dates are not only delicious but also a rich source of fibre. They contain soluble and insoluble fibre, which helps draw water into the digestive tract and promotes quicker bowel movements.
Dates can be eaten alone, added to dairy products like yoghurt, or used in baking to add natural sweetness and digestive benefits.
Grapes:
Grapes are a juicy fruit with a high water and fibre content, making them ideal for preventing and alleviating constipation. The skin of grapes contains insoluble fibre, which adds bulk to stool and speeds up its passage through the intestines.
Eating a small bowl of grapes often can contribute to a healthy digestive system and prevent the discomfort of constipation.
Milk:
While milk is not high in fibre, it can be part of a balanced diet to prevent constipation when combined with other fibre-rich foods. It is an excellent source of vitamins, proteins, and minerals, particularly calcium.
Some people find that warm milk can help stimulate bowel movements, although this can vary from person to person. It’s essential to monitor how your body responds to milk in your diet and adjust accordingly.
High-Fibre Fruits For Constipation Relief
Some fruits that can soften tools are:
Apples:
The timeworn slogan, “An apple a day keeps the doctor away,” still fits, especially when dealing with constipation. Apples are high in fibre, including pectin (a soluble fibre that aids bowel regularity). This is why they are great at softening tools, eventually leading to bowel movements. In addition, apples include pure sugars, including fructose, that can assist the digestive function by acting as a mild laxative.
How To Eat: Slice apples and have them as a snack, or add them to your salad.
Papayas:
Thanks to their high water and fibre levels, papayas are already popular as one of the best fruits for overall digestion. They are an excellent option for supporting gut wellness and reducing constipation because they are nutritious, sweet, and a great source of fibre, vitamins, and minerals.
How To Eat: Slice them and eat them raw. Or, if you want a bit of variety, grill them, add yoghurt, and sprinkle some cinnamon powder on them for a tasty dessert.
Conclusion
Constipation need not be a roadblock to your well-being. Adopting effective home remedies and seeking constipation treatment at Chirag Global Hospital can unlock relief and regain control over your digestive health. Incorporate high-fibre foods in your diet for constipation.
Don’t let constipation hinder your daily life — take proactive steps toward a comfortable and fulfilling lifestyle today! Book an appointment today for your ongoing constipation stress at Chirag Hospitals.
Continue reading here: High Fibre Food for Consitipation Relief
0 notes
Text
Best Exercises for People With Fissures

Anal fissures are small tears in the lining of the anus, often resulting from passing hard or large stools, leading to pain and discomfort during bowel movements. Incorporating specific exercises into your routine can aid in healing and prevent recurrence by strengthening the pelvic floor and surrounding muscles, improving blood flow, and promoting regular bowel movements. Here are seven effective exercises for individuals dealing with anal fissures. Fissures are a common type of anal disorder that can cause serious discomfort and even pain. Fortunately, many exercises can help alleviate the symptoms and reduce the chances of getting them in the future. Here’s a look at nine of the best exercises for people with fissures.
1. Kegel Exercises
Kegel exercises focus on strengthening the pelvic floor muscles, which support the rectum and help maintain proper bowel function. Strong pelvic floor muscles can reduce strain during bowel movements, facilitating fissure healing.
How to Perform Kegel Exercises:
Identify your pelvic floor muscles by attempting to stop the flow of urine midstream; the muscles engaged are your pelvic floor muscles.
Once identified, contract these muscles for five seconds, then relax for five seconds.
Repeat this process 10–15 times per session, aiming for at least three sessions daily.
Kegel exercises can be performed while sitting, standing, or lying down, making them versatile and easy to incorporate into your daily routine.
2. Squats
Squats strengthen the lower body muscles, including the glutes and thighs, which support pelvic stability and reduce pressure on the anal region.
How to Perform Squats:
Stand with your feet shoulder-width apart.
Lower your body by bending your knees and pushing your hips back as if sitting in a chair.
Keep your back straight and knees aligned with your toes.
Descend until your thighs are parallel to the ground, then rise back to the starting position.
Aim for two sets of 10 repetitions daily.
Proper form is crucial to prevent injury and maximize benefits.
3. Glute Bridges
Glute bridges target the gluteal muscles and lower back, enhancing support for the pelvic region and alleviating strain on the anal sphincter.
How to Perform Glute Bridges:
Lie on your back with knees bent and feet flat on the floor, hip-width apart.
Place your arms at your sides with palms facing down.
Tighten your abdominal and gluteal muscles, then lift your hips toward the ceiling, forming a straight line from shoulders to knees.
Hold this position for a few seconds before slowly lowering your hips back to the floor.
Perform two sets of 10–15 repetitions daily.
This exercise not only strengthens the glutes but also promotes flexibility in the hip area, contributing to overall pelvic health.
4. Lunges
Lunges improve lower body strength and flexibility, aiding in reducing pressure on the anal region during daily activities.
How to Perform Lunges:
Stand upright with feet hip-width apart.
Step forward with one leg, lowering your hips until both knees are bent at approximately 90-degree angles.
Ensure your front knee is directly above your ankle, and your back knee hovers just above the ground.
Push through the heel of your front foot to return to the starting position.
Repeat on the other leg, aiming for 10 repetitions per leg.
Incorporate two sets of lunges into your daily routine to enhance muscle support around the pelvic area.
5. Hip Extensions
Hip extensions strengthen the hip and lower back muscles, contributing to better support for the anal region and reducing discomfort associated with fissures.
How to Perform Hip Extensions:
Begin on all fours, with hands directly under shoulders and knees under hips.
Keeping your knee bent, lift one leg upward until your thigh is parallel to the floor.
Hold for a moment, then lower the leg back to the starting position.
Perform 10–15 repetitions on each leg, aiming for two sets daily.
This exercise enhances hip mobility and strengthens the muscles supporting the pelvic floor.
6. Clamshells
Clamshells target the hip abductors and gluteal muscles, which play a role in maintaining pelvic stability and reducing anal sphincter strain.
How to Perform Clamshells:
Lie on your side with your legs stacked and knees bent at a 90-degree angle.
Keep your feet together and your head resting on your lower arm.
Engage your core muscles, then lift your top knee as high as possible without shifting your hips or pelvis.
Hold for a few seconds, then lower the knee back down.
Repeat 10–15 times on each side, aiming for two sets daily.
Clamshells improve hip strength and flexibility, aiding in the prevention of fissure aggravation.
7. Low Back Extensions
Strengthening the lower back supports proper posture and reduces undue pressure on the anal region, facilitating fissure healing.
How to Perform Low Back Extensions:
Lie face down on the floor with arms extended alongside your body, palms down.
Engage your back muscles to lift your chest off the ground, keeping your neck neutral.
Hold for a few seconds, then lower back
For more information, visit us at Chirag Global Hospitals. We understand the importance of staying active and healthy, which is why we offer a variety of treatments and therapies to help patients manage anal fissures. Our team of highly qualified medical professionals is available to answer any questions about treatment options or lifestyle changes that can help prevent fissures. Call us today to learn more!
Continue reading here to know more: Exercises for People with Anal Fissures
0 notes
Text
Fruits that help to treat piles

Piles, also known as hemorrhoids, is a condition in which the veins in the anus and lower rectum become swollen and inflamed. It is a common condition that affects people of all ages and can cause discomfort, pain, and itching.
While many medical treatments are available for piles, incorporating certain fruits into your diet can also help treat this condition. This article will discuss the 9 best fruits that can help treat piles.
1. Apples
Apples are an excellent fibre source and help promote regular bowel movements. They contain both soluble and insoluble fibre, which can help to soften stools and prevent constipation. Constipation is a common cause of piles, and consuming apples can help to prevent and treat this condition.
Why It Helps:
Packed with pectin, which aids in stool formation.
Contains insoluble fibre that promotes bowel regularity.
Helps maintain hydration levels in stools for easy passage.
How to Eat:
Eat one whole apple with skin daily.
Add sliced apples to yogurt or oatmeal for extra gut-friendly benefits.
Drink homemade apple juice (without sugar) for a soothing effect.
2. Pears
Pears are another fruit that is high in fiber and can help to prevent constipation. They also contain pectin, which is a type of soluble fibre that can help to reduce inflammation and promote healing in the digestive tract.
Why It Helps:
One pear contains 6 grams of fiber, making it one of the best fruits for digestion.
Helps maintain bowel movement regularity.
Hydrating effect soothes irritated veins.
How to Eat:
Eat one pear daily with the skin on.
Blend into a smoothie with oats for extra fiber.
Make a warm pear compote as a dessert.
3. Bananas
Bananas are rich in fiber and can help to regulate bowel movements. They also contain potassium, which can help to reduce swelling and inflammation in the body. This makes them an excellent fruit for treating piles.
Why It Helps:
High in soluble fiber, which softens stools and prevents constipation.
Contains pectin, which regulates digestion and improves gut health.
Rich in potassium, reducing inflammation in rectal veins.
How to Eat:
Consume one ripe banana daily in the morning on an empty stomach.
Blend into smoothies with curd for a probiotic boost.
Avoid overripe bananas as they may cause bloating.
4. Berries
Berries, such as strawberries, blueberries, and raspberries, are rich in antioxidants and can help to reduce inflammation in the body. They are also high in fiber, which can help to promote regular bowel movements and prevent constipation.
Why They Help:
Strawberries, blueberries, blackberries, and raspberries are packed with fiber and antioxidants.
Rich in anthocyanins, which promote vein health and reduce inflammation.
Contains water and natural sugars to ease digestion.
How to Eat:
Add a handful of mixed berries to oatmeal or smoothies.
Eat them raw as snacks.
Make a berry yogurt parfait with flaxseeds for extra fiber.
5. Kiwi
Kiwi is a tropical fruit that is rich in fiber and can help to promote healthy digestion. It also contains enzymes that can help to break down food and prevent constipation. Kiwi is also rich in vitamin C, which can help to reduce inflammation and boost the immune system.
6. Prunes
Prunes, also known as dried plums, are an excellent source of fiber and can help to prevent constipation. They also contain sorbitol, which is a natural laxative that can help to soften stools and promote bowel movements.
Expert Care for Piles at Chirag Global Hospital
Incorporating these fruits into your diet can significantly ease piles of symptoms. However, for severe cases, professional medical care may be necessary. At Chirag Global Hospital, recognized as one of the best piles treatment hospitals in Bangalore, we offer advanced facilities and expert care for managing piles.
Our team of experienced doctors provides personalized treatment plans, ensuring patient comfort and recovery. With a commitment to excellence, we aim to deliver high-quality care and effective solutions for piles treatment.
Take the first step towards relief today. Consult our specialists and experience world-class care tailored to your needs.
Continue reading to know more about: Fruits That Help Treat Piles
0 notes
Text
What is Colon Cancer?

Colon cancer also referred to as colorectal cancer, is one of the most common cancer types worldwide. Recent research shows rising incidence rates of colon cancer across all age brackets, though the condition primarily gets detected in people between 65 and 74 years old. The pattern of colon cancer occurs most commonly in Western countries. Still, in India, people get rectal cancer more often, and this disease affects men to a higher degree than women.
The starting point of colorectal cancer occurs in the mucosa layer of the colon or rectum and spreads across various tissue levels. The severity of tissue penetration by the cancerous cells determines which stage of cancer a person has. Routine screening detection helps improve treatment success rates.
What are the Symptoms of Colon Cancer?
Colon cancer remains undetectable during its first stages. People with progressive disease typically encounter different health issues that include:
Persistent Changes in Bowel Habits: Pinkish-red or dark black stools signal internal bleeding. Bowel habits may become consistently loose or constipated, leading to a feeling of incomplete bowel emptying, known as tenesmus.
Blood in Stool: Bright red blood or dark, tarry stools are indicators of internal bleeding.
Anaemia: The condition results in reduced red blood cells from internal bleeding, which produces fatigue and dizziness and leads to pale skin appearance.
Unexplained Weight Loss: Losing weight without dietary or activity changes.
Loss of Appetite: Reduced hunger due to metabolic changes, digestive obstructions, or systemic inflammatory effects.
Fatigue: Persistent tiredness despite adequate rest.
Advanced Stage Symptoms: Abdominal pain, distension, severe constipation (obstipation), and abnormal connections between the colon and other organs (colovaginal or colovesical fistulae).
According to a study, rectal bleeding (37%), abdominal pain (34%), and anaemia (23%) were the most often occurring symptoms triggering diagnostic colonoscopies.
What are the Causes of Colon Cancer?
A combination of several risk elements leads to colon cancer formation, including:
Genetics: A family history of colorectal cancer or inherited syndromes such as Familial Adenomatous Polyposis (FAP) and Lynch syndrome increases the risk.
Lifestyle Factors: A combination of unhealthy eating habits, a sedentary life, smoking, and heavy alcohol use together raise the potential for colon cancer development.
Inflammatory Bowel Diseases (IBD): Conditions such as Crohn’s disease and ulcerative colitis cause chronic inflammation, increasing susceptibility to colon cancer.
Age: Routine screenings become essential for middle-aged people and those older than 50 years since they experience higher risks of developing colon cancer.
Environmental Factors: Exposure to toxins alongside environmental pollutants plays a part in developing colorectal cancer.
Mutations in DNA: When DNA undergoes mutations, the cells start uncontrollable growth, which forms malignant tumours.
Risk Factors for Colon Cancer
Older Age: Most colorectal cancer diagnoses occur in people fifty and above, although such cancers may emerge in any age period.
African-American Descent: Evidence shows that African-American people face an increased probability of developing colorectal cancer.
History of Colorectal Cancer or Polyps: People who have experienced colorectal cancer or polyps before have greater chances of getting a recurrence of the disease.
Inflammatory Bowel Disease: It represents one set of chronic conditions, which includes ulcerative colitis and Crohn’s disease.
Diet Low in Vegetables: Eating small amounts of vegetables increases colon cancer risks because such diets lack fibre.
Lack of Physical Activity: Regular physical exercise reduces the chances of developing cancer, thus lowering the risk.
Obesity, Smoking, and Alcohol Consumption: Studies reveal that obesity, together with smoking and alcohol consumption, consistently increases the risk for colorectal cancer development.
Radiation Therapy for Previous Cancer: Any previous cancer treatment with radiation makes the body more vulnerable to developing colorectal cancer.
How is Colon Cancer Diagnosed?
The early discovery of colon cancer leads to better treatment efficiency. Diagnostic methods include:
Screening Tests: Regular colonoscopy examinations and faecal occult blood tests (FOBT) identify developing abnormalities before symptoms emerge.
Colonoscopy: A colonoscopy enables a detailed examination of the colon and biopsy procedures to remove any detected polyps.
Imaging Tests: CT scans, alongside MRI and PET scans, provide medical experts with data on disease extent.
Treatment for Colon Cancer at Chirag Global Hospital
Doctors at Chirag Global Hospital determine colon cancer treatment based on the stage of the disease. They assess the tumour’s size, depth of invasion into the colon, and whether it has spread to other organs. These treatments primarily include:
Surgery: Tumour removal is the base treatment method for early-stage cancer patients.
Radiation Therapy: Targeted radiation minimises damage to surrounding healthy tissues while destroying cancer cells.
Chemotherapy: The medical treatment of chemotherapy functions for both advanced cancers and after surgery to eliminate any leftover cancer cells.
Hormonal and Biological Therapy: Treatment approaches in hormonal and biological therapy block cancer expansion signals by applying precision medicine techniques.
Local Ablative Therapy: Non-surgical methods such as radiofrequency ablation to destroy cancer cells.
Combination Therapy: The treatment approach for some cases involves surgical procedures, chemotherapy, and radiation therapy.
Conclusion
Colon cancer is a serious but preventable disease. People who have colorectal cancer can trust Chirag Global Hospital to provide them with expert medical care and cutting edge treatment choices. Your effort to include healthy behaviours in regular activities lowers your cancer risk and improves your long-term health.
Chirag Global Hospital is dedicated to giving colon cancer patients the best treatments possible by combining new ideas, careful planning, and caring support to give patients hope. The immediate medical evaluation of ongoing symptoms will help prevent serious medical outcomes. Active healthcare combined with early diagnosis work together greatly to stop the development of colon cancer.
Continue reading here: Colon Cancer
0 notes
Text
What is Kshara Sutra and Kshara Karma Therapy

Ayurveda, the ancient Indian system of medicine, offers a wide range of treatments for chronic diseases. Among Ayurvedic treatment procedures, Kshara Karma and Kshara Sutra therapy demonstrate excellence as minimally invasive therapies for treating anorectal conditions mainly involving haemorrhoids along with fistula-in-ano and fissures. These treatments are valued because they offer minimally invasive delivery, low recurrence risks, and affordable cost.
This article, backed by scientific studies, explores the principles, types, benefits, and applications of Kshara Karma and Kshara Sutra therapy.
What is Kshara Karma?
The Ayurvedic procedure Kshara Karma applies medicinal plant-derived alkaline extracts called Kshara to affected tissue areas for tissue incision, tissue excision, and tissue scraping.
Medical experts have proven that Kshara Karma is an effective treatment option for resolving both haemorrhoids and fistula-in-ano conditions.
The basic nature of Kshara helps control tissue breakdown, decreasing bleeding risks and infectious complications.
There are many medicinal plants from which Kshara is prepared. Based on various parameters of the disease and the patient, the plant is selected. The medicinal properties of tissue removal and healing make Apamarga (Achyranthes aspera) Kshara one of the most popular Ksharas used in the treatment.
Conditions and Diseases that Can be Treated with Kshara Karma Therapy
Ayurvedic doctors apply Kshara Karma therapy extensively to treat different medical cases, especially those affecting anorectal and dermatological disorders.
Haemorrhoids (Arsha): Kshara helps reduce haemorrhoidal tissue while stopping the recurrence of haemorrhoids (Arsha).
Fistula-in-Ano (Bhagandara): Kshara treatment for bhagandara (fistula-in-ano) usually involves kshara sutra (thread coated with kshara), where the unhealthy lining of the tract of the fistula is eroded, and healthy tissue growth is encouraged. This achieves better outcomes and minimal risk of recurrence.
Cervical Erosion (Karnini): Professionals demonstrate that Kshara therapy treats cervical erosion by supporting tissue healing in affected areas.
Nasal Polyps & Turbinate Hypertrophy: The treatment helps decrease abnormal nasal tissue growths, enhancing both nasal passage airflow and respiratory function.
Advantages of Kshara Therapy
Kshara therapy presents a multitude of benefits that turn it into a workable surgical substitute for standard surgical treatments.
Minimally invasive: This therapy involves minimal invasive major surgical procedures; thus, patients can expect quick healing.
Low recurrence rates: Based on many clinical investigations, Kshara therapy successfully minimises the return of fistula-in-ano.
Versatile application: Used for anorectal disorders, skin lesions, and nasal obstructions.
Types of Kshara Karma
Kshara Karma contains different applications that treat separate conditions effectively.
Pratisaraneeya Kshara (Topical Application)
The direct application of Kshara leads to controlled chemical cauterisation when used to treat affected tissues.
The remedy treats haemorrhoids, warts, and fistula and addresses cervical erosion.
The neutralising agent lemon juice protects tissues from excessive damage when used after Kshara’s application.
Shrinking tissues occur rapidly while healing occurs quickly, thus minimising pain experienced after the procedure.
It is one of the important treatments in non-healing wounds, where the unhealthy tissues are chemically cauterised, thereby making way for healthy tissue growth with proper post op care.
Chiraayu — a pioneering Ayurvedic wing dedicated exclusively to Proctology and digestive issues. This innovative integration of traditional wisdom of Ayurveda and Yoga, with modern allopathic expertise marks a significant milestone in our journey to provide comprehensive and holistic healthcare.
Conclusion
The Ayurvedic treatments Kshara Karma and Kshara Sutra provide successful minimally invasive procedures for treating systemic and anorectal medical conditions. Modern surgical procedures have a strong competing alternative in these treatments due to proven scientific results, reduced side effects, and cost-effectiveness.
Numerous studies report that these Ayurvedic procedures achieve high success rates by treating haemorrhoids, fistula-in-ano, and other conditions, leading to low recurrence rates. Due to increasing global awareness regarding Ayurvedic medicine, both treatments continue to establish themselves as safe, approachable therapeutic methods. Receiving Kshara-surgery treatment requires medical consultation with an Ayurvedic professional with proper qualifications.
Continue reading here to know more: Kshara Sutra and Kshara Karma Therapy
0 notes
Text
How Can Ayurveda Help to Manage Digestive Problems?

Ayurveda is an ancient form of medicine that focuses on a holistic approach to health. It talks about balancing body, mind, and spirit toward good health. In Ayurveda, health is not just about the absence of disease. Rather, it is about maintaining a balance of energy in the body (vata, pitta, and kapha). Everyone differs with respect to the physical makeup of the body, the condition of the patient’s mind, and their environment. So, the Ayurvedic approach ensures healing tailored to each person’s needs for long-term health and vitality. Let’s understand how it can help with managing digestive problems.
Understanding Ayurveda and Digestive Health
In Ayurveda, digestion is the core of health. The idea of Agni, or digestive fire, is a crucial part of this concept. Agni represents a person’s ability to digest, absorb, and assimilate food. A strong Agni signifies good digestion and absorption, while a weak Agni leads to indigestion and other digestive problems. A well-balanced digestive fire maintains overall energy and metabolism. Therefore, it is important to maintain strong Agni so that the body can digest food well and eliminate waste.
What Causes Digestive Problems?
Digestive problems are caused by many factors, like diet, stress, and lifestyle. A diet full of processed foods, sugar, and fried items messes up the body’s digestive system. Irregular eating habits or eating late at night can adversely affect the body’s digestive system. Stress also plays a significant role in affecting digestion. When the body is stressed, it goes into survival mode, and it takes precedence over digestion. Therefore, it results in bloating, indigestion, and acid reflux. Lack of physical activity or sleep and excessive sitting can easily make digestion unresponsive and low.
Environmental factors and emotions also affect digestion. Changes in seasons, weather, and even the air condition all affect doshas, which alter the function of the digestive system. Stress and anxiety are major factors causing emotional imbalances, leading to problems such as IBS or heartburn. Emotion balance, through meditation or mindfulness, can benefit digestion and overall health.
Dosha Imbalance
The three doshas — Vata, Pitta, and Kapha are the basic energies that run the body’s functions, such as digestion. Each dosha influences digestion differently. Ayurvedic digestive health focuses on ensuring a balance of these doshas:
Vata: This dosha governs the movement in the body and the movement of the food inside the digestive tract. Imbalance in Vata causes a disturbance in digestive functioning, and there can be irregular digestion, bloating, and constipation.
Pitta: It controls the digestion and metabolism. It determines the heat as well as the enzymes that break the food. Excess Pitta can lead to acidity, heartburn, or inflammation in the digestive system.
Kapha: Kapha is a force related to structure and lubrication. Kapha protects the integrity of the digestive organs. When Kapha is excessive, there is slow digestion, weight gain, and excessive mucus production.
Herbal and Dietary Interventions
Ayurveda for gut health employs numerous herbs and dietary practices. Herbs, including ginger, cumin, fennel, and Triphala, enhance Agni’s fire, support digestion, and treat common digestive issues. Dietary prescriptions are based on the dosha and digestive status of an individual. Ayurveda recommends mindful eating, proper food combinations and seasonal eating. These practices improve digestion and protect the body in the long term.
When to Seek Ayurvedic Doctor’s Consultation for Digestive Disorders?
You should see an Ayurvedic doctor when you experience a recurrence of bloating, indigestion, constipation, or acid reflux that cannot be relieved by drugs bought over the counter or if the same problems are persisting for many years, with mild relief only while taking medications. Professional support is necessary when you suffer from irregular bowel movements, excessive fatigue, or unintentional weight loss.
An Ayurvedic doctor at Chiraayu will holistically treat digestive problems. Our personalised treatment balances your doshas, strengthens Agni, and provides long-term solutions to digestive issues.
Conclusion
The traditional teaching of Ayurveda will provide digestive health with a holistic view through understanding the dosha and the digestive fire. Ayurvedic doctors focus on managing and preventing digestive disorders. Mindful eating and stress management help establish stress-free eating practices. It can lead to healthy digestion and well-being. A proper diet, lifestyle, and doshas balance can ensure optimal health. You can get in touch with ayurvedic doctors and surgeons at Chiraayu for long-term digestive health and wellness and create a custom plan to get your gut back into equilibrium.
Continue reading here to know more: How Ayurveda helps in digestive problems
0 notes
Text
Can Haemorrhoids Cause Constipation? Let’s Find Out
Haemorrhoids, often referred to as piles, are a common yet uncomfortable condition that affects millions of people worldwide. These swollen blood vessels in the lower rectum and anus can cause significant discomfort, itching, bleeding and pain, especially during bowel movements.
However, a question that frequently arises is, “Can haemorrhoids cause constipation?”
Understanding this connection is crucial for those who suffer from haemorrhoids and are looking for ways to alleviate their symptoms.
In this article, we will explore the relationship between haemorrhoids and constipation, addressing questions like “Can internal haemorrhoids cause constipation?” and “Can haemorrhoids cause constipation and gas?” to provide a comprehensive understanding of the issue.
Understanding Haemorrhoids or Piles Condition
Haemorrhoids are swollen blood vessels located in the lowest part of the rectum and anus. They can be internal, developing inside the anal canal, or external, forming under the skin around the anus.
Both types can cause discomfort, but internal haemorrhoids are more commonly associated with bleeding during bowel movements, while external haemorrhoids are known for causing pain and discomfort.
Haemorrhoids can complicate regular bowel movements, leading to discomfort and even fear of passing stools. This can result in a cycle of constipation, where the fear of pain or bleeding during defecation causes individuals to avoid going to the toilet, further exacerbating the problem.
The Connection Between Haemorrhoids and Constipation
Many people wonder, “Can haemorrhoids cause constipation?” The answer is not straightforward but can be explained through the symptoms and effects of haemorrhoids. While haemorrhoids themselves do not directly cause constipation, they can create conditions that make constipation more likely.
When you have haemorrhoids, especially when it is thrombosed, the pain and discomfort during bowel movements can lead to a reluctance to defecate. This avoidance can result in stools becoming harder and drier as they stay longer in the colon, which can, in turn, lead to constipation. This relationship between haemorrhoids and constipation is particularly evident in cases where individuals experience significant pain during defecation, prompting them to delay going to the toilet.
“Can internal haemorrhoids cause constipation?” is a common question. Internal haemorrhoids, located inside the rectum, may not be painful but can bleed and cause discomfort. The fear of aggravating these haemorrhoids during bowel movements can lead to voluntary constipation, where the person holds in their stools to avoid pain or bleeding or to avoid the protrusion of the pile mass outside.
While haemorrhoids themselves do not directly cause constipation, they can create conditions that make constipation more likely. The pain and discomfort associated with haemorrhoids can lead to a reluctance to pass stools, which can cause constipation and, in some cases, gas.
Addressing haemorrhoids through diet, lifestyle changes, and medical treatment can help prevent these complications and promote better digestive health.
If you’re experiencing haemorrhoids and the associated symptoms of constipation and gas, consider seeking professional advice and treatment to alleviate your discomfort and improve your quality of life.
If you’re experiencing the discomfort of piles, don’t wait for the condition to worsen. Contact Chirag Hospital today to schedule a consultation with our expert team. We offer personalised treatment plans, including advanced options like Infrared Coagulation, to help you find relief and get back to your everyday life.
Take the first step towards a pain-free future — reach out to Chirag Hospital now!
Continue reading here: Will Haemorrhoids Cause Constipation
#External Haemorrhoids#piles treatment#Different Types Of Piles#Foods To Avoid With Piles#Haemorrhoids Treatment
0 notes
Text
Know about Colon Cancer

What is Colon Cancer?
Colon and rectal cancer are more frequently observed and diagnosed among people aged 65 to 74 years (median age is 68 years), though lately, it is visible in the lower age groups also. In the Western world, colon cancer is observed more commonly than rectal cancer. In India, rectal cancer is more common with men being more commonly affected than women.
Best Colorectal Cancer Doctors say that Colorectal cancer usually starts in the innermost layer (mucosa) and will grow through some or all of the tissue layers that make up the colon and rectum (submucosa, muscularis and serosa ). The extent to which a cancer penetrates the various tissue layers determines the stage of the disease.
Symptoms of Colon Cancer
Changes in bowel patterns, such as diarrhoea, constipation, or more frequent bowel movements
Dark maroon or bright red blood in stool
Narrow stool
A feeling that your gut doesn’t empty fully
Abdominal pain
Unexplained or sudden Weight loss
Weakness or fatigue
Loss of appetite
Causes of Colon Cancer
Rectal cancer develops when the DNA of healthy cells in the rectum undergoes mutations. A cell's DNA includes the instructions that tell it what to do.
The alterations tell the cells to grow out of control and to live even when healthy cells would die. A tumour can arise as a result of the accumulated cells. Cancer cells can grow large enough to penetrate and destroy healthy tissue nearby over time. Cancerous cells can also break off and spread to other places of the body (metastasize).
It’s unclear what causes the mutations that cause rectal cancer to occur in most cases.
Inherited gene mutations that increase the risk of colon and rectal cancer
Gene mutations passed down from parents to children can raise the risk of colorectal cancer in some families. Only a small percentage of rectal tumours contain these mutations. Colorectal cancer genes raise the likelihood of developing the disease, but they do not make it inevitable.
Two well-defined genetic colorectal cancer syndromes are:
Lynch syndrome:
Two well-defined genetic colorectal cancer syndromes are: Lynch syndrome: Lynch syndrome is a condition that affects people. Hereditary non-polyposis colorectal cancer (HNPCC), often known as Lynch syndrome, raises the risk of colon cancer and other cancers. Lynch syndrome patients are more likely to get colon cancer before the age of 50.
Familial adenomatous polyposis (FAP):
These and additional, less common inherited colorectal cancer syndromes can be detected by genetic testing. If you’re concerned about a family history of colon cancer, consult a proctologist to see if your family history shows you’re at risk for these diseases and get it checked from them
Risk Factors of Colon Cancer
The same factors that enhance the risk of colon cancer can also increase the chance of rectal cancer.
The following are some of the risk factors for colorectal cancer:
Older age:
Colorectal cancer can be diagnosed at any age, although the majority of people diagnosed with it are over the age of 50. Colorectal cancer rates in persons under the age of 50 have been rising, but physicians or doctors aren’t sure why.
Too little exercise:
Colorectal cancer is more likely to occur if you are physically inactive. Regular physical activity may help to lower your cancer risk.
Treatment for Colon Cancer
The method of Colon Cancer treatment depends on the stage of the disease i.e, the status of its growth, how large the tumour has grown, how deeply it has invaded the layers of the colon or rectum, and whether it has spread to other organs like liver, lungs or any other parts of the body.
Colon cancer treatment options include:
Radiation therapy
Local ablative therapy
Chemotherapy
A combination of all 3 approaches
Hormonal and biological therapy
Chirag Global Hospital, renowned for its expertise in colon cancer treatment in Bangalore, stands out for its commitment to patient care and advanced medical solutions. With a focus on personalized treatment plans and cutting-edge technology, Chirag Global Hospital ensures that every patient receives comprehensive care tailored to their specific needs. Whether through state-of-the-art diagnostic procedures or compassionate support throughout the treatment journey, Chirag Global Hospital’s main motto remains clear: to empower patients with the best possible outcomes in their battle against colon cancer.
Continue reading more about: Colon Cancer
0 notes
Text
Know The Difference Between Piles, Fissures and Fistula
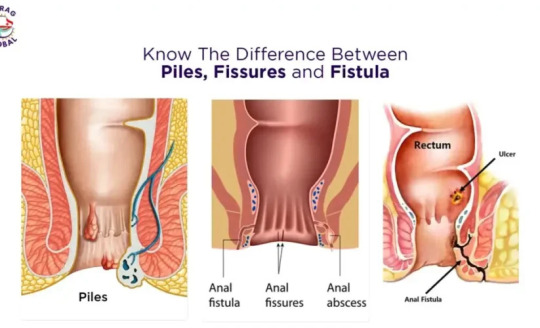
Anal and rectal conditions can be both painful and embarrassing, yet they are fairly common and often treatable. Understanding the difference between piles, fissures, and fistula is essential for proper diagnosis and treatment. While affecting similar body areas, these conditions have distinct causes, symptoms, and treatments.
This article aims to clarify the difference between piles, fissures, and fistulas so that you can better understand them and seek appropriate medical advice.
5 Key Differences Between Piles, Fissures, and Fistulas
Nature of the Condition:
Piles: When three bunches of blood vessels in the anal canal get enlarged and bleed.
Fissures: Small tears in the anal lining.
Fistulas: Abnormal connections between the bowel and the skin near the anus.
Primary Symptoms:
Piles: Bleeding during bowel movements, itching, Swelling and discomfort.
Fissures: Sharp pain during bowel movements and a visible tear.
Fistulas: Persistent pain, swelling, and discharge of pus or blood.
Causes:
* Piles: Straining during bowel movements, chronic constipation, prolonged sitting, and pregnancy.
Fissures: Passing large or hard stools, chronic diarrhoea, and inflammatory bowel diseases
Fistulas: Often follow an abscess or infection in the anal glands.
Treatment Methods:
Piles: medications, lifestyle changes, yoga, minimally invasive procedures or surgeries, depending on the stage of piles
Fissures: Dietary changes, stool softeners, topical anaesthetics, or surgery.
Fistulas: Generally require surgical intervention such as fistulotomy, seton placement, or laser treatment.
Location and Impact:
Piles: Occur inside or around the anus and primarily cause bleeding and discomfort.
Fissures: Located at the anal opening and cause sharp pain and visible tears.
Fistulas: Form an abnormal passageway, often leading to infection and discharge from opening close to the anal canal or pimple-like swelling near the anus.
What is Piles?
There are three bunches of blood vessels in the anal canal. When they enlarge and bleed, they are called Piles.
What are Some Causes of Piles?
Piles develop due to increased pressure in the blood vessels in the lower rectum. Common causes and risk factors include:
Chronic Constipation or Diarrhoea: Straining during bowel movements puts pressure on the rectal veins.
Prolonged Sitting: Sitting for long periods, especially on the toilet, can increase pressure on the veins in the anus and rectum.
Obesity: Excess body weight puts additional pressure on the pelvic veins.
Low-Fiber Diet: Low fibre can lead to hard stools and constipation, increasing the risk of piles.
Heavy Lifting: Repeated heavy lifting can strain the lower rectum.
What is Piles Laser Treatment?
Laser treatment is a modern and minimally invasive option for treating piles. It involves using a laser to shrink the haemorrhoids by cutting off their blood supply. This procedure is known for its precision, minimal discomfort, and quick recovery time. Here’s an overview of the process:
What’s the standard Procedure for Piles Laser Treatment?
Preparation: The patient is prepared for the procedure, usually under local anaesthesia or sedation.
Laser Application: A laser fibre is inserted into the haemorrhoid tissue. The laser energy coagulates the blood vessels, cutting off the blood supply to the haemorrhoid and causing it to shrink.
Minimal Incisions: Unlike traditional surgery, laser treatment involves minimal cutting, resulting in less pain and quicker healing.
What are the Advantages of Piles Laser Treatment?
Less Pain: Patients typically experience less post-operative pain compared to traditional hemorrhoidectomy.
Quick Recovery: The recovery period is shorter, allowing patients to return to normal activities sooner.
Reduced Bleeding: Laser treatment causes less bleeding during and after the procedure.
Minimal Risk of Infection: The precision of the laser reduces the risk of infection and complications.
What’s the Aftercare after Piles Laser Treatment?
Dietary Changes: A high-fibre diet and increased fluid intake are recommended to prevent constipation and straining.
Pain Management: Over-the-counter pain relievers and warm sitz baths can help manage discomfort.
Follow-Up: Regular follow-up with the doctor to monitor healing and address concerns.
(Know more about Piles Treatment)
What is a Fissure?
An anal fissure is a small tear or cut in the lining of the anus, which can cause pain and bleeding during bowel movements. Fissures are common and can occur at any age. They often result from trauma to the anal canal, causing a split in the skin.
What are Some Causes of Fissure?
Anal fissures are typically caused by trauma to the anal canal, which can occur due to:
Passing Large or Hard Stools: Straining to pass large or hard stools is the most common cause of fissures.
Chronic Diarrhea: Frequent loose stools can irritate and tear the anal lining.
Chronic Constipation: Constipation and the resulting straining can cause fissures.
Straining During Bowel Movements: Excessive straining can lead to tears in the anal tissue.
Inflammatory Bowel Diseases: Conditions like Crohn’s disease can increase the risk of fissures due to inflammation of the bowel lining.
What is a Fistula?
A fistula is an abnormal connection or passageway that forms between two organs or vessels that normally do not connect. In the context of the anal region, an anal fistula is an abnormal tunnel that develops between the inner lining of the anal canal and the skin near the anus.
This condition is often the result of an infection in an anal gland that leads to the formation of an abscess which may later form a fistula.
What are Some Causes of Fistula?
Anal fistulas are commonly caused by an infection that starts in an anal gland. The infection leads to an abscess that can form a fistula if not adequately treated.
Anal Abscesses: The primary cause of fistulas. An abscess is a collection of pus that forms due to infection.
Crohn’s Disease: An inflammatory bowel disease that causes chronic inflammation of the gastrointestinal tract, which can lead to fistulas.
Radiation Therapy: Used to treat cancer, radiation can damage tissues and lead to the formation of fistulas.
Trauma: Physical injury to the anal region.
Sexually Transmitted Infections (STIs): Certain STIs can lead to infections that cause fistulas.
Tuberculosis: An infectious disease that can cause fistulas in rare cases.
Diverticulitis: Inflammation or infection of small pouches that can form in the walls of the digestive tract.
What are Some Symptoms of Fistula?
The symptoms of an anal fistula can vary depending on the location and severity of the fistula.
Pain and Swelling: Around the anus, which can be constant or intermittent.
Discharge: Pus or blood discharge from an opening near the anus. The discharge can cause irritation and a foul smell.
Recurrent Abscesses: Frequent abscess formation in the anal area.
Irritation of the Skin: Around the anus due to constant discharge.
Fever and Chills: In the abscess stage.
Painful Bowel Movements: Due to the presence of the fistula and associated inflammation.
Difficulty Sitting: Discomfort or pain while sitting.
Conclusion
Understanding the difference between piles, fissures, and fistulas can significantly impact the approach to treatment and management.
If you’re struggling with piles, fissures, or fistulas and want expert guidance on the best treatment options, look no further than Chirag Global Hospitals. Our team of experienced specialists is dedicated to providing comprehensive care tailored to your needs. Don’t let discomfort and pain control your life any longer.
Contact Chirag Global Hospitals today and take the first step towards effective, compassionate treatment and a healthier, more comfortable life.
Continue reading here: Differences Between Piles, Fissures, and Fistulas
1 note
·
View note
Text
When to See a Doctor for Anal Swelling

Anal swellings are often a cause of discomfort and cause significant distress to many patients due to the presence of a swollen enlargement around the anus. Around 15% of individuals with anal swelling report severe pain, which may indicate a more serious condition requiring prompt medical evaluation. This article discusses the causes, symptoms, treatment options, and the crucial instances when seeking medical advice becomes imperative.
Causes of Anal Swelling
The inflammation or injury of the anal or rectal tissue causes proliferative anal disease. Common causes include:
Haemorrhoids (Piles): India has around 40 million haemorrhoid patients. It is caused by congestion of veins in the lower rectum or anus. Haemorrhoids can develop under the skin around the anus or inside the rectal wall.
Anal Fissures: Mucosal excoriation lining the anus presents with pain, swelling, and erythema because of tearing from constipation or passage of hard stool.
Infections: Infections of bacteria or viruses such as Sexually transmitted diseases (STIS), herpes, or Gonorrhea may cause swelling of the anus. About 5% of anal swelling cases are due to allergic reactions, which may necessitate medical advice for proper treatment.
Abscesses and Fistulas: Anal abscesses are pus accumulations derived from infected glands, which are tender and may present with signs of inflammation.
Inflammatory Bowel Disease (IBD): Chronic inflammations such as Crohn’s disease and ulcerative colitis can also lead to swelling in the anal region.
Anal Tumours: Some of the causes are pilling up of moles or growths that, although benign or malignant, cause swelling of the anal area.
Trauma: Injury to the area often comes from surgery or anal intercourse and from intense straining during defecation, which results in a temporary inflammation of the area.
Warts (Anal Warts): Anal warts are caused by the human papillomavirus (HPV) and can lead to visible swelling around the anus. These warts typically appear as small, fleshy lumps or bumps and can be itchy or cause discomfort, especially if they grow or form clusters.
Sentinel Tags (Skin Tags Around the Anus): Sentinel tags are small skin growths or tags that form around the anus, typically because of internal conditions like anal fissures.
Hidradenitis Suppurativa (HS): Hidradenitis Suppurativa is a chronic skin condition that forms painful abscesses and sinus tracts (tunnels under the skin). It commonly affects areas like the armpits, groin, and around the anus.
Internal Haemorrhoids — Stage 4: Internal haemorrhoids are swollen blood vessels inside the rectum, and when they reach Stage 4 (the most severe), they prolapse (protrude) outside the anus and cannot be manually pushed back in.
Rectal Prolapse: Rectal prolapse occurs when the rectum (lower part of the large intestine) slips out of its normal position and protrudes through the anus.
Rectal Mucosal Prolapse: Rectal mucosal prolapse is a condition in which only the inner lining (mucosa) of the rectum protrudes through the anus without involving the entire thickness of the rectal wall.
Common Symptoms Associated with Anal Swelling
Knowledge of the common symptoms associated with anal swelling will assist with their identification. Common anal infection symptoms include:
Pain or Discomfort: The pain usually associated with it can be mild to severe and increases when sitting or travelling for some patients.
Bleeding: Bright red blood may appear on toilet paper, in the stool, or in the toilet bowl, particularly in cases of haemorrhoids or anal fissures. Sometimes, blood clots or dark-coloured blood may also indicate tumours or growths in the rectum or anal canal.
Itching and Irritation: Persistent itching, medically referred to as pruritus ani, often accompanies swelling.
Lumps or Hardness: External haemorrhoids or thrombosed haemorrhoids or abscesses may manifest as hard, tender lumps near the anus.
Discharge or Odour: Anal abscesses and infections may cause pus discharge and an unpleasant smell.
Systemic Symptoms: In cases of severe infection, fever, fatigue, or malaise may occur, indicating the need for immediate medical attention.
Conclusion
Anal swelling is common and often caused by harmless conditions like haemorrhoids or minor infections. Symptoms such as pain, itching, and bleeding can be managed with simple lifestyle changes, good hygiene, and medical management. Timely consultation and treatment are key to resolving anal swelling and preventing further complications. If you have any concerns about anal swelling or related symptoms, we encourage you to schedule a consultation at Chirag Hospital, where we offer personalised, effective care based on your unique needs.
Continue reading about: Consulting a doctor for anal swelling
0 notes
Text
Ayurveda for Modern Living: Practical Tips for Everyday Wellness
Did you know that 80% of people prefer holistic treatments like Ayurveda? This Indian healing system focuses on nurturing the body, mind, and spirit to treat the root cause of health problems. The increasing burden of health issues makes us chase quick fixes and modern medicines. In this rush, we often overlook the importance of holistic health.
Ayurveda postulates that the physical constitution uniquely differs for everybody because of the dosha balance inside them. You can work on holistic health by learning to balance these doshas. In this blog, we will explore the basic principles of Ayurveda, which are doshas, Agni, and Ama. These core ideas will be the guide in helping you know your body and keep it balanced.
Understanding Doshas in Ayurveda
According to Ayurveda, doshas are basic constituents that control the body’s functions. At birth, your body has a natural constitution influenced by your parents’ body constitution. Many external and internal stimuli impact your body’s dosha, causing changes to the balance of these doshas. The diet you take, your habits, and your lifestyle all cause deficiency or excess of doshas, culminating in various illnesses.
Types of Doshas
The three doshas are Vata, Pitta, and Kapha. They determine an individual's physical and mental characteristics.
What is Vata Dosha?
Its qualities include lightness, dryness, coldness, and mobility. It controls bodily movements, circulations, and nerve functions. An imbalanced Vata brings forth symptoms such as anxiety, dry skin, constipation, joint pains, etc.
What is Pitta Dosha?
It is characterised by heat, sharpness, and oiliness. It governs body temperature, digestion, and metabolism. If there is an imbalance, it leads to digestive problems, inflammation, heartburn, etc.
What is Kapha Dosha?
It is marked with heaviness, coldness, and stability. It is responsible for lubricating joints, boosting immunity and storing energy in the body. Imbalance of kapha results in obesity, asthma, lethargy, etc.
Prakruthi — Deha Prakruthi (Constitution)
Prakruthi refers to the unique physical and mental constitution of an individual, as defined by Ayurveda. Each individual has a unique constitution. It is formulated on the ratio of three doshas in his body, namely Vata, Pitta, and Kapha. It helps in defining physical characteristics, mental predispositions, and health as a whole.
Deha Prakruthi is the state of a person’s physical constitution, as determined by the balance of the three doshas. Therefore, an individual’s strength, energy, and health vary. With knowledge of Deha Prakruthi, lifestyle decisions such as diet and exercise can be tailored to the individual’s need for maintaining health and addressing predisposition to specific conditions.
In Ayurveda practice, Prakruthi is evaluated to understand the prevailing dosha in a person. This helps in knowing a person’s strengths, weaknesses, and susceptibility toward an imbalance.
Conclusion
Ayurveda teaches us that life is a journey of balance in which the mind, body, and spirit work in harmony. It will enable you to make choices that help maintain wellness through your dosha and Agni. Ayurveda medicines and therapies lead to better digestion, disease prevention, and long-term health. It gives you the tools to thrive by understanding the transformative forces within the body. Following Ayurveda is about focusing on your body, nourishing it from within, and leading a balanced life so that you can combat health issues more effectively.
You can start following Ayurvedic principles by eating a healthy balanced diet and following an exercise routine. Consult with an Ayurvedic practitioner to learn more about the right Ayurvedic diet and lifestyle for your body for optimal health.
At Chirag Global Hospitals, we’re proud to announce the launch of “Chiraayu” — a pioneering Ayurvedic wing dedicated exclusively to Proctology and digestive issues. This innovative integration of traditional wisdom of Ayurveda and Yoga, with modern allopathic expertise marks a significant milestone in our journey to provide comprehensive and holistic healthcare.
Continue reading to learn more about: Ayurveda Basics
0 notes
Text
9 Best Fruits That Help Treat Piles

Piles, also known as hemorrhoids, occur when the veins in the anus and lower rectum become swollen and inflamed. This condition, which can cause discomfort, pain, and itching, is common across all age groups. While medical treatments are effective, dietary changes, including the consumption of certain fruits, can significantly alleviate symptoms and promote healing.
This article explores the top 9 fruits that can aid in managing and treating piles naturally.
1. Apples
Apples are a powerhouse of dietary fiber, offering both soluble and insoluble fiber. This combination helps soften stools, making them easier to pass and reducing the strain during bowel movements — a key factor in preventing and managing piles. Regular consumption of apples supports a healthy digestive system, minimizing the risk of constipation, a major contributor to hemorrhoids.
2. Pears
Pears are another fiber-rich fruit that promotes smooth digestion and prevents constipation. They are particularly high in pectin, a type of soluble fiber that soothes inflammation and fosters healing within the digestive tract. Including pears in your diet can provide relief from piles-related discomfort.
3. Bananas
Bananas are a natural remedy for digestive issues due to their high fiber content and easy digestibility. They are also rich in potassium, which helps reduce swelling and inflammation throughout the body, including the rectal area. A ripe banana a day can effectively support regular bowel movements and alleviate piles symptoms.
4. Berries
Berries like strawberries, blueberries, and raspberries are not only delicious but also packed with antioxidants and fiber. These nutrients work together to reduce inflammation and improve bowel regularity. Their natural sweetness makes them a healthy snack option for managing piles.
5. Kiwi
Kiwi is a tropical fruit known for its high fiber content and natural enzymes that promote digestion. It contains actinidin, an enzyme that aids in breaking down food efficiently and preventing constipation. Kiwi is also rich in vitamin C, which helps reduce inflammation and boosts the immune system, accelerating the healing process.
6. Prunes
Prunes, or dried plums, are a well-known natural laxative. They are loaded with dietary fiber and sorbitol, a sugar alcohol that draws water into the intestines, softening stools and facilitating smooth bowel movements. Regular intake of prunes can prevent constipation and ease piles symptoms.
7. Papaya
Papaya is a tropical favourite for digestive health. It contains papain, an enzyme that promotes healthy digestion and reduces inflammation in the digestive tract. The fruit’s high fiber content also helps regulate bowel movements, making it a great choice for those suffering from piles.
8. Grapes
Grapes are rich in antioxidants and dietary fiber, both of which support a healthy digestive system. Their natural hydrating properties and fiber content ensure smoother bowel movements, reducing the risk of constipation and piles flare-ups.
9. Oranges
Oranges are an excellent source of vitamin C and fiber. These nutrients work together to reduce inflammation, boost the immune system, and support digestive health. Regularly consuming oranges can help manage piles symptoms while promoting overall well-being.
Other foods that can help with piles include:
Sprouts: Contain fiber, vitamin C, calcium, and protein
Nuts and seeds: Almonds, walnuts, and chia seeds are high in fiber and soluble fat
Leafy greens: Broccoli, cauliflower, kale, and spinach are rich in fiber
Clear broths: Chicken bone broth is high in protein and can help strengthen intestinal walls
Herbal teas: Dandelion and mullein teas can help with inflammation and irritation
Take Away
These 9 best fruits for piles can help you manage your piles symptoms and keep your digestion under control. Apart from this, you also need to know that the major causes of piles in adults other than constipation are lack of exercise, a sedentary lifestyle, junk food, dairy products, spicy and salty food, processed food, caffeinated drinks and many more distorted habits.
Above all, eating lots of fiber and drinking lots of water can help you to fight constipation. But you have to have strict discipline and effort to get rid of the problem all in all. The dietary habits can, of course, diminish the symptoms but lifestyle changes do the real magic. However, if you do not see any improvements by trying, see your doctor or surgeon for the best treatment plan for piles. You can consult online for any queries about piles, fissures or fistulas.
Expert Care for Piles at Chirag Global Hospital
Incorporating these fruits into your diet can significantly ease piles of symptoms. However, for severe cases, professional medical care may be necessary. At Chirag Global Hospital, recognized as one of the best piles treatment hospitals in Bangalore, we offer advanced facilities and expert care for managing piles.
Our team of experienced doctors provides personalized treatment plans, ensuring patient comfort and recovery. With a commitment to excellence, we aim to deliver high-quality care and effective solutions for piles treatment.
Take the first step towards relief today. Consult our specialists and experience world-class care tailored to your needs.
Continue reading to know more about: Fruits That Help to Treat Piles
1 note
·
View note