#poor ovarian reserve
Explore tagged Tumblr posts
Text
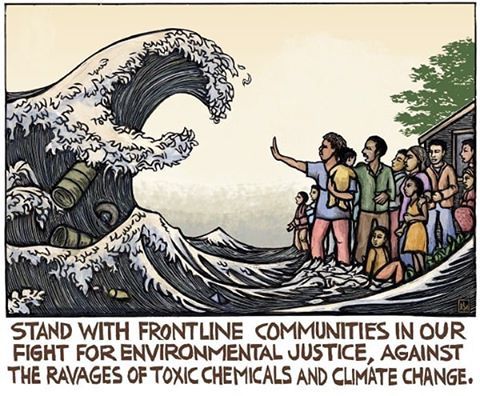
Chapter 7. Polluted Politics? Confronting Toxic Discourse, Sex Panic and Eco-Normativity by Giovanna Di Chiro
“Stereotypes and lies lodge in our bodies as surely as bullets. They live and fester there, stealing the body.”—Eli Clare
Queer ecology as defined by Mortimer-Sandilands (2005, 24) “both about seeing beauty in the wounds of the world and taking responsibility to care for the world as it is”. (200)
Environmental justice constructs an eco-politics that defines the environment as our communities: the places where ‘we live, work, play, and learn’ (200). Environmental justice activists embrace inhabited/built places---cities, villages, reservations, agricultural fields, workplaces, poor and low-income neighborhoods next to hazardous industrial facilities as environments worthy of recognition and protection (Di Chiro 1996)
There has been rising environmental anxiety that surrounds cultural fears of exposure to chemical and endocrine-disrupting toxins especially as it relates to the troubling and destabilizing of normal/natural gendered bodies of humans and other animal species aka the “chemical castration” or the “feminization of nature” (Cadbury 1998; Hayes 2002)--rising fears that we are “swimming in a sea of estrogen” (Raloff 1994b, 56; Sumpter and Jobling 1995 173) as a consequence of rising levels of estrogenic, synthetic chemical compounds emitted into our water, air and food known as estrogenic pollution (ova-pollution). (201)
Pop-science warning about the ‘instability of maleness’—warns that the rising incidences of male-to-female gender shifts and intersex conditions observed in the ‘lower’ species of animals, such as frogs, fish, and salamanders, represent the newest ‘canaries in the coalmine’ portending an uncertain fate for human maleness and for the future of ‘normal’ sexual reproduction (Robert 2003) (201) also anti-toxins discourse has concerns about estrogenic chemical toxins disrupting/preventing/disturbing ‘normal’ prenatal physiological development and natural reproductive processes, leading to rising cases of infertility and producing disabled, defective, and even monstrous bodies (201)…
What can develop is a “sex panic” that resuscitates familiar heterosexist, queerphobic, and eugenics arguments classifying some bodies as not normal: mistakes, perversions, burdens (I would add ‘freaks’)…under the guise of laudable goal/progressive goals, a certain type of anti-toxics environmentalism mobilizes knowledge/power of normalcy and normativity and reinforces compulsory social-environmental order based on a dominant regime of what and who are constructed as normal and natural (Davis 1995; Garland-Thompson 1997; McRuer 2006).
Disability becomes an environmental problem and lgbtq people become disabled—the unintended consequences of a contaminated and impure environment, unjustly impaired by chemical trespass. (202) The true scope of the mortality and morbidity of POPs (persistent organic pollutants) becomes distorted by alarmist focus. This fixation ends up de-emphasizing and worse--naturalizing and normalizing other serious health problems associated with POPs that are on the rise: breast, ovarian, prostate and testicular cancers, neurological and neurobehavioral problems, immune system breakdown, heart disease, diabetes and obesity (202).
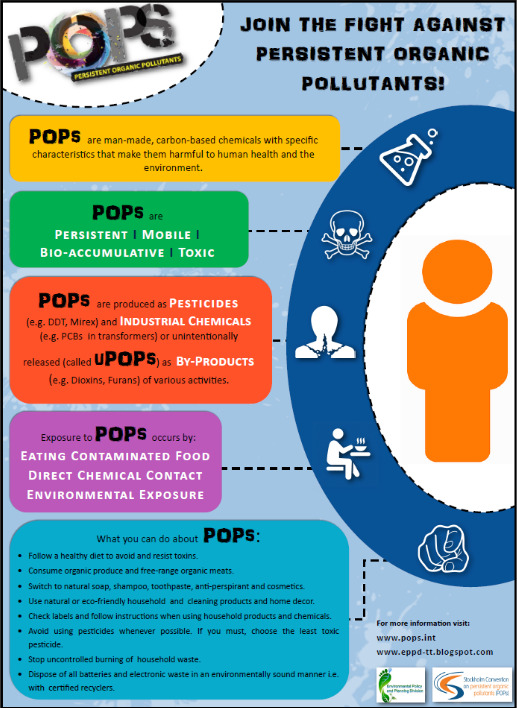
There is good reason for alarm concerning the continued use and accumulation of toxic chemicals that are wreaking havoc on the health and reproductive possibilities of the living world. Our cumulative exposures to endocrine disruptors, carcinogens, neurotoxins, asthmagens, and mutagens in our normal, everyday lives from our daily contact with plastic water bottles, shampoos, and kitchen cleaners to insect repellents, food preservatives, and factory farmed meats, among others, are most certainly putting at risk the health of our own bodies and our earth. (210) But where should the critical attention lie?
The hyperfocus on the world turning into hermaphrodites participates in a sexual titillation strategy summoning the familiar ‘crimes against’ nature’ credo and inviting culturally sanctioned homophobia while at the same time sidelining and naturalizing ‘normal’ environmental diseases such as cancer (211).
--
Environmental theory and politics in the US have historically mobilized ideas of the normal, to determine which bodies and environments/landscapes embody the distinctly American values of productive work, rugged individualism, masculinity, independence, potency, and moral virtue upon which environmental advocacy movements should be based (Haraway 1989; Cronon 1991). Critical histories of U.S. environmentalism have revealed the capitalist, patriarchal, colonialist, heteronormative, eugenicist, and ableist histories underlying its “progressive” exterior (Boag 2003; Darnovky 1992; Evans 2002; Gaard 2004; Jaquette 2005; Sutter 2001).
Eco-normativity (or eco[hetero]normativity) appear in alarmist discourse in the anti-toxins arm of the environmental movement. Their alarm about contaminants effect on sex/gender appeals to preexisting cultural norms of gender balance, normal sexual reproduction and the balance of nature. The use of “anti-normal” “anti-natural” in antitoxins discourse is highly questionable and risks reinforcing the dominant social and economic order (the forces actually responsible for environmental destruction and toxic contamination of all our bodies and environments) by naturalizing the multiple injustices that shore it up”…and thus creates what the author terms, polluted politics.
#queer ecologies: sex nature politics desire#econormativity#heteronormativity#critical ecology#queer ecology#ecology#environmental contamination#persistent organic pollutants#toxins#anti toxins#eugenics#ecofeminism#environmental politics#ecological science#environmental science
41 notes
·
View notes
Text

Anti-Müllerian Hormone (AMH) is an important marker of a woman’s ovarian reserve. Low AMH levels can be caused by advancing age, genetic factors, autoimmune disorders, endometriosis, lifestyle factors like smoking or poor diet, and certain medical treatments such as chemotherapy or ovarian surgery. Early diagnosis and expert care are essential for managing fertility.
0 notes
Text
How Many IVF Cycles Are Needed for Success?

Introduction
In vitro fertilization (IVF) has transformed fertility treatment, providing hope to couples facing conception challenges. A common question among patients is: How many IVF cycles are needed for success? The answer depends on various factors, such as age, underlying fertility issues, and the quality of treatment. This blog explores the key factors influencing IVF success rates and what couples can expect during multiple cycles. If you're looking for expert care, an IVF center in Ahmedabad can provide personalized guidance and advanced fertility solutions.
Understanding IVF Success Rates
IVF success rates are not uniform for all patients. The chances of conceiving through IVF depend on a combination of biological and medical factors. According to fertility specialists, success is often measured by live birth rates per cycle. Here’s a general breakdown based on age:
Women under 35: Around 50-60% success rate per cycle
Women aged 35-37: Around 40-50% success rate per cycle
Women aged 38-40: Around 25-35% success rate per cycle
Women over 40: Below 20% success rate per cycle
These rates indicate that younger women have a higher likelihood of success per cycle, but multiple cycles may still be necessary.
How Many IVF Cycles Are Typically Needed?
Studies suggest that the cumulative success rate increases with multiple IVF cycles. On average:
1 Cycle: Approximately 33-40% of couples conceive
2 Cycles: The cumulative success rate increases to around 60%
3 Cycles: Around 70-75% of couples achieve pregnancy
4-6 Cycles: The success rate can reach 80-90%
Many fertility clinics recommend at least three cycles for the best chances of success, as each cycle provides more opportunities for viable embryo implantation.
Factors Affecting IVF Success
Several factors determine how many cycles a couple may need, including:
1. Age of the Woman
Younger women generally have a higher number of high-quality eggs, improving success rates. Women over 40 may require more cycles or consider donor eggs.
2. Ovarian Reserve
A woman’s Anti-Müllerian Hormone (AMH) levels and Antral Follicle Count (AFC) help assess ovarian reserve. A lower ovarian reserve may mean fewer eggs retrieved, requiring additional cycles.
3. Embryo Quality
Embryos with chromosomal abnormalities are less likely to implant. Preimplantation genetic testing (PGT) can improve the selection of healthy embryos, potentially reducing the number of required cycles.
4. Underlying Medical Conditions
Conditions such as polycystic ovary syndrome (PCOS), endometriosis, or uterine fibroids can impact implantation and may necessitate more cycles.
5. Male Factor Infertility
If sperm quality is poor, techniques like Intracytoplasmic Sperm Injection (ICSI) may be needed, which could affect success rates.
6. Lifestyle Factors
Smoking, obesity, stress, and poor diet can affect fertility. Optimizing health before IVF can improve the chances of success in fewer cycles.
Financial Considerations
IVF treatment is expensive, and the cost per cycle can vary by country and clinic. Some couples opt for IVF refund programs or multi-cycle packages to manage costs effectively. Insurance coverage may also impact how many cycles couples can afford.
Emotional and Physical Aspects
IVF is physically and emotionally demanding. Couples may experience stress, anxiety, and financial strain. Support groups and counseling can help manage expectations and emotional challenges during multiple cycles.
Conclusion
While some couples may achieve pregnancy in their first IVF cycle, many require multiple attempts. On average, three IVF cycles at an IVF Hospital in Ahmedabad provide a strong chance of success, though individual factors influence the outcome. Consulting a fertility specialist for personalized advice is essential. With patience, perseverance, and medical support, IVF can be a successful path to parenthood for many couples.
#ivf center in ahmedabad#ivf doctor in ahmedabad#ivf hospital in ahmedabad#ivf center#best ivf treatment in ahmedabad#ivf treatment in ahmedabad#best ivf hospital in ahmedabad#ivf doctor#ivf specialist#ivf treatment
0 notes
Text
Who Should Consider ICSI? Key Indicators for This Fertility Treatment
Infertility is a challenging journey, but advancements in assisted reproductive technology have made parenthood possible for many couples. One such revolutionary procedure is Intracytoplasmic Sperm Injection (ICSI), a specialized form of In Vitro Fertilization (IVF) designed to address specific infertility issues. But who should consider ICSI? Let’s explore the key indicators that make this treatment the right choice for certain couples.
What is ICSI?
ICSI, or Intracytoplasmic Sperm Injection, is an advanced fertility treatment where a single, healthy sperm is directly injected into an egg to facilitate fertilization. This procedure is particularly beneficial for couples facing male factor infertility or cases where conventional IVF has not been successful.
If you are seeking ICSI infertility treatment in Bangalore, Kangaroo Care Fertility offers state-of-the-art facilities and experienced specialists to guide you through the process.
Key Indicators for ICSI Treatment
1. Severe Male Factor Infertility
Male infertility is one of the most common reasons couples opt for ICSI. This includes cases where:
Sperm count is extremely low (Oligospermia)
Sperm motility is poor (Asthenospermia)
Sperm morphology is abnormal (Teratospermia)
There is a complete absence of sperm in the ejaculate (Azoospermia), requiring sperm retrieval procedures like TESA or PESA
ICSI helps overcome these challenges by directly injecting a selected sperm into the egg, increasing the chances of fertilization.
2. Previous IVF Failure
Couples who have undergone conventional IVF but failed to achieve fertilization may benefit from ICSI. If the eggs and sperm do not naturally fertilize in a standard IVF cycle, ICSI can offer a more controlled and targeted approach, ensuring better results.
3. Unexplained Infertility
When no clear cause of infertility is identified despite thorough medical evaluations, ICSI can be a recommended treatment. Some cases of unexplained infertility may be due to subtle sperm abnormalities or egg-sperm interaction issues that are not easily detected through standard tests.
4. Poor Egg Quality or Low Ovarian Reserve
Women with poor egg quality or a diminished ovarian reserve often require specialized techniques to improve their chances of successful fertilization. Since ICSI involves selecting the best sperm and directly injecting it into the egg, it can enhance the probability of fertilization in such cases.
5. Genetic Concerns
Couples with a history of genetic disorders that could be passed on to their child may choose ICSI along with Preimplantation Genetic Testing (PGT). This ensures that only genetically healthy embryos are selected for implantation, reducing the risk of hereditary diseases.
6. Use of Frozen Sperm or Eggs
In cases where frozen sperm or eggs are used for fertility treatment, ICSI can help improve fertilization rates. Since thawed sperm may have lower motility compared to fresh sperm, direct injection into the egg increases the chances of successful fertilization.
7. Surgical Sperm Retrieval
Men who have undergone vasectomy, testicular failure, or other conditions that prevent sperm from being present in the ejaculate can still conceive with ICSI. Techniques such as Testicular Sperm Aspiration (TESA) or Percutaneous Epididymal Sperm Aspiration (PESA) allow sperm retrieval directly from the testicles or epididymis, which can then be used in ICSI.
Why Choose Kangaroo Care Fertility for ICSI?
If you are considering ICSI infertility treatment in Bangalore, choosing the right fertility clinic is crucial for success. At Kangaroo Care Fertility, our expert team of specialists offers:
Advanced diagnostic and fertility treatment options
High success rates in ICSI procedures
Personalized treatment plans tailored to individual needs
A compassionate and supportive approach to your fertility journey
Conclusion
ICSI is a highly effective treatment for couples facing male infertility, previous IVF failure, unexplained infertility, and other reproductive challenges. Understanding the key indicators for ICSI can help couples make informed decisions about their fertility treatment. If you are exploring ICSI infertility treatment in Bangalore, consult the experts at Kangaroo Care Fertility for a comprehensive evaluation and personalized treatment plan to maximize your chances of success.
0 notes
Text
PRP Success in IVF Treatment: A Game-Changer for Fertility Hope
For the average infertile couple, every cycle that does not work is a struggle against the odds. The physical, financial, and emotional cost of IVF is huge. Imagine if it was possible to improve success rates through the body's own healing capabilities. That's where PRP success in IVF treatment is making headlines.
Platelet-Rich Plasma (PRP) therapy is changing the arena of reproductive medicine, ushering new hope for patients who have experienced thin endometrial lining, poor ovarian reserve, or repeated implantation failure. In cosmopolitan metro cities such as Mumbai, where expensive fertility treatments are easily accessible, PRP therapy in Mumbai has become popular among top IVF specialists.

Here, we are going to see how PRP works, its benefits in IVF, and why it is gaining such popularity with patients seeking a successful pregnancy.
Understanding PRP in IVF: How It Works
PRP therapy utilizes the body’s natural growth factors to enhance tissue regeneration. It involves:
Drawing a small amount of the patient’s blood
Processing it to concentrate platelets rich in growth factors
Injecting the PRP into the ovaries or uterus to stimulate healing and improve fertility conditions
This technique is particularly beneficial for women with:
Thin Endometrial Lining – A healthy endometrium is crucial for embryo implantation. PRP helps by improving blood flow and promoting tissue regeneration.
Poor Ovarian Reserve – PRP can rejuvenate aging ovaries, potentially increasing egg quality and response to stimulation.
Repeated IVF Failures – Women who have experienced multiple implantation failures may benefit from PRP’s ability to enhance uterine receptivity.
The natural approach of PRP is what makes it stand out—it harnesses the body’s healing abilities to create a more favorable environment for pregnancy.
PRP Success in IVF Treatment: What the Research Says
PRP therapy is not just a trend; scientific research supports its effectiveness. Clinical studies have shown that PRP can significantly improve implantation rates and endometrial thickness.
A study published in the Journal of Assisted Reproduction and Genetics found that PRP treatment improved endometrial thickness in women who previously had inadequate lining for embryo transfer.
Another study in the International Journal of Reproductive BioMedicine observed increased ovarian response in women with poor ovarian reserve after undergoing PRP therapy.
These findings demonstrate why leading fertility specialists are integrating PRP into their IVF protocols, helping patients who previously had limited options.
Why PRP Therapy in Mumbai Is Gaining Popularity
Mumbai has emerged as a hub for advanced fertility treatments, with some of the country’s top IVF specialists adopting PRP therapy. Here’s why couples are opting for PRP therapy in Mumbai:
Expertise and Innovation – Mumbai’s fertility clinics stay at the forefront of reproductive medicine, ensuring the latest techniques are available.
Personalized Treatment Plans – IVF specialists assess each patient’s unique needs before recommending PRP, ensuring a customized approach.
Comprehensive Care – Clinics provide holistic fertility solutions, integrating PRP with IVF, ICSI, and even LIT therapy clinics in Mumbai for immune-related infertility cases.
The accessibility of advanced procedures, combined with world-class expertise, makes Mumbai an ideal destination for fertility treatments.
How PRP Enhances IVF Success Rates
PRP therapy directly impacts some of the most critical factors influencing IVF outcomes:
1. Endometrial Receptivity
A thick, well-vascularized endometrial lining is essential for successful implantation. PRP helps create the optimal environment for an embryo to attach and develop.
2. Ovarian Rejuvenation
For women with low ovarian reserve, PRP injections in the ovaries may enhance egg quality and improve response to ovarian stimulation.
3. Reduction in Recurrent Implantation Failure
Patients who have experienced multiple failed IVF attempts can benefit from PRP’s regenerative effects, improving their chances of implantation in subsequent cycles.
4. Minimal Risks, Maximum Benefits
Since PRP is derived from the patient’s own blood, the risk of adverse reactions is minimal, making it a safe complementary treatment.
PRP & LIT Therapy: A Powerful Combination for Immunological Infertility
While PRP acts on tissue regeneration, LIT Therapy clinics Mumbai also offer yet another new treatment—Lymphocyte Immunotherapy (LIT). LIT aids women with immune-related implantation failure by habituating the body to accept the embryo. PRP + LIT can be a game-changer for couples with unexplained infertility.
PRP enhances the uterine lining and promotes a receptive environment.
LIT therapy modulates the immune system, reducing the risk of rejection.
Together, these therapies provide a comprehensive approach to tackling complex infertility cases.
Is PRP Right for You?
PRP therapy is particularly beneficial for:
Women with thin endometrial lining resistant to standard treatments
Those with low ovarian reserve looking for improved egg quality
Patients with recurrent implantation failure despite good-quality embryos
Couples seeking natural, regenerative solutions to boost IVF success
While PRP is not a guarantee for pregnancy, it significantly enhances the chances of a successful embryo implantation.
PRP Success in IVF Treatment
Many patients who had lost hope have experienced success with PRP-enhanced IVF cycles. The treatment has shown remarkable results in improving endometrial lining, enhancing ovarian response, and increasing implantation rates. Success stories from individuals who previously faced repeated IVF failures highlight the effectiveness of PRP in reproductive medicine.
Conclusion: The Future of PRP in IVF
The increasing PRP success in IVF therapy is indicative of the manner in which regenerative medicine is revolutionizing fertility treatment. Through increasing research and clinical application, PRP treatment continues to open doors for couples who previously had few choices.
In cities like Mumbai, with third-generation reproductive technologies available, PRP is gaining popularity as an adjunct that is needed in IVF protocols. Whether it is to increase receptivity of the endometrium, increase ovarian function, or play a role in immune therapies like LIT therapy clinics Mumbai, PRP is emerging as a viable fertility treatment option.
If you are considering IVF and are curious about the new techniques to increase your success, PRP therapy could be the solution you are seeking. Discuss with a fertility specialist today how this groundbreaking therapy can aid your journey to parenthood.
Source: https://justpaste.it/euneu
0 notes
Text
When Should You Consider IVF? Key Signs & Medical Advice
For many couples struggling with infertility, IVF (In Vitro Fertilization) is a hopeful solution. However, knowing when to consider IVF can be challenging. Understanding the right time to opt for IVF can make the process smoother and more effective. In this blog, we will discuss key signs that indicate you may need IVF, along with expert medical advice.

What is IVF?
IVF is a fertility treatment where eggs are retrieved from the woman’s ovaries and fertilized with sperm in a lab. The resulting embryos are then transferred to the uterus, increasing the chances of pregnancy. IVF is widely offered at a reputed Fertility Center in Indore and is a popular choice for couples facing infertility.
Key Signs That Indicate You Should Consider IVF
If you are trying to conceive naturally but facing difficulties, here are some key signs that suggest IVF might be the right option for you.
1. Age-Related Infertility
A woman’s fertility declines with age, especially after 35. The quality and quantity of eggs decrease, making natural conception difficult. If you are in your late 30s or early 40s and unable to conceive, IVF can help improve your chances of pregnancy.
2. Blocked or Damaged Fallopian Tubes
The fallopian tubes play a crucial role in conception by allowing the sperm to meet the egg. If the tubes are blocked or damaged due to infections, surgeries, or endometriosis, IVF is a good option as it bypasses the tubes entirely.
3. Low Sperm Count or Poor Sperm Quality
Male infertility is a major reason for conception difficulties. If the sperm count is low or the sperm have poor motility, natural fertilization becomes harder. IVF with Intracytoplasmic Sperm Injection (ICSI) helps in such cases by directly injecting the sperm into the egg.
4. Endometriosis
Endometriosis is a condition where the tissue that lines the uterus grows outside it, affecting fertility. Women with severe endometriosis may struggle to conceive naturally, making IVF a recommended option.
5. Polycystic Ovary Syndrome (PCOS)
PCOS is a common hormonal disorder that causes irregular ovulation. Women with PCOS often have difficulty conceiving due to ovulation problems. IVF can be an effective treatment by stimulating egg production and fertilization.
6. Unexplained Infertility
Sometimes, couples face infertility without a clear medical reason. When all tests appear normal, but conception does not happen, IVF is often suggested as a solution.
7. Multiple Failed IUI Attempts
Intrauterine Insemination (IUI) is a less invasive fertility treatment. However, if a couple undergoes multiple IUI cycles without success, doctors often recommend moving to IVF for better chances of pregnancy.
8. Recurrent Miscarriages
If a woman has experienced multiple miscarriages, IVF can help by ensuring better embryo selection and improving the chances of a successful pregnancy.
Medical Advice on When to Start IVF
1. Consult an Infertility Specialist
Before deciding on IVF, consult an infertility specialist in Indore who can guide you based on your medical history and test results. A proper diagnosis can help determine if IVF is the right option.
2. Undergo Fertility Tests
Both partners should undergo fertility tests to identify the exact cause of infertility. Common tests include hormonal tests, ultrasound, semen analysis, and ovarian reserve testing.
3. Understand IVF Costs and Success Rates
The cost of IVF can vary based on the clinic, the number of cycles required, and additional treatments. Many couples research IVF cost in Indore before beginning treatment to plan their finances accordingly. Additionally, understanding success rates can help set realistic expectations.
4. Choose a Reputed IVF Center
Selecting the right fertility clinic is crucial. A Top IVF center in Indore will offer advanced technology, experienced specialists, and high success rates, ensuring the best possible outcome for your treatment.
Why Choose IVF?
IVF is one of the most advanced fertility treatments available. Here are some benefits:
Helps couples with severe fertility issues.
Increases the chances of pregnancy when natural methods fail.
Allows for genetic screening of embryos to ensure a healthy pregnancy.
Provides hope for couples with previous pregnancy failures.
Finding the Best IVF Treatment
If you are considering IVF, selecting a trusted fertility clinic is essential. A Best IVF Center in Indore will provide comprehensive fertility treatments, from initial consultation to embryo transfer. Experienced specialists and advanced technology improve the chances of a successful pregnancy.
Conclusion
IVF is a life-changing option for couples facing infertility. If you have been trying to conceive without success, it may be time to consult an IVF center in Indore to explore your options. With the right guidance, medical support, and treatment, you can take a step closer to parenthood. Remember, early diagnosis and timely intervention increase the chances of success, so do not hesitate to seek professional help.
0 notes
Text
Best Women’s Infertility Treatment In Thrissur

Infertility is a growing concern among women worldwide, and seeking the right specialist is crucial in overcoming this challenge. If you are looking for the most advanced women’s infertility treatment in Thrissur, Dr. Praveen R stands out as a leading expert. With years of experience in gynecological laparoscopy, fertility-enhancing surgeries, and hysteroscopy procedures, he has helped countless women fulfill their dream of motherhood. His compassionate approach and dedication to reproductive health ensure that every patient receives personalized care. From diagnosing underlying causes of infertility to providing cutting-edge treatments, Dr. Praveen R remains committed to helping women achieve successful pregnancies and improve their reproductive well-being.
Understanding Infertility in Women
Infertility is defined as the inability to conceive after one year of unprotected intercourse. Several factors contribute to female infertility, including hormonal imbalances, structural abnormalities, ovulation disorders, and underlying medical conditions. Lifestyle factors such as stress, poor diet, and lack of exercise can also play a significant role. Seeking early women’s infertility treatment in Thrissur can improve the chances of successful conception by addressing these issues through medical interventions, lifestyle modifications, and specialized treatments tailored to each patient’s unique condition. consult us today
Causes of Female Infertility
Ovulation Disorders: Conditions like PCOS (Polycystic Ovary Syndrome) can disrupt ovulation, leading to irregular or absent menstrual cycles, making it difficult to conceive naturally.
Fallopian Tube Blockage: Often caused by infections, surgeries, or endometriosis, blocked tubes prevent the egg from meeting the sperm, reducing pregnancy chances significantly.
Uterine Abnormalities: Issues like fibroids, polyps, or a septate uterus can hinder implantation, affecting the ability to carry a pregnancy to term and increasing the risk of miscarriage.
Endometriosis: A painful condition where uterine tissue grows outside the uterus, leading to scarring, inflammation, and interference with ovulation and implantation.
Hormonal Imbalances: Affecting ovulation and menstrual cycles, conditions like thyroid disorders, high prolactin levels, or insulin resistance can severely impact fertility.
Age-Related Factors: Fertility naturally declines with age due to a decrease in ovarian reserve and egg quality, increasing the chances of miscarriage and chromosomal abnormalities.
Dr. Praveen R specializes in diagnosing and treating these conditions with advanced techniques to ensure the best women’s infertility treatment in Thrissur.
Advanced Infertility Treatments by Dr. Praveen R
Dr. Praveen R specializes in cutting-edge infertility treatments tailored to address a wide range of reproductive challenges. With a patient-first approach, he ensures that every woman receives comprehensive care and the latest advancements in fertility treatments. His expertise in laparoscopic and hysteroscopic procedures has helped numerous women conceive successfully. By combining state-of-the-art technology with personalized treatment plans, Dr. Praveen R remains a trusted name in women’s infertility treatment in Thrissur. His commitment to excellence ensures optimal outcomes for couples struggling with infertility.
Dr. Praveen R offers a comprehensive range of treatments for infertility, including minimally invasive laparoscopic and hysteroscopic procedures. Let’s explore some of the key treatments available:
1. Laparoscopic Procedures for Infertility
Laparoscopy is a minimally invasive technique used to diagnose and treat various gynecological conditions affecting fertility. Women’s infertility treatment in Thrissur has significantly advanced with laparoscopic methods, offering high precision and faster recovery for patients.
Laparoscopic Hysterectomy: Used in cases where uterine abnormalities impact fertility. This procedure minimizes scarring and promotes quicker healing compared to traditional surgery.
Myomectomy: Surgical removal of fibroids while preserving the uterus, crucial for conception. Laparoscopic myomectomy allows women to maintain their reproductive potential with minimal downtime.
Ovarian Cystectomy: Removes cysts that may interfere with ovulation. This procedure is essential in preventing cyst-related complications that could hinder fertility.
Endometriosis Surgery: Treats endometriosis to improve implantation rates. Laparoscopic techniques effectively remove endometrial growths, reducing pain and increasing pregnancy chances.
Tubal Recanalization: Reopening blocked fallopian tubes to restore fertility. This procedure is crucial for women who have previously undergone tubal ligation or have suffered tubal blockages due to infections.
Ectopic Pregnancy Management: Ensures safe treatment of ectopic pregnancies, preventing future complications. Laparoscopic intervention helps in preserving reproductive organs and reducing risks for future pregnancies.
Adenomyomectomy: Removes adenomyosis, which can impact implantation. This surgical method enhances uterine health and significantly improves fertility outcomes.
2. Hysteroscopy for Infertility Treatment
Hysteroscopy is another vital technique in women’s infertility treatment in Thrissur that allows direct visualization and treatment of uterine abnormalities. This minimally invasive approach enables precise diagnosis and treatment, leading to improved pregnancy rates and better reproductive health outcomes.
Myomectomy for Submucosal Fibroids: Helps eliminate fibroids that impact implantation, ensuring a smoother uterine lining for embryo attachment.
Endometrial Polyp Removal: Ensures a healthy uterine environment for pregnancy by removing polyps that can interfere with embryo implantation.
Septoplasty & Metroplasty: Corrects structural abnormalities within the uterus, enhancing its shape and improving the chances of carrying a pregnancy to term.
Cornual Cannulation: Opens blocked fallopian tubes to enhance fertility, a crucial step for women facing tubal factor infertility.
Adhesiolysis: Removes uterine adhesions that may cause infertility, restoring a healthy endometrial lining necessary for conception and implantation.
Why Choose Dr. Praveen R for Women’s Infertility Treatment in Thrissur?
Expertise & Experience: With years of dedicated practice, Dr. Praveen R has mastered fertility-enhancing surgical techniques and has successfully treated a wide range of infertility cases.
State-of-the-Art Facilities: Treatments are conducted in leading hospitals, including Aswini Hospital, West Fort Hospital, and Bhavana Health Care, ensuring access to the best medical infrastructure.
Patient-Centered Approach: Each treatment plan is personalized based on individual needs, considering factors such as medical history, lifestyle, and fertility goals.
Advanced Minimally Invasive Procedures: Reducing recovery time and improving success rates, ensuring women can return to their daily activities with minimal discomfort.
Comprehensive Care: From initial diagnosis to treatment and post-surgical care, Dr. Praveen R provides ongoing support, guidance, and counseling to help couples navigate their fertility journey effectively.
High Success Rates: A proven track record of helping women conceive through cutting-edge treatments and advanced reproductive techniques.
Holistic Approach: Emphasizing not only medical treatments but also lifestyle modifications, nutritional guidance, and stress management for improved fertility outcomes.?
The Journey to Parenthood: What to Expect?
Embarking on the journey to parenthood can be an emotional and transformative experience. Understanding the steps involved in women’s infertility treatment in Thrissur helps patients feel more prepared and confident. With expert care from Dr. Praveen R, each stage of the treatment process is designed to offer clarity, comfort, and the best possible chances of success.?
When seeking women’s infertility treatment in Thrissur, the journey involves several steps that require careful planning, medical expertise, and emotional resilience. Each stage plays a crucial role in identifying the root causes of infertility and providing targeted solutions. Under the guidance of Dr. Praveen R, patients receive comprehensive care that enhances their chances of conception and a successful pregnancy.
Initial Consultation: A thorough evaluation of medical history and fertility challenges.
Diagnostic Tests: Including ultrasound, hormone analysis, and hysteroscopy.
Personalized Treatment Plan: Based on diagnosis, the best approach is chosen.
Surgical or Non-Surgical Treatment: Depending on the cause of infertility.
Post-Treatment Follow-Up: Ensuring optimal recovery and fertility success.
Finding the Right Infertility Specialist in Thrissur
Choosing the right doctor is crucial for successful treatment. Dr. Praveen R, with his vast expertise and compassionate approach, has become the go-to specialist for women’s infertility treatment in Thrissur. His patient-centric care, advanced surgical techniques, and commitment to improving reproductive health make him a trusted name in the field. Many couples have found hope and success under his guidance, benefiting from state-of-the-art treatments and a supportive healthcare environment.
Who is a Suitable Candidate for Infertility Treatment?
If you’ve been trying to conceive for a year (or six months if you’re over 35) without success, or if you have irregular menstrual cycles, recurrent miscarriages, or underlying reproductive conditions, you may benefit from women’s infertility treatment in Thrissur. Suitable candidates include:
Women with irregular or absent menstrual cycles
Those diagnosed with conditions like PCOS or endometriosis
Women with a history of pelvic infections or surgeries
Individuals with recurrent miscarriages
Couples experiencing unexplained infertility
Those considering fertility preservation before cancer treatments
Women with a family history of early menopause or diminished ovarian reserve
Those who have undergone multiple unsuccessful attempts with assisted reproductive techniques (ART)
Women with autoimmune disorders that may impact fertility
Individuals suffering from chronic medical conditions such as diabetes or thyroid disorders, which can affect reproductive health
Dr. Praveen R provides a comprehensive evaluation to determine the most effective treatment plan based on each patient’s medical history and condition.
Infertility Treatment Cost in Thrissur
The cost of women’s infertility treatment in Thrissur depends on various factors, including the complexity of the treatment, the need for surgical intervention, and the choice of fertility procedures. Some key elements influencing costs include:
Diagnostic tests
Medication and hormone therapy
Surgical procedures
Assisted reproductive techniques
Additional fertility-enhancing treatments like ovarian stimulation, embryo freezing, and genetic testing
Post-procedure follow-ups and monitoring to optimize treatment outcomes
What Should I Expect During Infertility Treatment?
If you choose women’s infertility treatment in Thrissur, your journey typically involves several crucial stages. From the initial consultation to post-treatment follow-ups, each step is designed to enhance fertility outcomes and increase the chances of conception. By opting for advanced treatments under the expertise of Dr. Praveen R, you receive a holistic approach that not only focuses on medical intervention but also considers lifestyle modifications, emotional well-being, and personalized care plans. The journey may be challenging, but with the right support and guidance, achieving parenthood becomes a real possibility.
1. Initial Consultation & Diagnosis
2. Treatment Plan Development
3. Assisted Reproductive Techniques (ART)
4. Follow-up & Monitoring
Questions to Ask Your Fertility Specialist
Before starting women’s infertility treatment in Thrissur, it’s essential to ask:
What could be causing my infertility?
What diagnostic tests do I need?
What treatment options are available for my condition?
What are the success rates of each treatment?
What are the risks or side effects of the treatment?
How many cycles of treatment should I try before considering other options?
What lifestyle changes can improve my fertility?
Are there alternative treatments or complementary therapies?
Dr. Praveen R ensures that all your questions are answered and that you feel confident about your fertility journey.
For consultations and appointments, contact Dr. Praveen R at:
Aswini Hospital | West Fort Hospital | Bhavana Health Care Call: +91 80893 33651
FAQ
What are the common causes of infertility in women?
Female infertility can be caused by ovulation disorders, blocked fallopian tubes, uterine abnormalities, endometriosis, hormonal imbalances, and age-related factors.
When should I consult a fertility specialist?
If you have been trying to conceive for over a year (or six months if over 35), or have irregular cycles, painful periods, or previous reproductive health issues, it’s best to consult a specialist.
What diagnostic tests are performed to evaluate infertility?
Common tests include ultrasound scans, hormone level assessments, hysterosalpingography (HSG) for tube blockages, hysteroscopy for uterine examination, and semen analysis for the partner.
What is the role of laparoscopic surgery in infertility treatment?
Laparoscopy helps diagnose and treat conditions like endometriosis, fibroids, ovarian cysts, and blocked fallopian tubes, improving the chances of natural conception.
How does hysteroscopy help in improving fertility?
Hysteroscopy allows direct visualization of the uterus to remove fibroids, polyps, adhesions, and correct structural abnormalities that may hinder implantation.
Are fertility treatments painful?
Most fertility treatments, including laparoscopy and hysteroscopy, are minimally invasive with mild discomfort and quick recovery times. Some medications and procedures may cause temporary side effects.
How effective are fertility treatments in Thrissur?
Success rates depend on age, underlying conditions, and the type of treatment. With expert care from specialists like Dr. Praveen R, many women achieve successful pregnancies.
Can lifestyle changes improve fertility?
Yes. Maintaining a healthy weight, eating a balanced diet, managing stress, avoiding smoking and alcohol, and regular exercise can improve fertility outcomes.
Is infertility treatment expensive?
Costs vary based on the procedure, medication, and hospital facilities. Consulting with a specialist like Dr. Praveen R helps determine the most cost-effective treatment plan.
Where can I get the best infertility treatment in Thrissur?
Dr. Praveen R provides expert infertility treatments at Aswini Hospital, West Fort Hospital, and Bhavana Health Care in Thrissur.
0 notes
Text
Can Ovarian Egg Rejuvenation (PRP Treatment) Improve Egg Quality?

Ovarian egg rejuvenation, also known as PRP (Platelet-Rich Plasma) therapy, is gaining popularity as a potential solution for women experiencing infertility or diminished ovarian reserve. But does it really work? Can PRP therapy improve egg quality? In this blog, we’ll explore the science behind ovarian PRP treatment and how it may benefit women seeking fertility treatments.
What is Ovarian PRP Treatment?
Ovarian PRP therapy is a cutting-edge procedure that involves using a woman’s own blood plasma, enriched with platelets, to rejuvenate the ovaries and potentially improve egg quality. The plasma is injected into the ovaries, where growth factors in the platelets can stimulate the growth of new, healthy eggs.
How Does PRP Therapy Work for Egg Quality?
PRP therapy works by increasing the blood supply to the ovaries, which can improve the environment for egg production. The platelets contain growth factors that encourage the regeneration of ovarian tissue and enhance follicular development. This can lead to better-quality eggs and possibly an improvement in fertility.
Does Ovarian PRP Improve Egg Quality?
While research on the effectiveness of ovarian PRP treatment is still in its early stages, some studies and patient testimonials suggest that PRP therapy may have a positive impact on egg quality. Women with reduced ovarian reserve or poor egg quality may benefit the most from this procedure, as it can potentially increase the chances of achieving a successful pregnancy.
Benefits of Ovarian PRP Therapy
Improved Egg Quality: Helps stimulate the ovaries to produce healthier eggs.
Enhanced Ovarian Function: Can improve ovarian reserve and function, especially in women with diminished ovarian reserve.
Non-Invasive: A minimally invasive procedure with fewer risks compared to traditional fertility treatments.
PRP Therapy for Infertility in Indore
For women in Indore seeking fertility treatments, PRP therapy for infertility in Indore is an option worth considering. Several fertility clinics in the region offer this innovative treatment, providing hope for those struggling with infertility due to poor egg quality.
Ovarian PRP therapy holds promise as a revolutionary treatment for improving egg quality and enhancing fertility. If you're struggling with infertility or egg quality issues, consulting with an infertility center in Indore, might be your next step in exploring whether PRP therapy could benefit you.
#prp therapy for infertility in indore#prp therapy for infertility indore#best prp therapy for infertility in indore#best prp therapy for infertility indore#infertility center in indore#infertility clinic in indore#best infertility clinic in indore#indore infertility clinic#infertility doctor in indore#infertility specialist in indore
0 notes
Text
How Pollution & Climate Change Affect Fertility Rates in 2025

Introduction
In 2025, the alarming effects of pollution and climate change on fertility rates have become a growing concern worldwide. Scientific research highlights how air pollution, rising global temperatures, and environmental toxins are disrupting reproductive health for both men and women. The link between climate change and infertility is no longer a theory but a reality affecting millions.
The Link Between Pollution & Declining Fertility Rates
Pollution, especially airborne toxins and industrial waste, has been found to directly impact fertility. Studies indicate that high levels of PM2.5, nitrogen oxides, and carbon monoxide can lead to:
✅ Reduced sperm count and motility in men
✅ Irregular menstrual cycles and ovulation disorders in women
✅ Increased risk of miscarriage and pregnancy complications
✅ Hormonal imbalances affecting overall reproductive health
How Climate Change is Disrupting Reproductive Health in 2025
Global warming is leading to extreme weather conditions, which negatively impact fertility. Heat stress and rising temperatures have been linked to:
🔥 Lower testosterone levels and decreased sperm quality
🔥 Disruptions in menstrual cycles due to thermal stress
🔥 Higher risks of congenital disabilities and preterm births
🔥 Altered pregnancy outcomes due to environmental stressors
Air Pollution & Infertility: What You Need to Know
Airborne pollutants, such as heavy metals, pesticides, and industrial chemicals, act as endocrine disruptors—chemicals that interfere with hormonal function. This exposure can lead to:
🌿 Early menopause and reduced ovarian reserve in women
🌿 DNA damage in sperm leading to infertility
🌿 Lower implantation rates during IVF treatments
🌿 Higher risks of pregnancy loss due to poor embryo development
Extreme Heat & Sperm Count: The Hidden Crisis
A major fertility crisis in 2025 is linked to rising global temperatures. Studies show that sperm count declines significantly when exposed to temperatures above 35°C (95°F). Heatwaves and urban heat islands further worsen the situation, leading to:
🔹 Reduced sperm viability and motility
🔹 Lower testosterone production
🔹 Increased testicular dysfunction
🔹 Reduced chances of natural conception
Hormonal Imbalances Due to Environmental Toxins
Many plastics, pesticides, and chemicals in the environment contain endocrine-disrupting compounds (EDCs) that mimic or block natural hormones. These include:
🔸 BPA & Phthalates (found in plastics) – Disrupt estrogen & testosterone balance
🔸 Dioxins & PCBs (industrial waste) – Reduce ovarian function
🔸 Pesticides & Herbicides – Cause sperm abnormalities
Plastic & Fertility: The Silent Threat of Microplastics
In 2025, scientists discovered microplastics in human blood, placenta, and reproductive organs. These microplastics are leading to:
♻️ Lower egg quality and increased miscarriage rates
♻️ Hormonal disruption affecting fertility treatments
♻️ Poor sperm morphology and function
♻️ Long-term reproductive health concerns for future generations
Can Climate Change Lead to Global Fertility Decline?
With fertility rates dropping in polluted regions, experts predict that by 2030, climate change could be a leading cause of global infertility. Climate change effects on fertility include:
☀️ Delayed puberty due to extreme weather
☀️ Decreased birth rates in high-pollution areas
☀️ Increased IVF dependence due to lower natural conception rates
☀️ Unpredictable reproductive cycles among women
Solutions: How to Protect Your Fertility from Pollution & Climate Change
Despite the crisis, there are proactive steps individuals can take:
✅ Use air purifiers to reduce indoor exposure to pollutants
✅ Eat organic foods to limit pesticide intake
✅ Avoid plastic packaging to reduce endocrine disruptor exposure
✅ Stay hydrated to flush toxins out of the body
✅ Maintain a healthy weight to regulate hormonal balance
✅ Consult fertility specialists for regular health check-ups
Conclusion
As pollution and climate change continue to worsen in 2025, their impact on fertility cannot be ignored. Rising temperatures, air pollution, and toxins are contributing to declining fertility rates globally. While scientific advancements may offer solutions, individuals must take steps to protect their reproductive health. The time to act is now!
#yellowivfgurgaon#fertility#ivf#health#Pollution and fertility rates 2025#Climate change and infertility#Air pollution affects fertility#Rising temperatures and sperm count#Environmental toxins and reproductive health#How pollution impacts pregnancy#Climate change and sperm quality#Microplastics and infertility#Fertility decline due to climate change#yellowivfcenter
0 notes
Text
Sattva Fertility Centre: The Best IVF Center in Bangalore Led by Dr. Rathnamani H. Arkachari
In the realm of fertility treatment, finding a center that combines advanced medical technology with compassionate care is paramount. In Bangalore, Sattva Fertility Centre, under the esteemed leadership of Dr. Rathnamani H. Arkachari, stands as a beacon of hope for countless couples navigating the challenges of infertility.
Dr. Rathnamani H. Arkachari: A Visionary in Fertility Treatment
Dr. Rathnamani H. Arkachari, the Founder and Director of Sattva Fertility Centre, brings over 18 years of dedicated experience in infertility treatment. She holds an MBBS from JJMMC Davangere and an MD in Obstetrics & Gynaecology from RIMS Ranchi. She further honed her expertise with a fellowship in Reproductive Medicine at CRAFT Kodungallur, Kerala.
Her commitment to excellence is evident through her active membership in prestigious organizations such as the Federation of Obstetric & Gynaecological Societies and the Indian Fertility Society. Throughout her illustrious career, Dr. Rathnamani has been at the forefront of addressing complex fertility issues, including recurrent miscarriages, genetic factors affecting fertility, poor ovarian reserve, and endometriosis.
Sattva Fertility Centre: Merging Technology with Compassion
Sattva Fertility Centre is more than just a medical facility; it's a sanctuary for couples seeking to realize their dreams of parenthood. The center offers a comprehensive suite of services tailored to address both male and female infertility challenges, including: IVF Center in Bangalore
1. In Vitro Fertilization (IVF)
A cornerstone procedure where eggs and sperm are combined outside the body, and the resulting embryos are implanted into the uterus.
2. Intracytoplasmic Sperm Injection (ICSI)
Designed for severe male infertility, this technique involves the direct injection of a single sperm into an egg to enhance fertilization.
3. Intrauterine Insemination (IUI)
This treatment involves the direct insertion of prepared sperm into the uterus, increasing the chances of fertilization.
4. Ovulation Induction
Using medications to stimulate the ovaries, this process encourages the release of eggs, facilitating natural conception.
5. Egg and Embryo Donation
For couples facing specific challenges, the center provides options for egg and embryo donation, offering alternative paths to parenthood.
6. Cryopreservation
The center offers services like egg freezing and embryo cryopreservation, allowing individuals and couples to preserve fertility for future family planning.
Beyond these treatments, Sattva Fertility Centre addresses various conditions that can impact fertility, such as:
Polycystic Ovary Syndrome (PCOS)
Endometriosis
Fallopian tube blockages
Ovarian cysts
Irregular periods
Ectopic pregnancies
Recurrent miscarriages
Patient-Centric Approach: Testimonials of Trust and Success
The true testament to Sattva Fertility Centre's excellence lies in the experiences of its patients. Numerous testimonials highlight the center’s commitment to personalized care and successful outcomes:
“Dr. Rathnamani in my opinion is one of the best fertility doctors out there. She is not only very qualified and proficient at her job but she is also polite, positive, and very practical in her approach.”
“We have had a great experience with Dr. Rathnamani. She is one of the best doctors, friendly in nature, within a month we received a positive result.”
“Thank you, madam, for giving us this good news. We have waited for so many years for this. No words to thank you. We are so happy, and you made us achieve this.”
These testimonials underscore the center’s dedication to providing medical solutions as well as emotional support throughout the fertility journey. IVF Clinic in Bangalore
Why Choose Sattva Fertility Centre?
Several factors distinguish Sattva Fertility Centre as a premier destination for fertility treatment:
1. Clinical Excellence
The center boasts high pregnancy success rates, backed by advanced technology and evidence-based practices.
2. Advanced Technology
Equipped with state-of-the-art facilities, Sattva ensures the best possible outcomes for its patients.
3. Innovative Treatments
The center offers a range of advanced treatments, including:
Laser-assisted hatching
Blastocyst culture and transfer
Preimplantation genetic testing
4. Affordable and Transparent Care
Sattva Fertility Centre believes in full transparency and maintains the highest ethical standards while providing affordable treatments.
5. Compassionate Support
Understanding the emotional challenges associated with infertility, the center ensures each patient’s comfort and safety throughout their treatment journey.
Conclusion
Embarking on the path to parenthood can be challenging, but with the right support and expertise, the journey becomes more manageable. Under the guidance of Dr. Rathnamani H. Arkachari, Sattva Fertility Centre is transforming lives and helping countless couples achieve their dream of parenthood.
For anyone seeking the best IVF center in Bangalore, Sattva Fertility Centre is the ultimate choice—where science meets compassion, and dreams turn into reality.
For more details, visit: Sattva Fertility
0 notes
Text
IVF Success Rates in Nepal: How to Improve Your Chances of a Successful Pregnancy

In recent years, Nepal has emerged as a preferred destination for In Vitro Fertilization (IVF) due to its affordable treatment options and growing number of advanced fertility centers. Many couples struggling with infertility turn to IVF treatment in Nepal, hoping to conceive successfully. However, the success of IVF is influenced by several factors, including age, health, lifestyle, and the expertise of the fertility clinic.
If you are planning to undergo IVF treatment in Nepal, understanding the success rates and knowing how to improve your chances of conception can make a significant difference. This article provides insights into IVF success rates in Nepal and effective ways to increase your likelihood of a successful pregnancy.
What Are the IVF Success Rates in Nepal?
IVF success rates vary depending on individual health conditions, clinic expertise, and treatment approaches. On average, the success rates for IVF in Nepal are:
Women under 35 years: 50% – 60% success rate
Women between 35-40 years: 35% – 45% success rate
Women over 40 years: 15% – 25% success rate
While these numbers provide a general estimate, individual cases may vary, and success depends on factors such as egg and sperm quality, the cause of infertility, and the clinic’s technology and expertise.
Key Factors Affecting IVF Success Rates in Nepal
Several medical and lifestyle factors influence IVF success rates in Nepal. Understanding and optimizing these factors can help improve your chances of a successful pregnancy.
1. Age and Egg Quality
Age is the most significant factor in IVF success. Younger women (below 35) generally have higher success rates because they produce healthier eggs. As women age, egg quality and ovarian reserve decline, making conception more challenging.
How to improve:
If you are over 35, discuss egg freezing or donor eggs with your doctor.
Undergo ovarian reserve testing to assess your fertility status.
2. Choosing the Right IVF Clinic
The success of your IVF treatment depends on the clinic’s technology, expertise, and laboratory standards. Some clinics in Nepal offer advanced techniques such as ICSI (Intracytoplasmic Sperm Injection), blastocyst culture, and embryo freezing, which can improve success rates.
How to improve:
Research and choose a well-established IVF center with high success rates.
Look for clinics with experienced embryologists and fertility specialists.
3. Sperm Quality and Male Factor Infertility
Male infertility issues, including low sperm count, poor motility, or DNA fragmentation, can significantly affect IVF success. Many clinics in Nepal offer advanced sperm selection techniques to improve outcomes.
How to improve:
Maintain a healthy diet and avoid alcohol and smoking, which can damage sperm quality.
Consider ICSI treatment, where the best sperm is selected for fertilization.
4. Lifestyle and Diet
A healthy lifestyle plays a crucial role in boosting fertility and improving the success of IVF. A balanced diet, exercise, and stress management can enhance overall reproductive health.
How to improve:
Eat a nutrient-rich diet including folic acid, protein, and antioxidants.
Avoid processed foods, caffeine, and excess sugar.
Practice yoga, meditation, or light exercise to reduce stress.
5. Hormonal Balance and Uterine Health
The uterine lining must be healthy enough to support embryo implantation. Hormonal imbalances, PCOS (Polycystic Ovary Syndrome), or endometriosis can lower IVF success rates.
How to improve:
Consult your doctor about hormonal treatments or medications to prepare the uterus for implantation.
Ensure that thyroid and other hormonal levels are balanced before IVF.
6. Multiple IVF Cycles and Embryo Transfer Strategy
Not all IVF attempts succeed on the first cycle. Many couples require multiple IVF cycles before achieving pregnancy. The embryo transfer technique also plays a role in success rates.
How to improve:
Opt for blastocyst transfer (Day 5 embryo transfer), which has higher success rates.
Discuss embryo freezing with your doctor if the first cycle is unsuccessful.
Steps to Improve Your IVF Success in Nepal
If you’re preparing for IVF treatment, follow these steps to maximize your chances of success:
✔ Start early: If you’re planning for IVF, consult a fertility specialist as soon as possible. ✔ Undergo fertility testing: Both partners should complete a thorough fertility assessment before starting treatment. ✔ Follow a personalized treatment plan: Every couple’s fertility journey is different. Work closely with your doctor to customize your IVF protocol. ✔ Maintain a positive mindset: Stress and anxiety can negatively impact IVF outcomes. Stay mentally and emotionally prepared for the journey. ✔ Consider fertility-enhancing supplements: Consult your doctor about vitamins like CoQ10, folic acid, and omega-3 fatty acids, which may improve egg and sperm quality.
Final Thoughts: Achieving IVF Success in Nepal
IVF success rates in Nepal are steadily improving, thanks to advancements in fertility treatments and the availability of state-of-the-art reproductive technologies. While success depends on multiple factors, choosing the right IVF clinic, maintaining a healthy lifestyle, and following expert medical advice can significantly enhance your chances of conception.
If you’re considering IVF treatment in Nepal, take time to research, consult top fertility specialists, and prepare your body and mind for the journey ahead. With the right approach and medical support, you can maximize your chances of fulfilling your dream of parenthood.
Are you ready to start your IVF journey in Nepal? Take the first step today and explore the best fertility options available.
0 notes
Text
Understanding the Causes of Low AMH Levels

If you’ve been trying to conceive and have come across the term “AMH” in your fertility evaluations, you’re not alone. AMH, or Anti-Müllerian Hormone, is a crucial marker used to assess a woman’s ovarian reserve—essentially, how many eggs she has left. Low AMH levels can be concerning, especially for women trying to conceive, but understanding the causes can help you make informed decisions about your fertility journey.
What is AMH?
Anti-Müllerian Hormone (AMH) is produced by small follicles in the ovaries. The amount of AMH in your blood gives doctors an idea of your egg reserve. While AMH does not predict the quality of your eggs, it does provide insight into quantity. Low AMH levels suggest a reduced ovarian reserve, which can affect fertility potential.
What Causes Low AMH Levels?
1. Age
One of the most common reasons for low AMH is age. As women get older, the number of eggs naturally declines. This decline usually begins in the late 20s and becomes more significant after age 35.
2. Genetic Factors
Some women may be genetically predisposed to having a lower ovarian reserve. Conditions like Turner syndrome or a family history of early menopause can influence AMH levels.
3. Autoimmune Disorders
Certain autoimmune diseases can attack the ovaries, damaging the follicles and reducing AMH levels. These disorders may go undiagnosed until fertility issues arise.
4. Lifestyle Factors
Smoking, excessive alcohol intake, poor diet, and high levels of stress can negatively impact ovarian health and reduce AMH levels.
5. Medical Treatments
Chemotherapy, radiation therapy, or ovarian surgeries can damage the ovaries, leading to a significant drop in AMH levels.
6. Polycystic Ovary Syndrome (PCOS) – Exception to the Rule
Interestingly, women with PCOS often have high AMH levels due to an increased number of small follicles. However, in some cases, PCOS can still lead to poor egg quality and irregular ovulation.
7. Endometriosis
Women with endometriosis may experience reduced ovarian reserve due to inflammation or surgical treatment for endometriotic cysts, which can lead to lower AMH levels.
What Should You Do If You Have Low AMH?
Low AMH levels do not mean pregnancy is impossible—they simply indicate that time might be a critical factor. There are many fertility treatment options available, such as:
IVF (In-Vitro Fertilization)
Ovarian stimulation protocols tailored for low AMH
Fertility preservation through egg freezing
Final Thoughts by Dr. Swapnil Langde
Every woman’s fertility journey is unique. At our fertility clinic, we take a personalized approach to help you understand your AMH levels and explore all possible options. Early assessment and intervention can make a significant difference.
If you’ve been diagnosed with low AMH or are worried about your fertility, book a consultation today. Together, we’ll take the next step toward your dream of parenthood.
0 notes
Text
ICSI Treatment for Couples Facing Fertility Challenges
ICSI treatment (Intracytoplasmic Sperm Injection) is a specialised form of IVF that offers hope to couples facing fertility challenges, particularly when sperm quality is a concern. It is an advanced form of IVF where a single sperm is injected directly into an egg using precision micromanipulation. This method is particularly effective for couples who face male infertility issues, such as low sperm count or poor sperm quality, that may make conventional IVF less likely to succeed.
ICSI treatment offers a precise and effective approach to overcoming male fertility issues and has become a go-to treatment for many couples seeking to conceive.

Essential Steps to Take Before Starting ICSI
For those considering ICSI treatment, several necessary steps should be followed to optimise the chances of success-
Health Check-Up- Both partners should undergo a full health evaluation, including screenings for STIs, diabetes, and thyroid function.
Semen Analysis- A thorough semen analysis is crucial to assess sperm quality and ensure sufficient healthy sperm for the procedure.
Ultrasound and AMH Testing- For women, a pelvic ultrasound and AMH (Anti-Müllerian Hormone) test help assess egg quality and ovarian reserve.
What Makes Us Stand Apart
Experienced and Skilled Team- A dedicated team of fertility experts with years of experience in ICSI treatment.
Advanced Technology- Access to the latest equipment, ensuring precision and optimal results.
Personalised Treatment- Tailored fertility plans designed to meet individual needs and optimise chances of success.
If you’re considering ICSI treatment in Melbourne, visit the website to discover how the expert team can help you take the next step toward building your family.
0 notes
Text
Perimenopause And IVF With Donor Egg – IVF After Menopause Success Rate

Before embarking on the main topic of perimenopause and IVF with donor egg, we have to understand perimenopause, and how IVF is possible for infertility couples or families. Fertility may be impacted by the hormonal changes that frequently accompany the perimenopause, the transitional period preceding menopause. Perimenopausal women may have problems like erratic ovulation, poorer egg quality, and decreased ovarian reserve. For women in this stage who want to become pregnant, IVF with donor eggs offers a viable option.
IVF using donor eggs involves fertilizing healthy eggs from a younger donor with sperm from the donor or spouse and transferring the resulting embryos into the woman’s uterus. Even for women in their late 40s or early 50s, the odds of a healthy pregnancy greatly increase because donor eggs are usually of excellent quality. Hormonal therapy prepares the uterus for implantation.
This method, which is generally regarded as safe and successful, gives women whose fertility has been affected by perimenopause hope. It is a feasible alternative for becoming a parent later in life because it also helps avoid the age-related drop in egg quality. To assess their health and go over individualized treatment regimens, women considering this route should speak with fertility specialists.
What Is The Success Rate Of IVF After Perimenopuae For Pregnancy?

Perimenopuae Pregnancy in India
The utilization of donor eggs, the woman’s general health, and the standard of medical treatment are some of the variables that affect the success rate of IVF following perimenopause. Perimenopausal women frequently have low ovarian reserves and low-quality eggs, which reduces the success of both natural conception and IVF using their eggs. The success rate rises dramatically when donor eggs are utilized, though, and is frequently on par with younger women having IVF.
Depending on the clinic and other specific conditions, the success rate for getting pregnant with donor eggs might vary from 50% to 70% per cycle. Utilizing superior donor eggs from younger women aids in overcoming the reduction in fertility that comes with aging. Furthermore, by guaranteeing the selection of viable embryos, medical technology developments like preimplantation genetic testing (PGT) might increase the chance of a healthy pregnancy.
Before beginning the treatment, women must have comprehensive medical tests to determine uterine health and handle any underlying issues, even though the prospects of success with donor eggs are good. Women can increase their chances of success and make well-informed decisions by speaking with a qualified fertility professional.
What Are The Causes Of Perimenopause Before Fertility Treatment Or Pregnancy?

Causes Of Perimenopause
Numerous causes might cause perimenopause, the period of transition before menopause, to occur earlier than anticipated, which can affect fertility and hopes for pregnancy. Among the frequent reasons are:
Age and Natural Decline
As people age naturally, their hormone levels and ovarian reserve gradually decrease, which frequently results in perimenopause. A lady usually starts this in her late 30s or early 40s.
The disorder known as premature ovarian insufficiency (POI) occurs when the ovaries cease to function normally before the age of forty. It may be brought on by autoimmune diseases, hereditary factors, or other unidentified causes.
Medical Treatments
Treatments that harm ovarian tissue and hasten the beginning of perimenopause include radiation therapy, chemotherapy, and ovarian surgery.
Lifestyle Factors
Poor nutrition, heavy alcohol use, and smoking can all hasten the deterioration of ovarian function.
Genetics
Women may be at risk for early perimenopause if there is a family history of early menopause or reproductive health problems.
Chronic Health Conditions
Illnesses including diabetes, autoimmune diseases, and thyroid issues can throw off the hormonal balance and cause early perimenopause.
Environmental Factors
Long-term exposure to substances that disrupt hormones and pollutants may have an impact on ovarian health.
Women can schedule reproductive procedures like IVF or egg freezing before their ovarian reserve drastically declines by identifying these factors early. To maximize reproductive possibilities and achieve optimal pregnancy outcomes, early intervention and contact with fertility specialists are essential.
What Are The Process Of IVF After Perimenopause For Successful Pregnancy?
IVF Procedure for a Successful Pregnancy After Perimenopause
To overcome the normal reduction in fertility and obtain a successful pregnancy, IVF (In Vitro Fertilization) following perimenopause requires specialist techniques. The detailed procedure is as follows:
Initial Assessment
To ascertain a patient’s suitability for IVF, a thorough assessment of their hormone levels, ovarian reserve, uterine health, and general medical history is carried out.
Donor Egg Selection (if necessary)
Donor eggs are usually used since perimenopause frequently results in a decreased ovarian reserve. These are chosen per the recipient’s genetic and physical preferences.
Endometrial Preparation
To guarantee a receptive endometrial lining, hormonal therapies like estrogen and progesterone are used to prepare the uterus for the embryo’s arrival.
Fertilization
Using cutting-edge methods like ICSI (Intracytoplasmic Sperm Injection), the donor eggs are fertilized in a lab with either the partner’s or the donor’s sperm.
Embryo Transfer
One or more of the developing embryos are placed inside the ready-made uterus. Accurate placement is guaranteed via ultrasound guidance.
Luteal Phase Support
Hormonal drugs are administered to promote implantation during the early stages of pregnancy following transfer.
Pregnancy Testing
To confirm pregnancy, a blood test is conducted two weeks later.
Monitoring and Care
Regular monitoring and prenatal care are crucial if pregnancy is obtained because pregnancies after perimenopause may be more problematic.
As long as their general health and uterine condition are favorable, many women can become pregnant successfully after perimenopause with the help of reproductive technology improvements and customized treatment plans.
What Happens To Eggs During Perimenopause With IVF Treatment?
A woman’s ovarian reserve, or the quantity and quality of eggs in her ovaries, drastically decreases throughout perimenopause. The efficiency of IVF procedures utilizing the woman’s eggs is impacted by this natural process. Women’s eggs frequently include chromosomal abnormalities as they get closer to menopause, which can lower their reproductive potential and raise their chance of miscarriage.
Several measures are made to overcome these issues in perimenopausal IVF treatment:
Ovarian Stimulation
To encourage the ovaries to generate more eggs, higher dosages of fertility drugs may be used. However, because of the decreased ovarian reserve, the response is usually smaller than in younger women.
Retrieval of Eggs
All viable eggs are recovered, however, the quantity and caliber might not be enough for effective fertilization and the growth of the embryo. Alternative Option: Donor eggs could be used if the retrieved eggs are not viable. Donor eggs are more likely to produce healthy embryos and fruitful pregnancies since they come from younger, healthier women.
Using the woman’s eggs during perimenopause makes IVF more difficult, however, donor egg IVF provides a very successful way to become a parent. To provide ideal conditions for embryo implantation, hormonal therapies are also utilized to prepare the uterus.
What Is The Best Treatment For Perimenopause? – Perimenopause And IVF With Donor Egg
The ideal course of treatment for perimenopause differs based on each person’s needs and symptoms. Managing symptoms like mood swings, hot flashes, irregular periods, sleep difficulties, and decreased fertility is the main objective of treatment. Typical therapies consist of:
The most successful treatment for severe perimenopausal symptoms is hormone therapy (HT). To control hormones and relieve symptoms including vaginal dryness, hot flashes, and night sweats, estrogen or a combination of estrogen and progesterone is administered.
Lifestyle Modifications
Leading a healthy lifestyle can aid in the efficient management of symptoms. For general well-being, a balanced diet high in calcium and vitamin D, regular exercise, stress-reduction strategies, and enough sleep are necessary.
Non-Hormonal Drugs
Antidepressants and hot flash medications (such as gabapentin) are examples of non-hormonal drugs that may be useful for women who are unable or unable to undergo hormone therapy.
Vaginal Estrogen
Creams, rings, or tablets containing vaginal estrogen can help relieve localized symptoms such as vaginal dryness or pain during sexual activity.
Herbal remedies and supplements
Some women utilize supplements such as evening primrose oil, soy isoflavones, or black cohosh, although their efficacy varies and they should be taken under a doctor’s supervision.
Fertility Treatment
IVF using a woman’s own or donor eggs may be an option for women attempting to conceive during perimenopause.
Women going through perimenopause should speak with a healthcare professional to choose the best course of action for them based on their lifestyle and current health.
How Can I Improve My Egg Quality In Perimenopause? – Perimenopause And IVF With Donor Egg

Improve Egg Quality In Perimenopause
Women who want to increase their chances of getting pregnant must improve the quality of their eggs during perimenopause. Although the amount and quality of eggs gradually decline with age, some lifestyle changes and medical treatments can promote improved reproductive outcomes:
Eat Well
A diet high in nutrients can enhance the quality of eggs. Pay attention to foods like fruits, vegetables, nuts, and whole grains that are high in antioxidants. Incorporate good fats that promote hormonal health, such as omega-3s from fish or flaxseeds.
Keep Your Weight in Check
Being underweight or overweight might throw off your hormone balance, which is important for the development of your eggs. To maximize fertility, strive for a healthy BMI.
Make Supplements to Increase Fertility
Vitamin D, folic acid, DHEA, and coenzyme Q10 (CoQ10) are frequently suggested for enhancing egg quality. Egg viability depends on mitochondrial function and cell health, which are supported by these nutrients.
Avoid Toxins
Smoking, excessive alcohol consumption, processed meals, and environmental pollutants can all have a detrimental effect on the health of eggs.
Handle Stress
Prolonged stress can throw off the hormone balance, which affects ovulation and the quality of eggs. Engage in stress-relieving practices such as mindfulness, yoga, or meditation.
Get Enough Sleep
Restful sleep promotes general health and controls hormones, particularly those linked to fertility. Try to get between 7 and 9 hours each night.
Examine Acupuncture
It is thought to enhance blood flow to the uterus and ovaries, which may promote the health of the egg.
Speak with a Fertility Specialist
If natural approaches prove inadequate, consult a fertility specialist. IVF utilizing your own or donor eggs, hormone therapy, and ovarian rejuvenation therapy are among possible treatments.
Making these adjustments early in perimenopause can increase your chances of a healthy pregnancy because improving egg quality takes time and consistency.
Who Is The Real Mother Of A Donor Egg Baby? – Best IVF Clinic In India

Real Mother Of A Donor Egg Baby in India
Motherhood in donor egg scenarios can be viewed from several perspectives, including legal, gestational, and genetic. In most cases, the mother bearing the child is recognized as the biological mother, even when the genesis of a donor egg child is unique. IVF Clinic India plays a crucial role in assisting intended parents in this journey. World Fertility Services provides expert care and advanced treatments to support hopeful parents in achieving their dream of parenthood.
Gestational Motherhood
The woman who carries the child during pregnancy is often considered the true mother because she raises the infant in her womb, provides the environment for its growth, and delivers birth. This physical and emotional connection forms a deep bond.
Legal Motherhood
According to the law, the mother is usually the one named on the child’s birth certificate and the one who decides to use the donor egg for reproductive therapy. The intended parent or parents who agree to the fertilization procedure are typically legally acknowledged as the parents, while laws on legal motherhood differ from nation to nation.
Emotional Motherhood
In both practical and emotional aspects, the intended mother, who is responsible for the child’s upbringing and care after birth, assumes the role of the child’s mother. When defining motherhood, this attachment frequently takes precedence over biological ties.
Genetic Contribution
Although the genetic material is provided by the egg donor, donors are typically not considered the “real” mothers. Depending on the laws in the nation where the donation takes place, they are frequently anonymous and have neither parental nor legal rights to the kid.
In conclusion, it is generally accepted that the woman who carries gives birth to, and raises a donor egg kid is the child’s true mother. The emotional, legal, and physical commitment she makes during the parenthood process is reflected in her viewpoint.
Which Country Is Best For Donor Egg IVF? – Perimenopause And IVF With Donor Egg

Perimenopause And IVF With Donor Egg
The best nation for donor egg IVF is determined by some criteria, such as accessibility, success rates, legal requirements, and cost. Although every nation has its advantages, the following locations are frequently regarded as the best options for donor egg IVF:
India – IVF After Menopause Success Rate
India is well known for providing high-quality fertility treatments at reasonable prices. At far lower prices than Western nations, it provides skilled fertility specialists and cutting-edge medical technologies. IVF using donor eggs is permitted by the nation’s legal system, and egg donors undergo extensive screening for genetic and medical disorders.
Spain – IVF With Donor Eggs Over 40
Because of its stringent rules protecting donor anonymity, great success rates, and first-rate medical facilities, Spain is one of the most favored countries for donor egg IVF. Spain is a popular destination for many foreign patients because of its renowned fertility clinics’ professionalism and commitment to patient care.
Ukraine – Can You Do IVF During Perimenopause
Ukraine is known for its highly skilled fertility specialists, affordable therapies, and permissive reproductive legislation. Modern technology is available in clinics, and the nation permits egg donation with little legal constraints.
United States – IVF Pros & Cons
IVF using donor eggs has among the best success rates in the United States, but it is also one of the priciest options. One significant benefit is the freedom to select donors, including anonymous ones, and cutting-edge facilities offer patients individualized treatment regimens.
Czech Republic – IVF Using Donor Egg
The country is renowned for its well-run egg donation programs and reasonably priced fertility treatments. Clinics uphold the highest moral and medical standards, and donors remain anonymous.
Things to Take Into Account – Perimenopause And IVF With Donor Egg
Cost
In comparison to the United States or Western Europe, nations like India and Ukraine provide more reasonably priced possibilities.
Success Rates
The United States and Spain, two nations with highly developed technology, frequently report greater success rates.
Legal Framework
Verify that the laws of the nation respect your wishes, particularly those about donor anonymity or information access.
Travel Accessibility
Take into account how simple it is to travel and whether patients from other countries can learn the language.
Final Wording – Perimenopause And IVF With Donor Egg
The conclusion is a significant role of the whole article in which we have elaborated all essential key elements for especially infertility couples or families who seeking fertility treatment with perimenopause disease. Read more interesting articles that we have published on the official website, for instance, www.worldfertilityservices.com where you can find your preference topics that will be related to your fertility treatment.
0 notes
Text
When to seek for IVF treatment

You should consider seeking IVF (In Vitro Fertilization) treatment if you have been trying to conceive for a prolonged period without success or if you have been diagnosed with specific fertility issues. Below are key indicators for when to seek IVF treatment:
1. Duration of Trying to Conceive (TTC)
Under 35 years old: If you have been trying for 12 months or more without success.
35–40 years old: And If you have been trying for near about 6 months without success.
Over 40 years old: You have to seek immediate evaluation and consultation with a fertility specialist, if you are over 40 years old.
2. Medical Conditions That May Require IVF
Blocked or damaged fallopian tubes: If anyone have blockage in fallopian tubes, it may prevent sperm from meeting the egg.
Endometriosis: If anyone is suffered from endometriosis, it could affect egg quality, implantation, and tubal function.
Poly Cystic Ovary Syndrome (PCOS): Irregular ovulation may make natural conception difficult.
Low ovarian reserve: Declining egg quantity and quality, especially with age.
Uterine or cervical issues: Abnormalities in the uterus or cervix can hinder implantation.
3. Male Factor Infertility
Low sperm count, poor motility, or abnormal sperm shape (morphology).
Previous history of testicular injury, infection, or surgery affecting sperm production.
4. Unexplained Infertility
When no clear cause is found after fertility tests but conception has not occurred, this situation is called unexplained infertility.
5. Recurrent Miscarriages
If you have experienced multiple pregnancy losses, IVF with genetic testing (PGT) can help identify healthy embryos.
6. Failed Fertility Treatments
If previous treatments like ovulation induction, intrauterine insemination (IUI), or medication (Clomid, Letrozole) have not worked then IVF treatment will work.
7. Genetic Disorders
If you or your partner have a known genetic condition and want to avoid passing it on, IVF with Preimplantation Genetic Testing (PGT) can help select healthy embryos.
8. Fertility Preservation Needs
Cancer patients: If undergoing chemotherapy/radiation, freezing eggs or embryos before treatment can preserve fertility.
Career or personal reasons: Women who wish to delay pregnancy can opt for egg freezing.
If any of these situations apply to you, it's a good idea to consult a fertility specialist to discuss your options IVF Treatment in Gurgaon. Would you like guidance on how to prepare for an IVF consultation?
0 notes
Text
There are many common reasons why IUIs fail.
For infertile couples, intrauterine insemination (IUI) is frequently regarded as the first line of treatment. Although it has the potential to be a very successful strategy, some things may make it less successful. Renowned fertility specialist and gynecologist Dr. Archana Salve discusses the most typical causes of IUI failure and how to deal with them.

1. Women’s Advanced Age
Age plays a crucial role in fertility. As women age, the quality and quantity of eggs tend to decline. For women above the age of 35, the chances of IUI success can significantly decrease due to diminished ovarian reserve and a higher risk of chromosomal abnormalities in eggs. Timely consultation and advanced fertility treatments may be required in such cases.
2. Poor Sperm Quality
IUI involves placing washed and concentrated sperm directly into the uterus. However, if the sperm quality is poor—including low sperm count, poor motility, or abnormal morphology—it can reduce the likelihood of successful fertilization. A detailed semen analysis and, if necessary, advanced techniques like IVF may be recommended.
3. Low Ovarian Reserve
Low ovarian reserve, characterized by a reduced number of viable eggs, is another common cause of IUI failure. This condition can be diagnosed using tests such as Anti-Müllerian Hormone (AMH) levels and antral follicle count (AFC). For women with low ovarian reserve, combining fertility medications with IUI or opting for IVF might increase the chances of success.
4. Timing of Conception
The timing of IUI is critical for success. If the procedure is not aligned with the ovulation window, the chances of sperm meeting the egg are minimal. Accurate monitoring of ovulation through ultrasound and hormonal tests is essential to ensure proper timing.
5. Unexplained Infertility
Sometimes, despite all tests being normal, couples may still face infertility issues, which is termed unexplained infertility. In such cases, IUI may not always yield successful results. Advanced treatments like IVF, which offer better control over the fertilization process, might be more suitable.
How to Improve Your Chances of IUI Success
1.Early Consultation:
Seek timely advice from a fertility specialist to address any underlying issues.
2.Lifestyle Changes:
Maintaining a healthy weight, avoiding smoking, and reducing stress can significantly improve fertility outcomes.
3.Advanced Techniques:
Consider combining IUI with ovulation induction or switching to IVF if IUI has failed multiple times.
Final Thoughts
IUI can be a stepping stone to parenthood for many couples, but it is important to understand that its success depends on several factors. Consulting an experienced fertility specialist like Dr. Archana Salve can help identify and address these challenges, paving the way for a successful outcome.
If you have questions about IUI or other fertility treatments, don’t hesitate to book a consultation with Dr. Archana Salve at Fertiprotect & Superspeciality Clinic in Kalyani Nagar & Viman Nagar
#Gynaecologist in Kalyani nagar#Best gynecologist in Kalyani nagar#Infertility Treatment in Kalyani nagar#IVF Treatment in Kalyani nagar#IVF Specialist in Kalyani nagar#IUI treatment in Kalyani nagar#Test Tube Baby treatment in Kalyani nagar#Fertility Treatment in Kalyani nagar#best gynecologist-obstetrician in Kalyani Nagar#Gynaecologist in Viman nagar#Best gynecologist in Viman nagar#Infertility Treatment in Viman nagar#IVF Treatment in Viman nagar#IVF Specialist in Viman nagar#IUI treatment in Viman nagar#Test Tube Baby treatment in Viman nagar#Fertility Treatment in Viman nagar#best gynecologist-obstetrician in Viman Nagar
0 notes