#post-acute sequelae of SARS-CoV-2
Explore tagged Tumblr posts
Text
and then what and then what, what then
— Julia Guez, "Still Life with Post-Acute Sequelae of SARS-CoV-2," The Certain Body
#quote#Julia Guez#poetry#The Certain Body#out of my collection#Still Life with Post-Acute Sequelae of SARS-CoV-2
699 notes
·
View notes
Text
Every time I explain I have Long Covid, people are like, 'So, you never got over having covid? So you're going to have a cold forever?'
And I get when we were in the pandemic, we all developed anxiety so severe we were afraid to touch our produce from the grocery store without wiping it down first. But the idea of Covid as "just a cold" is not the full story. That's mostly something that got pushed from people who didn't understand it, and as shorthand to explain the warning symptoms to people. Long Covid is not a cold. If I get one more person talking down to me about how I'll feel better if I just take a Vitamin C capsule every morning, I will riot.
Long Covid is currently not curable. It's manageable in the right circumstances. But there is currently no pill or therapy that is a cure for Long Covid. That includes lifestyle habits too. Maybe drinking a smoothie made out of half the vegetable aisle will be good for you, but it won't fix you magically. Please stop suggesting therapies to people. You're not their doctor, and all you're going to do is exasperate them. Worst case scenario, you put someone through another cycle of grief after they try it, and it doesn't work for them.
Why is that the case? Because Long Covid is highly complicated. Most doctors will acknowledge we don't know the half of it, as far as the complete effects. Long Covid, in short, is a very confusing amalgamation of the after-effects of getting Covid in the first place. Many experts have compared it to HIV in the way it continues to affect your body. That's why Long Covid is officially known as "Post-Acute Sequelae of SARS-CoV-2 Infection." Sequelae refers to the long-term or permanent effects aspect of it. It's a highly complicated thing that would most likely not be easily cured. Just like how someone recovered from severe Tuberculosis might still have issues with their lungs, people with Long Covid have to deal with the aftermath of Covid throughout their bodies.
Please stop trying to tell me, and people like me that it will just heal itself eventually. You're only frustrating people who've been dismissed so much already. Parts of it may get better with time, but the complete effect on your body is devastating and traumatic. Saying things like 'Well I did x,y, and z, and I feel totally better!' That's great, good for you. That doesn't mean it's going to work for everyone, let alone most people. Understand that it's a confusing illness. And please, for heavens sake, stop asking people 'So when are you going to get better?' We don't know. That's the point.
#long covid awareness#long covid#sars cov 2#chronic disability#chronic illness#chronic fatigue#chronically ill#invisible illness#living with disability#invisible disability#covid isn't over#covid#medical rant#medicine#covid 19#illness
414 notes
·
View notes
Text
COVID-19's long-term effects on the body: an incomplete list
COVID’s effect on the immune system, specifically on lymphocytes:
NYT article from 2020 (Studies cited: https://www.biorxiv.org/content/10.1101/2020.05.18.101717v1, https://www.biorxiv.org/content/10.1101/2020.05.20.106401v1, https://www.unboundmedicine.com/medline/citation/32405080/Decreased_T_cell_populations_contribute_to_the_increased_severity_of_COVID_19_, https://www.medrxiv.org/content/10.1101/2020.06.08.20125112v1)
https://www.biorxiv.org/content/10.1101/2022.01.10.475725v1
https://www.science.org/doi/10.1126/science.abc8511 (Published in Science)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9057012/
https://www.forbes.com/sites/williamhaseltine/2022/04/14/sars-cov-2-actively-infects-and-kills-lymphoid-cells/
https://www.cleveland.com/news/2022/10/in-cleveland-and-beyond-researchers-begin-to-unravel-the-mystery-of-long-covid-19.html
SARS-CoV-2 infection weakens immune-cell response to vaccination: NIH-funded study suggests need to boost CD8+ T cell response after infection
https://www.merckmanuals.com/professional/hematology-and-oncology/leukopenias/lymphocytopenia
https://thetyee.ca/Analysis/2022/11/07/COVID-Reinfections-And-Immunity/
Dendritic cell deficiencies persist seven months after SARS-CoV-2 infection
https://www.frontiersin.org/articles/10.3389/fimmu.2022.1034159/full
https://www.n-tv.de/politik/Lauterbach-warnt-vor-unheilbarer-Immunschwaeche-durch-Corona-article23860527.html (German Minister of Health)
Anecdotal evidence of COVID’s effects on white blood cells:
https://twitter.com/DrJohnHhess/status/1661837956875956224
https://x.com/TristanVeness/status/1661565201345564673
https://twitter.com/TristanVeness/status/1689996298408312832
Much more if you speak to Long Covid patients directly!
Related information of interest:
China approves Genuine Biotech's HIV drug for COVID patients
COVID as a “mass disabling event” and impact on the economy:
https://www.ctvnews.ca/health/report-says-long-covid-could-impact-economy-and-be-mass-disabling-event-in-canada-1.6306608
https://x.com/inkblue01/status/1742183209809453456?s=20
COVID’s impact on the heart:
https://www.dailystar.co.uk/news/world-news/deadly-virus-could-lead-heart-31751263 (Research from: Japan's Riken research institute)
https://www.brisbanetimes.com.au/national/queensland/unlike-flu-covid-19-attacks-dna-in-the-heart-new-research-20220929-p5bm10.html
https://www.mdpi.com/2077-0383/12/1/186
https://medicalxpress.com/news/2023-04-mild-covid-effects-cardiovascular-health.html
https://publichealth.jhu.edu/2022/covid-and-the-heart-it-spares-no-one
https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/coronavirus-and-your-health/is-coronavirus-a-disease-of-the-blood-vessels (British Heart Foundation)
COVID’s effect on the brain and cognitive function:
https://www.openaccessgovernment.org/article/brain-infection-by-sars-cov-2-lifelong-consequences/171391/
https://www.cidrap.umn.edu/covid-19/study-shows-covid-leaves-brain-injury-markers-blood
https://www.theguardian.com/world/2020/jul/08/warning-of-serious-brain-disorders-in-people-with-mild-covid-symptoms
Cognitive post-acute sequelae of SARS-CoV-2 (PASC) can occur after mild COVID-19
Neurologic Effects of SARS-CoV-2 Transmitted among Dogs
https://journals.lww.com/nsan/fulltext/2022/39030/neurological_manifestations_and_mortality_in.4.aspx
https://www.salon.com/2023/06/17/new-evidence-suggests-alters-the-brain--but-the-extent-of-changes-is-unclear/
https://www.scientificamerican.com/article/covid-virus-may-tunnel-through-nanotubes-from-nose-to-brain/
https://neurosciencenews.com/post-covid-brain-21904/
https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(22)00260-7/fulltext
https://medicalxpress.com/news/2022-08-covid-infection-crucial-brain-regions.html
https://news.ecu.edu/2022/08/04/covid-parkinsons-link/
Covid as a vascular/blood vessel disease:
https://www.salon.com/2020/06/01/coronavirus-is-a-blood-vessel-disease-study-says-and-its-mysteries-finally-make-sense/
https://www.salon.com/2023/12/27/brain-damage-caused-by-19-may-not-show-up-on-routine-tests-study-finds/
https://www.nih.gov/news-events/news-releases/sars-cov-2-infects-coronary-arteries-increases-plaque-inflammation
https://www.mdpi.com/2077-0383/12/6/2123
https://www.sciencedaily.com/releases/2021/10/211004104134.htm (microclots)
Long Covid:
Post-COVID-19 Condition in Canada: What we know, what we don’t know, and a framework for action
https://www.ctvnews.ca/health/coronavirus/more-than-two-years-of-long-covid-research-hasn-t-yielded-many-answers-scientific-review-1.6235227
https://www.cbc.ca/news/canada/london/cause-of-long-covid-symptoms-revealed-by-lung-imaging-research-at-western-university-1.6504318
https://www.cbc.ca/news/canada/montreal/long-covid-study-montreal-1.6521131
https://news.yale.edu/2023/12/19/study-helps-explain-post-covid-exercise-intolerance
Other:
- Viruses and mutation: https://typingmonkeys.substack.com/p/monkeys-on-typewriters
Measures taken by the rich and world leaders
Heightened risk of diabetes
https://jamanetwork.com/journals/jama/fullarticle/2805461
https://www.nature.com/articles/d41586-022-00912-y
Liver damage:
https://timesofindia.indiatimes.com/city/mumbai/46-of-covid-patients-have-liver-damage-study/articleshow/97809200.cms?from=mdr
tl;dr: covid is a vascular disease, not a respiratory illness. it can affect your blood and every organ in your body. every time you're reinfected, your chances of getting long covid increase.
avoid being infected. reduce the amount of viral load you're exposed to.
the gap between what the scientific community knows and ordinary people know is massive. collective action is needed.
#putting this somewhere at least as reference for... somebody hopefully#covid#disability#y'all. it is bleak out there but some very good people are doing their best to help#we need as many people aware and helping as possible
464 notes
·
View notes
Text
“You may now become who you thought was disposable”: COVID-19 Politics and Ableism - Published July 4, 2024
Unpaywalled link available in the link to our archive! A taste below!
“You may now become who you thought was disposable”: COVID-19 Politics and Ableism Andrea Kitta Journal of American Folklore, Volume 137, Number 545, Summer 2024, pp. 321-330 (Article) Published by American Folklore Society For additional information about this article muse.jhu.edu/article/931461[37.228.238.33] Project MUSE (2024-07-09 12:59 GMT) American Folklore Society
This essay critically examines the intersection of COVID-19, Long COVID, ableism, and health care disparities in the United States, emphasizing the transformative impact of COVID-19 as a mass disabling event with a disproportionate impact on marginalized communities. I also bring an autoethnographic lens to my experi- ence of COVID-19 and Long COVID, underscoring the importance of recognizing the diverse and often untellable experiences of individuals with disabilities and challenging the prevailing ableist perspectives embedded in society. I raise ethical considerations of storytelling in the context of Long COVID and urge researchers to embrace empathy and a more inclusive approach that challenges traditional notions of objectivity and distancing within academic research. I call for a collaborative approach between disability studies and folklore studies, encouraging scholars to interrogate and explore the traditions shaped by experiences of disability.
On December 13, 2020, disability advocate Imani Barbarin created a TikTok where she stated in the caption: “COVID is a mass disabling event. Things will never be the same. Never. You may now become who you thought was disposable” (Barbarin 2020). Barbarin was not overstating what is happening in the United States. In addition to the overwhelming number of US-based COVID-19 deaths (1.07 million as of November 1, 2022, according to the New York Times COVID-19 Tracker [New York Times 2023]), there is also an alarming number of cases of post-acute sequelae SARS-CoV-2 infection (PASC) or, as it’s more commonly known, Long COVID. Long COVID happens in anywhere from 5 percent to 50 percent of COVID-19 infections (although most medical experts agree the rate of Long COVID is somewhere around 20–30 percent of all infections). Long COVID affects women at a 22 percent higher rate than men (Sylvester et al. 2022:1391), and one study of Long COVID listed over 200 symptoms (Davis et al. 2021). The most common symptoms are fatigue, shortness of breath, cough, chest pain, brain fog, sleep disturbances, depression, joint pain, and dysautonomia (a dysfunction of the autonomic nervous system that typically presents as the inability to control temperature, breathing issues, and other things the body normally controls automatically).
Current estimates of those affected by Long COVID in the United States are between twenty and forty million. COVID-19 has also been shown to reactivate other viruses (Gold et al. 2021; Chen et al. 2022; Su et al. 2022), and one current theory is that Long COVID is the result of the COVID-19 virus continually being reactivated in the body (Klein et al. 2022). The latest research out of Yale University shows that COVID-19 cases entail cellular changes to the B and T cells, lower levels of cortisol, and that the virus can reactivate other viruses (Su et al. 2022:891–2). A recent study with more than 154,068 participants showed that “in the post-acute phase of COVID-19, there was increased risk of an array of incident neurologic sequelae including ischemic and hemorrhagic stroke, cognition and memory disorders, peripheral nervous system disorders, episodic disorders (for example, migraine and seizures), extrapyramidal and movement disorders, men tal health disorders, musculoskeletal disorders, sensory disorders, Guillain–Barré syndrome, and encephalitis or encephalopathy” (Xu, Xie, and Al-Aly 2022:2406).
Both COVID-19 and Long COVID exposed inequities in the US health care system, with Black, Indigenous, and people of color (BIPOC) populations dying from COVID-19 at much higher rates than White people at the beginning of the pandemic. Compared to White people, Alaskan Indian or Alaskan Natives died at 2.1 times the rate, Black people at 1.7 times the rate, Hispanic or Latinx people at 1.8 the rate, and Asian Americans at 0.8 times the rate (CDC 2023). According to the Washington Post’s analysis of CDC’s statistics, the rate of White people dying from COVID-19 became equal to the rate of other groups beginning in October 2021, then (except for the Omicron wave) increased, primarily due to White people being unvaccinated. Strangely enough, the equalizing trend wasn’t because death rates dropped for BIPOC people, but rather was due to the rise of the White death rate. Tasleem Padamsee, Assistant Professor at The Ohio State University who researched vaccine use and who is a member of the Ohio Department of Health’s work group on health equity, stated: “Usually, when we say a health disparity is disappearing, what we mean is that . . . the worse-off group is getting better. . . . We don’t usually mean that the group that had a systematic advantage got worse” (quoted in Johnson and Keating 2022).
Additionally, at the time of this writing in Spring 2023, the pandemic has been declared as “over” despite the fact that around 400 people are still dying per day in the United States and that those dying tend to be people with disabilities and the elderly (New York Times 2023). It’s difficult to imagine a situation where 400 deaths a day are deemed acceptable, yet here we are. Many people are desperate to “get back to normal” and seem to care more about going maskless or dining indoors than they do about those who are dying of COVID-19. Those who are unvaccinated and unmasked also seem to not understand (or not care) that the longer they continue on that path, the longer the pandemic will take to dissipate. Simply put, the majority of people do not seem to care about people with disabilities, including those who are immunocompromised, and their increased health risks due to the pandemic.
People with disabilities are an unrecognized health disparity population, and they died at much higher rates during COVID-19 (Krahn, Walker, and Correa-de-Araujo 2015). The National Council on Disability found that 181,000 people with disabilities in long-term care facilities died from COVID-19 in the first year of the pandemic, making up one-third of COVID-19 deaths at that time (National Council of Disabilities 2021). The report is worth quoting at length.
In addition to disproportionate fatalities, key findings of the report include:
People with disabilities faced a high risk of being triaged out of COVID-19 treatment when hospital beds, supplies, and personnel were scarce; were denied the use of their personal ventilator devices after admission to a hospital; and at times, were denied the assistance of critical support persons during hospital stays. Informal and formal Crisis Standards of Care (CSC), pronouncements that guided the provision of scarce health care resources in surge situations, targeted people with certain disabilities for denial of care (National Council of Disabilities 2021).
Students with disabilities were denied necessary educational services and supports during the pandemic and have experienced disruption and regression in their behavioral and educational goals (National Council of Disabilities 2021).
The growing shortage of direct care workers in existence prior to the pandemic became worse during the pandemic. Many such workers, who are women of color earning less than a living wage and lacking health benefits, left their positions for fear of contracting and spreading the virus, leaving people with disabilities and their caregivers without aid and some at risk of losing their independence or being institutionalized (National Council of Disabilities 2021).
Deaf, Hard of Hearing, Deaf-Blind, and Blind persons faced a profound communication gulf as masks became commonplace, making lip-reading impossible and sign language harder (National Council of Disabilities 2021).
#disability justice#disability politics#covid pandemic#covidー19#mask up#covid#pandemic#covid 19#coronavirus#wear a mask#sars cov 2#still coviding#public health#wear a respirator#ableism#covid eugenics
132 notes
·
View notes
Text
Evidence abounds showing that Vitamin C can tighten endothelial barriers and reverse endothelial dysfunction.
Walter M Chesnut
Oct 25, 2024
Plasma vitamin C levels and FMD during acute inflammation and following oral consumption of 2 g of Vitamin C in young and older adults. FMD data are missing for 1 older adult during vitamin C due to a low-quality FMD. Plasma vitamin C data are included for those who had data for the FMD and successful venipuncture (young adults, n = 7; older adults, n = 12), with data missing during the vitamin C time point for 2 younger adults and 2 older adults. aBaseline significantly different from inflammation, p < 0.05; bInflammation significantly different from vitamin C, p < 0.05; cBaseline significantly different from vitamin C, p < 0.05
The article I referenced in yesterday’s post, detailing the evidence supporting my Spike Protein Endothelial Disease (SPED) hypothesis, makes a very important point in its conclusion.
Treatments directed to EC (Endothelial Cells) protection and prevention of endothelial damage might be essential in the prevention and management of the post-sequelae effect of COVID-19.
Sustained vascular inflammatory effects of SARS-CoV-2 spike protein on human endothelial cells https://www.researchsquare.com/article/rs-5003230/v1
It is, therefore, fortuitous that the Friday Hope post I have worked on this week and am now presenting addresses this specific recommendation. Vitamin C is a readily available and safe natural therapeutic which provides protection of the endothelium and is able to reverse its dysfunction.
I will forgo the usual background of the therapeutic we are reviewing this week as knowledge of Vitamin C is ubiquitous.
First, with regards to SARS-CoV-2 and the Spike Protein in particular, intravenous Vitamin C has been shown to be an effective treatment.
Combined with traditional Chinese medicine, Yali used a large dose of vitamin C (20 g/60 kg per day) to treat COVID-19.[22] As a result of Yali treatment, the symptoms of fatigue, cough, dry throat, and shortness of breath were significantly improved, and no adverse events occurred.[22] Zhang used a large dose of vitamin C (24 g/day) at the rate of 12 mL/h to treat patients with COVID-19,[23] with the results revealing that the PaO2/FiO2 of patients increased steadily, and the 28 day mortality of patients decreased significantly.[23] Therefore, high-dose vitamin C infusion may be a significantly effective therapeutic agent in COVID-19 treatment.
High-dose vitamin C intravenous infusion in the treatment of patients with COVID-19
2 notes
·
View notes
Note
bro. U seem smart how tf do I even start treating me/cf in myself idk where to even look :(
hey sorry i’m so late getting back to this i’ve been exhausted lol. and wanted to give you a comprehensive response. The things I find are mostly from research articles. what sucks is because the condition isn’t fully understood there are a lot of relevant articles that use different names- cfs/me, post-viral fatigue syndrome (pvfs), long covid, post acute sequelae of SARS—CoV-2. I try to keep up to date and search these terms on pubmed every now and then. Medscape is a good app to quickly see which drugs are being used in clinical trials but i think it might be restricted to med students/ researchers/ clinicians but theres probably some way around that.
if you cbf with all that and just want recommendations: the worst csf/me symptoms for me are definitely neurocognitive and the biggest helper has been modafinil followed by dexamphetamine. i highly recommend some kind of stimulants if you can get your hands on them. other drugs and supplements that have shown high efficacy in studies:
coenzyme q10: i’ve been taking high doses (~900mg; up to 3000mg is recommended for disorders of mitochondrial dysfunction) and I do notice some physical improvement.
creatine monohydrate: 3-5g a day (may take several months to see effects however it’s cheap)
low dose naltrexone- lots of new interesting studies coming out about this. naltrexone is an opioid receptor antagonist usually prescribed to alcoholics and opioid addicts but also acts as an immunomodulatory agent at low doses. I started 2mg/day as of two days ago.
Zinc- i recommend zinc picolinate for higher bioavailability
B group vitamins- particularly B6, B9 and B12. There are relatively common mutations at the MTHFR gene (that may also contribute to cfs/me) that cause difficulty in metabolising B12 and B9- if you know your MTHFR genotype or experience weird side effects from B vitamins like insomnia or anxiety and paranoia, look into methylated forms (methylcobalamin and 5-methyltetrahydrofolic acid).
L-carnitine
nicotinamide adenine dinucleotide (NAD)
Methionine
N-acetylcysteine (NAC)
i haven't tried the last four yet but i'll be ordering them soon
7 notes
·
View notes
Text
This is important. Here's why:
- Accurate detection of viral persistence
- Identification of latent reactivation
- Single blood sample
- High sensitivity & specificity
- Distinguishes infection & vaccination
- Extend to other chronic illnesses
- Non-invasive
- Clinical biomarker
This looks promising. A blood test to find viral reactivation in Long Covid. Click View on Twitter to see the full Twitter post.
6 notes
·
View notes
Text
Persistent SARS-CoV-2 infections may act as viral reservoirs that could seed future outbreaks1,2,3,4,5, give rise to highly divergent lineages6,7,8 and contribute to cases with post-acute COVID-19 sequelae (long COVID)9,10. However, the population prevalence of persistent infections, their viral load kinetics and evolutionary dynamics over the course of infections remain largely unknown. Here, using viral sequence data collected as part of a national infection survey, we identified 381 individuals with SARS-CoV-2 RNA at high titre persisting for at least 30 days, of which 54 had viral RNA persisting at least 60 days. We refer to these as ‘persistent infections’ as available evidence suggests that they represent ongoing viral replication, although the persistence of non-replicating RNA cannot be ruled out in all. Individuals with persistent infection had more than 50% higher odds of self-reporting long COVID than individuals with non-persistent infection. We estimate that 0.1–0.5% of infections may become persistent with typically rebounding high viral loads and last for at least 60 days. In some individuals, we identified many viral amino acid substitutions, indicating periods of strong positive selection, whereas others had no consensus change in the sequences for prolonged periods, consistent with weak selection. Substitutions included mutations that are lineage defining for SARS-CoV-2 variants, at target sites for monoclonal antibodies and/or are commonly found in immunocompromised people.
4 notes
·
View notes
Text
Known COVID-19 Health Complications
Last Updated September 8, 2023
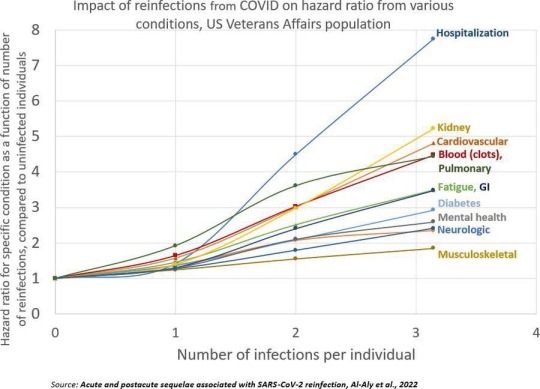
Repeat Infections
Summary: Repeat infections, even if mild during the acute phase, cause cumulative damage to the body and increase your risk of developing health complications or Long COVID. You should aim to limit the number of times you are infected as much as possible, even if you are not currently high risk (Note: Health complications post-COVID-19 infection can make you high risk) and have been vaccinated.
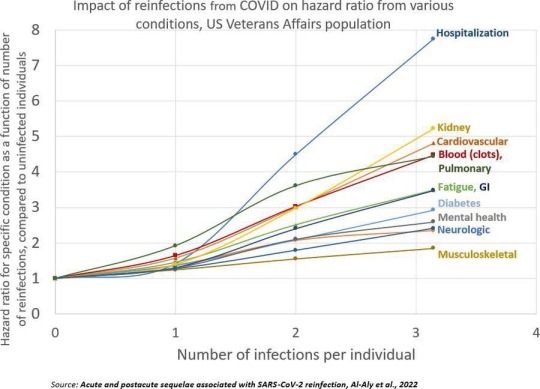
Published Research
Acute and postacute sequelae associated with SARS-CoV-2 reinfection | Nature Medicine Bowe, B., Xie, Y, & Al-Aly, Z. (2022).
Articles & Reports
Repeat COVID-19 infections increase risk of organ failure, death – Washington University School of Medicine in St. Louis (wustl.edu) Sauerwein, K. (2022).
Why Getting COVID-19 Multiple Times Is Risky For Your Health | Time Park, A. (2022).
Heart & Cardiovascular Damage
Summary: COVID-19 increases your risk of heart failure, heart attacks, strokes, pulmonary embolism, palpitations, arrhythmia, myocarditis, blood clots (thrombosis), etc. post-infection. Inflammation during the acute phase of a COVID-19 infection can damage the heart and blood vessels.
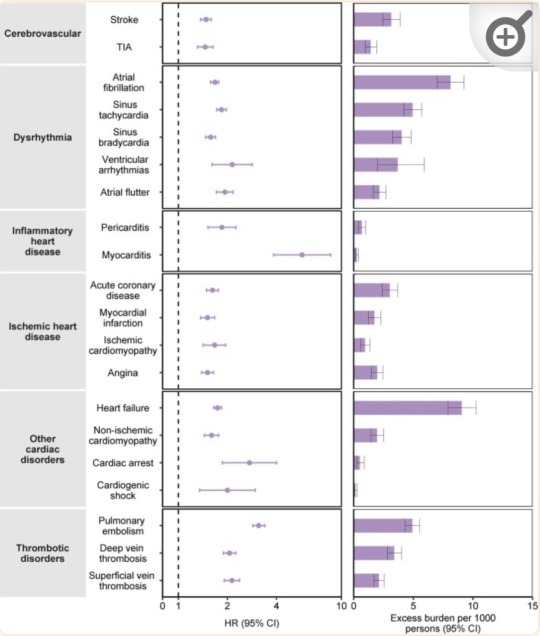
“Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes in participants without any history of cardiovascular outcomes prior to COVID-19 exposure compared to the contemporary control cohort.” (Xie et al., 2022)
Published Research
Core mitochondrial genes are down-regulated during SARS-CoV-2 infection of rodent and human hosts | Science Translational Medicine Guarnieri, J. W., Dybas, J. M., ... Wallace, D. C. (2023).
Long-term cardiovascular outcomes of COVID-19 - PMC (nih.gov) Xie, Y., Xu, E., Bowe, B., & Al-Aly, Z. (2022).
Articles & Reports
Blood Clotting Proteins Might Help Predict Long COVID Brain Fog - Scientific American Reardon, S. (2023, September 1).
SARS-CoV-2 can damage mitochondrion in heart, other organs, study finds | CIDRAP (umn.edu) Van Beusekom, M. (2023, August 9).
Your vascular system and COVID | Heart and Stroke Foundation Heart and Stroke Foundation. (2023).
COVID, heart disease and stroke | Heart and Stroke Foundation Heart and Stroke Foundation. (2023, April 17).
How does coronavirus affect your heart? - BHF British Heart Foundation. (2023, March 21).
COVID-19 and Heart Damage: What You Should Know (clevelandclinic.org) Cleveland Clinic. (2022, May 10).
Heart Problems after COVID-19 | Johns Hopkins Medicine Post, W. S., & Gilotra, N. A. (2022).
COVID and the Heart: It Spares No One | Johns Hopkins | Bloomberg School of Public Health (jhu.edu) Desmon, S., & Al-Aly, Z. (2022, March 14).
COVID-19 takes serious toll on heart health—a full year after recovery | Science | AAAS Wadman, M. (2022, February 9).
Brain & Neurological Damage
Summary: COVID-19 infection increases your risk of developing cognitive impairments, mental health issues, poor memory, early onset dementia, and permanent loss of smell due to brain damage and the atrophy of brain matter. "Brain fog" and problems concentrating are common complaints post-infection that have also been linked to brain damage. Damage to blood vessels due to inflammation during the infection may be responsible for this by restricting oxygen flow to the brain. COVID-19 may also directly infect the brain.
Published Research
Biology | Free Full-Text | Vascular Dysfunctions Contribute to the Long-Term Cognitive Deficits Following COVID-19 (mdpi.com) Shabani, Z., Liu, J., & Su, H. (2023).
Frontiers | COVCOG 2: Cognitive and Memory Deficits in Long COVID: A Second Publication From the COVID and Cognition Study (frontiersin.org) Guo, P., Ballesteros, B. A., Yeung, S. P., Liu, R., Saha, A., Curtis, L., Kaser, M., Haggard, M. P., & Cheke, L. G. (2022).
COVID-19 and cognitive impairment: neuroinvasive and blood‒brain barrier dysfunction - PMC (nih.gov) Chen, Y., Yang, W., Chen, F., & Cui, L. (2022).
Comparison of post-COVID depression and major depressive disorder | medRxiv Perlis, R. H., Santillana, M., Ognyanova, K., Green, J., Druckman, J., Lazer, D., & Baum, M. A. (2021).
Articles & Reports
Long COVID May Impair Memory, Cognition for Months (healthline.com) Rossiaky, D. (2022).
COVID Variants Can Affect the Brain in Different Ways - Neuroscience News (2023).
The hidden long-term cognitive effects of COVID-19 - Harvard Health Budson, A. E. (2021). Harvard Medical School.
Long Covid: Even mild Covid is linked to damage to the brain months after infection (nbcnews.com) Ryan, B. (2022). NBC News.
COVID-19 Can Affect the Brain Even Long After an Infection | Time Ducharme, J. (2023). Time.
Lung Damage
Summary: COVID-19 infections can cause lung damage or scarring, and can trigger pneumonia, bronchitis, ARDS, and sepsis. Additionally, some people experience shortness of breath (dyspnea) and difficulty exercising as a post-acute sequela after infection, or multiple infections.
Published Research
At a crossroads: COVID-19 recovery and the risk of pulmonary vascular disease - PMC (nih.gov) Cascino, T. M., Desai, A. A., & Kanthi, Y. (2021).
[Pulmonary manifestations in long COVID] - PubMed (nih.gov) Sommer, N., & Schmeck, B. (2022).
Residual Lung Abnormalities after COVID-19 Hospitalization: Interim Analysis of the UKILD Post-COVID-19 Study - PubMed (nih.gov) Stewart, I., Jacob, J., George, P. M., Molyneaux, P. L., Porter, J. C., Allen, R. J., Aslani, S., Baillie, J. K., Barratt, S. L., Beirne, P., Bianchi, S. M., Blaikley, J. F., ...Jenkins, G. R. (2023).
Articles & Reports
Even mild cases of COVID-19 may cause long-term lung damage - UPI.com HealthDay News. (2022). United Press International.
COVID-19 Lung Damage | Johns Hopkins Medicine Galiatsatos, P. (2022).
Immune System & Autoimmune Diseases
Summary: COVID-19 infection can impair the functioning of your immune system. This means that those who have previously been infected are potentially immunocompromised (higher risk). For some people, the way COVID-19 impairs their immune system results in the onset of autoimmune diseases.
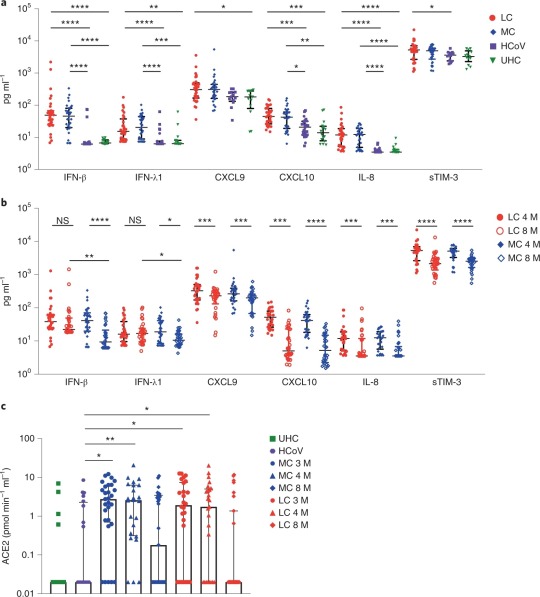
“Elevated levels of proinflammatory cytokines that persist more than 8 months following convalescence.” (Phetsouphanh et al., 2022)
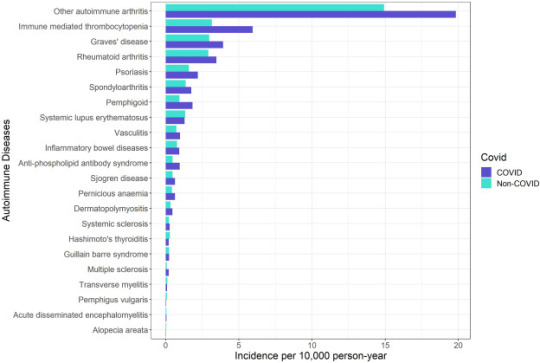
“Crude incidence of each autoimmune disease by COVID-19 and non-COVID groups.” (Peng et al., 2023)
Published Research
Immunological dysfunction persists for 8 months following initial mild-to-moderate SARS-CoV-2 infection | Nature Immunology Phetsouphanh, C., Darley, D. R., Wilson, D. B., Howe, A., Munier, M. L., Patel, S. K., Juno, J. A., Burrell, L. M., Kent, S. J., Dore, G. J., ... & Matthews, G. V. (2022).
Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection | BMC Medicine | Full Text (biomedcentral.com) Ryan, F. J., Hope, C. M., Masavuli, M. G., Lynn, M. A., Mekonnen, Z. A., Yeow, A. E. L., Garcia-Valtanen, P., Al-Delfi, Z., Gummow, J., Furguson, C., ... Lynn, D. J. (2022).
Risk of autoimmune diseases following COVID-19 and the potential protective effect from vaccination: a population-based cohort study - eClinicalMedicine (thelancet.com) Peng, K., Li, X., Yang, D., Chan, S. C. W., Zhou, J., & Wan, E. Y. F. (2023).
Long-term perturbation of the peripheral immune system months after SARS-CoV-2 infection | BMC Medicine | Full Text (biomedcentral.com) Winheim, E., Rinke, L., Lutz, K., Reischer, A., Leutbecher, A., Wolfram, L., Rausch, L., Kranich, J., Wratil, P. R., Huber, J. E., Baumjohann, D., ... Krug, A. B. (2021).
Articles & Reports
How COVID-19 Changes the Immune System | Time Park, A. (2023, August 18).
How COVID-19 alters the immune system -- ScienceDaily ScienceDaily. (2021, October 28).
Impacts of COVID on the immune system (medicalxpress.com) Herrero, L. (2022, September 19).
COVID-19's impact on the immune system, and how this may affect subsequent infections - ABC News Smith, B. (2022, December 1).
COVID-19 can derange immune system; survivors have autoimmune diseases (usatoday.com) Szabo, L. (2021, March 2).
Long COVID & PASC
Summary: Long COVID is an umbrella term that refers to the onset of disabling symptoms/conditions resulting from any of the previously mentioned organ, immune system, and vascular damage sustained during infection. These conditions are also referred to as "post-acute sequelae of COVID-19" (PASC). Vaccination can reduce the damage experienced by decreasing inflammation during an infection, but Long COVID/PASC can affect anyone. This is especially true in the case of multiple infections. Your risk of developing Long COVID, or worse/new symptoms, increases with each additional infection.
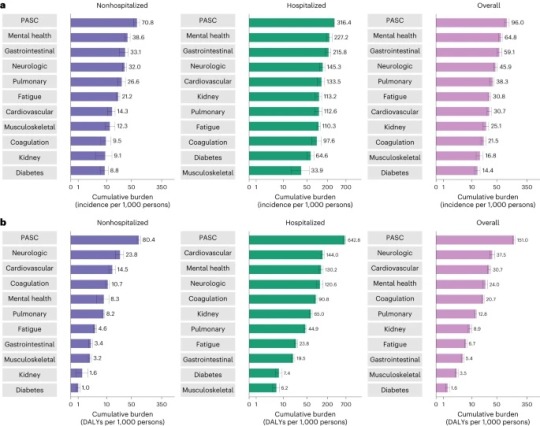
“Cumulative incidence and DALYs of postacute sequelae overall and by organ system at 2 years after infection.” (Bowe et al., 2023)
Published Research
T cell apoptosis characterizes severe Covid-19 disease - PubMed (nih.gov) André, S., Picard, M., Cezar, R., Roux-Dalvai, F., Alleaume-Butaux, A., Soundaramourty, C., Cruz, A. S., Mendes-Frias, A., Gotti, C., … Estaquier, J. (2022).
SARS-CoV-2 reservoir in post-acute sequelae of COVID-19 (PASC) | Nature Immunology Proal, A. D., VanElzakker, M. B., Aleman, S., Bach, K., Boribong, B. P., Buggert, M., Cherry, S., Chertow, D. S., Davies, H. E., Dupont, C. L., ... Wherry, E. J. (2023).
The immunology of long COVID | Nature Reviews Immunology Altmann, D. M., Whettlock, E. M., Liu, S., Arachchillage, D. J., & Boyton, R. J. (2023).
Long COVID: major findings, mechanisms and recommendations | Nature Reviews Microbiology Davis, H. E., McCorkell, L., Vogel, J. M., & Topol, E. J. (2023).
Long COVID prevalence and impact on quality of life 2 years after acute COVID-19 | Scientific Reports (nature.com) Kim, Y., Bae, S., Chang, H., & Kim, S. (2023).
Postacute sequelae of COVID-19 at 2 years | Nature Medicine Bowe, B., Xie, Y., & Al-Aly, Z. (2023).
Articles & Reports
Long COVID | NIH COVID-19 Research National Institutes of Health. (2023, June 8).
Long COVID or Post-COVID Conditions | CDC Centers for Disease Control and Prevention. (2023, July 20).
The Most Important Question About Long COVID | Harvard Medical School Pesheva, K. (2023, August 9).
Nearly One in Five American Adults Who Have Had COVID-19 Still Have "Long COVID" (cdc.gov) Centers for Disease Control and Prevention. (2022, June 22).
2 notes
·
View notes
Text
Postacute sequelae of COVID-19 (PASC), often referred to as Long COVID, has had a substantial and growing impact on the global population. Recent prevalence studies from the United States and the United Kingdom found that the complication has affected, on average, around 45 percent of survivors, regardless of hospitalization status.
No accurate tally of the number of people affected and its real global impact has yet been made, but conservative estimates of several hundred million and trillions in economic devastation would hardly be an exaggeration. Even in China, after the lifting of the Zero COVID policy late last fall and the tsunami of infections that followed, social media threads are now widespread with people complaining of chronic debilitating fatigue, heart palpitations and brain fog.
Yet, more than three years into the “forever” COVID pandemic, with Long COVID producing more than 200 symptoms, impacting nearly every organ system and causing such vast health problems for a significant population across the globe, it remains undefined and somewhat arbitrary in the clinical diagnosis. Additionally, the assurances given to study potential therapeutic agents have remained unfulfilled.
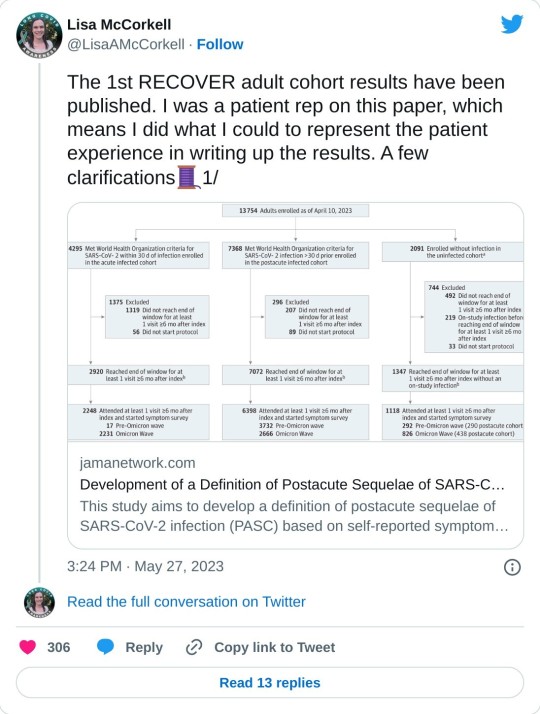
In this regard, a new Long COVID observational study called the “RECOVER [researching COVID to enhance recovery] initiative,” was published last week in the Journal of the American Medical Association, with almost 10,000 participants across the US. Funded by the National Institutes of Health (NIH), it attempts to provide a working definition for Long COVID (PASC).
While the study represents an advance from the standpoint of assessing the impact of Long COVID, and has been celebrated in media coverage, it must be viewed with several reservations and caveats. It is exclusively focused on describing the disease, rather than supporting efforts to alleviate its impact, let alone find a cure. And its definition, however preliminary, could well be misused by insurance companies and other profit-driven entities in the healthcare system to restrict diagnosis and care.
Comments by Dr. Leora Horwitz, one of the study authors and director of the Center for Healthcare Innovation and Delivery Science at New York University, give some sense of the misgivings felt by serious scientists. Horwitz stated, “This study is an important step toward defining Long COVID beyond any one individual symptom. This definition—which may evolve over time—will serve as a critical foundation for scientific discovery and treatment design.”
Certainly, a working definition that medical communities can agree on is critical. But after three years and nearly all the $1.2 billion given to the NIH already spent, one must ask how much another observational study contributes to answering pressing questions affecting patients that have not already been addressed in more than 13,000 previous reports, as tallied by the LitCOVID search engine?
Why have there been so many delays in conducting clinical trials studying potential treatments and preventative strategies in the acute phase of infection that could reduce or eliminate the post-acute sequelae? Where is the urgency at the NIH and in the Biden administration to expand funding and initiate an all-out drive to develop treatments for Long COVID like the $12.4 billion spent on the COVID vaccines?
Scoring post-acute symptoms
The findings in the recent study, published on May 25, 2023, in JAMA, titled, “Development of a Definition of Postacute Sequelae of SARS-CoV-2 Infection,” are somewhat limited and problematic in their current formulation. The authors have identified 12 primary symptoms that distinguish COVID survivors with Long COVID from those without those aftereffects. These include loss of smell or taste (8 points), post-exertional malaise (7 points), chronic cough (4 points), brain fog (3 points), thirst, (3 points), heart palpitations (2 points), chest pain (2 points), fatigue (1 point), dizziness (1 point), gastrointestinal symptoms (1 point), issues with sexual desire or capacity (1 point), and abnormal movements (1 point).
Assigning points to each of the 12 symptoms and adding them up gives a cumulative total for each patient. Anyone scoring 12 or higher would be diagnosed as afflicted with PASC, accounting for 23 percent of the total. In general, the higher the score, the greater the disability in performing daily activities.
The researchers also noted that certain symptom combinations occurred at higher rates in certain groups, leading to identifying four clusters of Long COVID based on symptomology patterns, ranging from least severe to most severe in terms of impact on quality of life. Why such clusters were seen remains uncertain.
Some symptoms were more common than others, and this did not correspond to the severity of the symptoms as measured approximately by the points. Symptoms of post-exertional malaise (87 percent), brain fog (64 percent), palpitations (57 percent), fatigue (85 percent), dizziness (62 percent), and gastrointestinal disturbances (59 percent) were most common.
The study’s lead author, Tanayott Thaweethai from Massachusetts General Hospital and Harvard Medical School, explained, “This offers a unifying framework for thinking about Long COVID, and it gives us a quantitative score we can use to understand whether people get better or worse over time.”
Andrea Foulkes, the corresponding author and principal investigator of the RECOVER Data Resource Core and professor at Harvard Medical School, said, “Now that we’re able to identify people with Long COVID, we can begin doing more in-depth studies to understand the mechanisms at play. These findings set the stage for identifying effective treatment strategies for people with Long COVID—understanding the biological underpinnings is going to be critical to that endeavor.”
The currently evolving definition could have significant implications, and not just medically. For instance, if people suffer only brain fog and post-exertional malaise and score less than 12 on their symptomology, they would not be construed as having PASC. Under such a construct, the definition could be used by employers and health insurers to deny compensation or treatment by telling people they don’t have a recognized Long COVID complication. Additionally, it is not clear how long these symptoms have to be present before the diagnosis is accepted.
Lisa McCorkell, one of the authors of the study, explained on her social media account, “If people didn’t meet the scoring threshold for PASC+, that doesn’t mean they don’t have PASC! It means they are unspecified. Unspecified includes people with Long COVID. Future iterations of the model will aim to refine this—that will include doing analysis using the updated RECOVER symptoms survey, adding in tests/clinical features and ultimately biomarkers. That is also why this isn’t meant to be an official prevalence study. The sample is not fully representative, but also, we know that there are people in the unspecified groups that have PASC.”
She continued, “It is very clear throughout the paper that in order for this to be actionable at all, iterative refinement is needed. In presenting this to NIH leadership, they are fully aware of that. But the press is not fully understanding the paper which could have dangerous downstream effects. Since the beginning of working on this paper I’ve done everything I could to ensure the model presented in this paper is not used clinically.”
Unfortunately, in the world of capitalism, such things take on a life of their own. The definitions will influence how health systems will choose to view these patients and demand their clinicians abide by prescribed diagnostic codes. This has the potential to dismiss millions with Long COVID symptoms and deny them access to potential treatments if and when they materialize.
The concerns of Elisa Perego
Dr. Elisa Perego, who suffers from Long COVID and coined the term, offered the following important observations.
In response to the publication, she wrote, “Presenting a salad of 12 symptoms, (many of which many patients might not even experience) as the most significant in #LongCOVID is also detrimental to new patients, who might be joining the community now, and might not recognize themselves in the symptom list.”
She added, “We are also in 2023. There are thousands and thousands of publications from across the world that discuss imaging, tests, clinical signs (=objective measurements), biomarkers, etc. related to acute and #LongCOVID. We have many insights into the pathophysiology already. The #LongCOVID and chronic illness community deserve more. Other diseases, including diseases linked to infections, have sadly been reduced to a checklist of symptoms in the past. This has made research, recognition, and a quest for treatment much more difficult.”
There are additional findings in the report worth underscoring as they provide a glimpse into the ever-growing crisis caused by forcing the world’s population to “live with the virus.”
Hannah Davis, a Long COVID advocate and researcher, with Dr. Eric Topol, Lisa McCorkell, and Julia Moore Vogel, wrote an important review on Long COVID in March, which was published in Nature. She said of the RECOVER study, “The overall prevalence of #LongCOVID is ten percent at six months. The prevalence for those who got Omicron (or later) AND were vaccinated is also ten percent … [However] reinfections had significantly higher levels of #LongCOVID. Even in those who had Omicron (or later) as their first infection, 9.7 percent with those infected once, but 20 percent of those who were reinfected had Long COVID at six months after infection.”
Furthermore, she said, “Reinfections also increased the severity of #LongCOVID. Twenty-seven percent of first infections were in cluster four (worst) versus 31 percent of reinfections.” These facts have considerable implications.
Immunologist and COVID advocate Dr. Anthony Leonardi wrote on these findings, “If Omicron reinfections average six months [based on current global patterns of infection], and Long COVID rates for reinfection remain 10 to 20 percent, the rate of long COVID in the USA per lifetime will be over 99.9 percent. In fact, the average person would have different manifestations of Long COVID at different times many times over. Some things reverse—like anosmia [loss of smell]. Others, like [lung] fibrosis don’t reverse so well.”
The work done by these authors deserves credit and support. Every effort to bring answers to these critical questions is vital. The criticism to be made is not directed at the researchers who work diligently putting in overtime to see the research is conducted with the utmost care and obligation it merits. Rather, it should be directed at the very institutions that have adopted “living with the virus” as a positive good for of public health.
The Biden administration neglects Long COVID
In a recent scathing critique of the Biden administration and the NIH by STAT News, Rachel Cohrs and Betsy Ladyzhets place the issue front and center. In their opening remarks, they write, “The federal government has burned through more than $1 billion to study Long COVID, an effort to help the millions of Americans who experience brain fog, fatigue, and other symptoms after recovering from a coronavirus infection. There’s basically nothing to show for it.”
They continue, “The NIH hasn’t signed up a single patient to test any potential treatments—despite a clear mandate from Congress to study them. And the few trials it is planning have already drawn a firestorm of criticism, especially one intervention that experts and advocates say may actually make some patients’ Long COVID symptoms worse.” This is in reference to a planned study where Long COVID patients would be asked to exercise as much as possible, when it has clearly been shown that such activities have exacerbated the symptoms of Long COVID patients.
As the report in STAT News explains, there has been a complete lack of accountability in how the NIH funds were used. Much of the work to run the RECOVER trial has been outsourced to major universities.
Michael Sieverts, a member of the Long COVID Patient-led Research Collaborative with expertise in federal budgeting for scientific research, told STAT, “Many of the research projects associated with RECOVER have been funded through these organizations rather than directly from the NIH. This process makes it hard to track how decisions are made or how money is spent through public databases.”
In April the Biden administration announced they were launching “Project Next Gen,” which is like the Trump-era COVID vaccine “Warp Speed Operation.” It has promised $5 billion to fund the development of the next iteration of vaccines through partnership with private-sector companies, monies freed up from prior coronavirus aid packages. Incredibly, it has left Long COVID out of the plan.
Indeed, this diverting of money back into the hands of the pharmaceuticals and selling it as the Biden administration’s continued proactive response to the ongoing pandemic, while divesting all interest in preventing or curing Long COVID, is on par with every effort the administration has made to peddle the myth that “the pandemic is really over.” Long COVID is one of the central elements of the worst public health threat in a century, in a pandemic that is far from ended.
2 notes
·
View notes
Text
The Science Behind Long COVID: Understanding The Persistent Presence Of SARS-CoV-2 Proteins
Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), has emerged as one of the most perplexing and concerning legacies of the COVID-19 pandemic. While the world gradually moves on, many individuals who recovered from their initial COVID-19 infection continue to experience debilitating symptoms. These lingering effects can manifest in the form of fatigue, cognitive…
#COVID#covid cases#Covid Patients#covid symptom#Covid symptoms#Covid-19#COVID-19 infection#Covid-19 pandemic#Epstein-Barr virus#Epstein-Barr virus (EBV)#long COVID#Long Covid cases#Long COVID patients#long covid symptoms#Long Covid Symptoms Study#Long COVID-19 Syndrome#SARS CoV 2#SARS-CoV-2 infection (PASC)#SARS-CoV-2 protein#SARS-CoV-2 proteins#SARS-CoV-2 virus#SARS-CoV-2 Virus Protein#SARS-CoV-2 virus variants#The Science Behind Long COVID: Understanding The Persistent Presence Of SARS-CoV-2 Proteins
0 notes
Text
Black Americans Are More Likely to Get Long COVID. These Clinical Trials Can Find a Cure - Published Sept 12, 2024
Millions of people worldwide, especially Black Americans, are experiencing long-term health effects after recovering from COVID-19, a condition known as Long COVID. While the initial stages of the pandemic saw significant progress in diagnosing and managing the virus itself, Long COVID remains a major public health challenge.
To address this growing concern, the National Institutes of Health (NIH) launched the Researching COVID to Enhance Recovery (RECOVER) Initiative. This initiative aims to understand, prevent, and ultimately treat Long COVID.
What is Long COVID? Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), is a condition that can develop in individuals who have recovered from COVID-19. It is characterized by a range of symptoms that persist for weeks or months after the initial infection. These symptoms can vary widely from person to person but commonly include fatigue, brain fog, shortness of breath, joint pain, chest pain, heart palpitations, and digestive problems.
The exact cause of Long COVID is still being investigated, but it is believed to be related to the body’s immune response to the virus. Some experts suggest the virus may damage organs or tissues, leading to long-term health problems. Others believe that the immune system may continue to attack the body even after the virus has been cleared, causing ongoing symptoms.
The severity and duration of Long COVID can vary greatly. Some people experience mild symptoms that resolve within a few weeks, while others suffer from severe symptoms that can significantly impact their daily lives.
Why are clinical trials for Long COVID important? There are currently no established treatments for Long COVID. Clinical trials are crucial for developing effective therapies. The RECOVER Initiative includes a program called RECOVER-CT, which is the largest national clinical trial network specifically designed to investigate treatments for Long COVID.
Why should Black Americans consider participating in Long COVID clinical trials? Studies suggest that Black Americans are disproportionately affected by Long COVID, experiencing a higher prevalence of symptoms compared to other races. Participating in clinical trials allows Black Americans to play a vital role in the development of treatments tailored to their specific needs.
What are RECOVER-CT trials studying? The RECOVER-CT program is exploring a wide range of interventions for Long COVID, including medications, rehabilitation strategies, and alternative therapies. These interventions target various Long COVID symptoms, such as fatigue, muscle aches, cognitive dysfunction, and sleep problems.
Early success and looking forward The RECOVER-CT program has already achieved significant milestones. It has initiated five clinical trial platforms, encompassing eight trials and testing thirteen interventions across more than 100 sites nationwide. The program’s success is further exemplified by the rapid enrollment of the first trial within nine months and low participant drop-out rates.
Trial's official website: www.rti.org/impact/long-covid-clinical-trials
#mask up#pandemic#covid#covid 19#wear a mask#coronavirus#public health#sars cov 2#still coviding#wear a respirator#long covid#covid is not over#covid conscious#covid is airborne
42 notes
·
View notes
Text
Understanding the Importance of Covid Microclot Testing

Introduction to Microclots and Their Significance
In recent years, COVID-19 has introduced new challenges in medical science, leading to an increased focus on microclots and their implications for patient health. Covid micro clot testing has emerged as a crucial tool in understanding the long-term effects of the virus, often referred to as post-acute sequelae of SARS-CoV-2 infection (PASC) or Long Covid. This comprehensive analysis explores the significance of microclots testing and how it helps in managing and diagnosing microclots effectively.
What Are Microclots?
Microclots are tiny blood clots that are not always visible in standard blood tests. They can disrupt blood flow and contribute to a range of health issues, particularly after a Covid-19 infection. Microclots are often found in the capillaries and can impede oxygen and nutrient delivery to various tissues and organs, potentially causing chronic symptoms and complications.
The Emergence of Covid Microclot Testing
Covid microclot testing has become essential due to the growing evidence that microclots play a significant role in the complications seen in Long Covid patients. Researchers and clinicians have observed that microclots can contribute to ongoing symptoms such as fatigue, brain fog, and cardiovascular issues. This testing aims to identify these microclots early, enabling targeted treatments and interventions.
How Does Microclots Testing Work?
Microclots testing involves advanced diagnostic techniques to detect and analyze these minute clots. Traditional blood tests may not always reveal these clots due to their small size. However, specialized assays and imaging techniques, such as microscopy and advanced clotting assays, are employed to identify and quantify the presence of microclots.
Microscopy Techniques: High-resolution microscopy allows for detailed visualization of microclots. This method can detect clots that are not visible with standard tests, providing a clearer picture of their impact on blood flow.
Advanced Clotting Assays: These assays are designed to measure clot formation and dissolution processes more precisely, offering insights into the presence and behavior of microclots in the bloodstream.
The Role of Covid Microclot Testing in Patient Care
Covid microclot testing plays a pivotal role in managing patients with Long Covid. By identifying microclots, healthcare providers can tailor treatments to address these specific issues, potentially alleviating symptoms and improving quality of life.
Tailored Treatment Plans: Understanding the presence of microclots allows for the development of personalized treatment plans. For example, anticoagulant therapies may be prescribed to manage clotting issues and reduce the risk of further complications.
Monitoring Disease Progression: Regular testing can help monitor the progression of the disease and the effectiveness of treatment. This ongoing assessment is crucial for adjusting therapies and ensuring optimal patient outcomes.
Benefits of Early Detection and Intervention
Early detection of microclots through microclots testing can lead to more effective interventions and better management of Long Covid symptoms. The benefits include:
Reduced Risk of Complications: Identifying microclots early can help prevent severe complications, such as stroke or myocardial infarction, by addressing clotting issues before they escalate.
Improved Patient Outcomes: Early intervention can lead to a more rapid and effective response to treatment, improving overall patient outcomes and quality of life.
LCA Community for Covid Microclot Testing
The LCA Community is at the forefront of advancing Covid microclot testing and promoting awareness about its importance. As a leading advocate in this field, the LCA Community is dedicated to providing cutting-edge research and resources to support both patients and healthcare providers.
Educational Resources: The LCA Community offers comprehensive resources on microclots testing, including detailed explanations of testing procedures, latest research findings, and best practices for managing microclots.
Support and Collaboration: By fostering collaboration among researchers, clinicians, and patients, the LCA Community aims to enhance the understanding and treatment of microclots. This collective effort is crucial for advancing medical knowledge and improving patient care.
Conclusion
Microclots testing is a vital component in the management and understanding of post-Covid-19 complications. As we continue to learn more about the impact of microclots on patient health, it is essential to stay informed and engage with the latest advancements in diagnostic and treatment options. The LCA Community plays a significant role in this endeavor, providing valuable support and resources to enhance our approach to COVID microclot testing and improve patient outcomes.
#covid microclot testing#long covid apheresis#apheresis treatment#long covid apheresis community#microclot testing#apheresistypes#typesofapheresis
0 notes
Text
Children and COVID is a bad combination.
6 notes
·
View notes
Text
Vaccination can prevent infection, even if it doesn’t prevent every infection.
Just because vaccination doesn’t prevent every infection with SARS-CoV-2 or every symptomatic case of COVID-19, doesn’t mean it doesn’t prevent any. Vaccination can can reduce viral load which means people may not carry enough virus to infect others.
This means that many people won’t get infected with SARS-CoV-2 after exposure. Reduced viral load can also mean milder illness. Milder illness means people won’t be so sick they need to be hospitalized. Less severe illness means many people won’t die.
Last year’s COVID-19 vaccines were 54% effective at preventing symptomatic COVID-19 compared to individuals who did not receive an updated vaccine last fall.
COVID-19 vaccines prevent between 8 and 20 million illnesses in the US every year. COVID-19 vaccines are estimated to have prevented 4-5 million hospitalizations and 400,000 - 500,000 deaths last year - and that’s with vaccination rates not exceeding 40-50% of the eligible population.
COVID-19 vaccines reduce hospitalizations by about 50%. Reduced illness severity can be the difference between managing illness at home or needing hospitalization. COVID-19 vaccines have been associated with reduced risk of developing post-acute sequelae of SARS-CoV-2 infection (PASC, colloquially long COVID).
#covid#covid 19#sars cov 2#vaccines#vaccine#vaccination#get vaccinated#long covid#tw death#illness#chronic illness#covid vaccine
1 note
·
View note
